Advanced Motion Correction Strategies for Large-Scale Neuroimaging: A Comprehensive Guide for Researchers
Motion artifacts present a significant challenge to the reliability and reproducibility of large-scale neuroimaging studies, particularly in pediatric and clinical populations.
Advanced Motion Correction Strategies for Large-Scale Neuroimaging: A Comprehensive Guide for Researchers
Abstract
Motion artifacts present a significant challenge to the reliability and reproducibility of large-scale neuroimaging studies, particularly in pediatric and clinical populations. This article provides a comprehensive overview of modern motion correction strategies, from foundational concepts to advanced applications. We explore the critical trade-offs between prospective and retrospective methods, hardware-based and data-driven software solutions, and their implementation in multi-site research. The content details robust analytical frameworks for handling imperfect data, offers optimization strategies for study design, and presents rigorous validation protocols for comparing traditional and AI-based techniques. Aimed at researchers and drug development professionals, this guide synthesizes current evidence and practical recommendations to enhance data quality, accelerate discovery, and improve the clinical utility of neuroimaging biomarkers.
Understanding the Motion Problem: Scale, Impact, and Fundamental Challenges in Neuroimaging
Head motion is a significant confounding variable in magnetic resonance imaging (MRI) that can compromise data quality and lead to erroneous research findings and clinical interpretations. Between 10-15% of all MRI scans need to be repeated due to excessive motion, with even higher rates in young children and individuals with disabilities [1]. Motion introduces various artifacts including blurring, ghosting, and ringing in images, which subsequently affect derived metrics such as cortical thickness, regional volumes, and functional connectivity estimates [2].
This technical guide addresses the characterization of motion across different populations and provides evidence-based troubleshooting methodologies for researchers conducting large-scale neuroimaging studies.
Quantitative Characterization of Motion Across Populations
Motion Prevalence by Age and Clinical Status
Table 1: Motion Prevalence and Characteristics Across Demographic and Clinical Groups
| Population Group | Relative Motion Level | Key Characteristics | Data Source |
|---|---|---|---|
| Children (5-10 years) | Highest | Exhibits the most movement in scanner; nonlinear cortical thickness associations disappear with stringent QC | [2] |
| Adolescents | Moderate | Dynamic brain development; motion shows test-retest reliability | [2] |
| Adults | Lower | Generally better motion control; intermediate rates of incidental findings | [3] |
| Older Adults (>40 years) | Increased | Higher motion returns; highest rates of incidental findings (54.9%) | [3] [2] |
| Autism Spectrum Disorder | Significantly elevated | Increased motion compared to controls; affects cortical thickness measurements | [2] |
| ADHD | Significantly elevated | Motion-related symptoms manifest as increased head movement | [2] |
| Psychotic Disorders | Significantly elevated | Reduced cortical thickness effect sizes attenuate when motion accounted for | [2] |
Quantitative Impact of Motion on Data Quality
Table 2: Motion Impact on Neuroimaging Metrics and Outcomes
| Metric | Impact of Motion | Clinical/Research Consequence | |
|---|---|---|---|
| Cortical Thickness | Overestimation of thinning | Spurious neurodevelopmental trajectories | [2] |
| Grey Matter Volumes | Significant negative association | Misinterpretation of structural differences | [2] |
| White Matter Metrics | Weakened age correlations | Altered developmental trajectories | [2] |
| Functional Connectivity | Increased spurious correlations | Invalid network connectivity patterns | [2] |
| Incidental Finding Rates | No significant association | Clinical findings not obscured by motion | [3] |
| Prediction Accuracy | Decreased reliability | Reduced brain-age prediction accuracy | [4] |
Frequently Asked Questions: Motion Characterization
Q1: How does motion prevalence differ between children and adults in neuroimaging studies?
Motion follows a U-shaped curve across the lifespan. Children aged 5-10 years exhibit the most movement, with decreasing motion through adolescence and adulthood, followed by increased motion again in older adults (>40 years) [2]. One large-scale study found that while 9.6% of children have incidental findings on MRI, this increases to 54.9% in adults, though motion itself doesn't significantly affect the detection of these clinical findings [3].
Q2: Which clinical populations show elevated motion levels and how does this affect data interpretation?
Patients with autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), and psychotic disorders (bipolar disorder and schizophrenia) consistently exhibit significantly increased motion compared to healthy controls [2]. This motion difference can confound clinical interpretations - for example, early studies of ASD that did not adequately control for motion found no cortical thickness differences, while subsequent studies with stringent motion correction revealed significantly thicker cortex in ASD participants, aligning with histological evidence [2].
Q3: What is the quantitative impact of motion on cortical thickness measurements?
Motion produces a systematic bias toward thinner cortical measurements. Research has demonstrated that without adequate motion correction, reported nonlinear cortical thickness associations with age disappear when more stringent quality control is applied [2]. The direction of this bias is particularly problematic for case-control studies of clinical populations, as those groups that move more (such as ASD and ADHD) will appear to have artificially thinner cortex, potentially masking true neurobiological differences.
Q4: How does motion affect functional connectivity measures?
Motion increases the proportion of spurious correlations throughout the brain in functional MRI data [2]. The effects are complex and variable depending on the type of motion, but generally inflate short-distance correlations while reducing long-distance correlations. This artifact is particularly problematic because it can create systematic differences between groups that differ in motion levels, such as clinical populations versus healthy controls.
Q5: Can motion artifacts be adequately corrected through post-processing alone?
While numerous post-processing approaches exist, evidence suggests that prospective correction (during acquisition) provides superior results. As noted by researchers, "sedation is not allowed for research studies involving MRI scans" [1], necessitating alternative motion compensation strategies. Modern approaches like the MPnRAGE technique can effectively minimize artifacts and transform previously unusable scans into clinically useful images [1].
Experimental Protocols for Motion Characterization
Protocol for Quantifying Motion in Large-Scale Studies
Purpose: To standardize motion quantification across multiple sites and scanner platforms for large-scale neuroimaging studies.
Equipment and Software:
- MRI scanner with compatible motion tracking (e.g., volumetric navigators, optical tracking)
- Automated image processing pipeline (e.g., Freesurfer for Euler number calculation)
- Motion parameter estimation tools (FSL mcflirt, AFNI 3dvolreg, or SPM realign)
Procedure:
- Acquire structural and functional images using standardized protocols
- Extract motion parameters (6 rigid-body parameters: x, y, z translations and rotations)
- Calculate quantitative metrics:
- Euler number from Freesurfer processing [3]
- Frame-wise displacement from functional time series
- Root mean square of motion parameters
- Apply quality control thresholds based on study requirements
- Correlate motion metrics with demographic and clinical variables
Validation: Compare quantitative motion metrics with radiologist-reported motion ratings to ensure clinical relevance [3].
Protocol for Motion Characterization Across Development
Purpose: To characterize typical motion patterns across developmental stages from childhood through older adulthood.
Participant Groups:
- Children (5-10 years), Adolescents (11-19 years), Young Adults (20-39 years), Middle-aged Adults (40-64 years), Older Adults (65+ years)
Procedure:
- Acquire T1-weighted structural images and resting-state fMRI
- Compute motion estimates for all participants
- Group participants by age decades and clinical status
- Compare motion parameters across groups using ANOVA with post-hoc tests
- Assess test-retest reliability in longitudinal subsets
Analysis: Model motion as a function of age using both linear and nonlinear (quadratic) models to capture the U-shaped relationship [2].
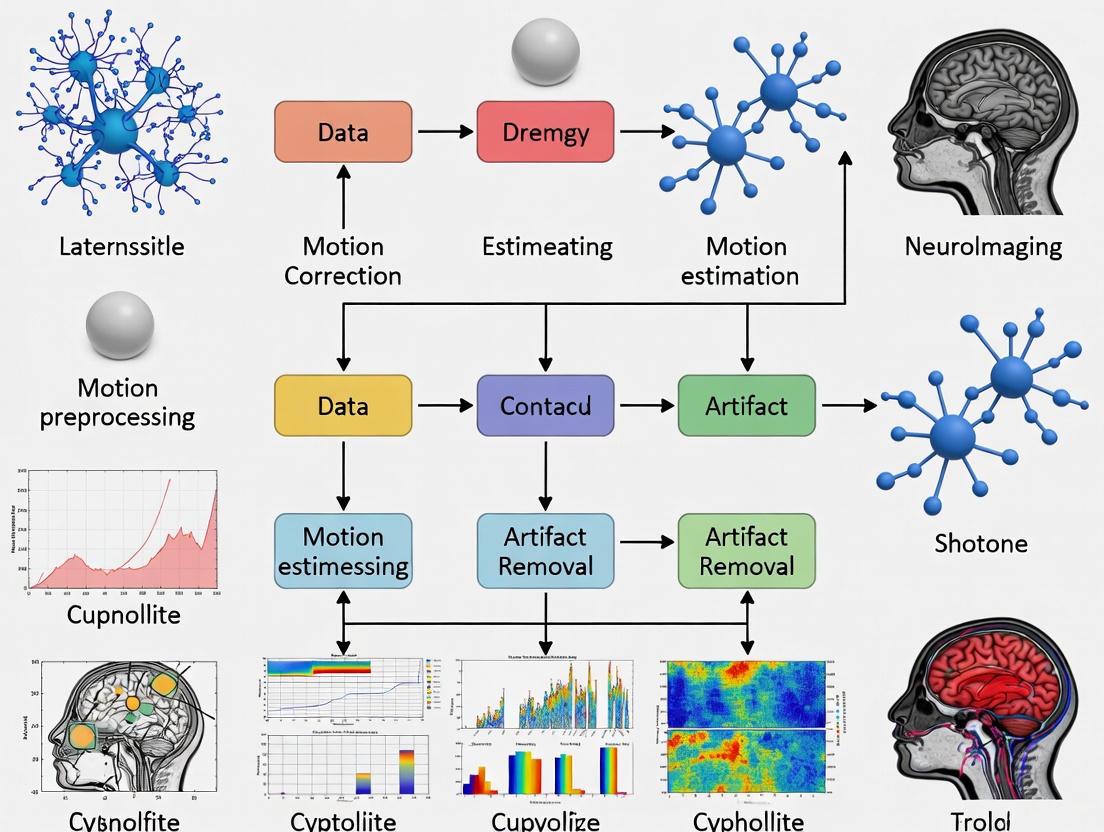
Motion Characterization Workflow
Diagram 1: Comprehensive motion characterization workflow for large-scale studies
Research Reagent Solutions
Table 3: Essential Tools and Methods for Motion Characterization and Correction
| Tool/Method | Type | Primary Function | Application Context |
|---|---|---|---|
| Euler Number | Quantitative Metric | Automated motion quantification from structural images | Large-scale studies requiring automated QC [3] |
| FSL mcflirt | Software Tool | Motion parameter estimation and correction | Functional MRI preprocessing [5] |
| Volumetric Navigators | Prospective Correction | Real-time motion tracking and correction | High-resolution angiography and structural imaging [6] |
| MPnRAGE | Pulse Sequence | Motion-robust structural imaging | Studies with populations prone to movement [1] |
| HERON Pipeline | AI-Driven Framework | Real-time motion assessment and re-acquisition | Fetal MRI and challenging populations [7] |
| 3DMC Algorithms | Retrospective Correction | Post-acquisition image realignment | Standard functional and structural processing [8] |
| Motion Covariates | Statistical Control | GLM incorporation of motion parameters | Removing residual motion artifacts in fMRI [5] |
Motion Correction Decision Pathway
Diagram 2: Decision pathway for motion management strategies based on population characteristics
Quantifying the pervasiveness of motion across age and clinical populations is essential for valid neuroimaging research. The evidence demonstrates clear demographic and clinical patterns in motion characteristics, with children, older adults, and individuals with neuropsychiatric conditions exhibiting elevated motion that systematically biases research findings. Implementation of the characterization protocols, troubleshooting guides, and decision pathways outlined in this technical support document will enhance the reliability and validity of large-scale neuroimaging studies.
The Direct Impact of Motion on Data Quality and Statistical Power
Troubleshooting Guides
Guide 1: Diagnosing and Correcting Motion Artifacts in Structural and Functional MRI
Problem: A structural MRI scan appears to have no major motion artifacts upon visual inspection, but subsequent morphometric analysis (e.g., cortical thickness or gray matter volume) shows significant bias and high variance, potentially confounding group-level statistics.
Explanation: Even subtle, "unnoticeable" motion can introduce systematic biases in morphometric analyses. When motion patterns differ between patient and control groups, this creates a significant confound, leading to erroneous conclusions about group differences [9]. Motion induces inconsistencies in k-space data, which after Fourier reconstruction, manifest as blurring, ghosting, or signal loss [10].
Solution:
- Step 1: Quantify Motion. Do not rely on visual inspection alone. Use the motion parameters (3 translations, 3 rotations) generated by your scanner or preprocessing software to quantify the maximum displacement and mean framewise displacement for each subject [11].
- Step 2: Implement Prospective Motion Correction (if available). If your scanner is equipped with a system like volumetric navigators (vNavs), use it. vNavs track the subject's head and update the imaging coordinates in real-time, significantly reducing motion-induced bias and variance in morphometry [9].
- Step 3: Aggressive Data Scrubbing. For datasets already acquired, implement stringent motion censoring. Identify and remove volumes with framewise displacement exceeding a strict threshold (e.g., 0.2 mm). In severe cases, exclude subjects with excessive motion from the analysis [9].
- Step 4: Include Motion Parameters as Covariates. In your statistical model (e.g., GLM for fMRI), include the motion parameters as regressors of no interest to account for residual variance related to head motion [11].
Prevention:
- Use comfortable but effective head immobilization (pads, tape).
- For patient populations prone to movement, prioritize sequences with built-in prospective motion correction.
- Provide clear instructions to subjects and practice staying still before the scan.
Guide 2: Addressing Motion Corruption in Magnetic Resonance Spectroscopy (MRS)
Problem: Single Voxel Spectroscopy (SVS) data shows poor spectral quality—broadened linewidth, low signal-to-noise, or unexplained lipid contamination—making metabolite quantification unreliable.
Explanation: MRS is exceptionally susceptible to motion because it requires long scan times and excellent B0 field homogeneity. Motion causes two primary issues: (1) incorrect voxel placement, leading to signals from outside the region of interest, and (2) degradation of B0 shimming, which broadens spectral lines and reduces resolution [12].
Solution:
- Step 1: Detect Corruption. For SVS, if data is acquired as a series of transients, inspect the individual transients for frequency and phase shifts. Spectroscopic imaging may show obvious spatial smearing [12].
- Step 2: Re-shim During Acquisition. The most effective solution is prospective correction with an internal navigator that can update both the voxel position and the B0 shim in real-time. This corrects for both localization and field homogeneity errors caused by motion [12].
- Step 3: Post-Processing Correction. If real-time correction is not available, use retrospective methods. This can include discarding motion-corrupted transients and performing spectral alignment (frequency and phase correction) on the remaining transients. Note that this cannot correct for the fact that data is averaged from different spatial locations [12].
Prevention:
- Use vendor-provided or custom prospective motion correction packages for MRS sequences.
- Minimize scan time where possible without compromising SNR.
- Ensure subjects are comfortably immobilized.
Frequently Asked Questions (FAQs)
FAQ 1: Why does motion reduce the statistical power of my fMRI study, even after motion correction?
Motion reduces statistical power primarily by increasing variance in the data. Motion artifacts add noise to the time series, which increases the residuals in your General Linear Model (GLM). Since statistical significance depends on the signal-to-noise ratio, higher noise reduces your ability to detect true activation [11]. While motion correction algorithms realign data and including motion parameters as covariates can help, they are imperfect and cannot fully reverse all spin history and magnetic field effects [11]. Therefore, the most effective strategy is to prevent motion from occurring in the first place.
FAQ 2: What is the difference between prospective and retrospective motion correction, and which should I use?
- Prospective Motion Correction: Motion is tracked during the scan (using cameras, MR markers, or navigators), and the imaging sequence is adaptively updated in real-time to follow the head's movement. The main advantage is that it acquires consistent, motion-free data from the start [9] [13].
- Retrospective Motion Correction: Motion is estimated after the scan from the acquired data itself, and corrections are applied during image reconstruction. This is more widely available but can be suboptimal as it cannot fully correct for spin history effects or changes in the magnetic field [10] [13].
You should use prospective correction whenever possible, as it directly addresses the root of the problem. Retrospective methods are a valuable fallback for existing data but are generally considered less comprehensive [13].
FAQ 3: We are planning a large-scale neuroimaging study. What is the minimum motion correction protocol we should implement?
For a large-scale study, a multi-layered approach is critical:
- Prevention: Standardize subject immobilization and communication across all sites.
- Prospective Correction: Mandate the use of prospective motion correction (e.g., vNavs, optical tracking) for all high-resolution structural and critical functional sequences [9].
- Quality Control: Implement an automated, quantitative motion assessment pipeline. Define clear, pre-registered exclusion criteria based on metrics like mean framewise displacement [9].
- Statistical Control: In your group-level analyses, include summary motion metrics as covariates to account for residual effects of motion across subjects.
FAQ 4: Can new Deep Learning methods correct for motion without the need for specialized hardware?
Yes, deep learning is a promising approach for retrospective motion correction directly in the image domain. Models like PI-MoCoNet and Res-MoCoDiff use architectures like U-Nets with Swin Transformer blocks to learn a mapping from motion-corrupted to motion-free images, leveraging both spatial and k-space information [14] [15]. These methods have shown significant improvements in metrics like PSNR and SSIM and have the advantage of not requiring raw k-space data or scanner modifications [14]. However, they require training on large datasets and there is a risk of "hallucinating" image features, so validation in a clinical context is ongoing.
Quantitative Data on Motion's Impact
Table 1: Impact of Motion and Correction on MRI Image Quality Metrics (Simulated Data)
| Motion Severity | Condition | PSNR (dB) | SSIM | NMSE (%) | Dataset |
|---|---|---|---|---|---|
| Minor | Motion-Corrupted | 34.15 | 0.87 | 0.55 | IXI [15] |
| After PI-MoCoNet Correction | 45.95 | 1.00 | 0.04 | ||
| Moderate | Motion-Corrupted | 30.23 | 0.80 | 1.32 | IXI [15] |
| After PI-MoCoNet Correction | 42.16 | 0.99 | 0.09 | ||
| Heavy | Motion-Corrupted | 27.99 | 0.75 | 2.21 | IXI [15] |
| After PI-MoCoNet Correction | 36.01 | 0.97 | 0.36 |
Table 2: Performance of Different Motion Correction Methods on a Clinical Dataset (MR-ART)
| Correction Method | PSNR (dB) | SSIM | NMSE (%) | Inference Time |
|---|---|---|---|---|
| No Correction (Low Artifact) | 23.15 | 0.72 | 10.08 | N/A |
| PI-MoCoNet (Low Artifact) | 33.01 | 0.87 | 6.24 | ~0.37s per batch [15] |
| No Correction (High Artifact) | 21.23 | 0.63 | 14.77 | N/A |
| PI-MoCoNet (High Artifact) | 31.72 | 0.83 | 8.32 | ~0.37s per batch [15] |
| Res-MoCoDiff (Various) | Up to 41.91 | Superior SSIM | Lowest NMSE | 0.37s per batch [14] |
Experimental Protocols for Motion Correction
Protocol A: Implementing Prospective Motion Correction with Volumetric Navigators (vNavs)
Purpose: To acquire structural MRI data (e.g., MPRAGE) with reduced motion-induced bias for brain morphometry.
Methodology:
- Sequence Modification: Embed a low-resolution volumetric navigator (vNav) into the dead time of the pulse sequence, typically once per TR. Each vNav acquires a 3D head volume in approximately 300 ms [9].
- Real-time Tracking: The vNav volumes are rapidly registered to a reference volume to estimate the subject's head position (6 degrees of freedom) [9].
- Prospective Update: The estimated motion parameters are used to update the imaging plane and frequency of the subsequent TR in real-time, ensuring data is acquired in head-relative coordinates [9].
- Retrospective Reacquisition (Optional): The system can be set to automatically reacquire TRs that are determined to have been severely motion-degraded based on the motion estimates, providing a further reduction in artifacts [9].
Key Parameters:
- vNav resolution: Typically isotropic ~8-16 mm.
- vNav update rate: Once per TR (e.g., every 2-3 seconds).
- Reacquisition threshold: Define a motion threshold beyond which data is reacquired.
Protocol B: Data-Driven Motion Correction for fMRI using GLM Covariates
Purpose: To mitigate the effects of residual motion on the statistical analysis of fMRI data after volume realignment.
Methodology:
- Motion Estimation: During preprocessing, a rigid-body registration algorithm (e.g., FSL FLIRT, SPM realign) is used to align each volume to a reference volume (often the first one), producing 6 time series (3 translations, 3 rotations) that parameterize the head motion [11].
- Noise Regression: In the General Linear Model (GLM) set up for the fMRI time series, include the 6 motion parameters as predictors of no interest (regressors). This accounts for variance in the signal that is linearly related to head motion [11].
- Extended Model (Recommended): To further reduce motion-related noise, also include the temporal derivatives of the 6 motion parameters, and the time points identified as "motion outliers" (e.g., using Framewise Displacement) as additional regressors.
Visual Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Motion Correction in Neuroimaging Research
| Tool / Reagent | Type | Primary Function | Key Considerations |
|---|---|---|---|
| Volumetric Navigators (vNavs) | MR-based Tracking | Embedded low-resolution 3D scans to track head pose and update imaging coordinates prospectively. | Reduces bias in morphometry; adds minimal scan time [9]. |
| Optical Motion Tracking | External Tracking | Camera system tracks markers on the subject's head to provide high-frame-rate pose data. | High precision; can be obstructed by RF coils at ultra-high field [10] [13]. |
| FID Navigators | MR-based Tracking | Rapid Free Induction Decay signals to detect motion without prolonging scan time. | Can be used for automated image quality prediction and early scan termination [16]. |
| Swin Transformer U-Net | Deep Learning Model | Neural network architecture for image restoration; excels at capturing long-range dependencies for artifact removal. | Core component of modern DL correction models like PI-MoCoNet and Res-MoCoDiff [14] [15]. |
| Data Consistency Loss | Algorithmic Component | A loss function used in DL training that enforces fidelity between the corrected image and the original k-space data. | Prevents image "hallucinations" and ensures physically plausible corrections [15]. |
| PROPELLER/MULTIBLADE | Self-Navigating Sequence | K-space sampling with rotating blades where the center of each blade acts as a navigator. | Enables motion detection and correction without external hardware [13]. |
Special Challenges in Pediatric and Neurodegenerative Disease Cohorts
Frequently Asked Questions (FAQs)
Q1: Why is head motion a more critical confound in neurodevelopmental and neurodegenerative disorder studies?
Head motion is a critical confound because it does not introduce random noise but rather spatially structured artifacts that can mimic or obscure genuine neurobiological effects. Specifically, motion adds spurious signal that is more similar at nearby voxels than at distant ones, creating a distance-dependent modulation of correlations in functional MRI (fMRI) [17]. This is particularly problematic when studying neurodevelopmental disorders (NDDs) or neurodegenerative diseases, as these patient populations often move more in the scanner than healthy control groups. Consequently, observed group differences in connectivity—such as the "underconnectivity" reported in children, the elderly, or autistic individuals—can be at least partially attributable to this motion artifact rather than the biology of the disorder itself [17] [18].
Q2: What are the specific challenges in normalizing brain images from pediatric cohorts?
A primary challenge is the use of standard brain templates, like those from the Montreal Neurological Institute (MNI), which are based on adult brains. Normalizing a child's brain to an adult template can introduce significant inaccuracies because children's brains are structurally different; their skulls are thinner, sinuses are not fully formed, and there is less space for cerebrospinal fluid around the brain [18]. Furthermore, childhood and adolescence are periods of dynamic neurodevelopment, with whole-brain volume growing by approximately 25%, gray matter by 13%, and white matter by a remarkable 74% [18]. Using an adult template fails to account for these rapid and non-linear developmental changes, potentially leading to misalignment and misinterpretation of data.
Q3: How can motion artifacts bias structural MRI analyses, such as T1-weighted scans?
In structural T1-weighted MRI, even small, visually undetectable head motions can create imaging artifacts that systematically reduce estimates of gray matter volume [19]. This poses a severe problem for neuromorphometric studies, as motion is often correlated with variables of interest. For example, since older adults or individuals with certain neurological conditions may move more, the observed reductions in their gray matter volume could be an overestimation caused by motion bias rather than a true anatomical difference [19].
Q4: What is the utility of optical head tracking compared to image-based motion estimation?
Optical head tracking using depth cameras offers a direct, external method for measuring head motion with high accuracy and high frequency, capturing even rapid, burst movements [19]. In contrast, common image-based methods, like calculating realignment parameters from an fMRI time series, provide a low-frequency estimate that aggregates motion over the acquisition of a full volume (often 0.5 to several seconds). This makes them less sensitive to short, sharp movements. Furthermore, fMRI-based estimates are themselves affected by intra-frame motion artifacts and are inapplicable to single-volume structural scans, though they are sometimes used as a proxy for motion in adjacent acquisitions [19].
Troubleshooting Guides
Guide 1: Mitigating Motion Artifacts in Functional Connectivity Analyses
Problem: Analysis of resting-state fMRI data from a cohort mixing patients and controls shows a pattern of stronger short-distance and weaker long-distance correlations in the patient group. You suspect motion may be causing a spurious, distance-dependent bias.
Solution: Implement a multi-step denoising pipeline that goes beyond simple realignment.
- Step 1: Quantify Motion Accurately. Calculate Framewise Displacement (FD) and DVARS for each subject. FD measures the volume-to-volume change in head position, while DVARS measures the rate of change of the BOLD signal across the entire brain at each timepoint [17] [20]. These metrics help characterize the extent of motion in your dataset.
- Step 2: Employ Rigorous Denoising Strategies. Use the motion parameters calculated in Step 1 to clean your data. Common strategies include:
- Regression: Include the 6 rigid-body realignment parameters (and optionally their derivatives and squares, making 24 regressors) as nuisance covariates in your model [20].
- * scrubbing:* Identify and censor volumes with excessive motion (e.g., FD > 0.2-0.5 mm) by adding additional regressors for those specific time points [20].
- Volume Interpolation: For motion outliers, replace the corrupted volume by interpolating from adjacent, non-corrupted volumes [20].
- Step 3: Control for Group-Level Motion Differences. Always test for and report whether your patient and control groups differ significantly in their mean FD or DVARS. If they do, include these motion metrics as covariates in your group-level statistical analyses to ensure that any observed effects are not driven by motion [17] [18].
Table 1: Common Motion Quantification Metrics
| Metric | Description | Typical Threshold | Primary Use |
|---|---|---|---|
| Framewise Displacement (FD) | Summarizes volume-to-volume changes in head position based on translation and rotation parameters [17]. | 0.2 - 0.5 mm | Identifying motion-contaminated volumes for scrubbing. |
| DVARS | Measures the root mean square change in BOLD signal across all voxels from one volume to the next [17] [20]. | 0.5% ΔBOLD | Detecting large, global signal shifts caused by motion or other artifacts. |
Guide 2: Addressing Pediatric-Specific Analysis Challenges
Problem: After processing structural MRI scans from a pediatric cohort using a standard adult-based pipeline, you notice poor normalization and segmentation, particularly in younger subjects.
Solution: Adapt your processing pipeline to be developmentally sensitive.
- Step 1: Use Pediatric Brain Templates. Instead of standard adult templates (e.g., MNI), warping participant brains to age-appropriate pediatric templates. These templates account for the smaller brain size and different structural proportions in children, leading to more accurate spatial normalization [18].
- Step 2: Account for Developmental Trajectories. Do not treat a pediatric cohort as a single, homogeneous group. The brain changes dramatically from childhood to adolescence. Your analysis should either:
- Step 3: Consider Psychotropic Medication Use. A significant proportion of children with NDDs may be taking psychotropic medications, which can alter brain structure and function. Document and, if possible, statistically account for medication use, as it is a potential confounding variable [18].
The following workflow diagram summarizes the key steps for handling data from these challenging cohorts:
Experimental Protocols & Reagent Solutions
This section details a protocol for evaluating motion correction strategies in a task-based fMRI study, relevant to clinical populations like those with Multiple Sclerosis [20].
Protocol: Systematic Comparison of Motion Correction Models in Task-fMRI
- 1. Data Acquisition: Acquire task-fMRI data (e.g., a visual or motor paradigm) from participant groups (e.g., patients and healthy controls).
- 2. Motion Parameter Estimation: Realign all fMRI volumes to a reference volume (e.g., the first volume) to generate the 6 rigid-body motion parameters (translations X, Y, Z; rotations pitch, roll, yaw).
- 3. Create Expanded Parameter Sets: Derive the expanded sets of motion regressors:
- 12-Parameter Set: The 6 original parameters plus their temporal derivatives.
- 24-Parameter Set: The 12 parameters plus their squared values [20].
- 4. Detect Motion Outliers: Calculate Framewise Displacement (FD) for each volume. Flag volumes as motion outliers where FD exceeds a defined threshold (e.g., 0.5 mm).
- 5. Implement Correction Models: Analyze the data using multiple General Linear Models (GLMs) that incorporate different motion correction strategies:
- Model A: Nuisance regressors for the 6 motion parameters.
- Model B: Nuisance regressors for the 24 motion parameters.
- Model C: Model A plus scrubbing regressors for motion outliers.
- Model D: Model A with volume interpolation for motion outliers.
- 6. Evaluate Model Performance: Compare the resulting task-activation maps from each model. Assess performance based on metrics like the sensitivity and specificity for detecting expected task-related activation, and the reduction of motion-related artifacts.
Table 2: Key Research Reagent Solutions for Motion Correction
| Tool / Resource | Type | Function in Research |
|---|---|---|
| Framewise Displacement (FD) | Software Metric | Quantifies volume-to-volume head movement to identify scans with excessive motion [17] [20]. |
| DVARS | Software Metric | Measures the rate of global BOLD signal change to identify motion-corrupted timepoints [17] [20]. |
| Volume Interpolation | Software Algorithm | Replaces signal from motion-corrupted volumes with data interpolated from adjacent clean volumes, preserving the temporal structure of the data [20]. |
| High-Frequency Optical Tracking | Hardware/Software System | Provides an external, direct measure of head motion with high temporal resolution, independent of MRI image data [19]. |
| Pediatric Brain Templates | Digital Atlas | Age-specific brain templates for spatial normalization, crucial for accurate processing of pediatric neuroimaging data [18]. |
Frequently Asked Questions (FAQs)
FAQ 1: Why is motion correction particularly critical for large, multi-site neuroimaging studies?
In large, multi-site studies, data is aggregated from different research facilities using scanners from various vendors and with differing acquisition protocols. This introduces "batch effects"—variations in the data not due to the biological phenomenon under study but to the peculiarities of the acquisition equipment and parameters [22]. Head motion is a significant source of such batch effects. If not corrected, motion-induced artifacts can create systematic biases that confound true biological signals, reduce the statistical power of the study, and lead to unreliable or misleading results when developing automated tools like deep learning models for diagnosis [22].
FAQ 2: What are the main classes of motion correction strategies, and how do they differ?
Motion correction strategies can be broadly categorized into two classes:
- Prospective Motion Correction: This method adjusts the imaging plane in real-time to follow the subject's head movements during the scan. It often requires external hardware, like optical tracking systems, or dedicated navigator pulses [23] [24].
- Retrospective Motion Correction: This approach does not require special hardware. Instead, it estimates motion from the acquired data itself and corrects for it during the image reconstruction process. Techniques like PROPELLER (for 2D motion) and those using 3D radial sampling fall into this category [23] [24]. Retrospective methods are often more practical for large consortia as they do not depend on specific, and potentially expensive, hardware available at all sites.
FAQ 3: How can we quantitatively assess the success of motion correction in a dataset?
The success of motion correction can be evaluated using both qualitative (human-led) and quantitative (automated) measures:
- Qualitative Scoring: Expert radiologists or trained technicians can review images using a standardized Likert scale (e.g., 0-unusable to 4-excellent) to score image quality before and after correction [23].
- Quantitative Metrics: Automated, reference-free metrics like the Tenengrad metric provide a numerical measure of image sharpness, which is often reduced by motion-induced blurring [23]. Statistical analysis of vessel conspicuity, lumen area, and hemodynamic markers like blood flow rate can also reveal significant improvements post-correction [25].
FAQ 4: Our multi-site study uses different MRI scanners. How can we ensure motion correction strategies are effective across all platforms?
Ensuring effectiveness across platforms involves a combination of strategic sequence design and data harmonization:
- Use Robust Acquisition Sequences: Implement imaging sequences that are inherently more resilient to motion. 3D radial sampling is highly advantageous because motion artifacts manifest as diffuse blurring rather than distinct ghosts, and the oversampled k-space center can be used for self-navigation [23] [25].
- Apply Data Harmonization Methods: After data collection, use harmonization techniques to explicitly minimize the impact of site-specific batch effects. This can involve quality control protocols, statistical harmonization, or using deep learning models designed to be invariant to these technical variations [22].
Troubleshooting Guides
Guide 1: Troubleshooting Poor Image Quality Due to Subject Motion
Problem: Reconstructed structural images (e.g., T1-weighted) show blurring or ghosts, making anatomical boundaries unclear.
| Step | Action & Rationale | Underlying Principle |
|---|---|---|
| 1 | Verify Motion Presence: Check for reported motion during the scan or use automated sharpness metrics (e.g., Tenengrad) on the raw images to confirm motion degradation [23]. | Establishes a baseline and confirms the root cause. |
| 2 | Apply Retrospective Correction: If a motion-resilient sequence (e.g., 3D radial) was used, employ a retrospective correction pipeline. This involves generating low-resolution 3D navigators from short-duration k-space data to estimate motion parameters via image registration, then applying these transforms to the k-space data before final reconstruction [23]. | Corrects for rigid-body motion after data acquisition without needing special hardware. |
| 3 | Optimize Navigator Parameters: If correction is suboptimal, adjust the resolution of the internal navigators. Very low resolution may miss subtle motion, while very high resolution may introduce aliasing. An optimal range (e.g., 5-7 mm) typically exists [23]. | Fine-tunes the motion estimation accuracy. |
| 4 | Re-score Image Quality: Have a blinded reviewer re-score the corrected image using a standardized scale and/or recalculate the sharpness metric to quantify improvement [23]. | Validates the effectiveness of the correction. |
Guide 2: Addressing Hemodynamic Bias in 4D-Flow MRI
Problem: Quantitative blood flow measurements in cerebral arteries are inconsistent or show unexpectedly high variability, potentially due to subject motion.
| Step | Action & Rationale | Underlying Principle |
|---|---|---|
| 1 | Identify Motion Bias: Compare quantitative flow rates, pulsatility indices, and lumen areas between subjects who moved and those who remained still. Look for significant differences that signal motion-induced bias [25]. | Diagnoses motion as a source of hemodynamic measurement error. |
| 2 | Implement Self-Navigated 4D-Flow: For new acquisitions, use a 3D radial trajectory with pseudorandom ordering. This allows the creation of high spatiotemporal resolution self-navigators from highly undersampled data for robust motion estimation [25]. | Acquires data that is well-suited for retrospective motion correction. |
| 3 | Apply Multi-Scale Motion Correction: Reconstruct the data using a multi-resolution low-rank regularization approach to support the motion correction process. Apply the derived rigid motion parameters to the 4D-Flow data [25]. | Corrects for motion throughout the acquisition, improving vessel sharpness and measurement accuracy. |
| 4 | Re-quantify Hemodynamics: Re-measure flow parameters after correction. Clinical exams have shown that motion correction can lead to statistically significant changes in these values, providing more reliable biomarkers [25]. | Yields more accurate and consistent quantitative results. |
Guide 3: Managing Batch Effects from Motion in Multi-Site DL Models
Problem: A deep learning model trained on aggregated multi-site data performs poorly on new data, likely because it learned site-specific motion artifacts instead of true biological features.
| Step | Action & Rationale | Underlying Principle |
|---|---|---|
| 1 | Detect the Batch Effect: Use a simple classifier (e.g., a CNN) to try and predict the scanner site or protocol from the images. High accuracy indicates strong, problematic batch effects that the model can exploit [22]. | Proves the presence of confounding technical variation. |
| 2 | Apply Data Harmonization: Use explicit methods to standardize the data across sites. This can include strict quality control to exclude severely motion-corrupted images or using algorithms like ComBat to remove site-specific technical effects [22]. | Explicitly minimizes unwanted technical variability before model training. |
| 3 | Utilize Domain Adaptation: Develop DL models that are inherently robust to domain shifts. Train the model on the multi-site data, using techniques that force it to learn features that are invariant to the source site, thereby ignoring site-specific artifacts [22]. | Creates a model that implicitly handles variability, improving generalizability. |
| 4 | Validate on External Data: Benchmark the harmonized or domain-adapted model on a completely independent dataset acquired with different protocols to ensure its robustness and clinical utility [22]. | Tests the true generalizability of the developed tool. |
Quantitative Data on Motion Correction Efficacy
Table 1: Impact of Retrospective Motion Correction on Structural Image Quality
Data derived from a study of 44 pediatric participants scanned with a motion-corrected MPnRAGE sequence [23].
| Metric | Non-Corrected Images | Motion-Corrected Images | Change & (P-Value) |
|---|---|---|---|
| Mean Likert Score (0-4 scale) | 3.0 | 3.8 | +0.8 |
| Standard Deviation (Likert) | 1.1 | 0.4 | -0.7 |
| Quality Improvement | -- | -- | Significant (P < 0.001) |
| Worst-case Improvement | Unusable (Score 0) | Good (Score 3) | +3 points |
Table 2: Effect of Motion Correction on Neurovascular 4D-Flow Hemodynamics
Data from clinical-research exams showing significant changes in quantitative flow metrics after motion correction [25].
| Cerebral Artery | Blood Flow (P-value) | Lumen Area (P-value) | Flow Pulsatility Index (P-value) |
|---|---|---|---|
| Left Internal Carotid (Lt ICA) | P < 0.001 | P < 0.001 | -- |
| Right Internal Carotid (Rt ICA) | P = 0.002 | P < 0.001 | P = 0.042 |
| Left Middle Cerebral (Lt MCA) | P = 0.004 | P = 0.004 | P = 0.002 |
| Right Middle Cerebral (Rt MCA) | P = 0.004 | P = 0.004 | -- |
Experimental Protocols for Motion-Corrected Imaging
Protocol 1: MPnRAGE with Integrated Motion Correction for Structural Imaging
This protocol is designed for acquiring high-resolution T1-weighted volumetric images in challenging populations (e.g., un-sedated pediatric participants) where motion is likely [23].
- Pulse Sequence: 3D radial sampling combined with an inversion-recovery magnetization preparation (MPnRAGE).
- Key Parameters:
- k-space View Ordering: Double bit-reversed scheduling to ensure pseudorandom sampling for both navigator formation and multi-contrast reconstruction.
- Navigator Formation: Subsets of consecutive radial views acquired between magnetization-preparation pulses (~400 views every 2 seconds) are used to form low-resolution 3D navigator images.
- Navigator Resolution: Reconstruct navigators at an isotropic resolution of 6 mm (optimized range 5-7 mm) by apodizing radial views with a Fermi filter.
- Motion Estimation: Use image coregistration tools (e.g., from the FSL library) on the navigator images to estimate 3D translational and rotational motion parameters.
- Final Reconstruction: Apply the estimated motion parameters to correct the k-space data before performing the full-resolution reconstruction.
Protocol 2: Self-Navigated 3D Radial 4D-Flow MRI for Hemodynamic Studies
This protocol enables retrospective rigid motion correction for neurovascular 4D-Flow MRI, crucial for accurate hemodynamic measurement in aging or other moving populations [25].
- Pulse Sequence: 4D-Flow MRI acquired using a 3D radial trajectory with pseudorandom view ordering.
- Key Components:
- Self-Navigation: The oversampled central k-space region of the 3D radial data is used to generate high spatiotemporal resolution navigators.
- Reconstruction Framework: A multi-scale low-rank reconstruction support is used to enable motion estimation from the extremely undersampled navigator data.
- Motion Correction: The rigid motion parameters derived from the self-navigators are applied retrospectively during the image reconstruction process.
- Outcome: This integrated approach reduces image blurring, increases vessel conspicuity, and decreases variability in quantitative hemodynamic markers.
Workflow Diagrams
Motion Correction in Multi-Site Studies
Retrospective Motion Correction Pipeline
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function & Application |
|---|---|
| 3D Radial Sequence | An MRI acquisition technique where k-space is sampled along spokes radiating from the center. It is inherently motion-resilient, as motion artifacts manifest as benign blurring rather than ghosts, and the oversampled center enables self-navigation for motion estimation [23] [25]. |
| Self-Navigation Framework | A software and algorithmic framework that uses intrinsically acquired data (e.g., the central k-space of radial scans) to track and estimate subject motion during an MRI scan, eliminating the need for external tracking hardware [23] [25]. |
| Tenengrad Sharpness Metric | A reference-free, quantitative image quality metric that measures the sharpness of an image by computing the squared magnitude of the gradient. It is highly correlated with human perception of motion-induced blurring and is used for automated quality control [23]. |
| Data Harmonization Tools (e.g., ComBat) | Statistical or algorithmic tools designed to remove site-specific "batch effects" from aggregated multi-site datasets. This ensures that variability in the data is due to biological rather than technical differences, which is critical for training generalizable models [22]. |
| Domain Adaptation DL Models | A class of deep learning models (e.g., Domain Adversarial Neural Networks) specifically designed to learn features that are invariant across different data domains (e.g., different scanner sites). This makes the models robust to unseen data from new sites [22]. |
Motion Correction Arsenal: From Prospective Tracking to AI-Driven Solutions
Prospective Motion Correction (PMC) is a sophisticated technique in magnetic resonance imaging (MRI) that addresses the persistent challenge of subject motion during scanning. Unlike retrospective methods that apply corrections after data acquisition, PMC operates in real-time by dynamically adjusting the imaging sequence to track and compensate for head movements as they occur. This approach is particularly crucial for high-resolution neuroimaging and functional MRI (fMRI) studies where even minor movements can significantly degrade data quality. PMC systems primarily utilize two technological approaches: external optical tracking devices that monitor head position using cameras and markers, and MR-based navigators (MR-Nav) that employ embedded sequence modifications to track motion directly from the acquired signal. Both methods enable continuous updating of scan planes by modifying gradient orientations and radiofrequency pulses, effectively "locking" the imaging volume to the moving anatomy. This technical framework is especially valuable for large-scale neuroimaging studies and drug development research where data consistency across subjects and sessions is paramount for reliable statistical analysis and outcome measurements [26] [27] [28].
Technical Foundations
Optical Tracking Systems
Optical tracking systems for PMC utilize camera-based monitoring of specialized markers attached to the subject's head to provide real-time motion data. These systems typically employ either single or multiple cameras positioned within the scanner bore or mounted directly on the head coil. The fundamental principle involves continuous tracking of reflective or active markers secured to the subject via various attachment methods, with mouthpieces generally providing superior rigidity compared to skin attachments. Advanced implementations may utilize two markers placed on the forehead to enhance system robustness through "adaptive tracking" - if one marker becomes obscured, the system can infer its position from the visible marker using known relative transforms. This configuration also enables "squint detection" by monitoring relative positional changes between markers that indicate non-rigid facial movements, allowing the system to pause data acquisition during these events to prevent artifact introduction [29] [27] [30].
A critical requirement for optical tracking systems is cross-calibration - the process of determining the precise spatial transformation between the camera's coordinate system and the MRI scanner's inherent coordinate system defined by its gradients. This calibration must be extremely accurate (substantially below 1 mm and 1°) to ensure effective motion correction, as errors propagate through to residual tracking inaccuracies. Recent methodological advances have streamlined this process using custom calibration tools with wireless active markers, reducing calibration time from approximately 30 minutes to under 30 seconds per installation while maintaining sufficient accuracy for clinical applications. This improvement addresses a significant barrier to clinical deployment of optical PMC systems [29] [31].
MR-Based Navigators
MR-based navigators (MR-Nav) represent an alternative approach that embeds brief, additional acquisitions within the primary imaging sequence to directly monitor subject position. These specialized acquisitions sample limited k-space data that can be rapidly reconstructed and analyzed for motion detection. The PROMO (PROspective MOtion correction) system exemplifies this approach, utilizing three orthogonal 2D spiral navigator acquisitions (SP-Navs) combined with an Extended Kalman Filter (EKF) algorithm for online motion measurement. This framework offers image-domain tracking within patient-specific regions-of-interest with reduced sensitivity to off-resonance-induced corruption of rigid-body motion estimates [32].
Spiral navigators provide efficient k-space coverage with parameters typically including: TE/TR = 3.4/14 ms, flip angle = 8° (to minimize impact on the acquired 3D volume), bandwidth = ±125 kHz, field-of-view = 32 cm, effective in-plane resolution = 10 × 10 mm, reconstruction matrix = 128 × 128, and slice thickness = 10 mm. The spiral readouts are particularly advantageous due to their efficient k-space coverage and reduced sensitivity to distortion, though they remain vulnerable to severe off-resonance effects (> ±100 Hz) which can be mitigated through center frequency correction before scanning. These navigators can be strategically inserted during intrinsic sequence dead time, such as the longitudinal recovery time in 3D inversion recovery spoiled gradient echo (IR-SPGR) and 3D fast spin echo (FSE) sequences, minimizing impact on total scan duration [32].
Table 1: Comparison of Optical and Navigator-Based PMC Approaches
| Feature | Optical Tracking | MR-Based Navigators |
|---|---|---|
| Tracking Principle | External camera monitors head-mounted markers | Embedded sequence modifications acquire limited k-space data |
| Hardware Requirements | MR-compatible camera system, markers, attachment method | No additional hardware required |
| Typical Accuracy | <0.1 mm position, <0.1° orientation [30] | <10% of motion magnitude, even for rotations >15° [32] |
| Key Advantages | Independent of MRI sequence, preserves magnetization steady state | No line-of-sight requirements, internal coordinate system |
| Primary Limitations | Line-of-sight requirements, marker attachment challenges | Sequence modification required, potential TR prolongation |
| Calibration Requirements | Cross-calibration between camera and scanner coordinates (<1 mm/1° accuracy) | No cross-calibration needed |
| Representative Systems | Moiré Phase Tracking (MPT), in-bore camera systems | PROMO with spiral navigators, cloverleaf navigators |
Experimental Protocols
Optical Tracking Implementation Protocol
Implementing optical PMC requires careful attention to system setup, calibration, and validation. The following protocol outlines the key steps for reliable operation:
System Setup and Cross-Calibration: Mount the camera securely on the head coil to maintain an unobstructed view of the marker throughout expected motion ranges. For systems requiring cross-calibration, use a calibration tool with integrated wireless active markers and optical tracking features. Perform the calibration scan by moving the tool through 10-20 poses including rotations about all three axes (maximum approximately 15°) while simultaneously tracking via both camera and active markers. This process typically requires approximately 30 seconds and needs repetition only if the camera position changes relative to the scanner. Implement a calibration adjustment method to automatically compensate for table motion between scans [29].
Marker Attachment and Validation: Attach the marker using a rigid attachment method. While skin adhesives are generally insufficient, custom-molded mouthpieces provide excellent rigidity. For forehead placement, consider using two markers to enable redundancy and squint detection. Validate marker rigidity by having the subject perform facial movements (e.g., squinting, talking) while monitoring relative marker positions. If significant motion (>0.5 mm or >0.5°) is detected between markers, reposition or reinforce the attachment [27] [30].
Sequence Integration: Integrate tracking data into the pulse sequence using libraries such as XPACE, applying motion compensation before each radiofrequency pulse to maintain consistent anatomical alignment. For multi-marker systems, implement logic to automatically switch tracking source if the primary marker becomes obscured, using the known relative transform between markers calculated during periods of simultaneous visibility [30].
MR-Navigator Implementation Protocol
Implementing MR-based navigators requires pulse sequence modification and optimization of navigator parameters:
PROMO with Spiral Navigators: Integrate three orthogonal 2D spiral navigator acquisitions (SP-Navs) into the pulse sequence, positioned during intrinsic dead time such as the T1 recovery periods in 3D sequences. For 3D IR-SPGR and 3D FSE sequences, acquire multiple SP-Navs during the recovery time (e.g., 5 SP-Navs over ~500 ms during a 700-1200 ms recovery period). Each SP-Nav requires approximately 42 ms for acquisition plus 6 ms for reconstruction of all three planes. Program the repetition time for each SP-Nav to 100 ms to allow ample time for estimation and feedback [32].
Motion Tracking and Correction: Implement the Extended Kalman Filter (EKF) algorithm for real-time motion estimation using the dynamic state-space model. The EKF provides recursive state estimates in nonlinear dynamic systems perturbed by Gaussian noise, with the system equation: xk = Axk-1 + w; P(w)~N(0,Q) and measurement equation: yk = h(xk) + v; P(v)~N(0,R). Apply motion compensation by updating the imaging volume position and orientation based on the EKF estimates [32].
Performance Validation: Validate tracking performance using staged motions and compare with known motion parameters. The steady-state error of SP-Nav/EKF motion estimates should be less than 10% of the motion magnitude, even for large compound motions including rotations over 15°. For functional studies, verify improvement in temporal signal-to-noise ratio (tSNR) and reduction of spin history effects [32] [27].
Troubleshooting Guides
Common Optical Tracking Issues
Problem: Poor Image Quality Despite PMC Activation
- Possible Cause 1: Inaccurate cross-calibration between camera and scanner
- Solution: Reperform cross-calibration using the rapid calibration method with the dedicated calibration tool. Ensure the tool moves through sufficient poses (10-20) with rotations about all three axes during calibration [29] [31].
- Possible Cause 2: Marker attachment flexibility
- Solution: Verify marker rigidity by monitoring relative position during facial movements. Switch to a custom-molded mouthpiece if skin attachments show excessive movement (>0.5 mm between markers) [27] [30].
- Possible Cause 3: Calibration drift due to table movement
- Solution: Implement automated calibration adjustment to compensate for table position changes between scans [29].
Problem: Intermittent Tracking Loss
- Possible Cause 1: Obstructed line-of-sight between camera and marker
- Solution: Reposition camera to maximize field of view within coil constraints. Implement two-marker tracking with automatic switching to maintain tracking when one marker is obscured [30].
- Possible Cause 2: Marker moving outside camera field of view
- Solution: Adjust camera angle or use wide-angle lens. For large motions, consider additional cameras or marker placement optimization [29].
Problem: Introduction of Artifacts During PMC
- Possible Cause 1: Non-rigid facial motions (squinting, talking)
- Solution: Implement two-marker system with squint detection. Pause data acquisition when non-rigid motion is detected (relative marker movement >0.5 mm or >0.5°) and resume once rigid-body conditions return [30].
- Possible Cause 2: Latency in tracking data processing
- Solution: Optimize tracking data pipeline. Ensure camera operates at sufficient frame rate (≥60 Hz) and minimize processing delays between motion detection and sequence update [29].
Common MR-Navigator Issues
Problem: Increased Scan Time with Navigators
- Possible Cause: Navigator acquisition extending repetition time
- Solution: Optimize navigator placement within sequence dead time. For 3D sequences, insert multiple navigators during T1 recovery periods rather than between excitations [32].
Problem: Poor Tracking Accuracy
- Possible Cause 1: Severe off-resonance effects
- Solution: Perform center frequency correction before scanning. For areas with pronounced field inhomogeneities, consider alternative navigator trajectories less sensitive to off-resonance [32].
- Possible Cause 2: Insufficient navigator resolution or coverage
- Solution: Optimize navigator parameters balancing accuracy and acquisition time. Spiral navigators with 10×10mm in-plane resolution and 10mm thickness typically provide sufficient accuracy [32].
Problem: Navigator Interference with Image Contrast
- Possible Cause: Saturation effects from navigator RF pulses
- Solution: Use low flip-angle navigators (e.g., 8°) to minimize impact on longitudinal magnetization [32].
Frequently Asked Questions (FAQs)
Q1: What are the key benefits of prospective versus retrospective motion correction?
Prospective motion correction addresses motion at its source by keeping the measurement coordinate system fixed relative to the patient throughout scanning, preventing data inconsistencies before they occur. This avoids several limitations of retrospective correction, including inability to fully correct for through-plane motion in 2D sequences, k-space data inconsistencies from interpolation errors, and spin history effects. PMC particularly benefits high-resolution acquisitions where even sub-millimeter motions can significantly degrade image quality [32] [26].
Q2: How does motion affect fMRI data quality specifically?
In fMRI, motion introduces temporal signal variations that confound the detection of BOLD activity through multiple mechanisms: (1) spin history effects from movement relative to RF excitation pulses; (2) intensity modulation from changing position relative to receiver coil sensitivity profiles; (3) partial-volume effect modulation from anatomical structures moving relative to voxel grids; and (4) B0 field modulation from head motion relative to static magnetic field inhomogeneities. These effects can increase false positives and reduce statistical significance of activation maps, particularly problematic in patient populations with limited compliance [26] [28].
Q3: What level of tracking accuracy is required for effective PMC?
The required accuracy depends on the application and expected motion range. For most neuroimaging applications, cross-calibration accuracy should be substantially below 1 mm and 1°. Optical tracking systems typically achieve <0.1 mm positional and <0.1° orientation accuracy. MR-navigator systems like PROMO maintain steady-state errors of less than 10% of motion magnitude, even for large rotations exceeding 15°. The general principle is that scans with smaller expected movements require less calibration accuracy than those involving larger movements [31] [30].
Q4: What attachment method is most reliable for optical markers?
Mouthpieces generally provide superior rigidity compared to skin attachments. While custom dentist-molded mouthpieces offer optimal performance, recent research shows that inexpensive, commercially available mouthpieces molded on-site can provide comparable results without the time and expense of dental visits. Skin attachments, particularly on the forehead, are susceptible to non-rigid motion from facial movements and typically show greater displacement relative to the skull [27] [30].
Q5: Can PMC improve data quality even in cooperative subjects instructed to remain still?
Yes, studies demonstrate that PMC provides benefits even in the absence of deliberate motion. In fMRI, PMC significantly increases temporal signal-to-noise ratio (tSNR) and improves the quality of resting-state networks and connectivity matrices, particularly at higher resolutions. The benefit is most apparent for multi-voxel pattern decoding where accurate voxel registration across time is essential [27] [28].
Table 2: Research Reagent Solutions for Prospective Motion Correction
| Component | Function | Examples & Specifications |
|---|---|---|
| Optical Tracking Camera | Tracks marker position and orientation | MR-compatible camera, 640×480 resolution, 60 Hz frame rate, monochrome [29] |
| Tracking Markers | Provides visual reference for tracking | Checkerboard optical marker (15×15mm), reflective or active markers, with unique identification barcodes [30] |
| Marker Attachment | Secures marker rigidly to subject | Custom-molded mouthpieces, skin-adhesive markers, dental impression material for on-site molding [27] |
| Calibration Tool | Enables camera-to-scanner cross-calibration | Sphere with integrated wireless active markers and optical marker, rigid construction [29] |
| Wireless Active Markers | Provides scanner-trackable reference for calibration | Small RF coils with water samples, detectable via specialized tracking sequences [29] |
| Spiral Navigators | MR-based motion tracking | 2D spiral acquisitions, TE/TR=3.4/14ms, 8° flip angle, 10mm thickness, 10×10mm in-plane resolution [32] |
| Software Libraries | Integration of tracking data into sequences | XPACE library for communication between tracker and sequence, Extended Kalman Filter implementation [32] [30] |
Workflow Diagrams
Frequently Asked Questions (FAQs)
FAQ 1: What is the core principle behind retrospective motion correction? Retrospective motion correction methods work by estimating motion from the acquired data itself, without the need for external tracking hardware. This is typically achieved through image-based registration techniques, where a series of low-resolution "navigator" images are reconstructed from subsets of the acquired data. These navigators are then coregistered to a reference volume to estimate rigid transformation parameters (rotations and translations), which are subsequently applied to the data during the final reconstruction process to create a motion-corrected image [23] [33].
FAQ 2: How does data-driven motion correction in PET differ from methods used in MRI? While both rely on estimating and correcting motion from the data, PET-specific methods often use list-mode data. An ultra-fast list-mode reconstruction framework partitions the data into very short time frames, reconstructs them to create a motion time series via image registration, and then performs a final event-by-event motion-corrected reconstruction. This approach can correct for both fast and slow intra-frame motion, which is crucial for long PET acquisitions [33].
FAQ 3: My motion-corrected images still show blurring or artifacts. What could be the cause? Several factors can lead to suboptimal correction:
- Insufficient Navigator Resolution: If the navigator images used for motion estimation are reconstructed at a suboptimal resolution, motion estimates can be inaccurate. One study found an optimal navigator resolution range of 5–7 mm for 3D radial MRI data [23].
- Irreversible Data Corruption: Some data points may be so severely corrupted by artifacts that they are irrecoverable. Techniques like "reliability masking," which exclude such unreliable data points from final analysis, can supplement motion correction [34].
- Residual Effects: Retrospective correction is limited because intra-slice and intra-voxel information is affected by motion, and computational methods can leave residual artifacts of their own [35].
FAQ 4: Can retrospective correction fully replace the need for sedation in pediatric imaging? Evidence suggests that robust motion correction can significantly reduce reliance on sedation. A prospective pediatric brain FDG-PET study demonstrated that motion-corrected images from scans with scripted motion were qualitatively and quantitatively indistinguishable from, or better than, images obtained without motion. This indicates that motion correction software can produce diagnostic-quality images from corrupted data, moving towards reduced sedation use [36].
FAQ 5: What are the key subject factors that predict higher levels of head motion during scanning? Knowledge of these factors helps in anticipating motion and planning studies. Analysis of a large cohort (n=40,969) from the UK Biobank revealed the following key indicators [35]:
Table 1: Key Indicators of fMRI Head Motion
| Indicator | Association with Head Motion | Effect Size (Adjusted β) |
|---|---|---|
| Body Mass Index (BMI) | Strongest positive association; a 10-point increase (e.g., "healthy" to "obese") linked to a 51% motion increase [35] | βadj = .050 [35] |
| Ethnicity | Significant association [35] | βadj = 0.068 [35] |
| Cognitive Task Performance | Associated with increased motion compared to rest [35] | t = 110.83 [35] |
| Prior Scan Experience | Associated with increased motion in follow-up scans [35] | t = 7.16 [35] |
| Disease Status (e.g., Hypertension) | Can be a significant indicator, but disease diagnosis alone is not a reliable predictor [35] | p = 0.048 [35] |
Troubleshooting Guide
Issue 1: Poor Registration Performance in Image-Based Motion Estimation
- Potential Cause: Inadequate signal-to-noise ratio (SNR) in the navigator images used for registration.
- Solution: Optimize the number of data views or the duration of each sub-scan used to reconstruct the navigators. Ensure the navigator resolution is appropriate; for a 3D radial MPnRAGE acquisition, a resolution of 6 mm was found to be optimal [23].
- Protocol: To determine the ideal navigator parameters, perform a pilot analysis using a reference-free sharpness metric (e.g., Tenengrad) on motion-corrected images reconstructed from navigators of varying resolutions [23].
Issue 2: High Variability in Quantitative Outcomes After Motion Correction
- Potential Cause: Motion-induced blurring increases the variability of quantitative measurements across subjects, reducing the statistical power of between-group differences.
- Solution: Implement a reliability masking step in your post-processing pipeline. This novel outlier rejection technique excludes irreversibly corrupted data points from the final analysis.
- Evidence: In a spinal cord DTI study, adding reliability masking to a processing chain (which already included registration and robust fitting) increased the statistical power of a between-group difference finding by 4.7%, primarily by reducing group-level variability [34].
Issue 3: Challenges in Handling Large-Scale, Multi-Site Neuroimaging Data
- Potential Cause: Traditional software may struggle with computational speed, memory allocation, and missing voxel-data common in aggregated datasets.
- Solution: Utilize a unified software framework like Image-Based Meta- & Mega-Analysis (IBMMA). This tool is designed for large-scale data, handles missing voxel-data robustly, uses parallel processing for efficiency, offers flexible statistical modeling, and can be implemented in R and Python [37].
Experimental Protocols for Validation
Protocol 1: Validating Motion Correction Performance in Phantom Studies
This protocol is used to validate a list-mode-based motion correction method for PET imaging [33].
- Phantom Setup: Use a Hoffman phantom or a Mini Hot Spot phantom filled with 18F solution.
- Acquisition:
- Perform a static, motion-free acquisition as a ground truth.
- Perform a second acquisition while introducing continuous, complex rotation and translation using a motorized system (e.g., QUASAR).
- Motion Tracking: Simultaneously track phantom motion with a high-accuracy optical tracking system (e.g., Polaris Vega Camera) to obtain ground-truth transformation parameters.
- Data Processing: Apply the retrospective motion correction method to the moving phantom data.
- Validation: Compare the motion parameters estimated by the software with the optical tracking ground truth. Visually and quantitatively compare the motion-corrected image against the motion-free ground truth and the uncorrected moving image.
Protocol 2: Assessing Impact on Clinical Quantitative Measures
This protocol evaluates the effect of motion correction on the longitudinal measurement of tau accumulation in Alzheimer's disease research [33].
- Subject Population: Recruit subjects for longitudinal PET studies (e.g., baseline and follow-up scans months apart) using a tracer like [18F]-MK6240.
- Data Acquisition & Reconstruction: Acquire list-mode PET data. Reconstruct each scan twice: with motion correction (MC) and without (NoMC).
- Quantitative Analysis: For each reconstruction, calculate the standard uptake value (SUV) in key brain regions of interest (e.g., entorhinal cortex, inferior temporal, precuneus).
- Longitudinal Calculation: For each subject and reconstruction type, compute the rate of tau accumulation as the difference in SUV between time points.
- Statistical Comparison: Calculate the standard deviation of the accumulation rate across subjects for both MC and NoMC images. A reduction in standard deviation with MC indicates improved measurement consistency.
Table 2: Impact of Motion Correction on Tau PET Quantitation (Sample Results)
| Brain Region | Reduction in Standard Deviation of Tau Accumulation Rate with Motion Correction |
|---|---|
| Entorhinal Cortex | -49% [33] |
| Inferior Temporal | -24% [33] |
| Precuneus | -18% [33] |
| Amygdala | -16% [33] |
Workflow Visualization
Generic Retrospective Motion Correction Workflow
List-Mode PET Motion Correction Workflow [33]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Retrospective Motion Correction Research
| Tool / Solution | Function | Example Use Case |
|---|---|---|
| FSL (FMRIB Software Library) | A comprehensive library of MRI and fMRI analysis tools. Includes MCFLIRT for motion estimation and FLIRT for image registration [38] [23] [35]. | Coregistering navigator images for motion parameter estimation [23]. |
| List-Mode Reconstruction Framework | Enables event-by-event motion correction by using ultra-fast reconstructions of short data frames for motion tracking [33]. | Correcting for both fast and slow head motion in long-duration PET studies [33] [36]. |
| 3D Radial Sampling | An MRI acquisition sequence where k-space is sampled along radiating spokes. More motion-robust than Cartesian sampling, causing blurring instead of ghosting [23]. | Used in MPnRAGE acquisitions to enable effective 3D motion estimation and correction [23]. |
| BIDS (Brain Imaging Data Structure) | A standard for organizing and describing neuroimaging data. | Simplifying data management and ensuring interoperability between different processing tools in large-scale studies [39]. |
| Containerized Pipelines (e.g., Docker/Apptainer) | Package processing software and its dependencies into a portable, reproducible environment [39]. | Ensuring consistent processing results across different computing systems and over time [39]. |
| IBMMA (Image-Based Meta- & Mega-Analysis) | A unified R/Python software package for analyzing large-scale, multi-site neuroimaging data [37]. | Handling missing voxel-data and complex statistical designs in aggregated datasets from multiple studies [37]. |
Troubleshooting Guides
FAQ: Data Quality and Preprocessing
My multi-modal dataset has fMRI data with different repetition times (TRs). Can I still use a unified framework?
Yes, this is a common challenge. Modern frameworks like BrainHarmonix are specifically designed to handle heterogeneous TRs. Their key innovation is a Temporal Adaptive Patch Embedding (TAPE) layer, which generates token representations with consistent temporal length regardless of the input TR. As a solution, you can also implement data augmentation by artificially downsampling high-resolution time series to create a hierarchy of TR levels, which improves model robustness [40].
How do I check if my motion correction was successful?
First, use visualization tools to inspect your data. Most software, like BrainVoyager, generates a motion correction movie that toggles between the first and last volume of a functional run before and after correction, allowing you to visually assess improvement [41]. You can also use the "Time Course Movie" tool to screen the functional time series for sudden intensity changes or residual movement across volumes [41]. Quantitatively, plot the estimated motion parameters (3 translations, 3 rotations) over time to identify any sudden motion spikes that might require additional processing [41].
A large portion of my volumes exceed the framewise displacement (FD) threshold. Should I censor them or use regression?
This is a critical decision that depends on your analysis goals and the extent of data loss.
- Censoring (Scrubbing): For task-based fMRI, one effective method is to "censor" high-motion time points by zeroing-out their entries in the design matrix and adding a single nuisance regressor for each censored time point (a stick regressor). This is recommended for significant motion artifacts that regression alone cannot fix [42].
- Regression: Including the motion parameters (e.g., 24-parameter model from Friston et al., 1996) as confounds in your General Linear Model (GLM) is a standard practice to mitigate motion-related variance [42].
- Best Practice: For the most rigorous approach, use both methods together. Motion correction (realignment) is the baseline. This should be followed by motion parameter regression in the GLM, and finally, censoring of volumes with extreme motion (e.g., FD > 0.5 mm) to prevent them from unduly influencing your results [42].
FAQ: Model Architecture and Integration
How can I architect a model to truly "unify" structure (sMRI) and function (fMRI) rather than just process them separately?
True unification requires an architecture that imposes neuroscientifically-grounded constraints. The Brain Harmony framework achieves this through a two-stage process:
- Unimodal Encoding: Train separate encoders for structure (e.g., a 3D Masked Autoencoder for T1 images) and function.
- Multimodal Fusion: Fuse the modality-specific representations using a set of shared, learnable "brain hub tokens." These tokens act as a representational bottleneck, explicitly trained to reconstruct both structural and functional latents, thereby creating a unified latent space. Crucially, the functional encoder incorporates a geometric pre-alignment step, using geometric harmonics derived from population-level cortical geometry to align functional dynamics with the underlying brain structure [40].
What fusion technique should I use for combining imaging and clinical data?
The choice of fusion technique depends on your model architecture and the nature of the data [43].
- Early Fusion: Combining raw or low-level features from different modalities before feeding them into the model. This can be powerful but is often challenging due to feature misalignment.
- Intermediate/Joint Fusion: Using architectures like Transformers or Graph Neural Networks (GNNs) to learn interactions between modalities within the model. Transformers use self-attention to weight the importance of different features [43], while GNNs can explicitly model clinical and imaging data as nodes in a non-Euclidean graph, preserving their natural relationships [43].
- Late Fusion: Training separate models for each modality and combining their final predictions. This is simpler but may fail to capture complex cross-modal interactions.
For cutting-edge applications, Graph Neural Networks (GNNs) are particularly promising for representing non-Euclidean relationships between heterogeneous data types, such as linking an imaging feature to a clinical parameter [43].
I encounter the error "Get rid of patches that are too close to edges" during motion correction. What does this mean?
This specific error, encountered in software like cryoSPARC, often occurs when using a patch-based motion correction method at extreme microscope magnifications. At very high magnifications, each patch may not contain enough signal for the algorithm to work reliably [44].
- Solution: The workaround is to switch from patch-based to full-frame motion correction, if the software allows it. If this option is not available in a real-time processing pipeline, you may need to adjust the "Override knots" parameter to a lower value to simplify the patch model [44].
My multimodal AI model requires extensive compute resources. Are there efficiency optimizations?
Yes, a key innovation is data compression into a compact representational space. Frameworks like BrainHarmonix deeply compress high-dimensional 3D volumes and 4D time series into unified, continuous-valued 1D tokens. This creates a highly compact latent space that significantly reduces the computational burden for downstream tasks while preserving critical information [40].
Experimental Protocols
Protocol 1: Implementing a Multi-Layer Motion Correction Pipeline for fMRI
This protocol details a robust, multi-stage approach to mitigate motion artifacts in fMRI data, combining real-time, retrospective, and regression-based techniques [42].
1. Real-Time Prospective Correction (During Acquisition):
- Objective: Minimize motion artifacts as data is collected.
- Method: Use internal navigators or an external tracking system (e.g., optical cameras) to monitor head position in real-time. The scanner's gradient and shim settings are updated for each volume to compensate for motion, ensuring optimal localization and B0 field homogeneity [12].
- Key Parameters: Tracking system precision (sub-millimeter and sub-degree), update rate (every TR).
2. Retrospective Volume Realignment (Post-Acquisition):
- Objective: Align all functional volumes to a common reference (e.g., the first volume).
- Method: Use a rigid-body transformation (6-parameters: 3 translations, 3 rotations) to realign each volume. Tools like FSL's MCFLIRT or SPM's realign are standard for this step [41] [42].
- Key Parameters: Interpolation method (e.g., trilinear, sinc). A trilinear/sinc combination is often recommended to balance accuracy and computation time [41].
3. Motion Parameter Regression (General Linear Model):
- Objective: Remove residual motion-related variance from the signal.
- Method: Include the 6 motion parameters (and their temporal derivatives, squares, etc., for a 24-parameter model) as nuisance regressors in your GLM to regress out any signal variance correlated with motion [42].
4. Motion Censoring (Scrubbing):
- Objective: Remove individual volumes that are severely contaminated by motion.
- Method: Calculate Framewise Displacement (FD) for each volume. Identify volumes exceeding a threshold (e.g., FD > 0.5 mm). For task-fMRI, censor these volumes by zeroing-out their entries in the design matrix and adding a single nuisance regressor for each censored time point [42].
Table 1: Key Metrics for Motion Quality Control
| Metric | Description | Recommended Threshold |
|---|---|---|
| Framewise Displacement (FD) | A scalar measure of volume-to-volume head movement [42]. | Task-fMRI: >0.5 mm; Rest-fMRI: Threshold may need adjustment for ultra-short TRs [42]. |
| DVARS | Measures the rate of change of BOLD signal across the entire brain at each time point [42]. | >1.5 standard deviations above the mean [42]. |
| Maximum Motion | The largest translation (mm) or rotation (degrees) relative to the reference volume [41]. | Study-specific; no universal threshold [41]. |
Protocol 2: Constructing a Unified Multi-Modal AI Framework
This protocol outlines the steps to create a foundation model that integrates structural MRI (sMRI) and functional MRI (fMRI) based on the Brain Harmony architecture [40].
1. Unimodal Encoding:
- Structural Encoder (BrainHarmonix-S):
- Input: 3D T1-weighted MRI volumes.
- Architecture: 3D Masked Autoencoder (MAE). The model is trained to reconstruct randomly masked patches of the input volume, learning a compressed structural representation [40].
- Functional Encoder (BrainHarmonix-F):
- Input: fMRI time series.
- Innovation 1 - Geometric Pre-alignment: Derive geometric harmonics from a population-level cortical surface mesh. Use these harmonics to create positional embeddings in the transformer, aligning functional dynamics with the brain's geometry [40].
- Innovation 2 - TAPE Layer: Use the Temporal Adaptive Patch Embedding (TAPE) layer to convert time series of any TR into tokens of a consistent length [40].
2. Multimodal Fusion:
- Input: Latent representations from the structural and functional encoders.
- Architecture: A set of shared, learnable "brain hub tokens." These tokens are trained via a pretext task that requires reconstructing both the structural and functional latents. This forces the hub tokens to form a unified latent space that captures information from both modalities [40].
3. Downstream Task Fine-Tuning:
- Objective: Adapt the pre-trained model for specific tasks like disorder classification or cognitive score prediction.
- Method: The unified model (or its extracted 1D token representations) can be fine-tuned with a smaller, labeled dataset for the target task [40].
Unified Multi-Modal Framework Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Components for a Multi-Modal AI Framework in Neuroimaging
| Item / Tool | Function / Rationale |
|---|---|
| Temporal Adaptive Patch Embedding (TAPE) | An embedding layer that allows a model to process fMRI time series with heterogeneous Repetition Times (TRs), enabling the integration of datasets from different scanners and protocols [40]. |
| Geometric Harmonics | Vibration patterns derived from cortical surface geometry. Used to create positional embeddings that pre-align functional data with structural constraints, incorporating the neuroscience principle "function follows structure" [40]. |
| Brain Hub Tokens | A set of learnable tokens that act as a representational bottleneck during multimodal fusion. They are trained to reconstruct both structural and functional latents, forcing the creation of a unified, compact latent space [40]. |
| Framewise Displacement (FD) & DVARS | Quantitative metrics for automated quality control. FD measures volume-to-volume head motion, while DVARS measures global BOLD signal change. Used to identify and censor motion-corrupted volumes [42]. |
| Graph Neural Networks (GNNs) | An architecture for fusing multimodal data (e.g., imaging, clinical, genetic) by representing them as nodes in a non-Euclidean graph. This explicitly models complex relationships without imposing artificial grid-like structures [43]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary differences between EDDY and IBMMA, and when should I use each tool?
EDDY and IBMMA are designed for different stages of the neuroimaging processing pipeline. EDDY is specialized for correcting eddy current-induced distortions and subject movement in diffusion MRI data [45] [46]. It uses a Gaussian Process model to predict what each diffusion-weighted image "should" look like based on other acquisitions and performs registration to align all volumes [46]. Use EDDY at the single-subject preprocessing stage for diffusion data.
IBMMA (Image-Based Meta- & Mega-Analysis) operates at a later stage, providing a unified framework for large-scale, multi-site statistical analysis of diverse neuroimaging features [37]. It handles challenges like missing voxel-data across sites and enables flexible statistical modeling. Use IBMMA for group-level analysis across multiple studies or sites.
Q2: My diffusion data was acquired on a half-sphere rather than a whole sphere. Can I still use EDDY effectively?
Yes, though optimal performance requires specific command-line parameters. EDDY works best with whole-sphere acquisition because the Gaussian Process prediction then serves as an undistorted target [46]. With half-sphere data, the average distortion for gradient components with non-zero means persists in the prediction. To address this, add the --slm=linear parameter to your EDDY command line [45] [46]. This specifies a linear spline model for better correction performance with suboptimal sampling schemes.
Q3: How does motion specifically affect different neuroimaging metrics in large-scale studies?
Motion artifacts have differential effects across various neuroimaging metrics, which is crucial for interpreting large-scale studies:
Table: Impact of Motion on Neuroimaging Metrics
| Neuroimaging Metric | Impact of Motion | Clinical Research Example |
|---|---|---|
| Cortical Thickness | Strong negative association; thinning observed with increased motion [2] | Effect sizes attenuated in bipolar disorder & schizophrenia when controlling for motion [2] |
| Grey/White Matter Contrast | Significantly affected [2] | More affected than volumetry in clinical populations [2] |
| Functional Connectivity | Introduces spurious correlations [2] | Motion correction improved ADHD subtype classification to 71-77% accuracy [2] |
| Diffusion Metrics (FA, MD) | Correlations with age weakened [2] | Reduced validity in developmental studies [2] |
Q4: What are the minimum data requirements for running EDDY on my diffusion dataset?
EDDY requires a minimum number of diffusion directions, which varies with b-value [45]:
- ~10-15 directions for b-value = 1500
- ~30-40 directions for b-value = 5000
These requirements ensure the Gaussian Process can reliably distinguish between signal variation caused by diffusion versus eddy currents/movements [45].
Troubleshooting Guides
Issue 1: Poor Correction Results with EDDY
Problem: EDDY corrections appear suboptimal, with residual distortions or misalignments.
Diagnosis Steps:
- Verify your acquisition scheme: Use the provided MATLAB code to visualize your diffusion directions [45] [46]: Check if your data spans the whole sphere (preferable) or only a half-sphere.
Check data quality: Ensure you have sufficient diffusion directions for your b-value [45].
Inspect for severe outliers: Use EDDY's
--repoloption to detect and replace outlier slices caused by extreme movement [45].
Solutions:
- For half-sphere data, use the
--slm=linearcommand-line option [45] [46]. - For data with limited directions (<30), consider if your dataset meets minimum requirements.
- Always include 2-3 b=0 volumes with opposing phase-encode (PE) directions for use with
topupto correct susceptibility distortions [45].
Issue 2: Handling Multi-Site Data with Missing Voxels in IBMMA
Problem: When pooling data across multiple sites for mega-analysis, some subjects have missing voxel-data, creating gaps in brain coverage and analysis failures.
Diagnosis Steps:
- Identify the extent and pattern of missing data across sites and cohorts.
- Determine if missingness is random or systematic (e.g., related to specific scanner protocols).
Solutions:
- Leverage IBMMA's built-in capabilities: IBMMA is specifically designed to handle missing voxel-data common in multi-site studies [37].
- Ensure proper preprocessing alignment: Verify all input images are in a standard space.
- Use IBMMA's parallel processing: For large datasets, utilize IBMMA's efficient parallel processing to manage computational load [37].
Issue 3: Managing Motion Artifacts in Clinical Populations
Problem: Clinical populations (e.g., children, patients with neurological disorders) often exhibit more motion, leading to higher exclusion rates and potential bias.
Diagnosis Steps:
- Quantify motion parameters for each group (patients vs. controls).
- Check for correlations between motion and clinical variables of interest.
- Assess the impact of different quality control (QC) stringency levels on your results.
Solutions:
- Implement prospective correction: Use real-time motion monitoring and correction systems like MoCAP, which uses structured light for prospective correction by adjusting MR gradients [47].
- Apply consistent QC thresholds: Establish and apply motion exclusion criteria consistently across all groups before analysis [2].
- Include motion as a covariate: In statistical models, include motion parameters as regressors to account for residual effects [2].
- Consider advanced correction methods: Explore deep learning-based approaches like Motion-Adaptive Diffusion Models (MADM) for severe artifacts [48].
Experimental Protocols & Workflows
Protocol 1: Optimal Diffusion Data Acquisition for EDDY
For researchers planning new data acquisition, this protocol maximizes EDDY's performance [45]:
| Acquisition Parameter | Recommendation for EDDY | Rationale |
|---|---|---|
| Total Volumes (N) | N < 80: Acquire N unique directions on whole sphere.N > 120: Acquire N/2 unique directions, each with two opposing PE-directions. | Balances angular sampling with correction efficacy via opposing PE directions [45]. |
| Diffusion Sampling | Whole sphere (not half-sphere) | Ensures Gaussian Process prediction is in undistorted space [46]. |
| b=0 Volumes | 2-3 with opposing PE-direction prior to DWI; intersperse additional b=0 (e.g., 1/16 volumes) | Enables topup susceptibility correction; provides baseline reference [45]. |
| Phase Encoding (PE) | For N > 120, use split opposing PE-directions (e.g., A->P and P->A) | Enables "least-squares reconstruction" to recover lost resolution [45]. |
Protocol 2: Implementing a Motion-Robust Large-Scale Analysis
This workflow integrates EDDY and IBMMA for a comprehensive multi-site study:
Key Steps:
- Standardized Acquisition: Implement consistent protocols across sites, including opposing PE b=0 volumes.
- Single-Subject Preprocessing: Correct each subject's diffusion data with EDDY [45] [46].
- Feature Extraction: Derise relevant metrics (e.g., FA, MD, cortical thickness, functional connectivity).
- Quality Control: Apply consistent motion-related exclusion criteria to all groups [2].
- IBMMA Mega-Analysis: Pool cleaned data across sites using IBMMA's parallel processing and missing data handling [37].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Software Tools for Motion Correction in Large-Scale Studies
| Tool / Resource | Function / Purpose | Application Context |
|---|---|---|
| FSL EDDY | Corrects eddy current distortions & subject movement in diffusion MRI | Single-subject DWI preprocessing [45] [46] |
| IBMMA | Performs image-based meta- and mega-analysis of large, multi-site datasets | Group-level statistical analysis [37] |
| MCFLIRT | Performs rigid-body motion correction for functional time-series data | fMRI preprocessing [49] |
| topup | Estimates and corrects susceptibility-induced off-resonance fields | Used alongside EDDY with opposing PE b=0 volumes [45] |
| MoCAP | Prospective motion correction using structured light tracking | Real-time motion compensation during scanning [47] |
| MADM | Corrects severe motion artifacts using Motion-Adaptive Diffusion Model | Deep learning-based correction for challenging cases [48] |
Optimizing Study Design and Pipeline Robustness for Real-World Data
In the realm of large-scale neuroimaging studies, particularly those investigating brain-wide associations (BWAS), researchers face a fundamental and costly dilemma: whether to prioritize the number of participants (sample size, N) or the amount of data collected per participant (scan time per participant, T). This trade-off is intensified by practical constraints, including limited funding, scanner availability, and participant pools, especially in rare populations. Furthermore, within the specific context of motion correction research, this decision directly influences data quality and the effectiveness of subsequent artifact correction algorithms. Underpowered studies lead to low reproducibility and inflated performance estimates, while insufficient scan time yields unreliable data that can corrupt even the most advanced motion correction techniques. This guide provides a cost-benefit framework to navigate this trade-off, ensuring that study designs are optimized for both scientific rigor and fiscal responsibility.
Key Concepts and Quantitative Evidence
The Interchangeability Principle and Its Limits
Empirical evidence reveals a foundational principle: for scan times up to approximately 20 minutes, sample size and scan time are broadly interchangeable in their contribution to phenotypic prediction accuracy. Prediction accuracy increases with the total scan duration, calculated as Sample Size (N) × Scan Time per Participant (T) [50] [4].
However, this interchangeability has limits. Beyond 20-30 minutes of scan time, diminishing returns become evident, where each additional minute of scanning provides a progressively smaller gain in accuracy compared to increasing the sample size by one participant [50] [4]. Consequently, while you can trade one for the other in the short term, sample size ultimately becomes more critical for achieving high prediction power.
Cost-Benefit Analysis and Optimal Scan Time
When the substantial overhead costs per participant (e.g., recruitment, screening) are factored in, the strategy of using longer scans can yield significant cost savings compared to only increasing the sample size.
Table 1: Cost-Benefit Analysis of Scan Time Choices
| Scan Time | Relative Cost Efficiency | Key Rationale and Evidence |
|---|---|---|
| 10 minutes | Highly Cost Inefficient | Provides insufficient data for reliable prediction, offering poor value for the invested resources [50] [4]. |
| 20 minutes | Viable Minimum | Sits at the lower bound of the recommended range for most scenarios to achieve acceptable reliability [50] [4]. |
| 30 minutes | Most Cost-Effective | On average, yields 22% cost savings over 10-minute scans; represents the optimal balance of data quality and cost [50] [4]. |
| >30 minutes | Cheaper to Overshoot | While subject to diminishing returns, overshooting the optimal scan time is financially cheaper than undershooting it [50]. |
The following diagram illustrates the logical workflow for determining your study's scan time and sample size based on your research goals and constraints.
Diagram 1: Logic Flow for Optimizing Scan Time and Sample Size.
Impact on Data Reliability and Motion Correction
The scan time and sample size decisions have a direct impact on the reliability of your data, which is a prerequisite for successful motion correction.
Table 2: Effect on Reliability and Motion-Related Considerations
| Factor | Effect on Reliability & Motion Correction | Key Evidence |
|---|---|---|
| Scan Duration | >10.8 minutes: Yields good reliability in Effective Connectivity (DCM analysis). Longer scans improve the signal-to-noise ratio, providing a more stable baseline for motion detection and correction algorithms [51]. | [51] |
| Sample Size | >40-70 subjects: Yields good reliability in Effective Connectivity (DCM analysis). Larger samples provide greater statistical power to distinguish true biological effects from motion-induced artifacts [51]. | [51] |
| Motion Artifacts | Motion causes ghosting, blurring, and signal loss. Retrospective correction (e.g., deep learning models) can significantly improve image quality and cortical surface reconstructions, salvaging data that would otherwise fail quality control [52]. | [10] [52] |
Experimental Protocols & Methodologies
Protocol: Establishing a Prediction Accuracy Curve
This protocol allows you to empirically determine the relationship between scan time, sample size, and prediction accuracy for your specific dataset and phenotype of interest, directly informing the trade-off.
- Step 1 - Data Preparation: For each participant in a large dataset (e.g., HCP, ABCD), calculate your primary imaging feature (e.g., a 419x419 Resting-State Functional Connectivity matrix) [50] [4].
- Step 2 - Variable Manipulation: Systematically vary the amount of data used per participant. For example, use only the first T minutes of fMRI data, varying T from 2 minutes up to the maximum available scan time in intervals of 2 minutes [50] [4].
- Step 3 - Prediction Modeling: Use the features from Step 2 as input to a prediction model (e.g., Kernel Ridge Regression). Repeat the analysis across different training sample sizes (N) using a nested cross-validation procedure to ensure comparability of prediction accuracy across different N and T [50] [4].
- Step 4 - Analysis and Modeling: Plot prediction accuracy against total scan duration (N × T). For scans ≤20 minutes, a logarithmic curve can often be fitted, explaining a high proportion of variance in accuracy (R² ~ 0.89) [50] [4].
Protocol: Cost-Effectiveness Calculation for Study Design
This methodology integrates economic evaluation into the neuroimaging study design process, following established frameworks for cost-effectiveness analysis in diagnostic imaging [53].
- Step 1 - Define the Decision Problem: State the research question, perspective (e.g., institutional, funder), comparators (e.g., 10-min vs. 30-min scan protocols), and relevant outcomes (e.g., prediction accuracy gain per dollar) [53].
- Step 2 - Develop a Decision Model: Create a model (e.g., a decision tree) that maps out the pathways and consequences of each scanning strategy. Key inputs include [50] [53]:
- Fixed overhead cost per participant (Coh): Recruitment, screening, consent.
- Variable cost per scan minute (Cscan): Scanner time, technician.
- Total Scan Duration (D): N × T.
- Prediction Accuracy [r], derived from your model in Protocol 3.1.
- Step 3 - Select Input Parameters and Calculate: Populate the model with your cost and accuracy data. The total cost for a study design is:
Total Cost = N * (C_oh + T * C_scan). Compare the incremental cost per unit of prediction accuracy gained between different (N, T) pairs [50] [53]. - Step 4 - Analyze Uncertainty: Perform sensitivity analyses to test how robust your conclusion is to changes in key assumptions (e.g., varying the overhead cost C_oh) [53].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for fMRI Study Design and Analysis
| Tool / Resource | Function in the Trade-Off Analysis | Key Details |
|---|---|---|
| Large-Scale Datasets | Provide the empirical data required to model the effects of N and T. | Datasets like HCP (57m scan time) and ABCD (20m scan time) are critical as they contain long scan times per participant, allowing for the simulation of shorter durations [50] [4]. |
| Online Calculator | Allows for interactive exploration of the trade-off based on local costs. | An empirically informed web application is available to help plan future studies by calculating optimal scan times given specific constraints [50]. |
| Kernel Ridge Regression | A machine learning algorithm used to measure the ultimate output of the study: individual-level phenotypic prediction accuracy. | Serves as a standard tool for evaluating how well brain imaging features predict behavioral or cognitive scores across different values of N and T [50] [4]. |
| Dynamic Causal Modeling | An advanced brain connectivity technique that can achieve good reliability with viable scan times and sample sizes. | DCM for Effective Connectivity analysis can yield good reliability with scan times >10.8 minutes and sample sizes >40 subjects, offering a potential solution when resources are limited [51]. |
| Retrospective Motion Correction | A deep learning tool to salvage data with motion artifacts, mitigating the data quality cost of opting for shorter scans. | A 3D CNN model trained on motion-simulated data can significantly improve image quality metrics and cortical surface reconstruction quality in real-world datasets with motion [52]. |
Frequently Asked Questions (FAQs)
Q1: My primary focus is task-fMRI, not resting-state. Is the optimal scan time shorter or longer? The most cost-effective scan time is generally shorter for task-fMRI compared to resting-state whole-brain BWAS. This is likely because task paradigms can evoke more robust and efficient brain responses in specific circuits per unit time [50] [4].
Q2: I am studying a rare patient population where large sample sizes are impossible. What should I do? When sample size (N) is severely limited, your best strategy is to maximize scan time (T) per participant. The interchangeability principle shows that longer scans can partially compensate for a smaller N. Furthermore, employing advanced analytical techniques like Dynamic Causal Modeling (DCM) may achieve acceptable reliability with more moderate sample sizes (e.g., N > 40) [51].
Q3: How does participant motion factor into this cost-benefit analysis? Motion is a critical hidden cost. While longer scans have a higher probability of including motion events, they also provide more clean data after censoring (removing high-motion frames). Furthermore, investing in prospective motion correction (real-time tracking and sequence adjustment) or advanced retrospective correction (deep learning models) can protect your investment in longer scan times by ensuring data quality [10] [52]. The cost of these techniques should be weighed against the cost of losing a participant's data entirely.
Q4: Our research group has a fixed budget for scanner hours. Should we scan more people for less time or fewer people for longer? With a fixed scanner-hour budget, the decision hinges on your overhead cost per participant (Coh). If Coh is low, scanning more people for less time (e.g., 15-20 minutes) is often beneficial. However, if C_oh is high (e.g., recruiting a rare population), you will likely find greater cost-efficiency in allocating more scanner time to fewer participants, aiming for ≥30-minute scans to maximize data yield per recruited individual [50].
Q5: Are there specific phenotypes where this trade-off is less important? The logarithmic relationship between total scan duration and prediction accuracy holds across a wide range of 76 phenotypes, including cognitive, emotional, and health measures. However, the strength of the relationship varies. Phenotypes that are more strongly encoded in brain function will show a steeper improvement with increasing N and T, making the trade-off more critical to optimize. For phenotypes weakly tied to brain function, achieving high prediction accuracy may be difficult regardless of design [50] [4].
Frequently Asked Questions (FAQs)
1. What causes missing voxel data in multi-site fMRI studies? Missing data in multi-site fMRI studies primarily results from two sources: acquisition limits and susceptibility artifacts. Acquisition limits occur when the image bounding box does not cover the entire brain, particularly in subjects with larger heads. Susceptibility artifacts cause signal loss and spatial distortion due to disruptions in the magnetic field, especially near tissue boundaries and air-filled cavities like sinuses. Furthermore, in multi-site studies, differences in scanner manufacturers, acquisition protocols, and hardware across sites introduce additional site-effect biases that can manifest as structured missingness or noisy data [54] [55] [56].
2. Why is simply omitting voxels with missing data a problematic approach? Omitting voxels from group analyses, a method known as available case analysis or listwise deletion, is problematic for several reasons. It can lead to:
- Increased Type II Errors (False Negatives): Excluding brain regions of theoretical or clinical interest reduces statistical power.
- Biased Inference: If the missing data is not Missing Completely at Random (MCAR), analyzing only the available data can bias effect size estimates.
- Increased Type I Errors (False Positives): When spatial extent thresholds are used, a smaller analysis space requires a smaller cluster size to reach significance, potentially identifying false clusters.
- Reduced Coverage: One study demonstrated that voxel omission reduced brain coverage by 35% compared to imputation methods [54] [56].
3. What are the different types of missing data mechanisms in fMRI?
- Missing Completely at Random (MCAR): The cause of missingness is unrelated to the data. Example: random variations in image acquisition or field inhomogeneities across subjects.
- Missing at Random (MAR): The probability of missingness depends on observed data but not the unobserved data. Example: a subject's head size (observed) predicts whether a voxel falls outside the acquisition box.
- Missing Not at Random (MNAR): The probability of missingness depends on the unobserved data itself. Example: systematic signal loss in regions affected by head motion during a speech task, where the motion is tied to the experimental condition [54] [56].
4. What advanced statistical methods can handle missing fMRI data? Several sophisticated methods are recommended over voxel omission:
- Multiple Imputation (MI): A "filling in" method that creates multiple plausible versions of the dataset by drawing values from the distribution of the observed data. It accounts for uncertainty and provides valid standard errors. It is particularly effective for data that are MCAR or MAR [57] [56].
- Full Information Maximum Likelihood (FIML): This method uses all available data to estimate model parameters without imputing values, making it efficient for longitudinal data analysis [57].
- Harmonization Methods (e.g., ComBat, ICA-DP): For multi-site data, these methods remove unwanted site effects, which are a major source of structured noise. The dual-projection ICA (ICA-DP) method has been shown to effectively separate and remove site-related effects while preserving biological signals of interest [55].
Troubleshooting Guides
Issue: Widespread Missing Data Compromising Whole-Brain Analysis
Problem: Your group-level analysis has excluded large portions of the brain due to missing voxels in a subset of subjects, limiting the interpretability of your results.
Solution: Implement a Multiple Imputation workflow.
Experimental Protocol:
- Identify Missingness Pattern: Determine if the missing data is MCAR, MAR, or MNAR by examining covariates like head size, motion parameters, and site scanner.
- Choose Predictors: Select variables to inform the imputation. These should include:
- Spatial Neighbors: The values from adjacent voxels are highly correlated.
- Subject Covariates: Head motion parameters, intracranial volume, age, sex.
- Experimental Conditions: Task regressors or group membership.
- Perform Imputation: Use a software package (e.g., R, Python) to create multiple (e.g., M=20-50) imputed datasets. For each missing voxel, a value is drawn from a predictive distribution based on the selected predictors.
- Analyze Imputed Datasets: Run your standard group-level analysis (e.g., GLM) separately on each of the M completed datasets.
- Pool Results: Combine the parameter estimates (e.g., beta weights, t-statistics) and their variances from the M analyses using Rubin's rules, which average the estimates and combine within- and between-imputation uncertainty [56].
Workflow for handling missing data with Multiple Imputation.
Issue: Site-Related Biases in Multi-Site Data
Problem: Your pooled data from multiple scanners shows strong site effects that are confounded with your effects of interest, such as group differences (e.g., patients vs. controls).
Solution: Apply a data harmonization method like the Dual-Projection based Independent Component Analysis (ICA-DP).
Experimental Protocol:
- Data Preprocessing: Standard preprocessing (motion correction, normalization, etc.) and calculation of functional modalities like Amplitude of Low-Frequency Fluctuation (ALFF) or Regional Homogeneity (ReHo).
- ICA Decomposition: Use ICA to decompose the multi-site data into a set of independent spatial components and their subject-wise courses.
- Component Classification: Classify each component as a signal component (correlated with age, sex, diagnosis), a noise component (correlated only with site), or a mixed component.
- Dual-Projection (DP):
- First Projection: For mixed components, separate the signal-related part from the site-related part using a linear projection.
- Second Projection: Create a final denoised dataset by projecting out all identified site-related components (both pure noise and the noise parts of mixed components) [55].
- Validation: Compare the harmonized data to ensure site effects are minimized while associations with non-imaging variables (e.g., age) are preserved.
Workflow for mitigating site-effects in multi-site studies using ICA-DP.
Table 1: Comparison of Missing Data Handling Methods for Group-Level fMRI Analysis
| Method | Key Principle | Best for Data Type | Advantages | Limitations |
|---|---|---|---|---|
| Voxel Omission (Listwise Deletion) | Removes any voxel missing in any subject. | MCAR (and even then, not ideal) | Simple to implement. | >35% reduced brain coverage [56]; High risk of Type I/II errors; Biased estimates if not MCAR [54] [57]. |
| Multiple Imputation (MI) | Fills in missing values with multiple plausible estimates. | MCAR, MAR | Increased coverage & power; Accounts for imputation uncertainty; Robust for small samples/high missingness [56]. | Computationally intensive; Requires careful model specification. |
| Full Information Maximum Likelihood (FIML) | Estimates model parameters using all available data points. | MCAR, MAR | Does not require imputation; Efficient for complex models (e.g., longitudinal) [57]. | Implementation can be model-specific; Less common for voxel-wise maps. |
| Harmonization (ICA-DP) | Removes site-specific biases from multi-site data. | Structured noise (Site effects) | Increases significance of true brain-behaviour relationships; Superior denoising vs. traditional ICA/ComBat [55]. | Primarily targets site noise, not general missingness. |
Table 2: Performance Outcomes of Different Methods from Empirical Studies
| Study / Method | Reported Outcome Metric | Result |
|---|---|---|
| Multiple Imputation [56] | Brain Coverage vs. Voxel Omission | +35% increase (from 33,323 to 45,071 voxels) |
| Multiple Imputation [56] | Significant Clusters vs. Voxel Omission | +58% increase in the size of significant clusters |
| ICA-DP Harmonization [55] | Association Strength (e.g., with age) | Increased significance of associations after site-effect removal |
The Scientist's Toolkit: Essential Research Reagents & Software
Table 3: Key Software Tools for Handling Missing and Multi-Site Data
| Tool / Resource | Function | Use Case |
|---|---|---|
| FSL (FEAT) | fMRI data preprocessing, including motion correction and spatial normalization. | Standard preprocessing pipeline before tackling missing data [55]. |
| DPABI | Toolbox for calculating functional modalities like ALFF and ReHo. | Generating derived maps for subsequent harmonization or analysis [55]. |
| R/Python Packages (e.g., mice in R) | Implementation of Multiple Imputation. | Creating and analyzing multiply imputed datasets [57] [56]. |
| ComBat | GLM-based harmonization using empirical Bayes. | Removing batch effects (site effects) from multi-site data [55]. |
| ICA-DP Code | Custom code for dual-projection ICA. | Advanced denoising and harmonization of multi-site data, preserving signals of interest [55]. |
| SAMON R Package | Sensitivity analysis for MNAR data. | Assessing the robustness of findings when data is suspected to be Missing Not at Random [54]. |
Core Concepts in Motion Correction
What are the fundamental types of motion correction in neuroimaging? Motion correction strategies can be broadly classified into two categories: prospective and retrospective. Prospective Motion Correction (PMC) performs real-time adaptive updates to the data acquisition based on detected head motion, preventing motion from occurring in the first place [10] [12]. Retrospective Motion Correction (RMC) applies algorithms to the already-acquired image data during the reconstruction process to minimize motion artifacts [58] [10]. The choice between these approaches depends on your study's goals, technical capabilities, and participant population.
How does motion degrade image quality and quantification? Head motion introduces complex artifacts that can compromise data integrity. For anatomical MRI, motion causes blurring, ghosting, and reduced boundary detail, which directly impacts the reliability of morphometric measurements like cortical thickness [58] [59]. In functional MRI (fMRI), even sub-millimeter motions can distort functional connectivity estimates, causing both false positives and false negatives in activation maps [60] [61]. For Magnetic Resonance Spectroscopy (MRS), motion degrades both localization and spectral quality by disrupting B0 field homogeneity, leading to inaccurate metabolite quantification [12].
Table: Motion Artifacts Across Neuroimaging Modalities
| Imaging Modality | Primary Motion Effects | Impact on Data Analysis |
|---|---|---|
| High-Resolution T1w (MPRAGE) | Blurring, reduced gray/white matter contrast [58] | Decreased reliability of volume and cortical thickness measures [59] |
| Resting-State fMRI | Altered correlation estimates (increased short-distance, decreased long-distance) [60] | False connectivity patterns; group differences confounded by motion [60] |
| MRS | Voxel displacement, line broadening, poor water suppression [12] | Inaccurate metabolite quantification (5-15% variability for primary metabolites) [12] |
| Ultra-High Resolution fMRI | Spurious activation at brain edges, false positives/negatives [61] | Compromised statistical maps after retrospective correction [61] |
Protocol Selection Guidelines
Which motion correction protocol should I choose for my participant population? Your participant population is the primary determinant in selecting an appropriate motion correction strategy.
Pediatric, Elderly, or Hyperkinetic Populations (ADHD, Movement Disorders): Implement Prospective Motion Correction (PMC) whenever available. Studies show MPRAGE+PMC sequences provide significantly higher intra-sequence reliability for morphometric measurements in participants with higher head motion [59]. PMC is also strongly recommended for MRS studies in children and patients with movement disorders to maintain consistent voxel placement and B0 shimming [12].
Adult Healthy Volunteers (Low Motion): Standard MPRAGE sequences with retrospective correction may be sufficient and yield better results on some quality control metrics [59]. For fMRI, combining RMC with motion parameters as nuisance regressors in the general linear model is a common and effective approach [60].
Ultra-High Field Studies (7T+): Consider hybrid approaches that combine PMC with retrospective methods. One effective protocol uses real-time multislice-to-volume motion correction integrated with slice-specific B1+ shimming, which has been shown to reduce motion, increase brain activation, and improve temporal SNR in 7T fMRI [16].
How do I match correction techniques to specific research goals? The analytical goals of your study should guide your technical choices.
Structural Morphometry (Cortical Thickness, Volume): Protocols with embedded PMC (e.g., MPRAGE+PMC) provide higher measurement reliability, which is critical for longitudinal studies or clinical trials detecting subtle change [59].
Functional Connectivity (rs-fMRI): Employ a multi-step retrospective pipeline including volume realignment, motion parameter regression, and identification of motion-contaminated volumes ("scrubbing") [60]. Be aware that in ultra-high resolution fMRI, standard RMC can introduce false activation near brain edges; using external motion tracking (e.g., optical systems) for validation is recommended [61].
Metabolite Quantification (MRS): Prospective correction with real-time B0 shim updating is essential for reliable measurement of low-concentration metabolites like GABA and glutathione. This combined correction for both localization and B0 field changes is necessary to achieve the <5% variability required for clinical applications [12].
Multimodal PET/MR Studies: For simultaneous acquisitions, implement tracer characteristic-based co-registration (TCBC) methods that leverage specific PET uptake patterns to improve MR-to-PET alignment and quantification accuracy [62].
Table: Technical Specifications for Motion Correction Performance
| Correction Method | Spatial Precision | Temporal Resolution | Key Advantages | Implementation Challenges |
|---|---|---|---|---|
| Optical Tracking (PMC) | <0.1 mm, <0.1° [61] | Up to 80 Hz [61] | Gold standard precision; corrects intra-scan motion [12] | Requires camera setup & cross-calibration [61] |
| Navigator-Based (PMC) | Sub-mm & sub-degree [12] | Every TR (~seconds) [12] | No external hardware; integrated with sequence | Prolongs scan time; contrast-dependent [63] |
| Image-Based (RMC) | Voxel-scale (0.6-2 mm) [61] | Post-acquisition | Universally available; no sequence modification | Cannot correct spin history effects [10] |
| Pilot Tone + Hybrid | High (with calibration) [63] | Continuous (kHz) [63] | No FOV limitations; enables PT model calibration | Subject-specific calibration required [63] |
Troubleshooting Common Problems
Why do I still see motion artifacts after applying retrospective correction? Residual artifacts after RMC typically occur because these methods cannot fully address all motion-related effects. RMC corrects for spatial misalignment but doesn't fix spin history effects (saturation changes from previous excitations) or B0 field inhomogeneity changes induced by motion [10] [12]. For MRS, this is particularly problematic as motion disrupts the carefully optimized B0 shim, broadening spectral lines [12]. Solution: For critical applications, implement prospective correction or hybrid methods that combine PMC with RMC to address residual latency-induced errors [16].
How can I handle intermittent, large motion spikes in fMRI? For large, transient motions, standard volume realignment is insufficient. Implement a multi-faceted approach: (1) Identify corrupted volumes using framewise displacement (FD) and DVARS metrics; (2) Implement "scrubbing" (removal) of motion-contaminated volumes; (3) Use motion parameters as nuisance regressors in statistical models [60]. Be cautious with scrubbing as it creates temporal gaps in data; consider interpolation techniques for minor contamination.
My motion-corrected ultra-high resolution fMRI shows suspicious edge activation. What's wrong? This indicates a retrospective correction artifact common in high-resolution fMRI with limited brain coverage. Image-based motion detection algorithms can misclassify stimulus-related brain activity as motion in regions with strong intensity gradients (e.g., brain edges) [61]. Solution: (1) Use external motion tracking (e.g., optical systems) for validation; (2) Ensure adequate brain coverage in acquisition; (3) For critical studies, employ prospective motion correction which doesn't suffer from this confound [61].
Implementation and Workflows
Motion Correction Protocol Selection
The Researcher's Toolkit
Essential Research Reagents and Solutions
Table: Key Motion Correction Technologies and Their Applications
| Tool/Technology | Function | Example Applications | Implementation Notes |
|---|---|---|---|
| Optical Motion Tracking (e.g., MPT) | External camera-based head pose tracking [61] | Prospective correction for fMRI, MRS; gold standard validation [12] [61] | Requires cross-calibration; high precision (<0.1mm) [61] |
| FID Navigators | Embedded sequence elements for motion detection [16] | Automated image quality prediction; motion detection without time penalty [16] | Deep learning models can predict diagnostic quality from FIDnav signals [16] |
| Pilot Tone Technology | RF signal for continuous motion sensing [63] | High temporal resolution motion tracking; hybrid approaches [63] | Requires subject-specific calibration; works with any sequence [63] |
| FLASH Scout + Guidance Lines | Rapid pre-scan and embedded k-space lines [16] | Retrospective motion correction for 2D TSE (T1w, T2w, FLAIR) [16] | Enables shot-by-shot motion estimation; contrast-matched [16] |
| Subspace-Based Self-Navigation | 3D navigators from acquired data itself [16] | Motion correction for ASL angiography/perfusion; radial imaging [16] | Accounts for varying contrast; no separate navigator acquisition needed [16] |
Retrospective fMRI Motion Correction Pipeline
FAQ: Addressing Common Researcher Questions
Should I exclude high-motion participants from my analysis? Exclusion should be a last resort, as it can introduce selection bias—particularly in clinical populations where motion may be correlated with the condition of interest [60]. Instead, implement robust motion correction protocols specifically designed for high-motion populations, and always include motion metrics as covariates in group-level analyses [60] [59].
Can I use frequency filtering to remove motion artifacts from fMRI? No, motion artifacts do not display band-limited frequency content and often contain low-frequency, autocorrelated trends that overlap with the typical resting-state frequency band (0.01-0.1 Hz) [60]. Frequency filtering alone is ineffective and may even smear motion contamination throughout your dataset.
What motion thresholds should I use for data quality control? For standard resolution fMRI (2-3mm voxels), common thresholds are <1mm translation and <1° rotation in any direction [61]. However, for ultra-high resolution fMRI (<1mm voxels), these thresholds may be insufficient. Base your quality criteria on voxel dimensions—smaller voxels require stricter motion control.
Is prospective motion correction worth the implementation effort? Yes, for studies involving challenging populations or requiring high measurement precision. PMC provides significant advantages: it prevents motion rather than correcting it, maintains consistent voxel placement throughout longer acquisitions, and enables compatibility with techniques that require stable head position like localized shimming for MRS [12] [59].
This guide provides technical support for researchers establishing quality control pipelines in large-scale neuroimaging studies.
Frequently Asked Questions
What are the practical consequences of not setting adequate motion tolerances? Without strict tolerances, motion artifacts introduce systematic bias, not just random noise. Analyses will consistently underestimate cortical thickness and overestimate cortical surface area. In large datasets like the ABCD Study, incorporating moderate-to-poor quality scans more than doubled the number of brain regions showing statistically significant group differences in some analyses, dangerously inflating effect sizes and increasing false discoveries [64].
My large dataset has already been collected. How can I manage motion artifacts? For existing data, implement robust retrospective correction and quality metrics. Use automated metrics like Surface Hole Number (SHN) to flag low-quality scans. For analysis, "stress-test" your findings by analyzing how effect sizes change as you systematically include or exclude scans based on quality ratings [64]. For PET/MR data, consider advanced co-registration methods like Tracer Characteristic-Based Co-registration (TCBC) that leverage specific uptake patterns to improve alignment [62].
We are designing a new large-scale study. What proactive measures should we implement? Implement prospective motion correction (PMC) where possible, using real-time head tracking to update data acquisition [10]. However, be aware that PMC can have latency issues, especially with periodic motion like breathing; a hybrid approach combining PMC with retrospective correction may be optimal [16]. For structural MRI, consider sequences like MPnRAGE that are inherently more robust to motion and can correct artifacts without reducing quality in motion-free scans [1].
Quantitative Motion Metrics and Tolerances
Table 1: Quality Rating Scale for Structural MRI Scans (Manual Rating)
| Quality Rating | Description | Impact on Analysis | Recommended Action |
|---|---|---|---|
| 1 (High) | Minimal manual correction needed [64] | Minimal bias [64] | Include in analysis |
| 2 (Moderate) | Moderate manual correction needed [64] | Introduces measurable bias; inflates effect sizes [64] | Use with caution; stress-test findings |
| 3 (Low) | Substantial manual correction needed [64] | Significant bias [64] | Consider excluding |
| 4 (Unusable) | Unusable data [64] | Severe bias [64] | Exclude from analysis |
Table 2: Automated Quality Metrics for Large-Scale Datasets
| Metric | Description | Performance | Practical Application |
|---|---|---|---|
| Surface Hole Number (SHN) | Estimates number of holes in cortical reconstruction [64] | Best automated proxy for manual ratings [64] | Use as covariate; to stratify data in sensitivity analyses [64] |
| 6 Rigid-Body Parameters | Translation (x,y,z) and rotation (pitch, roll, yaw) from motion correction [65] | Standard output from realignment software (e.g., BrainVoyager) [65] | Calculate Framewise Displacement; set threshold (e.g., > 0.5mm) to flag high-motion volumes |
| FID Navigators | Embedded navigator signals from free induction decay [16] | Can predict diagnostic image quality with high AUC (0.90) [16] | Enable real-time quality assessment and potential scan termination [16] |
Table 3: Motion Tolerance Guidelines by Imaging Modality
| Modality | Primary Motion Type | Common Correction Strategies | Tolerance Guidance |
|---|---|---|---|
| fMRI / sMRI | Rigid-body head motion [10] | Prospective tracking, retrospective realignment [10] [65] | Reject datasets with >1-2 voxels displacement [65]. Use manual or SHN quality control [64]. |
| Simultaneous PET/MR | Involuntary head motion causing PET-MR misalignment [62] | Tracer-specific co-registration (e.g., TCBC), Mutual Information methods [62] | Correct misalignment to improve PET quantification; TCBC outperforms MI-based methods in simulation [62]. |
| Whole-Body PET | Non-rigid motion (respiration, cardiac) [66] | Hardware-driven (sensors) and data-driven (from PET data) gating [66] | Implement gating to correct for respiratory & cardiac motion; crucial for accurate kinetic modeling [66]. |
The Scientist's Toolkit
Table 4: Essential Software and Analytical Reagents
| Tool / Reagent | Function | Application Context |
|---|---|---|
| IBMMA Software | Provides unified framework for meta- and mega-analysis of large-scale datasets; handles missing voxel-data [37] | Large-n, multi-site neuroimaging studies [37] |
| Surface Hole Number (SHN) | Automated quality metric for cortical reconstructions [64] | Proxy for manual quality rating in large datasets where manual inspection is impractical [64] |
| Tracer Characteristic-Based Co-registration (TCBC) | PET-to-MR co-registration using known tracer uptake patterns [62] | Simultaneous PET/MR studies, particularly for amyloid imaging [62] |
| MPnRAGE Sequence | Structural MRI sequence resistant to motion artifacts [1] | Acquiring high-quality T1-weighted images in populations prone to movement [1] |
| FID Navigators | Embedded signals for non-invasive motion tracking [16] | Predicting final image quality during acquisition; enabling real-time decisions [16] |
Experimental Protocols
Protocol 1: Implementing a Quality Control Pipeline for a Large Existing Dataset
- Data Extraction and Preprocessing: Extract preprocessed scans and corresponding quality metrics (e.g., motion parameters, SHN values) from your database or standardized pipeline (e.g., ABCD Study pipeline) [64].
- Automated Quality Screening: Calculate Framewise Displacement from 6 rigid-body parameters [65]. Use SHN or similar automated metrics to flag potentially low-quality scans [64].
- Manual Quality Rating (Sub-sample): If feasible, perform manual quality rating on a random sub-sample (e.g., 500-1000 scans) using a 4-point scale (1=high, 4=unusable) [64]. This validates your automated metrics.
- Stratified Analysis ("Stress-Testing"): Conduct your primary analysis on only the highest-quality scans (Rating 1). Then, incrementally add back lower-quality scans (e.g., add Rating 2, then Rating 3) and re-run the analysis.
- Result Interpretation: Observe how effect sizes and the number of significant findings change with the inclusion of lower-quality data. True effects will have stable effect sizes, while biased effects will inflate [64].
Protocol 2: Motion-Resistant Data Acquisition for Structural MRI
- Sequence Selection: Employ a motion-resistant acquisition sequence such as MPnRAGE [1].
- Parameter Configuration: Set up the sequence according to the manufacturer's and published guidelines. The key advantage of MPnRAGE is its incorporation of both low and high-frequency information, which allows for motion correction without degrading images that are already motion-free [1].
- Data Acquisition: Run the scan. MPnRAGE is particularly useful for populations where motion is anticipated, such as children or patients with disabilities [1].
- Reconstruction and Quality Check: Reconstruct the images. Use the sequence's inherent properties to correct for motion artifacts present in the raw data. Finally, perform a visual and quantitative quality check (e.g., using SHN) to confirm success [1] [64].
The following workflow diagram summarizes the key steps for managing motion in a large-scale study:
Next Steps in Motion Correction Research
Emerging research is focusing on deep learning-based quality assessment from navigator signals [16], hybrid motion correction that combines prospective and retrospective methods to compensate for system latency [16], and unified software frameworks like IBMMA for analyzing large-scale, multi-site datasets with inherent missing data [37]. Continuing to integrate these advanced methods into standardized pipelines is crucial for enhancing the reliability of neuroimaging findings.
Benchmarking Performance: Validating and Comparing Correction Efficacy
Frequently Asked Questions: Metric Troubleshooting
Q1: My interobserver ICC is low. Does this indicate a problem with my raters or the segmentation method? A low Intraclass Correlation Coefficient (ICC) suggests poor agreement between different raters or measurements. This can stem from either the raters themselves or the segmentation methodology. To improve consistency, consider implementing an automatic segmentation tool. Studies have shown that automatic segmentation can significantly improve ICC, bringing junior radiologists' performance in line with the manual segmentation of senior radiologists and increasing the average ICC to excellent levels (e.g., >0.85) [67].
Q2: What does a Dice score of 0.5 actually tell me about my segmentation performance? The Dice coefficient measures the spatial overlap between two segmentations, such as a predicted mask and a ground truth. A score of 0.5 indicates a moderate level of similarity. It means that the size of the overlapping area is exactly half of the average size of the two individual masks being compared [68]. In practice, this level of performance is often considered a baseline that should be improved upon. A score of 1 indicates perfect overlap, while 0 indicates no overlap at all.
Q3: I have a high CNR, but my image quality still seems poor. What other factors should I check? A high Contrast-to-Noise Ratio (CNR) confirms good signal differentiation between your region of interest (e.g., the substantia nigra) and the chosen background region. However, image quality can be degraded by other artifacts. A primary suspect in neuroimaging is subject motion, which can introduce blurring and spurious correlations without necessarily reducing the CNR calculated from a static image [17]. You should review your motion correction procedures and check for other artifacts related to the acquisition hardware.
Q4: How can I validate a machine learning model for neuroimaging if my dataset is small? When working with a small dataset, a simple train-test split can lead to overfitting and an unreliable performance estimate. A robust solution is to use (k)-fold cross-validation. This method involves splitting your data into (k) subsets (or "folds"). The model is trained on (k)-1 folds and tested on the remaining fold, a process repeated until each fold has been used as the test set once. The final performance is the average across all folds, providing a more stable out-of-sample estimate of your model's true predictive capability [69].
Metric Definitions and Characteristics
The table below summarizes the core attributes of these three key validation metrics.
| Metric | Full Name | Primary Use Case | Interpretation Range | Key Strengths |
|---|---|---|---|---|
| ICC [70] | Intraclass Correlation Coefficient | Assessing reliability and agreement between raters or measurements. | -1 to 1 (Commonly 0 to 1; >0.75 indicates good reliability) | Accounts for systematic differences between raters; can be used for more than two raters. |
| Dice [68] | Sørensen–Dice Coefficient | Measuring spatial overlap in image segmentation (e.g., vs. a ground truth). | 0 to 1 (1 indicates perfect overlap) | Simple to compute; robust to class imbalance; directly interprets spatial accuracy. |
| CNR [71] | Contrast-to-Noise Ratio | Quantifying the visibility of a structure of interest against its background. | 0 to ∞ (Higher is better) | Standardized measure of image quality; useful for optimizing scan protocols. |
Detailed Experimental Protocols
Protocol 1: Validating an Automatic Segmentation Tool
This protocol is designed to evaluate whether an automatic segmentation model improves consistency and reduces variability between raters with different experience levels [67].
1. Dataset Preparation:
- Population: A typical study might use data from hundreds of patients (e.g., 228 for training, 99 for testing) diagnosed with the condition of interest, such as prostate cancer [67].
- Image Acquisition: Acquire high-resolution MR images (e.g., T2-weighted fat-suppressed sequences on a 3T scanner) [67].
- Data Splitting: Divide the dataset into a training set for building the automatic segmentation model and a separate test set for final evaluation.
2. Reference Standard and Manual Segmentation:
- Have two expert chief radiologists manually segment the regions of interest (e.g., the prostate) to create a reference standard. All disagreements should be resolved by consensus [67].
- A group of radiators with varying experience (e.g., senior with >8 years, junior with 3 years) then performs manual segmentation on the test set.
3. Automatic Segmentation:
- Train an automatic segmentation model on the training set using an open-source platform like MONAI Label, which integrates with 3D Slicer. Use data augmentation (flipping, rotation, cropping) to improve model robustness [67].
- The same group of radiators then performs segmentation assisted by the automatic model on the test set.
4. Quantitative Analysis:
- Dice Coefficient: Calculate the spatial overlap between each rater's segmentation (both manual and auto-assisted) and the reference standard. A higher Dice score indicates better accuracy [67] [68].
- ICC Calculation: Use a statistical software package (R, Python, SPSS) to compute the ICC. This assesses the consistency of radiomics features (texture, shape, etc.) extracted from the different segmentations. The goal is to see if the ICC improves from manual to auto-assisted segmentation, especially among junior radiologists [67].
The following workflow diagram illustrates the key steps in this validation process:
Protocol 2: Calculating CNR in Neuromelanin-MRI
This protocol details the method for calculating CNR to quantify degeneration of the substantia nigra pars compacta (SNc) in Parkinson's disease research [71].
1. Image Acquisition:
- Use a 3.0 Tesla MRI scanner with a dedicated head and neck coil.
- Acquire neuromelanin-sensitive images using a 2D gradient echo sequence with magnetization transfer contrast (MTC). Typical parameters include: TR/TE=180/2.5 ms, flip angle=25°, and high in-plane resolution (e.g., 0.35x0.35 mm²) [71].
2. Region of Interest (ROI) Selection:
- SNc ROI: Manually delineate the SNc on the three lowest contiguous slices where it is visible, tracing the hyperintense area dorsal to the cerebral peduncle and ventral to the red nucleus. This should be performed by at least two trained raters blinded to the clinical status of subjects. The Dice similarity coefficient and ICC can be used to ensure inter-rater reliability is excellent (e.g., >0.80) [71].
- Background ROI (BND): Manually trace a background region in an area adjacent to the SNc, such as the cerebral peduncles [71].
3. Quantitative CNR Calculation:
- Extract the signal intensity for the SNc ROI ((Sig{SNc})) and the background ROI ((Sig{BND})).
- Calculate the standard deviation of the signal in the background ROI ((STD_{BND})).
- The CNR for each slice is computed as: ((Sig{SNc} - Sig{BND}) / STD_{BND}).
- The final CNR value for the subject is the mean CNR across all analyzed slices [71].
The process for calculating the CNR is summarized in the following diagram:
The Researcher's Toolkit
This table lists essential software and tools used in the featured experiments for image processing, analysis, and validation.
| Tool Name | Primary Function | Use Case in Validation |
|---|---|---|
| 3D Slicer [67] | Open-source software platform for medical image informatics and visualization. | Used for manual segmentation of regions of interest (e.g., prostate, SNc). |
| MONAI Label [67] | Intelligent, open-source image annotation and learning tool. | Enables the development and use of AI-assisted segmentation models. |
| FSL [71] | FMRIB Software Library, a comprehensive library of analysis tools for fMRI, MRI, and DTI brain imaging data. | Used for image registration, mathematical operations on ROIs (e.g., fslmaths), and feature calculation (e.g., fslstats). |
| FreeSurfer [71] | Software suite for processing and analyzing brain MRI images. | Provides tools for brain extraction, segmentation, and ROI delineation. |
| Statistical Parametric Mapping (SPM) [71] [72] | Software package for the analysis of brain imaging data sequences. | Used for image preprocessing, spatial normalization, and voxel-based statistical analysis. |
| PyRadiomics [67] | Open-source python package for the extraction of radiomics features from medical images. | Extracts quantitative features (texture, shape) from segmented ROIs for consistency analysis (ICC). |
| Python (with Scikit-learn) [69] [67] | General-purpose programming language with a machine learning library. | Used for implementing cross-validation, statistical analysis, and calculating performance metrics. |
FAQs and Troubleshooting Guide
Q1: What is DISORDER and how does it improve pediatric brain MRI?
A: DISORDER (Distributed and Incoherent Sample Orders for Reconstruction Deblurring using Encoding Redundancy) is a retrospective motion correction technique for structural MRI that uses a specialized k-space sampling scheme. Unlike conventional linear phase encoding, DISORDER ensures that every shot of acquired k-space data contains samples distributed incoherently throughout k-space. This provides both low and high-resolution information in each segment, significantly improving the ability to estimate head pose and perform high-quality motion-corrected reconstructions in the presence of rigid motion. The method jointly estimates motion parameters and the final image, alternating between motion estimation and reconstruction until convergence [73]. For pediatric imaging, this translates to more reliable morphometric measurements from scans that would otherwise be compromised by motion.
Q2: My DISORDER-acquired images show inconsistent cortical thickness measures in FreeSurfer for motion-corrupted scans. Is this expected?
A: Yes, this is an expected finding and actually demonstrates DISORDER's advantage. The validation study found that intraclass correlation coefficient (ICC) values for cortical measures were significantly less consistent in motion-corrupt conventional MPRAGE data (ICC: 0.09–0.74) compared to motion-free data (ICC: 0.76–0.98). When DISORDER was applied to motion-degraded scans, it improved the reliability of these measurements. If you're observing inconsistencies, ensure you're comparing DISORDER-corrected motion scans with motion-free conventional acquisitions as your benchmark, not motion-corrupted conventional images [74] [73].
Q3: Which brain structures show the most significant improvement with DISORDER correction?
A: The improvement varies by brain region. Hippocampal and cortical measures benefit most from DISORDER when motion is present, while subcortical grey matter volumes generally show good/excellent agreement even without specialized motion correction.
The table below summarizes the quantitative agreement (Intraclass Correlation Coefficients) for different structural measures between conventional MPRAGE and DISORDER:
| Brain Structure Category | Specific Structures | ICC (Motion-Free) | ICC (Motion-Corrupt) |
|---|---|---|---|
| Subcortical Grey Matter | Most structures (e.g., thalamus) | 0.75–0.96 | 0.62–0.98 |
| Subcortical Grey Matter | Amygdala, Nucleus Accumbens | 0.38–0.65 | 0.1–0.42 |
| Regional Brain Volumes | Various lobes | 0.47–0.99 | 0.54–0.99 |
| Hippocampal Volumes | Hippocampal subfields | 0.65–0.99 | 0.11–0.91 |
| Cortical Measures | Cortical thickness, surface area | 0.76–0.98 | 0.09–0.74 |
Data derived from Gal-Er et al. (2025) [74]
Q4: What segmentation software packages were validated for use with DISORDER data?
A: The DISORDER validation study specifically tested and recommends the following software packages for morphometric analysis with DISORDER-corrected images:
- FreeSurfer: For cortical morphometry and regional brain volume measurements [73]
- FSL-FIRST: For subcortical grey matter segmentation [73]
- HippUnfold: For hippocampal subfield segmentation and unfolding [73]
The study noted that FreeSurfer performs best for cortical analyses, while FSL-FIRST more closely approximates manual segmentation for subcortical grey matter in pediatric populations [73].
Q5: How does DISORDER compare to prospective motion correction methods?
A: DISORDER offers distinct advantages for pediatric imaging. While prospective methods require additional hardware for real-time head tracking and scanner modifications, DISORDER operates retrospectively without extra equipment. This makes it more readily implementable across existing scanner platforms. A key finding in pediatric cohorts indicates that retrospective techniques like DISORDER can improve T1-weighted image quality and automated segmentation compared to prospective motion correction approaches [73].
Experimental Protocols and Methodologies
Participant and Acquisition Protocol
The validation study for DISORDER was conducted on thirty-seven children aged 7-8 years as part of the ICONIC study. Two T1-weighted MPRAGE 3D datasets were acquired for each participant on a 3T Siemens MAGNETOM Vida scanner:
- Conventional MPRAGE: Linear phase encoding (TR = 2,200 ms, TE = 2.46 ms, flip angle = 8°, voxel size = 1.1 × 1.07 × 1.07 mm³, acceleration factor = 2, acquisition time = 4.15 min)
- DISORDER MPRAGE: DISORDER sampling scheme (TR = 2,200 ms, TE = 2.45 ms, flip angle = 8°, voxel size = 1.1 × 1.07 × 1.07 mm³, no acceleration, acquisition time = 7.39 min)
Participants were instructed to stay still while watching a movie. DISORDER reconstruction was performed using MATLAB R2018b based on its open-source implementation, alternating between motion estimation and image reconstruction until convergence [73].
Validation and Statistical Analysis Protocol
The validation protocol employed multiple analysis streams to comprehensively assess DISORDER's performance:
Validation Workflow for DISORDER
Image Quality Scoring: All MPRAGE images were visually assessed and scored as motion-free or motion-corrupt by trained evaluators [73]
Morphometric Analysis Pipeline:
- Cortical morphometry and regional brain volumes: Analyzed with FreeSurfer
- Subcortical grey matter: Segmented with FSL-FIRST
- Hippocampal subfields: Processed with HippUnfold [73]
Statistical Validation:
The Scientist's Toolkit: Research Reagent Solutions
| Tool/Software | Function | Application in DISORDER Validation |
|---|---|---|
| DISORDER Acquisition | Retrospective motion correction via incoherent k-space sampling | Motion-robust structural imaging [73] |
| FreeSurfer | Automated cortical reconstruction and volumetric segmentation | Cortical morphometry, regional brain volumes [73] |
| FSL-FIRST | Subcortical structure segmentation using shape/appearance models | Subcortical grey matter volume measurement [73] |
| HippUnfold | Hippocampal subfield segmentation and surface-based analysis | Hippocampal subfield volumetry [73] |
| FLIRT (FSL) | Linear image registration with 6 degrees of freedom | Motion correction in conventional RMC approaches [58] |
| MATLAB R2018b | Technical computing environment | DISORDER reconstruction implementation [73] |
Key Experimental Findings and Data Interpretation
Quantitative Performance Metrics
The comprehensive validation of DISORDER revealed several key performance characteristics critical for researchers implementing this technique:
| Performance Measure | Finding | Interpretation |
|---|---|---|
| Motion-Free Agreement | Good/excellent ICC for most structures | DISORDER comparable to conventional MPRAGE without motion [74] |
| Motion-Corrupt Improvement | Significant improvement in 22/58 structures | DISORDER superior for motion-degraded scans [74] |
| Segmentation Consistency | Higher ICC with DISORDER for motion scans | More reliable automated segmentation [73] |
| Clinical Utility | Validated for pediatric morphometry | Suitable for challenging populations [74] [73] |
Implementation Considerations
When implementing DISORDER in your research pipeline, consider these technical aspects:
Acquisition Time: DISORDER requires longer acquisition times (7.39 min) compared to conventional accelerated MPRAGE (4.15 min) due to the absence of parallel imaging acceleration [73]
Reconstruction Workflow: The reconstruction process is computationally intensive, requiring iterative motion estimation and image reconstruction until convergence [73]
Scanner Compatibility: The method has been implemented on Siemens scanners but could potentially be adapted to other platforms using the open-source implementation [73]
The validation evidence confirms DISORDER as a robust motion correction solution for pediatric brain morphometry studies, particularly valuable for populations where motion artifacts frequently compromise data quality.
Core Concepts: AI and Non-AI Segmentation
In the context of motion correction for large-scale neuroimaging studies, segmentation is a critical step for isolating anatomical structures for analysis. The methodologies for this task can be broadly divided into AI (Artificial Intelligence) and non-AI approaches.
AI-driven segmentation leverages deep learning models, a subset of machine learning, to automate the process of partitioning medical images. These models are trained on vast datasets to learn complex, non-linear relationships between image pixels, enabling them to perform tasks like anatomical segmentation and image enhancement directly [75]. A key strength of AI is its ability to perform instance segmentation, which not only classifies each pixel by type (e.g., 'gray matter') but also distinguishes between individual objects of the same type (e.g., differentiating between specific gyri in the brain) [76]. Advanced models include generative architectures like Generative Adversarial Networks (GANs) and Diffusion Models, which are powerful for tasks like correcting motion artifacts by learning to map motion-corrupted images to their clean counterparts [75] [48].
Non-AI segmentation, often referred to as manual or traditional segmentation, relies on human experts (e.g., radiologists, analysts) to review customer data or medical images and group individuals or delineate structures based on predefined factors like purchase history, demographics, or anatomical boundaries [77]. This approach is labor-intensive and requires periodic updates, making it slow and potentially inconsistent due to human error and fatigue [77] [64]. In neuroimaging, analyses that incorporate lower-quality data from non-AI or less rigorous pipelines can introduce systematic bias, for example, by underestimating cortical thickness and overestimating cortical surface area [64].
The following workflow illustrates the typical processes for AI versus manual segmentation in a data processing context:
Quantitative Comparison: Speed, Accuracy, and Scalability
The strategic choice between AI and non-AI segmentation has profound implications for the efficiency and validity of large-scale neuroimaging research. The table below summarizes the key performance differences, drawing parallels between commercial applications and their implications for neuroimaging.
Table 1: Performance Comparison of AI vs. Non-AI Segmentation
| Metric | AI Segmentation | Non-AI / Manual Segmentation |
|---|---|---|
| Processing Speed | Real-time updates and processing [77]. Automatically adjusts to data size [77]. | Batch processing at intervals [77]. Dependent on staff workload [77]. |
| Resource Requirements | Operates continuously with minimal supervision [77]. Scales without adding staff [77]. | Labor-intensive, limited to working hours [77]. Needs dedicated team members [77]. |
| Consistency & Accuracy | Algorithm-driven, minimizing human error and bias [77]. Can significantly improve image quality metrics (e.g., PSNR, SSIM) [75] [78]. | Prone to human error and inconsistencies [77]. Poor image quality can systematically bias results [64]. |
| Data Handling | Manages large, diverse datasets from multiple channels [77]. Efficiently handles large-scale datasets through parallel processing [37]. | Limited to fewer variables and channels [77]. Struggles with scale and complexity of multi-site data [37]. |
| Cost Efficiency | Fixed costs; reduces reliance on manual labor [77]. Can reduce need for repeat scans, lowering healthcare costs [75]. | Costs rise with workload; requires ongoing staff training [77]. Repeat scans due to motion artifacts incur high costs [75]. |
For neuroimaging specifically, the quantitative superiority of AI methods is evident in motion artifact correction. A systematic review and meta-analysis found that deep learning, particularly generative models, shows significant promise for improving MRI image quality by effectively addressing motion artifacts [75]. Specific AI models have demonstrated measurable improvements, such as reducing the Normalized Mean Squared Error (NMSE) by 0.0226 and improving key image quality metrics like the Peak Signal-to-Noise Ratio (PSNR) by 5.5558 and the Structural Similarity Index (SSIM) by 0.1160 [75].
Troubleshooting Guides and FAQs
FAQ 1: Why does my segmented neuroimaging data show systematic biases in cortical measurements, and how can I resolve this?
Answer: Systematic biases, such as underestimating cortical thickness and overestimating cortical surface area, are often introduced by incorporating low-quality MRI scans into your analysis [64]. This is a prevalent issue in large-scale datasets where manual or automated quality control may be insufficient.
Troubleshooting Steps:
- Implement Rigorous Quality Control: Do not rely solely on pass/fail metrics from standard processing pipelines. Manually rate a subset of scans to establish a ground truth for quality.
- Use a Proxy Metric: For large datasets where manual rating is impractical, employ an automated metric like Surface Hole Number (SHN). SHN estimates imperfections in cortical reconstruction and can effectively approximate manual quality ratings [64].
- Stress-Test Your Findings: Use SHN to test how your effect sizes change as you progressively exclude poorer-quality scans. If effect sizes inflate or change significantly upon adding lower-quality data, your results may be biased [64].
- Consider AI-Based Correction: For datasets already collected, explore AI-driven motion artifact correction tools. Deep learning models can retrospectively improve image quality, reducing the impact of motion and potentially mitigating these biases [75] [78].
FAQ 2: My AI model for motion artifact correction produces blurry outputs or artificial-looking features. What is causing this, and how can I improve the results?
Answer: This problem, often called "hallucination" or over-smoothing, is a known challenge in generative AI models. It can occur when the model is trained on limited or non-diverse data, lacks proper constraints, or uses an inadequate loss function.
Troubleshooting Steps:
- Verify Your Training Data: Ensure your training set includes a wide variety of motion patterns and anatomical variations. Models trained on narrow datasets struggle to generalize and may produce unrealistic features on new data [75].
- Inspect for Paired Data Reliance: Many models require paired data (motion-corrupted images with their motion-free counterparts). Acquiring such data is difficult. Consider using unpaired learning strategies like CycleGANs, which can learn to translate between corrupted and clean domains without strictly paired examples [75].
- Modify the Loss Function: Standard loss functions like Mean Squared Error (MSE) can lead to blurry results. Implement advanced loss functions that better preserve anatomical detail. For example, a gradient-based loss function can help maintain the integrity of brain anatomy throughout the correction process by prioritizing edges and structures [78].
- Explore Advanced Architectures: Move beyond basic models. Use frameworks that jointly handle multiple tasks, such as the Joint image Denoising and motion Artifact Correction (JDAC) framework, which iteratively cleans images and can progressively improve output quality while preserving details [78].
FAQ 3: What practical steps can I take to minimize motion artifacts in my scansbeforeusing AI correction, especially with challenging populations?
Answer: Prospective mitigation is always more effective than retrospective correction. For populations prone to movement, such as children or patients with neurological disorders, physical stabilization is key.
Troubleshooting Steps:
- Use a Head Stabilization Device: Employ devices like the Magnetic Resonance Minimal Motion (MR-MinMo) head stabiliser. This device uses inflatable pads and a halo structure to comfortably but firmly restrict head movement, significantly reducing motion at its source [79].
- Synergize Hardware with Software: A stabilizer not only reduces motion but also keeps the motion that does occur within a "correctable regime" for retrospective AI methods. Research shows that using the MR-MinMo device significantly improves the performance of subsequent retrospective motion correction algorithms like DISORDER [79].
- Optimize Scan Parameters: Where possible, use accelerated acquisition sequences to shorten scan time, thereby reducing the window for motion to occur.
Experimental Protocols
Protocol 1: Implementing an Iterative Learning Framework for Joint Denoising and Motion Artifact Correction
This protocol is based on the JDAC (Joint image Denoising and motion Artifact Correction) framework, which is designed to handle noisy MRIs with motion artifacts iteratively [78].
1. Hypothesis: An iterative learning framework that jointly performs image denoising and motion artifact correction will progressively improve the quality of 3D brain MRI more effectively than handling these tasks separately.
2. Materials and Reagents: Table 2: Research Reagent Solutions for JDAC Protocol
| Item Name | Function/Description |
|---|---|
| T1-weighted MRI Datasets (e.g., ADNI, MR-ART) | Provides source images for model training and validation. Requires pre-processing (skull stripping, intensity normalization) [78]. |
| U-Net Architecture (x2) | Deep learning model backbone. One U-Net serves as the adaptive denoiser; the other serves as the anti-artifact model [78]. |
| Noise Level Estimation Module | Quantitatively estimates image noise levels using the variance of the image gradient map. Conditions the denoising model and guides iteration stopping [78]. |
| Gradient-based Loss Function | A novel loss function used in the anti-artifact model to retain critical brain anatomy details during correction, preventing over-smoothing [78]. |
3. Methodology:
- Data Preparation: Pre-process all 3D volumetric MRI scans (skull stripping, intensity normalization to [0,1]). For the denoising model, generate training pairs by adding Gaussian noise to clean images. For the anti-artifact model, use paired motion-corrupted and motion-free images [78].
- Model Training:
- Train the Adaptive Denoising Model: Train the first U-Net to denoise images, using the noise level estimation as a conditional input to the network via feature normalization.
- Train the Anti-Artifact Model: Train the second U-Net to remove motion artifacts, using the gradient-based loss function to preserve anatomical integrity.
- Iterative Execution (JDAC Framework):
- Input a noisy, motion-corrupted MRI.
- Step 1: Pass the image through the adaptive denoising model.
- Step 2: Pass the denoised output through the anti-artifact model.
- Step 3: Feed the corrected image back into the denoising model. This loop continues iteratively.
- Early Stopping: Use the estimated noise level from the noise level estimation module to decide when to stop the iterations, preventing unnecessary computation and potential over-processing.
- Validation: Quantitatively validate the output on held-out test data using metrics like PSNR, SSIM, and NMSE. Qualitatively assess images for clarity and anatomical correctness against ground-truth, motion-free scans [78].
The workflow for this iterative framework is as follows:
Protocol 2: Evaluating a Hardware Solution for Motion Reduction in High-Resolution 7T MRI
This protocol outlines the testing of the MR-MinMo head stabilisation device, which can be used to acquire cleaner data, thereby improving the starting point for any subsequent segmentation or analysis [79].
1. Hypothesis: The MR-MinMo device will significantly reduce motion artifacts in long-duration, high-resolution 7T MRI scans, and will synergistically improve the performance of retrospective motion correction algorithms.
2. Experimental Design:
- A 2x2 factorial design is used, acquiring scans both with and without the MR-MinMo device, and with both standard linear k-space sampling and a motion-resilient sequence (DISORDER) that enables retrospective correction [79].
3. Methodology:
- Participant Preparation: Fit the participant with the MR-MinMo device according to manufacturer guidelines, which includes using a hairnet for comfort and force distribution. For control scans, remove the device.
- Image Acquisition: Acquire high-resolution 3D Multi-Echo Gradient Echo (ME-GRE) scans on a 7T scanner under four conditions:
- Condition A: Standard sampling, without MR-MinMo.
- Condition B: Standard sampling, with MR-MinMo.
- Condition C: DISORDER sampling, without MR-MinMo.
- Condition D: DISORDER sampling, with MR-MinMo.
- Image Analysis:
- Qualitative Assessment: Experts perform visual inspection of the images for ghosting, blurring, and other motion artifacts.
- Quantitative Assessment: Calculate the Normalized Gradient Squared (NGS) metric, where a higher value indicates sharper image quality.
- Advanced Quantification: Generate T2* maps from the multi-echo data and assess the standard deviation of R2* values in white matter. Lower variance indicates more precise and reliable quantitative mapping [79].
- Statistical Analysis: Perform a repeated-measures ANOVA on the NGS scores and R2* variances to determine the individual and interactive effects of the MR-MinMo device and the DISORDER reconstruction.
Troubleshooting Guides
Guide 1: Addressing Motion-Induced Variance in Functional Connectivity Analyses
Problem: A researcher finds a significant, distance-dependent correlation between subject motion and functional connectivity in their resting-state fMRI dataset. Short-range connections appear artificially strengthened, and long-range connections appear artificially weakened in high-motion subjects.
Symptoms:
- Spurious group differences in functional connectivity that align with known motion patterns (e.g., children, patients, or elderly showing systematically different connectivity patterns) [17].
- A significant correlation between framewise displacement (FD) and connectivity measures, particularly in long-range connections [17].
- Reports of "local overconnectivity but long-distance disconnection" in study groups that tend to move more [17].
Solution: Apply a multi-pronged denoising strategy to mitigate motion artifact without removing biological signal of interest.
Step-by-Step Resolution:
- Quantify Motion: Calculate Framewise Displacement (FD) and DVARS for your dataset. FD measures the volume-to-volume displacement of the head, while DVARS quantifies the rate of intensity change [42] [17].
- Implement Censoring ("Scrubbing"): Identify and censor volumes with excessive motion. A common threshold is FD > 0.5 mm, though this should be adjusted for studies with ultra-short TRs [42]. For task fMRI, create a nuisance regressor for each censored time point; for resting-state fMRI, remove the affected volumes and the volumes immediately before and after them [42].
- Incorporate Motion Regressors: Include motion parameters as confounds in your General Linear Model (GLM). For thoroughness, use a 24-parameter model (6 motion parameters, their temporal derivatives, and all these terms squared) to regress out motion-related variance [42].
- Validate the Correction: After denoising, re-check the correlation between FD and your connectivity measures. A successful correction will eliminate or drastically reduce this relationship [17].
Guide 2: Mitigating Motion Artifacts in Magnetic Resonance Spectroscopy (MRS)
Problem: An MRS study on a patient population prone to movement shows poor spectral quality, including broadened linewidth and unreliable quantification of low-concentration metabolites like GABA and GSH.
Symptoms:
- Broadened or split spectral lines, indicating degraded B0 field homogeneity due to movement [12].
- Unstable metabolite quantification, with variability exceeding the typical 5-15% range observed under ideal conditions [12].
- Presence of spurious signals, such as extracranial lipids, suggesting incorrect voxel localization [12].
Solution: Implement a prospective motion and B0 shim correction strategy, as retrospective methods are insufficient for correcting B0 field changes [12].
Step-by-Step Resolution:
- Choose a Tracking Method: Utilize an external tracking method (e.g., an optical camera) to monitor head position with sub-millimeter and sub-degree precision [12].
- Enable Real-Time Correction: Configure the scanner to update the MRS voxel localization in real-time based on the tracking data [12].
- Update B0 Shimming: Use an internal navigator to measure the B0 field inside the imaged volume and update the scanner's first-order shim hardware in real-time to maintain field homogeneity [12].
- Verify Performance: Ensure the motion correction system can detect and correct for motions smaller than 0.17 mm translation or 0.26-2.9 degrees rotation (depending on voxel location), as these can cause 5% changes in metabolite concentrations [12].
Guide 3: Correcting for Motion in Positron Emission Tomography (PET) Neuroimaging
Problem: Whole-body PET imaging reveals motion-induced blurring, particularly in the head region, leading to errors in tracer uptake measurements and complicating quantitative kinetic modeling.
Symptoms:
- Blurred images and misalignment between emission and transmission scans, causing incorrect attenuation correction [66].
- Errors in the definition of Regions of Interest (ROIs) and unreliable kinetic modeling parameters (e.g., distribution volume ratio) [66].
Solution: Implement a retrospective gating scheme to correct for involuntary head motion.
Step-by-Step Resolution:
- Select a Gating Approach:
- Apply Motion Correction: Reconstruct the PET data into specific time frames based on the recorded motion signal, creating multiple, motion-corrected images [66].
- Reconstruct Final Image: Use an iterative reconstruction algorithm to combine the motion-corrected frames into a single, high-quality image with reduced blurring [66].
- Verify Outcome: Check for improved image sharpness and ensure that tracer uptake measurements in the final image are stable and physiologically plausible [66].
Frequently Asked Questions (FAQs)
FAQ 1: After realigning my fMRI volumes, why do I need to regress out the motion parameters again in my model?
Volume realignment (e.g., using FSL's MCFLIRT) corrects for the misalignment of brain structures across time, ensuring that a given voxel index refers to the same anatomical location. However, it does not remove the spin-history artifacts caused by motion. When a subject moves, the nuclear spins in a given voxel may have a different history of RF excitation, leading to signal changes that are not related to neural activity. Including the motion parameters as regressors in the General Linear Model (GLM) helps to account for and remove this residual motion-related variance from the BOLD signal [42].
FAQ 2: What is the acceptable amount of head motion in an fMRI study?
There is no single, universally accepted threshold for head motion, as the acceptable level depends on factors like scanning parameters, experimental design, and the intended statistical analysis [41]. However, as a rule of thumb, framewise displacement (FD) should ideally be kept below 0.5 mm for a majority of volumes. Studies should report the mean and maximum FD for each subject and each group. Crucially, group comparisons must be checked to ensure that differences in motion are not driving the apparent neurobiological findings [17].
FAQ 3: How does subject motion specifically bias functional connectivity metrics?
Small head movements introduce structured, spurious noise into the fMRI signal. This noise is more similar at nearby voxels than at distant voxels. Consequently, motion artifact causes a distance-dependent modulation of correlation values: it inflates short-range functional connections and suppresses long-range connections [17]. Because certain populations (e.g., children, patients with neurological disorders, the elderly) often move more, this artifact can create false group differences that mimic theories of "underconnectivity" or "local overconnectivity" [17].
FAQ 4: What are the key performance specifications for a motion correction system in MRS?
For MRS, a motion correction system must address both localization and B0 field homogeneity. To maintain metabolite quantification stability within 5%, the system should be able to [12]:
- Detect translations with a precision better than 0.17 mm.
- Detect rotations with a precision better than 0.26-2.9 degrees (angle varies with distance from the rotation axis).
- Update the scanner's shim hardware in real-time to correct for B0 field changes induced by motion.
FAQ 5: In large-scale studies, can increasing sample size compensate for motion artifacts?
Increasing sample size improves the statistical power of a study but does not correct for the systematic bias introduced by motion. If motion is correlated with a group variable (e.g., patients vs. controls), a larger sample might even strengthen the false positive findings. The primary solution is rigorous motion correction at the preprocessing and denoising stages. Furthermore, large-scale phenotypic prediction studies show that prediction accuracy from neuroimaging data plateaus at a level far from perfect, suggesting that data quality, including effective motion correction, is a critical limiting factor [80].
Data Presentation
Table 1: Quantitative Specifications for Effective Motion Correction
This table consolidates key numerical guidelines for motion correction performance and data quality assurance across different neuroimaging modalities.
| Modality | Metric | Target Threshold | Impact of Non-Compliance | Source |
|---|---|---|---|---|
| fMRI (General) | Framewise Displacement (FD) | < 0.5 mm (common threshold) | Introduction of distance-dependent correlation bias; false group differences | [42] [17] |
| MRS | Translation Precision | < 0.17 mm | >5% change in metabolite concentration estimates | [12] |
| MRS | Rotation Precision | < 0.26 - 2.9 degrees (context-dependent) | >5% change in metabolite concentration estimates | [12] |
| MRS | Metabolite Quantification Stability | < 5% variability (for primary metabolites) | Reduced sensitivity to detect cross-sectional or longitudinal clinical changes | [12] |
| Large-Scale Prediction | Sample Size for Improved Accuracy | 1,000 to 1,000,000 participants | Prediction accuracy for cognitive/mental health phenotypes remains low despite large samples | [80] |
Table 2: Motion Correction Strategies and Their Applications
This table compares the primary motion correction approaches, their methodologies, and their suitability for different imaging contexts.
| Strategy | Methodology | Key Tools/Parameters | Best For | Limitations |
|---|---|---|---|---|
| Prospective Correction | Real-time adjustment of acquisition parameters based on head position. | Optical tracking, NMR probes, internal navigators (for B0 shim) [12] | MRS, where B0 homogeneity is critical; studies with predictable, slow drifts. | Limited availability on clinical scanners; requires specialized hardware/software. |
| Retrospective Correction: Volume Realignment | Post-hoc alignment of all image volumes to a reference volume. | Rigid-body transformation (3 translations, 3 rotations) [41] | Standard preprocessing for fMRI and structural MRI; all studies. | Does not correct spin-history artifacts; is a baseline step requiring further denoising. |
| Retrospective Denoising: Regression | Including motion parameters as nuisance regressors in the statistical model. | 6, 12, or 24 motion parameters; Framewise Displacement (FD) [42] | Removing residual motion-related variance after realignment in fMRI. | May remove neural signal if motion is task-correlated; does not handle motion "spikes". |
| Retrospective Denoising: Censoring (Scrubbing) | Removing high-motion timepoints from analysis. | FD (>0.5mm) and DVARS thresholds; removing N volumes surrounding a bad volume [42] | Dealing with severe, sporadic motion "spikes" in both task and resting-state fMRI. | Reduces temporal degrees of freedom; can be problematic for block designs or short scans. |
| Motion Gating (PET) | Sorting or correcting data based on phase of motion cycle (e.g., respiration). | Hardware-driven (external sensors) or Data-driven (from raw PET data) [66] | Whole-body PET imaging to correct for respiratory and cardiac motion. | Increases scan time or reduces counts; data-driven methods are still being optimized. |
Experimental Protocols
Protocol 1: Integrated Motion Correction Pipeline for Resting-State fMRI
This protocol details a comprehensive approach to mitigate motion artifacts in resting-state fMRI data, suitable for large-scale studies.
1. Data Acquisition:
- Acquire resting-state BOLD data using a standardized sequence (e.g., EPI).
- If possible, acquire multiband sequences to allow for shorter TRs, which can improve motion correction.
2. Preprocessing & Motion Estimation:
- Perform volume realignment using a tool like FSL's MCFLIRT [42] or an equivalent to generate the six rigid-body motion parameters (3 translations, 3 rotations) for each volume.
- Calculate Framewise Displacement (FD) and DVARS for the entire time series [42] [17].
3. Denoising Strategy:
- Motion Regression: Incorporate a 24-parameter model (the 6 motion parameters, their derivatives, and the squares of all 12) as confounds in your GLM [42].
- Censoring: Identify volumes with FD exceeding a chosen threshold (e.g., 0.5 mm). For resting-state data, censor the identified volume as well as the one preceding and following it to account for the slowness of the hemodynamic response [42].
- Include Other Nuisance Regressors: Consider combining motion correction with regressors for white matter and cerebrospinal fluid signals, global signal regression, and band-pass filtering.
4. Quality Control and Validation:
- Plot the motion parameters (translation/rotation) and FD over time for each subject to identify problematic runs.
- After denoising, verify that there is no significant correlation between the mean FD of a subject and their overall functional connectivity measures, particularly for long-range connections [17].
Protocol 2: Prospective Motion and Shim Correction for Single Voxel MRS
This protocol ensures high-quality, quantifiable MRS data by correcting for motion and B0 field changes in real-time.
1. Subject Preparation and Immobilization:
- Use comfortable head restraints to minimize voluntary motion, acknowledging that this alone is insufficient [12].
2. System Setup:
- Enable Optical Tracking: Position an optical camera to track a marker firmly attached to the subject's head. The system should provide sub-millimeter and sub-degree precision [12].
- Configure Shim Correction: Ensure the system is capable of running a fast, internal B0 field navigator (e.g., a B0 map) immediately before or during the MRS sequence.
3. Real-Time Acquisition:
- The tracking system continuously monitors head position.
- If motion exceeds a predefined threshold (e.g., >0.1 mm translation), the system updates the center frequency, transmit gain, and the spatial coordinates of the MRS voxel for the next TR.
- Simultaneously, the B0 navigator measures the current field and updates the first-order shim currents to re-optimize B0 homogeneity for the new head position [12].
4. Post-Processing and Quantification:
- Process the motion-corrected data with standard fitting algorithms (e.g., LCModel).
- Compare the spectral linewidth and metabolite concentration estimates (e.g., for NAA, Cr, Cho) to values obtained from a stable, control subject to ensure the variability is within the target 5-15% range [12].
Mandatory Visualization
Diagram 1: Integrated Motion Correction Workflow for fMRI
Diagram 2: Decision Tree for Motion-Related Troubleshooting
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Motion Correction
This table lists key software tools, data components, and parameters that are essential for implementing effective motion correction protocols.
| Item Name | Type | Function / Purpose | Example / Notes |
|---|---|---|---|
| Framewise Displacement (FD) | Quantitative Metric | Summarizes volume-to-volume head movement by combining translation and rotation parameters. | Critical for identifying motion-contaminated volumes in fMRI; a threshold of 0.5 mm is commonly used for censoring [42] [17]. |
| DVARS | Quantitative Metric | Measures the rate of change of the BOLD signal across the entire brain at each timepoint. | Helps identify sudden intensity jumps caused by motion; often used in conjunction with FD for scrubbing [42]. |
| 24-Parameter Model | Nuisance Regressor Set | A comprehensive set of regressors to remove motion-related variance from the BOLD signal in a GLM. | Includes 6 motion parameters, their derivatives, and their squares, as recommended to model motion artifacts more completely than 6 parameters alone [42]. |
| Optical Motion Tracking System | Hardware | Provides real-time, high-precision measurements of head position for prospective motion correction. | Systems like Moiré Phase Tracking (MPT) are used in MRS and fMRI to update voxel position with sub-millimeter precision [12]. |
| fMRIPrep | Software Pipeline | A robust, standardized software tool for preprocessing of fMRI data. | Includes integrated steps for motion correction, calculation of FD/DVARS, and generation of confound tables, promoting reproducibility [42] [81]. |
| Real-time Shim Update | Scanner Functionality | Corrects for B0 field inhomogeneity changes caused by subject motion, critical for MRS. | An internal navigator sequence measures the B0 field, and scanner hardware updates shim currents within a single TR [12]. |
| ANTs / FSL / SPM | Software Library | Provides algorithms for image registration and motion correction (realignment). | Foundational tools for performing the initial volume realignment that is a prerequisite for all subsequent denoising steps [82]. |
Conclusion
Motion correction is no longer a peripheral concern but a central component of robust, large-scale neuroimaging science. The integration of diverse strategies—from prospective hardware-based tracking to sophisticated retrospective and AI-driven software solutions—is essential for mitigating artifacts that obscure true biological signals. Key takeaways include the critical balance between scan duration and sample size for cost-effective power, the demonstrated efficacy of modern pipelines in mitigating motion-induced bias, and the promising role of unified, data-driven models for multi-modal data. Future directions point toward the increased adoption of AI to enhance speed and accuracy without sacrificing interpretability, the development of standardized validation frameworks across consortia, and the translation of these advanced correction techniques to improve the diagnostic precision and clinical utility of neuroimaging in drug development and personalized medicine.
References
- 1. Researchers unveil new strategy to correct for motion during ... [https://www.waisman.wisc.edu/2018/08/23/researchers-unveil-new-strategy-to-correct-for-motion-during-mri-scans/]
- 2. Head motion: the dirty little secret of neuroimaging in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6306289/]
- 3. Age, Motion, Medical, and Psychiatric Associations With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10865144/]
- 4. Longer scans boost prediction and cut costs in brain-wide ... [https://www.nature.com/articles/s41586-025-09250-1]
- 5. Motion correction and the use of motion covariates in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6871380/]
- 6. Motion-Robust MRI: Reconstruction & Motion Correction [https://www.ismrm.org/25/program-files/O-05.htm]
- 7. HERON: High-Efficiency Real-Time Motion Quantification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617990/]
- 8. Motion Detection and Correction [https://www.brainvoyager.com/bvqx/doc/UsersGuide/Preprocessing/MotionDetectionAndCorrection.html]
- 9. Prospective motion correction with volumetric navigators (vNavs) reduces the bias and variance in brain morphometry induced by subject motion - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1053811915010770]
- 10. Motion correction in MRI of the brain - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4930872/]
- 11. Tutorial 5: Motion [http://www.newbi4fmri.com/tutorial-5-motion]
- 12. Motion Correction Methods for Magnetic Resonance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7855523/]
- 13. Motion correction [https://www.sciencedirect.com/science/article/abs/pii/B9780323998987000225]
- 14. Res-MoCoDiff: residual-guided diffusion models for motion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532098/]
- 15. A Physics-Informed Deep Learning Model for MRI Brain Motion Correction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11844622/]
- 16. ISMRM24 - Motion Correction: Neuroimaging [https://www.ismrm.org/24/pf/D-12.htm]
- 17. Recent progress and outstanding issues in motion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4262543/]
- 18. Advances, challenges, and promises in pediatric ... [https://www.sciencedirect.com/science/article/abs/pii/S014976341730711X]
- 19. Quantifying MR head motion in the Rhineland Study [https://pmc.ncbi.nlm.nih.gov/articles/PMC10287097/]
- 20. Task-based functional MRI challenges in clinical ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2022.1017211/full]
- 21. Challenges and Opportunities for Neuroimaging in Young ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7855317/]
- 22. Deep Learning in Large and Multi-Site Structural Brain MR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8811356/]
- 23. Robust Motion Correction Strategy for Structural MRI in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6192848/]
- 24. Reducing motion artifacts [https://mriquestions.com/reducing-motion-artifacts.html]
- 25. Motion-corrected 4D-Flow MRI for neurovascular applications [https://www.sciencedirect.com/science/article/pii/S1053811922008321]
- 26. Prospective Motion Correction in Functional MRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5427003/]
- 27. Prospective motion correction improves the sensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6175330/]
- 28. Prospective motion correction of fMRI: Improving the quality ... [https://www.sciencedirect.com/science/article/pii/S1053811920300811]
- 29. Prospective motion correction using coil-mounted cameras [https://pmc.ncbi.nlm.nih.gov/articles/PMC5899426/]
- 30. Optical Tracking With Two Markers for Robust Prospective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5259555/]
- 31. Propagation of Calibration Errors in Prospective Motion ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3975823/]
- 32. PROMO – Real-time Prospective Motion Correction in MRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2892665/]
- 33. Impact of motion correction on [18F]-MK6240 tau PET ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10278956/]
- 34. The efficiency of retrospective artifact correction methods in ... [https://www.sciencedirect.com/science/article/pii/S1053811917305220]
- 35. Comparison of MRI head motion indicators in ... [https://www.nature.com/articles/s41598-024-79827-9]
- 36. Prospective Evaluation of the Impact of Motion Correction ... [https://jnm.snmjournals.org/content/65/supplement_2/241273]
- 37. Image-Based Meta- and Mega-Analysis (IBMMA): A Unified ... [https://www.sciencedirect.com/science/article/pii/S1053811925005579]
- 38. Fieldmap-Free Retrospective Registration and Distortion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2702772/]
- 39. Challenging the status quo: A guide to open and reproducible ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319985/]
- 40. Brain Harmony: A Multimodal Foundation Model Unifying ... [https://arxiv.org/html/2509.24693v1]
- 41. Motion Correction [https://helpdesk.brainvoyager.com/364032-Motion-Correction]
- 42. Doubt regarding Motion Correction in resting state fMRI [https://neurostars.org/t/doubt-regarding-motion-correction-in-resting-state-fmri/849]
- 43. The future of multimodal artificial intelligence models for ... [https://dirjournal.org/articles/the-future-of-multimodal-artificial-intelligence-models-for-integrating-imaging-and-clinical-metadata-a-narrative-review/dir.2024.242631]
- 44. Cryosparc live motion correction failure - Troubleshooting [https://discuss.cryosparc.com/t/cryosparc-live-motion-correction-failure/7373]
- 45. eddy [https://web.mit.edu/fsl_v5.0.10/fsl/doc/wiki/eddy.html]
- 46. EDDY - FSL - FMRIB Software Library [https://fsl.fmrib.ox.ac.uk/fsl/docs/diffusion/eddy/index.html]
- 47. ISMRM23 - Motion Correction I [https://www.ismrm.org/23/program-files/D-03.htm]
- 48. Correction of Motion-Affected MRI Images via ... [https://archive.ismrm.org/2025/3980.html]
- 49. Chapter 3: Motion Correction - Andy's Brain Book! [https://andysbrainbook.readthedocs.io/en/latest/fMRI_Short_Course/Preprocessing/Motion_Correction.html]
- 50. Longer scans boost prediction and cut costs in brain-wide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10889017/]
- 51. Effect of scanning duration and sample size on reliability in ... [https://www.sciencedirect.com/science/article/pii/S1053811924000995]
- 52. Retrospective motion artifact correction of structural MRI ... [https://www.sciencedirect.com/science/article/pii/S1053811921000331]
- 53. Cost-effectiveness modelling in diagnostic imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC4636534/]
- 54. Methods for the Analysis of Missing Data in FMRI Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC6510494/]
- 55. Harmonization of multi-site functional MRI data with dual- ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1225606/full]
- 56. Multiple imputation of missing fMRI data in whole brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3328786/]
- 57. Missing data approaches for longitudinal neuroimaging ... [https://www.sciencedirect.com/science/article/pii/S1878929325000581]
- 58. Retrospective motion correction protocol for high‐resolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6871401/]
- 59. Is it time to switch your T1W sequence? Assessing the ... [https://www.sciencedirect.com/science/article/pii/S1053811920310703]
- 60. Resting State fMRI: Going Through the Motions [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2019.00825/full]
- 61. False fMRI activation after motion correction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5553448/]
- 62. Motion correction of simultaneous brain PET/MR images ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311070/]
- 63. ISMRM23 - Motion Detection & Correction Techniques [https://www.ismrm.org/23/program-files/O-05.htm]
- 64. Poor image quality introduces systematic bias into MRI data [https://www.thetransmitter.org/spectrum/poor-image-quality-introduces-systematic-bias-into-large-neuroimaging-datasets/]
- 65. Motion Detection and Correction [https://www.brainvoyager.com/bv/doc/UsersGuide/Preprocessing/MotionDetectionAndCorrection.html]
- 66. Motion-correction strategies for enhancing whole-body ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11308502/]
- 67. Interobserver Agreement in Automatic Segmentation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10740636/]
- 68. Dice Coefficient! What is it? - Lathashree Harisha [https://lathashreeh.medium.com/dice-coefficient-what-is-it-ff090ec97bda]
- 69. 20. Validation [https://neuroimaging-data-science.org/content/007-ml/004-validation.html]
- 70. Intraclass correlation [https://en.wikipedia.org/wiki/Intraclass_correlation]
- 71. Regional nigral neuromelanin degeneration in ... [https://www.nature.com/articles/s41598-024-59074-8]
- 72. Machine learning classifiers and fMRI: a tutorial overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2892746/]
- 73. Verifying the concordance between motion corrected and ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1534924/full]
- 74. Verifying the concordance between motion corrected and ... [https://pubmed.ncbi.nlm.nih.gov/40415888/]
- 75. Systematic Review and Meta-analysis of AI-driven MRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425023/]
- 76. Semantic Segmentation vs Instance Segmentation (2025 ... [https://averroes.ai/blog/semantic-segmentation-vs-instance-segmentation]
- 77. AI vs. Manual Customer Segmentation: Key Differences [https://dialzara.com/blog/ai-vs-manual-customer-segmentation-key-differences]
- 78. Iterative Learning for Joint Image Denoising and Motion ... [https://www.sciencedirect.com/science/article/abs/pii/S1361841525004189]
- 79. Reducing motion artefact in high resolution 7T MRI using ... [https://www.medrxiv.org/content/10.1101/2025.10.10.25337727v1.full-text]
- 80. Performance reserves in brain-imaging-based phenotype ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11215805/]
- 81. Best practices in data analysis and sharing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5685169/]
- 82. Medical Image Preprocessing: Key Techniques & Best Practices [https://collectiveminds.health/articles/the-ultimate-guide-to-preprocessing-medical-images-techniques-tools-and-best-practices-for-enhanced-diagnosis]