Advances in Non-Sedated Pediatric MRI: A Research-Focused Review on Motion Artifact Reduction for Enhanced Neuroimaging and Drug Development
This article synthesizes current evidence and methodologies for obtaining high-quality, motion-free pediatric MRI without sedation, a critical objective for minimizing anesthetic neurotoxicity risks and streamlining clinical trial imaging.
Advances in Non-Sedated Pediatric MRI: A Research-Focused Review on Motion Artifact Reduction for Enhanced Neuroimaging and Drug Development
Abstract
This article synthesizes current evidence and methodologies for obtaining high-quality, motion-free pediatric MRI without sedation, a critical objective for minimizing anesthetic neurotoxicity risks and streamlining clinical trial imaging. We explore the foundational rationale, including risks of sedation and parental preferences, and detail a multi-faceted framework of non-pharmacological interventions. This framework encompasses patient preparation strategies, technological advancements in audiovisual distraction, rapid imaging protocols, and motion-correction algorithms. We further evaluate the efficacy and clinical validation of these approaches through recent trial data and discuss optimization strategies for troubleshooting common challenges. For researchers and drug development professionals, this review provides a comprehensive evidence base to support the implementation of robust, sedation-free imaging protocols in pediatric populations, thereby improving safety and data quality in clinical research.
The Imperative for Sedation-Free Pediatric MRI: Risks, Rationale, and Clinical Demand
FAQs: Sedation Neurotoxicity and Risk Mitigation in Pediatric Research
Q1: What is the primary evidence for anesthesia-related neurotoxicity in the developing brain? Preclinical studies demonstrate that exposure to sedatives and anesthetics during critical periods of brain development can cause widespread apoptotic neurodegeneration and permanent neurocognitive impairment. The mechanism is linked to the modulation of NMDA and GABAA receptors, similar to the established neurotoxidrome of fetal alcohol syndrome. In rodent and non-human primate models, exposure to agents like midazolam, nitrous oxide, isoflurane, and ketamine has been associated with neuroapoptosis and persistent deficits in memory, learning, and task performance [1]. The window of vulnerability is during peak synaptogenesis, and effects appear to be dose-dependent, with amplified toxicity from multiple exposures [1].
Q2: How do findings from human studies compare to animal models? Human retrospective studies show an association between early childhood anesthesia exposure and adverse neurodevelopmental outcomes, but the strength of this association is weak (hazard ratios typically less than 2) and inconsistent [1]. Crucially, recent high-quality prospective studies suggest that single, brief exposures (under one hour) do not produce measurable neurodevelopmental deficits. The General Anesthesia Compared to Spinal Anesthesia (GAS) trial found no evidence of adverse neurodevelopment at 2 years of age in neonates receiving brief sevoflorane anesthesia [1]. Similarly, the Pediatric Anesthesia NeuroDevelopment Assessment (PANDA) study found no difference in IQ scores among healthy children exposed to a single anesthetic before 36 months of age compared to their unexposed siblings [1]. However, higher cumulative doses of specific agents like ketamine have been associated with poorer motor performance at 18 months in vulnerable populations, such as infants with congenital heart disease [2].
Q3: What is the clinical significance of the FDA warning on anesthetic and sedative drugs? The U.S. Food and Drug Administration (FDA) has mandated a warning label indicating that repeated or lengthy (>3 hours) use of general anesthetic and sedation drugs during surgeries or procedures in children younger than 3 years or in pregnant women during the third trimester may affect the child's developing brain [1]. This warning is based largely on robust animal data. The clinical consensus, endorsed by organizations like SmartTots, the American Academy of Pediatrics, and the Society for Pediatric Anesthesia, is that concerns about the unknown risk of anesthetic exposure must be weighed against the potential harm of canceling or delaying a needed procedure [1].
Q4: What are the primary strategies for reducing sedation in pediatric MRI? Strategies can be categorized as follows:
- Behavioral and Non-Pharmacological: Parental presence, feed-and-swaddle techniques for infants, mock MRI scanners, child life specialist-led preparation, video goggles, and scheduling scans during evening hours to leverage natural sleep cycles [3] [4] [5].
- Technical and Protocol-Based: Using accelerated imaging techniques like parallel imaging, compressed sensing, and simultaneous multislice acquisition to shorten scan times. Employing motion-robust sequences like radial sampling to minimize motion artifacts without sedation [6] [7].
- Protocol Abbreviation: Focusing imaging protocols on essential "reporting elements" for a specific clinical indication to avoid unnecessary sequences and reduce the time a child must remain still [7].
Table 1: Key Findings from Human Studies on Anesthesia/Sedation Exposure and Neurodevelopment
| Study (Design) | Population | Exposure | Findings |
|---|---|---|---|
| GAS Trial [1] (Randomized Controlled Trial) | Neonates undergoing hernia repair | General anesthesia (sevoflorane) <1 hour vs. spinal anesthesia | No evidence of adverse neurodevelopment at 2 years of age. |
| PANDA Study [1] (Sibling-Matched Cohort) | Healthy children with inguinal hernia repair | Single anesthetic exposure before 36 months | No difference in IQ scores in later childhood compared to unexposed siblings. |
| Wilder et al. [1] (Retrospective Birth Cohort) | Children <4 years | Varied; single vs. multiple exposures | Two-fold increase in risk of learning disabilities among multiply exposed children. |
| Congenital Heart Disease Cohort [2] (Prospective Observational) | Infants with congenital heart disease | Cumulative inpatient sedative/anesthetic exposure | Each mg/kg increase in ketamine exposure was associated with a 0.34 point decrease in Bayley-III Motor scores at 18 months. No association found for volatile anesthetics, opioids, or benzodiazepines. |
Table 2: Efficacy of Non-Sedation Strategies for Pediatric MRI
| Intervention | Study Design | Population | Key Outcome |
|---|---|---|---|
| Parental Presence [3] | Randomized Controlled Trial | Children 3-10 years | Significantly improved MRI success without sedation in children aged 3-6 years (OR=6.50). No significant benefit in children 7-10 years. |
| Movie Watching & Real-time Feedback [8] | Behavioral Intervention | Children 5-15 years | Head motion was significantly reduced during movie watching and when receiving real-time feedback, with effects driven by children aged 5-10 years. |
| Accelerated/Abbreviated Protocols [7] | Technical Review | Pediatric patients | Using accelerated imaging and protocol abbreviation based on clinical indication can reduce or eliminate the need for sedation. |
Experimental Protocols: Detailed Methodologies
Protocol 1: Evaluating Parental Presence for Non-Sedated MRI This protocol is based on a prospective, single-center, randomized controlled trial [3].
- Participant Recruitment: Children aged 3–10 years referred for pituitary MRI due to suspected growth hormone deficiency. Exclusions include diagnosed intellectual disability or neurodevelopmental disorder.
- Randomization: Participants are stratified by age (3–6 and 7–10 years) and randomly assigned to "parent present" or "parent absent" groups using block randomization.
- Preparation: All children receive standardized MRI preparation from a child life specialist or pediatrician, including verbal reassurance, printed materials, and a soft toy with a wooden mock MRI scanner.
- Intervention: For the "parent present" group, a parent accompanies the child into the scan room, sits on a chair next to the scanner, and is instructed to remain calm and speak gently to help prevent movement. In the "parent absent" group, a radiologic technologist accompanies the child.
- Outcome Measures:
- Step 1 - Completion: Successful completion of all MRI sequences.
- Step 2 - Image Quality: Blinded evaluation of image artifacts (none, mild, or severe).
- Step 3 - Final Success: Completion of MRI with no or only mild artifacts.
Protocol 2: Systematic Neurotoxicity Assessment in Immunotherapy Trials This protocol was developed for prospective evaluation of neurotoxicity in a Phase I anti-CD22 CAR-T cell trial [9].
- CNS Disease Evaluation: Includes routine lumbar punctures pre- and post-therapy for CSF analysis (cell count, protein, glucose, cytospin, flow cytometry for CAR-T cells) and a baseline brain MRI.
- Cognitive Assessment: A brief cognitive battery administered pre- and post-infusion by a psychologist, assessing:
- Attention and Cognitive Flexibility: Dimensional Change Card Sort Test (DCCS).
- Inhibitory Control: Flanker Inhibitory Control and Attention Test.
- Working Memory: List Sorting Working Memory Test.
- Processing Speed: Wechsler Processing Speed Index (Symbol Search and Cancellation subtests).
- Neurologic Symptom Checklist (NSC): An observer-reported checklist completed by the caregiver at baseline, day 14, and day 21-28. It rates the severity and duration of symptoms like hallucinations, disorientation, and depressed mood.
- Biomarker Analysis: Serial serum cytokine levels are measured and correlated with neurotoxicity symptoms and severity to explore etiology.
Signaling Pathways and Experimental Workflows
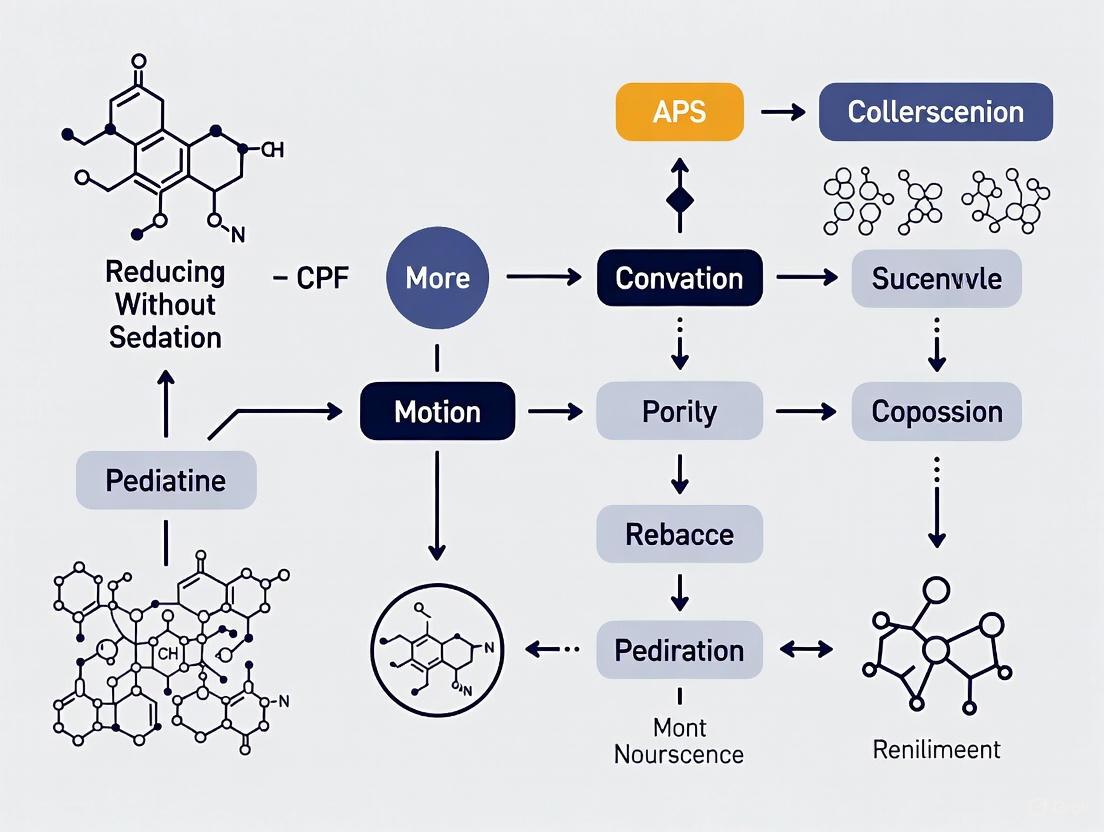
Diagram 1: Anesthetic Neurotoxicity Pathway
Diagram 2: Non-Sedated MRI Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Pediatric Neurotoxicity and Imaging Research
| Item / Reagent | Function / Application | Specific Examples / Notes |
|---|---|---|
| Bayley Scales of Infant & Toddler Development, 3rd Ed. (Bayley-III) | Gold-standard assessment of neurodevelopment in infants and toddlers (1-42 months). Provides composite scores for cognitive, language, and motor domains. | Used as a primary outcome measure in clinical studies like the GAS trial and cardiac cohort studies [1] [2]. |
| NIH Toolbox Cognition Battery | Computerized battery for assessing cognitive function in children and young adults. Efficient for serial testing. | Includes Dimensional Change Card Sort (cognitive flexibility), Flanker (inhibitory control), and List Sorting (working memory) tests [9]. |
| Wechsler Processing Speed Index (PSI) | Paper-and-pencil test from Wechsler intelligence scales to assess cognitive processing speed. | Comprises Symbol Search and Cancellation subtests; used in conjunction with other batteries [9]. |
| Neurologic Symptom Checklist (NSC) | Observer-reported checklist to systematically capture the type, severity, and duration of neurotoxic symptoms. | Custom-developed for CAR-T trials; can be adapted for sedation studies to document subtle symptoms [9]. |
| Accelerated MRI Sequences | Technical methods to reduce scan time and motion sensitivity, enabling non-sedated MRI. | Includes Parallel Imaging, Compressed Sensing, Simultaneous Multi-Slice, and Radial Sampling [6] [7]. |
| Mock MRI Scanner | A simulated MRI environment used to acclimate children to the sounds and confinement of a real scan. | Often made of wood or other non-magnetic materials; used with toy models for play therapy to reduce anxiety [3] [5]. |
FAQs for a Pediatric Imaging Research Core
FAQ 1: What are the most effective non-sedation techniques for reducing motion in pediatric MRI, and what is their typical success rate?
Several non-sedation techniques have proven effective. A 2025 quality improvement project demonstrated that audiovisual distraction (AVD) technology, when implemented as part of a structured "awake MRI" program, reduced the need for minimal and moderate sedation by 28.8 percentage points while maintaining a 100% diagnostic success rate across the cohort [10]. Furthermore, a 2025 randomized controlled trial found that for children aged 3-6 years, the simple, low-cost intervention of parental presence in the MRI room significantly improved the success rate of non-sedated MRI, with a success rate of 59.1% compared to 18.2% when the parent was absent [11]. These methods are complemented by preparatory techniques involving certified child life specialists and mock scanner training [10] [11].
FAQ 2: Which advanced imaging techniques can help salvage a study affected by motion artifacts?
Beyond behavioral techniques, technological and methodological advancements are crucial for mitigating motion. The following table summarizes key methods, particularly for abdominal MRI, where motion is a significant challenge [6]:
| Method | Brief Explanation | Primary Benefit |
|---|---|---|
| Parallel Imaging | Accelerates data acquisition by using multiple receiver coils. | Reduces scan time, thereby decreasing the window for motion. |
| Simultaneous Multislice Imaging | Acquires multiple MRI slices at the same time. | Significantly shortens acquisition time. |
| Radial k-Space Sampling | Acquires data in a radial pattern, making it less sensitive to motion. | Inherently motion-insensitive, dispersing artifacts. |
| Compressed Sensing | Acquires fewer data points and uses algorithms to reconstruct the image. | Enables high-quality images from undersampled data, cutting scan time. |
| AI-Based Reconstruction | Uses deep learning models to reconstruct images from limited data. | Reduces scan times and can correct for motion artifacts [10]. |
For post-processing, deep learning methods, particularly Generative Adversarial Networks (GANs), show promise in actively correcting motion artifacts in already-acquired images, potentially saving time and money by reducing the need for repeat scans [12].
FAQ 3: From a logistical standpoint, how can we improve workflow efficiency to reduce patient wait times and increase scanner throughput?
Optimizing patient flow logistics (PFL) is essential. Studies show that structured PFL interventions can drastically reduce hospital length of stay and emergency department boarding [13]. Key strategies include:
- Real-Time Dashboards: Implementing dashboards to monitor key performance indicators (KPIs) allows for rapid identification of bottlenecks and reallocation of resources [13].
- Process Mapping and Redesign: Analyze the patient journey from scheduling to discharge to eliminate redundancies. This can include implementing online pre-registration and staggered appointment scheduling to smooth patient flow [14] [15].
- Predictive Analytics: Using historical data to forecast busy periods and adjust staffing and scheduling accordingly prevents bottlenecks before they occur [14].
Troubleshooting Guides
Guide 1: Addressing High Sedation Rates in a Research Cohort
Problem: A high percentage of pediatric research participants in your study require sedation to complete MRI scans, introducing cost, risk, and logistical complexity.
Solution: Implement a systematic, tiered screening and intervention protocol.
Diagram: Tiered Screening and Intervention Protocol for Non-Sedated MRI.
Steps:
- Pre-Appointment Screening: Triage patients based on age, developmental level, and past medical experiences. Children 4 years and older should be considered potential candidates for non-sedated MRI [10].
- In-Person Assessment: On the day of the scan, a team (e.g., certified child life specialist, nurse, sedation provider) assesses the child's anxiety, understanding, and temperament [10].
- Apply Tiered Interventions:
- Failover Protocol: For children who cannot tolerate the scan without sedation, have a protocol for immediate, same-day sedation to avoid rescheduling and delays, thus maintaining workflow efficiency [10].
Guide 2: Managing Motion Artifacts in Acquired Image Data
Problem: Acquired research MRI datasets are degraded by motion artifacts, compromising their diagnostic and analytical quality.
Solution: A combined approach of proactive acquisition and post-processing correction.
Diagram: Decision Workflow for Managing Motion Artifacts.
Steps:
- Prevention: Utilize fast acquisition sequences like parallel imaging or compressed sensing to minimize the time during which motion can occur [6].
- Assessment: Determine the severity of the artifact and whether the participant can tolerate a repeat sequence.
- Action:
- If reseaming is feasible: Re-acquire the images using a more motion-robust sequence (e.g., radial k-space sampling) [6].
- If reseaming is not feasible: Employ a post-processing correction algorithm. Deep learning models, particularly those based on a Generative Adversarial Network (GAN) framework, have been shown to effectively remove motion artifacts, restoring image quality for analysis [12].
Experimental Protocols
Protocol 1: Implementing an Audiovisual Distraction (AVD) Program
This protocol is based on a successful quality improvement project that reduced sedation use by 28.8% [10].
- Objective: To establish a reproducible workflow for conducting pediatric MRI without sedation using in-bore AVD technology.
- Materials:
- MRI-compatible AVD system (e.g., MRI in-bore video projector).
- Standard clinical MRI scanner.
- Multidisciplinary team (radiologists, technologists, sedation providers, certified child life specialists).
- Methodology:
- Planning: Convene a stakeholder group to design the workflow and select appropriate AVD technology.
- Screening: Identify eligible patients (e.g., initially ages 7+, expanding to 4+, without severe developmental delays) during the scheduling process [10].
- Preparation: On the day of the scan, a child life specialist or nurse prepares the child using age-appropriate explanations and mock scanners.
- In-Room Procedure: The child is positioned in the scanner. The AVD system is activated, and the child selects a movie. A parent may be present to provide additional comfort.
- Exit Strategy: If the child becomes distressed and cannot continue, a pre-arranged protocol for same-day sedation is activated to avoid rescheduling [10].
- Outcome Measures:
- Primary: Percentage reduction in minimal/moderate sedation use.
- Secondary: Rate of diagnostic quality studies, percentage of studies completed within allotted exam time.
Protocol 2: Randomized Controlled Trial of Parental Presence
This protocol summarizes the methods from a 2025 prospective RCT [11].
- Objective: To quantitatively evaluate the effect of parental presence on the success rate of non-sedated pituitary MRI in children aged 3-10 years.
- Materials:
- Standard 1.5T or 3T MRI scanner.
- Soft toy and wooden mock MRI scanner for preparation.
- Subject Population: Children aged 3-10 years requiring MRI for short stature evaluation, excluding those with known intellectual disabilities.
- Methodology:
- Randomization: Participants are stratified by age (3-6 and 7-10 years) and randomly assigned to "parent present" or "parent absent" groups using block randomization [11].
- Intervention: For the "parent present" group, a parent sits on a chair next to the MRI scanner, within reach of the child, and is instructed to speak gently to prevent movement. In the "parent absent" group, a radiologic technologist accompanies the child.
- Blinding: Image quality is assessed by pediatricians blinded to the group assignment.
- Outcome Assessment: Success is evaluated in three steps:
- Step 1: Completion of all MRI sequences.
- Step 2: Image quality (no, mild, or severe artifacts).
- Step 3: Final success, defined as completion with no or only mild artifacts [11].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key non-pharmacological "reagents" or tools for a research program focused on reducing motion without sedation.
| Item / Solution | Function in the Research Context |
|---|---|
| MRI-Compatible AVD System | The core technological intervention for behavioral distraction; projects video content into the MRI bore to engage pediatric patients and reduce anxiety and movement [10]. |
| Certified Child Life Specialist (CCLS) | A specialized human resource who prepares children for procedures using developmental support, education, and mock scanners to increase cooperation and success rates [10] [11]. |
| Mock MRI Scanner | A non-functioning replica of an MRI scanner used to acclimate children to the environment, sounds, and confinement, reducing fear and failure rates [11]. |
| Motion-Robust MRI Sequences | Advanced pulse sequences (e.g., radial k-space, compressed sensing) that are less susceptible to motion artifacts, serving as a technical buffer against data loss [6]. |
| AI-Based Artifact Correction Software | A computational tool employing deep learning (e.g., GANs) to post-process and correct for motion artifacts in image data, salvaging otherwise non-diagnostic scans [12]. |
| Parental Presence Protocol | A standardized operational guideline defining the role and positioning of a parent within the MRI suite to provide comfort and improve the child's ability to remain still [11]. |
This technical support guide provides resources for researchers investigating methods to reduce motion artifacts in pediatric medical imaging without sedation. A primary challenge in this field is that patient motion during scanning compromises image quality, often necessitating sedation with its associated risks, costs, and neurodevelopmental concerns. This document synthesizes current evidence and provides practical protocols for implementing and evaluating non-sedation approaches, with a specific focus on parental involvement and patient-centered care strategies.
Frequently Asked Questions (FAQs): Core Concepts in Sedation-Free Imaging
Q1: What is the evidence for parental presence as a motion-reduction strategy? A1: Recent Level I evidence demonstrates that parental presence significantly improves MRI success rates without sedation, particularly in young children. A 2025 randomized controlled trial found that for children aged 3-6 years, scan completion rates were significantly higher when a parent was present (59.1%) compared to when the child was alone (18.2%) [3] [11]. The final success rate (completion with no or mild artifacts) was significantly higher in the parent-present group for this age subgroup, with an odds ratio of 6.50 [3].
Q2: How do technological and preparation interventions compare in effectiveness? A2: Different non-pharmacological approaches show varying effectiveness across age groups, as summarized in Table 1 below. Multi-faceted programs that combine preparation, environmental modification, and distraction typically yield the highest success rates.
Q3: What factors should inform patient selection for non-sedated protocols? A3: Key considerations include:
- Age: Children 3-6 years benefit most from parental presence; those ≥7 years often succeed with preparation alone [3] [11]
- Developmental status: Children with neurodevelopmental disorders often require specialized approaches [16]
- Scan characteristics: Protocol length and motion sensitivity significantly impact success [16]
- Temperament: Baseline anxiety levels influence intervention selection [17]
Q4: How can researchers objectively measure intervention success? A4: Standardized metrics include:
- Completion rate: Percentage of scans fully acquired [3] [16]
- Image quality: Blindly scored artifact assessment using standardized scales [3] [18] [17]
- Anxiety measures: Validated instruments like the State-Trait Anxiety Inventory for Children [17]
- Process measures: Scan time, need for rescans, parental satisfaction [19]
Troubleshooting Guides: Implementing Non-Sedation Protocols
Guide: Implementing Parental Presence Protocols
Problem: Inconsistent implementation of parental presence reduces potential benefits. Solution: Standardize parental involvement through this workflow:
Validation Data: This protocol achieved 70.0% final success rate versus 55.0% in parent-absent groups, with the most significant benefits in children aged 3-6 years (P=0.012) [3].
Guide: Optimizing Scan Environment and Protocols
Problem: Standard MRI environments increase pediatric anxiety and motion. Solution: Implement child-centered modifications:
- Acoustic noise reduction: Apply quiet imaging sequences (e.g., Quiet Suite) with maximal noise reduction for localizer scans [3]
- Visual modifications: Use projected visuals/themes in bore; coordinate lighting [19]
- Rapid imaging protocols: Implement parallel imaging, simultaneous multisection imaging, and compressed sensing [18] [16]
- Mock scanner training: Familiarize children using toy scanners and simulation [19]
Technical Specifications: Optimized protocols reduced average scan duration from 45±10 minutes to approximately 20-25 minutes while maintaining diagnostic quality [18] [17].
Quantitative Outcomes: Evidence Tables for Research Design
Table 1: Comparative Effectiveness of Non-Sedation Interventions
| Intervention Type | Age Group | Success Rate | Key Metrics | Study Design |
|---|---|---|---|---|
| Parental Presence [3] [11] | 3-6 years | 70.0% | OR=6.50 (95% CI: 1.64-25.76) for final success | RCT, n=80 |
| Audiovisual Distraction (AVD) [16] | 4-18 years | 100% completion | 28.8% reduction in sedation use | Quality Improvement, n=92 |
| Child-Centered Care Program [19] | 4-10 years | 88% child comfort | 92% parental security vs. 79% control | Prospective Survey, n=265 |
| Audiovisual Preparation [17] | 7-11 years | Significantly improved image quality (P=0.005) | Reduced state anxiety (P=0.004) | RCT, n=48 |
Table 2: Motion Artifact Classification for Image Quality Assessment
| Artifact Grade | Definition | Research Implications | Sample Distribution |
|---|---|---|---|
| None | No motion artifacts detected; fully diagnostic | Optimal for quantitative analysis | 23/52 (44.2%) [3] |
| Mild | Minor artifacts not affecting diagnostic quality | Acceptable for most clinical research | 27/52 (51.9%) [3] |
| Severe | Significant artifacts compromising diagnostic utility | Requires scan repetition or exclusion | 2/52 (3.8%) [3] |
Experimental Protocols: Standardized Methodologies for Research
Protocol: Randomized Evaluation of Parental Presence
Objective: To quantitatively assess the impact of parental presence on MRI success rates without sedation.
Population: Children aged 3-10 years without neurodevelopmental disorders [3].
Stratification and Randomization:
- Stratify by age groups (3-6 and 7-10 years)
- Use block randomization within strata (blocks of 4)
- Allocate to parent present vs. absent groups [3] [11]
Intervention Protocol:
- Parent present group: Parent accompanies child, sits beside scanner, provides calm reassurance
- Parent absent group: Child accompanied by radiologic technologist only
- Standardized preparation: Both groups receive identical preparation by child life specialist or pediatrician [3]
Outcome Assessment:
- Step 1 - Completion: Ability to complete all MRI sequences
- Step 2 - Image Quality: Blinded assessment of artifacts (none, mild, severe)
- Step 3 - Final Success: Completion with no or mild artifacts only [3]
Statistical Considerations:
- Sample size: 40 per group (total n=80) provides adequate power for primary endpoint
- Analysis: Intention-to-treat with appropriate tests for categorical outcomes [3]
Protocol: Implementation of Audiovisual Distraction Systems
Equipment Setup:
- MRI-compatible AVD system (e.g., in-bore video projection)
- Child-friendly content selection (validated for anxiety reduction)
- Hearing protection with integrated audio capability [16] [17]
Patient Selection Criteria:
- Inclusion: Age ≥4 years, head-first positioning, scan duration <60 minutes (initial phase)
- Exclusion: Visual impairment, severe developmental delay, severe ASD [16]
Implementation Workflow:
Quality Control: All studies reviewed by radiologist before exam conclusion; motion sensitivity scoring for protocol optimization [16].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Pediatric Imaging Research
| Research Tool | Specifications | Research Application | Evidence |
|---|---|---|---|
| Mock MRI Scanner | Wooden or plastic simulator with noise playback | Patient familiarization and training | [3] [19] |
| Audiovisual Distraction System | MRI-compatible projection with child-friendly content | Anxiety reduction during scanning | [16] [17] |
| Standardized Anxiety Assessment | State-Trait Anxiety Inventory for Children (STAIC) | Quantifying intervention effectiveness | [17] |
| Image Quality Rating Scale | 3-point artifact scale (none, mild, severe) | Primary outcome assessment | [3] |
| Child Life Specialist Protocol | Standardized preparation and support procedures | Ensuring consistent patient preparation | [3] [16] |
| Accelerated MRI Sequences | Parallel imaging, compressed sensing, AI reconstruction | Reducing scan time and motion sensitivity | [18] [16] |
Motion artifacts represent one of the most significant obstacles in pediatric magnetic resonance imaging (MRI), often rendering scans non-diagnostic and compromising research outcomes. Unlike adult patients, children present unique physiological and psychological challenges that complicate motion-free imaging. The conventional solution of sedation introduces its own risks, including potential neurotoxicity and respiratory complications, driving the urgent need for effective non-pharmacological motion mitigation strategies. This technical support guide examines the fundamental barriers to motion-free imaging in children and provides evidence-based troubleshooting methodologies for researchers and clinical scientists working to reduce sedation in pediatric imaging research.
Frequently Asked Questions: Understanding Motion in Pediatric Imaging
What specific types of motion most severely degrade pediatric image quality?
Research utilizing electromagnetic motion tracking has identified key metrics that correlate with image quality degradation. In a study of 77 pediatric patients, both motion-free time (as a ratio of total scan time) and average displacement from a reference position were highly correlated with image quality, whereas maximum displacement was a less reliable predictor. Notably, 14.3% of patients with average displacements greater than 0.5 mm and 18.2% with less than 90% motion-free time resulted in non-diagnostic images [20]. The most problematic motions are those occurring during the acquisition of k-space center, which generate more pronounced artifacts [20] [21].
Which age groups present the greatest challenges for non-sedated imaging?
Success rates for non-sedated MRI vary significantly by developmental stage. Children aged 3-6 years present particular difficulties, with one study showing only 18.2% completion rates without parental presence. However, with intervention strategies like parental presence, completion rates in this age group can increase to 59.1% [3]. Infants (0-2 years) often respond well to feed-and-wrap techniques, while children over 7 years generally demonstrate better cooperation, especially with distraction techniques [18] [22] [3].
What are the quantified risks of sedation that justify alternative approaches?
Recent evidence indicates that 8.6% of children under sedation/anesthesia experience adverse events, with 57.7% of these occurring during MRI scans [20]. A 2025 quality improvement project reported that institutional sedation rates for pediatric MRI referrals reached 92% prior to implementing alternatives, with 55% requiring deep sedation [16]. These risks, coupled with concerns about potential neurotoxicity, have accelerated the development of non-sedated imaging protocols [23] [16].
How effective are current motion correction technologies?
Emerging technologies show promising results. The Scout Accelerated Motion Estimation and Reduction (SAMER) technique, evaluated in 2025, demonstrated motion artifact improvement in 79% of cases (19/24), with 50% of previously non-diagnostic cases reclassified as diagnostic after correction [24]. Deep learning-based reconstruction techniques like Deep Resolve have enabled scan time reductions of up to 50% for musculoskeletal protocols while maintaining diagnostic quality [22].
Troubleshooting Guide: Implementing Non-Sedated Imaging Protocols
Preparation Phase Challenges
Problem: Patient anxiety and non-cooperation during positioning
Solution: Implement comprehensive preparation protocols
- Mock scanner training: Utilize practice sessions with simulated MRI environments to familiarize children with the procedure [3] [16].
- Preparation media: Develop institution-specific videos demonstrating the MRI process, facilities, and staff to reduce pre-procedural anxiety [22].
- Child Life Specialist involvement: Engage specialists to provide age-appropriate explanation and coping strategies [3] [16].
- Parental education: Instruct parents on preparation techniques, including keeping infants awake before appointments and timing feeding schedules [22] [21].
Problem: Inadequate screening for procedure suitability
Solution: Establish tiered assessment criteria
- Develop motion sensitivity scores for different protocols to match patient capabilities with appropriate techniques [16].
- Implement in-person assessments by Child Life Specialists, nurses, and sedation providers to evaluate cooperation potential [16].
- Consider developmental age, previous medical experiences, and specific anxieties when determining approach [3].
Acquisition Phase Challenges
Problem: Motion artifacts degrading image quality
Solution: Implement multi-layered motion mitigation strategies
Table: Motion Reduction Techniques and Applications
| Technique | Mechanism | Best Applications | Efficacy |
|---|---|---|---|
| Fast Imaging Sequences (GRE, EPI, bSSFP) | Reduced acquisition time | All pediatric populations, especially uncooperative children | Scan time reduction up to 50% [22] |
| Parallel Imaging | Simultaneous data acquisition with multiple coils | General pediatric imaging | 40% scan time reduction [3] |
| Compressed Sensing | Random k-space undersampling with iterative reconstruction | 3D isotropic imaging | Isotropic 3D MRI in under 3 minutes [21] |
| Radial k-space Sampling (PROPELLER/BLADE) | Oversampling of k-space center | High-contrast structures (neuroimaging) | Effective for moderate motion [21] |
| SAMER Method | Retrospective motion correction using scout data | Brain imaging in awake patients | 79% improvement in motion artifacts [24] |
Problem: In-bore anxiety and movement during acquisition
Solution: Create supportive scanning environment
- Audiovisual distraction: Implement MRI-compatible systems allowing movie viewing or music listening during scans [22] [16].
- Parental presence: Allow parents to remain within reach of the child during scanning, particularly effective for ages 3-6 years [3].
- Proper immobilization: Use specialized pediatric positioning aids, foam padding, and vacuum immobilizers to minimize movement while maintaining comfort [22] [21] [25].
- Acoustic noise reduction: Utilize quiet imaging sequences, hearing protection, and noise-insulating techniques to reduce startle responses [3] [16].
Technical Optimization Challenges
Problem: Suboptimal protocol parameters for pediatric populations
Solution: Implement age-specific protocol modifications
Table: Age-Specific Protocol Considerations
| Age Group | Key Challenges | Recommended Technical Adjustments | Success Rate Improvements |
|---|---|---|---|
| Infants (0-2 years) | Inability to follow instructions, temperature regulation | Feed-and-wrap technique, smaller FOV, thinner slices, longer TR for improved SNR | 90-95% success with feed-and-wrap [16] |
| Young Children (3-6 years) | High anxiety, limited impulse control | Parental presence, rapid sequences, AVD, immobilization devices | Completion increased from 18.2% to 59.1% with parental presence [3] |
| Older Children (7+ years) | Boredom, discomfort with prolonged stillness | Audiovisual distraction, explanation of procedure, comfortable positioning | 75% completion with AVD vs. 55% without [3] [16] |
Problem: Balancing scan time with diagnostic image quality
Solution: Implement accelerated protocols with AI reconstruction
- Utilize deep learning-based reconstruction (e.g., Deep Resolve) to maintain image quality despite reduced acquisition times [22].
- Develop protocol-specific acceleration factors based on motion sensitivity scores [16].
- Combine multiple acceleration techniques (parallel imaging + compressed sensing) for synergistic time reduction [21].
Experimental Protocols and Methodologies
Protocol 1: Awake MRI Program with Audiovisual Distraction
Based on quality improvement project with 320 patients [16]
Inclusion Criteria:
- Age ≥4 years (initially ≥7 years, expanded after PDSA cycles)
- Head-first MRI position
- Any scan duration (initially <60 minutes, restrictions removed)
- Absence of severe developmental delay or autism spectrum disorder
Workflow:
- Pre-procedural screening: Identification of eligible candidates through clinical information review and family communication
- In-person assessment: Evaluation by Child Life Specialist, nurse, and sedation provider on day of scan
- AVD setup: Installation of MRI-compatible video projection system (e.g., MRI in-bore video system)
- Positioning: Head-first positioning with appropriate immobilization devices
- Acquisition: Implementation of accelerated MRI protocols with noise reduction techniques
- Contingency planning: Immediate conversion to sedation for failed awake attempts
Outcomes: 28.8 percentage point reduction in minimal/moderate sedation use, 100% diagnostic quality achieved in AVD group, 96% of studies completed within allotted exam time [16]
Protocol 2: Quantitative Motion Measurement and Correlation
Based on study of 77 pediatric patients [20]
Motion Tracking Method:
- Electromagnetic tracker with two forehead sensors
- Modified T1-weighted 3D GRE sequence with embedded bipolar gradients
- Real-time position recording relative to magnet isocenter
- Accuracy: +/- 0.1 mm (phantom-validated)
Motion Metrics:
- Maximum displacement from reference position
- Mean displacement from reference (when k-space center acquired)
- Motion-free time (% of scan with <0.2 mm displacement)
Image Quality Assessment:
- Blind radiologic evaluation using 4-point Likert scale
- Grade 1: Non-diagnostic (severe motion artifacts)
- Grade 4: No visible motion artifacts
Key Findings: Both motion-free time ratio and average displacement highly correlated with image quality, providing thresholds for predicting diagnostic acceptability [20]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Resources for Pediatric Motion-Free Imaging Research
| Item | Function/Application | Example Products/Protocols |
|---|---|---|
| Electromagnetic Motion Tracking | Quantitative measurement of patient motion during acquisition | Robin Medical Inc. tracker [20] |
| MRI-Compatible Audiovisual Systems | Patient distraction and anxiety reduction during scanning | NordicNeuroLab AS visualization systems; PDC Inc. in-bore video projection [22] [16] |
| Pediatric Immobilization Devices | Gentle motion restriction while maintaining comfort | Pearl Technology Multipads; Domico Med-Device Huggers, MedVac Immobilization System [22] [25] |
| Accelerated MRI Sequences | Reduced acquisition time to minimize motion opportunities | Deep Resolve; PROPELLER; Compressed Sensing; Parallel Imaging [22] [21] |
| Motion Correction Algorithms | Retrospective correction of motion artifacts in acquired data | SAMER (Scout Accelerated Motion Estimation and Reduction) [24] |
| Quiet Imaging Packages | Acoustic noise reduction to minimize startle response | Siemens Quiet Suite [3] |
| Mock MRI Scanners | Patient preparation and anxiety desensitization | Wooden mock scanners; simulation environments [3] [16] |
Experimental Workflow and Decision Pathways
Research Gaps and Future Directions
Despite significant advances, several research challenges remain in optimizing motion-free pediatric imaging. Future research priorities include:
- Predictive Modeling: Development of robust algorithms to predict individual patient motion risk based on age, developmental stage, and previous medical experiences
- Real-Time Adaptive Imaging: Creation of MRI sequences that dynamically adjust to detected motion during acquisition
- Standardized Outcome Metrics: Establishment of consensus measures for motion artifact quantification and image quality assessment across research studies
- Cost-Benefit Analysis: Comprehensive evaluation of the economic and clinical tradeoffs between sedation and non-sedated imaging protocols
- Novel Sensor Technologies: Integration of non-contact motion detection systems (camera-based, physiological monitoring) for more accurate motion tracking
The field continues to evolve rapidly, with artificial intelligence playing an increasingly central role in both acquisition acceleration and motion correction. By addressing these fundamental physiological and psychological barriers, researchers can continue to advance toward the ultimate goal of reliable, diagnostic-quality pediatric imaging without sedation.
A Multimodal Toolkit: Evidence-Based Techniques for Motion Reduction Without Sedation
Minimizing motion artifacts is a critical challenge in pediatric magnetic resonance imaging (MRI) research. The use of sedation, while effective for ensuring stillness, carries risks including respiratory depression, potential neurotoxicity, and prolonged hospital visits, making non-sedation approaches methodologically and ethically preferable for research protocols [16] [10]. This guide details evidence-based, non-pharmacological strategies for successful MRI acquisition in child participants. Implementing these patient preparation and environmental adaptation techniques is essential for reducing data loss, improving image quality, and upholding the highest ethical standards in developmental neuroscience and pediatric drug development research.
Troubleshooting Guides and FAQs for Common Research Scenarios
FAQ 1: Which children are the best candidates for non-sedated MRI in a research setting? Success is highly age-dependent. Children aged 3-6 years represent the most challenging cohort, but studies show parental presence can significantly improve success rates in this group [3] [11]. Older children (7-10 years) are often capable of following instructions and may benefit less from parental presence but more from technological aids like audiovisual distraction (AVD) [3] [16]. For infants, the feed-and-swaddle technique is highly effective, with success rates ranging from 90-95% [16] [26]. Researchers should screen for neurodevelopmental disorders, severe anxiety, or sensory impairments that may require alternative strategies [16] [10].
FAQ 2: A participant cannot tolerate the scanner noise. What are the immediate steps? First, ensure universal hearing protection is correctly applied, using both earplugs and noise-attenuating headphones [26]. Second, employ "quiet" MRI scanning sequences. These protocols, available on modern scanners (e.g., Siemens' Quiet Suite), can significantly reduce acoustic noise by modifying gradient slew rates and pulse sequences [3] [27]. As a preemptive measure, incorporate exposure to recorded scanner noises during mock training sessions to desensitize participants [3] [28].
FAQ 3: How can we predict which participants will succeed without sedation? While no single predictor is perfect, a pre-scan behavioral assessment is highly recommended. This can be conducted by a child life specialist or a trained researcher and should evaluate the child's temperament, anxiety level, and understanding of the procedure [16] [10]. Interestingly, a study found that easily obtainable factors like "crying during routine vaccinations" or "number of siblings" were not reliable predictors of MRI success, underscoring the need for a tailored, in-person assessment [3] [29].
FAQ 4: What is the first-line intervention for a young child (3-6 years) showing distress during scan preparation? The evidence strongly supports implementing parental presence as a first-line strategy. A recent randomized controlled trial demonstrated that for children aged 3-6 years, having a parent in the scan room significantly increased the completion rate from 18.2% to 59.1% [3] [11]. Instruct the parent to remain calm, speak gently to their child, and provide reassurance without physical intervention that could cause motion [3].
FAQ 5: Our motion artifact rates are high despite participant cooperation. What technical solutions can we implement? Integrate advanced acquisition and reconstruction technologies into your protocol. Parallel imaging and simultaneous multi-slice scanning can reduce scan time, thereby decreasing the window for motion [16] [18]. Furthermore, utilize motion correction algorithms, which can be based on external optical tracking or software-based navigators [27] [18]. For post-processing, artificial intelligence (AI) and deep learning models are now capable of reconstructing high-quality images from motion-corrupted data and performing super-resolution enhancement [27].
The following tables consolidate key performance metrics for various interventions, providing a basis for protocol selection and power calculations.
Table 1: Success Rates of Primary Non-Sedation Interventions
| Intervention | Target Age Group | Reported Success Rate / Key Metric | Key Research Context |
|---|---|---|---|
| Parental Presence [3] | 3-6 years | 59.1% completion rate vs. 18.2% without parent | Prospective RCT; pituitary MRI |
| Audiovisual Distraction (AVD) [16] | 4-18 years | 100% completion (92/92 patients); 28.8% reduction in sedation use | Quality improvement project |
| Mock Scanner Training [28] | 6-9 years | Significant reduction in head motion after a 5.5-minute training | Growth curve study |
| Feed-and-Swaddle [26] | Infants | 51% of sites reported >75%-100% success | International survey |
| Child Life Specialist [26] | Children/Teens | Most sites reported >50%-75% success; crucial for preparation | International survey |
Table 2: Impact of Protocol Optimization on Key Workflow Metrics
| Performance Metric | Before Optimization [18] | After Optimization [18] | Key Changes Implemented |
|---|---|---|---|
| Mean Scan Duration | 45 ± 10 minutes | 25 ± 7 minutes | Fast sequences (e.g., single-shot FSE), parallel imaging |
| Sedation Rate | 70% | 25% | Combined non-pharmacological strategies & protocol tweaks |
| Scans with Motion Artifacts | 40% (in infants & young children) | Significantly reduced (p<0.05) | Motion correction software, age-specific parameters |
Detailed Experimental Protocols
Protocol for Parental Presence in MRI
This protocol is based on a prospective, single-center, randomized controlled trial that demonstrated high efficacy for children aged 3-6 years [3] [11].
Methodology:
- Participant Stratification: Stratify participants by age (e.g., 3-6 years and 7-10 years) to account for developmental differences.
- Randomization: Use block randomization within each age group to assign participants to either "parent present" or "parent absent" groups.
- Parent Preparation: For the parent-present group, provide brief, standardized instructions prior to the scan. Parents should be instructed to:
- Remain calm and speak in a gentle, reassuring tone.
- Avoid sudden movements.
- Focus on providing verbal reassurance rather than physical contact that could cause motion.
- Safety Screening: Screen all accompanying parents for MRI contraindications (e.g., metal implants, pregnancy) before allowing them into the scan room.
- Procedure: The parent is provided with a wooden or non-metallic chair placed next to the scanner bore, within reach of the child. They remain there for the duration of the scan [3].
- Success Metrics:
Protocol for Audiovisual Distraction (AVD) Implementation
This protocol is derived from a successful quality improvement project that significantly reduced sedation needs [16] [10].
Methodology:
- Technology Setup: Implement an MRI-compatible in-bore AVD system (e.g., a video projector that displays a movie onto the inner surface of the scanner bore). This is typically suitable only for head-first positioning [16].
- Candidate Selection: Use a multi-step screening process:
- Pre-appointment Review: Identify potential candidates based on age (start with ≥7 years, can expand to ≥4 years), diagnosis, and scan type/duration [16].
- In-person Assessment: On the day of the scan, a certified child life specialist (CCLS), nurse, and sedation provider conduct a joint assessment of the child's temperament, demeanor, and anxiety level to determine final eligibility [10].
- Workflow Integration: Create a clear "awake MRI" pathway. Children who fail the AVD attempt should be seamlessly converted to a sedated protocol on the same day to avoid rescheduling and data loss [16].
- Outcome Measures:
- Primary: Percentage reduction in the use of minimal/moderate sedation.
- Balance Measures: Proportion of diagnostic studies and adherence to allotted exam times [10].
Protocol for Mock Scanner Training
This protocol leverages findings that a brief mock scan training can effectively suppress head motion in children and adolescents [28].
Methodology:
- Mock Scanner Session: Conduct a training session in a mock MRI scanner that replicates the look, sound, and confined space of a real scanner. The session should include:
- Exposure to simulated scanner noises.
- Practice lying still.
- Training on a motion-tracking feedback system, if available.
- Duration: A single, short session (e.g., 5.5 minutes) has been shown to be effective [28].
- Target Group: The intervention is particularly beneficial for younger children (aged 6-9 years) who demonstrate increased head motion [28].
- Success Metric: The primary outcome is a reduction in head motion parameters (e.g., framewise displacement) during the subsequent real MRI scan compared to pre-training baselines or control groups.
Implementation Workflows
The following diagrams outline logical workflows for integrating these strategies into a research pipeline.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Resources for Non-Sedated Pediatric MRI Research
| Item / Resource | Specification / Function | Research Application |
|---|---|---|
| Mock MRI Scanner | Replicates scanner environment (bore, noise); can be full-scale or small-scale. | Participant acclimatization and behavioral training to reduce anxiety and motion [28] [26]. |
| MRI-Compatible AVD System | In-bore video projection or goggle systems; must be MR-safe. | Provides cognitive distraction during scanning, improving compliance and stillness [16]. |
| Child Life Specialist (CCLS) | Certified professional trained in child development and healthcare coping. | Conducts pre-scan preparation, in-person assessments, and provides procedural support [16] [30] [26]. |
| Quiet MRI Sequences | Pulse sequences with reduced gradient slew rates (e.g., Quiet Suite). | Minimizes acoustic noise, a major stressor, facilitating natural sleep or quiet rest [3] [27]. |
| Motion Correction Software | Algorithms for prospective (real-time) or retrospective motion correction. | Mitigates the impact of residual motion on image quality, salvaging otherwise corrupted data [27] [18]. |
| Pediatric RF Coils | Head, torso, and extremity coils sized for infants and children. | Improve signal-to-noise ratio (SNR) and spatial resolution for smaller anatomical structures [27] [18]. |
Technical Support Center
Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q1: Our pediatric participants are still exhibiting high stress levels upon entering the MRI suite, despite the AVD system being functional. What preparatory protocols are recommended?
A1: Implement a structured preparatory protocol that begins before the child enters the scanning room.
- Filmed Modeling (FM): Prior to the scan, show children a short, child-friendly video that models the MRI procedure. The video should feature a peer successfully undergoing the scan, demonstrating appropriate behavior and familiarizing the child with the environment and sounds [31].
- Control and Choice: Empower children by allowing them to choose the first video or audiovisual content they will watch during the scan. This sense of control has been shown to improve calmness and cooperation [32].
- Combined Approach: Research indicates that a combination of AVD and filmed modeling is more effective in reducing anxiety and fear than either technique used alone [31].
Q2: We are experiencing significant motion artifacts in our imaging data from younger children (aged 6-10). How can the AVD content be optimized to reduce this?
A2: Motion artifacts are often a direct result of anxiety and a failure to engage the child's attention. Optimize content specifically for this age group.
- Content Pacing: Use calming, slow-paced visuals. Fast-paced content can overstimulate children and reduce their ability to follow instructions or regulate movement [32].
- Visual Focus: Design or select content where character movement is focused on the center of the screen. This helps minimize head motion and eye movements that can cause artifacts [32].
- Content Integration: A study on pediatric MRI found that a child-friendly audiovisual intervention significantly reduced scan issues (such as repeated sequences) and staff-reported stress levels specifically in children aged 6-10 years [32].
Q3: What are the most reliable physiological and psychometric metrics to quantitatively assess the efficacy of our AVD intervention in reducing anxiety?
A3: A multi-modal assessment strategy is recommended to capture both physiological and psychological dimensions of anxiety.
Table 1: Metrics for Assessing AVD Efficacy in Pediatric Anxiety Reduction
| Metric Category | Specific Metric | Description and Application | Evidence of Use |
|---|---|---|---|
| Physiological | Salivary Cortisol | Stress hormone measured from saliva samples pre- and post-intervention. A decrease indicates reduced physiological stress [31]. | [31] |
| Pulse Rate | Monitored via pulse oximeter. A significant decrease from pre- to post-procedure is associated with lower anxiety [31]. | [31] | |
| Psychometric Scales | Facial Image Scale (FIS) | A visual scale of facial expressions from happy to very unhappy; used for children to self-report feelings [31]. | [31] |
| Fear Assessment Picture Scale (FAPS) | A picture-based scale used to assess a child's level of fear in a medical setting [31]. | [31] | |
| State-Trait Anxiety Inventory for Children (STAIC) | A questionnaire used to measure state anxiety (transient) and trait anxiety (dispositional) in children [33]. | [33] | |
| Behavioral Observation | Modified Yale Preoperative Anxiety Scale | An observational scale where staff rate behaviors (e.g., crying, clinging) exhibited by the child in the medical setting [32]. | [32] |
| Staff-Reported Stress Question | Staff answer "How stressed was the child?" on a Likert scale (e.g., 1-6) at multiple time points [32]. | [32] |
Q4: We are encountering technical failures with our in-bore AVD system. What are common complex AV issues and their solutions in a research environment?
A4: Research environments demand high reliability. Common issues often extend beyond simple connections.
Table 2: Troubleshooting Complex AV System Issues
| Problem | Potential Root Cause | Recommended Solution |
|---|---|---|
| System-wide Control Failure | Control system software crash or firmware incompatibility. | Perform root cause analysis on interconnected devices. Leverage system diagnostic logs. Ensure all firmware is updated and compatible [34]. |
| No Video/Audio Feed to In-Bore Display | Connection failure (e.g., HDMI), network disruption, or incorrect source selection on the control system. | Check physical connections and network stability. Use diagnostic software to verify signal path. Reboot and reconfigure the control system interface [34] [35]. |
| Electromagnetic Interference (EMI) | EMI from the MRI scanner affecting AV equipment or cables. | Use MRI-compatible and properly shielded AV equipment and cables. Assess cable routing to minimize interference [34]. |
| Integration Challenge with Legacy Systems | New AVD components conflicting with existing hospital or lab IT/AV infrastructure due to unsupported protocols. | Simulate the problem scenario to isolate the conflict. Collaborate with AV specialists familiar with the MRI environment to resolve compatibility issues [34]. |
Experimental Protocols
Detailed Methodology: Evaluating AVD with Filmed Modeling for Pediatric MRI
This protocol synthesizes methodologies from recent clinical studies to provide a framework for research on AVD systems [31] [33] [32].
1. Study Design and Population
- Design: Randomized Controlled Trial (RCT). Participants are randomly assigned to an intervention group (AVD + FM) or a control group (standard care without AVD).
- Participants: Pediatric patients aged 6-12 years, scheduled for a first, awake MRI. Exclusion criteria typically include neurological disorders affecting stillness, developmental/cognitive disorders, or conditions requiring sedation [33] [32].
- Sample Size: Calculation should be based on a power analysis. For reference, recent studies have utilized samples ranging from 48 to 175 participants [33] [32].
2. Intervention Protocol
- AVD System: Utilize an MRI-compatible system with an in-bore screen (visible via a head-mounted mirror), a sound system, and optional ambient lighting [32].
- Intervention Group:
- Preparatory Phase (Filmed Modeling): Before entering the scan room, children view a 5-10 minute filmed modeling video. This video features a peer model calmly undergoing the MRI procedure, explaining the sounds and demonstrating cooperation [31].
- In-Bore Phase (AVD): During the scan, children watch specially designed, calming audiovisual content (e.g., slow-paced animated clips with central visual focus). The child is given a choice of content to enhance perceived control [32].
- Control Group: Undergoes the MRI scan with standard clinical care and staff reassurance, but without the structured AVD or FM intervention [31] [32].
3. Data Collection and Outcome Measures Data is collected at multiple time points: Pre-intervention (T1), Post-intervention/Pre-scan (T2), During scan (T3), and Post-scan (T4).
- Primary Outcomes:
- Secondary Outcomes: Physiological measures (e.g., pulse rate, salivary cortisol) where feasible [31].
4. Data Analysis
- Employ repeated-measures Analysis of Variance (ANOVA) to compare changes in anxiety scores over time between the intervention and control groups [32].
- Use ANOVA or Analysis of Covariance (ANCOVA) to compare the number of repeated sequences and image quality scores between groups, potentially controlling for covariates like the total number of sequences [32].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for AVD Experiments
| Item | Function in Research | Specification Notes |
|---|---|---|
| MRI-Compatible AVD System | Core intervention delivery. Displays video and plays audio within the MRI suite without causing interference. | Must include in-bore screen or projector, head-mounted mirror, MRI-safe headphones, and a media player. Systems like "Ambient Experience" are specifically designed for this [32]. |
| Validated Psychometric Scales | Quantify the primary psychological outcome (anxiety). | Use age-appropriate, validated scales. Examples: State-Trait Anxiety Inventory for Children (STAIC), Facial Image Scale (FIS) [31] [33]. |
| Physiological Data Acquisition Tools | Provide objective, biometric data on stress and anxiety levels. | Pulse oximeter (for pulse rate), saliva collection kits (for cortisol analysis), digital thermometer [31]. |
| Child-Friendly Audiovisual Content Library | The active ingredient of the distraction intervention. | Content should be slow-paced, have center-screen visual focus, and feature familiar, calming characters. Collaboration with content creators (e.g., animation studios) may be beneficial [32]. |
| Filmed Modeling (FM) Video | Prepares the child for the procedure, reducing fear of the unknown. | Video should be ~10 minutes, feature a peer model, and explicitly address procedural steps, sounds, and desired behaviors [31]. |
| Data Logging & Analysis Software | For extracting and analyzing scan performance metrics. | Software capable of parsing MRI system logfiles to extract metrics like exam length, number of sequence repeats, and pauses [32]. Statistical software (e.g., SPSS, R) is essential for data analysis. |
Workflow and Pathway Diagrams
FAQs: Optimizing Hardware and Protocols for Pediatric MRI
FAQ 1: What are the most effective hardware solutions for reducing motion in awake pediatric patients? Specialized head stabilization devices are highly effective. For instance, the MR-MinMo head stabilizer was specifically designed for high-resolution neuroimaging in awake participants, typically aged 6 and older. It uses a polycarbonate frame with inflatable pads and a hinged halo to gently immobilize the head, significantly reducing motion artifacts, particularly in pediatric volunteers [36]. Furthermore, MRI-compatible audiovisual distraction (AVD) systems, such as an in-bore video projector, allow children to watch movies during the scan, addressing anxiety and boredom that lead to movement [10].
FAQ 2: Which protocol modifications are key to shortening scan times and minimizing motion? Implementing fast imaging sequences is fundamental. Key techniques include:
- Parallel Imaging: Techniques like GRAPPA accelerate acquisition by undersampling k-space [11].
- Simultaneous Multi-Slice Imaging: Acquires data from multiple slices at once, dramatically reducing scan time [27].
- Compressed Sensing: Leverages image sparsity to reconstruct high-quality images from significantly fewer data points [10] [27].
- Single-Shot Sequences: Such as single-shot fast spin echo, are highly resilient to motion [18]. Integrating these into age-specific protocols with adjusted FOV, slice thickness, and TR further optimizes efficiency and signal-to-noise ratio [18].
FAQ 3: How can researchers quantitatively assess the effectiveness of their motion reduction strategies? Mean Framewise Displacement (FFD) is a standard quantitative metric for measuring head motion in functional MRI. It provides a scalar value (in mm) of how much a participant's head moves from one volume to the next throughout a scan. Analyzing the distribution of mean FFD values and the percentage of scans kept under specific thresholds (e.g., 0.10 mm, 0.15 mm) allows for objective comparison between different intervention groups [37].
FAQ 4: What non-hardware-based practices improve success rates for non-sedated MRI? A combination of preparatory and in-scanner techniques is highly effective:
- Mock Scanner Training: Placing participants in a simulated MRI environment to desensitize them and practice remaining still [37].
- Parental Presence: For children aged 3-6 years, having a parent in the scan room significantly improves the success rate of completing a non-sedated MRI [11].
- Child Life Specialists: These professionals use age-appropriate preparation, education, and support to reduce anxiety and improve cooperation [10] [26].
- In-Scan Incentive Systems: Providing positive reinforcement for keeping still during the scan can improve compliance in pediatric participants [37].
Troubleshooting Guides
Problem: Excessive Motion Artifacts in School-Age Children (7-12 Years)
Potential Causes and Solutions:
- Cause 1: Anxiety and lack of preparation leading to an inability to lie still.
- Solution: Implement a comprehensive mock scanner protocol. This should include familiarization with scanner sounds, training on keeping still, and practice in a simulated environment. Combine this with an in-scan incentive system to motivate the child [37].
- Cause 2: Boredom and discomfort during long acquisition times.
- Cause 3: Inadequate physical stabilization.
- Solution: Beyond standard foam padding, employ a dedicated pediatric head stabilizer like the MR-MinMo device. This provides comfortable but firm immobilization, keeping motion within a correctable regime for post-processing algorithms [36].
Problem: Suboptimal Image Quality in Preschool Children (3-6 Years) Without Sedation
Potential Causes and Solutions:
- Cause 1: High anxiety and developmental inability to understand and follow instructions.
- Solution: Leverage parental presence as a first-line strategy. A randomized study found parental presence in the scan room significantly improved non-sedated MRI success in this age group [11].
- Solution: Engage a Certified Child Life Specialist (CCLS). The CCLS should perform an in-person assessment on the day of the scan to evaluate the child's readiness and provide tailored, hands-on preparation and support [10].
- Cause 2: Protocol not optimized for faster acquisition.
Quantitative Data on Motion Reduction Strategies
The table below summarizes key performance data from recent studies on motion reduction techniques.
Table 1: Efficacy of Non-Sedation Motion Reduction Strategies in Pediatric MRI
| Technique | Study Population | Key Outcome Measure | Result | Source |
|---|---|---|---|---|
| Audiovisual (AVD) Distraction | Children aged 4-18 years | Reduction in minimal/moderate sedation use | 28.8 percentage point decrease | [10] |
| MR-MinMo Head Stabilizer | Pediatric & adult volunteers (7T) | Reduction in motion artifacts (NGS metric) | Significant reduction, particularly in pediatric subjects | [36] |
| Parental Presence | Children aged 3-6 years | Odds Ratio for MRI success | OR: 6.50 (95% CI: 1.64–25.76) | [11] |
| Mock Scanner + Incentives | Children aged 7-17 years | Scans exceeding 0.20 mm mean FFD threshold | 4.17% of scans (vs. 33.9% in control group) | [37] |
| Feed-and-Swaddle (Infants) | International survey of institutions | Success rate reported by sites | 51% of sites reported >75%-100% success | [26] |
Experimental Protocols for Motion Reduction
Detailed Protocol 1: Mock Scanner Training for Long-Duration fMRI
This protocol is designed to prepare children for 60-minute scan sessions, enabling the collection of high-quality, low-motion data [37].
- Primary Goal: To desensitize participants to the MRI environment and train them to minimize head movement.
- Materials: Mock MRI scanner (replica with sound system for playing recorded scanner noises), weighted blanket or bean bag, communication system, incentive system (e.g., token economy).
- Procedure:
- Pre-training: Explain the importance of keeping still using simple terms and visual aids.
- Familiarization: Have the child lie in the mock scanner. Introduce the sounds of various sequences (e.g., T1, fMRI) at gradually increasing volumes.
- Motion Training: Place a weighted blanket or bean bag on the child's forehead. Provide real-time feedback on head movement and practice correction.
- Practice Sessions: Conduct several practice runs, simulating the duration and sequence order of the actual scan protocol.
- In-Scan Procedures: During the actual MRI, use the weighted blanket and a simple incentive system (e.g., earning a reward for low motion) to reinforce behavior.
Table 2: Research Reagent Solutions for Motion Reduction
| Item | Function/Explanation |
|---|---|
| MR-MinMo Device | A specialized head stabilizer that uses a frame with inflatable pads and a locking halo to minimize head motion during high-resolution scans [36]. |
| Audiovisual Distraction (AVD) System | MRI-safe video goggles or an in-bore projection system that displays movies to distract and calm the pediatric participant [10] [26]. |
| Mock MRI Scanner | A full-scale or small-scale replica of an MRI scanner used to acclimate children to the environment, sounds, and confinement of a real scan [37]. |
| Weighted Blanket | Used during mock and real scans to provide deep pressure touch, which has a calming effect and provides physical feedback about movement [37]. |
| Framewise Displacement (FFD) | A software metric calculated from fMRI data to quantify head motion; used as a primary outcome measure for motion reduction interventions [37]. |
Detailed Protocol 2: Implementing an Awake MRI Program with Audiovisual Distraction
This quality improvement framework outlines the steps for establishing a clinical service for scanning children without sedation [10].
- Primary Goal: To reduce the utilization of minimal/moderate sedation by at least 20% while maintaining diagnostic image quality.
- Materials: MRI-compatible AVD system (e.g., in-bore video projector), screening forms, trained multidisciplinary team (radiologists, technologists, sedation providers, child life specialists).
- Procedure (via PDSA Cycles):
- Planning: Convene a stakeholder group. Perform a retrospective review to establish baseline sedation rates.
- Targeting (Cycle 1): Install AVD technology. Develop an "awake MRI" workflow. Start with strict, low-risk inclusion criteria (e.g., children ≥7 years, head-first scans <60 minutes).
- Broadening Scope (Cycles 2 & 3): Successively broaden inclusion criteria to include any diagnosis and lower the age limit to 4 years, based on initial success.
- Optimization (Cycle 4): Implement a neuroradiology motion sensitivity score to guide sequence selection. Eliminate restrictions on scan duration.
- Reinforcement (Cycle 5): Install new AVD technology that allows scanning in any body position. Re-educate staff to reinforce the cultural shift towards awake MRI.
Workflow and Logical Diagrams
This technical support center resource is framed within a research thesis focused on reducing motion without sedation in pediatric imaging. For researchers and scientists, patient motion remains a primary confounder, degrading image quality and compromising data integrity. This guide details methodologies for implementing advanced acceleration technologies—Parallel Imaging (PI), Compressed Sensing (CS), and Deep Learning (DL) reconstruction—which are critical for shortening acquisition times to sub-minute durations and thereby mitigating motion artifacts in pediatric populations [38] [18]. The following sections provide foundational knowledge, troubleshooting guides for common experimental challenges, and detailed protocols for their application in a research setting.
Core Technical Foundations
The following table summarizes the key acceleration techniques, their operating principles, and relevance to motion reduction.
Table 1: Core Technical Foundations of Accelerated MRI
| Technique | Primary Operating Principle | Key Technical Parameters | Clinical Acceleration Factor | Relevance to Pediatric Motion Reduction |
|---|---|---|---|---|
| Parallel Imaging (PI) [38] | Uses spatial information from multiple receiver coils to reconstruct undersampled data. | Acceleration Factor (R), Geometry Factor (g-factor). | R = 2 to 4 [38] | Directly reduces scan time, limiting the window for motion. Noise amplification (g-factor) can be limiting. |
| Compressed Sensing (CS) [38] [39] | Reconstructs images from randomly undersampled data by enforcing sparsity in a transform domain (e.g., wavelet). | Undersampling pattern, sparsity transform, regularization parameter (β). | R = 2.5 to 3 [38] | Random undersampling is key; allows for greater acceleration than PI alone but has long reconstruction times. |
| Deep Learning (DL) Reconstruction [38] [39] [22] | Learns a mapping from undersampled to fully-sampled data using neural networks trained on large datasets. | Network architecture (e.g., UNet), training loss function, amount of training data. | R = 4 to 8+ (in research) | Enables very high acceleration and near-instantaneous reconstruction; can be integrated with PI and CS. |
The logical integration of these techniques for maximizing motion robustness is depicted in the following workflow.
Troubleshooting Guides
Guide 1: Addressing Residual Aliasing Artifacts and Noise Amplification
Problem: Reconstructed images show significant noise or aliasing artifacts, often resembling overlapping ghosts or a "corduroy" pattern.
Investigation & Resolution:
Step 1: Check the Acceleration Factor (R).
- Symptoms: Severe noise that increases uniformly across the image.
- Cause: The overall acceleration factor (e.g., R = PI-factor × CS-factor) may be too high, leading to noise amplification characterized by a high g-factor in PI [38].
- Action: Systematically reduce the acceleration factor (R) in your protocol. For PI, clinical systems typically perform robustly at R = 2-4 [38].
Step 2: Verify the Sampling Pattern (for CS).
- Symptoms: Structured, coherent aliasing artifacts.
- Cause: The pseudo-random undersampling pattern used in CS may not be sufficiently "incoherent" relative to the sparsity transform [38].
- Action: Ensure the sampling mask uses a variable-density Poisson-disc or similar pattern that oversamples the low-frequency center of k-space.
Step 3: Calibrate Coil Sensitivity Maps (for PI).
- Symptoms: Aliasing artifacts localized to specific areas, often at the image periphery.
- Cause: Inaccurate estimation of coil sensitivity profiles used in SENSE-type reconstructions [38].
- Action: Ensure the auto-calibration scan is acquired with adequate signal-to-noise ratio (SNR) and is free of motion. Manually inspect the generated sensitivity maps for accuracy.
Guide 2: Managing Blurring and Loss of High-Frequency Detail
Problem: Reconstructed images appear overly smooth, lacking fine textural detail or having blurred edges.
Investigation & Resolution:
Step 1: Interrogate the DL Model.
- Symptoms: General loss of sharpness and texture; images may have a "painted" look.
- Cause: The deep learning model may be over-regularized or was trained on data that did not preserve high-frequency information. This is a known limitation of some CS algorithms without DL [38].
- Action: If using a commercially implemented DL tool (e.g., Deep Resolve [22]), adjust the "strength" or "sharpness" parameter if available. For custom models, review the training loss function and ensure it includes a term that preserves high-frequency details.
Step 2: Review CS Regularization Parameters.
- Symptoms: Images appear cartoon-like, with blocky or patchy areas.
- Cause: The regularization parameter (β) in the CS optimization is set too high, over-enforcing sparsity and suppressing fine details [38] [39].
- Action: In a research environment, gradually reduce the β parameter in the reconstruction algorithm and observe the output for a return of texture without introducing noise.
Frequently Asked Questions (FAQs)
Q1: Can these techniques be combined for greater acceleration? A1: Yes, they are highly synergistic. A common and powerful approach is to use PI for a moderate acceleration (e.g., R=2) and then apply CS or DL on top to achieve a higher net acceleration (e.g., R=4-6). Many state-of-the-art DL methods are unrolled networks that explicitly incorporate the data consistency steps of CS and the coil sensitivity information of PI [38] [39].
Q2: What are the key requirements for training a custom DL reconstruction model? A2: You need a large dataset of high-quality, fully-sampled k-space data as your ground truth. This is typically difficult to acquire clinically. A common workaround is to use publicly available datasets like fastMRI [38] [40]. The training requires significant computational resources (GPUs) and expertise in defining an appropriate loss function that balances artifact suppression with detail preservation [38].
Q3: How can I validate that an accelerated protocol is diagnostically reliable? A3: Beyond qualitative assessment, use quantitative metrics to compare against a fully-sampled reference. Common metrics include Structural Similarity Index (SSIM), Peak Signal-to-Noise Ratio (PSNR), and Normalized Mean Squared Error (NMSE) [38] [39]. For a clinical trial, a blinded review by radiologists to evaluate diagnostic confidence compared to a standard clinical scan is the gold standard [18].
Q4: We are seeing good results in older children but poor success in 3-6 year olds. What non-technical factors should we optimize? A4: Technical acceleration must be paired with patient-centered preparation. Evidence shows that for the 3-6 year age group, parental presence in the scan room significantly improves success rates [3]. Other effective strategies include dedicated patient preparation (e.g., using mock scanners or preparation videos [22]), in-bore entertainment systems, and collaboration with child life specialists to reduce anxiety [3] [18] [22].
Experimental Protocols & Data
Detailed Protocol: Implementing an Integrated DL-Reconstruction Sequence
This protocol is adapted from clinical implementations of vendor-integrated AI solutions like Deep Resolve [22].
- Objective: To reduce scan time by ≥50% for a T2-weighted TSE sequence in a pediatric neuroimaging protocol while maintaining diagnostic image quality for motion reduction.
- Materials:
- MRI scanner (e.g., 3T system, implementation based on Siemens MAGNETOM Vida with syngo MR XA50 [22]).
- Appropriate head coil array.
- Integrated AI reconstruction software (e.g., Deep Resolve Sharp/Boost).
- Method:
- Setup: Position the patient using comfortable immobilization aids (e.g., inflatable pads) to minimize gross motion. Use an in-bore entertainment system if available.
- Baseline Scan: Acquire the standard clinical T2-weighted TSE sequence with parameters set by your institution's protocol. Record the acquisition time (TAstandard).
- Accelerated Scan: Without moving the patient, acquire the same sequence with identical geometric parameters (FOV, resolution) but:
- Increase the parallel imaging acceleration factor (e.g., from R=2 to R=3).
- Reduce the number of averages.
- Enable the integrated DL reconstruction (e.g., Deep Resolve Boost and Sharp [22]).
- Record the new acquisition time (TAAI).
- Data Analysis:
- Calculate the time reduction: Time Reduction (%) = [(TAstandard - TAAI) / TA_standard] * 100.
- Qualitatively score both image sets for diagnostic quality, sharpness, noise, and presence of artifacts using a 5-point Likert scale (1=non-diagnostic, 5=excellent) by two blinded radiologists.
- Compute quantitative metrics (SSIM, PSNR) if a fully-sampled reference is available.
The following diagram illustrates the experimental workflow.
Quantitative Data from Key Studies
Table 2: Performance Metrics of Accelerated Imaging Techniques
| Study / Technique | Acceleration Factor | Key Quantitative Result | Clinical Outcome / Context |
|---|---|---|---|
| Conventional CS [38] | 2.5 - 3 | Limited acceleration due to inability to fully reconstruct high-frequency texture. | Reconstruction times can be slow. |
| DL-CS Integration [38] [39] | 4 - 8+ | Superior SSIM and PSNR compared to CS alone at the same acceleration factor. | Enables much higher acceleration with faster reconstruction. |
| Deep Resolve (Commercial DL) [22] | ~50% time reduction | Reports maintained image quality with a ~50% reduction in scan time for MSK protocols. | Directly reduces sedation needs in pediatric scanning. |
| Optimized Pediatric Protocols [18] | Not specified | 75% of post-implementation scans rated "Good" or "Excellent" vs. 25% pre-implementation. | Combined faster sequences, motion correction, and non-pharmacological methods. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Advanced MRI Reconstruction Research
| Item | Function / Application | Example / Note |
|---|---|---|
| Public Datasets | Provides ground-truth, fully-sampled k-space data for training and benchmarking DL models. | fastMRI [38] [40]: A large-scale dataset including both brain and knee MRI data. |
| GitHub Repository | A curated list of up-to-date publications, code, and resources in the field. | Awesome-DL-based-CS-MRI [38] [39] [40]: A dedicated repository for DL-based MRI reconstruction. |
| DL Framework | Provides the software environment for developing, training, and testing reconstruction networks. | PyTorch or TensorFlow: Common open-source frameworks used in published research [38]. |
| Vendor AI Solutions | Implements validated, commercially available DL reconstruction on clinical scanners. | Deep Resolve (Siemens), AIR Recon (GE), Compressed SENSE (Philips). Useful for applied clinical research [22]. |
| Phantom | An object with known properties used for standardized quality control and algorithm validation. | Use an ACR MRI phantom or custom phantom to test for artifacts and measure SNR/CNR across protocol changes. |
Minimizing motion artifacts in pediatric magnetic resonance imaging (MRI) without sedation is a critical challenge in clinical research, directly impacting data quality and study validity. Success hinges on deploying age-specific, non-pharmacological strategies that address the distinct physiological and psychological profiles of children from infancy through adolescence. This guide provides a structured, evidence-based approach for researchers aiming to optimize imaging protocols for motion-free data acquisition in pediatric populations. The methodologies outlined are synthesized from current clinical practices and quality improvement projects, offering a foundation for standardized implementation in research settings [41] [16] [18].
Frequently Asked Questions (FAQs) for Researchers
Q1: What is the primary rationale for avoiding sedation in pediatric imaging research? A1: Beyond clinical risks, sedation in research introduces confounding variables, such as potential neurophysiological effects that may interfere with functional or neurological endpoints [41] [42]. Eliminating sedation removes these potential confounders, reduces operational complexity and cost for research studies, and aligns with the ethical principle of minimizing risk to participants, especially in healthy pediatric cohorts [16] [18].
Q2: Which age group presents the greatest challenge for non-sedated MRI, and why? A2: Children aged approximately 6 months to 6 years are the most challenging. Infants younger than 6 months can often be imaged while naturally asleep, while children older than 6 years are typically more capable of understanding instructions and remaining still. The 6-month to 6-year period is characterized by rapid cognitive development, stranger anxiety, and a limited capacity for prolonged stillness, often necessitating a more diverse and creative toolkit of strategies [41] [11].
Q3: How can a research team quickly predict which subjects might succeed with a non-sedated scan? A3: While comprehensive screening is ideal, one rapid predictive tool is in-person assessment by a trained provider on the scan day. One quality improvement project used a quick check for cooperation and calmness, which allowed them to successfully include children as young as 4 years old in a non-sedated pathway [16]. For younger children (3-6 years), the simple, low-resource intervention of parental presence has been shown to significantly improve success rates, making it a valuable first-line strategy to trial [11].
Troubleshooting Guide: Common Scenarios and Evidence-Based Solutions
Scenario 1: Excessive Motion Artifacts in a 3-Year-Old Subject
- Problem: The subject is fidgeting and crying, resulting in non-diagnostic image quality.
- Solution:
- Immediate Action: If not already implemented, invite a parent into the scan room. A randomized study found this significantly improved success rates in the 3-6 year age group (59.1% with parent vs. 18.2% without) [11].
- Protocol Adjustment: Switch to faster, motion-robust sequences (e.g., single-shot T2-weighted sequences) to acquire critical data points quickly before tolerance wanes [41] [42].
- Future Workflow: Integrate a mock scanner session or a preparation video before the actual scan to familiarize the child with the environment [41] [22].
Scenario 2: A 7-Year-Old Subject is Anxious but Cooperative
- Problem: The subject is able to follow commands but reports being scared, which may lead to movement.
- Solution:
- Engage Audiovisual Distraction (AVD): Utilize an MRI-compatible video system. One project using in-bore AVD technology successfully reduced sedation needs by 28.8 percentage points in children aged 4-18, with 96% of studies completed within the allotted time [16].
- Optimize the Environment: Create a child-friendly atmosphere with themed decorations or projected scenes to reduce the perceived threat of the scanner [41].
- Leverage Hardware: Use pediatric-specific coils and faster 3T scanners to decrease scan time, thereby reducing the window for anxiety to build and motion to occur [43] [18].
Scenario 3: An Infant Subject Wakes Up During Scan Acquisition
- Problem: A neonate being scanned using a "feed-and-sleep" technique awakens mid-protocol.
- Solution:
- Preventive Measures: Combine feeding with swaddling using a specialized device like a "cocoon" to promote comfort and security, which can improve success rates to over 90% for brain MRI [22].
- Protocol Prioritization: Structure the imaging protocol so that the loudest sequences (e.g., Diffusion-weighted Imaging) are performed last to minimize the chance of waking the infant [41].
- Sequence Selection: Implement accelerated protocols that leverage deep learning-based reconstruction (e.g., Deep Resolve) to obtain diagnostic images in a fraction of the time, which is crucial for this patient group [22].
Table 1: Efficacy of Non-Sedated MRI Strategies Across Age Groups
| Age Group | Primary Strategy | Reported Success Rate | Key Metric/Outcome | Source |
|---|---|---|---|---|
| Neonates & Infants (<6 mos) | Feed-and-Swaddle/Bundle | ~90% success for brain MRI | Technique involves feeding, swaddling, and using sucrose to encourage natural sleep. | [41] [22] |
| Young Children (3-6 years) | Parental Presence | 59.1% completion vs. 18.2% (no parent) | Randomized controlled trial showing significant improvement in scan completion. | [11] |
| Children (4-18 years) | Audiovisual Distraction (AVD) | 28.8 percentage point reduction in sedation | 100% of AVD-triaged studies were diagnostic; 96% within allotted time. | [16] |
| All Ages | Protocol Optimization (Fast Sequences) | 65% to 91% acceptable image quality | Post-optimization, motion artifacts reduced, and sedation use dropped from 70% to 30%. | [18] |
Table 2: Impact of Protocol Optimization on Scan Efficiency
| Parameter | Baseline Protocol | Optimized Protocol | Improvement | Source |
|---|---|---|---|---|
| Average Scan Duration | 45 ± 10 minutes | Significantly Reduced | Faster protocols (e.g., single-excitation T2W) can reduce time per sequence by 50%. | [41] [18] |
| Image Quality (Rated Excellent) | 25% | 65% | Use of parallel imaging, motion correction, and AI-based reconstruction. | [18] |
| Sedation Rate | 70% | 30% | Achieved via a bundle of non-sedation strategies and faster imaging. | [18] |
Detailed Experimental Protocols for Research Implementation
Protocol 1: The "Feed-and-Swaddle" Technique for Infants (0-6 months)
Objective: To acquire motion-free MRI images from infants using natural sleep without pharmacological sedation. Methodology:
- Pre-Procedure Preparation:
- Subject Preparation:
- Feeding: Feed the infant in a quiet, calm environment immediately before the scan. The use of non-nutritive sucking and sucrose can be employed to reduce discomfort [41].
- Swaddling: Snugly swaddle the infant using a blanket or a specialized immobilization device like the "Babyfix Cocoon" to provide comfort and restrict movement [41] [22].
- Hearing Protection: Securely fit MRI-compatible hearing protection.
- Data Acquisition:
Protocol 2: Audiovisual Distraction (AVD) for Children (4+ years)
Objective: To enable successful MRI completion in awake, cooperative children by reducing anxiety and boredom. Methodology:
- Subject Screening and Preparation:
- Eligibility: Screen for children who are cognitively able to understand and engage with the AVD system. Exclude those with severe visual impairment or developmental conditions that would preclude its use [16].
- Familiarization: Use a certified child life specialist or trained researcher to prepare the child, explaining the process and allowing them to choose a movie or show [41] [16].
- Setup and Equipment:
- Imaging Execution:
- Monitoring: A researcher or child life specialist should provide continuous encouragement and monitor the child's comfort throughout the scan.
- Protocol Adherence: Utilize pre-optimized, fast imaging protocols to ensure the total scan time remains within the child's attention span. The goal should be to complete scans within 60 minutes or less, with one study reporting 96% success in staying within allotted exam times [16].
Workflow and Strategic Decision Pathways
Non-Sedated Pediatric MRI Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Resources for Non-Sedated Pediatric MRI Research
| Item Category | Specific Example | Research Function | Implementation Notes |
|---|---|---|---|
| Immobilization Aids | Swaddling Cocoon (e.g., Babyfix), Inflatable Pads (e.g., Multipad) | Provides comfort and restricts involuntary movement, crucial for infant and toddler studies. | Standardizes positioning across subjects; reduces variability from researcher technique [41] [22]. |
| Audiovisual Distraction (AVD) | MRI-compatible video goggles (e.g., NordicNeuroLab), In-bore projection systems | Reduces anxiety and boredom, increasing compliance and stillness in older children. | Shown to reduce sedation needs by 15-35% in clinical practice; a key variable for success [41] [16] [22]. |
| Acquisition Sequences | Single-Shot Fast Spin-Echo (e.g., HASTE, SSFSE), PROPELLER/BLADE, Compressed Sensing | Enables rapid data acquisition and/or inherent motion correction, salvaging data quality. | Vendor-neutral names vary. Deep learning reconstructions (e.g., Deep Resolve) can further enhance speed and quality [41] [22] [42]. |
| Simulation Equipment | Mock MRI Scanner, Storybooks, Preparation Videos | Familiarizes the child with the MRI environment, desensitizing them to sounds and confinement. | Prepares the subject psychologically, improving the likelihood of a successful scan [41] [11]. |
| High-Field Scanners & Coils | 3T MRI systems, High-channel pediatric phased-array coils | Increases signal-to-noise ratio (SNR), allowing for faster acquisitions or higher resolution. | Essential for leveraging parallel imaging and other acceleration techniques [43] [18]. |
Troubleshooting Motion Artifacts: Protocol Refinement and Problem-Solving in Research Settings
Technical Support Center: Troubleshooting Guides and FAQs
This guide provides technical support for researchers implementing motion correction algorithms in pediatric imaging studies, specifically focused on reducing the need for sedation.
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between prospective and retrospective motion correction?
- A1: Prospective motion correction (e.g., PROMO) actively tracks motion during the scan and adjusts the imaging sequence in real-time to compensate for it [44] [45]. Retrospective motion correction (e.g., certain PROPELLER and deep learning methods) acquires data that is resilient to motion or contains motion information, and the corrections are applied during the image reconstruction process after the scan is complete [46] [45].
Q2: For pediatric abdominal imaging, our DL-reconstructed T1-weighted images show pronounced respiratory motion artifacts. What could be the cause?
- A2: This is a known issue. One study found that not respiratory-gated DL-reconstructed T1-weighted images demonstrated more pronounced respiratory motion artefacts compared to conventional reconstruction. The solution is to ensure proper respiratory gating for T1-weighted sequences, as no difference was found for respiratory-gated T2-weighted images [47].
Q3: Why does a PROPELLER acquisition take longer than a standard Cartesian scan, and how can this be mitigated?
- A3: PROPELLER requires oversampling the center of k-space, which increases scan time by a factor of approximately π/2 (about 1.57 times) compared to conventional Cartesian sequences [47] [48]. Mitigation strategies include combining PROPELLER with accelerated protocols using deep learning reconstruction, which allows for fewer acquisitions or shorter scan times while maintaining image quality [47] [49].
Q4: We are implementing a motion correction method that uses low-resolution navigators. What is the optimal navigator resolution?
- A4: Research on a 3D radial motion correction method found that navigator resolution significantly impacts performance. The optimal range for navigator resolution is 5-7 mm, with a mid-range value of 6 mm providing maximum image sharpness and consistent results [46].
Q5: Can deep learning models for motion correction generalize across different MRI sites and scanner brands?
- A5: Evidence suggests that with proper training, they can. One study trained a model on multichannel data from multiple sites and with multiple contrasts. The model's performance was independent of pathology and generalizable to a new center unseen during training [50].
Troubleshooting Guide
| Problem | Possible Cause | Solution |
|---|---|---|
| Severe streaking in PROPELLER images | Gaps in k-space coverage between blades; insufficient blade overlap [48]. | Increase the "blade coverage factor" (or vendor-equivalent parameter) to >100%, up to 157% for gapless coverage. |
| DL-reconstructed images appear overly smooth or synthetic | Loss function in DL network may over-prioritize noise reduction at the expense of texture [45]. | Use a network that incorporates perceptual (LPIPS) and data consistency loss functions to better preserve textural information and anatomical detail [51]. |
| PROMO scan takes excessively long | The subject is moving frequently, triggering automatic reacquisition of data partitions [44]. | This is a feature, not a bug, ensuring diagnostic quality. For motion-prone populations, consider supplementing with audio-visual aids to calm the child and reduce motion [52]. |
| Poor motion correction in through-plane direction | 2D PROPELLER and some 2D navigators primarily correct for in-plane motion only [48]. | Implement a 3D acquisition sequence with 3D motion tracking capabilities, such as a 3D radial sequence [46]. |
The following tables summarize key quantitative findings from recent studies on motion correction.
Table 1: Quantitative Impact of Deep Learning PROPELLER Reconstruction in Pediatric Body MRI (n=21 children) [47]
| Metric | Conventional Reconstruction | DL-Based Reconstruction | P-Value |
|---|---|---|---|
| Liver SNR (T1-weighted) | Baseline | Significantly Higher | < 0.001 |
| Liver CNR (T1-weighted) | Baseline | Significantly Higher | < 0.001 |
| Spleen SNR (T2-weighted) | Baseline | Significantly Higher | < 0.001 |
| Spleen CNR (T2-weighted) | Baseline | Significantly Higher | < 0.001 |
| Scan Time per Slice (T1-w) | 6.3 s (median) | 4.8 s (median) | - |
| Scan Time per Slice (T2-w) | 5.6 s (median) | 4.2 s (median) | - |
Table 2: Efficacy of Retrospective Motion Correction in Pediatric Brain MRI (n=44 participants) [46]
| Evaluation Method | Non-Corrected Images (Mean) | Motion-Corrected Images (Mean) | P-Value |
|---|---|---|---|
| Radiologist Likert Score (Reviewer 1) | 3.0 | 3.8 | < .001 |
| Radiologist Likert Score (Reviewer 2) | 3.0 | 3.8 | < .001 |
| Image Sharpness (Tenengrad Metric) | Baseline | Up to 35% Improvement | < .0005 |
Table 3: Performance of a Deep Learning Model (PI-MoCoNet) for Brain MRI Motion Correction [51]
| Artifact Severity | Metric | Before Correction | After Correction |
|---|---|---|---|
| Minor Artifacts | PSNR (dB) | 34.15 | 45.95 |
| SSIM | 0.87 | 1.00 | |
| NMSE (%) | 0.55 | 0.04 | |
| Moderate Artifacts | PSNR (dB) | 30.23 | 42.16 |
| SSIM | 0.80 | 0.99 | |
| NMSE (%) | 1.32 | 0.09 | |
| Heavy Artifacts | PSNR (dB) | 27.99 | 36.01 |
| SSIM | 0.75 | 0.97 | |
| NMSE (%) | 2.21 | 0.36 |
Detailed Experimental Protocols
This protocol is designed for a retrospective study comparing conventional and DL-based image reconstruction.
- Patient Population: Children undergoing thoraco-abdominal MRI. Example: 21 children (median age 7 years).
- Imaging Hardware: 1.5-T or 3-T MRI scanner (e.g., Signa Artist, GE HealthCare) with multichannel surface coils.
- Pulse Sequences: Axial T1-weighted PROPELLER (without respiratory gating) and respiratory-gated axial T2-weighted PROPELLER with fat saturation.
- Accelerated Protocol Parameters (Example):
- T1-weighted: TR ~793 ms, TE ~22 ms, matrix 280²–420², NEX 1.7.
- T2-weighted: TR ~3158 ms, TE ~98 ms, matrix 280²–400², NEX 1.7.
- Reconstruction: Raw k-space data from the same acquisition is processed through both the conventional pipeline and the DL-based pipeline (e.g., AIR Recon DL).
- Image Analysis:
- Quantitative: Calculate Signal-to-Noise Ratio (SNR) and Contrast-to-Noise Ratio (CNR) for organs of interest (e.g., liver, spleen).
- Qualitative: Three blinded observers should rate images using a 4-point Likert scale for noise, motion artifact, depiction of anatomical structures, and sharpness.
- Statistical Testing: Compare SNR/CNR using paired t-tests and qualitative scores using the Wilcoxon signed-rank test.
This protocol uses navigators from the acquisition itself for motion estimation.
- Pulse Sequence: 3D radial sampling sequence such as MPnRAGE.
- Key Parameters: Isotropic resolution (e.g., 1.0 mm), ~438 inversion-recovery contrasts, imaging time ~8.5 minutes.
- Motion Tracking:
- Reconstruct a series of low-resolution 3D navigator images from subsets of consecutive k-space views (e.g., views acquired between magnetization-preparation pulses, ~2-second intervals).
- The optimal navigator resolution is 6 mm.
- Motion Estimation & Correction:
- Use image-based registration tools (e.g., from the FSL library) to estimate translational and rotational motion parameters from the navigator series.
- Apply these motion parameters to correct the k-space data before final full-resolution image reconstruction.
- Validation:
- Compare motion-corrected and non-corrected images using a 5-point Likert scale (0-4) rated by experienced neuroradiologists.
- Calculate the Tenengrad metric as an objective, reference-free measure of image sharpness.
This protocol uses real-time motion tracking to adjust the scan.
- Pulse Sequence: 3D T1-weighted sequence (e.g., IR-SPGR).
- Navigator Acquisition: Intersperse low flip angle, single-shot spiral navigator scans (S-Navs) within the dead time of the main sequence.
- Example: Five sets of three orthogonal S-Navs.
- Real-Time Processing:
- Use an extended Kalman filter (EKF) algorithm to process navigator data and track head position as a six-element vector (translations and rotations).
- The imaging coordinate system is adjusted in real-time based on these estimates.
- Data acquired during intervals of high motion are automatically reacquired.
- Outcome Measures:
- A radiologist, blinded to the correction method, rates all images using a 5-point image quality scale (0-4).
- Compare the distribution of ratings for PROMO-on and PROMO-off scans using the Mann-Whitney U test.
Workflow and Signaling Pathways
PROPELLER MRI Acquisition and Correction Workflow
Deep Learning Motion Correction Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Software for Motion Correction Research
| Item | Function/Description | Example/Note |
|---|---|---|
| 3T MRI Scanner | Provides the main magnetic field for imaging. High-field strength improves signal-to-noise ratio. | Often a minimum requirement for advanced research sequences. |
| Multichannel Head/Body Coil | Phased-array coils for parallel imaging, which accelerates acquisition. | Essential for techniques like BladeNet that use multichannel data [50] [49]. |
| PROPELLER Sequence | Pulse sequence that acquires k-space in rotating blades for inherent motion robustness. | Vendor names: GE (PROPELLER), Siemens (BLADE), Philips (MultiVane) [48]. |
| 3D Radial Sequence (e.g., MPnRAGE) | Volumetric sequence that oversamples the k-space center, enabling accurate motion estimation [46]. | |
| Deep Learning Reconstruction Software | Software package that uses trained neural networks to denoise or correct motion in images. | e.g., AIR Recon DL, or custom frameworks like BladeNet [47] [49]. |
| Image Registration Toolbox | Software library for performing image-based registration to estimate motion parameters. | e.g., FSL (FMRIB Software Library) [46]. |
| Neural Network Architectures | Pre-defined model designs for image restoration and synthesis. | U-Net, ResNet, Generative Adversarial Networks (GANs) are commonly used [49] [45] [51]. |
| Training Datasets | Large collections of MRI data, sometimes with simulated motion, for training DL models. | e.g., fastMRI dataset; can be augmented with simulated rigid motion [50] [51]. |
FAQs on Abbreviated MRI (AB-MRI) and Non-Sedation Practices
Q1: What is the core principle behind designing an abbreviated MRI protocol? AB-MRI protocols are built by identifying and retaining only the MRI sequences that are most critical for answering a specific clinical question, while eliminating redundant or non-essential sequences. This prioritization significantly reduces scan time, which is crucial for motion-prone populations like unsedated children [53] [54] [55]. The diagnostic performance of the abbreviated protocol must be validated against the full standard protocol to ensure no significant loss of accuracy [53].
Q2: For pediatric AB-MRI, what are the key benefits of reducing scan time? Reducing scan time directly addresses the primary challenge of pediatric imaging: motion artifact. Shorter scans are easier for children to tolerate, which decreases the failure rate of studies and reduces the need for sedation or general anesthesia. This avoids the associated risks, costs, and longer wait times for sedated appointments [3] [54] [26].
Q3: What non-pharmacological techniques can improve success in unsedated pediatric MRI? Multiple evidence-based techniques can be employed, often in combination. Success rates are highly dependent on the child's age and the specific method used [3] [56] [26]. The table below summarizes common techniques and their reported effectiveness.
Table 1: Non-Sedation Techniques for Pediatric MRI
| Technique | Description | Reported Success/Application |
|---|---|---|
| Parental Presence [3] | A parent stays within the child's reach in the scan room. | Significantly improved success in children aged 3-6 years (59.1% vs 18.2% completion). No significant benefit in children 7-10 years. |
| Feed-and-Swaddle [26] | For infants; feeding followed by swaddling for comfort and immobilization. | 51% of institutions reported a high success rate (>75-100%) in infants. |
| Video Goggles / Movies [56] [26] | Distraction via watched media. | 50% of institutions reported high success; significantly reduces head motion compared to rest, especially in younger children. |
| Child Life Specialist [3] [26] | Specialist-led preparation using verbal reassurance, mock scanners, and toys. | 71% of institutions use this; most often reported with moderate success (>50-75%). |
| Real-time Motion Feedback [56] | Visual feedback is provided to the participant about their head motion. | Significantly reduces framewise displacement (FD), particularly in younger children. |
| Vacuum Immobilizers [57] [58] | Devices like vacuum pillows or the MR-MinMo to gently restrict movement. | Successful in 94% of neonatal attempts; significantly reduces motion artifacts in high-resolution scans. |
Q4: How does the diagnostic performance of AB-MRI compare to full protocols? Studies across various body parts show that well-designed AB-MRI protocols can achieve diagnostic performance comparable to full protocols, particularly for detection tasks. However, some trade-offs exist. For example, a study on breast cancer detection found that an abbreviated protocol achieved 100% sensitivity (equal to the full protocol) in identifying malignant lesions, but with a lower specificity (53.5%-73.3%) compared to 100% for the full protocol, indicating a higher false-positive rate [53]. In pediatric traumatic brain injury (TBI), AB-MRI has demonstrated high sensitivity (92.8%) and specificity (96.2%) when compared to CT [54].
Troubleshooting Guides
Issue 1: Excessive Motion Artifact in Pediatric Scans
Problem: Scans from unsedated children are consistently degraded by motion, leading to nondiagnostic images and study failure.
Solution: Implement a systematic, multi-layered approach.
- Step 1: Pre-Scan Preparation and Screening
- Utilize a Mock Scanner: When possible, have children undergo a simulation session to acclimate them to the environment and noises [26].
- Age-Based Strategy: Adopt a standardized workflow based on the child's age. The following diagram outlines a potential decision pathway.
- Step 2: In-Scanner Interventions
- Employ Distraction: Use video goggles or movies, which have been proven to reduce head motion compared to a "rest" state [56].
- Use Immobilization Devices: Implement vacuum pillows or specialized devices like the "MR-MinMo" head stabilizer. One study found the MR-MinMo significantly reduced motion artifacts, particularly in pediatric volunteers [58].
- Provide Real-time Feedback: If the hardware/software is available, provide children with visual feedback on their head motion. The Framewise Integrated Real-time MRI Monitoring (FIRMM) software is one such system that has shown efficacy [56].
Issue 2: Designing and Validating an Abbreviated Protocol
Problem: Researchers need to create a shortened MRI protocol for a specific clinical application (e.g., liver metastasis screening) but are unsure how to select sequences and validate the protocol.
Solution: Follow a structured protocol optimization methodology.
Step 1: Define the Clinical Question
Step 2: Identify and Prioritize Core Sequences
- Analyze the full diagnostic protocol to identify sequences that provide the most critical information for your defined question. This often involves selecting the most sensitive sequences for the pathology of interest. The table below provides examples from the literature.
Table 2: Example AB-MRI Protocols from Literature
| Clinical Application | Example Abbreviated Protocol Sequences | Reported Scan Time | Key Performance Metrics |
|---|---|---|---|
| Breast Cancer Detection [53] | Unenhanced & early arterial-phase dynamic T1-weighted sequences. | ~4.7 minutes | Sensitivity: 100% (vs. full protocol) Specificity: 53.5-73.3% (lower than full) |
| Pediatric Traumatic Brain Injury [54] | Non-contrast protocol focused on hemorrhage detection (e.g., Gradient Recall Echo/SWI). | < 10 minutes | Sensitivity: 92.8%, Specificity: 96.2% (vs. CT) |
| Liver Metastasis Detection [55] | T2-weighted, Diffusion-Weighted Imaging (DWI), and Hepatobiliary Phase (HBP) T1-weighted. | ~5 - 10 minutes | Similar diagnostic performance to full protocol (35-50 min) |
| Prostate Cancer Screening [55] | Axial T2-weighted and Diffusion-Weighted Imaging (DWI). | ~10 minutes | Comparable diagnostic performance to 30-minute multiparametric MRI |
- Step 3: Validate the Protocol
- Statistical Decision Analysis: For a rigorous, quantitative approach, model tissues with Probability Density Functions (PDFs) of their parameters (T1, T2, etc.). The imaging process maps these from tissue parameter space to signal strength space. The optimal protocol is the one that best separates the signal distributions of the tissues relevant to your clinical question, maximizing diagnostic accuracy [59].
- Retrospective Reader Study: The most common method. Extract the abbreviated protocol sequences from a dataset of full-protocol exams. Have blinded radiologists read the abbreviated studies and compare their findings (sensitivity, specificity, area under the ROC curve) against the reference standard (e.g., full protocol report or biopsy results) [53].
The Scientist's Toolkit: Essential Materials for Non-Sedation MRI Research
Table 3: Key Research Reagent Solutions and Equipment
| Item / Solution | Function / Application in Research |
|---|---|
| Mock MRI Scanner | A non-functional replica of an MRI scanner used to acclimate participants (especially children) to the scanning environment, reducing anxiety and motion during the actual scan [26]. |
| Vacuum Immobilization Devices | Molds or pillows that can be shaped to an individual's head and body and then vacuum-sealed to provide comfortable, customized immobilization, reducing motion artifact [57] [58]. |
| Real-time Motion Tracking Software (e.g., FIRMM) | Software that provides framewise displacement (FD) data in real-time during the scan. This allows researchers to monitor data quality, provide feedback to participants, or terminate a scan that has been compromised by motion [56]. |
| Video Goggle Systems | Audiovisual systems that display movies to participants inside the scanner. Serves as a powerful distractor to help children remain still for extended sequences [56] [26]. |
| Probability Density Functions (PDFs) of Tissue Parameters | A mathematical model used in advanced protocol optimization. PDFs describe the natural variability of tissue parameters (T1, T2) across a patient population. This model helps select pulse sequences that best discriminate between tissue types for a specific diagnostic task [59]. |
Troubleshooting Guide & FAQs
This technical support center provides evidence-based solutions for researchers encountering challenges in pediatric imaging studies involving children with autism spectrum disorder (ASD) and developmental delays, particularly within the context of reducing motion without sedation.
Frequently Asked Questions
Q: What non-pharmacological strategies are most effective for reducing motion in children with ASD during MRI? A: Multiple evidence-based approaches exist. Parental presence significantly improves success rates, particularly in children aged 3-6 years, with one study showing a 6.5 times higher success rate when parents were present [3]. Audiovisual distraction (AVD) systems can reduce sedation needs by 28.8 percentage points while maintaining diagnostic quality [16]. Environmental modifications are also crucial; this includes creating a low-stimulus environment with dim lighting and minimized loud sounds, which is particularly important for children with ASD who often have sensory sensitivities [60].
Q: How can researchers prepare children with developmental delays for a non-sedated MRI? A: Comprehensive preparation is essential. Utilize visual supports like social stories, visual schedules, and video previews of the MRI process to set expectations [22] [60]. Collaborate with child life specialists who can use mock MRI scanners and toys to simulate the experience [16]. Conduct pre-procedure planning with parents to identify the child's communication styles, sensory triggers, and calming techniques [60].
Q: Which children are suitable candidates for non-sedated MRI protocols? A: Success depends on multiple factors. Children aged 5 years and above are often capable of following instructions, while those aged 3-6 years present more challenges but can succeed with appropriate support [3] [22]. Developmental capacity is a key consideration; children with severe developmental delay or ASD that would prevent understanding of the procedure may be less suitable for non-sedated protocols [16]. Medical stability and the procedure length are also important, with shorter scan times (initially under 60 minutes) being more feasible for awake protocols [16].
Q: What technical adaptations can minimize motion artifacts in pediatric imaging? A: Implement accelerated MRI sequences such as parallel imaging and simultaneous multisection imaging to reduce acquisition times [16]. Utilize advanced reconstruction algorithms including AI-based deep learning models and compressed sensing to maintain image quality despite shorter scan times or minor motion [22] [16]. Apply noise-reduction strategies like quiet imaging sequences, acoustic insulation, and proper ear protection to reduce anxiety triggers [16].
Quantitative Evidence for Non-Sedated MRI Approaches
Table 1: Efficacy of Parental Presence in Non-Sedated MRI [3]
| Age Group | Parent Present Success Rate | Parent Absent Success Rate | Odds Ratio |
|---|---|---|---|
| 3-6 years | 59.1% (13/22) | 18.2% (4/22) | 6.50 (CI: 1.64-25.76) |
| 7-10 years | No significant difference | No significant difference | Not significant |
| Overall (3-10 years) | 75.0% (30/40) | 55.0% (22/40) | Not significant |
Table 2: Impact of Audiovisual Distraction (AVD) on Sedation Reduction [16]
| Metric | Pre-AVD Implementation | Post-AVD Implementation | Change |
|---|---|---|---|
| Minimal/moderate sedation rate | 92% of referrals | 71.3% of referrals | -28.8 percentage points |
| Successful non-sedated MRI completion | 6% (n=20) | 100% of triaged patients (n=92) | +94 percentage points |
| Diagnostic quality maintenance | Baseline | 100% of AVD studies | No degradation |
| Exam time adherence | Baseline | 96% within allotted time | Minimal disruption |
Experimental Protocols for Non-Sedated Imaging Research
Protocol 1: Parental Presence Intervention [3]
- Population: Children aged 3-10 years referred for pituitary MRI, stratified into younger (3-6 years) and older (7-10 years) cohorts. Exclude children with diagnosed intellectual disabilities or conditions associated with cognitive impairment.
- Randomization: Block randomization within age strata, with blocks of four participants to ensure balanced allocation between parent present and parent absent groups.
- Intervention: For the parent-present group, a parent accompanies the child into the MRI scan room, sits in a chair next to the scanner, and is instructed to remain calm, speak gently, and help prevent movement. No distraction tools are used.
- Outcome Measures:
- Step 1 - Completion: Ability to complete all MRI sequences.
- Step 2 - Image Quality: Blinded assessment of images for no, mild, or severe artifacts by two pediatricians.
- Step 3 - Final Success: Defined as completion with no or mild artifacts only.
- Procedure: Standardized pituitary MRI protocols with parallel imaging and quiet sequences. Total imaging time approximately 12 minutes. Sessions are terminated if a child cannot cooperate within five minutes or exhibits excessive motion.
Protocol 2: Audiovisual Distraction (AVD) Implementation [16]
- Study Design: Quality improvement project using Plan-Do-Study-Act (PDSA) cycles over 28 months.
- Participants: Children aged 4-18 years referred for MRI, initially targeting those eligible for minimal/moderate sedation. Exclusion criteria include visual impairment, severe developmental delay, or severe ASD precluding AVD use.
- AVD System: Open-bore MRI video system projecting movies onto the upper inner surface of the bore, suitable for head-first positioning.
- Workflow:
- Screening: Sedation staff identify eligible candidates via record review and family contact.
- Assessment: In-person evaluation by certified child life specialist, nurse, and sedation provider on exam day to trial awake vs. sedated MRI.
- AVD Session: Patients triaged to AVD watch content during MRI.
- Contingency: Immediate sedation available for AVD failures at same appointment.
- PDSA Evolution: Criteria broadened successively from initial narrow criteria (age ≥7, CNS tumors) to include various diagnoses, younger ages (≥4 years), and longer scan durations.
Research Workflow: Implementing Non-Sedated MRI Protocols
The Researcher's Toolkit: Essential Materials & Solutions
Table 3: Key Research Reagent Solutions for Pediatric Imaging Studies
| Item | Function/Application | Research Utility |
|---|---|---|
| Audiovisual Distraction (AVD) Systems [16] | In-bore video projection or MRI-compatible goggles to display movies/content | Primary intervention for anxiety reduction and motion minimization; enables measurement of sedation reduction rates |
| Mock MRI Scanner [16] | Replica or simulated MRI environment for practice sessions | Desensitization tool; allows for pre-screening of participant tolerance and acclimatization |
| Child Life Specialist (CLS) [16] | Healthcare professional trained in developmental approaches to prepare children for procedures | Standardizes preparation protocols; improves participant compliance and study retention |
| Positioning Aids [22] | Inflatable pads, vacuum cushions, and head immobilization devices | Reduces involuntary motion artifacts; improves comfort and stability during scanning |
| Quiet MRI Sequences [16] | Pulse sequences with reduced acoustic noise output (e.g., Quiet Suite) | Minimizes sensory trigger for sound-sensitive populations; controls for environmental variable |
| Accelerated MRI Protocols [22] [16] | Techniques like parallel imaging, compressed sensing, and AI reconstruction | Redows acquisition time, a key variable in success rates; allows study of speed vs. quality trade-offs |
| Parental Presence Protocol [3] | Standardized guidelines for parent involvement in the scan room | Critical co-factor intervention; requires safety screening and instruction for consistent application |
Frequently Asked Questions: Troubleshooting Non-Sedation MRI
What is a 'Try Without' pathway? A 'Try Without' pathway is a structured clinical protocol where children are given a low-stakes opportunity to complete an MRI scan without sedation or general anesthesia before it is scheduled as a sedated procedure. This involves using non-pharmacological techniques to facilitate success and having a clear, pre-defined plan to convert to sedation if the child is unable to tolerate the scan [26]. The core principle is to have a "low threshold to try MRI without GA" and to model a "readiness to accept failure" as a normal part of the process [26].
How do we define 'success' and 'failure' for a non-sedation MRI attempt? Clear, multi-stage criteria are essential for objective measurement. Based on clinical research, success is often defined in steps:
- Step 1: Completion: The child completes all planned MRI sequences [3].
- Step 2: Image Quality: The acquired images are of diagnostic quality, rated as having no or only mild motion artifacts by blinded evaluators [3].
- Final Success: The procedure meets both completion and quality criteria. A scan is typically considered a failure if the child is unable to cooperate during positioning, exhibits behavioral distress preventing initiation, or if excessive motion during scanning makes image acquisition impossible [3].
Which children are the best candidates for a 'Try Without' pathway? Success rates vary significantly by age. Evidence shows that parental presence, for instance, significantly improves success rates in children aged 3–6 years but shows no significant difference in children aged 7–10 years, who are generally more capable of following instructions [3]. Candidates are typically identified based on age, developmental ability, scan type, and anticipated scan duration. Children with severe developmental delays or autism spectrum disorder that would preclude understanding of the process may be excluded [16].
What are the most effective non-sedation practices? International surveys show that multiple techniques are used with varying success. The most common and successful practices include the feed-and-swaddle technique for infants, audiovisual distraction (AVD) using video goggles and headphones, and preparation with Child Life Specialists (CLS) [26]. A recent quality improvement project using AVD technology successfully reduced sedation needs by 28.8 percentage points while maintaining a high rate of diagnostic studies [16].
Experimental Protocols & Methodologies
Protocol 1: Evaluating Parental Presence as a Non-Sedation Intervention
- Objective: To evaluate the impact of parental presence in the MRI scan room on the success rate of non-sedated MRI in children aged 3–10 years [3].
- Study Design: Prospective, single-center, randomized controlled trial [3].
- Participants: Children aged 3–10 years referred for short stature evaluation who required pituitary MRI. Exclusions included intellectual disabilities or neurodevelopmental disorders [3].
- Randomization: Participants were stratified by age (3–6 and 7–10 years) and randomized to parent-present or parent-absent groups using block randomization [3].
- Intervention: For the parent-present group, a parent sat next to the MRI scanner, instructed to remain calm, speak gently, and help prevent movement. The parent-absent group was accompanied by a radiologic technologist only [3].
- Outcome Measures:
- Step 1: Completion of all MRI sequences.
- Step 2: Image quality (rated as no, mild, or severe artifact).
- Final Success: Completion with no or mild artifacts [3].
Protocol 2: Implementing an Audiovisual Distraction (AVD) Quality Improvement Project
- Objective: To reduce the utilization of minimal/moderate sedation by at least 20% in children aged 4–18 years through an awake MRI program using AVD technology [16].
- Context: A quality improvement project using Plan-Do-Study-Act (PDSA) cycles at a pediatric sedation clinic [16].
- Intervention: Implementation of an open-bore MRI AVD system that projects a movie inside the scanner bore. A new workflow was created to screen and triage eligible patients [16].
- PDSA Cycles:
- Cycle 1: Targeted patients aged ≥7 years with CNS tumors, head-first scans under 60 minutes.
- Cycle 2: Broadened scope to include any diagnosis for head-first scans.
- Cycle 3: Lowered the age threshold to any patient ≥4 years old deemed cooperative after in-person assessment.
- Cycle 4: Removed scan duration limits and introduced a "motion sensitivity score" to classify protocol difficulty [16].
- Measures:
- Outcome: Percentage of patients completing MRI with AVD without sedation.
- Process: Number of children eligible for AVD per month.
- Balance: Number of non-diagnostic studies and studies exceeding allotted exam time [16].
Data Presentation: Efficacy of Non-Sedation Strategies
Table 1: Success Rates of Common Non-Sedation Practices from an International Survey [26]
| Non-Sedation Practice | Percentage of Sites Using Practice | Reported Success Rate (>75-100% of patients) |
|---|---|---|
| Feed and Swaddle (for infants) | 96% | 51% |
| Video Goggles | 61% | 50% |
| Headphones | 82% | 46% |
| Child Life Specialist | 71% | Most often "moderate" success |
| Natural Sleep | <50% | Most often "fair" success |
Table 2: Quantitative Outcomes from Specific Intervention Studies
| Study & Intervention | Study Design | Key Quantitative Result |
|---|---|---|
| Parental Presence [3] | Randomized Controlled Trial (n=80) | In children aged 3-6, success was significantly higher with a parent present (59.1% vs 18.2%, P=0.012). Final success overall was 70.0% (parent present) vs 55.0% (parent absent). |
| Audiovisual Distraction (AVD) [16] | Quality Improvement Project (n=320 eligible) | Reduced monthly minimal/moderate sedation needs by 28.8 percentage points. 100% of the 92 patients triaged to AVD completed their MRI successfully without sedation. |
| No Sedation Protocol [61] | Cohort Study (n=26 at follow-up) | A no-sedation protocol for mechanically ventilated ICU patients did not increase the risk of long-term psychological sequelae (e.g., PTSD, anxiety, depression) compared to a sedation strategy. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Non-Sedation Pediatric Imaging Research
| Item / Technique | Function in the Experimental Context |
|---|---|
| Audiovisual Distraction (AVD) Systems | MRI-compatible video goggles or in-bore projectors display movies to distract and engage the child during the scanning procedure [16] [26]. |
| Mock MRI Scanner | A full-scale or small-scale simulator familiarizes the child with the MRI environment, sounds, and confinement, building comfort and assessing readiness for a real scan [26]. |
| Child Life Specialist (CLS) | A certified professional who prepares children for procedures using age-appropriate education, psychological support, and coping techniques to reduce anxiety and improve cooperation [3] [26]. |
| Noise-Reduction Strategies | Quiet imaging sequences, insulated magnet bores, and ear protection (headphones/earplugs) mitigate the loud, potentially frightening acoustic noise of the MRI scanner [3] [16]. |
| Accelerated MRI Protocols | Imaging techniques (parallel imaging, compressed sensing, AI reconstruction) reduce scan times, decreasing the duration a child must remain still and increasing the likelihood of success [16]. |
Workflow Visualization: The 'Try Without' Pathway
The following diagram outlines a generalized operational workflow for implementing a 'Try Without' pathway, synthesizing elements from the cited research and quality improvement projects.
Decision Pathway for Non-Sedation MRI
Evaluating Efficacy: Clinical Validation, Comparative Outcomes, and Metrics for Success
Technical Support Center: FAQs for Motion Reduction in Pediatric Imaging Research
This technical support center provides troubleshooting guides and FAQs for researchers developing and evaluating methods to reduce motion in pediatric MRI without sedation. The content is framed within a broader thesis on improving scan success and maintaining diagnostic image quality.
Frequently Asked Questions (FAQs)
Q1: What is a realistic target for reducing sedation use in a pediatric MRI program?
A realistic and evidence-based target is a reduction of approximately 20-30% in sedation utilization. A recent 2025 quality improvement project implemented an awake MRI program using audiovisual distraction (AVD) for children aged 4 to 18 years. The project achieved an average monthly decrease in minimal/moderate sedation use of 28.8 percentage points, successfully meeting and exceeding its 20% goal. This was accomplished while maintaining high diagnostic quality and adhering to scheduled exam times [62].
Q2: What scan success rates can we expect for unsedated young children (ages 2-5)?
Success rates are highly variable and depend on the child's age and cognitive ability. The data below summarizes success rates from research studies involving unsedated young children. Note that "success" can be defined as completing all scan sequences or only some.
Table 1: Scan Success Rates in Young Children Without Sedation
| Age Group | Success Definition | Success Rate | Key Findings | Source |
|---|---|---|---|---|
| 2.0 - 5.0 years | Completed 1 of 3 structural sequences | 72% | Cognitive scores were higher in successful children. | [63] |
| 2.0 - 5.0 years | High-quality data for all 3 structural sequences | 48% | Mock scanner training showed limited advantage. | [63] |
| 5 - 7 years | Completed all 4 fMRI tasks | ~50% | Sample sizes should be scaled up by 50% for this age group. | [64] |
| 8 - 18 years | Completed all 4 fMRI tasks | ~67% | Sample sizes should be scaled up by 33% for this age group. | [64] |
Q3: What are the primary reasons scans fail with unsedated children?
Understanding failure modes is critical for improving protocols. The most common reasons for failure, in order of prevalence, are [64]:
- Anxiety and Fear: The child is frightened by claustrophobia or scanner noise.
- Discomfort: The child is unwilling or unable to lie still for the required duration.
- Excessive Motion: Even if the child remains in the scanner, head or body motion creates artifacts that render the data unusable.
- Technical Errors: Issues with scanner hardware, stimulus-presentation software, or audio/video equipment.
- Unspecified: No clear reason documented by the subject or technologist.
Q4: How do motion artifacts impact diagnostic accuracy, particularly for AI tools?
Motion artifacts significantly reduce diagnostic accuracy, and this impact can be more pronounced for AI tools than for human readers. A 2025 study on stroke MRI found that [65]:
- Motion artifacts were present in 7.4% of scans from suspected stroke patients.
- These artifacts significantly reduced the accuracy of detecting intracranial hemorrhage.
- The reduction was greater for an AI deep learning tool (accuracy dropped from 88% to 67%) than for radiology reports (accuracy dropped from 100% to 93%).
Q5: Are there automated methods to quantify motion artifacts in large datasets?
Yes, deep learning methods are being developed to automate the quality control process. One proposed method uses a Deep Convolutional Neural Network (CNN) to rate motion artifacts on volumetric MR images [66].
- Method: The approach involves transfer learning and fine-tuning of 2D CNNs using annotated T1-weighted volumetric acquisitions.
- Output: The model provides a probability score ( p\in[0,1] ) for the entire acquisition, where higher p-values represent higher severity of motion artifact.
- Utility: This allows for rapid, reference-free screening of large imaging datasets to identify motion-corrupted images, minimizing the time spent on visual quality control [66].
Detailed Experimental Protocols
Protocol 1: Implementation of an Awake MRI Program with Audiovisual Distraction (AVD)
This protocol is based on a successful quality improvement project that significantly reduced sedation rates [62].
- Objective: To reduce the utilization of minimal/moderate sedation by at least 20% in children aged 4 to 18 years while maintaining diagnostic quality.
- Materials:
- MRI scanner with integrated AVD system (capable of playing movies or other content).
- Child-friendly preparation materials.
- Methodology:
- Patient Selection: Identify patients scheduled for MRI who are eligible for either minimal/moderate sedation or an awake scan with AVD.
- Preparation: Prior to the scan, familiarize the child and family with the MRI environment and procedures using child-friendly language and resources.
- AVD Setup: Upon entering the scanner, the child is fitted with headphones and positioned to comfortably view the AVD display.
- Scanning: The AVD system plays a movie of the child's choice throughout the acquisition. A parent remains beside the child for reassurance.
- Quality Control: All studies are reviewed for diagnostic quality. Scan times are monitored to ensure they remain within the allotted schedule.
- Outcome Measures:
- Primary: Percentage reduction in sedation referrals.
- Balance Measures: Percentage of non-diagnostic studies and percentage of studies exceeding allotted exam time.
Protocol 2: Systematic Desensitization for Pediatric fMRI Research
This protocol outlines the preparation steps used to achieve high success rates in unsedated fMRI studies, particularly in longitudinal research [64].
- Objective: To acclimate children to the MRI environment to maximize the success of obtaining high-quality, unsedated fMRI data.
- Materials:
- Mock MRI scanner (optional but beneficial).
- Child-friendly explanatory materials (e.g., storybooks, videos about MRI).
- MR-compatible audiovisual system for communication and stimulus delivery.
- Toys and small gifts for rewards.
- Methodology:
- Child-Friendly Team: A study coordinator and MR technologist trained to work effectively with children lead the process.
- Pre-Visit Preparation: Provide families with links to audio, video, and website resources about MRI scanning, including an e-book that incorporates the scanning procedure into a story.
- Mock Scanner Session (Optional): Offer a training session on a mock scanner within the week prior to the real MRI. This session includes practicing lying still, watching a movie, and listening to recorded MRI sounds.
- On-Scan Day Preparation:
- A research assistant plays short games to build rapport.
- The "rocketship story" or similar narrative is read to overview expectations.
- The child is given a teddy bear to take into the scanner.
- The family is taken to the scanner for a brief familiarization (~5 minutes).
- In-Scanner Support: The child is shown the equipment and positioned. A parent remains nearby. The child is reminded to "hold still like a statue" during scans. The team frequently "checks in" via the audio system [64].
Experimental Workflow Diagram
The following diagram illustrates the logical workflow for implementing a pediatric motion-reduction protocol, from patient selection to outcome analysis.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Materials for Pediatric Motion-Reduction Research
| Item | Function / Application | Examples / Notes |
|---|---|---|
| Audiovisual Distraction (AVD) System | Provides visual and auditory engagement to reduce anxiety and promote stillness during scans. | Integrated MRI-compatible video goggles and headphones. Content is typically age-appropriate movies [62]. |
| Mock MRI Scanner | A simulated scanner environment used to desensitize and train children for the real MRI experience. | Often decorated with child-friendly themes (e.g., rocket ship). Used to practice lying still and acclimating to sounds [63] [64]. |
| Child-Friendly Preparation Materials | Resources to explain the MRI procedure in an understandable and non-threatening way. | Custom e-books, videos, and websites that frame the MRI as an adventure [63] [64]. |
| Deep Convolutional Neural Network (CNN) | An automated tool for rating motion artifacts on MR images, enabling high-throughput quality control. | Used to provide a probability score of motion corruption, minimizing reliance on subjective visual inspection [66]. |
| Behavioral Assessment Tools | To evaluate cognitive and behavioral factors that may predict scan success. | Bayley-III Cognitive Composite, NEPSY-II Phonological Processing. Higher scores are associated with higher success rates [63]. |
This technical support center provides a structured, evidence-based comparison of three primary intervention categories for reducing patient motion in pediatric imaging without sedation. The following guides and FAQs are designed to help researchers and scientists select, implement, and troubleshoot these methodologies within their own experimental frameworks and clinical studies.
# Intervention Comparison Tables
The table below provides a quantitative comparison of the three major intervention categories for reducing motion in pediatric imaging.
| Intervention Category | Reported Sedation Reduction | Key Patient Population | Typical Diagnostic Quality Success Rate | Common Implementation Challenges |
|---|---|---|---|---|
| Audiovisual Distraction (AVD) | 28.8 percentage point decrease [10] | Children aged 4+ without severe developmental delay [10] | 100% diagnostic studies reported [10] | Limited to head-first positioning for some systems; requires patient cooperation [10] |
| Preparation Programs (e.g., MRIamaHero!) | Information Missing | Children aged 4-15 [67] | Information Missing | Requires dedicated child life specialist (CCLS) staff; program setup resources [67] |
| Technical Accelerations (AI, Sequences) | Information Missing | All ages, particularly beneficial for non-cooperative patients [10] | Information Missing | High computational costs; integration with existing scanner software [10] |
The table below outlines the resource and training requirements for implementing each type of intervention.
| Intervention Category | Staffing & Expertise Requirements | Key Hardware/Software Needs | Estimated Implementation Timeline |
|---|---|---|---|
| Audiovisual Distraction (AVD) | CCLS, sedation provider, MRI technologist [10] | MRI-compatible in-bore video projection system [10] | Several months for workflow integration [10] |
| Preparation Programs | Certified Child Life Specialist (CCLS) essential [67] | Mock MRI scanner, educational materials, superhero-themed kits [67] | Information Missing |
| Technical Accelerations | MRI physicists, AI specialists, sequence developers [10] | Advanced sequence software, AI-based reconstruction software/hardware [10] | Information Missing |
# Experimental Protocols & Methodologies
Protocol 1: Implementing an Audiovisual Distraction (AVD) Workflow
This protocol is based on a successful quality improvement project that reduced minimal/moderate sedation needs by an average of 28.8 percentage points per month [10].
1. Pre-Appointment Screening and Planning:
- Patient Identification: Screen referrals for children aged 4 years and older. Key exclusion criteria are visual impairment, severe developmental delay, or severe autism spectrum disorder that would preclude understanding the technology [10].
- Family Communication: Contact the family by phone before the appointment to explain the awake MRI process, assess potential suitability, and manage expectations [10].
2. In-Person Assessment Day of MRI:
- Multidisciplinary Evaluation: A team including a Certified Child Life Specialist (CCLS), nurse, and sedation provider conducts an in-person assessment [10].
- Evaluation Criteria: Assess the child's temperament, demeanor, verbal and body language, anxiety level, and understanding of the procedure after education and preparation [10].
- Trial and Fallback: Patients who fail the awake MRI trial should be immediately scheduled for sedation at the same-day appointment to avoid delays [10].
3. AVD Setup and Execution:
- Technology: Use an MRI-compatible in-bore video system that projects a movie onto the upper inner surface of the magnet bore. Ensure it is suitable for the patient's positioning (initially head-first only in the cited study) [10].
- Preparation: The CCLS uses age-appropriate education and preparation to familiarize the child with the MRI environment and sounds.
- Monitoring: Technologists and staff monitor the patient throughout the scan via camera and two-way communication.
Protocol 2: Running a Mock MRI Preparation Program
This protocol outlines the key components of a superhero-themed program designed to reduce fear and the need for sedation [67].
1. Pre-MRI Education and Familiarization:
- Program Introduction: Enroll the child in a program like "MRIamaHero!" which frames the MRI experience as a superhero mission [67].
- Sensory Familiarization: Use a mock MRI scanner to teach children what the real machine will look like and sound like, allowing them to practice lying still [67].
- Child Life Specialist Role: A CCLS leads the preparation, using play and therapeutic activities to explain the procedure in an age-appropriate manner [67].
2. Gamification and Engagement on Scan Day:
- Theming: Provide the child with a superhero gown and a plush toy to create a positive and empowering association [67].
- Positive Reinforcement: Throughout the process, encourage the child and praise their ability to stay still.
- Reward: Upon successful completion of the MRI, present the child with a "badge of honor," such as a real superhero cape, to celebrate their achievement [67].
Protocol 3: Applying Technical Accelerations for Motion Reduction
This protocol summarizes technical strategies to minimize motion artifacts and scan time, thereby reducing the need for sedation.
1. Scan Time Reduction:
- Implement Advanced Sequences: Utilize parallel imaging and simultaneous multi-slice imaging to acquire data more rapidly [10].
- Apply AI Reconstruction: Employ deep learning models to reconstruct high-quality images from significantly undersampled data, which directly reduces acquisition time [10].
2. Noise-Reduction Strategies:
- Use Acoustic Dampening: Insulate the inner bore of the magnet and use a combination of earplugs and noise-attenuating headphones to reduce the perceived noise level for the patient [10].
- Optimize Sequence Parameters: Use pulse sequences with diminished gradient slew rates and slow ramps for k-space readout to lower acoustic noise output [10].
# Troubleshooting Guides and FAQs
Audiovisual Distraction (AVD) Troubleshooting
Q: What is the first step if a patient consistently moves when the AVD system is active? A: First, verify that the patient can comfortably see the video projection. Then, involve the CCLS to reassess the content; the movie may not be engaging for that particular child. Ensure the audio is clear and at a comfortable volume. If movement persists, the patient may not be a candidate for AVD and should be escalated to the sedation pathway [10].
Q: Our AVD system is only used for head-first scans. How can we accommodate body scans? A: The cited study initially faced this limitation. A potential solution, implemented in a later PDSA cycle, is to install new AVD technology that allows for scanning in any body position, such as MRI-compatible goggles or a more flexible display system [10].
Preparation Program Troubleshooting
Q: A child completes the mock scanner session successfully but becomes highly anxious and uncooperative in the real MRI scanner. What should we do? A: This is a known risk. The protocol should include an immediate fallback plan. Discontinue the awake attempt and reschedule the child for a sedated study. To prevent this, ensure the mock scanner experience is as realistic as possible, including playing recorded MRI sounds at full volume [67].
Q: How can we justify the cost of a dedicated Child Life Specialist to institutional administrators? A: Frame the argument in terms of return on investment. The presence of a CCLS has been shown to reduce sedation rates. Sedation is resource-intensive, requiring more highly trained staff (anesthesiologists, nurses), longer room turnover times, and carries inherent medical risks. Reducing sedation use through CCLS-led programs improves patient throughput and safety [67].
Technical Acceleration Troubleshooting
Q: Our AI-reconstructed images show peculiar artifacts not seen in standard images. What is the cause? A: This is a common challenge. These artifacts may arise from a mismatch between the training data of the AI model and your specific patient population or scanner hardware. Troubleshoot by validating the AI model on a local dataset before full clinical deployment and ensuring your imaging parameters match those recommended by the software vendor [10].
Q: We've implemented noise-reduction sequences, but patients still report the scanner is too loud. What else can be done? A: Technical sequences reduce noise at the source, but complementary passive methods are critical. Ensure you are using a double-layered hearing protection strategy: properly fitted earplugs PLUS MRI-safe noise-attenuating headphones that actively cancel sound. This combined approach is most effective [10].
# Research Reagent Solutions: Essential Materials
The table below lists key materials and technologies used in the featured interventions.
| Item Name | Function/Application in Research | Key Considerations |
|---|---|---|
| MRI-compatible AVD System | Provides audiovisual stimulation to distract pediatric patients during scanning, enabling them to remain still. | Check compatibility with scanner bore size and patient positioning (e.g., head-only vs. whole-body). |
| Certified Child Life Specialist (CCLS) | A trained professional who uses developmental interventions to prepare children for procedures, reducing anxiety and fear. | Essential for both AVD and preparation programs; expertise in child development is key. |
| Mock MRI Scanner | A replica scanner used to acclimate children to the MRI environment, sounds, and confinement without the pressure of a real exam. | Fidelity to the real scanner (appearance and sounds) improves the success rate of the acclimatization. |
| AI-Based Reconstruction Software | Reduces MRI scan times by reconstructing high-quality images from undersampled data, minimizing motion artifact probability. | Requires significant computational resources (e.g., GPUs) and validation for clinical use. |
# Workflow and Pathway Diagrams
Pediatric MRI Motion Reduction Pathway
Intervention Integration Logic
This technical support guide provides methodologies for validating image quality in pediatric imaging research, specifically within the critical context of reducing motion without sedation. For researchers and scientists, rigorous validation using standardized scoring and blinded assessments is paramount for generating reliable, publishable data on novel motion reduction techniques. This document outlines established protocols, troubleshooting tips, and essential tools to ensure the highest standards of experimental integrity.
Frequently Asked Questions (FAQs)
What is a typical standardized scoring system for MRI motion artifacts?
A widely adopted approach uses a 5-point Likert scale to grade the severity of motion artifacts in a standardized and quantifiable manner. This system allows for consistent evaluation across different reviewers and studies.
Table 1: Example 5-Point Motion Artifact Scoring System [24]
| Grade | Severity Level | Description of Image Quality |
|---|---|---|
| 1 | Severe | Non-diagnostic; profound blurring/ghosting obscures anatomic detail |
| 2 | Moderate | Diagnostic confidence significantly reduced; obvious blurring/ghosting |
| 3 | Mild | Some blurring/ghosting present but does not impair diagnostic utility |
| 4 | Minimal | Barely perceptible blurring/ghosting; high diagnostic quality |
| 5 | None | No motion artifacts detected; excellent diagnostic quality |
How do I implement a blinded assessment for my image quality study?
A robust blinded assessment involves a side-by-side review of image pairs by multiple, independent readers who are masked to the experimental conditions. The core protocol is as follows [24]:
- Image Preparation: Create image pairs (e.g., with and without motion correction). Anonymize and randomize the order to prevent reviewers from knowing which is the experimental or control image.
- Independent Review: Two or more board-certified radiologists or experienced reviewers assess the images independently.
- Standardized Scoring: Reviewers use the predefined 5-point scale (see Table 1) to grade each image.
- Statistical Analysis: Calculate the improvement in motion score by subtracting the post-correction score from the pre-correction score. Use statistical tests like the intraclass correlation coefficient (ICC) to evaluate inter-rater reliability. An ICC > 0.75 is considered excellent agreement [68].
What quantitative metrics can I use to validate a new motion correction technique?
Validation should combine qualitative human scoring with quantitative metrics. A comprehensive experimental protocol should report the outcomes listed in the table below. These data were demonstrated in a study of the Scout Accelerated Motion Estimation and Reduction (SAMER) technique [24].
Table 2: Key Validation Metrics from a Motion Correction Study [24]
| Metric | Pre-Correction Result | Post-Correction Result |
|---|---|---|
| Cases with motion artifacts | 73% (24/33 cases) | Not explicitly stated, but artifacts were improved in 79% of cases |
| Severity of artifacts | 15% (5/33) severe; 9% (3/33) moderate | Most notable improvements in moderate-to-severe cases |
| Reclassification of non-diagnostic scans | 8 cases initially non-diagnostic | 50% (4/8) reclassified as diagnostic after correction |
What are common pitfalls in image quality assessment studies?
- Inadequate Blinding: If reviewers can deduce which image is the "improved" one, it introduces bias.
- Poorly Defined Scoring Criteria: Vague descriptors lead to inconsistent scoring between reviewers. Use clear, descriptive anchors for each point on your scale.
- Low Statistical Power: Using too few reviewers or cases can make it impossible to detect statistically significant differences.
- Ignoring Inter-Rater Reliability: Failing to measure and report agreement between reviewers (e.g., using ICC) undermines the credibility of your qualitative scores [68].
Troubleshooting Guides
Issue: Low Inter-Rater Reliability (Poor Agreement Between Reviewers)
Potential Causes and Solutions:
- Cause: Ambiguous or subjective scoring criteria.
- Solution: Organize a consensus meeting before the study. Review sample images representing each score on the scale to calibrate all reviewers.
- Cause: Reviewer fatigue or drift in scoring standards over time.
- Solution: Break the scoring sessions into shorter blocks. Re-calibrate periodically by re-scoring a small set of benchmark images.
- Cause: Insufficient reviewer training.
- Solution: Ensure all reviewers are familiar with the specific appearance of motion artifacts (e.g., blurring, ghosting) and can distinguish them from other artifacts like noise [69].
Issue: Inconclusive Results When Validating a New Motion Reduction Technique
Potential Causes and Solutions:
- Cause: The patient cohort had predominantly mild motion, leaving little room for improvement ("ceiling effect").
- Solution: Target your study population to include a sufficient number of cases with moderate-to-severe motion, as these show the most dramatic improvement with correction techniques [24].
- Cause: The imaging protocol itself is too long, inducing motion that overwhelms the correction method.
- Cause: The quantitative metric is not sensitive enough to detect subtle improvements.
- Solution: Combine qualitative human scoring with multiple quantitative measures, such as signal-to-noise ratio (SNR) or sharpness metrics, to build a more compelling case.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials and Tools for Image Quality Validation Research
| Item | Function in Research | Example / Note |
|---|---|---|
| Standardized Scoring Rubric | Provides a consistent, predefined scale for qualitative image assessment. | A 5-point motion artifact scale is the industry standard [24]. |
| DICOM Viewing Software | Allows for anonymization, randomization, and side-by-side display of images for blinded review. | Software should allow reviewers to adjust window/level. |
| Statistical Analysis Software | Calculates inter-rater reliability and statistical significance of findings. | SPSS, R, or Python with appropriate statistical packages [68]. |
| Audiovisual Distraction (AVD) Systems | A non-pharmacological intervention to reduce patient motion and anxiety. | MRI-safe in-bore video projectors can reduce sedation needs by ~29% [10]. |
| Motion Correction Software | The algorithm or technique under investigation (e.g., SAMER). | Can be prospective (during scan) or retrospective (during reconstruction) [24]. |
| Certified Child Life Specialist (CCLS) | A professional who prepares children for procedures, reducing anxiety and motion. | Critical for successful awake MRI in pediatric cohorts [10]. |
Experimental Protocols & Workflows
Core Protocol: Validating a Motion Correction Technique
This workflow synthesizes methodologies from clinical studies on motion correction and radiology resident evaluation [68] [24].
Protocol: Implementing an Awake Pediatric MRI Program
This workflow is derived from a successful quality improvement project that significantly reduced sedation use [10].
Frequently Asked Questions (FAQs)
FAQ 1: What non-pharmacological interventions are most effective for reducing anxiety and ensuring MRI success in children aged 3-6 years?
Answer: For children aged 3-6, the most effective and resource-efficient intervention is parental presence in the MRI scan room. A recent randomized controlled trial demonstrated that for this age group, the presence of a parent significantly improved the success rate of non-sedated MRI. In the study, children aged 3-6 in the parent-present group had a 59.1% completion rate, compared to only 18.2% in the parent-absent group, representing a six-fold increase in odds of success [3]. Parents should be instructed to remain calm, speak gently, and help prevent the child from moving. This simple, low-cost strategy is recommended as a first-line intervention for younger children [3]. Other supportive practices include preparation with a child life specialist and the use of a mock scanner to familiarize the child with the environment [3] [26].
FAQ 2: How effective is audiovisual distraction (AVD) technology, and what are the key criteria for selecting pediatric patients for an "awake MRI" program?
Answer: Audiovisual distraction (AVD) is highly effective for reducing sedation. One quality improvement project reported that 100% (92/92) of patients triaged to AVD successfully completed their MRI without sedation, and all studies were diagnostic [16]. Key patient selection criteria have been successfully refined through Plan-Do-Study-Act (PDSA) cycles. The recommended criteria are now:
- Age: 4 years and older (broadened from an initial 7 years and older) [16].
- Cooperation: The child is assessed as cooperative, calm, and likely to remain still based on in-person evaluation by a child life specialist, nurse, and sedation provider [16].
- Exclusion Criteria: Patients with severe developmental delay or severe autism spectrum disorder that would preclude understanding the technology or tolerating the confined space are generally excluded [16]. The program can be successfully applied to various diagnostic needs, not just central nervous system imaging [16].
FAQ 3: What patient factors are the strongest predictors of successful non-sedated MRI, and how can they guide research recruitment?
Answer: Research has identified several key patient factors independently associated with successful non-sedated imaging. A large single-institution study (n=731) of a "Scan Without Anesthesia Program" (SWAP) found a 95% success rate and identified the following independent predictors of success [70]:
- Older Age: Success rates increase with patient age.
- Absence of Developmental Delay: Children without developmental delays are significantly more likely to complete the scan successfully.
- Female Sex: The study found female sex was an independent predictor of success, though the underlying reasons require further investigation [70]. These factors are crucial for structuring research inclusion criteria and stratifying participants in clinical trials to ensure balanced study arms and accurate outcome analysis.
Troubleshooting Guides
Problem: High rate of motion artifacts in successful scans, reducing diagnostic quality.
Potential Causes and Solutions:
- Cause 1: Inadequate physical stabilization.
- Solution: Implement standardized positioning and fixation equipment. Use inflatable pads and other positioning aids to comfortably immobilize the patient. This reduces variability and minimizes movement, particularly in the head and extremities [22].
- Cause 2: Scan protocols are not optimized for pediatric populations.
- Solution: Integrate advanced MRI technologies that accelerate acquisition. Utilize deep learning-based reconstruction software (e.g., Deep Resolve) to reduce scan times by up to 50% for certain musculoskeletal protocols, thereby narrowing the window for motion to occur [22]. Additionally, employ rapid imaging sequences like single-shot fast spin echo and parallel imaging to minimize scan duration [18].
- Cause 3: Guidance for the child during the scan is unclear or not age-appropriate.
- Solution: Implement a pediatric-specific in-bore guidance system. Use automated voice messages with a friendly, encouraging tone and child-friendly terminology (e.g., "We are going to take a picture" instead of "initiating scan"). These messages should inform the child about the progress and duration of the examination in a way they can understand, as young children often lack a concrete sense of time [71].
Problem: Significant variability in success rates across different age subgroups.
Potential Causes and Solutions:
- Cause: A "one-size-fits-all" approach is being applied to a heterogeneous pediatric population.
- Solution: Adopt an age-stratified protocol. Evidence strongly supports tailoring interventions to specific age groups [26]:
- Infants (0-2 years): Utilize the "feed-and-swaddle" or "feed-and-wrap" technique, which has a high success rate (>75% at many sites) [26] [22].
- Young Children (3-6 years): Rely heavily on parental presence and preparation with child life specialists [3].
- Older Children (7+ years): Implement audiovisual distraction (video goggles, in-bore movies) as the primary intervention [16] [22].
- Solution: Adopt an age-stratified protocol. Evidence strongly supports tailoring interventions to specific age groups [26]:
Data Presentation: Quantitative Outcomes of Non-Sedation Practices
The following tables summarize key quantitative findings from recent studies on non-sedation practices in pediatric MRI.
Table 1: Success Rates of Primary Non-Sedation Interventions
| Intervention | Target Age Group | Success Rate / Key Finding | Study Details / Effect Size |
|---|---|---|---|
| Parental Presence [3] | 3-6 years | 59.1% completion vs. 18.2% (parent absent) | Odds Ratio (OR) = 6.50; 95% CI: 1.64-25.76 |
| Audiovisual Distraction (AVD) [16] | 4-18 years | 100% success (92/92 patients) | 28.8 percentage point reduction in monthly sedation use |
| Feed-and-Swaddle [26] | Infants | 51% of sites reported >75%-100% success | Most commonly used non-sedation practice (96% of sites) |
| Scan Without Anesthesia Program [70] | Pediatric (mean ~10 years) | 95% success (698/731 patients) | Female sex and absence of developmental delay were independent predictors |
Table 2: Motion Analysis and Economic Impact
| Metric | Findings Without General Anesthesia | Findings With General Anesthesia |
|---|---|---|
| Head Motion [72] | Median mean displacement: 2.19 ± 0.93 mm | Median mean displacement: 1.12 ± 0.35 mm |
| Predominant Motion Type [72] | Translation along z-axis (out of scanner); Significantly more nodding rotation | Translation along z-axis (out of scanner) |
| Economic Impact | Labor cost savings: $139,367.80/year [70] | Increased cost due to anesthetist and monitoring [72] |
| Wait Times [26] | ~17 days | ~30 days |
Experimental Protocol: Evaluating Parental Presence for MRI in Young Children
Objective: To quantitatively evaluate the impact of parental presence in the scan room on the success rate of non-sedated pituitary MRI in children aged 3-10 years.
Methodology (as described in the prospective RCT):
- Participant Recruitment: Children (3-10 years) referred for short stature evaluation and requiring pituitary MRI were eligible. Exclusions included diagnosed intellectual disabilities or neurodevelopmental disorders [3].
- Randomization: Participants were stratified by age (3-6 and 7-10 years) and randomly assigned to "parent present" or "parent absent" groups using block randomization to ensure balanced allocation [3].
- Intervention:
- All children received standardized preparation, including verbal reassurance, printed materials, and a mock MRI session [3].
- Parent Present Group: A parent accompanied the child into the scan room, remained within reach, and was instructed to speak gently and help prevent movement [3].
- Parent Absent Group: The child was accompanied by a radiologic technologist only [3].
- Outcome Measures: Success was assessed in three steps [3]:
- Step 1 (Completion): Ability to complete all MRI sequences.
- Step 2 (Image Quality): Two pediatricians blindly graded images for artifacts (no, mild, or severe).
- Step 3 (Final Success): Defined as completion of MRI with no or only mild artifacts.
Workflow and Pathway Diagrams
Non-Sedation MRI Decision Pathway
Key Motion Patterns in Pediatric MRI
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Non-Sedation Pediatric MRI Research
| Item / Solution | Function in Research | Example / Specification |
|---|---|---|
| Mock MRI Scanner | Familiarizes children with the scanner environment, reducing anxiety and predicting success. Can be full-scale or a small model [3] [26]. | Wooden mock scanner [3]; Educational scanner (e.g., Kitten Scanner) [71]. |
| Audiovisual Distraction (AVD) System | Engages and distracts the child during scanning; a key independent variable in intervention studies. | In-bore video projector systems (e.g., from NordicNeuroLab, PDC Inc.); MRI-compatible video goggles [16] [26] [22]. |
| Child-Friendly In-Bore Guidance | Provides age-appropriate instructions; standardizes communication as part of an experimental protocol. | Pediatric AutoVoice systems using consistent, friendly terminology and characters (e.g., Ollie the Elephant) [71]. |
| Positioning and Fixation Equipment | Minimizes movement artifacts; a controlled variable for ensuring consistent physical setup across participants. | Inflatable pads (e.g., Multipad), head pads, MRI-safe cocoons (e.g., Babyfix) [22]. |
| Motion Tracking System | Quantifies head motion as a primary outcome measure, providing continuous, objective data for analysis. | Markerless tracking systems (e.g., Tracoline) that estimate 3D head position at high frequency [72]. |
| Accelerated MRI Sequences | Reduces scan time, a key confounding variable; enables comparison of diagnostic quality vs. scan duration. | Deep learning reconstruction (e.g., Deep Resolve), parallel imaging, single-shot sequences [18] [22]. |
Conclusion
The collective evidence firmly establishes that a systematic, multi-component approach can successfully replace sedation for a substantial proportion of pediatric MRI examinations. Success hinges on integrating patient-centered non-pharmacological techniques with cutting-edge technological innovations in rapid imaging and motion correction. For the research and drug development community, the widespread adoption of these protocols is paramount. It mitigates the confounding variable of anesthetic agents in neurodevelopmental studies, enhances patient safety in clinical trials, and improves operational efficiency. Future directions must focus on the standardization of these practices across sites to ensure reproducibility, the development of more engaging and effective real-time guidance systems, and the validation of these methods in more diverse and clinically complex pediatric populations. Continued research into the long-term impact of replacing sedation with these alternative strategies will further solidify their role in advancing pediatric biomedical research.
References
- 1. Anesthetic-related Neurotoxicity and Neuroimaging in Children [https://pmc.ncbi.nlm.nih.gov/articles/PMC5407309/]
- 2. Anesthesia and sedation exposure and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10527982/]
- 3. Parental presence improves pediatric MRI success without ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12230062/]
- 4. Imaging Children: Tips and Tricks [https://www.sciencedirect.com/science/article/abs/pii/S1546084307000089]
- 5. Safety challenges related to the use of sedation and ... [https://link.springer.com/article/10.1007/s00247-021-05044-5]
- 6. Newly Developed Methods for Reducing Motion Artifacts in ... [https://pubmed.ncbi.nlm.nih.gov/32023117/]
- 7. Reducing sedation for pediatric body MRI using ... [https://pubmed.ncbi.nlm.nih.gov/29292482/]
- 8. Behavioral interventions for reducing head motion during ... [https://www.sciencedirect.com/science/article/pii/S1053811918300235]
- 9. Systematic Evaluation of Neurotoxicity in Children and Young ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6086728/]
- 10. A quality improvement project to reduce magnetic resonance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12513907/]
- 11. Parental presence improves pediatric MRI success without ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1559935/full]
- 12. Motion artifact correction in fetal MRI based on a ... [https://www.sciencedirect.com/science/article/pii/S1746809422009387]
- 13. Optimizing patient flow logistics: strategic challenges, tactical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538950/]
- 14. How To Reduce Patient Wait Time: Real Solutions That Work [https://www.simbie.ai/reduce-patient-wait-time/]
- 15. Why Flow Efficiency Matters More Than Ever in an Era of Cost ... [https://innolution.com/blog/why-flow-efficiency-matters-more-than-ever-in-an-era-of-cost-cutting]
- 16. A quality improvement project to reduce magnetic ... [https://link.springer.com/article/10.1007/s00247-025-06293-4]
- 17. Using audiovisual intervention to reduce anxiety and ... [https://link.springer.com/article/10.1007/s00247-025-06276-5]
- 18. Effective MRI Practices for Pediatric Patients: Optimizing ... [https://advradiology.org/articles/effective-mri-practices-for-pediatric-patients-optimizing-imaging-protocols-for-safety-and-quality/AdvRadiolImaging.galenos.2025.02486]
- 19. Children Centered Care: child and parent perspectives on a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11805776/]
- 20. Evaluation of motion and its effect on brain magnetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5083190/]
- 21. MRI Motion Artifacts (Ghosting Artifact) [https://mrimaster.com/mri-artifacts/]
- 22. optimizing Musculoskeletal and Neuro Imaging procedures [https://www.pearl-technology.ch/en/blog/sedation-free-pediatric-imaging-optimizing-musculoskeletal-and-neuro-imaging-procedures]
- 23. Free-breathing unsedated MRI in children: Justification and ... [https://pubmed.ncbi.nlm.nih.gov/30635955/]
- 24. Clinical evaluation of scout accelerated motion estimation and ... [https://pubmed.ncbi.nlm.nih.gov/40347259/]
- 25. A Comprehensive Guide to Pediatric Patient Positioning in ... [https://www.domicomed.com/blog/a-comprehensive-guide-to-pediatric-patient-positioning-in-diagnostic-imaging]
- 26. Non-Sedation Practices for Pediatric MRI Deserve Wider ... [https://advances.massgeneral.org/radiology/journal.aspx?id=2606]
- 27. Innovative technologies push pediatric MRI beyond ... [https://www.news-medical.net/news/20250730/Innovative-technologies-push-pediatric-MRI-beyond-diagnostics.aspx]
- 28. Brief mock-scan training reduces head motion during real ... [https://www.sciencedirect.com/science/article/pii/S187892932300049X]
- 29. Parental presence improves pediatric MRI success without ... [https://pubmed.ncbi.nlm.nih.gov/40625391/]
- 30. Prescribing Joy: Child Life Makes a Difference [https://www.shrinerschildrens.org/en/news-and-media/news/2025/05/prescribing-joy-child-life]
- 31. Effectiveness of Audiovisual Distraction Technique and Filmed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10507312/]
- 32. impact of a child-friendly audio-visual intervention [https://link.springer.com/article/10.1007/s00247-025-06308-0]
- 33. Using audiovisual intervention to reduce anxiety and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321924/]
- 34. A Guide to Troubleshooting Complex AV Issues [https://starlite.com/av-troubleshooting/]
- 35. AV Issues: Common Problems and Best Solutions [https://www.ir.com/guides/av-issues-and-solutions]
- 36. Reducing motion artefact in high resolution 7T MRI using ... [https://www.medrxiv.org/content/10.1101/2025.10.10.25337727v1.full-text]
- 37. Low-motion fMRI data can be obtained in pediatric ... [https://www.nature.com/articles/s41598-020-78885-z]
- 38. Advancing MRI reconstruction: A systematic review of deep ... [https://www.sciencedirect.com/science/article/abs/pii/S174680942500802X]
- 39. Advancing MRI Reconstruction: A Systematic Review of Deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11838702/]
- 40. Advancing MRI Reconstruction: A Systematic Review of ... [https://arxiv.org/abs/2501.14158]
- 41. Strategies to perform magnetic resonance imaging in infants and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8027290/]
- 42. (PDF) Pediatric neuro MRI: tricks to minimize sedation [https://www.academia.edu/86356533/Pediatric_neuro_MRI_tricks_to_minimize_sedation]
- 43. State-of-the-Art in Pediatric Body and Musculoskeletal ... [https://www.sciencedirect.com/science/article/abs/pii/S0887217110000077]
- 44. Prospective motion correction improves diagnostic utility of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3933373/]
- 45. Deep learning-based rigid motion correction for magnetic ... [https://www.sciencedirect.com/science/article/pii/S2950162823000012]
- 46. Robust Motion Correction Strategy for Structural MRI in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6192848/]
- 47. Deep learning-based denoising image reconstruction of body ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12119730/]
- 48. PROPELLER/BLADE [https://mriquestions.com/propellerblade.html]
- 49. BladeNet [https://cds.ismrm.org/protected/22MProceedings/PDFfiles/0684.html]
- 50. Deep-learning-based motion correction using multichannel ... [https://pubmed.ncbi.nlm.nih.gov/38808752/]
- 51. A Physics-Informed Deep Learning Model for MRI Brain ... [https://arxiv.org/abs/2502.09296]
- 52. Pediatric neuro MRI: tricks to minimize sedation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5651215/]
- 53. The Diagnostic Accuracy of an Abbreviated vs. a Full MRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12192039/]
- 54. Emergency department implementation of abbreviated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7593499/]
- 55. Abbreviated magnetic resonance imaging protocols in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10551741/]
- 56. BEHAVIORAL INTERVENTIONS FOR REDUCING HEAD ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5857466/]
- 57. Magnetic resonance imaging studies without sedation in ... [https://pubmed.ncbi.nlm.nih.gov/20697244/]
- 58. Reducing motion artefact in high resolution 7T MRI using ... [https://www.medrxiv.org/content/10.1101/2025.10.10.25337727v1]
- 59. Optimization of MR Protocols: A Statistical Decision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2396265/]
- 60. Autism and developmental disability: Management of ... [https://www.rch.org.au/clinicalguide/guideline_index/Autism_and_developmental_disability__Management_of_distress/agitation/]
- 61. Long-term psychological effects of a no-sedation protocol in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3388632/]
- 62. A quality improvement project to reduce magnetic ... [https://pubmed.ncbi.nlm.nih.gov/40768097/]
- 63. Factors Associated With Successful MRI Scanning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5972312/]
- 64. Success Rates for Functional MR Imaging in Children - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7965301/]
- 65. Motion artifacts and image quality in stroke MRI [https://pubmed.ncbi.nlm.nih.gov/40664863/]
- 66. Automatic MR image quality evaluation using a Deep CNN [https://www.sciencedirect.com/science/article/abs/pii/S0895611121000458]
- 67. Pediatric Imaging | Patient Care [https://weillcornell.org/pediatric-radiology]
- 68. DeepSeek-R1 for automated scoring in radiology residency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607140/]
- 69. Motion Artefacts in MRI: a Complex Problem with Many Partial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4517972/]
- 70. Factors and Labor Cost Savings Associated with ... [https://www.sciencedirect.com/science/article/pii/S1076633222006973]
- 71. Improving Pediatric Patients' Magnetic Resonance Imaging ... [https://games.jmir.org/2025/1/e55720]
- 72. Characterisation of Children's Head Motion for Magnetic ... [https://www.frontiersin.org/journals/radiology/articles/10.3389/fradi.2021.789632/full]