Beyond the Clinic: How VR is Outperforming Traditional Neuropsychological Tests in Sensitivity and Ecological Validity
This article systematically compares the sensitivity and validity of Virtual Reality (VR)-based neuropsychological assessments against traditional tools like the MoCA and ACE-III.
Beyond the Clinic: How VR is Outperforming Traditional Neuropsychological Tests in Sensitivity and Ecological Validity
Abstract
This article systematically compares the sensitivity and validity of Virtual Reality (VR)-based neuropsychological assessments against traditional tools like the MoCA and ACE-III. For researchers and drug development professionals, we explore the foundational theory of ecological validity, present current methodological applications across conditions from mTBI to Alzheimer's, analyze troubleshooting for technical and adoption barriers, and synthesize validation studies demonstrating VR's superior predictive power for real-world functioning. Evidence indicates VR assessments offer enhanced sensitivity for early cognitive impairment detection, better prediction of functional outcomes like return to work, and more granular, objective data capture, positioning them as transformative tools for clinical trials and diagnostic precision.
The Ecological Validity Gap: Why Traditional Neuropsychological Tests Fail to Predict Real-World Functioning
Defining Veridicality vs. Verisimilitude in Cognitive Assessment
In neuropsychological assessment, ecological validity refers to the degree to which test performance predicts behaviors in real-world settings or mimics real-life cognitive demands [1]. The pursuit of ecological validity has become increasingly important as clinicians and researchers seek to translate controlled testing environments into meaningful predictions about daily functioning. This quest has given rise to two distinct methodological approaches: veridicality and verisimilitude. Within the rapidly evolving field of cognitive assessment, particularly with the emergence of virtual reality (VR) technologies, understanding the distinction between these approaches is critical for researchers, scientists, and drug development professionals evaluating cognitive outcomes. While veridicality concerns the statistical relationship between test scores and real-world functioning, verisimilitude focuses on the surface resemblance between test tasks and everyday activities [2] [3] [1]. This article examines how these approaches manifest across traditional and VR-based assessment paradigms, comparing their methodological foundations, experimental support, and implications for cognitive sensitivity research.
Conceptual Frameworks: Distinguishing the Two Approaches
Veridicality: The Statistical Correlation Approach
Veridicality represents a quantitative approach to ecological validity that emphasizes statistical relationships between test performance and measurable real-world outcomes [1] [4]. This methodology prioritizes predictive power through established correlation metrics between standardized test scores and criteria of everyday functioning. The veridicality approach underpins many traditional neuropsychological assessments, where the primary goal is to establish statistical associations that can forecast functioning in specific domains.
The theoretical foundation of veridicality assumes that cognitive processes measured in controlled environments have consistent, predictable relationships with real-world performance. For instance, a test exhibiting high veridicality would demonstrate strong correlation coefficients between its scores and independent measures of daily functioning, such as instrumental activities of daily living (IADL) scales or occupational performance metrics [5]. This approach enables researchers to make evidence-based predictions about functional capacity based on test performance, which is particularly valuable in clinical contexts where decisions about diagnosis, treatment planning, or competency determinations are required.
Verisimilitude: The Appearance of Reality Approach
In contrast, verisimilitude emphasizes phenomenological resemblance between testing environments and real-world contexts [1] [4]. Rather than focusing primarily on statistical prediction, this approach aims to create tasks that closely mimic everyday cognitive challenges in their surface features, contextual demands, and required processing strategies. The term literally means "the appearance of being true or real," and in cognitive assessment, it translates to designing tests that engage perceptual, cognitive, and motor systems in ways that closely approximate real-world scenarios.
The theoretical premise of verisimilitude is that environmental context significantly influences cognitive processing, and therefore, assessments that incorporate realistic contextual cues will provide better insights into everyday functioning. This approach often involves simulating real-world environments where participants perform tasks that resemble daily activities, such as preparing a meal, navigating a neighborhood, or shopping in a virtual store [6] [4]. By embedding cognitive demands within familiar scenarios, verisimilitude-based assessments aim to capture cognitive functioning in contexts that more closely mirror the challenges individuals face in their daily lives.
Conceptual Relationship and Distinctions
The relationship between veridicality and verisimilitude represents a fundamental distinction in assessment philosophy. Importantly, these approaches can dissociate—a test high in verisimilitude does not necessarily demonstrate strong veridicality, and vice versa [3]. For example, one study examining social perception in schizophrenia found that a task using real-life social stimuli (high verisimilitude) effectively discriminated between patients and controls but failed to correlate with community functioning (poor veridicality) [3].
This dissociation highlights that surface realism does not guarantee predictive utility, and conversely, that statistically predictive tests may lack face validity. Understanding this distinction is crucial when selecting assessment tools for specific research or clinical purposes, particularly in pharmaceutical trials where cognitive outcomes may serve as primary or secondary endpoints.
Table 1: Core Conceptual Differences Between Veridicality and Verisimilitude
| Dimension | Veridicality | Verisimilitude |
|---|---|---|
| Primary Focus | Statistical prediction of real-world functioning | Surface resemblance to real-world tasks |
| Methodology | Correlation with outcome measures | Simulation of everyday environments |
| Strength | Established predictive validity | Enhanced face validity and participant engagement |
| Limitation | May overlook contextual factors | resemblance doesn't ensure predictive power |
| Common Assessment Types | Traditional neuropsychological batteries | Virtual reality and simulated environments |
Traditional Neuropsychological Assessment: A Veridicality-Based Paradigm
Predominant Approach and Methodologies
Traditional neuropsychological assessments predominantly embrace the veridicality approach to ecological validity [4]. Established instruments like the Montreal Cognitive Assessment (MoCA), Mini-Mental State Examination (MMSE), and Clock Drawing Test (CDT) rely on correlating test scores with measures of daily functioning, caregiver reports, or clinical outcomes [7] [8]. These assessments are typically administered in controlled clinical environments using standardized paper-and-pencil or verbal formats designed to minimize distractions and maximize performance [1].
The experimental protocol for establishing veridicality typically involves cross-sectional correlations or longitudinal predictive studies that examine relationships between test scores and independent functional measures. For example, researchers might administer the MoCA to a cohort of patients with mild cognitive impairment and then examine the correlation between MoCA scores and instrumental activities of daily living (IADL) ratings provided by caregivers [4]. Alternatively, longitudinal studies might investigate how well baseline test scores predict future functional decline or conversion to dementia.
Experimental Evidence and Limitations
Research indicates that traditional neuropsychological tests demonstrate moderate ecological validity when predicting everyday cognitive functioning, with the strongest relationships observed when the outcome measure corresponds specifically to the cognitive domain assessed by the tests [5]. For instance, executive function tests tend to correlate better with complex daily living tasks than with basic self-care activities. However, the veridicality of these traditional measures is moderated by several factors, including population characteristics, illness severity, time since injury, and the specific outcome measures employed [5].
A significant limitation of the veridicality approach emerges from its methodological constraints. The veridicality paradigm is constrained by potential inaccuracies in the outcome measures selected for comparison, limited perspectives on a person's daily behavior, and oversight of compensatory mechanisms that might facilitate real-world functioning despite cognitive impairment [4]. Furthermore, this approach often fails to capture the complex, integrated nature of cognitive functioning in daily life, where multiple processes interact within specific environmental contexts.
Virtual Reality Assessment: Advancing Verisimilitude
Technological Foundations and Methodologies
Virtual reality technologies have enabled significant advances in verisimilitude-based assessment by creating immersive, interactive environments that closely simulate real-world contexts [7] [4]. VR systems can faithfully reproduce naturalistic environments through head-mounted displays (HMDs), hand tracking technology, and three-dimensional virtual environments that mimic both basic and instrumental activities of daily living [6] [4]. Unlike traditional assessments that abstract cognitive processes into discrete tasks, VR-based assessments embed cognitive demands within familiar scenarios that maintain the complexity and contextual cues of everyday life.
The experimental protocol for VR assessment typically involves immersive scenario-based testing where participants interact with virtual environments through natural movements and decisions. For example, the CAVIRE-2 system comprises 14 discrete scenes, including a starting tutorial and 13 virtual scenes simulating daily living activities in familiar residential and community settings [4]. Tasks might include making a sandwich, using the bathroom, tidying up a playroom, choosing a book, navigating a neighborhood, or shopping in a virtual store [6] [4]. These environments are designed with a high degree of realism to bridge the gap between unfamiliar testing environments and participants' real-world experiences.
Experimental Evidence and Advantages
Studies demonstrate that VR-based assessments offer enhanced ecological validity, engagement, and diagnostic sensitivity compared to traditional methods [7]. A feasibility study on VR-based cognitive training for Alzheimer's patients using the MentiTree software reported a 93% feasibility rate with minimal adverse effects, suggesting good tolerability even in cognitively impaired populations [6]. The CAVIRE-2 system has shown moderate concurrent validity with established tools like the MoCA while demonstrating good test-retest reliability (ICC = 0.89) and strong discriminative ability (AUC = 0.88) between cognitively normal and impaired individuals [4].
The advantages of VR-based verisimilitude approaches include automated data collection of performance metrics beyond simple accuracy scores, including response times, error patterns, navigation efficiency, and behavioral sequences [7] [4]. This provides richer, more objective data on cognitive functioning in contexts that closely approximate real-world demands. Additionally, the engaging nature of VR assessments may reduce testing anxiety and improve motivation, potentially yielding more valid representations of cognitive abilities [7] [4].
Comparative Analysis: Quantitative Data and Experimental Protocols
Direct Comparison of Assessment Approaches
Table 2: Performance Comparison Between Traditional and VR Assessment Methods
| Metric | Traditional (Veridicality) | VR-Based (Verisimilitude) | Experimental Context |
|---|---|---|---|
| Ecological Validity | Moderate [5] | Enhanced [7] | Multiple study comparisons |
| Sensitivity/Specificity | MoCA: 86%/88% for MCI [8] | CAVIRE-2: 88.9%/70.5% [4] | Discrimination of cognitive status |
| Test-Retest Reliability | Varies by instrument | ICC = 0.89 for CAVIRE-2 [4] | Repeated assessment studies |
| Participant Engagement | Often limited [7] | High immersion and motivation [9] | User experience reports |
| Cultural/Linguistic Bias | Significant concerns [10] [8] | Potentially reduced through customization | Multi-ethnic population studies |
Detailed Experimental Protocols
Traditional Assessment Protocol (Veridicality-Focused)
The standard administration of the Montreal Cognitive Assessment (MoCA) exemplifies the veridicality approach [8]. The experimental protocol involves:
- Environment: Controlled, quiet room with minimal distractions
- Administration: Trained examiner provides standardized instructions
- Tasks: Assessment across eight cognitive domains (visuospatial abilities, naming, memory, attention, language, abstraction, delayed recall, and orientation) using paper-based materials
- Scoring: Predetermined criteria with maximum score of 30 points
- Validation: Statistical correlation with clinical diagnoses and functional outcomes
The MoCA demonstrates discriminative ability through significant performance differences across clinical groups (young adults > older adults > people with Parkinson's Disease) [8]. However, limitations include susceptibility to educational and cultural biases, with Arabic-speaking cohorts demonstrating significantly lower scores despite similar clinical status [8].
VR Assessment Protocol (Verisimilitude-Focused)
The CAVIRE-2 assessment system exemplifies the verisimilitude approach [4]. The experimental protocol involves:
- Equipment: Head-mounted display (Oculus Rift S) with hand tracking technology
- Environment: 13 immersive virtual scenes simulating daily activities in residential and community settings
- Tasks: Performance of both basic and instrumental activities of daily living (BADL and IADL) with automatic difficulty adjustment
- Duration: Approximately 10 minutes for complete assessment
- Metrics: Automated scoring based on performance matrix of scores and completion time across six cognitive domains
This protocol has demonstrated strong discriminative ability (AUC = 0.88) in distinguishing cognitively healthy older adults from those with mild cognitive impairment in primary care settings [4].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Methodological Components for Ecological Validity Research
| Research Component | Function | Implementation Examples |
|---|---|---|
| Head-Mounted Displays (HMDs) | Creates immersive virtual environments | Oculus Rift S (2560 × 1440 resolution, 115-degree FOV) [6] |
| Hand Tracking Technology | Enables natural interaction with virtual objects | Sensor-based movement recognition projecting real-hand movements to virtual hands [6] |
| Virtual Scenario Libraries | Provides verisimilitude-based task environments | CAVIRE-2's 13 scenes including meal preparation, navigation, shopping [4] |
| Automated Scoring Algorithms | Standardizes assessment and reduces administrator variability | Performance matrices combining accuracy, time, and efficiency metrics [4] |
| Cultural Adaptation Frameworks | Addresses demographic diversity in assessment | Community-specific modifications in test development, administration, and scoring [8] |
| Real-World Outcome Measures | Establishes veridicality through correlation | Instrumental Activities of Daily Living (IADL) scales, caregiver reports, community functioning measures [5] [3] |
The comparison between veridicality and verisimilitude approaches in cognitive assessment reveals complementary strengths rather than mutually exclusive methodologies. Traditional veridicality-based assessments provide established statistical relationships with functional outcomes, while verisimilitude-based VR approaches offer enhanced ecological validity through realistic task environments. For researchers and drug development professionals, the optimal approach may involve integrating both methodologies to leverage their respective advantages.
Future directions should focus on developing hybrid assessment models that incorporate verisimilitude's realistic task environments with veridicality's robust predictive validation. Additionally, addressing technical challenges, establishing standardized protocols, and ensuring accessibility across diverse populations will be crucial for advancing both approaches [7]. As cognitive assessment continues to evolve, the thoughtful integration of veridicality and verisimilitude principles will enhance the sensitivity and clinical relevance of cognitive outcomes in research and therapeutic development.
Limitations of Pen-and-Paper Tests (MoCA, ACE-III, MMSE) in Isolated Settings
In the clinical and research assessment of cognitive impairment, traditional pen-and-paper tests such as the Montreal Cognitive Assessment (MoCA), Addenbrooke's Cognitive Examination (ACE-III), and Mini-Mental State Examination (MMSE) have long been the standard tools. Their widespread use is attributed to their brevity, ease of administration, and established presence in protocols. However, when used in isolated settings—deployed as stand-alone instruments without the context of a full clinical workup—significant limitations emerge that can compromise diagnostic accuracy and ecological validity. These tests, while useful for gross screening, are increasingly found to lack the sensitivity, specificity, and real-world applicability required for early detection and nuanced monitoring of cognitive decline, particularly in the context of progressive neurodegenerative diseases [11]. This guide objectively compares the performance of these traditional tools against emerging alternatives, such as computerized and Virtual Reality (VR)-based assessments, by synthesizing data from recent experimental studies. The analysis is framed within broader research on enhancing the sensitivity of neuropsychological evaluation.
Comparative Performance Data of Traditional Tests
The following tables summarize key experimental data on the performance and limitations of the MoCA, ACE-III, and MMSE, as identified in recent literature.
Table 1: Diagnostic Accuracy and Key Limitations of Traditional Tests
| Test | Primary Reported Strengths | Documented Limitations in Isolated Use | Reported Sensitivity/Specificity Variability |
|---|---|---|---|
| MoCA | Superior to MMSE in detecting Mild Cognitive Impairment (MCI); assesses multiple domains including executive function [12] [13]. | Scores are significantly influenced by age and education (these factors account for up to 49% of score variance [14]); cut-off scores are not universally generalizable across cultures [14]. | Sensitivity for MCI: Variable, 75%-97% (at different thresholds); Specificity: Can be low (4%-77%), leading to high false positives, depending on population and threshold [15]. |
| ACE-III | Provides a holistic profile across five cognitive subdomains; sensitive to a wider spectrum of severity than MMSE [16]. | Lacks ecological validity; tasks do not correspond well to real-world functional demands [11]. Optimal thresholds for dementia/MCI are not firmly established, leading to application variability [15]. | Specificity is highly variable (32% to 100%), indicating a risk of both false positives and negatives when used as a stand-alone screen [15]. |
| MMSE | Well-known, widely used for global cognitive screening [17]. | Insensitive to MCI and early dementia; significant ceiling effects; poor predictor of conversion from MCI to dementia [17] [13]. | For predicting conversion from MCI to all-cause dementia: Sensitivity 23%-76%, Specificity 40%-94% [17]. |
Table 2: Comparative Data from Emerging Assessment Modalities
| Study Focus | Experimental Protocol | Key Comparative Findings |
|---|---|---|
| AI-Enhanced Computerized Test (ICA) [18] | 230 participants (95 healthy, 80 MCI, 55 mild AD) completed the 5-minute ICA, MoCA, and ACE. An AI model analyzed ICA performance. | The ICA's correlation with years of education (r=0.17) was significantly lower than MoCA (r=0.34) and ACE (r=0.41). The AI model detected MCI with an AUC of 81% and mild AD with an AUC of 88%. |
| VR-Based Assessment [11] | 82 young participants (18-28 years) completed both traditional ACE-III and goal-oriented VR/3D mobile games. Correlative and regression analyses were performed. | Game-based scores showed a positive correlation with ACE-III. Game performances provided more granular, time-based data and revealed real-world traits (e.g., hand-use confusion) not captured by ACE-III. |
| VR for Executive Function [19] | Meta-analysis of 9 studies investigating the correlation between VR-based assessments and traditional neuropsychological tests for executive function. | A statistically significant correlation was found between VR-based assessments and traditional measures across subcomponents of executive function (cognitive flexibility, attention, inhibition), supporting VR's validity. |
Detailed Experimental Protocols and Methodologies
Protocol: Validation of a Computerized AI-Based Assessment
A 2021 study directly compared the Integrated Cognitive Assessment (ICA) against MoCA and ACE-III [18].
- Participants: 230 individuals, including 95 healthy controls, 80 with MCI, and 55 with mild Alzheimer's disease.
- Methodology: All participants completed the ICA, MoCA, and ACE. The ICA is a 5-minute, language-independent, computerized test involving a rapid visual categorization task (distinguishing animal from non-animal images) with backward masking to reduce recurrent neural processing. An artificial intelligence (AI) model was trained on the test performance data to classify cognitive status.
- Outcome Measures: The study assessed convergent validity (correlation with MoCA/ACE), diagnostic accuracy (Area Under the Curve - AUC), and bias (correlation with years of education).
- Key Finding: The AI model demonstrated generalizable performance in detecting cognitive impairment, with the ICA showing significantly less education bias than the traditional paper-and-pencil tests [18].
Protocol: Validation of VR/3D Game-Based Assessment against ACE-III
A 2024 study piloted a novel approach using VR and mobile games for cognitive assessment in a young cohort [11].
- Participants: 82 young participants aged 18-28 years.
- Methodology: Participants underwent a traditional ACE-III assessment and also played three goal-oriented games (two in VR, one on a 3D mobile platform). The games were designed to simulate real-world cognitive challenges.
- Analysis: Researchers employed three main analysis methods:
- Correlative Analysis: To measure the relationship between game-based scores and ACE-III scores.
- Z-score Analysis: To compare the distribution of game scores and ACE-III scores.
- Regression Analysis: To explore the association between both scoring methods and cognitive health factors (e.g., age, smoking).
- Key Finding: The study established the plausibility of using goal-oriented games for more granular, time-based, and functional cognitive assessment that can inform about real-world behaviors, a dimension lacking in ACE-III [11].
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 3: Essential Materials and Tools for Cognitive Assessment Research
| Research Reagent / Tool | Function in Experimental Context |
|---|---|
| Montreal Cognitive Assessment (MoCA) | A 30-point, one-page pen-and-paper test administered in ~10 minutes to screen for mild cognitive impairment. It assesses multiple domains: attention, executive functions, memory, language, abstraction, and orientation [18] [13]. |
| Addenbrooke's Cognitive Examination-III (ACE-III) | A more detailed 100-point paper-based cognitive screen assessing five domains: attention and orientation, memory, verbal fluency, language, and visuospatial abilities. Typically takes about 20 minutes to administer [18] [16]. |
| Integrated Cognitive Assessment (ICA) | A 5-minute, computerized cognitive test using a rapid visual categorization task. It employs an AI model to improve accuracy in detecting cognitive impairment and is designed to be unbiased by language, culture, and education [18]. |
| Virtual Reality (VR) Headsets (e.g., Meta Quest) | Standalone VR hardware used to create immersive, ecologically valid testing environments. It allows for natural movement recognition and the simulation of real-world activities for cognitive assessment [20] [11]. |
| VR Cognitive Games (e.g., Enhance VR) | A library of gamified cognitive exercises in VR that assess domains like memory, attention, and cognitive flexibility. These games adapt difficulty based on user performance and provide time-factored, objective metrics [20]. |
| CANTAB (Cambridge Neuropsychological Test Automated Battery) | A computer-based cognitive assessment system consisting of a battery of tests. It is widely used in research and clinical trials to precisely measure core cognitive functions while minimizing human administrator bias [19]. |
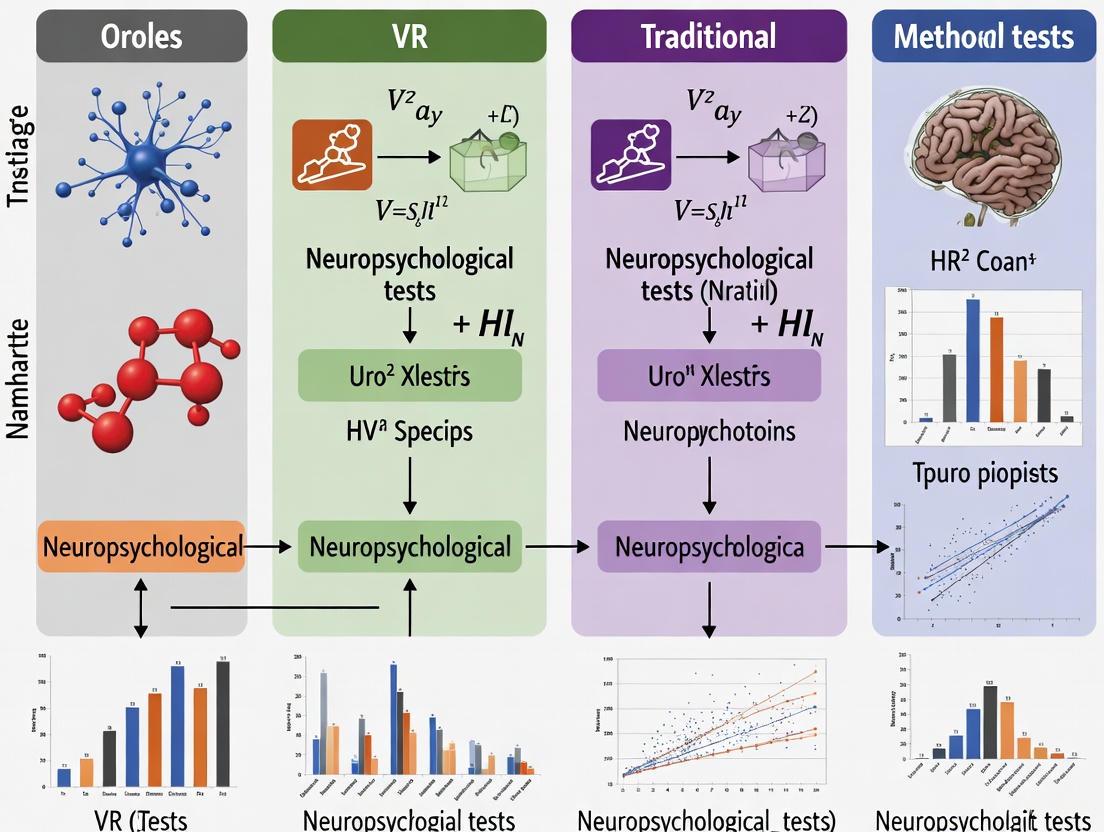
Visualizing the Research Paradigm Shift
The following diagram illustrates the logical relationship and key differentiators between the traditional pen-and-paper assessment paradigm and the emerging technology-enhanced approach.
Virtual reality (VR) has emerged as a transformative tool in cognitive neuroscience and neuropsychological assessment, primarily due to its capacity to mimic real-life cognitive demands with high ecological validity. Traditional neuropsychological tests, while standardized and reliable, often lack realism and fail to capture how cognitive impairments manifest in daily living situations [7] [21]. In contrast, VR creates immersive, interactive environments that simulate the complexity of real-world scenarios, engaging multiple cognitive domains simultaneously within a controlled setting [7]. This article examines the theoretical foundations supporting VR's effectiveness, compares its sensitivity to traditional methods, and presents experimental data validating its use in research and clinical practice.
Theoretical Foundations: Ecological Validity and Cognitive Engagement
The superior ecological validity of VR-based assessments represents their core theoretical advantage. Ecological validity refers to the degree to which test conditions replicate real-world settings and the extent to which findings can be generalized to everyday life [21]. Traditional paper-and-pencil tests are typically administered in quiet, distraction-free environments, which contrasts sharply with the multisensory, dynamic nature of real-world cognitive challenges [21]. VR bridges this gap by creating immersive simulations that preserve experimental control while mimicking environmental complexity.
Key theoretical mechanisms through which VR enhances cognitive assessment include:
- Multi-sensory Integration: VR engages visual, auditory, and sometimes haptic sensory channels simultaneously, creating a more realistic cognitive load that mirrors daily challenges [7].
- Dynamic Environment Interaction: Unlike static traditional tests, VR environments are interactive and evolve based on user decisions, requiring continuous updating of mental representations and strategic planning [7].
- Contextualized Cognitive Demands: VR embeds cognitive tasks within meaningful scenarios (e.g., virtual cooking, navigation, shopping), making assessments more representative of real-world functioning [21].
- Enhanced Patient Engagement: The immersive nature of VR increases motivation and engagement, potentially leading to more accurate performance measures by reducing test fatigue and increasing compliance [7] [22].
The following diagram illustrates the conceptual pathway from traditional assessment limitations to VR solutions and their resulting benefits in neurocognitive evaluation:
Comparative Sensitivity: VR Versus Traditional Neuropsychological Measures
A growing body of research demonstrates that VR-based assessments often show superior sensitivity compared to traditional neuropsychological tests in detecting subtle cognitive impairments, particularly in executive functions, spatial memory, and complex attention.
Sensitivity in Detecting Residual Cognitive Deficits
VR environments have proven particularly effective in identifying lingering cognitive abnormalities in populations where traditional tests may indicate full recovery. A study on sport-related concussions found that VR-based assessment detected residual cognitive impairments in clinically asymptomatic athletes who had normal results on conventional tests [23].
Table 1: Sensitivity and Specificity of VR-Based Assessment for Detecting Residual Cognitive Abnormalities Following Concussion
| Cognitive Domain | VR Assessment Module | Sensitivity | Specificity | Effect Size (Cohen's d) |
|---|---|---|---|---|
| Spatial Navigation | Virtual navigation tasks | 95.8% | 91.4% | 1.89 |
| Whole Body Reaction | Motor response in VR | 95.2% | 89.1% | 1.50 |
| Combined VR Modules | Multiple domains | 95.8% | 96.1% | 3.59 |
The significantly high sensitivity and specificity values, particularly the remarkable effect size for combined VR modules (d=3.59), demonstrate VR's enhanced capability to detect subtle cognitive abnormalities that traditional assessments might miss [23].
Predictive Power for Age-Related Cognitive Decline
Comparative studies have examined the relative predictive power of VR tasks versus traditional measures for identifying age-related cognitive changes. One study directly compared immersive VR tasks with traditional executive function measures like the Stroop test and Trail Making Test (TMT) [24].
Table 2: Comparison of Predictive Power for Age-Related Cognitive Decline: VR vs. Traditional Measures
| Assessment Method | Specific Task/Measure | Contribution to Explained Variance in Age | Statistical Significance |
|---|---|---|---|
| Immersive VR Tasks | Parking simulator levels completed | Significant primary contributor | p < 0.001 |
| Objects placed in seating arrangement | Significant primary contributor | p < 0.001 | |
| Items located in chemistry lab | Significant contributor | p < 0.01 | |
| Traditional Measures | Stroop Color-Word Test | Lesser contributor | Not specified |
| Trail Making Test (TMT) | Lesser contributor | Not specified |
The VR measures were found to be stronger contributors than existing traditional neuropsychological tasks in predicting age-related cognitive decline, highlighting their enhanced sensitivity to cognitive changes associated with aging [24].
Experimental Evidence and Methodological Protocols
VR Cognitive Training in Older Adults
A cluster randomized controlled trial examined the effects of immersive leisure-based VR cognitive training in community-dwelling older adults, employing rigorous methodology to compare VR interventions with active control conditions [25].
Table 3: Experimental Protocol: VR Cognitive Training for Community-Dwelling Older Adults
| Methodological Component | VR Group Protocol | Control Group Protocol |
|---|---|---|
| Study Design | Cluster randomized controlled trial | Cluster randomized controlled trial |
| Participants | 137 community-dwelling older adults (≥60 years), MMSE ≥21 | Same participant characteristics |
| Intervention | Fully immersive VR gardening activities (planting, fertilizing, harvesting) using HTC VIVE PRO | Well-arranged leisure activities without cognitive focus |
| Session Duration & Frequency | 60 minutes daily, 2 days per week, for 8 weeks | Identical duration and frequency |
| Cognitive Challenges | Seven difficulty levels targeting attention, processing speed, memory, spatial relations, executive function | No focused cognitive challenges |
| Primary Outcomes | MoCA, WMS-Digit Span Sequencing (DSS), Timed Up and Go (TUG) | Identical measures |
| Key Findings | Significant improvements in MoCA (p<0.001), WMS-DSS (p=0.015), and TUG (p=0.008) compared to control | Lesser improvements on outcome measures |
The experimental protocol ensured comparable intervention intensity between groups while isolating the effect of the VR cognitive training component. The significant improvements in global cognition, working memory, and physical function demonstrate VR's effectiveness when compared to an active control group, addressing methodological limitations of earlier studies that used passive control groups [25].
Meta-Analytic Evidence for Mild Cognitive Impairment
A comprehensive meta-analysis of 30 randomized controlled trials evaluated the effects of VR-based interventions on cognitive function in adults with mild cognitive impairment (MCI), providing robust evidence across multiple studies [26].
Table 4: Effects of VR-Based Interventions on Cognitive Function in MCI: Meta-Analysis Results
| Cognitive Domain | Assessment Tool | Standardized Mean Difference (SMD) | Statistical Significance | Certainty of Evidence (GRADE) |
|---|---|---|---|---|
| Global Cognition | Montreal Cognitive Assessment (MoCA) | 0.82 | p = 0.003 | Moderate |
| Global Cognition | Mini-Mental State Examination (MMSE) | 0.83 | p = 0.0001 | Low |
| Attention | Digit Span Backward (DSB) | 0.61 | p = 0.003 | Low |
| Attention | Digit Span Forward (DSF) | 0.89 | p = 0.002 | Low |
| Quality of Life | Instrumental Activities of Daily Living (IADL) | 0.22 | p = 0.049 | Moderate |
The meta-analysis revealed that optimal cognitive outcomes were associated with specific VR parameters: semi-immersive systems, session durations of ≤60 minutes, intervention frequencies exceeding twice per week, and participant groups with lower male proportion (≤40%) [26]. These findings provide guidance for researchers designing VR-based cognitive interventions.
The following workflow diagram illustrates a typical experimental protocol for VR-based cognitive assessment, highlighting the integration of traditional and VR methodologies:
Implementing VR-based cognitive assessment requires specific hardware, software, and methodological resources. The following table details key components of a VR research toolkit and their functions in cognitive assessment protocols.
Table 5: Essential Research Toolkit for VR-Based Cognitive Assessment
| Tool/Resource | Function in Research | Example Applications | Considerations |
|---|---|---|---|
| Head-Mounted Displays (HMD) | Provides fully immersive VR experience | HTC VIVE PRO [25]; Oculus Rift | Consumer-grade vs. clinical-grade systems; resolution and field of view |
| VR Authoring Software | Enables creation of custom virtual environments | Unity 3D; Unreal Engine | Programming expertise required; asset libraries available |
| 360-Degree Video Capture | Records real-world environments for VR | Medical training simulations [27] | Special 360-degree camera equipment needed |
| Integrated VR Treadmills | Allows natural locomotion in VR | Motekforce Link treadmill [28] | Enables walking-based cognitive assessment |
| Physiological Monitoring | Records concurrent physiological data | EEG systems [29]; heart rate monitors | Synchronization with VR events crucial |
| Traditional Assessment Tools | Provides baseline and validation measures | MoCA [25] [26]; Digit Span [25] [26]; Trail Making Test [24] | Essential for establishing convergent validity |
| Data Analysis Platforms | Processes behavioral metrics from VR | Custom MATLAB/Python scripts; commercial analytics | Automated performance scoring advantageous |
VR technology represents a paradigm shift in neurocognitive assessment by successfully mimicking real-life cognitive demands through immersive, ecologically valid environments. The experimental evidence demonstrates that VR-based assessments frequently show superior sensitivity compared to traditional measures, particularly for detecting subtle cognitive impairments, predicting age-related decline, and evaluating complex cognitive domains like executive function and spatial memory. The theoretical strength of VR lies in its ability to engage multiple cognitive processes simultaneously within realistic contexts while maintaining experimental control. As research methodologies continue to refine VR protocols and address current limitations regarding standardization and accessibility, VR is poised to become an increasingly essential tool in cognitive neuroscience research and clinical neuropsychological practice.
A core challenge in neuropsychology and drug development is the ecological validity gap: the limited ability of traditional cognitive assessments to predict a patient's real-world functioning. Conventional pen-and-paper neuropsychological tests, while standardized and reliable, are administered in controlled clinical settings that poorly simulate the cognitive demands of daily life [21]. This creates a significant disconnect between clinical scores and actual functional capacity, complicating therapeutic development and clinical decision-making.
Virtual Reality (VR) emerges as a transformative solution by enabling verisimilitude—designing assessments where cognitive demands mirror those in naturalistic environments [4]. By immersing patients in simulated real-world scenarios, VR-based tools can capture a more dynamic and functionally relevant picture of cognitive health, thereby creating a more powerful predictive link between assessment results and real-world outcomes.
Comparative Analysis: VR vs. Traditional Neuropsychological Tests
The table below summarizes key performance metrics from recent studies directly comparing VR-based cognitive assessments with traditional tools.
Table 1: Quantitative Comparison of VR and Traditional Cognitive Assessments
| Study & Assessment Tool | Study Population | Key Correlation with Traditional Tests | Association with Real-World Function (ADL) | Discriminatory Power (e.g., AUC) |
|---|---|---|---|---|
| CAVIR [30] | 70 patients with mood/psychosis disorders & 70 HC | Moderate correlation with global neuropsychological test scores (rₛ = 0.60, p<0.001) | Weak-moderate association with ADL process skills (r = 0.40, p<0.01); superior to traditional tests | Sensitive to impairment; differentiated employment status |
| CAVIRE-2 [4] | 280 multi-ethnic older adults | Moderate concurrent validity with MoCA | Based on verisimilitude paradigm (simulated ADLs) | AUC=0.88 for distinguishing cognitive status |
| VEGS [31] | 156 young adults, healthy older adults, & clinical older adults | Highly correlated with CVLT-II on all variables | Assesses memory in realistic, distracting environments | N/A |
| SLOF (Rating Scale) [32] | 198 adults with schizophrenia | N/A (itself a functional rating scale) | Superior predictor of performance-based ability measures | N/A |
HC: Healthy Controls; ADL: Activities of Daily Living; AUC: Area Under the Curve; MoCA: Montreal Cognitive Assessment; CVLT-II: California Verbal Learning Test, Second Edition; SLOF: Specific Levels of Functioning Scale.
Detailed Experimental Protocols and Methodologies
Protocol: Cognition Assessment in Virtual Reality (CAVIR)
The CAVIR test was designed to assess daily-life cognitive skills within an immersive virtual reality kitchen scenario [30].
- Objective: To investigate the validity and sensitivity of CAVIR and its association with Activities of Daily Living (ADL) in patients with mood or psychosis spectrum disorders.
- Participants: 70 symptomatically stable patients and 70 healthy controls.
- Procedure:
- Participants completed the CAVIR assessment, which involves performing a series of goal-directed tasks in a virtual kitchen.
- They also underwent a battery of standard neuropsychological tests.
- Clinical symptoms, functional capacity, and subjective cognition were rated.
- Patients' real-world ADL ability was evaluated using the Assessment of Motor and Process Skills (AMPS), an observational assessment of performance in everyday tasks.
- Outcome Measures: The primary analyses focused on correlations between global CAVIR performance, global neuropsychological test scores, and AMPS scores.
Protocol: Virtual Environment Grocery Store (VEGS) vs. CVLT-II
This study compared a VR-based memory test with a traditional list-learning test [31].
- Objective: To compare episodic memory performance on the VEGS and the CVLT-II across young adults, healthy older adults, and older adults with a neurocognitive diagnosis.
- Participants: 156 participants (53 young adults, 85 healthy older adults, 18 clinical older adults).
- Procedure:
- Participants were administered the CVLT-II, a standard verbal list-learning test.
- They also completed the VEGS, a VR-based task where they navigate a virtual grocery store and are asked to memorize items to purchase amidst everyday auditory and visual distractors.
- The Delis–Kaplan Executive Function System Color-Word Interference Test (D-KEFS CWIT) was administered to assess executive function.
- Outcome Measures: Correlations between VEGS and CVLT-II scores, comparison of recall scores between the two tests, and analysis of their relationship with executive function measures.
Protocol: Validation of CAVIRE-2 as a Cognitive Screening Tool
This study validated a fully immersive, automated VR system for comprehensive cognitive assessment [4].
- Objective: To validate the CAVIRE-2 software as a tool to distinguish between cognitively healthy and impaired older adults in a primary care setting.
- Participants: 280 multi-ethnic Asian adults aged 55-84 recruited from a primary care clinic.
- Procedure:
- Participants completed the CAVIRE-2 assessment, which consists of 13 scenarios simulating Basic and Instrumental Activities of Daily Living (BADL and IADL) in local community settings.
- Performance was automatically scored based on a matrix of accuracy and completion time across the six cognitive domains.
- All participants were independently assessed using the Montreal Cognitive Assessment (MoCA).
- Outcome Measures: Concurrent validity (correlation with MoCA), test-retest reliability, internal consistency, and discriminative ability (AUC) to identify cognitive impairment.
Logical Workflow: From Assessment to Functional Prediction
The following diagram illustrates the conceptual pathway through which VR-based assessments create a more robust predictive model for real-world functioning compared to traditional methods.
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers seeking to implement or develop VR-based functional assessments, the following toolkit details essential components and their functions derived from the cited experimental protocols.
Table 2: Research Reagent Solutions for VR Functional Assessment
| Toolkit Component | Function & Rationale | Exemplar Tools from Research |
|---|---|---|
| Immersive VR Hardware | Provides a controlled yet ecologically valid sensory environment for assessment. | Head-Mounted Displays (HMDs) for full immersion [21] [4] |
| Software/VR Platform | Generates standardized, interactive scenarios simulating real-world cognitive demands. | CAVIR (kitchen scenario) [30]; VEGS (grocery store) [31]; CAVIRE-2 (community & residential settings) [4] |
| Performance Metrics Algorithm | Automates scoring to reduce administrator bias and enhance objectivity; captures multi-dimensional data. | CAVIRE-2's matrix of scores and completion time [4]; Error type and latency profiles [33] |
| Traditional Neuropsychological Battery | Serves as a criterion for establishing convergent validity of the novel VR tool. | MoCA [4]; CVLT-II [31]; MCCB, UPSA-B [32] |
| Real-World Function Criterion | Provides a benchmark for validating the ecological and predictive validity of the VR assessment. | Assessment of Motor and Process Skills (AMPS) [30]; Specific Levels of Functioning (SLOF) scale [32] |
The evidence demonstrates a clear paradigm shift in cognitive assessment. VR-based tools like CAVIR, VEGS, and CAVIRE-2 consistently show moderate to strong correlations with traditional tests, proving they measure core cognitive constructs. More importantly, they establish a superior predictive link to real-world functioning by leveraging immersive, ecologically valid environments. For researchers and drug developers, this enhanced functional prediction is critical. It enables more sensitive detection of cognitive changes in clinical trials and provides more meaningful endpoints that truly reflect a treatment's potential impact on a patient's daily life.
VR in Action: Methodological Approaches and Applications in Cognitive Assessment
In the context of comparing Virtual Reality (VR) with traditional neuropsychological tests, a critical technical distinction lies in the level of immersion offered by different systems. The choice between immersive and non-immersive VR is not merely one of hardware preference but fundamentally influences the ecological validity, user engagement, and, consequently, the sensitivity of cognitive assessments [34] [4]. Immersive systems typically use Head-Mounted Displays (HMDs) to fully surround the user in a digital environment, whereas non-immersive systems rely on standard monitors, providing a window into a virtual world [35]. This guide objectively compares these systems based on hardware, software, and experimental data, providing researchers and drug development professionals with a framework for selecting appropriate technologies for sensitive neuropsychological research.
Hardware and System Architecture
The core difference between immersive and non-immersive VR systems stems from their fundamental hardware architecture, which directly dictates the user's level of sensory engagement and the system's application potential.
Table 1: Core Hardware Comparison
| Feature | Immersive VR (HMD-Based) | Non-Immersive VR (Desktop-Based) |
|---|---|---|
| Primary Display | Head-Mounted Display (HMD) with stereoscopic lenses [36] [35] | Standard monitor, television, or smartphone screen [35] |
| Tracking Systems | Advanced inside-out tracking with multiple cameras; head, hand, and controller tracking with 6 degrees of freedom (6DoF) [36] [37] | Limited to traditional input; no positional tracking of the user's head [35] |
| User Input | Advanced motion controllers, data gloves, and vision-based hand tracking [36] [35] | Traditional peripherals (mouse, keyboard, gamepad) [35] |
| Level of Immersion | High to very high; designed to shut out the physical world and create a strong sense of "presence" [34] [35] | Low; user remains fully aware of their physical surroundings [35] |
| Example Hardware | Meta Quest 3, Sony PlayStation VR2, Apple Vision Pro, HTC Vive Pro 2 [38] [39] [40] | Standard PC or laptop setup without a headset [35] |
The Immersion Spectrum and Associated Technologies
VR systems exist on a spectrum of immersion, largely defined by hardware. Fully Immersive VR represents the highest level, where HMDs completely occupy the user's visual and auditory fields to create a compelling sense of "presence" – the psychological feeling of being in the virtual environment [36] [35]. Key enabling technologies include high-resolution displays (often exceeding 4K per eye), high refresh rates (90Hz or higher) to prevent motion sickness, and pancake lenses that allow for slimmer headset designs [36] [37]. Non-Immersive VR, in contrast, provides a windowed experience on a standard screen, with interaction mediated by traditional peripherals [35]. A middle ground, Semi-Immersive VR, often uses large projection systems or multiple monitors to dominate the user's field of view without completely isolating them, commonly found in flight simulators [35].
Experimental Protocols and Empirical Findings
The structural differences between immersive and non-immersive VR systems lead to measurable variations in user experience and cognitive outcomes, which are critical for research design.
Key Comparative Experimental Protocols
Controlled studies often expose participants to the same virtual environment via different hardware systems to isolate the effect of immersion.
- Museum Environment Study: A 2025 controlled study involved 87 college students randomly assigned to either an HMD (immersive) or a non-immersive (desktop) version of the same virtual museum—a digital twin of the "L'altro Renaissance" exhibition. The objective was to measure the effects on spatial learning, aesthetic appreciation, and behavioral intention [34].
- Protocol: After the virtual exploration, participants completed questionnaires assessing their sense of immersion, the pleasantness of the experience, and their willingness to repeat a similar museum experience. This protocol directly links the hardware interface to psychological and behavioral outcomes [34].
- Cognitive Assessment Validation (CAVIRE-2): A separate study validated a fully immersive VR system (CAVIRE-2) as a tool for assessing six cognitive domains in older adults (aged 55-84) in a primary care setting. Participants completed both the VR assessment and the traditional Montreal Cognitive Assessment (MoCA) [4].
- Protocol: The CAVIRE-2 software presented participants with 13 scenarios in virtual environments simulating basic and instrumental activities of daily living (BADL and IADL). Performance was automatically scored based on a matrix of accuracy and completion time, providing a multi-domain cognitive profile with high ecological validity [4].
Empirical data consistently shows that the level of immersion significantly impacts user experience and can influence cognitive measures.
Table 2: Comparative Experimental Data from Key Studies
| Study Focus | Immersive VR (HMD) Findings | Non-Immersive VR (Desktop) Findings |
|---|---|---|
| Museum Experience | Produced a greater sense of immersion, was rated as more pleasant, and led to a higher intention to repeat the experience [34]. | Was perceived as less immersive and less pleasant compared to the HMD condition [34]. |
| Spatial Navigation & Learning | Mixed results: Some studies show enhanced engagement but sometimes poorer spatial recall when physical movement is restricted, potentially due to a lack of idiothetic cues [34]. | Can sometimes lead to better spatial recall (e.g., map drawing) and causes less motion sickness and lower cognitive workload [34]. |
| Cognitive Assessment | Shows high sensitivity and ecological validity. CAVIRE-2 demonstrated an Area Under Curve (AUC) of 0.88 for discriminating cognitive status, with 88.9% sensitivity and 70.5% specificity [4]. | Not typically used for comprehensive, automated cognitive assessments in the same ecological manner as systems like CAVIRE-2 [4]. |
| Educational Learning | Enhances engagement and long-term retention by cultivating longer visual attention and fostering a higher sense of immersion [34]. | Provides a viable and often more accessible option, though with lower engagement and long-term retention potential [34]. |
A systematic review of Extended Reality (XR) for neurocognitive assessment further supports these findings, concluding that VR-based tools ( predominantly HMD) are more sensitive, ecologically valid, and engaging compared to traditional assessment tools [41] [7].
The Scientist's Toolkit: Key Research Reagents and Materials
For researchers designing experiments comparing VR systems, the following "reagents" or core components are essential.
Table 3: Essential Research Materials for VR System Comparison
| Item | Function in Research | Considerations for Selection |
|---|---|---|
| Head-Mounted Display (HMD) | The primary hardware for delivering the fully immersive VR condition. Creates stereoscopic 3D visuals and tracks head movement [36] [35]. | Key specs include per-eye resolution, field of view (FOV), refresh rate, and tracking capabilities (e.g., inside-out). Comfort for extended sessions is critical [38] [37]. |
| VR Motion Controllers | Enable natural interaction within the immersive virtual environment. Provide input and often include haptic feedback [36] [39]. | Evaluate tracking accuracy, ergonomics, and battery life. Consider systems that also support vision-based hand tracking for more natural input [38] [37]. |
| High-Performance PC/Console | Required to run high-fidelity VR experiences, either by rendering content for PC-connected headsets or for developing complex virtual environments [39] [40]. | A powerful GPU and CPU are necessary. For standalone HMDs, the onboard processor is key (e.g., Snapdragon XR2 Gen 2) [38] [39]. |
| Standard Desktop Computer | The hardware platform for the non-immersive VR condition. Runs the virtual environment on a standard monitor [35]. | Should have sufficient graphics capability to run the 3D environment smoothly to ensure performance differences are not due to lag or low frame rates. |
| Identical Virtual Environment Software | The core experimental stimulus. To ensure a valid comparison, the virtual environment (VE) must be functionally identical across immersive and non-immersive conditions [34]. | The software platform must support deployment to both HMD and desktop formats without altering the core logic or visual fidelity of the tasks. |
| Validated Questionnaires | Measure psychological constructs affected by immersion, such as sense of presence, user engagement, simulator sickness, and usability [34]. | Use standardized scales (e.g., Igroup Presence Questionnaire, Simulator Sickness Questionnaire) to allow for comparison with existing literature. |
The decision between immersive and non-immersive VR systems is a fundamental one that directly impacts the ecological validity, user engagement, and sensitivity of neuropsychological research. Immersive HMD-based systems consistently demonstrate a superior capacity to elicit a sense of presence and show great promise as highly sensitive tools for ecological cognitive assessment, as evidenced by their growing use in clinical validation studies [4] [7]. Non-immersive systems, while less sensorially engaging, offer greater accessibility, reduced risk of simulator sickness, and can be perfectly adequate for certain cognitive tasks [34] [35]. The choice is not which system is universally better, but which is most appropriate for the specific research question, target population, and experimental constraints. As the technology continues to evolve, this hardware-level comparison will remain a cornerstone of rigorous experimental design in VR-based cognitive science and drug development.
Virtual reality (VR) is reshaping neuropsychological assessment by introducing dynamic, ecologically valid tools for evaluating core cognitive domains. This guide provides a comparative analysis of VR-based and traditional methods for assessing memory, attention, and executive functions, synthesizing current research data to inform researcher and practitioner selection.
Comparative Performance Data Across Cognitive Domains
The table below summarizes quantitative findings from recent studies directly comparing VR and traditional neuropsychological assessments.
| Cognitive Domain | Assessment Tool | Key Comparative Findings | Research Context |
|---|---|---|---|
| Working Memory | Digit Span Task (DST) | Similar performance between PC and VR versions [42]. | Study with 66 healthy adults [42]. |
| Visuospatial Working Memory | Corsi Block Task (CBT) | PC version enabled better performance (e.g., longer sequence recall) than VR version [42]. | Study with 66 healthy adults [42]. |
| Processing Speed / Psychomotor | Deary-Liewald Reaction Time Task (DLRTT) | Significantly faster reaction times (RT) on PC than in VR [42]. | Study with 66 healthy adults [42]. |
| Processing Speed | Beat Saber VR Training | Significant increase in processing speed (p=.035) and reduced errors (p<.001) post-VR training [43]. | RCT with 100 TBI patients [43]. |
| Global Cognition & Daily Function | Cognition Assessment in VR (CAVIR) | Moderate correlation with standard neuropsychological tests (r𝑠=0.60, p<.001). Moderate association with daily living (r=0.40, p<.01), outperforming traditional tests [30]. | Study with 70 patients & 70 controls [30]. |
| Reaction Time | Novel VR vs. Computerized RT | RTs were significantly longer in VR (p<.001). Moderate-to-strong correlations between platforms (r≥0.642) confirm validity [44]. | Study with 48 participants [44]. |
Detailed Experimental Protocols
Understanding the methodology behind key studies is crucial for evaluating their findings.
Protocol: Comparative Validity of VR Working Memory and Psychomotor Assessments
- Objective: To investigate the convergent validity, user experience, and usability of VR-based versus PC-based assessments of short-term memory, working memory, and psychomotor skills [42].
- Design: Within-subjects comparative study.
- Participants: 66 adults (aged 18-45) [42].
- Intervention & Comparison:
- VR Assessments: Administered using an HTC Vive Pro Eye headset. Participants performed immersive versions of the Digit Span Task (DST), Corsi Block Task (CBT), and Deary-Liewald Reaction Time Task (DLRTT) using hand controllers for naturalistic interaction [42].
- PC Assessments: Identical cognitive tasks were hosted on the PsyToolkit platform. Participants responded using standard computer interfaces (e.g., keyboard, mouse) [42].
- Outcome Measures: Primary outcomes were performance scores on cognitive tasks. Secondary measures included user experience and system usability ratings, and the influence of demographic and IT skills [42].
Protocol: VR Cognitive Training for Traumatic Brain Injury (TBI)
- Objective: To evaluate the effect of a commercial VR game on sustained attention (primary outcome), processing speed, and working memory (secondary outcomes) after TBI [43].
- Design: Randomized Controlled Trial (RCT) with 1:1 allocation.
- Participants: 100 individuals aged 18-65 with complicated mild-to-severe TBI [43].
- Intervention: The VR training group played Beat Saber for 30 minutes per day, 5 days a week, for 5 weeks. This rhythm game requires sustained attention and rapid motor responses [43].
- Control: The active control group received information about everyday activities that might impact cognition [43].
- Outcome Measures: The primary outcome was sustained attention measured by the Conners' Continuous Performance Test (CPT-3). Secondary outcomes included processing speed (CPT-3 Hit Reaction Time), working memory (WAIS-IV digit span), and self-report measures of executive function and quality of life [43].
Protocol: Ecological Validity of a VR Kitchen Task
- Objective: To validate the novel Cognition Assessment in Virtual Reality (CAVIR) test and investigate its association with neuropsychological performance and real-world activities of daily living (ADL) [30].
- Design: Cross-sectional study.
- Participants: 70 symptomatically stable patients with mood or psychosis spectrum disorders and 70 healthy controls [30].
- Intervention: All participants completed the CAVIR test, which involves performing daily-life cognitive tasks within an immersive virtual reality kitchen scenario [30].
- Comparison: Participants also completed a standard battery of neuropsychological tests. In patients, ADL ability was evaluated using the Assessment of Motor and Process Skills (AMPS) [30].
- Outcome Measures: The primary outcomes were the correlation between global CAVIR performance and global neuropsychological test scores, and the correlation between CAVIR performance and AMPS scores in patients [30].
The Scientist's Toolkit: Research Reagent Solutions
This table details key materials and their functions for researchers designing VR neuropsychological assessment studies.
| Tool / Solution | Primary Function in Research | Example in Use |
|---|---|---|
| Head-Mounted Display (HMD) | Presents immersive, 3D environments; blocks external distractions. | HTC Vive Pro Eye (with eye-tracking) used for DST, CBT, and DLRTT assessments [42]. |
| Game-Engine Software | Platform for developing and running controlled, interactive VR assessment scenarios. | Unity 2019.3 used to build ergonomic VR neuropsychological tests [42]. |
| Hand Motion Controllers | Enables naturalistic, embodied interaction with the virtual environment, replacing keyboard/mouse. | SteamVR controllers used to manipulate virtual objects in CBT and DLRTT [42]. |
| Traditional Neuropsychological Batteries | Provides the standardized, gold-standard metric for establishing convergent validity of new VR tools. | WAIS-IV Digit Span, Corsi Block, and CPT-3 used as benchmarks for VR task performance [43] [30] [42]. |
| Activities of Daily Living (ADL) Scales | Provides an ecologically valid criterion to test if VR assessments better predict real-world function. | Assessment of Motor and Process Skills (AMPS) used to validate CAVIR [30]. |
| User Experience & Usability Questionnaires | Quantifies participant acceptance, comfort, and perceived usability of the VR assessment system. | Higher ratings for VR vs. PC assessments on usability and experience metrics [42]. |
VR Assessment Workflow and Validation
The following diagram illustrates the typical workflow for developing and validating a VR-based neuropsychological assessment, leading to its key comparative advantages.
Interpretation of Key Findings
- Ecological Validity is a Key Advantage: The strong point of VR assessment is not necessarily replicating traditional test scores, but in its enhanced ecological validity. The CAVIR test's correlation with daily living skills, where traditional tests showed none, demonstrates VR's unique capacity to predict real-world functioning [30].
- Longer Reaction Times in VR are Informative: While VR reaction times are often slower, this likely reflects the increased cognitive load of more complex, lifelike tasks rather than poor test quality. These measures may be more representative of real-world performance [44].
- VR Mitigates Technological Bias: A significant finding is that performance on traditional PC tests was influenced by age and computing experience, whereas VR performance was largely independent of these factors. This suggests VR could offer a fairer assessment for populations with low digital literacy [42].
- Platform Selection is Goal-Dependent: For isolating specific cognitive processes in a controlled setting, traditional tests remain excellent. For predicting a patient's ability to function in daily life, VR assessments show distinct promise [30] [42].
This case study provides a comparative analysis of the Cognition Assessment in Virtual Reality (CAVIR) tool against traditional neuropsychological tests. With growing interest in ecologically valid cognitive assessments, immersive technologies like virtual reality (VR) offer promising alternatives to conventional paper-and-pencil methods. We examine experimental data from the CAVIR validation study, detailing its methodology, performance metrics, and comparative advantages in assessing functional cognitive domains relevant to primary care settings. The findings demonstrate CAVIR's enhanced sensitivity in evaluating daily-life cognitive skills and its stronger correlation with real-world functional outcomes, positioning it as a valuable tool for comprehensive cognitive assessment in mood and psychosis spectrum disorders.
The assessment of neurocognitive functions is pivotal for diagnosing and managing various psychiatric and neurological conditions. Traditional neuropsychological tests, while well-established, often face criticism for their limited ecological validity, as they may not adequately reflect cognitive challenges encountered in daily life [7]. The growing demand for more realistic assessment tools has catalyzed the exploration of immersive technologies, particularly within the broader research on VR and traditional neuropsychological test sensitivity [7].
Extended Reality (XR) technologies, encompassing virtual reality (VR), augmented reality (AR), and mixed reality (MR), have emerged as transformative tools. They create interactive, simulated environments that can closely mimic real-world scenarios, thereby offering a potentially more accurate measure of a person's functional cognitive abilities [41] [7]. A 2025 systematic review on XR for neurocognitive assessment identified 28 relevant studies, the majority of which (n=26) utilized VR-based tools, highlighting the academic and clinical interest in this domain [41] [7].
The CAVIR (Cognition Assessment in Virtual Reality) test represents a significant innovation in this field. It is designed as an immersive virtual kitchen scenario to assess daily-life cognitive skills in patients with mood or psychosis spectrum disorders [45]. This case study will objectively compare CAVIR's performance against traditional alternatives, presenting supporting experimental data within the context of primary care.
Methodology: CAVIR Experiment Protocol
Participant Recruitment and Characteristics
The validation study for the CAVIR test employed a case-control design to establish its sensitivity and validity [45].
- Sample Size: The study enrolled a total of 140 participants.
- Clinical Group: 70 symptomatically stable patients with diagnosed mood or psychosis spectrum disorders.
- Control Group: 70 healthy controls matched for relevant demographics.
- Key Inclusion/Exclusion: Patients were required to be symptomatically stable. A noted limitation was the presence of concomitant medication in the clinical group [45].
Assessment Tools and Procedures
Each participant underwent a multi-modal assessment battery to allow for comparative analysis between CAVIR, traditional tests, and functional outcomes.
- CAVIR Test: Participants completed the Cognition Assessment in Virtual Reality, which involves performing a series of tasks in an immersive virtual kitchen environment. The test is designed to evaluate cognitive skills as they would be applied in daily life [45].
- Traditional Neuropsychological Tests: A battery of standard neuropsychological tests was administered to all participants to establish convergent validity [45].
- Functional and Clinical Measures:
- Activities of Daily Living (ADL): The Assessment of Motor and Process Skills (AMPS) was used to objectively evaluate patients' ADL ability, specifically measuring the process skills required for task completion [45].
- Clinical Symptoms: Interviewer-rated scales were used to assess clinical symptom severity.
- Functional Capacity: Performance-based measures were used to evaluate functional capacity.
- Subjective Cognition: Participants' self-reported cognitive perceptions were recorded [45].
Data Analysis
Statistical analyses focused on establishing the validity and utility of the CAVIR test through several key methods [45]:
- Correlational Analysis: Spearman's correlation was used to examine the relationship between global CAVIR performance, global neuropsychological test scores, and ADL process ability.
- Group Comparisons: The sensitivity of CAVIR to cognitive impairments was tested by comparing performance between the patient and control groups.
- Covariate Adjustment: Key analyses, such as the association with ADL ability, were repeated after adjusting for sex and age to ensure robustness of findings.
Results and Comparative Performance Data
Correlation with Traditional Neuropsychological Tests
The CAVIR test demonstrated a statistically significant and moderate positive correlation with traditional neuropsychological test batteries.
Table 1: Correlation between CAVIR and Traditional Neuropsychological Tests
| Assessment Comparison | Correlation Coefficient (rs) | P-value | Sample Size (n) |
|---|---|---|---|
| Global CAVIR performance vs. Global neuropsychological test scores | 0.60 | < 0.001 | 138 |
This correlation of rs(138) = 0.60, p < 0.001 indicates that CAVIR performance shares a meaningful relationship with cognitive abilities measured by traditional tools, thereby supporting its construct validity [45]. However, the strength of the correlation also confirms that CAVIR captures distinct aspects of cognition not fully measured by traditional means.
Predictive Validity for Real-World Functioning
A key finding was CAVIR's superior ability to predict real-world functional outcomes compared to other assessment methods.
Table 2: Association with Activities of Daily Living (ADL) in Patients
| Assessment Method | Correlation with ADL Process Ability (r) | P-value | Statistical Significance after Adjusting for Sex & Age |
|---|---|---|---|
| CAVIR (Global Performance) | 0.40 | < 0.01 | Yes (p ≤ 0.03) |
| Traditional Neuropsychological Tests | Not Reported | ≥ 0.09 | Not Applicable |
| Interviewer-based Functional Capacity | Not Reported | ≥ 0.09 | Not Applicable |
| Subjective Cognition | Not Reported | ≥ 0.09 | Not Applicable |
The data reveal that CAVIR performance showed a weak-to-moderate significant association with ADL process skills (r(45) = 0.40, p < 0.01), which remained significant after controlling for sex and age. In stark contrast, traditional neuropsychological performance, interviewer-rated functional capacity, and subjective cognition measures showed no significant association with ADL ability (ps ≥ 0.09) [45]. This underscores CAVIR's enhanced ecological validity.
Sensitivity and Discriminative Validity
The CAVIR test proved highly effective in differentiating between patient and control groups, confirming its sensitivity to cognitive impairments associated with psychiatric disorders [45]. Furthermore, the test was able to differentiate between patients who were capable of regular employment and those who were not, highlighting its practical relevance for assessing functional outcomes like workforce participation [45].
Comparative Analysis: VR vs. Traditional Assessment
The findings from the CAVIR study align with broader research on VR's role in clinical assessment. The table below summarizes key comparative characteristics based on the current literature.
Table 3: Characteristics of VR-Based vs. Traditional Neurocognitive Assessment
| Characteristic | VR-Based Assessment (e.g., CAVIR) | Traditional Neuropsychological Tests |
|---|---|---|
| Ecological Validity | High - Mimics real-world environments (e.g., kitchen) [45] [7] | Low - Abstract, decontextualized paper-and-pencil tasks [7] |
| Sensitivity to ADL | Significant association with daily-life skills [45] | Often no significant association found [45] |
| Patient Engagement | High - Reported as more immersive and engaging [41] [7] | Variable - Can be repetitive and lack engagement [7] |
| Data Collection | Automated, objective metrics (response times, errors) [7] | Often relies on clinician timing and scoring [7] |
| Primary Advantage | Assesses "shows how" in realistic contexts; better predicts real-world function. | Standardized, extensive normative data; efficient for core cognitive domains. |
| Key Challenge | Cost, technical requirements, need for standardized protocols [41] [7] | Limited ecological validity and predictive power for daily function [45] [7] |
This comparison is supported by a separate systematic review which concluded that XR technologies are "more sensitive, ecologically valid, and engaging compared to traditional assessment tools" [41] [7].
The Researcher's Toolkit: Essential Components for VR Cognitive Assessment
Implementing a VR-based assessment like CAVIR requires a specific set of technological and methodological components.
Table 4: Research Reagent Solutions for VR Cognitive Assessment
| Item / Solution | Function / Description | Example from CAVIR Study |
|---|---|---|
| Immersive VR Hardware | Head-Mounted Display (HMD) and controllers to create a sense of presence and enable interaction. | A specific VR headset and controllers were used for the kitchen scenario [45]. |
| VR Assessment Software | The programmed environment and task logic defining the cognitive assessment scenario. | "Cognition Assessment in Virtual Reality (CAVIR)" software with a virtual kitchen [45]. |
| Traditional Test Battery | Standardized neuropsychological tests used for validation and correlation analysis. | A battery of standard tests was administered to all participants [45]. |
| Functional Outcome Measure | An objective tool to measure real-world performance, crucial for establishing ecological validity. | "Assessment of Motor and Process Skills (AMPS)" [45]. |
| Data Recording & Analysis Platform | Software to automatically record performance metrics (time, errors, paths) and analyze results. | Automated data collection is a key advantage of XR [7]. |
Discussion and Future Directions
The experimental data from the CAVIR study provides compelling evidence for the utility of VR-based assessments in primary care and specialist settings. The moderate correlation with traditional tests ensures that CAVIR measures established cognitive constructs, while its superior link to ADL performance demonstrates a critical advancement over existing tools [45]. This aligns with the broader thesis that VR assessments offer enhanced sensitivity to the cognitive challenges that impact patients' daily lives.
The feasibility of integrating VR into structured assessment protocols has been demonstrated not only in clinical psychology but also in medical education, where VR-based stations have been successfully incorporated into Objective Structured Clinical Examinations (OSCEs) [46]. However, challenges remain, including the initial high costs, need for technical support, and the current lack of standardized protocols across different VR assessment tools [41] [7]. Future research should focus on developing these standards, validating VR assessments in diverse patient populations and primary care settings, and further exploring their cost-effectiveness in long-term health management.
Novel VR Protocols for mTBI, Alzheimer's, and MCI Populations
Virtual Reality (VR) is emerging as a transformative tool in neurocognitive assessment, offering enhanced ecological validity and sensitivity for detecting mild cognitive impairment (MCI), Alzheimer's disease, and mild traumatic brain injury (mTBI). This guide compares the performance of novel VR-based protocols against traditional neuropsychological tests, synthesizing current experimental data to inform researchers and drug development professionals. Evidence indicates VR assessments demonstrate superior sensitivity in identifying subtle cognitive-motor integration deficits and functional impairments often missed by conventional paper-and-pencil tests, though results vary by clinical population and protocol design.
Traditional neuropsychological assessments like the Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA) have long been standard tools for detecting cognitive impairment. However, these paper-and-pencil tests lack ecological validity as they fail to replicate real-world situations where patients ultimately live and function [11]. Studies indicate these conventional tools explain only 5-21% of variance in patients' daily functioning, risking poor dementia prognosis [11]. The limitations of traditional assessments have accelerated the development of VR-based paradigms that create immersive, ecologically valid environments for detecting subtle neurological deficits.
VR technology offers several distinct advantages for neurocognitive assessment: (1) creation of controlled yet complex environments that mimic real-world challenges; (2) precise measurement of behavioral metrics including response latency, movement trajectory, and hesitation; (3) standardized administration across diverse populations and settings; and (4) enhanced patient engagement through immersive experiences [7]. These capabilities position VR as a powerful methodology for early detection of neurological conditions in both clinical and research settings.
Comparative Performance Data: VR vs. Traditional Assessments
Diagnostic Accuracy Across Conditions
Table 1: Diagnostic Performance of VR Assessments vs. Traditional Tools
| Condition | VR Assessment | Traditional Tool | Sensitivity | Specificity | AUC | Citation |
|---|---|---|---|---|---|---|
| MCI | VR Stroop Test | MoCA | 96.7% (hesitation latency) | 92.9% (hesitation latency) | 0.967 | [47] |
| MCI | VR Stroop Test | MoCA | 97.9% (3D trajectory) | 94.6% (3D trajectory) | 0.981 | [47] |
| MCI | Various VR tests | Paper-pencil tests | 89% (pooled) | 91% (pooled) | 0.95 | [48] |
| mTBI | Eye-Tracking/VR | Clinical criteria | Not significant | Not significant | N/A | [49] |
| mTBI | Virtual Tunnel Paradigm | BOT-2 balance test | Significant deficits detected | Not significant | N/A | [50] |
Correlation Between VR and Traditional Executive Function Measures
Table 2: Concurrent Validity of VR Assessments for Executive Function
| Cognitive Domain | VR Task Type | Traditional Correlation | Effect Size | Citation |
|---|---|---|---|---|
| Overall Executive Function | Multiple VR assessments | Significant correlation | Moderate | [19] |
| Cognitive Flexibility | VR adaptations (TMT-B) | Significant correlation | Moderate | [19] |
| Attention | VR continuous performance | Significant correlation | Moderate | [19] |
| Inhibition | VR Stroop-like tasks | Significant correlation | Moderate | [19] |
| Working Memory | VR vs. PC-based CBT | Significant correlation | Similar performance | [51] |
Detailed Experimental Protocols
VR Stroop Test for MCI Detection
The VR Stroop Test (VRST) was developed to detect executive dysfunction in MCI through an embodied cognitive-motor interaction paradigm [47]. The protocol simulates a real-life clothing-sorting task involving incongruent word-color stimuli that engages inhibitory control.
Methodology:
- Participants: 413 older adults (224 healthy controls, 189 with MCI)
- Apparatus: Unity-based application presented on 23-inch LCD monitor with HTC Vive Controller
- Task: Participants sort virtual clothing items (shirts, pants, socks) into semantically correct boxes while ignoring salient color distractors
- Trial Structure: 20 incongruent stimuli, three 2-minute trials with 30-second breaks
- Data Collection: 90Hz sampling rate of controller movement via Unity's XR Interaction Toolkit
- Primary Metrics:
- Task completion time
- 3D trajectory length of controller
- Hesitation latency
- Control Assessments: Korean MoCA, paper-based Stroop test, Corsi Block Test, Box and Block Test, Grooved Pegboard Test
This protocol's strength lies in its embodied cognition approach, requiring participants to physically interact with virtual objects while suppressing pre-potent responses, thereby engaging both cognitive and motor systems [47].
Eye-Tracking with VR for mTBI in Emergency Settings
This explorative, prospective, single-arm accuracy study evaluated the feasibility of VR-based eye-tracking for diagnosing mTBI in an emergency department setting [49].
Methodology:
- Participants: 82 patients presenting within 24 hours of head trauma
- Apparatus: EyeTrax VR glasses with Dual AMOLED 3.6 displays
- Oculomotor Assessment: Standardized sequence testing saccades, smooth pursuit, vergence, vestibulo-ocular reflex, anti-saccades, and pupil responses
- Design: Patients divided into mTBI and non-TBI subgroups by independent clinical experts blinded to VR results
- Analysis: 52 oculomotor parameters analyzed with statistical comparison to expert diagnosis
- Control: All patients received standard clinical workup including neuroimaging when indicated
Despite comprehensive assessment, this study found no statistically significant differences in oculomotor function between mTBI and control groups, highlighting the challenges of acute mTBI diagnosis in emergency settings [49].
Virtual Tunnel Paradigm for Pediatric mTBI
This protocol assessed long-lasting postural deficits in children with mTBI using dynamic visual stimulations in a controlled VR environment [50].
Methodology:
- Participants: 38 children with mTBI and 38 matched controls (ages 9-18)
- Apparatus: Fully immersive CAVE system (Fakespace)
- Stimulus: Virtual tunnel with checkerboard pattern moving in antero-posterior direction
- Conditions: Static (0Hz) and dynamic (0.125, 0.25, 0.5Hz) tunnel movements
- Metrics: Body sway amplitude (BSA) and postural instability (vRMS)
- Timeline: Assessments at 2 weeks, 3 months, and 12 months post-injury
- Control Measures: BOT-2, timed balance tasks, Post-Concussion Symptom Scale-Revised
The protocol successfully identified persistent postural deficits at 3 months post-injury that were not detected by standard clinical balance measures, demonstrating VR's enhanced sensitivity to subtle neurological impairments [50].
Visualization of VR Assessment Workflows
Cognitive-Motor Integration in VR Assessment
Neurocognitive Domains Assessed Through VR
Table 3: Research Reagent Solutions for VR Neurocognitive Assessment
| Tool/Resource | Function | Example Applications | Technical Specifications |
|---|---|---|---|
| EyeTrax VR Glasses | Eye-tracking integrated with VR | Oculomotor assessment in mTBI | Dual AMOLED 3.6 displays, pupil tracking [49] |
| HTC Vive Controller | 3D motion tracking | VR Stroop test, movement trajectory | 90Hz sampling, 6 degrees of freedom [47] |
| Unity XR Interaction Toolkit | VR development framework | Task implementation, data collection | Cross-platform XR support, input system [47] |
| CAVE System | Fully immersive VR environment | Virtual tunnel paradigm for postural control | Projector-based, room-scale tracking [50] |
| VRST Protocol | Standardized inhibitory control task | MCI detection through embodied cognition | 20 incongruent stimuli, 3 trials [47] |
| Virtual Tunnel Paradigm | Dynamic visual stimulation | Postural assessment in pediatric mTBI | Sinusoidal translation (0.125-0.5Hz) [50] |
VR-based neurocognitive assessments demonstrate significant advantages over traditional methods, particularly for detecting subtle deficits in MCI through embodied cognitive-motor tasks. The high diagnostic accuracy (AUC 0.95-0.98) of protocols like the VR Stroop Test highlights VR's potential for early detection of cognitive decline [47] [48]. However, applications for acute mTBI diagnosis show more variable results, with some protocols failing to distinguish patients from controls in emergency settings [49], while others successfully identify persistent postural deficits missed by standard clinical tests [50].
Future research directions should address current limitations, including: (1) standardization of VR protocols across sites; (2) validation in diverse populations; (3) development of normative databases; and (4) longitudinal assessment of cognitive change. For drug development professionals, VR assessments offer sensitive endpoints for clinical trials, particularly for detecting early treatment effects on functional cognition. As the field evolves, VR technologies are poised to transform neurocognitive assessment paradigms from symptom-based inventories to precise measurements of real-world functional abilities.
Navigating the Virtual Frontier: Overcoming Technical and Clinical Hurdles
Mitigating Cybersickness and Enhancing User Experience for Elderly Populations
Extended reality (XR) technologies, particularly fully immersive virtual reality (VR), are transforming neurocognitive assessment by providing interactive environments that transcend the limitations of traditional paper-and-pencil tests [41]. These technologies offer enhanced ecological validity, allowing researchers to create controlled yet realistic assessment scenarios that more closely mimic real-world cognitive demands [51] [41]. For elderly populations, VR presents both unique opportunities for engaging cognitive assessment and challenges related to cybersickness and technology acceptance that must be systematically addressed [52].
The sensory conflict theory provides the predominant framework for understanding cybersickness, which arises from discrepancies between expected and actual sensory input across visual, vestibular, and proprioceptive modalities [53]. While VR sickness shares symptom domains with traditional simulator sickness, disorientation symptoms such as dizziness and vertigo are typically more prominent in VR environments [53]. This review examines comparative evidence between VR and traditional assessment modalities, with specific focus on mitigating cybersickness and enhancing usability for elderly populations.
Comparative Analysis: VR vs. Traditional Neuropsychological Assessment
Performance Characteristics Across Assessment Modalities
Table 1: Comparison of VR and traditional neuropsychological assessment performance
| Assessment Metric | VR-Based Assessment | Traditional Computerized | Traditional Paper-Based | Key Findings |
|---|---|---|---|---|
| Working Memory (Digit Span) | Comparable performance | Comparable performance | Not tested | No significant difference between VR and PC formats [51] |
| Visuospatial Memory (Corsi Block) | Lower scores | Higher scores | Not tested | PC enabled better performance than VR [51] |
| Psychomotor Speed | Slower reaction times | Faster reaction times | Not tested | Significant advantage for PC-based assessments [51] |
| Discriminatory Power (AUC) | Superior (eMMSE: 0.82) | Not applicable | Inferior (MMSE: 0.65) | Digital tests showed better diagnostic accuracy [54] |
| Cultural/Literacy Bias | Minimal influence | Significant influence | Significant influence | VR performance largely independent of computing experience [51] |
| User Experience Ratings | Higher ratings | Lower ratings | Not applicable | VR received superior usability scores [51] |
Table 2: Cybersickness prevalence and mitigation in elderly populations
| Factor | Impact on Cybersickness | Age-Related Considerations | Empirical Evidence |
|---|---|---|---|
| Visual-Vestibular Conflict | Primary cause of nausea/disorientation | Older adults may have pre-existing vestibular issues | Deliberately removing optic flow minimized sickness [53] |
| Sensorimotor Mismatch | Minimal impact when isolated | Older adults showed high tolerance | No significant sickness increase with proprioceptive mismatches [53] |
| Age Susceptibility | Counterintuitive age effect | Older adults reported weaker symptoms | Younger participants had worse SSQ scores [53] |
| Cognitive Load | Secondary contributor | Higher exhaustion/frustration in mismatch conditions | Mismatch group reported more exhaustion despite similar SSQ [53] |
| Interaction Design | Critical mitigation factor | Simplified controls reduce disorientation | Self-paced interactions and intuitive interfaces recommended [52] |
Experimental Protocols and Methodologies
Protocol 1: Sensorimotor Mismatch and Cybersickness (2025)
- Participants: 104 healthy right-handed adults (19-84 years, mean 50.0±21.7)
- VR System: Oculus Rift S HMD (1280×1440 per eye, 80Hz refresh rate)
- Task: Seated ball-throwing with deliberately induced proprioceptive mismatches
- Design: Randomized controlled trial with three intervention groups (Mismatch, Error-based, Errorless)
- Measures: Simulator Sickness Questionnaire (SSQ), custom user experience questionnaire
- Key Finding: No significant differences in SSQ scores among groups despite sensorimotor mismatches [53]
Protocol 2: Comparative Validity of VR Assessment (2025)
- Participants: 66 adults performing cognitive tasks in both VR and PC formats
- Tasks: Digit Span Task (DST), Corsi Block Task (CBT), Deary-Liewald Reaction Time Task (DLRTT)
- Design: Within-subjects crossover with counterbalanced conditions
- Analysis: Convergent validity, regression analyses for demographic influences
- Key Finding: VR assessments showed minimal reliance on prior IT experience compared to PC versions [51]
Protocol 3: Digital Cognitive Screening Validation (2025)
- Participants: 47 community-dwelling older adults (65+ years)
- Design: Randomized crossover comparing paper-based and digital MMSE/CDT
- Measures: Correlation coefficients, AUC analysis, usability questionnaires
- Key Finding: Electronic MMSE showed superior discriminatory power (AUC=0.82) versus paper-based MMSE (AUC=0.65) [54]
Technical and Design Considerations for Elderly Populations
Research Reagent Solutions for VR Implementation
Table 3: Essential materials and their functions in VR research with elderly populations
| Research Tool | Function/Specification | Application in Elderly Research |
|---|---|---|
| Oculus Rift S HMD | 1280×1440 pixels per eye, 80Hz refresh rate, inside-out tracking with 5 cameras | Motor task research with seated participants to minimize vestibular conflict [53] |
| Meta Quest 2 HMD | Standalone VR headset with hand-tracking capability | Road-crossing training applications ("Wegfest") with natural interactions [55] |
| Simulator Sickness Questionnaire (SSQ) | 16-item measure of nausea, oculomotor, disorientation symptoms | Primary outcome measure for cybersickness in controlled trials [53] |
| System Usability Scale (SUS) | 10-item scale measuring perceived usability | Comparative usability assessment between digital and traditional formats [56] |
| Usefulness, Satisfaction, Ease of Use (USE) | Multidimensional usability questionnaire | Evaluating practicality of digital cognitive screening in primary care [54] |
| Unity Engine with C# | Development environment for custom VR applications | Creating tailored scenarios for specific research questions [53] [55] |
Visualizing Cybersickness Mitigation Pathways
Diagram 1: Cybersickness pathways and mitigation strategies for elderly populations. Note the paradoxical finding that older age may reduce sickness susceptibility despite increased need for structured training.
Elderly-Friendly VR Design Framework
Diagram 2: Comprehensive design framework for elderly-friendly VR systems showing the relationship between design principles, implementation strategies, and target outcomes.
Discussion and Research Implications
Cybersickness Paradox in Elderly Populations
Contrary to conventional assumptions, recent evidence indicates that older adults may experience less severe cybersickness than younger users in controlled VR environments [53]. This paradoxical finding emerged from a randomized controlled trial where younger participants reported significantly worse simulator sickness questionnaire (SSQ) scores despite identical exposure conditions [53]. The critical design factor appears to be the elimination of visual-vestibular conflict through seated tasks without optic flow, suggesting that targeted design interventions can effectively mitigate the primary driver of cybersickness regardless of age.
However, older adults reported higher levels of exhaustion and frustration in sensorimotor mismatch conditions, indicating that cognitive load and task difficulty remain significant considerations for this demographic [53]. This dissociation between traditional cybersickness symptoms and cognitive strain highlights the need for multidimensional assessment approaches that capture both physical discomfort and cognitive fatigue in elderly VR users.
Ecological Validity and Diagnostic Sensitivity
VR-based neurocognitive assessments demonstrate superior ecological validity compared to traditional computerized tests, creating environments that more closely mimic real-world cognitive demands [41]. This enhanced realism comes with methodological advantages, including reduced cultural and educational bias in assessment outcomes [51]. While traditional computerized test performance strongly correlates with prior computing experience and gaming familiarity, VR assessment performance remains largely independent of these factors [51], potentially offering more equitable assessment across diverse demographic groups.
The diagnostic sensitivity of VR-based assessments shows particular promise. In direct comparisons, electronic MMSE implementations demonstrated substantially better discriminatory power (AUC=0.82) than paper-based versions (AUC=0.65) for detecting mild cognitive impairment [54]. This enhanced sensitivity, combined with automated scoring and standardized administration, positions VR assessment as a valuable intermediary between brief cognitive screeners and comprehensive neuropsychological evaluations [57].
Implementation Challenges and Future Directions
Despite promising results, VR implementation in elderly populations faces significant practical challenges. Technical complexity, cost considerations, and the need for specialized support remain barriers to widespread adoption [41]. Additionally, while older adults show positive attitudes toward VR after initial exposure [58], pre-existing anxiety about technology and limited digital literacy can impede initial acceptance [52] [58].
Future research should prioritize the development of standardized VR assessment batteries with established psychometric properties for elderly populations. Longitudinal studies examining both the cognitive benefits and potential side effects of repeated VR exposure are needed to establish safety guidelines. Additionally, more sophisticated adaptive algorithms that automatically adjust task difficulty and sensory stimulation based on real-time performance and comfort metrics could further enhance the accessibility and effectiveness of VR-based assessment and intervention for older adults.
Virtual reality represents a transformative approach to neuropsychological assessment that offers substantial advantages in ecological validity, diagnostic sensitivity, and reduced demographic bias compared to traditional methods. For elderly populations, targeted design interventions—particularly the elimination of visual-vestibular conflict through seated tasks, simplified control schemes, and structured training protocols—can effectively mitigate cybersickness while maintaining engagement. The paradoxical finding of reduced cybersickness susceptibility in older adults under controlled conditions challenges conventional assumptions and highlights the potential of well-designed VR systems for geriatric neuropsychology. As technical accessibility improves and evidence bases expand, VR methodologies are poised to bridge critical gaps between brief cognitive screening and comprehensive neuropsychological assessment, ultimately enhancing early detection and intervention for age-related cognitive decline.
Multi-center clinical trials are essential for recruiting diverse patient populations and generating robust, generalizable results. However, their complexity introduces significant challenges in maintaining standardization and ensuring scalable operations. Modern trials increasingly depend on technological solutions and standardized methodologies to overcome these hurdles, particularly in specialized fields like neuropsychological assessment where measurement consistency across sites is critical for data validity. The growing integration of innovative technologies, including extended reality (XR) platforms and electronic data capture systems, represents a transformative shift in how researchers address these persistent challenges [59] [60].
This guide examines the core operational and methodological challenges in multi-center trials, with a specific focus on comparing traditional and virtual reality-based neuropsychological assessments. We provide an objective analysis of technological solutions and their efficacy data to inform researchers, scientists, and drug development professionals in optimizing trial design and implementation.
Operational and Methodological Hurdles in Multi-Center Research
Core Operational Challenges
Managing multi-center clinical trials presents four common operational challenges that directly impact data quality and trial efficiency:
- Lack of Workflow Standardization: Different sites often implement unique processes and document management practices, making it difficult to locate critical documents and maintain consistent procedures across locations [59].
- Limited Visibility and Collaboration: Regulatory agencies require coordinating centers to maintain oversight of all participating sites, but stretched resources often leave staff struggling to maintain visibility into site performance and study status [59].
- Coordinator Turnover: High staff turnover rates combined with increasing trial workloads create knowledge gaps and consistency challenges, potentially compromising data integrity and requiring repeated training [59].
- Site Training and Support Needs: Implementing standardized workflows requires comprehensive training and ongoing support, which demands significant resources from coordinating centers [59].
Data Management Inefficiencies
In oncology trials specifically, manual data handling processes consume substantial time and resources. Research staff must manually extract, transcribe, and validate clinical data from electronic health records (EHRs) into electronic data capture (EDC) systems [60]. Quantitative analyses reveal that:
- More than 50% of clinical trial data is duplicated between research systems and hospital EHRs
- Approximately 20% of total study costs are typically allocated to data duplication and verification
- Study personnel spend at least three minutes per data point in Phase II-III oncology trials, with complex entries requiring five to ten minutes [60]
For a study with 10 patients contributing 10,000 data points each, the cumulative workload reaches 5,000 hours, creating significant scalability challenges for larger trials [60].
Table 1: Time and Cost Implications of Manual Data Management in Oncology Trials
| Trial Scale | Data Points per Patient | Estimated Manual Effort | Estimated Transcription Cost |
|---|---|---|---|
| Small (10 patients) | 10,000 | 5,000 hours | $300,000-$500,000 |
| Phase III (200 patients) | 10,000 | 100,000 hours | $6,000,000-$10,000,000 |
Technological Solutions for Standardization and Scalability
Centralized Platform Solutions
Centralized digital platforms address standardization challenges by deploying predefined workflows and document structures across all research sites. These systems provide:
- Standardized Site File Structures: Predefined document structures and naming conventions deployed at trial start enable quick location of critical documents across all sites [59].
- Real-time Oversight Capabilities: Consolidated dashboards and reports give coordinating centers visibility into site progress and study status without micromanaging [59].
- Automated Compliance Tracking: Built-in audit trails and "always-on" compliance monitoring ensure adherence to 21 CFR Part 11 and other regulatory requirements [59].
Early adopters of integrated eSource technology, including Memorial Sloan Kettering, Mayo Clinic, and MD Anderson Cancer Center, have reported significant improvements in trial efficiency, with some achieving approximately 50% reduction in site burden and data entry times [60].
Interoperability and Data Standardization
A primary technical challenge in scaling digital solutions is interoperability between hospital EHRs and research ECD systems. Successful implementation requires:
- Structured Data Frameworks: Adoption of standards like FHIR, HL7, SNOMED CT, and LOINC to enable automated EHR-to-EDC data transfers [60].
- Data Dictionary Mapping: Early mapping of data dictionaries to ensure reliable extraction and standardization across systems [60].
- Unstructured Data Processing: AI-powered automation to process unstructured data, such as physician notes, imaging, and pathology reports [60].
At UK Essen, the challenge is magnified by nearly 500 source systems requiring continuous updates and fine-tuning to map to FHIR repositories [60].
Neuropsychological Assessment in Multi-Center Trials: Traditional vs. VR Approaches
Diagnostic Criteria and Prognostic Value
Neuropsychological assessment in multi-center trials requires careful standardization of diagnostic criteria. Research comparing Conventional (Petersen/Winblad) and Neuropsychological (Jak/Bondi) criteria for Mild Cognitive Impairment (MCI) reveals important considerations:
- Baseline Prognostic Value: Across a 12-year study period, both Conventional and Neuropsychological criteria showed comparable ability to predict progression to dementia [61].
- Diagnostic Stability: The Neuropsychological criteria demonstrated superior diagnostic consistency (63.2% vs. 43.2%) compared to Conventional criteria [61].
- Methodological Differences: Conventional criteria require subjective cognitive complaints and objective impairment (≥1.5 SD below normative mean on one test), while Neuropsychological criteria require objective impairment only (≥1.0 SD below normative mean on two tests within the same domain) [61].
Table 2: Comparison of MCI Diagnostic Criteria Performance Over 12 Years
| Performance Metric | Conventional Criteria | Neuropsychological Criteria |
|---|---|---|
| Sensitivity for Dementia | 35.9% | 66.2% |
| Specificity for Dementia | 84.7% | 60.3% |
| Positive Predictive Value | 30.1% | 23.4% |
| Negative Predictive Value | 87.8% | 90.7% |
| Diagnostic Consistency | 43.2% | 63.2% |
Extended Reality (XR) Assessment Platforms
Extended reality technologies, particularly virtual reality (VR), offer innovative approaches to neurocognitive assessment in multi-center trials. A systematic review of 28 studies reveals:
- Domain Coverage: VR-based tools effectively assess multiple cognitive domains including memory, attention, and executive function through immersive environments [41] [7].
- Comparative Advantages: XR technologies demonstrate enhanced ecological validity, patient engagement, and diagnostic sensitivity compared to traditional assessment tools [7].
- Implementation Gaps: Among the reviewed studies, VR dominated (n=26) with limited augmented reality (AR) application (n=2) and no mixed reality (MR) utilization for neurocognitive assessment [41] [7].
Methodological Standardization Challenges
Both traditional and VR-based assessments face standardization challenges in multi-center implementations:
- Traditional Test Limitations: Conventional assessments like the Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), and Clock Drawing Test (CDT) show susceptibility to educational and cultural biases, and rely heavily on clinician interpretation [7].
- XR Technical Barriers: VR assessment platforms face challenges including high costs, lack of standardized protocols, and technical issues such as motion sickness [7].
- Remote Administration: XR technologies enable remote assessments, potentially increasing accessibility while maintaining standardized administration across sites [7].
Experimental Protocols and Methodologies
Implementation Framework for eSource Technology
A qualitative study across six oncology research centers established a structured methodology for implementing eSource technology [60]:
- Pre-Implementation Mapping: Comprehensive mapping of data dictionaries to EHR structures before trial initiation
- Staged Deployment: Phased implementation beginning with structured data transfer (laboratory values, vital signs)
- AI Integration: Incorporation of artificial intelligence for processing unstructured data elements
- Continuous Validation: Ongoing data quality checks and system validation throughout the trial lifecycle
This methodology reduced transcription errors and decreased data transcription times from 15 minutes to under two minutes per subject at implementing centers [60].
Validation Study for VR Neurocognitive Assessment
A systematic review of XR technologies established rigorous methodology for evaluating neurocognitive assessment tools [7]:
Diagram 1: VR Assessment Validation Methodology
Multi-Center Neuropsychological Criteria Comparison
A 12-year population-based study directly compared diagnostic criteria for MCI using comprehensive methodology [61]:
- Study Population: 1,021 older adults without dementia (70-74 years at baseline)
- Assessment Intervals: Periodic multidimensional assessments across 12 years
- Diagnostic Frameworks: Concurrent application of Conventional (Petersen/Winblad) and Neuropsychological (Jak/Bondi) criteria
- Outcome Measures: Progression to dementia, diagnostic stability, consistency of classification
This longitudinal design enabled direct comparison of how each diagnostic framework performed in predicting clinical outcomes and maintaining diagnostic consistency over time [61].
Comparative Efficacy Data: Traditional vs. Technological Approaches
Efficiency Metrics for Technological Solutions
Implementation data from early adopters of technological solutions provides quantitative evidence of their impact on trial efficiency:
- eSource Implementation: Automated EHR-to-EDC data transfer reduced transcription errors entirely and decreased data transcription times from 15 minutes to under two minutes per subject [60].
- Centralized Platform Deployment: Reduced individual site start-up time by as much as 50% through standardized workflows and document templates [59].
- Cost Implications: eSource adoption results in approximately $15,000 cost savings per patient by reducing manual data entry and associated verification processes [60].
Performance Metrics for Assessment Methodologies
Table 3: Comparison of Neuropsychological Assessment Methodologies
| Assessment Characteristic | Traditional Paper-Pencil | VR-Based Assessment |
|---|---|---|
| Ecological Validity | Limited | Enhanced through real-world simulation |
| Standardization Across Sites | Variable, depends on administrator training | High, with automated administration |
| Data Collection Capabilities | Manual scoring and interpretation | Automated performance metrics |
| Cultural/Ethical Bias | Moderate to high susceptibility | Potentially reduced through customizable scenarios |
| Administrative Burden | High, requires trained staff | Reduced after initial setup |
| Remote Administration Capability | Limited with traditional telemedicine | Fully supported |
| Equipment Costs | Low | High initial investment |
The Researcher's Toolkit: Essential Solutions for Multi-Center Trials
Technological Infrastructure
Table 4: Essential Research Reagent Solutions for Multi-Center Trials
| Solution Category | Representative Examples | Primary Function |
|---|---|---|
| Centralized Management Platforms | Florence eBinders | Standardize document workflows and provide oversight across sites |
| Electronic Data Capture | TRIALPAL ePRO/eDiary | Capture patient-reported outcomes and clinical data electronically |
| eSource Integration | EHR2EDC automated transfer | Eliminate redundant data entry between EHR and EDC systems |
| Data Visualization Tools | Maraca plots, Tendril plots | Communicate complex trial results through intuitive visualizations |
| Extended Reality Assessment | VR neurocognitive batteries | Administer ecologically valid cognitive assessments in standardized environments |
Methodological Frameworks
Successful multi-center trials require both technological tools and methodological standards:
- Structured Diagnostic Criteria: Neuropsychological criteria requiring two impaired test scores within the same cognitive domain improve diagnostic consistency compared to conventional approaches [61].
- Standardized Data Protocols: Implementation of FHIR, HL7, SNOMED CT, and LOINC standards enables interoperability between hospital systems and research platforms [60].
- Validation Methodologies: Systematic approaches to validating novel assessment technologies, including comparison with traditional measures and longitudinal outcome tracking [7] [62].
Addressing standardization and scalability challenges in multi-center clinical trials requires integrated technological and methodological solutions. Evidence indicates that centralized management platforms, eSource integration, and standardized assessment protocols significantly improve efficiency and data quality across research sites. For neuropsychological assessment specifically, VR-based approaches offer enhanced ecological validity and standardization potential, though they require further validation and cost reduction for widespread implementation.
The comparative data presented in this guide demonstrates that while technological solutions require substantial initial investment, they offer significant long-term benefits for trial scalability, data integrity, and operational efficiency. Researchers should prioritize interoperability, staff training, and methodological rigor when implementing these solutions to maximize their impact on multi-center trial success.
The table below summarizes key quantitative findings from recent studies comparing Virtual Reality (VR) and traditional neuropsychological assessments, with a specific focus on the influence of users' digital literacy and technological experience.
Table 1: Comparative Performance of VR and Traditional Neuropsychological Assessments
| Performance Metric | VR-Based Assessment | Traditional PC-Based Assessment |
|---|---|---|
| Influence of Computing Experience | Minimal to no significant influence on performance [51] | Significant influence on performance; predicts outcomes [51] |
| Influence of Gaming Experience | Limited impact (only noted in complex tasks like backward recall) [51] | Significant influence across multiple tasks [51] |
| User Experience & Usability | Higher ratings for engagement and usability [51] | Lower ratings compared to VR [51] |
| Ecological Validity | High; effectively captures real-world cognitive challenges [4] [63] | Limited; poor correlation with real-world functional performance [4] [63] |
| Sensitivity & Discriminative Ability | High; AUC of 0.88 for distinguishing cognitive status [4] | Moderate; reliant on veridicality-based methodology [4] |
| Test Reliability | High; Intraclass Correlation Coefficient of 0.89 for test-retest [4] | Varies; well-established but can be influenced by administrator [57] |
Traditional neuropsychological assessments, while reliable, face significant limitations concerning ecological validity—the ability to predict real-world functioning [4] [63]. A critical, often underexplored limitation is their susceptibility to technological bias. Performance on traditional computerized tests can be influenced by an individual's familiarity with computers, mice, and interfaces, creating a confounding variable that is independent of the cognitive construct being measured [51] [64].
Immersive Virtual Reality (VR) presents a paradigm shift. By leveraging intuitive, gesture-based interactions in spatially coherent environments, VR assessments demonstrate a remarkable independence from prior digital literacy, promising a more equitable and accurate platform for cognitive assessment [51]. This guide objectively compares the experimental data supporting VR's reduced technological bias against traditional methods.
Experimental Data and Protocols
Direct Comparison of VR vs. PC-Based Cognitive Tasks
A foundational 2025 study by Kourtesis et al. provides direct, head-to-head experimental data on the influence of technological experience [51].
- Experimental Protocol: Sixty-six participants performed established cognitive tasks—the Digit Span Task (DST), Corsi Block Task (CBT), and Deary-Liewald Reaction Time Task (DLRTT)—in both VR-based and PC-based formats. Researchers quantitatively assessed participants' experience with computers, smartphones, and video games.
- Key Findings: While the two modalities showed significant correlations, supporting convergent validity, a critical difference emerged in regression analyses. Performance on PC versions was directly influenced by computing and gaming experience. In contrast, performance on VR versions was largely independent of these factors, with gaming experience being a predictor only for the most complex task (CBT backward recall) [51].
- Interpretation: This suggests that VR's naturalistic interaction paradigm reduces the cognitive load and skill required to operate the interface itself, thereby isolating the measurement to the target cognitive domain.
Validation of a Comprehensive VR Assessment Tool
Research on the "Cognitive Assessment using VIrtual REality" (CAVIRE-2) system in a primary care setting further underscores VR's clinical utility, which is built upon its accessibility [4].
- Experimental Protocol: The study involved 280 multi-ethnic Asian adults aged 55-84. Participants completed both the CAVIRE-2 assessment, which comprises 13 scenarios simulating daily living, and the traditional Montreal Cognitive Assessment (MoCA).
- Key Findings: CAVIRE-2 demonstrated high discriminative ability (Area Under the Curve = 0.88) in distinguishing cognitively healthy individuals from those with impairment, showing strong agreement with the MoCA [4]. The system's design, modeled after local residential and community settings, creates an intuitive environment that does not feel like a complex computer test, thereby mitigating barriers related to digital unfamiliarity [4].
Enhanced Ecological Validity in Specific Populations
Studies on specific clinical groups, such as adults with Attention-Deficit/Hyperactivity Disorder (ADHD), highlight how VR's reduced bias translates to more valid assessments.
- Experimental Protocol: Fifty-three adults, including 25 with ADHD, completed both the traditional Trail Making Test (TMT) and a VR-adapted version (TMT-VR) [63].
- Key Findings: The TMT-VR showed strong correlations with the traditional test and higher ecological validity. Notably, the ADHD group exhibited greater performance differences in the VR environment, suggesting VR more effectively captures the real-world cognitive challenges they face [63]. The study also found that user-friendly interaction modes like eye-tracking were highly accurate even for non-gamers, emphasizing VR's applicability across diverse technological proficiencies [63].
Methodology: How VR Minimizes Technological Bias
The experimental superiority of VR in mitigating digital literacy bias stems from core methodological differences in its design and interaction logic.
Workflow Comparison: Traditional Digital vs. VR Assessment
The diagram below contrasts the underlying processes of traditional computerized tests and VR assessments, highlighting points where digital literacy introduces bias.
Key Technical Factors Reducing Bias
- Intuitive Interaction Modalities: VR systems use head movement, eye-tracking, and simple hand gestures to interact with virtual objects. These modalities leverage innate human motor skills, unlike the learned skill of using a computer mouse [63].
- Sensory Immersion and Presence: The immersive nature of a VR Head-Mounted Display (HMD) creates a strong sense of presence, or "being there" [65]. This promotes cognitive immersion in the task itself, shifting focus away from the "interface" and toward the activity, similar to real-world scenarios [65].
- Verisimilitude Approach to Design: VR assessments are designed with verisimilitude, meaning the cognitive demands of the tasks closely mirror those encountered in naturalistic environments [4]. For example, the CAVIRE-2 system uses scenarios set in familiar local residential and community settings, making the tasks intuitively understandable regardless of technical background [4].
The Scientist's Toolkit: Essential Research Reagents for VR Cognitive Assessment
For research teams aiming to develop or validate VR cognitive assessments, the following components are critical.
Table 2: Key Research Reagents for VR Cognitive Assessment
| Tool / Component | Function & Research Purpose | Examples from Literature |
|---|---|---|
| Immersive HMD | Presents 3D virtual environments; critical for inducing sensory immersion and presence. | Systems like the Oculus Rift/Meta Quest used in multiple studies [51] [4] [63]. |
| Interaction Controllers / Hand Tracking | Enables user interaction with the virtual environment (e.g., grabbing, pointing). | Motion controllers for tasks like the VR Corsi Block [51]. |
| Eye-Tracking Module | Provides high-accuracy input for assessments; found superior for non-gamers in TMT-VR study [63]. | Integrated eye-tracking in HMDs for tasks like the Trail Making Test-VR [63]. |
| VR Assessment Software | The core experimental protocol defining tasks, environments, and data collection. | CAVIRE-2 software with 13 daily-living scenarios [4]; Custom VR jigsaw puzzles [65]. |
| Data Logging Framework | Captures objective, high-density performance metrics beyond simple accuracy. | Logs of completion time, path efficiency, error type, dwell time, and kinematic data [51] [33]. |
| Biometric Sensors | Provides objective physiological data to complement behavioral metrics and measure states like immersion. | EEG to identify biomarkers of cognitive immersion [65]. |
The consolidated experimental evidence confirms that VR neurocognitive assessments offer a significant advantage over traditional digital methods by drastically reducing bias associated with digital literacy. The key differentiator is VR's capacity to leverage innate human sensorimotor skills for interaction, thereby isolating the measurement of cognitive function from prior technological experience.
For researchers and drug development professionals, this translates to:
- Cleaner Data: Reduced noise from confounding variables in clinical trials and studies [51] [33].
- Greater Accessibility: More equitable participant recruitment and assessment across diverse demographic and socioeconomic groups [51].
- Enhanced Predictive Power: Improved ecological validity means VR assessment data are more likely to correlate with real-world functional outcomes, a critical endpoint in therapeutic development [4] [63].
Future research will focus on standardizing these VR tools across larger populations, further validating their predictive power for real-world functioning, and integrating multimodal biometrics like EEG to objectively quantify cognitive states during assessment [65]. The ongoing maturation of VR technology solidifies its role as a more equitable and precise instrument in the future of neuropsychological research and clinical trial endpoints.
Cost-Benefit Analysis and Implementation Strategies for Clinical Settings
This guide provides an objective comparison between Virtual Reality (VR)-based assessments and traditional neuropsychological tests, focusing on their sensitivity, cost-benefit profiles, and implementation practicality for clinical settings. VR demonstrates superior diagnostic accuracy for conditions like Mild Cognitive Impairment (MCI), with sensitivity reaching 0.944 and specificity of 0.964 in controlled studies, significantly outperforming established tools like the Montreal Cognitive Assessment (MoCA) [66]. While VR requires a higher initial investment, its cost-effectiveness becomes apparent over time due to automation and reusability, with studies showing it becomes less expensive than live drills when extrapolated over three years [67]. Key implementation strategies include selecting systems with strong ecological validity, planning for phased rollout to manage upfront costs, and ensuring staff training for seamless integration into existing clinical workflows.
Comparative Performance Analysis
Diagnostic Sensitivity and Specificity
VR-based spatial memory tests show significantly better performance in discriminating MCI from healthy aging compared to traditional paper-and-pencil tests.
Table 1: Comparison of Diagnostic Accuracy between VR and Traditional Tests
| Assessment Tool | Sensitivity | Specificity | Cognitive Domains Assessed | Key Findings |
|---|---|---|---|---|
| VR Spatial Memory Test (SCT-VR) | 0.944 [66] | 0.964 [66] | Spatial memory, navigation, hippocampal function | Better discriminates MCI from healthy controls than MoCA-K [66]. |
| Montreal Cognitive Assessment (MoCA-K) | 0.857 [66] | 0.746 [66] | Global cognitive function, visuospatial/executive, memory, attention | Lower sensitivity and specificity for MCI compared to SCT-VR [66]. |
| Traditional Neuropsychological Battery | Variable; often low for MCI [68] | Variable [68] | Intelligence, attention, memory, language, executive function | Can lack ecological validity; may not predict real-world function well [69]. |
Ecological Validity and Real-World Predictiveness
A primary advantage of VR assessment is its enhanced ecological validity, meaning it better approximates real-world cognitive challenges.
- Verisimilitude: VR environments mimic the complexity of daily activities, requiring multi-step processing and integration of sensory information that is missing from traditional tests [69]. For example, navigating a virtual city to recall a route assesses memory in a context more representative of real-life challenges than recalling a word list [70].
- Veridicality: Performance on VR tasks has shown a stronger correlation with actual everyday functioning. Studies have demonstrated that patient performance in virtual environments is a more robust indicator of their future performance on daily tasks than scores on traditional neuropsychological assessments [70].
Traditional tests like the Wisconsin Card Sorting Test (WCST) or the Stroop test were developed to measure specific cognitive constructs but were not designed to predict how a patient functions in daily life, creating a gap between test results and real-world capability [69].
Experimental Data and Protocols
Key VR Experiment in MCI Detection
Objective: To investigate whether a VR-based spatial memory task has higher predictive power for MCI than the MoCA-K [66].
Population: 36 older adults with amnestic MCI and 56 healthy controls [66].
Protocol:
- SCT-VR Task: Participants used a joystick to navigate an open arena virtual environment with boundary cues (e.g., an ocean, rocks). They were instructed to move toward a gem and then, after reaching it, to return to their original starting location from memory. This was repeated over 10 sessions [66].
- Outcome Measure: The primary metric was the Euclidean distance between the actual and the participant-estimated starting location. A shorter distance indicated better spatial memory [66].
- Comparison: All participants also completed the MoCA-K and the Wechsler Adult Intelligence Scale-Revised Block Design Test (WAIS-BDT) [66].
Workflow Diagram:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials for VR-Based Neuropsychological Research
| Item | Function in Research | Example in SCT-VR Protocol [66] |
|---|---|---|
| VR Development Platform | Software engine to create and run controlled virtual environments. | Unity game engine. |
| Immersive Display System | Head-Mounted Display (HMD) to provide a 360-degree, immersive experience. | Oculus Rift HMD [67] or similar. |
| Navigation Interface | Device allowing users to interact and move within the virtual environment. | Joystick. |
| Spatial Memory Task | A standardized protocol designed to assess hippocampal-dependent navigation and recall. | Hidden goal task (e.g., returning to start location in an open arena). |
| Data Logging System | Software component that automatically records behavioral performance metrics. | Automated logging of Euclidean distance (error in meters). |
| Traditional Neuropsychological Battery | Gold-standard assessments for benchmarking and establishing concurrent validity. | MoCA, WAIS-BDT, or other standardized tests. |
Cost-Benefit and Implementation Analysis
Economic Evaluation
The financial implications of implementing VR involve significant upfront costs but offer potential long-term savings and enhanced value.
- Initial Investment vs. Long-Term Value: A cost analysis of VR training for disaster preparedness found a higher initial cost per participant for VR ($327.78) compared to a live drill ($229.79). However, because VR development costs can be spread across many trainees and repeated uses over multiple years, it becomes the less expensive option over time (projected at $115.43 per participant over three years) [67]. Live exercises, in contrast, incur recurring costs that scale with the number of participants [67].
- Inpatient Pain Management: An economic model of using VR for inpatient pain management suggested that a VR program could be cost-saving for a hospital system, primarily if it reduces the patient's length of stay (LOS) by 14.6% or more. Savings from reduced opioid use alone were not sufficient to offset program costs, highlighting that the primary financial benefit may come from improving key hospital efficiency metrics [71].
Table 3: Comparative Cost Analysis: VR vs. Traditional Methods
| Cost Factor | VR-Based Assessment/Training | Traditional Live Drill/Assessment |
|---|---|---|
| Initial Development/Setup | High (software development, hardware purchase) [67]. | Low to moderate (planning meetings, material preparation) [67]. |
| Cost per Participant (Initial) | Higher [67]. | Lower [67]. |
| Cost per Participant (3-Year Horizon) | Lower (development costs amortized) [67]. | Remains fixed (costs scale with participants) [67]. |
| Primary Driver of Cost-Savings | Reusability, automation, reduced staff time, potential to reduce hospital LOS [67] [71]. | N/A (costs are recurrent) |
| Scalability | High (can be deployed to many users asynchronously) [67]. | Low (limited by space, time, and trainer availability) [67]. |
Implementation Roadmap
Decision Pathway for Clinical Implementation:
Successful implementation depends on several key factors:
- Addressing Technical and Methodological Pitfalls: When procuring or developing a VR system, clinicians should ensure it meets criteria set by major neuropsychological organizations. This includes demonstrating safety (low cybersickness), robust psychometric properties (reliability and validity), and data security [72].
- Phased Rollout and Staff Training: Begin with a pilot program to validate the tool in a specific clinical context (e.g., MCI screening). Invest in training for staff to administer and interpret the tests, which is less specialized than that required for full neuropsychological assessment [57].
- Managing Upfront Costs: The initial investment in hardware and software can be a barrier. The economic model shows that achieving cost savings is highly sensitive to the number of patients using the system. Therefore, implementing VR for high-volume populations is crucial for demonstrating a return on investment [71].
Head-to-Head: Validation Studies and Comparative Sensitivity of VR vs. Traditional Tests
The integration of virtual reality (VR) into neuropsychological assessment represents a paradigm shift, moving evaluation beyond the confines of the clinic and into simulated real-world environments. This transition necessitates rigorous validation against established traditional tests. Convergent validity examines the extent to which VR and traditional tests measuring the same cognitive construct produce correlated results, while divergent validity ensures that tests measuring different constructs are not unduly correlated. For researchers and pharmaceutical developers, understanding these psychometric relationships is critical for adopting VR tools that can enhance ecological validity—the ability to predict real-world functioning—and potentially reduce demographic biases inherent in some traditional paper-and-pencil tests [63] [4]. This guide provides a structured comparison of performance data and methodological protocols to inform the selection and implementation of VR-based cognitive assessments.
Quantitative Comparison of VR and Traditional Test Scores
The following tables summarize key experimental data from recent studies, providing a direct comparison of performance and validity correlations between VR-based and traditional neuropsychological tests.
Table 1: Correlation Data (Convergent Validity) Between VR and Traditional Tests
| Cognitive Domain | VR Test | Traditional Test | Correlation Coefficient | Study/Context |
|---|---|---|---|---|
| Verbal Memory | Mindmore Remote RAVLT [73] | Rey Auditory Verbal Learning Test | r = .71 - .83 | Healthy Adults (Remote vs. On-site) |
| Executive Function | Trail Making Test-VR (TMT-VR) [63] | Traditional Trail Making Test | Significant positive correlation (p-value not reported) | Adults with ADHD |
| Global Cognition | CAVIRE-2 [4] | Montreal Cognitive Assessment (MoCA) | Moderate Concurrent Validity | Multi-ethnic Asian Adults (MCI vs. Healthy) |
| Visuospatial Memory | Mindmore Remote Corsi Block [73] | Traditional Corsi Block | r = .48 - .71 | Healthy Adults (Remote vs. On-site) |
| Psychomotor Speed | VR Deary-Liewald Task [42] | PC Deary-Liewald Task | Moderate-to-strong correlation | Neurotypical Adults |
Table 2: Performance Score Differences Between VR and Traditional/PC-Based Tests
| Test Modality | Cognitive Test | Key Performance Finding | Implied Divergent Validity |
|---|---|---|---|
| PC-Based | Corsi Block Task (CBT) | Better recall performance vs. VR [42] | Method may influence visuospatial memory scores. |
| PC-Based | Deary-Liewald Reaction Time | Faster reaction times vs. VR [42] | Method influences psychomotor speed measurement. |
| VR-Based | Digit Span Task (DST) | Similar performance to PC-based version [42] | Suggests modality does not affect verbal working memory. |
| VR-Based | Parkour Test (Motor Skills) | Significant differences in movement time/accuracy vs. Real Environment [74] | VR captures unique motor coordination data. |
Experimental Protocols for Key Validation Studies
To ensure the replicability and critical appraisal of VR validation studies, this section outlines the detailed methodologies from several pivotal experiments.
Protocol: Validation of a Comprehensive VR Cognitive Battery (CAVIRE-2)
The Cognitive Assessment using VIrtual REality (CAVIRE-2) was developed to assess the six domains of cognition (perceptual-motor, executive, complex attention, social, learning/memory, language) automatically in 10 minutes [4].
- Participants: 280 multi-ethnic Asian adults aged 55-84 were recruited from a primary care clinic in Singapore. Based on MoCA scores, 244 were classified as cognitively normal and 36 as cognitively impaired.
- Procedure: Each participant underwent both the CAVIRE-2 assessment and the standard MoCA. The VR assessment consisted of 13 scenarios simulating basic and instrumental activities of daily living (BADL and IADL) within a high-fidelity virtual environment.
- Measures: The study evaluated concurrent validity (against MoCA), convergent validity (against MMSE), test-retest reliability, internal consistency, and discriminative ability (to distinguish cognitive status) of CAVIRE-2.
- Key Outcomes: CAVIRE-2 demonstrated moderate concurrent validity with the MoCA and good test-retest reliability (ICC=0.89). It showed high discriminative ability with an AUC of 0.88, sensitivity of 88.9%, and specificity of 70.5% at an optimal cut-off score [4].
Protocol: Direct Comparison of Working Memory and Psychomotor Tasks in VR vs. PC
A controlled study directly compared performance, user experience, and the influence of individual differences on VR and PC versions of common tests [42].
- Participants: 66 neurotypical adults (aged 18-45) participated.
- Procedure: Participants performed the Digit Span Task (DST), Corsi Block Task (CBT), and Deary-Liewald Reaction Time Task (DLRTT) in both immersive VR (HTC Vive Pro Eye) and on a PC (via PsyToolkit), with the order randomized.
- Measures: The primary measures were test performance scores and reaction times. The study also assessed user experience, usability, and participants' computing and gaming skills via questionnaires.
- Key Outcomes: While the DST showed similar performance across modalities, the PC version yielded better performance on the CBT and faster reaction times. However, regression analyses revealed a critical finding: PC-based performance was influenced by age, computing, and gaming experience, whereas VR-based performance was largely independent of these factors, except for gaming experience predicting CBT backward recall [42].
Protocol: Validation of a Remote Self-Administered Test Battery (Mindmore Remote)
This study assessed the feasibility and convergent validity of a remote, digital test battery conducted by participants at home [73].
- Participants: 52 healthy adults.
- Design: A randomized cross-over design where participants completed either the Mindmore Remote battery at home or traditional paper-based testing on-site first, followed by the other session within two weeks.
- Procedure: The Mindmore Remote battery was self-administered on the participant's home computer and included tests like the Symbol Digit Processing Test and RAVLT. The traditional tests were administered by a psychologist in a clinical setting.
- Measures: Convergent validity was evaluated by correlating scores from parallel tests across the two modalities.
- Key Outcomes: Strong correlations were found for verbal tests (r = .71–.83), while non-verbal tests requiring visuo-motor interaction (e.g., Corsi Block) showed weaker correlations (r = .48–.71). The study also noted that correlations were stronger for participants using a computer mouse compared to a touchpad [73].
Visualizing the Relationship Between Testing Modalities and Validity
The following diagram illustrates the conceptual relationships and key factors involved in establishing convergent and divergent validity between VR and traditional neuropsychological assessments.
This diagram shows how convergent validity is established when VR and traditional tests that target the same underlying cognitive construct produce correlated results. A key proposed advantage of VR is its potentially stronger link to real-world functioning (ecological validity). The diagram also highlights factors that can lead to divergent results, such as the influence of technology bias on traditional computerized tests and the unique modality-specific demands of VR environments [73] [42].
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers aiming to conduct similar validation studies, the following table details key hardware, software, and assessment tools referenced in the featured experiments.
Table 3: Essential Materials for VR vs. Traditional Test Validation Research
| Tool Name | Type | Primary Function | Example Use in Research |
|---|---|---|---|
| HTC Vive Pro Eye | Hardware: VR Headset | Provides immersive VR experience with integrated eye-tracking. | Used for administering VR versions of DST, CBT, and DLRTT [42]. |
| CAVIRE-2 Software | Software: VR Assessment | Automated battery assessing six cognitive domains via 13 daily living scenarios. | Validated against MoCA for distinguishing MCI in a primary care population [4]. |
| Mindmore Remote | Software: Remote Assessment | Self-administered digital test battery for remote cognitive assessment. | Used to study convergent validity of remote vs. in-person testing [73]. |
| Montreal Cognitive Assessment (MoCA) | Tool: Traditional Test | Standardized brief cognitive screening tool. | Served as the reference standard for classifying cognitive status and validating CAVIRE-2 [4]. |
| Unity 2019.3.f1 | Software: Game Engine | Platform for developing and prototyping interactive VR experiences. | Used to build the software for VR cognitive tasks [42]. |
| PsyToolkit | Software: Online Research | Platform for creating and running computerized behavioral experiments. | Hosted the PC-based versions of the DST, CBT, and DLRTT [42]. |
The early and accurate detection of mild cognitive impairment (MCI) and mild traumatic brain injury (mTBI) represents a critical challenge in clinical neuroscience. Traditional neuropsychological assessments, while foundational, are constrained by issues of ecological validity, subjective interpretation, and insufficient sensitivity to subtle deficits. Virtual reality (VR) technology has emerged as a transformative tool, creating controlled, immersive environments that closely simulate real-world cognitive demands. This review synthesizes current evidence on the superior sensitivity of VR-based assessments compared to traditional tools for detecting MCI and mTBI, providing researchers and drug development professionals with a data-driven comparison of their performance.
Theoretical Foundations: Why VR Enhances Sensitivity
VR technology enhances assessment sensitivity through two primary mechanisms: ecological validity and multidimensional data capture.
Enhanced Ecological Validity
Traditional paper-and-pencil tests often lack verisimilitude—the degree to which test demands mirror those encountered in naturalistic environments [4]. VR addresses this limitation by immersing individuals in simulated daily activities, such as navigating a supermarket or sorting clothing, thereby engaging brain networks in a more authentic context. This approach reveals subtle deficits that may not manifest in artificial testing environments [7] [4].
High-Density Behavioral Data Capture
VR systems automatically and precisely record a rich array of behavioral metrics beyond simple accuracy and time. These include hand movement trajectory in 3D space, hesitation latency, head movement, and gait patterns under dynamic sensory conditions [47] [50] [75]. This granular data provides a more sensitive measure of functional integrity than traditional scores, capturing subclinical impairments that standard tests miss [75].
Quantitative Performance Comparison: VR vs. Traditional Tests
Detection of Mild Cognitive Impairment (MCI)
Table 1: Performance Comparison of VR-Based vs. Traditional Tests for MCI Detection
| Assessment Tool | Sensitivity (%) | Specificity (%) | Area Under Curve (AUC) | Key Differentiating Metrics |
|---|---|---|---|---|
| VR Stroop Test (VRST) [47] | 97.9 | 96.9 | 0.981 (3D Trajectory) | 3D trajectory length, hesitation latency |
| VR Tests (Meta-Analysis) [48] | 89 | 91 | 0.95 | Performance in simulated IADLs* |
| CAVIRE-2 System [4] | 88.9 | 70.5 | 0.88 | Composite score across 13 VR scenarios |
| Montreal Cognitive Assessment (MoCA) [48] | ~80-85 | ~75-80 | ~0.86-0.90 | Standard composite score |
*IADLs: Instrumental Activities of Daily Living
A systematic review and meta-analysis of 14 studies found that VR-based tests demonstrated a collective sensitivity of 0.89 and specificity of 0.91 for discriminating adults with MCI from healthy controls, with a summary Area Under the Curve (AUC) of 0.95 [48]. These values indicate that VR tests collectively offer superior detection performance compared to the Montreal Cognitive Assessment (MoCA), a widely used traditional tool [48].
The VR Stroop Test (VRST), which requires users to sort virtual clothing items while ignoring distracting color information, achieved near-perfect discrimination. The 3D trajectory length of hand movements was the most powerful biomarker, yielding an AUC of 0.981, sensitivity of 97.9%, and specificity of 96.9% [47].
Detection of Mild Traumatic Brain Injury (mTBI)
Table 2: Performance of VR-Based Assessments for mTBI Detection
| Assessment Paradigm | Target Deficit | Key Differentiating Metrics | Reported Accuracy / Effect |
|---|---|---|---|
| Sensorimotor Conflict during Walking [75] | Dynamic Balance | Lower limb acceleration, Hip strategy utilization | Average Accuracy ≈ 0.90 |
| Virtual Tunnel (Optic Flow) [50] | Postural Control | Body sway amplitude (BSA), Postural instability (vRMS) | Detection at 3 months post-injury |
| VR Eye-Tracking (ET/VR) [49] | Oculomotor Function | 52 oculomotor parameters | Not statistically significant |
The application of VR for mTBI assessment shows more variable outcomes, highly dependent on the specific paradigm and deficits targeted.
Research using provocative sensorimotor conflicts during walking in an immersive virtual environment demonstrated high accuracy (≈0.90) in discriminating between individuals with mTBI and healthy controls. This approach was significantly more sensitive than standard clinical tests like the Balance Evaluation Systems Test (BESTest) or the Dynamic Gait Index, which failed to differentiate the groups [75].
Similarly, a study using a Virtual Tunnel Paradigm to deliver dynamic visual stimuli (optic flow) found that children with mTBI exhibited significantly greater body sway amplitude and postural instability at 3 months post-injury compared to matched controls. These deficits were detected using the VR paradigm despite being undetectable with the Bruininks-Oseretsky Test of Motor Proficiency (BOT-2) [50].
In contrast, a 2025 study exploring VR-based eye-tracking in an emergency department setting found no statistically significant difference in oculomotor function between mTBI and control groups, concluding that the technology in its current form could not be recommended for acute mTBI diagnosis [49]. This highlights that the superior sensitivity of VR is not universal and is contingent on appropriate task design and targeted functional domains.
Detailed Experimental Protocols
VR Stroop Test (VRST) for MCI
- Objective: To detect executive dysfunction, specifically inhibitory control, in MCI through an ecologically valid task [47].
- Virtual Environment: Participants are immersed in a scenario where they must sort virtual clothing items (e.g., shirts, pants) into semantically correct storage boxes [47].
- Task: The test uses a reverse Stroop paradigm. Participants must ignore the salient color of the item (e.g., a yellow shirt) and categorize it based on its semantic identity (e.g., place it in the "shirts" box, which may be red). This creates continuous inhibitory demand [47].
- Data Collection: Behavioral responses are captured at 90 Hz using a hand controller. The system records:
- Total completion time
- 3D trajectory length of the controller (physical efficiency)
- Hesitation latency before initiating movement [47].
- Analysis: Machine learning or statistical models are used to classify participants based on these embodied behavioral metrics.
Sensorimotor Conflict for mTBI
- Objective: To uncover subtle, persistent balance impairments in mTBI by challenging the sensorimotor system with conflicting sensory inputs [75].
- Setup: Computer-Assisted Rehabilitation Environment (CAREN) system, comprising an instrumented treadmill on a motion base within a 360° projection dome [75].
- Protocol:
- Participants walk at a comfortable pace in a virtual hallway.
- Perturbations are systematically introduced:
- Visual: The virtual scene unexpectedly shifts.
- Proprioceptive: The treadmill platform tilts or translates rapidly.
- These perturbations create conflicts between visual, vestibular, and proprioceptive sensory signals [75].
- Data Collection: High-precision motion capture, wearable sensors, and lower limb accelerometry capture the participant's postural and gait responses [75].
- Analysis: Features such as lower limb acceleration metrics, step variability, and the use of hip vs. ankle balance strategies are extracted and used for group classification.
The Researcher's Toolkit: Key Solutions for VR Assessment
Table 3: Essential Research Reagents and Platforms for VR Neuroassessment
| Solution / Platform | Type | Primary Research Application | Key Function |
|---|---|---|---|
| CAVIRE-2 System [4] | Fully Immersive VR Software | Comprehensive MCI Screening | Automatically assesses 6 cognitive domains via 13 daily-living scenarios. |
| VR Stroop Test (VRST) [47] | VR Software Task | Executive Function in MCI | Quantifies inhibitory control via embodied 3D hand trajectories. |
| CAREN System [75] | Integrated Hardware/Platform | Sensorimotor & Gait Analysis in mTBI | Delivers controlled sensorimotor perturbations during walking. |
| Virtual Tunnel Paradigm [50] | VR Visual Stimulation | Postural Control in mTBI | Generates dynamic optic flow to challenge visuo-vestibular integration. |
| EyeTrax VR Glasses [49] | VR with Integrated Eye-Tracking | Oculomotor Assessment | Tracks saccades, smooth pursuit, and pupil response in a VR headset. |
| Nesplora Aula [76] | Immersive VR Assessment | ADHD & Neurodevelopmental | Assesses attention in a simulated classroom with real-world distractions. |
Evidence consistently demonstrates that well-designed VR-based assessments can achieve superior sensitivity compared to traditional neuropsychological tests for detecting MCI and specific, persistent deficits in mTBI. The key advantage lies in the technology's ability to capture high-density, ecologically valid behavioral data during the performance of complex tasks that closely mirror real-world cognitive and physical demands.
For MCI detection, VR paradigms that challenge executive functions and memory in simulated daily activities show particularly strong diagnostic performance, often exceeding that of the MoCA. For mTBI, the picture is more nuanced: VR is highly sensitive for uncovering lingering balance and sensorimotor integration deficits, especially when using provocative conflict paradigms during dynamic tasks like walking. However, its utility for acute diagnosis based on oculomotor metrics alone requires further development.
For researchers and drug development professionals, VR technology offers a powerful tool for identifying subtle neurocognitive deficits, potentially enabling earlier intervention and providing sensitive, objective endpoints for clinical trials. Future efforts should focus on standardizing protocols, improving accessibility, and validating systems across diverse populations and clinical settings.
This guide provides an objective comparison between Virtual Reality (VR)-based assessments and traditional neuropsychological tests for predicting return-to-work (RTW) outcomes and evaluating daily functioning. While traditional paper-and-pencil tests have long been the clinical standard, emerging VR technologies demonstrate superior ecological validity and predictive power by simulating real-world environments and tasks. The analysis synthesizes current research findings, detailed experimental protocols, and performance data, offering researchers and drug development professionals a evidence-based framework for evaluating these assessment tools.
Quantitative Comparison: VR vs. Traditional Assessments
The table below summarizes key performance metrics from recent studies, directly comparing VR-based assessment tools with traditional neuropsychological tests.
Table 1: Performance Metrics of VR vs. Traditional Cognitive Assessments
| Assessment Tool | Study Population | Sensitivity | Specificity | Area Under Curve (AUC) | Key Predictive Findings |
|---|---|---|---|---|---|
| CAVIRE-2 (VR) [4] | Older adults (55-84 years), Primary care clinic (n=280) | 88.9% | 70.5% | 0.88 (95% CI: 0.81–0.95) | Effectively discriminates between cognitively healthy and impaired individuals [4]. |
| Virtual Kitchen Test (VR) [77] | Young healthy adults (n=42) | Quantitative performance decline reported | Quantitative performance decline reported | N/A | Performance quantitatively declined as executive functional load increased [77]. |
| MentiTree (VR) [6] | Mild-Moderate Alzheimer's patients (n=13) | Feasibility of 93% reported | Feasibility of 93% reported | N/A | Safe, feasible (93%), and showed a tendency to improve visual recognition memory (p=0.034) [6]. |
| Montreal Cognitive Assessment (MoCA) (Traditional) [4] | Older adults (55-84 years), Primary care clinic (n=280) | Benchmark for CAVIRE-2 | Benchmark for CAVIRE-2 | N/A | Used as the reference standard; CAVIRE-2 showed moderate convergent validity with it [4]. |
Table 2: Comparative Advantages of VR and Traditional Assessments
| Feature | VR-Based Assessments | Traditional Neuropsychological Tests |
|---|---|---|
| Ecological Validity | High (Verisimilitude): Mirrors real-world cognitive demands via immersive environments [4] [7]. | Low to Moderate (Veridicality): Correlates scores with outcomes but lacks real-world task simulation [4]. |
| Data Collection | Automated, detailed metrics (response time, errors, movement patterns) [7]. | Manual, reliant on clinician scoring and interpretation [7]. |
| Patient Engagement | Higher, due to immersive and interactive nature [7]. | Can be lower, potentially leading to test-taking fatigue or anxiety [4]. |
| Standardization | High, through automated administration [4]. | Variable, can depend on clinician experience [7]. |
| Sensitivity to Executive Function | High, effectively captures decline under load and in daily tasks [77] [4]. | Variable, may not fully capture real-world executive functioning [4]. |
Experimental Protocols in VR Assessment Research
Protocol 1: Validation of a Comprehensive VR Cognitive Battery
This protocol outlines the methodology for validating the CAVIRE-2 system, a tool designed to assess all six cognitive domains [4].
- Objective: To validate the CAVIRE-2 VR system as an independent tool for differentiating cognitive status in older adults within a primary care setting [4].
- Study Population:
- Participants: 280 multi-ethnic Asian adults aged 55–84 years.
- Setting: Recruited from a public primary care clinic in Singapore.
- Grouping: Based on MoCA scores, 244 were cognitively normal and 36 were cognitively impaired [4].
- VR Apparatus & Software:
- Software: The "Cognitive Assessment using VIrtual REality" (CAVIRE-2) software.
- Environment: A fully immersive VR system with 14 discrete scenes (1 tutorial, 13 test scenarios). The environments simulate local residential and community settings to enhance familiarity and ecological validity [4].
- Assessment Tasks: The 13 test scenarios simulate Basic and Instrumental Activities of Daily Living (BADL and IADL). The software automatically generates a performance matrix based on scores and completion time for tasks across the six cognitive domains: perceptual-motor, executive function, complex attention, social cognition, learning and memory, and language [4].
- Comparative Measure: The Montreal Cognitive Assessment (MoCA) was administered independently to all participants as the reference standard [4].
- Outcome Metrics:
Protocol 2: Feasibility of VR Cognitive Training for Alzheimer's Disease
This protocol describes an intervention study examining the safety and potential efficacy of VR cognitive training.
- Objective: To investigate the safety, feasibility, and clinical efficacy of VR-based cognitive training for patients with mild to moderate Alzheimer's Disease (AD) [6].
- Study Population:
- Participants: 13 individuals diagnosed with mild to moderate AD.
- Inclusion Criteria: Adults aged 50–90, CDR Global score of 0.5–2, stable treatment for >12 weeks [6].
- VR Apparatus & Software:
- Software: MentiTree cognitive training software.
- Hardware: Oculus Rift S head-mounted display (HMD) with hand tracking technology [6].
- Intervention Protocol:
- Duration: 9 weeks.
- Frequency: Two 30-minute sessions per week (total 18 sessions, 540 minutes) [6].
- Content: Alternating indoor and outdoor background cognitive tasks. The difficulty level automatically adjusted based on the participant's performance. Example tasks included making a sandwich, tidying a room, shopping, and finding directions [6].
- Assessment Metrics:
- Primary: Safety (adverse effects) and feasibility (adherence rate).
- Secondary: Cognitive functions assessed pre- and post-intervention using the Korean MMSE-2, CDR, GDS, and the Literacy Independent Cognitive Assessment (LICA) [6].
Workflow and Conceptual Diagrams
The following diagram illustrates the typical workflow of a comparative study validating a VR assessment tool against traditional methods.
Comparative Study Validation Workflow
This diagram outlines the logical relationship between the core concepts discussed, highlighting the unique advantages of VR assessments.
Logic of Enhanced Predictive Power
Table 3: Key Research Reagent Solutions for VR Assessment Studies
| Tool / Component | Specification / Example | Primary Function in Research |
|---|---|---|
| Immersive VR Headset | Oculus Rift S (as used in MentiTree study) [6] | Presents the virtual environment; critical for user immersion and presence. Key specs include resolution, field of view, and refresh rate. |
| VR Assessment Software | CAVIRE-2 [4], MentiTree [6], VRFCAT (Modified Kitchen Test) [77] | Creates the standardized cognitive tasks and environments. The software design directly impacts ecological validity and the cognitive domains assessed. |
| Interaction Technology | Hand Tracking Sensors [6] | Enables natural user interaction with the virtual environment (e.g., grabbing objects), replacing controllers to reduce barriers for non-tech-savvy populations. |
| Performance Data Logger | Integrated automated system (e.g., in CAVIRE-2) [4] | Captures rich, objective outcome measures like task completion time, error rates, and sequence of actions, which are essential for predictive modeling. |
| Traditional Benchmark Tests | Montreal Cognitive Assessment (MoCA) [4] [7], Mini-Mental State Examination (MMSE) [7] | Serves as the reference standard for validating new VR tools and establishing concurrent validity. |
| Domain-Specific Outcome Measures | Literacy Independent Cognitive Assessment (LICA) [6], Work Capacity at Discharge [78] | Provides targeted metrics for specific research goals, such as assessing low-education populations or measuring concrete RTW outcomes. |
The body of evidence demonstrates that VR-based assessments hold significant promise for surpassing traditional neuropsychological tests in predicting real-world functioning and RTW outcomes. The core advantage of VR lies in its high ecological validity, or verisimilitude, which allows it to simulate the complex cognitive demands of daily life and work environments more effectively than paper-and-pencil tests [4] [7]. Tools like CAVIRE-2 show strong discriminative power and reliability, indicating their potential as valid clinical and research tools [4]. For researchers and drug development professionals, integrating VR assessments into clinical trials could provide more sensitive, objective, and functionally meaningful endpoints for evaluating cognitive outcomes and intervention efficacy.
Traditional neuropsychological assessments, while foundational to clinical neuroscience, are constrained by their static, paper-and-pencil format. They typically produce outcome-based scores (e.g., total correct, time to completion) that offer limited insight into the dynamic cognitive processes underlying task performance. This creates a data fidelity gap—a disconnect between the abstract cognitive constructs measured in the clinic and their manifestation in real-world, daily activities [69]. Virtual Reality (VR) bridges this gap by providing a controlled, yet ecologically valid, environment that captures rich, time-based performance metrics. For researchers and drug development professionals, this paradigm shift offers unprecedented granularity in quantifying cognitive function and tracking intervention efficacy.
Theoretical Foundation: Ecological Validity and Metric Richness
The superior data capture capabilities of VR are grounded in the concept of ecological validity, which encompasses both veridicality (the ability of a test to predict real-world functioning) and verisimilitude (the degree to which test demands mirror those of daily life) [69] [4].
Traditional tests often operate at the veridicality level, using scores from contrived tasks to infer real-world ability. In contrast, VR employs a verisimilitude-based approach, immersing individuals in simulated real-world scenarios like a virtual supermarket or apartment [4]. This immersion generates cognitive and behavioral demands that closely mimic everyday life, thereby yielding data that is more directly generalizable to a patient's functional status.
Furthermore, traditional paper-and-pencil tests are limited in the metrics they can capture. VR, however, automatically and precisely logs a vast array of performance data throughout the entire task, transforming assessment from a snapshot into a detailed movie of cognitive and behavioral processes.
Table 1: Core Theoretical Advantages of VR in Data Capture
| Dimension | Traditional Neuropsychological Tests | VR-Based Assessments |
|---|---|---|
| Primary Data Type | Outcome-based scores (e.g., total errors) | Process-based, time-series data |
| Ecological Approach | Veridicality (correlation with function) | Verisimilitude (simulation of function) |
| Temporal Resolution | Low (e.g., total time for a task) | High (e.g., millisecond-level reaction times, movement paths) |
| Metric Spectrum | Narrow (accuracy, time) | Broad (navigation efficiency, head tracking, kinematic data) |
| Context | Sterile, laboratory setting | Dynamic, contextually embedded environment |
Quantitative Comparisons: VR vs. Traditional Methods
Empirical studies directly comparing VR and traditional methods consistently demonstrate VR's enhanced sensitivity and specificity in detecting subtle cognitive abnormalities.
Detecting Residual Cognitive Deficits
A seminal study on sport-related concussion assessed clinically asymptomatic athletes using a VR-based neuropsychological tool. The results, summarized in Table 2, show that VR modules were exceptionally effective at identifying lingering cognitive deficits that were no longer apparent through standard clinical diagnosis [23].
Table 2: Sensitivity and Specificity of a VR Tool for Detecting Residual Concussion Abnormalities [23]
| Assessment Module | Sensitivity | Specificity | Effect Size (Cohen's d) |
|---|---|---|---|
| Spatial Navigation | 95.8% | 91.4% | 1.89 |
| Whole Body Reaction Time | 95.2% | 89.1% | 1.50 |
| Combined VR Modules | 95.8% | 96.1% | 3.59 |
The combined VR assessment achieved a remarkable effect size (d=3.59), indicating a powerful ability to discriminate between concussed and control athletes based on performance metrics alone [23].
Discriminating Mild Cognitive Impairment
In the context of aging and neurodegenerative disease, the "Cognitive Assessment using VIrtual REality" (CAVIRE-2) system was validated against the established Montreal Cognitive Assessment (MoCA). CAVIRE-2 automatically assesses performance across 13 scenarios simulating daily activities in about 10 minutes [4].
Table 3: Performance of CAVIRE-2 vs. MoCA in Discriminating Cognitive Status [4]
| Metric | MoCA | CAVIRE-2 |
|---|---|---|
| Assessment Duration | ~10-15 minutes | ~10 minutes |
| Ecological Validity | Low (veridicality-based) | High (verisimilitude-based) |
| Data Automation | Low (examiner-dependent) | High (fully automated) |
| Discriminative Power (AUC) | Reference Standard | 0.88 |
| Sensitivity/Specificity | Varies by cutoff | 88.9% / 70.5% |
The study concluded that CAVIRE-2 is a valid and reliable tool with good test-retest reliability (ICC=0.89) and internal consistency (Cronbach’s α=0.87), demonstrating that automated VR assessment can rival traditional methods in diagnostic accuracy while offering superior ecological validity [4].
Experimental Protocols and Methodologies
To ensure reproducible results, researchers must adhere to rigorous experimental designs. Below are detailed methodologies for key types of VR cognitive assessment studies.
- Objective: To determine the sensitivity and specificity of a VR-based neuropsychological tool for detecting residual cognitive abnormalities following a sport-related concussion in clinically asymptomatic athletes.
- Participants: 128 control athletes with no concussion history and 24 concussed athletes.
- VR Apparatus: An immersive VR system with components for spatial navigation, whole-body reaction time, attention, and balance assessment.
- Procedure:
- Testing Timeline: Concussed athletes were tested within 10 days of injury (Mean = 8.33 days), once they were clinically asymptomatic.
- Module Administration:
- Spatial Navigation: Participants navigated through a virtual environment to assess spatial memory and planning.
- Whole Body Reaction Time: Participants responded to visual stimuli using full-body movements, capturing reaction speed and motor control.
- Attention & Balance: Integrated tasks required maintaining balance while performing attention-demanding activities.
- Data Capture: The system automatically logged accuracy, completion time, path efficiency, and kinematic data for each module.
- Analysis: Sensitivity and specificity were calculated for each module and for the combined battery. Effect sizes (Cohen's d) were computed to determine the magnitude of difference between concussed and control groups.
- Objective: To validate the CAVIRE-2 VR system as a tool for distinguishing cognitively healthy older adults from those with mild cognitive impairment (MCI).
- Study Design: Cross-sectional study in a primary care setting.
- Participants: 280 multi-ethnic Asian adults aged 55-84 years.
- Procedure:
- Traditional Assessment: All participants completed the MoCA and MMSE.
- VR Assessment: Participants then completed the CAVIRE-2 assessment, which includes 13 scenarios in a virtual environment modeled after local residential and community settings. Tasks simulate both Basic and Instrumental Activities of Daily Living (BADL and IADL).
- Performance Metrics: CAVIRE-2 automatically generates a total score based on a matrix of accuracy and time-to-completion across all tasks.
- Analysis:
- Convergent Validity: Correlation between CAVIRE-2 scores and MoCA/MMSE scores.
- Reliability: Test-retest reliability assessed with Intraclass Correlation Coefficient (ICC) and internal consistency with Cronbach's alpha.
- Discriminative Ability: Area Under the Curve (AUC) analysis to determine how well CAVIRE-2 scores differentiate between cognitively normal and impaired participants (as defined by MoCA cut-off).
The Researcher's Toolkit: Essential Reagents & Materials
Successful implementation of VR-based cognitive assessment requires specific hardware, software, and methodological components.
Table 4: Key Research Reagent Solutions for VR Cognitive Assessment
| Item | Function & Importance | Exemplars / Specifications |
|---|---|---|
| Immersive Head-Mounted Display (HMD) | Presents the 3D virtual environment; critical for inducing a sense of presence and ecological validity. | Meta Quest series, HTC Vive Focus 3, Pico Neo 3 Pro [79] [20] |
| VR Assessment Software | Administers standardized cognitive tasks and automatically logs performance data; the core of the experimental intervention. | CAVIRE-2 [4], Enhance VR [20], STEP-VR [80] [81] |
| Motion Controllers | Enable user interaction with the virtual environment (e.g., pointing, grabbing, manipulating objects). | Typically paired with the HMD (e.g., Oculus Touch, Vive controllers) |
| Data Analytics Platform | Processes the rich, time-series data generated by the VR system (e.g., navigation paths, reaction times, errors). | Custom dashboards or integrated software analytics (e.g., tracking completion rates, skill competency) [79] |
| Standardized Traditional Battery | Serves as the clinical reference standard for validating the novel VR assessment. | Montreal Cognitive Assessment (MoCA), Stroop Task, Trail Making Test [4] [20] |
Visualizing Workflows and Conceptual Frameworks
The following diagrams, generated using Graphviz DOT language, illustrate the core concepts and experimental workflows discussed in this guide.
Conceptual Framework of VR's Ecological Validity
Typical VR Cognitive Assessment Experimental Workflow
The evidence compellingly demonstrates that VR provides a superior framework for objective data capture in cognitive assessment. By moving beyond static scores to capture rich, time-based performance metrics within ecologically valid environments, VR offers researchers and clinicians a more sensitive and functionally relevant toolset. This is evidenced by high sensitivity and specificity in detecting residual concussion deficits [23] and strong discriminative power in identifying mild cognitive impairment [4].
For the field of drug development, these advancements are particularly significant. The ability to capture granular, objective data on cognitive function can lead to more sensitive endpoints for clinical trials, potentially reducing sample sizes and trial durations by detecting treatment effects that traditional measures would miss. Future work should focus on standardizing VR assessment protocols across research sites, further integrating biometric data streams (e.g., eye-tracking, EEG), and leveraging artificial intelligence to identify complex patterns within the rich datasets that VR generates [82] [83]. This will solidify VR's role as an indispensable tool in the modern cognitive scientist's and drug developer's arsenal.
Conclusion
The accumulated evidence strongly positions VR-based neuropsychological assessments as a superior alternative to traditional tests for detecting subtle cognitive impairments and predicting real-world functional outcomes. Key takeaways include VR's enhanced ecological validity, demonstrated through its high sensitivity and specificity in discriminating cognitive status and forecasting critical milestones like return to work. For biomedical and clinical research, this translates into more sensitive endpoints for clinical trials, earlier intervention opportunities, and tools that better reflect a treatment's impact on daily life. Future directions must focus on developing standardized VR batteries, establishing normative data across populations, and further integrating biometric data to solidify VR's role as the next generation of cognitive assessment.
References
- 1. Ecological validity | Definition & Examples [https://www.britannica.com/science/ecological-validity]
- 2. Veridicality vs. Verisimilitude [http://futureofcio.blogspot.com/2024/11/veridicality-vs-verisimilitude.html]
- 3. The challenges of ecological validity in the ... - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/19752651/]
- 4. Validity and reliability of a virtual reality system as an ... [https://link.springer.com/article/10.1007/s10055-025-01187-0]
- 5. The ecological validity of neuropsychological tests [https://pubmed.ncbi.nlm.nih.gov/15000225/]
- 6. Preliminary study on the feasibility of virtual reality-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495198/]
- 7. Extended reality for neurocognitive assessment [https://www.sciencedirect.com/science/article/abs/pii/S002239562500189X]
- 8. online administration of MoCA in diverse populations [https://www.nature.com/articles/s41746-025-01787-9]
- 9. The study of the effect of virtual reality technology ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1579909/full]
- 10. Racial/ethnic differences in neuropsychological test ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12545695/]
- 11. Validation and comparison of virtual reality and 3D mobile ... [https://www.nature.com/articles/s41598-024-75065-1]
- 12. Examining the Validity and Utility of Montreal Cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10123003/]
- 13. Cognitive Tests - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/cognitive-tests]
- 14. Regression-based normative scores for the Montreal ... [https://www.nature.com/articles/s41598-025-03167-5]
- 15. Addenbrooke's Cognitive Examination III (ACE‐III) and mini ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6916534/]
- 16. Interpreting Addenbrooke's Cognitive Examination‐III ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207243/]
- 17. Mini‐Mental State Examination (MMSE) for the detection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6464748/]
- 18. Validity and Cultural Generalisability of a 5-Minute AI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8339427/]
- 19. Concurrent Validity of Virtual Reality-Based Assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11595626/]
- 20. Evaluating cognitive performance using virtual reality ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2023.1153145/full]
- 21. Systematic review of memory assessment in virtual reality [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2024.1380575/full]
- 22. The role of virtual reality-based cognitive training in ... [https://www.nature.com/articles/s41598-025-08173-1]
- 23. Determining sensitivity/specificity of virtual reality-based ... [https://pubmed.ncbi.nlm.nih.gov/27045961/]
- 24. A comparison of immersive virtual reality with traditional ... [https://pubmed.ncbi.nlm.nih.gov/28482936/]
- 25. Effects of immersive leisure-based virtual reality cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11960153/]
- 26. Effects of virtual reality-based interventions on cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12000106/]
- 27. An Experimental Study On Usefulness Of Virtual Reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6826194/]
- 28. Cross-Sectional Study Using Virtual Reality to Measure ... [https://www.frontiersin.org/journals/sports-and-active-living/articles/10.3389/fspor.2020.543676/full]
- 29. Cognitive efficiency in VR simulated natural indoor ... [https://www.nature.com/articles/s41598-025-18629-z]
- 30. Cognition Assessment in Virtual Reality (CAVIR) ... [https://www.sciencedirect.com/science/article/pii/S0165032724017956]
- 31. Comparison of Traditional and Virtual Reality-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9406179/]
- 32. Validating the Measurement of Real-World Functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3670945/]
- 33. Virtual Reality Clinical Trials: Step Inside the Future of ... [https://ccrps.org/clinical-research-blog/virtual-reality-clinical-trials-step-inside-the-future-of-medicine-2025]
- 34. Comparing Immersive and Non-Immersive VR: Effects on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384383/]
- 35. What Are the 3 Types of Virtual Reality: A Deep Dive into ... [https://inairspace.com/blogs/learn-with-inair/what-are-the-3-types-of-virtual-reality-a-deep-dive-into-immersive-digital-worlds?srsltid=AfmBOorW5X2qtDHgqZXSiC2uzC7fCykApd_XA_RfzS1fAO0QSS6Mm6Ja]
- 36. Virtual Reality Guide 2025: Complete VR Technology ... [https://treeview.studio/blog/virtual-reality-complete-guide]
- 37. Virtual Reality Headset Comparison 2025: The Ultimate ... [https://inairspace.com/blogs/learn-with-inair/virtual-reality-headset-comparison-2025-the-ultimate-buyers-guide?srsltid=AfmBOooEIx8dwLe970we_fxmLUgcMQ8P8RyCMeitX4pK1yGMOc565NG-]
- 38. The Best VR Headsets We've Tested for 2025 [https://www.pcmag.com/picks/the-best-vr-headsets]
- 39. Best VR headset in 2025: my top picks for stunning virtual ... [https://www.pcgamer.com/best-vr-headset/]
- 40. The best VR headset in 2025: All the latest devices compared [https://www.gamesradar.com/the-best-vr-headset/]
- 41. Extended reality for neurocognitive assessment [https://pubmed.ncbi.nlm.nih.gov/40133021/]
- 42. Immersive Virtual Reality Assessments of Working Memory ... [https://arxiv.org/html/2503.06333v2]
- 43. Virtual Reality in Training of Sustained Attention ... [https://www.sciencedirect.com/science/article/pii/S0003999325008019]
- 44. A novel reaction time assessment in virtual reality [https://link.springer.com/article/10.3758/s13428-025-02752-w]
- 45. Cognition Assessment in Virtual Reality (CAVIR) [https://pubmed.ncbi.nlm.nih.gov/39447982/]
- 46. Comparing Virtual Reality–Based and Traditional Physical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11759906/]
- 47. Detection of mild cognitive impairment using a virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12335173/]
- 48. Virtual reality technology in the detection of mild cognitive ... [https://www.sciencedirect.com/science/article/abs/pii/S156816372300048X]
- 49. Diagnosis of mTBI in an ER Setting Using Eye-Tracking and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562693/]
- 50. Dynamic Visual Stimulations Produced in a Controlled ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2021.596615/full]
- 51. Immersive virtual reality assessments of working memory ... [https://pubmed.ncbi.nlm.nih.gov/41056132/]
- 52. Immersive virtual reality for older adults: Challenges and ... [https://www.sciencedirect.com/science/article/pii/S1568163725001175]
- 53. Impact of sensorimotor mismatch on virtual reality sickness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12226871/]
- 54. Validity and usability for digital cognitive assessment tools to ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-025-01665-1]
- 55. Virtual reality for older people: effectiveness of a training ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1553318/full]
- 56. Moving toward the digitalization of neuropsychological tests [https://pmc.ncbi.nlm.nih.gov/articles/PMC12059415/]
- 57. Traditional Neuropsychological Testing is Limited [https://creyos.com/blog/neuropsychological-testing]
- 58. Older Adults' Acceptance of a Virtual Reality Group ... [https://humanfactors.jmir.org/2024/1/e56278/]
- 59. Overcoming 4 Challenges in Multicenter Clinical Trials [https://www.florencehc.com/overcoming-four-common-challenges-in-multicenter-research/]
- 60. Scaling eSource-Enabled Clinical Trials: Hospital ... [https://www.appliedclinicaltrialsonline.com/view/scaling-esource-enabled-clinical-trials-hospital-perspectives]
- 61. Conventional and neuropsychological criteria for mild ... [https://www.nature.com/articles/s41598-025-04275-y]
- 62. Rethinking neuropsychological test validity in dementia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540449/]
- 63. The Trail Making Test in Virtual Reality (TMT-VR) [https://www.mdpi.com/2673-5318/6/1/31]
- 64. What traditional neuropsychological assessment got wrong ... [https://pubmed.ncbi.nlm.nih.gov/39066740/]
- 65. Biomarkers of Immersion in Virtual Reality Based on Features ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11119742/]
- 66. Can the Virtual Reality-Based Spatial Memory Test Better ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9408476/]
- 67. Comparative Cost of Virtual Reality Training and Live ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7231540/]
- 68. Neuropsychological Assessment - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK513310/]
- 69. Virtual Reality for Enhanced Ecological Validity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4675850/]
- 70. The Role of Virtual Reality in Screening, Diagnosing, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7893135/]
- 71. Economic analysis of implementing virtual reality therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6550142/]
- 72. How immersive virtual reality methods may meet the ... [https://www.sciencedirect.com/science/article/pii/S2451958821000993]
- 73. Remote Neuropsychological Testing as an Alternative to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12378557/]
- 74. Reliability and validity of a self-developed virtual reality- ... [https://www.nature.com/articles/s41598-025-89385-3]
- 75. Sensorimotor conflict tests in an immersive virtual ... [https://www.nature.com/articles/s41598-020-71611-9]
- 76. Virtual Reality in Neuropsychological Assessment [https://nesplora.com/en/blog/virtual-reality-in-neuropsychological-assessment-a-conversation-with-dr-nichols/]
- 77. Functional performance in a virtual reality task with ... [https://www.sciencedirect.com/science/article/pii/S245195882030035X]
- 78. Machine learning to predict return to work after medical ... [https://www.researchsquare.com/article/rs-7254539/latest]
- 79. VR Training vs Traditional Training: What Works Best in ... [https://www.autovrse.com/blogs/vr-training-vs-traditional-training]
- 80. Comparing Virtual Reality-Based and Traditional Physical ... [https://pubmed.ncbi.nlm.nih.gov/39793025/]
- 81. Comparing Virtual Reality–Based and Traditional Physical ... [https://www.jmir.org/2025/1/e55066/]
- 82. Virtual reality in drug design: Benefits, applications and ... [https://www.sciencedirect.com/science/article/pii/S0959440X25000624]
- 83. Artificial Intelligence in Drug & Biological Product Development [https://ctti-clinicaltrials.org/2025-ai-in-drug-biological-product-development/]