Motion Correction Algorithms in Biomedical Imaging: A Performance Comparison Across Modalities and Applications
This article provides a comprehensive comparison of motion correction algorithms, addressing a critical challenge in biomedical imaging and drug development.
Motion Correction Algorithms in Biomedical Imaging: A Performance Comparison Across Modalities and Applications
Abstract
This article provides a comprehensive comparison of motion correction algorithms, addressing a critical challenge in biomedical imaging and drug development. It explores the foundational principles of motion artifacts and their impact on quantitative analysis, examines the diverse methodologies from deep learning to model-based approaches, and discusses optimization strategies for real-world applications. By presenting a cross-modality performance analysis and validation frameworks, this review serves as a strategic guide for researchers and professionals selecting and implementing motion correction techniques to enhance data quality, improve diagnostic accuracy, and accelerate model-informed drug development.
Understanding Motion Artifacts: Origins, Impact, and Fundamental Correction Principles
The Critical Challenge of Motion in Quantitative Imaging
Motion artifacts represent one of the most significant and universal challenges in quantitative imaging, compromising data integrity across modalities from functional magnetic resonance imaging (fMRI) and computed tomography (CT) to functional near-infrared spectroscopy (fNIRS). In clinical and research settings, even sub-millimeter movements can introduce artifacts that mimic or obscure true physiological signals, ultimately leading to misdiagnosis, reduced statistical power in research studies, and compromised drug development pipelines. The fundamental goal of motion correction is to maximize sensitivity to true biological signals while minimizing false activations or measurements related to movement, a balance that requires sophisticated algorithmic approaches [1]. As quantitative imaging increasingly serves as a biomarker for therapeutic response in clinical trials, the ability to accurately correct for motion has become paramount for ensuring measurement reliability and reproducibility across single and multi-site studies [2] [3].
This guide provides a comprehensive comparison of motion correction techniques across multiple imaging modalities, presenting experimental data on their performance characteristics and offering detailed methodologies for implementation. By objectively evaluating the strengths and limitations of current approaches, we aim to inform researchers, scientists, and drug development professionals in selecting appropriate motion correction strategies for their specific quantitative imaging applications.
Motion Correction Algorithms: A Cross-Modality Comparison
Retrospective Correction in Functional MRI
In fMRI, motion correction typically involves estimating rigid body movement parameters and applying transformations to realign a time series of brain images. Current approaches iteratively maximize similarity measures between each time point and a reference image, producing six parameters (x, y, and z translations and rotations) for realignment. Commonly used tools include AIR, AFNI 3dvolreg, FSL mcflirt, and SPM realign tools [1].
A critical consideration in fMRI is whether to include motion parameters as covariates of no interest in the general linear model (GLM). Research has demonstrated that for rapid event-related designs, including motion covariates generally increases GLM sensitivity, with little difference whether motion correction is actually applied to the data. Conversely, for block designs, motion covariate inclusion can have a deleterious impact on sensitivity when even moderate correlation exists between motion and experimental design [1].
Table 1: Comparison of fMRI Motion Correction Strategies
| Strategy | Description | Best Application | Key Findings |
|---|---|---|---|
| No Motion Correction | Analysis without motion correction | Low-motion paradigms | High risk of artifactual activations with task-correlated motion |
| Motion Correction Alone (MC) | Estimation and realignment of data | General purpose use | Reduces motion artifacts but leaves residual variance |
| MC + Motion Covariates (MC+COV) | Realignment with motion parameters in GLM | Event-related designs | Increases sensitivity for event-related data; minimal benefit for block designs |
| Non-MC + Covariates (NONMC+COV) | Motion parameters in GLM without realignment | Specific event-related applications | Similar efficacy to MC+COV for event-related designs |
Prospective Motion Correction in Anatomical MRI
Prospective motion correction (PMC) represents a fundamentally different approach that actively monitors head position and adjusts imaging parameters in real-time during acquisition. Unlike retrospective methods that operate on already-corrupted data, PMC aims to prevent motion artifacts from occurring initially. Marker-based PMC systems typically use optical tracking of markers rigidly attached to a subject's head, updating gradient directions, RF pulses, and receiver phase accordingly [4].
The effectiveness of PMC depends heavily on marker fixation method. Comparative studies have evaluated different fixation approaches:
- Mouth guard fixation: Provides stable attachment but may cause patient discomfort
- Nose bridge fixation: Better patient tolerance but potentially less stability
Quantitative evaluation demonstrates that mouth guard fixation achieves better PMC performance compared to nose bridge approaches, highlighting the importance of hardware configuration in motion correction efficacy [4].
Motion Correction in Coronary CT Angiography
In cardiac CT, motion correction must address specific challenges related to heart motion throughout the cardiac cycle. First-generation motion correction algorithms like SnapShot Freeze (SSF1) track and compensate for coronary artery motion using data from three adjacent phases, significantly improving image quality in patients with high heart rates. However, SSF1 only addresses coronary structures, leaving other cardiac motion artifacts uncorrected [5].
The second-generation SSF2 algorithm extends correction to the entire heart, providing more comprehensive motion artifact reduction. A recent retrospective study of 151 patients demonstrated SSF2's superiority: the algorithm significantly improved image quality scores (median = 3.67 for SSF2 vs. 3.0 for SSF1 and standard reconstruction, p < 0.001) and enhanced diagnostic performance for both stenosis assessment and CT fractional flow reserve (CT-FFR) calculations [5].
Table 2: Performance Comparison of CT Motion Correction Algorithms
| Metric | Standard Reconstruction | SSF1 Algorithm | SSF2 Algorithm |
|---|---|---|---|
| Overall Quality Score (median) | 3.0 | 3.0 | 3.67* |
| Correlation with invasive FFR | r = 0.552 | r = 0.593 | r = 0.652* |
| AUC for Ischemic Lesion Diagnosis (per-lesion) | 0.742 | 0.795 | 0.887* |
| AUC for Ischemic Lesion Diagnosis (per-patient) | 0.768 | 0.812 | 0.901* |
*Statistically significant improvement over other methods (p < 0.001)
Motion Artifact Correction in fNIRS
Functional near-infrared spectroscopy faces unique motion challenges, particularly in pediatric populations where data typically contains more artifacts than adult studies. Research comparing six prevalent motion correction techniques with child participants (ages 6-12) performing language tasks has revealed differential effectiveness across artifact types [6].
Motion artifacts in fNIRS are categorized into four distinct types:
- Type A: Sudden spikes (>50 SD from mean within 1 second)
- Type B: Peaks (100 SD from mean, 1-5 seconds duration)
- Type C: Gentle slopes (300 SD from mean, 5-30 seconds duration)
- Type D: Slow baseline shifts (>500 SD from mean, >30 seconds duration)
Evaluation of correction methods using five predefined metrics identified that moving average and wavelet methods yielded the best outcomes for pediatric fNIRS data, though optimal approach selection depends on the specific artifact types prevalent in the dataset [6].
Experimental Protocols and Methodologies
Framework for Prospective Motion Correction Evaluation
Establishing a robust framework for evaluating PMC performance requires addressing the challenge of variable intrinsic motion patterns between acquisitions. One developed methodology uses recorded motion trajectories from human subjects replayed in phantom experiments to enable controlled comparisons [4].
Experimental Protocol:
- Motion Tracking: Record head motion trajectories from human subjects during T1-weighted MRI scans using optical marker-based tracking
- Phantom Replay: Reproduce identical motion patterns in phantom experiments by modulating imaging parameters according to in-vivo recordings
- Image Quality Assessment: Quantify motion-induced degradation using:
- Average Edge Strength (AES): Measures image blurring at edges
- Haralick Texture Entropy (CoEnt): Captures diffuse artifacts and texture changes using gray level co-occurrence matrix analysis
Statistical Analysis: Incorporate motion pattern variability as a covariate in models comparing correction techniques to account for intrinsic differences in motion severity and pattern between scans [4].
Deep Learning Approaches for MRI Motion Correction
Emerging deep learning techniques offer promising alternatives to traditional motion correction algorithms. One recently developed approach uses a deep network to reduce the joint image-motion parameter search to a search over rigid motion parameters alone [7].
Methodology:
- Network Training: Train reconstruction network using simulated motion-corrupted k-space data with known motion parameters
- Network Architecture: Design network that produces reconstruction from two inputs: corrupted k-space data and motion parameters
- Test-Time Estimation: Estimate unknown motion parameters by minimizing data consistency loss between motion parameters, network-based reconstruction, and acquired measurements
Experimental Validation: Intra-slice motion correction experiments on simulated and realistic 2D fast spin echo brain MRI demonstrate high reconstruction fidelity while maintaining explicit data consistency optimization [7].
Comparative Evaluation of fNIRS Correction Techniques
A systematic comparison of fNIRS motion correction methods evaluated six prevalent techniques on data from children (ages 6-12) performing a language task [6].
Experimental Design:
- Participants: 12 children (8 females, mean age = 9.9 years, SD = 1.75)
- Task: Auditory grammatical judgment with rapid event-related design (60 trials total)
- fNIRS Setup: TechEN-CW6 system with 690 and 830 nm wavelengths, 3 channels sampled at 10 Hz over left inferior frontal gyrus
- Data Processing: Implemented using Homer2 fNIRS processing package and custom MATLAB tools
Correction Methods Compared:
- Wavelet-based correction
- Spline interpolation
- Principal component analysis (PCA)
- Moving average (MA)
- Correlation-based signal improvement (CBSI)
- Combined wavelet and MA approach
Evaluation Metrics: Five predefined metrics assessing artifact reduction and signal preservation
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Computational Tools for Motion Correction Research
| Tool/Reagent | Function | Application Context | Key Features |
|---|---|---|---|
| Optical Motion Tracking Systems | Real-time head position monitoring | Prospective motion correction in MRI | MR-compatible cameras, marker-based tracking, real-time parameter updates |
| Moiré Phase Tracking Marker | Reference for optical tracking | Prospective motion correction | Rigid attachment to subject, precise motion capture |
| Homer2 Software Package | fNIRS data processing | Optical brain imaging analysis | Modular pipeline for motion correction, artifact detection, and signal processing |
| SnapShot Freeze Algorithms | Cardiac motion correction | Coronary CT angiography | SSF1: coronary-specific correction; SSF2: whole-heart correction |
| FSL mcflirt & SPM Realign | Image realignment | fMRI preprocessing | Rigid-body registration, integration with analysis pipelines |
| Deep Motion Correction Networks | Learning-based reconstruction | MRI motion correction | Data-consistent reconstructions, motion parameter estimation |
| Geometric Phantoms | Controlled validation | Algorithm performance testing | Anatomically realistic shapes, known ground truth geometry |
Implications for Drug Development and Quantitative Biomarkers
The reliability of motion correction has profound implications for drug development, where quantitative imaging often serves as a pharmacodynamic biomarker in clinical trials. Regulatory agencies like the FDA and EMA have established formal processes for qualifying technologies such as fMRI for specific contexts of use in drug development [2]. However, the burden of proof for biomarker qualification is high, requiring characterization of precision and reproducibility across multiple trials.
Motion artifacts directly impact the value of fMRI readouts for assessing CNS drug effects, as these measurements must be both reproducible and modifiable by pharmacological intervention. Inconsistent motion correction can introduce variability that obscures true drug effects or creates false positives. The Quantitative Imaging Network (QIN) specifically addresses these challenges by promoting research and development of quantitative imaging tools with appropriate correction for technical confounds like motion [3].
Effective motion correction is particularly critical for:
- Target engagement studies: Establishing CNS effects of pharmacological treatment
- Dose-response relationships: Guiding dose selection for later trial phases
- Multi-site trials: Ensuring consistency across different scanning sites and protocols
- Longitudinal studies: Maintaining measurement consistency across multiple time points
Motion correction remains a critical challenge in quantitative imaging, with optimal approach selection highly dependent on imaging modality, experimental design, and subject population. Our comparative analysis demonstrates that while substantial progress has been made across all modalities, each technique carries specific strengths and limitations.
Key findings indicate:
- In fMRI, motion covariate inclusion benefits event-related designs but may harm block design analyses
- Prospective motion correction in MRI shows promise but depends on robust marker fixation
- Second-generation CT motion correction algorithms (SSF2) significantly outperform first-generation approaches
- For pediatric fNIRS, moving average and wavelet methods provide optimal artifact reduction
- Emerging deep learning approaches offer new paradigms for data-consistent motion correction
Future developments will likely focus on integrating multiple correction strategies, developing more sophisticated subject-specific approaches, and creating standardized validation frameworks that account for intrinsic motion variability. As quantitative imaging continues to expand its role in clinical trials and therapeutic development, robust motion correction will remain essential for generating reliable, reproducible biomarkers capable of informing clinical decision-making.
In biomedical imaging, patient or subject motion presents a significant challenge that can compromise image quality and diagnostic utility. Motion artifacts manifest differently across modalities, from blurring and ghosting in Magnetic Resonance Imaging (MRI) to misregistration and quantitative inaccuracies in Positron Emission Tomography/Computed Tomography (PET/CT). Understanding and correcting for these motions is paramount in both clinical and research settings, particularly in drug development where precise image-based biomarkers are essential. Motion can be broadly categorized into rigid body motion, involving simple translation and rotation of a volume, and non-rigid deformation, which includes complex, localized changes in shape [8]. This guide provides a comparative analysis of contemporary motion correction algorithms, detailing their performance, underlying methodologies, and appropriate applications.
Characterizing Motion Types and Artifacts
Rigid Body Motion
Rigid body motion describes the movement of an object where the relative distance between any two points within the object remains unchanged. In the context of head and brain MRI, this is often modeled with six degrees of freedom: translations along the x, y, and z axes, and rotations around these same axes (pitch, roll, yaw) [8] [9]. According to the Fourier shift theorem, such motion induces specific changes in the acquired k-space data: object translation causes a linear phase ramp, while object rotation results in an identical rotation of the k-space data [8]. In images, this typically leads to ghosting artifacts (from periodic motion) or general blurring (from random motion patterns).
Non-Rigid Deformations
Non-rigid deformations involve more complex movements where the object's internal geometry changes. This is common in thoracic and abdominal imaging due to respiratory and cardiac cycles, as well as in soft tissues. These deformations cannot be described by a simple set of global parameters and often require sophisticated models accounting for local displacement fields. The 3D affine motion model, for instance, extends the rigid model to include 12 degrees of freedom, incorporating shearing and scaling in addition to translation and rotation [8]. Artifacts from non-rigid motion are often more diffuse and challenging to correct, leading to regional distortions and inaccurate quantitation.
Comparative Analysis of Motion Correction Algorithms
The performance of motion correction algorithms varies significantly based on the imaging modality, the type of motion, and the specific clinical or research question. The table below provides a structured comparison of several advanced methods.
Table 1: Performance Comparison of Motion Correction Algorithms
| Algorithm Name | Imaging Modality | Correction Type | Reported Performance Metrics | Key Advantages |
|---|---|---|---|---|
| UNet+JE [9] | 3D MRI (MPRAGE) | Hybrid Deep Learning & Joint Estimation | No significant quality difference vs. JE; Median runtime reduction: 2.00-4.05x vs. JE. | Combines robustness of physics-based JE with speed of deep learning; less susceptible to data distribution shifts. |
| SnapShot Freeze 2 (SSF2) [5] | Coronary CT Angiography (CCTA) | Prospective Motion Correction | Overall quality score: 3.67 (vs. 3.0 for STD/SSF1); Best correlation with invasive FFR (r=0.652). | Whole-heart motion correction; improves diagnostic accuracy for stenosis and CT-FFR calculations. |
| Elastic Motion Correction with Deblurring (EMCD) [10] | Oncologic PET/CT (FDG/DOTATATE) | Data-Driven Motion Correction | Lesion SUVmax: ~10.75 (vs. 9.00 for UG); CNR: ~9.0 (vs. 7.89 for UG and 6.31 for BG-OG). | Utilizes all PET counts, improving quantitation (SUVmax, CNR) and lesion detectability without increasing noise. |
| Joint Estimation (JE) [9] | 3D MRI (MPRAGE) | Retrospective Motion Correction | Benchmark for image correction quality; used as a reference for evaluating UNet+JE. | Physics-based model; does not require specialized hardware or pulse sequences. |
Experimental Protocols and Methodologies
Protocol for 3D MRI Motion Correction (UNet+JE vs. JE)
A study evaluating the UNet+JE and JE algorithms utilized T1-weighted 3D MPRAGE scans from healthy participants with both simulated (n=40) and in vivo (n=10) motion corruption [9].
- Data Simulation: Motion corruption was introduced by applying random, piecewise-constant rigid-body motion trajectories to the k-space data of motion-free scans. The motion states, defined by six parameters (3 translations, 3 rotations), were prescribed over segments of the sampling pattern ("shots").
- Algorithm Workflow: The JE method solves a large-scale optimization problem, alternating between estimating the motion-corrected image and the motion trajectory that minimizes data consistency errors between the acquired motion-corrupted k-space and the motion-model-corrected projected data [9]. The UNet+JE hybrid approach integrates a neural network (UNetmag) within the JE framework to provide an initial, rapidly improved image, which accelerates the convergence of the subsequent JE process.
- Performance Evaluation: Image quality was compared using quantitative metrics like Structural Similarity Index (SSIM) and Normalized Root Mean Square Error (NRMSE). Computational runtime was also a key metric.
Protocol for CCTA Motion Correction (SSF2 vs. SSF1)
A retrospective study involved 151 patients who underwent CCTA and invasive coronary angiography (ICA) or FFR within three months [5].
- Image Reconstruction: CCTA images for each patient were processed in three ways: standard iterative reconstruction (STD), with the first-generation motion correction algorithm SSF1, and with the second-generation SSF2.
- SSF1 Methodology: SSF1 tracks and compensates for coronary artery motion using data from three adjacent phases in the same cardiac cycle. It characterizes the motion path to estimate vessel position at a target phase [5].
- SSF2 Methodology: SSF2 extends the motion correction range to encompass the entire heart, providing a more comprehensive correction that improves lumen segmentation [5].
- Performance Evaluation: Image quality was scored by blinded readers. Diagnostic performance for detecting obstructive stenosis (≥50% in left main artery or ≥70% in other vessels) and ischemic lesions (FFR ≤0.8) was assessed against ICA/FFR as a reference. The correlation and consistency between CT-FFR values derived from each method and the invasive FFR were calculated.
Protocol for Oncologic PET/CT Motion Correction (EMCD vs. OG)
A prospective study enrolled 78 adults undergoing standard-of-care FDG or DOTATATE PET/CT [10].
- Image Reconstruction: For each subject, four types of images were reconstructed:
- Ungated (UG): Standard reconstruction without motion correction.
- Belt-Gating Optimal Gate (BG-OG): Reconstruction using only a fraction (typically 33-50%) of PET data corresponding to a specific respiratory phase.
- BG-EMCD: Elastic motion correction using the respiratory signal from a belt.
- DDG-EMCD: Elastic motion correction using a data-driven gating signal extracted from the PET raw data itself.
- EMCD Methodology: Unlike OG, which discards a substantial portion of acquired counts, EMCD utilizes 100% of the PET data. It estimates and corrects for respiratory motion by elastically deforming the image volume, effectively "deblurring" the image without the noise penalty associated with data rejection [10].
- Performance Evaluation: Tracer-avid lesions in the lower chest/upper abdomen were segmented. Quantitative metrics including maximum standardized uptake value (SUVmax) and contrast-to-noise ratio (CNR) were extracted. Two blinded readers independently assessed overall image quality and lesion count.
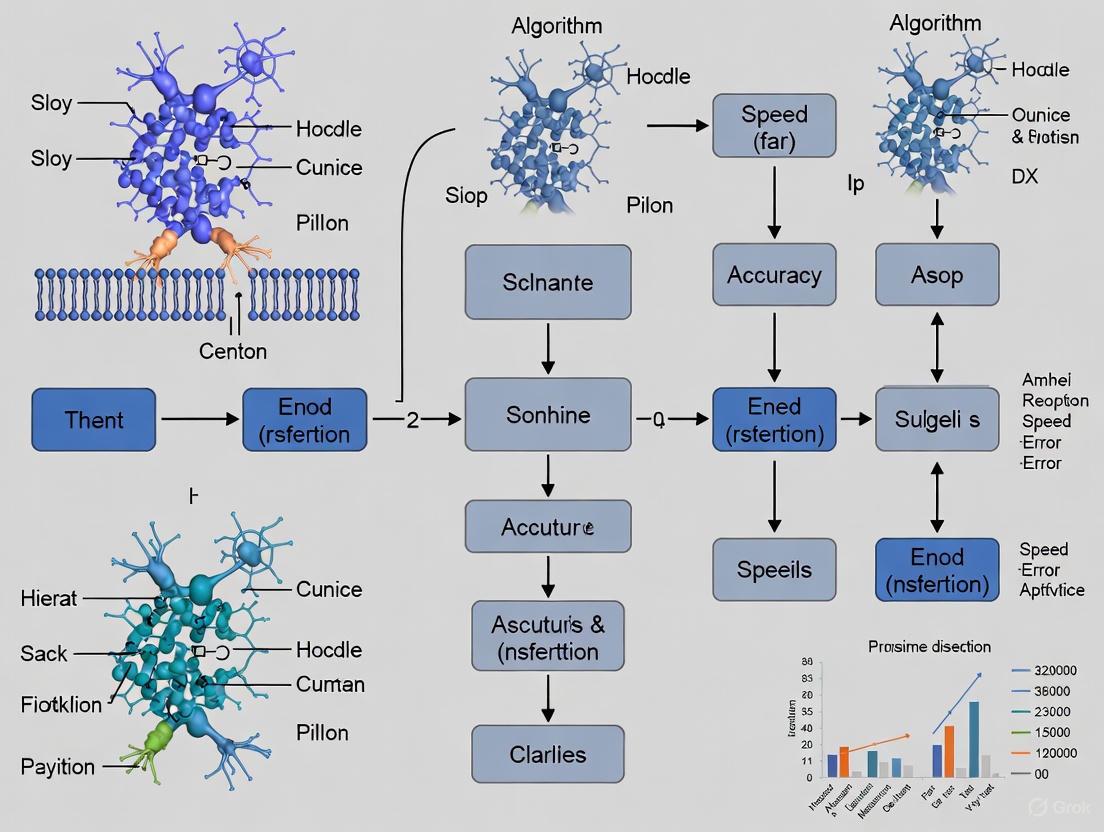
Signaling Pathways and Workflow Visualization
Motion Correction Decision Workflow
Hybrid Deep Learning and Joint Estimation
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Computational Tools for Motion Correction Research
| Item/Tool Name | Function/Application | Relevance in Motion Correction Research |
|---|---|---|
| andi-datasets Python Package [11] | Generation of simulated single-particle trajectories. | Provides ground truth data for developing and benchmarking methods that detect changes in dynamic behavior, such as diffusion coefficient or motion mode. |
| PyMoCo_v2 [9] | Publicly available source code for 3D hybrid DL-JE algorithm. | Enables replication and extension of the UNet+JE method for 3D MRI motion correction; a key tool for algorithmic development. |
| Fractional Brownian Motion (FBM) Model [11] | Simulation of particle trajectories with tunable anomalous diffusion. | Serves as a model to generate realistic biological motion data with controlled parameters for objective method evaluation. |
| Data Consistency Cost Function [9] | Core component of Joint Estimation (JE) algorithms. | A physical model that measures discrepancy between acquired and motion-corrected projected data; drives the optimization in model-based correction. |
| Elastic Motion Correction with Deblurring (EMCD) [10] | Advanced reconstruction for respiratory motion in PET. | A state-of-the-art tool for correcting non-rigid motion in oncologic PET, improving quantitative accuracy and lesion detection. |
Motion artifacts represent a significant challenge in medical imaging, directly compromising the quantitative data essential for research and clinical decision-making. The performance of motion correction algorithms is therefore not merely a technical metric but a fundamental determinant of data fidelity. This guide provides a comparative analysis of contemporary motion correction techniques, framing their performance within a broader thesis on algorithm evaluation. It objectively assesses their impact on quantitative measurements of metabolic activity, blood flow, and tissue micro-architecture across multiple imaging modalities, including Positron Emission Tomography (PET), Computed Tomography (CT), and Magnetic Resonance Imaging (MRI). The analysis is supported by experimental data from recent phantom and human studies, with methodologies and outcomes structured for direct comparison.
Comparative Performance of Motion Correction Algorithms
The following tables synthesize quantitative data from recent studies, enabling a direct comparison of how different motion correction methods affect key analytical measurements.
Table 1: Impact of Motion Correction on Metabolic PET Quantification (Brain Imaging)
| Metric / Parameter | No Motion Correction (NMC) | Post-Reconstruction Registration (PRR) | Frame-Based MC (UMT Frame) | Event-by-Event MC (UMT EBE) |
|---|---|---|---|---|
| Image Quality (Visual) | Noticeable blurring [12] | Mitigated motion blurring [12] | Mitigated motion blurring [12] | Most distinct gyri/sulci depiction [12] |
| TAC Smoothness (Residual SD) | Largest deviation [12] | Large deviations from intraframe motion [12] | Large deviations from intraframe motion [12] | Smoothest TAC; lowest residual SD [12] |
| Quantitative SUV Accuracy (Relative Error) | Not quantified in study | Not quantified in study | SUV~mean~: -2.5% ± 1.7%; SUV~SD~: -8.6% ± 4.7% [13] | SUV~mean~: 0.3% ± 0.8%; SUV~SD~: 1.1% ± 2.5% [13] |
| Motion Estimation Accuracy (MME) | Not Applicable | Not Applicable | 4.8 ± 1.0 mm [13] | 1.3 ± 0.2 mm [13] |
Table 2: Performance in Cardiothoracic and Vascular Imaging
| Metric / Parameter | Standard Reconstruction (STD) | First-Gen MC (SSF1) | Second-Gen MC (SSF2) | Data-Driven Gating + RRA |
|---|---|---|---|---|
| Image Quality Score (Median) | 3.0 [5] | 3.0 [5] | 3.67 [5] | 3.90 ± 0.86 [14] |
| CT-FFR vs. Invasive FFR Correlation (r) | Not reported | 0.795 [5] | 0.887 [5] | Not Applicable |
| Lesion SUV~max~ Change (Δ%) | Not Applicable | Not Applicable | Not Applicable | +3.9% (p < 0.001) [14] |
| Lesion Volume Change (Δ%) | Not Applicable | Not Applicable | Not Applicable | -18.4% (p < 0.001) [14] |
| T1/T2 Map Reconstruction Time | Not Applicable | Not Applicable | Not Applicable | 2.5 hours (Reference) [15] |
| Deep Learning MC Reconstruction Time | Not Applicable | Not Applicable | Not Applicable | 24 seconds [15] |
Detailed Experimental Protocols
To ensure reproducibility and critical assessment, this section outlines the core methodologies from the studies cited in the comparative tables.
Protocol 1: Multi-Tracer Human Brain PET on Ultra-High Performance System
This protocol evaluated motion correction methods for quantifying metabolic and receptor binding parameters.
- Imaging System: Ultra-high performance brain PET system (NeuroEXPLORER) [12].
- Tracers & Subjects: Scans were performed with three tracers:
18F-FE-PE2I(dopamine transporters, n=2),11C-PHNO(dopamine D2/D3 receptors, n=2), and18F-SynVesT-1(SV2A, n=2) [12]. - Motion Tracking: A markerless motion tracking system (United Healthcare UMT) collected motion data at 30 Hz throughout all scans [12].
- Data Reconstruction: List-mode data were reconstructed using Motion-compensation OSEM List-mode Algorithm for Resolution-recovery reconstruction (MOLAR) with 0.8-mm voxels [12].
- Compared Methods:
- NMC: No motion correction.
- PRR: Post-reconstruction registration using FLIRT.
- UMT Frame MC: Frame-based correction using average patient position from UMT data.
- UMT EBE MC: Event-by-event correction using UMT data. Both UMT methods corrected for attenuation mismatch [12].
- Quantitative Analysis: Time-activity curves (TACs) were derived from the AAL template. The standard deviation of the residuals around fitted TACs was computed to measure noise and instability introduced by motion [12].
Protocol 2: Machine Learning-Enhanced Motion Correction in Pediatric PET
This protocol assessed a learning-based method to improve motion estimation in low-count scenarios, crucial for pediatric imaging and dose reduction.
- Imaging System: GE Discovery MI Gen 2 PET/CT scanner [13].
- Data Acquisition: 18F-FDG brain PET in pediatric patients (<21 years old), including a scripted head movement period. List-mode data were down-sampled to simulate 1/9 of the injected dose [13].
- Motion Correction Framework:
- List-mode data were reconstructed into 0.5s frames with 55k (reduced-count) and 500k (full-count) events.
- A patch-based Artificial Neural Network (ANN) was trained to enhance the quality of the reduced-count 55k-event frames.
- Rigid image registration was performed using the reduced-count frames, the ANN-enhanced frames, and the full-count frames to derive three sets of motion vectors [13].
- Outcome Measures:
- Motion Estimation Accuracy: Mean Mesh Error (MME) compared to the full-count reference.
- Image Quality: Normalized Mean Square Error (NMSE) of final reconstructed images.
- Quantitative Accuracy: Relative error in standardized uptake values (SUVs) across 8 brain ROIs [13].
Protocol 3: Motion Correction for CT Fractional Flow Reserve (CT-FFR)
This study validated motion correction algorithms for improving the diagnostic accuracy of coronary CT angiography and derived CT-FFR.
- Study Population: 151 patients who underwent CCTA and invasive coronary angiography/FFR within 3 months [5].
- Image Processing: CCTA images were reconstructed using an iterative technique and then processed with two motion correction algorithms: first-generation (SSF1) and second-generation (SSF2) SnapShot Freeze [5].
- Analysis:
- Image Quality: Scored by radiologists on a 5-point scale.
- Stenosis Assessment: Obstructive stenosis was defined based on diameter stenosis (DS).
- CT-FFR Calculation: Performed on standard, SSF1-, and SSF2-corrected images [5].
- Reference Standard: Invasive FFR ≤ 0.8 or ≥ 90% diameter stenosis was considered an ischemic lesion [5].
Protocol 4: Data-Driven Gating for Lung Cancer PET/CT
This protocol used phantom and patient studies to validate a data-driven gating (DDG) method with a Reconstruct, Register, and Average (RRA) motion correction algorithm.
- Phantom Validation: A motion platform moved a phantom containing spheres (10-28 mm) with varying amplitudes (2-4 cm) and durations (3-5 s). Metrics included SUV~max~, SUV~mean~, volume, and contrast-to-noise ratio (CNR) relative to a static ground truth [14].
- Patient Study: 30 lung cancer patients with 76 lung lesions (<3 cm) were prospectively enrolled [14].
- Comparison: Ungated PET images were compared to RRA motion-corrected PET images.
- Outcome Measures:
- Visual Quality: Scored by two radiologists on a 5-point scale.
- Quantitative Metrics: SUV~max~, SUV~mean~, SUV~peak~, metabolic volume, and CNR of the lung lesions [14].
Visualization of Workflows and Relationships
The following diagrams illustrate the core experimental workflows and conceptual hierarchies derived from the analyzed studies.
Data-Driven Motion Correction Workflow
Motion Correction Algorithm Performance Hierarchy
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Solutions for Motion Correction Research
| Item | Function / Application in Research | Example from Search Results |
|---|---|---|
| 18F-FE-PE2I | PET radiopharmaceutical for imaging dopamine transporters in the brain. [12] | Used in multi-tracer human study on NeuroEXPLORER. [12] |
| 11C-PHNO | PET radiopharmaceutical for imaging dopamine D2/D3 receptors. [12] | Used in multi-tracer human study on NeuroEXPLORER. [12] |
| 18F-SynVesT-1 | PET radiopharmaceutical for imaging synaptic density (SV2A protein). [12] | Used in multi-tracer human study on NeuroEXPLORER. [12] |
| 18F-FDG | PET radiopharmaceutical for measuring glucose metabolism. [13] | Used in pediatric brain PET study for machine learning motion correction. [13] |
| SnapShot Freeze 2 (SSF2) | A second-generation, whole-heart motion correction algorithm for CCTA. [5] | Improved image quality and CT-FFR diagnostic accuracy. [5] |
| MOLAR | Motion-compensation OSEM List-mode Algorithm for Resolution-recovery reconstruction. [12] | Used for reconstruction on the NeuroEXPLORER system. [12] |
| alignedSENSE | A data-driven motion correction algorithm based on the SENSE model for MRI. [16] | Combined with DISORDER trajectory for motion correction in ultra-low-field MRI. [16] |
This guide provides an objective comparison of three fundamental motion correction paradigms used in medical imaging: sinogram-based, image-based, and data-driven approaches. It is designed to assist researchers and scientists in selecting appropriate methodologies for mitigating motion artifacts to ensure data integrity in clinical and research applications.
Motion artifacts present a significant challenge across various medical imaging modalities, including Computed Tomography (CT), Magnetic Resonance Imaging (MRI), and Positron Emission Tomography (PET). These artifacts can degrade image quality, reduce diagnostic value, and lead to inaccurate quantification. This guide systematically compares three core motion correction paradigms—sinogram-based, image-based, and data-driven approaches—by outlining their underlying principles, providing experimental protocols, and presenting quantitative performance data from seminal studies. The objective is to furnish professionals with the necessary information to evaluate and implement these algorithms effectively within their own research and development workflows.
◥ Comparative Analysis of Correction Paradigms
The table below summarizes the core characteristics, strengths, and limitations of the three motion correction paradigms.
Table 1: Fundamental Comparison of Motion Correction Paradigms
| Paradigm | Core Principle | Typical Modalities | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| Sinogram-Based | Corrects or models motion directly in the raw projection data (sinogram) before image reconstruction. | CT, HR-pQCT [17], PET [18] | Addresses the root cause of artifacts; can be highly accurate for rigid motion [17] [18]. | Requires access to raw projection data; motion model may oversimplify complex in-vivo motion [17]. |
| Image-Based | Corrects for motion after image reconstruction by registering and aligning individual image volumes. | fMRI [19], MRI [20], PET | Widely available in software tools (SPM, FSL, AFNI); does not require raw data [19]. | Cannot correct for through-plane motion in 2D sequences or data inconsistencies from spin history effects [20] [19]. |
| Data-Driven | Extracts motion information directly from the acquired imaging data itself without external hardware. | PET [21] [22], NIRS [23] | No additional hardware needed; integrates seamlessly into clinical workflows; enables event-by-event correction [21] [22]. | Performance depends on data statistics and count rates; may miss very slow drifts [21]. |
◥ Sinogram-Based Motion Correction
Sinogram-based approaches operate on the raw projection data acquired by the scanner. A prominent application is the correction of rigid motion in High-Resolution peripheral Quantitative CT (HR-pQCT).
▍ Experimental Protocol: ESWGAN-GP for HR-pQCT
The following workflow was designed to correct for rigid motion artifacts such as cortical bone streaking and trabecular smearing [17].
- Motion Simulation: A motion simulation model applies random in-plane rotations to the 2D object, introducing alterations to the sinogram. The motion-corrupted sinogram is then reconstructed using the Simultaneous Iterative Reconstruction Technique (SIRT) to generate a motion-artifacted image [17].
- Dataset Creation: This process creates a paired dataset consisting of the motion-corrupted image and the original motion-free ground truth image, suitable for supervised learning [17].
- Network Training: An Edge-enhanced Self-attention Wasserstein Generative Adversarial Network with Gradient Penalty (ESWGAN-GP) is trained on the paired dataset.
- Generator: A U-Net architecture incorporates Sobel-kernel-based convolutional layers in its skip connections to enhance and preserve bone microstructure edges.
- Self-Attention: Both generator and discriminator use self-attention mechanisms to capture long-range spatial dependencies.
- Loss Functions: The model employs a composite loss function, including adversarial loss, a VGG-based perceptual loss to reconstruct fine micro-structures, and pixel-wise/total variation loss [17].
- Validation: Performance is quantitatively evaluated on both simulated (source) and real-world (target) datasets using Signal-to-Noise Ratio (SNR), Structural Similarity Index Measure (SSIM), and Visual Information Fidelity (VIF) metrics [17].
▍ Performance Data
Table 2: Quantitative Performance of the ESWGAN-GP Model on HR-pQCT Data
| Dataset | Signal-to-Noise Ratio (SNR) | Structural Similarity (SSIM) | Visual Information Fidelity (VIF) |
|---|---|---|---|
| Simulated (Source) | 26.78 | 0.81 | 0.76 |
| Real-World (Target) | 29.31 | 0.87 | 0.81 |
The following diagram illustrates the experimental workflow for the sinogram-based ESWGAN-GP correction method.
Diagram 1: Sinogram-based ESWGAN-GP motion correction workflow.
◥ Data-Driven Motion Correction
Data-driven methods extract motion information solely from the acquired data. In brain PET, these approaches are crucial for correcting head motion that degrades image resolution and quantitative accuracy.
▍ Experimental Protocol: Centroid of Distribution (COD) in PET
This protocol details a data-driven method for detecting and correcting rigid head motion in list-mode PET data [21].
- Data Acquisition: A dynamic PET scan is acquired in list-mode format, where each detected event is recorded with its time stamp and line-of-response (LOR) coordinates.
- Motion Detection - COD Trace Generation:
- The central coordinates (Xi, Yi, Zi) of each event's LOR are calculated.
- These coordinates are averaged over short time intervals (e.g., 1 second) to generate raw COD traces for lateral (CX), anterior-posterior (CY), and superior-inferior (CZ) directions [21].
- Motion Detection - Time Point Identification:
- The COD direction with the highest variance after injection is selected for motion detection, denoted C(t).
- A median filter is applied to C(t) to create a smoothed trace M(t).
- The forward difference D(t) = M(t + Δt) - M(t) is calculated. Time points (t~i~) where D(t) exceeds a user-defined threshold are flagged as motion events.
- Additional motion time points can be added manually via visual assessment to capture slower drifts [21].
- Motion-Compensated Reconstruction:
- The list of motion time points divides the acquisition into motion-free frames (MFFs).
- Each MFF is reconstructed without attenuation correction and rigidly registered to a reference frame.
- The resulting transformation matrices are applied to perform a final motion-compensated reconstruction of the entire dataset [21].
▍ Performance Data
Table 3: Quantitative Impact of Data-Driven Motion Correction on PET SUV
| Motion Correction Method | ¹⁸F-FDG SUV Difference vs. HMT | ¹¹C-UCB-J SUV Difference vs. HMT |
|---|---|---|
| No Motion Correction (NMC) | -15.7% ± 12.2% | -20.5% ± 15.8% |
| Frame-Based Image Registration (FIR) | -4.7% ± 6.9% | -6.2% ± 11.0% |
| Data-Driven COD Method | 1.0% ± 3.2% | 3.7% ± 5.4% |
HMT: Hardware-based Motion Tracking (Gold Standard). Data presented as mean ± SD [21].
◥ Image-Based Motion Correction
Image-based correction is one of the most common strategies, particularly in fMRI and MRI, where it is applied to reconstructed image volumes.
▍ Experimental Protocol: Prospective Motion Correction (PROMO) in MRI
The PROMO framework prospectively corrects for motion during the MRI scan itself, preventing artifacts from occurring [20].
- Navigator Acquisition: Three orthogonal, low flip-angle, thick-slice, single-shot spiral acquisitions (SP-Navs) are played out during the intrinsic longitudinal recovery time (e.g., T1 recovery) of the main pulse sequence. These are acquired in the axial, sagittal, and coronal planes [20].
- Real-Time Processing: Each SP-Nav is immediately reconstructed into a low-resolution image.
- Motion Tracking: The reconstructed SP-Nav images are fed as input to an Extended Kalman Filter (EKF) algorithm. The EKF performs recursive state estimation to track the 3D rigid-body motion of the head in real-time [20].
- Prospective Correction: The estimated motion parameters are fed back to the scanner's pulse sequence in real-time. The coordinate system for all subsequent RF pulses and gradient fields is updated to remain fixed relative to the patient's head, effectively negating the motion [20].
The diagram below illustrates this real-time feedback loop.
Diagram 2: Prospective motion correction (PROMO) real-time feedback loop in MRI.
▍ Performance Data
A comparative study of image-based motion correction tools in fMRI evaluated packages including AFNI, AIR, BrainVoyager, FSL, and SPM2. The study used both phantom data with known motion and human fMRI data.
- Motion Estimation Accuracy: In phantom studies, AFNI and SPM2 yielded the most accurate motion estimation parameters [19].
- Computational Efficiency: AFNI was found to be the fastest package among those tested [19].
- Impact on Activation Detection: In human data, all packages provided significant benefits, with motion correction improving the magnitude of detected activations by up to 20% and the cluster size by up to 100%. However, no single software package produced dramatically better activation results than the others, indicating that the choice of tool may be less critical than the decision to apply motion correction in the first place [19].
◥ The Scientist's Toolkit
The table below lists key software tools and algorithms essential for implementing the motion correction paradigms discussed in this guide.
Table 4: Essential Research Reagents and Tools for Motion Correction
| Tool / Algorithm Name | Paradigm | Primary Modality | Function and Application |
|---|---|---|---|
| ESWGAN-GP [17] | Sinogram-Based | HR-pQCT/CT | A deep learning network for correcting rigid motion artifacts; uses edge-enhancement and self-attention to preserve bone micro-structures. |
| Centroid of Distribution (COD) [21] | Data-Driven | PET | A data-driven algorithm that detects head motion from changes in the center of distribution of PET list-mode events, enabling event-by-event correction. |
| PROMO (SP-Nav/EKF) [20] | Image-Based / Prospective | MRI | An image-based framework using spiral navigators and an Extended Kalman Filter for real-time prospective motion correction in high-resolution 3D MRI. |
| AFNI [19] | Image-Based | fMRI | A software suite offering fast and accurate volume registration for motion correction of BOLD fMRI time series data. |
| SPM2 [19] | Image-Based | fMRI | A widely used software package for processing brain imaging data, including robust motion correction algorithms for fMRI. |
| FSL [19] | Image-Based | fMRI | FMRIB's Software Library containing tools for fMRI analysis, such as the MCFLIRT tool for rigid-body motion correction. |
Algorithmic Approaches: From Deep Learning to Model-Based Correction Methods
This guide provides an objective comparison of three deep learning architectures—ESWGAN-GP, 3D-ResNet, and Self-Attention Mechanisms—for motion correction in medical imaging, a critical step for ensuring data quality in drug development and clinical research.
Performance Comparison at a Glance
The table below summarizes the quantitative performance of the featured architectures across different medical imaging applications.
| Architecture | Application & Task | Key Performance Metrics | Reported Performance | Inference Speed |
|---|---|---|---|---|
| ESWGAN-GP (Edge-enhanced Self-attention WGAN-GP) | HR-pQCT Bone Imaging; Motion artifact correction [17] [24] | Structural Similarity Index Measure (SSIM)Signal-to-Noise Ratio (SNR)Visual Information Fidelity (VIF) | SSIM: 0.81 (Simulated), 0.87 (Real-world) [24]SNR: 26.78 (Simulated), 29.31 (Real-world) [24] | Information missing |
| 3D-ResNet with Positional Encodings | 13N-ammonia PET-MPI; Frame-by-frame motion correction [25] | Lin’s Concordance CorrelationBland-Altman Limits of Agreement (MBF) | MBF Concordance: 0.9938 [25]Agreement: -0.28 to 0.21 [mL/g/min] (Mean diff: -0.03) [25] | <1 second per study [25] |
| 3D-ResNet | 18F-flurpiridaz PET-MPI; Frame-by-frame motion correction [26] | Area Under the Curve (AUC) for CAD detectionBland-Altman Limits of Agreement (MBF) | AUC for Stress MBF: 0.897 [26]Agreement: ± 0.24 mL/g/min (Mean diff: 0.00) [26] | Significantly faster than manual [26] |
| Self-Attention Model | fMRI; Slice-to-volume registration [27] | Euclidean Distance (Target Registration Error)Registration Speed | Euclidean Distance: 0.93 mm [27]Registration Speed: 0.096 s [27] | 0.096 seconds (vs. 1.17s for conventional) [27] |
Detailed Experimental Protocols and Methodologies
ESWGAN-GP for HR-pQCT Motion Correction
The ESWGAN-GP framework was designed to correct rigid-motion artifacts like cortical bone streaking and trabecular smearing in high-resolution peripheral quantitative computed tomography (HR-pQCT) [17] [24].
- Data Preparation: A motion simulation model was first used to create paired datasets. This model applied random in-plane rotations to the 2D object being imaged, introducing alterations in the sinogram data. These corrupted sinograms were then reconstructed using the Simultaneous Iterative Reconstruction Technique (SIRT) to generate motion-corrupted images, with the original images serving as the ground truth [24].
- Network Architecture: The model uses a U-Net shaped generator within a Wasserstein GAN with Gradient Penalty (WGAN-GP) backbone for stable training. Key enhancements include [17] [24]:
- Sobel-kernel-based CNN (SCNN): Integrated into skip connections to enhance and preserve trabecular bone edges.
- Self-attention mechanisms: Incorporated in both generator and discriminator to capture long-range spatial dependencies across the image.
- Loss Functions: The model employs a combination of adversarial loss from the WGAN-GP, a VGG-based perceptual loss to reconstruct fine micro-structural features, and for one variant (ESWGAN-GPv1), pixel-wise L1 loss and Total Variation (TV) loss for smoother outputs [17] [24].
3D-ResNet for PET Motion Correction
This architecture addresses frame-by-frame motion in dynamic positron emission tomography (PET) studies, such as those for myocardial perfusion imaging (MPI) with 18F-flurpiridaz or 13N-ammonia [26] [25].
- Data and Ground Truth: The models were trained on multi-site clinical trial data. For each patient study, an experienced operator performed manual frame-by-frame motion correction, and the resulting motion vectors were used as the ground truth [26] [25].
- Network Architecture and Training: The core of the model is a 3D ResNet-based architecture that takes 3D PET volumes as input and outputs motion vectors (tx, ty, tz) representing the translation needed for correction [26] [25].
- Positional Embeddings: In the version for 13N-ammonia, positional encodings were added to provide the model with contextual information about the temporal order of the frames [25].
- Training and Validation: The network was trained to minimize the error between its predicted motion vectors and the ground-truth vectors from manual correction. Robustness was enhanced through data augmentation using simulated motion vectors, and performance was validated via external cross-validation across different clinical sites [26] [25].
Self-Attention for fMRI Slice-to-Volume Registration
This model performs retrospective, slice-level motion correction for functional MRI (fMRI) by registering 2D slices to a 3D reference volume [27].
- Data and Simulation: The model was trained on the publicly available Healthy Brain Network (HBN) dataset. To simulate motion, a wide range of rigid transformations were applied to reference volumes. Slices were then sampled according to a standard acquisition protocol to generate a large dataset of 3D volume-2D slice pairs for training and evaluation [27].
- Network Architecture: The model uses independent encoders for the 2D slice and the 3D reference volume. The core innovation is a self-attention mechanism that assigns a pixel-wise score to each slice. This allows the model to weight the relevance of different slices and focus on the most reliable features for registration, thereby enhancing robustness against input uncertainty and variation [27].
The Scientist's Toolkit: Essential Research Reagents & Materials
The table below lists key computational tools and data components essential for developing motion correction algorithms in this field.
| Item Name | Function / Application | Specific Example / Note |
|---|---|---|
| WGAN-GP (Wasserstein GAN with Gradient Penalty) | Stable training of generative models for tasks like image-to-image translation and artifact correction [17] [24]. | Used as the backbone for ESWGAN-GP; replaces discriminator with a critic, uses Wasserstein distance and gradient penalty for stability [17]. |
| Sobel-Kernel-based CNN (SCNN) | Edge enhancement and preservation in generated images [17] [24]. | Integrated into the U-Net skip connections of the ESWGAN-GP generator to preserve trabecular bone edges [17]. |
| VGG-based Perceptual Loss | Improves reconstruction of high-level, perceptually relevant features and micro-structures [17] [24]. | Used in ESWGAN-GP to complement adversarial and pixel-wise losses [17]. |
| 3D ResNet Architecture | Spatiotemporal feature extraction from 3D volumetric data (e.g., dynamic PET) [26] [25]. | Core network for mapping 3D PET volumes to rigid motion vectors [26]. |
| Positional Encodings/Embeddings | Provides model with contextual information about temporal or spatial order [25]. | Added to 3D-ResNet to inform the model about the frame sequence in dynamic PET [25]. |
| Self-Attention Mechanism | Captures long-range dependencies and spatial relationships in data [17] [27]. | Used in ESWGAN-GP for global features and in fMRI SVR for scoring slice relevance [17] [27]. |
| Paired Dataset (Motion-Corrupted & Ground Truth) | Essential for supervised training of motion correction networks [17] [24]. | Created via sinogram simulation for HR-pQCT [17]; from manual expert correction for PET [26]. |
Workflow and Architecture Diagrams
ESWGAN-GP for Motion Correction
3D-ResNet for PET Motion Correction
Self-Attention for Slice-to-Volume Registration
Generative Adversarial Networks for Motion Artifact Reduction and Image Synthesis
Motion artifacts represent a prevalent source of image degradation in medical imaging, particularly in modalities requiring longer acquisition times such as magnetic resonance imaging (MRI) and positron emission tomography (PET). These artifacts arise from both voluntary and involuntary patient movement during scanning, manifesting as blurring, ghosting, or streaking in reconstructed images. In MRI, motion alters the static magnetic field, induces susceptibility artifacts, affects spin history leading to signal loss, and causes inconsistencies in k-space sampling that violate Nyquist criteria [28]. The clinical impact is substantial, with an estimated 15-20% of neuroimaging exams requiring repeat acquisitions, potentially incurring additional annual costs exceeding $300,000 per scanner [28].
Motion correction strategies are broadly classified into two categories: prospective and retrospective methods. Prospective motion correction occurs during image acquisition through techniques like external optical tracking systems, physiologic gating, or sequence-embedded navigators [28]. While effective, these approaches often require hardware modifications, rigid coupling of sensors to anatomy, or increased sequence complexity, limiting their clinical applicability. In contrast, retrospective motion correction operates on already-acquired data without requiring additional hardware, using computational approaches to mitigate artifacts [28]. Recent advances in deep learning, particularly generative adversarial networks (GANs), have revolutionized retrospective correction by learning direct mappings between corrupted and clean images, often yielding improved perceptual quality and reduced reconstruction time compared to conventional iterative algorithms.
Performance Comparison of Motion Correction Algorithms
Quantitative Performance Metrics Across Modalities
Table 1: Performance Comparison of Motion Correction Algorithms in Medical Imaging
| Imaging Modality | Correction Method | Network Architecture | Performance Metrics | Reference |
|---|---|---|---|---|
| Head MRI (T2-weighted) | CGAN | Generator: Autoencoder with Residual blocks & SE; Discriminator: Sequential CNN | SSIM: 0.9+, PSNR: >29 dB | [29] |
| Fetal MRI | GAN with Autoencoder | Generator: Autoencoder with Residual blocks & SE; Discriminator: Sequential CNN | SSIM: 93.7%, PSNR: 33.5 dB | [30] |
| Brain PET (NeuroEXPLORER) | Event-by-event motion correction | MOLAR reconstruction with UMT tracking | Lowest residual SD in TACs | [12] |
| mGRE MRI | LEARN-IMG, LEARN-BIO | Convolutional Neural Networks | Significant artifact reduction, detail preservation | [31] |
| Lung Cancer PET/CT | Data-driven gating with RRA | N/A | SUVmax: +3.9%, Volume: -18.4% | [14] |
| Cone-beam CT | DLME with TriForceNet | Sequential Hybrid Transformer-CNN | Superior to unsupervised and supervised benchmarks | [32] |
Comparative Effectiveness Across Correction Approaches
The quantitative data reveals distinct performance patterns across motion correction approaches. For GAN-based methods applied to MRI, structural similarity index (SSIM) values consistently exceed 0.9, with peak signal-to-noise ratio (PSNR) reaching 33.5 dB in fetal MRI applications [29] [30]. These metrics indicate excellent preservation of structural information and noise reduction capabilities. In PET imaging, event-by-event motion correction using external tracking systems demonstrates superior performance compared to frame-based methods, effectively addressing intraframe motion and achieving the lowest standard deviation in time-activity curves [12]. Data-driven gating approaches in lung cancer PET/CT show substantial improvements in quantification accuracy, with lesion volume reduction of 18.4% and increased standardized uptake values [14].
Notably, GAN-based methods outperform traditional approaches like BM3D, RED-Net, and non-local means filtering across multiple evaluation metrics [30]. The integration of hybrid architectures, such as sequential transformer-CNN designs in cone-beam CT, further extends performance gains by leveraging both local pattern recognition and global dependency modeling [32]. This consistent outperformance highlights the transformative potential of deep learning approaches, particularly GANs, in motion artifact reduction across diverse imaging modalities and anatomical regions.
Experimental Protocols and Methodologies
GAN Architecture Design and Implementation
Table 2: Key Architectural Components in GAN-based Motion Correction
| Component | Variants | Function | Application Examples |
|---|---|---|---|
| Generator | U-Net, Autoencoder with Residual blocks, Encoder-Decoder | Transforms motion-corrupted input to corrected output | Fetal MRI [30], Head MRI [29] |
| Discriminator | Sequential CNN, PatchGAN | Distinguishes between corrected and motion-free images | Head MRI [29], PET/MRI synthesis [33] |
| Loss Functions | WGAN, L1, Perceptual, Combined losses | Guides network training through multiple constraints | Fetal MRI (WGAN + L1 + perceptual) [30] |
| Conditional Input | cGAN, bi-c-GAN | Incorporates additional data to guide generation | Multi-contrast MRI [33] |
| Training Framework | Supervised, Unsupervised, Cycle-consistent | Determines data requirements and training approach | CBCT (unsupervised) [32] |
Dataset Preparation and Training Protocols
Experimental protocols for GAN-based motion correction consistently emphasize rigorous dataset preparation. For head MRI applications, datasets typically comprise thousands of image pairs (5,500 in one study) with simulated motion artifacts generated through Fourier transform modifications of k-space data [29]. These simulations incorporate both translational and rotational motions, with artifacts aligned to phase-encoding directions. Training-validation-test splits generally follow 90%-5%-5% distributions, with pixel value normalization to (0,1) or (0,255) ranges [29].
In fetal MRI implementations, networks are trained on synthetic motion artifacts created through random k-space modifications, with validation on real motion-affected clinical images [30]. This approach addresses the challenge of obtaining paired motion-corrupted and motion-free clinical data. For multi-modal applications like PET/MRI synthesis, bi-task architectures with shared latent representations enable synergistic learning from complementary data sources [33]. Training typically employs combined loss functions incorporating adversarial, structural (SSIM), and intensity (L1/L2) components to balance perceptual quality with quantitative accuracy [30] [33].
Advanced implementations incorporate specialized training strategies. The sequential hybrid transformer-CNN (SeqHTC) in TriForceNet for cone-beam CT combines local feature extraction with global relationship modeling [32]. Multi-resolution heatmap learning and auxiliary segmentation heads further enhance landmark detection accuracy, enabling precise motion parameter estimation without external markers or motion-free references [32].
Diagram 1: Experimental workflow for GAN-based motion artifact reduction, showing the iterative process from data preparation to model evaluation.
GAN Architectures for Motion Correction
Core Architectural Components and Variations
Generative adversarial networks for motion artifact reduction typically employ encoder-decoder architectures with specialized components tailored to medical imaging challenges. The generator commonly utilizes U-Net or autoencoder structures with skip connections to preserve fine anatomical details [29] [30]. Advanced implementations incorporate residual blocks with squeeze-and-excitation (SE) modules to enhance feature representation and gradient flow [30]. The discriminator typically employs convolutional neural networks, with PatchGAN architectures providing localized discrimination to preserve high-frequency details [29].
Conditional GANs (cGANs) represent a significant advancement, enabling controlled generation through additional input channels. In motion correction, cGANs utilize motion-corrupted images as inputs with motion-free images as targets, learning the specific transformation between these states [29]. For multi-modal applications, bi-c-GAN architectures process complementary inputs like ultra-low-dose PET and T1-weighted MRI to synthesize high-quality PET images, leveraging shared latent representations between tasks [33]. This approach demonstrates the capability of GANs to integrate heterogeneous data sources for enhanced artifact reduction.
Loss Function Design and Optimization
Loss function design critically influences GAN performance in medical applications. Standard approaches combine multiple loss components: adversarial loss (Wasserstein GAN or standard GAN) for realistic output generation; pixel-wise loss (L1 or L2) for intensity fidelity; and perceptual loss for structural preservation [30]. The adversarial component encourages output distributions matching motion-free images, while pixel-wise constraints maintain quantitative accuracy essential for diagnostic applications.
In fetal MRI implementations, weighted combinations of WGAN, L1, and perceptual losses have demonstrated superior performance compared to single-loss alternatives [30]. For multi-modal synthesis, combined losses incorporating mean absolute error, structural similarity, and bias terms effectively balance intensity accuracy with structural preservation [33]. These sophisticated loss functions enable GANs to overcome limitations of conventional approaches, which often produce overly smooth outputs lacking visual authenticity [29].
Diagram 2: GAN architecture for motion artifact reduction showing the adversarial training process between generator and discriminator networks.
Critical Datasets and Software Frameworks
Table 3: Essential Research Resources for GAN-based Motion Correction Studies
| Resource Category | Specific Examples | Application Context | Function in Research |
|---|---|---|---|
| Public Datasets | XCAT, CQ500, VSD full body | CBCT motion correction [32] | Provide standardized evaluation benchmarks |
| Simulation Tools | K-space modification, Fourier transform | MRI motion artifact simulation [29] | Generate training data with controlled artifacts |
| Deep Learning Frameworks | TensorFlow, PyTorch | Network implementation [29] [30] | Enable model development and training |
| Evaluation Metrics | SSIM, PSNR, NRMSE, CNR | Quantitative performance assessment [29] [30] | Provide objective comparison of correction efficacy |
| Motion Tracking Systems | United Healthcare Motion Tracking (UMT) | PET motion correction [12] | Provide ground truth motion data |
Successful implementation of GAN-based motion correction requires careful consideration of computational resources and implementation details. Training typically demands GPU acceleration, with memory requirements scaling with image resolution and batch size. For high-resolution applications, specialized approaches like Diffusion-4K with Scale Consistent Variational Auto-Encoders and wavelet-based latent fine-tuning enable efficient 4K image processing [34]. Data preprocessing pipelines must accommodate domain-specific requirements, including k-space manipulation for MRI [29] [30], sinogram processing for CT [32], and list-mode event handling for PET [12].
Hyperparameter optimization remains challenging, with learning rates, batch sizes, and network depth requiring careful tuning for specific applications. Benchmark studies indicate that GAN-based frameworks like Pix2Pix can outperform diffusion models and flow matching techniques in terms of structural fidelity, image quality, and computational efficiency for certain medical image translation tasks [35]. However, architectural choices must balance computational complexity with performance, particularly for clinical deployment where inference speed may be critical.
Future Directions and Research Challenges
Despite significant advances, GAN-based motion correction faces several persistent challenges. Limited generalizability across scanner platforms, imaging protocols, and patient populations remains a concern [28]. Many approaches rely on paired training data (motion-corrupted and motion-free images from the same subject), which is difficult to obtain in clinical practice [28] [32]. There is also risk of introducing visually plausible but anatomically inaccurate features through over-aggressive correction [28].
Future research directions focus on addressing these limitations through improved data augmentation, unsupervised learning techniques, and domain adaptation methods. For cone-beam CT, unsupervised approaches like Dynamic Landmark Motion Estimation (DLME) eliminate the need for motion-free references by leveraging anatomical landmarks and geometric constraints [32]. In MRI, continued development of comprehensive public datasets and standardized reporting protocols for artifact levels will facilitate more rigorous benchmarking [28]. Architectural innovations, particularly the integration of transformer components with convolutional networks, show promise for capturing long-range dependencies relevant to complex motion patterns [32].
As generative models continue evolving, their application to motion artifact reduction will likely expand beyond simple artifact removal to include integrated acquisition-reconstruction frameworks capable of jointly optimizing data collection and image formation. These advances hold potential to substantially enhance diagnostic accuracy, reduce healthcare costs, and improve patient experience by minimizing repeated scans.
Cone beam computed tomography (CBCT) is an essential imaging tool for patient positioning verification in radiotherapy and for guidance during interventional procedures [36] [37]. However, a significant challenge in acquiring high-quality CBCT images is the degradation caused by physiological motion from breathing, bowel activity, or patient movement [36]. These motion artifacts manifest as blurs or streaks in reconstructed images, compromising diagnostic accuracy and treatment precision [32]. Conventional motion mitigation strategies, such as gating techniques, often assume periodic motion and are consequently restricted to regular respiratory patterns, failing to address irregular, a-periodic motion [36]. This limitation has driven the development of advanced, gate-less reconstruction frameworks capable of correcting for both periodic and non-periodic motion without relying on surrogate signals or extended acquisitions.
Experimental Protocols and Methodologies
The CBCT-MOTUS Framework: Core Protocol
The CBCT-MOTUS framework operates on a joint reconstruction principle, simultaneously estimating both the underlying image and the motion-fields. The methodology can be broken down into several key stages [36]:
- Initialization: The process begins with a motion-corrupted image volume, reconstructed from acquired projections without any motion compensation. This initial volume serves as the reference image ( x_0 ).
- Signal Model: The acquired projection data are modeled as line integrals. The relationship between the reference image, the motion-fields, and the measured projections is formalized as: ( yt = At x0[Dt(r)] ) where ( yt ) is the integral signal at time ( t ), ( At ) is the system matrix, ( x0 ) is the reference image, and ( Dt ) is the motion-field that deforms ( x_0 ) to match the object's state at time ( t ) [36].
- Alternating Optimization: The framework iteratively alternates between two steps until convergence:
- Motion Estimation: Motion-fields are estimated directly in the projection space by comparing the acquired projections with simulated projections generated from the motion-deformed reference image. This model-based approach ensures consistency with the raw measurement data.
- Image Correction: The estimated motion-fields are used to compensate for the motion in the image volume, producing an updated, motion-corrected reference image.
- Motion Model Parameterization: To render the high-dimensional motion estimation problem tractable, CBCT-MOTUS incorporates several a priori assumptions:
- B-spline Compression: Motion-fields are compressed using B-spline parameterization, drastically reducing the number of parameters to be estimated [36].
- Low-Rank Model: The spatio-temporal correlation of motion is exploited using a low-rank motion model [36].
- Spatial Regularization: Smoothness of the motion-fields is enforced to include physiological knowledge [36].
This protocol has been validated on in silico datasets, physical phantoms, and clinical in vivo acquisitions, demonstrating its capability to correct for non-rigid motion with a high temporal resolution of 182 ms per projection [36] [38].
Comparator Algorithm Protocols
CAVAREC with Automated Bone Removal (C+Z)
CAVAREC is an iterative motion-compensated reconstruction algorithm designed for clinical CBCT data. Its experimental protocol is as follows [37]:
- Motion Estimation: The algorithm estimates the motion of each projection image relative to a sparse reference image. This reference image is created from the motion-corrupted initial reconstruction by applying a windowing function to focus the motion compensation on high-intensity structures like contrast-enhanced vessels.
- Bone Removal Integration: The proprietary deep-learning algorithm ZIBOS performs automated bone segmentation and removal. By eliminating high-contrast bones from the initial reconstruction, the subsequent windowing in CAVAREC primarily leaves vessels, thereby focusing the motion compensation more effectively on the vasculature of interest [37].
- Validation: A two-center study evaluated this approach on 48 clinical liver CBCTs, using both quantitative vessel sharpness measurements and qualitative reader studies by interventional radiologists for assessment [37].
Dynamic Landmark Motion Estimation (DLME)
DLME is an unsupervised method that relies on anatomical landmark detection rather than external markers or motion-free references [32]:
- Landmark Detection: The core of this method is TriForceNet, a deep learning framework for detecting anatomical landmarks in 2D projection images. It integrates a sequential hybrid transformer-CNN (SeqHTC) encoder, multiresolution heatmap learning, and a multitask learning strategy with an auxiliary segmentation head.
- Motion Estimation: The DLME algorithm uses the geometric relationships between landmarks across different projection views to estimate motion parameters. It incorporates constraints to mitigate high-frequency noise from landmark detection errors and to ensure physically plausible motion trajectories [32].
- Validation: Experiments were conducted on the numerical XCAT phantom, the clinical CQ500 dataset, and the VSD full body dataset, comparing its performance against both unsupervised and supervised motion artifact reduction methods [32].
Performance Data and Comparative Analysis
Quantitative Performance Metrics
The following table summarizes key quantitative findings from evaluations of the discussed motion correction algorithms.
Table 1: Quantitative Performance Comparison of Motion Correction Algorithms
| Algorithm | Temporal Resolution | Key Quantitative Outcome | Validation Dataset |
|---|---|---|---|
| CBCT-MOTUS [36] | 182 ms/projection | Improved image features, reduction of motion artifacts, and deblurring of organ interfaces. | In silico, phantom, clinical in vivo |
| CAVAREC [37] | Not specified | Vessel sharpness: 0.287 (±0.04), a significant improvement (P=0.02) over uncorrected images (0.281±0.04). | 48 clinical liver CBCTs |
| CAVAREC + ZIBOS (C+Z) [37] | Not specified | Vessel sharpness: 0.284 (±0.04), not significantly different from CAVAREC alone (P>0.05). | 48 clinical liver CBCTs |
| DLME (with TriForceNet) [32] | Not specified | Outperformed traditional unsupervised motion compensation techniques and surpassed supervised, image-based motion artifact reduction methods. | XCAT, CQ500, VSD full body |
Qualitative Clinical Evaluation
In the clinical reader study for CAVAREC, both the algorithm alone and combined with bone removal (C+Z) demonstrated significant qualitative improvements over uncorrected images [37]:
- Overall Image Quality: Scored on a 0-100 scale, both CAVAREC and C+Z significantly improved the mean score from 45 (±14) for uncorrected images to 53 (CAVAREC: ±16; C+Z: ±17), with P < 0.001 [37].
- Specific Image Features: On a scale of -50 to +50 relative to uncorrected images, readers showed a mean preference of +4.3 to +9.5 for CAVAREC and C+Z across parameters like large vessels, small vessels, vessel sharpness, and streak artifacts (P < 0.001). Improvement for tumor blush was not statistically significant [37].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents and Computational Tools in CBCT Motion Correction
| Item / Solution | Function / Application in Research |
|---|---|
| B-spline Parameterization | Compresses the high-dimensional motion-field data, reducing the number of parameters to be estimated in model-based frameworks like CBCT-MOTUS [36]. |
| Low-Rank Motion Model | Exploits the inherent spatio-temporal correlations in physiological motion, providing a compact representation for efficient computation [36]. |
| Spatial Regularizer | Enforces smoothness in the estimated motion-fields, incorporating a priori knowledge that physical motion is typically continuous and non-abrupt [36]. |
| Deep Learning Landmark Detector (TriForceNet) | Accurately identifies anatomical landmarks in 2D projection images, providing the essential input for unsupervised motion estimation methods like DLME [32]. |
| Sequential Hybrid Transformer-CNN (SeqHTC) | An encoder architecture that combines the local feature extraction power of CNNs with the global context understanding of transformers, improving landmark detection accuracy [32]. |
| Sparse Reference Image | Used in algorithms like CAVAREC; a windowed version of the initial reconstruction that highlights high-contrast structures to guide the motion estimation process [37]. |
| Automated Bone Segmentation (ZIBOS) | A deep-learning-based tool to remove bone structures from reconstructions, potentially focusing motion correction algorithms on soft-tissue vasculature [37]. |
Workflow and Algorithmic Relationships
The following diagram illustrates the core iterative workflow of the CBCT-MOTUS framework.
The diagram below maps the taxonomic relationships between different algorithmic approaches to the motion correction problem in CBCT, highlighting the position of CBCT-MOTUS.
The comparative analysis of gate-less motion correction frameworks reveals distinct advantages and potential applications for each approach. CBCT-MOTUS represents a principled, model-based approach that achieves high temporal resolution and effectively handles both periodic and irregular, non-rigid motion without external surrogates [36]. Its strength lies in its direct physical model and data consistency, providing a transparent and understandable correction process. The CAVAREC algorithm, particularly in a clinical interventional setting, demonstrates significant and reliable improvement in image quality for hepatic vasculature visualization, with the added finding that automated bone removal does not degrade this performance [37]. This integration can be streamlined into clinical workflows. The DLME method offers a powerful alternative by leveraging advanced deep learning for landmark detection, eliminating the need for paired motion-free data and avoiding the marker-based methods' logistical hurdles [32].
In conclusion, the evolution of motion correction in CBCT is advancing toward more flexible, gate-less frameworks that can cope with the complexities of physiological motion. CBCT-MOTUS, with its foundation in low-rank motion models and model-based reconstruction, establishes a strong benchmark for performance, particularly in applications requiring high temporal fidelity and correction of a-periodic motion. The ongoing integration of deep learning components, as seen in landmark detection and bone removal, promises to further enhance the robustness and clinical applicability of these technologies, ultimately improving the precision of radiotherapy and interventional oncology procedures.
This guide provides an objective comparison of traditional signal processing techniques—Wavelet Transform, Principal Component Analysis, and Correlation-Based Methods—framed within research on motion correction algorithms. The performance data and methodologies summarized are crucial for researchers and scientists selecting appropriate techniques for medical imaging and signal processing applications.
Experimental Performance Comparison
The following tables summarize quantitative performance data for the featured techniques from controlled experiments.
Table 1: Performance in Lightning Stroke Classification on Transmission Lines [39]
| Technique | Key Advantage | Key Limitation | Classification Accuracy with ANN | Key Metric Performance |
|---|---|---|---|---|
| Principal Component Analysis (PCA) | Extracts optimal mother functions automatically; Overcomes mother wavelet selection challenge [39] | Assumes orthogonal relationship between signal and artifact, which is often incorrect [40] | Better results than Wavelet Transform [39] | Improved several characteristics over WT [39] |
| Wavelet Transform (WT) | Effective for analyzing non-stationary signals with transients [39] | Performance highly dependent on manual selection of mother wavelet and decomposition level [39] [40] | Acceptable performance [39] | Performance reliant on correct mother function selection [39] |
Table 2: Performance in EEG Eye-Blink Artifact Removal [40]
| Technique | Key Advantage | Key Limitation | NRMSE | PSNR | Correlation Coefficient (ρ) |
|---|---|---|---|---|---|
| Proposed ASWT (Automatic Stationary WT) | Low complexity; automatic level selection; suitable for real-time processing [40] | Requires selection of mother wavelet [40] | Smaller [40] | Larger [40] | Larger [40] |
| AWICA & Enhanced AWICA | Automatic; combines BSS and WT advantages [40] | Computationally expensive; performance sensitive to 5 pre-set parameters [40] | Larger [40] | Smaller [40] | Smaller [40] |
Table 3: Performance in Neuronal Cell Isolation [41]
| Technique | Key Advantage | Key Limitation | Best Performing Configuration | Clustering Quality (L-ratio & Isolation Distance) |
|---|---|---|---|---|
| WT + PCA | Powerful denoising and feature extraction; improves single-unit isolation [41] | Mother wavelet selection strongly influences results [41] | Daubechies 4 mother wavelet with Minimax thresholding scheme [41] | Improved with correct mother wavelet [41] |
Detailed Experimental Protocols
This experiment assessed the ability of PCA and WT to classify lightning strokes that either cause faults or do not on transmission lines.
- Data Collection: Simulated lightning-induced overvoltage signals using the ATP/EMTP (Analysis Transient Program/Electromagnetic Transients Program) on a model 230 kV power system with 6 buses, 5 transmission lines, 2 transformers, and 6 generators [39].
- Signal Processing & Feature Extraction:
- WT Methodology: Processed signals using Multiresolution Analysis (MRA). The mother wavelet and decomposition levels were varied extensively (e.g., Daubechies 8). The resulting wavelet coefficients were used as input features for classifiers [39].
- PCA Methodology: Applied to the raw signal data to extract patterns and eigenvectors, which were used as mother functions and input features [39].
- Pattern Classification: Processed features from both techniques were fed into three different classifiers: Artificial Neural Network (ANN), k-Nearest Neighbors (k-NN), and Support Vector Machine (SVM) for final classification [39].
- Performance Evaluation: Compared the classification accuracy of the two SPTs across the different classifiers and assessed features like extraction speed and orthogonal functions [39].
This experiment evaluated a proposed Automatic Stationary Wavelet Transform method against established hybrid methods for removing eye-blink artifacts from electroencephalogram signals.
- Data: EEG signals corrupted with eye-blink artifacts, characterized by low frequency (<4 Hz) and high amplitude [40].
- Proposed ASWT Methodology:
- Decomposition: Applied Stationary Wavelet Transform (SWT) using the Daubechies 'db4' mother wavelet, chosen for its morphological similarity to eye-blink signals [40].
- Automatic Level Selection: The decomposition level was automatically determined by calculating the difference in skewness between the approximation coefficients of two consecutive levels. Decomposition stopped when this difference indicated the level containing the artifact [40].
- Reconstruction: The detail coefficients associated with the identified artifact levels were thresholded or removed, and the signal was reconstructed from the remaining coefficients [40].
- Comparative Methods: Compared against AWICA and Enhanced AWICA, which combine wavelet decomposition with Independent Component Analysis [40].
- Performance Metrics: Quantitative evaluation used Normalized Root Mean Square Error (NRMSE), Peak Signal-to-Noise Ratio (PSNR), and the correlation coefficient (ρ) between the filtered signal and a pure EEG ground truth. Execution speed was also measured [40].
This research aimed to isolate action potentials from single neurons in noisy extracellular recordings.
- Data: Both simulated single-unit activity from Neurocube software and real neural recordings from an awake, behaving primate [41].
- WT Denoising Methodology:
- Decomposition: The raw neural signal was decomposed using the Discrete Wavelet Transform with one of five tested mother wavelets (Biorthogonal, Daubechies, discrete Meyer, Symmetric, Coifman) [41].
- Thresholding: Wavelet coefficients were thresholded using one of three schemes (Fixed form, Stein’s Unbiased Estimate of Risk, Minimax) and one of two rules (soft, hard thresholding) [41].
- Reconstruction: The denoised signal was reconstructed from the thresholded coefficients [41].
- Feature Extraction & Clustering: PCA was applied to the denoised spike waveforms for dimensionality reduction and feature extraction. The resulting principal components were then used for spike sorting and clustering [41].
- Performance Evaluation:
Technique Workflows and Relationships
The diagram below illustrates the standard workflow for applying Wavelet Transform and PCA, either independently or in combination, for signal denoising and feature extraction.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 4: Essential Materials and Tools for Signal Processing Experiments
| Item | Function in Research |
|---|---|
| ATP/EMTP Software [39] | Industry-standard software for simulating electromagnetic transients (e.g., lightning strokes) in power systems to generate test signals. |
| Neurocube Software [41] | A tool for generating realistic simulations of single-unit neural activity in a customizable 3D tissue cube, providing controlled data. |
| Stationary Wavelet Transform (SWT) [40] | A wavelet transform variant that is translation-invariant, providing better temporal resolution for artifact removal than DWT. |
| Daubechies (db4) Mother Wavelet [40] | A commonly chosen mother wavelet in biomedical processing due to its morphological similarity to physiological signals like eye blinks. |
| Independent Component Analysis (ICA) [40] | A blind source separation method used to statistically isolate independent source signals from a mixed recording. |
| k-Nearest Neighbors (k-NN) [39] | A simple, instance-based classification algorithm used to evaluate the quality of features extracted by WT or PCA. |
| Normalized Root Mean Square Error (NRMSE) [40] | A standard metric for quantifying the difference between a processed signal and a ground truth reference. |
| L-ratio & Isolation Distance [41] | Statistical metrics used in neuroscience to evaluate the quality of clustering in spike sorting, indicating how well neural units are isolated. |
Motion artifacts represent a fundamental challenge in medical imaging, often compromising diagnostic accuracy, quantitative analysis, and downstream clinical decision-making. Effective motion correction is not merely an image enhancement tool but a critical component for ensuring data integrity, particularly in dynamic studies, low-signal environments, and quantitative functional imaging. The development of modality-specific correction algorithms has become a central focus in imaging science, driven by the need for non-invasive assessment in neurology, oncology, and cardiology. This guide objectively compares the performance of contemporary motion correction algorithms across five imaging modalities—CT, PET, MRI, fNIRS, and Cryo-EM—by synthesizing experimental data from recent studies. The analysis is framed within a broader thesis on evaluating algorithmic performance through standardized metrics such as signal-to-noise ratio (SNR), quantitative parameter accuracy, and expert quality scores, providing researchers and drug development professionals with a evidence-based resource for technology selection.
Motion Correction in Computed Tomography (CT)
Experimental Protocol: Coronary CT Angiography (CCTA)
A recent retrospective study investigated the diagnostic performance of two motion correction algorithms for Coronary CT Angiography (CCTA) in 151 patients with suspected coronary artery disease [5]. All patients underwent CCTA followed by invasive coronary angiography (ICA) and fractional flow reserve (FFR) measurement within three months. CCTA images were reconstructed using three methods: standard iterative reconstruction (STD), first-generation SnapShot Freeze (SSF1), and second-generation SnapShot Freeze 2 (SSF2). SSF1 tracks coronary artery motion using data from three adjacent cardiac phases to compensate for residual motion, while SSF2 extends motion correction to the entire heart [5]. Objective image quality was scored on a 5-point scale. Obstructive stenosis was defined as ≥50% diameter reduction in the left main artery or ≥70% in other vessels. Ischemic stenosis was defined by an invasive FFR ≤0.8 or ≥90% diameter stenosis. CT-derived FFR (CT-FFR) values were computationally simulated from the three image sets and compared against the invasive FFR reference.
Performance Data and Analysis
The study demonstrated significant improvement in image quality and diagnostic accuracy with the advanced motion correction algorithm, particularly SSF2.
Table 1: Performance of Motion Correction Algorithms in Coronary CT Angiography
| Metric | STD (Standard) | SSF1 (First-Gen) | SSF2 (Second-Gen) | P-Value |
|---|---|---|---|---|
| Overall Image Quality Score (Median) | 3.0 | 3.0 | 3.67 | < 0.001 (SSF2 vs. both) |
| Correlation with Invasive FFR (r-value) | Not Reported | 0.595 | 0.652 | < 0.001 |
| Consistency with Invasive FFR (Mean Difference) | Not Reported | 0.07 | 0.04 | N/A |
| AUC for Diagnosing Ischemic Lesions (Per-Lesion) | Not Reported | 0.795 | 0.887 | < 0.001 |
Source: [5]
The data shows that SSF2 provided superior image quality compared to both STD and SSF1 [5]. Furthermore, CT-FFR calculations derived from SSF2-corrected images showed the strongest correlation and best agreement with invasive FFR values, leading to a statistically significant improvement in the area under the curve (AUC) for diagnosing ischemic lesions. This confirms that whole-heart motion correction (SSF2) enhances lumen segmentation accuracy and the reliability of computational fluid dynamics simulations for CT-FFR.
Research Reagent Solutions for CCTA Motion Correction
Table 2: Key Reagents and Materials for CCTA Motion Correction Studies
| Item | Function in Experiment |
|---|---|
| CT Contrast Agent (Iodinated) | Opacifies coronary artery lumen for visualization of stenosis. |
| Iterative Reconstruction Software | Base image reconstruction method, providing the dataset for subsequent motion correction. |
| SnapShot Freeze (SSF1 & SSF2) Algorithms | Software modules for performing targeted (SSF1) or whole-heart (SSF2) motion correction. |
| Invasive FFR Measurement System | Provides the reference standard for hemodynamically significant stenosis. |
Motion Correction in Positron Emission Tomography (PET)
Multi-Tracer Brain PET Protocol
A study evaluated motion correction methods on the ultra-high-performance NeuroEXPLORER (NX) brain PET system using multiple tracers: 18F-FE-PE2I (dopamine transporters), 11C-PHNO (dopamine D2/D3 receptors), and 18F-SynVesT-1 (SV2A) [12]. List-mode data were acquired over 90 minutes. The evaluated methods included: No Motion Correction (NMC), Post-Reconstruction Registration (PRR), frame-based motion correction using an external United Healthcare Motion Tracking system (UMT Frame MC), and event-by-event motion correction with the same system (UMT EBE MC). The UMT system collected motion data at 30 Hz. The primary outcome was the smoothness of time-activity curves (TACs), quantified by the standard deviation (SD) of residuals around fitted curves, expressed as a percentage of the mean value [12].
Respiratory Motion Correction in Lung Cancer PET/CT Protocol
A separate study validated a data-driven gating (DDG) algorithm with a Reconstruct, Register, and Average (RRA) motion correction method for respiratory motion in lung cancer PET/CT [14]. Validation involved a phantom with moving spheres (10-28 mm diameter) and a prospective study of 30 patients with 76 lung lesions <3 cm. The phantom provided a ground-truth static PET for comparison. In patients, ungated and RRA-corrected PET images were compared. Metrics included SUV~max~, SUV~mean~, SUV~peak~, lesion volume, contrast-to-noise ratio (CNR), and expert visual quality scores (5-point scale) [14].
Performance Data and Analysis
Table 3: Performance of Motion Correction Methods in PET Imaging
| Application & Metric | No Correction / Ungated | Basic Correction (PRR/Frame MC) | Advanced Correction (UMT EBE MC / RRA) |
|---|---|---|---|
| Brain PET (NX) [12] | |||
| TAC Residual SD (%)* | Highest | Reduced | Lowest |
| Image Sharpness | Blurred | Improved | Most distinct gyri/sulci |
| Lung PET/CT (Patient) [14] | |||
| Lesion SUV~max~ | Baseline | N/A | +3.9% |
| Lesion SUV~mean~ | Baseline | N/A | +6.5% |
| Lesion Volume | Baseline | N/A | -18.4% |
| Image Quality Score | 3.03 ± 1.19 | N/A | 3.90 ± 0.86 |
*TAC: Time-Activity Curve; SD: Standard Deviation. A lower SD indicates a smoother, more stable curve.
In brain PET, UMT EBE MC outperformed all other methods by effectively eliminating rapid intraframe motion, resulting in the smoothest TACs and best visual resolution [12]. In lung PET/CT, the DDG+RRA method significantly improved quantitative accuracy by increasing SUV metrics and CNR while reducing overestimated lesion volumes, alongside significantly better visual quality scores [14].
Workflow: Data-Driven Respiratory Gating in PET/CT
The following diagram illustrates the workflow of the data-driven gating (DDG) and Reconstruct, Register, and Average (RRA) motion correction process used in the lung cancer PET/CT study.
Motion Correction in Magnetic Resonance Imaging (MRI)
Experimental Protocol: Joint Denoising and Artifact Correction
A novel Joint image Denoising and motion Artifact Correction (JDAC) framework was developed for 3D brain MRI to handle severe noise and motion artifacts simultaneously [42]. The method uses an iterative learning strategy with an adaptive denoising model and an anti-artifact model. The denoising model was trained on 9,544 T1-weighted MRIs from the ADNI database with added Gaussian noise. The anti-artifact model was trained on 552 T1-weighted MRIs with motion artifacts and their paired motion-free images. Validation was performed on public datasets and a clinical study with motion-affected MRIs. Key innovations included a noise level estimation strategy based on gradient map variance and a gradient-based loss function to preserve brain anatomy [42]. Performance was compared against state-of-the-art methods like BM4D using metrics such as Peak Signal-to-Noise Ratio (PSNR) and Structural Similarity Index (SSIM).
Ultra-Low Field (ULF) MRI Protocol
Another study focused on motion correction for brain MRI at 64 mT, an ultra-low field (ULF) system requiring long scan times prone to motion [16]. The approach combined alignedSENSE, a data-driven motion correction algorithm based on the SENSE model, with the self-navigated DISORDER phase encoding sampling trajectory. The method also corrected for within-scan phase variations from other system imperfections. The technique was applied without increasing scan time, and image quality was assessed qualitatively [16].
Performance Data and Analysis
The JDAC framework demonstrated superior performance in jointly addressing noise and motion. On a clinical motion-affected dataset, JDAC achieved a PSNR of 33.21 and SSIM of 0.926, outperforming other methods [42]. The integrated approach progressively improved image quality through iterative learning, effectively handling cases where severe degradation types co-occur. For ULF MRI, the proposed motion+phase correction improved image quality in all tested cases, making the low-field systems more clinically viable [16].
Research Reagent Solutions for MRI Motion Correction
Table 4: Key Reagents and Materials for MRI Motion Correction Studies
| Item | Function in Experiment |
|---|---|
| T1-weighted MRI Sequences | Provides the primary anatomical imaging data for processing. |
| Public Datasets (e.g., ADNI) | Provides large-scale, annotated data for training and validating algorithms. |
| Noise Simulation Software | Generates training data with controlled noise levels for denoising models. |
| Motion Simulation Software | Synthesizes motion artifacts for training anti-artifact models. |
| alignedSENSE & DISORDER Trajectory | Software and sampling methods for data-driven motion correction in ULF MRI. |
Motion Correction in Functional Near-Infrared Spectroscopy (fNIRS)
fNIRS is a non-invasive, optical neuroimaging technique that measures cortical hemodynamic changes (oxygenated and deoxygenated hemoglobin) associated with neural activity [43]. Unlike MRI and PET, fNIRS allows for measurements in naturalistic settings but is highly susceptible to confounding signals from systemic physiology and motion artifacts. The fNIRS signal comprises multiple components, with the task-evoked, neuronal, cerebral hemodynamic response being the target; all other components (e.g., motion, blood pressure oscillations) are considered physiological noise that must be removed [43]. Motion artifacts are a primary challenge, often causing signal shifts an order of magnitude larger than the functional signal of interest, necessitating robust correction methods before fNIRS can be reliably used in clinical individual-level applications.
Research Reagent Solutions for fNIRS
Table 5: Key Components in fNIRS Research
| Item | Function in Experiment |
|---|---|
| fNIRS System (Sources & Detectors) | Hardware that emits NIR light and detects attenuated light after tissue passage. |
| Probe Geometry/Holder | Arrangement of optodes on the scalp defining measurement channels and regions. |
| Motion Tracking System (e.g., Accelerometers) | Provides independent measurement of head motion to inform artifact correction. |
| Signal Processing Suite | Software containing algorithms for motion artifact detection, correction, and signal filtering. |
Motion Correction in Cryo-Electron Microscopy (Cryo-EM)
Note: Based on the provided search results, no specific case studies on motion correction for Cryo-EM were available. The following section outlines the general framework based on standard practice.
In Cryo-EM, "motion" refers to the movement and deformation of the frozen-hydrated specimen during electron beam exposure, a critical issue that blurs high-resolution information. Motion correction is an essential early step in the single-particle analysis workflow. The process involves collecting movie frames over a single exposure. Algorithmic approaches like MotionCor2 estimate and correct for the complex motion of individual particles or the whole frame. This correction is crucial for achieving near-atomic resolution structures.
Conceptual Workflow: Single-Particle Cryo-EM Processing
The diagram below outlines the general image processing workflow in single-particle Cryo-EM, highlighting the foundational role of motion correction.
Cross-Modality Performance Analysis and Future Directions
The presented case studies reveal a clear trend across modalities: the move towards more integrated, data-driven, and holistic correction approaches. In CT and PET, newer algorithms (SSF2, RRA, EBE MC) outperform their predecessors by correcting motion over larger domains (whole heart vs. coronaries) or with higher temporal fidelity (event-by-event vs. frame-based). In MRI, the JDAC framework demonstrates the power of jointly solving multiple degradation problems (noise and motion) that were traditionally handled separately. fNIRS development is focused on disentangling complex signal mixtures to isolate motion artifacts.
Table 6: Cross-Modality Comparison of Motion Correction Performance
| Modality | Primary Motion Challenge | Exemplar Algorithm | Key Performance Outcome |
|---|---|---|---|
| CT | Cardiac & respiratory motion | SnapShot Freeze 2 (SSF2) | ↑ Image Quality Score; ↑ AUC for ischemia diagnosis to 0.887 [5] |
| PET | Brain: Intraframe head motionLung: Respiratory motion | UMT EBE MC [12]DDG + RRA [14] | ↓ TAC residual SD; ↑ visual sharpness↑ SUV~max~ (3.9%), ↓ Lesion Volume (18.4%) [14] |
| MRI | Bulk head motion; Simultaneous noise | JDAC Framework [42] | ↑ PSNR (33.21) & SSIM (0.926) on clinical data [42] |
| fNIRS | Scalp hemodynamics; subject movement | Signal Processing Pipelines [43] | Critical for isolating neuronal signal; enables naturalistic studies |
Future Outlook
Future directions in motion correction research will likely focus on deep learning-based methods that can directly learn the mapping from corrupted to clean data, the standardization of correction procedures for clinical application (especially in fNIRS and MRI), and the development of real-time correction that adapts during acquisition. Furthermore, as total-body PET systems become more established [44], their ultra-high sensitivity will enable new motion correction strategies and place greater emphasis on minimizing artifacts to fully leverage their quantitative potential. The convergence of high-performance hardware and intelligent, integrated software algorithms will continue to push the boundaries of diagnostic and research imaging.
Implementation Challenges and Optimization Strategies for Robust Performance
Addressing Computational Demands and Real-Time Processing Requirements
Motion correction is a critical step in medical imaging, directly impacting the diagnostic quality of scans in modalities from MRI to PET and CT. However, the computational load and processing speed required for effective correction, especially in real-time applications like biofeedback or interventional guidance, present significant challenges. This guide objectively compares the performance of various motion correction algorithms, with a focused analysis on their computational demands and ability to meet real-time processing requirements. As imaging technologies advance toward higher resolutions and faster acquisitions, the efficiency of correction algorithms becomes paramount not only for image quality but also for clinical feasibility. We synthesize experimental data from recent studies to provide researchers and developers with a clear framework for selecting appropriate motion correction strategies based on their computational characteristics.
Comparative Performance Analysis of Motion Correction Algorithms
The table below summarizes key performance metrics and computational characteristics of various motion correction algorithms, highlighting their suitability for real-time processing.
Table 1: Computational Performance Comparison of Motion Correction Algorithms
| Algorithm | Imaging Modality | Computational Approach | Key Performance Metrics | Real-Time Capability |
|---|---|---|---|---|
| PROMO [45] | MRI | Image-based tracking with Extended Kalman filter | Steady-state error <10% of motion magnitude even for large motions (>15° rotations) | Prospective (real-time) correction during scan |
| GPU-Accelerated Motion Correction [46] | fMRI | GPU-accelerated, uses interleaved acquisition | Comparable to standard offline methods; outperforms zero-order interpolation | Minimal processing delay; enables real-time biofeedback |
| Deep Learning MCA for CCTA [47] | Coronary CT | Deep learning-based motion correction | Enables reliable evaluation with up to 4% phase deviation at high heart rates | Post-processing, not real-time during acquisition |
| SSF2 Motion Correction [5] | Coronary CT | Second-generation motion correction algorithm | Improved image quality (median score: 3.67 vs 3.0 for STD); better CT-FFR diagnostic accuracy (AUC=0.887) | Post-processing application |
| UniMo Framework [48] | Multi-modal (MRI, CT) | Unified DL for rigid & non-rigid motion | Generalizes across modalities without retraining; real-time inference | Real-time capable; cross-modality application |
| Machine Learning PET Correction [13] | Pediatric Brain PET | Patch-based Artificial Neural Network (ANN) | Reduced motion estimation error (1.3±0.2mm vs 4.8±1.0mm); improved quantitative accuracy | Enables motion correction from reduced-count data |
| UNet+JE Hybrid [9] | 3D MRI | Hybrid DL with Joint Estimation | Comparable quality to JE alone; 2-4x runtime reduction vs standard JE | Faster processing while maintaining correction quality |
Key Computational Performance Insights
Real-Time Performance: The GPU-accelerated approach for fMRI demonstrates that specialized hardware implementation can achieve minimal processing delay (essentially no delay) while maintaining correction quality comparable to offline methods [46]. This enables applications like real-time biofeedback where immediate processing is critical.
Deep Learning Efficiency: The UNet+JE hybrid model for 3D MRI shows that combining deep learning with traditional optimization can reduce runtimes by a factor of 2-4× while preserving image correction quality, making 3D motion correction more practical for clinical settings [9].
Cross-Modality Generalization: UniMo's framework demonstrates that a single model can achieve motion correction across multiple imaging modalities (fetal MRI, lung CT, BraTS) without retraining, significantly reducing development and computational costs for implementing motion correction across diverse imaging platforms [48].
Experimental Protocols and Methodologies
GPU-Accelerated Real-Time fMRI Motion Correction
The validation protocol for the GPU-accelerated motion correction algorithm utilized empirical data from real-time fMRI scans to assess both quality and timing performance [46]:
Data Acquisition: fMRI data was acquired using standard interleaved protocols where odd-numbered slices are acquired first followed by even-numbered slices.
Processing Pipeline: The system waits until all odd slices of frame n are acquired, then orders these with even slices from frame n-1 to create frame n-½. This composite frame is rigidly registered to a reference frame during acquisition of the even slices of frame n, resulting in minimal processing delay.
Optimization Method: A hill-climb optimization minimized a sum of square differences (SSD) objective function using a three-stage multi-resolution technique with isotropic resampling, Gaussian smoothing (FWHM of 4mm then 2mm), and downsampling (rate of 4 then 2).
Performance Validation: Motion correction quality was compared against standard offline methods and other real-time methods using zero-order interpolation of motion parameters. The algorithm performed comparably to standard offline methods while achieving essentially no processing delay.
Unified Deep Learning Framework (UniMo) Evaluation
The UniMo framework was evaluated through comprehensive experiments across multiple modalities and motion types [48]:
Architecture: The framework uses an alternating optimization scheme with: (1) an equivariant neural network for global rigid motion correction, and (2) an encoder-decoder network for local deformations. It incorporates both image intensities and shape information for robustness.
Training Protocol: Initially trained on fetal MRI (particularly challenging due to both large rigid and non-rigid motion with wide appearance variations) without retraining for other modalities.
Testing Protocol: The trained model was evaluated on MedMNIST, lung CT, and BraTS datasets to assess cross-modality performance without retraining.
Validation Metrics: Performance was measured using accuracy of motion estimation, stability across modalities, and computational efficiency for real-time inference. UniMo surpassed existing methods in accuracy while maintaining stability across unseen datasets.
Hybrid Deep Learning-Joint Estimation for 3D MRI
The UNet+JE method was rigorously evaluated on 3D MPRAGE scans with varying motion corruption levels [9]:
Data Preparation: Created training datasets with different distributions of motion corruption severity (mild to severe). Included both simulated motion (n=40) and in vivo motion corruption (n=10).
Algorithm Implementation: Combined a UNetmag neural network with a physics-informed JE algorithm that alternates between estimating the image and motion trajectory using conjugate gradient and quasi-Newton methods.
Comparison Framework: Compared five method variations: UNetmag trained on two different datasets, UNet+JE similarly trained on two datasets, and JE as a benchmark.
Evaluation Metrics: Assessed image quality improvement, residual artifacts, runtime performance, and robustness to data distribution shifts. UNet+JE provided better motion correction than UNetmag alone while reducing runtimes by 2-4× compared to JE.
Algorithmic Relationships and Workflow Visualization
The diagram below illustrates the relationships between major motion correction approaches and their progression toward addressing computational demands.
Motion Correction Algorithm Evolution shows the progression from traditional methods to modern approaches, highlighting how hybrid techniques integrate multiple advancements.
The experimental workflow for evaluating computational performance typically follows a structured pipeline, as visualized below for the hybrid UNet+JE approach:
Computational Workflow Assessment outlines the standard evaluation methodology for motion correction algorithms.
Research Reagent Solutions: Essential Computational Tools
The table below details key computational tools and frameworks essential for implementing and evaluating motion correction algorithms in research settings.
Table 2: Essential Research Reagents for Motion Correction Development
| Tool/Framework | Primary Function | Application Context | Implementation Notes |
|---|---|---|---|
| GPU Acceleration (CUDA) | Parallel processing of registration operations | Real-time fMRI [46], 3D MRI correction [9] | Critical for reducing processing delays; enables real-time biofeedback |
| Extended Kalman Filter | Online motion estimation and prediction | PROMO MRI correction [45] | Provides robust tracking with reduced sensitivity to off-resonance effects |
| Unified Motion Framework (UniMo) | Combined rigid and non-rigid correction | Multi-modal applications [48] | Eliminates retraining needs across modalities; uses both intensity and shape data |
| Joint Estimation (JE) | Physics-informed motion modeling | 3D MRI correction [9] | Based on Fourier transform properties under rotation/translation; computationally intensive |
| Deep Learning Denoisers | Artifact reduction in corrupted images | Hybrid approaches (UNet+JE) [9] | Provides fast initial improvement; reduces iterations needed for convergence |
| Snapshot Freeze Algorithms | Cardiac motion tracking | Coronary CT angiography [47] [5] | Uses data from adjacent cardiac phases for motion compensation |
| ANN Enhancement Networks | Quality improvement for low-count data | Pediatric PET imaging [13] | Enables motion correction from reduced-count data without sacrificing accuracy |
The computational demands and real-time processing requirements of motion correction algorithms present both challenges and opportunities for medical imaging research. Traditional approaches like PROMO and GPU-accelerated methods established that real-time correction was feasible through specialized tracking and hardware optimization [45] [46]. Deep learning approaches have since expanded these capabilities, with unified frameworks like UniMo demonstrating cross-modality application without retraining [48], and hybrid approaches like UNet+JE achieving significant runtime reductions while maintaining correction quality [9]. The evolution toward hybrid methods that combine the physical modeling strengths of traditional approaches with the speed and adaptability of deep learning represents the most promising direction for addressing the dual challenges of computational efficiency and correction accuracy. As medical imaging continues to advance toward higher resolutions and more complex applications, the development of computationally efficient motion correction will remain essential for both clinical utility and research advancement.
Mitigating Over-Correction and Signal Loss in Automated Systems
In biomedical imaging and automated analysis systems, the accurate correction of motion is paramount for achieving reliable data. However, the correction process itself can introduce significant artifacts, including signal loss and over-correction, which ultimately compromise data integrity and clinical utility. Motion-induced signal loss occurs when uncorrected motion during data acquisition leads to phase changes and signal dephasing, particularly in techniques utilizing strong encoding gradients like diffusion-weighted imaging (DWI) [49]. Conversely, over-correction typically arises from improper implementation of motion compensation algorithms, often due to inaccurate tracking, registration errors, or the introduction of interpolation artifacts during spatial transformation [50]. This guide objectively compares the performance of various motion correction algorithms across different imaging modalities, focusing on their efficacy in mitigating these twin challenges. We present experimental data and detailed methodologies to help researchers, scientists, and drug development professionals select appropriate correction strategies for their specific applications.
Performance Comparison of Motion Correction Algorithms
The table below summarizes quantitative performance data for various motion correction algorithms across different imaging modalities, highlighting their effectiveness in mitigating signal loss and over-correction.
Table 1: Quantitative Performance Comparison of Motion Correction Algorithms
| Modality | Algorithm/System | Key Metric | Performance Result | Reference |
|---|---|---|---|---|
| DWI-MRI | Real-time Optical Tracking with Moment Restoration | Prevention of motion-induced signal loss | Improved reproducibility and reliability of diffusion tensor measures | [49] |
| CCTA | SnapShot Freeze 2 (SSF2) | Image Quality Score (Median) | 3.67 (vs. 3.0 for STD and SSF1) | [5] |
| CCTA | SnapShot Freeze 2 (SSF2) | Correlation with invasive FFR (r) | r = 0.652 | [5] |
| PET | Data-Driven Motion Correction (DDMC) | Contrast-to-Noise Ratio (CNR) | Improves for small targets with high motion amplitude; decreases for larger spheres due to 36% increase in background noise | [51] |
| Quantitative MRI (T1 mapping) | Image Registration & Trilinear Interpolation | Error in T1 Estimation | ~10% of the signal in brain's gray and white matter | [50] |
Analysis of Comparative Performance
The data reveals that prospective correction methods, which adjust imaging parameters in real-time, are highly effective in preventing signal loss at its source. In DWI, the combination of real-time optical tracking and a moment-restoring gradient blip successfully prevented signal dephasing and improved the robustness of quantitative measures, which is crucial for clinical populations prone to movement [49]. Similarly, in coronary CT angiography (CCTA), the second-generation SnapShot Freeze 2 (SSF2) whole-heart motion correction algorithm significantly outperformed its predecessor by extending the correction range beyond just the coronary arteries to the entire heart. This resulted in superior image quality scores and the strongest correlation with invasive fractional flow reserve (FFR) measurements, demonstrating enhanced accuracy in functional assessment [5].
A critical trade-off emerges in data-driven methods. In PET imaging, Data-Driven Motion Correction (DDMC) improves the contrast recovery of lesions affected by respiratory motion. However, this comes at the cost of increased background noise, which subsequently reduces the contrast-to-noise ratio (CNR) for larger targets. This underscores a potential form of over-correction, where the algorithmic enhancement of one image characteristic (contrast) detrimentally impacts another (noise), potentially limiting detectability [51]. Furthermore, all registration-based methods are susceptible to interpolation errors. As demonstrated in quantitative T1 mapping, the process of interpolation and resampling during motion correction can introduce errors in the estimated physical properties of tissue, such as T1 relaxation times, with reported inaccuracies of around 10% [50]. This error is contrast-dependent and highlights a fundamental limitation of post-processing correction techniques that involve spatial transformation.
Detailed Experimental Protocols
To facilitate a deeper understanding of the comparative data, this section outlines the key experimental methodologies from the cited studies.
Protocol 1: Real-Time Motion Correction in DWI-MRI
This protocol [49] was designed to prevent motion-induced signal loss prospectively.
- Imaging Platform: Experiments were performed on a Siemens 3 T TIM Trio scanner.
- Pulse Sequence: A twice-refocused spin-echo echo-planar imaging (EPI) DWI sequence was modified.
- Motion Tracking: A prototype Moiré Phase Tracking (MPT) system operating at 80 frames per second tracked head motion via a camera mounted inside the scanner bore, following a target attached to the subject's forehead.
- Correction Implementation:
- Prospective Slice Correction: The head pose data were used to update the position and orientation of the imaging volume before the acquisition of each slice.
- Gradient Moment Restoration: The motion-induced gradient moment imbalance during diffusion encoding was calculated in real-time. A brief, tailored gradient "blip" was inserted immediately before the signal readout to restore the moment balance and counteract signal dephasing.
- Evaluation: The method was validated in both phantom experiments and human subjects, assessing the reduction in signal loss and the improvement in the reproducibility of diffusion tensor measures.
Protocol 2: Evaluating Motion Correction in CCTA for CT-FFR
This clinical study [5] compared the diagnostic performance of CT-derived fractional flow reserve (CT-FFR) using different motion correction levels.
- Patient Population: 151 patients who underwent both CCTA and invasive coronary angiography (ICA) or FFR within three months were retrospectively included.
- Image Acquisition & Reconstruction: CCTA images were acquired and initially reconstructed using an iterative reconstruction technique.
- Experimental Groups: The images were processed into three groups for comparison:
- STD: Standard images with iterative reconstruction.
- SSF1: Images processed with the first-generation SnapShot Freeze algorithm (corrects coronary arteries only).
- SSF2: Images processed with the second-generation SnapShot Freeze 2 algorithm (corrects the entire heart).
- Outcome Measures:
- Image Quality: Scored subjectively.
- Diagnostic Accuracy: For detecting obstructive stenosis (defined by diameter stenosis) and ischemic lesions (defined by FFR ≤ 0.80), using ICA/FFR as the reference standard.
- Correlation: Between CT-FFR values and invasive FFR values.
Protocol 3: Phantom Evaluation of Data-Driven PET Motion Correction
This controlled study [51] quantified the impact of DDMC on lesion detectability.
- Phantom Model: A NEMA-IEC body phantom with six hollow spheres of different sizes was used.
- Motion Simulation: A moving platform simulated respiratory motion with varying amplitudes (0, 7, 10, 20, 30 mm) in the superior-inferior direction.
- Tracer Distribution: The background and spheres were filled with Fluorine-18 to achieve different target-to-background ratios (TBR: 2, 5, 10.5).
- Image Acquisition and Processing: The phantom was scanned on a Siemens Vision BIOGRAPH 600 PET-CT. Data were reconstructed with and without the DDMC application (Siemens OncoFreeze AI).
- Quantitative Analysis:
- Recovery Coefficient (RC): Measured both maximum and mean RC to assess contrast recovery.
- Contrast-to-Noise Ratio (CNR): Calculated to evaluate the trade-off between contrast improvement and noise introduction.
Signaling Pathways and Workflow Diagrams
The following diagrams illustrate the logical workflows and key decision points for the motion correction strategies discussed.
Motion Correction Decision Pathway
Prospective vs. Retrospective Correction Logic
The Scientist's Toolkit: Research Reagent Solutions
The following table details key components and technologies essential for implementing and evaluating motion correction algorithms in experimental setups.
Table 2: Essential Research Tools for Motion Correction Studies
| Tool / Reagent | Function / Purpose | Example Use-Case |
|---|---|---|
| Optical Motion Tracking System (e.g., MPT) | Tracks subject/phantom motion in real-time with 6 degrees of freedom. Provides data for prospective correction. | Real-time update of slice positions and gradient calculations in DWI-MRI [49]. |
| Anthropomorphic Phantoms (e.g., NEMA-IEC) | Provides a controlled, reproducible platform with known structures and activity concentrations to quantify algorithm performance. | Evaluating recovery coefficients (RC) and contrast-to-noise ratio (CNR) in PET motion correction studies [51]. |
| Motion Simulation Platforms | Physically moves phantoms to simulate physiological motions (e.g., respiration, cardiac cycle). | Simulating respiratory motion with variable amplitudes and periods in PET and CT studies [51]. |
| Quantitative Mapping Phantoms | Phantoms with well-defined T1/T2 relaxation properties. | Validating the accuracy of quantitative MRI parameter maps (e.g., T1) after motion correction, assessing interpolation errors [50]. |
| Data-Driven Motion Correction Software (e.g., DDMC) | Uses internal data features (e.g., respiratory signals from PET raw data) to guide motion correction without external devices. | Retrospective correction of respiratory motion in whole-body oncological PET scans [51]. |
| Motion-Corrected Reconstruction Algorithms (e.g., MOLAR) | Incorporates motion trajectories directly into the image reconstruction process. | Event-by-event motion correction in high-resolution brain PET to eliminate intraframe motion effects [12]. |
Parameter Optimization and Domain Adaptation Across Imaging Protocols
Motion artifacts present a significant challenge in medical imaging, often compromising diagnostic quality and quantitative accuracy. The performance of motion correction algorithms is highly dependent on proper parameter optimization and their ability to adapt across diverse imaging protocols and domains. This comparison guide provides an objective evaluation of current motion correction technologies, examining their performance across various imaging modalities including MRI, PET, and CT. As medical imaging continues to advance toward quantitative precision medicine, understanding the capabilities and limitations of these correction methods becomes crucial for researchers, scientists, and drug development professionals who rely on accurate image data for their work. This analysis focuses specifically on the interplay between parameter optimization strategies and domain adaptation approaches that enable algorithms to perform consistently across varying acquisition protocols and patient populations.
Experimental Protocols and Methodologies
Framework for Prospective Motion Correction Evaluation
A comprehensive framework for evaluating prospective motion correction (PMC) in MRI was established to address the challenge of variable intrinsic motion patterns between scans. This methodology employs recorded motion trajectories from human subjects replayed in phantom experiments to enable unbiased comparisons between correction setups. The experimental protocol involved:
Subject and Motion Tracking: Five volunteers underwent T1-weighted MRI with an optical Moiré Phase Tracking marker rigidly attached via two fixation methods: a mouth guard and a nose bridge mount [4]. Motion was tracked using an in-bore camera system while the modified 3D-MPRAGE sequence updated imaging parameters in real-time using the XPACE library.
Phantom Motion Replay: The same MRI protocol was applied to a phantom where motion artifacts were induced by modulating imaging parameters according to the recorded in-vivo motion trajectories. This created a controlled reference for expected in-vivo artifacts when prospective motion correction was disabled [4].
Image Quality Metrics: Two quantitative indicators were employed: (1) Average Edge Strength (AES) to quantify image blurring at edges, and (2) Haralick texture entropy (CoEnt) derived from gray-level co-occurrence matrices to capture diffuse artifacts not limited to edges [4].
Deep Learning Motion Correction in CEST MRI
A novel neural network architecture was developed specifically for motion artifact correction in Chemical Exchange Saturation Transfer (CEST) MRI, operating directly in the Z-spectral frequency domain (MOCOΩ) rather than the spatial domain. The methodology included:
Motion Simulation: For supervised learning, "clean" motion-free saturation-weighted images were transformed using rigid-body motion parameters randomly sampled from ranges of ±2 mm translation and ±1° rotation in all directions [52]. The transformation incorporated both translation and rotation matrices applied to 3D saturation-weighted images at each frequency offset.
Network Architecture and Training: The model incorporated a saturation-contrast-specific loss function designed to preserve amide proton transfer (APT) contrast while enforcing alignment between motion-corrected and ground-truth images [52]. This approach specifically addressed the challenge of intensity-based registration failures in CEST MRI where motion artifacts are comparable to target CEST signal contrasts (~1%).
Validation: The framework was evaluated on numerical phantoms, healthy volunteers (n=7), and brain tumor patients (n=7) using a 3T scanner with multi-saturation frequency offsets [52]. Performance was compared against existing methods including mutual information-based correction, low-rank approximation, and robust principal component analysis approaches.
Data-Driven Motion Correction in Clinical Brain PET
A fully data-driven motion estimation and correction approach for clinical brain PET imaging was evaluated through a reader-based study and atlas-based quantitative analysis:
Motion Estimation: Ultrafast reconstructions of very short frames (0.6-1.8 seconds) were performed to achieve high temporal resolution (~1 Hz) motion estimation via image-based registration [22]. The motion estimates demonstrated accuracy of <1 mm mean error in absolute displacement.
Motion-Corrected Reconstruction: List-mode time-of-flight reconstruction with event-by-event motion correction was implemented, incorporating system matrix, motion-aware scatter contributions, randoms correction, attenuation correction factors, and scanner sensitivity factors [22].
Clinical Validation: Fifty clinical 18F-FDG brain PET datasets were categorized into motion groups (low, offset, medium, high) based on median displacement metrics [22]. Reader studies and atlas-based quantitative analyses across eight brain regions were performed to assess diagnostic quality and quantitative accuracy improvements.
Motion Correction Algorithm in CT Angiography
A randomized controlled trial evaluated the Snapshot-Freeze (SSF) motion correction algorithm in patients undergoing coronary CT angiography:
Study Design: 140 patients were randomized to receive beta-blockers (BB) or no beta-blockers (non-BB) before coronary CT [53]. All images were reconstructed with both SSF and standard reconstruction (STD) algorithms.
Image Quality Assessment: Images were evaluated using a 4-point Likert score (1: excellent, 2: good, 3: adequate, 4: non-diagnostic) with specific notation of motion artifact presence [53]. Analysis included 64 patients in the BB group (mean HR 56±4 bpm) and 51 in the non-BB group (mean HR 67±7 bpm).
Performance Comparison Data
Quantitative Performance Metrics Across Modalities
Table 1: Motion Correction Performance Across Imaging Modalities
| Modality | Algorithm | Performance Metrics | Subject Population | Key Results |
|---|---|---|---|---|
| MRI | Prospective Motion Correction | AES, CoEnt | 5 volunteers | Mouth guard fixation outperformed nose bridge; Statistical significance dependent on motion pattern consideration [4] |
| CEST MRI | MOCOΩ (Frequency domain) | APT RMSE (%) | 7 healthy volunteers, 7 brain tumor patients | RMSE reduction: 4.7%→2.1% (1μT, moderate motion); 8.7%→2.8% (1μT, severe motion) [52] |
| Brain PET | Data-driven motion correction | Qualitative reader scores, regional SUV | 50 clinical patients | 8% of datasets improved from non-diagnostic to diagnostic quality; Significant quantitative improvement in 7/8 brain regions with high motion [22] |
| CT Angiography | Snapshot-Freeze | Likert scores, artifact prevalence | 115 patients (64 BB, 51 non-BB) | Excellent images increased: 44%→59% (BB), 8%→25% (non-BB); Motion artifacts reduced: 31%→11% (BB), 75%→49% (non-BB) [53] |
Domain Adaptation Capabilities
Table 2: Domain Adaptation and Parameter Optimization Approaches
| Algorithm | Domain Adaptation Method | Parameter Optimization Strategy | Protocol Compatibility |
|---|---|---|---|
| PMC Framework [4] | Motion trajectory replay in phantom experiments | Covariate adjustment for intrinsic motion patterns | T1-weighted MRI; Compatible with various tracking marker configurations |
| MOCOΩ [52] | Deep learning in Z-spectral domain | Saturation-contrast-specific loss function | Multiple saturation frequency offsets; B0/B1 inhomogeneity tolerance |
| Data-driven PET [22] | Automated motion estimation from projection data | Ultrashort frame duration optimization (0.6-1.8s) | Multiple PET/CT and PET/MRI systems; Vendor-agnostic |
| Snapshot-Freeze [53] | Heart rate-adaptive processing | Reconstruction parameter tuning | Coronary CTA protocols; Beta-blocker administration states |
| HyDA [54] | Hypernetwork-generated model weights | Test-time domain adaptation without target data | Multi-site MRI; Chest X-ray classification |
Visualization of Methodologies
Prospective Motion Correction Framework
Motion Correction Evaluation Workflow: This diagram illustrates the comprehensive framework for evaluating prospective motion correction systems, incorporating both in-vivo motion tracking and phantom validation to eliminate bias from variable intrinsic motion patterns [4].
Deep Learning Motion Correction Architecture
Deep Learning Correction Architecture: This workflow details the MOCOΩ approach for CEST MRI motion correction, highlighting the frequency-domain neural network with saturation-contrast-specific loss preservation [52].
The Scientist's Toolkit
Essential Research Reagent Solutions
Table 3: Key Research Materials and Analytical Tools
| Tool/Reagent | Function | Application Context |
|---|---|---|
| Moiré Phase Tracking Marker | Optical motion tracking | Prospective motion correction in MRI [4] |
| Custom Mouth Guard | Rigid marker fixation to skull | Reduced skin slippage for accurate motion tracking [4] |
| Motion Simulation Software | Rigid-body transformation of images | Generating training data for deep learning correction [52] |
| Average Edge Strength (AES) | Quantification of image blurring | Edge sharpness evaluation in motion-affected images [4] |
| Haralick Texture Entropy | Diffuse artifact characterization | Non-edge based image quality assessment [4] |
| Z-spectrum Normalization | Signal intensity standardization | CEST MRI motion correction in frequency domain [52] |
| List-mode Reconstruction | Event-by-event motion correction | Data-driven motion compensation in PET [22] |
| Snapshot-Freeze Algorithm | Motion artifact reduction in CT | Coronary CT angiography improvement [53] |
| Hypernetwork Framework (HyDA) | Test-time domain adaptation | MRI brain age prediction across protocols [54] |
Discussion and Future Directions
The comparative analysis reveals significant differences in how motion correction algorithms approach parameter optimization and domain adaptation. The prospective motion correction framework demonstrates the critical importance of accounting for intrinsic motion variability when evaluating different correction configurations [4]. Without considering motion patterns as a covariate, statistical significance in comparing fixation methods was altered, potentially leading to incorrect conclusions about system performance.
The deep learning approach (MOCOΩ) showcases the advantage of operating in the Z-spectral domain for CEST MRI, effectively preserving saturation transfer contrast while correcting motion artifacts [52]. This domain-specific optimization highlights how algorithm performance depends on adapting to the unique characteristics of each imaging modality rather than applying generic correction methods.
Data-driven methods in PET imaging demonstrate the clinical impact of motion correction, with 8% of studies improving from non-diagnostic to diagnostic quality [22]. This represents a significant advancement for quantitative imaging in drug development where consistent image quality is essential for longitudinal studies.
The HyDA framework points toward the future of domain adaptation with its hypernetwork approach that generates model weights dynamically at inference time [54]. This method effectively interpolates to unseen domains without requiring extensive retraining, addressing a key challenge in deploying motion correction algorithms across diverse clinical sites with varying protocols.
For researchers and drug development professionals, these findings emphasize that optimal motion correction requires both parameter tuning for specific imaging contexts and adaptation strategies for cross-protocol compatibility. Future developments will likely focus on increasing the autonomy of adaptation processes while maintaining or improving correction efficacy across increasingly diverse imaging scenarios.
Irregular motion from a-periodic breathing and neurological tremors presents a significant challenge in medical imaging and neurophysiology. Unlike predictable, periodic motion, these irregular patterns can severely degrade data quality, compromising diagnostic accuracy and research validity. This guide compares the performance of modern motion correction algorithms designed to handle such complex, patient-specific variability, providing a objective analysis based on recent experimental data.
Motion Correction Algorithms: A Comparative Analysis
The table below summarizes the core performance data of various motion correction techniques when confronted with irregular motion.
Table 1: Performance Comparison of Motion Correction Algorithms
| Algorithm Name | Modality | Motion Type Addressed | Key Performance Metrics | Reported Performance | Primary Experimental Validation |
|---|---|---|---|---|---|
| MEDiCINe [55] | Electrophysiology (Spike sorting) | Slow drift, high-frequency noise, discrete jumps in probe position | Accuracy of motion estimation, spike sorting accuracy | Outperforms existing methods on simulated data; accurate in primate/rodent recordings | Extensive suite of simulated neurophysiology recordings with known ground-truth motion |
| Patient-Specific PROCO [56] | Cardiac MRI | Respiratory motion (including patient-specific patterns) | Residual motion (Range/RMSE in mm) | Reduced residual motion to 4.08±1.4 / 0.90±0.3 mm; 100% acquisition efficiency [56] | 11 volunteers; comparison against free-breathing and navigator-gated scans |
| MARC (CNN) [57] | Abdominal MRI | Transient severe motion (TSM) from respiration | Motion artifact score (4-point scale), lesion conspicuity | Significantly improved motion scores; improved conspicuity in 72% of severe artifacts [57] | 192 patient datasets; expert radiologist evaluation of image quality |
| Adaptive Filter with Selective Averaging [58] | fMRI | Cardiac and respiratory cycles | Reduction in temporal standard deviation (SDt) | Average SDt reduction of 9.2% (respiratory) and 12.5% (cardiac) [58] | 6 normal volunteers; comparison with RETROICOR method |
| Phase-Based Correction (RCP) [59] | fMRI | Respiratory noise | Correlation with reference respiration signal | High correlation (0.82 to 0.96) between phase time series and respiration [59] | Resting-state fMRI data from 3 subjects; comparison with RETROICOR |
Experimental Protocols for Algorithm Validation
A critical aspect of comparing these technologies is understanding the rigorous experimental methods used to validate their performance against irregular motion.
Protocol for Validating Electrophysiology Motion Correction (MEDiCINe)
MEDiCINe was designed to correct for motion in neural recordings from high-density laminar arrays, which can be affected by pulsation, changes in intracranial pressure, and tissue decompression [55].
- Data Representation: The input data consists of spiking events, each represented as a triple
(time, depth, amplitude)[55]. - Core Methodology: The algorithm learns two differentiable functions:
- A Motion Function, M(d,t), that estimates the displacement
Δdat a given depth and time. - A Classification Network, C(d,a), that outputs the probability a spike originates from the neural dataset versus a uniform null distribution.
- A Motion Function, M(d,t), that estimates the displacement
- Training and Loss Function: The functions are trained jointly using gradient descent to minimize a binary cross-entropy loss. This pressures the motion-corrected dataset to form a sparse distribution in depth-amplitude space, which is highly discriminable from random noise [55].
- Validation: The method was tested on an extensive suite of simulated datasets with known ground-truth motion and on real primate and rodent Neuropixels recordings [55].
Protocol for Validating Patient-Specific Respiratory Correction (PROCO)
This method aims for 100% acquisition efficiency in free-breathing cardiac MRI by creating a patient-specific motion model [56].
- Training Scan: A short training scan acquires ~50 single-heartbeat images in two orthogonal views (e.g., short-axis and 2-chamber). Each image is preceded by a diaphragmatic navigator pulse to record respiratory position [56].
- Motion Extraction: Non-rigid image registration is performed on all training frames against a reference end-expiratory frame. This generates deformation fields that characterize the 3D motion of the heart [56].
- Model Fitting: The average translational motion within a region of interest is fitted to the navigator signal using fractional polynomial regression, creating a patient-specific model that can predict heart motion based on diaphragm position [56].
- Prospective Correction: During the main scan, this model is used in real-time to update the imaging plane position before each single-shot acquisition, based on the current navigator reading [56].
Protocol for Validating Deep Learning Motion Correction (MARC)
The MARC filter uses a convolutional neural network (CNN) to reduce respiratory motion artifacts in gadoxetate disodium–enhanced liver MRI [57].
- Network Architecture: The CNN consists of seven layers, each comprising two-dimensional convolutions, batch normalization, and rectified linear units (ReLUs) [57].
- Training Data Generation: The network was trained on a dataset of 14,190 cropped images. Artifacts were simulated by adding periodic k-space domain noise to clean images, modeling rigid motion with periodic and random respiration [57].
- Validation Method: The study involved 192 patients. Original and filtered image sets (1,344 total) were evaluated by blinded radiologists using a 4-point motion artifact scale. Lesion conspicuity was also ranked via side-by-side comparison [57].
Signaling Pathways and Workflows
The following diagrams illustrate the logical workflows of the key motion correction strategies discussed, highlighting their approach to handling irregular motion.
Motion Correction Workflow for Neural Data
Patient-Specific Motion Model for MRI
The Scientist's Toolkit: Essential Research Reagents and Materials
The experimental protocols rely on a combination of specialized hardware, software, and data resources.
Table 2: Key Research Reagents and Materials for Motion Correction Studies
| Item Name / Category | Function / Purpose | Example Use Case |
|---|---|---|
| High-Density Laminar Arrays (e.g., Neuropixels) | Records activity of hundreds of neurons simultaneously; subject to motion from pulsation and tissue decompression [55]. | Validating electrophysiology motion correction (MEDiCINe) [55]. |
| Diaphragmatic Navigator Echo | Provides a robust signal correlated with respiratory phase; used for gating or building motion models [56]. | Patient-specific prospective motion correction (PROCO) in cardiac MRI [56]. |
| External Physiological Monitor | Records cardiac and respiratory cycles via pulse oximetry and respiratory bellows during scanning [58]. | Providing a reference signal for adaptive filtering or RETROICOR methods [58]. |
| Motion Tracking Camera System | Tracks the position of an optical marker attached to the subject for high-precision, real-time motion detection [60]. | Prospective motion correction (PMC) in high-resolution anatomical MRI [60]. |
| Convolutional Neural Network (CNN) | Learns to identify and remove motion artifacts directly from image data after being trained on clean and corrupted image pairs [57]. | Deep learning-based artifact reduction (MARC) in liver MRI [57]. |
| Simulated Motion Dataset | Provides a benchmark with known ground-truth motion for controlled algorithm testing and validation [55]. | Quantitative evaluation of motion estimation accuracy in spike sorting [55]. |
The choice of a motion correction strategy is highly dependent on the imaging modality, the nature of the motion, and the required output. For handling the specific challenges of a-periodic breathing and patient-specific variability, model-based approaches like PROCO show significant promise by adapting to individual patient anatomy. For tremors and irregular neural probe motion, distributional inference methods like MEDiCINe offer robust performance. Meanwhile, deep learning techniques such as MARC provide a powerful, flexible post-processing solution that does not require protocol modification. Researchers must weigh factors such as acquisition efficiency, need for real-time correction, and availability of training data when selecting the optimal algorithm for their specific application.
Data Augmentation and Transfer Learning for Limited Training Datasets
In the field of medical imaging and computational drug development, the performance of deep learning models is often constrained by the limited availability of annotated training data. This challenge is particularly acute in specialized domains such as motion correction algorithm research, where acquiring large, well-annotated datasets is costly and time-consuming. Two predominant techniques have emerged to address this data scarcity problem: data augmentation and transfer learning [61].
Data augmentation artificially expands the training dataset by applying label-preserving transformations to existing data, while transfer learning leverages knowledge from pre-trained models developed for related tasks [62] [63]. Both approaches aim to enhance model generalization and prevent overfitting, though they operate through distinct mechanisms. This guide provides an objective comparison of these methodologies, supported by experimental data from medical imaging applications, to inform researchers and drug development professionals in selecting and implementing these strategies effectively.
Technical Foundations
Understanding Data Augmentation
Data augmentation encompasses a family of techniques that generate diversified training samples by applying transformations to existing data while preserving semantic meaning [62]. This approach falls under the broader category of regularization methods that help models capture generalizable properties rather than memorizing training specifics [62].
Common augmentation techniques include:
- Geometric transformations: Rotation, horizontal flip, zoom, shear transformation, and shifting [63]
- Photometric transformations: Brightness adjustment and channel shifting [63]
- Advanced techniques: CutMix and MixUp, which create new training examples by blending multiple images and their labels [63]
In medical imaging contexts, it is crucial to select augmentations that preserve clinical relevance. For bone morphology studies in femoroacetabular impingement research, affine transformations are often preferred as they retain the essential shape characteristics of bony structures [62].
Understanding Transfer Learning
Transfer learning repurposes knowledge gained from a source domain to improve learning in a target domain [62]. Formally, given a source domain (Ds) with task (Ts) and target domain (Dt) with task (Tt), transfer learning aims to enhance the target predictive function (fT(.)) using related information from (Ds) and (Ts), where (Ds \neq Dt) or (Ts \neq T_t) [62].
Common transfer learning implementation strategies:
- Replacing the head layer: Substituting the final classification layer to accommodate new output classes while freezing earlier layers [63]
- Adding a new dense network: Inserting additional layers before the output layer to capture task-specific features [63]
- Selective unfreezing: Gradually unfreezing and fine-tuning portions of the pre-trained network [63]
A critical limitation is that transfer learning requires architectural similarity between source and target models, particularly in their convolutional layers [62].
Comparative Performance Analysis
Experimental Data from Medical Imaging
A direct comparison study evaluated both techniques for segmenting bony structures of the hip joint from 3D MR images of patients with femoroacetabular impingement [62]. The researchers trained a deep learning model under three conditions: using data augmentation alone, transfer learning alone (from a shoulder joint segmentation model), and compared their performance against manual segmentations as ground truth.
Table 1: Performance Comparison of Data Augmentation vs. Transfer Learning for Hip Joint Segmentation
| Anatomical Region | Technique | Dice Similarity Coefficient | Accuracy |
|---|---|---|---|
| Acetabulum | Data Augmentation | 0.84 | 0.95 |
| Acetabulum | Transfer Learning | 0.78 | 0.87 |
| Femur | Data Augmentation | 0.89 | 0.97 |
| Femur | Transfer Learning | 0.88 | 0.96 |
The results demonstrate that data augmentation outperformed transfer learning for the acetabulum segmentation, while both techniques achieved comparable results for the femur [62]. The researchers hypothesized that transfer learning worked better for the femur because it resembles the humerus from the source domain (shoulder joint), while the acetabulum has a different topology than the glenoid, leading to poorer knowledge transfer [62].
Complementary Benefits and Limitations
Table 2: Characteristics of Data Augmentation and Transfer Learning
| Characteristic | Data Augmentation | Transfer Learning |
|---|---|---|
| Primary mechanism | Artificially expands dataset diversity | Leverages pre-trained model weights |
| Data requirements | Limited initial dataset sufficient | Requires large source dataset for pre-training |
| Computational cost | Generally low | Moderate to high (depending on fine-tuning extent) |
| Domain similarity sensitivity | Low | High (performance depends on source-target similarity) |
| Risk of negative transfer | None | Possible if domains are too dissimilar |
| Implementation complexity | Simple to moderate | Moderate to complex |
Methodology for Motion Correction Research
Experimental Protocols
In motion correction research for medical imaging, specific experimental protocols have been developed to validate both data augmentation and transfer learning approaches.
Data Augmentation Protocol for Motion-Corrupted Images:
- Acquire a baseline dataset of motion-affected images (e.g., from pediatric fNIRS or PET studies) [64] [65]
- Apply motion-specific transformations including simulated rigid body transformations, signal spikes (Type A artifacts: SDThresh=50, tMotion=1s), and slow baseline shifts (Type D artifacts) [64]
- Incorporate advanced techniques like MixUp for blended examples: Mixed_image = λ × image1 + (1-λ) × image2 with mixed labels [63]
- Train models on the augmented dataset with appropriate regularization
Transfer Learning Protocol for Motion Correction:
- Select a model pre-trained on a related domain (e.g., shoulder joint segmentation for hip applications, or natural images for medical imaging) [62]
- Adapt the model architecture by replacing the final layers to match motion correction tasks
- Employ progressive fine-tuning, starting with higher learning rates for new layers
- Validate on target domain data with different motion patterns (e.g., respiratory motion in abdominal MRI vs. head motion in PET) [66] [65]
Research Reagent Solutions
Table 3: Essential Research Tools for Limited Data Scenarios
| Research Tool | Type | Function in Research |
|---|---|---|
| HOMER2 Software Package [64] | Software | fNIRS processing and motion artifact identification |
| Deep Learning Frameworks (PyTorch/TensorFlow) | Software | Implementing and fine-tuning neural network models |
| Dual-Camera Tracking Systems [66] | Hardware | Markerless motion tracking for generating ground truth data |
| Pilot-Tone Navigation [66] | Method | Motion detection without external sensors for abdominal MRI |
| Supervised Deep Learning with Attention (DL-HMC++) [65] | Algorithm | PET head motion estimation using attention mechanisms |
| Wavelet-Based Correction [64] | Algorithm | Motion artifact correction in fNIRS data |
| MixUp and CutMix [63] | Data Augmentation | Advanced regularization through image blending and patching |
| Pre-trained Models (e.g., VGG16) [63] | Model Architecture | Transfer learning backbone for feature extraction |
Implementation Workflows
Data Augmentation Workflow
The following diagram illustrates the systematic workflow for implementing data augmentation in motion correction studies:
Transfer Learning Workflow
For transfer learning implementation, the following systematic approach has proven effective:
Integration in Motion Correction Algorithms
Application in Medical Imaging Modalities
The comparative effectiveness of data augmentation and transfer learning varies across medical imaging modalities used in motion correction research:
fNIRS Motion Correction: Wavelet-based methods and moving average techniques have shown superior performance for correcting motion artifacts in pediatric functional near-infrared spectroscopy data [64]. Data augmentation is particularly valuable here due to the challenging nature of acquiring clean data from children populations.
PET Head Motion Correction: Deep learning approaches with attention mechanisms (DL-HMC++) have successfully estimated rigid head motion from 3D PET raw data, achieving performance comparable to hardware-based motion tracking with average difference ratios of 1.2±0.5% for HRRT scanners [65]. Transfer learning can accelerate deployment across different radiotracers.
Musculoskeletal MRI: At low-field strengths (0.4T), deep learning reconstruction networks like CIRIM have enabled up to four-fold acceleration, demonstrating how transfer learning from high-field applications can enhance accessibility [66].
Synergistic Implementation
The most effective motion correction pipelines often combine both techniques strategically:
- Initial Phase: Utilize transfer learning to bootstrap models with general feature extraction capabilities from related domains [62] [61]
- Refinement Phase: Apply domain-specific data augmentation to enhance robustness to specific motion artifacts prevalent in the target application [64]
- Validation Phase: Employ rigorous testing against multiple artifact types (Type A-D) to ensure comprehensive performance [64]
This combined approach leverages the knowledge transfer benefits of pre-trained models while exploiting the regularization advantages of data augmentation, ultimately yielding models with superior generalization across diverse motion scenarios encountered in clinical and research settings.
Performance Metrics, Clinical Validation, and Cross-Algorithm Benchmarking
In the field of medical imaging, motion correction algorithms are essential for mitigating artifacts introduced by patient movement, thereby enhancing diagnostic clarity and quantitative analysis. Evaluating the efficacy of these algorithms relies heavily on a suite of objective, quantitative performance metrics. This guide provides a comparative analysis of contemporary motion correction methods, focusing on their performance as measured by key indicators such as Signal-to-Noise Ratio (SNR), Structural Similarity Index Measure (SSIM), Visual Information Fidelity (VIF), and Resolution Measurements. These metrics offer insights into different aspects of image quality, from noise levels and structural preservation to perceptual quality and sharpness. The following sections synthesize experimental data from recent research, present detailed methodologies, and provide visualizations to aid researchers, scientists, and drug development professionals in objectively assessing the landscape of motion correction technologies.
Comparative Performance of Motion Correction Algorithms
The following tables summarize the quantitative performance of various deep learning-based motion correction algorithms as reported in recent scientific studies. The data is drawn from evaluations on different medical imaging modalities, including High-Resolution peripheral Quantitative Computed Tomography (HR-pQCT) and Magnetic Resonance Imaging (MRI).
Table 1: Performance Comparison of Motion Correction Algorithms on HR-pQCT Data
| Algorithm | Dataset | SNR (dB) | SSIM | VIF | Key Architectural Features |
|---|---|---|---|---|---|
| ESWGAN-GP [17] | Source (Simulated) | 26.78 | 0.81 | 0.76 | Wasserstein GAN with Gradient Penalty, Self-Attention, Edge-enhancing Skip Connections |
| ESWGAN-GP [17] | Target (Real-world) | 29.31 | 0.87 | 0.81 | Wasserstein GAN with Gradient Penalty, Self-Attention, Edge-enhancing Skip Connections |
Table 2: Performance of MRI Motion Correction Algorithms across Different Distortion Levels
| Algorithm | Distortion Level | PSNR (dB) | SSIM | NMSE | Key Architectural Features |
|---|---|---|---|---|---|
| Res-MoCoDiff [67] | Minor | 41.91 ± 2.94 | Not Specified | Lowest | Residual-guided Diffusion, Swin Transformer, 4-Step Reverse Process |
| Res-MoCoDiff [67] | Moderate | High (Best) | High (Best) | Lowest | Residual-guided Diffusion, Swin Transformer, 4-Step Reverse Process |
| Res-MoCoDiff [67] | Heavy | High (Best) | High (Best) | Lowest | Residual-guided Diffusion, Swin Transformer, 4-Step Reverse Process |
| CycleGAN [67] | Various | Lower | Lower | Higher | Cycle-Consistent Adversarial Networks |
| Pix2Pix [67] | Various | Lower | Lower | Higher | Conditional Adversarial Networks |
Detailed Experimental Protocols and Methodologies
Protocol for HR-pQCT Motion Correction with ESWGAN-GP
The development and validation of the ESWGAN-GP model for HR-pQCT involved a structured pipeline comprising motion simulation, model training, and quantitative evaluation [17].
- Motion Simulation and Paired Dataset Creation: A critical first step was the generation of a large-scale paired dataset. Researchers optimized a sinogram-based method to simulate in-plane rigid motion artifacts in originally motion-free HR-pQCT images. This process involved applying random alterations to the sinogram data, which were then reconstructed using the Simultaneous Iterative Reconstruction Technique (SIRT) to produce realistic motion-corrupted images. This created the necessary paired data (motion-corrupted and ground truth) for supervised learning [17].
- Network Architecture and Training: The proposed ESWGAN-GP model incorporates several advanced components. The backbone is a Wasserstein Generative Adversarial Network with Gradient Penalty (WGAN-GP) to improve training stability. The generator is a U-Net equipped with Sobel-kernel-based convolutional layers in its skip connections to explicitly preserve and enhance trabecular bone edges. Furthermore, self-attention mechanisms are used in both the generator and discriminator to capture long-range spatial dependencies within the image. The model was trained using a combination of adversarial loss and a VGG-based perceptual loss to ensure the reconstruction of fine micro-structural features [17].
- Quantitative Validation: The model's performance was quantitatively assessed on both a simulated source dataset and a real-world target dataset. The evaluation employed the metrics of SNR, SSIM, and VIF to measure noise reduction, structural preservation, and perceptual image fidelity, respectively [17].
Protocol for MRI Motion Correction with Res-MoCoDiff
The Res-MoCoDiff framework introduced an efficient diffusion model tailored for correcting motion artifacts in brain MRI.
- Problem Formulation and Residual Guidance: Unlike conventional denoising diffusion probabilistic models (DDPMs) that start the reverse process from pure Gaussian noise, Res-MoCoDiff leverages the residual error ((r = y - x)) between the motion-corrupted image ((y)) and the motion-free ground truth ((x)). This residual is integrated into the forward diffusion process, resulting in a noisy image whose probability distribution closely matches the corrupted data. This key innovation allows the reverse diffusion process to accurately reconstruct the image in as few as four steps, drastically reducing inference time [67].
- Model Architecture: The model utilizes a U-Net backbone where standard attention layers are replaced with Swin Transformer blocks. This enhances the model's robustness and its ability to handle features across different resolutions. The training process also incorporates a combined ( \ell 1 + \ell 2 ) loss function to minimize pixel-level errors while promoting image sharpness [67].
- Experimental Evaluation: The model was rigorously evaluated on both an in-silico dataset, generated using a realistic motion simulation framework, and an in-vivo dataset with clinical motion artifacts. Performance was compared against established baselines like CycleGAN and Pix2Pix using PSNR, SSIM, and Normalized Mean Squared Error (NMSE). Res-MoCoDiff achieved superior scores across all distortion levels (minor, moderate, and heavy) and reduced the average sampling time to 0.37 seconds per batch of image slices [67].
General Workflow for Motion Correction Analysis
The experimental process for developing and validating a motion correction algorithm typically follows a logical sequence, from data preparation to final evaluation, as visualized below.
The Scientist's Toolkit: Essential Research Reagents and Materials
The experimental studies referenced rely on a combination of software, hardware, and phantom models to conduct controlled and valid research.
Table 3: Key Research Reagents and Materials for Motion Correction Studies
| Item Name | Type | Function in Research | Example/Reference |
|---|---|---|---|
| NEMA-IEC Body Phantom | Physical Phantom | A standardized phantom used to simulate human anatomy and lesions in a controlled environment, allowing for quantitative measurement of recovery coefficients and contrast-to-noise ratio. | Used in PET-CT motion correction studies [68] [51]. |
| Motion Simulation Platform | Hardware/Software | A system to physically move a phantom or to computationally simulate motion in software. It introduces known, reproducible motion artifacts for algorithm training and testing. | Custom moving platform for PET-CT [68]; Sinogram-domain simulation for HR-pQCT [17]. |
| ESWGAN-GP Model | Software Algorithm | A deep learning model designed to correct rigid motion artifacts by combining adversarial training, edge enhancement, and self-attention mechanisms. | Used for HR-pQCT bone image correction [17]. |
| Res-MoCoDiff Model | Software Algorithm | An efficient diffusion model that uses residual guidance for fast (4-step) and high-fidelity correction of motion artifacts in MRI. | Used for brain MRI motion correction [67]. |
| Data-Driven Motion Correction (DDMC) | Software Algorithm | A vendor-implemented technique, often incorporating AI, that uses PET raw data to estimate and correct for respiratory motion without external devices. | OncoFreeze AI (Siemens) [68] [51]. |
Phantom Studies and Ground Truth Validation for Technical Assessment
The rigorous technical assessment of medical imaging technologies, particularly motion correction algorithms, relies on a foundational principle: the ability to measure performance against a known standard. Phantom studies provide this controlled, reproducible framework, while the concept of ground truth validation ensures that measurements accurately reflect reality. Within the context of comparing motion correction algorithms, these methodologies are indispensable for generating objective, comparable performance data free from the biological variability and unknown ground truths inherent in clinical patient studies. This guide details the experimental frameworks and analytical tools required for such technical comparisons, providing a standardized approach for researchers and development professionals.
The Role of Phantoms and Ground Truth in Technical Assessment
Phantom studies serve as the cornerstone for the controlled evaluation of imaging technologies across all modalities. They provide a reproducible environment for technology validation, performance benchmarking, protocol optimization, and quality assurance [69]. In the specific context of motion correction algorithm research, their value is twofold. First, they allow for the precise introduction and control of motion patterns, which is often difficult or unethical in patient studies. Second, and more critically, they provide a known ground truth—the exact, uncontested state of the system being imaged, be it an object's position, shape, or internal activity concentration.
Ground truth validation is the process of verifying that an algorithm's output matches this known state. Without it, performance claims are relative at best. For example, a motion correction algorithm can only be proven to work if the "correct" or "true" position of a structure is known beforehand, allowing for a direct measurement of the algorithm's correction error [70] [71]. This is distinct from clinical validation, where the "truth" is often a clinical diagnosis or outcome. Technical assessment via phantoms provides a necessary, intermediate step of proving algorithmic efficacy under controlled conditions before proceeding to more variable clinical trials.
Experimental Design and Methodologies
Core Principles for Phantom Study Design
A well-designed phantom study begins with a precisely defined scientific question. The objectives must be explicit, structured, and maintained throughout the research to avoid ambiguous conclusions or retrospective "p-hacking" of data [69].
Table 1: Framing Study Objectives for Motion Correction Algorithm Comparison
| Purpose Category | Well-Defined Objective Example | Poorly-Defined Objective to Avoid |
|---|---|---|
| Technology Validation | "To evaluate the accuracy of a novel deep-learning motion correction algorithm in reducing motion artifacts in cardiac CT using an anthropomorphic phantom with simulated arrhythmia." | "To see if this AI algorithm makes cardiac images better." |
| Performance Comparison | "To compare the motion-induced error in coronary artery sharpness and myocardial wall definition for algorithms A, B, and C using a physical dynamic cardiac phantom." | "To see which motion correction algorithm is best." |
| Protocol Optimization | "To determine the optimal acquisition window for the SCULLI motion correction algorithm across a range of simulated heart rates (40-120 bpm) in an XCAT software phantom." | "To find the best settings for our scanner." |
Beyond objective-setting, key methodological considerations include:
- Phantom Selection: The choice of phantom must align with the study's goal. Standard synthetic phantoms (e.g., PMMA) are ideal for measuring basic parameters like resolution and noise, while anthropomorphic phantoms are necessary for evaluating anatomical realism and algorithm performance in a clinically relevant context [69] [72].
- Quantitative Analysis: Image quality must be assessed through objective, quantitative metrics. Common measures include Signal-to-Noise Ratio (SNR), Contrast-to-Noise Ratio (CNR), and metrics for spatial resolution like the Modulation Transfer Function (MTF) [69] [73].
- Qualitative Assessment: When human readers are involved, studies must employ rigorous methodology including reader training, blinding, randomization, and validated rating scales to minimize bias [69].
- Statistical Rigor: The study must include an appropriate sample size calculation, correct statistical tests for group comparisons, and assessments of inter-rater agreement for qualitative data [69].
Detailed Experimental Protocols
The following are detailed methodologies for key experiment types cited in motion correction research.
1. Ground Truth Validation for a Respiratory Motion Model This protocol, adapted from a study validating a 5DCT technique for lung cancer radiotherapy, outlines how to use acquired images as a ground truth [70].
- Objective: To assess the accuracy of a breathing phase-specific volume image generation process using the original free-breathing CT scans as ground truths.
- Phantom/Subjects: In a clinical setting, this uses patients or a highly realistic anthropomorphic phantom. Sixteen lung cancer patients were scanned under an IRB-approved protocol [70].
- Image Acquisition: Acquire multiple (e.g., 25) fast helical CT scans of the thoracic region simultaneously with a breathing surrogate signal (e.g., an abdominal bellows). The fast acquisition (e.g., 0.23 seconds per slice) "freezes" motion, providing a static, instantaneous representation of anatomy that serves as the ground truth [70].
- Motion Model Construction: Arbitrarily select one scan as a reference image. Use a state-of-the-art deformable image registration (DIR) algorithm to register the reference to the other 24 scans, generating 24 deformation vector fields (DVFs). Relate these DVFs to the recorded breathing amplitude and rate to build a patient-specific motion model [70].
- Ground Truth Comparison: Use the motion model to reconstruct ("simulate") the original 25 scans. Deformably register the simulated images to their original ground truth counterparts. The magnitude of the resulting deformation vector at each voxel is the direct measure of the motion model's misalignment error [70].
- Outcome Measures: Grand mean misalignment error across all scans (e.g., 1.15 ± 0.37 mm) and the grand mean of the 95th percentile error (e.g., 2.47 ± 0.78 mm) to characterize worst-case performance [70].
2. Phantom-Based Validation of a Deep-Learning Denoising Algorithm This protocol demonstrates how phantoms with known properties can systematically evaluate AI performance [74].
- Objective: To investigate the performance, limitations, and generalizability of a deep-learning algorithm for denoising ultra-low-count PET images.
- Phantom: A NEMA PET body phantom filled with
[^18F]FDGwith known sphere-to-background activity concentration ratios (e.g., 4:1 and 10:1). To simulate obese patients, the phantom can be wrapped in material that increases attenuation [74]. - Image Acquisition: Scan the phantom in list mode for a long duration (e.g., 900 s). This allows the dataset to be reconstructed into 13 different frame durations, simulating a range from ultra-low to high count statistics [74].
- Algorithm Processing: Process the reconstructed images from all acquisition durations with the deep-learning network (e.g., a pix2pixHD GAN) to generate AI-enhanced PET (AI-PET) images.
- Outcome Measures:
- Quantitative Accuracy: Recovery coefficients for spheres of different sizes, SUV differences from known activity.
- Image Quality: Structural Similarity Index Metric (SSIM), Contrast-to-Noise Ratio (CNR).
- Lesion Detectability: The minimum lesion size and count level at which the algorithm fails to recover a lesion.
3. Motion Correction Validation from Phantom to Clinical Experience This protocol describes a stepwise approach for validating a cardiac motion correction algorithm (SCULLI) [75].
- Objective: To explore the motion correction capability of an algorithm for both coronary arteries and other heart structures, including the myocardial wall.
- Software Phantom Test: Use a digital phantom (e.g., XCAT) with a known ground truth geometry. Simulate a CT acquisition process, introducing known motion patterns. Reconstruct images with and without the motion correction algorithm.
- Physical Phantom Test: Use a commercially available dynamic physical phantom (e.g., Mocomo). Scan the phantom while it executes programmed motion. Use the stationary scan as a ground truth for comparison.
- Outcome Measures:
- Software Phantom: Structural similarity (SSIM) of coronary arteries and the whole heart; Root Mean Square Error (RMSE) of the whole heart image compared to the static ground truth.
- Physical Phantom: Qualitative scoring by experienced radiologists (e.g., on a 1-5 scale for coronary artery visualization).
- In-Vivo Studies: Proceed to animal and human studies to confirm performance in a biological, clinical context after phantom validation [75].
Comparative Performance Data
The following tables synthesize quantitative data from phantom studies to enable direct comparison of technologies and their performance under specific test conditions.
Table 2: Quantitative Motion Model Accuracy from Ground Truth Validation
| Motion Model / Application | Ground Truth Method | Mean Error | 95th Percentile Error | Key Finding |
|---|---|---|---|---|
| 5DCT Respiratory Motion Model [70] | Fast helical CT scans (0.23s/slice) | 1.15 ± 0.37 mm | 2.47 ± 0.78 mm | Technique accurately reproduced original scans despite varied breathing patterns. |
| Cardiac CT (SCULLI) on XCAT Phantom [75] | Static XCAT software phantom | RMSE: 20.27 (Proposed) vs 25.33 (FBP) | Not Reported | Motion correction significantly reduced deviation from static ground truth (p=0.01). |
| Cardiac CT (SCULLI) on XCAT Phantom [75] | Static XCAT software phantom | SSIM: 0.94 (Proposed) vs 0.77 (FBP) | Not Provided | Significant improvement in structural similarity of coronary arteries (p<0.001). |
Table 3: Phantom-Based AI Algorithm Performance Assessment
| AI Algorithm / Application | Phantom & Test Conditions | Key Performance Metrics | Identified Limitations |
|---|---|---|---|
| Deep-learning Denoising for PET [74] | NEMA body phantom; Spheres: 10-37mm; Statistics: 5-900s. | Performs well denoising ultra-low count images. Accurately recovers quant. measures for large lesions (≥37mm). Outperforms Gaussian post-filtering. | Strong SUV underestimation in small lesions (≤17mm). Fails to recognize small lesions (≤13mm) in low-count/contrast. Increases noise in ultra-high count scans. |
| CNN-based Denoising for fMRI [71] | Dynamic "resting-state" phantom. | 4- to 7-fold increase in Standardized SNR. 40-70% increase in Dynamic Fidelity. Outperformed bandpass & PCA filtering. | Scanner-induced non-linearity found in 8-19% of voxels. |
Table 4: System-to-System Technical Performance Comparison
| Imaging Systems / Modality | Performance Metric | Result Range | Implication |
|---|---|---|---|
| Five Digital Breast Tomosynthesis (DBT) Systems [73] | In-Plane Resolution (MTF₅₀) | 1.1 - 1.6 mm⁻¹ (tube direction)1.5 - 4.1 mm⁻¹ (chest-wall-nipple) | Clear anisotropy and system-level differences that may impact clinical detection. |
| Five Digital Breast Tomosynthesis (DBT) Systems [73] | Artefact Spread (ASF-FWHM) | 3.5 - 10.7 mm | Remarkable variation, with wider angular ranges generally providing improved depth resolution. |
Visualizing Workflows and Relationships
Ground Truth Validation Workflow
The following diagram illustrates the multi-stage process for validating a motion model against a known ground truth.
Motion Correction Algorithm Comparison Framework
This diagram outlines the high-level strategy for comparing multiple motion correction algorithms in a standardized and objective manner.
The Scientist's Toolkit
Table 5: Essential Research Reagents and Materials for Phantom Studies
| Item | Function / Application | Key Characteristics |
|---|---|---|
| NEMA PET Body Phantom [74] | Validating quantitative accuracy, lesion detectability, and noise properties in PET. | Contains spheres of various sizes for recovery coefficients; fillable with known activity concentrations. |
| Anthropomorphic Phantoms (e.g., Alderson Rando) [72] | Dosimetry, protocol optimization, and clinically-relevant algorithm testing. | Mimics human anatomy and tissue properties (attenuation, density). |
| Software Phantoms (e.g., XCAT) [75] | Flexible, high-precision testing of image reconstruction and motion correction algorithms. | Digital models offering perfect ground truth and total control over parameters. |
| Dynamic Motion Phantoms (e.g., Mocomo) [75] | Specific validation of motion correction algorithms. | Capable of programmed, reproducible movements (linear, rotational, complex). |
| Deformable Image Registration (DIR) Algorithm [70] | Core component for building motion models and calculating voxel-wise errors. | High accuracy and ability to handle sliding motion (e.g., deeds algorithm). |
| Standardized Image Quality Phantoms (e.g., PMMA) [69] [73] | Measuring fundamental parameters: MTF, NPS, CNR, SNR. | Made of simple, well-characterized, tissue-equivalent materials. |
Clinical Reader Studies and Diagnostic Quality Evaluation
Clinical reader studies are structured research protocols in which multiple radiologists or physicians evaluate sets of medical images to assess diagnostic accuracy, compare imaging technologies, or validate artificial intelligence algorithms [76]. These studies form the backbone of evidence-based imaging research and are crucial for translating technological advances into clinical practice. Within the hierarchical model of diagnostic efficacy proposed by Fryback and Thornbury, reader studies primarily operate at Level 2, which addresses diagnostic accuracy, sensitivity, and specificity associated with image interpretation [77]. This level is fundamental as it demonstrates whether an improvement in technical image quality translates into genuine clinical benefits for patient diagnosis [77].
The design and execution of reader studies are particularly relevant for evaluating motion correction algorithms in medical imaging. Patient motion during image acquisition—especially in cardiac magnetic resonance (CMR) perfusion examinations or neurological MRI—can introduce artifacts that reduce diagnostic value [78] [9]. Reader studies provide the methodological framework to determine whether proposed motion correction techniques meaningfully improve diagnostic interpretation compared to existing methods or uncorrected images.
Designing the "Perfect" Reader Study
Core Components of Study Design
A well-designed reader study requires careful planning and consideration of multiple factors to create a controlled environment that produces reliable, statistically significant results while maintaining real-world applicability [76]. The key components, as illustrated in the diagram below, form an interconnected framework where decisions in one area directly impact others.
Diagram Title: Core Components of Reader Study Design
Essential Research Reagents and Materials
The following table details key components required for implementing a robust reader study, particularly in the context of evaluating motion correction algorithms:
| Research Component | Function & Purpose | Specification Guidelines |
|---|---|---|
| Reader Panel | Provide expert image interpretation and diagnostic decisions | 3-20 radiologists with relevant subspecialty expertise; balance experience levels [76] |
| Case Collection | Represent target patient population and clinical scenarios | Include range of disease prevalence, case difficulty, image quality; sufficient sample size for statistical power [77] [76] |
| Reference Standard | Establish ground truth for diagnostic accuracy assessment | Use histology, clinical follow-up, or expert consensus; apply consistently to all cases [79] [77] |
| Reading Environment | Standardize interpretation conditions across readers | Consistent display monitors, calibrated equipment, controlled lighting, ergonomic setup [76] |
| Motion Correction Algorithms | Target interventions for performance comparison | Include multiple algorithmic approaches (rigid, affine, non-rigid); benchmark against ground truth [78] |
Controlling Bias in Reader Studies
Minimizing bias is crucial for ensuring reader study validity and generalizability. The table below outlines common bias types and their control strategies:
| Bias Type | Impact on Results | Control Strategies |
|---|---|---|
| Reader/Interpretation Bias | Inconsistent application of diagnostic criteria | Standardized reader training, clear reporting criteria, structured response forms [77] [76] |
| Context Bias | Prior knowledge influences current interpretation | Randomize case presentation, blind readers to clinical information not normally available [79] [77] |
| Recall/Memory Bias | Reader remembers previous cases | Separate reading sessions with washout periods, counterbalanced reading order [77] |
| Prevalence Bias | Abnormal case frequency affects sensitivity | Realistic disease prevalence in case selection, avoid enriched datasets [76] |
| Verification Bias | Reference standard not applied uniformly | Apply reference standard to all cases regardless of test results [77] |
Motion Correction Algorithms: A Case Study in Reader Study Implementation
Motion Correction Algorithm Comparison Framework
The evaluation of motion correction algorithms presents a compelling application of reader study methodology. In cardiac MRI, for example, motion between frames due to breathing must be corrected before quantitative analysis of myocardial blood flow [78]. Several algorithmic approaches have been developed, employing different motion models and similarity metrics. The diagram below illustrates a generalized workflow for comparing these algorithms through a reader study:
Diagram Title: Motion Correction Algorithm Evaluation Workflow
Benchmark Data: Motion Correction Algorithm Performance
An open benchmark challenge compared 19 different motion correction algorithms for cardiac MR perfusion imaging, employing the rigorous reader study methodology outlined above [78]. The quantitative results from this benchmark provide valuable comparative data:
Table: Motion Correction Algorithm Performance in Cardiac MR Perfusion Benchmark
| Algorithm Category | Similarity Metric | Motion Model | Myocardial Blood Flow (Ktrans) Bias | Myocardial Perfusion Reserve (MPR) | Statistical Significance |
|---|---|---|---|---|---|
| Rigid Transformation | Sum-of-Squared Differences | Translation + Rotation | No significant bias | Comparable to ground truth | No significant difference |
| Global Affine | Mutual Information | Scaling + Shear + Rotation | No significant bias | Comparable to ground truth | No significant difference |
| Local Deformation | Cross-Correlation | Non-rigid/Free-form | Significant bias detected | Comparable to ground truth | p < 0.05 for Ktrans bias |
| Multiple Approaches | Various | Various | No significant bias for most metrics | Comparable across methods | No benefit of non-rigid over simpler methods |
This comprehensive comparison demonstrated that there was no statistically significant benefit of non-rigid registration techniques over simpler rigid or affine transformations for quantifying myocardial perfusion [78]. This finding highlights the importance of empirical validation through well-designed reader studies, as theoretical advantages of more complex algorithms do not always translate to improved clinical performance.
Advanced Hybrid Approaches in Motion Correction
Recent methodological advances have focused on hybrid approaches that combine deep learning with physical models of motion corruption. The UNet+JE method, for example, integrates a neural network with a physics-informed joint estimation algorithm for 3D motion correction [9]. This hybrid approach demonstrated several advantages in reader study evaluations:
Performance: UNet+JE provided significantly better motion correction than neural-network-only approaches (p < 10⁻² for all metrics) and matched the quality of traditional joint estimation methods (p > 0.05 for all metrics) while being substantially faster [9]
Efficiency: The method reduced runtimes by a median reduction factor between 2.00 to 4.05 compared to conventional joint estimation approaches [9]
Robustness: UNet+JE exhibited less susceptibility to data distribution shifts than neural-network-only methods, maintaining performance across varying levels of motion corruption severity [9]
Best Practices in Reader Study Implementation
Reader Management and Standardization
The human element of reader studies requires careful management to ensure consistent and reliable results. Key considerations include:
Reader Selection: Balance subspecialty expertise, clinical experience, and time availability. Most studies require between 3-20 readers, with the exact number determined by statistical power requirements [76]
Training and Standardization: Conduct comprehensive training sessions before formal reading sessions to establish clear interpretation criteria and familiarize readers with assessment tools [76]
Reading Session Management: Limit reading sessions to 2-3 hours to minimize fatigue effects; randomize case presentation order across readers to counterbalance learning and memory effects [77] [76]
Statistical Considerations and Sample Size
Robust statistical design is essential for drawing valid conclusions from reader studies:
Multi-reader, Multi-case (MRMC) Design: Account for both reader and case variability in the analysis, typically using specialized statistical methods like MRMC variance analysis of ROC curves [77]
Sample Size Calculation: Determine case and reader numbers based on expected effect size, desired statistical power (typically 80% or higher), and anticipated variability between readers [76]
Appropriate Metrics: Select primary endpoints that match study objectives, such as area under the ROC curve (AUC) for diagnostic accuracy, sensitivity and specificity for classification performance, or quantitative perfusion parameters for motion correction studies [78] [77]
Clinical reader studies provide an essential methodological framework for evaluating motion correction algorithms and other medical imaging technologies. The rigorous comparison of 19 different motion correction methods [78] demonstrates how well-designed reader studies can generate evidence-based insights that challenge conventional assumptions—in this case, revealing that computationally complex non-rigid registration techniques offered no significant advantage over simpler methods for perfusion quantification.
As motion correction algorithms continue to evolve, particularly with the integration of deep learning and physical modeling approaches [9], reader studies will remain indispensable for validating their clinical utility. By adhering to established best practices in study design, reader management, bias control, and statistical analysis, researchers can ensure their findings are both scientifically valid and clinically relevant, ultimately supporting the advancement of medical imaging for improved patient diagnosis and care.
Motion artifacts present a significant challenge across various medical imaging modalities, compromising image quality and diagnostic accuracy. The pursuit of robust motion correction has led to the development of three predominant methodological approaches: traditional/model-based, classical machine learning (ML), and deep learning (DL) techniques. Traditional methods often rely on explicit physical or geometric models of motion, while classical ML algorithms learn patterns from hand-crafted features. In contrast, deep learning models, particularly deep neural networks, learn hierarchical feature representations directly from raw data. This guide provides a comparative analysis of these methodologies, focusing on their architectural principles, performance metrics, and suitability for different clinical and research scenarios within medical imaging.
Performance Comparison at a Glance
The table below summarizes the core characteristics and quantitative performance of the three main motion correction methodologies based on recent research.
Table 1: Comparative Analysis of Motion Correction Methodologies
| Aspect | Traditional/Model-Based Methods | Classical Machine Learning Methods | Deep Learning Methods |
|---|---|---|---|
| Core Principle | Incorporates physical/motion models directly into reconstruction [36] [80] | Uses algorithms to learn patterns from pre-defined features [81] [82] | Learns hierarchical features directly from raw data using multi-layered neural networks [81] [48] |
| Data Requirements | Often uses the acquired projection or k-space data itself [36] | Effective with small-to-medium, structured datasets [81] [82] | Requires large-scale datasets (thousands to millions of examples) [81] [82] |
| Feature Engineering | Not applicable; relies on model parameters | Heavy reliance on manual feature engineering and domain expertise [81] [82] | Automatic feature learning; minimal manual engineering [81] [48] |
| Key Example | MCIR [80], CBCT-MOTUS [36] | Feature-based registration [81] | UniMo [48], Res-MoCoDiff [67], MC-RED [83] |
| Reported Performance (SSIM) | Information not explicitly quantified in results | Information not explicitly quantified in results | Up to ~0.95 (Res-MoCoDiff on minor distortions) [67] |
| Reported Performance (PSNR) | Information not explicitly quantified in results | Information not explicitly quantified in results | Up to 41.91 dB (Res-MoCoDiff) [67] |
| Computational Cost | High (iterative optimization on non-convex functions) [48] | Lower; runs on CPUs, faster training/inference [81] [82] | Very High; requires GPUs/TPUs, longer training [81] [48] |
| Strengths | Strong theoretical foundation, direct data usage [36] [80] | Interpretability, efficiency with small data, lower cost [81] [82] | High accuracy on complex tasks, handles unstructured data, state-of-the-art performance [81] [48] [67] |
| Weaknesses | Narrow capture range for large motions, can be slow [48] | Performance plateaus with complex data, requires domain expertise for features [81] | "Black box" nature, high data and compute needs, longer training times [81] [82] |
Detailed Experimental Protocols
To ensure the reproducibility of the results cited in this guide, this section outlines the key experimental methodologies employed in the featured studies.
Deep Learning Protocol: The UniMo Framework
The Unified Motion Correction (UniMo) framework is designed to correct both rigid and non-rigid motion across multiple imaging modalities without requiring retraining [48].
- Architecture: The model uses an alternating optimization scheme. It integrates an equivariant neural network for global rigid motion correction and an encoder-decoder network for estimating local deformations. A geometric deformation augmenter enhances robustness by addressing distortions and generating augmented training data [48].
- Training: The framework was trained on fetal MRI, a challenging application due to large rigid and non-rigid motion coupled with wide appearance variations. The model was trained using a unified loss function that jointly optimizes for both types of motion [48].
- Validation: The trained model was evaluated, without any retraining, on several unseen datasets including MedMNIST, lung CT, and BraTS. Performance was measured against existing motion correction methods in terms of accuracy and stability [48].
Deep Learning Protocol: The Res-MoCoDiff Model
Res-MoCoDiff is an efficient diffusion model designed for MRI motion artifact correction [67].
- Architecture: The model employs a U-net backbone where standard attention layers are replaced with Swin Transformer blocks to enhance robustness across resolutions. Its key innovation is a novel residual error shifting mechanism during the forward diffusion process, which incorporates information from the motion-corrupted images [67].
- Training: The model was trained with a combined ( \ell1 + \ell2 ) loss function to promote image sharpness and reduce pixel-level errors. It was evaluated on both an in-silico dataset (generated using a realistic motion simulation framework) and an in-vivo dataset with movement-related artifacts [67].
- Validation: Quantitative metrics included Peak Signal-to-Noise Ratio (PSNR), Structural Similarity Index Measure (SSIM), and Normalized Mean Squared Error (NMSE). Res-MoCoDiff was compared against established methods like cycle-GAN, Pix2Pix, and a Vision Transformer-based diffusion model [67].
Model-Based Protocol: The CBCT-MOTUS Framework
CBCT-MOTUS is a gate-less, model-based method for motion correction in Cone Beam CT [36].
- Architecture: The framework performs joint reconstruction by alternating between a motion estimation step and an image correction step. Motion estimation is model-based, performed directly in projection space by comparing acquired projections to simulated projections that account for motion-fields. The model exploits motion's spatio-temporal correlation using a low-rank motion model and enforces smoothness via spatial regularization [36].
- Validation: The method was tested in silico, on phantoms, and on clinical in vivo acquisitions. It was designed to estimate motion with high temporal resolution (182 ms per projection) and correct for both periodic and irregular motion without relying on periodicity assumptions [36].
Traditional Protocol: MCIR vs. RTA in PET
This study statistically compared two fundamental motion-correction approaches in Positron Emission Tomography (PET) [80].
- Method 1: Reconstruct-Transform-Average (RTA)
- Individual reconstructions of each gated data are performed.
- These reconstructions are then transformed into a reference gate.
- Finally, the transformed images are averaged together [80].
- Method 2: Motion-Compensated Image Reconstruction (MCIR)
- Motion information is directly incorporated within the iterative reconstruction algorithm itself (based on the Ordered Subsets Expectation Maximization algorithm) [80].
- Experimental Setup: Motion information was obtained from a dynamic MR acquisition on a human volunteer. Concurrent PET data were simulated from this dynamic MR data. Both techniques were assessed using multiple realizations to accurately define the noise properties and bias in the reconstructed images [80].
Workflow and Signaling Diagrams
The following diagrams illustrate the logical workflows and core architectures of the key motion correction methods discussed.
Traditional Model-Based Motion Correction Workflow
Deep Learning Motion Correction Workflow
Res-MoCoDiff Residual-Guided Diffusion Process
The Scientist's Toolkit
This section details key computational tools, software libraries, and data resources essential for implementing and experimenting with the motion correction methods discussed.
Table 2: Essential Research Reagents and Tools for Motion Correction Research
| Tool/Resource Name | Type | Primary Function | Relevant Context |
|---|---|---|---|
| PyTorch / TensorFlow | Software Library | Open-source frameworks for building and training deep learning models. | Essential for implementing DL architectures like UniMo [48] and Res-MoCoDiff [67]. |
| scikit-learn / XGBoost | Software Library | Provides efficient implementations of classical ML algorithms. | Ideal for developing and deploying traditional ML models for structured data tasks [81]. |
| U-Net | Neural Network Architecture | A convolutional auto-encoder with skip connections, excellent for image-to-image tasks. | Used as the backbone in many image-based correction models, including Res-MoCoDiff [67]. |
| Swin Transformer | Neural Network Component | A transformer architecture with hierarchical feature maps and shifted windows for efficiency. | Replaced attention layers in Res-MoCoDiff to enhance robustness across resolutions [67]. |
| Generative Adversarial Network (GAN) | Neural Network Architecture | A framework where two networks (generator and discriminator) compete to generate realistic data. | Used as a benchmark (cycle-GAN) against newer models like Res-MoCoDiff [67]. |
| GPU (e.g., NVIDIA) | Hardware | Graphics Processing Unit, optimized for parallel computations required for DL training and inference. | Critical for training deep learning models in a feasible amount of time [81] [82]. |
| Public Datasets (MedMNIST, BraTS) | Data Resource | Curated, often annotated, medical imaging datasets for training and benchmarking algorithms. | Used to evaluate the generalizability of models like UniMo on unseen data [48]. |
| Open-Source Code (e.g., UniMo) | Software Resource | Publicly available implementations of published algorithms. | Allows for validation, reproduction, and extension of research findings (e.g., UniMo on GitHub) [48]. |
Motion artifacts represent a significant challenge in medical imaging, adversely affecting image quality and, consequently, the accuracy of subsequent quantitative analyses. As imaging systems achieve increasingly higher spatial resolutions, even minor patient movements can substantially degrade diagnostic utility. This guide provides an objective comparison of motion correction algorithm performance, focusing specifically on their impact on critical downstream tasks including segmentation accuracy, flow quantification, and diagnostic decision-making. We synthesize experimental data from recent clinical and technical studies across multiple imaging modalities to evaluate how different correction approaches preserve quantitative accuracy in research and clinical environments.
Comparative Performance of Motion Correction Algorithms
The table below summarizes quantitative findings from recent studies evaluating motion correction algorithms across various imaging modalities and clinical applications.
Table 1: Quantitative Impact of Motion Correction on Downstream Tasks
| Imaging Modality | Correction Algorithm | Performance Improvement | Experimental Context |
|---|---|---|---|
| Brain PET [12] | Event-by-Event (EBE) MC with UMT | Lowest residual SD in TACs; superior visualization of gyri/sulci | Ultra-high performance PET (NeuroEXPLORER) with multiple tracers |
| Brain PET [22] | Data-driven Rigid Motion Correction | 8% of datasets improved from diagnostically unacceptable to acceptable | Clinical 18F-FDG PET; reader study (n=50) |
| Coronary CCTA [5] | SnapShot Freeze 2 (SSF2) | Best correlation with invasive FFR (r=0.652); highest diagnostic performance for ischemic lesions | Coronary CT angiography (n=151 patients) |
| Cardiac PET-MPI [84] | Automated Motion Correction | Stress MBF AUC for CAD: 0.76 vs. 0.73 without MC; processing time: <12s vs. 10min | 82Rb PET myocardial perfusion imaging (n=341) |
| Lung Cancer PET/CT [14] | Data-Driven Gating + RRA | SUVmax increased 3.9%; lesion volume decreased 18.4%; image quality scores improved | Phantom validation and patient studies (n=30) |
| Phase Contrast MRI [85] | Machine Learning Segmentation | Near-perfect correlation with manual segmentation (r=0.99); analysis time: <0.01 min/case | Aortic flow quantification (n=190) |
| Real-time PC-MRI [86] | Convolutional Neural Network (CNN) | Dice score: 0.90 vs. 0.93 human inter-observer; resilient to heart rate variability | Left atrial flow quantification in AF patients (n=44) |
Experimental Protocols and Methodologies
Neurological PET Imaging
In ultra-high performance brain PET studies, researchers evaluated multiple motion correction approaches for the NeuroEXPLORER system, which offers spatial resolution below 2 mm. The experimental protocol involved human scans with various tracers (18F-FE-PE2I, 11C-PHNO, 18F-SynVesT-1) with list-mode data acquisition over 90 minutes [12].
Key Methodological Components:
- Motion Tracking: A markerless United Healthcare Motion Tracking system collected motion data at 30 Hz
- Reconstruction: OSEM reconstruction with point spread function modeling
- Comparison Conditions:
- No motion correction (NMC)
- Post-reconstruction registration (PRR)
- Frame-based UMT correction
- Event-by-event UMT correction
- Evaluation Metrics: Standard deviation of residuals around fitted time-activity curves; visual assessment of gyral/sulcal detail
The results demonstrated that event-by-event motion correction outperformed frame-based methods, particularly in addressing rapid intraframe motion that caused significant deviations in quantitative measurements [12].
Cardiac Flow Quantification
For phase contrast cardiovascular magnetic resonance, researchers developed a machine learning model to automate aortic flow quantification, addressing the time-intensive nature of manual segmentation [85].
Experimental Workflow:
- Model Training: Neural network trained on 150 patient datasets
- Validation: Prospective testing in 190 coronary artery disease patients
- Comparison: Against manual segmentation and commercial automated approaches
- External Validation: Testing on separate cohort from different site/CMR vendor
The algorithm achieved near-perfect correlation with manual segmentation (r=0.99) while reducing processing time from approximately 4 minutes per case to less than 0.01 minutes [85]. In patients with mitral regurgitation, the method appropriately detected differences between forward stroke volume and left ventricular volumetric stroke volume, validating its physiological accuracy.
Coronary CT Angiography
A comprehensive comparison of motion correction algorithms for CCTA evaluated their impact on CT fractional flow reserve calculations, using invasive angiography as reference standard [5].
Study Design:
- Population: 151 patients with invasive coronary angiography/FFR within 3 months
- Interventions: Standard images (STD) versus first-generation (SSF1) and second-generation (SSF2) SnapShot Freeze algorithms
- Outcome Measures:
- Image quality scores
- Correlation between CT-FFR and invasive FFR
- Diagnostic accuracy for obstructive and ischemic stenosis
SSF2, which extends correction to the entire heart rather than just coronary arteries, demonstrated significantly improved correlation with invasive FFR measurements and superior diagnostic performance for identifying ischemic lesions compared to both standard imaging and SSF1 [5].
Visualizing Motion Correction Workflows
The following diagram illustrates a generalized workflow for motion correction in medical imaging, integrating elements from the various methodologies discussed.
Diagram 1: Motion correction workflow integrating multiple methodologies and performance metrics.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Computational Tools for Motion Correction Research
| Tool/Reagent | Function | Example Implementation |
|---|---|---|
| United Motion Tracking (UMT) | Markerless optical motion tracking at 30Hz | NeuroEXPLORER Brain PET [12] |
| MOLAR Reconstruction | Motion-compensation OSEM list-mode algorithm with resolution recovery | Ultra-high performance PET systems [12] |
| Data-Driven Gating (DDG) | Extracts respiratory signal from raw PET data without external devices | Lung cancer PET/CT motion correction [14] |
| Reconstruct-Register-Average (RRA) | Combines data-driven gating with motion-corrected reconstruction | Respiratory motion artifact reduction [14] |
| QPET Software | Automated left ventricular contouring for myocardial flow analysis | 82Rb PET myocardial perfusion imaging [84] |
| 3D U-Net with DenseNet Blocks | Deep learning architecture for segmentation of dynamic imaging | Left atrial flow quantification in phase contrast MRI [86] |
| UniMo Framework | Unified deep learning for both rigid and non-rigid motion correction | Generalizable across modalities without retraining [48] |
| GRAPPA-GRASP Reconstruction | Parallel imaging and compressed sensing for radial MRI | Real-time phase contrast MRI in atrial fibrillation [86] |
Implications for Diagnostic Decision-Making
The consistent theme across studies is that effective motion correction directly enhances diagnostic performance. In coronary CCTA, SSF2 motion correction significantly improved the diagnostic accuracy of CT-FFR for identifying ischemic lesions, with the area under the curve increasing from 0.795 to 0.887 at the per-lesion level [5]. Similarly, in cardiac PET, automated motion correction significantly improved the predictive value of myocardial blood flow for significant coronary artery disease (AUC 0.76 with MC vs. 0.73 without) [84].
Perhaps most notably, in clinical brain PET, data-driven motion correction transformed 8% of studies from diagnostically unacceptable to acceptable quality without repeating the scan [22]. This demonstrates the critical role of motion correction not only in refining quantitative measurements but also in preserving diagnostic utility in challenging imaging scenarios.
Motion correction algorithms significantly impact downstream analytical tasks across imaging modalities. The evidence consistently demonstrates that advanced correction methods, particularly event-by-event tracking in PET, data-driven approaches, and machine learning-based methods, substantially improve segmentation accuracy, flow quantification reliability, and ultimately, diagnostic performance. The choice of correction method should be guided by the specific imaging modality, the nature of expected motion, and the particular quantitative tasks required. As imaging technologies continue advancing toward higher resolutions, the importance of sophisticated motion correction will only increase, making these algorithms indispensable components of the quantitative medical imaging pipeline.
Conclusion
The evolution of motion correction algorithms demonstrates a clear trajectory toward integrated, data-driven approaches that combine the strengths of deep learning with robust physical models. Performance comparisons reveal that no single algorithm universally outperforms others across all modalities, with optimal selection depending on specific application requirements, motion characteristics, and available computational resources. The integration of self-attention mechanisms, edge preservation, and perceptual loss in deep learning frameworks shows particular promise for maintaining structural integrity while correcting artifacts. Future directions should focus on developing standardized validation frameworks, improving generalizability across imaging centers, and creating more efficient models for real-time clinical implementation. As motion correction becomes increasingly crucial for quantitative imaging in both clinical diagnostics and drug development, these advancements will play a pivotal role in enhancing measurement precision, reducing scan repetitions, and ultimately improving patient outcomes through more reliable image-based assessment.
References
- 1. Motion correction and the use of motion covariates in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6871380/]
- 2. The role of fMRI in drug development - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5931333/]
- 3. Quantitative Imaging Network (QIN) [https://dctd.cancer.gov/research/networks/qin]
- 4. Quantitative framework for prospective motion correction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4567538/]
- 5. Novel motion correction algorithm improves diagnostic ... [https://www.sciencedirect.com/science/article/abs/pii/S0720048X24002547]
- 6. Comparison of motion correction techniques applied to ... [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-20/issue-12/126003/Comparison-of-motion-correction-techniques-applied-to-functional-near-infrared/10.1117/1.JBO.20.12.126003.full]
- 7. Data Consistent Deep Rigid MRI Motion Correction [https://arxiv.org/abs/2301.10365]
- 8. Motion correction in MRI of the brain - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4930872/]
- 9. A network‐assisted joint image and motion estimation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620172/]
- 10. Quantitative and Visual Benefits of Data-Driven Motion ... [https://www.sciencedirect.com/science/article/pii/S1076633224009644]
- 11. Quantitative evaluation of methods to analyze motion ... [https://www.nature.com/articles/s41467-025-61949-x]
- 12. Evaluation of motion correction methods in ultra-high ... [https://jnm.snmjournals.org/content/66/supplement_1/251680]
- 13. Machine learning enhanced motion correction in reduced ... [https://jnm.snmjournals.org/content/66/supplement_1/252240]
- 14. Evaluation of a motion correction algorithm in lung cancer ... [https://pubmed.ncbi.nlm.nih.gov/40280889/]
- 15. End-to-End Deep Learning-Based Motion Correction and ... [https://www.sciencedirect.com/science/article/pii/S0730725X25000803]
- 16. (ISMRM 2025) Motion-corrected brain MRI at 64 mT [https://archive.ismrm.org/2025/4442.html]
- 17. Simulating Sinogram-Domain Motion and Correcting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574536/]
- 18. Sinogram domain metal artifact correction of CT via deep ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482523001750]
- 19. Comparison of fMRI motion correction software tools [https://www.sciencedirect.com/science/article/abs/pii/S1053811905004337]
- 20. PROMO – Real-time Prospective Motion Correction in MRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2892665/]
- 21. Data-Driven Motion Detection and Event-by-Event Correction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7456171/]
- 22. Evaluation of Data-Driven Rigid Motion Correction in Clinical ... [https://jnm.snmjournals.org/content/63/10/1604]
- 23. A Systematic Comparison of Motion Artifact Correction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3468891/]
- 24. Simulating Sinogram-Domain Motion and Correcting Image- ... [https://arxiv.org/html/2509.10961v1]
- 25. Dynamic frame-by-frame motion correction for 13N-ammonia ... [https://jnm.snmjournals.org/content/66/supplement_1/252089]
- 26. Dynamic frame-by-frame motion correction for 18F ... [https://pubmed.ncbi.nlm.nih.gov/41261210/]
- 27. A self-attention model for robust rigid slice-to-volume ... [https://pubmed.ncbi.nlm.nih.gov/40997675/]
- 28. Systematic Review and Meta-analysis of AI-driven MRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425023/]
- 29. Evaluation of motion artefact reduction depending on the ... [https://www.nature.com/articles/s41598-023-35794-1]
- 30. Motion artifact correction in fetal MRI based on a ... [https://www.sciencedirect.com/science/article/pii/S1746809422009387]
- 31. Learning-based motion artifact removal networks for ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/35257400/]
- 32. Unsupervised motion artifacts reduction for cone-beam CT ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417425008802]
- 33. High-quality PET image synthesis from ultra-low-dose PET ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9703111/]
- 34. Ultra-High-Resolution Image Synthesis: Data, Method and ... [https://arxiv.org/abs/2506.01331]
- 35. Benchmarking GANs, Diffusion Models, and Flow Matching ... [https://arxiv.org/abs/2507.14575]
- 36. Motion correction in CBCT imaging using gate‐less model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12509791/]
- 37. Improving cone-beam computed tomography image quality ... [https://clinicalimagingscience.org/improving-cone-beam-computed-tomography-image-quality-for-transarterial-therapy-of-liver-malignancies-evaluation-of-a-motion-correction-algorithm-with-and-without-automated-bone-removal/]
- 38. Motion correction in CBCT imaging using gate-less model ... [https://researchinformation.umcutrecht.nl/en/publications/motion-correction-in-cbct-imaging-using-gate-less-model-based-rec/]
- 39. Comparison between Principal Component Analysis and ... [https://www.sciencedirect.com/science/article/abs/pii/S0378779614002065]
- 40. Low Complexity Automatic Stationary Wavelet Transform ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6955982/]
- 41. Wavelet methodology to improve single unit isolation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5101837/]
- 42. Iterative Learning for Joint Image Denoising and Motion ... [https://www.sciencedirect.com/science/article/abs/pii/S1361841525004189]
- 43. A Mini-Review on Functional Near-Infrared Spectroscopy ... [https://www.mdpi.com/2304-6732/6/3/87]
- 44. Performance and application of the total-body PET/CT scanner [https://ejnmmires.springeropen.com/articles/10.1186/s13550-023-01059-1]
- 45. Real-time prospective motion correction in MRI using image ... [https://pubmed.ncbi.nlm.nih.gov/20027635/]
- 46. A Graphics Processing Unit Accelerated Motion Correction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3644525/]
- 47. Deep learning-based motion correction algorithm for ... [https://pubmed.ncbi.nlm.nih.gov/37485892/]
- 48. A Unified Deep Learning Framework for Motion Correction ... [https://arxiv.org/html/2409.14204v3]
- 49. Prevention of Motion-Induced Signal Loss in Diffusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4420624/]
- 50. The effect of motion correction interpolation on quantitative ... [https://www.sciencedirect.com/science/article/abs/pii/S1361841518301567]
- 51. Effect of data-driven motion correction for respiratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12254103/]
- 52. Learning‐based motion artifact correction in the Z‐spectral domain for chemical exchange saturation transfer MRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12021334/]
- 53. Impact of a motion correction algorithm on image quality in patients undergoing CT angiography: A randomized controlled trial - PubMed [https://pubmed.ncbi.nlm.nih.gov/27838576/]
- 54. HyDA: Hypernetworks for Test Time Domain Adaptation in ... [https://arxiv.org/abs/2503.04979]
- 55. MEDiCINe: Motion Correction for Neural Electrophysiology Recordings - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11896784/]
- 56. Patient specific prospective respiratory motion correction for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6814292/]
- 57. Reduction of respiratory motion artifacts in gadoxetate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7651696/]
- 58. An Adaptive Filter for Suppression of Cardiac and Respiratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1716734/]
- 59. Respiratory noise correction using phase information [https://www.sciencedirect.com/science/article/pii/S0730725X09003063]
- 60. Comprehensive ultrahigh resolution whole brain in vivo MRI dataset as a human phantom | Scientific Data [https://www.nature.com/articles/s41597-021-00923-w]
- 61. Data augmentation and transfer learning ... [https://milvus.io/ai-quick-reference/what-is-the-relationship-between-data-augmentation-and-transfer-learning]
- 62. The impact of data augmentation and transfer learning on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11308385/]
- 63. What Is Transfer Learning and Data Augmentation? [https://www.tredence.com/blog/transfer-learning-and-data-augmentation-in-deep-learning]
- 64. Comparison of motion correction techniques applied to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9900395/]
- 65. PET Head Motion Estimation Using Supervised Deep ... [https://arxiv.org/abs/2510.12758]
- 66. ISMRM25 - Image Recon / Motion Correction / AI [https://www.ismrm.org/25/program-files/T-02.htm]
- 67. Res-MoCoDiff: residual-guided diffusion models for motion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532098/]
- 68. Effect of data-driven motion correction for respiratory ... [https://ejnmmiphys.springeropen.com/articles/10.1186/s40658-025-00784-x]
- 69. Phantom studies in medical imaging (PSMI) - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583249/]
- 70. A Method for Assessing Ground-Truth Accuracy of the 5DCT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4634638/]
- 71. Ground-truth “resting-state” signal provides data-driven ... [https://www.sciencedirect.com/science/article/pii/S1053811920310697]
- 72. Comparison of six phantoms for entrance skin dose evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5723512/]
- 73. A phantom study comparing technical image quality of five ... [https://www.sciencedirect.com/science/article/abs/pii/S112017971930136X]
- 74. External phantom-based validation of a deep-learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12003253/]
- 75. Validation of a novel cardiac motion correction algorithm for x ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0239511]
- 76. Reader Studies in Medical Imaging: Design & Best Practices [https://collectiveminds.health/articles/understanding-reader-studies-in-medical-imaging-a-comprehensive-guide]
- 77. Review The “perfect” reader study [https://www.sciencedirect.com/science/article/abs/pii/S0720048X18300974]
- 78. An Open Benchmark Challenge for Motion Correction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5658235/]
- 79. Accuracy of diagnostic tests read with and without clinical ... [https://www.ncbi.nlm.nih.gov/books/NBK70994/]
- 80. Analysis and comparison of two methods for motion ... [https://research.rug.nl/en/publications/analysis-and-comparison-of-two-methods-for-motion-correction-in-p/]
- 81. Deep Learning vs Machine Learning: Key Differences [https://labelyourdata.com/articles/deep-learning-vs-machine-learning]
- 82. Deep Learning vs Machine Learning: Key Differences [https://ischool.syracuse.edu/deep-learning-vs-machine-learning/]
- 83. A deep learning network for motion correction in 3D CEST ... [https://pubmed.ncbi.nlm.nih.gov/40495308/]
- 84. Automated Motion Correction for Myocardial Blood Flow ... [https://jnm.snmjournals.org/content/65/1/139]
- 85. Machine learning derived segmentation of phase velocity ... [https://www.sciencedirect.com/science/article/pii/S1097664723001746]
- 86. Deep learning based automated left atrial segmentation ... [https://link.springer.com/article/10.1007/s10554-025-03407-9]