Motion Sensitivity in MRI Pulse Sequences: A Comprehensive Guide for Researchers and Drug Development
This article provides a systematic comparison of motion sensitivity across various MRI pulse sequences, a critical consideration for researchers and professionals in drug development and clinical research.
Motion Sensitivity in MRI Pulse Sequences: A Comprehensive Guide for Researchers and Drug Development
Abstract
This article provides a systematic comparison of motion sensitivity across various MRI pulse sequences, a critical consideration for researchers and professionals in drug development and clinical research. It explores the fundamental physical principles behind motion artifacts, details advanced methodological corrections like navigator echoes and prospective motion correction, and offers a practical troubleshooting guide for optimizing protocols. The content further synthesizes validation strategies and comparative performance metrics across sequences such as T2*-GRE, EPI, ZTE, and SSFP, providing an evidence-based framework for selecting the most motion-robust techniques in sensitive imaging scenarios.
The Physics of Motion Artifacts: Why MRI is Sensitive and How Artifacts Manifest
Magnetic Resonance Imaging (MRI) is a powerful non-invasive imaging modality, but its data acquisition process is inherently slow, making it highly sensitive to patient motion. Unlike photographic imaging, where motion causes localized blurring, motion in MRI can corrupt the entire image because data are acquired sequentially in the spatial frequency domain (k-space), not directly in image space [1] [2]. The appearance of motion artifacts is a complex interplay between the type and timing of patient movement and the specific k-space sampling strategy employed by the pulse sequence [1]. Understanding these fundamental k-space principles is crucial for selecting appropriate imaging sequences, developing effective motion correction strategies, and accurately interpreting clinical and research images.
This review examines how motion corrupts MR image formation through the lens of k-space physics, providing a comparative analysis of motion sensitivity across different pulse sequences. We synthesize experimental data and theoretical frameworks to offer researchers and imaging scientists a foundation for optimizing acquisition protocols in motion-prone scenarios, particularly in populations such as pediatric, elderly, or neurologically impaired patients where motion control is challenging.
K-Space Fundamentals and Motion Physics
The Relationship Between K-Space and Image Quality
In MRI, spatial encoding is achieved through the sequential acquisition of data in k-space, the spatial frequency domain of the image. Each sample in k-space contains information about the spatial frequencies that compose the entire image; consequently, inconsistencies in k-space data affect the whole image rather than localized regions [1] [2]. The center of k-space (low spatial frequencies) determines overall image contrast and signal-to-noise ratio, while the periphery (high spatial frequencies) defines edge detail and resolution. This global nature of k-space encoding explains why motion during MRI acquisition can have such devastating effects on image quality compared to other imaging modalities.
Physical Mechanisms of Motion Artifacts
Motion during MRI acquisition causes inconsistencies in the k-space data, violating the fundamental assumption of a stationary object during Fourier reconstruction. The specific manifestation of artifacts depends on both the nature of the motion (translation, rotation, periodic, sudden) and the k-space trajectory used for acquisition [1].
- Translational motion produces a linear phase shift in k-space [2].
- Object rotation causes a corresponding rotation of the k-space data [2].
- Periodic motion (e.g., respiration, cardiac pulsation) results in coherent ghosting artifacts where the moving structure is replicated at regular intervals across the image [1].
- Sudden, non-periodic movements cause more complex signal modulations that lead to incoherent ghosting and general image degradation [1].
The timing of motion relative to k-space acquisition is critical. Movements occurring near the k-space center (low frequencies) tend to cause ghosting artifacts, while motions toward the k-space periphery (high frequencies) typically produce blurring and edge degradation [3].
K-Space Trajectories and Motion Sensitivity
The k-space sampling trajectory fundamentally determines how motion artifacts manifest in the final image. The most common trajectories used in clinical and research MRI are Cartesian and radial sampling, each with distinct motion sensitivity profiles.
Cartesian Sampling and Ghosting Artifacts
Cartesian sampling acquires k-space data along rectilinear grid lines, typically proceeding line-by-line in the phase-encoding direction. This approach allows computationally efficient reconstruction using the Fast Fourier Transform but creates specific vulnerabilities to motion [1]. With Cartesian sampling, motion causes inconsistencies between different phase-encoding lines, resulting in ghosting artifacts that appear as replicated structures along the phase-encoding direction [2]. The appearance of these ghosts depends on motion characteristics: periodic motion produces coherent, discrete ghosts, while random motion creates more diffuse, incoherent ghosting throughout the image [1].
Radial Sampling and Motion Robustness
Radial sampling (e.g., stack-of-stars) acquires k-space data along projections passing through the k-space center at different angles. This approach offers inherent motion robustness through two key mechanisms: oversampling of the k-space center and incoherent artifact distribution [4] [2]. Since each radial view passes through the center of k-space, motion effects are distributed throughout the image as noise-like artifacts or blurring rather than structured ghosting [2]. This generally makes radial sampling more tolerant to motion compared to Cartesian trajectories, though at the potential cost of more complex reconstruction requirements [4].
Table: Comparative Characteristics of K-Space Trajectories Regarding Motion Sensitivity
| Feature | Cartesian Sampling | Radial Sampling (e.g., Stack-of-Stars) |
|---|---|---|
| Primary Motion Artifact | Structured ghosting along phase-encoding direction | Diffuse blurring or streaking artifacts |
| Motion Artifact Appearance | Discrete replicas of moving structures | Noise-like artifacts distributed throughout image |
| Central K-Space Sampling | Once per TR period | Every single projection |
| Inconsistency Impact | Affects specific phase-encoding lines | Distributed across all projections |
| Reconstruction Method | Fast Fourier Transform (FFT) | Filtered back-projection or iterative methods |
| Computational Efficiency | High | Moderate to high |
Comparative Analysis of Pulse Sequence Motion Resilience
Experimental studies directly comparing different pulse sequences provide valuable insights into their relative motion robustness and diagnostic performance in clinical scenarios.
Cartesian MPRAGE vs. Radial Stack-of-Stars Sequence
A prospective, two-center observational study directly compared the standard magnetization-prepared rapid gradient-echo (MPRAGE) sequence with a motion-resistant radial stack-of-stars (SOS) echo-unbalanced T1 relaxation-enhanced steady-state (SOS echo-uT1RESS) sequence in brain tumor imaging [4]. The study enrolled 34 adult patients with known brain tumors and evaluated both sequences for overall image quality, lesion conspicuity, and image artifacts using a 4-point Likert scale assessed by three blinded fellowship-trained neuroradiologists [4].
Table: Quantitative Comparison of MPRAGE and SOS echo-uT1RESS in Brain Tumor Imaging
| Performance Metric | MPRAGE | SOS echo-uT1RESS | Statistical Significance | Effect Size |
|---|---|---|---|---|
| Contrast-to-Noise Ratio (CNR) | 29.4 ± 21.4 | 28.2 ± 16.5 | p = 0.80 | r = 0.03 |
| Tumor-to-Brain Contrast | 0.4 ± 0.3 | 0.7 ± 0.4 | p < 0.001 | r = 0.81 |
| Lesion Conspicuity | Reference | Significantly improved | p < 0.001 | r = 0.51 |
| Overall Image Quality | Comparable | Comparable | Not significant | - |
| Image Artifacts | Comparable | Comparable | Not significant | - |
| Diagnostic Performance | Reference | Significantly improved | p < 0.001 | r = 0.53 |
| Scan Time | 4 minutes 52 seconds | 6 minutes 51 seconds | - | - |
The SOS echo-uT1RESS sequence demonstrated a 1.8-fold improvement in tumor-to-brain contrast while maintaining comparable overall image quality and artifact levels [4]. This sequence was particularly effective for visualizing small metastases, attributable to its motion-resistant stack-of-stars acquisition and inherent dark-blood effect that suppresses background tissue signal while preserving gadolinium-enhancing lesion visibility [4].
Zero Echo Time (ZTE) Sequence for Motion-Resistant Osseous Imaging
Zero Echo Time (ZTE) sequences represent another approach to motion resilience by virtually eliminating the delay between excitation and signal readout. A recent study evaluated ZTE MRI for assessing osseous and cartilage changes in osteoarthritis of the knee joint, demonstrating its superior performance for bony abnormality detection compared to conventional proton density with fat suppression (PD-FS) sequences [5]. For osseous changes, ZTE achieved sensitivity of 91.5-92.3% and accuracy of 92.2-93.8% across readers, outperforming PD-FS (sensitivity: 85.9-87.2%, accuracy: 86.1-88.6%) [5]. This enhanced performance for bony structures, combined with ZTE's inherent motion tolerance due to extremely short echo times, makes it valuable for musculoskeletal and other motion-prone applications.
Advanced Motion Correction Methodologies
Physics-Based Modeling and Deep Learning Approaches
Traditional motion correction techniques have included prospective methods (such as navigator echoes and external tracking systems) and retrospective methods (such as post-processing algorithms) [1]. Recently, hybrid approaches combining physics-based modeling with deep learning have shown significant promise. MIT researchers have developed a deep learning model that computationally constructs motion-free images from motion-corrupted data without altering the scanning procedure [6]. This method enforces data consistency between the reconstructed image and the actual acquired measurements, avoiding the creation of physically inaccurate "hallucinations" that could lead to misdiagnosis [6]. Such approaches are particularly valuable for populations prone to motion, including children and patients with neurological disorders causing involuntary movement.
K-Space Motion Modeling for Data Augmentation
A sophisticated k-space motion model has been developed to generate realistic motion artifacts from artifact-free MRI data for deep learning frameworks [3]. This approach models patient movement as a sequence of rigid 3D affine transforms, resamples artifact-free volumes according to a "demeaned" movement model, and combines these in k-space to create motion-corrupted training data [3]. By augmenting training datasets with these physically realistic artifacts, convolutional neural networks can be trained to perform more reliably on real-world motion-affected data, with segmentation models that generalize better and provide uncertainty measures reflective of artifact presence [3].
Experimental Protocols for Motion Sensitivity Assessment
Quantitative Motion Artifact Characterization
Robust assessment of sequence motion sensitivity requires standardized experimental protocols. Quantitative analysis typically includes region-of-interest (ROI) measurements of signal intensity in enhancing lesions, normal white matter, and background air to calculate objective metrics [4]. The contrast-to-noise ratio (CNR) is calculated as CNR = (SItumor - SIWM) / SDair, where SItumor and SIWM are signal intensities in tumor and white matter, respectively, and SDair is the standard deviation of background air signal [4]. Weber contrast (also referred to as tumor-to-brain contrast) provides a complementary metric calculated as (SItumor - SIWM) / SI_WM, offering a measure of lesion visibility independent of background noise [4].
Qualitative Image Assessment Framework
Qualitative assessment by expert readers provides essential clinical context to quantitative metrics. Standardized protocols typically employ Likert scales (commonly 4-point or 5-point) evaluated by multiple blinded readers to assess parameters including [4] [5]:
- Overall image quality: Diagnostic acceptability and general image clarity
- Lesion conspicuity: Visibility and demarcation of pathological findings
- Image artifacts: Presence and severity of motion-related and other artifacts
- Anatomical detail: Clarity of specific structural features relevant to diagnostic tasks
Inter-reader reliability should be assessed using statistical measures such as Cohen's kappa, with values interpreted according to established guidelines (e.g., <0.20 slight agreement; 0.21-0.40 fair; 0.41-0.60 moderate; 0.61-0.80 substantial; 0.81-1.00 almost perfect) [5].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Research Solutions for MRI Motion Artifact Investigation
| Research Tool | Function/Application | Example Implementation |
|---|---|---|
| 3T MRI Systems | High-field platforms providing signal-to-noise ratio necessary for advanced sequence development | Siemens MAGNETOM Skyra systems used in SOS echo-uT1RESS validation [4] |
| Radial k-Space Trajectories | Motion-robust acquisition schemes that distribute artifacts incoherently | Stack-of-stars sampling with golden view angle rotation [4] |
| Deep Learning Frameworks | Hybrid physics-AI models for motion correction and artifact reduction | Data-consistent rigid motion correction combining physical models with convolutional neural networks [6] |
| Synthetic MRI Phantoms | Digital and physical phantoms for controlled motion artifact simulation | Modified Shepp-Logan phantom with added grid structures for motion simulation [1] |
| Gadolinium-Based Contrast Agents | Enhancement of lesion visibility for quantitative contrast assessment | Gadobutrol (Gadavist) at 0.1 mmol/kg dosage [4] |
| K-Space Motion Models | Generation of realistic motion artifacts for algorithm training and validation | Sequence of demeaned rigid 3D affine transforms combined in k-space [3] |
| Parallel Imaging Algorithms | Acceleration techniques requiring specialized artifact mitigation | SENSE (SENSitivity Encoding) and GRAPPA (GeneRalized Autocalibrating Partially Parallel Acquisitions) [7] [8] |
Motion artifacts remain a significant challenge in MRI, but understanding their origins in k-space physics enables more effective mitigation strategies. The comparative analysis presented here demonstrates that k-space trajectory selection profoundly impacts motion sensitivity, with radial approaches like stack-of-stars sampling offering inherent robustness through incoherent artifact distribution. Advanced reconstruction methods combining physical models with deep learning show promise for next-generation motion correction without protocol modifications. As MRI continues to expand into challenging populations and applications, these motion-resistant strategies will play an increasingly vital role in maintaining diagnostic image quality and quantitative accuracy across diverse clinical and research scenarios.
Motion artefacts are a significant challenge in magnetic resonance imaging (MRI), arising when the object being imaged moves during the data acquisition process. These artefacts manifest primarily as blurring, ghosting, and signal loss, which can degrade image quality and compromise diagnostic accuracy [9] [1]. Understanding and classifying these artefacts is crucial for developing effective mitigation strategies, particularly when comparing the motion sensitivity of different MRI pulse sequences. The appearance and severity of these artefacts are influenced by a complex interaction between the type of motion, the specific pulse sequence used, and the k-space sampling strategy [1]. This guide provides a systematic classification of motion artefacts and an objective comparison of how different pulse sequences perform in their presence, supported by experimental data and methodologies relevant to research in the field.
Fundamental Physics and Classification of Motion Artefacts
The primary source of motion artefacts in MRI lies in the discrepancy between the assumption of a stationary object during image acquisition and the reality of patient or physiological movement. Spatial encoding in MRI is a sequential process that occurs in Fourier space (k-space), and any motion during this encoding leads to inconsistencies in the acquired data [1].
K-Space and the Impact of Motion
K-space represents the spatial frequency spectrum of the imaged object. During a Cartesian acquisition, k-space is filled line by line, with each line representing a specific phase encoding step. Motion during this process violates the fundamental assumption of a static object, leading to data inconsistencies that manifest as artefacts after Fourier transformation [1]. The effect of motion depends critically on its timing relative to the k-space acquisition order. Slow, continuous motion (e.g., muscle relaxation) may cause simple blurring, while periodic motion (e.g., respiration, cardiac pulsation) typically results in coherent ghosting artefacts. Sudden, abrupt motion can cause severe ghosting and signal loss [1].
A Triad of Artefacts: Blurring, Ghosting, and Signal Loss
Motion-induced artefacts in MRI can be categorized into three principal types, each with distinct appearances and underlying causes.
Blurring: This artefact presents as a loss of sharpness in image details and edges, making structures appear out of focus. It is intuitively similar to the blurring observed in photography when the subject moves during exposure [1]. Blurring occurs when there is continuous, non-periodic motion throughout the k-space acquisition, effectively smearing the spatial information.
Ghosting: Ghosting appears as replicated, semi-transparent images of a moving structure displaced along the phase-encoding direction in the final image [9] [10]. These "ghosts" can be coherent (sharp replicas) or incoherent (smeared stripes), depending on the periodicity of the motion. Coherent ghosting results from periodic motion synchronized with the sequence repetition, such as cardiac pulsation, while incoherent ghosting arises from non-periodic movements [1]. The American College of Radiology (ACR) has a standardized metric for quantifying this artefact, termed "Percent Signal Ghosting" [10].
Signal Loss: This artefact involves a localized reduction or complete absence of signal from moving tissues. It is primarily caused by spin dephasing within a voxel or the movement of excited spins out of the imaging slice between excitation and readout [1] [11]. Signal loss is particularly problematic in gradient-echo sequences and in imaging scenarios involving turbulent flow or rapid, complex motion.
The table below summarizes the key characteristics, causes, and common manifestations of these three primary motion artefacts.
Table 1: Classification and Characteristics of Primary MRI Motion Artefacts
| Artefact Type | Visual Manifestation | Primary Cause | Common Occurrence |
|---|---|---|---|
| Blurring | Loss of sharpness, smeared edges [1] | Continuous, non-periodic motion during acquisition [1] | Patient drifting, slow muscular relaxation [1] |
| Ghosting | Replicated images of moving structure along phase-encoding direction [9] [1] | Periodic or abrupt motion causing k-space inconsistency [9] [1] | Respiration, cardiac pulsation, swallowing [9] [11] |
| Signal Loss | Localized signal reduction or void [1] | Spin dephasing or movement of spins out of imaging slice [1] [11] | Turbulent blood flow, abdominal peristalsis [1] |
The following diagram illustrates the logical relationship between different types of patient motion and the resulting primary artefacts.
Diagram 1: Relationship between motion types and resulting artefacts.
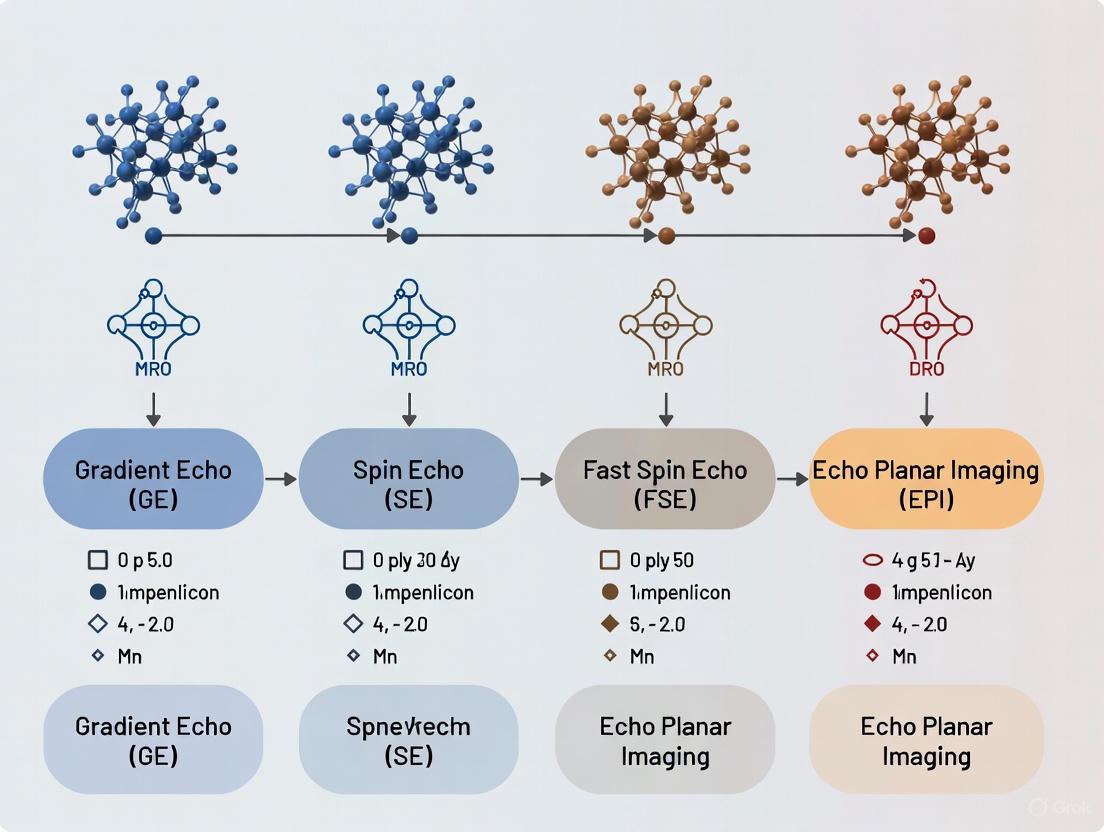
Motion Sensitivity Comparison Across Pulse Sequences
The sensitivity of an MRI examination to motion is heavily dependent on the choice of pulse sequence. Sequences vary in their acquisition speed, k-space trajectory, and inherent contrast mechanisms, leading to significant differences in their vulnerability to and manifestation of motion artefacts.
The table below provides a comparative overview of common MRI pulse sequences, focusing on their relative motion sensitivity and the typical artefacts they produce.
Table 2: Motion Sensitivity and Typical Artefacts Across MRI Pulse Sequences
| Pulse Sequence | Relative Acquisition Speed | Primary Motion Artefacts | Inherent Motion Robustness | Key Clinical Context |
|---|---|---|---|---|
| Conventional Spin Echo (CSE) | Slow | Significant ghosting and blurring [1] | Low | Standard T1 and T2 weighting; highly sensitive to motion [12] |
| Fast/Turbo Spin Echo (FSE/TSE) | Moderate | Ghosting (especially with interleaved acquisition) [1] | Moderate | Faster than CSE; but interleaving can increase ghosting from slow motion [1] |
| Single-Shot FSE (e.g., SSFSE, HASTE) | Very Fast | Minimal ghosting, some blurring [13] | High | Abdominal imaging, uncooperative patients; acquires all k-space lines in one TR [13] |
| Gradient Echo (GRE) | Fast to Moderate | Signal loss, severe ghosting [9] | Low | Dynamic contrast-enhanced, abdominal, cardiac; sensitive to magnetic field inhomogeneity [9] |
| Echo-Planar Imaging (EPI) | Very Fast | N/2 ghosting, geometric distortion [9] | Moderate (for speed) | fMRI, DWI; very fast but prone to specific ghosting and susceptibility artefacts [9] [14] |
| Radial (e.g., BLADE, PROPELLER) | Moderate | Reduced ghosting, streaking artefacts possible [9] [15] | High | Motion-prone environments; oversamples k-space center, blurring instead of ghosting [9] [15] |
Experimental Data from Sequence Comparisons
Quantitative studies provide evidence for the performance differences outlined above. A study comparing sequences for cervical spinal cord imaging found that Short-Tau Inversion-Recovery Fast Spin-Echo (STIR-FSE) demonstrated a significantly higher contrast-to-noise ratio (CNR) for demyelinating lesions compared to both Conventional Spin-Echo (CSE) and standard FSE [16]. Furthermore, STIR-FSE images revealed a significantly higher number of lesions in patients with multiple sclerosis, with additional lesions identified in 9 out of 30 patients [16]. This indicates that sequence choice not only affects artefact burden but also directly impacts diagnostic sensitivity.
In abdominal imaging, where respiratory motion is a major concern, radial k-space sampling techniques (e.g., "stack-of-stars" with golden-angle profiling) have been shown to provide higher motion robustness and greater protocol flexibility compared to conventional Cartesian sampling [15]. These techniques achieve this by continuously sampling the center of k-space, which contains the most important image contrast information, making them less susceptible to producing discrete ghost artefacts from motion [9] [15].
Experimental Protocols for Artefact Assessment
Robust experimental design is essential for objectively evaluating motion sensitivity and the efficacy of correction algorithms. The following protocols outline standardized methodologies for such assessments.
Simulation-Based Evaluation of Susceptibility and Motion
Computational simulation offers a ground-truth approach for quantitative evaluation. The POSSUM (Physics-Oriented Simulated Scanner) MR simulator, combined with a diffusion-weighted imaging framework, can generate realistic datasets with known motion and artefact parameters [14].
Protocol: Simulating Dynamic Susceptibility Artefacts
- Input Generation: Create a digital object from a brain segmentation of high-resolution T1- and T2-weighted structural images [14].
- Motion and Field Modelling: Define motion parameters (e.g., translation, rotation) and a map of magnetic field inhomogeneities (B0 fieldmap) to simulate the susceptibility-induced off-resonance field [14].
- Data Synthesis: Use the simulator to solve Bloch's and Maxwell's equations, generating complex k-space data for a specified pulse sequence (e.g., Spin-Echo EPI). The simulator outputs the distorted DW-MR data and a ground-truth displacement field mapping the geometric distortions [14].
- Correction and Validation: Apply the correction method under evaluation (e.g., fieldmap-based, reverse phase-encode). Quantify performance by comparing the method's estimated displacement field against the simulator's ground truth, measuring the ability to correct geometry and recover signal in compressed regions [14].
Phantom-Based Quantification of Ghosting
The American College of Radiology (ACR) provides a standardized phantom test for quality control, which includes a metric for quantifying ghosting artefacts [10].
Protocol: ACR Percent Signal Ghosting Measurement
- Phantom Imaging: Acquire images of the large ACR MRI phantom using the sequence and parameters to be assessed.
- Region of Interest (ROI) Analysis: Measure the mean pixel intensity in five predefined ROIs [10]:
- S: A large central area within the phantom.
- T, B, L, R: Four regions placed in the air outside the phantom, located at the top, bottom, left, and right edges of the image.
- Calculation: Compute the Percent Signal Ghosting (G) using the formula: G = | (T + B) - (L + R) | / (2 × S) [10]. A result of less than 0.025–0.03 (2.5–3%) is typically considered acceptable, though specific thresholds may vary [10].
The workflow for a comprehensive motion artefact experiment, from setup to data analysis, is outlined below.
Diagram 2: Workflow for motion artefact assessment experiments.
The Scientist's Toolkit: Research Reagents and Solutions
This section details key methodological "reagents" – essential techniques, algorithms, and hardware – used in the study and mitigation of MRI motion artefacts.
Table 3: Essential Research Reagents for Motion Artefact Investigation
| Research Reagent | Category | Primary Function | Application in Motion Research |
|---|---|---|---|
| POSSUM Simulator | Software Tool | Generates realistic MRI data with a known ground truth by solving physical equations [14] | Gold-standard validation for correction algorithms; isolates motion/susceptibility effects from other confounds [14] |
| Respiratory Gating/Triggering | Hardware/Software | Controls data acquisition based on respiratory cycle, e.g., using bellows or navigator echoes [9] [15] | Reduces respiratory ghosting in abdominal/chest imaging; enables free-breathing studies with predictable motion [9] [15] |
| Radial/Propeller k-Space | Pulse Sequence | Samples k-space in a radial or blade-like pattern, oversampling the center [9] [15] | Mitigates ghosting by transforming discrete ghosts into diffuse blurring; basis for advanced motion-robust sequences [9] [15] |
| Parallel Imaging (SENSE, GRAPPA) | Acceleration | Reduces acquisition time by undersampling k-space using coil sensitivity maps [13] | Shortens scan time to reduce motion occurrence; can be combined with other techniques like compressed sensing [9] [13] |
| Deep Learning (Generative Models) | Algorithm | AI-driven detection and correction of motion artefacts in image or k-space domain [17] | Post-processing correction; shows promise for improving image quality but faces challenges in generalizability [17] |
| Navigator Echoes | Pulse Sequence | Measures the position of an organ boundary (e.g., the diaphragm) in real-time during acquisition [9] | Provides data for prospective or retrospective motion correction without external hardware [9] |
Magnetic resonance imaging (MRI) pulse sequences employ distinct k-space sampling trajectories, each with unique characteristics that determine their vulnerability to specific artifacts. The spin warp (Cartesian) technique, echo planar imaging (EPI), and radial trajectories represent three fundamental approaches with differing resilience to common MRI challenges including off-resonance effects, motion, and hardware imperfections [18] [19]. Understanding these intrinsic vulnerabilities is crucial for selecting appropriate sequences in both clinical and research settings, particularly for applications requiring high temporal resolution or encountering significant magnetic field inhomogeneities [20].
This guide provides an objective comparison of these three trajectory classes, focusing on their performance characteristics, artifact susceptibility, and optimal application domains. We synthesize experimental data from recent studies to deliver evidence-based recommendations for researchers and drug development professionals working with advanced MRI methodologies.
Comparative Analysis of Key Performance Metrics
Table 1: Quantitative comparison of intrinsic sequence vulnerabilities
| Performance Metric | Spin Warp (Cartesian) | Echo Planar Imaging (EPI) | Radial Trajectories |
|---|---|---|---|
| Off-resonance sensitivity | Low (spatial shifts only) [19] | High (severe distortion & signal loss) [19] [21] | Medium (blurring artifacts) [19] |
| Motion artifact resilience | Low (ghosting along phase-encode) [22] | Low to Medium (severe ghosting) [22] | High (streaking artifacts, central k-space oversampling) [23] [21] |
| Temporal resolution potential | Low to Medium | Very High (single-shot acquisition) [20] | Medium to High [20] |
| Susceptibility artifact resilience | Low | Low [21] | High [21] |
| Typical acceleration compatibility | SENSE, GRAPPA [20] | SENSE, GRAPPA, Multi-band [20] [24] | Parallel imaging, compressed sensing [20] |
| Common reconstruction method | Direct FFT [23] | FFT with correction [19] | Gridding or Polar FT [23] |
Table 2: Experimental geometric distortion measurements near metal implants (adapted from Kim et al. 2022)
| Sequence Type | Specific Sequence | Distortion Near Clip (mm) | Artifact Length (mm) | Image Quality Score (1-4) |
|---|---|---|---|---|
| Spin Warp | RESOLVE DWI | Moderate | Moderate | 2.8 |
| EPI | SS-EPI DWI | Severe | Large | 1.9 |
| Radial | TGSE-BLADE DWI | Minimal | Smallest | 3.5 |
Experimental Protocols and Validation Data
Phantom and In Vivo Validation of Distortion Artifacts
Recent experimental studies provide quantitative validation of the intrinsic vulnerabilities summarized above. Kim et al. (2022) conducted a systematic comparison using a phantom with an embedded aneurysm clip and in vivo measurements in both healthy volunteers and post-neurosurgical patients [21]. Their methodology involved:
- Phantom design: A cylindrical container filled with agarose gel with a centrally embedded titanium aneurysm clip
- Participant cohort: 17 healthy volunteers and 20 patients with cerebral aneurysm clips
- Scan parameters: All sequences performed on 3T scanners (Siemens Skyra or Prisma) with comparable resolution and diffusion weighting
- Quantitative analysis: Measurement of geometric distortion at air-tissue interfaces (temporal tip, frontal sinus, cerebellum near mastoid) and near metallic implants
- Qualitative assessment: Expert radiologist scoring of geometric distortion, susceptibility artifacts, and overall image quality using a 4-point Likert scale
The results demonstrated significantly reduced distortion in radial TGSE-BLADE DWI compared to both readout-segmented spin warp (RESOLVE) and single-shot EPI sequences, particularly near susceptibility interfaces (P < 0.001) [21].
Motion Artifact Characterization Protocol
The motion resilience of radial sequences has been quantitatively evaluated through:
- Volunteer studies: Scanning healthy subjects instructed to perform deliberate head motion during acquisition
- Quantitative metrics: Displacement measurements between reference T2-weighted images and DWIs, signal variation analysis in uniform tissue regions
- PSF analysis: Evaluation of how undersampling artifacts manifest differently across trajectories [23]
These experiments consistently demonstrate that radial sampling concentrates undersampling artifacts as background noise rather than structured ghosts, with preserved central resolution making it particularly suitable for focused region-of-interest imaging [23].
Visualization of K-Space Properties and Artifact Mechanisms
This diagram illustrates how fundamental k-space sampling properties dictate characteristic artifact patterns for each trajectory class. The relationship between acquisition strategy and resulting artifacts demonstrates why each sequence exhibits distinct vulnerability profiles.
The Scientist's Toolkit: Essential Research Solutions
Table 3: Key research reagents and computational tools for trajectory studies
| Tool/Category | Specific Examples | Function/Application | Implementation Considerations |
|---|---|---|---|
| Parallel Imaging | SENSE, GRAPPA [20] | Acceleration by exploiting multi-channel arrays | Clinical acceleration rates typically 4×; higher factors increase noise [20] |
| Reconstruction Frameworks | Gadgetron, ICE [20] [23] | Open-source platforms for advanced reconstruction | GPU acceleration crucial for non-Cartesian real-time applications [20] |
| Non-Cartesian Reconstruction | Gridding, Polar Fourier Transform [23] | Direct reconstruction of radial data | PFT preserves central resolution but has longer computation time [23] |
| Motion Correction | Prospective motion correction, navigators [22] | Rigid-body motion detection and compensation | Optical tracking provides high temporal resolution for prospective correction [22] |
| Multi-band Excitation | CMRR MB-EPI sequences [24] | Simultaneous multi-slice acceleration | Reduces scan time but increases g-factor noise penalty [24] |
| Field Monitoring | Field camera systems [25] | Monitoring gradient field imperfections | Essential for high-resolution non-Cartesian imaging [25] |
Discussion and Clinical Translation
The experimental evidence clearly demonstrates that sequence selection involves inherent trade-offs between different types of vulnerability. No single trajectory excels across all performance metrics, necessitating careful matching of sequence properties to specific application requirements [20] [21].
For neuroimaging applications requiring minimal distortion near susceptibility interfaces (e.g., postoperative imaging, brainstem studies), radial techniques like TGSE-BLADE provide superior performance despite potentially longer reconstruction times [21]. When maximum temporal resolution is paramount (e.g., fMRI, dynamic contrast studies), EPI remains the preferred choice despite its vulnerability to off-resonance artifacts [20] [26]. Conventional spin warp sequences offer the advantage of robust, straightforward reconstruction with predictable artifact patterns, making them suitable for standard anatomical imaging when motion can be controlled [19].
Future directions in trajectory development focus on hybrid approaches that combine the strengths of different sampling patterns. The tilted hexagonal sampling (T-Hex) method, for instance, provides flexible k-space segmentation that can be combined with either spiral or EPI readouts to optimize timing parameters for specific contrast and resolution requirements [25]. Similarly, advanced reconstruction techniques including compressed sensing and deep learning are increasingly being applied to mitigate the intrinsic vulnerabilities of each trajectory type [27].
For drug development professionals utilizing MRI as a biomarker, this comparative analysis supports informed sequence selection based on the specific tissue targets and potential confounding factors in their experimental models. The tabulated performance metrics provide a practical reference for protocol optimization in preclinical and clinical trial settings.
In magnetic resonance imaging (MRI), patient motion presents a dual challenge. The first component is the physical movement of the object within the imaging coordinate system. The second, more complex component is the alteration of the main magnetic field (B0) induced by this motion. Even minor head pose changes can cause substantial and spatially complex B0 field changes in the brain. For rotations and translations of approximately 5° and 5 mm at 7 Tesla, the subject-induced field component alone generates a resonance frequency shift over the brain with a standard deviation of about 10 Hz [28]. These field changes lead to image-corrupting phase errors, particularly problematic in multi-shot T2*-weighted acquisitions and advanced techniques like chemical exchange saturation transfer (CEST) MRI, where signal effects are often only a few percent of the water signal [28] [29].
The complexity arises because motion-induced B0 changes have multiple sources. The total field (TF) experienced by spins in the brain changes with head pose due to: (1) the external field (EF) from the main magnet and shim coils, and (2) the subject's field (SF) from the subject's own inhomogeneous magnetization, which includes contributions from both the head and the stationary torso [28]. Understanding these sources is crucial for developing effective correction strategies, as motion-related artifacts can severely impact diagnostic quality and confound research findings, even mimicking pathological changes such as cortical atrophy [30].
Quantitative Comparison of Motion Sensitivity Across MRI Pulse Sequences
Different MRI pulse sequences exhibit varying sensitivity to motion and B0 field fluctuations. The following table summarizes experimental performance data for several sequence types in the context of motion corruption.
Table 1: Quantitative Performance Comparison of MRI Sequences Under Motion Conditions
| Sequence Type | Key Motion Mitigation Feature | Reported Performance Metric | Quantitative Result | Experimental Context |
|---|---|---|---|---|
| Radial MultiVane XD (MVXD) [31] | PROPELLER-based radial sampling with parallel imaging | Urethral visibility score (1-5 scale) | Significantly higher (4.09 ± 0.15) vs. SSFSE (2.95 ± 0.22); P < 0.0001 [31] | Prostate MRI simulation, 3T, n=22 patients |
| Cartesian Single-Shot Fast Spin-Echo (SSFSE) [31] | Rapid single-shot acquisition | Urethral visibility score (1-5 scale) | 2.95 ± 0.22 [31] | Prostate MRI simulation, 3T, n=22 patients |
| Stack-of-Stars echo-uT1RESS [4] | 3D radial (SOS) k-space trajectory | Tumor-to-brain contrast | 1.8-fold improvement vs. MPRAGE (0.7 ± 0.4 vs. 0.4 ± 0.3; p < 0.001) [4] | Brain tumor imaging, 3T, n=34 patients |
| MPRAGE (Cartesian) [4] | Standard Cartesian sampling | Tumor-to-brain contrast | 0.4 ± 0.3 [4] | Brain tumor imaging, 3T, n=34 patients |
| Standard Cartesian T2*-weighted [28] | Multi-shot acquisition for high resolution | B0 change from 5°/5mm motion | Standard deviation of ~10 Hz in resonance frequency over the brain at 7T [28] | B0 field mapping, 7T, n=5 volunteers |
The data reveal a clear performance trend favoring non-Cartesian k-space trajectories. Radial sampling techniques (MultiVane XD and Stack-of-Stars) demonstrate superior motion robustness and improved visualization of anatomical structures compared to their Cartesian counterparts. The MVXD sequence maintained high image quality despite generating more artifacts, as these artifacts tended to appear in the periphery without obscuring the region of interest [31]. The SOS echo-uT1RESS sequence achieved significantly better lesion conspicuity for brain tumors while maintaining comparable overall image quality, making it a promising motion-robust alternative for diagnostic imaging [4].
Experimental Protocols for Assessing Motion and B0 Field Effects
Protocol 1: B0 Field Change Quantification During Head Motion
This protocol, adapted from a 7 Tesla study, systematically measures how head motion alters the B0 field [28].
- Subject Preparation: Participants are instructed to move their head to various poses (right, left, up, down) and remain still during subsequent scanning.
- Field Map Acquisition: B0 field data are acquired at each pose using a 2D multi-echo gradient-echo (GRE) sequence with five echoes (spaced by 1.2 ms) and 2 mm isotropic resolution.
- Field Calculation: Field maps are calculated based on the unwrapped phase difference between echoes. A first-order navigator echo along the read-out direction is acquired for each shot to correct for dynamic frequency changes from scanner instability or respiration.
- Pose Determination: Head poses are determined via rigid-body co-registration of the GRE magnitude images, returning 6-parameter rotation and translation information.
- Data Processing: Frequency data are detrended based on the average frequency in a central brain region to reduce scanner field drift. The total field (TF) is separated into external (EF) and subject-derived (SF) components using a spherical phantom and subject-specific susceptibility models.
Protocol 2: Paired Motion-Corrupted and Motion-Free Data Acquisition
This protocol, utilized by the MR-ART dataset, enables direct evaluation of motion artifacts by acquiring matched data from the same participants [30].
- Participant Instruction: For the standard scan (STAND), participants are instructed not to move. For motion-corrupted scans (HM1, HM2), participants perform head nods (tilting down and up along the sagittal plane) when cued.
- Motion Level Control: Different artifact levels are created by varying cue frequency—5 times for low motion (HM1) and 10 times for high motion (HM2) evenly spaced during acquisition.
- Image Acquisition: T1-weighted 3D MPRAGE anatomical images are acquired with isotropic 1 mm³ resolution (TR = 2300 ms, TE = 3 ms) on a 3T scanner.
- Quality Assessment: Images are rated by expert neuroradiologists on a 3-point scale (1=clinically good, 2=medium, 3=bad quality) and processed through MRIQC for standardized image quality metrics (IQMs) like signal-to-noise ratio (SNR) and entropy focus criterion (EFC).
Protocol 3: Motion Artifact Reproduction for PMC Validation
This method enables precise reproduction of motion artifacts corrected by Prospective Motion Correction (PMC) systems for validation purposes [32].
- Motion Tracking: An MR-compatible optical tracking system (e.g., Metria Innovation) records head position in six degrees of freedom (6 DoF) at up to 85 fps during a PMC-enabled scan.
- Data Logging: All tracking data are logged to a file during the initial patient scan.
- Artifact Reproduction: The logged motion data (with motion direction reversed) are fed back to the scanner during a subsequent experiment on a stationary volunteer or phantom.
- System Operation: A dedicated software library (e.g., libXPACE) uses the position data to dynamically update the scanning coordinate system, replicating the original relative motion between the scanning volume and the object without requiring patient motion.
Visualization of Motion Impact and Correction Workflows
Diagram 1: Motion-Induced B0 Changes and Correction Pathways
Diagram 2: Motion Sensitivity Comparison of k-Space Sampling Strategies
Table 2: Key Resources for Motion and B0 Field Change Research
| Resource Category | Specific Tool / Resource | Function / Application | Example Implementation |
|---|---|---|---|
| Motion-Corrupted Datasets | MR-ART Dataset [30] | Provides paired motion-free and motion-corrupted T1w brain scans from the same participants for algorithm validation. | 148 healthy adults; STAND, HM1, HM2 scans with expert artefact scores. |
| Motion Tracking Systems | Optical Motion Tracking [32] | Provides real-time 6 DoF head pose data for prospective motion correction (PMC). | MR-compatible camera system (e.g., Metria Innovation) tracking encoded markers at up to 85 fps. |
| Field Monitoring Hardware | Magnetic Field Probes [28] | Measures B0 field dynamics outside the head during motion to inform field modeling. | Array of field probes placed around the head for dynamic B0 field measurement. |
| Motion Correction Software | Prospective Correction Library (libXPACE) [32] | Software interface for real-time coordinate system updates in MRI sequences. | Integrates with tracking data to adjust gradients and RF pulses during sequence execution. |
| Image Quality Metrics | MRIQC [30] | Automated extraction of objective image quality metrics for artifact quantification. | Calculates SNR, EFC, CJV; provides standardized reports for quality control. |
| Unified Correction Frameworks | AI-Based Motion Correction [33] | Deep learning framework for correcting motion artifacts across multi-modal MRI. | Transformer model predicting motion degradation scores; Mixture of Experts for final correction. |
The interplay between head motion and induced B0 field changes represents a complex challenge that demands integrated solutions. Quantitative evidence demonstrates that pulse sequences with inherent motion robustness, particularly those employing radial k-space trajectories like MultiVane XD and Stack-of-Stars, provide significantly improved image quality in the presence of motion compared to conventional Cartesian sequences [31] [4]. However, even with optimized sequences, residual B0 field changes at high field strengths can remain problematic for quantitative techniques [28] [29].
Future progress will likely come from combined approaches that leverage motion-robust acquisition, real-time field monitoring, and advanced post-processing using deep learning [33]. The availability of high-quality, paired datasets like MR-ART will be crucial for validating these emerging methods [30]. For researchers and clinicians, selecting the appropriate motion mitigation strategy requires careful consideration of the clinical question, patient population, and available technical resources, with the understanding that effectively addressing the dual challenge of motion and B0 field changes is essential for achieving diagnostic image quality and robust research outcomes.
The Impact of Magnetic Field Strength on Motion Sensitivity
Motion sensitivity remains a significant challenge in magnetic resonance imaging (MRI), impacting diagnostic quality and quantitative analysis. The strength of the main static magnetic field (B₀) is a fundamental parameter influencing every aspect of the MR signal chain, from signal-to-noise ratio (SNR) to artifact manifestation. This guide provides an objective comparison of motion sensitivity across different MRI field strengths, synthesizing current research to inform scanner selection and protocol optimization for researchers and development professionals. Understanding these relationships is crucial for advancing motion-robust imaging techniques across neuroimaging, musculoskeletal applications, and drug development studies where motion confounds can compromise data integrity.
Comparative Analysis of Field Strengths and Motion Characteristics
Technical Performance Metrics Across Field Strengths
Table 1: Comparative Analysis of MRI Field Strengths and Motion Sensitivity
| Field Strength Category | Typical SNR Profile | Primary Motion Artifacts | Susceptibility Artifact Severity | Typical Spatial Resolution | Key Advantages for Motion Management |
|---|---|---|---|---|---|
| Low-Field (<0.5 T) | Low inherent SNR [34] | Blurring, ghosting [35] | Significantly reduced [34] | Lower (clinical protocols) | Portable/bedside use [34] [36]; Reduced metallic implant artifacts [34] |
| Mid-Field (1.5 T) | Moderate SNR | Ghosting, phase encoding artifacts | Moderate | Standard clinical (1-2mm) | Established motion correction protocols; Balanced performance |
| High-Field (3.0 T) | High SNR [34] | pronounced ghosting, physiological noise | Pronounced [34] | High (sub-millimeter possible) | Faster acquisitions reducing motion window; Advanced acceleration techniques |
| Ultra-High Field (7 T+) | Very high SNR [37] | Severe physiological noise, flow artifacts | Severe [37] | Ultra-high (sub-millimeter to micron) [37] | Temporal resolution trade-off for spatial precision; Enhanced susceptibility-weighted contrast |
Quantitative Performance Data
Table 2: Experimental Performance Metrics in Motion-Prone Scenarios
| Field Strength | Motion Detection Accuracy | Portability & Point-of-Care Application | Susceptibility Artifact Reduction | Key Supporting Evidence |
|---|---|---|---|---|
| Low-Field (0.064 T) | N/A | Full portability demonstrated [36]; Bedside ICH detection with 80.4% sensitivity, 96.6% specificity [36] | Significant reduction near metallic hardware [34] | Portable MRI for intracerebral hemorrhage evaluation [36] |
| 1.5 T | N/A | Limited (fixed installations) | Moderate | Current clinical reference standard |
| 3.0 T | N/A | Limited (fixed installations) | Higher than 1.5T | High-resolution clinical and research applications |
| 7 T | Enables micro-motion detection | Not portable | Most severe | Precision neuroimaging with enhanced spatial resolution [37] |
Experimental Protocols for Motion Sensitivity Assessment
Radial Spoke Energy Method for Motion Detection
The radial spoke energy technique provides a self-navigated approach for motion detection without external hardware or sequence modifications, particularly effective in 3D radial imaging [35].
Experimental Protocol:
- Pulse Sequence: 3D radial acquisition with golden-angle or spiral phyllotaxis sampling [35]
- Data Collection: Acquire N radial spokes across M receiver coils, storing raw k-space data
- Spoke Energy Calculation: Compute energy for each spoke (i) and coil (j): Eij = ∑k|kij[k]|² where k represents discrete frequency components [35]
- Temporal Analysis: Apply sliding window summation to improve robustness of motion detection
- Multi-coil Integration: Use second principal component analysis (2ndPCA) to combine motion-sensitive signals across coils [35]
- Motion Quantification: Monitor energy fluctuations across successive spokes; significant variations indicate motion-induced anatomical shifts relative to coil sensitivities [35]
Validation Approach: Correlate spoke energy fluctuations with known motion patterns in ankle, knee, and head imaging, comparing to external tracking systems where available [35].
Low-Field Portable MRI for Clinical Motion Scenarios
This protocol evaluates the Hyperfine Swoop portable MRI (0.064 T) in intensive care settings where patient motion is common [36].
Experimental Protocol:
- Scanner Setup: Deploy portable 0.064 T MRI system at hospital bedside [36]
- Subject Population: Include critically ill patients with intracerebral hemorrhage (ICH) or acute ischemic stroke (AIS) alongside healthy controls [36]
- Imaging Protocol: Implement T2-weighted and FLAIR sequences (mean exam time: 17:51 minutes) [36]
- Safety Monitoring: Maintain all intravenous lines and ICU monitoring equipment during scanning [36]
- Image Analysis: Two board-certified neuroradiologists evaluate ICH detection, localization accuracy, and volume quantification [36]
- Statistical Analysis: Calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) against conventional imaging reference standards [36]
High-Field Precision Imaging with Motion Compensation
This protocol utilizes 7T MRI for motion-sensitive quantitative imaging, leveraging high SNR for motion-resolved reconstructions [37].
Experimental Protocol:
- Scanner Setup: 7T Terra Siemens with 32-channel head coil [37]
- Session Design: Three imaging sessions per participant with multi-modal acquisitions [37]
- Structural Imaging: MP2RAGE (0.5 mm isovoxels) for cortical morphology; diffusion MRI (b-values 0, 300, 700, 2000 s/mm²) for connectomes [37]
- Functional Imaging: Multi-echo fMRI (1.9 mm isovoxels) during resting-state and task paradigms [37]
- Motion Management: Implement prospective motion correction and quantitative motion metrics [37]
- Data Analysis: Extract cortical gradients and connectomes to characterize motion-related variations in network organization [37]
Visualization of Motion Detection Methodology
Figure 1: Radial Spoke Energy Motion Detection Workflow. This self-navigated method detects motion through k-space energy variations without external hardware [35].
Table 3: Key Research Reagent Solutions for Motion Sensitivity Studies
| Resource Category | Specific Examples | Research Function | Field Strength Considerations |
|---|---|---|---|
| Pulse Sequences | 3D radial sampling with golden-angle [35] | Motion-robust k-space trajectory; Enables retrospective correction | Effective across field strengths; Particularly valuable at high-field where motion artifacts are pronounced |
| Motion Detection Algorithms | Spoke energy analysis [35], FIDnav [35] | Self-navigated motion sensing without sequence modification | Computational efficiency enables real-time application across platforms |
| Portable MRI Systems | Hyperfine Swoop (0.064 T) [36] | Bedside imaging in motion-prone clinical settings; Enables studies previously impossible with fixed scanners | Unique to low-field due to reduced infrastructure requirements [34] |
| Multi-channel Coil Arrays | 32-channel head coils (7T) [37] | Enhanced parallel imaging for accelerated acquisitions; Reduced motion window through faster scanning | Critical for high-field systems to leverage intrinsic SNR advantages |
| Quantitative MRI Phantoms | Motion simulation devices | Controlled motion validation across field strengths | Essential for standardized performance comparisons |
| Advanced Reconstruction Frameworks | AI-based denoising, compressed sensing [34] | SNR enhancement and motion artifact suppression | Particularly impactful for low-field to address inherent SNR limitations [34] |
Discussion and Future Directions
The relationship between magnetic field strength and motion sensitivity presents a complex trade-off space for researchers. Low-field systems (≤0.5 T) offer inherent advantages through portability and reduced susceptibility artifacts, enabling novel applications in point-of-care settings where motion is unavoidable [34] [36]. Conversely, high-field systems (≥3 T) provide superior SNR and spatial resolution but require more sophisticated motion compensation techniques to realize their potential [37].
Emerging approaches like spoke energy motion detection demonstrate that computational methods can effectively address motion sensitivity across field strengths [35]. The integration of artificial intelligence with multi-modal data fusion further promises to extract motion-robust information from compromised datasets [38]. Future research directions should focus on quantifying motion tolerance thresholds across field strengths, developing standardized motion phantoms, and establishing cross-platform correction algorithms that maintain consistency in longitudinal studies.
For drug development professionals, these insights are particularly relevant when designing multi-site trials incorporating MRI biomarkers. Scanner selection should align with motion risk profiles of the participant population, with low-field portable options offering advantages for critically ill subjects, while high-field systems remain preferable for cooperative participants where microscopic resolution is paramount.
Advanced Motion Correction Methodologies: From Navigators to Novel Sequences
Motion artifacts remain a significant challenge in magnetic resonance imaging (MRI), particularly in advanced applications requiring high spatial resolution. Navigator-based techniques have emerged as powerful tools for measuring and correcting motion-induced artifacts and field fluctuations. This guide objectively compares the performance of volumetric Echo-Planar Imaging (EPI) navigators and field monitoring systems within the broader context of motion sensitivity across MRI pulse sequences. As the demand for higher field strengths and resolution grows, so does the vulnerability of MRI to both head motion and dynamic B0 field changes, necessitating sophisticated correction approaches that can operate concurrently with imaging sequences [39] [40].
Volumetric EPI Phase Navigators
Volumetric EPI phase navigators (PN) represent an advanced method for measuring head motion and B0 field changes simultaneously. This technique incorporates a rapidly acquired, highly accelerated volumetric EPI navigator immediately after excitation but before the primary T2*-weighted gradient echo (GRE) imaging data acquisition. This strategic timing ensures the navigator does not extend the scan duration while providing crucial field monitoring capabilities [39].
The implementation described uses a 3D GRE sequence with an integrated EPI navigator acquired at a shorter echo time than the primary imaging data. Through parallel imaging acceleration factors (R = Ry · Rz) in phase-encoding directions, temporal resolution of 0.54 seconds can be achieved with 4 mm isotropic spatial resolution. This design provides motion estimation accuracy better than 0.2° for rotation and 0.1 mm for translation, while B0 measurement errors typically range between -1.8 and 1.5 Hz at 7T [39].
Reconstruction involves several sophisticated steps: EPI ghost correction using blipless reference data, 2D-GRAPPA reconstruction with kernels of 3×2×2, and B0 distortion correction based on field maps generated from dual navigators. The magnitude of combined images uses sum of magnitudes rather than root sum of squares to minimize bias from B1 profiles, while phase images combine through magnitude-weighted averaging after normalization to a reference channel [39].
Field Monitoring Approaches
Field monitoring techniques encompass a spectrum of approaches for tracking dynamic B0 variations. Early methods included one-dimensional navigators and fat navigators that primarily addressed linear field changes, but these proved inadequate for capturing more complex, nonlinear field variations resulting from head motion [39]. More advanced methods like Field Probe monitoring systems utilize NMR field probes positioned around the subject to sample magnetic field variations independently of imaging, enabling real-time shim updates [41].
FID navigators (FIDnavs) represent a particularly efficient approach that measures signal from receiver coils without spatial encoding, enabling extremely rapid acquisition with minimal sequence impact. This method leverages the spatial encoding information inherent in multi-channel coil arrays to characterize spatiotemporal B0 fluctuations through a forward model based on a complex-valued reference image. The technique can model field inhomogeneity coefficients using spherical harmonic functions up to second order, comprising five independent parameters that capture the essential field variations affecting image quality [41].
Performance Comparison
The table below summarizes key performance characteristics of major navigator-based correction techniques:
Table 1: Performance comparison of navigator-based correction techniques
| Technique | Spatial Resolution | Temporal Resolution | Motion Accuracy | B0 Accuracy | Sequence Impact |
|---|---|---|---|---|---|
| Volumetric EPI PN | 4 mm isotropic | 0.54 s | <0.2° rotation, <0.1 mm translation | -1.8 to 1.5 Hz error at 7T | No scan time increase |
| FID Navigators | Voxel-wise (via model) | Per-slice (minimal TR increase) | Not specialized | Enables dynamic distortion correction | Minimal TR increase |
| Field Monitoring Probes | Limited by probe count & placement | ~100 ms (hardware dependent) | Not specialized | Direct field measurement | Requires additional hardware |
| Double Volumetric Navigators (DvNavs) | Low-resolution 3D | Per-volume (significant burden) | 3D rigid motion | Spatially-resolved field maps | Substantial acquisition burden |
Correction Efficacy and Artifact Reduction
Volumetric EPI navigators demonstrate particular strength in correcting artifacts in T2*-weighted MRI at high field strengths. The combination of motion estimation and B0 field monitoring enables comprehensive correction that addresses both rigid body motion and the consequent field changes that particularly affect susceptibility-weighted sequences. This dual correction capability is crucial at high fields where susceptibility effects scale with B0 strength [39] [40].
In functional MRI applications, FID navigators have shown significant improvements in temporal signal-to-noise ratio (tSNR). During experiments involving continuous motion (nose touching task), FIDnav-based dynamic distortion correction yielded tSNR gains of 30% in gray matter. Even following image realignment to account for global shifts, residual tSNR improvements of 3% were achieved, demonstrating the value of addressing distortion beyond simple motion correction [41].
Comparative Performance in Challenging Scenarios
When addressing large head motions, prospective motion correction (PMC) utilizing external tracking has demonstrated superior performance compared to retrospective methods (RMC). In Cartesian 3D-encoded MPRAGE sequences, PMC maintains more consistent k-space sampling despite head rotations, reducing Nyquist violations that cannot be fully corrected retrospectively. However, increasing the correction frequency in RMC—applying corrections within echo trains rather than only between them—significantly improves performance, narrowing the gap with prospective approaches [42].
For challenging populations where motion is anticipated, such as pediatric imaging or clinical populations unable to remain still, navigator methods demonstrate particular value. One study implementing a GRAPPA-accelerated EPI sequence with tailored reconstruction successfully produced diagnostic-quality diffusion tensor imaging in 99.8% of 1600 pediatric cases, failing in only 3 subjects despite significant motion challenges [43].
Experimental Protocols
Implementation of Volumetric EPI Phase Navigators
The following workflow details the implementation of volumetric EPI phase navigators for motion and B0 correction:
Table 2: Key parameters for volumetric EPI navigator implementation
| Parameter | Specification | Purpose |
|---|---|---|
| Navigator Type | Volumetric EPI | Simultaneous motion and field monitoring |
| Spatial Resolution | 4 mm isotropic | Balance between accuracy and speed |
| Temporal Resolution | 0.54 s | Capture physiological field variations |
| Acceleration Factor | R = Ry · Rz (2D-GRAPPA) | Enable rapid acquisition |
| Kernel Size | 3×2×2 (readout × PE × PE) | GRAPPA reconstruction |
| B0 Accuracy | -1.8 to 1.5 Hz error range | Precise field monitoring |
The pulse sequence design interleaves two consecutive navigators after slab-selective RF excitation but before GRE imaging data collection. The k-space trajectory for navigators uses controlled 2D-aliasing with phase-encoding positions cycled through k-space by varying initial offsets. A full navigator covering entire k-space is obtained every set of R fast navigators, providing flexibility to select motion-free periods for autocalibration signal (ACS) data [39].
Reconstruction begins with EPI ghost correction using nearest blipless data as reference, followed by global B0-related phase correction for each readout line according to its echo time. Fast navigator images are reconstructed using 2D-GRAPPA, with the GRAPPA kernel applied in accelerated phase-encoding directions. The motion-free period for ACS identification is determined based on phase of blipless data, specifically selecting periods where global B0 frequency variation remains below 2 Hz [39].
FID Navigator Implementation for Dynamic Distortion Correction
FIDnav implementation utilizes a forward model based on a complex-valued multi-channel reference image with matched contrast properties to estimate B0 field changes. The model represents dynamic field variations as a series of low-spatial-order basis functions: ΔB0,n(r) = ΔB0,0(r) + β(r)bn, where r denotes spatial coordinate and n indexes time [41].
The forward model simulating FIDnav signals is expressed as: [ \begin{bmatrix} y{1,n} \ y{2,n} \ \vdots \ y{Nc,n}
\end{bmatrix}
\begin{bmatrix} S{1,0} \ S{2,0} \ \vdots \ S{Nc,0} \end{bmatrix} \exp(i\gamma\tau{\text{NAV}}\beta bn) ] where (y{j,n}) is the measured FIDnav from coil j at acquisition n, each (S{j,0}) is a vector of complex pixel intensities from the reference image for coil j, γ is the gyromagnetic ratio, (\tau{\text{NAV}}) matches the reference echo time to FIDnav sampling, β represents basis functions, and (bn) contains inhomogeneity coefficients at acquisition n [41].
Unknown coefficients are computed using a non-linear algorithm minimizing residual sum-of-squares between forward model predictions and measured FIDnavs: [ \hat{b}n = \arg \min{bn} \| yn - f(b_n) \|^2 ] This approach enables estimation of in-plane spherical harmonic functions up to second order, represented by five inhomogeneity coefficients, without requiring spatial encoding, image reconstruction, or phase unwrapping [41].
Visualization of Technical Relationships
Diagram 1: Relationship between artifact sources, correction approaches, and outcomes in navigator-based MRI
The Scientist's Toolkit
Table 3: Essential research reagents and solutions for navigator-based MRI
| Tool | Function | Application Context |
|---|---|---|
| Volumetric EPI Navigator | Simultaneous motion and B0 field monitoring | High-resolution T2*-weighted MRI at high field |
| FID Navigators | Rapid B0 field measurement without spatial encoding | Dynamic distortion correction in EPI time series |
| External Field Probes | Direct magnetic field sampling independent of imaging | Real-time shim correction for high-field systems |
| Optical Motion Tracking | Markerless head pose estimation via surface scanning | Prospective motion correction in structural sequences |
| GRAPPA/Parallel Imaging | Accelerated k-space acquisition and reconstruction | Enable rapid navigator acquisition with minimal overhead |
| Non-uniform FFT (NUFFT) | Reconstruction of non-Cartesian k-space data | Retrospective motion correction with rotated trajectories |
| Blip-Up/Blip-Down Acquisition | Paired EPI with reversed phase encoding | Static field map estimation for distortion correction |
| Free-Water DTI Model | Computational separation of tissue and free-water compartments | Improved specificity in diffusion metrics for neurodegenerative disease |
Volumetric EPI navigators and field monitoring techniques represent complementary approaches addressing the intertwined challenges of head motion and B0 field fluctuations in MRI. Volumetric EPI navigators excel in applications requiring simultaneous high-resolution motion and field monitoring without extending scan time, particularly beneficial for high-field T2*-weighted imaging. Field monitoring methods, including FID navigators and field probes, offer specialized solutions for dynamic distortion correction and real-time shim updates. The optimal choice depends on specific application requirements: volumetric EPI for comprehensive correction in structural imaging, FID navigators for efficient distortion correction in fMRI, and field probes for highest precision B0 control in demanding high-field applications. As MRI continues toward higher fields and resolutions, integrated approaches combining multiple navigator techniques likely represent the future of robust, high-quality neuroimaging.
Subject motion remains a significant challenge in magnetic resonance imaging (MRI), often degrading image quality and introducing biases in both clinical and research settings [44] [45]. Motion artifacts can reduce the diagnostic value of clinical scans and increase variance in research data, sometimes necessitating sequence repeats that incur substantial additional costs estimated at approximately $115,000 per scanner annually [44]. Two primary technological paradigms have emerged to address this problem: Prospective Motion Correction (PMC) and Retrospective Motion Correction (RMC). This guide provides an objective comparison of these operational paradigms, focusing on their methodological principles, performance characteristics, and implementation requirements to assist researchers and professionals in selecting appropriate correction strategies for their specific applications.
Operational Paradigms: Core Principles and Workflows
Prospective Motion Correction (PMC)
PMC operates on a real-time prevention principle. It continuously monitors head position during data acquisition and dynamically adjusts the imaging field-of-view (FOV) to remain stationary relative to the patient's head [44] [46]. This approach requires continuous, low-latency estimation of the rigid body position and orientation (pose) throughout the scan.
Motion Tracking Modalities: PMC implementations utilize various tracking approaches:
- Optical tracking systems using cameras (e.g., markerless tracking with structured light or Moiré phase markers) [44] [46]
- MR-based navigator techniques embedded within the pulse sequence [44]
- Radiofrequency (RF) field monitoring [45]
The crucial operational characteristic of PMC is that it modifies the acquisition process itself, updating imaging gradients, RF frequency, and phase to maintain consistent spatial encoding relative to the moving head [46]. Correction can be applied at different frequencies, from before each echo train (Before-ET) to more frequent updates within echo trains (Within-ET), with higher frequencies demonstrating superior artifact reduction [44].
Retrospective Motion Correction (RMC)
RMC functions on a post-acquisition compensation principle. It estimates motion that occurred during the scan and corrects for it during image reconstruction [44] [47]. Unlike PMC, RMC does not modify the acquisition process in real-time.
Motion Estimation Approaches:
- External motion tracking data recorded during acquisition [44]
- Image-based registration techniques [45]
- Navigator-based methods [48]
- Data-driven approaches utilizing information from multiple receiver coils [44]
The core reconstruction process involves adjusting k-space trajectories according to measured motion, followed by reconstruction using non-uniform Fast Fourier Transform (NUFFT) to account for the resulting irregular k-space sampling [44]. RMC preserves the original uncorrected data and operates independently of real-time latency constraints, but cannot address spin-history effects or fully compensate for Nyquist violations caused by rotational motion [44] [45].
Operational Workflow Comparison
The diagram below illustrates the fundamental operational differences between PMC and RMC workflows:
Performance Comparison: Experimental Data
Quantitative Comparison in Neuroanatomical MRI
A direct comparison study evaluated PMC and RMC performance in Cartesian 3D-encoded MPRAGE scans using the same markerless optical tracking system [44] [49]. The study employed quantitative quality assessment using the structural similarity index measure (SSIM) relative to motion-free reference scans.
Table 1: Quantitative Performance Comparison of Motion Correction Techniques
| Correction Method | Correction Frequency | Image Quality (SSIM) | Key Advantages | Key Limitations |
|---|---|---|---|---|
| PMC | Before each echo train (Before-ET) | Superior to equivalent RMC [44] | Reduces local Nyquist violations; Handles spin-history effects [44] [45] | Requires sequence modification; Dependent on low-latency tracking [44] |
| PMC | Within echo train (Within-ET) | Highest overall [44] | Minimizes intra-echo-train motion artifacts [44] | Highest hardware/sequence demands [44] |
| RMC | Before each echo train | Inferior to PMC [44] | No sequence modification; Preserves original data [44] | Cannot correct spin-history effects; Limited by Nyquist violations [44] [45] |
| RMC | Within echo train | Improved over Before-ET RMC [44] | Higher correction frequency improves performance [44] | Computational reconstruction complexity [44] |
| Hybrid (PMC+RMC) | Within-ET retrospective on Before-ET PMC | Reduced motion artifacts vs. Before-ET PMC alone [44] | Addresses residual intra-echo-train motion [44] | Combined implementation complexity [44] |
Sequence-Specific Performance Considerations
Functional MRI (fMRI): PMC in fMRI reduces false positives and increases sensitivity compared to RMC, particularly with substantial motion [45]. PMC effectively addresses spin-history effects and intra-volume inconsistencies that RMC cannot fully correct [45]. The combination of PMC with dynamic distortion correction provides particularly advantageous performance for fMRI applications [45].
Diffusion-Weighted MRI: PMC maintains diffusion encoding direction coherence during motion by updating the gradient coordinate system in real-time [48]. RMC faces challenges in diffusion imaging due to strong signal and contrast changes between serial image volumes with different diffusion weightings, which limit the effectiveness of image registration methods [48].
High-Resolution Quantitative MRI: PMC significantly improves precision in quantitative maps, with reported 11-25% improvements in coefficient of variation in cortical sub-regions during deliberate head motion [46]. Importantly, PMC does not introduce extraneous artifacts in the absence of motion, making it safe for routine implementation [46].
Experimental Protocols and Methodologies
Phantom and In Vivo Experimental Design
Comprehensive motion correction studies typically employ phantom and in vivo experiments with controlled motion paradigms [44]. The typical methodology includes:
Motion Tracking Implementation:
- Markerless optical tracking using systems like Tracoline TCL3.1 with 3D surface scans via structured light at 30Hz [44]
- Rigid-body transformation computation using iterative closest point algorithms [44]
- Cross-calibration between scanner and tracking system coordinates [44]
- Temporal calibration between tracking and scanner computers [44]
Experimental Conditions:
- Motion-free reference scans for baseline quality assessment [44]
- Controlled motion conditions with deliberate subject movement [44] [46]
- Factorized designs permuting motion/no motion and PMC on/off conditions [46]
- Correction frequency variations (e.g., Before-ET vs. Within-ET) [44]
Quantitative Assessment:
- Structural similarity index measure (SSIM) relative to reference [44]
- Visual artifact assessment by experienced reviewers [44]
- Precision quantification via coefficient of variation in tissue-specific regions [46]
Parallel Imaging Considerations
Studies specifically investigate GRAPPA calibration schemes to isolate motion correction effects:
- Integrated ACS (auto-calibration signal) acquired with motion present
- Pre-scan ACS acquired without intentional motion [44]
- Non-accelerated acquisitions to remove parallel imaging confounds [44]
The performance gap between PMC and RMC persists even with pre-scan ACS without intentional motion and without any GRAPPA acceleration, indicating fundamental advantages of prospective correction beyond parallel imaging interactions [44].
Motion Tracking and Correction Solutions
Table 2: Essential Research Tools for Motion Correction Implementation
| Tool/Resource | Type | Function/Application | Key Characteristics |
|---|---|---|---|
| Markerless Optical Tracking (Tracoline TCL3.1) [44] | Hardware | Head motion estimation via 3D surface scanning | 30Hz tracking rate; Structured light; No physical markers required |
| Moiré Phase Marker Systems (KinetiCor) [46] | Hardware | Head motion tracking with passive markers | 80Hz frame rate; sub-50μm precision; Requires mouthpiece mounting |
| retroMoCoBox [44] | Software | RMC implementation package | Adjusts k-space trajectories; GPU-based NUFFT reconstruction |
| FID Navigators [48] | Sequence | Motion detection via k-space center monitoring | Minimal sequence impact; Motion-sensitive DC component |
| mtrk Framework [50] | Software | Vendor-agnostic sequence development | Enables PMC-integrated sequences; Graphical sequence design |
| Pulseq [50] | Software | Open-source sequence prototyping | Standardized sequence representation; Vendor-neutral format |
Implementation Requirements Checklist
PMC Implementation Requires:
- Pulse sequence modification capability [44] [50]
- Real-time tracking data interface [44]
- Low-latency pose estimation (<100ms) [44]
- Geometric and temporal calibration procedures [44]
- Tracking marker mounting solution (e.g., custom mouthpieces) [46]
RMC Implementation Requires:
- Motion trajectory recording during acquisition [44]
- Computation resources for NUFFT reconstruction [44]
- K-space trajectory adjustment algorithms [44]
- Compatibility with reconstruction pipeline [44]
Emerging Trends and Future Directions
Artificial Intelligence and Deep Learning
Deep learning approaches represent a growing trend in both motion estimation and artifact correction [51] [47]. Neural networks are being applied for:
- Motion artifact reduction in image and frequency domains [51] [47]
- Motion estimation from corrupted data [51]
- Motion-corrected reconstruction [51]
These approaches show promise for handling complex motion patterns but face challenges in generalizing across diverse acquisition sequences, anatomies, and motion characteristics [47].
Hybrid Correction Strategies
Combining PMC and RMC leverages their complementary strengths [44]. Hybrid approaches apply Within-ET retrospective correction to Before-ET prospective corrected data, addressing residual intra-echo-train motion that pure PMC might miss [44]. This demonstrates that even prospective methods benefit from supplemental retrospective refinement.
Hardware and Sequence Innovations
High-performance gradient systems with increased strength (400-1000 mT/m) and slew rates (1000-9000 T/m/s) enable faster acquisitions less susceptible to motion [52]. Advanced RF coils including cryogenically-cooled arrays and implantable detectors provide SNR improvements that enhance motion correction effectiveness [52]. Open-source sequence development platforms like mtrk and Pulseq facilitate broader implementation of motion-corrected sequences across vendor platforms [50].
In magnetic resonance imaging (MRI), physiological motion—from respiration, cardiac pulsation, and patient movement—is a primary source of image degradation, potentially obscuring pathologies and compromising diagnostic accuracy. Conventional Cartesian k-space sampling sequences, which acquire data in a sequential rectilinear grid, are particularly vulnerable to these motion artifacts, as even minor displacements can cause significant blurring or ghosting. This guide provides a objective comparison of three prominent motion-resilient k-space sampling techniques: PROPELLER (Periodically Rotated Overlapping Parallel Lines with Enhanced Reconstruction), BLADE (a proprietary implementation of the PROPELLET technique), and Radial sampling. Framed within a broader thesis on motion sensitivity, this analysis synthesizes current experimental data and detailed methodologies to aid researchers and drug development professionals in selecting and optimizing sequences for robust imaging in clinical trials and biomedical research.
Core Technical Principles and Motion Resilience Mechanisms
Each technique's resilience stems from its distinct k-space trajectory, which determines how it samples the spatial frequency data that constitutes an MR image.
PROPELLER/BLADE: The PROPELLER (Periodically Rotated Overlapping Parallel Lines with Enhanced Reconstruction) technique, known commercially as BLADE (Siemens) or MultiVane (Philps), acquires data in rectangular "blades" rotated around the center of k-space [53]. Each blade contains a bundle of parallel phase-encoding lines, and successive blades are rotated at different angles around the k-space origin. This design provides two powerful mechanisms for motion correction. First, the central region of k-space, which contains the dominant image contrast information, is redundantly sampled with each blade rotation. Second, the inherent oversampling of the k-space center allows the reconstruction algorithm to detect and correct for in-plane rotations and translations between blades before final image formation.
Radial: Radial sampling (also known as projection reconstruction) acquires data along spokes radiating from the center of k-space at successively rotated angles [54]. Unlike Cartesian sampling, which fully encodes one line of k-space per repetition time (TR), radial techniques repeatedly sample the central k-space with every projection. This continuous oversampling of central k-space information makes radial sequences inherently less sensitive to motion artifacts, as motion effects are distributed radially across the image rather than creating coherent ghosting artifacts. Furthermore, specific implementations like the 3D VANE XD sequence use radial in-plane sampling with pseudo-golden-angle filling, enhancing their motion-averaging properties [54].
Figure 1: K-space sampling trajectories and their fundamental motion sensitivity characteristics. PROPELLER/BLADE and Radial techniques leverage oversampling for inherent motion resilience.
Experimental Comparison: Quantitative and Qualitative Performance
Recent prospective clinical studies provide direct comparative data on the performance of these motion-resistant sequences against conventional techniques and each other.
Thoracic Spine Imaging: Radial Versus Cartesian Sampling
A 2025 prospective study directly compared free-breathing radial sampling against Cartesian sequences for contrast-enhanced T1-weighted MRI of the thoracic spine, a region notoriously susceptible to cardiac and respiratory motion artifacts [54]. The study enrolled 48 patients with thoracic vertebral lesions, acquiring three transverse sequences after contrast administration: conventional 2D T1-weighted imaging with modified Dixon turbo spin echo (2D T1WI-mDixon-TSE, Cartesian), breath-hold 3D T1-weighted imaging with modified Dixon gradient echo (3D T1WI-mDixon-GRE, Cartesian), and free-breathing 3D VANE XD (radial). Quantitative and qualitative assessments revealed significant differences.
Table 1: Objective and Subjective Image Quality in Thoracic Spine MRI (n=48)
| Sequence Type | Specific Sequence | Signal-to-Noise Ratio (SNR) | Artifact Suppression Score (1-4) | Anatomical Clarity Score (1-4) | Overall Quality Score (1-4) |
|---|---|---|---|---|---|
| Radial | Free-breathing 3D VANE XD | 15.8 ± 3.2 | 3.90 (3.81, 3.95) | 3.85 (3.80, 3.95) | 3.90 (3.85, 3.95) |
| Cartesian (3D) | Breath-hold 3D T1WI-mDixon-GRE | 14.9 ± 2.8 | 3.55 (3.50, 3.70) | 3.45 (3.35, 3.60) | 3.50 (3.40, 3.65) |
| Cartesian (2D) | 2D T1WI-mDixon-TSE | 11.3 ± 2.5 | 2.90 (2.75, 3.08) | 2.80 (2.70, 3.00) | 2.85 (2.75, 3.00) |
Data presented as mean ± standard deviation or median (interquartile range). All differences between radial and both Cartesian sequences were statistically significant (p<0.01). SNR measured in paraspinal muscles; subjective scores based on 4-point Likert scale assessed by two radiologists [54].
The 3D VANE XD sequence demonstrated significantly higher SNR compared to both Cartesian sequences (p<0.01), attributed to its radial acquisition and oversampling of k-space center [54]. In subjective evaluations, it achieved superior scores across all domains—artifact suppression, anatomical clarity, and overall quality—with researchers concluding it "significantly improved the image quality" and supported "its integration into routine clinical practice."
Knee Joint Imaging: PROPELLER Technique for Structural Assessment
A 2025 study evaluated the diagnostic performance of different sequences in assessing osseous and cartilage changes in osteoarthritis of the knee joint [5]. While this study compared Zero Echo Time (ZTE) sequences with Proton Density Fat Saturated (PD-FS) sequences, it provides relevant context for PROPELLER applications, as it highlights how specialized sequences can optimize visualization of specific tissues. The study involved 55 patients who underwent MRI followed by arthroscopy within 3-7 days.
Table 2: Diagnostic Performance for Osseous Abnormalities in Knee Osteoarthritis
| MRI Sequence | Reader | Sensitivity (%) | Specificity (%) | Accuracy (%) |
|---|---|---|---|---|
| ZTE | 1 | 91.5 | 89.4 | 92.2 |
| PD-FS | 1 | 87.2 | 86.2 | 88.6 |
| ZTE | 2 | 92.3 | 90.7 | 93.8 |
| PD-FS | 2 | 85.9 | 87.2 | 86.1 |
Using arthroscopy as reference standard, the ZTE sequence demonstrated significantly better performance for osseous abnormalities (p<0.05) [5]. PROPELLER sequences are similarly optimized for specific clinical scenarios.
This methodology demonstrates the critical importance of matching sequence selection to diagnostic goals—a principle that extends to PROPELLER techniques, which are often employed in neurological and musculoskeletal imaging where motion artifact suppression is paramount.
Experimental Protocols and Methodologies
To enable replication and critical appraisal, this section details key experimental methodologies from the cited studies.
Thoracic Spine MRI Protocol with Radial Sampling
The prospective comparative study of thoracic spine MRI utilized a standardized protocol on a 3T MRI scanner (Philips Ingenia CX) with a 24-channel head-neck coil combined with dStream table-embedded posterior coil [54].
- Patient Population: 48 adult patients with suspected thoracic vertebral lesions; exclusion criteria included MRI contraindications, prior related treatment, or negative MRI findings.
- Contrast Administration: Gadobutrol (Gadavist, Bayer AG) administered by hand-injected intravenous bolus at 0.1 mL/kg body weight, followed by 20 mL 0.9% sodium chloride flush.
- Comparative Sequences:
- 2D T1WI-mDixon-TSE (Cartesian): Modified Dixon turbo spin echo; acquisition time: 168s
- 3D T1WI-mDixon-GRE (Cartesian): Breath-hold 3D modified Dixon gradient echo; acquisition time: 14s
- 3D VANE XD (Radial): Free-breathing radial sampling with Cartesian inter-slice acquisition; in-plane radial percentage 220%; acquisition time: 91s
- Image Analysis: Quantitative SNR measurements from paraspinal muscles; two radiologists blinded to sequence type performed subjective scoring using 4-point Likert scales for artifact suppression, anatomical clarity, and overall quality.
Knee MRI Protocol with Advanced Sequences
The knee osteoarthritis study implemented a comprehensive imaging protocol on a 1.5T scanner (Philips Ingenia) with a dedicated 16-channel knee coil [5].
- Patient Population: 55 adult patients with chronic knee pain for >1 year; exclusion criteria included metallic devices, prior knee surgery, or significant motion artifacts.
- Sequence Parameters:
- PD-FS: Sagittal, axial, and coronal planes; typical parameters: TR/TE 2000-3000/30-40ms, slice thickness 3mm
- ZTE: Sagittal, axial, and coronal planes; volumetric acquisition with ultrashort echo times
- Reference Standard: Arthroscopy performed within 3-7 days post-MRI, with direct visualization of cartilage and osseous structures.
- Image Analysis: Two musculoskeletal radiologists independently evaluated cartilage changes in 14 articular subregions using a 5-point grading system (0=normal, 4=full-thickness defect). Osseous abnormalities were assessed using a 3-point confidence scale. Sensitivity, specificity, and accuracy were calculated relative to arthroscopic findings.
Figure 2: Standardized experimental workflow for comparative evaluation of motion-resilient MRI sequences, incorporating quantitative metrics and clinical validation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Materials for Motion-Resilient MRI Studies
| Item | Function/Application | Example Specifications |
|---|---|---|
| 3T MRI Scanner | High-field imaging platform for sequence development and testing | Philips Ingenia CX 3.0T; 24-channel head-neck coil with dStream table-embedded posterior coil [54] |
| Dedicated Coil Arrays | Region-specific signal reception for optimized image quality | 16-channel dedicated knee coil (musculoskeletal studies); thoracic/abdominal coil arrays [5] |
| Contrast Agents | Enhancement of vascular and pathological tissues | Gadobutrol (Gadavist, Bayer AG) at 0.1 mL/kg body weight [54] |
| Phantom Materials | Standardized testing of sequence performance | Agarose gel phantoms with embedded magnetic particles for thermometry; structural phantoms for resolution assessment [55] |
| Motion Simulation Systems | Controlled evaluation of motion resilience | Programmable platforms for simulating respiratory, cardiac, and bulk patient motion |
| Image Analysis Software | Quantitative assessment of image quality | SNR measurements, contrast-to-noise calculations, qualitative scoring modules [54] |
The comparative evidence demonstrates that both radial and PROPELLER/BLADE techniques offer substantial advantages over conventional Cartesian sequences in motion-prone imaging scenarios. The radial 3D VANE XD sequence shows particular promise for thoracic imaging where respiratory and cardiac motion cannot be controlled, providing excellent SNR and artifact suppression in free-breathing patients. PROPELLER/BLADE techniques remain valuable for neurological and musculoskeletal applications where their motion correction algorithms effectively address both bulk patient motion and physiological pulsations.
For researchers designing clinical trials and drug development professionals establishing imaging endpoints, the strategic selection of motion-resilient sequences should be guided by the anatomical region, patient population, and specific physiological motions anticipated. Implementation of these techniques can significantly reduce scan failures and rescans, improve quantitative imaging reliability, and ultimately enhance the detection of true treatment effects by minimizing motion-induced artifacts. As MRI technology evolves, integration of artificial intelligence with these acquisition techniques—such as Philips' SmartSpeed with Adaptive-CS-Net—further promises to accelerate acquisition times while maintaining or improving motion robustness [56].
Magnetic Resonance Imaging (MRI) has long been hindered by an inherent limitation: the inability to effectively visualize tissues with very short T2 relaxation times, such as cortical bone. Conventional MRI sequences with echo times (TEs) of several milliseconds cannot capture the rapidly decaying signals from these tissues before they disappear. Zero Echo Time (ZTE) MRI represents a paradigm shift in magnetic resonance technology, utilizing ultrafast readouts with nominal TE = 0 to directly capture signals from short-T2 tissues that are otherwise MR-invisible [57] [58].
This technical advancement carries profound implications for both musculoskeletal and neurological imaging, particularly within the context of motion sensitivity comparison across MRI pulse sequences. ZTE's fundamental physics principles—including 3D center-out radial k-space sampling and nearly silent operation—provide inherent resistance to motion artifacts that commonly plague clinical imaging [57] [58]. This article provides a comprehensive comparison of ZTE's performance against established imaging alternatives, examining its growing role as a viable radiation-free substitute for CT in bone imaging while analyzing its technical capabilities relative to other motion-resistant sequences.
Technical Principles and Motion Resistance of ZTE
Fundamental Physics of ZTE Imaging
ZTE MRI operates on principles distinct from conventional pulse sequences. The technique is based on the Rotating Ultra-Fast Imaging Sequence (RUFIS) concept, employing a constant readout gradient amplitude in combination with short block-pulse RF excitation [57]. With the readout gradient maintained constant, spatial signal encoding commences immediately at RF excitation, resulting in nominal zero echo time (TE = 0) free induction decay (FID) acquisition [57]. This enables capture of short-lived MRI signals from tissues with extremely brief T2 times, such as cortical bone, tendons, and ligaments [57] [58].
The sequence utilizes 3D center-out radial k-space sampling, where the direction (but not amplitude) of the x, y, z readout gradient updates between repetitions [57]. By arranging 3D radial spokes so their endpoints follow a smooth spiral trajectory along the surface of 3D spherical k-space, gradient switching reduces to inaudible levels, enabling near-silent imaging [58]. This approach additionally provides exceptionally short repetition times (TR) and inherent resistance to MRI artifacts, including those from eddy currents and patient motion [57] [58].
Motion-Insensitive Properties and Comparative Advantages
ZTE's inherent motion resistance stems from its radial k-space sampling scheme. Unlike Cartesian sequences that sample k-space in a rectilinear grid, radial techniques acquire data along spokes passing through k-space center, providing oversampling of central k-space that confers natural robustness to motion artifacts [57] [58]. This characteristic proves particularly valuable for imaging anatomies prone to involuntary motion (e.g., head and neck, joints) and for patients unable to remain still.
The silent operation of ZTE sequences further enhances motion resistance by reducing patient anxiety and startle responses [58]. Table 1 compares ZTE's technical specifications against other motion-resistant MRI sequences, highlighting its unique combination of features for challenging imaging scenarios.
Table 1: Technical Comparison of Motion-Resistant MRI Sequences
| Sequence | K-Space Trajectory | Echo Time (TE) | Acoustic Noise | Key Motion-Resistant Features | Primary Clinical Applications |
|---|---|---|---|---|---|
| ZTE | 3D radial center-out | ~0 μs (nominal) | Near-silent | Oversampled central k-space, short TR | Bone imaging, silent neuroimaging, pediatric imaging |
| Radial MultiVane (PROPELLER) | 2D radial blades | Conventional (e.g., 80 ms) | Moderate | Blade-based oversampling, phase correction [59] [31] | Prostate urethra visualization, abdominal imaging |
| Single-Shot Fast Spin Echo (SSFSE) | Cartesian | Conventional (e.g., 80 ms) | Moderate | Complete k-space coverage in single shot [59] [31] | Fetal MRI, abdominal imaging, motion-prone patients |
Musculoskeletal Applications: ZTE as a CT Alternative
Glenoid Assessment in Shoulder Instability
The evaluation of glenoid bone loss represents a critical application where ZTE demonstrates particular promise as a CT alternative. In a comprehensive study comparing 3D ZTE MRI against 3D CT for glenoid assessment, researchers implemented a rigorous experimental protocol on both ex vivo specimens and in vivo patients with glenohumeral instability [60].
Table 2: Experimental Protocol for Glenoid Assessment Study [60]
| Parameter | Ex Vivo Specimens | In Vivo Patients | CT Protocol |
|---|---|---|---|
| Sample Size | 6 shoulder specimens | 10 patients with instability | Same patients |
| ZTE Resolutions | 1.0 mm³, 0.8 mm³, 0.6 mm³ | 1.0 mm³, 0.8 mm³, 0.7 mm³ | 0.625 mm slice thickness |
| ZTE Parameters | TE/TR: 0/0.8-1.1 ms, Flip angle: 1°, Bandwidth: ±62.50 kHz | Same as ex vivo | 120 kVp, pitch 0.98 |
| Analysis Method | 3D volume-rendered images, glenoid width measurement | Identical method | Identical method |
| Readers | Two musculoskeletal radiologists (10 and 8 years' experience) | Same readers | Same readers |
The study results demonstrated remarkable agreement between ZTE and CT reference standards. Intraclass correlation coefficients (ICCs) for intermodality assessment showed almost perfect agreement for both readers, ranging from 0.949-0.991 for the ex vivo study and 0.955-0.987 for in vivo patients [60]. Excellent interobserver agreement was also demonstrated for both ex vivo (ICCs ≥ 0.98) and in vivo (ICCs ≥ 0.92) studies [60]. Bland-Altman analyses revealed minimal mean differences in glenoid width measurements: 0.3-0.6 mm at 0.8 mm³ MRI resolution for ex vivo specimens and 0.5-0.6 mm at 0.8 mm³ resolution for patients [60]. Post-processing times to generate 3D glenoid images were clinically practical, ranging from 33-64 seconds for ZTE MRI compared to 32-46 seconds for CT [60].
Temporomandibular Joint (TMJ) Osseous Evaluation
ZTE's capability for bone assessment extends to the complex anatomy of the temporomandibular joint. A 2020 study evaluated ZTE-MRI against cone-beam CT (CBCT) for detecting osseous changes in TMJ disorder, employing a protocol with isotropic three-dimensional proton-density weighted ZTE scans (TE/TR: 0/785 ms, flip angle: 4°, resolution: 1.0 mm) [61].
Two radiologists independently evaluated 40 joints from 20 patients for osseous changes including flattening, erosion, osteophyte, and sclerosis [61]. The study reported nearly perfect agreement between ZTE-MRI and CBCT for flattening, osteophyte, and sclerosis of the condyle, and all types of bone changes in the mandibular fossa (κ = 0.80–0.90) [61]. Erosion of the condyle showed substantial agreement (κ = 0.65–0.70) [61]. Both intraexaminer and interexaminer agreement analyses demonstrated high reproducibility (κ > 0.80) comparable to CBCT [61]. These findings position ZTE-MRI as a comprehensive diagnostic tool for TMJ disorders, potentially enabling simultaneous assessment of both disc pathology and bone changes within a single MRI examination without ionizing radiation.
Neurological Applications: Silent Imaging and Bone Visualization
Head and Neck Neuroimaging
In neurological applications, ZTE addresses two significant challenges: acoustic noise that causes patient discomfort and inability to directly visualize bony structures. ZTE neuroimaging operates at significantly reduced acoustic noise levels compared to conventional sequences, as gradient switching is minimized to inaudible levels [58]. This silent operation proves particularly beneficial for pediatric patients, individuals with anxiety disorders, and functional studies where startle responses confound results.
ZTE's capacity for direct bone visualization in the head and neck enables robust applications including assessment of craniofacial malformations, trauma, tumors, and interventional procedures [57]. The technique generates "CT-like" images of the skull base, calvarium, and facial bones while simultaneously providing conventional soft tissue MRI contrasts [57] [58]. This facilitates a "one-stop-shop" approach where both soft tissue and bony anatomy can be evaluated in a single acquisition without patient repositioning or multiple examinations.
Technical Implementation in Neuroimaging
Implementing ZTE in neurological protocols requires specific technical considerations. The sequence employs non-selective volume excitation with 3D radial center-out k-space encoding, maintaining constant readout gradient amplitude throughout scanning with only minor directional updates between repetitions [57]. For a typical ZTE neuroimaging protocol with imaging bandwidth BWRX = 62.5 kHz and 3D isotropic image matrix of 256³ points, the repetition time is exceptionally short (TR ~2 ms), enabling rapid acquisition [57].
A limitation in conventional ZTE implementations is the flip angle restriction to approximately 4°, though recent advances in pulse encoding have enabled higher flip angle excitations by extending RF pulse duration [57]. Image reconstruction requires 3D gridding algorithms to handle the non-Cartesian radial sampling, with advanced methods including parallel imaging, total generalized variation regularization, compressed sensing, and deep learning reconstruction now available through open-source toolboxes [57].
Figure 1: ZTE MRI pulse sequence workflow demonstrating the continuous acquisition process with immediate signal readout and silent gradient updates that enable motion-resistant imaging.
Comparative Performance Analysis Across Anatomical Regions
Quantitative Comparison of ZTE Performance
The efficacy of ZTE imaging must be evaluated against established reference standards across different anatomical regions. Table 3 summarizes quantitative performance metrics from multiple clinical studies, providing objective data for sequence comparison.
Table 3: Quantitative Performance of ZTE Across Anatomical Regions
| Anatomical Region | Reference Standard | Agreement Metric | Performance Outcome | Key Clinical Advantage |
|---|---|---|---|---|
| TMJ (Osseous Changes) | CBCT | Prevalence-adjusted κ | 0.80-0.90 (near perfect) for all parameters except erosion (0.65-0.70, substantial) [61] | Simultaneous disc and bone assessment without radiation |
| Glenoid Width Measurement | CT | ICC (Intermodality) | 0.949-0.991 (ex vivo), 0.955-0.987 (in vivo) [60] | Eliminates need for separate CT in instability workup |
| Glenoid Width Measurement | CT | Bland-Altman Mean Difference | 0.3-0.6 mm (0.8 mm³ resolution, ex vivo) [60] | Submillimeter accuracy comparable to CT |
| General Bone Neuroimaging | CT | Qualitative Assessment | Excellent for craniofacial malformations, trauma, tumors [57] | One-stop-shop neuroimaging with radiation dose reduction |
Comparison With Other Motion-Resistant Sequences
While ZTE offers unique advantages for short-T2 tissue visualization, other motion-resistant sequences excel in specific clinical scenarios. The radial PROPELLER-based sequence (MultiVane XD) demonstrated superior performance for prostatic urethra visualization compared to single-shot fast-spin echo (SSFSE) in prostate cancer MR simulation [59] [31]. In this application, readers scored urethral visibility significantly higher in radial MultiVane XD series compared to SSFSE (18/22 and 17/22 cases for two readers, P < 0.0001) [59] [31].
This comparative analysis reveals a fundamental principle in motion-resistant MRI: different motion mitigation strategies benefit specific clinical applications. ZTE's strength lies in its direct bone visualization and silent operation, while radial PROPELLER techniques excel in soft tissue contrast maintenance with motion correction. Single-shot methods provide the fastest acquisition for uncooperative patients but may sacrifice resolution and contrast.
The Scientist's Toolkit: Essential Research Reagents and Materials
Implementing ZTE research requires specific technical resources and methodological tools. The following reagents and solutions represent core components for experimental investigations in ZTE methodology and applications.
Table 4: Essential Research Toolkit for ZTE Imaging Investigations
| Research Reagent/Resource | Function/Application | Example Specifications | Experimental Purpose |
|---|---|---|---|
| 3D ZTE Pulse Sequence | Core imaging sequence | TE/TR: 0/0.8-1.1 ms, Flip angle: 1-4°, Radial spokes: N² [57] [60] | Primary data acquisition for short-T2 tissues |
| RIESLING Reconstruction Toolbox | Open-source image reconstruction | 3D gridding, parallel imaging, compressed sensing [57] | Reconstruction of radial k-space data |
| High-Performance Gradient System | Enable ultrafast switching | Amplitude: 40-80 mT/m, Slew rate: 150-200 T/m/s [57] | Support for short TR and constant gradients |
| Multi-Channel RF Coils | Signal reception | 8-64 channels, region-specific designs [60] | Signal-to-noise ratio optimization |
| CT/CBCT Reference Images | Validation standard | Isotropic resolution (0.5-1.0 mm) [61] [60] | Gold standard comparison for bone imaging |
| Digital Phantom Objects | Sequence validation | Materials with known short-T2 properties [57] | Technical validation and optimization |
Zero Echo Time MRI represents a significant advancement in musculoskeletal and neurological imaging, with proven capabilities for direct visualization of short-T2 tissues and inherent motion resistance. The technology demonstrates remarkable agreement with CT for osseous assessment across multiple anatomical regions (ICC 0.949-0.991) while eliminating ionizing radiation exposure [61] [60]. ZTE's near-silent operation and 3D radial sampling provide inherent motion robustness superior to conventional Cartesian sequences [57] [58].
Future developments in ZTE technology will likely focus on expanding contrast mechanisms through magnetization preparation, enabling T1, T2, T2*, magnetization transfer, angiographic, and diffusion contrasts within the ZTE framework [57] [58]. Reconstruction algorithms will continue to evolve, incorporating deep learning methods to further reduce scan times and enhance image quality [57]. As these technical refinements progress, ZTE is positioned to expand its clinical role in comprehensive "one-stop-shop" examinations, pediatric imaging, and interventional procedures where silent operation and bone visualization provide distinct diagnostic advantages.
The motion sensitivity comparison across MRI pulse sequences reveals a diversified landscape where ZTE, radial PROPELLER, and single-shot techniques each occupy complementary niches. ZTE's unique combination of direct bone imaging, silent operation, and inherent motion resistance establishes it as a valuable addition to the MRI pulse sequence arsenal, particularly for applications where CT avoidance is prioritized and for patient populations requiring minimal-acoustic noise environments.
Pharmacological MRI (phMRI) has emerged as a powerful, non-invasive technology for evaluating drug effects on the central nervous system (CNS) in vivo, offering tremendous potential to make CNS drug development more efficient [62]. By assessing changes in brain function in response to pharmacological challenges, phMRI provides objective data on drug action in the living brain, mapping the systems and networks targeted by psychoactive compounds [63] [62]. However, the technique faces a fundamental challenge: its pronounced sensitivity to subject motion, which can compromise data integrity and confound the interpretation of drug-induced hemodynamic changes [1].
This inherent vulnerability stems from MRI's prolonged data acquisition time, which far exceeds the timescale of most physiological motions, including involuntary movements, cardiac and respiratory cycles, and blood pulsation [1]. The problem is particularly acute in phMRI for several reasons. First, studies often involve animal models (especially mice), where small brain size, rapid metabolic rates, and the need for anesthesia present additional complications [63]. Second, patient populations with CNS disorders may have limited ability to remain still during scanning. Third, the drugs being investigated may themselves induce motion, either through direct effects on movement or by reducing a subject's capacity to comply with instructions to remain still [62]. Consequently, understanding and mitigating motion artifacts is not merely a technical concern but a fundamental prerequisite for reliable phMRI application in drug development pipelines.
Motion Artifacts in MRI: Physics, Origins, and Manifestations
Physical Principles of Motion Artefacts
Subject motion during MRI introduces inconsistencies in the acquired data, leading to various image artifacts. Spatial encoding in MRI is an intrinsically slow and sequential process that occurs in Fourier or "k-space," which corresponds to the spatial frequency spectrum of the imaged object [1]. Each sample in k-space contains global information about the entire image; therefore, any inconsistency between different portions of k-space data resulting from motion violates the fundamental assumption of a stationary object during image reconstruction [1].
The interaction between motion type and k-space sampling strategy determines the specific artifact manifestation. Periodic motion synchronized with k-space acquisition produces coherent ghosting—partial or complete replication of structures along the phase-encoding direction. Sudden motion causes inconsistent data segments, resulting in blurring and incoherent ghosting, which appears as multiple overlapping replicas or stripes. Slow continuous drifts primarily affect sequences with interleaved k-space acquisitions, such as Turbo Spin Echo (TSE) sequences [1].
Unique Manifestations in phMRI
In phMRI studies, motion artifacts pose a particularly insidious problem because they can masquerade as—or obscure—genuine drug-induced hemodynamic changes. A subject's slight movement after drug administration might produce signal changes that could be misinterpreted as neurovascular coupling responses to the pharmacological challenge. This risk is amplified when using intravascular contrast agents like ultrasmall superparamagnetic iron oxide (USPIO) particles, which themselves alter magnetic susceptibility [63] [64]. The resulting susceptibility artifacts can combine with motion-induced distortions, creating complex artifacts that challenge conventional correction methods [64].
Comparative Analysis of Motion Sensitivity Across Pulse Sequences
Different MRI pulse sequences exhibit varying susceptibility to motion artifacts, making sequence selection crucial for successful phMRI experiments. The table below summarizes the motion sensitivity and optimal use cases of sequences relevant to phMRI.
Table 1: Motion Sensitivity Comparison of MRI Pulse Sequences
| Pulse Sequence | Motion Sensitivity | Primary Artifact Types | Pros for phMRI | Cons for phMRI |
|---|---|---|---|---|
| Gradient-Echo (GRE) [63] | High | Ghosting, signal loss | High sensitivity to BOLD/CBV contrast; essential for functional imaging | Strong sensitivity to magnetic field inhomogeneities |
| Fast Spin Echo (FSE/TSE) [65] | Moderate | Blurring (with slow drifts) | Faster acquisition than conventional SE; good T2 contrast | Multiple 180° refocusing pulses can extend acquisition time |
| Single-Shot FSE (SSFSE/HASTE) [59] [65] | Low | Minimal ghosting | Very rapid acquisition; freezes motion | Lower spatial resolution; reduced SNR |
| Radial (BLADE/PROPELLER) [1] [59] | Low | Streaking | Innate motion correction; oversampled center of k-space | Longer reconstruction times; specific contrast properties |
| Steady-State Free Precession (TrueFISP/FIESTA) [65] | Moderate | Banding artifacts | High SNR efficiency; good for cardiac imaging | Sensitive to field inhomogeneities |
As evidenced by clinical studies, sequences with inherent motion resistance demonstrate superior performance in challenging imaging scenarios. In a comparison of motion-insensitive T2-weighted sequences for prostate imaging, the radial sampling-based Multivane XD (MVXD) sequence significantly outperformed Single-Shot Fast Spin Echo (SSFSE) in visualizing the prostatic urethra, with experts assigning higher visibility scores in the majority of cases [59]. This demonstrates the practical advantage of motion-robust sequences in clinical applications where subject movement is anticipated.
Motion Challenges in phMRI Across Drug Development Phases
The impact of motion artifacts and the utility of motion-corrected phMRI vary significantly across different phases of CNS drug development, as summarized in the table below.
Table 2: phMRI Motion Challenges and Solutions Across Drug Development Phases
| Phase | Primary Goals | Motion Challenges | Motion Mitigation Strategies |
|---|---|---|---|
| Phase I [62] | Assess CNS penetration, target engagement, dosing | First-in-human anxiety; drug-induced side effects; healthy volunteer movement | Motion-insensitive sequences; physiological monitoring; rapid acquisition |
| Phase II [62] | Establish efficacy, dose-response, side effect profile | Patient populations with movement disorders; drug-induced movements; placebo response variability | Advanced motion correction; physiological monitoring; patient-specific protocols |
| Phase III [62] | Confirm efficacy, monitor adverse reactions, compare to standard treatments | Multi-center protocol standardization; diverse patient populations | Standardized motion-correction pipelines; centralized quality control |
In Phase I trials, phMRI can objectively demonstrate CNS penetration and target engagement, even for drugs not amenable to positron emission tomography (PET) imaging [62]. Motion control is crucial here, as artifacts could misleadingly suggest either CNS activity or lack thereof. For Phase II studies, phMRI helps differentiate drug efficacy from placebo effects—a significant challenge in CNS trials where placebo response rates have progressively increased [62]. Motion artifacts can contribute to this variance, necessitating robust acquisition and processing methods. In Phase III, standardized motion correction across multiple sites ensures consistent data quality for regulatory decision-making [62].
Motion Correction Methodologies: From Acquisition to Reconstruction
Acquisition-Based Strategies
Proactive motion prevention begins with patient preparation, comfort optimization, and clear communication. For animal studies, appropriate anesthesia and physiological monitoring are essential, as demonstrated in murine phMRI protocols where body temperature, respiration, and anesthesia levels were meticulously maintained [63].
Sequence selection represents the most fundamental acquisition-based strategy. Single-shot techniques like SSFSE/HASTE effectively "freeze" motion by acquiring all necessary k-space data after a single excitation pulse [59] [65]. Radial (PROPELLER/BLADE) sequences acquire data in rotating "blades" around k-space center, providing inherent oversampling of central k-space that facilitates both motion detection and correction during reconstruction [1] [59].
Post-Processing Correction Techniques
For phMRI data requiring high temporal resolution, post-processing methods are indispensable. Image-based registration algorithms estimate and correct for motion between successive volumes. However, these methods have limitations—they cannot correct for distortions caused by through-plane motion or spin history effects.
Diagram: Motion Correction Workflow for Parametric fMRI Data
For parametric imaging data, such as multi-echo acquisitions used for T2* mapping, motion correction should be performed using the I0-parameter maps (proportional to proton density), which provide more reliable motion estimation than individual echo images or the resulting T2* parameter maps themselves [66]. The estimated motion parameters can then be applied to correct the T2* maps [66].
Experimental Protocols for phMRI Motion Management
Murine phMRI Cocaine Challenge Protocol
A comprehensive phMRI protocol from cocaine challenge studies in mice illustrates multiple motion mitigation strategies [63]:
- Animal Preparation: Female C57BL/6J mice were anesthetized with isoflurane (1.5-1.7% in N2/O2 70%/30%). Rectal temperature was maintained at 36-38°C using heated air. Respiratory rate was maintained at 80-120 breaths/minute.
- Contrast Agent Administration: USPIO contrast agents (MION, MoldayION, or P904) were administered via tail vein catheter to enhance CBV-weighted contrast.
- Image Acquisition: Imaging was performed at 7T using a 2D multiple gradient echo sequence with TR=600ms, four echoes (TE=2.5, 6.0, 9.5, 13ms), and temporal resolution of one minute.
- Motion Management: An integrated head mask minimized head motion. Physiological monitoring ensured stable anesthesia depth. Pre-imaging autoshimming achieved a 1H linewidth <0.13ppm to reduce susceptibility artifacts.
- Pharmacological Challenge: Cocaine (30mg/kg) was administered via intraperitoneal catheter while the animal remained positioned inside the magnet.
This protocol highlights how meticulous preparation and specialized hardware can mitigate motion in preclinical phMRI, revealing cocaine-induced CBV reductions particularly pronounced in the nucleus accumbens [63].
Optimized Pulse Sequence Design
Emerging approaches address motion sensitivity through fundamentally redesigned pulse sequences. Magnetic Resonance Fingerprinting (MRF) uses highly undersampled, varying acquisition parameters to generate unique signal time courses for different tissues [67]. This approach enables simultaneous quantification of multiple tissue parameters (T1, T2, PD) from a single rapid acquisition.
Recent algorithmic design of MRF pulse sequences has discovered patterns with intrinsic robustness to undersampling artifacts and phase variation—common sources of shading artifacts in quantitative parameter maps [67]. These optimized sequences achieve fourfold shorter scan times than human-designed sequences of equivalent precision, significantly reducing motion vulnerability [67].
Diagram: Magnetic Resonance Fingerprinting (MRF) Optimization
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for phMRI Motion Management
| Item | Function | Example/Specification |
|---|---|---|
| USPIO Contrast Agents [63] | CBV-weighting for enhanced phMRI sensitivity | MION (~40nm), MoldayION (~30nm), P904 (25-30nm); doses of 15-35 mg/kg |
| Animal Monitoring Systems [63] | Physiological parameter maintenance during anesthesia | Respiratory monitoring (BIOPAC Systems), temperature monitoring (Opsens OTG-M) |
| Radial Sampling Sequences [59] | Motion-insensitive data acquisition | MVXD/PROPELLER with SENSE acceleration; 2-3 minute acquisition times |
| Motion Correction Algorithms [66] | Post-processing motion compensation | Parametric fMRI correction using I0 maps for motion estimation |
| Digital Phantoms [67] | Pulse sequence optimization | Accelerated digital phantoms for systematic error evaluation in MRF |
| Multi-echo Acquisition [66] | Robust parameter mapping | Multiple TEs for T2* mapping; motion correction from I0 parameter maps |
Motion artifacts present a formidable challenge in pharmacological MRI, potentially compromising data integrity and confounding the interpretation of drug effects on brain function. However, through strategic pulse sequence selection, meticulous experimental design, and advanced processing techniques, researchers can effectively mitigate these challenges. Motion-resistant sequences like radial acquisitions and single-shot methods provide robust foundations for phMRI studies, while emerging technologies like optimized MRF offer promising avenues for inherently motion-robust quantitative imaging. As phMRI continues to evolve as a critical tool in CNS drug development, integrating these motion management strategies will be essential for generating reliable, interpretable data across all phases of clinical trials, ultimately contributing to more efficient development of novel therapeutics for brain disorders.
Optimizing Protocols and Troubleshooting Motion Artefacts in Practice
Patient motion remains a significant challenge in magnetic resonance imaging (MRI), often compromising diagnostic image quality and leading to scan repetitions, increased costs, and patient discomfort. While pre-scan preparation strategies encompassing patient comfort, clear instruction, and physical stabilization are fundamental, the inherent motion sensitivity of MRI pulse sequences varies substantially. Within the broader context of motion sensitivity comparison across MRI pulse sequences research, this guide objectively compares the performance of motion-resistant sequences against conventional alternatives. We present supporting experimental data and detailed methodologies to assist researchers, scientists, and drug development professionals in selecting optimal sequences for clinical trials and imaging studies where motion control is paramount. The subsequent sections provide a quantitative analysis of motion-insensitive sequences, delineate experimental protocols, and visualize the logical framework for sequence selection.
Comparative Analysis of Motion-Resistant MRI Sequences
The selection of a pulse sequence is a critical determinant of an image's susceptibility to motion artifacts. Conventional Cartesian k-space sampling (used in sequences like MPRAGE and SSFSE) is highly vulnerable to motion, which can disrupt the orderly filling of k-space and create glaring ghosts or blurring. In contrast, motion-resistant sequences employ non-Cartesian k-space trajectories, such as radial (stack-of-stars) or PROPELLER (Periodically Rotated Overlapping Parallel Lines with Enhanced Reconstruction) sampling. These techniques oversample the center of k-space, making the final image more resilient to motion because any disruption is spread across the entire image as a minor noise-like artifact rather than a coherent artifact.
The quantitative performance of several motion-resistant sequences is summarized in the table below, with data extracted from recent comparative studies.
Table 1: Performance Comparison of Motion-Resistant vs. Conventional MRI Sequences
| Anatomical Region | Motion-Resistant Sequence | Conventional Sequence | Key Performance Metric | Motion-Resistant Performance | Conventional Sequence Performance | P-value |
|---|---|---|---|---|---|---|
| Brain (Tumor) | SOS echo-uT1RESS [4] | MPRAGE [4] | Tumor-to-Brain Contrast | 0.7 ± 0.4 [4] | 0.4 ± 0.3 [4] | < 0.001 [4] |
| Brain (Tumor) | SOS echo-uT1RESS [4] | MPRAGE [4] | Lesion Conspicuity (4-point scale) | Significantly improved [4] | Baseline [4] | < 0.001 [4] |
| Prostate (Urethra) | MultiVane XD (MVXD) [31] | Single-Shot FSE (SSFSE) [31] | Urethral Visibility (5-point scale) | Superior in ~80% of cases [31] | Lower in majority of cases [31] | < 0.0001 [31] |
| Prostate (Urethra) | MultiVane XD (MVXD) [31] | Single-Shot FSE (SSFSE) [31] | Signal-to-Noise Ratio (SNR) | Superior in all cases [31] | Lower in all cases [31] | Not specified [31] |
| Knee (Bone) | Zero Echo Time (ZTE) [5] | PD-FS [5] | Sensitivity for Bony Abnormalities | 91.5% - 92.3% [5] | 85.9% - 87.2% [5] | < 0.05 [5] |
| Knee (Bone) | Zero Echo Time (ZTE) [5] | PD-FS [5] | Accuracy for Bony Abnormalities | 92.2% - 93.8% [5] | 86.1% - 88.6% [5] | < 0.05 [5] |
The data demonstrates a clear trend: motion-resistant sequences consistently outperform their conventional counterparts in the presence of motion, providing higher diagnostic confidence. The radial sampling in SOS echo-uT1RESS not only mitigates motion but also provides a inherent dark-blood effect, improving lesion conspicuity for brain tumors [4]. For prostate imaging, the MVXD sequence (a PROPELLER-based technique) proved vastly superior for visualizing the prostatic urethra without a Foley catheter, a critical advancement for radiation therapy simulation [31]. Meanwhile, ZTE sequences, by capturing data almost immediately after excitation, are exceptionally robust to motion and provide CT-like bone visualization, outperforming standard PD-FS sequences in detecting osseous abnormalities in the knee [5].
Experimental Protocols for Motion Sensitivity Evaluation
To ensure the validity and reproducibility of motion sensitivity comparisons, a structured experimental approach is essential. The following methodologies are synthesized from the cited studies.
Protocol 1: Evaluation of Brain Tumor Sequences
This protocol is designed to compare sequences for visualizing enhancing brain lesions, particularly in the context of patient motion.
- Patient Cohort: A prospective, two-center study design is recommended. Participants should have known contrast-enhancing brain tumors (e.g., primary intra-axial, metastases, extra-axial). Standard exclusion criteria include general MRI contraindications and impaired renal function [4].
- MRI Acquisition: All patients undergo 3T MRI. The protocol must include the standard sequence (e.g., MPRAGE) and the motion-resistant prototype (e.g., SOS echo-uT1RESS) after administration of 0.1 mmol/kg of gadolinium-based contrast. Key parameters for SOS echo-uT1RESS include: a stack-of-stars k-space trajectory, non-selective saturation recovery preparation, and a 3D reversed fast imaging with steady-state free precession (PSIF) readout [4].
- Quantitative Analysis:
- Region-of-Interest (ROI) Measurement: Signal intensity (SI) is measured in the enhancing lesion (excluding necrosis), normal white matter, and adjacent air.
- Tumor-to-Brain Contrast: Calculate using the formula: (SItumor - SIWM) / SIWM [4].
- Contrast-to-Noise Ratio (CNR): Calculate using the formula: (SItumor - SIWM) / SDair [4].
- Qualitative Analysis: Blinded readers score overall image quality, lesion conspicuity, and image artifacts on a 4-point Likert scale. Side-by-side comparison of diagnostic performance for features like vascular involvement is crucial [4].
Protocol 2: Evaluation of Prostatic Urethra Visualization
This protocol assesses sequences for delineating delicate anatomy susceptible to motion from respiration and peristalsis.
- Patient Cohort: Patients undergoing MRI simulation for prostate cancer radiation therapy, imaged without a Foley catheter to avoid discomfort and anatomical displacement [31].
- MRI Acquisition: Imaging is performed on a 3T scanner. The compared sequences should include a radial sequence (e.g., MVXD) and a Cartesian single-shot sequence (e.g., SSFSE), both acquired in the sagittal plane with high in-plane resolution and SENSE acceleration [31].
- Qualitative Analysis:
- Primary Endpoint: Prostatic urethra visibility is scored independently by multiple radiologists on a 1-to-5 scale.
- Secondary Endpoints: Readers also score signal-to-noise ratio and the presence/severity of artifacts in each series [31].
- Statistical Analysis: Use paired Student's t-tests to compare mean visibility scores and Cohen's kappa to evaluate inter-observer agreement [31].
Visualizing Sequence Selection and Experimental Workflow
The following diagrams map the logical decision process for selecting a motion-resistant sequence and the generalized workflow for a comparative motion sensitivity study.
Diagram 1: Motion-Resistant MRI Sequence Selector.
Diagram 2: Motion Sensitivity Experiment Workflow.
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers designing experiments in motion-sensitive MRI, specific "reagents" or specialized materials are required. The following table details these key components.
Table 2: Essential Materials for Motion Sensitivity Research in MRI
| Item | Function/Description | Example Applications in Research |
|---|---|---|
| 3T MRI Scanner | Provides the high main magnetic field strength necessary for advanced sequence development and high signal-to-noise ratio imaging [4] [68] [31]. | Used in all cited studies for evaluating brain, prostate, and knee imaging [4] [5] [31]. |
| Motion-Resistant Sequence Package | Vendor-provided software enabling non-Cartesian k-space trajectories (e.g., radial, PROPELLER, ZTE). | SOS echo-uT1RESS (Siemens) [4], MultiVane XD (Philips) [31], ZTE (various platforms) [5]. |
| Multi-Channel Receiver Coils | High-density phased-array coils (e.g., 32-channel head coil, combined torso arrays) essential for parallel imaging and achieving high spatial resolution [68] [31]. | Critical for accelerating acquisitions and maintaining image quality in prostate [31] and neurological [4] imaging. |
| Digital Twin Simulation Framework | A computational model of the MRI operational environment used to simulate patient arrivals, scan durations, and optimize scheduling without disrupting clinical workflow [69]. | Testing scheduling policies to minimize patient waiting times and motion from prolonged stays, thereby indirectly improving image quality [69]. |
| Phantom Test Objects | Physical objects with known properties (e.g., spheres, grids) used for system calibration and controlled motion studies. | Validating sequence performance and quantifying artifact levels before human subject studies. |
| Blinded Reader Software | A picture archiving and communication system (PACS) workstation or dedicated software that randomizes and presents images to readers for qualitative scoring [4]. | Enabling unbiased assessment of image quality, artifact presence, and diagnostic confidence in comparative studies [4] [31]. |
The strategic implementation of motion-resistant MRI pulse sequences represents a powerful tool for mitigating one of the most persistent challenges in diagnostic imaging. As the experimental data demonstrates, sequences employing radial, PROPELLER, and ZTE acquisitions consistently outperform conventional Cartesian sequences in the presence of motion, providing superior visualization of critical anatomy from the brain to the joints. For the research and drug development community, the adoption of these sequences, coupled with the rigorous experimental frameworks and tools outlined in this guide, can significantly enhance the quality and reliability of imaging data in clinical trials. This approach ensures that pre-scan prevention extends beyond patient comfort and instruction to include the fundamental technological selection of the imaging protocol itself.
This guide provides a comparative analysis of parameter adjustment in MRI, focusing on TR/TE, NEX, and Echo Train Length (ETL) optimization. The content is framed within a broader research thesis on motion sensitivity comparison across MRI pulse sequences. For researchers and drug development professionals, understanding these relationships is crucial for designing robust imaging protocols that minimize motion artifacts while maximizing data quality in clinical and preclinical studies. The integration of advanced hardware and reconstruction software has redefined traditional parameter trade-offs, enabling unprecedented resolution in functional and structural imaging, particularly for the brain [70].
Core Parameter Definitions and Motion Sensitivity
Key Parameters and Their Physiological Interactions
- Repetition Time (TR) directly controls the scan time and influences T1-weighted contrast. Shorter TR values increase the sequence's sensitivity to patient motion, as any movement during the rapidly repeated sequence can lead to significant data corruption across multiple k-space lines.
- Echo Time (TE) is a primary determinant of T2-weighted contrast. Longer TE values amplify the impact of motion due to increased susceptibility to T2* signal decay and spin dephasing during the extended signal readout period, which is exacerbated in fluid-filled tissues or areas with magnetic field inhomogeneities [70].
- Number of Excitations (NEX), also known as averages, improves signal-to-noise ratio (SNR) at the cost of prolonged acquisition time. While increasing NEX can average out random motion effects, it simultaneously increases the probability of motion occurrence throughout the lengthened scan, creating a complex relationship with motion sensitivity [71].
- Echo Train Length (ETL) defines how many k-space lines are filled per TR in fast spin-echo sequences. Longer ETL reduces scan time but extends the readout duration for each TR, potentially increasing blurring and motion sensitivity within the echo train, particularly when motion occurs during the extended sampling window [70].
Quantitative Impact on Signal and Quality
Table 1: Parameter Impact on Image Quality and Acquisition
| Parameter | Primary Effect | Impact on Scan Time | Motion Sensitivity Relationship |
|---|---|---|---|
| TR | T1 weighting | Directly proportional (↑TR = ↑Time) | Shorter TR more sensitive to periodic motion |
| TE | T2 weighting | Minimal direct effect | Longer TE increases sensitivity to B0 inhomogeneity and motion-induced dephasing |
| NEX | Signal-to-Noise Ratio (SNR) | Directly proportional (↑NEX = ↑Time) | Higher NEX can average out random motion but increases chance of motion occurrence |
| ETL | Blurring/Point Spread Function | Inversely proportional (↑ETL = ↓Time) | Longer ETL increases sensitivity to motion within the echo train |
Experimental Comparison of Sequence Performance
Ultra-High-Resolution Neuroimaging at 7T
Advanced gradient systems enable dramatic parameter adjustments that fundamentally change motion sensitivity profiles. The NexGen 7T scanner with Impulse gradient coil achieves performance metrics of 200 mT/m amplitude and 900 T/m/s slew rate, allowing for significantly shorter echo spacing and TE compared to conventional systems [70].
Table 2: Gradient Performance Comparison for High-Resolution fMRI
| Gradient Coil | Max Amplitude (mT/m) | Max Slew Rate (T/m/s) | Minimum Echo Spacing (ms) | Achievable Resolution (iso, mm) | Minimum TE for 0.5mm (ms) |
|---|---|---|---|---|---|
| Impulse (Head-only) | 200 | 900 | 0.58 | 0.45 | 23 |
| AC84 (Head-only) | 80 | 400 | ~0.80 | 0.61 | ~35 |
| SC72 (Whole-body) | 80 | 200 | 1.41 | 0.70 | 45 |
Experimental protocol for evaluating resolution limits: Researchers compared three gradient coils using constant TE, FOV, and phase encode lines to maintain consistent T2* decay and relative point spread function across systems. The Impulse coil demonstrated a 36% improvement in achievable resolution (0.45 mm isotropic) compared to the standard whole-body SC72 gradient (0.70 mm isotropic) under identical physiological constraints [70].
The point spread function (PSF), critical for evaluating image blurring, remains smaller for the Impulse gradient coil across resolutions, with an inflection point at approximately 0.5 mm isotropic resolution beyond which PSF begins to increase due to extended echo train length. This represents a significant advantage over conventional systems whose PSF degradation begins at much coarser resolutions [70].
Knee MRI Protocol Optimization
A prospective ethics-approved study compared a single 3D proton density nDixon TSE sequence against a conventional 2D TSE protocol for knee imaging at 3T. The experimental protocol implemented the following parameters [72]:
- 3D nDixon TSE: Voxel size = 0.7 × 0.7 × 0.7 mm³, Acquisition time = 5 minutes 55 seconds
- Conventional 2D TSE: Multiple sequence acquisitions, Total time = 12 minutes 6 seconds
The study included 32 symptomatic subjects and evaluated SNR, CNR, and diagnostic performance for cartilaginous, meniscal, and ligamentous lesions. Results demonstrated no significant difference in diagnostic performance despite a 51% reduction in acquisition time with the 3D approach. This highlights how 3D sequences with optimized parameters can maintain diagnostic quality while reducing motion vulnerability through shorter scan times [72].
Motion Artifact Reduction Techniques
Hardware and Sequence-Based Approaches
Traditional motion mitigation strategies directly interact with parameter optimization:
- Patient stabilization through comfortable positioning, foam pads, taping, or snug wrapping reduces motion at its source, potentially allowing for longer TR/TE or higher NEX values when needed for contrast or SNR [71].
- Peripheral nerve stimulation (PNS) limitations fundamentally constrain gradient performance. The NexGen 7T scanner's Impulse gradient incorporates a third winding layer specifically to minimize PNS, enabling higher slew rates (900 T/m/s) without exceeding physiological limits [70].
- Signal suppression techniques including spatial saturation pulses and fat suppression null signals from moving tissues, reducing their contribution to artifacts [71].
- Gating methods synchronize acquisition with physiological motion (cardiac, respiratory) through thoracic belts, EKG, or peripheral pulse devices, potentially extending required TR but motion-corrupting acquisitions [71].
Deep Learning for Motion Correction
Advanced reconstruction algorithms now complement parameter optimization for motion mitigation. One study trained a conditional generative adversarial network (CGAN) using 5,500 T2-weighted head MRI simulations with motion artifacts in phase-encoding directions [73].
Experimental protocol included:
- Motion simulation: Combining translational (±10 pixels) and rotational (±5°) movements applied to k-space data
- Network training: CGAN with generator-discriminator architecture compared against autoencoder and U-net models
- Evaluation metrics: Structural similarity (SSIM) and peak signal-to-noise ratio (PSNR) compared to motion-free ground truth
Results demonstrated that CGAN achieved SSIM >0.9 and PSNR >29 dB across motion directions, with approximately 26% improvement in SSIM and 7.7% improvement in PSNR compared to uncorrected images. This approach enables diagnostic quality recovery from motion-corrupted data without altering acquisition parameters [73].
An alternative approach combining CNN filtering with compressed sensing reconstruction detected and utilized only motion-unaffected phase-encoding lines (35%-50% of k-space). This method achieved PSNR of 36.1-41.5 and SSIM of 0.95-0.98, proving effective for motion artifact alleviation while preserving image details [74].
Research Toolkit: Essential Materials and Methods
Table 3: Research Reagent Solutions for Motion-Robust MRI
| Item | Function/Application | Example Implementation |
|---|---|---|
| Ultra-High Performance Gradients | Enables shorter TE/echo spacing for reduced motion sensitivity | Impulse head gradient (200 mT/m, 900 T/m/s) for 0.45 mm isotropic resolution [70] |
| Multi-Channel RF Coils | Increases SNR and parallel imaging acceleration | 96-channel receiver array with 16-channel transmit for improved g-factor and reduced PNS limitations [70] |
| Deep Learning Reconstruction | Corrects motion artifacts post-acquisition | CGAN model trained on simulated motion data (SSIM >0.9, PSNR >29 dB) [73] |
| Compressed Sensing Sequences | Enables k-space undersampling with motion robustness | Split Bregman method reconstruction from motion-unaffected PE lines only [74] |
| 3D TSE with Dixon | Provides multi-contrast imaging with reduced acquisition time | Single 3D nDixon TSE sequence (5:55 min) replacing multi-sequence 2D protocol (12:06 min) for knee MRI [72] |
Parameter Optimization Workflows
The relationship between parameter selection, hardware capability, and reconstruction methodology follows a logical progression for optimizing motion sensitivity:
Diagram 1: Parameter optimization workflow for motion-sensitive MRI applications. The process begins with clear objective definition and proceeds through iterative optimization of hardware capabilities, parameter selection, and motion mitigation strategies.
Optimizing TR/TE, NEX, and echo train length requires careful consideration of intrinsic motion sensitivity trade-offs. Current experimental data demonstrates that integrated system design combining high-performance hardware (200 mT/m gradients, 96-channel arrays) with advanced reconstruction algorithms (CGAN, compressed sensing) enables unprecedented resolution (0.45 mm isotropic) while mitigating motion sensitivity. For research applications, particularly in drug development where longitudinal consistency is crucial, 3D sequences with deep learning reconstruction provide the most promising approach for maintaining diagnostic quality despite motion challenges. The continued co-development of acquisition parameters and reconstruction technologies suggests a future where motion sensitivity may cease to be the primary limiting factor in MRI resolution and quantitative accuracy.
In magnetic resonance imaging (MRI), signal suppression techniques are indispensable for isolating pathological processes, enhancing contrast-to-noise ratios, and improving diagnostic accuracy. Among these techniques, fat suppression and spatial saturation play particularly critical roles in a wide range of clinical and research applications. The need for these strategies becomes even more pronounced when considering motion sensitivity—a fundamental challenge in MRI that can compromise image quality and quantitative measurements. Motion artifacts, stemming from both patient movement and physiological processes, represent a prevalent source of image degradation that can obscure subtle pathological changes and lead to clinical misinterpretation [75]. Within this context, the selection of appropriate signal suppression strategies must balance effectiveness with inherent sequence robustness to motion. This guide provides an objective comparison of current signal suppression methodologies, with a specific focus on their performance characteristics, motion sensitivity, and implementation across various pulse sequences.
Technical Fundamentals of Signal Suppression
Fat Suppression Mechanisms
Fat suppression techniques can be broadly categorized based on their physical principles, each with distinct mechanisms and trade-offs between robustness and scan efficiency.
Spectral Fat Saturation employs frequency-selective radiofrequency (RF) pulses tuned to the resonance frequency of fat protons, followed by spoiler gradients to dephase their magnetization. While effective under ideal homogeneous magnetic field conditions, this technique is highly susceptible to B0 inhomogeneity, particularly near metal implants or air-tissue interfaces, where off-resonance effects can lead to incomplete fat suppression and significant artifacts [76] [77].
Water Excitation (WE) techniques, including binomial pulses like 1-1 BORR (Binomial Off-resonant Rectangular), LIBRE (Lipid Insensitive Binomial Off-resonant RF Excitation), and LIBOR (Lipid Insensitive Binomial Off-resonant), achieve fat suppression by selectively exciting water protons while leaving fat magnetization largely undisturbed. These methods are generally more robust to B0 and B1 inhomogeneity compared to spectral saturation [78]. A recent technological advancement, Diffusion-Presaturated STIR, combines diffusion preparation with short tau inversion recovery to enable robust fat suppression in the presence of metal implants, where traditional frequency-based methods fail [76].
Inversion Recovery-based Methods such as STIR (Short Tau Inversion Recovery) utilize an inversion pulse followed by a specific inversion time to null the fat signal based on its T1 relaxation properties. This technique provides excellent B0 inhomogeneity tolerance but sacrifices scan efficiency and reduces available signal-to-noise ratio (SNR) due to T1-dependent nulling.
Spatial Saturation Principles
Spatial saturation, also known as regional saturation, employs frequency-selective saturation pulses to suppress signals from specific anatomical regions, typically to eliminate unwanted flow artifacts or signal from tissues adjacent to the region of interest. These spatially tailored RF pulses, often applied as pre-saturation bands, excite and subsequently dephase magnetization within a defined volume. Common applications include suppressing vascular flow artifacts, respiratory motion artifacts, and signals from subcutaneous fat. While highly effective for artifact reduction, spatial saturation pulses disrupt the steady-state equilibrium in quantitative sequences like variable flip angle T1-mapping and dynamic contrast-enhanced MRI, potentially introducing systematic bias in parameter estimates if not properly accounted for in signal modeling [79].
Table 1: Core Technical Characteristics of Signal Suppression Methods
| Suppression Technique | Physical Basis | Primary Applications | Key Limitations |
|---|---|---|---|
| Spectral Fat Saturation | Chemical shift difference | Musculoskeletal, abdominal imaging | Sensitive to B0 inhomogeneity |
| Water Excitation (WE) | Spectral-spatial excitation | Cardiac, breast imaging | Increased SAR, complex implementation |
| STIR | T1 relaxation differences | Field inhomogeneity regions | Reduced SNR, long scan times |
| Diffusion-Presaturated STIR | Combined diffusion and T1 nulling | Imaging near metal implants | Emerging technique, limited validation |
| Spatial Saturation Bands | Regional RF saturation | Vascular artifact suppression | Disrupts steady-state for quantification |
Comparative Performance in Motion-Prone Environments
Motion sensitivity represents a critical performance metric for signal suppression techniques, particularly in free-running acquisitions and examinations of uncooperative patients. Different suppression methods demonstrate varying degrees of robustness to motion, with significant implications for image quality and quantitative accuracy.
Motion-Robust Fat Suppression in Radial MRI
Non-Cartesian k-space trajectories, particularly radial acquisitions, present unique challenges for fat suppression due to their inherent motion resistance and continuous central k-space sampling. In free-running whole-heart MRI using 3D radial balanced steady-state free precession (bSSFP), inadequate fat suppression introduces significant artifacts that can obscure critical anatomical structures [78]. A comprehensive comparison of fat suppression methods in this motion-prone environment revealed that specialized water excitation pulses—LIBOR, LIBRE, and BORR—achieved excellent fat suppression with minimal streaking artifacts, even without motion correction [78]. The LIBOR technique demonstrated a particularly favorable profile, providing robust fat suppression while reducing specific absorption rate (SAR) by up to sixfold compared to Fast Interrupted Steady-State (FISS) sequences, making it ideal for SAR-intensive applications [80] [78].
Motion Compensation Through Sequence Design
Radial sampling techniques inherently compensate for motion through repeated central k-space sampling, maintaining image quality even when traditional fat suppression methods might fail. In prostate MRI simulation, a radial T2-weighted MultiVane XD sequence significantly outperformed Cartesian single-shot fast-spin-echo (SSFSE) for prostatic urethra visualization, with superior scores in 18 of 22 cases for Reader 1 and 17 of 22 cases for Reader 2 (p < 0.0001) [31]. This demonstrates how sequence architecture can complement suppression techniques in motion-prone anatomical regions.
Quantitative Performance Under Motion
The effectiveness of fat suppression techniques directly influences the accuracy of quantitative MRI methods under motion conditions. For proton-resonance frequency shift (PRFS) MR thermometry, the residual fat signal after imperfect suppression leads to temperature errors that oscillate with echo time and increase with fat content [77]. Experimental measurements in tissue-mimicking phantoms revealed that water excitation more effectively attenuates the main methylene fat peak (2% residual amplitude) compared to spectral fat saturation (22% residual) [77]. Despite this improvement, both techniques demonstrate residual signals from olefinic and glycerol fat peaks that introduce temperature miscalculations, highlighting the complex interaction between suppression efficacy and quantitative accuracy in motion-affected acquisitions.
Table 2: Quantitative Performance of Fat Suppression Techniques
| Technique | CNRWater-Fat (Phantom) | SAR Profile | Residual Fat Signal | Motion Robustness |
|---|---|---|---|---|
| LIBOR | 276.8 ± 2.5 [78] | Lowest (up to 6× reduction vs FISS) [78] | Not reported | High in free-running cardiac MRI [78] |
| LIBRE | 268.1 ± 2.6 [78] | Moderate | Not reported | High in free-running cardiac MRI [78] |
| BORR | 249.9 ± 2.2 [78] | Moderate | Not reported | High in free-running cardiac MRI [78] |
| FISS | 212.7 ± 2.7 [78] | Highest | Not reported | High in free-running cardiac MRI [78] |
| Spectral Fat Sat | Not reported | Low | 22% (main methylene peak) [77] | Low (fails with B0 inhomogeneity) [76] |
| Water Excitation | Not reported | Moderate | 2% (main methylene peak) [77] | Moderate |
Experimental Protocols and Methodologies
Protocol for Evaluating Fat Suppression Efficacy
The quantitative assessment of fat suppression techniques requires a standardized experimental approach to enable valid comparisons across different platforms and applications.
Phantom Preparation: Utilize standardized fat-water phantoms with known volumetric compositions, including 10% and 30% fat fractions to simulate physiological conditions [77]. The Gold Standard T1 phantom provides reference values for validating quantitative sequences [79].
Pulse Sequence Parameters: For free-running whole-heart MRI at 1.5T, implement a 3D radial bSSFP sequence with the following typical parameters: TR 3.2-3.5 ms, flip angle 40-60°, isotropic resolution 1.3-1.5 mm³, 512 radial views, and scan time 8-14 minutes [78]. Incorporate LIBOR, LIBRE, BORR, and FISS fat suppression modules for direct comparison.
Quantitative Metrics: Measure signal-to-noise ratio (SNR) in the ventricular blood pool and contrast-to-noise ratios between water-fat (phantom) and blood-myocardium (in vivo) [78]. Calculate residual fat signal fractions for each major spectral peak using water-fat decomposition algorithms [77].
Protocol for Spatial Saturation Impact Assessment
Evaluating the effect of spatial saturation pulses on quantitative accuracy requires careful control of sequence timing and magnetization state.
Sequence Configuration: Implement an interrupted spoiled gradient-echo (I-SPGR) sequence with variable flip angles (VFA) for T1-mapping. Incorporate spatial saturation pulses with typical duration of 10-20 ms during the steady-state interruption gap [79].
Data Acquisition: Acquire images at multiple flip angles (e.g., 2°, 5°, 10°, 15°) with constant TR. Maintain identical positioning between sequences with and without saturation pulses to enable paired comparisons.
Model Validation: Compare T1 values obtained with conventional steady-state model and the proposed interrupted steady-state model against reference values from inversion-recovery sequences in phantom experiments [79]. Perform Bland-Altman analysis to quantify bias and limits of agreement.
Advanced Integrated Techniques
Motion-Insistent Acquisition with Integrated Suppression
Emerging MRI sequences combine inherent motion robustness with integrated signal suppression strategies, offering comprehensive solutions for challenging imaging scenarios. The stack-of-stars echo-unbalanced T1 relaxation-enhanced steady-state (SOS echo-uT1RESS) sequence implements a radial "stack-of-stars" k-space trajectory to provide inherent motion resistance while simultaneously delivering robust background tissue suppression and pronounced dark-blood effects [4]. In brain tumor imaging, this sequence demonstrated a 1.8-fold improvement in tumor-to-brain contrast compared to standard MPRAGE (0.7 ± 0.4 vs. 0.4 ± 0.3, p < 0.001) while maintaining comparable overall image quality [4]. The radial sampling scheme effectively compensates for the sequence's inherent sensitivity to head motion, particularly beneficial for pediatric, elderly, or neurologically impaired patients [4].
Navigator-Based Motion Tracking with Fat Suppression
Fat-navigators (FatNavs) represent an innovative approach that leverages fat signal itself for motion tracking and correction. These techniques employ spectrally selective RF excitation to acquire subcutaneous fat images, which serve as high-resolution head-motion navigators [75]. In comparative studies, markerless optical systems (MOS) generally outperform FatNavs for tracking primary head rotations and unintentional translations, with FatNavs showing marginally better accuracy for subtle secondary rotations [75]. Neck-masking of fat-navigators further improves pitch rotation estimates, demonstrating how targeted signal suppression and utilization can synergistically enhance motion correction [75].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Materials for Signal Suppression Studies
| Reagent/Resource | Function/Application | Specification Notes |
|---|---|---|
| Fat-Water Phantoms | Validation of suppression efficacy | 10%/30% fat fractions; multiple spectral peaks [77] |
| Gold Standard T1 Phantom | Quantitative sequence validation | Reference T1 values across physiological range [79] |
| 3D Radial bSSFP Sequence | Free-running motion-robust acquisition | Non-Cartesian sampling; motion-resolved reconstruction [78] |
| Water Excitation Pulses (LIBOR/LIBRE/BORR) | Robust fat suppression | Binomial 1-1 pattern; flexible duration [78] |
| RetroMocoBox Toolbox | Motion correction implementation | Navigator processing; Fourier-space correction [75] |
| Numerical Bloch Simulation | Signal behavior prediction | Models magnetization evolution with preparation pulses [79] |
Signal suppression strategies represent a critical frontier in the ongoing effort to mitigate motion artifacts in MRI while maintaining diagnostic quality and quantitative accuracy. The comparative data presented in this guide demonstrates that no single technique universally outperforms others across all motion scenarios and anatomical regions. Instead, the optimal approach depends on a careful balance of technical constraints, including magnetic field homogeneity, specific absorption rate limitations, and the specific motion challenges inherent to each clinical or research application. Advanced integrated techniques that combine motion-resistant acquisitions with robust suppression methods show particular promise for challenging imaging scenarios, offering a path toward more reliable quantitative measurements and improved diagnostic confidence in the presence of patient movement. As motion compensation continues to evolve as a central theme in MRI research, signal suppression strategies will undoubtedly remain essential components of the comprehensive motion management toolkit.
Workflow for Motion-Robust Signal Suppression Strategy
Fat Suppression Technical Decision Pathway
Magnetic resonance imaging (MRI) is profoundly sensitive to subject motion, which can introduce artifacts that degrade image quality and compromise diagnostic and research data. Physiological synchronization techniques, namely gating and triggering, are essential for managing periodic motion originating from the cardiac and respiratory cycles. These methods synchronize data acquisition with specific phases of physiological activity, thereby minimizing motion artifacts and improving the accuracy of quantitative imaging. In the broader context of motion sensitivity comparison across MRI pulse sequences research, understanding and implementing robust synchronization strategies is fundamental for achieving reproducible results, particularly in cardiac, vascular, and functional neuroimaging.
The core principle is to use physiological signals—typically from an electrocardiogram (ECG) or a peripheral pulse sensor—to control the timing of the MRI sequence. This control can be executed prospectively (triggering) or retrospectively (gating), with the choice of method impacting the type of motion correction, the scan efficiency, and the specific clinical or research applications that are feasible [81].
Fundamental Concepts: Gating vs. Triggering
Although the terms are often used interchangeably, a subtle but important technical distinction exists between cardiac gating and cardiac triggering.
Triggering (Prospective Gating): In this approach, the detection of a specific physiological event, such as the R-wave of an ECG or the systolic upslope of a peripheral pulse, initiates a predefined data acquisition window. The scanner waits for this "trigger" before collecting data, typically during a quiescent period of the cardiac cycle. This method is ideally suited for acquiring static images at a specific, consistent physiological phase [81].
Gating (Retrospective): This is a broader term. In retrospective gating, MRI data are acquired continuously throughout the physiological cycle, independent of the timing of specific events. The physiological signal (ECG or pulse) is recorded simultaneously. During post-processing, the acquired data are sorted and grouped based on the recorded phase of the cardiac cycle. This approach is the standard method for creating cine-loop images that depict motion, such as cardiac wall motion or valve function [81].
The following diagram illustrates the logical workflow and fundamental difference between these two core synchronization strategies.
Experimental Comparisons and Performance Data
Selecting an appropriate synchronization technique is critical, as the choice directly influences image quality and quantitative accuracy. The following table summarizes key findings from recent experimental comparisons between different triggering methods.
Table 1: Quantitative Comparison of ECG and Finger-Pulse Triggering for Cardiac T1 Mapping
| Performance Metric | ECG Triggering | Finger-Pulse Triggering | Statistical Significance (P-value) |
|---|---|---|---|
| Diagnostic Image Quality (Median Likert Score) | 4.0 | 4.0 | P = 0.655 [82] |
| Interobserver Agreement (Kendall's W) | 0.861 | 0.838 | P < 0.001 for both [82] |
| Native T1 Values | No significant difference | No significant difference | All P > 0.05 [82] |
| Key Advantage | Direct measurement of cardiac electrical activity | Immunity to magnetohydrodynamic (MHD) effect [82] | |
| Key Limitation | Susceptible to MHD artifacts at high fields (≥3.0T) [82] | Requires compensation for pulse transit time delay (~200-250 ms) [82] |
Beyond the Heart: Synchronization in Neuroimaging
While vital for cardiac imaging, the principles of motion management are equally critical in other domains, such as functional MRI (fMRI). Here, head motion is a major confound, and "gating" in this context often refers to advanced post-processing techniques like "JumpCor," which identifies and corrects for large, infrequent head movements in populations like sleeping infants [83]. Furthermore, physiological noise from cardiac pulsatility and respiration can induce structured artifacts in resting-state networks, necessitating data-driven cleaning methods to disentangle neural signals from physiological noise [84].
Detailed Experimental Protocols
To ensure reproducibility, below are detailed methodologies for key experiments cited in this guide.
Protocol: Comparison of ECG vs. Finger-Pulse Triggering for T1 Mapping
This protocol is adapted from a 2025 study evaluating finger-pulse triggering as a substitute for ECG in cardiac MR T1 mapping [82].
- Patient Population: Patients with a clinical indication for cardiac MR; exclusion criteria include arrhythmia (e.g., atrial fibrillation), rapid heart rate (>100 bpm), or peripheral circulation disorders.
- Hardware: 3.0T MRI scanner (e.g., MAGNETOM Skyra); 18-channel body coil and 32-channel spine-array coil; standard ECG setup and MRI-compatible finger-pulse clip.
- Triggering Setup:
- ECG: Place electrodes per manufacturer guidelines; select the lead with the highest R-wave and lowest T-wave amplitude.
- Pulse: Place clip on the index finger; trigger on the highest pulse wave. Apply a temporal offset of 200–250 ms to compensate for pulse transit time.
- Sequence: Modified Look-Locker Inversion Recovery (MOLLI) 5(3)3 sequence for pre-contrast T1 mapping.
- Acquisition Parameters: Acquire identical T1 maps in short-axis views (basal, mid, apical) using both triggering methods. Typical parameters: TR = 3.2 ms, TE = 1.2 ms, flip angle = 35°, slice thickness = 5 mm, matrix size = 256 × 192.
- Image Analysis:
- Qualitative: Three independent, blinded radiologists score general image quality on a 5-point Likert scale.
- Quantitative: Two radiologists manually delineate myocardial regions of interest (ROIs) on native T1 maps to quantify segmental T1 values.
- Statistical Analysis: Use paired t-tests or Wilcoxon signed-rank tests for comparisons. Assess agreement with Bland-Altman plots and intraclass correlation coefficients (ICCs).
Protocol: Motion-Robust Brain Tumor Imaging with Radial Acquisition
This protocol highlights an alternative approach to motion management through sequence design, using a motion-resistant radial "stack-of-stars" k-space trajectory [4].
- Patient Population: Adult patients with known enhancing brain tumors (e.g., primary, metastases).
- Sequence Comparison:
- Standard: Magnetization-prepared rapid gradient-echo (MPRAGE).
- Experimental: Prototype stack-of-stars echo-unbalanced T1 relaxation-enhanced steady-state (SOS echo-uT1RESS).
- SOS echo-uT1RESS Parameters: Axial 3D acquisition; TR = 6.9 ms, TE = 4.16 ms, 1.0 mm isotropic resolution, 512 radial views, bandwidth = 690 Hz/pixel.
- Post-Processing: Employ multiplanar reconstruction to generate sagittal and coronal views from the original axial images for both quantitative and qualitative analysis.
- Quantitative Analysis:
- Measure signal intensity in enhancing lesion, normal white matter, and air.
- Calculate Weber contrast (Tumor-to-Brain Contrast) as (SIlesion - SIWM) / SIWM.
- Calculate Contrast-to-Noise Ratio (CNR) as (SIlesion - SIWM) / SDair.
- Qualitative Analysis: Three blinded neuroradiologists score overall image quality, lesion conspicuity, and artifacts on a 4-point Likert scale in randomized image sets.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of gating and triggering requires specific hardware and software components. The following table details key solutions for researchers.
Table 2: Essential Materials for Physiological Synchronization Experiments in MRI
| Item Name | Function/Description | Example Application/Note |
|---|---|---|
| ECG Triggering System | Non-magnetic amplifier and electrodes for detecting the heart's electrical activity. | Susceptible to magnetohydrodynamic (MHD) effect at 3T and above, which can distort the T-wave [82]. |
| Pulse Oximeter (Finger Clip) | Photoplethysmography-based system detecting blood volume changes for peripheral pulse triggering. | Immune to MHD effect; wave peak is broad and stable in magnetic fields [82]. |
| 32-Channel Receive-Only RF Head Coil | Multi-channel array coil for high signal-to-noise ratio (SNR) and accelerated acquisition. | Spatially non-uniform sensitivity can make fMRI signals sensitive to head motion within the coil [83]. |
| Motion Correction Software (e.g., AFNI, FSL) | Software packages implementing algorithms for rigid-body realignment and advanced correction (e.g., "JumpCor"). | "JumpCor" treats large, infrequent head motions as separate imaging runs, adding nuisance regressors for each stable segment [83]. |
| B0 Field Map Correction (e.g., FSL "topup") | Algorithm to correct for EPI geometric distortions using images acquired with reversed phase-encoding directions. | Critical for correcting distortion artifacts in EPI-based sequences like fMRI and DSC perfusion [85]. |
| Radial k-Space Sequence (e.g., SOS, PROPELLER) | Pulse sequences using radial (non-Cartesian) k-space sampling to oversample the center of k-space. | Inherently more resistant to motion artifacts. SOS is used in neuroimaging [4]; PROPELLER/BLADE is available on GE/Siemens systems [65]. |
Gating and triggering are indispensable tools for synchronizing MRI acquisition with physiological motion. The experimental data demonstrate that finger-pulse triggering is a clinically viable alternative to ECG for cardiac T1 mapping, offering equivalent image quality and T1 quantification while overcoming the MHD artifact limitation at high fields [82]. Furthermore, motion mitigation extends beyond cardiac synchronization to include advanced sequence design (e.g., radial SOS) [4] and sophisticated post-processing techniques for managing both head motion and physiological noise in fMRI [83] [84]. The choice of strategy must be guided by the specific physiological motion targeted, the pulse sequence employed, and the intended clinical or research output. Integrating robust synchronization methods is a critical step in minimizing motion-related artifacts and enhancing the validity of quantitative imaging biomarkers across diverse MRI applications.
This guide provides an objective comparison of magnetic resonance imaging (MRI) pulse sequences, focusing on their performance in motion-prone scenarios. For researchers in drug development and biomedical science, selecting the appropriate sequence is critical for generating reliable, high-quality data in studies involving physiological motion (e.g., respiration, cardiac pulsation) or patient movement.
Motion has long been a fundamental challenge in MRI, causing artifacts that degrade image quality and compromise diagnostic and research data. Traditional Cartesian sampling sequences, which fill k-space line by line, are particularly vulnerable to motion, which disrupts the precise phase encoding required for accurate image reconstruction. Even minor movements can result in blurring, ghosting, or other artifacts that obscure critical anatomical details. This guide synthesizes recent evidence to compare motion-robust sequences, providing a framework for selecting the optimal protocol based on specific experimental needs and motion challenges.
Comparative Performance of Motion-Robust Sequences
The following table summarizes key performance metrics for several advanced MRI sequences as reported in recent experimental studies.
Table 1: Quantitative Performance Comparison of Motion-Robust MRI Sequences
| Anatomical Region | Sequence(s) Evaluated | Comparison Sequence(s) | Key Performance Metrics | Experimental Findings | Reference |
|---|---|---|---|---|---|
| Knee Joint | Zero Echo Time (ZTE) | Proton Density with Fat Suppression (PD-FS) | Sensitivity: 91.5-92.3%Specificity: 89.4-90.7%Accuracy: 92.2-93.8% | ZTE demonstrated superior performance for depicting osseous abnormalities (e.g., erosions, osteophytes) compared to PD-FS. | [5] |
| Prostate Urethra | MultiVane XD (MVXD) | Single-Shot Fast-Spin-Echo (SSFSE) | Urethral Visibility Score (1-5 scale): Significantly higher (P<0.0001)Reader Preference: 18/22 and 17/22 cases | The radial MVXD sequence provided superior visualization of the prostatic urethra without Foley catheter, despite more peripheral artifacts. | [31] |
| Brain Tumors | Stack-of-Stars echo-uT1RESS (SOS echo-uT1RESS) | Magnetization-Prepared Rapid Gradient-Echo (MPRAGE) | Tumor-to-Brain Contrast: 1.8-fold improvement (0.7 vs. 0.4, p<0.001)Lesion Conspicuity: Improved (p<0.001) | SOS echo-uT1RESS significantly enhanced lesion visibility, particularly for small metastases, while maintaining comparable overall image quality. | [4] |
Detailed Experimental Protocols and Methodologies
Understanding the experimental design behind the data is crucial for its application. Below are the methodologies from the key studies cited.
Protocol: Evaluating ZTE for Osseous Abnormalities in Knee OA
This 2025 prospective study aimed to validate the Zero Echo Time (ZTE) sequence against the standard PD-FS sequence for assessing knee osteoarthritis, using arthroscopy as the reference standard [5].
- Patients: 55 adult patients with chronic knee pain were enrolled. MRI was performed 3-7 days prior to arthroscopy.
- MRI Acquisition: Scans were conducted on a 1.5T Philips Ingenia scanner using a 16-channel knee coil. Both ZTE and PD-FS sequences were acquired in sagittal, axial, and coronal planes.
- Image Assessment: Two musculoskeletal radiologists independently evaluated the images. They assessed cartilage changes in 14 articular subregions using a 0-4 grading scale and evaluated osseous abnormalities (osteophytes, erosions, sclerosis).
- Statistical Analysis: Sensitivity, specificity, and accuracy for both sequences were calculated using arthroscopic findings as the ground truth. Inter-reader reliability was assessed using Cohen's kappa.
Protocol: Comparing Radial vs. Cartesian Sequences for Prostate Urethra Visualization
This 2019 clinical investigation compared two motion-insensitive T2-weighted sequences for visualizing the prostatic urethra during MR simulation for radiation therapy, a common challenge due to respiratory motion and benign prostatic hyperplasia [31].
- Patients: 22 patients undergoing MRI simulation for prostate cancer without Foley catheters.
- MRI Acquisition: Imaging was performed on a 3T Philips Ingenia scanner. Sagittal multislice data were acquired using both the radial MVXD sequence and a Cartesian SSFSE sequence, each with an acquisition time of 2-3 minutes.
- Image Assessment: Two genitourinary radiologists, blinded to the sequence used, scored the datasets. They rated urethral visibility on a 5-point scale, as well as signal-to-noise ratio and the presence of artifacts.
- Statistical Analysis: A paired Student's t-test was used to compare the visibility scores between sequences. Interobserver agreement was calculated with Cohen's kappa.
Protocol: Assessing SOS echo-uT1RESS for Brain Tumor Conspicuity
This 2025 prospective, two-center study aimed to compare a novel motion-robust sequence against the established standard for brain tumor imaging [4].
- Patients: 34 adult patients with known primary brain tumors or metastases.
- MRI Acquisition: A 3T Siemens Skyra scanner was used. The protocol included standard post-contrast MPRAGE and the prototype SOS echo-uT1RESS sequence.
- Image Analysis:
- Quantitative: A radiology trainee measured signal intensity in enhancing lesions, normal white matter, and air to calculate contrast-to-noise ratio (CNR) and tumor-to-brain contrast (Weber contrast).
- Qualitative: Three fellowship-trained neuroradiologists independently evaluated overall image quality, lesion conspicuity, and image artifacts on a 4-point Likert scale.
- Statistical Analysis: Quantitative metrics were compared using statistical tests, and qualitative scores were analyzed for significant differences.
Decision Workflow and Technical Integration
The following diagram illustrates a strategic approach to selecting and integrating motion-robust sequences based on the primary source of motion and the anatomical target.
MRI Motion Compensation Strategy
Advanced Motion Compensation Techniques
Beyond pulse sequence selection, integrated hardware and software solutions are critical for managing motion. Recent research highlights several effective strategies:
- Prospective Motion Correction with Navigators: This technique actively adjusts the MRI field of view during acquisition to track and compensate for motion. Volumetric navigators are used for head motion correction, enabling ultra-high-resolution imaging (e.g., 0.16 mm isotropic angiography) [86]. For respiratory motion, methods like the ACROBATIC framework correct for both breathing and bulk patient motion in free-running 5D whole-heart MRI [86].
- External Optical Tracking and Gating: Optical systems provide an MRI-sequence-agnostic method for motion detection. One study used an MR-compatible camera and a computer vision algorithm to track the movement of a live insect on a treadmill. This real-time motion data was then used for prospective gating, acquiring k-space lines only during periods of minimal motion to drastically reduce artifacts [87].
- Advanced Model-Based Reconstruction: Instead of preventing motion during acquisition, these techniques correct for it during image reconstruction. For example, k-space-based motion correction (K-CC-MoCo) can correct respiratory motion directly in k-space for highly accelerated (up to 50x) cardiac perfusion scans, outperforming image-based methods [86]. Similarly, unsupervised reconstruction methods using implicit neural representations (INR) can jointly estimate time-varying coil sensitivities and image content, enabling high-quality reconstruction from free-breathing abdominal and cardiac data without the need for pre-trained models [88].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials and Technologies for Motion-Robust MRI Experiments
| Item / Technology | Function / Application in Motion-Prone MRI | Representative Examples / Notes |
|---|---|---|
| Radial K-Space Trajectory | Acquires data along rotating spokes, dispersing motion artifacts and making sequences inherently more motion-robust. | Core principle behind MVXD (PROPELLER) [31] and Stack-of-Stars [4]. |
| Zero Echo Time (ZTE) | Uses nearly instantaneous signal acquisition to capture signals from tissues with very short T2 times (like bone), creating CT-like images without radiation. | Superior for osseous detail in knee [5] and skull [89]. |
| MR-Compatible Optical Camera | Provides external, real-time motion tracking for prospective gating or correction without interfering with the magnetic field. | Used for tracking insect motion on a treadmill inside the magnet [87]. |
| Prospective Navigators | Small, repeated MRI acquisitions that measure and correct for motion (e.g., head position, diaphragm position) in real-time before it corrupts the main image data. | Enables high-resolution TOF-MRA and free-running whole-heart imaging [86]. |
| Implicit Neural Representation (INR) | An unsupervised deep learning technique that represents an image as a continuous function, improving reconstruction from undersampled, motion-corrupted k-space data. | Used in IMJ-PLUS method for free-breathing dynamic MRI [88]. |
Validation Frameworks and Comparative Analysis of Sequence Performance
In the field of motion-sensitive magnetic resonance imaging (MRI), the validation of novel imaging sequences and biomechanical models is a critical step before their translation to clinical practice. Brain-mimicking phantoms serve as indispensable tools in this process, providing a controlled, reproducible, and ethically uncomplicated means of establishing ground truth for validating technologies like amplified MRI (aMRI) and Magnetic Resonance Elastography (MRE) [90]. These phantoms address a fundamental challenge in brain biomechanics: the brain's frequency-dependent mechanical behavior. Without phantoms that accurately mimic the broadband mechanical response of real brain tissue, it is impossible to rigorously validate the mechanical biomarkers that have demonstrated diagnostic value for conditions such as brain tumors, Alzheimer's disease, and Chiari Malformation [91] [90]. This review provides a comparative analysis of state-of-the-art brain-mimicking phantoms, detailing their composition, experimental protocols, and performance in validating motion-sensitive MRI techniques.
Comparative Analysis of Brain-Mimicking Phantom Technologies
Key Phantom Classifications and Their Applications
Phantoms can be broadly classified into physical (hardware) and numerical (software) types, each with distinct advantages. Physical phantoms are tangible objects designed to mimic the physical properties of human tissues, while numerical phantoms offer fully controlled microgeometries and contrast mechanisms for in-silico testing [92] [93]. The recent emergence of "super phantoms" represents a significant advancement, bridging the gap between simple phantoms and highly complex human tissues by replicating both anatomic and functional imaging biomarkers [94].
Table 1: Classification of Phantoms for Brain Microstructural MRI Validation
| Phantom Type | Key Characteristics | Primary Applications | Notable Advantages | Inherent Limitations |
|---|---|---|---|---|
| Standard Synthetic [95] | Simple, well-characterized materials (e.g., polymers, gels) | Quality control, basic system parameter evaluation (resolution, contrast) | High reproducibility, stability, ease of manufacture | Lacks anatomical and microstructural complexity |
| Anthropomorphic [95] | Replicates human anatomy and tissue heterogeneity using tissue-equivalent materials | Protocol optimization, evaluation of image reconstruction techniques | Closer approximation to clinical conditions | Complex to manufacture; may not fully capture functional properties |
| Biomimetic Microstructural [92] [93] | Incorporates microstructural features (e.g., hollow fibers, capillaries) to mimic cellular environments | Validation of biophysical models for dMRI, NODDI, DKI | Provides microstructural "ground truth" for advanced models | Challenging to manufacture reproducibly at micrometer scales |
| Numerical (Software) [92] [93] | Computer-simulated environments and microgeometries (e.g., Monte Carlo simulations) | Biophysical model validation, fiber tracking algorithms, sequence optimization | Total control over properties and microenvironments | May overlook complex physical interactions present in real systems |
| Super Phantoms [94] | Replicates both anatomic and functional imaging biomarkers (e.g., flow, perfusion) | Early evaluation of disruptive imaging technologies, AI training | Bridges the gap between simple phantoms and in-vivo testing | Technologically complex and resource-intensive to develop |
Advanced Frequencies and Material Properties
A pivotal innovation in the field is the development of a novel phantom test setup that enables both low and high-frequency mechanical responses to be captured on the same model [91] [90]. This system uniquely combines two vibration sources: a pneumatic actuator for low-frequency/intrinsic motion (∼1 Hz) to simulate cardiac-induced pulsatility for aMRI, and a piezoelectric actuator for high-frequency actuation (30–60 Hz) required for MRE [90]. This design acknowledges that soft tissues are viscoelastic and exhibit different mechanical behaviors under varying loading frequencies.
The phantom material itself is a critical component. For biomechanical validation, the phantom must have viscoelastic properties comparable to real brain tissue. Furthermore, for diffusion MRI validation, phantoms often use polymer polyvinylpyrrolidone (PVP) in aqueous solution, where increasing polymer concentrations yield decreasing apparent diffusion coefficient (ADC) values, creating a quantifiable reference for validating diffusion measurements [96].
Table 2: Quantitative Performance of Phantom Configurations in Motion-Sensitive MRI
| Phantom & Actuation Configuration | Key Performance Metrics | Quantitative Results | Implication for Validation |
|---|---|---|---|
| Homogeneous Brain-Mimicking Phantom with Pneumatic Actuation (for aMRI) [90] | Linearity of motion amplification | aMRI linearly amplified motion up to an amplification factor of at least 9 | Validates aMRI's capability to detect both visible and sub-voxel motion |
| Homogeneous Brain-Mimicking Phantom with Piezoelectric Actuation (for MRE) [91] [90] | Shear wave attenuation vs. frequency | Propagating shear waves attenuated faster at higher driving frequencies (30-60 Hz) | Consistent with known literature on brain tissue's frequency-dependent behavior |
| MRE with Different Actuator Coupling [90] | Effect of coupling on wave amplitude | Weaker coupling caused lower amplitude wave field images | Highlights critical importance of actuator-phantom interface for reproducible results |
| NIST/QIBA Diffusion Phantom (Multi-Scanner Study) [96] | Coefficient of Variation (CoV) for ADC measurements | CoV consistently < 5%, except at lowest ADC values; Sagittal orientation showed highest CoV | Establishes phantom as a highly reproducible reference for multi-site studies |
| Fiber-Ring Diffusion Phantom (DTI/DKI/NODDI) [97] | Coefficient of Variation (CoV) for DTI metrics | CoV for FA = 1.03%; CoV for MD = 2.34% across multiple days | Demonstrates high longitudinal reproducibility for complex diffusion models |
Experimental Protocols for Phantom Validation
Protocol for Biomechanical Property Validation
The validation of motion-sensitive techniques like aMRI and MRE requires a structured approach. The following protocol, adapted from Ozkaya et al., details the steps for a combined aMRI/MRE validation study [90]:
- Phantom Preparation and Setup: A brain-mimicking material with viscoelastic properties matching the human brain is cast into a phantom holder designed to fit a standard MR head coil. The setup includes integrated ports for actuator attachment.
- Actuator Configuration:
- For low-frequency aMRI validation, a flexible membrane is incorporated and connected to a pneumatic pump system outside the scanner room. The pump is programmed to generate cyclic inflation/deflation at ~1 Hz, simulating cardiac pulsation.
- For high-frequency MRE validation, a piezoelectric actuator is coupled to the phantom. Coupling can be configured as mid-surface shear, top-surface shear, or compression loading to study wave propagation from different sources.
- Image Acquisition:
- aMRI: A cardiac-gated cine MRI sequence is used. The pneumatic actuation power is varied (e.g., 40%–80%) while acquiring images to test the linearity of motion amplification.
- MRE: Motion-encoding gradients are synchronized with the piezoelectric actuator, driven at frequencies typically between 30-60 Hz. Wave images are captured at several phase offsets.
- Data Analysis:
- aMRI Data: The amplified motion waveforms are analyzed, and displacement amplitudes are quantified and compared against the known input actuation or external video analysis to validate amplification linearity.
- MRE Data: The acquired wave fields are processed using an inversion algorithm to generate elastograms (stiffness maps). Wave amplitude and attenuation are measured across different frequencies and loading configurations.
Protocol for Multi-Scanner Diffusion Phantom Validation
For validating quantitative diffusion MRI biomarkers across a fleet of scanners, a standardized protocol is essential [96]:
- Phantom Preparation: A NIST-traceable diffusion phantom (e.g., CaliberMRI) is filled with ice water and allowed to equilibrate to 0°C ± 0.2°C to eliminate temperature sensitivity of diffusion.
- Scanner Calibration: The phantom is imaged on multiple MRI scanners from different vendors and field strengths (1.5T and 3T) using a harmonized acquisition protocol.
- Image Acquisition: A single-shot echo-planar imaging (EPI) sequence with multiple b-values (e.g., 0, 500, 900, 2000 s/mm²) is used. The phantom is scanned in all three primary orientations (axial, coronal, sagittal) to probe for orientation-dependent eddy current effects.
- Data Analysis: User-directed regions of interest (ROIs) are placed on each vial within the phantom. The apparent diffusion coefficient (ADC) is calculated for each vial and compared against the NIST-provided reference values. The coefficient of variation (CoV) and Bland-Altman analysis are used to assess inter-scanner reproducibility and bias.
Figure 1: A generalized workflow for conducting phantom validation studies for motion-sensitive MRI techniques, covering the key phases from preparation to final analysis.
The Scientist's Toolkit: Essential Research Reagent Solutions
The development and implementation of advanced brain-mimicking phantoms require a suite of specialized materials and instruments.
Table 3: Essential Research Reagents for Brain-Mimicking Phantom Development
| Reagent / Instrument | Function in Phantom Development | Specific Application Examples |
|---|---|---|
| Polyvinylpyrrolidone (PVP) [96] | Aqueous polymer solution used to create a range of predictable apparent diffusion coefficient (ADC) values. | Core material in NIST-traceable diffusion phantoms for DWI/ADC validation across scanner fleets. |
| Agarose or Silicone-based Gels [92] [93] | Form the base of the tissue-mimicking material, providing tunable viscoelastic properties similar to brain tissue. | Creating the bulk matrix for biomechanical phantoms used in aMRI and MRE validation. |
| Hollow Microfibers / Capillaries [92] [93] | Mimic the restricted diffusion environment of axons, introducing microstructural complexity and anisotropy. | Fabricating biomimetic phantoms for validating advanced dMRI models (DTI, NODDI). |
| Pneumatic Actuation System [91] [90] | Generates low-frequency (∼1 Hz), large-displacement motion to simulate cardiac-induced pulsations. | Providing the "intrinsic" motion input for validating Amplified MRI (aMRI) techniques. |
| Piezoelectric Actuator [91] [90] | Generates high-frequency (30-60 Hz), small-amplitude vibrations for generating shear waves. | The external vibration source required for Magnetic Resonance Elastography (MRE) experiments. |
| NIST-Traceable Reference Phantom [96] | Provides a gold standard with known, stable diffusion properties for inter-scanner calibration. | Quality assurance and harmonization of quantitative diffusion MRI across multiple sites and vendors. |
The frontier of phantom technology is moving towards "super phantoms" that more fully capture the anatomic, functional, and pathophysiological complexity of human organs [94]. These advanced models, which can be digital, physical, or even ex vivo organs maintained under physiological conditions, will be crucial for validating the next generation of AI-driven imaging biomarkers and for conducting rigorous virtual imaging trials before human studies begin.
In conclusion, brain-mimicking phantoms are the cornerstone of rigorous validation for motion-sensitive MRI techniques. The development of phantoms capable of mimicking the brain's broadband mechanical response has been a significant breakthrough, enabling the direct comparison of aMRI and MRE on a single platform [90]. Furthermore, the standardization of diffusion phantoms is paving the way for reliable, multi-center quantitative imaging studies [96] [97]. As these technologies evolve, they will continue to bridge the critical gap between technical innovation and confident clinical application, ensuring that new biomechanical biomarkers are validated against a known ground truth before being used to diagnose and monitor neurological diseases.
Motion artifacts remain a significant challenge in magnetic resonance imaging (MRI), particularly in clinical and research populations prone to movement such as infants, elderly patients, and those with neurological conditions. These artifacts manifest primarily as image ghosting, reduced signal-to-noise ratio (SNR), and compromised anatomical fidelity, potentially confounding diagnostic interpretation and quantitative analysis. The pursuit of motion-robust MRI necessitates standardized metrics and rigorous comparison frameworks to evaluate pulse sequence performance under realistic movement conditions.
This guide provides a systematic comparison of contemporary MRI pulse sequences, focusing on quantitative metrics for ghosting, SNR, and anatomical fidelity. We present experimental data and methodologies essential for researchers and drug development professionals conducting motion sensitivity analyses, with particular emphasis on structural T1-weighted imaging applications where anatomical precision is paramount.
Quantitative Metrics for Motion Resilience
Core Image Quality Metrics
The assessment of motion resilience relies on quantifiable metrics that capture different aspects of image degradation. The most clinically relevant metrics include:
Signal-to-Noise Ratio (SNR) measures the strength of a desired signal relative to background noise. Motion often causes signal dropout and noise enhancement, leading to reduced SNR values. It is calculated as
SNR = SItissue / SDbackground, where SItissue is the mean signal intensity in a tissue region-of-interest (ROI) and SDbackground is the standard deviation of the signal in a background ROI [4] [30].Contrast-to-Noise Ratio (CNR) quantifies the ability to distinguish between different tissues. Motion-induced blurring reduces CNR. It is calculated as
CNR = |SItissue1 - SItissue2| / SDbackground[4].Entropy Focus Criterion (EFC) is a focus metric from information theory. It increases with image blurring, making it a sensitive indicator of motion artifacts [30].
Coefficient of Joint Variation (CJV) assesses intensity uniformity by measuring the dispersion of intensity distributions in two segmented tissue types (e.g., gray and white matter). Motion artifacts typically increase the CJV, indicating reduced image homogeneity [30].
Ghosting Artifacts result from inconsistencies in k-space data caused by motion. The mathematical description of ghosting involves analyzing amplitude and phase discontinuities in the phase-encoding direction, which create replicated "ghost" images of the moving structure [98] [1].
Experimental Protocols for Motion Assessment
Standardized experimental protocols are crucial for valid comparisons of motion resilience across different MRI sequences.
Controlled Motion Datasets: The Movement-Related ARTefacts (MR-ART) dataset provides a benchmark for evaluating motion correction algorithms and sequence robustness. It includes matched T1-weighted structural scans from the same participants acquired under three conditions: no motion (
STAND), low motion (HM1), and high motion (HM2). Motion was induced in a controlled manner using visual cues for head nodding, the most prominent type of head motion [30].Clinical Quality Scoring: Expert neuroradiologist assessment provides a clinically grounded quality score, typically on a 3-point scale: 1 (clinically good), 2 (medium quality), and 3 (bad/unusable quality). This subjective scoring is essential for correlating quantitative metrics with diagnostic utility [30].
Quantitative Analysis Workflow: A standard workflow involves acquiring images with different sequences in the same session or under identical motion conditions. Researchers then place ROIs in relevant anatomical structures and background air to calculate SNR, CNR, and Weber contrast (calculated as
(SItissue1 - SItissue2) / SItissue2). These are analyzed alongside automated IQMs from tools like MRIQC [4] [30].
Diagram 1: Experimental workflow for quantifying motion resilience in MRI sequences, integrating both quantitative metrics and qualitative clinical scoring.
Comparative Performance of MRI Pulse Sequences
Structural Neuroimaging Sequences
Table 1: Performance comparison of MPRAGE, SOS echo-uT1RESS, and ZTE sequences for structural imaging.
| Sequence | k-Space Trajectory | Key Strength | Motion Resilience | Tumor-to-Brain Contrast | Diagnostic Performance |
|---|---|---|---|---|---|
| MPRAGE [4] [30] | 3D Cartesian | Excellent gray-white matter contrast | Low | 0.4 ± 0.3 (Reference) | Baseline |
| SOS echo-uT1RESS [4] | 3D Radial Stack-of-Stars | High lesion conspicuity, dark-blood effect | High | 0.7 ± 0.4 (1.8x improvement) | Superior for small metastases |
| ZTE [5] | 3D Radial | Superior bone detail, CT-like contrast | High for osseous structures | Not Reported | Superior for osseous abnormalities |
The stack-of-stars (SOS) echo-unbalanced T1 relaxation-enhanced steady-state (echo-uT1RESS) sequence demonstrates a significant 1.8-fold improvement in tumor-to-brain contrast compared to standard MPRAGE (0.7 ± 0.4 vs. 0.4 ± 0.3, p < 0.001) while maintaining comparable CNR (28.2 ± 16.5 vs. 29.4 ± 21.4, p = 0.80) [4]. This sequence employs a radial k-space trajectory where each "star" is acquired as a single shot, conferring inherent motion robustness. While overall image quality and artifact scores were similar to MPRAGE, SOS echo-uT1RESS showed significantly improved lesion conspicuity (p < 0.001) and diagnostic performance (p < 0.001), particularly for small metastases [4].
The Zero Echo Time (ZTE) sequence also uses 3D radial acquisition but is particularly valuable for visualizing osseous and calcified tissues with ultrashort T2 times. In evaluating knee osteoarthritis, ZTE demonstrated superior diagnostic performance for bony abnormalities compared to conventional proton density with fat suppression (PD-FS) sequences, with sensitivity of 91.5-92.3% vs. 85.9-87.2% and accuracy of 92.2-93.8% vs. 86.1-88.6% [5].
Impact of Motion on Quantitative Metrics
Table 2: Effect of controlled head motion on image quality metrics in T1-weighted MPRAGE sequences. [30]
| Acquisition Condition | Total SNR | Entropy Focus Criterion (EFC) | Coefficient of Joint Variation (CJV) | Clinical Quality Score (1-3) |
|---|---|---|---|---|
| STAND (No Motion) | 100% (Reference) | 100% (Reference) | 100% (Reference) | 1 (Good) |
| HM1 (Low Motion) | -6.5% | +12.1% | +8.7% | 1-2 (Good-Medium) |
| HM2 (High Motion) | -15.2% | +25.8% | +18.3% | 2-3 (Medium-Bad) |
Controlled motion significantly degrades all image quality metrics. The MR-ART dataset shows that high head motion (HM2) reduces total SNR by over 15% while increasing EFC (blurring metric) by ~26% and CJV (intensity inhomogeneity) by ~18% compared to motion-free (STAND) acquisitions [30]. This degradation correlates with clinical quality ratings, where excessive motion often renders images diagnostically unusable (score of 3) [30].
Table 3: Key software tools and datasets for MRI motion resilience research.
| Tool Name | Type | Primary Function | Relevance to Motion Research |
|---|---|---|---|
| MR-ART Dataset [30] | Data | Matched motion-corrupted/clean T1w brain scans | Provides ground-truth data for validating motion correction algorithms and sequence performance. |
| MRIQC [30] | Software | Automated extraction of image quality metrics | Quantifies motion effects via SNR, EFC, CJV, and other metrics without a reference standard. |
| FIRMM [99] | Software | Real-time head motion monitoring | Enables proactive scan reacquisition by providing motion estimates during fMRI acquisition. |
| RIESLING [100] | Software | Reconstruction toolbox for 3D radial ZTE images | Enables fast, high-quality reconstruction of motion-robust radial data. |
| PyPulseq [100] | Software | Open-source, vendor-neutral pulse sequence design | Facilitates development and testing of custom motion-robust sequences. |
| Radial Stack-of-Stars [4] | Sequence | Motion-resistant k-space trajectory | Reduces motion artifacts through oversampling of k-space center and incoherent artifact patterns. |
Diagram 2: Relationship between k-space trajectory and motion artifact patterns, explaining the inherent robustness of radial methods.
The quantitative comparison presented herein demonstrates that pulse sequence selection significantly impacts motion resilience in MRI. Sequences employing radial k-space trajectories (SOS echo-uT1RESS, ZTE) consistently outperform conventional Cartesian sequences (MPRAGE) in the presence of motion, particularly for critical tasks like lesion detection and osseous assessment. The documented 1.8-fold improvement in tumor-to-brain contrast with SOS echo-uT1RESS, coupled with its inherent motion robustness, underscores its value in clinical and research imaging of motion-prone populations.
Standardized metrics—SNR, CNR, EFC, and CJV—provide an objective framework for evaluating motion resilience, while resources like the MR-ART dataset and MRIQC software enable reproducible benchmarking. For researchers and drug development professionals, adopting these motion-robust sequences and quantitative assessment methodologies can enhance data quality, improve measurement reliability, and ultimately strengthen conclusions drawn from longitudinal and clinical trial imaging studies.
Magnetic resonance imaging (MRI) pulse sequence selection represents a critical decision point in experimental design and clinical protocol development, with motion tolerance serving as a paramount consideration. Subject motion during MRI examinations has been problematic since its introduction as a clinical imaging modality, affecting a majority of clinical applications as one of the most frequent sources of artefacts [1]. Compared to other imaging modalities, MRI is particularly sensitive to subject motion primarily due to the prolonged time required for most sequences to collect sufficient data to form an image—far longer than the timescale of most types of physiological motion [1]. This comprehensive analysis objectively compares the motion sensitivity and performance characteristics of four fundamental sequence families: T2-Weighted Gradient Echo (T2-GRE), Diffusion Echo Planar Imaging (Diffusion EPI), Steady-State Free Precession (SSFP), and advanced Rapid Imaging Sequences. By examining their fundamental physics, quantitative performance metrics, and motion robustness within the context of contemporary research applications, this guide provides a framework for optimal sequence selection in demanding imaging scenarios where motion presents a significant constraint.
Physical Principles and Motion Sensitivity Mechanisms
Fundamental Sequence Physics and Motion Interrogation
Each MRI pulse sequence family possesses distinct signal generation mechanisms that dictate its inherent sensitivity to motion, which manifests primarily through two physical pathways: spin history effects (uncontrolled evolution of magnetization between excitations) and phase errors (velocity-induced phase shifts during gradient applications) [1].
T2-GRE: This sequence employs a gradient recalled echo without a 180° refocusing pulse, making it exquisitely sensitive to magnetic field inhomogeneities. T2 relaxation reflects the decay of the transverse magnetization vector caused by the combination of tissue itself and inhomogeneity of the main magnetic field [101]. This sensitivity extends to microscopic magnetic field perturbations caused by deoxygenated blood, iron deposits, or calcifications, but also makes the sequence vulnerable to motion-induced field distortions [101] [102].
Diffusion EPI: This technique utilizes a spin-echo preparation with strong diffusion-sensitizing gradients followed by a rapid EPI readout. The diffusion weighting is extraordinarily sensitive to microscopic water motion (Brownian movement), but consequently also to macroscopic patient movement [103]. The prolonged EPI readout (typically 30-80 ms) makes the sequence vulnerable to phase errors accumulating throughout the echo train, particularly in regions of field inhomogeneity [104] [105].
SSFP (Balanced): Balanced SSFP maintains coherent transverse magnetization across TR intervals by using fully balanced gradients in all three axes [106]. The signal derives from a steady-state equilibrium of both longitudinal and transverse magnetization components, resulting in very high signal-to-noise efficiency. However, this equilibrium is highly sensitive to off-resonance effects, including those induced by motion through time-varying field perturbations [106] [4].
Radial/UGRADE Rapid Imaging: These sequences employ non-Cartesian k-space trajectories (e.g., radial, spiral, or stack-of-stars) that oversample the center of k-space [4] [9]. This design provides inherent motion robustness because motion artifacts become distributed radially across the image rather than creating coherent ghosts, and data inconsistencies can be detected and corrected without compromising the entire acquisition [4] [1].
Visualizing Motion Sensitivity Pathways
The following diagram illustrates how different motion types interact with fundamental sequence components to generate artifacts, highlighting critical points of vulnerability and robustness across the four sequence families.
Quantitative Performance Comparison Under Motion
Sequence Performance Metrics in Motion-Affected Scenarios
Table 1: Quantitative Performance Metrics of MRI Pulse Sequences Under Motion Conditions
| Sequence | Typical Acquisition Time | Motion Sensitivity Profile | Primary Motion Artifacts | Key Performance Metrics | Optimal Motion-Robust Parameters |
|---|---|---|---|---|---|
| T2*-GRE | 2-5 minutes | High sensitivity to magnetic field inhomogeneities | Ghosting, signal loss, susceptibility artifacts | T2* contrast-to-noise ratio: 29.4 ± 21.4 [4] | Shortest TR/TE, 90° flip angle [106] |
| Diffusion EPI | 1-4 minutes | Extreme sensitivity to microscopic and macroscopic motion | Image distortion, ghosting, signal dropout | ADC accuracy: 1.97×10⁻³ mm²/s vs. reference 2.0×10⁻³ mm²/s [104] | Cardiac gating, navigator echoes, reduced FOV |
| SSFP (Balanced) | 1-3 minutes | Moderate sensitivity (off-resonance artifacts) | Banding artifacts, signal oscillation | Contrast dynamic range: Narrow but optimizable [106] | Shortest TR/TE, 90° flip angle with preparation [106] |
| SOS echo-uT1RESS (Advanced Radial) | 6 min 51 s | Low sensitivity (inherent motion robustness) | Structured noise, minimal ghosting | Tumor-to-brain contrast: 0.7 ± 0.4 (1.8× improvement) [4] | Radial views: 512, Bandwidth: 690 Hz/pixel [4] |
Motion-Specific Performance Characteristics
Table 2: Motion-Specific Performance Characteristics and Mitigation Approaches
| Sequence | Respiratory Motion Impact | Cardiac Pulsation Impact | Bulk Patient Motion Impact | Effective Motion Mitigation Strategies |
|---|---|---|---|---|
| T2*-GRE | Moderate (ghosting along phase-encode) | High (significant ghosting) | High (severe image degradation) | Patient immobilization, respiratory gating, shortest TE [9] |
| Diffusion EPI | Severe (image distortion + ghosting) | Severe (signal dropout) | Critical (non-diagnostic images) | Cardiac gating, navigator echoes, FOV reduction, parallel imaging [103] |
| SSFP (Balanced) | Low-Moderate (minor banding changes) | Moderate (banding artifact shifts) | Moderate (contrast alteration) | Frequency cycling, magnet shimming, TR minimization [106] |
| Radial/UGRADE Sequences | Low (streaking artifacts only) | Low (minimal impact) | Low (preserved image integrity) | View-angle optimization, self-navigation, iterative reconstruction [4] [9] |
Experimental Protocols for Motion Sensitivity Assessment
Standardized Motion Phantom Validation Methodology
To quantitatively evaluate sequence motion tolerance, researchers employ standardized motion phantom studies that simulate physiological patterns:
Phantom Design: Use a motion platform with programmable translation/rotation capabilities, incorporating tissue-mimicking materials with appropriate T1/T2 values. The motion should replicate common physiological patterns (respiratory: 12-15 cycles/minute; cardiac: 60-80 cycles/minute; bulk motion: sudden shifts of 1-10mm) [1].
Data Acquisition: Each sequence should be tested under identical motion conditions with a static acquisition as reference. For T2*-GRE, utilize parameters: TR=700ms, TE=25ms, flip angle=20° [102]. For Diffusion EPI, use b-values=0, 500, 1000 s/mm², and multiple diffusion directions. For SSFP, implement TR=4ms, TE=2ms, flip angle=60°. For radial sequences, employ 512 radial views with golden-angle rotation [4].
Quantitative Analysis: Calculate motion-induced artifact magnitude using normalized root mean square error (NRMSE) relative to static reference, structural similarity index (SSIM), and lesion detectability using contrast-to-noise ratio in regions of interest [4].
In Vivo Validation Protocol for Neuroimaging Applications
For practical validation in research settings, implement the following protocol in volunteer studies with simulated motion:
Subject Preparation: Position subjects comfortably with head immobilization, then introduce controlled motion paradigms (verbal instructions for periodic head rotation, simulated tremors using mechanical actuators, or breathing maneuvers without head restraint) [9].
Sequence Parameters: Acquire matched anatomical locations with each sequence protocol. Specifically for the SOS echo-uT1RESS sequence, implement: TR=6.9ms, TE=4.16ms, 1.0mm isotropic resolution, 512 radial views, bandwidth=690 Hz/pixel [4]. For comparative T2-GRE, use multi-echo protocols with TE=5-30ms for T2 mapping [105].
Quantitative Assessment: Measure lesion conspicuity using Weber contrast calculations: (SIlesion - SIreference)/SI_reference, where SI represents signal intensity [4]. Calculate contrast-to-noise ratio (CNR) and evaluate diagnostic confidence using Likert scales (1-5) by blinded readers [4].
Research Toolkit: Essential Materials and Reagents
Table 3: Essential Research Toolkit for Motion Sensitivity Investigations
| Tool/Reagent | Specifications | Research Function | Example Application |
|---|---|---|---|
| Motion Phantom Systems | Programmable 3D motion, tissue-equivalent materials | Controlled motion simulation | Quantifying sequence motion tolerance [1] |
| Navigator Echo Components | 2D selective pulses, acceptance window adjustment | Respiratory motion compensation | Free-breathing abdominal imaging [9] |
| Diffusion Encoding Gradients | High amplitude (≥40 mT/m), bipolar designs | Diffusion sensitization without motion artifact | DP-FISP sequence implementation [104] |
| Radial Reconstruction Software | Iterative reconstruction, view-angle optimization | Motion-robust image formation | SOS echo-uT1RESS processing [4] |
| Quantitative Analysis Packages | NRMSE, SSIM, CNR calculation algorithms | Objective image quality assessment | Performance comparison across sequences [4] |
Diagram: Motion Compensation Technique Selection
The following workflow diagram provides a systematic approach for selecting appropriate motion compensation strategies based on sequence type and motion characteristics, integrating both acquisition and reconstruction solutions.
Discussion and Research Implications
Motion Robustness Trade-offs and Sequence Selection
The comparative analysis reveals fundamental trade-offs between conventional and advanced sequences in motion-affected environments. T2*-GRE provides valuable susceptibility contrast but demonstrates high motion sensitivity, requiring careful motion mitigation. Diffusion EPI offers unique microscopic mobility information but suffers from profound vulnerability to both macroscopic motion and magnetic field distortions. SSFP sequences deliver exceptional signal-to-noise efficiency but remain constrained by banding artifacts from off-resonance effects, including those induced by motion [106].
Advanced radial implementations such as SOS echo-uT1RESS represent a paradigm shift in motion management, moving from motion prevention to motion resilience [4]. By employing stack-of-stars k-space trajectories with view-angle optimization, these sequences distribute motion artifacts as low-level structured noise rather than image-degrading ghosts, maintaining diagnostic integrity even in challenging imaging scenarios [4] [9]. The quantitative demonstration of 1.8-fold improvement in tumor-to-brain contrast compared to standard MPRAGE sequences, while maintaining comparable overall image quality, highlights the clinical potential of these motion-robust approaches [4].
Future Directions in Motion-Insensitive Sequence Development
The evolution of MRI pulse sequences continues to address the persistent challenge of motion sensitivity through multiple technological pathways. Integration of compressed sensing with non-Cartesian trajectories provides accelerated acquisition while maintaining motion tolerance [9]. Magnetic field monitoring systems offer real-time correction of field fluctuations induced by motion. Deep learning reconstruction techniques enable substantial undersampling by learning optimal image representations from large datasets, potentially allowing scan times shorter than typical motion cycles.
For research applications requiring quantitative measurements, sequences with inherent motion robustness must be prioritized, particularly in pediatric, geriatric, and neurologically impaired populations where compliance with breath-holding and remaining still is challenging [4] [1]. The development of comprehensive motion-robust quantitative imaging protocols will expand the utility of MRI in both clinical research and drug development, particularly for longitudinal studies where scan-to-scan consistency is essential for detecting subtle therapeutic effects.
Echo planar imaging (EPI) has become the dominant method for acquiring diffusion-weighted images and functional MRI data due to its fast acquisition times [107]. However, EPI introduces significant geometric distortions stemming from inhomogeneities in the underlying B0 magnetic field, which arise from the varying magnetic susceptibilities of air, bone, and tissue [107] [108]. These susceptibility-induced EPI distortions compromise the anatomical fidelity of images, complicate accurate measurements, and pose challenges for multimodal investigations that integrate data from EPI and non-EPI images [107].
Correction of these distortions, known as "unwarping," represents a critical early processing step that significantly influences subsequent analytical outcomes [107] [108]. Two predominant methodological approaches have emerged: acquisition-based correction using B0 field maps and post-processing-based correction using nonlinear registration to structural images. Field mapping requires acquiring supplementary phase images at two different echo times during the scanning session to directly calculate and correct pixel shifts [107]. In contrast, nonlinear registration methods correct distortions by warping EPI images to match anatomically accurate non-EPI structural scans using advanced algorithms like symmetric normalization (SyN) [107] [108].
This guide provides an objective comparison of these approaches, focusing on their reliability in scientific and clinical contexts, particularly for researchers investigating motion sensitivity across MRI pulse sequences. We present experimental data, detailed methodologies, and practical recommendations to inform method selection in neuroimaging and drug development research.
Field Map-Based Distortion Correction
Field map-based unwarping directly addresses the physical source of EPI distortions. The method requires the acquisition of two phase images at different echo times (e.g., TE1 = 2.25 ms, TE2 = 3.25 ms) [107]. From these images, the phase difference is calculated, allowing quantification of the magnetic field inhomogeneity across the imaging volume. This information enables computation of a pixel-shift map along the phase-encode direction, which is then applied to the original EPI images with an equal and opposite transformation to "unwarp" the geometric distortions [107] [108]. This method is acquisition-dependent and must be implemented during the scanning session.
Nonlinear Registration-Based Correction
Nonlinear registration offers a computational alternative that does not require specialized acquisitions. This approach uses sophisticated algorithms like Symmetric Normalization (SyN) implemented in Advanced Normalization Tools (ANTs) to calculate a nonlinear transformation that aligns the distorted EPI image with a matching structural image (e.g., T1-weighted MPRAGE) acquired in the same session [107] [109]. The resulting warp field effectively corrects distortions by maximizing the similarity between the two image types. This method is particularly valuable for legacy datasets that lack the supplementary field map acquisitions [107].
Experimental Comparison: Reliability and Performance
Key Comparative Studies
A comprehensive 2017 study directly compared these two unwarping methods using two different test-retest datasets (Udall: N=39; Boekel: N=32) acquired at differing sites [107] [108] [109]. The research evaluated reliability by examining test-retest consistency of fractional anisotropy (FA) maps derived from diffusion tensor imaging after processing through popular analysis pipelines like Tract-Based Spatial Statistics (TBSS) [107].
Table 1: Test-Retest Reliability Comparison of Unwarping Methods
| Dataset | Field Map Reliability | Nonlinear Registration Reliability | Superior Method |
|---|---|---|---|
| Udall (N=39) | Lower test-retest reliability | Higher test-retest reliability | Nonlinear Registration |
| Boekel (N=32) | Lower test-retest reliability | Higher test-retest reliability | Nonlinear Registration |
| Combined Conclusion | Optimal only with ideal field map acquisition | Consistently higher reliability across conditions | Nonlinear Registration |
The findings revealed that nonlinear registration provided higher test-retest reliability of output FA maps than field map-based unwarping in both datasets, even after accounting for the effects of interpolation on image smoothness [107]. The study concluded that field map-based unwarping was preferable "if and only if the field maps were acquired optimally" [107] [109], suggesting nonlinear registration offers more consistent performance across varying acquisition conditions.
Clinical Impact of Distortion Correction
The clinical significance of proper distortion correction extends beyond methodological preferences to tangible patient outcomes, particularly in radiation oncology. A 2025 retrospective analysis of 419 brain metastases in 189 patients treated with stereotactic radiotherapy investigated the impact of MRI distortion correction on local control [110].
Table 2: Clinical Impact of MRI Distortion Correction in Radiotherapy
| Parameter | 2D Distortion-Corrected MRI | Uncorrected MRI |
|---|---|---|
| Number of Lesions | 220 (52.5%) | 199 (47.5%) |
| Local Progression (12 months) | 14.3% | 21.2% |
| Local Progression (24 months) | 18.7% | 28.6% |
| Hazard Ratio for Local Progression (Multivariate Analysis) | Reference (HR=1.0) | 0.55 (p=0.020) |
The analysis demonstrated that 2D distortion correction was associated with significantly improved local control at both 12 and 24 months [110]. After adjusting for confounding factors including histology, tumor volume, and radiation dose, the use of distortion correction remained independently associated with improved local control (HR 0.55, p=0.020) [110]. This study provides crucial clinical validation for implementing rigorous distortion correction methods in treatment planning.
Experimental Protocols
Field Map Acquisition Protocol
The Udall study implemented field mapping using a 3D interleaved dual echo gradient echo pulse sequence with the following parameters [107] [108]:
- Pulse Sequence: 3D interleaved dual echo gradient echo
- Matrix Size: 256 × 256 × 75
- Field of View: 256 × 256 × 150 mm
- Repetition Time (TR): 10 ms
- Echo Times (TE): TE1 = 2.25 ms, TE2 = 3.25 ms
- Frequency Offset Bound: ±500 Hz (unaliased)
This specific acquisition protocol bounded the unaliased frequency offsets, creating optimal conditions for field map calculation [107].
Nonlinear Registration Protocol
The comparative study utilized Advanced Normalization Tools (ANTs) with the Symmetric Normalization (SyN) algorithm for nonlinear registration [107] [109]. The registration process involved:
- Input Images: Distorted EPI images and corresponding T1-weighted structural images
- Algorithm: Symmetric diffeomorphic mapping with cross-correlation similarity metric
- Transformation: Nonlinear warp field calculation from EPI to structural space
- Application: Warping of EPI images using the calculated transformation
This method effectively corrects distortions by maximizing the alignment between the EPI and structural image spaces without requiring specialized acquisitions [107].
Workflow Visualization
Diagram 1: Workflow comparison between field map and nonlinear registration approaches for EPI distortion correction.
The Scientist's Toolkit
Essential Research Reagents and Solutions
Table 3: Essential Tools for MRI Distortion Correction Research
| Tool/Software | Function | Application Context |
|---|---|---|
| Advanced Normalization Tools (ANTs) | Nonlinear image registration | Symmetric normalization (SyN) for distortion correction |
| FSL (FMRIB Software Library) | Diffusion MRI processing | Alternative processing pipeline including 'topup' |
| Spherical Harmonic Expansions | Gradient field characterization | Modeling gradient nonlinearities for distortion correction |
| Quantitative Susceptibility Mapping (QSM) | Tissue magnetic susceptibility quantification | Advanced field mapping for iron detection and quantification |
| MultiVane XD (Philips) | Motion-insensitive radial acquisition | PROPELLER-based T2-weighted imaging for moving organs |
| 3D Slicer | Semiautomatic segmentation | Volumetric analysis of tumor progression |
Acquisition Parameters for Optimal Field Mapping
Based on the experimental protocols from the comparative studies, optimal field map acquisition should include [107] [108]:
- Dual Echo Acquisition: Two phase images with appropriate echo time difference
- Matching Geometry: Precisely matched geometry between field map and EPI acquisitions
- Adequate Coverage: Sufficient spatial coverage to characterize field inhomogeneities
- Optimal Timing Parameters: TE1/TE2 combination that maximizes phase difference without aliasing
The comparison between field map and nonlinear registration methods for EPI distortion correction reveals a nuanced landscape where methodological advantages depend on specific acquisition conditions and research objectives. Nonlinear registration techniques, particularly those employing symmetric normalization algorithms in ANTs, demonstrate superior test-retest reliability in diffusion MRI applications, making them particularly valuable for studies requiring high measurement consistency [107] [109]. However, field map-based methods retain importance when optimal acquisition parameters can be ensured and when direct physical modeling of field inhomogeneities is methodologically preferable.
The clinical significance of proper distortion correction is substantiated by improved local control outcomes in stereotactic radiotherapy [110], underscoring the translational importance of these methodological considerations. For researchers investigating motion sensitivity across MRI pulse sequences, the choice between these approaches should be guided by acquisition constraints, dataset characteristics, and specific analytical requirements, with nonlinear registration offering particular advantages for legacy data and multi-site studies where acquisition standardization may be challenging.
The Role of fMRI and Quantitative MRI as Biomarkers in Clinical Trials
Functional Magnetic Resonance Imaging (fMRI) and quantitative MRI (qMRI) are transforming clinical trial design by providing non-invasive, objective biomarkers that can predict treatment response, monitor disease progression, and elucidate therapeutic mechanisms. Unlike conventional anatomical imaging, these techniques capture dynamic physiological and functional processes, offering unprecedented insights into brain function and pathology. The development of reliable biomarkers represents a critical advancement for clinical trials, particularly in neurological and psychiatric disorders where objective endpoints are scarce. Resting-state functional connectivity (rsFC), for instance, shows great promise for developing psychiatric disorder biomarkers due to its simplicity, versatility, interpretability, and sensitivity to individual variations [111]. However, creating reliable and practical biomarkers requires overcoming significant challenges, including motion sensitivity, variability in imaging protocols, and the need for robust analytical frameworks [111] [1].
This review examines the evolving roles of fMRI and qMRI as biomarkers, focusing on their technical capabilities, experimental validation, and comparative strengths in the context of clinical trial applications. A critical theme throughout is the impact of motion sensitivity—a fundamental challenge in MRI—on data quality and biomarker reliability, and the pulse sequence innovations developed to mitigate these effects.
fMRI as a Clinical Trial Biomarker: Mechanisms and Applications
Fundamental Principles and Biomarker Types
fMRI measures brain activity by detecting changes in blood oxygenation, known as the Blood-Oxygen-Level-Dependent (BOLD) effect. This indirect marker of neural activity has been leveraged to develop several classes of biomarkers:
- Resting-State Functional Connectivity (rsFC): Measures spontaneous, low-frequency fluctuations in the BOLD signal to map functional networks without task performance. rsFC biomarkers are increasingly used for psychiatric disorders, though development of reliable and practical biomarkers remains challenging due to issues with generalizability, robustness, and accuracy [111].
- Task-Based fMRI: Assesses brain activation in response to specific cognitive, sensory, or motor paradigms.
- Dynamic Connectivity: Captures time-varying changes in functional networks, potentially offering more sensitive biomarkers for neurological and psychiatric conditions.
Advanced acquisition techniques like multi-band echo-volumar imaging (MB-EVI) are pushing spatial and temporal resolution limits, enabling high-speed task-based and resting-state fMRI with millimeter spatial resolution and sub-second temporal resolution at 3 Tesla [112]. These advancements are crucial for detecting subtle functional changes in clinical trials.
Experimental Evidence and Clinical Validation
Recent large-scale studies have demonstrated the potential of fMRI biomarkers across multiple disorders:
Multicenter Psychiatric Disorder Biomarkers: A comprehensive analysis leveraging over 1500 runs of 10-minute resting-state data from 84 traveling-subjects across 29 sites and 900 participants with major depressive disorder (MDD), schizophrenia (SCZ), and autism spectrum disorder (ASD) revealed that ensemble sparse classifiers can develop biomarkers that generalize well across multicenter data [111]. The study found hierarchical variations in individual functional connectivity, ranging from within-subject across-run variations, individual differences, disease effects, inter-scanner discrepancies, and protocol differences. Machine learning algorithms effectively inverted this hierarchy by suppressing individual differences and within-subject variations relative to disorder-related differences, improving the signal-to-noise ratio (disorder effect/participant related variabilities) almost 15 times [111].
Migraine Classification with Explainable AI: A 2025 study demonstrated the power of combining fMRI with interpretable artificial intelligence for migraine classification. Using resting-state fMRI data from 64 participants, GoogleNet models with regional functional connectivity strength (RFCS) indicators achieved >98.44% accuracy and an AUC of 0.99. Explainable AI techniques identified the precuneus and cuneus as the most discriminative brain regions, providing visual explanations for migraine progression and offering promising applications for clinical diagnosis [113].
Table 1: fMRI Biomarker Performance in Disorder Classification
| Disorder | fMRI Modality | Classification Performance | Key Discriminative Regions |
|---|---|---|---|
| Major Depressive Disorder | Resting-state FC | AUC: 0.74 [111] | Frontoparietal networks, default mode network |
| Schizophrenia | Resting-state FC | AUC: 0.82 [111] | Dorsal attention network |
| Autism Spectrum Disorder | Resting-state FC | AUC: 0.66-0.81 [111] | Somatomotor, visual networks |
| Migraine | Regional FC strength | Accuracy: >98.44%, AUC: 0.99 [113] | Precuneus, cuneus, frontal gyrus |
Motion Sensitivity and Mitigation Strategies in fMRI
fMRI is particularly vulnerable to motion artifacts due to its prolonged acquisition times and sensitivity to magnetic field inhomogeneities caused by subject movement. Even minor head motion can cause significant signal changes that confound functional connectivity measurements [1]. In multicenter studies, motion sensitivity compounds with other variability sources including imaging protocol differences, scanner factors, and within-subject across-run variations [111].
Recent technical developments aim to address these limitations:
- Real-time fMRI with MB-EVI: Combining multi-band encoding with accelerated echo-volumar imaging enables higher temporal resolution, reducing motion sensitivity through faster acquisition. MB-EVI achieves temporal resolution as short as 118-650 ms, allowing sensitive mapping of high-frequency resting-state connectivity above 0.3 Hz [112].
- Prospective Motion Correction: Advanced tracking systems monitor head position and adjust imaging parameters in real-time to compensate for motion.
- Advanced Reconstruction: Methods like compressed sensing and NORDIC denoising allow for significant acceleration while maintaining image quality and BOLD sensitivity [112].
Quantitative MRI Biomarkers: Technical Advances and Clinical Applications
qMRI Biomarker Classes and Physical Principles
Quantitative MRI focuses on measuring biophysical parameters with established relationships to tissue properties, offering greater standardization across sites compared to qualitative MRI. Key qMRI biomarkers include:
- Magnetic Susceptibility: Quantified through QSM (Quantitative Susceptibility Mapping) to measure iron deposition and myelin content.
- Perfusion: Measures tissue blood flow using arterial spin labeling (ASL) or dynamic susceptibility contrast (DSC) techniques.
- Microstructural Parameters: Derived from diffusion MRI to assess tissue integrity and organization.
- Myelin Mapping: Techniques like simultaneous myelin and myelin water mapping using Dual-echo STAIR-Cones sequences provide biomarkers for neuroinflammatory and neurodegenerative diseases [26].
Emerging Clinical Applications in Trials
qMRI biomarkers are demonstrating significant value across multiple therapeutic areas:
Neurodegenerative Disease Trials: Whole-brain magnetic susceptibility mapping at 0.3 mm isotropic mesoscale resolution with motion and B0-shift corrections at 7T provides a reliable tool for assessing neurodegenerations [26]. Similarly, whole-brain perfusion mapping in mouse models for Alzheimer's disease using dynamic BOLD MRI with transient hypoxia can demonstrate cerebral perfusion changes before volume decline, suggesting potential as an early biomarker for dementia screening [26].
Oncology Clinical Trials: Hyperpolarized 13C Pyruvate MRI is being evaluated as a response biomarker in multiple oncology trials. At UCSF, ongoing clinical trials are investigating this technology for response monitoring in prostate cancer and for evaluating metabolic changes in fatty liver disease [114]. The technique shows promise for early treatment response assessment by measuring alterations in cellular metabolism.
Motion-Robust Quantitative Sequences: Technical innovations are addressing motion sensitivity in qMRI. For example, self-navigated simultaneous multi-slab 3D DWI eliminates navigator scans through optimized sampling and multiband-specific GRAPPA reconstruction, reducing scanning time by approximately 30% while maintaining image quality [26]. Similarly, the integration of EPTI with prospective motion correction enhances DWI's clinical utility by providing high-resolution, distortion-free imaging for motion-sensitive patients, including children and Alzheimer's disease patients [26].
Table 2: Quantitative MRI Biomarkers in Clinical Research
| qMRI Technique | Measured Parameters | Clinical Trial Applications | Motion Sensitivity Considerations |
|---|---|---|---|
| Hyperpolarized 13C MRI | kPL (pyruvate-to-lactate conversion rate) | Early response assessment in prostate cancer [114] | Requires breath-holding; oxygen administration improves tolerance |
| Dynamic BOLD with hypoxia | Cerebral perfusion | Early biomarker for dementia [26] | Controlled hypoxia challenge requires physiological monitoring |
| Magnetic Susceptibility Mapping | Iron deposition, myelin content | Neurodegeneration assessment [26] | B0-shift corrections essential for quantitative accuracy |
| Multi-slab DMRI | Microstructure parameters | High SNR efficiency for advanced microstructure studies [26] | Self-navigated approaches reduce motion sensitivity |
Comparative Analysis: fMRI vs. Quantitative MRI as Biomarkers
Technical and Practical Considerations for Clinical Trials
When selecting imaging biomarkers for clinical trials, researchers must balance multiple factors including reliability, practicality, and sensitivity to therapeutic effects.
Reliability and Variability Sources: Both fMRI and qMRI face challenges with multicenter reliability. For rsFC biomarkers, variability arises from multiple sources including within-subject across-run variations (median magnitude: 0.133-0.138), individual differences (median: 0.080-0.107), disease effects, inter-scanner discrepancies (median: 0.026-0.037), and protocol differences (median: 0.016) [111]. Machine learning approaches can mitigate these by reweighting the contribution of individual functional connections to prioritize disease-related variations.
Motion Sensitivity Profiles: The two modalities present distinct motion sensitivity challenges. fMRI BOLD signals are contaminated by motion-induced magnetic field perturbations, while qMRI techniques like diffusion imaging are sensitive to both bulk motion and micro-movements that disrupt quantitative parameter estimation. Motion sensitivity also varies significantly by pulse sequence design, with techniques like PROPELLER-based acquisitions demonstrating superior motion robustness [31].
Regulatory and Standardization Considerations: qMRI parameters generally offer better standardization across platforms, as they measure intrinsic tissue properties rather than relative functional changes. However, both modalities require careful protocol harmonization for multicenter trials. Emerging technologies like universal pulses at ultra-high field (11.7T) aim to improve reproducibility for techniques like QSM and R2* mapping [26].
Biomarker Development Workflow
The process of developing and validating neuroimaging biomarkers follows a structured pathway from discovery to clinical application, with particular attention to motion-related confounds at each stage.
Biomarker Development and Validation Workflow
Methodological Standards and Experimental Protocols
Essential Methodologies for Robust Biomarker Development
Multicenter Traveling Subject Studies: The SRPBS and Brain/Minds Beyond projects implemented rigorous experimental designs where 84 traveling subjects were scanned across 29 sites to quantitatively estimate various components of functional connectivity variability [111]. This approach allowed researchers to disentangle disorder-related differences from disorder-unrelated variations attributed to individual differences, within-subject across-runs changes, imaging protocol, and scanner factors.
Motion-Insensitive Pulse Sequence Comparison: A 2019 study compared two motion-insensitive T2-weighted MRI pulse sequences for visualization of the prostatic urethra during MR simulation [31]. Twenty-two patients were imaged using both MultiVane XD (a radial sampling sequence) and single-shot fast-spin-echo sequences. Two expert radiologists scored image quality, finding significantly better urethral visibility with the radial sequence (p<0.0001), demonstrating the importance of sequence selection for motion-prone applications.
Advanced Acquisition Protocols: The MB-EVI protocol combines multiple acceleration approaches including multi-band encoding of up to 6 slabs with CAIPI shifting, accelerated EVI encoding within slabs using up to 4-fold GRAPPA accelerations, 2-shot kz-segmentation and partial Fourier acquisitions [112]. This comprehensive approach enables high spatial-temporal resolution while mitigating motion sensitivity through dramatically reduced acquisition times.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Tools for fMRI and qMRI Biomarker Research
| Tool/Category | Specific Examples | Function in Biomarker Development |
|---|---|---|
| Pulse Sequences | MB-EVI [112], MultiVane XD [31], PROPELLER | Motion-robust data acquisition with optimized spatial-temporal resolution |
| Analysis Frameworks | Ensemble sparse classifiers [111], Graph Neural Networks [115] | Multivariate pattern analysis for disorder classification |
| Motion Correction | Prospective motion correction [26], NORDIC denoising [112] | Artifact reduction and data quality preservation |
| Explainable AI | Gradient-weighted class activation mapping, self-attention mechanisms [113] | Model interpretation and biomarker localization |
| Quantitative Mapping | QSM, HP 13C Pyruvate MRI [114], DE-STAIR-Cones [26] | Objective measurement of tissue properties and metabolism |
Future Directions and Implementation Guidelines
Emerging Trends and Innovation Pathways
The field of neuroimaging biomarkers is rapidly evolving along several key trajectories:
Explainable AI for Biomarker Discovery: The integration of interpretable artificial intelligence with fMRI analysis represents a paradigm shift, moving beyond "black box" classification to identify clinically actionable biomarkers [113]. By visualizing discriminative brain regions, these approaches build clinician trust and facilitate translation to diagnostic applications.
Motion-Insensitive Acquisition Revolution: Continued development of motion-robust sequences is critical for expanding MRI applications to challenging populations including children, elderly patients, and those with neurological conditions affecting movement. Techniques like radial sampling, PROPELLER, and real-time motion correction are becoming increasingly sophisticated [31].
Standardization and Harmonization: As biomarker development moves toward clinical application, extensive efforts are underway to establish standardized acquisition protocols, processing pipelines, and analytical frameworks. Universal pulse designs for ultra-high field systems and harmonized analysis approaches address critical barriers to multicenter reproducibility [26].
Motion Sensitivity Relationships in MRI Biomarkers
The relationship between motion sensitivity and biomarker reliability is complex, involving multiple technical and physiological factors that interact throughout the imaging pipeline.
Motion Sensitivity Relationships in MRI Biomarkers
fMRI and quantitative MRI have matured into powerful biomarker technologies with diverse applications across neurological, psychiatric, and oncological clinical trials. Each modality offers distinct advantages: fMRI provides unparalleled insights into brain function and network organization, while qMRI delivers objective, quantitative measures of tissue properties with excellent standardization potential. Both face significant motion sensitivity challenges that must be addressed through sophisticated acquisition strategies, pulse sequence design, and analytical approaches.
The future of neuroimaging biomarkers lies in the continued refinement of motion-robust acquisition techniques, the development of explainable AI frameworks for biomarker localization, and the implementation of rigorous multicenter validation standards. As these technologies evolve, they promise to transform clinical trial design by providing objective, mechanistically grounded endpoints that can detect therapeutic effects earlier and with greater sensitivity than conventional clinical measures.
Conclusion
Motion sensitivity is not a uniform property but varies significantly across MRI pulse sequences due to differences in their underlying physics, k-space trajectories, and acquisition times. A multifaceted 'toolbox' approach is essential, combining foundational understanding, advanced correction methodologies, practical protocol optimization, and rigorous validation. For researchers and drug development professionals, the choice of sequence and correction strategy must be guided by the specific application, weighing factors like the required contrast, the type of motion, and the need for quantitative accuracy. Future directions will likely involve the increased integration of AI for real-time correction, the development of even more motion-robust ultra-fast sequences, and the standardization of motion correction protocols to enhance the reliability of MRI biomarkers in multi-center clinical trials.
References
- 1. Motion Artefacts in MRI: a Complex Problem with Many Partial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4517972/]
- 2. Basic Theory of Motion Artifacts in MRI [https://cds.ismrm.org/protected/21MProceedings/PDFfiles/E5763.html]
- 3. A k-Space Model of Movement Artefacts [https://pmc.ncbi.nlm.nih.gov/articles/PMC7116018/]
- 4. 3 Tesla stack-of-stars echo unbalanced T1 relaxation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357450/]
- 5. Diagnostic value of Zero Echo Time (ZTE) MRI pulse ... [https://ejrnm.springeropen.com/articles/10.1186/s43055-025-01581-3]
- 6. MIT researchers combine deep learning and physics to fix ... [https://www.csail.mit.edu/news/mit-researchers-combine-deep-learning-and-physics-fix-motion-corrupted-mri-scans]
- 7. Parallel Imaging (PI): artifacts - MRI Questions [https://mriquestions.com/artifacts-in-pi.html]
- 8. Parallel imaging artifact [https://mrimaster.com/parallel-imaging-artifact/]
- 9. MRI Motion Artifacts (Ghosting Artifact) [https://mrimaster.com/mri-artifacts/]
- 10. Ghosting? [https://mriquestions.com/ghosting.html]
- 11. The Basics of MRI [https://www.cis.rit.edu/htbooks/mri/chap-11/chap-11.htm]
- 12. MRI Physics: MRI Pulse Sequences - XRayPhysics [http://xrayphysics.com/sequences.html]
- 13. Pulse Sequences and Techniques for Body MRI | SpringerLink [https://link.springer.com/chapter/10.1007/978-3-031-90554-4_10]
- 14. Quantitative assessment of the susceptibility artefact and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5624609/]
- 15. Motion Mitigation in Abdominal MRI [https://www.rsna.org/news/2025/january/motion-mitigation-abdominal-mri]
- 16. Comparison of MRI pulse sequences for investigation of lesions of the cervical spinal cord - PubMed [https://pubmed.ncbi.nlm.nih.gov/11071441/]
- 17. Systematic Review and Meta-analysis of AI-driven MRI ... [https://arxiv.org/abs/2509.05071]
- 18. k-space: trajectories [https://mriquestions.com/k-space-trajectories.html]
- 19. MRI artifacts and correction strategies - Open Access Journals [https://www.openaccessjournals.com/articles/mri-artifacts-and-correction-strategies-11010.html]
- 20. MR sequences and rapid acquisition for MR guided ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4621782/]
- 21. Comparison of TGSE-BLADE DWI, RESOLVE DWI, and SS ... [https://www.nature.com/articles/s41598-022-22760-6]
- 22. Motion correction in MRI of the brain - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4930872/]
- 23. Polar Fourier transform in practice: its efficiency and ... [https://link.springer.com/article/10.1007/s10334-025-01284-w]
- 24. Multi-Band Accelerated EPI Pulse Sequences [https://www.cmrr.umn.edu/multiband/]
- 25. Speed and flexibility for high‐resolution 3D imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9292510/]
- 26. ISMRM25 - Pulse Sequences for Neuroimaging [https://www.ismrm.org/25/program-files/D-13.htm]
- 27. Unsolved problems and unmet needs - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620149/]
- 28. Effect of Head Motion on MRI B0 Field Distribution - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6239980/]
- 29. Motion and magnetic field inhomogeneity correction ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/39532518/]
- 30. Movement-related artefacts (MR-ART) dataset of matched ... [https://www.nature.com/articles/s41597-022-01694-8]
- 31. Comparison of Motion-Insensitive T2-Weighted MRI Pulse ... [https://www.sciencedirect.com/science/article/abs/pii/S1879850019301808]
- 32. Reproduction of Motion Artifacts for Performance Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3674114/]
- 33. Unified Motion Correction Model for Multi-modal MRI [https://archive.ismrm.org/2025/0745.html]
- 34. Low-field and portable MRI technology - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12549457/]
- 35. Radial spoke energy for self-navigated motion detection ... [https://arxiv.org/html/2509.01833v1]
- 36. Portable, bedside, low-field magnetic resonance imaging ... [https://www.nature.com/articles/s41467-021-25441-6]
- 37. Multimodal precision MRI of the individual human brain at ... [https://www.nature.com/articles/s41597-025-04863-7]
- 38. Learning Spatiotemporal Brain Dynamics in Adolescents ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11240882/]
- 39. Reducing motion sensitivity in 3D high-resolution T2 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6981037/]
- 40. Simultaneous feedback control for joint field and motion ... [https://www.sciencedirect.com/science/article/pii/S1053811920307722]
- 41. Dynamic distortion correction for functional MRI using FID ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7718422/]
- 42. Comparison of prospective and retrospective motion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8635810/]
- 43. Diffusion tensor imaging (DTI) with retrospective motion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3443529/]
- 44. Comparison of prospective and retrospective motion correction in 3D-encoded neuroanatomical MRI - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8635810/]
- 45. Prospective Motion Correction in Functional MRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5427003/]
- 46. An evaluation of prospective motion correction (PMC) for ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2015.00097/full]
- 47. Deep Learning for Retrospective Motion Correction in MRI: A Comprehensive Review - PubMed [https://pubmed.ncbi.nlm.nih.gov/37831582/]
- 48. Prospective and retrospective motion correction in diffusion ... [https://www.sciencedirect.com/science/article/abs/pii/S1053811911007646]
- 49. Comparison of prospective and retrospective motion correction in 3D-encoded neuroanatomical MRI - PubMed [https://pubmed.ncbi.nlm.nih.gov/34490929/]
- 50. mtrk—A flexible environment for developing open-source ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12543096/]
- 51. Stop moving: MR motion correction as an opportunity for artificial intelligence - PubMed [https://pubmed.ncbi.nlm.nih.gov/38386151/]
- 52. Advanced preclinical functional magnetic resonance ... [https://www.nature.com/articles/s44303-025-00085-z]
- 53. Optimizing MRI sequence classification performance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12559157/]
- 54. Comparison of radial versus cartesian k-space sampling in T1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465981/]
- 55. On the optimization of imaging parameters for magnetic ... [https://www.sciencedirect.com/science/article/abs/pii/S109078072100197X]
- 56. MRI innovation developments – Feature [https://www.philips.com/a-w/about/news/archive/features/2025/innovation-spotlight-finding-new-ways-of-enhancing-magnetic-resonance-imaging.html]
- 57. Zero-TE MRI: principles and applications in the head and neck [https://pmc.ncbi.nlm.nih.gov/articles/PMC10162052/]
- 58. Silent zero TE MR neuroimaging: Current state-of-the-art ... [https://www.sciencedirect.com/science/article/pii/S007965652100011X]
- 59. Comparison of Motion-insensitive T2-weighted MRI Pulse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6832802/]
- 60. 3D Zero Echo Time (ZTE) MRI versus 3D CT for Glenoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7483823/]
- 61. CT-like MRI using the zero-TE technique for osseous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7068078/]
- 62. Use of functional imaging across clinical phases in CNS ... [https://www.nature.com/articles/tp201343]
- 63. Quantitative pharmacologic MRI in mice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3292675/]
- 64. Contrast media related artifacts [https://mrimaster.com/contrast-media-related-artifacts/]
- 65. Findings and procedure details - EPOS™ [https://epos.myesr.org/poster/esr/ecr2025/C-17211/findings%20and%20procedure%20details]
- 66. Motion Correction of Parametric fMRI Data From Multi-Slice ... [https://pubmed.ncbi.nlm.nih.gov/11675657/]
- 67. Automated design of pulse sequences for magnetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8501900/]
- 68. MRI Equipment Breakthroughs 2025 [https://openmedscience.com/mri-equipment-breakthroughs-how-2025-innovations-transform-patient-care/]
- 69. Optimizing MRI Scheduling in High-Complexity Hospitals [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189641/]
- 70. Next-generation MRI scanner designed for ultra-high ... [https://www.nature.com/articles/s41592-023-02068-7]
- 71. Reducing motion artifacts [https://mriquestions.com/reducing-motion-artifacts.html]
- 72. 3D proton density turbo spin echo nDixon sequence vs. 2D ... [https://www.sciencedirect.com/science/article/pii/S0720048X25006382]
- 73. Evaluation of motion artefact reduction depending on the ... [https://www.nature.com/articles/s41598-023-35794-1]
- 74. Motion artifact reduction for magnetic resonance imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9815594/]
- 75. An in-vivo approach to quantify in-MRI head motion ... [https://www.medrxiv.org/content/10.1101/2025.04.23.25326185v1.full-text]
- 76. Diffusion-presatured STIR for fat suppression during ... [https://archive.ismrm.org/2025/5427.html]
- 77. Effectiveness of fat suppression methods and influence on ... [https://www.sciencedirect.com/science/article/pii/S0730725X25000220]
- 78. Comparison between fast-interrupted steady-state (FISS) ... [https://link.springer.com/article/10.1007/s10334-025-01273-z]
- 79. A signal model for fat‐suppressed T1‐mapping and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11617136/]
- 80. Comparison between fast-interrupted steady-state (FISS) ... [https://pubmed.ncbi.nlm.nih.gov/40549260/]
- 81. Gating v triggering MRI [https://mriquestions.com/gating-v-triggering.html]
- 82. Feasibility of finger-pulse triggering as a substitute for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12514587/]
- 83. Reduction of Motion Artifacts in Functional Connectivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9618388/]
- 84. Physiological and motion signatures in static and time- ... [https://elifesciences.org/articles/62324]
- 85. DSC Perfusion MRI Artefact Reduction Strategies: A Short ... [https://www.mdpi.com/2077-0383/14/13/4776]
- 86. Motion-Robust MRI: Reconstruction & Motion Correction [https://www.ismrm.org/25/program-files/O-05.htm]
- 87. Motion compensated magnetic resonance imaging of an ... [https://www.nature.com/articles/s41598-025-27800-5]
- 88. 上海交大魏红江团队在自由呼吸动态磁共振成像上取得进展 [https://bme.sjtu.edu.cn/Web/Show/4046]
- 89. Current State-of-the-Art 3D MRI Sequences for Assessing ... [https://pubmed.ncbi.nlm.nih.gov/40962128/]
- 90. Brain-mimicking phantom for biomechanical validation of ... [https://www.sciencedirect.com/science/article/abs/pii/S1751616121003556]
- 91. Brain-mimicking phantom for biomechanical validation of motion sensitive MR imaging techniques - PubMed [https://pubmed.ncbi.nlm.nih.gov/34271404/]
- 92. Physical and Numerical Phantoms for the validation of brain microstructural MRI: A Cookbook - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6175674/]
- 93. Physical and numerical phantoms for the validation of brain microstructural MRI: A cookbook - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1053811918305536]
- 94. Super phantoms: advanced models for testing medical imaging technologies | Communications Engineering [https://www.nature.com/articles/s44172-024-00218-z]
- 95. Phantom studies in medical imaging (PSMI): a guide with ... [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-025-00641-7]
- 96. Quantitative evaluation of apparent diffusion coefficient in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12637080/]
- 97. Assessment of a diffusion phantom for quality assurance in ... [https://www.nature.com/articles/s41598-025-12777-y]
- 98. Quantification and Reduction of Ghosting Artifacts in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2396297/]
- 99. Real-time motion monitoring improves functional MRI data ... [https://www.sciencedirect.com/science/article/pii/S1878929322000597]
- 100. Software Tools for Development, Data Processing & Analysis [https://www.ismrm.org/21/program-files/D-116.htm]
- 101. GRE T2∗-Weighted MRI: Principles and Clinical Applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC4009216/]
- 102. Superiority of SWI over GRE [https://mriquestions.com/whats-wrong-with-gre.html]
- 103. Diffusion weighted imaging: Technique and applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5039674/]
- 104. A Rapid Diffusion MRI Technique at 7T - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3297727/]
- 105. Optimization of Gradient-Echo Echo-Planar Imaging for T2* ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10610880/]
- 106. Comparative study of FAST gradient echo MRI sequences [https://pubmed.ncbi.nlm.nih.gov/15558562/]
- 107. Evaluation of Field Map and Nonlinear Registration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5318394/]
- 108. Evaluation of Field Map and Nonlinear Registration ... [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2017.00017/full]
- 109. Evaluation of Field Map and Nonlinear Registration ... [https://pubmed.ncbi.nlm.nih.gov/28270762/]
- 110. MRI distortion correction is associated with improved local ... [https://www.nature.com/articles/s41598-025-93255-3]
- 111. Computational mechanisms of neuroimaging biomarkers ... [https://www.nature.com/articles/s41380-025-03134-6]
- 112. Real-time fMRI using multi-band echo-volumar imaging ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1543206/full]
- 113. Interpretable Artificial Intelligence Analysis of Functional ... [https://pubmed.ncbi.nlm.nih.gov/40903006/]
- 114. UCSF MRI Clinical Trials for 2025 — San Francisco Bay Area [https://clinicaltrials.ucsf.edu/mri]
- 115. Discovering robust biomarkers of psychiatric disorders from ... [https://www.sciencedirect.com/science/article/pii/S1053811925004252]