Overcoming the Pitfalls in Reproducible Brain-Phenotype Signatures: A Roadmap for Researchers and Drug Developers
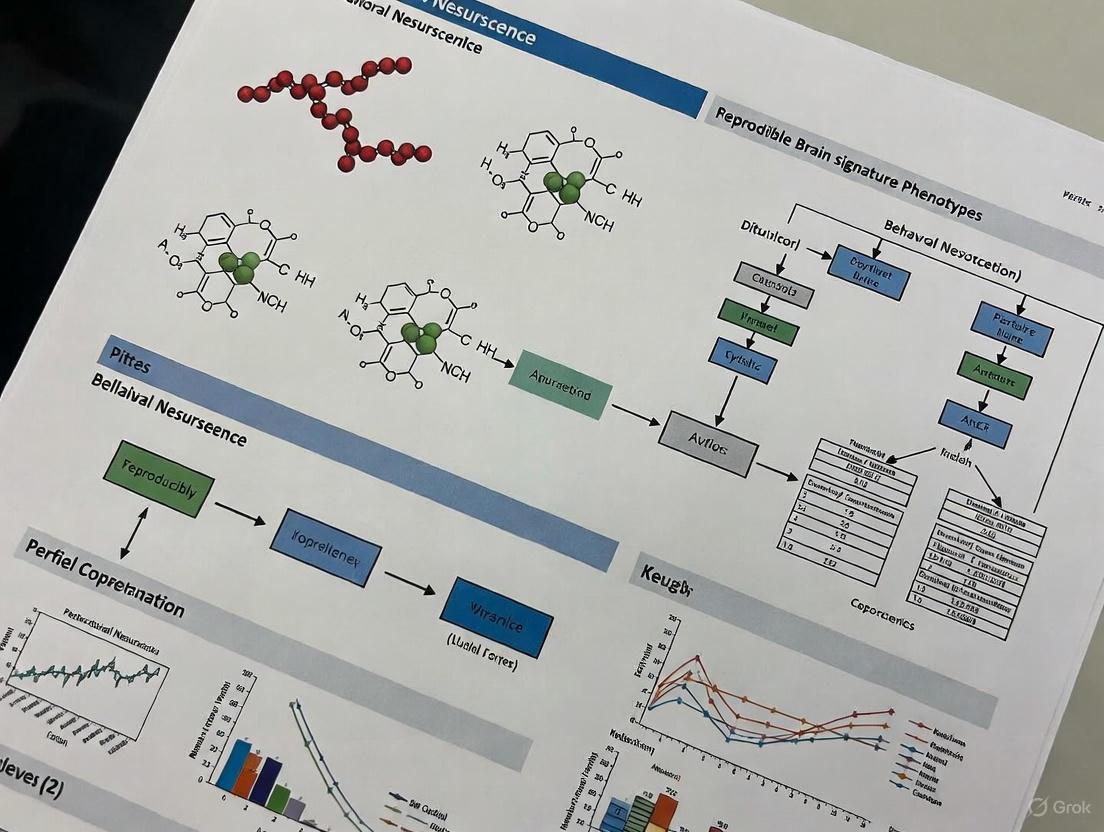
This article provides a comprehensive framework for establishing reproducible brain-phenotype signatures, a critical challenge in neuroscience and neuropharmacology.
Overcoming the Pitfalls in Reproducible Brain-Phenotype Signatures: A Roadmap for Researchers and Drug Developers
Abstract
This article provides a comprehensive framework for establishing reproducible brain-phenotype signatures, a critical challenge in neuroscience and neuropharmacology. We explore the foundational obstacles—from sample size limitations and phenotypic harmonization to data quality and access—that have plagued brain-wide association studies (BWAS). The piece details methodological advances in data processing, harmonization, and predictive modeling that enhance reproducibility. It further offers troubleshooting strategies for common technical and analytical pitfalls and outlines rigorous validation and comparative frameworks to ensure generalizability. Designed for researchers, scientists, and drug development professionals, this guide synthesizes the latest evidence and best practices to foster robust, clinically translatable neuroscience.
Why Brain-Phenotype Associations Fail: Unpacking the Foundational Challenges
Frequently Asked Questions
1. What is the "sample size crisis" in Brain-Wide Association Studies (BWAS)? The sample size crisis refers to the widespread failure of BWAS to produce reproducible findings because typical study samples are too small. These studies aim to link individual differences in brain structure or function to complex cognitive or mental health traits, but the true effects are much smaller than previously assumed. Consequently, small-scale studies are statistically underpowered, leading to inflated effect sizes and replication failures [1] [2].
2. Why do BWAS require such large sample sizes compared to other neuroimaging studies? BWAS investigates correlations between common, subtle variations in the brain and complex behaviors. These brain-behavior associations are inherently small. Research shows the median univariate effect size (|r|) in a large, rigorously denoised sample is approximately 0.01 [1]. Detecting such minuscule effects reliably requires very large samples to overcome sampling variability, whereas classical brain mapping studies (e.g., identifying the region activated by a specific task) often have larger effects and can succeed with smaller samples [1] [2].
3. My lab can't collect thousands of participants. Is BWAS research impossible for us? Not necessarily, but it requires a shift in strategy. The most straightforward approach is to leverage large, publicly available datasets like the Adolescent Brain Cognitive Development (ABCD) Study, the UK Biobank (UKB), or the Human Connectome Project (HCP) [1] [2]. Alternatively, focus on forming large consortia to aggregate data across multiple labs [3] [2]. If collecting new data is essential, our guide on optimizing scan time versus sample size below can help maximize the value of your resources.
4. How does scan duration interact with sample size in fMRI-based BWAS? There is a trade-off between the number of participants (sample size) and the amount of data collected per participant (scan time). Initially, for scans of ≤20 minutes, total scan duration (sample size × scan time per participant) is a key determinant of prediction accuracy, making sample size and scan time somewhat interchangeable [4]. However, sample size is ultimately more critical. Once scan time reaches a certain point (e.g., beyond 20-30 minutes), increasing the sample size yields greater improvements in prediction accuracy than further increasing scan time [4].
5. What is a realistic expectation for prediction accuracy in BWAS? Even with large samples, prediction accuracy for complex cognitive and mental health phenotypes is often modest. Analyses show that increasing the sample size from 1,000 to 1 million participants can lead to a 3- to 9-fold improvement in performance. However, the extrapolated accuracy remains worryingly low for many traits, suggesting a fundamental limit to the predictive information contained in current brain imaging data for these phenotypes [5].
Quantitative Data at a Glance
Table 1: Observed Effect Sizes and Replicability in BWAS (from Marek et al., 2022) [1]
| Metric | Typical Small Study (n=25) | Large-Scale Study (n~3,900) | Key Finding | ||||
|---|---|---|---|---|---|---|---|
| Median | r | effect size | Often reported > 0.2 | ~0.01 | Extreme effect size inflation in small samples. | ||
| Top 1% of | r | effects | Highly inflated | > 0.06 | Largest reproducible effect was | r | = 0.16. |
| 99% Confidence Interval | ± 0.52 | Narrowed substantially | Small samples can produce opposite conclusions. | ||||
| Replication Rate | Very Low | Begins to improve in the thousands | Thousands of participants are needed for reproducibility. |
Table 2: Prediction Performance as a Function of Sample Size (from Schulz et al., 2023) [5]
| Sample Size | Prediction Performance (Relative Gain) | Implication for Study Design |
|---|---|---|
| 1,000 | Baseline | This is a modern minimum for meaningful prediction attempts. |
| 10,000 | Improves by several fold | Similar to major current datasets (e.g., ABCD, UKB substudies). |
| 100,000 | Continued improvement | Necessary for robustly detecting finer-grained effects. |
| 1,000,000 | 3- to 9-fold gain over n=1,000 | Performance reserves exist but accuracy for some phenotypes may remain low. |
Table 3: Cost-Effective Scan Time for fMRI BWAS (from Lydon-Staley et al., 2025) [4] This table summarizes the trade-off between scan time and sample size for a fixed budget, considering overhead costs like recruitment.
| Scenario | Recommended Minimum Scan Time | Rationale |
|---|---|---|
| General Resting-State fMRI | At least 30 minutes | This was, on average, the most cost-effective duration, yielding ~22% savings over 10-min scans. |
| Task-based fMRI | Can be shorter than for resting-state | The structured evoked activity can sometimes lead to higher efficiency. |
| Subcortical-to-Whole-Brain BWAS | Longer than for resting-state | May require more data to achieve stable connectivity estimates. |
Experimental Protocols for Robust BWAS
Protocol 1: Designing a New BWAS with Optimized Resources
This protocol helps balance participant recruitment and scan duration when resources are limited.
- Budget Calculation: Determine your total budget. Subtract the fixed overhead costs per participant (recruitment, screening, clinician time) [4]. The remainder determines how you can trade off between the number of participants (N) and scan time per participant (T).
- Feasibility Space: Calculate multiple feasible (N, T) pairs within your budget.
- Optimization: Use the established principle that prediction accuracy increases with the logarithm of the total scan duration (N × T) [4].
- Decision Rule: While sample size and scan time are initially interchangeable, always prioritize a larger sample size. However, do not reduce scan time below 20-30 minutes, as this is empirically cost-inefficient and leads to poor data quality [4]. Overshooting the optimal scan time is cheaper than undershooting it.
Protocol 2: Conducting a Power Analysis for BWAS
Traditional power analysis is challenging because true effect sizes are small and poorly characterized. Use this practical approach.
- Use Realistic Effect Sizes: Do not rely on inflated effects from small-scale literature. Use tools like the BrainEffeX web app to explore realistic, empirically derived effect sizes from large datasets for analyses similar to yours [6].
- Define Your Target: Determine the smallest effect size of practical interest (SESOI). For complex behaviors, even correlations of r = 0.1 - 0.3 may be meaningful [3].
- Calculate Sample Size: Use standard power calculation software (e.g., G*Power [7]) with the empirically derived effect size, a power of at least 0.8, and an alpha of 0.05. Be prepared for the required N to be in the thousands.
- Leverage Large Public Datasets: For a pilot study or initial discovery, always consider using an existing large-scale dataset like UK Biobank or ABCD to obtain stable, reproducible effect estimates before collecting new data [1] [5].
Protocol 3: Mitigating Bias in Brain-Phenotype Models
Models can fail for individuals who defy stereotypical profiles associated with a phenotype, such as certain sociodemographic or clinical covariates [8].
- Test for Structured Failure: After building a predictive model, don't just look at overall accuracy. Analyze if misclassification is random or systematic. Reliable, phenotype-specific model failure indicates potential bias [8].
- Interrogate the Phenotype: Critically assess if your behavioral or clinical measure is a pure reflection of the intended construct, or if it is confounded by sociodemographic, cultural, or clinical factors [8].
- Report Transparently: Clearly report effect sizes and confidence intervals for all analyses, regardless of statistical significance. This provides a more accurate picture of the association strength for future meta-science and power analyses [1] [2].
The Scientist's Toolkit
Table 4: Essential Resources for reproducible BWAS
| Resource Name | Type | Primary Function | Relevance to BWAS |
|---|---|---|---|
| ABCD, UK Biobank, HCP | Data Repository | Provides large-scale, open-access neuroimaging and behavioral data. | Enables high-powered discovery and replication without new data collection [1] [5]. |
| BrainEffeX | Web Application | Interactive explorer for empirically derived fMRI effect sizes from large datasets. | Informs realistic power calculations and study planning [6]. |
| G*Power / OpenEpi | Software Tool | Performs prospective statistical power analyses for various study designs. | Calculates necessary sample size given an effect size estimate, power, and alpha [7]. |
| Optimal Scan Time Calculator | Online Calculator | Models the trade-off between fMRI scan time and sample size for prediction accuracy. | Helps optimize study design for cost-effectiveness [4]. |
| Regularized Linear Models | Analysis Method | Machine learning technique (e.g., kernel ridge regression) for phenotype prediction. | A robust and highly competitive approach for building predictive models from high-dimensional brain data [4] [5]. |
Troubleshooting Guide: Navigating Bifactor Model Harmonization
This guide addresses common challenges researchers face when harmonizing disparate psychiatric assessments using bifactor models and provides step-by-step solutions.
1. Problem: Poor Model Fit After Harmonization
- Symptoms: The bifactor model shows unacceptable fit indices (e.g., CFI < 0.90, RMSEA > 0.08) when applied to harmonized items from different instruments.
- Impact: Results are unreliable and may not be valid for cross-study comparisons, undermining the entire harmonization effort.
- Diagnostic Checks:
- Confirm that item content is semantically equivalent across instruments.
- Check factor loadings; weak loadings (< 0.3) on the general or specific factors indicate poor item performance.
- Test for instrument-specific measurement non-invariance.
- Solutions:
- Quick Fix: Re-specify the model by removing items with consistently low factor loadings.
- Standard Resolution: Use a phenotypic reference panel—a supplemental sample with complete data on all items from all instruments—to improve model linking [9].
- Root Cause Fix: Implement a Bi-Factor Integration Model (BFIM) that explicitly models a general factor across all studies and orthogonal specific factors that capture cohort-specific variances [9].
2. Problem: Specific Factors Lack Reliability
- Symptoms: The specific factors (e.g., internalizing, externalizing) in the bifactor model show low reliability indices (e.g., H-index < 0.7, Factor Determinacy < 0.8) despite a reliable p-factor.
- Impact: Specific dimensions of psychopathology cannot be interpreted meaningfully, limiting the clinical utility of the model.
- Diagnostic Checks:
- Calculate model-based reliability indices (OmegaH, ECV) for each specific factor.
- Check if the specific factors predict relevant external criteria (e.g., symptom impact on daily life).
- Solutions:
- Quick Fix: Focus analysis and interpretation only on the general p-factor, which typically demonstrates higher and more consistent reliability [10] [11].
- Standard Resolution: Test different established bifactor model configurations from the literature to find one with acceptable reliability for your specific data and harmonization goal [11].
- Root Cause Fix: Acknowledge that harmonized specific factors may have inherently limited reliability. Use them only in conjunction with other validating evidence and clearly communicate this limitation in research findings.
3. Problem: Low Authenticity of Harmonized Factor Scores
- Symptoms: Factor scores derived from the harmonized (limited item pool) model show low correlation (> 0.5 Z-score difference) with scores from the original full-item models.
- Impact: The harmonized measure does not adequately represent the original construct, leading to misinterpretation of results.
- Diagnostic Checks:
- Calculate the correlation between factor scores from the harmonized and original models.
- Determine the percentage of participants for whom the factor score difference exceeds 0.5 Z-scores.
- Solutions:
- Quick Fix: Use the harmonized models only for the general p-factor, which typically shows high authenticity (correlations > 0.89 with original models) [10].
- Standard Resolution: Be transparent about authenticity limitations, especially for specific factors, and perform sensitivity analyses to quantify its impact on your main conclusions.
- Root Cause Fix: Select a harmonization model that has demonstrated high authenticity in previous studies, even if it requires using a larger set of common items.
4. Problem: Failure of Measurement Invariance Across Instruments
- Symptoms: The bifactor model structure or parameters differ significantly between the original instruments being harmonized.
- Impact: Observed score differences may reflect methodological artifacts rather than true psychological differences, making combined analysis invalid.
- Diagnostic Checks:
- Conduct multi-group confirmatory factor analysis to test for configural, metric, and scalar invariance.
- Look for significant differences in model fit when factor loadings and item thresholds are constrained to be equal across groups.
- Solutions:
- Quick Fix: Report the lack of invariance as a significant limitation of the harmonized measure.
- Standard Resolution: Use a harmonization model that has been previously validated for instrument invariance. Research suggests that only about 40% of bifactor model configurations (5 out of 12 in one study) demonstrate instrument invariance [10].
- Root Cause Fix: Implement a moderated non-linear factor analysis (MNLFA) that allows item parameters to vary systematically by instrument, thereby formally modeling the measurement differences rather than assuming they don't exist [9].
Frequently Asked Questions
Q1: What is phenotype harmonization and why is it particularly challenging in psychiatric research? Phenotype harmonization is the process of combining data from different assessment instruments to measure the same underlying construct, which is essential for large-scale consortium research [10]. It is particularly challenging in psychiatry because most constructs (e.g., depression, aggression) are latent traits measured indirectly through questionnaires with varying items, response scales, and cultural interpretations. Different questionnaires often tap into different aspects of a behavioral phenotype, and simply creating sum scores of available items ignores these systematic measurement differences, introducing heterogeneity and reducing power in subsequent analyses [9].
Q2: What are the key advantages of using bifactor models for harmonization? Bifactor models provide a sophisticated approach to harmonization by simultaneously modeling a general psychopathology factor (p-factor) that is common to all items and specific factors that capture additional variance from subsets of items [10] [9]. Key advantages include:
- Separating general psychopathology from specific dimensions (e.g., internalizing, externalizing)
- Accounting for measurement error in the phenotype score
- Allowing items from different instruments to contribute differentially to the underlying trait
- Providing a common metric for the phenotype across different studies and instruments [9]
Q3: Our team is harmonizing CBCL and GOASSESS data. How many bifactor model configurations should we consider? Your team should be aware that there are at least 11 published bifactor models for the CBCL alone, ranging from 39 to 116 items [11]. When harmonizing CBCL with GOASSESS, empirical evidence suggests that only about 5 out of 12 model configurations demonstrated both acceptable model fit and instrument invariance [10]. Systematic evaluation of these existing models is recommended rather than developing a new model from scratch.
Q4: What is a "phenotypic reference panel" and when is it necessary for harmonization? A phenotypic reference panel is a supplemental sample of participants who have completed all items from all instruments being harmonized [9]. This panel is particularly necessary when the primary studies have completely non-overlapping items (e.g., Study A uses Instrument X, Study B uses Instrument Y). The reference panel provides the necessary linking information to place scores from all participants on a common metric. Simulations have shown that such a panel is crucial for realizing power gains in subsequent genetic association analyses [9].
Q5: How reproducible are brain-behavior associations in harmonized studies, and what sample sizes are needed? Reproducible brain-wide association studies (BWAS) require much larger samples than previously thought. While the median neuroimaging study has about 25 participants, BWAS typically show very small effect sizes (median |r| = 0.01), with the top 1% of associations reaching only |r| = 0.06 [1]. At small sample sizes (n = 25), confidence intervals for these associations are extremely wide (r ± 0.52), leading to both false positives and false negatives. Reproducibility begins to improve significantly only when sample sizes reach the thousands [1].
Experimental Protocols & Data
Table 1: Performance Metrics of Bifactor Models in CBCL-GOASSESS Harmonization [10]
| Model Performance Indicator | P-Factor | Internalizing Factor | Externalizing Factor | Attention Factor |
|---|---|---|---|---|
| Factor Score Correlation (Harmonized vs. Original) | > 0.89 | 0.12 - 0.81 | 0.31 - 0.72 | 0.45 - 0.68 |
| Participants with >0.5 Z-score Difference | 6.3% | 18.5% - 50.9% | 15.2% - 41.7% | 12.8% - 29.4% |
| Typical Reliability (H-index) | Acceptable in most models | Variable | Variable | Acceptable in most models |
| Prediction of Symptom Impact | Consistent across models | Inconsistent | Inconsistent | Consistent across models |
Table 2: Essential Research Reagents for Phenotype Harmonization Studies [10] [9] [12]
| Research Reagent | Function in Harmonization | Implementation Example |
|---|---|---|
| Bi-Factor Integration Model (BFIM) | Provides a single common phenotype score while accounting for study-specific variability | Models a general factor across all studies and orthogonal specific factors for cohort-specific variance [9] |
| Phenotypic Reference Panel | Enables linking of different instruments by providing complete data on all items | Supplemental sample that completes all questionnaires from all contributing studies [9] |
| Measurement Invariance Testing | Determines if the measurement model is equivalent across instruments or groups | Multi-group confirmatory factor analysis testing configural, metric, and scalar invariance [10] |
| Authenticity Analysis | Quantifies how well harmonized scores approximate original instrument scores | Correlation and difference scores between harmonized and full-item model factor scores [10] |
Methodological Workflows
Harmonization Workflow with Quality Checkpoints
Bifactor Model Structure for Instrument Harmonization
FAQs: Foundational Knowledge
Q1: What is technical variability in neuroimaging, and why is it a problem for reproducibility? Technical variability refers to non-biological differences in brain imaging data introduced by factors like scanner manufacturer, model, software version, imaging site, and data processing methods. Because MRI intensities are acquired in arbitrary units, differences between scanning parameters can often be larger than the biological differences of interest [13]. This variability acts as a significant confound, potentially leading to spurious associations and replication failures in brain-wide association studies (BWAS) [1].
Q2: How does sample size interact with technical variability? Brain-wide association studies require thousands of individuals to produce reproducible results because true brain-behaviour associations are typically much smaller than previously assumed (median |r| ≈ 0.01) [1]. Small sample sizes are highly vulnerable to technical confounds and sampling variability, with one study demonstrating that at a sample size of n=25, the 99% confidence interval for univariate associations was r ± 0.52, meaning two independent samples could reach opposite conclusions about the same brain-behaviour association purely by chance [1].
Q3: What are the main sources of technical variability in functional connectomics? A systematic evaluation of 768 fMRI data-processing pipelines revealed that choices in brain parcellation, connectivity definition, and global signal regression create vast differences in network reconstruction [14]. The majority of pipelines failed at least one criterion for reliable network topology, demonstrating that inappropriate pipeline selection can produce systematically misleading results [14].
FAQs: Troubleshooting Technical Variability
Q1: How can I identify suboptimal perfusion MRI (DSC-MRI) data in my experiments? Practical guidance suggests evaluating these key metrics [15]:
- Check contrast agent timing and administration: Ensure proper preload dose (approximately 5-6 minutes before DSC sequence) and bolus injection rate (typically 3-5 mL/s)
- Assess signal quality: Calculate voxel-wise contrast-to-noise ratio (CNR); values less than 4 produce highly unreliable results and can falsely overestimate rCBV
- Verify arterial input function: Visually inspect the DSC signal profile in arterial regions
- Inspect for susceptibility artifacts: Look for signal dropouts in regions near air-tissue interfaces
Q2: What methods can remove technical variability after standard intensity normalization? RAVEL (Removal of Artificial Voxel Effect by Linear regression) is a specialized tool designed to remove residual technical variability after intensity normalization. Inspired by batch effect correction methods in genomics, RAVEL decomposes voxel intensities into biological and unwanted variation components, using control regions (typically cerebrospinal fluid) where intensities are unassociated with disease status [13]. In studies of Alzheimer's disease, RAVEL-corrected intensities showed marked improvement in distinguishing between MCI subjects and healthy controls using mean hippocampal intensity (AUC=67%) compared to intensity normalization alone [13].
Q3: How should I choose a functional connectivity processing pipeline to minimize variability? Based on a systematic evaluation of 768 pipelines, these criteria help identify optimal pipelines [14]:
- Minimize motion confounds and spurious test-retest discrepancies in network topology
- Maintain sensitivity to inter-subject differences and experimental effects
- Demonstrate reliability across different datasets and time intervals (minutes, weeks, months)
- Show generalizability across different acquisition parameters and preprocessing methods
Experimental Protocols for Managing Technical Variability
Protocol 1: RAVEL Implementation for Structural MRI
Purpose: Remove residual technical variability from intensity-normalized T1-weighted images [13]
Materials:
- T1-weighted MRI scans registered to common template
- Control region mask (cerebrospinal fluid)
- Computing environment with singular value decomposition (SVD) capability
Methodology:
- Perform standard intensity normalization (histogram matching or White Stripe)
- Extract voxel intensities from control region (CSF) across all subjects
- Perform singular value decomposition (SVD) of control voxels to estimate unwanted variation factors
- Estimate unwanted factors using linear regression for every brain voxel
- Use residuals from regression as RAVEL-corrected intensities
- Validate using biological positive controls (e.g., hippocampal intensity in AD vs. controls)
Protocol 2: Functional Connectivity Pipeline Validation
Purpose: Identify optimal fMRI processing pipelines that minimize technical variability while preserving biological signal [14]
Materials:
- Resting-state fMRI data with test-retest sessions
- Multiple parcellation schemes (anatomical, functional, multimodal)
- Connectivity metrics (Pearson correlation, mutual information)
- Network filtering approaches (density-based, weight-based, data-driven)
- Portrait divergence (PDiv) measure for network topology comparison
Methodology:
- Preprocessing: Apply standardized denoising (e.g., anatomical CompCor or FIX-ICA)
- Node Definition: Test multiple parcellation types (anatomical, functional, multimodal) and resolutions (100, 200, 300-400 nodes)
- Edge Definition: Calculate functional connectivity using Pearson correlation and mutual information
- Network Filtering: Apply multiple edge retention strategies (fixed density, minimum weight, data-driven)
- Evaluation: Assess each pipeline using multiple criteria:
- Test-retest reliability of network topology
- Sensitivity to individual differences
- Sensitivity to experimental manipulations
- Resistance to motion confounds
- Validation: Verify performance across independent datasets with different acquisition parameters
Table 1: Pipeline Evaluation Criteria for Functional Connectomics
| Criterion | Optimal Performance Characteristic | Measurement Approach |
|---|---|---|
| Test-Retest Reliability | Minimal portrait divergence (PDiv) between repeated scans | PDiv < threshold across short (minutes) and long-term (months) intervals |
| Individual Differences Sensitivity | Significant association with behavioral phenotypes | Correlation with cognitive measures or clinical status |
| Experimental Effect Detection | Significant topology changes with experimental manipulation | PDiv between pre/post intervention states |
| Motion Resistance | Low correlation between network metrics and motion parameters | Non-significant correlation with framewise displacement |
| Generalizability | Consistent performance across datasets | Similar reliability in independent cohorts (e.g., HCP, UK Biobank) |
Protocol 3: Quality Assurance for DSC-MRI Perfusion Imaging
Purpose: Identify and troubleshoot suboptimal DSC-MRI data for cerebral blood volume mapping [15]
Materials:
- DSC-MRI sequences (GRE-EPI recommended)
- Gadolinium-based contrast agent with power injector
- Leakage correction software (e.g., delta R2*-based model)
- Signal-to-noise and contrast-to-noise calculation tools
Methodology:
- Acquisition Protocol:
- Use gradient-echo EPI sequence with TE ≈ 30ms, TR ≈ 1250ms
- Administer preload contrast dose 5-6 minutes before DSC sequence
- Inject bolus at 3-5 mL/s approximately 60 seconds into acquisition
- Collect 30-50 baseline timepoints before bolus arrival
Quality Assessment:
- Calculate voxel-wise SNR and temporal SNR across the brain
- Compute contrast-to-noise ratio (CNR) of concentration-time curves
- Flag datasets with CNR < 4 for careful interpretation
- Visually inspect arterial input function (AIF) signal profile
- Verify whole-brain DSC signal time-course characteristics
Post-processing:
- Apply leakage correction for T1 and T2* effects
- Use standardized normalization to white matter reference regions
- Generate relative CBV maps using established algorithms
Table 2: Troubleshooting Guide for Common DSC-MRI Issues
| Issue | Indicators | Mitigation Strategies |
|---|---|---|
| Contrast Agent Timing | AIF peak misaligned, poor bolus shape | Verify injection timing, use power injector, train staff |
| Low Signal Quality | Low CNR (<4), noisy timecourses | Check coil function, optimize parameters, ensure adequate dose |
| Leakage Effects | rCBV underestimation in enhancing lesions | Apply mathematical leakage correction, use preload dose |
| Susceptibility Artifacts | Signal dropouts near sinuses/ear canals | Adjust positioning, use shimming, consider SE-EPI sequences |
| Inadequate Baseline | Insufficient pre-bolus timepoints | Ensure 30-50 baseline volumes, adjust bolus timing |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Managing Technical Variability
| Resource | Function/Purpose | Example Applications |
|---|---|---|
| RAVEL Algorithm [13] | Removes residual technical variability after intensity normalization | Multi-site structural MRI studies, disease classification |
| Portrait Divergence (PDiv) [14] | Measures dissimilarity between network topologies across all scales | Pipeline optimization, test-retest reliability assessment |
| Control Regions (CSF) [13] | Provides reference tissue free from biological signal of interest | Estimating unwanted variation factors in RAVEL |
| Consensus DSC-MRI Protocol [15] | Standardized acquisition for perfusion imaging | Multi-site tumor imaging, treatment response monitoring |
| Multiple Parcellation Schemes [14] | Different brain region definitions for network construction | Functional connectomics, individual differences research |
| Standardized Processing Pipelines [16] | Reproducible data processing across datasets | Large-scale consortium studies, open data resources |
| Quality Metrics (SNR, CNR, tSNR) [15] | Quantifies technical data quality | Data quality control, exclusion criteria definition |
FAQs: Core Concepts and Impact
Q1: What is the "motion conundrum" in neuroimaging research? The motion conundrum describes the critical challenge where in-scanner head motion creates data quality artifacts that can be misinterpreted as genuine biological signals. This is particularly problematic in resting-state fMRI (rs‐fMRI) where excluding participants for excessive motion (a standard quality control procedure) can systematically bias the sample, as motion is related to a broad spectrum of participant characteristics such as age, clinical conditions, and demographic factors [17]. Researchers must therefore balance the need for high data quality against the risk of introducing systematic bias through the exclusion of data.
Q2: How can artifacts be mistaken for true brain signatures? Artifacts can mimic or obscure genuine neural activity because they introduce uncontrolled variability into the data [18]. For example:
- Eye blink and movement artifacts produce high-amplitude deflections in frontal electrodes, with spectral power in the delta and theta bands, which can be confused with cognitive processes [18] [19].
- Muscle artifacts generate high-frequency noise that overlaps with the beta and gamma bands, potentially masking signals related to motor activity or cognition [18] [19].
- Cardiac artifacts create rhythmic waveforms that may be mistaken for genuine neural oscillations [18]. This overlap in spectral and temporal characteristics means that without proper correction, analyses may report artifact-driven findings as novel neural phenomena [17] [18].
Q3: Why does this conundrum pose a special threat to reproducible phenotyping? Reproducible brain phenotyping relies on stable, generalizable neural signatures. Motion-related artifacts and the subsequent data exclusion practices threaten this in two key ways:
- Biased Samples: List-wise deletion of participants with high motion creates a sample that is no longer representative of the intended population. Since motion correlates with traits like age, clinical status, and executive functioning, the analyzed sample may systematically differ from the original cohort, leading to biased estimates of brain-behavior relationships [17].
- Inconsistent Signatures: The same phenotype defined in different labs may be based on differently biased samples if QC thresholds are not harmonized. Furthermore, artifacts that vary across sessions or individuals can alter the derived neural signature, reducing its reliability and cross-study validity [17] [20].
Troubleshooting Guides
Identifying Common Artifacts
Table 1: Common Physiological and Technical Artifacts
| Artifact Type | Origin | Key Characteristics in Data | Potential Misinterpretation |
|---|---|---|---|
| Eye Blink/Movement [18] [19] | Corneo-retinal potential from eye movement | High-amplitude, slow deflections; most prominent in frontal electrodes; spectral power in delta/theta bands. | Slow cortical potentials, cognitive processes like attention. |
| Muscle (EMG) [18] [19] | Contraction of head, jaw, or neck muscles | High-frequency, broadband noise; spectral power in beta/gamma ranges. | Enhanced high-frequency oscillatory activity, cognitive or motor signals. |
| Cardiac (ECG/Pulse) [18] [19] | Electrical activity of the heart or pulse-induced movement | Rhythmic, spike-like waveforms recurring at heart rate; often visible in central/temporal electrodes near arteries. | Epileptiform activity, rhythmic neural oscillations. |
| Head Motion [17] [20] | Participant movement in the scanner | Large, non-linear signal shifts; spin-history effects; can affect the entire brain volume. | Altered functional connectivity, group differences correlated with motion-prone populations (e.g., children, clinical groups). |
| Electrode Pop [18] [19] | Sudden change in electrode-skin impedance | Abrupt, high-amplitude transients often isolated to a single channel. | Epileptic spike, a neural response to a stimulus. |
| Line Noise [18] [19] | Electromagnetic interference from AC power | Persistent 50/60 Hz oscillation across all channels. | Pathological high-frequency oscillation. |
Step-by-Step QC and Mitigation Protocol
The following workflow provides a structured approach to managing data quality, from study planning to processing, to minimize the impact of motion and other artifacts.
Phase 1: QC During Study Planning [20]
- Define QC Measures: Identify a priori regions of interest (ROIs) and determine which QC measures (e.g., temporal-signal-to-noise ratio - TSNR) will best support your study's goals.
- Standardize Protocols: Develop clear, written instructions for participants to minimize head motion and for experimenters to ensure consistent procedures across all scanning sessions.
Phase 2: QC During Data Acquisition [20]
- Real-Time Monitoring: Visually inspect incoming data for obvious artifacts, gross head motion, and ensure consistent field of view across scans.
- Behavioral Logs: Meticulously record participant behavior, feedback, and any unexpected events during the scan. This contextual information is crucial for later interpretation.
Phase 3: QC Soon After Acquisition [20]
- Compute Intrinsic Metrics: Calculate basic, intrinsic quality metrics such as Signal-to-Noise Ratio (SNR) and TSNR for the entire brain and for your specific ROIs.
- Initial Inspection: Check for accurate functional-to-anatomical alignment and look for obvious spatial and temporal artifacts before proceeding to full analysis.
Phase 4: QC During Data Processing [17] [18] [20]
- Artifact Removal: Employ techniques like Independent Component Analysis (ICA) to separate and remove artifact components from EEG data. For fMRI, censoring (scrubbing) of high-motion volumes can be effective, though it may introduce missing data [17] [18].
- Account for Missing Data: When data exclusion is necessary, avoid simple list-wise deletion. Instead, use statistical techniques like multiple imputation to formally account for the missing data and reduce bias, as exclusions are often not random [17].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools and Methods for Robust Brain Phenotyping
| Tool/Method | Function | Key Consideration |
|---|---|---|
| Multiple Imputation [17] | Statistical technique to handle missing data resulting from the exclusion of poor-quality scans, reducing bias. | Preferable to list-wise deletion when data is missing not-at-random (e.g., related to participant traits). |
| Independent Component Analysis (ICA) [18] | A blind source separation method used to isolate and remove artifact components (e.g., eye, muscle) from EEG and fMRI data. | Effective for separating physiological artifacts from neural signals but requires careful component classification. |
| Path Signature Methods [21] | A feature extraction technique for time-series data (e.g., EEG) that is invariant to translation and time reparametrization. | Provides robust features against inter-user variability and noise, useful for Brain-Computer Interface (BCI) applications. |
| Computational Phenotyping Framework [22] | A systematic pipeline for defining and validating disease phenotypes by integrating multiple data sources (EHR, questionnaires, registries). | Enhances reproducibility and generalizability by using multi-layered validation against incidence patterns, risk factors, and genetic correlations. |
| Temporal-Signal-to-Noise Ratio (TSNR) [20] | A key intrinsic QC metric for fMRI that measures the stability of the signal over time. | Lower TSNR in specific ROIs can indicate excessive noise or artifact contamination, flagging potential problems for hypothesis testing. |
Advanced Methodologies & Data Presentation
Quantitative Framework for Motion Bias Assessment
The following table summarizes findings from an investigation into how quality control decisions can systematically bias sample composition in a large-scale study, demonstrating the motion conundrum empirically.
Table 3: Participant Characteristics Associated with Exclusion Due to Motion in the ABCD Study [17]
| Participant Characteristic Category | Specific Example Variables | Impact on Exclusion Odds |
|---|---|---|
| Demographic Factors | Lower socioeconomic status, specific race/ethnicity categories | Increased odds of exclusion |
| Health & Physiological Metrics | Higher body mass index (BMI) | Increased odds of exclusion |
| Behavioral & Cognitive Metrics | Lower executive functioning, higher psychopathology | Increased odds of exclusion |
| Environmental & Neighborhood Factors | Area Deprivation Index (ADI), Child Opportunity Index (COI) | Increased odds of exclusion |
Experimental Protocol for Assessing QC-Related Bias:
- Cohort: Utilize a large-scale, deeply phenotyped dataset like the Adolescent Brain Cognitive Development (ABCD) Study [17].
- Procedure: Apply a range of realistic QC procedures (e.g., varying motion scrubbing thresholds) to the neuroimaging data to generate different inclusion/exclusion conditions.
- Analysis: For each condition, use statistical models (e.g., logistic regression) to test whether the odds of a participant's exclusion are significantly predicted by a wide array of their baseline characteristics, such as demographic, behavioral, and health-related variables [17].
- Outcome: The demonstration that exclusion is systematically related to participant traits confirms that list-wise deletion introduces bias, arguing for the use of missing data handling techniques in functional connectivity analyses [17].
Troubleshooting Guides
Troubleshooting Data Sharing Barriers
Problem: A researcher cannot share the underlying data for a manuscript that has been accepted for publication because the process is too time-consuming.
- Possible Cause: The researcher lacks the dedicated time required to curate, annotate, and format the data for public consumption.
- Solution: Integrate data curation tasks into the research team's workflow from the project's outset. Utilize data management plans to predefine formats and metadata schemas, distributing preparation time across the project lifecycle [23].
Problem: A research team is uncertain if they have the legal rights to share their collected data.
- Possible Cause: Unclear data ownership policies within the institution or collaboration, or the use of data subject to third-party licensing agreements.
- Solution: Consult with your institution's legal or technology transfer office before data collection begins. Draft data sharing agreements that explicitly outline rights and responsibilities for all consortium members at the start of a project [23].
Problem: A team lacks the technical knowledge to deposit data into a public repository.
- Possible Cause: Insufficient institutional support or training for data sharing practices.
- Solution: Request tailored training programs from your institution's library or research infrastructure group. Utilize online resources and protocols from established data repositories which often provide step-by-step submission guides [23].
Problem: A researcher believes there is no incentive or cultural support within their team to share data.
- Possible Cause: A perceived lack of professional reward for data sharing and a research culture that does not prioritize open science.
- Solution: Advocate for institutional recognition of data sharing as a valuable scholarly contribution. Cite journal and funder mandates on data sharing to build a case. Start by sharing data within a controlled-access framework if full openness is a concern [23] [24].
Troubleshooting Reproducibility in Brain Phenotype Research
Problem: A brain-wide association study (BWAS) fails to replicate in an independent sample.
- Possible Cause: The study is statistically underpowered due to a small sample size. BWAS effects are typically much smaller (e.g., median |r| ~ 0.01) than previously assumed, requiring thousands of individuals for reproducible results [1].
- Solution: Prioritize large sample sizes, ideally in the thousands. Collaborate with consortia to access larger datasets. Use multivariate methods, which can offer more robust effects than univariate approaches [1].
Problem: A discovered brain signature performs well in the discovery cohort but poorly in a validation cohort.
- Possible Cause: Inflated effect sizes due to sampling variability and model overfitting to the specific discovery sample.
- Solution: Implement a rigorous validation pipeline. Derive consensus signatures using multiple, randomly selected discovery subsets from your data. Validate the final model's fit and explanatory power in completely separate, held-out cohorts [25].
Problem: The brain signature derived from one cognitive domain (e.g., neuropsychological test) does not generalize to another related domain (e.g., everyday memory).
- Possible Cause: The brain substrates for the two domains may not be identical, even if they are strongly shared.
- Solution: Develop and validate separate, data-driven signatures for each specific behavioral domain of interest. Do not assume that a signature for one cognitive measure will perfectly map to another, even if they are conceptually related [25].
Frequently Asked Questions (FAQs)
FAQ: What are the most common barriers researchers face when trying to share their data?
Survey data from health and life sciences researchers identifies several prevalent barriers [23]:
- Lack of time to prepare data (reported "usually" or "always" by 34% of researchers).
- Process complexity and the perception that sharing is "too complicated."
- Large dataset management challenges ("too many data files," "difficulty sharing large datasets").
- Unclear rights to share the data (affected 27% of respondents).
- Inadequate infrastructure and technical support (noted by 15%).
- Lack of knowledge on how to share data effectively.
- Absence of cultural incentives ("my team doesn't do it").
FAQ: Why is sample size so critical for reproducible brain-wide association studies?
Brain-behavior associations are often very weak. In large-scale studies, the median correlation between a brain feature and a behavioral phenotype is around |r| = 0.01 [1]. With typical small sample sizes (e.g., n=25), confidence intervals for these correlations are enormous (r ± 0.52), leading to effect size inflation and high replication failure rates. Only with samples in the thousands do these associations begin to stabilize and become reproducible [1].
FAQ: How can we balance ethical data sharing with the needs of open science?
This requires a "balance between ethical and responsible data sharing and open science practices" [24]. Strategies include:
- Using controlled-access repositories where data access is granted to qualified researchers under specific terms.
- Implementing robust de-identification protocols to protect participant privacy.
- Employing data use agreements to ensure responsible reuse.
- Making other research components, like code and analysis workflows, openly available to enhance reproducibility, even when the raw data itself must be protected [24].
FAQ: What is a "brain signature," and how is it different from a standard brain-behavior correlation?
A brain signature is a data-driven, multivariate set of brain regions (e.g., based on gray matter thickness) that, in combination, are most strongly associated with a specific behavioral outcome [25]. Unlike a standard univariate correlation that might link a single brain region to a behavior, a signature uses a statistical model to identify a pattern of regions that collectively account for more variance in the behavior, offering a more complete picture of the brain substrates involved.
FAQ: Our research is innovative, but we fear it will be difficult to get funded through traditional grant channels. Is this a known problem?
Yes. The current peer-review system for grants has been criticized for potentially stifling innovation. There are documented cases where research that later won the Nobel Prize was initially denied funding [26]. Reviewers, who are often competitors of the applicant, may be risk-averse and favor incremental projects with extensive preliminary data over truly novel, exploratory work [26]. This can slow the progress of transformative science.
Data Tables
Table 1: Prevalence of Perceived Data Sharing Barriers Among Researchers
| Barrier | Prevalence ("Usually" or "Always") | Mean Score (0-3 scale) |
|---|---|---|
| Lack of time to prepare data | 34% | 1.19 (Self) / 1.42 (Others) |
| Not having the rights to share data | 27% | Information Missing |
| Process is too complicated | Information Missing | High (Ranked 2nd) |
| Insufficient technical support | 15% | Information Missing |
| Team culture doesn't support it | Information Missing | High (Ranked 2nd for "Others") |
| Managing too many data files | Information Missing | High (Ranked 3rd) |
| Lack of knowledge on how to share | Information Missing | High (Ranked in Top 8) |
Source: Adapted from a survey of 143 Health and Life Sciences researchers [23]. Mean scores are from survey parts where statements were framed personally (Self) and about colleagues (Others).
Table 2: Brain-Wide Association Study (BWAS) Replicability and Sample Size
| Sample Size (n) | Median Effect Size (|r|) | Replication Outlook | Key Considerations |
|---|---|---|---|
| n = 25 (Median of many studies) | Information Missing | Very Low - High sampling variability (99% CI: r ± 0.52) leads to opposite conclusions in different samples. | Studies at this size are statistically underpowered and prone to effect size inflation [1]. |
| n = 3,928 (Large, denoised sample) | 0.01 | Improving - Strongest replicable effects are still small (~|r|=0.16). | Multivariate methods and functional MRI data tend to yield more robust effects than univariate/structural MRI [1]. |
| n = 50,000 (Consortium-level) | Information Missing | High - Associations stabilize and replication rates significantly improve. | Very large samples are necessary to reliably detect the small effects that characterize most brain-behavior relationships [1]. |
Source: Synthesized from analyses of large datasets (ABCD, HCP, UK Biobank) involving up to 50,000 individuals [1].
Experimental Protocols
Protocol: Validating a Robust Brain Signature Phenotype
Aim: To develop and validate a data-driven brain signature for a cognitive domain (e.g., episodic memory) that demonstrates replicability across independent cohorts.
Materials:
- Imaging Data: T1-weighted structural MRI scans from discovery and validation cohorts.
- Behavioral Data: Standardized cognitive test scores for the domain of interest (e.g., memory composite).
- Software: Image processing pipelines (e.g., for gray matter thickness), statistical computing software (e.g., R, Python).
Methodology:
- Discovery Phase:
- Data Processing: Process T1 images to extract whole-brain gray matter thickness maps for each subject in the discovery cohort(s) [25].
- Subset Sampling: Randomly select multiple subsets (e.g., 40 subsets of n=400) from the full discovery cohort to mitigate sampling bias [25].
- Voxel-Wise Regression: In each subset, perform a voxel-wise regression between gray matter thickness at every brain point and the behavioral outcome [25].
- Consensus Mask Creation: Generate spatial overlap frequency maps from all subsets. Define the final "consensus" signature mask by selecting brain regions that are consistently (at a high frequency) associated with the behavior [25].
- Validation Phase:
- Signature Application: Apply the consensus signature mask from the discovery phase to the held-out validation cohort. Calculate a single summary value for each subject in the validation set based on their gray matter thickness within the signature regions [25].
- Model Fit Replicability: Test the association between the signature summary value and the behavioral outcome in the validation cohort. Evaluate the consistency of model fit and its explanatory power (e.g., R²) compared to the discovery phase [25].
- Comparison with Other Models: Compare the signature model's performance against theory-based or lesion-driven models to demonstrate its superior explanatory power [25].
Workflow Diagram: Brain Signature Validation Pipeline
The Scientist's Toolkit: Research Reagent Solutions
| Resource / Solution | Function in Research |
|---|---|
| Large-Scale Neuroimaging Consortia (e.g., UK Biobank, ADNI, ABCD) | Provides the large sample sizes (n > 10,000) necessary for adequately powered, reproducible Brain-Wide Association Studies (BWAS) [1]. |
| Validated Brain Signatures | Serves as a robust, data-driven phenotypic measure that can be applied across studies to reliably investigate brain substrates of behavior [25]. |
| Data Use Agreements (DUA) | Enables secure and ethical sharing of sensitive human data, balancing open science goals with participant privacy and legal constraints [24]. |
| High-Performance Computing (HPC) & Cloud Resources | Facilitates the computationally intensive processing of large MRI datasets and the running of complex, voxel-wise statistical models [27]. |
| Structured Data Management Plan | Outlines data collection, formatting, and sharing protocols from a project's start, mitigating the time barrier to data sharing later on [23]. |
Building Robust Signatures: Methodological Advances and Practical Applications
Implementing Reproducible Processing Pipelines with C-PAC, FreeSurfer, and DataLad
A technical support guide for overcoming computational pitfalls in neuroimaging research
This technical support center provides targeted troubleshooting guides and FAQs for researchers building reproducible processing pipelines with C-PAC, FreeSurfer, and DataLad. These solutions address critical bottlenecks in computational neuroscience and drug development research where reproducible brain signatures are essential.
Troubleshooting Guides
FreeSurfer License Configuration Errors
Problem: Pipeline fails with "FreeSurfer license file not found" error, even when the --fs-license-file path is correct [28].
Diagnosis: The error often occurs within containerized environments (Docker/Singularity) where the license file path inside the container differs from the host path [28].
Solution:
- Set Environment Variable: Export
FS_LICENSEenvironment variable to point to the license file in the container's filesystem - Copy License File: Manually copy the license file to the expected container location (e.g.,
/opt/freesurfer/license.txt) during container execution - Docker Flag Verification: When using
fmriprep-docker, ensure the--fs-license-fileflag properly mounts the license file into the container
Verification Command:
C-PAC and FreeSurfer Pipeline Hanging
Problem: End-to-end surface pipeline with ABCD post-processing stalls during timeseries warp-to-template, particularly when running recon-all and ABCD surface post-processing in the same pipeline [29].
Diagnosis: Resource conflicts between FreeSurfer's recon-all and subsequent ABCD-HCP surface processing stages.
Solutions:
- Preferred Workaround: Run FreeSurfer
recon-allfirst, then ingress its outputs into C-PAC rather than running both simultaneously [29] - Alternative Approach: Cancel the stalled pipeline and restart with warm restart (preserving the Nipype working directory) [29]
- Planned Resolution: Future C-PAC versions will remove integrated
recon-all, requiring FreeSurfer outputs as input for surface analysis configurations [29]
C-PAC BIDS Validator Missing Error
Problem: Pipeline crashes with "bids-validator: command not found" when running C-PAC with input BIDS directory without --skip_bids_validator flag [29].
Solutions:
- Immediate Fix: Add
--skip_bids_validatorflag to your run command (validate BIDS data separately before processing) [29] - Alternative Approach: Use a data configuration file instead of direct BIDS directory input [29]
- Configuration Note: This affects C-PAC versions where bids-validator is missing from the container image [29]
Memory Allocation Failures in C-PAC
Problem: Pipeline crashes with memory errors, particularly when resampling scans to higher resolutions [29].
Diagnosis: Functional images, templates, and resampled outputs are all loaded into memory simultaneously, exceeding available RAM [29].
Memory Estimation Formula:
Example: 100MB uncompressed scan resampled from 3mm to 1mm (27× voxel increase) requires ~2.7GB plus system overhead [29].
Solutions:
- Increase available RAM or reduce parallel subject processing
- Process fewer subjects simultaneously (multiply estimate by number of concurrent subjects) [29]
- Adjust resampling parameters to less memory-intensive methods
DataLad Dataset Nesting Permissions
Problem: DataLad operations fail with permission errors when creating or accessing nested subdatasets [30].
Diagnosis: Python package permission conflicts or incorrect PATH configuration for virtual environments [30].
Solutions:
- Avoid using
sudofor Python package installation [30] - Use
--userflag to install virtualenvwrapper for single-user access [30] - Manually set PATH if
virtualenvwrapper.shisn't found:export PATH="/home/<USER>/.local/bin:$PATH"[30] - For persistent issues, add environment variables to shell configuration file (
~/.bashrc) [30]
Frequently Asked Questions
How do I handle version compatibility between FreeSurfer 8.0.0 and existing pipelines?
FreeSurfer 8.0.0 represents a major release with significant changes including use of SynthSeg, SynthStrip, and SynthMorph deep learning algorithms. While processing time decreases substantially (~2h vs ~8h), note that [31]:
- GPU is not required despite DL modules
- Longitudinal processing has caveats (volumetric segmentation not fully longitudinal)
- Set
FS_ALLOW_DEEP=1environment variable for version 8.0.0-beta - Known issues include csvprint utility failing on systems without Python2
What are the recommended C-PAC commands for different processing scenarios?
Table: Essential C-PAC Run Commands
| Scenario | Command | Key Flags |
|---|---|---|
| Configuration Testing | cpac run <DATA_DIR> <OUTPUT_DIR> test_config |
Generates template pipeline and data configs |
| Single Subject Processing | cpac run <DATA_DIR> <OUTPUT_DIR> participant |
--data_config_file, --pipeline_file |
| Group Level Analysis | cpac run <DATA_DIR> <OUTPUT_DIR> group |
--group_file, --data_config_file |
| Sample Data Test | cpac run cpac_sample_data output participant |
--data_config_file, --pipeline_file |
How can I inspect C-PAC crash files for debugging?
- C-PAC ≥1.8.0: Crash files are plain text—view with any text editor [29]
- C-PAC ≤1.7.2: Use
cpac crash /path/to/crash-file.pklzor enter container and usenipypecli crash crash-file.pklz[29]
What are the key differences in anatomical atlas paths between Neuroparc v0 and v1?
Several atlas paths changed in Neuroparc v1.0 (July 2020). Pipelines based on C-PAC 1.6.2a or older require configuration updates [29]:
Table: Neuroparc Atlas Path Changes
| Neuroparc v0 | Neuroparc v1 |
|---|---|
aal_space-MNI152NLin6_res-1x1x1.nii.gz |
AAL_space-MNI152NLin6_res-1x1x1.nii.gz |
brodmann_space-MNI152NLin6_res-1x1x1.nii.gz |
Brodmann_space-MNI152NLin6_res-1x1x1.nii.gz |
desikan_space-MNI152NLin6_res-1x1x1.nii.gz |
Desikan_space-MNI152NLin6_res-1x1x1.nii.gz |
schaefer2018-200-node_space-MNI152NLin6_res-1x1x1.nii.gz |
Schaefer200_space-MNI152NLin6_res-1x1x1.nii.gz |
How does fMRIPrep 25.0.0 improve pre-computed derivative handling?
fMRIPrep 25.0.0 (March 2025) substantially improves support for pre-computed derivatives with the recommended command [32]:
Multiple derivatives can be specified (e.g., anat=PRECOMPUTED_ANATOMICAL_DIR func=PRECOMPUTED_FUNCTIONAL_DIR), with last-found files taking precedence [32].
Experimental Protocols & Workflows
Protocol 1: Multi-Software Validation for Skull-Stripping
Purpose: Assess analytical flexibility by comparing brain extraction results across multiple tools [33].
Methodology:
- Dataset: Use standardized test dataset (ds005072 from OpenNeuro) [33]
- Tools: Apply at least two distinct skull-stripping tools (e.g., AFNI, FSL, SPM)
- Evaluation: Quantitative comparison of extracted brain volumes and spatial overlap
- Implementation: Containerize each tool to ensure version consistency [33]
Interpretation: Measure result variability attributable to tool selection rather than biological factors [33].
Protocol 2: Numerical Stability Assessment
Purpose: Evaluate pipeline robustness to computational environment variations [33].
Methodology:
- Operation Selection: Focus on mathematically complex operations (e.g., FreeSurfer skull-stripping) [33]
- Environment Variation: Execute identical pipeline across different OS, compiler versions, and libraries
- Output Comparison: Quantify floating-point differences in resulting files
- Pertubation Modeling: Systematically introduce numerical variations to assess stability [33]
Significance: Determines whether environmental differences meaningfully impact analytical results [33].
Workflow Diagrams
Troubleshooting Logic for Pipeline Failures
DataLad Dataset Nesting Structure
The Scientist's Toolkit
Table: Essential Research Reagent Solutions
| Tool/Category | Specific Implementation | Function in Reproducible Research |
|---|---|---|
| Containerization | Docker, Singularity | Environment consistency across computational platforms [33] |
| Workflow Engines | Nipype, Nextflow | Organize and re-execute analytical computation sequences [33] |
| Data Management | DataLad, Git-annex | Version control and provenance tracking for large datasets [34] |
| Pipeline Platforms | C-PAC, fMRIPrep | Standardized preprocessing with reduced configuration burden [33] |
| Provenance Tracking | BIDS-URIs, DatasetLinks | Machine-readable tracking of data transformations [32] |
| Numerical Stability | Verificarlo, Precise | Assess impact of floating-point variations on results [33] |
In the quest to identify reproducible brain signatures of psychiatric conditions, a significant obstacle arises from the use of different assessment instruments across research datasets. Data harmonization—the process of integrating data from distinct measurement tools—is essential for advancing reproducible psychiatric research [10]. The bifactor model has emerged as a powerful statistical framework for this purpose, as it can parse psychopathology into a general factor (often called the p-factor) that captures shared variance across all symptoms, and specific factors that represent unique variances of symptom clusters [35]. This technical support guide provides practical solutions for implementing bifactor models to create harmonized psychiatric phenotypes, directly addressing key methodological challenges in reproducible brain signature research.
Frequently Asked Questions (FAQs)
Q1: What is the core advantage of using bifactor models for data harmonization?
Bifactor models provide a principled approach to harmonizing different psychopathology instruments by separating what is general from what is specific in mental health problems. This separation allows researchers to:
- Extract a transdiagnostic p-factor that represents shared liability to psychopathology across different instruments [35]
- Obtain specific factors (e.g., internalizing, externalizing) that capture unique variance beyond the general factor [10]
- Account for measurement differences between instruments while isolating substantive constructs of interest
- Enable more precise mapping of brain-behavior relationships by distinguishing shared from unique psychopathological dimensions
Q2: How do I select appropriate indicators for a harmonized bifactor model?
Indicator selection requires careful consideration of both theoretical and empirical factors:
- Perform semantic matching: Identify items from different instruments that measure similar constructs based on content [10]
- Balance comprehensiveness and parsimony: Models with 39-116 items have been successfully implemented, suggesting flexibility in indicator selection [35]
- Ensure content coverage: Select items that adequately represent both the general factor and the specific domains of interest
- Test multiple configurations: Empirical evidence suggests that different bifactor models using varying items often yield highly correlated p-factors (r = 0.88-0.99), providing some flexibility in indicator selection [35]
Q3: What are the key reliability indices I should report for my bifactor model?
When evaluating and reporting bifactor models, several reliability indices are essential:
Table: Key Reliability Indices for Bifactor Models
| Index Name | Purpose | Acceptable Threshold | Common Findings |
|---|---|---|---|
| Factor Determinacy | Assesses how well factor scores represent the latent construct | >0.90 for precise individual scores | Generally acceptable for p-factors, internalizing, externalizing, and somatic factors [35] |
| H Index | Measures how well a factor is defined by its indicators | >0.70 considered acceptable | Typically adequate for p-factors but variable for specific factors [35] |
| Omega Hierarchical (ωH) | Proportion of total score variance attributable to the general factor | >0.70 suggests strong general factor | Varies by model specification and instrument |
| Omega Subscale (ωS) | Proportion of subscale score variance attributable to specific factor after accounting for general factor | No universal threshold; higher values indicate more reliable specific factors | Often lower than ωH, indicating specific factors may capture less reliable variance |
Q4: How can I assess whether my harmonized model is successful?
Successful harmonization requires evidence from multiple assessment strategies:
- Model fit indices: Acceptable global model fit (e.g., CFI > 0.90, RMSEA < 0.08) [10]
- Measurement invariance: Test whether the factor structure holds across different instruments, demographics, and clinical characteristics [35]
- Authenticity assessment: Calculate correlations between factor scores from harmonized (limited item) models and original (full item) models [10]
- Criterion validity: Examine whether factors predict relevant external variables (e.g., daily life functioning, treatment response)
Q5: What are the most common specific factors that demonstrate adequate reliability?
Research using the Child Behavior Checklist has identified several specific factors that consistently show adequate reliability in bifactor models:
Table: Reliability Patterns of Specific Factors in Bifactor Models
| Specific Factor | Reliability Profile | Clinical Relevance |
|---|---|---|
| Internalizing | Generally acceptable reliability in most models [35] | Captures distress-based disorders (anxiety, depression) |
| Externalizing | Generally acceptable reliability in most models [35] | Captures behavioral regulation problems (ADHD, conduct problems) |
| Somatic | Generally acceptable reliability in most models [35] | Reflects physical complaints without clear medical cause |
| Attention | Consistently predicts symptom impact in daily life [35] | Particularly relevant for ADHD and cognitive dysfunction |
| Thought Problems | Variable reliability across studies | May relate to psychotic-like experiences |
Troubleshooting Guides
Problem: Poor Factor Determinacy for Specific Factors
Symptoms:
- Specific factor scores correlate weakly with theoretical constructs they purport to measure
- Low H indices for specific factors (<0.70)
- Specific factors fail to predict relevant external criteria
Solutions:
- Review indicator selection: Ensure adequate number of strong indicators for each specific factor
- Check factor intercorrelations: If specific factors are highly correlated, consider whether a different model structure might be more appropriate
- Assess instrument limitations: Some instruments may not provide adequate coverage of specific domains—consider supplementing with additional measures
- Report transparency: Clearly communicate limitations of specific factors with low determinacy and interpret findings cautiously
Problem: Measurement Non-Invariance Across Instruments
Symptoms:
- Significant deterioration in model fit when constraining factor loadings across instruments
- Different factor structures emerge for different assessment tools
- Meaningful differences in factor scores attributable to instrument rather than underlying construct
Solutions:
- Test for partial invariance: Identify which specific items show non-invariance and consider whether they can be excluded without compromising content validity [10]
- Use alignment optimization: Modern methods can estimate approximate invariance even when exact invariance doesn't hold
- Apply instrument correction: Include method factors to account for systematic variance associated with particular instruments
- Report differential functioning: Clearly document any instrument-related differences and consider them in interpretation
Problem: Low Authenticity Between Harmonized and Original Models
Symptoms:
- Low correlations (<0.70) between factor scores from harmonized models and original full-item models
- Large differences (>0.5 z-score) in factor scores between harmonized and original models for substantial portions of participants (e.g., >20%)
Solutions:
- Optimize item selection: Focus on items with strongest loadings in original models when creating harmonized versions [10]
- Assess impact strategically: Research shows p-factors typically show high authenticity (>0.89), while specific factors show more variable authenticity (0.12-0.81)—prioritize accordingly based on research questions [10]
- Consider sample-specific calibration: When possible, collect supplemental data to establish crosswalk between harmonized and original scores
- Acknowledge limitations: Be transparent about the trade-offs between harmonization breadth and measurement precision
Problem: Inconsistent Associations with External Validators
Symptoms:
- Bifactor dimensions fail to predict expected external criteria (e.g., neurocognitive performance, real-world functioning)
- Discrepant patterns of association across studies or samples
Solutions:
- Verify reliability first: Ensure factors have adequate reliability before interpreting validity coefficients
- Consider hierarchical specificity: Recognize that only some specific factors (particularly attention) consistently predict daily life impact beyond the p-factor [35]
- Use appropriate statistical controls: When examining specific factors, always control for the general factor to isolate unique variance
- Test multiple external validators: Include a range of criteria to comprehensively assess construct validity
Essential Experimental Protocols
Protocol 1: Bifactor Model Specification and Testing
Purpose: To establish an appropriate bifactor model for data harmonization
Workflow:
Procedural Details:
- Item harmonization: Identify semantically similar items across instruments through expert consensus and literature review [10]
- Model specification: Define a general factor (all items load) and specific factors (theoretically coherent item subsets)
- Model estimation: Use robust estimation methods appropriate for ordinal data (e.g., WLSMV or MLR estimators)
- Fit assessment: Evaluate multiple indices: CFI (>0.90), TLI (>0.90), RMSEA (<0.08), SRMR (<0.08)
- Reliability calculation: Compute factor determinacy, H index, omega hierarchical, and omega subscale
- Invariance testing: Test configural, metric, and scalar invariance across instruments and demographic groups
- Validation: Examine associations with relevant external variables (e.g., functional impairment, treatment response)
Protocol 2: Authenticity Assessment of Harmonized Measures
Purpose: To evaluate how well harmonized models reproduce results from original full-item models
Procedural Details:
- Estimate original models: Fit established bifactor models using complete item sets for each instrument
- Estimate harmonized models: Fit bifactor models using only the harmonized item subset
- Calculate factor scores: Extract factor scores from both original and harmonized models
- Assess correlation: Compute correlations between factor scores from original and harmonized models
- Compute difference scores: Calculate absolute differences between original and harmonized factor scores
- Flag cases with differences >0.5 z-score for further inspection [10]
- Interpret impact: Consider whether observed differences meaningfully affect substantive conclusions
Research Reagent Solutions
Table: Essential Methodological Tools for Bifactor Harmonization
| Tool Category | Specific Examples | Function/Purpose |
|---|---|---|
| Statistical Software | Mplus, R (lavaan package), OpenMx | Model estimation and fit assessment |
| Reliability Calculators | Omega, Factor Determinacy scripts | Quantifying measurement precision |
| Invariance Testing Protocols | SEM Tools R package, Mplus MODEL TEST | Establishing measurement equivalence |
| Data Harmonization Platforms | Reproducible Brain Charts (RBC) initiative | Cross-study data integration infrastructure [10] [35] |
| Psychopathology Instruments | Child Behavior Checklist (CBCL), GOASSESS | Source instruments for symptom assessment [10] |
Advanced Applications in Reproducible Brain Research
Implementing robust bifactor models for psychiatric phenotyping creates crucial foundations for reproducible brain signature research. By establishing harmonized phenotypes with known reliability and validity, researchers can more effectively:
- Identify neural correlates of general versus specific psychopathology dimensions
- Distinguish shared from unique brain-behavior relationships
- Enhance reproducibility by creating standardized phenotypic measures across studies
- Facilitate large-scale consortia efforts by enabling data integration across different assessment protocols
The methodologies outlined in this guide provide essential tools for overcoming the phenotypic harmonization challenges that often undermine reproducibility in neuropsychiatric research [36].
Frequently Asked Questions & Troubleshooting Guides
This technical support resource addresses common challenges in reproducible brain-signature phenotype research, providing practical solutions grounded in recent methodological advances.
General Predictive Modeling
Q: Why does my predictive model perform well in cross-validation but fail on a separate, held-out dataset?
A: This is a classic sign of overfitting, where a model learns patterns specific to your training sample that do not generalize. A study of 250 neuroimaging papers found that performance on a true holdout ("lockbox") dataset was, on average, 13% less accurate than performance estimated through cross-validation alone [37].
- Troubleshooting Steps:
- Implement a Strict Lockbox Method: From the outset, partition your data into a training set and a completely held-out test set. The test set should be touched only once for the final model evaluation [37].
- Increase Sample Size: Brain-wide association studies (BWAS) require large samples to produce reproducible effects. Models trained on small samples (e.g., n=25) are highly susceptible to effect size inflation and failure to replicate. Samples in the thousands are often necessary for robust results [1].
- Simplify Your Model: Use regularization techniques (e.g., Lasso, Ridge) or feature selection to enforce model parsimony and reduce complexity [37].
Q: What is the difference between a correlation and a true prediction in the context of brain-behavior research?
A: Many studies loosely use "predicts" as a synonym for "correlates with." However, a true prediction uses a model trained on one dataset to generate outcomes in a novel, independent dataset. Correlation models often overfit the data and fail to generalize. Using cross-validation is a key methodological step that transforms a correlational finding into a generalizable predictive model [38].
Connectome-Based Predictive Modeling (CPM)
Q: My CPM model has low predictive power. What are potential sources of this issue and how can I address them?
A: Low predictive power can stem from several sources, including the choice of functional connectivity features, prediction algorithms, and data quality.
- Troubleshooting Steps:
- Compare Connectivity Measures: While Pearson's correlation is the most common metric, consider testing other features like accordance (for in-phase synchronization) and discordance (for out-of-phase anti-correlation). These may capture different, behaviorally relevant neural signals [39].
- Try Different Algorithms: The standard linear regression in CPM can be compared against other methods like Partial Least Squares (PLS) regression. Evidence suggests PLS regression can sometimes offer a numerical improvement in prediction accuracy, particularly for resting-state data [39].
- Validate Externally: Always test your model on at least one completely independent dataset. Internal validation (e.g., leave-one-out cross-validation) is necessary but not sufficient to prove that a model generalizes across different populations and scanning sites [39].
Q: What are the detailed steps for implementing a Connectome-Based Predictive Modeling (CPM) protocol?
A: The CPM protocol is a data-driven method for building predictive models of brain-behavior relationships from connectivity data. The workflow involves the following key steps [38]:
Table: CPM Protocol Steps
| Step | Description | Key Consideration |
|---|---|---|
| 1. Feature Selection | Identify brain connections (edges) that are significantly correlated with the behavioral measure of interest across subjects in the training set. | Use a univariate correlation threshold (e.g., p < 0.01) to select positively and negatively correlated edges. [38] [39] |
| 2. Feature Summarization | For each subject, sum the strengths of all selected positive edges into one summary score and all negative edges into another. | These summary scores represent the subject's "network strength" for behaviorally relevant networks. [38] |
| 3. Model Building | Fit a linear model (e.g., using leave-one-out cross-validation) where the behavioral score is predicted from the positive and negative network strength scores. | The output is a linear equation that can be applied to new subjects' connectivity data. [38] |
| 4. Assessment of Significance | Use permutation testing (e.g., 1000 iterations) to determine if the model's prediction performance (correlation between predicted and observed scores) is significantly above chance. | This step provides a p-value for the model's overall predictive power. [38] |
Data & Reproducibility
Q: How many participants do I need for a reproducible brain-wide association study (BWAS)?
A: The required sample size is heavily influenced by the expected effect size. Recent large-scale studies show that univariate brain-behavior associations are typically much smaller than previously thought.
Table: BWAS Sample Size and Effect Size Guidelines
| Sample Size (n) | Implications for Reproducibility | Median |r| Effect Size (Top 1%) | Recommendation |
|---|---|---|---|
| n = 25 (Median of many studies) | Very Low. High sampling variability; 99% confidence interval for an effect is r ± 0.52. Opposite conclusions about the same association are possible. | Highly Inflated | Results are likely non-reproducible. [1] |
| n = 3,928 (Large sample) | Improved. Effects are more stable, but the largest observed effects are still often inflated. | ~0.06 [1] | A minimum starting point for reliable estimation. |
| n = 32,572 (Very large sample) | High. Required for robustly characterizing the typically small effects in brain-wide association studies. | ~0.16 (Largest replicated effect) [1] | Necessary for reproducible BWAS, similar to genomics. |
Q: What open data resources are available for testing and developing predictive models?
A: Leveraging large, open datasets is crucial for building generalizable models. Key resources include:
- Reproducible Brain Charts (RBC): An open resource integrating data from 5 large studies of youth brain development (N=6,346). It provides harmonized psychiatric phenotypes and uniformly processed imaging data, shared without a data use agreement [16].
- Other Consortia: The Human Connectome Project (HCP), the ADHD-200 Consortium, and the Philadelphia Neurodevelopmental Cohort (PNC) offer large samples of imaging and behavioral data for building and testing models [38] [39].
Table: Key Resources for Predictive Modeling in Neuroimaging
| Resource Category | Example(s) | Function / Application |
|---|---|---|
| Software & Libraries | Scikit-learn, TensorFlow [37] | Provides accessible, off-the-shelf machine learning algorithms for building predictive models from neuroimaging data. |
| Computational Protocols | Connectome-Based Predictive Modeling (CPM) [38] | A specific, linear protocol for developing predictive models of brain-behavior relationships from whole-brain connectivity data. |
| Open Data Repositories | Reproducible Brain Charts (RBC), Human Connectome Project (HCP), ADHD-200, UK Biobank [38] [1] [16] | Provide large-scale, well-characterized datasets necessary for training models and testing their generalizability across samples. |
| Quality Control Tools | Rigorous denoising strategies for head motion (e.g., frame censoring) [1] | Critical data preprocessing steps to improve measurement reliability and the validity of observed brain-behavior associations. |
Sample Size and Reproducibility Relationship
The relationship between sample size and the reproducibility of a brain-wide association is fundamental. As sample size increases, the estimated effect size stabilizes and becomes less susceptible to inflation, dramatically increasing the likelihood that a finding will replicate [1].
FAQs: Conceptual Foundations and Significance
What is "precision neurodiversity," and how does it differ from traditional diagnostic approaches? Precision neurodiversity marks a paradigm shift in neuroscience, moving from pathological models to personalized frameworks that view neurological differences as adaptive variations in human brain organization. Unlike traditional categorical diagnoses (e.g., DSM-5), which group individuals based on shared behavioral symptoms, precision neurodiversity uses a data-driven approach to identify individual-specific biological subtypes. This integrates the neurodiversity movement's emphasis on neurological differences as natural human variations with precision medicine's focus on individual-level data and mechanisms [40] [41]. The goal is to understand the unique neurobiological profile of each individual to guide personalized support and interventions.
Why is personalized brain network architecture crucial for subgroup discovery in neurodevelopmental conditions? Conventional diagnostic criteria for conditions like autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) encompass enormous clinical and biological heterogeneity. This heterogeneity has obscured the discovery of reliable biomarkers and targeted treatments. Research shows that an individual's unique "neural fingerprint"—their personalized brain network architecture—can reliably predict cognitive, behavioral, and sensory profiles [40]. By analyzing this architecture, researchers can discover biologically distinct subgroups that are invisible to traditional behavioral diagnostics. For example, distinct neurobiological subtypes have been identified in ADHD (Delayed Brain Growth ADHD and Prenatal Brain Growth ADHD) that have significant differences in functional organization at the network level, despite being indistinguishable by standard criteria [40].
What are the main genetic findings supporting biologically distinct subtypes in autism? A major 2025 study analyzing over 5,000 children identified four clinically and biologically distinct subtypes of autism. Crucially, each subtype was linked to a distinct genetic profile [42]:
- The "Broadly Affected" group showed the highest proportion of damaging de novo mutations (not inherited).
- The "Mixed ASD with Developmental Delay" group was more likely to carry rare inherited genetic variants.
- The "Social and Behavioral Challenges" group had mutations in genes that become active later in childhood, suggesting biological mechanisms may emerge postnatally. These findings demonstrate that different genetic pathways can lead to clinically distinct forms of autism, which require different approaches to research and care [42].
FAQs: Methodological and Technical Execution
What are the key methodological requirements for robust personalized brain network analysis? Robust analysis requires a specific toolkit and rigorous approach:
- High-Resolution Neuroimaging: Use of functional Magnetic Resonance Imaging (fMRI) and Diffusion Tensor Imaging (DTI) to map the brain's functional and structural connectivity [40].
- Computational Modeling: Application of graph theory to quantify brain network organization, characterizing it as a set of nodes (brain regions) and edges (connections). Key metrics include clustering coefficient, path length, and centrality [40].
- Advanced Machine Learning: Employing connectome-based prediction modeling, normative modeling, and dynamic fingerprinting to characterize individual-specific neural networks and identify subgroups [40] [43].
- Large Sample Sizes: Reproducible brain-wide association studies require thousands of individuals to overcome small effect sizes and avoid replication failures. Samples in the thousands are necessary for stable, generalizable results [1].
Which experimental workflows are recommended for subgroup identification? The following workflow, derived from recent large-scale studies, provides a roadmap for reproducible subgroup discovery.
What essential reagents and computational tools are required for this research? The table below details key solutions and resources needed to establish a pipeline for precision neurodiversity research.
| Research Reagent / Tool | Function / Application | Key Considerations |
|---|---|---|
| High-Resolution MRI Scanners | Acquire structural and functional brain connectivity data. | Essential for deriving individual-specific network architecture (the "neural fingerprint") [40]. |
| SPARK / UK Biobank-scale Cohorts | Provide large-scale, deeply phenotyped datasets for analysis. | Sample sizes in the thousands are critical for reproducibility and detecting small effect sizes [42] [1]. |
| DCANBOLD Preprocessing Pipeline | Rigorous denoising of fMRI data (e.g., for head motion). | Strict denoising strategies are required to mitigate confounding factors in brain-wide association studies [1]. |
| Graph Theory Analysis Software | Quantify network topology (clustering, path length, centrality). | Provides the mathematical framework for modeling the brain as a network of nodes and edges [40]. |
| Conditional Variational Autoencoders (cVAE) | Deep generative models for synthesizing individual connectomes. | Enables data augmentation and prediction of individual therapeutic responses from baseline characteristics [40]. |
Troubleshooting Guides: Overcoming Experimental Pitfalls
Challenge: Inability to replicate brain-behavior associations across studies.
- Problem: Many published brain-wide associations fail to replicate, leading to inconsistent findings.
- Solution: Increase sample size dramatically. The 2022 Nature study demonstrated that reproducible brain-wide association studies (BWAS) require thousands of individuals. At typical sample sizes (e.g., n=25), sampling variability is extreme, leading to inflated effect sizes and replication failure. As samples grow into the thousands, replication rates improve and effect size inflation decreases [1].
- Protocol: Prioritize access to large-scale datasets like the UK Biobank (N=35,735) or the ABCD Study (N=11,874). If collecting new data, plan for multi-site consortia to achieve sufficient sample power. For any analysis, explicitly report the sample size and its adequacy for detecting the effects of interest.
Challenge: High heterogeneity within diagnosed groups obscures meaningful subgroups.
- Problem: Standard diagnoses (e.g., "ASD") encompass individuals with vastly different biological and clinical profiles, making it impossible to find a single unifying biomarker or mechanism.
- Solution: Adopt a "person-centered" clustering approach before seeking biological explanations. Do not search for a biological explanation that encompasses all individuals with a given diagnosis. Instead, first decompose the phenotypic heterogeneity by using computational models to group individuals based on their combinations of over 200 clinical and behavioral traits [42].
- Protocol: As in the Troyanskaya et al. (2025) study, use unsupervised machine learning on a broad range of traits (social, behavioral, developmental, psychiatric) to define initial data-driven subgroups. Only after establishing clinically meaningful subgroups should you interrogate their distinct genetic and neurobiological underpinnings [42].
Challenge: Inability to distinguish between correlation and causation in brain network findings.
- Problem: Identified brain network differences may be consequences of other factors (e.g., medication, co-occurring conditions) rather than core to the neurodivergent phenotype.
- Solution: Integrate genetic data to hypothesize causal pathways. Link the personalized brain network profiles to specific genetic variations to move beyond correlation. For instance, the finding that one autism subtype had a high burden of de novo mutations while another was enriched for rare inherited variants suggests distinct causal, biological narratives for each subgroup [42].
- Protocol: For defined subgroups, perform genetic analyses to identify associated variants (e.g., de novo mutations, rare inherited variants). Then, map these genetic findings to the affected biological pathways and their predicted impact on brain development and network formation across the lifespan.
Challenge: Ethical implementation and community acceptance of subgrouping.
- *Problem: * Subgrouping research could be misused to stigmatize or withhold services from certain individuals.
- Solution: Embed the research within the neurodiversity framework and ensure community participation. The neurodiversity movement redefines neurodevelopmental conditions as adaptive variations and emphasizes the rights and value of neurodivergent people [44] [41]. Successful translation requires overcoming challenges related to ethical implementation and community participation [40].
- Protocol: Collaborate closely with autistic and neurodivergent people throughout the research process to increase the face validity of concepts and methodologies. Frame the goal of subgrouping not as a search for "defects" but as a way to understand different neurotypes to provide more tailored support and create more favorable social and environmental conditions [41].
Technical FAQs: Addressing Core Methodological Challenges
FAQ 1: What does the Brain Age Gap (BAG) actually represent in a developmental population? The Brain Age Gap (BAG) represents the deviation between an individual's predicted brain age and their chronological age. In children and adolescents, a positive BAG (where brain age exceeds chronological age) is often interpreted as accelerated maturation, while a negative BAG suggests delayed maturation [45]. However, interpreting BAG is complex in youth due to the dynamic, non-linear nature of brain development. Different brain regions mature at different rates; for example, subcortical structures like the amygdala mature earlier than the prefrontal cortex. A global BAG score might average out these regional variations, potentially overlooking important neurodevelopmental nuances [45].
FAQ 2: Why is my brain age model inaccurate when applied to a new dataset? A primary reason is age bias, a fundamental statistical pitfall in brain age analysis. Brain age models inherently show regression toward the mean, meaning older individuals tend to have negative BAGs and younger individuals positive BAGs, on average [46]. This makes the BAG dependent on chronological age itself. Consequently, any observed group differences in BAG could be artifactual, stemming from differences in the age distributions of the groups rather than true biological differences [46] [47]. Applying a model trained on one age range to a population outside that range (e.g., an adult-trained model on children) exacerbates this issue [45].
FAQ 3: How can I improve the reproducibility and real-world utility of my brain age model? To enhance reproducibility, adopt standardized evaluation frameworks like the Brain Age Standardized Evaluation (BASE) [48]. This involves:
- Using multi-site, test-retest, and longitudinal datasets for robust training and validation.
- Repeated model training and evaluation on a comprehensive set of performance metrics.
- A statistical evaluation framework using linear mixed-effects models for rigorous comparison. Furthermore, while multimodal models (using multiple MRI sequences or data types) often achieve the highest prediction accuracy, this does not always translate to superior clinical utility for all phenotypes. In some cases, unimodal models may be equally or more sensitive to specific conditions [49].
FAQ 4: What are the key pitfalls in relating BAG to cognitive or clinical outcomes in youth? The relationship between BAG and cognition in youth is inconsistent, with studies reporting positive, negative, or no correlation [45]. This ambiguity arises from:
- Variability in cognitive measures (e.g., composite batteries vs. specific tasks).
- Differences in model features and sample characteristics.
- The dynamic nature of development, where the same BAG might have different implications at different ages. For clinical translation, BAG must be validated against age- and sex-specific reference charts from large, harmonized cohorts. Its incremental validity over established clinical and demographic predictors must be demonstrated before it can be used as an individual-level biomarker [45].
Troubleshooting Guides
Troubleshooting Model Validity and Biological Interpretation
| Symptom | Potential Cause | Solution |
|---|---|---|
| BAG is strongly correlated with chronological age in your sample. | The inherent age bias (regression toward the mean) in BAG estimation [46]. | Statistically adjust for age dependence using bias-correction methods. However, be aware that some corrections can artificially inflate model accuracy metrics [46] [47]. |
| BAG shows no association with a clinical outcome of interest. | The brain age model may lack clinical validity. The BAG might not be a proxy for the underlying biological aging process you are investigating [50]. | Validate that your BAG marker is prognostic. Test if baseline BAG predicts future clinical decline or brain atrophy in longitudinal analyses [50]. |
| Inconsistent BAG findings across different mental health disorders. | BAG is a global summary metric that may obscure disorder-specific regional patterns of maturation or atrophy [45]. | Consider supplementing the global BAG with regional brain age assessments or other more localized neuroimaging biomarkers. |
| Model performs poorly on data from a new scanner or site. | Scanner and acquisition differences introducing site-specific variance that the model cannot generalize across [45] [48]. | Use harmonization tools (e.g., ComBat) during pre-processing. Train and test your model on multi-site datasets, and explicitly evaluate its performance on "unseen site" data [48]. |
Guide: Mitigating Age Bias in Brain Age Gap Analysis
A critical step for robust analysis is to account for the spurious correlation between the Brain Age Gap (BAG) and chronological age. The following workflow outlines this mitigation strategy.
Title: Age Bias Correction Workflow
Procedure:
- Calculate Initial BAG: Compute the raw brain age gap as
BAG_raw = Predicted Brain Age - Chronological Age[46]. - Perform Linear Regression: Fit a linear model with
BAG_rawas the dependent variable andChronological Ageas the independent variable. This models the unwanted age-dependent variance [46] [47]. - Extract Residuals: The residuals from this regression become your age-adjusted BAG. This metric is statistically orthogonal to chronological age and should be used in all subsequent analyses relating BAG to other variables or group status [46].
- Interpret with Caution: Note that while this correction mitigates age-confounding, it can artificially inflate model accuracy statistics (like R²), so reported metrics should be interpreted with this in mind [46] [47].
Experimental Protocols & Data Presentation
Standardized Protocol for Brain Age Model Evaluation
For reproducible brain age research, adhering to a standardized evaluation protocol is crucial. The following diagram outlines the key stages of the BASE framework [48].
Title: BASE Evaluation Framework
Detailed Methodology [48]:
- Data Curation: Assemble a standardized dataset that includes multi-site data (to test generalizability), test-retest data (to assess reliability), and longitudinal data (to track within-subject changes). Data should be curated in Brain Imaging Data Structure (BIDS) format.
- Evaluation Protocol: Implement repeated model training (e.g., via k-fold cross-validation) to ensure stable performance estimates.
- Comprehensive Metrics:
- Accuracy: Mean Absolute Error (MAE) is the primary metric, quantifying the average absolute difference between predicted and chronological age.
- Robustness: Evaluate the model on data from an entirely unseen site or scanner to test real-world generalizability.
- Reproducibility: Calculate the intra-class correlation (ICC) or coefficient of variation (CoV) from test-retest data.
- Statistical Framework: Use linear mixed-effects models for the final performance assessment, which can account for nested data structures (e.g., multiple scans per subject, subjects from different sites).
Quantitative Comparison of Brain Age Studies and Modalities
The table below summarizes key quantitative findings from recent brain age studies, highlighting performance across modalities and populations.
Table 1: Comparison of Brain Age Prediction Model Performance
| Study / Model | Population / Focus | Modality | Key Performance Metric | Primary Finding / Utility |
|---|---|---|---|---|
| BASE Framework [48] | Multi-site, Test-Retest, Longitudinal | T1-weighted MRI | MAE: ~2-3 years (Deep Learning) | Established a standardized evaluation protocol for reproducible brain age research. |
| Deep-learning Multi-modal [51] | Alzheimer's Disease Cohorts (Adults) | T1-weighted MRI + Demographics | MAE: 3.30 years (CN adults) | A multi-modal framework that also predicted cognitive status (AUC ~0.95) and amyloid pathology. |
| Systematic Review (Pediatric) [52] | Children (0-12 years) | MRI, EEG | N/A (Review) | Kernel-based algorithms and CNNs were most common. Prediction accuracy may improve with multiple modalities. |
| Public Package Comparison [50] | Cognitive Normal, MCI, Alzheimer's (Adults) | T1-weighted MRI (6 packages) | N/A | Brain age differed between diagnostic groups, but had limited prognostic validity for clinical progression. |
| Multimodal Systematic Review [49] | Chronic Brain Disorders | Multi-modal vs. Uni-modal MRI | N/A (Review) | Multimodal models were most accurate and sensitive to brain disorders, but unimodal fMRI models were often more sensitive to a broader array of phenotypes. |
Abbreviations: MAE (Mean Absolute Error), CNN (Convolutional Neural Network), MCI (Mild Cognitive Impairment), CN (Cognitively Normal), AUC (Area Under the Curve).
The Scientist's Toolkit
Table 2: Essential Research Reagents & Computational Solutions
| Item / Resource | Type | Function / Application |
|---|---|---|
| Public Brain Age Packages (e.g., brainageR, DeepBrainNet) [50] | Software Package | Pre-trained models that allow researchers to extract brain age estimates from structural MRI data without training a new model from scratch. |
| Standardized Evaluation Framework (BASE) [48] | Code/Protocol | Provides a reproducible pipeline and metrics for fairly comparing different brain age prediction models. |
| Harmonized Neurodevelopmental Datasets (e.g., ADNI, OASIS, IXI) [51] [52] | Data | Large-scale, often public, datasets that are essential for training robust models and for external validation. |
| Data Harmonization Tools (e.g., ComBat) | Statistical Tool | Algorithms used to remove site-specific effects (scanner, protocol) from multi-site neuroimaging data, improving generalizability [45] [48]. |
| Bias-Adjustment Scripts | Statistical Code | Code for performing the age-bias correction, a critical step to avoid spurious correlations in downstream analyses [46] [47]. |
| Multi-modal Integration Framework [51] | Model Architecture | A deep-learning framework capable of integrating 3D MRI data with demographic/clinical variables (e.g., sex, APOE genotype) for improved prediction. |
Troubleshooting and Optimization: A Guide to Mitigating Pitfalls
In reproducible brain signature phenotype research, a major challenge is the presence of unwanted technical variation in data collected across different scanners, sites, or protocols. These technical differences, known as batch effects, can confound true biological signals and compromise the validity and generalizability of research findings [53]. Statistical harmonization techniques are designed to remove these batch effects, allowing researchers to combine datasets and increase statistical power while preserving biological variability of interest. This technical support center provides guidance on implementing these methods effectively.
Foundational Concepts: FAQs on Harmonization
What are batch effects in neuroimaging? Batch effects are technical sources of variation introduced due to differences in data acquisition. In multi-site neuroimaging studies, these can arise from using different scanner manufacturers, model types, software versions, or acquisition protocols [53]. If not corrected, they can introduce significant confounding and lead to biased results and non-reproducible findings.
Why is statistical harmonization critical for brain-wide association studies (BWAS)? Brain-wide association studies often investigate subtle brain-behaviour relationships. Recent research demonstrates that these associations are typically much smaller (median |r| ≈ 0.01) than previously assumed, requiring sample sizes in the thousands for robust detection [1]. Batch effects can easily obscure these small effects. Harmonization reduces non-biological variance, thereby enhancing the statistical power and reproducibility of these studies [1].
What is the difference between statistical and deep learning harmonization methods? Statistical harmonization methods, such as ComBat and its variants, operate on derived features or measurements (e.g., regional brain volumes) to adjust for batch effects using statistical models [53] [54]. Deep learning harmonization methods, such as DeepHarmony and HACA3, are image-based and use neural networks to translate images from one acquisition protocol to another, creating a consistent set of images for subsequent analysis [54].
Troubleshooting Guide: Common Harmonization Scenarios
Scenario 1: Inconsistent Results After Multi-Site Data Pooling
- Symptoms: Strong site or scanner effects are visible in data visualizations (e.g., PCA plots); statistical models identify "site" as a highly significant predictor, overshadowing biological variables of interest.
- Root Cause: The data contain significant batch effects that have not been adequately corrected before analysis [53].
- Resolution:
- Diagnose: Conduct an exploratory data analysis to visualize and quantify the batch effects. A Principal Component Analysis (PCA) plot coloured by site or scanner is an effective diagnostic tool.
- Choose a Method: Select an appropriate harmonization technique. For feature-level data (e.g., cortical thickness values), use a statistical method like neuroCombat [54]. For raw image data, consider an image-based method like HACA3 or DeepHarmony [54].
- Apply and Validate: Apply the chosen harmonization method and then repeat the diagnostic visualization to confirm the reduction of batch-related clustering.
Scenario 2: Failed Replication of a Previously Identified Brain Signature
- Symptoms: A brain-phenotype association identified in one dataset fails to replicate in another, even when the cohorts are demographically similar.
- Root Cause: The association in the original study may have been inflated by sampling variability (a common issue in small-sample studies), or the replication attempt may be confounded by unaccounted-for acquisition differences between the two datasets [1].
- Resolution:
- Power Assessment: Ensure that the sample size for the replication attempt is sufficient to detect the expected effect size. BWAS often requires thousands of individuals for replicable results [1].
- Retrospective Harmonization: Apply harmonization techniques to the combined original and replication datasets to remove systematic differences between them before re-running the association analysis [53].
- Check Measurement Reliability: Low reliability of the imaging measures (e.g., functional connectivity) can attenuate observed effect sizes. Use reliability metrics to assess data quality [1].
Scenario 3: Choosing Between Harmonization Methods
- Symptoms: Uncertainty about whether to use a statistical method like ComBat or a deep learning-based method for a new study.
- Root Cause: Each method has distinct strengths, weaknesses, and data requirements [54].
- Resolution: Use the following table to guide method selection based on your data and research goals.
Scenario 4: Loss of Biological Signal After Harmonization
- Symptoms: After harmonization, the biological signal of interest (e.g., a disease effect) appears weakened or removed.
- Root Cause: Overly aggressive harmonization can sometimes remove meaningful biological variance if it is correlated with batch [53].
- Resolution:
- Use Preserved Variables for Validation: When applying harmonization, use variables known a priori to be unaffected by the experimental condition (e.g., age effects in a control group) to validate that biological signals are preserved.
- Incorporate Biological Covariates: Many harmonization methods allow for the inclusion of biological covariates (e.g., age, sex) in the model to protect these signals during the batch effect removal process [53].
- Compare Methods: Try multiple harmonization methods and compare their performance on validation metrics to select the one that best preserves the known biological effect.
Quantitative Comparison of Harmonization Techniques
The following tables summarize findings from a 2025 evaluation study that compared the performance of neuroCombat, DeepHarmony, and HACA3 on T1-weighted MRI data [54].
- Table 1: Performance in Achieving Volumetric Consistency This table compares the ability of each method to reduce measurement variation across two different acquisition protocols (GRE and MPRAGE) in regions of the brain.
| Brain Region | Unharmonized AVDP | neuroCombat AVDP | DeepHarmony AVDP | HACA3 AVDP |
|---|---|---|---|---|
| Cortical Gray Matter | >5% | 3-5% | 2-4% | <2% |
| Hippocampus | >8% | 4-6% | 3-5% | <2% |
| White Matter | >4% | 3-4% | 2-3% | <1.5% |
| Ventricles | >7% | 4-6% | 3-5% | <2% |
Abbreviation: AVDP, Absolute Volume Difference Percentage. [54]
- Table 2: Overall Method Performance Metrics This table provides a high-level summary of key performance indicators from the same study.
| Performance Metric | neuroCombat | DeepHarmony | HACA3 |
|---|---|---|---|
| Overall AVDP (Mean) | Higher | Moderate | Lowest (<3%) |
| Coefficient of Variation (CV) Agreement | Moderate | Good | Best (Mean diff: 0.12) |
| Intra-class Correlation (ICC) | Good (ICC >0.8) | Good (ICC >0.85) | Best (ICC >0.9) |
| Atrophy Detection Accuracy | Good (with training) | Improved | Best |
| Key Limitation | Requires careful parameter tuning; may not detect subtle changes without training data. | Requires paired image data for supervised training. | Complex implementation. |
Experimental Protocols & Workflows
Protocol 1: Standardized Data Preprocessing for Harmonization
Effective harmonization requires a consistent preprocessing foundation. A typical workflow for T1-weighted structural images is as follows [54]:
- Format Conversion: Convert raw DICOM images to the NIfTI-1 file format for compatibility with neuroimaging software tools.
- Inhomogeneity Correction: Apply the N4ITK algorithm to correct for low-frequency intensity non-uniformity (bias field) caused by scanner imperfections.
- Spatial Registration: For studies involving multiple image types per subject, perform a rigid registration (e.g., using ANTs or FSL FLIRT) to align all images to a common space within the subject.
- Skull Stripping: Remove non-brain tissue from the images.
- Tissue Segmentation: Use automated tools (e.g., FSL FAST, FreeSurfer, or SAMSEG) to segment the brain into gray matter, white matter, and cerebrospinal fluid.
- Feature Extraction: Derive quantitative features, such as regional cortical thickness or volumetric measures, for statistical harmonization.
The following diagram illustrates the key decision points in selecting and applying a harmonization method.
Protocol 2: Implementing neuroCombat for Volumetric Data
This protocol outlines the steps for applying the neuroCombat tool to harmonize regional brain volume measures across multiple sites [54].
- Input Data Preparation: Compile a data matrix (features × samples). The rows are the brain region volumes (e.g., hippocampal volume, cortical gray matter volume) for each subject. The columns are the different subjects across all batches (sites/scanners).
- Covariate Collection: Create a design matrix that includes biological covariates of interest (e.g., age, sex, diagnosis) that should be preserved.
- Batch Definition: Define a batch variable that indicates the site or scanner for each subject.
- Model Fitting: Run the neuroCombat algorithm, specifying the data matrix, batch variable, and biological covariates.
- Output: The algorithm returns a harmonized data matrix where the mean and variance of each feature have been adjusted to remove batch effects.
The Scientist's Toolkit: Research Reagent Solutions
The following table lists key software tools and resources essential for conducting statistical harmonization in neuroimaging research.
| Tool / Resource | Type | Primary Function | Application Context |
|---|---|---|---|
| neuroCombat [54] | Statistical R/Python Package | Removes batch effects from feature-level data using an empirical Bayes framework. | Harmonizing derived measures (volumes, thickness) in multi-site studies. |
| HACA3 [54] | Deep Learning Model | Unsupervised image-to-image translation for harmonizing raw MRI data to a common protocol. | Generating a consistent set of images when a single target protocol is desired. |
| DeepHarmony [54] | Deep Learning Model | Supervised image-to-image translation using a U-Net architecture to map images to a target contrast. | Harmonizing images when paired data (source and target protocol) is available. |
| Reproducible Brain Charts (RBC) [16] | Data Resource | An open resource providing harmonized neuroimaging and phenotypic data from multiple developmental studies. | Accessing a pre-harmonized, large-scale dataset for developmental neuroscience. |
| ABCD, UKB, HCP [1] | Data Resources | Large-scale, multi-site neuroimaging datasets that are often used for developing and testing harmonization methods. | Serving as benchmark or training data for harmonization algorithms. |
| ANTs [54] | Software Library | A comprehensive toolkit for medical image registration and segmentation. | Preprocessing steps such as spatial normalization and tissue segmentation. |
In brain signature phenotype research, quality control is not merely a procedural formality but the foundational element that determines the validity and reproducibility of scientific findings. The field faces a critical challenge: predictive brain-phenotype models often fail for individuals who defy stereotypical profiles, revealing how biased phenotypic measurements can limit practical utility [55]. This technical support center provides actionable guidance to overcome these pitfalls through rigorous QC frameworks that ensure brain signatures serve as robust, reliable biomarkers. The implementation of these protocols requires understanding both the statistical underpinnings of quality metrics and the practical troubleshooting approaches that address real-world experimental challenges.
Core Principles of Quality Control in Research
Defining Quality Control and Its Components
Quality control represents a systematic approach to ensuring research outputs meet specified standards through testing and inspection, while quality assurance focuses on preventing quality issues through process design and standardization [56].
- Quality Control Process: The overarching framework that ensures quality is maintained at every stage—from raw materials to final deliverables. It encompasses setting standards, implementing inspection methods, training employees, monitoring performance, and continuous improvement [57].
- Quality Control Procedures: Specific, repeatable actions within the overall QC process, such as standardized inspection protocols, calibration procedures, and data validation checks [57].
- Quality Assurance: The proactive processes that prevent quality issues through systematic activities including process design, standardization, and long-term improvement plans [56].
Essential QC Metrics and Statistical Foundations
Effective quality control relies on quantitative metrics that provide objective assessment of research quality. The Six Sigma methodology offers a world-class quality standard that is particularly valuable for high-impact research applications [58].
Table 1: Sigma Metrics and Corresponding Quality Levels
| Sigma Level | Defects Per Million | Quality Assessment |
|---|---|---|
| 1σ | 690,000 | Unacceptable |
| 2σ | 308,000 | Unacceptable |
| 3σ | 66,800 | Minimum acceptable |
| 4σ | 6,210 | Good |
| 5σ | 230 | Very good |
| 6σ | 3.4 | Excellent |
Sigma metrics are calculated using the formula: σ = (TEa - bias) / CV%, where TEa represents the total allowable error, bias measures inaccuracy, and CV% (coefficient of variation) measures imprecision [58]. For brain phenotype research, a sigma value of 3 is considered the minimum acceptable level, with values below 3 indicating unstable processes that require immediate corrective action [58].
Implementing QC Protocols: A Step-by-Step Framework
QC Planning and Design
The purpose of QC planning is to select procedures that deliver required quality at minimum cost. This requires designing QC strategies on a test-by-test basis, considering the specific quality requirements for each experimental outcome [59].
- Define Quality Requirements: Establish standards based on clinical or analytical needs, such as medically important changes or analytical quality requirements [59].
- Assess Method Performance: Estimate bias and imprecision from initial evaluation studies or ongoing QC results [59].
- Select Appropriate Control Rules: Utilize quantitative planning tools like OPSpecs charts to identify control rules and the number of control measurements needed [59].
- Develop Total QC Strategy: Balance statistical QC with non-statistical components including preventive maintenance, instrument checks, and validation tests [59].
Practical Implementation Guide
Proper implementation transforms QC plans into actionable protocols:
- Control Material Selection: Choose materials that monitor critical decision levels and working ranges. Most applications require two levels of controls, though hematology and coagulation tests often need three [59].
- Establish Baseline Performance: Analyze control materials to obtain a minimum of 20 measurements over 10-20 days to characterize actual method performance [59].
- Calculate Statistics and Control Limits: Determine mean and standard deviation of control measurements, then establish control limits. Use laboratory-derived values rather than manufacturer specifications [59].
- Document Procedures: Prepare written guidelines detailing when and how many control samples to analyze, their placement in analytical runs, interpretation criteria, and corrective actions for out-of-control situations [59].
Diagram 1: QC Implementation Workflow. This process ensures systematic establishment of reliable quality control protocols.
Troubleshooting Guides: Addressing QC Failures
Systematic Troubleshooting Methodology
When experiments produce unexpected results, follow a structured approach to identify root causes [60]:
- Repeat the Experiment: Unless cost or time prohibitive, repetition may reveal simple mistakes in execution [61].
- Verify Experimental Failure: Consider whether alternative scientific explanations exist for unexpected results before assuming protocol failure [61].
- Validate Controls: Ensure appropriate positive and negative controls are in place. Positive controls verify the experimental system works, while negative controls identify contamination or background signals [61].
- Inspect Equipment and Materials: Check for proper storage conditions, expiration dates, and potential degradation of reagents [61].
- Change Variables Systematically: Isolate and test one variable at a time to identify contributing factors [61].
Advanced Troubleshooting: The Pipettes and Problem Solving Approach
For complex research scenarios, formal troubleshooting frameworks like "Pipettes and Problem Solving" provide structured methodologies [62]:
- Scenario Presentation: An experienced researcher presents a hypothetical experiment with unexpected outcomes.
- Group Investigation: Participants ask specific questions about experimental conditions and potential confounding factors.
- Consensus Experimentation: The group proposes a limited number of experiments to identify problem sources.
- Iterative Refinement: Based on mock results from proposed experiments, the group refines hypotheses until reaching consensus on the root cause [62].
This approach teaches fundamental troubleshooting skills including proper control usage, hypothesis development, and analytical technique refinement [62].
Diagram 2: Troubleshooting Decision Tree. A structured approach to identifying and resolving experimental quality issues.
QC in Brain Phenotype Research: Special Considerations
Addressing Model Failure in Heterogeneous Populations
Brain-phenotype models frequently fail when applied to individuals who defy stereotypical profiles, revealing significant limitations in one-size-fits-all modeling approaches [55]. This structured failure is reliable, phenotype-specific, and generalizable across datasets, indicating that models often represent neurocognitive constructs intertwined with sociodemographic and clinical covariates rather than unitary phenotypes [55].
Strategies to mitigate biased model performance:
- Validate Across Diverse Populations: Ensure representation across demographic, clinical, and socioeconomic spectra in both discovery and validation cohorts.
- Test for Structured Failure: Actively assess whether models perform differently across population subgroups.
- Incorporate Covariate Awareness: Explicitly account for potential confounding factors during model development.
- Implement Continuous Monitoring: Establish ongoing QC procedures to detect performance degradation when applied to new populations.
Validation of Brain Signatures as Robust Phenotypes
The validation of brain signatures requires demonstrating both model fit replicability and consistent spatial selection of signature regions across multiple independent datasets [25]. Key validation components include:
- Cross-Dataset Generalization: Test signature performance in completely independent cohorts not used in discovery.
- Spatial Reproducibility: Assess whether signature regions converge across different discovery datasets.
- Outcome Prediction Accuracy: Evaluate whether signatures explain significant variance in target phenotypes beyond chance levels.
- Comparative Performance: Benchmark against theory-driven or lesion-based approaches to demonstrate added value [25].
Table 2: QC Metrics for Brain Phenotype Research Validation
| Validation Metric | Assessment Method | Acceptance Criteria |
|---|---|---|
| Model Fit Replicability | Correlation of fits in validation subsets | r > 0.8 with p < 0.05 |
| Spatial Extent Reproducibility | Overlap frequency maps | >70% regional consistency |
| Cross-Dataset Generalization | Performance in independent cohorts | >80% maintained accuracy |
| Phenotype Specificity | Misclassification frequency correlation | Logical organization by cognitive domain |
Essential Research Reagent Solutions
Table 3: Key Research Reagents for QC in Brain Phenotype Studies
| Reagent/Category | Function | QC Application |
|---|---|---|
| Control Materials (Bio-Rad) | Internal quality monitoring | Daily performance verification [58] |
| Standard Reference Materials (NIST) | Method calibration | Establishing measurement traceability |
| Pooled QC Samples | Process variability assessment | Monitoring analytical stability [63] |
| System Suitability Test Mixes | Instrument performance verification | Pre-run analytical validation [63] |
| Certified Calibrators | Quantitative standardization | Ensuring measurement accuracy |
Frequently Asked Questions (FAQs)
Q1: How often should we run quality control samples in brain phenotype studies? Answer: The frequency should be determined by the sigma metric of your analytical process. For parameters with sigma >6, standard QC frequency is sufficient. For sigma 3-6, increase QC frequency. For sigma <3, take corrective action before proceeding [58]. In practice, analyze control materials with each analytical run, with at least two different control materials per CLIA regulations [59].
Q2: What are the most common causes of QC failures in experimental research? Answer: Common causes include: (1) methodological flaws in experimental design, (2) inadequate controls, (3) poor sample selection, (4) insufficient data collection methods, and (5) external variables affecting outcomes [60]. In brain phenotype research specifically, model failures often occur when individuals defy stereotypical profiles used in training [55].
Q3: How can we distinguish between random experimental error and systematic bias? Answer: Random errors appear as inconsistent variations in results, while systematic biases produce consistent directional deviations. Use control charts to identify patterns: random errors typically show scattered points outside control limits, while systematic biases manifest as shifts or trends in multiple consecutive measurements [56]. The 13s and R4s QC rules are more sensitive to random errors, whereas rules like 22s and 2of32s detect systematic errors [59].
Q4: What documentation is essential for maintaining QC compliance? Answer: Essential documentation includes: (1) Standard Operating Procedures, (2) Quality Control Manuals, (3) Inspection Records, (4) Training Materials, and (5) Audit Reports [56]. Maintain QC records for appropriate periods (typically two years), with maintenance records kept for the instrument's lifetime [59].
Q5: How do we implement effective corrective actions when QC failures occur? Answer: Follow a structured approach: (1) Identify root causes of defects using tools like Ishikawa diagrams or 5-Why analysis, (2) Implement immediate corrective measures, (3) Establish preventive actions to avoid recurrence, and (4) Document all steps taken for future reference [57] [56]. For persistent issues, consider formal troubleshooting frameworks like Pipettes and Problem Solving [62].
Frequently Asked Questions (FAQs)
1. What is dataset shift and why is it a critical problem in biomarker research? Dataset shift occurs when the statistical properties of the data used to train a predictive model differ from the data it encounters in real-world use. In biomarker research, this is critical because shifts in patient populations, clinical protocols, or measurement techniques can render a previously accurate model unreliable, directly impacting the reproducibility of brain signature phenotypes and the success of drug development programs [64] [65] [66].
2. What are the common types of dataset shift we might encounter? The main types of shift include:
- Covariate Shift: The distribution of input features (e.g., patient demographics or sample sources) changes, but the relationship between features and the target outcome remains the same [65].
- Concept Shift: The underlying relationship between the input features and the target outcome changes. For example, a biomarker's association with a disease might evolve over time [65].
- Prior Probability Shift: The distribution of the target outcomes themselves changes, such as the prevalence of a disease in a new population [66].
3. How can we proactively monitor for dataset shift in our projects? Proactive monitoring involves tracking key distributions over time and comparing them to your baseline training data. Essential aspects to monitor include [65]:
- Dataset Distribution: Shifts in clinical note sources, medical specialties, or document types.
- Entity Distribution: Changes in the ratio of key entities (e.g., the frequency of specific biomarker mentions in clinical text).
- Confidence Distribution: Fluctuations in your model's prediction confidence for different data cohorts.
4. Our model is performing poorly on new data. What is the first step in troubleshooting? The first step is to start simple. Reproduce the problem on a small, controlled subset of data. Simplify your architecture, use sensible hyper-parameter defaults, and normalize your inputs. This helps isolate whether the issue stems from the model, the data, or their interaction [67].
5. What are some statistical measures to quantitatively assess dataset shift? Two key complementary measures are the Population Stability Index (PSI) and the Population Accuracy Index (PAI) [66].
- PSI measures any change in the distribution of the input variables.
- PAI measures how this change affects the model's prognostic accuracy. Used together, they provide a comprehensive view of model stability.
Troubleshooting Guide: Diagnosing and Addressing Dataset Shift
Follow this structured guide to diagnose and remediate performance issues caused by dataset shift.
Phase 1: Detection and Assessment
Step 1: Monitor Key Distributions Continuously track the following dimensions of your incoming data against the training set baseline [65]:
- Data Source & Type: Frequency of documents from new hospitals, providers, or specialties (e.g., a shift from oncology to cardiology notes).
- Entity Ratios: Proportion of key named entities (e.g., patient names, dates, specific biomarker terms).
- Model Confidence: Statistical distribution of prediction confidence scores across different data sub-cohorts.
Step 2: Calculate Stability Metrics For a quantitative assessment, implement the following measures [66]:
- Population Stability Index (PSI): Use this to detect changes in the input feature distributions.
- Population Accuracy Index (PAI): Use this to understand the impact of distributional changes on your model's accuracy.
The table below summarizes the purpose and interpretation of these key metrics.
| Metric Name | Primary Function | Interpretation |
|---|---|---|
| Population Stability Index (PSI) [66] | Measures any change in the distribution of input variables. | A high PSI value indicates a significant shift in the data distribution that the model was not trained on. |
| Population Accuracy Index (PAI) [66] | Measures how a distribution change impacts the model's prognostic accuracy. | A low PAI value indicates that the model's predictive performance has degraded due to the shift. |
Phase 2: Remediation and Model Improvement
Step 3: Annotate and Retrain If a significant shift is detected:
- Sample Annotation: Manually annotate a representative sample from the new, shifted dataset [65].
- Retraining: Incorporate this newly annotated data into your training set and retrain the model to adapt it to the new patterns [65].
- Validation: Rigorously validate the updated model's performance on the new dataset before deployment [65].
Step 4: Implement Robust Data Practices Prevent future issues by strengthening your data pipeline:
- Handle Data Imbalance: Ensure all classes are adequately represented in training data. Use techniques like resampling or data augmentation to address imbalances that can bias models [68] [69].
- Manage Outliers: Identify and handle outliers using algorithms like Isolation Forests or by applying log transformations to prevent them from unduly influencing the model [69].
- Cross-Validation: Use cross-validation techniques to ensure your model generalizes well and is not overfitted to a specific data split [68].
The following workflow diagram illustrates the core process for maintaining model performance in the face of dataset shift.
Phase 3: Advanced Proactive Strategies
For long-term project stability, consider these advanced strategies:
- Continuous Monitoring: Implement automated systems to regularly analyze incoming data and compare it to historical baselines using statistical tests like Kolmogorov-Smirnov or the Page-Hinkley method [69].
- Adaptive Model Training: Utilize algorithms that can automatically adjust model parameters in response to detected changes in data distribution [69].
- Data Version Control: Employ systems like lakeFS to version control large datasets and model artifacts, enabling you to track changes and roll back if necessary [70].
The Scientist's Toolkit
The table below lists key reagents, software, and methodological approaches essential for experimenting with and mitigating dataset shift in biomarker research.
| Tool / Reagent | Type | Primary Function in Context |
|---|---|---|
| Apache Iceberg | Software (Data Format) | An open table format for managing large datasets in data lakes, crucial for building reproducible, version-controlled data pipelines [70]. |
| Population Stability Index (PSI) | Statistical Metric | A measure used to monitor the stability of the input data distribution over time, signaling potential dataset shift [66]. |
| Isolation Forests | Algorithm | An unsupervised learning algorithm used to detect outliers in high-dimensional datasets, which can be a source of shift and model instability [69]. |
| Kolmogorov-Smirnov Test | Statistical Test | A non-parametric test used in continuous monitoring to detect changes in the underlying distribution of a dataset [69]. |
| AWS Glue | Service (Data Catalog) | A managed data catalog service that can serve as a neutral hub to prevent vendor lock-in and maintain flexibility in data strategy [70]. |
| Cross-Validation | Methodological Practice | A resampling technique used to assess how a model will generalize to an independent dataset, helping to identify overfitting and instability early [68]. |
Addressing Age Bias and Non-Linear Trajectories in Developmental Brain Age Models
Troubleshooting Guides
Guide 1: Addressing Systematic Bias in Brain Age Gap (BAG) Estimation
Problem: The predicted age difference (PAD) or Brain Age Gap from your model shows systematic correlation with chronological age, even after common bias-correction methods are applied. This bias makes it difficult to determine if the BAG is a true biological signal or a statistical artifact [71].
Solution: Implement an age-level bias correction method.
- Steps:
- Diagnose the Bias: After building your initial model and calculating the BAG, plot BAG values against chronological age. A significant correlation (e.g., a slope significantly different from zero) indicates persistent systematic bias.
- Apply Age-Level Correction: Instead of a single sample-level correction, apply bias correction procedures that are specific to each age level within your sample range. This accounts for the fact that bias may not be uniform across all ages [71].
- Validate in Numerical Experiments: Test the efficacy of your correction method on simulated data or through cross-validation experiments where the ground truth is known, to ensure it effectively removes the age-related bias without eliminating true biological signals [71].
Application Example: A study aiming to link older BAG to adolescent psychosis must first confirm that the observed BAG is not driven by systematic underestimation of brain age in their specific adolescent age group before drawing clinical conclusions [45] [71].
Guide 2: Managing Non-Linear Brain Development in Lifespan Models
Problem: A model trained on a wide age range collapses complex, non-linear brain changes into a single, linear metric. This can obscure important developmental phases and lead to misinterpretation of an individual's brain age [72] [45].
Solution: Identify topological turning points to define developmental epochs and account for non-linearity.
- Steps:
- Gather Lifespan Data: Use a large dataset (N > 4000) covering a broad age range (e.g., 0-90 years) from multiple cohorts to ensure sufficient density across the lifespan [72].
- Project into Manifold Spaces: Employ non-linear dimensionality reduction techniques, such as Uniform Manifold Approximation and Projection (UMAP), to project high-dimensional brain topological data (e.g., graph theory metrics) into a low-dimensional space that preserves the intrinsic structure of developmental trajectories [72].
- Identify Turning Points: Within the manifold, identify significant shifts in the overall trajectory of topological organization. These "turning points" define major developmental epochs [72].
- Model by Epoch: Develop and apply brain age models within these distinct epochs rather than across the entire lifespan. This ensures that the model's predictions are relevant to the specific phase of brain development.
Application Example: Research has identified four major topological turning points around ages 9, 32, 66, and 83, creating five distinct epochs of brain development. A brain age model for a 20-year-old should be built using data from the epoch defined by ages 9-32, not from a lifespan model that also includes 70-year-olds [72].
The table below summarizes the key topological changes at these turning points.
| Topological Turning Point (Age) | Preceding Epoch Characteristics | Subsequent Epoch Characteristics |
|---|---|---|
| ~9 years old [72] | High-density, less efficient networks around birth [72] | Increasing integration and efficiency [72] |
| ~32 years old [72] | Peak global efficiency and integration; minimal modularity [72] | Decline in global efficiency; increase in modularity and segregation [72] |
| ~66 years old [72] | Gradual decline in integration [72] | Accelerated decline in integration; increased segregation and centrality [72] |
| ~83 years old [72] | Sparse, highly segregated networks [72] | Networks with highest segregation and centrality measures [72] |
Guide 3: Avoiding Stereotypical Profiles in Brain-Phenotype Models
Problem: Your brain-based model predicts cognitive performance well for some individuals but consistently fails for others. The model may not be learning the intended neurocognitive construct but rather a "stereotypical profile" intertwined with sociodemographic or clinical covariates [8].
Solution: Systematically analyze model failure to identify and account for biased phenotypic measures.
- Steps:
- Check Misclassification Frequency: Calculate how often each participant is misclassified across multiple model iterations (e.g., cross-validation folds). A U-shaped distribution—where most participants are either consistently correct or consistently wrong—indicates structured failure [8].
- Profile the "Surprisers": Investigate the group of consistently misclassified individuals. Do they defy a stereotypical profile? For example, do they have high cognitive scores but also have sociodemographic factors (e.g., lower education, different primary language) that are atypical for high scorers in your training data? [8]
- Re-evaluate Phenotypic Measurement: Scrutinize your cognitive tests for potential biases, such as construct bias (universalism fallacy), administration bias, or interpretation bias [8].
- Develop Specific Models: If subgroups are identified, consider developing separate, tailored models for these populations rather than relying on a one-size-fits-all approach [8].
Model Failure Analysis Workflow
Guide 4: Ensuring Robust Validation of Brain Signatures
Problem: A brain signature of cognition derived in one cohort fails to replicate or generalize to a new dataset, limiting its utility as a robust phenotype [25].
Solution: Implement a validation-heavy signature development process that assesses both spatial replicability and model fit replicability.
- Steps:
- Leverage Multiple Discovery Sets: In your discovery phase, do not rely on a single cohort. Instead, derive your brain-behavior associations in many randomly selected subsets (e.g., size n=400) from one or more large discovery cohorts [25].
- Create Consensus Signature Masks: Generate spatial overlap frequency maps from these multiple discovery runs. Define your final "consensus" signature as the regions that appear with high frequency, indicating stability [25].
- Test Fit Replicability: In independent validation datasets, evaluate how well the model fit (e.g., correlation with the outcome) of your consensus signature replicates. High correlations across many random subsets of the validation cohort indicate a robust signature [25].
- Compare to Theory-Based Models: Validate the signature's utility by demonstrating that it outperforms models based on pre-defined theoretical regions of interest in explaining behavioral variance [25].
Frequently Asked Questions (FAQs)
FAQ 1: What does the Brain Age Gap (BAG) actually represent in a child?
The interpretation of BAG in youth is complex and not fully settled. An older BAG is often interpreted as "accelerated maturation," while a younger BAG may indicate "delayed maturation" [45]. However, caution is required because brain development is asynchronous—different brain regions mature at different rates. A global BAG might average out these regional differences, masking important nuances. For example, a child's brain could appear "on time" globally while having a more mature subcortical system and a less mature prefrontal cortex [45].
FAQ 2: My brain-age model works well for adults. Why can't I just apply it to my pediatric dataset?
Applying a model trained on an adult brain to a pediatric brain is highly discouraged. The dynamic, non-linear nature of brain development in youth means the patterns an adult model has learned are not representative of a developing brain [45]. This can introduce severe bias and lead to inaccurate predictions. Always use a model trained on a developmentally appropriate age range.
FAQ 3: The relationship between Brain Age Gap and cognition in my study is inconsistent. Why?
Mixed findings regarding BAG and cognition in youth are common in the literature, with studies reporting positive, negative, or no relationship [45]. This can be due to several factors:
- Different Age Ranges: The relationship may change across developmental epochs.
- Varied Cognitive Measures: Studies use everything from specific tasks (e.g., Flanker) to composite IQ scores, which may tap into different neural systems.
- Model Features: Models using different neuroimaging features (e.g., cortical thickness vs. functional connectivity) may capture different aspects of the brain-cognition relationship [45] [25].
FAQ 4: What are the key non-brain factors I need to account for in developmental brain age models?
Beyond chronological age, two critical factors are:
- Pubertal Development: Earlier pubertal timing and higher pubertal development scale (PDS) scores are consistently linked to an older BAG [45]. Ignoring pubertal stage can confound your results.
- Sociodemographic and Environmental Factors: Socioeconomic status, neighborhood disadvantage, and exposure to adversity have all been linked to BAG [45]. Failing to account for these can lead to models that reflect social stereotypes rather than pure neurobiology [8].
The Scientist's Toolkit: Research Reagent Solutions
| Tool / Solution | Function in Experiment | Key Consideration |
|---|---|---|
| UMAP (Uniform Manifold Approximation & Projection) [72] | Non-linear dimensionality reduction to identify topological turning points and define developmental epochs in high-dimensional brain data. [72] | Captures both local and global data patterns more efficiently than similar methods (e.g., t-SNE). [72] |
| Consensus Signature Mask [25] | A data-driven map of brain regions most associated with a behavior, derived from multiple discovery subsets to ensure spatial stability and robustness. [25] | Requires large datasets and multiple iterations to achieve replicability; helps avoid inflated associations from small samples. [25] |
| Age-Level Bias Correction [71] | A statistical method to remove systematic bias in the Brain Age Gap that is correlated with chronological age, applied at specific age levels rather than universally. [71] | Essential for ensuring the BAG is a reliable phenotype for downstream analysis; sample-level correction alone may be insufficient. [71] |
| Workflow Management System (e.g., Nextflow, Snakemake) [73] | Streamlines pipeline execution, provides error logs for debugging, and enhances the reproducibility of complex analytical workflows. [73] | Critical for managing multi-stage processing of neuroimaging data and ensuring consistent results across compute environments. [73] |
| Biological Experimental Design Concept Inventory (BEDCI) [74] | A validated diagnostic tool to identify non-expert-like thinking in experimental design, covering concepts like controls, replication, and bias. [74] | Useful for training researchers and ensuring a foundational understanding of robust experimental principles before model development. [74] |
The proliferation of complex "black-box" models in scientific research has created a critical paradox: while these models often deliver superior predictive performance, their opacity threatens the very foundation of scientific understanding and reproducibility. This challenge is particularly acute in brain signature phenotype research and drug development, where understanding why a model makes a specific prediction is as important as the prediction itself. Explainable AI (XAI) has emerged as an essential discipline that provides tools and methodologies to peer inside these black boxes, making model decisions transparent, interpretable, and ultimately, trustworthy [75] [76].
The need for interpretability extends beyond mere curiosity. In domains where model predictions influence medical treatments or scientific discoveries, explanations become necessary for establishing trust, ensuring fairness, debugging models, and complying with regulatory standards [75] [76]. Furthermore, the ability to interpret feature contributions can itself become a scientific discovery tool, potentially revealing previously unknown relationships within complex biological systems [77]. This technical support center provides practical guidance for researchers navigating the challenges of interpreting feature contributions, with particular emphasis on applications in neuroimaging and pharmaceutical development.
Core Concepts: Explainability vs. Interpretability
Explainability refers to the ability of a model to provide explicit, human-understandable reasons for its decisions or predictions. It answers the "why" behind a model's output by explaining the internal logic or mechanisms used to arrive at a particular decision [76].
Interpretability, meanwhile, concerns the degree to which a human can consistently predict a model's outcome based on its input data and internal workings. It involves translating the model's technical explanations into insights that non-technical stakeholders can understand, such as which features the model prioritized and why [76].
In practice, these concepts form a continuum from fully transparent, intrinsically interpretable models (like linear regression) to complex black boxes (like deep neural networks) that require post-hoc explanation techniques [78].
Table: Levels of Model Interpretability
| Level | Model Examples | Interpretability Characteristics | Typical Applications |
|---|---|---|---|
| Intrinsically Interpretable | Linear models, Decision trees | Model structure itself provides explanations through coefficients or rules | Regulatory compliance, High-stakes decisions |
| Post-hoc Explainable | Random forests, Gradient boosting | Require additional tools (SHAP, LIME) to explain predictions | Most research applications, Complex pattern detection |
| Black Box | Deep neural networks, Large language models | Extremely complex internal states; challenging to interpret directly | Image recognition, Natural language processing |
FAQ: Addressing Common Interpretability Challenges
Q1: Why does my complex model achieve high accuracy but provides seemingly nonsensical feature importance?
This common issue typically stems from one of several technical challenges:
Confounding Variables: Unaccounted confounding factors can distort feature importance measures. In brain-wide association studies, variables like head motion, age, or site-specific effects in multi-site datasets can create spurious associations that inflate the apparent importance of certain features [79] [1]. Solution: Implement rigorous confounder control through preprocessing harmonization methods (ComBat) and include relevant covariates in your model.
Feature Correlations (Multicollinearity): When features are highly correlated, feature importance can become arbitrarily distributed among them. Solution: Use regularization techniques, variance inflation factor analysis, or create composite features to reduce multicollinearity.
Insufficient Sample Size: Brain-phenotype associations are typically much smaller than previously assumed, requiring samples in the thousands for stable estimates [1]. Small samples lead to inflated effect sizes and unreliable feature importance. Solution: Ensure adequate sample sizes through power analysis and consider collaborative multi-site studies.
Q2: How can I validate that my feature importance scores are reliable and not artifacts?
Validation requires a multi-faceted approach:
Stability Testing: Assess how consistent your feature importance scores are across different data splits, subsamples, or slightly perturbed datasets. Unstable importance scores across different splits indicate unreliable interpretations [79].
Ablation Studies: Systematically remove or perturb top features and observe the impact on model performance. Genuinely important features should cause significant performance degradation when altered.
Null Hypothesis Testing: Generate permutation-based null distributions for your feature importance scores to distinguish statistically significant importance from random fluctuations [80].
Multi-method Consensus: Compare results across different interpretability methods (e.g., both SHAP and LIME). Features consistently identified as important across multiple methods are more likely to be genuinely relevant.
Q3: What are the practical differences between SHAP and LIME, and when should I choose one over the other?
Table: SHAP vs. LIME Comparison
| Aspect | SHAP (SHapley Additive exPlanations) | LIME (Local Interpretable Model-agnostic Explanations) |
|---|---|---|
| Theoretical Foundation | Game theory (Shapley values) | Perturbation-based local surrogate modeling |
| Scope | Both local and global explanations | Primarily local (single prediction) explanations |
| Consistency | Theoretical guarantees of consistency | No theoretical consistency guarantees |
| Computational Cost | Higher, especially for large datasets | Generally lower |
| Implementation | shap.TreeExplainer(model).shap_values(X) |
lime.LimeTabularExplainer() with explain_instance() |
| Ideal Use Case | When you need mathematically consistent explanations for both individual predictions and overall model behavior | When you need quick explanations for specific predictions and computational efficiency is a concern |
SHAP is generally preferred when you need a unified framework for both local and global interpretability with strong theoretical foundations, while LIME excels in scenarios requiring rapid prototyping or explanation of specific individual predictions [75] [76].
Q4: In brain signature research, how can I ensure my interpretability results are reproducible across different parcellations or preprocessing pipelines?
Reproducibility requires standardization and validation across methodological variations:
Multi-atlas Validation: Replicate your findings across different brain parcellation schemes (e.g., AAL, Harvard-Oxford, Craddock) [80]. Features that consistently appear important across different parcellations are more robust.
Pipeline Robustness Testing: Intentionally vary preprocessing parameters (e.g., smoothing kernels, motion correction thresholds) to ensure your interpretations aren't sensitive to specific pipeline choices [79].
Measurement Reliability Assessment: Evaluate the test-retest reliability of both your imaging features and behavioral phenotypes. Low measurement reliability inherently limits reproducible interpretations [1].
Technical Protocols: Implementing Interpretability Methods
Protocol 1: Computing SHAP Values for Model Interpretation
SHAP (SHapley Additive exPlanations) values provide a unified approach to explaining model predictions by quantifying the contribution of each feature to the final prediction [75].
Interpretation Guidelines:
- The base value represents the model's average prediction across the training data
- Feature values in pink increase the prediction, while blue values decrease it
- The summary plot shows the distribution of SHAP values for each feature, with colors indicating feature values (high vs low)
- Features are ordered by their mean absolute SHAP values, indicating overall importance [75]
Protocol 2: Leverage Score Sampling for Stable Brain Signature Identification
This methodology, adapted from neuroimaging research, identifies robust neural features that capture individual-specific signatures while remaining stable across age groups and parcellations [80].
Key Considerations:
- Leverage scores identify features with high influence in capturing population-level variability
- This method is particularly valuable for high-dimensional neuroimaging data where the number of features (functional connections) far exceeds sample size
- The approach maintains interpretability as each selected feature corresponds to a specific brain connection between two regions [80]
Protocol 3: Permutation Feature Importance for Nonlinear Models
Permutation feature importance measures the decrease in model performance when a single feature is randomly shuffled, breaking its relationship with the target.
Interpretation:
- Features with higher weight values have greater importance
- The ± values indicate the variability of importance across permutations
- This method is particularly useful for identifying which features the model relies on most heavily for predictions [75]
Visual Guide: Interpretability Workflows
Interpretability Method Selection Algorithm
Brain Signature Interpretability Pipeline
Research Reagent Solutions: Essential Tools for Interpretable Research
Table: Essential Interpretability Tools and Their Applications
| Tool/Technique | Primary Function | Advantages | Limitations | Implementation |
|---|---|---|---|---|
| SHAP | Unified framework for explaining model predictions using game theory | Consistent explanations, both local and global interpretability | Computationally intensive for large datasets | Python shap library |
| LIME | Creates local surrogate models to explain individual predictions | Model-agnostic, computationally efficient | No global consistency guarantees | Python lime package |
| Leverage Score Sampling | Identifies high-influence features in high-dimensional data [80] | Theoretical guarantees, maintains interpretability | Limited to linear feature relationships | Custom implementation in Python/Matlab |
| Permutation Feature Importance | Measures feature importance by permutation | Intuitive, model-agnostic | Can be biased for correlated features | eli5 library |
| Partial Dependence Plots | Visualizes relationship between feature and prediction | Intuitive visualization of feature effects | Assumes feature independence | PDPbox library |
| Functional Connectome Preprocessing | Processes fMRI data for brain network analysis [80] | Standardized pipeline for neuroimaging | Sensitive to parameter choices | Custom pipelines based on established software (FSL, AFNI) |
| Cross-Validation Strategies | Assesses model stability and generalizability | Reduces overfitting, provides performance estimates | Can mask instability with small effect sizes [1] | scikit-learn |
Advanced Troubleshooting: Addressing Complex Scenarios
Scenario: Inconsistent Feature Importance Across Similar Datasets
Problem: Your model identifies different features as important when trained on datasets that should capture similar biological phenomena (e.g., different cohorts studying the same brain-phenotype relationship).
Diagnosis Steps:
- Effect Size Assessment: Check if the observed associations are sufficiently large relative to your sample size. Brain-phenotype associations are typically much smaller (median |r| ~ 0.01-0.16) than often assumed, requiring thousands of samples for stable estimation [1].
- Measurement Consistency: Evaluate whether the same constructs are being measured consistently across datasets. Subtle differences in phenotypic assessments can dramatically alter relationships.
- Confounder Analysis: Systematically test for differential confounding across datasets (e.g., age distributions, data acquisition protocols, preprocessing pipelines) [79].
Solutions:
- Apply harmonization methods (ComBat, longitudinal) to remove technical artifacts while preserving biological signals
- Use multivariate methods that are generally more robust than univariate approaches [1]
- Implement cross-dataset validation frameworks where feature importance is explicitly tested for consistency
Scenario: Interpretation Conflicts Between Different Methods
Problem: SHAP, LIME, and permutation importance identify different features as most important in the same model and dataset.
Diagnosis Steps:
- Method Alignment Check: Confirm each method is answering the same question. SHAP explains output value composition, permutation importance explains predictive contribution, and LIME explains local decision boundaries.
- Feature Correlation Analysis: High feature correlations can cause interpretation instability, where different but correlated features appear important across methods.
- Model Linearity Assessment: Check if your model relies on strong interactive effects, which different methods capture differently.
Solutions:
- Use hierarchical clustering on feature correlations to create feature groups
- Report consensus importance across multiple methods rather than relying on a single approach
- For high-stakes interpretations, perform ablation studies to ground-truth feature importance
Moving beyond black boxes requires more than just technical solutions—it demands a fundamental shift in how we approach model development and validation in scientific research. By integrating interpretability as a core component of the modeling lifecycle rather than an afterthought, researchers can transform opaque predictions into meaningful scientific insights. The methodologies outlined in this technical support center provide a foundation for this transition, offering practical pathways to reconcile the predictive power of complex models with the explanatory depth necessary for scientific progress.
In brain signature research and drug development specifically, where the stakes for misinterpretation are high and the biological complexity is profound, these interpretability techniques become not just useful tools but essential components of rigorous, reproducible science. As the field advances, the integration of domain knowledge with model explanations will likely become the gold standard, ensuring that our most powerful predictive models also serve as windows into the biological systems they seek to emulate.
Ensuring Generalizability: Validation Frameworks and Comparative Analysis
The pursuit of reproducible brain-behavior relationships represents a central challenge in modern neuroscience. Predictive neuroimaging, which uses brain features to predict behavioral phenotypes, holds tremendous promise for precision medicine but has been hampered by widespread replication failures [81]. A critical paradigm shift from isolated group-level studies to robust, generalizable individual-level predictions is underway. This technical support center provides targeted guidance to overcome the specific pitfalls in validating brain-phenotype models, ensuring your findings are not only statistically significant but also scientifically and clinically meaningful.
A primary challenge has been replicating associations between inter-individual differences in brain structure or function and complex cognitive or mental health phenotypes [1]. Research settings often remove between-site variations by design, creating artificial harmonization that does not exist in real-world clinical scenarios [82]. The following sections provide actionable solutions for establishing rigorous validation benchmarks through detailed troubleshooting guides, experimental protocols, and visual workflows.
Troubleshooting Guide: Common Cross-Validation Challenges
FAQ 1: Why does my model perform well internally but fail on external datasets?
- Problem: This classic sign of overfitting occurs when models learn dataset-specific noise rather than generalizable brain-phenotype relationships. Small sample sizes exacerbate this issue, as they lead to inflated effect size estimates and poor stability [1].
- Solution:
- Increase Sample Size: Brain-wide association studies (BWAS) require thousands of individuals for reproducible results. Univariate associations are often surprisingly small (median |r| ≈ 0.01), requiring large samples for accurate estimation [1].
- Incorporate Diversity at Source: Intentionally train models on data from multiple sites, protocols, and demographic backgrounds. Remarkably, for some datasets, the best predictions come not from training and testing within the same dataset, but from models trained on more diverse external data [82] [83].
- Apply Regularization: Use ridge regression or other penalization methods to constrain model complexity and prevent overfitting to training set idiosyncrasies [82].
FAQ 2: How can I determine if my model is capturing biological signals or sociodemographic stereotypes?
- Problem: Models may reflect not unitary cognitive constructs but rather neurocognitive scores intertwined with sociodemographic and clinical covariates. They often fail when applied to individuals who defy these stereotypical profiles [55].
- Solution:
- Stratified Error Analysis: Systematically evaluate whether model failure is structured by checking if prediction errors are higher for specific demographic subgroups [55].
- Covariate Control: Test model performance while controlling for age, sex, socioeconomic status, and clinical symptom burden to ensure brain features provide unique predictive power [82].
- Interpretability Analysis: Use feature importance methods (beta weights, stability metrics) to identify which brain networks drive predictions and assess their neurobiological plausibility [81].
FAQ 3: What are the minimum sample size requirements for reproducible brain-phenotype predictions?
- Problem: Most neuroimaging studies are severely underpowered, with a median sample size of only 25 participants [1] [84]. At this size, the 99% confidence interval for univariate associations is r ± 0.52, making extreme effect size inflation likely.
- Solution:
- Consortium-Level Data: Leverage large-scale datasets like UK Biobank (n > 35,000), ABCD (n > 11,000), or HCP (n > 1,200) whenever possible [1].
- Multi-Site Collaboration: For original data collection, plan multi-site studies with samples in the thousands, not hundreds.
- Power Calculations: Base sample size calculations on realistic effect sizes (r < 0.2) rather than the inflated estimates from underpowered literature.
Table 1: Sample Size Requirements for Brain-Wide Association Studies
| Analysis Type | Typical Sample Size in Literature | Recommended Minimum Sample Size | Effect Size Reality (Median | r | ) |
|---|---|---|---|---|---|
| Univariate BWAS | 25 [1] | 3,000+ [1] | 0.01 [1] | ||
| Multivariate Predictive Modeling | 50-100 | 1,000+ [82] | Varies by method | ||
| Cross-Dataset Validation | Rarely done [82] | 2+ independent datasets with different characteristics [82] [83] | Cross-dataset r = 0.13-0.35 for successful models [82] |
Experimental Protocols for Cross-Dataset Validation
Protocol: Rigorous Cross-Dataset Validation Framework
This protocol provides a step-by-step methodology for evaluating model generalizability across diverse, unharmonized datasets, based on approaches that have successfully demonstrated cross-dataset prediction [82] [83].
Research Reagent Solutions:
- Dataset Selection: Choose datasets with intentional heterogeneity in imaging parameters, demographic characteristics, and behavioral measures.
- Computational Environment: Standardized software containers (Docker, Singularity) ensure reproducible analysis environments.
- Parcellation Scheme: Use standardized brain atlases (e.g., Shen 268) [82] for feature extraction across datasets.
Methodology:
Intentional Dataset Selection:
- Select at least three independent datasets with differing characteristics (e.g., Philadelphia Neurodevelopmental Cohort, Healthy Brain Network, Human Connectome Project in Development) [82].
- Prioritize datasets with variations in: age distribution, sex, racial/ethnic representation, recruitment geography, clinical symptom burdens, fMRI tasks/sequences, and behavioral measures [82] [83].
Feature Engineering:
- Create connectomes using a standardized brain atlas applied consistently across all datasets.
- Combine connectomes across all available fMRI data (resting-state and tasks) to improve reliability and predictive power [82].
- Derive latent behavioral factors using Principal Component Analysis (PCA) within each dataset separately, estimating PCA parameters using participants without imaging data to maintain proper separation of training and testing data [82].
Model Training and Testing:
- Apply ridge regression Connectome-Based Predictive Modeling (CPM) or similar regularized approaches.
- Implement a comprehensive validation framework:
- Within-dataset: 100 iterations of 10-fold cross-validation
- Cross-dataset: Train on each dataset, test on all others
- For cross-dataset predictions, apply models trained on one dataset directly to the feature data of another without retraining [82].
Performance Evaluation:
- Use Pearson's correlation (r) between predicted and observed scores as primary metric.
- Calculate cross-validated coefficient of determination (q²) and mean square error.
- Assess significance via permutation testing (1000 iterations with randomly shuffled behavioral labels) [82].
The following workflow diagram illustrates this comprehensive validation framework:
Protocol: Structured Analysis of Model Failure
This protocol addresses the critical but often overlooked need to systematically analyze when and why models fail, turning failure analysis into a diagnostic tool [55].
Methodology:
Misclassification Frequency Calculation:
- For classification models, calculate misclassification frequency for each participant across multiple cross-validation iterations.
- Compare distribution to permutation-based null models (shuffled labels) [55].
Structured Error Analysis:
- Test consistency of misclassification across different in-scanner conditions for the same phenotypic measure.
- Evaluate phenotype specificity by correlating misclassification patterns across similar versus dissimilar cognitive measures [55].
Sociodemographic Profiling:
- Test whether participants who are consistently misclassified share specific sociodemographic or clinical characteristics.
- Determine if models work better for specific population subgroups and worse for others [55].
Table 2: Interpretation Methods for Predictive Neuroimaging Models
| Interpretability Approach | Description | Best Use Cases | Cautions |
|---|---|---|---|
| Beta Weight-Based Metrics [81] | Uses regression coefficients as feature importance indicators | Initial feature screening; models with low multicollinearity | Requires standardized features; sensitive to correlated predictors |
| Stability-Based Metrics [81] | Determines feature contribution by occurrence frequency over multiple models | Identifying robust features across validation folds; high-dimensional data | Requires thresholding; may miss consistently small-but-important features |
| Prediction Performance-Based Metrics [81] | Evaluates importance by performance change when features are excluded | Establishing causal contribution of specific networks; virtual lesion analysis | Computationally intensive; network size may confound results |
Advanced Validation Techniques and Visualization
Interpretation Workflow for Predictive Models
Moving beyond prediction accuracy to neurobiological interpretation is essential for scientific progress and clinical translation [81]. The following diagram outlines a comprehensive workflow for interpreting predictive models:
Implementation Checklist for Cross-Dataset Validation
- Intentional Heterogeneity: Select datasets with deliberate variations in acquisition parameters, demographics, and behavioral measures [82] [83]
- Appropriate Scaling: Ensure sample sizes reach thousands, not dozens, for reproducible associations [1]
- Rigorous Cross-Validation: Implement both within-dataset and cross-dataset validation frameworks [82]
- Structured Failure Analysis: Systematically examine which participants are misclassified and why [55]
- Model Interpretation: Apply multiple interpretability approaches to uncover neurobiological mechanisms [81]
- Transparent Reporting: Share data, code, and detailed protocols to enable true reproducibility [85]
Establishing robust benchmarks for cross-dataset and cross-sample validation is not merely a technical exercise but a fundamental requirement for building clinically useful neuroimaging biomarkers. By implementing the troubleshooting guides, experimental protocols, and validation frameworks outlined in this technical support center, researchers can dramatically improve the reproducibility and generalizability of their findings. The future of predictive neuroimaging lies not in pursuing maximum prediction accuracy at all costs, but in developing interpretable, robust, and equitable models that generate genuine neurobiological insights and can reliably inform clinical decision-making [81]. Through rigorous validation practices that embrace rather than remove real-world heterogeneity, we can translate technical advances into concrete improvements in precision medicine.
FAQ: Addressing Common Challenges in Reproducible Research
FAQ 1: Why do my brain-wide association studies (BWAS) fail to replicate in new samples?
The primary reason for replication failure is inadequate statistical power. BWAS associations are typically much smaller than previously assumed. In large samples (n~50,000), the median univariate effect size (|r|) is approximately 0.01, with the top 1% of associations reaching only |r| > 0.06 [1]. At traditional sample sizes (e.g., n=25), the 99% confidence interval for these associations is r ± 0.52, meaning studies are severely underpowered and susceptible to effect size inflation [1]. Solutions include using samples of thousands of individuals, pre-registering hypotheses, and employing multivariate methods which show more robust effects [1].
FAQ 2: How reliable are my neuroimaging-derived phenotypes (IDPs), and how does this impact my findings?
Measurement reliability directly limits the maximum observable correlation between brain measures and phenotypes. While structural measures like cortical thickness have high test-retest reliability (r > 0.96), functional connectivity measures can be more variable (e.g., RSFC reliability: r = 0.39-0.79 across datasets) [1]. This measurement error attenuates observed effect sizes. Before launching large-scale studies, assess the test-retest reliability of your specific imaging phenotypes in a pilot sample.
FAQ 3: What is "external validation," and why is it more informative than cross-validation within my dataset?
External validation tests a predictive model on a completely independent dataset, providing the strongest evidence for generalizability. In contrast, cross-validation within a single dataset can overfit to that dataset's idiosyncrasies [86]. Studies show that internal (within-dataset) prediction performance is typically within r=0.2 of external (cross-dataset) performance, but the latter provides a more realistic estimate of real-world utility [86]. Power for external validation depends on both training and external dataset sizes, which must be considered in study design [86].
FAQ 4: How can I harmonize data across different platforms or biobanks to enable larger meta-analyses?
The Global Biobank Meta-analysis Initiative (GBMI) provides a model for cross-biobank collaboration. Success requires: (1) Genetic data harmonization using standardized imputation and quality control; (2) Phenotype harmonization by mapping to common data models like phecodes from ICD codes; and (3) Ancestry-aware analysis using genetic principal components to account for population structure [87]. GBMI has successfully integrated 23 biobanks representing over 2.2 million individuals, identifying 183 novel loci for 14 diseases through this approach [87].
Troubleshooting Guides
Guide 1: Diagnosing and Resolving Power Deficiencies in BWAS
Table: Sample Size Requirements for BWAS Detection Power (80% power, α=0.05)
| Effect Size ( | r | ) | Required N | Example Phenotypes |
|---|---|---|---|---|
| 0.01 | ~78,000 | Most brain-behaviour associations [1] | ||
| 0.05 | ~3,100 | Strongest univariate associations [1] | ||
| 0.10 | ~780 | Task fMRI activation differences [1] | ||
| 0.15 | ~345 | Lesion-deficit mappings [1] |
Symptoms of Underpowered Studies:
- Wide confidence intervals in effect size estimates
- Failure to replicate in independent samples
- Effect size inflation (especially in samples <1000)
- Inconsistent results across similar studies
Remedial Actions:
- Pool resources through consortia like GBMI [87] or ENIGMA
- Use multivariate methods (e.g., CCA, SVR) that aggregate signal across multiple features [1]
- Focus on cognitive measures rather than mental health questionnaires, as they typically show stronger associations [1]
- Apply strict multiple comparison correction and avoid data mining without hypothesis pre-registration
Guide 2: Implementing Robust Quality Control for Multi-Site Studies
Table: Automated QC Failure Rates in Clinical vs. Research Settings
| QC Metric | ABCD (Research) | OBHC (Clinical) | Recommended Threshold |
|---|---|---|---|
| Mean Framewise Displacement | ~15% flagged [1] | 14-24% flagged [88] | <0.2mm mean FD [86] |
| Visual QC Failure | N/A | 0-2.4% after inspection [88] | Manual inspection required |
| Data completeness | >8 min RSFC post-censoring [1] | Core clinical sequences prioritized [88] | Protocol-specific |
Troubleshooting QC Failures:
- High motion artifacts: Implement rigorous motion censoring (e.g., filtered-FD < 0.08mm) [1], collect more data per participant
- Site/scanner effects: Use harmonization protocols like those in UK Biobank [88], include site as covariate
- Missing data: Prioritize core sequences (T1, T2-FLAIR) for clinical populations [88]
Guide 3: Designing Effective External Validation Studies
Power Calculation for External Validation: Power depends on both training set size (Ntrain) and external validation set size (Nexternal). Simulations show that prior external validation studies used sample sizes prone to low power, leading to false negatives and effect size inflation [86]. For a target effect size of r=0.2, you need N_external > 500 to achieve 80% power, even with a well-powered training set [86].
Protocol for External Validation:
- Training Phase: Develop predictive model using cross-validation within your primary dataset
- Model Freezing: Finalize all model parameters and preprocessing steps without further modification
- External Testing: Apply the frozen model to completely independent data from different sites/scanners
- Performance Assessment: Evaluate using correlation (r) or R² between predicted and observed values
- Comparison: Expect external performance to be within r=0.2 of internal performance [86]
Table: Key Large-Scale Datasets for Reproducible Brain Phenotype Research
| Resource | Sample Size | Key Features | Access |
|---|---|---|---|
| UK Biobank (UKB) | ~35,735 imaging; >500,000 total [1] | Multi-modal imaging, genetics, health records; age 40-69 | Application required |
| ABCD Study | ~11,875 [89] | Developmental focus (age 9-10+), twin subsample, substance use focus | NDA controlled access |
| Global Biobank Meta-analysis Initiative (GBMI) | >2.2 million [87] | 23 biobanks across 4 continents, diverse ancestries, EHR-derived phenotypes | Summary statistics available |
| HCP Development | ~424-605 [86] | Lifespan developmental sample (age 8-22), deep phenotyping | Controlled access |
| Oxford Brain Health Clinic | ~213 [88] | Memory clinic population, dementia-informed IDPs, UKB-aligned protocol | Research collaborations |
Table: Statistical & Computational Tools for Reproducible Analysis
| Tool Category | Specific Solutions | Application |
|---|---|---|
| Quality Control | MRIQC, QUAD, DSE decomposition [88] | Automated quality assessment of neuroimaging data |
| Harmonization | ComBat, NeuroHarmonize [90] | Removing site and scanner effects in multi-center studies |
| Prediction Modeling | Ridge regression with feature selection [86] | Creating generalizable brain-phenotype models |
| Multiple Comparison Correction | Hierarchical FDR [88] | Account for dependency structure in imaging data |
| Version Control | Git, GitHub [90] | Track analytical decisions and maintain code reproducibility |
Experimental Protocols for Reproducible Brain Phenotype Research
Protocol 1: UK Biobank Imaging-Derived Phenotype Extraction
Objective: Generate standardized imaging phenotypes from raw neuroimaging data that are comparable across studies.
Materials:
- T1-weighted structural MRI (acquisition parameters: UK Biobank protocol)
- Resting-state fMRI (6-60 minutes, depending on dataset)
- Processing pipelines: FSL, FreeSurfer, BioImage Suite [86] [90]
Method:
- Preprocessing:
- Structural: Brain extraction, tissue segmentation, cortical reconstruction
- Functional: Head motion correction, registration, band-pass filtering
- Apply consistent denoising strategies (e.g., 24-parameter motion regression) [86]
Feature Extraction:
- Structural IDPs: Cortical thickness, subcortical volumes, white matter hyperintensity load
- Functional IDPs: Resting-state network connectivity, amplitude of low-frequency fluctuations
- Generate both standard (n=5,683) and dementia-informed (n=110) IDPs for clinical populations [88]
Quality Control:
- Automated QC with MRIQC/QUAD
- Visual inspection of flagged outputs (expect 0-2.4% exclusion after inspection) [88]
- Exclusion criteria: Excessive motion (>0.2mm mean FD), poor coverage, artifacts
Protocol 2: Cross-Biobank Meta-Analysis Following GBMI Standards
Objective: Identify robust genetic variants associated with diseases by harmonizing across biobanks.
Materials:
- Genotype data from multiple biobanks (e.g., UKB, BioBank Japan, FinnGen)
- Phenotype data mapped to phecodes
- Computing resources for large-scale GWAS
Method:
- Genotype Harmonization:
- Impute to common reference panel (e.g., TOPMed)
- Standard QC: MAF > 0.01, imputation quality > 0.3, HWE violations [87]
Phenotype Harmonization:
- Map ICD codes to phecodes across biobanks
- Account for differences in prevalence across healthcare systems [87]
Ancestry Stratification:
- Project all samples to common genetic PCA space
- Analyze ancestry groups separately (EUR, EAS, AFR, etc.) [87]
Meta-Analysis:
- Perform inverse-variance weighted fixed-effects meta-analysis
- Apply genomic control to correct for residual population stratification
- Validate with leave-one-biobank-out sensitivity analyses
Troubleshooting Guide & FAQ
This guide addresses common challenges researchers face when validating brain signatures and linking them to external genetic and clinical criteria.
FAQ 1: Why do my brain-wide association studies (BWAS) fail to replicate?
- Problem: Many BWAS produce findings that are not reproducible in subsequent studies.
- Solution: The primary issue is often insufficient sample size. Brain-behaviour associations are typically much smaller than previously assumed. Reproducible BWAS require samples in the thousands, not the tens or hundreds that were once standard [1]. Furthermore, ensure you are not using "opaque thresholding," where all data below an arbitrary statistical threshold is hidden. This practice contributes to selection bias and irreproducibility. Instead, use "transparent thresholding" to highlight significant results while still showing the full range of your data [91].
FAQ 2: How can I rigorously link a genetic signature to a brain-based phenotype?
- Problem: Establishing a predictive, rather than just correlative, relationship between genetic markers and brain outcomes is complex.
- Solution: Employ longitudinal designs and robust statistical models. One effective approach is to use regression modeling coupled with dynamic Bayesian network analysis to identify predictive causal relationships between gene expression and behavioral or cognitive outcomes over time [92]. This can reveal how specific genes (e.g., FABP5 family or immunoglobulin-related genes) predict changes in social-cognitive trajectories.
FAQ 3: What is the best way to document an experimental protocol for maximum reproducibility?
- Problem: Incomplete protocol descriptions make it impossible for other labs to reproduce experiments.
- Solution: Your protocol should be a detailed "recipe" that a trained researcher from outside your lab could follow exactly [93]. It must include all necessary and sufficient information [94]. Use a structured checklist to ensure completeness. Key data elements include:
- Reagents and Equipment: Include catalog numbers, manufacturers, and specific experimental parameters [94].
- Step-by-Step Workflow: Describe all actions in detail, including timing, temperatures, and specific software settings.
- Data Acquisition Parameters: For neuroimaging, this includes pulse sequences, resolution, and head motion criteria [95] [1].
- Quality Control Steps: Define accuracy criteria for participant practice trials and procedures for monitoring data quality during collection [93].
FAQ 4: How do I account for the influence of environmental risk factors like childhood adversity?
- Problem: Genetic and environmental risk factors are often correlated and can have overlapping neural signatures.
- Solution: Use multivariate statistical techniques to disentangle shared and unique variance. Canonical Correlation Analysis (CCA) can reveal dimensions of shared genetic liability across multiple mental health phenotypes and how they relate to adversity [95]. Partial Least Squares (PLS) can then be used to identify the cortico-limbic signature that is common to both genetic liability and environmental adversity [95].
Essential Experimental Protocols
Protocol 1: Conducting a Reproducible Brain-Wide Association Study (BWAS)
This protocol outlines key steps for a robust BWAS, based on lessons from large-scale analyses [1].
- Sample Size Planning: Power your study appropriately. For reliable detection of univariate brain-behaviour associations, plan for sample sizes of several thousand individuals [1].
- Data Acquisition and Preprocessing:
- MRI Data: Collect high-quality structural and/or functional MRI data. For resting-state fMRI, aim for at least 10 minutes of data after rigorous motion censoring (e.g., framewise displacement < 0.08 mm) [1].
- Phenotyping: Use well-validated behavioural and cognitive tests with high test-retest reliability.
- Denoising: Apply strict denoising strategies to mitigate the effects of head motion and other nuisance variables.
- Data Analysis:
- Avoid opaque, all-or-nothing statistical thresholding. Instead, use transparent thresholding practices that highlight significant results while also showing the full body of evidence [91].
- For univariate analyses, correlate brain features (e.g., cortical thickness, functional connectivity edges) with phenotypic measures.
- Always adjust for key sociodemographic covariates, as this reduces effect size inflation [1].
- Replication: Validate your findings in an independent, held-out dataset or a different large-scale cohort (e.g., UK Biobank, HCP, ABCD) [1].
Protocol 2: Validating a Genetic Signature in a Clinical Population
This protocol is based on longitudinal studies of individuals at ultra-high risk for psychosis [92].
- Participant Recruitment: Recruit a well-characterized clinical cohort (e.g., individuals at ultra-high risk for psychosis) and a matched healthy control group.
- Baseline Assessment:
- Genetic Data: Collect biospecimens (e.g., blood, saliva) for genotyping and gene expression analysis. Calculate polygenic risk scores for relevant phenotypes [95].
- Clinical and Cognitive Phenotyping: Administer a comprehensive battery of tests assessing social cognition, memory, and executive function.
- Longitudinal Follow-up: Conduct repeated assessments at regular intervals (e.g., every 6 months) over an extended period (e.g., 24 months).
- Statistical Analysis:
- Use regression modeling (e.g., linear regression) to test if baseline genetic markers predict future social-cognitive outcomes.
- Employ dynamic Bayesian network analysis to uncover temporal dependencies and identify central nodes (e.g., specific genes like FCGRT) that mediate the relationship between genetic markers and behavioural changes [92].
Data Presentation Tables
Table 1: BWAS Effect Sizes and Required Sample Sizes
Table based on analysis of large datasets (n ~50,000) showing the relationship between sample size and effect size reproducibility [1].
| Sample Size (n) | Median Univariate Effect Size (|r|) | Top 1% Effect Size (|r|) | Replication Outcome |
|---|---|---|---|
| ~25 (Typical historic) | Highly Inflated & Variable | >0.2 (inflated) | Very Low (High failure rate) |
| ~3,900 (Large) | 0.01 | >0.06 | Improved (Largest replicable effect ~0.16) |
| Thousands | Stable, accurate estimation | Stable, accurate estimation | High |
Table 2: Key Protocols for Reproducible Research
Summary of critical methodologies to overcome common pitfalls.
| Research Stage | Pitfall | Recommended Protocol | Key Reference |
|---|---|---|---|
| Results Reporting | Opaque thresholding; hiding non-significant results | Use transparent thresholding: highlight significant results while showing full data. | [91] |
| Study Design | Underpowered brain-behaviour associations | Plan for sample sizes in the thousands, not dozens. | [1] |
| Genetic Validation | Correlative, non-predictive models | Use longitudinal designs with regression and Bayesian network analysis. | [92] |
| Protocol Documentation | Incomplete methods, preventing replication | Use a detailed checklist for all reagents, steps, and parameters. | [94] [93] |
Signaling Pathways and Workflows
Brain Signature Validation Workflow
Sample Size vs. Reproducibility Relationship
Genetic Risk to Clinical Outcome Pathway
The Scientist's Toolkit: Research Reagent Solutions
Key materials and tools for linking brain signatures to external criteria.
| Item / Resource | Function / Purpose | Example(s) / Notes |
|---|---|---|
| Polygenic Risk Scores (PRS) | Quantifies an individual's genetic liability for a specific trait or disorder based on genome-wide association studies. | Calculated for ADHD, Depression, etc., using software like PRSice-2 [95]. |
| Structured Clinical Interviews & Checklists | Provides standardized, reliable phenotyping of psychopathology and cognitive function. | Child Behavior Checklist (CBCL), Prodromal Psychosis Scale (PPS) [95]. |
| Public Neuroimaging Datasets | Provides large-sample data for discovery, validation, and methodological development. | ABCD Study [95] [1], UK Biobank [1], Human Connectome Project [1]. |
| Multivariate Analysis Tools | Models relationships between large sets of brain and behavioural/genetic variables. | Canonical Correlation Analysis (CCA), Partial Least Squares (PLS) [95]. |
| Network Analysis Software | Identifies temporal dependencies and central nodes in longitudinal genetic-behavioural data. | Dynamic Bayesian Network Analysis [92]. |
| Standardized Protocol Checklist | Ensures experimental methods are reported with sufficient detail for replication. | Based on guidelines from SMART Protocols Ontology; includes 17 key data elements [94]. |
Frequently Asked Questions (FAQs)
Core Concepts and Framework Design
Q1: What is the primary advantage of a multi-source, multi-ontology phenotyping framework over traditional methods? A1: Traditional phenotyping often relies on single data sources (e.g., only EHR or only self-report), leading to fragmented and non-portable definitions. A multi-source, multi-ontology framework integrates diverse data (EHR, registries, questionnaires) and harmonizes medical ontologies (like Read v2, CTV3, ICD-10, OPCS-4). This integration enhances accuracy, enables comprehensive disease characterization, and facilitates reproducible research across different biobanks and populations [22].
Q2: Why is sample size so critical for reproducible brain-wide association studies (BWAS)? A2: Brain-wide association studies often report small effect sizes (e.g., median |r| = 0.01). Small samples (e.g., n=25) are highly vulnerable to sampling variability, effect size inflation, and replication failures. Samples in the thousands are required to stabilize associations, accurately estimate effect sizes, and achieve reproducible results [1].
Q3: What are the common pitfalls when interpreting predictive models in neuroimaging? A3: Common pitfalls include treating interpretation as a secondary goal, relying solely on prediction accuracy, and using "black-box" models without understanding feature contribution. Arbitrary interpretation without rigorous validation can obscure the true neural underpinnings of behavioral traits. It is crucial to use interpretable models and validate biomarkers across multiple datasets [81].
Data Integration and Ontology Mapping
Q4: Our team is struggling to map clinical text to Human Phenotype Ontology (HPO) terms accurately. What tools can we use? A4: Traditional concept recognition tools (Doc2HPO, ClinPhen) use dictionary-based matching and can miss nuanced contexts. For improved accuracy, consider tools leveraging Large Language Models (LLMs) with Retrieval-Augmented Generation (RAG), such as RAG-HPO. This approach uses a dynamic vector database for real-time retrieval and contextual matching, significantly improving precision and recall in HPO term assignment [96].
Q5: How can we effectively integrate multiple biomedical ontologies to improve semantic representation? A5: The Multi-Ontology Refined Embeddings (MORE) framework is a hybrid model that combines structured knowledge from multiple ontologies (like MeSH) with corpus-based distributional semantics. This integration improves the accuracy of learned word embeddings and enhances the clustering of similar biomedical concepts, which is vital for analyzing patient records and improving data interoperability [97].
Q6: What is the recommended file and directory organization for a computational phenotyping project?
A6: Organize projects under a common root directory. Use a logical top-level structure (e.g., data, results, doc, src). Within data and results, use chronological organization (e.g., 2025-11-27_experiment_name) instead of purely logical names to make the project's evolution clear. Maintain a detailed, dated lab notebook (e.g., a wiki or blog) to record progress, observations, and commands [98].
Validation and Reproducibility
Q7: What are the key layers for validating a computationally derived phenotype? A7: A robust validation strategy should include multiple layers [22]:
- Data Source Concordance: Check agreement between cases identified via different sources (e.g., primary care, hospital records).
- Epidemiological Plausibility: Assess if age and sex-specific incidence and prevalence patterns match known epidemiology.
- External Comparison: Compare prevalence estimates with a representative external cohort.
- Association Validation: Replicate known associations with modifiable risk factors.
- Genetic Validation: Evaluate genetic correlations with external genome-wide association studies (GWAS).
Q8: How can we assess the quality of phenotype annotations when multiple curators are involved? A8: Develop a expert-curated gold standard dataset where annotations are created by consensus among multiple curators. Use ontology-aware metrics to evaluate annotations from human curators or automated tools against this gold standard. These metrics go beyond simple precision/recall to account for semantic similarity between ontology terms [99].
Troubleshooting Guides
Low Phenotyping Accuracy or Consistency
Problem: Your phenotype definitions are yielding inconsistent case counts, missing true cases (low recall), or including false positives (low precision).
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Incomplete Ontology Mapping | Check if clinical concepts in your data lack corresponding codes in the ontologies you are using. | Manually review and add missing terms to your ontology set. Use Augmented or Merged ontologies that have broader coverage [99]. |
| Single-Source Reliance | Compare case counts identified from your primary source (e.g., EHR) with other sources (e.g., self-report, registry). | Develop an integrated definition that uses multiple data sources (EHR, questionnaire, registry) to identify cases, which boosts statistical power and accuracy [22]. |
| Poor Context Handling in NLP | Manually review a sample of clinical text where your tool failed to assign the correct HPO term. | Switch from pure concept-recognition tools to an LLM-based approach like RAG-HPO, which uses retrieval-augmented generation to better understand context and reduce errors [96]. |
Irreproducible Brain-Behavior Associations
Problem: Your brain-wide association study (BWAS) fails to replicate in a different sample or shows inflated effect sizes.
| Possible Cause | Diagnostic Steps | Solution | ||
|---|---|---|---|---|
| Insufficient Sample Size | Calculate the statistical power of your study given the expected effect sizes (often | r | < 0.10). | Aim for sample sizes in the thousands. Use consortium data (e.g., UK Biobank, ABCD) where possible. Clearly report the effect sizes and confidence intervals [1]. |
| Inadequate Denoising | Correlate your primary behavioral measure with head motion metrics. | Apply strict denoising strategies for neuroimaging data (e.g., frame censoring). Document and report all preprocessing steps meticulously [1]. | ||
| Over-reliance on Univariate Analysis | Check if your multivariate model's performance is significantly better than univariate models. | Use multivariate prediction models that can tap into rich, multimodal information distributed across the brain [81]. |
Poor Interpretability of Predictive Models
Problem: Your predictive neuroimaging model has good accuracy, but you cannot determine which brain features are driving the predictions.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Use of "Black-Box" Models | Check if your model (e.g., some deep learning architectures) inherently lacks feature importance output. | Employ interpretable models or post-hoc interpretation strategies. Use beta weights from linear models or stability selection across cross-validation folds to identify robust features [81]. |
| Unstable Feature Importance | Check the consistency of top features across different splits of your data. | Use stability-based metrics. Report only features that consistently appear (e.g., 100% occurrence) across multiple resampling runs or cross-validation folds [81]. |
| High Feature Collinearity | Calculate correlations between your top predictive features. | Use techniques like relative importance analysis to disentangle the contribution of correlated features. Virtual lesion analysis (systematically removing features) can also test their unique contribution [81]. |
Experimental Protocols & Methodologies
Protocol: Building a Multi-Source Phenotyping Algorithm
This protocol outlines the key steps for defining a computational phenotype using the UK Biobank as a model, integrating multiple data sources and ontologies [22].
1. Data Source Harmonization:
- Identify Sources: Gather data from primary care EHR, hospital admissions, cancer and death registries, and self-reported questionnaires.
- Map Ontologies: Extract and harmonize diagnostic and procedure codes across all medical ontologies used (Read v2, CTV3, ICD-10, OPCS-4).
- Translate Codes: Use forward-mapping files (e.g., NHS TRUD) to bootstrap translation between ontologies (e.g., Read v2 to CTV3), followed by manual review by clinical experts.
2. Algorithm Definition:
- Create Code Lists: For each condition, manually curate a list of relevant diagnosis/procedure codes from all ontologies.
- Incorporate Self-Report: Identify relevant self-reported medical history and custom data fields from baseline assessments.
- Define Case Logic: Establish rules for combining data sources to define a case (e.g., presence of at least one code from any source).
3. Multi-Layer Validation:
- Perform the validation steps outlined in FAQ A7 (Data source concordance, Epidemiological plausibility, etc.).
Protocol: Framework for Reproducible BWAS
This protocol describes best practices for conducting a reproducible Brain-Wide Association Study [1] [81].
1. Data Collection & Preprocessing:
- Sample Size Planning: Plan for the largest sample size possible, ideally in the thousands, based on expected effect sizes (|r| ~0.01-0.10).
- Rigorous Denoising: Apply strict denoising to neuroimaging data. For fMRI, use frame censoring (e.g., framewise displacement < 0.08 mm) to mitigate head motion effects.
- Standardize Processing: Use consistent, reproducible processing pipelines (e.g., those from Reproducible Brain Charts) across the entire dataset.
2. Predictive Modeling & Interpretation:
- Multivariate Model: Use multivariate methods (e.g., support vector regression, canonical correlation analysis) over univariate analyses.
- Cross-Validation: Train and test models within a nested cross-validation framework to avoid overfitting and obtain robust performance estimates.
- Feature Interpretation: Apply interpretability strategies:
- Beta Weights: Use regression coefficients from linear models, averaged over cross-validation folds.
- Stability Selection: Count the frequency of feature selection across resampling iterations.
- Virtual Lesion: Measure the drop in performance when a specific set of features (e.g., a brain network) is ablated from the model.
The Scientist's Toolkit: Research Reagent Solutions
| Tool / Resource | Type | Primary Function |
|---|---|---|
| RAG-HPO [96] | Software Tool | Extracts phenotypic phrases from clinical text and accurately maps them to HPO terms using Retrieval-Augmented Generation (RAG) with LLMs. |
| Semantic CharaParser [99] | NLP Tool | Parses character descriptions from comparative anatomy literature to generate Entity-Quality (EQ) phenotype annotations using ontologies. |
| MORE Framework [97] | Semantic Model | A hybrid multi-ontology and corpus-based model that learns accurate semantic representations (embeddings) of biomedical concepts. |
| UK Biobank [22] [1] | Data Resource | A large-scale biomedical database containing deep genetic, phenotypic, and imaging data from ~500,000 participants. |
| Reproducible Brain Charts (RBC) [16] | Data Resource | An open resource providing harmonized neuroimaging and psychiatric phenotype data, processed with uniform, reproducible pipelines. |
| Human Phenotype Ontology (HPO) [96] | Ontology | A standardized, hierarchical vocabulary for describing human phenotypic abnormalities. |
Workflow and Conceptual Diagrams
Multi-Source Phenotyping Framework
This diagram illustrates the computational framework for defining and validating disease phenotypes by integrating multiple data sources and ontologies [22].
RAG-HPO Workflow for Phenotype Extraction
This diagram details the workflow of the RAG-HPO tool, which uses Retrieval-Augmented Generation to improve HPO term assignment from clinical text [96].
Strategies for Interpreting Predictive Neuroimaging Models
This diagram outlines the three primary strategies for interpreting feature importance in regression-based predictive neuroimaging models [81].
Frequently Asked Questions (FAQs)
FAQ 1: What are normative brain charts and why are they suddenly critical for my research? Normative brain charts are standardized statistical references that model expected brain structure across the human lifespan, much like pediatric growth charts for height and weight. They are critical because they provide a benchmark to quantify individual-level deviations from a typical population, moving beyond simplistic group-level (case-control) comparisons. This shift is essential for personalized clinical decision-making and for understanding the biological heterogeneity underlying brain disorders [100] [101]. Without these charts, researchers risk building models that only work for stereotypical subgroups and fail for individuals who defy these profiles, a major pitfall in reproducible brain phenotype research [55].
FAQ 2: My brain-phenotype model performs well on average but fails for many individuals. Why? This common issue often stems from a "one-size-fits-all" modelling approach. Predictive models trained on heterogeneous datasets can learn not just the core cognitive construct but also the sociodemographic and clinical covariates intertwined with it in that specific sample. The model effectively learns a stereotypical profile. It subsequently fails for individuals who do not fit this profile, leading to reliable and structured—not random—model failure [55]. Normative charts help correct this by providing a standardized baseline to account for expected variation due to factors like age and sex.
FAQ 3: How can I validate a brain signature to ensure it is robust and generalizable? A robust validation requires demonstrating both spatial replicability and model fit replicability across independent datasets [25]. This involves:
- Discovery in large, heterogeneous cohorts: Use large samples to derive data-driven brain signatures associated with your behavioral outcome of interest.
- Consensus through resampling: Perform the discovery process across many randomly selected subsets of your discovery cohort and aggregate the results to create a consensus signature. This improves reproducibility [25].
- Independent validation: Test the explanatory power and model fit of your consensus signature on completely separate, held-out validation datasets [25].
FAQ 4: I have found a significant association between a plasma protein and a brain structure. How can I probe its potential causal nature and relevance to disease? A powerful framework for this involves Mendelian Randomization (MR). As demonstrated in large-scale studies, you can use genetic data to perform bidirectional MR analysis [102]:
- Causal Direction: Test if genetic variants influencing the protein level are associated with the brain structure, and vice-versa.
- Link to Disorders: Further, test if genetic variants influencing the protein level are associated with the risk of specific brain disorders. This can help triangulate the protein's potential causal role in disease pathogenesis via brain structure alterations.
Troubleshooting Guides
Problem: Model Performance is Inflated and Fails to Generalize
Symptoms: High accuracy/metrics in your training or discovery dataset, but a significant performance drop when applied to a new validation cohort or external dataset.
| Potential Cause | Diagnostic Checks | Corrective Actions |
|---|---|---|
| Insufficient Discovery Sample Size | Check if discovery set has fewer than several hundred participants [25]. | Aggregate data from multiple sites or use public data (e.g., UK Biobank) to increase discovery sample size into the thousands [25] [102]. |
| Unaccounted Site/Scanner Effects | Check if data comes from a single scanner or site. Model may fail on data from a new site. | Use statistical harmonization methods (e.g., ComBat) during preprocessing. Include site as a covariate in your normative model [100] [101]. |
| Biased Phenotypic Measures | Analyze if your phenotypic measure is correlated with sociodemographic factors (e.g., education, language). Check if model failure is systematic for certain subgroups [55]. | Use normative charts to derive deviation scores (centiles) that are adjusted for age and sex, isolating the phenotype of interest from expected population variation [100] [101]. |
Problem: High Uncertainty in Classifying Variants of Uncertain Significance (VUS)
Symptoms: In genetic studies of neurodevelopmental disorders, a high burden of VUS classifications limits clinical interpretation and biological insights.
| Potential Cause | Diagnostic Checks | Corrective Actions |
|---|---|---|
| Siloed Clinical Variant Data | Check if your variant is novel to ClinVar or has conflicting/uncertain classifications. One study found 42.5% of clinical variants were novel to ClinVar [103]. | Participate in or utilize data from registries like the Brain Gene Registry (BGR) that pair clinical variants with deep, standardized phenotypic data [103]. |
| Incomplete Phenotypic Profiling | Phenotypic information in genetic databases is often limited to test requisition forms, which can be inaccurate or incomplete [103]. | Implement a rapid virtual neurobehavioral assessment to systematically characterize domains like cognition, adaptive functioning, and motor/sensory skills [103]. |
Experimental Protocols & Workflows
Protocol 1: Creating a Normative Model for a Brain Structure Phenotype
This protocol outlines the steps to create a lifespan normative model for a neuroimaging-derived measure, such as cortical thickness or subcortical volume.
Data Curation and Harmonization:
Quality Control (QC):
- Perform both automated and manual QC on all neuroimaging data. Maintain a manually quality-checked subset for validation purposes [101].
Model Fitting:
Model Validation:
- Split data into training and test sets, stratified by site.
- Evaluate models using out-of-sample metrics that quantify central tendency and distributional accuracy (e.g., R², root mean squared error, Z-score deviation maps) [101].
- Package the pre-trained models with code to allow other researchers to transfer them to new datasets.
The following workflow diagram illustrates the key stages of this protocol:
Protocol 2: Validating a Robust Brain-Behavior Signature
This protocol details a method for computing and validating a data-driven brain signature for a behavioral domain (e.g., episodic memory).
Discovery of Consensus Signature:
- Within your discovery cohort, randomly select multiple subsets (e.g., 40 subsets of size 400) [25].
- In each subset, perform a voxel- or vertex-wise analysis to identify brain areas associated with the behavioral outcome.
- Aggregate results across all iterations to create a spatial overlap frequency map. Define high-frequency regions as your "consensus signature" mask [25].
Validation of Signature:
- Apply the consensus signature mask to independent validation datasets.
- Evaluate the model's explanatory power for the behavioral outcome in the validation sets.
- Compare the performance of your data-driven signature model against theory-driven or lesion-driven models [25].
The logical flow of the signature validation process is shown below:
Key Data and Quantitative Summaries
Table 1: Key Metrics from Large-Scale Normative Charting Studies
| Study / Dataset | Sample Size (N) | Age Range | Key Finding / Metric |
|---|---|---|---|
| Lifespan Brain Charts [100] | >100,000 | 16 pcw - 100 years | Cortical GM volume peaks at 5.9 years; WM volume peaks at 28.7 years. |
| High-Spatial Precision Charts [101] | 58,836 | 2 - 100 years | Models explained up to 80% of variance (R²) out-of-sample for cortical thickness. |
| UK Biobank Proteomics [102] | 4,900 | ~63 years (mean) | Identified 5,358 significant associations between 1,143 plasma proteins and 256 brain structure measures. |
| Item / Resource | Function / Purpose | Example from Literature |
|---|---|---|
| Large-Scale Neuroimaging Datasets (e.g., UK Biobank, ADNI) | Provide the necessary sample size and heterogeneity for discovery and validation of robust phenotypes. | UK Biobank (N=4,997+) used to map proteomic signatures of brain structure [102]. |
| Data Harmonization Tools (e.g., ComBat, Deep Learning methods) | Reduce site and scanner effects in multi-site data, increasing generalizability. | Statistically-based methods were used in initial brain charts; deep-learning methods show promise for improved performance [100]. |
| Normative Modeling Software (e.g., PCNtoolkit) | Enables fitting of normative models to quantify individual deviations from a reference population. | Used to create lifespan charts for cortical thickness and subcortical volume [101]. |
| Genetic & Phenotypic Registries (e.g., Brain Gene Registry - BGR) | Provides paired genomic and deep phenotypic data to accelerate variant interpretation and gene-disease validity curation. | BGR found 34.6% of clinical variants were absent from all major genetic databases [103]. |
| Mendelian Randomization (MR) Framework | A statistical method using genetic variants to probe causal relationships between an exposure (e.g., protein) and an outcome (e.g., brain structure/disease). | Used to identify 33 putative causal associations between 32 proteins and 23 brain measures [102]. |
Conclusion
The path to reproducible brain-phenotype signatures requires a fundamental shift from small-scale, isolated studies to large-scale, collaborative, and open science. Success hinges on assembling large, diverse samples, implementing rigorous and harmonized processing methods, and adopting transparent, robust validation practices. The convergence of advanced computational frameworks, predictive modeling, and precision neurodiversity approaches offers unprecedented opportunity. For clinical translation and drug development, future efforts must focus on establishing standardized benchmarks, developing dynamic and multimodal brain charts, and demonstrating incremental validity over existing biomarkers. By systematically overcoming these pitfalls, the field can move toward generalizable and clinically actionable insights that truly advance our understanding of the brain in health and disease.
References
- 1. Reproducible brain-wide association studies require ... [https://www.nature.com/articles/s41586-022-04492-9]
- 2. Stats Study Reveals Reason for Replication Crisis in ... [https://www.technologynetworks.com/neuroscience/news/stats-study-reveals-reason-for-replicability-crisis-in-neuroscience-359637]
- 3. Opportunities for increased reproducibility and replicability of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7779745/]
- 4. Longer scans boost prediction and cut costs in brain-wide ... [https://www.nature.com/articles/s41586-025-09250-1]
- 5. Performance reserves in brain-imaging-based phenotype ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11215805/]
- 6. BrainEffeX: A web app for exploring fMRI effect sizes [https://apertureneuro.org/article/146251-braineffex-a-web-app-for-exploring-fmri-effect-sizes]
- 7. Sample size determination: A practical guide for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000262/]
- 8. Brain–phenotype models fail for individuals who defy ... [https://www.nature.com/articles/s41586-022-05118-w]
- 9. Data Integration Methods for Phenotype Harmonization in ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2019.01227/full]
- 10. Harmonizing bifactor models of psychopathology between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10485343/]
- 11. Reliability and Validity of Bifactor Models of Dimensional ... [https://www.medrxiv.org/content/10.1101/2021.06.27.21259601v1]
- 12. Toward identifying reproducible brain signatures of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7023814/]
- 13. Removing inter-subject technical variability in magnetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5540379/]
- 14. Systematic evaluation of fMRI data-processing pipelines for ... [https://www.nature.com/articles/s41467-024-48781-5]
- 15. Practical guidance to identify and troubleshoot suboptimal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10913595/]
- 16. Reproducible Brain Charts: An open data resource for ... [https://www.sciencedirect.com/science/article/abs/pii/S0896627325006610]
- 17. Balancing Data Quality and Bias: Investigating Functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11717557/]
- 18. Getting to know EEG artifacts and how to handle them in ... [https://pressrelease.brainproducts.com/eeg-artifacts-handling-in-analyzer/]
- 19. EEG Artifacts: Types, Detection, and Removal Techniques ... [https://www.bitbrain.com/blog/eeg-artifacts]
- 20. The art and science of using quality control to understand ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1100544/full]
- 21. Signature methods for brain-computer interfaces [https://www.nature.com/articles/s41598-023-41326-8]
- 22. A computational framework for defining and validating ... [https://www.nature.com/articles/s41598-025-05838-9]
- 23. The most prevalent perceived barriers to sharing research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12375187/]
- 24. Balancing ethical data sharing and open science for ... [https://www.sciencedirect.com/science/article/pii/S2666379125001533]
- 25. Toward a statistical validation of brain signatures as robust ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10171525/]
- 26. 'Science by consensus' impedes scientific creativity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11126901/]
- 27. Science and innovation relies on successful collaboration [https://www.weforum.org/stories/2022/02/why-collaboration-is-key-to-scientific-discovery/]
- 28. Freesurfer License Problems · Issue #2164 · nipreps/fmriprep [https://github.com/poldracklab/fmriprep/issues/2164]
- 29. Troubleshooting and Help - C-PAC 1.8.7.dev1 Beta ... [https://fcp-indi.github.io/docs/latest/user/help]
- 30. C-PAC fMRI data preproc-docs [https://github.com/GT-EmoryMINDlab/preproc-docs]
- 31. ReleaseNotes - Free Surfer Wiki [https://surfer.nmr.mgh.harvard.edu/fswiki/ReleaseNotes]
- 32. What's new — fmriprep version documentation [https://fmriprep.org/en/25.0.0/changes.html]
- 33. Open-source platforms to investigate analytical flexibility in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12330840/]
- 34. Basic principles — DataLad 1.2.3 documentation [http://docs.datalad.org/en/stable/basics.html]
- 35. Reliability and Validity of Bifactor Models of Dimensional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9328119/]
- 36. Variability and Reproducibility of Brain Imaging | Frontiers Research ... [https://www.frontiersin.org/research-topics/45300/variability-and-reproducibility-of-brain-imaging/authors]
- 37. Challenges to reproducible predictive modeling in resting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8942606/]
- 38. Using connectome-based predictive modeling to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5526681/]
- 39. Connectome-based predictive modeling of attention [https://www.sciencedirect.com/science/article/abs/pii/S1053811917309175]
- 40. Precision neurodiversity: personalized brain network ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1669431/full]
- 41. Does the current state of biomarker discovery in autism reflect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9992810/]
- 42. Major autism study uncovers biologically distinct subtypes, ... [https://www.princeton.edu/news/2025/07/09/major-autism-study-uncovers-biologically-distinct-subtypes-paving-way-precision]
- 43. personalized brain network architecture as a window into ... [https://doaj.org/article/a375663b3dc44954ae1c46c256384fed]
- 44. Neurodiversity FAQ [https://thinkingautismguide.com/neurodiversity-faq]
- 45. Current challenges and future directions for brain age ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368027/]
- 46. Pitfalls in brain age analyses - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8357007/]
- 47. Pitfalls in brain age analyses - PubMed [https://pubmed.ncbi.nlm.nih.gov/34190372/]
- 48. BASE: Brain Age Standardized Evaluation [https://www.sciencedirect.com/science/article/pii/S1053811923006183]
- 49. A systematic review of multimodal brain age studies [https://www.sciencedirect.com/science/article/pii/S2666389923000491]
- 50. Prediction of brain age using structural magnetic ... [https://www.medrxiv.org/content/10.1101/2025.03.13.25323902v3.full-text]
- 51. Deep-learning based multi-modal models for brain age ... [https://alzres.biomedcentral.com/articles/10.1186/s13195-025-01773-z]
- 52. Quantitative assessment of neurodevelopmental maturation [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2024.1496143/full]
- 53. Image harmonization: A review of statistical and deep ... [https://www.sciencedirect.com/science/article/pii/S1053811923002719]
- 54. An evaluation of image-based and statistical techniques for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12330838/]
- 55. Brain–phenotype models fail for individuals who defy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9433326/]
- 56. Quality Control in Manufacturing: Overview and Best ... [https://www.6sigma.us/manufacturing/quality-control-in-manufacturing/]
- 57. Quality Control Procedures & Process: How to Ensure ... - Whale [https://usewhale.io/blog/quality-control-procedures/]
- 58. Sigma metrics - A guide to quality control strategy in clinical ... [https://ijcbr.in/archive/volume/7/issue/2/article/15336]
- 59. Basic QC Practices [https://www.westgard.com/qc-applications/basic-qc-practices/qcapp10.html]
- 60. A Guide to Effective Troubleshooting in Experimental Design ... [https://www.bioprecisioncrafted.ca/post/uncovering-the-root-causes-a-guide-to-effective-troubleshooting-in-experimental-design-failures]
- 61. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 62. Teaching troubleshooting skills to graduate students - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11407763/]
- 63. Establishing a framework for best practices for quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10861687/]
- 64. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 65. Detecting a Dataset Shift in PHI Data to Ensure De- ... [https://medium.com/john-snow-labs/detecting-a-dataset-shift-in-phi-data-to-ensure-de-identification-model-performance-on-future-data-f42043d0c09b]
- 66. Dataset shift assessment measures in monitoring ... [https://www.sciencedirect.com/science/article/pii/S1877050921018512]
- 67. Lecture 7: Troubleshooting Deep Neural Networks [https://fullstackdeeplearning.com/spring2021/lecture-7/]
- 68. The Lazy Data Scientist's Guide to AI/ML Troubleshooting [https://odsc.medium.com/the-lazy-data-scientists-guide-to-ai-ml-troubleshooting-abaf20479317?source=post_internal_links---------0----------------------------]
- 69. Fix Model Training Errors: Overfitting & Data Imbalance [https://viso.ai/deep-learning/model-training-errors/]
- 70. The State of Data and AI Engineering 2025 [https://lakefs.io/blog/the-state-of-data-ai-engineering-2025/]
- 71. Age-level bias correction in brain age prediction [https://www.sciencedirect.com/science/article/pii/S2213158223000086]
- 72. Topological turning points across the human lifespan [https://www.nature.com/articles/s41467-025-65974-8]
- 73. Bioinformatics Pipeline Troubleshooting [https://www.meegle.com/en_us/topics/bioinformatics-pipeline/bioinformatics-pipeline-troubleshooting]
- 74. Development of the Biological Experimental Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4152214/]
- 75. Unlocking the Power of Explainable AI in Modern Tech [https://viso.ai/deep-learning/explainable-ai/]
- 76. ML and AI Model Explainability and Interpretability [https://www.analyticsvidhya.com/blog/2025/01/explainability-and-interpretability/]
- 77. Explainable Artificial Intelligence in the Field of Drug Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12129466/]
- 78. Interpretable and explainable machine learning methods ... [https://link.springer.com/article/10.1007/s10462-025-11399-0]
- 79. Overview of Challenges in Brain-based Predictive Modeling [https://www.sciencedirect.com/science/article/pii/S000632232501460X]
- 80. Characterizing changes to individual-specific brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12263593/]
- 81. Interpreting Brain Biomarkers: Challenges and solutions in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9880880/]
- 82. Brain-phenotype predictions can survive across diverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10849571/]
- 83. Brain-phenotype predictions of language and executive ... [https://www.sciencedirect.com/science/article/pii/S1878929324001257]
- 84. Solving the Reproducibility Problem in Biomedical Research [https://www.kolaido.com/solving-the-reproducibility-problem-in-biomedical-research/]
- 85. A Practical Guide for Improving Transparency and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4936733/]
- 86. Power and reproducibility in the external validation of brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10634903/]
- 87. Global Biobank Meta-analysis Initiative: Powering genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9903716/]
- 88. From Big Data to the Clinic: Methodological and Statistical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11837031/]
- 89. The ABCD study: understanding the development of risk for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7304245/]
- 90. Reproducibility in Neuroimaging Analysis: Challenges and ... [https://www.sciencedirect.com/science/article/abs/pii/S245190222200341X]
- 91. Highlight Results, Don't Hide Them: Enhance interpretation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10233921/]
- 92. Genetic Signatures Predict Social-Cognitive Trajectories in ... [https://www.sciencedirect.com/science/article/pii/S1876201825003922]
- 93. Chapter 15 Experimental protocols | Lab Handbook [https://ccmorey.github.io/labHandbook/experimental-protocols.html]
- 94. A guideline for reporting experimental protocols in life sciences [https://pmc.ncbi.nlm.nih.gov/articles/PMC5978404/]
- 95. A common neural signature between genetic and ... [https://www.nature.com/articles/s41398-025-03513-1]
- 96. Improving automated deep phenotyping through large ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01521-w]
- 97. A hybrid multi-ontology and corpus-based semantic ... [https://www.sciencedirect.com/science/article/pii/S1532046420302094]
- 98. A Quick Guide to Organizing Computational Biology Projects [https://pmc.ncbi.nlm.nih.gov/articles/PMC2709440/]
- 99. Annotation of phenotypes using ontologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC6301375/]
- 100. Charting Normative Brain Variability Across the Human Lifespan [https://pmc.ncbi.nlm.nih.gov/articles/PMC9905390/]
- 101. Charting brain growth and aging at high spatial precision [https://elifesciences.org/articles/72904]
- 102. Atlas of proteomic signatures of brain structure and its links ... [https://www.nature.com/articles/s41467-025-60185-7]
- 103. Clinical variants paired with phenotype: A rich resource for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10939875/]