Validating Brain Signatures Across Multiple Cohorts: A Roadmap for Robust Biomarker Development in Neuroscience
This article provides a comprehensive framework for the development and validation of brain signatures as reliable biomarkers across independent cohorts—a critical step for their translation into clinical and research applications.
Validating Brain Signatures Across Multiple Cohorts: A Roadmap for Robust Biomarker Development in Neuroscience
Abstract
This article provides a comprehensive framework for the development and validation of brain signatures as reliable biomarkers across independent cohorts—a critical step for their translation into clinical and research applications. We explore the foundational concepts of data-driven brain signatures and their evolution from theory-based approaches. The article details rigorous methodological frameworks, including multi-cohort discovery designs and machine learning applications, that enhance generalizability. It addresses common pitfalls in reproducibility and offers optimization strategies for handling cohort heterogeneity and data integration challenges. Finally, we present established validation protocols and comparative analyses demonstrating how validated multi-cohort signatures outperform traditional measures in explaining behavioral outcomes and predicting clinical status. This guide equips researchers and drug development professionals with practical strategies for creating neurologically informative and clinically actionable biomarkers.
The Foundation of Brain Signatures: From Theoretical Constructs to Data-Driven Discovery
In the pursuit of translating neurobiological insights into clinical applications, the field of cognitive neuroscience has increasingly embraced data-driven approaches to delineate robust brain-behavior relationships. The concept of a "brain signature" has emerged as a powerful paradigm, referring to a data-driven, exploratory approach to identify key brain regions most strongly associated with specific cognitive functions or behavioral outcomes [1]. Unlike theory-driven or lesion-based approaches that dominated earlier research, brain signatures aim to characterize brain substrates of behavioral outcomes through comprehensive exploratory searches that select features based solely on performance metrics of prediction or classification [2]. This methodological evolution has been catalyzed by the availability of larger datasets, improved computational resources, and high-quality brain parcellation atlases that enable more comprehensive mapping of brain-behavior associations [1].
Statistical Regions of Interest (sROIs or statROIs) represent a core implementation of the brain signature concept, providing an alternative to predefined anatomical atlas regions [1]. The fundamental advantage of this approach lies in its ability to detect associations that may cross traditional ROI boundaries, potentially recruiting subsets of multiple regions without using the entirety of any single region [1]. This property allows sROIs to more accurately reflect the underlying brain architecture supporting specific cognitive functions or affected by pathological processes. The clinical promise of this approach is substantial—by providing maximally informative biomarkers, validated brain signatures could enhance early diagnosis, improve prognostic accuracy, guide targeted interventions, and serve as endpoints in clinical trials for neurological and psychiatric disorders [2] [3].
Methodological Framework: Computational Approaches for Signature Derivation
Core Computational Techniques
The derivation of brain signatures employs diverse computational techniques ranging from voxel-wise parametric methods to multivariate machine learning algorithms. Voxel-aggregation approaches implement direct computation of voxel-based regressions with multiple comparison corrections to generate regional masks corresponding to different association strength levels with behavioral outcomes [2]. This method delineates 'non-standard' regions that may not conform to prespecified atlas parcellations but more accurately reflect relevant brain architecture. Machine learning techniques include support vector machines (SVM) for classification [3], relevant vector regression (RVR) for predicting continuous variables [1] [2], and deep learning using convolutional neural nets [1]. Additionally, multivariate pattern analysis methods leverage information distributed across multiple brain systems to provide quantitative, falsifiable predictions and establish mappings between brain and mind [4].
Table 1: Computational Techniques for Brain Signature Derivation
| Technique | Primary Use | Key Advantages | Limitations |
|---|---|---|---|
| Voxel-Wise Regression & Aggregation | Continuous outcomes | Creates non-atlas dependent regions; High interpretability | Computationally intensive for large datasets |
| Support Vector Machines (SVM) | Binary classification | Effective for categorical outcomes; Handles high-dimensional data | Limited native probabilistic output |
| Relevant Vector Regression (RVR) | Continuous outcomes | Sparse solution; Probabilistic predictions | Model can be like a "black box" |
| Spatial Patterns of Abnormalities (SPARE) Framework | Disease severity indexing | Quantifies individual-level expression; Cross-validated | Requires large training datasets |
| Multivariate Information Theory | High-order interactions | Captures synergistic subsystems beyond pairwise correlations | Computationally complex; Emerging methodology |
Essential Methodological Considerations
Several methodological considerations are critical for deriving robust brain signatures. Feature selection must balance comprehensiveness with specificity, avoiding both overly restrictive anatomical constraints and uncontrolled multiple comparisons. Model interpretability remains challenging, particularly for complex machine learning approaches, though methods like layer-wise relevance propagation are emerging to address this "black box" problem [1]. Statistical validation requires rigorous approaches, including surrogate time series to assess coupling significance and bootstrap techniques to generate confidence intervals for individual estimates [5]. The level of analysis must also be considered—while pairwise functional connectivity has been valuable, high-order interactions (HOIs) investigating statistical interactions involving more than two network nodes may better capture the brain's functional complexity [5].
Validation Protocols: Ensuring Robustness and Generalizability
Multi-Cohort Validation Framework
Robust validation of brain signatures requires demonstrating replicability across multiple independent datasets beyond the discovery set where they were developed [1]. The validation protocol encompasses two key properties: model fit replicability (consistent performance in explaining outcome variance) and spatial extent replicability (consistent selection of signature regions across cohorts) [1]. A rigorous approach involves:
- Discovery in multiple subsets: Deriving regional brain associations in numerous randomly selected discovery subsets (e.g., 40 subsets of size 400) within each cohort [1].
- Consensus mask generation: Creating spatial overlap frequency maps and defining high-frequency regions as "consensus" signature masks [1].
- Independent validation: Evaluating replicability using completely separate validation datasets [1] [2].
- Performance comparison: Comparing signature model fits with each other and with competing theory-based models [1].
This protocol was successfully implemented in a 2023 study validating gray matter thickness signatures for memory domains, which demonstrated that consensus signature model fits were highly correlated across validation cohorts and outperformed other models [1].
Handling Population Heterogeneity
Population heterogeneity represents a significant challenge for brain signature validation. Demographic differences and other factors outside primary scientific interest can substantially impact predictive accuracy and pattern stability [6]. Evidence suggests that larger, more diverse cohorts often yield poorer prediction performance despite better representing true population diversity [6]. Propensity scores can serve as a composite confound index to quantify diversity arising from major sources of population variation [6]. Studies indicate that population heterogeneity particularly affects pattern stability in default mode network regions [6], highlighting the limitations of prevailing deconfounding practices and the need for explicit consideration of diversity in validation frameworks.
Experimental Protocols: From Signature Derivation to Application
Protocol 1: Voxel-Based Signature Derivation for Continuous Outcomes
This protocol details the derivation of brain signatures for continuous behavioral outcomes (e.g., cognitive test scores) using voxel-based methods:
- Image Processing: Process T1-weighted structural images through pipelines including brain extraction, tissue segmentation, and registration to standardized space [1] [2].
- Voxel-Wise Analysis: Perform whole-brain voxel-wise regression between gray matter measures and the behavioral outcome, correcting for multiple comparisons [2].
- Threshold Determination: Establish association strength thresholds based on statistical significance and spatial extent criteria [2].
- Region Aggregation: Aggregate significant voxels into contiguous regions, applying morphological operations to ensure spatial coherence [2].
- Mask Creation: Create binary masks representing the signature regions in standardized template space [2].
This approach has successfully generated replicable signatures for episodic memory performance in cohorts encompassing normal cognition, mild cognitive impairment, and dementia [2].
Protocol 2: Machine Learning-Based Signature Derivation
This protocol outlines the use of machine learning for deriving brain signatures, as implemented in the SPARE (Spatial Patterns of Abnormalities for Recognition) framework [3]:
- Data Harmonization: Process and harmonize MRI data across multiple cohorts to minimize site effects [3].
- Feature Extraction: Extract comprehensive neuroimaging features from structural MRI, including regional volumes, cortical thickness, and white matter hyperintensities [3].
- Model Training: Train support vector classification models to distinguish between presence and absence of specific conditions using neuroimaging patterns [3].
- Pattern Expression Scoring: Compute individual expression scores for each participant, reflecting the degree to which their brain features match the signature pattern [3].
- Validation: Validate models in independent datasets and assess robustness across demographic subgroups [3].
This protocol has been successfully applied to derive signatures for various cardiovascular and metabolic risk factors in cognitively unimpaired individuals [3].
Clinical Applications and Exemplary Findings
Validated Signatures Across Domains
Brain signature approaches have yielded robust, clinically relevant biomarkers across multiple domains:
Table 2: Exemplary Validated Brain Signatures and Their Characteristics
| Domain | Signature Basis | Key Brain Regions | Clinical Application | Validation Status |
|---|---|---|---|---|
| Episodic Memory | Gray matter thickness | Medial temporal, precuneus, temporal regions [2] | Tracking cognitive decline in aging and early AD [2] | Validated across 3 independent cohorts [2] |
| Everyday Memory | Gray matter thickness | Strongly shared substrates with neuropsychological memory [1] | Assessing subtle functional changes in older adults [1] | Cross-validated in UCD and ADNI cohorts [1] |
| Social Inference | fMRI activation patterns | Right pSTS, TPJ, temporal poles, mPFC [7] | Predicting real-world social contacts; ASD assessment [7] | Validated in neurotypical and ASD samples [7] |
| Cardiovascular & Metabolic Risks | Structural MRI patterns | Frontal GM, insula, temporal regions [3] | Early risk detection in cognitively unimpaired [3] | Large multinational dataset (N=37,096) [3] |
| Preclinical AD | Glucose metabolism | Precuneus, posterior cingulate, temporal gyrus [8] | Ultra-early diagnosis in cognitively normal [8] | Cross-validated in Chinese and American cohorts [8] |
Performance Metrics and Effect Sizes
Quantitative performance assessments demonstrate the utility of validated brain signatures:
- Episodic memory signatures derived through voxel-aggregation approaches better explained baseline and longitudinal memory than theory-driven 'standard' models and other data-driven models [2].
- Cardiometabolic risk signatures developed using machine learning outperformed conventional structural MRI markers with a ten-fold increase in effect sizes and detected subtle patterns at sub-clinical stages [3].
- Social inference signatures predicted the number of real-life social contacts in neurotypical adults and autism symptom severity in ASD individuals, demonstrating generalization to neurodiverse populations [7].
- Preclinical AD metabolic patterns showed significant correlations with CSF tau biomarkers but not with amyloid deposition, suggesting sensitivity to downstream neurodegeneration [8].
Successful brain signature research requires specific data resources and analytical tools:
Table 3: Essential Resources for Brain Signature Research
| Resource Category | Specific Examples | Key Utility | Access Considerations |
|---|---|---|---|
| Multi-Cohort Datasets | ADNI, UC Davis Aging and Diversity Cohort, UK Biobank, iSTAGING [1] [8] [3] | Provides diverse samples for discovery and validation | Data use agreements; Ethical approvals |
| Image Processing Pipelines | FreeSurfer, SPM, FSL, CNN-based extraction [1] [2] | Standardized feature extraction | Computational infrastructure requirements |
| Statistical Platforms | R, Python (scikit-learn, nilearn) [3] [6] | Implementation of machine learning models | Open-source with specific dependency packages |
| Validation Frameworks | Cross-validation utilities, permutation testing tools [7] [5] | Robust validation of signature performance | Custom implementation often required |
| Cloud Computing Resources | XSEDE, Google Cloud Platform, AWS [3] | Handles computational demands of large datasets | Cost and data transfer considerations |
Methodological Considerations for Implementation
When implementing brain signature research, several methodological considerations prove critical:
- Cohort Size and Diversity: Signatures derived from discovery sets numbering in the thousands demonstrate better replicability, with heterogeneous cohorts better representing true population variability [1] [6].
- Multisite Harmonization: When pooling data across multiple acquisition sites, implementing harmonization techniques is essential to mitigate site effects while preserving biological variability [3] [6].
- Statistical Power Considerations: Pitfalls of using undersized discovery sets include inflated strengths of associations and loss of reproducibility [1].
- Clinical Ground Truth: Precise phenotypic characterization and standardized behavioral assessment are crucial for meaningful signature development [1] [7].
The development of validated brain signatures represents a paradigm shift in neuroimaging research, moving from localized brain-behavior associations toward integrated, predictive models of mental events that leverage information distributed across multiple brain systems [4]. The methodological framework outlined—encompassing rigorous multi-cohort validation, sophisticated computational approaches, and attention to population heterogeneity—provides a roadmap for creating robust biomarkers with genuine clinical utility.
The most promising future directions include: (1) the integration of multimodal imaging data to capture complementary aspects of brain structure and function; (2) the development of dynamic signatures that track change over time; (3) the application of high-order interaction analyses to capture the complex, synergistic nature of brain networks [5]; and (4) the implementation of federated learning approaches to leverage large datasets while preserving privacy. As these methodologies mature and validation standards become more rigorous, brain signatures are poised to transition from research tools to clinically useful biomarkers, ultimately fulfilling their promise for precision medicine in neurology and psychiatry.
The Evolution from Theory-Driven to Data-Driven Exploratory Approaches
Human neuroimaging research has undergone a significant paradigm shift, transitioning from traditional brain mapping approaches toward developing integrated, multivariate brain models of mental events [9]. Traditional theory-driven methods analyzed brain-mind associations within isolated brain regions or voxels tested one at a time, treating local brain responses as outcomes to be explained by statistical models [9]. This approach was grounded in modular views of mental processes implemented in isolated brain regions, often informed by lesion studies [9]. In recent years, the "brain signature of cognition" concept has garnered interest as a data-driven, exploratory approach to better understand key brain regions involved in specific cognitive functions, with the potential to maximally characterize brain substrates of behavioral outcomes [1] [10]. This evolution represents a fundamental reorientation: where traditional approaches analyzed brain responses as outcomes, modern predictive models specify how to combine brain measurements to predict mental states and behavior [9].
Table 1: Core Differences Between Theory-Driven and Data-Driven Approaches
| Feature | Theory-Driven Approaches | Data-Driven Exploratory Approaches |
|---|---|---|
| Theoretical Basis | Modular view of mental processes [9] | Population coding and distributed representation [9] |
| Analysis Focus | Isolated brain regions/voxels [9] | Multivariate patterns across brain systems [9] |
| Primary Outcome | Local brain responses [9] | Behavioral and mental state predictions [1] |
| ROI Definition | Predefined anatomical or functional regions [1] | Data-driven statistical ROIs (sROIs) [1] |
| Validation Approach | Single-cohort hypothesis testing | Multi-cohort replicability and model fit [1] |
| Information Encoding | Assumed localized encoding | Distributed population coding [9] |
Theoretical Foundations and Advantages
Theoretical Underpinnings of Data-Driven Approaches
Data-driven exploratory approaches emerge from theories grounded in neural population coding and distributed representation [9]. Neurophysiological studies have established that information about mind and behavior is encoded in the activity of intermixed populations of neurons, where joint activity across cell populations often predicts behavior more accurately than individual neurons [9]. This distributed representation permits combinatorial coding, providing the capacity to represent extensive information with limited neural resources [9]. Multivariate modeling of how activity spanning many brain voxels jointly encodes behavioral outcomes represents an extension of these population coding concepts to human neuroimaging [9].
Advantages of Data-Driven Signature Approaches
Data-driven brain signature approaches offer several distinct advantages over traditional methods:
- Larger Effect Sizes: Multivariate models demonstrate larger effect sizes in brain-outcome associations than standard local region-based approaches [9].
- Quantitative Predictions: These models provide quantitative predictions about outcomes that can be empirically falsified, moving beyond descriptive mapping [9].
- Cross-Validation Capability: Models with defined measurement properties can be tested and validated across studies and laboratories [1] [10].
- Boundary Flexibility: Unlike predefined ROI approaches that may miss associations crossing ROI boundaries, signature approaches can detect subtle effects that recruit subsets of multiple regions [1].
- Interpretative Power: The approach offers a path toward validating mental constructs and understanding how psychological distinctions parallel neurological ones [9].
Quantitative Validation Metrics Across Cohorts
Rigorous validation across multiple cohorts is essential for establishing robust brain signatures. Recent research demonstrates the performance advantages of data-driven signature approaches when validated across independent datasets.
Table 2: Validation Metrics for Brain Signature Models Across Cohorts
| Validation Metric | Discovery Cohorts (UCD & ADNI 3) | Validation Cohorts (UCD & ADNI 1) | Performance Outcome |
|---|---|---|---|
| Sample Size | 578 (UCD), 831 (ADNI 3) [1] | 348 (UCD), 435 (ADNI 1) [1] | Large samples enable replicability [1] |
| Discovery Subsets | 40 randomly selected subsets of size 400 [1] | 50 random subsets for replicability testing [1] | High replicability in validation subsets [1] |
| Spatial Convergence | Convergent consensus signature regions [1] | Spatial replication produced convergent regions [1] | High-frequency regions defined as consensus masks [1] |
| Model Fit Correlation | N/A | Highly correlated in validation subsets [1] | Indicates high replicability [1] |
| Explanatory Power | Signature models developed | Outperformed theory-based models in full cohorts [1] | Better explanatory power than competing models [1] |
Application Notes: Implementing Data-Driven Signature Methods
Protocol 1: Computing Robust Gray Matter Signatures for Behavioral Domains
Purpose: To compute data-driven brain signatures of behavioral domains (e.g., episodic memory, everyday cognition) that replicate across multiple cohorts.
Materials and Reagents:
- Structural T1-weighted MRI scans
- Gray matter thickness pipeline [1]
- Cognitive assessment batteries (e.g., SENAS, ADNI-Mem) [1]
- Everyday function measures (e.g., ECog) [1]
- High-performance computing resources
Procedure:
- Cohort Selection: Identify discovery and validation cohorts with appropriate sample sizes (N > 400 per cohort) [1].
- Image Processing:
- Cognitive Assessment: Administer standardized neuropsychological tests (e.g., episodic memory tests) and everyday function measures (e.g., ECog) [1].
- Discovery Phase:
- Validation Phase:
Troubleshooting:
- If discovery-validation bias appears, increase discovery sample size or number of random subsets [1].
- For poor spatial convergence, ensure cohort heterogeneity representing full variability in pathology and cognition [1].
Protocol 2: Identifying Endogenous Brain States Through Trial-Variability Clustering
Purpose: To discover endogenous brain state variability relevant to cognition using data-driven clustering of trial-level activity.
Materials and Reagents:
- High-density EEG system
- Behavioral task with multiple coherence levels (e.g., motion discrimination) [11]
- Modularity-maximization clustering algorithms [11]
- Computational modeling frameworks for decision thresholds [11]
Procedure:
- Experimental Design:
- EEG Acquisition: Collect high-density EEG data throughout task performance [11].
- Data-Driven Clustering:
- Behavioral Correlation:
- Computational Modeling:
Troubleshooting:
- If clusters do not separate cleanly, optimize modularity parameters or feature selection.
- For weak behavioral correlations, increase trial numbers or optimize task design.
Brain Signature Development and Validation Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Computational Tools
| Tool/Reagent | Specification | Function/Application |
|---|---|---|
| Structural MRI T1-weighted | High-resolution 3D sequences | Gray matter thickness measurement and voxel-based morphometry [1] |
| Cognitive Batteries | SENAS, ADNI-Mem, ECog | Standardized assessment of episodic memory and everyday function [1] |
| EEG Systems | High-density (64+ channels) | Recording spatial-temporal brain activity patterns during tasks [11] |
| Modularity-Maximization Clustering | Data-driven algorithm | Identifying consistent spatial-temporal EEG patterns across trials [11] |
| Voxel-Based Regression | Whole-brain analysis | Computing regional brain-behavior associations without predefined ROIs [1] |
| Computational Decision Models | Threshold adjustment frameworks | Interpreting behavioral differences between brain state subtypes [11] |
| Population Coding Frameworks | Theoretical foundation | Guiding multivariate analysis based on distributed neural representation [9] |
Discussion and Future Directions
The evolution from theory-driven to data-driven exploratory approaches represents a fundamental advancement in cognitive neuroscience methodology. Data-driven brain signatures offer robust, replicable measures for modeling substrates of behavioral domains, outperforming traditional theory-based models in explanatory power [1] [10]. The strength of these approaches lies in their ability to detect distributed patterns that cross traditional anatomical boundaries and their capacity for quantitative prediction and cross-validation [9].
Future developments in this field will likely focus on several key areas. First, addressing the interpretability challenges of complex multivariate models, particularly as machine learning and deep learning approaches become more prevalent [1]. Second, developing standardized protocols for multi-cohort validation to ensure robustness across diverse populations. Third, integrating multimodal data (fMRI, EEG, structural imaging) to create more comprehensive models of brain-behavior relationships [9]. Finally, establishing clearer connections between population coding principles from cellular neuroscience and distributed representations in human neuroimaging [9].
The paradigm shift toward data-driven exploratory approaches positions the field to develop increasingly accurate models of how distributed brain patterns represent mental constructs, ultimately advancing both basic neuroscience and clinical applications in drug development and personalized medicine.
The "brain signature of cognition" concept has garnered significant interest as a data-driven, exploratory approach to better understand key brain regions involved in specific cognitive functions [1]. This paradigm represents an evolution from theory-driven or lesion-driven approaches, offering the potential to more completely characterize brain substrates of behavioral outcomes by discovering statistical regions of interest (sROIs or statROIs) associated with specific cognitive domains [1]. The validation of robust brain signatures across multiple cohorts represents a critical advancement for neuroscience research and drug development, providing reliable measures for modeling the neuroanatomical substrates of behavioral domains.
For brain signatures to be considered robust biological measures, they require rigorous validation of model performance across diverse cohorts [1]. This includes demonstrating both spatial replicability (consistent identification of signature brain regions across discovery datasets) and model fit replicability (consistent explanatory power for behavioral outcomes in independent validation datasets) [1]. The emergence of large-scale neuroimaging datasets has enabled the development of signature approaches that can overcome limitations of earlier methods, which potentially missed subtler but significant effects in brain-behavior associations [1].
Domain-Specific Brain Signatures: Application Notes
Episodic Memory Signature
Episodic memory, the ability to encode, store, and retrieve personal experiences, has been a primary focus for brain signature development. Validation studies have employed neuropsychological assessments such as the Spanish and English Neuropsychological Assessment Scales (SENAS) and the ADNI memory composite (ADNI-Mem) to quantify episodic memory performance [1]. These instruments are specifically designed to be sensitive to individual differences across the full range of episodic memory performance, from intact to impaired functioning.
Research has established that robust episodic memory signatures involve distributed brain networks rather than isolated regions. The validation of these signatures requires demonstrating that model fits to outcome are highly correlated across multiple random subsets of validation cohorts, indicating high replicability [1]. When properly validated, signature models for episodic memory have been shown to outperform other commonly used neuroanatomical measures in explanatory power [1].
Everyday Cognition Signature
Everyday cognition represents a crucial domain for assessing functional impact of cognitive changes, measured through informant-based scales such as the Everyday Cognition scales (ECog) [1]. The ECog is specifically designed to address functional abilities of older adults, focusing on subtle changes in everyday function spanning preclinical Alzheimer's disease to moderate dementia [1]. This domain captures clinically meaningful aspects of cognition that may not be fully apparent in traditional neuropsychological testing environments.
Studies comparing brain signatures for everyday memory (ECogMem) and neuropsychological memory have found strongly shared brain substrates, suggesting convergent validity across these assessment modalities [1]. The successful extension of the signature method to this behavioral domain illustrates its usefulness for discerning and comparing brain substrates across different behavioral domains [1].
Executive Function Considerations
While executive function represents another crucial brain-behavior domain, the provided search results focus primarily on memory-related domains. However, the methodological framework for developing and validating brain signatures can be extended to executive function measures, which typically assess higher-order cognitive processes including working memory, cognitive flexibility, and inhibitory control.
Table 1: Key Brain-Behavior Domains and Associated Assessment Measures
| Brain-Behavior Domain | Primary Assessment Measures | Population Applications | Key Strengths |
|---|---|---|---|
| Episodic Memory | SENAS, ADNI-Mem | Cognitively diverse older adults | Sensitive across full performance range |
| Everyday Cognition | Everyday Cognition (ECog) scales | Preclinical AD to moderate dementia | Captures clinically meaningful function |
| Neuropsychological Memory | Composite list learning tests | General adult populations | Standardized quantitative metrics |
Experimental Protocols for Signature Validation
Multi-Cohort Validation Protocol
The validation of brain signatures requires a rigorous multi-cohort approach to ensure generalizability and robustness. The following protocol outlines the key steps for establishing validated brain signatures:
Discovery Cohort Selection: Identify multiple independent cohorts with appropriate sample sizes. Studies suggest samples in the thousands may be needed for optimal replicability, though smaller carefully selected cohorts can still yield meaningful results [1]. Example cohorts include the UC Davis Alzheimer's Disease Research Center Longitudinal Diversity Cohort (n=578) and Alzheimer's Disease Neuroimaging Initiative Phase 3 (n=831) [1].
Feature Selection: Compute regional brain gray matter associations for behavioral outcomes of interest. Implement voxel-based regressions without predefined ROI boundaries to allow fully data-driven feature selection [1].
Consensus Mask Generation: Run multiple iterations (e.g., 40 randomly selected discovery subsets) to generate spatial overlap frequency maps. Define high-frequency regions as "consensus" signature masks [1].
Independent Validation: Evaluate replicability using separate validation datasets (e.g., additional participants from original cohorts or independent studies). Assess both spatial convergence and model fit to behavioral outcomes [1].
Performance Comparison: Compare signature model fits with competing theory-based models to establish explanatory superiority [1].
Neuroimaging Data Processing Protocol
Standardized image processing is essential for reproducible brain signature development. The following protocol details key processing steps:
Image Acquisition: Acquire high-quality T1-weighted structural MRI images using standardized sequences. For functional signatures, acquire resting-state or task-based fMRI sequences [12].
Preprocessing: Process images through established pipelines including:
Quality Control: Implement rigorous quality control procedures at each processing stage, including human review of automated processing outputs [1].
Feature Extraction: Extract gray matter thickness values or functional connectivity measures for signature development.
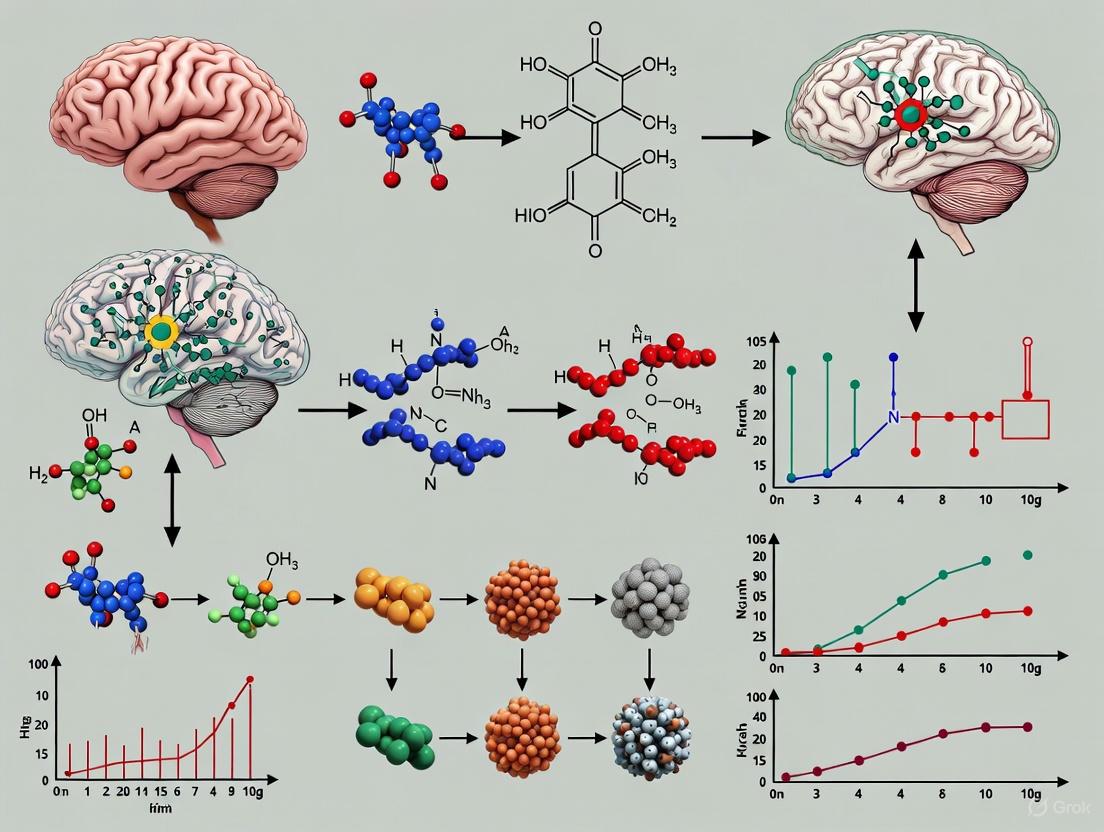
Figure 1: Brain Signature Validation Workflow
Advanced Methodological Approaches
Topological Data Analysis for Brain Dynamics
Beyond structural brain signatures, topological data analysis (TDA) represents an innovative framework for capturing individual differences in brain function. This approach characterizes the non-linear, high-dimensional structure of brain dynamics through persistent homology, identifying topological features such as loops and voids that describe how data points are organized in space and evolve over time [13].
The TDA protocol involves:
- Delay Embedding: Reconstruct one-dimensional time series into high-dimensional state space using optimal embedding dimensions and time delays [13].
- Persistent Homology Analysis: Perform 0-dimensional (H0) and 1-dimensional (H1) persistent homology analysis to extract topological features [13].
- Persistence Landscape Construction: Describe the birth and death of topological holes across different dimensions for analyzable feature sets [13].
Research has demonstrated that topological features exhibit high test-retest reliability and enable accurate individual identification across sessions [13]. In classification tasks, these features have outperformed commonly used temporal features in predicting gender and have shown significant associations with cognitive measures and psychopathological risks through canonical correlation analysis [13].
Machine Learning Considerations
Machine learning approaches represent powerful alternatives for developing brain-behavior models, with algorithms including support vector machines, support vector classification, relevant vector regression, and deep learning using convolutional neural nets [1]. However, these methods present distinct challenges for interpretation, as complex models can function as "black boxes" [1].
Key considerations for machine learning applications include:
- Overfitting Prevention: Implement rigorous cross-validation strategies and independent validation to prevent performance inflation [14].
- Confounding Control: Identify and mitigate confounding variables that can bias brain-behavior relationship examinations [14].
- Multisite Harmonization: Apply appropriate harmonization strategies to reduce unwanted variability in multisite datasets [14].
- Model Interpretability: Utilize post hoc interpretation methods to enhance model transparency while avoiding misinterpretation [14].
Table 2: Analytical Approaches for Brain-Behavior Signature Development
| Methodological Approach | Key Features | Advantages | Limitations |
|---|---|---|---|
| Voxel-Based Signature | Data-driven voxel selection without predefined ROIs | Comprehensive brain coverage; avoids ROI boundary constraints | Requires large samples; multiple comparison challenges |
| Topological Data Analysis | Persistent homology to capture topological features | Robust to noise; captures non-linear dynamics | Computationally intensive; complex interpretation |
| Machine Learning | Multivariate pattern analysis; predictive modeling | High predictive power; handles complex relationships | Black box problem; risk of overfitting |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Resources for Brain Signature Validation
| Resource Category | Specific Tools | Application Purpose | Key Features |
|---|---|---|---|
| Cognitive Assessment | SENAS, ADNI-Mem, Everyday Cognition (ECog) scales | Quantification of behavioral domains | Validation across cognitive ranges; sensitivity to change |
| Image Processing Software | In-house pipelines; established software packages | Structural and functional image analysis | Quality control procedures; standardized processing |
| Statistical Analysis Platforms | R, Python with specialized neuroimaging packages | Signature development and validation | Multivariate analysis; cross-validation capabilities |
| Data Harmonization Tools | ComBat; other cross-scanner harmonization methods | Multi-site data integration | Adjustment for scanner and site effects |
| Topological Analysis | Giotto-TDA toolkit | Persistent homology feature extraction | Delay embedding; persistence landscape construction |
The development of validated brain signatures for key behavioral domains represents a transformative approach in neuroscience with significant implications for drug development and clinical trial design. The rigorous multi-cohort validation framework ensures that resulting signatures are robust and generalizable, providing reliable neuroanatomical substrates for episodic memory, everyday cognition, and other behavioral domains.
Future directions in the field should include:
- Increased sample sizes and diversity to enhance generalizability [1]
- Multimodal approaches combining structural, functional, and topological features [13] [15]
- Advanced harmonization methods for multisite studies [14]
- Integration of genetic and environmental factors to comprehensively model brain-behavior relationships [15]
As these methodologies continue to evolve, validated brain signatures offer promising pathways for precision medicine approaches in neurology and psychiatry, enabling more targeted interventions and personalized treatment strategies based on individual neurocognitive profiles.
The Critical Need for Multi-Cohort Validation in Neurodegenerative Disease Research
Neurodegenerative diseases (NDs), including Alzheimer's disease (AD) and Parkinson's disease (PD), represent a significant and growing global health challenge, affecting over 57 million people worldwide [16]. These conditions are characterized by substantial heterogeneity in their clinical presentation and underlying pathology, which has consistently hampered the development of effective diagnostics and therapeutics. A predominant factor in the high failure rate of clinical trials is the limited generalizability of findings derived from single-cohort studies, which often fail to capture the full spectrum of disease variability across different populations. Multi-cohort validation has emerged as a critical methodological framework to address these challenges, enabling the identification of robust, reproducible biomarkers and signatures that transcend cohort-specific biases and technical variations. This approach is rapidly becoming the gold standard in neurodegenerative disease research, providing the statistical power and diversity necessary to accelerate the development of precision medicine approaches.
The Imperative for Multi-Cohort Approaches
Limitations of Single-Cohort Studies
Single-cohort studies are frequently limited by cohort-specific characteristics, including unique demographic distributions, recruitment strategies, clinical assessment protocols, and biospecimen handling procedures. These factors introduce biases that can lead to the identification of putative biomarkers that fail to replicate in independent populations [17]. Furthermore, the statistical power of single-cohort studies is often constrained by sample size limitations, particularly for less common neurodegenerative conditions such as frontotemporal dementia (FTD) or amyotrophic lateral sclerosis (ALS). The siloing of data among a fragmented research community has been a significant barrier to biomarker discovery, as many research institutions have historically maintained restricted access to their datasets [16].
Advantages of Multi-Cohort Validation
Multi-cohort analysis significantly enhances the robustness and generalizability of research findings by explicitly addressing and quantifying inter-cohort heterogeneity. By integrating data from multiple independent sources, researchers can distinguish consistently dysregulated biomarkers from those that are cohort-specific artifacts. A key demonstration of this principle comes from a PD cognitive impairment study, which found that multi-cohort models provided greater performance stability over single-cohort models while retaining competitive average performance [17]. Similarly, in AD research, a three-cohort cerebrospinal fluid (CSF) proteomics study identified a 10-protein signature that achieved exceptional predictive accuracy (AUC > 0.90) across independent validation sets [18]. This level of validation provides greater confidence in the potential clinical utility of such signatures.
Table 1: Performance Comparison of Single vs. Multi-Cohort Machine Learning Models in Parkinson's Disease Cognitive Impairment Prediction
| Model Type | Prediction Task | Performance Metric | Performance Value | Notes |
|---|---|---|---|---|
| Single-Cohort (LuxPARK) | PD-MCI Classification | Hold-out AUC | 0.70 | Highest performing single cohort |
| Single-Cohort (PPMI) | PD-MCI Classification | Hold-out AUC | 0.69 | Comparable performance |
| Multi-Cohort (Cross-cohort) | PD-MCI Classification | Hold-out AUC | 0.67 | Competitive performance with improved stability |
| Single-Cohort (PPMI) | Time-to-SCD Analysis | Hold-out C-index | 0.76 | Highest performing single cohort |
| Multi-Cohort (Cross-cohort) | Time-to-SCD Analysis | Hold-out C-index | 0.72 | Similar performance with greater robustness |
Experimental Protocols for Multi-Cohort Studies
Protocol 1: Multi-Cohort Proteomic Analysis for Biomarker Discovery
This protocol outlines a standardized workflow for identifying and validating protein biomarkers across multiple cohorts, based on established methodologies from recent large-scale consortia [16].
Sample Preparation and Data Generation
- Cohort Selection: Identify and collaborate with 3-5 independent cohorts with available biospecimens (plasma, CSF) and associated clinical data. Ensure diversity in geographic location, recruitment criteria, and demographic characteristics.
- Sample Processing: Use standardized SOPs for sample collection, processing, and storage across all sites. Aliquot samples to avoid freeze-thaw cycles.
- Proteomic Profiling: Utilize high-throughput proteomic platforms (e.g., SomaScan, Olink) to quantify protein levels. Include internal quality controls and inter-plate calibrators to monitor technical variability.
- Data Preprocessing: Perform normalization within and across batches using robust statistical methods (e.g., quantile normalization, ComBat). Implement rigorous quality control metrics to exclude poor-quality samples.
Statistical Analysis and Validation
- Discovery Phase: Conduct differential abundance analysis in the largest cohort (or meta-analyze across multiple discovery cohorts) using appropriate linear models, adjusting for key covariates (age, sex, technical factors).
- Replication Phase: Test significantly dysregulated proteins (FDR < 0.05) in independent replication cohorts using pre-specified statistical models.
- Meta-Analysis: Perform an inverse-variance weighted fixed-effects or random-effects meta-analysis across all cohorts to obtain pooled effect estimates and assess heterogeneity (I² statistic).
- Machine Learning: Develop predictive models (e.g., LASSO regression) on the discovery set and validate on held-out cohorts. Assess performance using AUC, sensitivity, specificity.
Protocol 2: Multi-Cohort Transcriptomic Meta-Analysis
This protocol describes an integrated meta-analysis approach for identifying conserved transcriptional signatures across neurodegenerative diseases, adapted from a pioneering study that analyzed 1,270 post-mortem CNS tissue samples [19].
Data Collection and Preprocessing
- Dataset Curation: Search public repositories (e.g., GEO, ArrayExpress) for gene expression datasets from neurodegenerative disease studies. Apply inclusion criteria: ≥5 cases and ≥5 controls, human post-mortem CNS tissue, genome-wide profiling.
- Data Harmonization: Log2-transform and quantile-normalize gene expression values for each dataset. Map microarray probes to standard gene symbols, resolving many-to-many relationships by creating additional records.
- Cohort Stratification: Divide datasets into discovery (smaller cohorts) and validation (larger cohorts) sets. Ensure representation of different CNS regions affected by each disease.
Meta-Analysis Execution
- Effect Size Calculation: Compute standardized mean differences (Hedge's adjusted g) for each gene in each dataset. For multiple probes mapping to the same gene, summarize effect sizes using fixed-effects inverse-variance model.
- Cross-Study Integration: Combine study-specific effect sizes using random-effects inverse-variance models to obtain pooled effect sizes and standard errors.
- Robustness Validation: Perform leave-one-disease-out analyses to identify genes consistently dysregulated across different combinations of neurodegenerative conditions.
- Functional Interpretation: Conduct pathway enrichment analysis, cell-type deconvolution, and upstream regulator prediction using established bioinformatics resources.
Table 2: Key Stages in Multi-Cohort Transcriptomic Meta-Analysis with Sample Sizes
| Stage | Description | Sample Size | Number of Cohorts | Key Outcome |
|---|---|---|---|---|
| Discovery Meta-Analysis | Initial integration of gene expression data | 1,270 samples | 13 patient cohorts | 243 differentially expressed genes |
| Leave-One-Disease-Out Analysis | Iterative exclusion of each disease | 1,270 samples | 13 patient cohorts | Common Neurodegeneration Module (CNM) |
| Independent Validation | Validation in larger cohorts | 985 samples | 3 patient cohorts | Confirmed conserved signature |
| Secondary Validation | Extension to additional diseases | 205 samples | 15 patient cohorts | Signature applicable to 7 neurodegenerative diseases |
Key Research Reagent Solutions
Successful multi-cohort studies require standardized reagents and platforms to ensure comparability across sites and datasets. The following table outlines essential research reagents and their applications in multi-cohort neurodegenerative disease research.
Table 3: Essential Research Reagent Solutions for Multi-Cohort Neurodegeneration Research
| Reagent/Platform | Type | Primary Function | Example Use Case |
|---|---|---|---|
| SomaScan Assay | Proteomic Platform | High-throughput protein quantification (7,029 analytes) | CSF proteomic analysis across Knight ADRC, FACE, ADNI cohorts [20] |
| Olink Proximity Extension Assay | Proteomic Platform | Multiplex protein quantification with high specificity | Plasma proteomic profiling in GNPC consortium [16] |
| Montreal Cognitive Assessment (MoCA) | Clinical Assessment | Cognitive screening and mild cognitive impairment detection | Predictor of cognitive impairment in PD multi-cohort study [17] |
| Benton Judgment of Line Orientation (JLO) | Neuropsychological Test | Visuospatial ability assessment | Key predictor for PD-MCI in multi-cohort analysis [17] |
| MDS-UPDRS Parts I-IV | Clinical Rating Scale | Comprehensive assessment of Parkinson's disease symptoms | Motor and non-motor predictor integration in PD models [17] |
| OMOP Common Data Model | Data Standardization Framework | Harmonization of observational data across different sources | Cohort data management system interoperability [21] |
Case Studies in Multi-Cohort Validation
The Global Neurodegeneration Proteomics Consortium (GNPC)
The GNPC represents a paradigmatic example of large-scale multi-cohort collaboration, establishing one of the world's largest harmonized proteomic datasets for neurodegenerative diseases [16]. This public-private partnership includes approximately 250 million unique protein measurements from multiple platforms from more than 35,000 biofluid samples (plasma, serum, and CSF) contributed by 23 partners. The consortium has established a secure cloud-based environment (AD Workbench) for data access and analysis, addressing critical challenges in data siloing and harmonization. The GNPC has successfully identified disease-specific differential protein abundance patterns and transdiagnostic proteomic signatures of clinical severity that are reproducible across different neurodegenerative conditions. Particularly notable is the discovery of a robust plasma proteomic signature of APOE ε4 carriership that is consistent across AD, PD, FTD, and ALS, suggesting shared biological pathways influenced by this major genetic risk factor.
Multi-Cohort CSF Proteomics in Alzheimer's Disease
A landmark three-stage multi-cohort study of CSF proteomics in AD exemplifies the power of this approach for biomarker discovery [18]. The analysis employed a rigorous design with distinct discovery (Knight ADRC and FACE cohorts, n=1,170), replication (ADNI and Barcelona-1 cohorts, n=593), and validation (Stanford ADRC, n=107) phases. This study identified 2,173 analytes (2,029 unique proteins) dysregulated in AD, of which 1,164 (57%) were novel associations. Machine learning approaches applied to this data yielded highly accurate and replicable models (AUC > 0.90) for predicting AD biomarker positivity and clinical status. Furthermore, the analysis revealed that proteomic changes in AD follow four distinct pseudo-trajectories across the disease continuum, with specific pathway enrichments at different stages: neuronal death and apoptosis (early stages), microglia dysregulation and endolysosomal dysfunction (mid-stages), brain plasticity and longevity (mid-stages), and microglia-neuron crosstalk (late stages).
Cross-Disease Transcriptional Meta-Analysis
An integrated multi-cohort transcriptional meta-analysis of neurodegenerative diseases revealed conserved molecular pathways across distinct clinical conditions [19]. The study analyzed 1,270 post-mortem CNS tissue samples from 13 patient cohorts covering four neurodegenerative diseases (AD, PD, HD, and ALS), with validation in an additional 15 cohorts (205 samples) including seven neurodegenerative diseases. This approach identified 243 differentially expressed genes that were similarly dysregulated across multiple conditions, with the signature correlating with histologic disease severity. The analysis highlighted pervasive bioenergetic deficits, M1-type microglial activation, and gliosis as unifying themes of neurodegeneration. Notably, metallothioneins featured prominently among the differentially expressed genes, and functional pathway analysis identified specific convergent themes of dysregulation. The study also demonstrated how removal of genes common to neurodegeneration from disease-specific signatures revealed uniquely robust immune response and JAK-STAT signaling in ALS, illustrating the power of this approach to distinguish shared from distinct disease mechanisms.
Implementation Considerations and Best Practices
Cohort Data Management Systems (CDMS)
Effective multi-cohort research requires sophisticated data management infrastructure. Modern Cohort Data Management Systems (CDMS) must address both functional requirements (data collection, processing, analysis) and non-functional requirements (flexibility, security, usability) [21]. These systems facilitate cohort studies through comprehensive data operations, secure access controls, user engagement features, and interoperability with other research platforms. Key considerations include:
- Data Harmonization: Implementation of common data models (e.g., OMOP CDM) and standardized terminologies to enable cross-cohort analyses.
- Privacy and Security: Adherence to regulatory frameworks (GDPR, HIPAA) through de-identification, access controls, and audit trails.
- Interoperability: Support for integration with electronic health records, multi-omics platforms, and analysis tools through API-based architectures.
- Scalability: Capacity to handle exponentially increasing data volumes from digital health technologies and high-throughput molecular profiling.
Analytical Considerations
Robust multi-cohort analysis requires careful attention to methodological challenges:
- Cross-Study Normalization: Application of appropriate batch correction methods (e.g., ComBat, cross-study normalization) to address technical variability while preserving biological signals [17].
- Heterogeneity Assessment: Quantification of between-cohort heterogeneity using metrics such as I² statistics, with application of random-effects models when substantial heterogeneity is present.
- Stratified Analysis: Exploration of sex-specific, ancestry-specific, and disease-stage-specific effects through pre-specified subgroup analyses.
- Confounding Control: Standardized adjustment for key demographic and clinical variables across cohorts to enhance comparability.
Multi-cohort validation represents a transformative approach in neurodegenerative disease research, directly addressing the challenges of disease heterogeneity and limited reproducibility that have plagued the field. Through the integration of diverse, independent datasets, researchers can distinguish robust, generalizable biomarkers from cohort-specific artifacts, accelerating the development of clinically applicable tools. The establishment of large-scale consortia such as the GNPC, together with standardized protocols for cross-cohort analysis and data management, provides a foundational framework for future discoveries. As the field advances, multi-cohort approaches will be increasingly essential for the development of precision medicine strategies that can deliver the right intervention to the right patient at the right time, ultimately transforming the prognosis for millions affected by these devastating conditions.
Methodological Frameworks: Building Robust Signatures with Machine Learning and Multi-Cohort Designs
Application Notes: The Role of Multi-Cohort Designs in Validating Brain Signatures
Rationale and Scientific Foundation
Multi-cohort discovery designs have emerged as a critical methodology in neuroscience research to address critical limitations of single-cohort studies, including limited generalizability, cohort-specific biases, and reduced statistical power. These designs enable researchers to develop and validate robust brain signatures—data-driven patterns of brain structure or function that serve as reliable biomarkers for cognitive status, disease progression, and treatment response. By leveraging multiple independent cohorts, researchers can distinguish consistent neurobiological patterns from cohort-specific artifacts, producing findings that translate across diverse populations and clinical settings [1] [22].
The validation of brain signatures across multiple cohorts represents a paradigm shift from theory-driven approaches to data-driven discovery of brain-behavior relationships. This approach leverages high-dimensional data from neuroimaging, cognitive assessments, and biomarkers to identify complex patterns that may not be evident through hypothesis-testing alone. As noted in recent research, "The 'brain signature of cognition' concept has garnered interest as a data-driven, exploratory approach to better understand key brain regions involved in specific cognitive functions, with the potential to maximally characterize brain substrates of behavioral outcomes" [1]. This methodological evolution has been facilitated by the growing availability of large-scale, multimodal datasets from international consortia and advances in computational power and machine learning algorithms.
Key Advantages and Applications
Multi-cohort designs offer several distinct advantages over traditional single-cohort studies. They significantly enhance the robustness and generalizability of findings by testing associations across diverse populations with varying recruitment criteria, measurement protocols, and demographic characteristics. These designs improve statistical power for detecting subtle but consistent effects by combining data across multiple sources. They also enable the identification of cohort-invariant biological patterns that reflect core disease processes rather than cohort-specific characteristics. Furthermore, multi-cohort designs facilitate the development of comprehensive disease models by integrating complementary variables measured across different studies [23] [22].
The applications of multi-cohort designs in brain signature validation span multiple domains: early detection and risk stratification for neurodegenerative diseases, tracking disease progression and treatment response, parsing heterogeneity within clinical syndromes, and providing robust endpoints for clinical trials. For instance, a recent study demonstrated that a "Union Signature" derived from multiple behavioral domains showed stronger associations with clinical outcomes than traditionally used brain measures and excelled at classifying clinical syndromes across the cognitive normalcy-to-dementia spectrum [22].
Experimental Protocols and Methodologies
Cohort Selection and Data Harmonization
Cohort Selection Criteria: The foundation of a successful multi-cohort study lies in the strategic selection of complementary datasets. Ideal cohorts should have: (1) clearly defined diagnostic criteria consistently applied across all participants (e.g., NINCDS-ADRDA criteria for Alzheimer's disease); (2) sufficient sample sizes per diagnostic group (typically >10 participants per group, though larger samples are preferred); (3) multimodal data collection encompassing imaging, clinical, cognitive, and biomarker assessments; and (4) diversity in recruitment strategies and population characteristics to enhance generalizability [23] [24].
Data Harmonization Protocols: Cross-cohort data harmonization is a critical step that requires meticulous attention to technical and methodological variability. Key harmonization procedures include: (1) imaging data processing through standardized pipelines (e.g., FreeSurfer for volumetric measures, DiReCT for gray matter thickness); (2) cross-study normalization to adjust for scanner and protocol differences; (3) cognitive score harmonization using equating procedures or factor analysis; and (4) covariate adjustment for demographic and clinical variables [1] [25]. The normalization of volumetric measures should account for intracranial volume differences using the formula: VRa = VR/tICV * mean(tICV), where VRa is the adjusted volume, VR is the raw volume, and tICV is total intracranial volume [25].
Table 1: Exemplar Cohorts for Multi-Cohort Brain Signature Research
| Cohort Name | Primary Focus | Sample Characteristics | Key Data Modalities | Access Information |
|---|---|---|---|---|
| ADNI [26] [27] | Alzheimer's disease biomarkers | 229 normal, 398 MCI, 192 AD (baseline) [24] | MRI, PET, CSF biomarkers, genetics, cognitive tests | LONI IDA repository with data use agreement [27] |
| UCD ADRC [22] | Diverse cognitive aging | 946 normal, 418 MCI, 140 dementia (diverse ethnic/racial composition) | Structural MRI, cognitive tests, clinical assessments | Requires institutional approval and data use agreement |
| MCR Consortium [25] | Motoric cognitive risk | N=1987 across 6 international cohorts | Gait measures, volumetric MRI, cognitive tests | Collaborative consortium approval required |
| LuxPARK [17] | Parkinson's disease cognitive impairment | Luxembourgish PD cohort with cognitive assessments | Clinical measures, cognitive tests, motor assessments | Requires individual cohort data use agreements |
Brain Signature Discovery and Validation Workflow
The validation of brain signatures through multi-cohort designs follows a rigorous multi-stage process that emphasizes generalizability and robustness at each step.
Discovery Phase Protocol:
- Feature Selection: Identify candidate brain features (e.g., voxel-wise gray matter thickness, regional volumes) associated with behavioral outcomes of interest. Use whole-brain exploratory analyses without pre-specified regions of interest to avoid confirmation bias.
- Multi-Subset Discovery: Generate 40+ randomly selected subsets (n=400 each) from the discovery cohort to compute regions of interest significantly associated with the behavioral outcome in each subset [1] [22].
- Consensus Mask Creation: Calculate voxel-wise overlaps across discovery subsets. Define "consensus" signature regions as those appearing in at least 70% of discovery subsets, ensuring robustness against sampling variability [22].
- Initial Model Building: Develop predictive models using machine learning algorithms (e.g., gradient boosting, regularized regression) that incorporate the identified signature regions.
Validation Phase Protocol:
- Cross-Cohort Validation: Test the discovered signatures in completely independent validation cohorts that were not used in the discovery phase. This assesses generalizability across different populations and measurement protocols.
- Performance Benchmarking: Compare signature performance against theory-based models (e.g., hippocampal volume for memory) and established biomarkers using metrics such as AUC for classification, C-index for time-to-event analysis, and R² for continuous outcomes [17] [22].
- Clinical Utility Assessment: Evaluate the signature's ability to predict clinically relevant outcomes such as conversion from MCI to dementia, functional decline, or treatment response.
Multi-Cohort Machine Learning Protocol: For predictive model development across multiple cohorts, the following protocol has demonstrated efficacy:
- Data Integration: Combine data from multiple cohorts while preserving cohort identities to account for systematic differences.
- Cross-Cohort Normalization: Apply harmonization methods to minimize technical variability while preserving biological signals.
- Algorithm Selection: Implement machine learning methods suitable for multi-cohort data, such as mixed-effects models, domain adaptation techniques, or ensemble methods that account for cohort heterogeneity.
- Explainable AI (XAI) Integration: Incorporate interpretability methods such as SHapley Additive exPlanations (SHAP) to identify robust predictors across cohorts and enhance clinical translatability [17].
Diagram 1: Multi-Cohort Brain Signature Validation Workflow
Statistical Validation Framework
Robust validation of brain signatures requires a comprehensive statistical framework that addresses both model performance and spatial reproducibility:
Model Fit Replicability:
- Evaluate signature-outcome associations across multiple random subsets (50+)
- Test correlation of model fits between discovery and validation cohorts
- Assess performance stability across cross-validation cycles [1]
Spatial Extent Replicability:
- Quantify overlap between signature regions identified in different cohorts
- Calculate spatial correlation metrics (e.g., Dice coefficient)
- Identify consistently engaged neural systems across cohorts [1]
Performance Metrics:
- For classification tasks: AUC, sensitivity, specificity, precision
- For survival analysis: C-index, time-dependent AUC
- For continuous outcomes: R², mean squared error, correlation coefficients [17]
Table 2: Key Analytical Methods for Multi-Cohort Studies
| Method Category | Specific Techniques | Application Context | Key Considerations |
|---|---|---|---|
| Event-Based Modeling [23] | Probabilistic event sequences, Meta-sequence aggregation | Disease staging, Biomarker ordering | Handles partially overlapping variables across cohorts |
| Machine Learning [17] | Gradient boosting, Regularized regression, Explainable AI (SHAP) | Prediction of conversion, Cognitive decline | Requires careful cross-cohort normalization |
| Signature Discovery [22] | Voxel-wise regression, Consensus masking, Union signatures | Brain-behavior mapping, Multi-domain assessment | Balances discovery and validation sample sizes |
| Clustering Methods [25] | HYDRA (Heterogeneity through Discriminative Analysis) | Disease subtyping, Heterogeneity analysis | Uses reference population to control for normal variation |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Multi-Cohort Brain Signature Research
| Resource Category | Specific Resources | Function/Purpose | Access Information |
|---|---|---|---|
| Data Repositories | ADNI (LONI IDA) [26] [27] | Primary data source for Alzheimer's disease biomarkers | Online application with data use agreement [27] |
| Analysis Platforms | FreeSurfer, FSL, SPM, CAT12 | Image processing and volumetric analysis | Open-source or licensed software packages |
| Computational Tools | Python (scikit-learn, nilearn, PyTorch), R (brainGraph, ebmc) | Machine learning, statistical analysis, signature development | Open-source programming languages and libraries |
| Validation Frameworks | Cross-validation, leave-one-cohort-out, bootstrap aggregation | Robustness assessment, generalizability testing | Implemented in statistical software environments |
| Consortium Data | MCR Consortium [25], ADNI, UCD ADRC, LuxPARK [17] | Multi-cohort validation, increased sample diversity | Varied access procedures from open to restricted |
Case Studies and Empirical Evidence
Multi-Cohort Validation of Parkinson's Disease Cognitive Impairment Signatures
A recent large-scale study demonstrated the power of multi-cohort designs by integrating data from three independent Parkinson's disease cohorts (LuxPARK, PPMI, and ICEBERG) to develop machine learning models predicting cognitive impairment. The study found that multi-cohort models showed greater performance stability over single-cohort models while retaining competitive average performance (hold-out AUC 0.67 for PD-MCI classification). Key predictors included age at diagnosis and visuospatial ability, with significant sex differences observed in cognitive impairment patterns. The study highlighted that "multi-cohort models provided more stable performance statistics than single-cohort models across cross-validation cycles," demonstrating the value of incorporating diverse populations to improve model robustness and reduce cohort-specific biases [17].
Event-Based Modeling Across Alzheimer's Disease Cohorts
A comprehensive analysis of ten independent AD cohort studies revealed both consistency and variability in event-based model sequences derived from different datasets. The average pairwise Kendall's tau correlation coefficient across cohorts was 0.69 (±0.28), indicating general consistency but also notable variability mainly in the positioning of imaging variables. The researchers developed a novel rank aggregation algorithm to combine partially overlapping event sequences into a meta-sequence that integrated complementary information from each cohort. The resulting meta-sequence aligned with current understanding of AD progression, starting with CSF amyloid beta abnormalities, followed by tauopathy, memory impairment, FDG-PET changes, and ultimately brain atrophy and visual memory deficits. This approach demonstrated that "aggregation of data-driven results can combine complementary strengths and information of patient-level datasets" to create more comprehensive disease models [23].
Union Signature Development for Multiple Cognitive Domains
A groundbreaking study developed a "Union Signature" derived from four behavior-specific brain signatures (neuropsychological and informant-rated memory and executive function). This generalized signature demonstrated stronger associations with clinical outcomes than traditionally used brain measures and excelled at classifying clinical syndromes. The Union Signature's associations with episodic memory, executive function, and Clinical Dementia Rating Sum of Boxes were stronger than those of several standardly accepted brain measures (e.g., hippocampal volume, cortical gray matter) and other previously developed brain signatures. The study concluded that "the Union Signature is a powerful, multipurpose correlate of clinically relevant outcomes and a strong classifier of clinical syndromes," highlighting the potential of data-driven approaches to discover brain substrates that explain more variance in clinical outcomes than theory-guided measures [22].
Diagram 2: Multi-Cohort Analytical Approaches and Signature Outcomes
Implementation Considerations and Best Practices
Methodological Challenges and Solutions
Cohort Heterogeneity: Variability in recruitment criteria, measurement protocols, and population characteristics across cohorts can introduce systematic biases. Solution: Implement robust normalization procedures, use mixed-effects models to account for cohort-level variance, and explicitly test for cohort-by-predictor interactions [17] [23].
Missing Data: Different cohorts typically collect partially overlapping sets of variables. Solution: Apply appropriate missing data methods (e.g., multiple imputation), develop models using only commonly assessed variables, or use meta-analytic approaches that combine results from different variable sets [23].
Computational Complexity: Multi-cohort analyses involve large, heterogeneous datasets that require substantial computational resources. Solution: Utilize high-performance computing infrastructure, implement efficient algorithms, and consider distributed computing approaches [1] [22].
Reproducibility: Ensuring that findings replicate across cohorts requires careful methodological planning. Solution: Pre-register analysis plans, implement rigorous cross-validation schemes, and use independent cohorts for discovery and validation [1].
Optimization Strategies
- Sample Size Planning: Balance between cohort diversity and statistical power—include enough cohorts to ensure generalizability but maintain sufficient sample size within each cohort for reliable estimation.
- Variable Selection: Prioritize variables that are measured consistently across cohorts and have established reliability and validity.
- Validation Sequence: Use a stepped validation approach—first within-cohort cross-validation, then between-cohort validation, and finally validation in completely independent datasets.
- Clinical Translation: Engage clinical stakeholders throughout the process to ensure that identified signatures have practical utility and align with clinical decision-making needs.
The implementation of multi-cohort discovery designs represents a significant advancement in neuroscience methodology, addressing critical limitations of single-cohort studies while leveraging the complementary strengths of diverse datasets. As research in this area continues to evolve, these approaches promise to yield more robust, generalizable, and clinically meaningful brain signatures that enhance our understanding of brain-behavior relationships and improve patient care across neurodegenerative and neuropsychiatric conditions.
Within the evolving paradigm of precision medicine, the development of robust, biologically grounded biomarkers is paramount. The concept of a "brain signature of cognition" has garnered significant interest as a data-driven, exploratory approach to identify key brain regions associated with specific cognitive functions or disease states, offering the potential to maximally characterize the brain substrates of behavioral and clinical outcomes [1]. However, for such signatures to transition from research tools to clinically viable biomarkers, they must demonstrate robust validation across diverse, independent cohorts. A critical methodological challenge lies in moving beyond signatures derived from single cohorts or simplistic analyses, which often fail to generalize. This Application Note details a refined protocol for consensus signature development, leveraging spatial overlap frequency and aggregation techniques to create neuroanatomical signatures that are reproducible, reliable, and capable of outperforming theory-based models [1] [10]. This methodology is framed within a broader thesis on cross-cohort validation, providing a foundational technique for ensuring that brain signatures are not merely artifacts of a particular dataset but represent consistent biological phenomena.
Core Principles and Definitions
A brain signature is a multivariate pattern derived from neuroimaging data (e.g., gray matter thickness, white matter hyperintensities) that is systematically associated with a behavioral domain (e.g., episodic memory), clinical status (e.g., Alzheimer's disease), or a specific risk factor (e.g., hypertension) [1] [3]. The signature approach represents an evolution from theory-driven or lesion-driven approaches, aiming to provide a more complete accounting of complex brain-behavior relationships.
The transition to a consensus signature involves a deliberate shift from single-cohort discovery to multi-source evidence aggregation. The core principle is that a robust signature should be identifiable across numerous randomly selected subsets of a discovery cohort. Regions that consistently appear across these subsets are considered part of a "consensus" signature mask, thereby enhancing generalizability and mitigating the pitfalls of overfitting and bias inherent in single-dataset discovery [1]. This process is fundamentally based on analyzing the spatial overlap frequency of features (e.g., voxels, regions of interest) associated with the outcome of interest, defining consensus regions as those that exceed a pre-defined frequency threshold [1].
Computational Protocols
Workflow for Consensus Signature Generation
The following diagram illustrates the end-to-end workflow for developing a consensus signature, from data preparation through to final validation.
Detailed Methodological Steps
Step 1: Repeated Subsampling of Discovery Cohorts
- Objective: To ensure the signature is not dependent on a specific sample composition.
- Protocol: From each discovery cohort, generate a large number (e.g., 40) of random subsets without replacement. The subset size (e.g., n=400) should be chosen to be large enough for stable estimation but small enough to allow for numerous iterations [1].
- Rationale: This step directly addresses population heterogeneity, a major factor affecting the predictive accuracy of brain imaging [6]. It allows for the assessment of a signature's stability across variations in sample makeup.
Step 2: Voxel-wise Association Analysis
- Objective: To identify brain regions associated with the target outcome within each subset.
- Protocol: For each subsample, perform a mass-univariate or multivariate analysis relating the neuroimaging variable (e.g., gray matter thickness) to the outcome (e.g., memory score). This can be implemented using voxel-based regressions or machine learning algorithms like support vector machines [1].
- Output: For each of the 40 subsets, a statistical map (e.g., t-map, beta-map) indicating the strength and direction of association for every voxel.
Step 3: Generation of Spatial Overlap Frequency Maps
- Objective: To quantify the spatial consistency of associations across all subsamples.
- Protocol:
- Thresholding: Convert each statistical map from Step 2 into a binary map by applying a significance threshold (e.g., p < 0.01, FDR-corrected).
- Aggregation: Sum all binary maps across the 40 subsets. This creates a single frequency map where the value at each voxel represents the number of subsamples in which it was significantly associated with the outcome.
- Output: A 3D frequency map where voxel intensities range from 0 to the total number of subsamples (e.g., 40).
Step 4: Consensus Mask Definition
- Objective: To define the final set of regions constituting the consensus signature.
- Protocol: Apply a frequency threshold to the map from Step 3. For instance, only voxels that are significant in more than 70% of the subsamples (e.g., >28 out of 40) are retained. This threshold can be determined empirically or via cross-validation [1].
- Output: A binary "consensus signature mask" that identifies the most robustly associated brain regions.
Validation Framework
The validation of a consensus signature is a multi-faceted process, as depicted in the workflow. The core activities in this phase are detailed below.
Step 6 & 7: Model Fit Evaluation and Comparison
- Objective: To rigorously test the performance and utility of the consensus signature in independent data.
- Protocol:
- Replicability of Model Fits: Apply the consensus signature to 50 random subsets of the validation cohort. High correlation of the signature's model fit (e.g., R²) across these subsets indicates high replicability [1].
- Explanatory Power Comparison: Test whether the consensus signature model explains significantly more variance in the outcome variable than competing theory-based models (e.g., those based on pre-defined regions from the literature) in the full validation cohort [1].
- Generalizability Check: Validate the signature in cohorts with different demographic or clinical characteristics to assess its broad applicability [8].
Table 1: Key Quantitative Benchmarks for Validation Based on Fletcher et al. [1]
| Validation Metric | Experimental Procedure | Benchmark for Success |
|---|---|---|
| Spatial Convergence | Visual and quantitative comparison of consensus regions derived from independent discovery cohorts. | High spatial overlap between consensus masks from different cohorts. |
| Model Fit Replicability | Correlation of signature model fits across 50 random validation subsets. | High correlation coefficient (e.g., >0.8) indicating stable performance. |
| Explanatory Power | Variance explained (R²) in the outcome by the signature model versus competing models in the full validation cohort. | Signature model significantly outperforms (e.g., higher R²) theory-based models. |
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Consensus Signature Development
| Reagent / Resource | Function and Role in the Protocol |
|---|---|
| Multi-Cohort Neuroimaging Data (e.g., ADNI, iSTAGING) [1] [3] | Provides the necessary discovery and validation datasets with varying demographics and scanner types, which is crucial for assessing generalizability. |
| High-Quality Brain Parcellation Atlases [1] | Enables a more exploratory, data-driven approach by providing a predefined organizational structure for initial region-based analyses. |
| Computational Pipelines for Image Processing (e.g., in-house pipelines, FSL, FreeSurfer) [1] | Handles critical pre-processing steps such as brain extraction, tissue segmentation (GM, WM, CSF), and registration to a standard template, ensuring data quality and comparability. |
| Statistical Computing Environment (e.g., R, Python with NumPy/SciKit-learn) | Provides the framework for performing repeated subsampling, voxel-wise regression analyses, and spatial frequency map calculations. |
| Support Vector Machine (SVM) Libraries [1] [3] | Offer an alternative machine learning implementation for exploratory feature selection when moving beyond mass-univariate methods. |
Advanced Analysis and Interpretation
Interpreting Consensus Signature Maps
The consensus signature is more than a simple average; it represents a robust spatial pattern validated through resampling. The frequency value of a voxel in the consensus map is a direct measure of its reliability. Regions with very high frequency (e.g., >90%) are core components of the signature, while those with lower but still threshold-exceeding frequencies may represent more variable elements that are nonetheless important. Inter-signature comparisons, for instance between memory and everyday function, can reveal strongly shared brain substrates, providing insights into common neurobiological pathways [1].
Logical Framework for Signature Validation
The following diagram outlines the logical decision process for assessing a signature's robustness and clinical utility, guiding researchers from initial development to final application.
Application Notes and Troubleshooting
Critical Parameters for Success
- Discovery Set Size: Pitfalls of using overly small discovery sets include inflated strengths of association and a critical loss of reproducibility. Studies suggest that discovery sets should number in the hundreds to thousands for stable signature derivation [1].
- Cohort Heterogeneity: The replicability of model fit and consistent spatial selection is highly dependent on cohort heterogeneity, which should encompass a full range of variability in brain pathology and cognitive function [1]. While heterogeneity can initially make prediction more challenging, it is essential for developing generalizable signatures [6].
- Aggregation Technique: The method of aggregation (e.g., frequency thresholding) is superior to single-shot discovery as it explicitly models and accounts for variability across different sample compositions.
Common Challenges and Solutions
- Challenge: Low spatial overlap between signatures from two discovery cohorts.
- Solution: Ensure cohorts are matched for key clinical and demographic variables. If mismatch persists, inspect frequency maps at a lower threshold to identify a stable core of regions shared between cohorts.
- Challenge: Consensus signature performs well in discovery but poorly in validation.
- Solution: Re-evaluate the pre-processing and harmonization of the validation cohort data. Check for unaccounted-for confounders (e.g., scanner effects, population diversity) that were not present in the discovery data [6].
- Challenge: Signature is not associated with relevant clinical biomarkers.
- Solution: This may indicate the signature is capturing a real but distinct biological process. Re-assess the clinical construct being targeted and ensure the outcome measure used for signature development is itself biologically grounded.
The protocol for consensus signature development using spatial overlap frequency and aggregation techniques provides a rigorous, data-driven framework for creating robust neuroimaging biomarkers. By moving beyond single-cohort discoveries and emphasizing replication through resampling and independent validation, this methodology directly addresses the critical need for generalizability in computational neuroscience and psychiatry. When integrated into a broader thesis on cross-cohort validation, this approach lays the groundwork for the development of brain signatures that are not only statistically sound but also clinically meaningful, capable of informing drug development by providing reliable endpoints for tracking disease progression and therapeutic response.
Machine Learning and Explainable AI (XAI) for Signature Identification in Parkinson's and Alzheimer's Disease
The identification of robust brain signatures for Parkinson's disease (PD) and Alzheimer's disease (AD) represents a transformative approach to understanding disease mechanisms, enabling early detection, and facilitating personalized therapeutic interventions. Brain signatures are defined as data-driven, multivariate patterns of brain alterations—captured via neuroimaging, biofluid biomarkers, or other modalities—that are consistently associated with specific disease states or behavioral outcomes [1]. The integration of machine learning (ML) with Explainable AI (XAI) techniques is critical for extracting these signatures in a way that is not only predictive but also interpretable to researchers and clinicians [28]. This is particularly vital within a multi-cohort validation framework, which ensures that identified signatures are generalizable and reproducible across diverse populations, moving beyond findings limited to single studies [1] [17]. This document provides detailed application notes and experimental protocols for the discovery and validation of such signatures, specifically tailored for research scientists and drug development professionals.
Application Notes: Core Concepts and Workflow
The Role of XAI in Neurodegenerative Disease Research
In medical ML, the need for transparency is paramount. Models can be categorized as inherently interpretable "white box" models (e.g., linear models, decision trees) or complex "black box" models (e.g., deep neural networks, ensemble methods) which require post-hoc XAI techniques to explain their predictions [28]. The application of XAI is not merely a technical exercise; it is an ethical and legal imperative. Regulations like the General Data Protection Regulation (GDPR) establish a right to explanation for automated decisions, a principle that directly applies to clinical decision support systems [28]. In practice, XAI helps to:
- Build trust among clinicians and patients by providing transparent reasoning for model outputs.
- Verify biological plausibility by ensuring that a model's decisions align with known or suspected neuropathology.
- Generate novel hypotheses by uncovering previously unknown predictive features or interactions from complex, high-dimensional data [28] [29].
Foundational Requirements for Multi-Cohort Validation
A brain signature's true utility is determined by its robustness across different patient cohorts. Key requirements for successful multi-cohort validation include:
- Spatial and Model Fit Replicability: A validated signature must demonstrate both consistent spatial identification of brain regions (spatial extent) and stable performance in predicting the outcome of interest (model fit) across independent datasets [1].
- Handling of Cohort Heterogeneity: Discovery and validation cohorts should encompass the full spectrum of variability in pathology, cognitive function, and demographic factors to ensure broad applicability. Studies have shown that replicability depends on large discovery set sizes, often in the thousands, to avoid inflated performance estimates and ensure reproducibility [1].
- Standardized Pre-analytical Protocols: For biofluid-based signatures, variations in sample handling can introduce significant pre-analytical variability. Adherence to evidence-based protocols for sample collection, processing, and storage is critical for reliable biomarker measurement, especially for sensitive analytes like Aβ42 and Aβ40 [30].
Experimental Protocols
This section outlines a standardized, step-by-step protocol for the discovery and validation of ML-derived brain signatures.
Protocol 1: Signature Discovery and Cross-Cohort Validation
Aim: To identify a robust neuroimaging-based brain signature for a specific disease (e.g., AD or PD) and validate its generalizability across multiple independent cohorts.
Table 1: Key Components for Multi-Cohort Signature Discovery
| Component | Description | Example/Cohort Consideration |
|---|---|---|
| Data Cohorts | Use large, diverse datasets for discovery and hold-out cohorts for validation. | Leverage consortium data (e.g., iSTAGING, ADNI, PPMI, UK Biobank). Ensure cohorts have relevant imaging and clinical data [1] [3] [17]. |
| Feature Set | Multivariate patterns from structural MRI. | Features can include voxel-based measures of gray matter volume/thickness and white matter hyperintensities (WMH) [3]. |
| ML Model | Support vector machines (SVM) or other classifiers. | SVM has been successfully used to derive SPARE (Spatial Patterns of Abnormalities for Recognition) indices for various diseases and risk factors [3]. |
| Validation Method | Hold-out test set validation and external validation on unseen cohorts. | Assess both model fit (e.g., AUC, C-index) and spatial reproducibility of the signature [1]. |
| XAI Technique | Model-agnostic interpretation of feature contributions. | SHAP (SHapley Additive exPlanations) is widely used to quantify the contribution of each feature to individual predictions [29] [17]. |
Workflow Diagram: Signature Discovery and Validation Pipeline
Step-by-Step Procedure:
- Cohort Aggregation and Harmonization: Assemble data from multiple cohorts (e.g., N > 20,000 across 10 studies is ideal [3]). Apply stringent quality control and harmonize imaging data to a common coordinate system and processing pipeline to mitigate site-specific biases [1] [3].
- Feature Extraction: Extract relevant neuroimaging features from structural MRI (sMRI) data. This typically involves calculating regional gray matter thickness, volume, and white matter hyperintensity volumes across the brain [3].
- Model Training and Signature Discovery: Train a machine learning model (e.g., Support Vector Machine) to distinguish between disease states or predict clinical outcomes based on the imaging features. The learned multivariate pattern of feature weights constitutes the initial brain signature [3].
- Internal and External Validation:
- Internal Validation: Use resampling methods (e.g., 40 randomly selected discovery subsets of size 400) to generate spatial overlap frequency maps. Define high-frequency regions as the "consensus" signature mask [1].
- External Validation: Apply the consensus signature model to completely independent validation cohorts. Evaluate performance by comparing signature model fits against theory-based models and assess the correlation of model fits across many random subsets of the validation cohort [1].
- XAI Interpretation: Apply XAI methods like SHAP to the validated model. This provides both global interpretability (which features are most important overall) and local interpretability (why a specific patient received a particular prediction), offering insights into the biological basis of the signature [29] [17].
Protocol 2: A Multi-Modal Protocol for PD Cognitive Impairment Prediction
Aim: To develop an explainable ML model for predicting cognitive impairment (CI) in Parkinson's disease using integrated, multi-modal clinical data from several cohorts.
Table 2: Predictors for Cognitive Impairment in Parkinson's Disease
| Predictor Category | Specific Measure | Association with CI |
|---|---|---|
| Demographic | Age at PD Diagnosis | Consistently identified as a top predictor; older age increases risk [17]. |
| Global Cognition | Baseline MoCA Score | Lower scores associated with higher risk of progression to PD-MCI [17]. |
| Visuospatial Function | Benton Judgment of Line Orientation (JLO) | Emerged as a key predictor; better performance lowers PD-MCI risk [17]. |
| Motor Symptoms | MDS-UPDRS Part II (Motor Experiences of Daily Living) | Higher scores (greater impairment) associated with increased CI risk [17]. |
| Non-Motor Symptoms | SCOPA-AUT (Autonomic Dysfunction) | Gastrointestinal and urinary symptoms are predictors of subjective cognitive decline [17]. |
Workflow Diagram: PD Cognitive Impairment Prediction Model
Step-by-Step Procedure:
- Data Integration: Pool de-identified clinical data from multiple PD cohorts (e.g., LuxPARK, PPMI, ICEBERG). Implement cross-study normalization techniques to harmonize the data and reduce cohort-specific biases [17].
- Feature Selection and Engineering: Based on prior literature, select a core set of clinical variables known to be associated with CI in PD. Key predictors often include age at diagnosis, baseline MoCA scores, specific cognitive domain tests (like Benton JLO for visuospatial function), and measures of motor and autonomic function [17].
- Multi-Cohort Model Training: Train models using a multi-cohort approach rather than single-cohort models. This has been shown to provide more stable performance statistics and greater robustness, despite the challenging nature of the prediction task [17]. Use algorithms like XGBoost for classification and Cox proportional hazards or gradient-boosted survival models for time-to-event analysis.
- Prediction and Validation: Train models to predict both objective mild cognitive impairment (PD-MCI) and subjective cognitive decline (SCD) within a defined timeframe (e.g., four years). Validate model performance on held-out test sets from the integrated cohorts using metrics like Area Under the Curve (AUC) for classification and the C-index for survival analysis [17].
- Explainability and Stratification: Apply SHAP analysis to the validated model to identify the most consistent and reliable predictors of CI across cohorts. Conduct sex-stratified analyses, as significant differences in predictor importance and SCD reporting have been observed between men and women [17].
Table 3: Essential Research Reagent Solutions for Signature Identification Studies
| Item | Function/Application | Technical Notes |
|---|---|---|
| K2EDTA Blood Collection Tubes | Standardized plasma collection for biomarker analysis. | The primary collection tube type significantly impacts biomarker levels (e.g., Aβ, NfL, pTau); strict standardization is required [30]. |
| Simoa, Lumipulse, MSD Platforms | High-sensitivity measurement of core and non-core blood-based biomarkers (BBMs). | Used for quantifying Aβ42/40, pTau isoforms (181, 217, 231), GFAP, and NfL. Cross-platform validation is advised [30]. |
| SHAP (SHapley Additive exPlanations) | Post-hoc explainability framework for interpreting ML model outputs. | Provides both global feature importance and local, patient-specific explanations, crucial for clinical translation [29] [17]. |
| SVM with Linear Kernel | For deriving interpretable, linear brain signatures (e.g., SPARE models). | Provides a multivariate weight map where each brain region's contribution to the signature is transparent [3]. |
| XGBoost Classifier | A powerful, tree-based ensemble algorithm for structured clinical data. | Often achieves high accuracy; its built-in feature importance can be supplemented with SHAP for enhanced explainability [29] [17]. |
| Harmonized MRI Processing Pipeline | Consistent feature extraction from structural MRI across cohorts. | In-house or standardized pipelines (e.g., FSL, FreeSurfer) for tissue segmentation, registration, and calculation of regional volumes/thickness [1] [3]. |
Concluding Remarks
The integration of machine learning with explainable AI provides a powerful, systematic framework for identifying and validating robust brain signatures in Alzheimer's and Parkinson's diseases. The protocols outlined here emphasize that rigor in study design—particularly through the use of large, multi-cohort datasets, standardized processing methods, and a commitment to model interpretability—is non-negotiable for generating biologically insightful and clinically actionable results. As the field progresses, these validated, explainable signatures will be indispensable for stratifying patients in clinical trials, monitoring disease progression, and ultimately, for developing personalized therapeutic strategies.
Cardiovascular and metabolic risk factors (CVM) are estimated to contribute to up to 50% of all incident dementia cases globally, with population-attributable risks of 23.8% for hypertension, 14.1% for smoking, 20.9% for obesity, and 12.5% for type 2 diabetes [3]. Understanding the distinct associations between specific CVMs and in vivo brain changes is crucial for disentangling their combined effects and prioritizing intervention targets. The SPARE framework (Spatial Patterns of Abnormalities for Risk Evaluation) represents a machine learning approach to quantify subtle, spatially distributed structural magnetic resonance imaging (sMRI) patterns associated with specific CVMs at the individual patient level [3]. This protocol details the implementation and application of SPARE-CVM models for quantifying these neuroanatomical signatures in cognitively unimpaired individuals.
Experimental Protocols
Data Collection and Cohort Characteristics
The SPARE-CVM framework was developed and validated using harmonized MRI data from 37,096 participants aged 45-85 years from a large multinational dataset comprising 10 cohort studies [3]. An independent validation dataset of 17,096 participants from the UK Biobank study was used for external validation [3].
Table 1: Cohort Characteristics for SPARE-CVM Development
| Characteristic | Training Cohort (iSTAGING) | Validation Cohort (UK Biobank) |
|---|---|---|
| Total Participants | 20,000 | 17,096 |
| Age Range | 45-85 years | 45-85 years |
| Mean Age (SD) | 64.1 (8) years | 65.4 (7.4) years |
| Female Percentage | 54.5% | 53.4% |
| Cognitive Status | Cognitively Unimpaired | Cognitively Unimpaired |
| CVM Conditions | Hypertension, Hyperlipidemia, Smoking, Obesity, Type 2 Diabetes | Hypertension, Hyperlipidemia, Smoking, Obesity, Type 2 Diabetes |
CVM Status Definitions and Ground Truth Labeling
CVM statuses were dichotomized as present (CVM+) or absent (CVM-) based on study-provided categorical responses and medication status where available, augmented using traditional cut-offs applied to continuous clinical measures [3].
MRI Data Acquisition and Preprocessing
All structural MRI data underwent harmonization across the multiple cohorts to ensure compatibility. The specific preprocessing pipeline included:
- Image Quality Control: Visual inspection and automated quality metrics
- Spatial Normalization: Registration to standardized template space
- Tissue Segmentation: Gray matter (GM), white matter (WM), and white matter hyperintensity (WMH) segmentation
- Feature Extraction: Regional volume measurements and intensity features
Machine Learning Model Development
Five separate support vector classification models were trained to detect and quantify spatial sMRI patterns for each CVM: hypertension (HTN), hyperlipidemia (HL), smoking (SM), obesity (OB), and type 2 diabetes mellitus (T2D) [3]. The models were configured to derive SPARE-HTN, SPARE-HL, SPARE-SM, SPARE-OB, and SPARE-T2D indices, respectively.
Model Validation and Statistical Analysis
The SPARE-CVM models underwent rigorous validation using bootstrap resampling to estimate 95% confidence intervals and assess feature stability [31]. Performance was evaluated using:
- Receiver Operating Characteristic (ROC) analysis
- Effect size comparisons with conventional MRI markers
- Association testing with cognitive performance measures
- Cross-validation across demographic subgroups
Results and Performance Metrics
Model Performance Characteristics
The SPARE-CVM models demonstrated robust performance in classifying CVM-related neuroanatomical patterns, with performance metrics detailed in Table 2.
Table 2: SPARE-CVM Model Performance Metrics
| SPARE Model | Training AUC | Validation AUC | Effect Size vs Conventional MRI | Key Sensitive Age Group |
|---|---|---|---|---|
| SPARE-HTN | 0.68 | 0.69 | 10-fold increase | 45-64 years |
| SPARE-HL | 0.67 | 0.66 | 10-fold increase | 45-64 years |
| SPARE-SM | 0.64 | 0.63 | 10-fold increase | 45-64 years |
| SPARE-OB | 0.70 | 0.72 | 10-fold increase | 45-64 years |
| SPARE-T2D | 0.66 | 0.67 | 10-fold increase | 45-64 years |
Neuroanatomical Patterns of Specific CVMs
The SPARE-CVM models revealed distinct spatial patterns of brain alterations associated with each CVM condition, as summarized in Table 3.
Table 3: Distinct Neuroanatomical Signatures of CVMs
| CVM Condition | Cortical GM Patterns | Deep GM Patterns | White Matter Patterns |
|---|---|---|---|
| Hypertension | Atrophy in frontal GM (anterior/posterior insula, frontal/central opercular regions, inferior frontal gyri), parietal regions (postcentral/supramarginal gyri), temporal GM (planum polare/temporale) | Lower volumes in accumbens area | Increased WMH in frontal-parietal regions |
| Hyperlipidemia | Atrophy in middle frontal gyri, orbital gyri, subcallosal area; relatively preserved hippocampal volume | Lower thalamic volumes; higher putamen volumes | Moderate WMH increases |
| Smoking | Global volume loss pattern; specific atrophy in middle frontal gyri, orbital gyri, angular gyrus, entorhinal area, superior temporal gyri, lingual gyri | Lower volumes in accumbens, thalamus, pallidum | Diffuse WMH distribution |
| Obesity | Atrophy in subcallosal area, entorhinal area; relatively preserved volumes in middle occipital gyri, cingulate gyri, supplementary motor cortex, precuneus | Lower volumes in accumbens, pallidum; relatively preserved hippocampal volume | Focal WMH in temporal regions |
| Type 2 Diabetes | Atrophy in posterior orbital gyri, angular gyrus, entorhinal area, superior temporal gyri, lingual gyri, cuneus, calcarine cortices | Lower volumes in accumbens, thalamus, pallidum | Severe WMH in posterior regions |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials and Analytical Tools
| Resource Category | Specific Tool/Resource | Function/Application |
|---|---|---|
| Data Harmonization | iSTAGING Platform | Multi-cohort MRI data integration and harmonization |
| Machine Learning | Support Vector Classification | CVM-specific pattern detection and quantification |
| Model Interpretation | SHAP (SHapley Additive exPlanations) | Feature importance analysis in complex models [32] [31] |
| Dimensionality Reduction | t-SNE (t-distributed Stochastic Neighbor Embedding) | High-dimensional data visualization and clustering [31] |
| Statistical Analysis | Random Forest with Bootstrap Resampling | Predictive modeling with confidence interval estimation [31] |
| Performance Validation | ROC Analysis | Model discrimination capability assessment |
| Cohort Data | UK Biobank MRI | Independent validation dataset |
Analytical Framework for Multi-Cohort Validation
The validation of brain signatures across multiple cohorts requires a standardized analytical framework, as illustrated below:
Discussion and Implementation Guidelines
The SPARE-CVM framework provides a robust methodology for quantifying subtle neuroanatomical changes associated with cardiovascular and metabolic diseases in cognitively unimpaired individuals. The models demonstrated several key advantages:
Enhanced Sensitivity: SPARE-CVM indices outperformed conventional structural MRI markers with a ten-fold increase in effect sizes, capturing subtle patterns at sub-clinical CVM stages [3].
Age-Specific Detection: The models were most sensitive in mid-life (45-64 years), highlighting the importance of early intervention during this critical period [3].
Clinical Relevance: SPARE-CVM scores showed stronger associations with cognitive performance than diagnostic CVM status alone and were associated with brain beta-amyloid status, suggesting relevance for dementia risk stratification [3].
Technical Considerations: Implementation requires careful attention to MRI data harmonization, appropriate validation across diverse populations, and integration with clinical assessments for comprehensive risk evaluation.
The SPARE-CVM framework represents a significant advance in precision medicine for brain health, enabling early detection of CVM-related brain changes and providing a foundation for targeted interventions to mitigate dementia risk.
Application Notes
Rationale and Scientific Foundation
Multimodal integration of structural MRI (sMRI), white matter microstructure, and genetic data represents a transformative approach for identifying robust brain signatures that can predict clinical outcomes and elucidate neurobiological mechanisms. This integration is critical because each modality provides complementary insights: sMRI reveals macroscopic cortical and subcortical structure, diffusion MRI (dMRI) quantifies microstructural white matter integrity and structural connectivity, and genetics uncover the biological underpinnings of brain architecture [33] [34]. The convergence of these modalities is particularly powerful for validating brain signatures across multiple cohorts, as it captures different aspects of brain organization that collectively provide a more complete picture of brain health and disease susceptibility.
Large-scale genome-wide association studies (GWAS) have demonstrated that white matter microstructure is highly heritable, with SNP-based heritability estimates for diffusion tensor imaging (DTI) parameters ranging from 22.4% to 66.5% across different tracts [33]. These genetic influences on white matter organization colocalize with risk loci for brain disorders including glioma, stroke, and psychiatric conditions, establishing a genetic bridge between microstructural abnormalities and clinical endpoints [33]. Simultaneously, machine learning approaches applied to sMRI have successfully derived individualized neuroanatomical signatures for cardiovascular and metabolic risk factors that outperform conventional MRI markers, demonstrating the predictive power of multivariate pattern analysis [3].
Key Applications and Validation Studies
Table 1: Representative Studies of Multimodal Integration for Brain Signature Validation
| Study Focus | Cohort Details | Modalities Integrated | Key Findings | Validation Approach |
|---|---|---|---|---|
| Genetic Architecture of WM Microstructure [33] | 43,802 individuals from UKB, ABCD, HCP, PING, PNC | dMRI (FA, MD, RD, AD, MO), Genotyping arrays | Identified 109 genetic loci associated with WM microstructure; 30 detected via tract-specific functional PCA | Cross-cohort replication in independent samples; LD score regression |
| Multimodal Prediction of Mental Health [34] | >10,000 children from ABCD Study | sMRI, dMRI, Genetics, Behavioral assessments | Two multimodal brain signatures at age 9-10 predicted depression/anxiety symptoms from 9-12 years | Split-half validation in independent subsets; twin discordance analysis |
| CVM-Specific Neuroanatomical Signatures [3] | 37,096 participants from 10 cohorts (iSTAGING+UK Biobank) | sMRI (GM, WM volumes), Clinical CVM status | SPARE-CVM indices captured distinct spatial patterns for hypertension, diabetes, etc.; 10x effect size vs. conventional markers | External validation in UK Biobank; robustness across demographics |
| Alzheimer's Aβ Burden Prediction [35] | 150 ADNI + 101 SILCODE participants | Plasma biomarkers, sMRI, Genetics (PRS, APOE) | Multimodal integration improved Aβ prediction (R²=0.64) vs. plasma+clinical only (R²=0.56) | Cross-cohort validation (ADNI→SILCODE) |
The integration of these modalities has demonstrated particular utility in predicting mental health outcomes. In the large population-based ABCD Study, linked independent component analysis identified multimodal brain signatures in childhood that predicted subsequent depression and anxiety symptoms [34]. These signatures combined cortical variations in association, limbic, and default mode regions with peripheral white matter microstructure, suggesting that the foundational architecture of emotion regulation networks emerges before clinical symptoms manifest.
For neurodegenerative disorders, multimodal integration significantly improves the non-invasive prediction of Alzheimer's disease pathology. The combination of plasma biomarkers, MRI-derived structural features, and genetic risk profiles achieved an R² of 0.64 for predicting cerebral amyloid burden, substantially outperforming models using plasma biomarkers alone (R²=0.56) [35]. This demonstrates how genetic context enhances the predictive power of biochemical and neuroimaging biomarkers.
Experimental Protocols
Multimodal Data Acquisition Protocol
Table 2: Standardized Acquisition Parameters for Multimodal Imaging
| Modality | Recommended Sequences | Key Parameters | Quality Control Measures |
|---|---|---|---|
| Structural MRI | 3D T1-weighted (MPRAGE, SPGR) | Isotropic resolution ≤1mm³; TI=900-1100ms; TR=2300-3000ms; TE=2-3ms | Visual inspection for artifacts; SNR >20; CNR >1.5 |
| Diffusion MRI | Single-shot spin-echo EPI | Multishell: b=1000, 2000 s/mm²; ≥64 directions; Isotropic ≤2mm³; TR=8000-12000ms; TE=80-110ms | Eddy current correction; head motion assessment; FWE <0.5mm |
| Genetic Data | Whole-genome genotyping arrays | Standard platforms (e.g., Illumina Global Screening Array, UK Biobank Axiom) | Call rate >98%; HWE p>1×10⁻⁶; relatedness analysis |
All imaging data should be organized according to the Brain Imaging Data Structure (BIDS) standard to facilitate data sharing and cross-cohort validation [36]. For genetic data, standard quality control procedures should include genotype calling, imputation to reference panels (e.g., 1000 Genomes), and principal component analysis to account for population stratification.
Genetic Association Analysis Protocol for Imaging Traits
Protocol 1: Genome-Wide Association Study for White Matter Microstructure
Phenotype Processing:
- Process dMRI data using standardized pipelines (e.g., ENIGMA-DTI) [33]
- Extract both tract-averaged parameters (FA, MD, RD, AD, MO) and tract-specific functional principal components (FPCA)
- Apply rank-based inverse normal transformation to ensure normality
Quality Control:
- Apply standard GWAS QC: sample call rate >98%, variant call rate >95%, HWE p>1×10⁻⁶, minor allele frequency >1%
- Remove related individuals (KING kinship coefficient >0.044)
- Control for population stratification using genetic principal components
Association Testing:
- Perform linear regression under an additive genetic model
- Covariates: age, sex, imaging site, genetic principal components, intracranial volume (for sMRI)
- For discovery: p<5×10⁻⁸ for genome-wide significance
- For replication: test lead variants in independent cohort with consistent effect direction
Post-GWAS Analyses:
- Heritability estimation using LD score regression [33]
- Genetic correlation with neuropsychiatric disorders and cognitive traits
- Colocalization analysis to identify shared genetic signals with brain disorders
Figure 1: Workflow for Genetic Analysis of Multimodal Imaging Data
Multimodal Integration and Machine Learning Protocol
Protocol 2: Machine Learning Framework for Multimodal Brain Signatures
Feature Extraction:
- sMRI: Regional cortical thickness, surface area, subcortical volumes (FreeSurfer, FSL)
- dMRI: Tract-based fractional anisotropy, mean diffusivity, tract-specific FPCA components [33]
- Genetics: Polygenic risk scores, GWAS-derived weights, or individual SNP genotypes
Feature Harmonization:
- Apply ComBat or cross-platform harmonization to remove site/scanner effects
- Standardize features (z-score) within each cohort
- Handle missing data using multiple imputation or complete-case analysis
Model Training:
- Algorithm: Support vector machines, penalized regression, or random forests
- Training set: 70% of discovery cohort
- Hyperparameter tuning via nested cross-validation
- Regularization to prevent overfitting in high-dimensional feature space
Validation:
- Internal validation: 30% hold-out from discovery cohort
- External validation: Independent cohort with different demographic characteristics
- Performance metrics: AUC, R², mean squared error based on prediction task
Figure 2: Multimodal Integration and Machine Learning Pipeline
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Category | Tool/Resource | Function | Implementation Notes |
|---|---|---|---|
| Data Repositories | UK Biobank, ABCD Study, ADNI, WAND [36] | Provide large-scale multimodal datasets for discovery and validation | Data access applications required; BIDS format recommended |
| Genetic Analysis | PLINK, REGENIE, LDSC, PRSice-2 | GWAS, heritability estimation, polygenic risk scoring | Cloud-optimized versions available for large cohorts |
| Neuroimaging Processing | FSL, FreeSurfer, MRtrix3, ENIGMA-DTI [33] | Structural segmentation, tractography, diffusion parameter estimation | Containerized versions (Docker/Singularity) ensure reproducibility |
| Multimodal Fusion | Linked ICA [34], SMRI-DMRI-Genetics fusion | Identifies covariation across modalities | Python/R implementations available |
| Machine Learning | scikit-learn, XGBoost, BrainLearn [3] | Predictive modeling of brain-behavior relationships | SPARE framework for individualized indices [3] |
| Validation Frameworks | Cross-validation, split-half, twin discordance [34] | Tests robustness and generalizability of signatures | Should include demographic subgroups for bias assessment |
Validation Across Multiple Cohorts
The critical final step in establishing robust brain signatures is rigorous validation across multiple independent cohorts. This process should include:
Technical Validation: Reproducibility of feature extraction and signature calculation across different scanners and acquisition protocols [1]
Generalizability Assessment: Performance consistency across diverse populations (age, sex, ancestry, clinical characteristics) [3]
Longitudinal Validation: Stability of signatures over time and ability to predict future outcomes [34]
Discordant Twin Designs: Testing whether signatures differentiate within twin pairs discordant for behaviors or symptoms [34]
The most robust multimodal signatures will demonstrate small to medium effect sizes (e.g., R²=0.05-0.15 for behavioral outcomes) but consistent replication across these validation frameworks [34]. This multi-cohort validation approach ensures that identified signatures reflect fundamental neurobiological relationships rather than cohort-specific artifacts, making them suitable for translation to clinical applications in early risk detection and personalized intervention.
Overcoming Reproducibility Challenges: Strategies for Reliable and Generalizable Signatures
The pursuit of robust brain signatures—multivariate patterns of brain structure or function that reliably predict behavioral or cognitive phenotypes—is a central goal in modern neuroscience. However, the validity and generalizability of these signatures are critically dependent on the sample sizes used in their discovery. Research consistently demonstrates that small discovery sets are prone to inflation bias and replication failure, fundamentally undermining their utility for cross-cohort validation and drug development pipelines. Brain-wide association studies (BWAS) aimed at linking inter-individual brain variability to complex traits have historically relied on sample sizes appropriate for classical brain mapping (median n≈25), yet these are likely severely underpowered for capturing reproducible brain-behavioral associations [37]. This application note details the quantitative sample size requirements, methodological pitfalls, and experimental protocols necessary to generate brain signatures that maintain predictive validity across diverse populations—a prerequisite for their translation into clinical trials and therapeutic development.
Quantitative Evidence: Sample Size Requirements for Robust Discovery
The Relationship Between Sample Size, Effect Size, and Discovery Likelihood
The probability of successfully detecting true effects in a discovery set is a direct function of sample size and the underlying effect size of the phenomenon under investigation. The following table, adapted from problem discovery sampling principles, illustrates this relationship for a range of plausible effect sizes in neuroimaging research [38].
Table 1: Discovery Likelihood (%) by Sample Size and Problem Probability (Effect Size)
| Sample Size (n) | Effect Size (p) = 0.01 | p = 0.05 | p = 0.10 | p = 0.15 | p = 0.25 | p = 0.50 |
|---|---|---|---|---|---|---|
| 5 | 5% | 23% | 41% | 56% | 76% | 97% |
| 10 | 10% | 40% | 65% | 80% | 94% | ~100% |
| 15 | 14% | 54% | 79% | 91% | 99% | ~100% |
| 20 | 18% | 64% | 88% | 96% | ~100% | ~100% |
| 25 | 22% | 72% | 93% | 98% | ~100% | ~100% |
This table demonstrates that with sample sizes of n=25—typical in many neuroimaging studies—researchers have only a 22% probability of detecting subtle effects affecting 1% of the population. Even for more substantial effects (p=0.15), there remains a 2% chance of complete failure to detect the effect. These principles directly translate to brain signature discovery, where multivariate patterns may comprise both strong and weak neural contributors.
Empirical Evidence from Large-Scale Brain-Wide Association Studies
Analysis of major neuroimaging datasets (total n≈50,000) has quantified the dramatic impact of sample size on reproducibility in brain-behavior mapping. The median univariate effect size (|r|) for brain-wide associations is approximately 0.01, with the top 1% of associations reaching only |r| > 0.06 [37]. At small sample sizes (n=25), the 99% confidence interval for these associations is r ± 0.52, indicating that effect sizes are severely inflated by chance. This inflation decreases as sample sizes grow into the thousands, with replication rates improving accordingly [37].
Table 2: BWAS Reproducibility and Effect Size Inflation vs. Sample Size
| Sample Size (n) | 99% CI for Univariate Associations | Effect Size Inflation (Top 1% Effects) | Replication Outcome |
|---|---|---|---|
| 25 | r ± 0.52 | Extreme | Frequent failure; opposite conclusions possible |
| 500 | r ± 0.12 | Substantial (~78%) | Inconsistent |
| 1,964 (Split-half) | r ± 0.06 | Moderate (~78%) | Improving |
| 3,928 (Full ABCD) | r ± 0.04 | Minimal | Reliable |
The implications are clear: studies with sample sizes in the hundreds—let alone dozens—are essentially guaranteed to produce inflated, unreliable effect estimates that fail to validate in independent cohorts. For context, other population-based sciences like genomics have increased sample sizes from below 100 to over 1,000,000 to robustly characterize small effects [37].
Consequences of Inadequate Sample Sizes
Effect Size Inflation and P-Hacking
Small discovery sets create a perfect environment for effect size inflation and various forms of p-hacking—the practice of collecting, selecting, or analyzing data until non-significant results become significant [39]. Common p-hacking practices include conducting analyses midway through experiments to decide whether to continue collecting data, recording many response variables and deciding which to report post-analysis, and excluding outliers or including covariates post-analysis [39]. These practices, combined with publication bias toward statistically significant results, lead to a literature filled with inflated effects and spurious findings.
Visual examination of p-curves—the distribution of p-values for a set of studies—can reveal p-hacking through an overabundance of p-values just below 0.05 [39]. When researchers p-hack in the presence of a true effect, the p-curve shows a right skew but with an overrepresentation of p-values in the 0.04-0.05 range.
Test Statistic Bias and Inflation in High-Dimensional Data
Epigenome- and transcriptome-wide association studies (EWAS/TWAS) face analogous challenges to brain signature discovery, with test statistics prone to both inflation (overestimation of significance) and bias (deviation of the mode from zero) [40]. These artifacts introduce spurious findings if unaddressed and persist even after applying state-of-the-art confounder adjustment methods [40]. The standard genomic inflation factor commonly used in GWAS is unsuitable for EWAS/TWAS as it overestimates true inflation and fails to address bias [40].
Figure 1: Consequences of small discovery sets on brain signature research. Small samples introduce multiple statistical artifacts that ultimately lead to failed replication and spurious findings in the literature.
Experimental Protocols for Mitigating Inflation Bias
Protocol 1: Multi-Cohort Consensus Brain Signature Discovery
This protocol outlines a method for generating robust brain signatures through aggregation across multiple discovery subsets, as validated in recent research [1] [10].
Objective: To derive a consensus brain signature that demonstrates replicability across population subsamples and independent cohorts.
Materials:
- Data from at least two independent cohorts with neuroimaging and behavioral/cognitive phenotyping
- Sample size of minimum n=400 per discovery cohort subset [1]
- Processing pipeline for regional brain measures (e.g., gray matter thickness)
Procedure:
- Random Subset Selection: In each discovery cohort, randomly select 40 subsets of size n=400. If cohort size is limited, use bootstrapping approaches.
- Feature Association Mapping: For each subset, compute associations between brain features (e.g., voxel-wise gray matter thickness) and the behavioral outcome of interest.
- Spatial Overlap Frequency Maps: Generate frequency maps indicating how often each brain region is selected as significantly associated across the 40 subsets.
- Consensus Signature Definition: Define "consensus" signature regions as those appearing with high frequency (e.g., >80%) across subsets.
- Independent Validation: Test the consensus signature in completely separate validation cohorts, comparing its explanatory power to theory-based models.
Validation Metrics:
- Model fit replicability across multiple random subsets of the validation cohort
- Spatial reproducibility between signatures derived from different discovery cohorts
- Comparative explanatory power versus competing models on full validation cohorts
Recent implementation of this protocol demonstrated high replicability of model fits and spatial convergence of signature regions for episodic memory, outperforming theory-based models [1].
Protocol 2: Empirical Null Estimation and Bias Correction
This protocol addresses test statistic bias and inflation directly through estimation of the empirical null distribution, adapting methods developed for EWAS/TWAS to brain signature research [40].
Objective: To control false positive rates and correct effect size inflation in brain signature discovery.
Materials:
- High-dimensional brain imaging data (e.g., voxel-wise measures, connectivity matrices)
- Behavioral or cognitive phenotype data
- Computational resources for Bayesian mixture modeling
Procedure:
- Initial Association Testing: Perform mass-univariate or multivariate associations between all brain features and the phenotype of interest.
- Empirical Null Estimation: Apply a Bayesian mixture model to estimate the empirical null distribution from the observed test statistics:
- Fit a three-component normal mixture to the test statistics
- One component represents the null distribution (parameters estimate bias and inflation)
- The other two components capture true associations with positive and negative effects
- Bias and Inflation Correction: Use the estimated empirical null distribution (mean = bias, SD = inflation) to calibrate test statistics.
- Confounder Adjustment: Apply state-of-the-art batch correction methods (e.g., SVA, RUV, CATE) prior to empirical null estimation.
- False Discovery Rate Control: Use the calibrated test statistics for inference, controlling the false positive rate at the desired level.
This approach has been shown to maximize power while properly controlling the false positive rate in high-dimensional association studies [40].
Figure 2: Workflow for empirical null estimation and bias correction in brain signature discovery. This protocol controls false positives in high-dimensional brain-behavior association studies.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Computational Tools for Brain Signature Validation
| Reagent/Tool | Function | Implementation Notes |
|---|---|---|
| Multi-Cohort Data Repositories | Provides sufficient sample sizes for discovery and validation | UK Biobank (n=35,735), ABCD Study (n=11,874), ADNI, iSTAGING consortium [37] [3] |
| Harmonized MRI Processing Pipelines | Standardized extraction of brain features across cohorts | DCANBOLD preprocessing, FSL, FreeSurfer, SPM; Critical for cross-cohort compatibility [37] |
| Bayesian Empirical Null Estimation (BACON) | Controls test statistic bias and inflation in high-dimensional data | R/Bioconductor package; Specifically designed for EWAS/TWAS; Adaptable to neuroimaging [40] |
| Machine Learning Frameworks | Multivariate pattern analysis for signature development | Support Vector Machines, Support Vector Regression, Canonical Correlation Analysis [37] [3] |
| Spatial Overlap Frequency Mapping | Identifies consensus signature regions across discovery subsets | Custom scripts generating frequency maps of significant associations across resamples [1] |
| Cross-Validation Frameworks | Internal validation of signature performance | k-fold cross-validation, leave-one-site-out validation for multi-site studies |
The development of brain signatures that generalize across populations requires a fundamental shift in sample size planning and statistical rigor. Based on the evidence presented, the following recommendations are critical for advancing the field:
Plan for Thousands, Not Dozens: Brain-behavior associations are typically much smaller than previously assumed (median |r| ≈ 0.01). Discovery sample sizes should be in the thousands, not the tens or hundreds, to achieve reproducible results [37].
Implement Multi-Cohort Consensus Approaches: The multi-cohort consensus signature protocol provides a robust framework for generating generalizable brain signatures, aggregating across discovery subsets to achieve stability [1].
Address Bias and Inflation Directly: Standard statistical controls are insufficient for high-dimensional brain data. Empirical null estimation methods specifically designed for ome-wide studies should be adapted and applied to neuroimaging [40].
Validate Extensively in Independent Cohorts: Even with adequate discovery sample sizes, independent validation in cohorts with different demographic and clinical characteristics remains essential [1] [3].
Embrace Large-Scale Collaboration: The logistics and costs of acquiring adequate sample sizes necessitate collaborative consortia and data sharing. The field must prioritize resource pooling over small, isolated studies [37] [3].
By adopting these practices, researchers can develop brain signatures with the robustness required for cross-cohort validation, clinical application, and drug development—finally realizing the potential of neuroimaging to illuminate the neural substrates of behavior and cognition.
The validation of robust brain signatures across multiple cohorts is a fundamental challenge in modern neuroscience and clinical drug development. Cohort heterogeneity—arising from demographic, clinical, and technical differences—can significantly confound the identification and generalizability of these signatures. Evidence demonstrates that models trained on data from multiple cohorts perform significantly better in new, unseen settings compared to models developed from a single cohort, even when the total amount of training data is equivalent [41]. This document provides detailed application notes and protocols to systematically account for and manage this heterogeneity, thereby enhancing the reliability and translational potential of cross-cohort brain signature research.
Effective management of heterogeneity begins with a quantitative understanding of the relative impact of different variability sources. The following tables summarize key findings from studies that have quantified these effects.
Table 1: Impact of Technical vs. Population-Based Factors on Model Fairness in Medical AI Based on an analysis of ~1M chest X-ray images from 49 datasets [42].
| Factor Category | Specific Factor | Metric Affected | Effect Size Range |
|---|---|---|---|
| Technical Variability | Imaging Site / Scanner | Deep Features | 0.1 to 0.6 |
| X-ray Energy | Classification Scores | Significant (precise range not provided) | |
| Population-Based Factors | Sex | Deep Features | Up to 0.2 |
| Race | Classification Scores / CAMs | < 0.1 |
Table 2: Statistical Summaries for Comparing Quantitative Data Across Groups General framework for summarizing cohort differences [43].
| Group | Sample Size (n) | Mean | Standard Deviation | Interquartile Range (IQR) |
|---|---|---|---|---|
| Cohort A (e.g., Younger) | 14 | 2.22 | 1.270 | To be calculated from data |
| Cohort B (e.g., Older) | 11 | 0.91 | 1.131 | To be calculated from data |
| Difference (A - B) | N/A | 1.31 | N/A | N/A |
Experimental Protocols for Managing Heterogeneity
Protocol: Multi-Cohort Model Development and Validation
This protocol outlines a procedure for developing a generalizable machine learning model by leveraging multiple cohorts to dilute cohort-specific patterns [41].
I. Materials and Reagents
- Data: Access to at least three distinct patient cohorts. Example: VU University Medical Center (VUMC), Zaans Medical Center (ZMC), and Beth Israel Deaconess Medical Center (BIDMC) cohorts for blood culture prediction [41].
- Software: Standard machine learning libraries (e.g., scikit-learn, TensorFlow, PyTorch) and statistical computing environments (e.g., R, Python).
II. Procedure
- Data Extraction and Harmonization:
- Extract the relevant variables (e.g., laboratory results, vital signs) and the target outcome (e.g., positive blood culture) from each cohort according to a predefined and consistent data dictionary.
- Apply consistent data cleaning and preprocessing rules across all cohorts.
- Experimental Arms:
- Arm 1 (Single-Cohort Training): Train a model on a large sample from a single cohort (e.g., 6000 patients from VUMC).
- Arm 2 (Multi-Cohort Training): Train a model on a mixed dataset from two cohorts, keeping the total sample size equal to Arm 1 (e.g., 3000 patients from VUMC and 3000 from ZMC).
- Model Training:
- Use an identical model architecture and training procedure for both arms.
- Perform hyperparameter tuning using cross-validation within the training set.
- Model Validation:
- Validate the models from both arms on a held-out, completely separate third cohort (e.g., the complete BIDMC cohort, n=27,706).
- Performance and Statistical Comparison:
- Calculate the Area Under the Curve (AUC) for all models in the validation cohort.
- Compare the AUCs of the single-cohort and multi-cohort models.
- Estimate the 95% confidence interval around the difference in AUC using bootstrap resampling (e.g., 10,000 samples) to determine statistical significance.
- Calibration Assessment:
- Generate calibration plots for all models. Note that multi-cohort models may exhibit overconfidence and require recalibration for specific deployment settings [41].
Protocol: Computing and Validating Robust Brain Signatures
This protocol details a method for deriving data-driven brain signatures that are robust across validation cohorts, using an aggregation approach to ensure reproducibility [1].
I. Materials and Reagents
- Imaging Data: T1-weighted structural MRI scans.
- Discovery Cohorts: UC Davis Alzheimer's Disease Research Center (UCD ADRC) Longitudinal Diversity Cohort (n=578) and Alzheimer's Disease Neuroimaging Initiative Phase 3 (ADNI 3) (n=831).
- Validation Cohorts: Separate participants from UCD (n=348) and ADNI Phase 1 (ADNI 1) (n=435).
- Behavioral Data: Cognitive assessments (e.g., neuropsychological memory tests, Everyday Cognition (ECog) scales).
- Software: MRI processing pipelines (e.g., FSL, FreeSurfer), statistical software (R, MATLAB).
II. Procedure
- Image Processing:
- Process T1-weighted MRI scans to extract regional cortical gray matter thickness for each region of interest (ROI) based on a standard atlas (e.g., Desikan-Killiany with 308 ROIs).
- Discovery Phase - Consensus Signature Generation:
- For each discovery cohort (UCD and ADNI 3), randomly select 40 subsets of a fixed size (e.g., n=400 participants).
- Within each subset, compute the association (e.g., via regression) between gray matter thickness in each ROI and the behavioral outcome of interest (e.g., episodic memory score).
- Generate spatial overlap frequency maps from the 40 subsets.
- Define "consensus" signature masks by selecting ROIs that appear as significantly associated with the outcome at a high frequency across the random subsets.
- Validation Phase - Model Fit Replicability:
- Apply the consensus signature models derived from each discovery cohort to the independent validation cohorts.
- Evaluate the replicability of the model fits to the behavioral outcome in 50 random subsets of each validation cohort.
- Calculate the correlation between the model fits from signatures derived from different discovery cohorts to assess consistency.
- Explanatory Power Comparison:
- Compare the explanatory power (e.g., R²) of the data-driven consensus signature models against theory-based or atlas-based models in the full validation cohorts.
Visualization of Workflows
The following diagrams, generated using Graphviz DOT language, illustrate the core logical workflows for the protocols described above.
Multi Cohort Validation
Brain Signature Discovery
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for Multi-Cohort Brain Signature Research
| Item / Reagent | Function / Application | Example Details / Notes |
|---|---|---|
| Multi-Cohort Data | Serves as the foundational substrate for developing generalizable models, diluting cohort-specific patterns. | Example: VUMC, ZMC, BIDMC for clinical prediction; UCD ADRC & ADNI for neuroimaging [41] [1]. |
| Cohort Data Management System (CDMS) | Manages complex, longitudinal cohort data; ensures data integrity, security, and facilitates interoperability. | Must meet key functional (data processing, analysis) and non-functional (security, usability) requirements [21]. |
| Standardized Flow Cytometry Panel | Immunophenotyping to identify cell populations and assess biological variation (e.g., immune signatures). | A 10-color panel for identifying major PBMC populations and T-cell subsets [44]. |
| MRI Data Processing Pipeline | Processes raw MRI data to extract quantitative features (e.g., gray matter thickness, morphometric similarity). | In-house or established pipelines (e.g., Freesurfer) for tissue segmentation, registration, and feature extraction [1] [45]. |
| Morphometric Similarity Network (MSN) | A proxy for structural brain connectivity, derived from multimodal MRI features, used to compute SFC. | Constructed from features like cortical thickness, sulcal depth, and fractional anisotropy [45]. |
| Allen Human Brain Atlas (AHBA) | Provides brain-wide gene expression data to link macroscale imaging findings to molecular mechanisms. | Used for transcriptomic decoding of neuroimaging phenotypes like structure-function coupling variability [45]. |
| Neurotransmitter Atlas | Maps the distribution of neurotransmitter receptors/transporters to interpret neuroimaging findings. | PET-derived maps of serotonin, glutamate, GABA, and opioid systems [45]. |
Harmonizing Multi-Omics and Unmatched Data from Independent Studies
Core Challenge: Data Heterogeneity in Multi-Cohort Studies
Integrating multi-omics data from independent studies presents significant bioinformatics challenges, particularly when samples are unmatched across datasets. This "unmatched multi-omics" scenario requires sophisticated computational approaches to reconcile data generated from different samples, technologies, and experimental designs [46].
The fundamental obstacles include:
- Technical Variability: Different platforms, protocols, and batch effects create systematic noise [46] [47]
- Biological Variability: Population differences, sample collection methods, and cohort-specific characteristics [48]
- Data Structure Incompatibility: Diverse statistical distributions, measurement scales, and data formats across omics layers [46]
- Missing Data Patterns: Incomplete omics layers across different cohorts create analytical gaps [47]
Methodologies for Data Harmonization and Integration
Pre-processing and Quality Control Standards
Effective harmonization begins with rigorous pre-processing of each omics dataset independently [46]:
Genomics/Transcriptomics:
- Format conversion (FASTQ to BAM to count matrices)
- Quality control (FastQC, MultiQC)
- Normalization (TPM, FPKM for RNA-seq) [47]
- Batch effect correction (ComBat, Remove Unwanted Variation) [47]
Proteomics/Metabolomics:
- Peak alignment and annotation
- Intensity normalization
- Missing value imputation (k-NN, matrix factorization) [47]
- Quality-based filtering
Table 1: Data Normalization Standards by Omics Type
| Omics Layer | Normalization Method | Quality Metrics | Common Tools |
|---|---|---|---|
| Genomics | Read depth normalization | Mapping rate >90%, Coverage uniformity | SAMtools, GATK |
| Transcriptomics | TPM, FPKM | RIN >7, Library complexity | featureCounts, DESeq2 |
| Proteomics | Median intensity normalization | CV <20%, Missing data <30% | MaxQuant, OpenMS |
| Metabolomics | Probabilistic Quotient Normalization | QC pool CV <30%, Signal drift <15% | XCMS, MetaboAnalyst |
Integration Strategies for Unmatched Data
Diagonal Integration approaches address the challenge of combining omics from different samples, technologies, and studies [46]:
Multi-Omics Integration Algorithms enable biological insights from unmatched data:
Table 2: Computational Methods for Unmatched Multi-Omics Integration
| Method | Category | Mechanism | Use Case | Implementation |
|---|---|---|---|---|
| Similarity Network Fusion (SNF) | Network-based | Fuses sample-similarity networks from each omics layer | Disease subtyping across cohorts | R: SNFtool [46] |
| MOFA/MOFA+ | Factorization | Discovers latent factors across multiple omics datasets | Identifying shared biological signals | R/Python: MOFA2 [46] |
| DIABLO | Supervised integration | Multiblock sPLS-DA for classification with phenotype guidance | Biomarker discovery with clinical outcomes | R: mixOmics [46] |
| Multi-CCA | Correlation-based | Finds maximal correlation between omics datasets from different samples | Cross-cohort pattern recognition | R: PMA [46] |
Experimental Protocol: Multi-Cohort Brain Signature Validation
Study Design and Cohort Selection
Objective: Validate OXPHOS-related gene signature in grade II/III gliomas across multiple independent cohorts [49] [50].
Cohorts:
- Discovery Cohort: TCGA lower-grade glioma dataset (n=512 samples) [50]
- Validation Cohorts: CGGA (Chinese Glioma Genome Atlas), institutional cohorts
- Clinical Annotation: Overall survival, disease-free survival, tumor grade, treatment history
Inclusion Criteria:
- Histologically confirmed grade II/III glioma
- Available transcriptomic data (RNA-seq or microarray)
- Minimum 2 years clinical follow-up
- Institutional review board approval
Molecular Subtyping Workflow
Protocol Details:
Step 1: Gene Selection and Pre-processing
- Extract expression values for 200 mitochondrial OXPHOS-related genes
- Perform variance-stabilizing transformation on count data
- Normalize using quantile normalization across cohorts
Step 2: Molecular Subtyping using NMF
- Apply non-negative matrix factorization (NMF) to expression matrix of 77 prognostic genes
- Determine optimal cluster number (k=2) using cophenetic correlation coefficient and residual sum of squares [50]
- Assign samples to C1 (favorable prognosis) or C2 (poor prognosis) subtypes
Step 3: Multi-cohort Validation
- Apply consistent subtyping algorithm to independent validation cohorts
- Assess reproducibility using silhouette width and cluster stability metrics
- Validate prognostic significance using Kaplan-Meier survival analysis
Immune Microenvironment Characterization
Computational Deconvolution Methods:
- ESTIMATE: Calculate immune/stromal scores from bulk transcriptomes [50]
- CIBERSORT: Quantify 22 immune cell subpopulations using LM22 signature matrix
- MCP-counter: Absolute abundance estimation of 8 immune and 2 stromal cell types
Table 3: Tumor Microenvironment Analysis in Multi-Cohort Studies
| Analysis Type | Method | Key Findings in C2 Subtype | Biological Interpretation |
|---|---|---|---|
| Global Immune Scoring | ESTIMATE Algorithm | Higher immune scores | Increased tumor-infiltrating lymphocytes |
| Cellular Deconvolution | CIBERSORT | M2 macrophage dominance | Immunosuppressive microenvironment |
| Stromal Assessment | MCP-counter | Elevated stromal scores | Extracellular matrix remodeling |
| Functional Annotation | GSVA, ssGSEA | TGF-β signaling enrichment | T-cell suppression and exclusion |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Resources for Multi-Omics Brain Signature Validation
| Resource Category | Specific Solution | Application | Key Features |
|---|---|---|---|
| Data Integration Platforms | Omics Playground | No-code multi-omics analysis | Implements SNF, MOFA, DIABLO; guided workflows [46] |
| Bioinformatics Suites | Lifebit AI Platform | Federated multi-omics analysis | Autoencoders, GCNs for data integration across sites [47] |
| Molecular Databases | TCGA, CGGA, GEO | Cross-cohort validation | Annotated multi-omics data with clinical outcomes [49] [50] |
| Statistical Environments | R/Bioconductor | Comprehensive omics analysis | Limma (DEGs), survival analysis, NMF clustering [50] |
| Visualization Tools | ggplot2, ComplexHeatmaps | Multi-omics data visualization | Publication-quality figures for integrative results |
| Network Analysis | Cytoscape with omics plugins | Biological pathway integration | Multi-layer network construction and visualization [48] |
Validation Framework for Brain Signatures
Analytical Validation Protocol
Cross-Platform Reproducibility Assessment:
- Technical validation using different sequencing platforms (RNA-seq, microarrays)
- Cross-laboratory reproducibility with standardized protocols
- Computational validation using multiple algorithms and parameter settings
Statistical Robustness Metrics:
- Concordance index for prognostic performance
- Time-dependent ROC analysis at 1, 3, and 5 years
- Multivariate Cox regression adjusting for clinical covariates
Biological Validation Workflow
Experimental Validation Steps:
Step 1: Protein-level Confirmation
- Perform immunohistochemistry on independent glioma specimens
- Quantify expression of MAOB, IGFBP2, SERPINA1, LGR6 proteins
- Correlate protein expression with transcript levels and patient outcomes
Step 2: Functional Validation
- Measure OXPHOS complex activity in subtype-stratified samples
- Assess metabolic dependencies using Seahorse extracellular flux analysis
- Validate signature genes using CRISPR-based perturbation approaches
Step 3: Clinical Utility Assessment
- Evaluate signature performance in treatment-stratified subgroups
- Assess predictive value for targeted therapy response
- Establish clinical decision thresholds using maximum selection statistics
This comprehensive protocol enables robust harmonization of multi-omics data across independent studies, facilitating the validation of molecular signatures in brain cancer research with direct applications to precision medicine and therapeutic development.
The development of robust brain signatures—multivariate patterns of brain activity or structure that predict mental processes, clinical outcomes, or disease progression—represents a paradigm shift in neuroimaging research [9]. Unlike traditional brain mapping approaches that analyze local effects in isolation, predictive brain models combine information distributed across multiple brain systems to generate quantitative, falsifiable predictions about individual subjects [9]. However, the transition from single-study brain maps to clinically applicable models requires rigorous validation across multiple, independent cohorts, a challenge that remains inadequately addressed in the field.
Leave-One-Cohort-Out (LOCO) analysis provides a stringent framework for assessing the generalizability of these brain signatures across diverse populations, scanning sites, and acquisition protocols. This method involves iteratively training a model on all but one cohort and validating it on the held-out cohort, providing a conservative estimate of real-world performance [51]. Despite its theoretical advantages, LOCO analysis introduces unique overfitting challenges that, if unaddressed, can compromise the validity of brain signatures and hinder their translation to clinical applications, particularly in drug development where accurate prediction of treatment response is paramount.
Overfitting occurs when a model learns not only the underlying patterns in the training data but also cohort-specific noise and idiosyncrasies, resulting in excellent performance on training cohorts but poor generalization to unseen cohorts [52] [53]. This review presents a comprehensive framework for optimizing model performance and mitigating overfitting in LOCO analyses, with specific applications to the validation of brain signatures across multiple cohorts.
Theoretical Foundations: Overfitting Mechanisms in LOCO Analysis
The Bias-Variance Tradeoff in Multi-Cohort Studies
The challenge of overfitting in LOCO analysis can be understood through the lens of the bias-variance tradeoff, a fundamental concept in machine learning [54] [52]. Models with high bias (overly simplistic) fail to capture genuine brain-behavior relationships (underfitting), while models with high variance (overly complex) are excessively sensitive to fluctuations in the training cohorts (overfitting).
In LOCO analysis, this tradeoff is further complicated by cross-cohort heterogeneity—systematic differences in participant characteristics, data acquisition protocols, and clinical assessments across cohorts. A model that performs well in internal validation (e.g., cross-validation within training cohorts) may fail dramatically when applied to held-out cohorts due to these heterogeneities, indicating overfitting to cohort-specific features rather than learning generalizable brain-behavior relationships [51].
Two primary sources of overfitting in LOCO analyses deserve particular attention:
Population Differences: Variations in demographic characteristics, clinical subtypes, disease severity, and comorbidities across cohorts can introduce spurious patterns that do not generalize [51]. For instance, a brain signature developed primarily on cohorts from academic research centers may fail when applied to community-based populations due to spectrum bias.
Measurement Variability: Differences in MRI scanner manufacturers, field strengths, acquisition parameters, and preprocessing pipelines create technical variability that can be inadvertently learned by complex models [3]. Without proper mitigation, models may learn to recognize "scanner signatures" rather than biologically meaningful patterns.
Methodological Framework: Protocols for Mitigating Overfitting
Protocol 1: Model Complexity Control through Regularization
Objective: To constrain model complexity and prevent overfitting to cohort-specific noise while retaining sensitivity to genuine biological signals.
Experimental Workflow:
Regularization Technique Selection:
- Implement L1 (Lasso) regularization to encourage sparsity in feature weights, effectively performing feature selection [52] [53].
- Implement L2 (Ridge) regularization to discourage large weights without necessarily eliminating features [52] [53].
- Consider Elastic Net regularization (combining L1 and L2) for scenarios with correlated neuroimaging features [52].
Hyperparameter Tuning:
- Define a grid of regularization strength (λ) values spanning several orders of magnitude.
- For each λ value, perform LOCO analysis, tracking performance on both training and held-out cohorts.
- Select the λ value that optimizes performance on the held-out cohorts while maintaining reasonable training performance.
Validation:
- Compare regularized models against unregularized baseline using metrics sensitive to overfitting (e.g., train-test performance gap).
Figure 1: Regularization protocol workflow for controlling model complexity in LOCO analysis.
Protocol 2: Dimensionality Reduction in High-Dimensional Neuroimaging Data
Objective: To reduce the feature-to-sample ratio that predisposes models to overfitting in neuroimaging data, where features often vastly exceed subjects.
Experimental Workflow:
Feature Selection:
- Apply univariate filtering to retain features most strongly associated with the outcome.
- Implement recursive feature elimination to identify minimal feature sets.
- Use domain knowledge to select biologically plausible features.
Feature Extraction:
- Apply Principal Component Analysis (PCA) to transform correlated neuroimaging features into uncorrelated components.
- Consider independent components analysis (ICA) for identifying spatially independent networks.
- Explore autoencoders for non-linear dimensionality reduction in large-scale datasets.
Validation:
- Compare predictive performance of dimensionality-reduced models against full-feature models in LOCO framework.
- Assess stability of selected features across training folds.
Protocol 3: Ensemble Methods with Controlled Complexity
Objective: To leverage the predictive power of complex models while mitigating overfitting through aggregation.
Experimental Workflow:
Base Model Selection:
- Train multiple decision trees with controlled depth (e.g., maximum depth of 3-6) [54].
- Apply feature bagging at each split to ensure diversity among base learners.
Ensemble Construction:
Validation:
- Compare ensemble performance against individual decision trees in LOCO analysis.
- Monitor out-of-bag error during training as an estimate of generalization error.
Performance Evaluation Framework
Quantitative Metrics for Detecting Overfitting in LOCO Analysis
Systematic evaluation of model performance across multiple metrics provides a comprehensive assessment of overfitting. The following table summarizes key evaluation metrics and their interpretation in the context of LOCO analysis:
Table 1: Performance Metrics for Detecting Overfitting in LOCO Analysis
| Metric | Formula | Interpretation | Overfitting Indicator |
|---|---|---|---|
| Train-Test Performance Gap | AUROCtrain - AUROCtest | Difference between training and held-out cohort performance | >0.1 indicates significant overfitting [52] |
| LOCO Variance | σ²(AUROCi) across i cohorts | Variability in performance across different held-out cohorts | High variance indicates sensitivity to cohort characteristics |
| Performance Degradation Slope | Δ(AUROCtrain - AUROCtest) vs Model Complexity | Rate at which generalization gap increases with model complexity | Steep positive slope indicates overfitting with complexity |
| Cross-Cohort Calibration Error | ECE = ∑i=1M∣Bi∣/n ∣acc(Bi) - conf(Bi)∣ | Difference between predicted and observed probabilities across cohorts | High ECE indicates poor probability estimation in new cohorts |
Case Study: SPARE-CVM Framework for Cardiovascular-Metabolic Risk Factors
A recent large-scale study demonstrates effective mitigation of overfitting in multi-cohort neuroimaging analysis [3]. The SPARE-CVM framework developed individual-level brain signatures for five cardiovascular-metabolic risk factors (hypertension, hyperlipidemia, smoking, obesity, and type 2 diabetes) using harmonized MRI data from 37,096 participants across 10 cohorts.
Key strategies employed to minimize overfitting included:
- Harmonization: Combatting scanner effects through advanced harmonization techniques.
- Regularized Models: Using support vector machines with appropriate regularization.
- External Validation: Testing in completely independent datasets (UK Biobank).
- Complexity Control: Selecting models with optimal complexity tradeoffs.
The resulting brain signatures demonstrated significantly larger effect sizes (ten-fold increase) compared to conventional MRI markers while maintaining generalizability across cohorts, supporting their validity for individualized risk assessment [3].
Table 2: Performance of SPARE-CVM Signatures in Multi-Cohort Validation
| CVM Signature | Training AUC | Validation AUC | Effect Size vs Conventional Markers | Optimal Detection Age |
|---|---|---|---|---|
| Hypertension (SPARE-HTN) | 0.68 | 0.67 | 10.2x | 45-64 years |
| Hyperlipidemia (SPARE-HL) | 0.66 | 0.65 | 8.7x | 45-64 years |
| Smoking (SPARE-SM) | 0.64 | 0.63 | 6.5x | 45-64 years |
| Obesity (SPARE-OB) | 0.70 | 0.72 | 12.1x | 45-64 years |
| Type 2 Diabetes (SPARE-T2D) | 0.69 | 0.68 | 9.8x | 45-64 years |
Case Study: Predicting Cognitive Decline in Multiple Sclerosis
A 5-year longitudinal study in multiple sclerosis (MS) patients employed penalized regression (GLMnet) to identify multi-modal MRI signatures predictive of cognitive decline while mitigating overfitting [56]. The study utilized 70 multi-modal MRI measures from 43 MS patients assessed at baseline and 5-year follow-up.
Key methodological considerations included:
- Feature Selection: The penalized regression approach automatically selected the most predictive features from the high-dimensional feature space.
- Multi-Modal Integration: Combining structural, spectroscopic, and diffusion MRI measures provided complementary information while reducing reliance on any single modality.
- Appropriate Complexity: The optimal model for predicting change in total ARCS score included only 16 of 70 possible features, demonstrating effective complexity control.
The final model explained 54% of variance in cognitive decline (R²=0.54) and predicted cognitive decline with >90% accuracy (AUC=0.92), demonstrating that appropriately regularized models can achieve high predictive performance without overfitting, even in relatively small samples [56].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Computational Tools for Mitigating Overfitting in LOCO Analysis
| Tool Category | Specific Solutions | Function | Application Context |
|---|---|---|---|
| Machine Learning Libraries | Scikit-learn (Python) | Provides regularization, cross-validation, and feature selection methods | General-purpose ML implementation [57] |
| GLMnet (R) | Efficient implementation of penalized regression models | High-dimensional linear modeling [56] | |
| TensorFlow/PyTorch | Deep learning with dropout and early stopping | Complex neural network architectures [57] | |
| Neuroimaging-Specific Tools | SPARE Framework | Individualized index of disease-related patterns | Multi-cohort aging and neurodegenerative studies [3] |
| iSTAGING Consortium | Harmonized MRI processing pipeline | Large-scale multi-cohort neuroimaging [3] | |
| Validation Frameworks | LOCO Cross-Validation | Stringent assessment of cross-cohort generalizability | Final model evaluation before clinical application |
| k-Fold Cross-Validation | Internal performance estimation | Hyperparameter tuning during model development [58] |
Integrated Workflow for LOCO Analysis in Brain Signature Validation
Figure 2: Integrated workflow for brain signature validation with overfitting checks.
The validation of brain signatures across multiple cohorts using LOCO analysis represents a crucial step toward clinically applicable neuroimaging biomarkers. By implementing the protocols and frameworks outlined in this review, researchers can significantly mitigate overfitting risks and develop more generalizable models. Future directions include the integration of explainable AI techniques to enhance model interpretability, federated learning approaches to leverage distributed data while preserving privacy, and advanced regularization methods that incorporate biological constraints. As these methodologies mature, they promise to accelerate the translation of brain signatures from research tools to clinically actionable biomarkers for personalized medicine and drug development.
Application Notes: The Imperative for Explainable AI in Clinical Brain Signature Validation
The application of advanced Machine Learning (ML) in clinical neuroscience, particularly for validating brain signatures across multiple cohorts, presents a fundamental challenge: leveraging complex, high-performance models while ensuring their decisions remain transparent and trustworthy for clinicians and researchers. The "black-box" nature of many sophisticated algorithms can be a significant barrier to clinical adoption, as understanding the "how" and "why" behind a prediction is often as critical as the prediction itself for diagnostic and therapeutic decision-making [28].
The integration of Explainable Artificial Intelligence (XAI) techniques is therefore not merely an academic exercise but a practical necessity. It bridges the gap between computational output and clinical insight, ensuring that models are reliable and their predictions are actionable [28]. This is especially crucial when identifying robust, individual-specific brain signatures that remain stable across diverse aging cohorts or patient populations, as the goal is often to distinguish subtle pathological signals from normal variations [59] [60]. The ethical and legal frameworks for automated decision-making, such as the European Union's General Data Protection Regulation (GDPR), further underscore the right to an explanation, making model interpretability a compliance requirement in addition to a clinical one [28].
Experimental Protocols for Interpretable Model Development and Validation
The following protocols provide a structured methodology for developing and validating interpretable ML models tailored to clinical brain signature research.
Protocol 1: Model Training with Integrated Explainability
Objective: To construct a predictive model for early neurological deterioration (END) in patients with symptomatic intracranial atherosclerotic stenosis (SICAS) using an interpretable machine learning workflow [61].
Step 1: Cohort Definition and Data Preparation
- Population: Retrospectively enroll a cohort of patients meeting specific criteria for SICAS (e.g., ≥45 years, time from symptom onset ≤72 h, MRA-confirmed stenosis ≥30%) [61].
- Data Collection: Extract multi-dimensional clinical data, including:
- Demographics: Age, sex, BMI.
- Comorbidities: Hypertension, diabetes, coronary heart disease.
- Clinical Assessment: Admission NIHSS score, initial systolic and diastolic blood pressure.
- Laboratory Investigations: White blood cell count, lipid profiles, fasting blood glucose. Calculate derived indices like the Triglyceride Glucose (TyG) index [61].
- Imaging Data: Quantify intracranial artery stenosis severity using the WASID method on MRA scans [61].
- Data Preprocessing: Handle missing data (e.g., exclude variables with >5% missingness, impute others). Randomly split the dataset into a training set (70%) and a validation set (30%) [61].
Step 2: Predictive Feature Selection
- Apply the Least Absolute Shrinkage and Selection Operator (LASSO) regression on the training set to select features with non-zero coefficients, thus reducing dimensionality and identifying the most predictive variables from the clinical and imaging dataset [61].
- Incorporate 10-fold cross-validation during LASSO feature selection to maximize the area under the ROC curve (AUC) [61].
Step 3: Model Building and Training
- Train multiple ML algorithms (e.g., Logistic Regression, Extreme Gradient Boosting (XGBoost), Gaussian Naive Bayes) on the training set using the selected features [61].
- Address class imbalance in the training data using techniques like the Synthetic Minority Over-sampling Technique (SMOTE) [61].
- Employ 10-fold cross-validation on the training set to tune model hyperparameters and prevent overfitting [61].
Step 4: Model Interpretation with SHAP
- Apply SHapley Additive exPlanations (SHAP) to the best-performing model (e.g., XGBoost) to interpret its output [61].
- Use SHAP summary plots and dependence plots to quantify the contribution of each feature (e.g., NIHSS score, stenosis severity, TyG index) to individual predictions, identifying the strongest drivers of the model's output [61].
Protocol 2: Leverage-Score Sampling for Stable Brain Signature Identification
Objective: To identify a stable subset of individual-specific neural features from functional connectomes that are resilient to age-related changes, facilitating validation across multiple cohorts and age groups [60].
Step 1: Neuroimaging Data Acquisition and Preprocessing
- Dataset: Utilize a publicly available dataset like the Cambridge Center for Aging and Neuroscience (Cam-CAN), which includes resting-state and task-based fMRI from a cohort aged 18-88 years [60].
- Preprocessing: Process fMRI data through a standardized pipeline including realignment (motion correction), co-registration to structural images, spatial normalization, and smoothing [60].
- Connectome Construction: For each subject and atlas (e.g., AAL, HOA, Craddock), parcellate the brain into regions and compute a Functional Connectome (FC). This is a Pearson Correlation matrix
Cwhere each entry(i, j)represents the correlation between the time-series of regionsiandj[60].
Step 2: Data Structuring for Group Analysis
- Vectorize each subject's symmetric FC matrix by extracting the upper triangular elements.
- Stack these vectors to form a population-level matrix
Mfor each task (e.g.,M_rest,M_movie), where rows represent FC features (edges) and columns represent subjects [60]. - For age-specific analysis, partition the subjects into non-overlapping age cohorts and form cohort-specific matrices [60].
Step 3: Feature Selection via Leverage-Score Sampling
- Compute the leverage score for each row (FC feature) in a cohort-specific matrix
M. The leverage score for thei-th row is defined asl_i = ||U_{i*}||², whereUis an orthonormal matrix spanning the columns ofM[60]. - Sort the leverage scores in descending order. The highest-scoring features are those with the most influence in capturing population-level variability within the cohort.
- Retain the top
kfeatures to obtain a compact, informative set of neural signatures that are highly specific to individuals [60].
- Compute the leverage score for each row (FC feature) in a cohort-specific matrix
Step 4: Cross-Cohort and Cross-Atlas Validation
- Assess the consistency of the selected neural features by measuring the overlap (e.g., ~50%) between signature sets identified in consecutive age groups [60].
- Validate the stability of the methodology by repeating the leverage-score sampling across different brain parcellation atlases (e.g., AAL, HOA, Craddock) and confirming a significant overlap in the identified features [60].
Data Presentation
Table 1: Machine Learning Models and Explainability Techniques in Brain Disease Studies
This table summarizes models and techniques identified from a systematic review of 133 studies (2014-2023) on explainable ML in brain diseases [28].
| Category | Name | Key Characteristics | Primary Application in Clinical Context |
|---|---|---|---|
| Explainable ("White Box") ML Models | Logistic Regression | Intrinsically interpretable; provides coefficients showing feature influence. | Baseline model for clinical prediction rules; suitable when relationships are primarily linear [61]. |
| Gaussian Naive Bayes | Based on Bayesian probability; simple and fast. | A distinct benchmark for probabilistic classification compared to more complex models [61]. | |
| Non-Explainable ("Black Box") ML Models | Extreme Gradient Boosting (XGBoost) | High-performance gradient boosting; robust to non-linear relationships. | High-accuracy prediction of clinical outcomes (e.g., Early Neurological Deterioration) [61]. |
| Gradient Boosting Decision Trees (GBDT) | Classical implementation of gradient boosting. | Modeling complex, non-linear relationships in multi-dimensional clinical data [61]. | |
| Light Gradient Boosting Machine (LightGBM) | Computational efficiency with high performance on large datasets. | Ideal for processing large-scale datasets, such as those from multi-center cohorts [61]. | |
| Explainability Techniques (ETs) | SHapley Additive exPlanations (SHAP) | Game theory-based; provides unified feature importance for individual predictions. | Interpreting "black-box" models like XGBoost; reveals key clinical drivers (e.g., NIHSS score, stenosis severity) [61]. |
| Leverage-Score Sampling | Matrix sampling technique to identify high-influence data points. | Identifying a stable subset of individual-specific neural features from functional connectomes for cross-cohort validation [60]. |
Table 2: Core Clinical and Imaging Predictors for Neurological Deterioration
This table details key predictors identified by an interpretable ML model (XGBoost + SHAP) for forecasting END in SICAS patients [61].
| Predictor Variable | Data Type / Units | Description & Measurement | Role in Model (from SHAP) |
|---|---|---|---|
| NIHSS Score | Continuous / Integer | Admission National Institutes of Health Stroke Scale score; assessed by certified neurologists. | Strongest driver of END risk prediction. |
| Vascular Stenosis Severity | Categorical / % | Measured via MRA using WASID criteria: Mild (30-50%), Moderate (50-70%), Severe (>70%). | Key predictor; higher severity increases END risk. |
| TyG Index | Continuous | Triglyceride Glucose Index = Ln[TG (mg/dL) × FBG (mg/dL)/2]; marker of insulin resistance. | Major metabolic predictor of END risk. |
| Age | Continuous / Years | Patient age at admission. | Significant contributor; advanced age increases risk. |
| Initial Systolic Blood Pressure | Continuous / mmHg | First recorded systolic blood pressure upon admission. | Important hemodynamic factor. |
| Diabetes | Binary (Yes/No) | History of diabetes mellitus, as a comorbidity. | Contributing comorbidity to END risk. |
Visualization
Model Interpretation Workflow
Brain Signature Validation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Analytical Tools for Interpretable ML Research
| Item / Tool | Function / Purpose | Application Note |
|---|---|---|
| 3.0 Tesla Siemens MRI Scanner | Acquires high-resolution structural and functional neuroimaging data. | Used for obtaining T1-weighted, T2-weighted, FLAIR, and Time-of-Flight (TOF) MRA images essential for quantifying intracranial stenosis and lesion identification [61]. |
| Python & R Open-Source Libraries | Provides the computational environment for data analysis, model building, and interpretation. | Key libraries include Scikit-learn for models (LR, GNB), XGBoost/LightGBM for boosting, SHAP for explainability, and PyTorch/TensorFlow for deep learning [61]. |
| SHAP (SHapley Additive exPlanations) | Explains the output of any ML model by quantifying the marginal contribution of each feature. | Critical for interpreting "black-box" models like XGBoost; generates global feature importance and local explanations for individual patient predictions [61]. |
| LASSO Regression | A regularization technique for feature selection that penalizes absolute coefficient size. | Applied to high-dimensional clinical data to select a parsimonious set of predictive features for model building, reducing overfitting [61]. |
| SMOTE (Synthetic Minority Over-sampling Technique) | Addresses class imbalance in datasets by generating synthetic samples of the minority class. | Used in the training phase to prevent model bias against the less frequent outcome (e.g., patients who experience END), improving predictive accuracy for the target class [61]. |
| Standardized Brain Atlases (AAL, HOA, Craddock) | Provide anatomical or functional parcellations of the brain into distinct regions. | Used to define nodes for functional connectome analysis; enables consistency and reproducibility in neuroimaging studies across different research groups [60]. |
Validation Protocols and Comparative Performance: Establishing Clinical Utility
The development of reliable biomarkers and brain signatures for personalized medicine requires research strategies that rigorously test and validate findings. A foundational principle underlying these strategies is the physical or temporal separation of data used for initial discovery from data used for validation. This separation is critical for demonstrating that results are not artifacts of a specific dataset but are robust and generalizable across different populations and settings [62]. This paper outlines the core principles, methodologies, and protocols for implementing robust validation paradigms in research aimed at validating brain signatures across multiple cohorts.
Core Principles and Cohort Definitions
The separation of discovery and validation cohorts mitigates overoptimism and statistical overfitting that occur when models are tested on the same data from which they were derived. This process ensures that identified signatures can generalize to new, unseen patient populations [62] [17].
Comparison of Cohort Types and Designs
The table below summarizes the key characteristics, advantages, and challenges of different cohort designs used in stratified medicine.
Table 1: Comparison of Cohort Designs for Discovery and Validation
| Cohort Aspect | Prospective Cohorts | Retrospective Cohorts | Integrated Multi-Cohorts |
|---|---|---|---|
| Primary Use | Hypothesis testing, validation of preliminary findings | Initial discovery, hypothesis generation | Enhancing generalizability and statistical power |
| Key Advantage | Enables optimal measurement quality control; minimizes bias [62] | Rapid, cost-effective access to existing data and samples [62] | Improves model robustness and reduces cohort-specific bias [17] |
| Key Challenge | Time-consuming and expensive to establish and follow | Potential for missing or inconsistent data [62] | Requires harmonization of data from different sources [63] |
| Data Generation | Standardized protocols at study onset | Relies on historically collected data | Combined prospective and retrospective data |
| Sample Size | Defined by pre-study calculation | Limited by available archived data | Large, pooled samples from multiple sources [63] |
Foundational Validation Framework: The V3 Model
A comprehensive framework for evaluating biometric monitoring technologies (BioMeTs) and, by extension, biomarker signatures, is the Verification, Analytical Validation, and Clinical Validation (V3) model [64]. This framework is directly supported by the physical separation of cohorts, with verification and analytical validation often performed on the discovery cohort, and clinical validation requiring a distinct, independent cohort.
The Three Components of the V3 Framework
- Verification: A systematic, often technical, evaluation of the tool or assay itself. This step asks, "Was the tool built correctly?" It involves testing sensor outputs, algorithm performance, and system stability, typically in silico or in vitro [64].
- Analytical Validation: This step assesses whether the tool or signature accurately measures the analyte or biological phenomenon it intends to measure. It translates evaluation from the bench to in vivo settings and is performed to ensure the data processing pipeline generates accurate and precise metrics [64].
- Clinical Validation: This critical step demonstrates that the signature acceptably identifies, measures, or predicts a clinically relevant state or outcome in the intended population and context of use. It must be performed on independent cohorts of patients with and without the phenotype of interest [64].
Experimental Workflow for Multi-Cohort Validation
The following diagram illustrates a generalized workflow for a validation study that adheres to the V3 framework and utilizes separate discovery and validation cohorts.
Diagram 1: Multi-Cohort Validation Workflow
Detailed Protocols and Application Notes
Protocol: Machine Learning for Predictor Identification in Multi-Cohort Studies
This protocol is adapted from a study identifying predictors of cognitive impairment in Parkinson's disease using three independent cohorts (LuxPARK, PPMI, ICEBERG) [17].
Table 2: Key Reagents and Computational Tools for Multi-Cohort ML
| Research Reagent / Solution | Function / Explanation |
|---|---|
| Independent Patient Cohorts | Source of data for discovery and validation; provides clinical, imaging, and omics data. Essential for testing generalizability. |
| Data Harmonization Tools | Software and statistical methods (e.g., cross-study normalization, batch effect correction) to minimize technical variance between cohorts. |
| Machine Learning Algorithms | Algorithms (e.g., Random Forest, LASSO) used to identify patterns and build predictive models from high-dimensional data. |
| Resampling Methods (e.g., k-fold CV) | Technique used within the discovery cohort to assess model stability and prevent overfitting during the development phase. |
| Explainable AI (XAI) Tools | Methods like SHapley Additive exPlanations (SHAP) to interpret model predictions and identify key biomarkers or predictors. |
Procedure:
- Cohort Integration and Pre-processing: Pool data from multiple independent cohorts. Apply stringent pre-processing and cross-study normalization to correct for technical variance and batch effects [17] [63].
- Cohort Stratification: Designate one or more cohorts as the discovery set and hold out at least one entirely independent cohort for validation. Alternative approaches include "leave-one-cohort-out" analysis [17].
- Feature Selection and Model Training in Discovery Cohort: Implement a robust feature selection process within the discovery cohort. For example, use a repeated k-fold cross-validation (e.g., 10-fold) combined with multiple algorithms (e.g., LASSO, Boruta). Retain only features identified as robust across a high percentage (e.g., 80%) of models and folds [63].
- Model Building: Construct a final model (e.g., a Random Forest classifier) using the robustly selected features on the entire discovery dataset.
- Clinical Validation: Apply the locked model to the held-out validation cohort(s) without any further model tuning. Evaluate performance using pre-specified metrics (e.g., AUC, C-index) [17].
- Interpretation and Validation: Use XAI to interpret the validated model and identify the most consistent predictors across cohorts (e.g., age at diagnosis and visuospatial ability in the PD study) [17].
Protocol: Robust Biomarker Discovery from Integrated Transcriptomic Data
This protocol is based on a study identifying a composite biomarker for pancreatic ductal adenocarcinoma (PDAC) metastasis using RNAseq data from five public repositories [63].
Procedure:
- Data Sourcing and Stratification: Obtain data from multiple public repositories (e.g., TCGA, GEO, ICGC). Stratify samples into "non-metastasis" and "metastasis" groups based on clinical staging. Split datasets into a training set (for discovery) and a hold-out validation set (e.g., CPTAC-PDAC, GSE79668) [63].
- Data Pre-processing and Integration: Normalize data (e.g., using TMM normalization) and filter out lowly expressed genes. Perform batch effect correction (e.g., using ARSyN) on the combined training and validation data to remove technical variance while preserving biological signal [63].
- Robust Variable Selection in Training Set: On the training set only, execute a multi-step variable selection pipeline:
- Perform 10-fold cross-validation.
- Within each fold, run 100 models that combine multiple selection algorithms (LASSO, Boruta, and backwards selection).
- Define a consensus list of biomarker candidates as genes that appear in a high consensus threshold (e.g., ≥80% of models and ≥5 folds) [63].
- Model Construction and Validation: Build a random forest model using the consensus genes on the training data. Evaluate its predictive performance on the held-out validation dataset using metrics appropriate for imbalanced data (e.g., Precision, Recall, F1 score) [63].
- Biological Contextualization: Perform pathway analysis on the validated gene set to understand their biological relevance and link to disease mechanisms [63].
The rigorous separation of discovery and validation cohorts is a non-negotiable standard for generating credible, clinically relevant research findings. By adopting the V3 framework and implementing the detailed protocols for multi-cohort machine learning and biomarker discovery, researchers can significantly enhance the robustness, generalizability, and translational potential of their work on brain signatures and other biomarkers.
Assessing Model Fit Replicability and Spatial Extent Consistency Across Cohorts
Validating brain signatures across multiple cohorts is a critical step in establishing robust, generalizable biomarkers for neurological diseases and cognitive functions. The core of this validation lies in demonstrating two key properties: model fit replicability (the ability of a signature to reliably predict an outcome in independent datasets) and spatial extent consistency (the reproducibility of the neuroanatomical regions selected by the signature across different populations) [1]. This protocol details application notes and experimental methodologies for rigorously assessing these properties, framed within a multi-cohort research paradigm essential for drug development and translational neuroscience.
Quantitative Benchmarks and Performance Standards
The tables below summarize key quantitative benchmarks for evaluating model performance and spatial consistency, derived from recent validation studies.
Table 1: Performance Benchmarks for Model Fit Replicability in Multi-Cohort Studies
| Metric | Reported Performance | Cohort Details | Interpretation |
|---|---|---|---|
| Model Fit Correlation | >0.90 correlation of model fits in 50 random validation subsets [1] | Alzheimer's Disease Neuroimaging Initiative (ADNI) and UC Davis ADRC [1] | Indicates high replicability of the signature's predictive power. |
| Explanatory Power (R²) | Outperformed competing theory-based models in full-cohort comparisons [1] | ADNI and UC Davis ADRC [1] | Signature model captures more outcome variance than established alternatives. |
| Cognitive Decline Prediction | >90% accuracy (AUC=0.92) in predicting 5-year cognitive decline [56] | Multiple Sclerosis cohort (N=43) [56] | Demonstrates high prognostic value in a clinical population. |
| Prediction Variance (R²) | Explained 54% of variation (R²=0.54) in cognitive change over 5 years [56] | Multiple Sclerosis cohort (N=43) [56] | Multi-modal signatures account for a substantial portion of outcome variance. |
Table 2: Standards for Assessing Spatial Extent Consistency
| Metric | Reported Benchmark | Cohort/Paradigm Details | Interpretation |
|---|---|---|---|
| Spatial Overlap | Convergent consensus signature regions from spatial overlap frequency maps [1] | Discovery in 40 random subsets of 400 participants each [1] | High-frequency regions are reliably associated with the outcome. |
| Cross-Cohort Agreement | Mean spatial correlation of r = 0.57 (SD = 0.18) for g-morphometry associations [65] | Meta-analysis of UK Biobank, GenScot, LBC1936 (N=38,379) [65] | Indicates moderate to good cross-cohort consistency of brain-cognition maps. |
| Individual Heterogeneity | No more than 27% of preterm adults shared extranormal deviations in the same cortical region [66] | Bavarian Longitudinal Study (BLS) [66] | Highlights substantial individual variability against which consistency must be measured. |
| Feature Stability | ~50% overlap of top leverage score features between consecutive age groups [60] | Cam-CAN cohort (Ages 18-87) [60] | Suggests a stable core of individual-specific features across the adult lifespan. |
Core Experimental Protocols
Protocol for Discovery of Consensus Brain Signatures
This protocol is designed to generate a robust, data-driven brain signature in the discovery phase, minimizing overfitting and maximizing the potential for replicability [1].
Primary Application: Initial feature selection and model generation for a behavioral or clinical outcome.
Workflow Overview:
- Input Data Preparation: Utilize T1-weighted structural MRI scans. Process images through a standardized pipeline (e.g., FreeSurfer) to extract vertex-wise or region-wise morphometric data (e.g., cortical thickness, surface area) [1] [65].
- Multi-Subset Discovery: a. Random Sampling: From your discovery cohort(s), randomly generate a large number (e.g., 40) of subsets. The subset size (e.g., n=400) should be chosen to balance computational feasibility and statistical power [1]. b. Feature-Outcome Association: Within each subset, perform a mass-univariate analysis (e.g., voxel-wise or vertex-wise regression) to identify brain areas where the structural metric is associated with the outcome of interest (e.g., episodic memory score). c. Spatial Overlap Mapping: For each analysis, create a binary map of significant regions. Aggregate these maps across all subsets to create a spatial frequency map, which indicates how often each brain area was selected.
- Consensus Mask Definition: Define the final "consensus signature" as the regions that appear in a high proportion (e.g., >70%) of the discovery subsets. This mask represents the most reliably associated neuroanatomical substrate [1].
Protocol for Validation of Model Fit Replicability
This protocol tests whether the discovered signature generalizes to entirely independent cohorts, which is the ultimate test of a useful biomarker.
Primary Application: Testing the generalizability and stability of a pre-defined brain signature.
Workflow Overview:
- Validation Cohort Curation: Assemble one or more independent validation cohorts that are distinct from the discovery data. These cohorts should have the same MRI sequences and outcome measures but can differ in demographic or clinical characteristics to test broad generalizability.
- Model Application: a. For each subject in the validation cohort, extract the average value of the imaging metric (e.g., mean cortical thickness) within the pre-defined consensus signature mask. b. Use this extracted value in a statistical model (e.g., linear regression) to predict the outcome variable in the validation cohort.
- Replicability Assessment: a. Correlation of Fits: Calculate the correlation between the predicted outcome values from the signature model when applied to multiple random halves of the validation cohort. A high correlation (>0.9) indicates excellent replicability [1]. b. Explanatory Power: Compare the variance explained (R²) by the signature model to that of competing models (e.g., theory-based ROI models). The signature model should demonstrate superior or equivalent performance [1]. c. Resampling Validation: Repeat the model fitting in numerous (e.g., 50) bootstrapped or randomly sampled subsets of the validation cohort to generate a distribution of model performance metrics and ensure stability [1].
Protocol for Assessment of Spatial Extent Consistency
This protocol evaluates the anatomical consistency of the discovered features across different populations and datasets.
Primary Application: Quantifying the neuroanatomical reproducibility of a brain signature.
Workflow Overview:
- Multi-Cohort Mapping: Independently derive brain-outcome association maps for the same outcome variable in two or more separate cohorts. This can be done using the full cohorts or via the multi-subset discovery method outlined in Protocol 3.1.
- Spatial Correlation Analysis: a. Register all association maps to a common standard space (e.g., fsaverage, MNI). b. Calculate the spatial correlation (e.g., Pearson's r) between the entire brain maps (vectorized) from different cohorts. This provides a whole-cortex measure of pattern similarity [65].
- Regional Overlap Analysis: a. Binarize the association maps from each cohort using an appropriate statistical threshold. b. Calculate the Dice coefficient or similar overlap metric to quantify the spatial agreement of significant clusters between cohorts. c. Visually inspect and report regions of convergence and divergence [66].
- Leverage Score Analysis for Feature Stability (Alternative Method): a. From the functional or structural connectome of each subject, compute a matrix of features (e.g., all pairwise connections). b. For a given age or diagnostic cohort, compute the leverage scores for each feature, which quantify its importance in explaining the population-level data structure. c. Identify the top-k features with the highest leverage scores as the "signature" for that cohort. d. Assess the consistency of this signature by calculating the overlap (e.g., Jaccard index) of the top-k features between different cohorts or age groups [60].
Visualization of Workflows
The following diagrams illustrate the logical relationships and workflows for the core protocols.
Signature Derivation and Validation
Diagram 1: Integrated workflow for deriving a consensus brain signature from discovery cohorts and subsequently validating its model fit replicability and spatial extent consistency in independent cohorts.
Multi-Cohort Federated Learning Paradigm
Diagram 2: The federated learning paradigm for multi-cohort analysis. This privacy-preserving approach allows models to be trained on data from multiple institutions without transferring the raw data itself, thereby enhancing the generalizability and robustness of derived signatures [67].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Multi-Cohort Signature Validation
| Item/Tool | Function/Application | Example/Notes |
|---|---|---|
| FreeSurfer | Automated cortical reconstruction and subcortical segmentation from T1-weighted MRI. Generates morphometric data (thickness, volume, area). | Primary software for generating input features for structural brain signatures [1] [67]. |
| SynthSR & LoHiResGAN | Deep learning models for enhancing ultra-low-field (ULF) MRI to be quantitatively comparable with high-field (3T) MRI. | Critical for harmonizing data across different scanner types and improving accessibility [68]. |
| UK Biobank, ADNI, Cam-CAN | Large-scale, publicly available neuroimaging datasets with cognitive and biomarker data. | Essential validation cohorts for testing signature generalizability [65] [69] [60]. |
| Leverage Score Sampling | A deterministic feature selection method to identify the most influential functional connectome edges for individual fingerprints. | Used to find stable, individual-specific neural features across the lifespan [60]. |
| BrainChart Framework | A normative reference model for human brain development across the lifespan, based on ~100,000 subjects. | Allows quantification of individual deviation from typical aging trajectories [66]. |
| Federated Learning Infrastructure | A distributed machine learning approach that trains models across multiple decentralized data holders without sharing the data. | Enables validation across privacy-restricted cohorts (e.g., healthcare systems) [67]. |
| Centiloid & CenTauR Scales | Standardized scales for harmonizing amyloid-β PET and tau PET measurements across different tracers and scanners. | Key for validating signatures against core Alzheimer's disease pathologies [70]. |
The validation of robust brain signatures is a critical endeavor in neuroimaging, particularly for their application in diagnostic and therapeutic development for neurodegenerative diseases. This document outlines application notes and experimental protocols for benchmarking data-driven brain signature models against established theory-based measures, with a specific focus on hippocampal volume. Framed within a broader thesis on cross-cohort validation, these protocols provide researchers and drug development professionals with standardized methods for assessing the performance, generalizability, and explanatory power of emerging biomarker models. The comparative framework emphasizes rigorous statistical validation across multiple, independent cohorts to ensure that signature models offer genuine advantages over conventional approaches in explaining cognitive outcomes, particularly in the domain of episodic memory.
Quantitative Performance Benchmarks
The table below summarizes key quantitative findings from studies that have directly compared the performance of signature models, theory-based models, and hippocampal volume measures in explaining cognitive variance.
Table 1: Comparative Performance of Brain Measurement Models in Explaining Episodic Memory
| Model Type | Specific Model | Cohort(s) Tested | Performance Metric | Reported Value | Key Comparative Finding |
|---|---|---|---|---|---|
| Data-Driven Signature | Voxel-Aggregation Signature ROI [2] | ADC, ADNI1, ADNI2/GO | Adjusted R² (Baseline Memory) | Not Specified | Outperformed theory-driven and other data-driven models [2]. |
| Data-Driven Signature | Consensus Signature Model [10] | Multiple Validation Cohorts | Model Fit to Outcome | Not Specified | Outperformed competing theory-based models [10]. |
| Theory-Based Measure | Hippocampal Volume [71] | AD Patients (n=40) | Correlation with MMSE | r = ~0.54 (Moderately Strong) | Manual volumetry superior to visual rating [71]. |
| Theory-Based Measure | Hippocampal Subfield Volume (CA1) [72] | aMCI Patients (n=38) | Prediction of Memory Performance | Significant Predictor | CA1 volume predicted concurrent memory performance in aMCI [72]. |
| Theory-Based Measure | Multi-Region Theory-Driven Model [2] | ADC, ADNI1, ADNI2/GO | Adjusted R² (Baseline Memory) | Not Specified | Outperformed by the voxel-aggregation signature model [2]. |
Experimental Protocols for Benchmarking Studies
Protocol: Cross-Cohort Signature Validation
This protocol is designed to test the robustness and generalizability of a brain signature model by deriving it in one cohort and validating its performance in independent cohorts [2] [10].
1. Objective: To determine whether a signature region of interest (ROI) generated in one imaging cohort replicates its performance level when explaining cognitive outcomes in separate, independent cohorts.
2. Materials and Reagents:
- Imaging Data: T1-weighted structural MRI scans from at least three non-overlapping cohorts.
- Cohort Characteristics: Cohorts should include a spectrum of cognitive states (e.g., cognitively normal, mild cognitive impairment, dementia) to test model robustness [2].
- Cognitive Data: Standardized episodic memory assessments (e.g., ADNI-Mem, SENAS) [2].
- Software: Image processing and statistical analysis software (e.g., Freesurfer, SPM, R/Python).
3. Procedure:
- Step 1: Cohort Selection. Secure data from three independent, non-overlapping cohorts (e.g., UC Davis ADC, ADNI1, ADNI2/GO) [2].
- Step 2: Image Processing. Process all T1-weighted MRI scans using a standardized pipeline. This includes spatial normalization, tissue segmentation into grey matter, white matter, and CSF, and smoothing.
- Step 3: Signature Derivation (Discovery). In one "discovery" cohort (e.g., ADC), perform a voxel-wise regression analysis with baseline episodic memory as the outcome variable. Correct for multiple comparisons. Aggregate significant voxels to create a signature ROI mask [2].
- Step 4: Model Application (Validation). Extract the mean grey matter value from the signature ROI in the other "validation" cohorts (e.g., ADNI1, ADNI2/GO).
- Step 5: Performance Benchmarking. In each validation cohort, fit a regression model with the extracted signature value predicting episodic memory. Record the model's explanatory power (e.g., Adjusted R²).
- Step 6: Comparative Analysis. Compare the signature model's Adjusted R² against the performance of pre-specified theory-based models (e.g., hippocampal volume, medial temporal lobe volume) within the same validation cohorts [2].
4. Analysis: A signature is considered robustly validated if it explains a similar or greater amount of variance (Adjusted R²) in the independent validation cohorts compared to both the discovery cohort and theory-based benchmarks.
Protocol: Longitudinal Memory Change Analysis
This protocol assesses the sensitivity of different models to predict change in cognitive function over time, a key metric for clinical trials.
1. Objective: To evaluate whether baseline structural measures (signature ROI vs. hippocampal volume) can predict longitudinal episodic memory decline.
2. Materials and Reagents:
- Longitudinal Data: MRI and cognitive test data from at least two time points, with a minimum of one year between assessments [2].
- Software: Longitudinal image processing pipelines (e.g., Freesurfer longitudinal stream) are recommended.
3. Procedure:
- Step 1: Data Processing. Process longitudinal MRI scans using a specialized longitudinal pipeline to reduce intra-subject variability. Extract baseline volumes for the signature ROI and hippocampal volume.
- Step 2: Cognitive Change Score. Calculate the change in episodic memory score between baseline and follow-up for each subject.
- Step 3: Predictive Modeling. Fit separate regression models with the baseline structural measure (either signature ROI value or hippocampal volume) as the predictor and memory change score as the outcome. Control for relevant covariates like baseline age, sex, and intracranial volume.
- Step 4: Model Comparison. Statistically compare the explanatory power (e.g., via adjusted R² or AIC) of the signature model and the hippocampal volume model.
4. Analysis: A model demonstrating a stronger statistical association with future memory decline is considered more sensitive for prognostic applications. Studies have shown signature models can better explain longitudinal memory change than theory-driven models [2].
Protocol: Hippocampal Subfield Analysis in MCI Subtypes
This protocol provides a more granular, theory-driven approach by focusing on hippocampal subfields, which can serve as a high-performance benchmark for broader signatures [72].
1. Objective: To differentiate hippocampal subfield volumes between amnestic and non-amnestic MCI subtypes and identify associations with memory performance.
2. Materials and Reagents:
- Imaging Data: High-resolution T1-weighted MRI scans (3D T1-weighted sequences are ideal).
- Software: Automated hippocampal subfield segmentation software (e.g., FreeSurfer's hippocampal subfield module).
- Participants: Well-characterized cohorts of aMCI, naMCI, and subjective memory complaint controls [72].
3. Procedure:
- Step 1: Participant Diagnosis. Diagnose participants using stringent criteria, classifying aMCI based on deficits in delayed recall rather than encoding alone [72].
- Step 2: Subfield Segmentation. Process T1-weighted datasets through the hippocampal subfield pipeline in FreeSurfer to obtain volumes for subfields including Subiculum, CA1, CA4, Dentate Gyrus, etc.
- Step 3: Group Comparison. Conduct ANCOVA tests to compare subfield volumes between diagnostic groups (aMCI vs. naMCI vs. control), covarying for age, sex, and total intracranial volume.
- Step 4: Correlation with Memory. Within the aMCI group, perform correlation or regression analyses between significantly different subfield volumes and scores on verbal learning and memory tests (e.g., RAVLT, Logical Memory).
4. Analysis: This protocol validates a theory-based model by establishing a specific neuroanatomical link. For example, it has been shown that CA1 subfield volume specifically predicts concurrent memory performance in aMCI, providing a mechanistic benchmark [72].
Conceptual Workflow for Model Benchmarking
The following diagram illustrates the logical flow and decision points in a comprehensive benchmarking study, from initial model development to final validation and comparison.
Diagram 1: Benchmarking workflow for robust brain signature validation across multiple cohorts.
The Scientist's Toolkit: Research Reagent Solutions
The table below catalogs essential materials, software, and data resources required for executing the protocols outlined in this document.
Table 2: Essential Research Tools for Brain Signature Benchmarking
| Item Name | Type | Function/Application | Example/Reference |
|---|---|---|---|
| Structural T1-weighted MRI Data | Data | Primary imaging data for volumetric analysis and signature derivation. | ADNI, Cam-CAN, Local Cohorts [2] [60] |
| Standardized Cognitive Batteries | Assessment | To obtain reliable and consistent episodic memory scores across cohorts. | ADNI-Mem, SENAS, RAVLT, Logical Memory [2] [72] |
| FreeSurfer Software Suite | Software | Automated cortical reconstruction, hippocampal subfield segmentation, and volumetric analysis. | https://freesurfer.net/ [72] [73] |
| Statistical Parametric Mapping (SPM) | Software | Voxel-wise statistical analysis, image processing, and normalization. | https://www.fil.ion.ucl.ac.uk/spm/ [2] |
| nnU-Net for Hippocampal Segmentation | Software | Deep learning-based pipeline for highly accurate and reliable hippocampal volumetry. | Isensee et al., 2021 [74] |
| R or Python (with neuroimaging libs) | Software | Statistical analysis, model comparison, and data visualization. | R (lme4, nlme), Python (nilearn, scikit-learn) |
| Validated Hippocampal Protocol | Protocol | Reference standard for manual hippocampal delineation on MRI. | EADC-ADNI Harmonized Protocol [73] |
Application Notes
Theoretical Foundations of Predictive Brain Signatures
The development of predictive brain signatures for mild cognitive impairment (MCI) and dementia represents a paradigm shift from traditional localized brain mapping to multivariate predictive models that capture distributed neural patterns across multiple brain systems [75]. These signatures leverage population coding theory, where information is encoded across ensembles of neurons rather than isolated regions, providing superior predictive accuracy for behavioral and cognitive outcomes [75]. This approach has demonstrated particular value in identifying shared neurobiological features between psychiatric and neurodegenerative conditions, revealing that schizophrenia patients exhibit neuroanatomical patterns remarkably similar to behavioral variant frontotemporal dementia (bvFTD) rather than Alzheimer's disease [76].
The validation of these signatures across multiple cohorts requires rigorous methodological standards as outlined in CONSORT 2025 guidelines, which emphasize transparency in trial registration, data sharing, and detailed reporting of analytical methods [77]. These guidelines are essential for establishing the reproducibility of brain signatures across diverse populations and clinical settings. Furthermore, the integration of multimodal data sources including structural MRI, genetic risk scores, and clinical measures has strengthened the predictive validity of these signatures for identifying individuals at highest risk for cognitive decline [76].
Performance Metrics Across Diagnostic Categories
Table 1: Signature Performance in Differentiating Neurodegenerative Conditions
| Diagnostic Category | Signature Type | Classification Accuracy | Key Discriminating Regions | Cohort Validation |
|---|---|---|---|---|
| Behavioral variant FTD | Structural MRI | Balanced Accuracy: 77.6% [76] | Prefrontal, insular, limbic volumes [76] | 1870 participants across 5 groups [76] |
| Alzheimer's Disease | Structural MRI | Balanced Accuracy: 85.1% [76] | Temporolimbic regions [76] | 140 participants (44 AD + 96 MCI/early AD) [76] |
| Schizophrenia with bvFTD pattern | Structural MRI | 41.2% expression rate [76] | Prefrontal-insular-salience system [76] | 157 schizophrenia patients [76] |
| MCI Progression to Dementia | Multimodal ML | Patent-pending system [78] | To be determined | Pre-clinical development [78] |
Prognostic Utility for Cognitive Decline
The translational value of brain signatures extends beyond diagnostic classification to predicting longitudinal cognitive trajectories. Research demonstrates that expression of bvFTD patterns in schizophrenia patients correlates with more severe phenotypic presentations, unfavorable disease course, and elevated polygenic risk scores for both schizophrenia and dementia [76]. Similarly, in clinical high-risk (CHR) states for psychosis, the presence of these neurodegenerative patterns predicts psychosocial disability at 2-year follow-up, highlighting their prognostic value [76].
Critically, the progression of bvFTD/schizophrenia patterns over one year distinguishes patients who do not recover from those who retain recovery potential, establishing these signatures as dynamic biomarkers of disease trajectory [76]. This temporal dimension provides particular utility for clinical trials targeting cognitive decline, where brain signatures can serve as intermediate endpoints to assess therapeutic efficacy.
Experimental Protocols
Multimodal Classification Protocol
This protocol details the methodology for deriving and validating diagnostic brain signatures using structural neuroimaging data, adapted from the machine learning approach described by Koutsouleris et al. (2025) [76].
2.1.1. Participant Selection and Inclusion Criteria
- Recruit five diagnostic groups: bvFTD patients (n = 108), established AD (n = 44), MCI or early AD (n = 96), schizophrenia (n = 157), and major depression (n = 102)
- Include healthy controls (n = 1042) for age-related and cohort-related data calibration
- Ensure all participants provide written informed consent according to Declaration of Helsinki principles
- Obtain approval from local research ethics committees before study initiation
2.1.2. MRI Data Acquisition and Preprocessing
- Acquire T1-weighted structural MRI scans using standardized protocols across sites
- Perform quality control to exclude scans with excessive motion artifacts or technical issues
- Process images using automated pipelines for:
- Spatial normalization to standard stereotactic space (e.g., MNI template)
- Tissue segmentation into gray matter, white matter, and cerebrospinal fluid
- Extraction of gray matter volume maps
- Age standardization and inter-group adjustment of volume maps
2.1.3. Machine Learning Classification
- Utilize machine learning software (e.g., NeuroMiner version 1.05) for pattern analysis
- Train four separate diagnostic classifiers to distinguish healthy controls from:
- bvFTD patients
- Established AD patients
- MCI or early AD patients
- Schizophrenia patients
- Employ support vector machine (SVM) algorithms with repeated nested cross-validation
- Measure model complexity (Cx) through CV1 cross-validation partitions
- Compute performance metrics including sensitivity, specificity, balanced accuracy, and AUC
- Validate statistical significance using 1000 label permutation tests
2.1.4. Pattern Expression Analysis
- Apply trained diagnostic classifiers to all individuals not participating in model generation
- Calculate decision scores representing expression levels of each diagnostic pattern
- Compare pattern expression across diagnostic groups using appropriate statistical tests (McNemar, Quade)
- Correct for multiple comparisons using false discovery rate and Dunn-Šidák methods
Longitudinal Prognostication Protocol
This protocol enables the assessment of brain signature progression over time to predict cognitive decline trajectories.
2.2.1. Baseline and Follow-up Assessment
- Conduct comprehensive clinical and cognitive assessments at baseline
- Acquire structural MRI scans using identical acquisition parameters at baseline and follow-up (e.g., 1-year interval)
- Include measures of psychosocial functioning, symptom severity, and cognitive performance
- For clinical high-risk populations, track conversion to full-threshold disorders
2.2.2. Pattern Progression Quantification
- Calculate baseline expression of relevant brain signatures (e.g., bvFTD pattern) using trained classifiers
- Compute change in pattern expression between baseline and follow-up
- Establish threshold for significant pattern progression based on healthy control stability data
- Correlate pattern progression with clinical and cognitive decline measures
2.2.3. Polygenic Risk Integration
- Obtain genetic data from participants where available
- Calculate polygenic risk scores for FTD, AD, and schizophrenia using established methods
- Examine relationships between polygenic risk, baseline pattern expression, and pattern progression
Visualizing Analytical Workflows
Multimodal Classification Workflow
Signature Validation Framework
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Resources for Brain Signature Research
| Resource Category | Specific Solution | Function/Purpose | Implementation Example |
|---|---|---|---|
| Machine Learning Platform | NeuroMiner (v1.05) [76] | Diagnostic classifier generation with cross-validation | Derivation of bvFTD, AD, and schizophrenia patterns [76] |
| Neuroimaging Analysis | Support Vector Machines (SVM) [76] | Multivariate pattern classification | Optimal separation hyperplane definition for patient/control discrimination [76] |
| Genetic Analysis Tools | Polygenic Risk Scoring [76] | Quantification of inherited risk burden | Prediction of bvFTD pattern expression via FTD, AD, and schizophrenia polygenic scores [76] |
| Statistical Validation | Repeated Nested Cross-Validation [76] | Robust performance estimation | Model generalization assessment across multiple data partitions [76] |
| Data Standardization | Age-Standardized Gray Matter Volumes [76] | Inter-group comparison normalization | Calibration of structural MRI data across diverse cohorts [76] |
| Performance Metrics | Balanced Accuracy, AUC, Sensitivity/Specificity [76] | Comprehensive classifier evaluation | Reporting of diagnostic pattern performance characteristics [76] |
| Prognostic Assessment | Longitudinal Pattern Progression [76] | Tracking of signature changes over time | Differentiation of recovered vs. non-recovered patients [76] |
| Reporting Standards | CONSORT 2025 Guidelines [77] | Transparent research reporting | Adherence to updated clinical trial reporting standards [77] |
Performance Benchmarking and Clinical Utility
Table 3: Prognostic Performance for Cognitive Decline
| Predictor Variable | Outcome Measure | Effect Size / Predictive Value | Population | Timeframe |
|---|---|---|---|---|
| bvFTD Pattern Expression | 2-year psychosocial disability | Predictive of social/occupational impairment [76] | Clinical High-Risk (CHR) | 2 years |
| Schizophrenia Pattern Expression | 2-year psychosocial disability | Predictive of functional outcomes [76] | Recent Onset Depression | 2 years |
| bvFTD/Schizophrenia Pattern Progression | Clinical recovery status | Differentiates non-recovered patients [76] | Mixed patient cohort | 1 year |
| Polygenic Risk Scores (FTD+SCZ) | Pattern expression | Associated with higher signature expression [76] | Cross-diagnostic | Baseline |
| Body Mass Index | bvFTD pattern expression | Predictive of neurodegenerative pattern (R² = 0.11) [76] | Mixed patient cohort | Baseline |
The clinical translation of brain signatures for classifying MCI, dementia, and predicting cognitive decline requires rigorous multi-cohort validation and standardization of analytical protocols. The evidence indicates that multivariate neuroanatomical patterns show significant promise for both diagnostic classification and prognostic prediction, particularly when integrating multimodal data sources. Adherence to methodological standards such as those outlined in CONSORT 2025 and implementation of reproducible machine learning workflows will be essential for advancing these signatures toward clinical application. Future directions should focus on refining predictive accuracy across diverse populations and establishing clear thresholds for clinical implementation in both diagnostic and therapeutic contexts.
Application Note: Multimodal Biomarkers for CNS Disorders
The development of valid biomarkers for central nervous system (CNS) disorders represents one of the most significant challenges in modern neuroscience and drug development. The complexity of brain disorders, heterogeneous patient responses to therapeutics, and recent failures in novel chemical therapeutics in psychiatric clinical trials have highlighted the pressing need for validated, fit-for-purpose biomarkers [79]. These biomarkers are essential as quantitative indicators of disease risk, diagnosis, prognosis, patient stratification, and treatment response monitoring [79]. The declining investment in neuroscience research and development by the pharmaceutical industry further underscores the urgent need to change the paradigm for CNS biomarker development and application [79].
This application note outlines contemporary approaches for developing and validating multimodal biomarker signatures that can track disease progression across multiple domains in CNS clinical trials. We focus specifically on the framework of validating these signatures across multiple cohorts to ensure robustness and generalizability, addressing a critical gap in current neurological and psychiatric drug development pipelines.
Current Biomarker Landscape in CNS Disorders
The field of CNS biomarkers has evolved substantially from single-modal approaches to integrated, multimodal frameworks. Current biomarker approaches can be categorized into several domains:
Fluid-Based Biomarkers: Cerebrospinal fluid (CSF) and plasma biomarkers have shown promise for several CNS conditions. For Alzheimer's disease, a multiplexed panel of three markers—amyloid-β1-42 (Aβ1-42), total tau, and phosphorylated tau assays—has demonstrated reliability in diagnosing AD with dementia and identifying prodromal AD in mild cognitive impairment cases [79]. Similarly, markers of neuronal loss (TDP-43, phosphorylated neurofilament heavy subunit) and glial activity (complement C3) in CSF samples show potential for inclusion in diagnostic and prognostic biomarker panels for amyotrophic lateral sclerosis (ALS) [79].
Imaging Biomarkers: Structural and functional neuroimaging techniques provide sensitive indices for early detection of abnormal circuit function. Pharmacological MRI serves as a translational measure of a drug's pharmacodynamic action in the brain, guiding dose selection in drug development [79]. Positron emission tomography (PET) imaging of glucose utilization and amyloid burden can monitor disease progression in Alzheimer's disease, while structural MRI and diffusion tensor imaging (DTI) reliably grade the extent of white and gray matter damage in multiple sclerosis and ALS [79].
Digital Biomarkers: Eye movements have emerged as particularly promising objective biomarkers, now trackable with just a laptop and webcam [80]. disruptions in saccadic latency, gain, velocity, fixation stability, and intrusion frequency occur across conditions including ALS, Parkinson's disease, and multiple sclerosis, providing sensitive reflections of brain dysfunction [80].
Exosome-Based Biomarkers: CNS cell-derived exosomes cross the blood-brain barrier and enter peripheral circulation, carrying molecular cargo that reflects the functional state of their cells of origin [81]. These vesicles provide an accessible window into cellular processes of the brain and spinal cord, with potential applications in Alzheimer's disease, Parkinson's disease, ALS, frontotemporal dementia, and other neurodegenerative conditions [81].
Table 1: Biomarker Modalities for CNS Disorders
| Modality | Examples | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| Fluid-Based | CSF Aβ1-42, tau, plasma TDP-43 | Diagnosis, prognosis, treatment monitoring | Molecular specificity | Invasive procedures, variable plasma results |
| Imaging | fMRI, PET, DTI, structural MRI | Disease staging, treatment response, dose selection | Whole-brain coverage, non-invasive | High cost, technical variability |
| Digital | Eye movement metrics, computer cognitive batteries | Early detection, progression monitoring, trial endpoints | Scalable, objective, low cost | Emerging validation frameworks |
| Exosome-Based | CNS-derived exosome proteins/RNA | Early diagnosis, pathological monitoring | Blood-based, cell-type specific | Isolation methodology challenges |
Protocol 1: Validation of Brain Signatures Across Multiple Cohorts
Experimental Principle and Scope
This protocol outlines a rigorous statistical framework for validating brain signatures as robust phenotypes across multiple independent cohorts. The method addresses the critical need for reproducible brain-behavior associations that generalize beyond single discovery datasets, which is essential for their application in clinical trials and biomarker development [1]. The approach employs data-driven signature derivation with extensive validation to ensure reliability and utility for modeling substrates of behavioral domains.
Materials and Equipment
Research Reagent Solutions
Table 2: Essential Research Reagents and Materials
| Item | Specification | Function/Application |
|---|---|---|
| MRI Scanner | 3T minimum field strength | Structural and functional brain imaging |
| T1-weighted Sequence | MPRAGE or equivalent | Gray matter thickness and volume analysis |
| Image Processing Pipeline | Custom or standardized (e.g., FSL, FreeSurfer) | Brain extraction, tissue segmentation, registration |
| Cognitive Assessment Tools | SENAS, ADNI-Mem, ECog | Episodic memory and everyday function measurement |
| Quality Control Tools | Automated and manual QC protocols | Data quality assurance and standardization |
| Statistical Software | R, Python with appropriate libraries | Signature computation and validation analyses |
Procedure
Cohort Selection and Preparation
Select Discovery Cohorts: Identify multiple independent cohorts with relevant neuroimaging and behavioral data. Example cohorts include:
- UC Davis Alzheimer's Disease Research Center Longitudinal Diversity Cohort (N=578)
- Alzheimer's Disease Neuroimaging Initiative Phase 3 (ADNI 3) cohort (N=831) [1]
Define Validation Cohorts: Secure completely separate validation cohorts not used in discovery:
- Additional participants from original cohorts (N=348 from UCD)
- Independent cohort (ADNI Phase 1, N=435) [1]
Standardize Image Acquisition: Implement harmonized MRI acquisition protocols across sites, including:
- Whole-head structural T1 MRI sequences
- Standardized positioning and parameters
Process Imaging Data:
- Perform brain extraction using convolutional neural net recognition of intracranial cavity
- Conduct human quality control on extractions
- Implement affine and B-spline registration to structural template
- Perform native-space tissue segmentation into gray matter, white matter, and CSF [1]
Signature Derivation
Random Subset Selection: In each discovery cohort, randomly select 40 subsets of size 400 participants [1].
Voxel-Based Analysis: Compute voxel-based regressions between gray matter thickness and behavioral outcomes of interest across all subsets.
Consensus Mask Generation:
- Generate spatial overlap frequency maps from the multiple discovery subsets
- Define high-frequency regions as "consensus" signature masks [1]
Model Fitting: Evaluate replicability of cohort-based consensus model fits and explanatory power in validation datasets.
Validation and Replication Assessment
Spatial Replication: Assess convergent consensus signature regions across independent cohorts.
Model Fit Correlation: Compute correlation of consensus signature model fits in 50 random subsets of each validation cohort.
Comparative Performance: Compare signature models against theory-based models in full cohort analyses [1].
Computational Visualization
Diagram 1: Signature Validation Workflow
Protocol 2: Multimodal Progression Biomarkers for CNS Clinical Trials
Experimental Principle and Scope
This protocol describes the integration of multiple biomarker modalities to track disease progression in CNS clinical trials, with emphasis on practical implementation, standardization, and validation across sites. The approach addresses the limitations of single biomarkers through multimodal integration, leveraging the complementary strengths of different biomarker types to provide a more comprehensive assessment of disease progression and treatment response [79].
Materials and Equipment
Multimodal Biomarker Equipment
Table 3: Equipment for Multimodal Biomarker Assessment
| Equipment Type | Specifications | Biomarker Applications |
|---|---|---|
| MRI Scanner | 3T with standardized sequences | Structural, functional, and connectivity measures |
| Eye Tracking System | Webcam-based with AI algorithms | Saccadic metrics, fixation stability, intrusions |
| Cognitive Assessment | Computerized batteries (e.g., Bracket) | Early detection of cognitive impairment |
| Biospecimen Collection | Standardized CSF and plasma kits | Fluid biomarker analysis |
| Data Harmonization | Centralized processing pipelines | Cross-site data standardization |
Procedure
Multimodal Data Acquisition
Imaging Biomarkers:
- Acquire structural MRI (T1-weighted) for volumetric analysis
- Implement resting-state fMRI for functional connectivity assessment
- Utilize diffusion tensor imaging for white matter integrity
- Standardize acquisition parameters across all trial sites [79]
Oculometric Biomarkers:
- Set up eye-tracking using standard laptop and webcam
- Implement 10-minute assessment protocol including:
- Saccadic tasks (latency, velocity, accuracy)
- Fixation stability measurements
- Smooth pursuit tasks
- Assessment of saccadic intrusions [80]
- Ensure consistent lighting and positioning across sites
Cognitive and Functional Biomarkers:
- Administer computerized cognitive test batteries
- Collect informant-based everyday function ratings (e.g., ECog)
- Implement standardized neuropsychological assessments [1]
Fluid Biomarkers:
- Collect CSF according to standardized protocols (if applicable)
- Draw plasma samples using standardized collection tubes
- Process and bank samples according to consensus guidelines [79]
Data Processing and Harmonization
Centralized Quality Control:
- Implement rigorous quality assurance for all data modalities
- Apply standardized preprocessing pipelines
- Conduct manual checking of automated quality metrics
Data Harmonization:
- Utilize ComBat or similar methods for cross-site harmonization
- Apply standardized normalization procedures
- Implement batch effect correction
Multimodal Integration:
- Extract features from each modality
- Normalize features across platforms
- Apply machine learning algorithms for integrated signature development
Computational Visualization
Diagram 2: Multimodal Integration Pathway
Data Analysis and Interpretation
Statistical Validation Framework
Robust validation of biomarker signatures requires multiple complementary approaches:
Spatial Replicability: Assess consistency of signature regions across independent cohorts through spatial overlap frequency maps [1].
Model Fit Stability: Evaluate correlation of signature model fits across multiple random subsets of validation cohorts.
Performance Comparison: Compare signature models against established theory-based models using appropriate metrics (e.g., R², AUC).
Longitudinal Sensitivity: Assess sensitivity to disease progression through association with clinical progression and cognitive decline.
Quantitative Performance Metrics
Table 4: Performance Metrics for Biomarker Validation
| Metric Category | Specific Metrics | Target Threshold | Interpretation |
|---|---|---|---|
| Discriminative Power | AUC, Sensitivity, Specificity | AUC > 0.70 | Ability to distinguish disease states |
| Associative Strength | R², Effect Size | R² > 0.10, Effect Size > 0.5 | Association with clinical outcomes |
| Reliability | ICC, Cohen's Kappa | ICC > 0.70 | Test-retest and inter-rater reliability |
| Progressive Sensitivity | Slope estimates, Hazard ratios | p < 0.05 | Ability to track change over time |
| Practical Utility | NNT, Sample size estimates | >30% reduction in sample size | Impact on clinical trial design |
Cross-Cohort Harmonization Methods
Implement advanced statistical methods for cross-cohort harmonization:
ComBat Harmonization: Remove batch effects while preserving biological signals.
Linear Mixed Effects Models: Account for site-specific variability.
Reference-Based Alignment: Align distributions to a common reference standard.
Application in Clinical Trial Design
Biomarker-Driven Endpoints
The integration of validated multimodal biomarkers transforms clinical trial design through:
Endpoint Development: Progression biomarkers serve as sensitive endpoints that can detect treatment effects earlier than clinical measures.
Patient Stratification: Biomarker signatures identify homogeneous patient subgroups for enrichment strategies.
Target Engagement: Biomarkers provide evidence of biological activity at the intended molecular target.
Go/No-Go Decisions: Objective progression biomarkers inform early portfolio decisions.
Practical Implementation Considerations
Successful implementation requires attention to practical considerations:
Feasibility: Balance comprehensiveness with practical constraints of multicenter trials.
Standardization: Implement standardized operating procedures across all sites.
Training: Ensure consistent administration and interpretation across raters and sites.
Regulatory Alignment: Engage early with regulatory agencies on biomarker qualification.
The development and validation of union signatures for multiple domains and progression biomarkers represents a paradigm shift in CNS drug development. Through rigorous multi-cohort validation frameworks and multimodal integration, these biomarkers offer the potential to de-risk clinical development, accelerate therapeutic discovery, and ultimately deliver effective treatments to patients suffering from devastating neurological and psychiatric disorders. The protocols outlined herein provide a roadmap for researchers to develop, validate, and implement these crucial tools in CNS clinical trials.
Conclusion
The rigorous validation of brain signatures across multiple, independent cohorts is paramount for establishing them as reliable biomarkers in neuroscience research and drug development. This synthesis demonstrates that robust methodological frameworks—incorporating multi-cohort discovery, machine learning, and stringent validation protocols—can produce signatures that outperform traditional brain measures in explaining behavioral variance and classifying clinical syndromes. Key takeaways include the necessity of large, diverse cohorts to ensure generalizability, the power of consensus approaches to enhance reproducibility, and the emerging potential of multimodal data integration. Future directions should focus on standardizing validation practices across studies, further developing interpretable AI models, and translating these validated signatures into sensitive endpoints for clinical trials. Ultimately, these advances will accelerate the development of personalized interventions and provide more precise tools for early detection and monitoring of neurodegenerative diseases.
References
- 1. Toward a statistical validation of brain signatures as robust ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10171525/]
- 2. A robust brain signature region approach for episodic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8105039/]
- 3. Machine learning reveals distinct neuroanatomical ... [https://www.nature.com/articles/s41467-025-57867-7]
- 4. Representation, Pattern Information, and Brain Signatures [https://www.sciencedirect.com/science/article/pii/S089662731830477X]
- 5. Statistical Approaches to Identify Pairwise and High-Order ... [https://www.mdpi.com/2075-1729/13/10/2075]
- 6. Population heterogeneity in clinical cohorts affects the ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3001627]
- 7. Neural signatures of social inferences predict the number ... [https://www.nature.com/articles/s41467-023-40078-3]
- 8. A cross-validation study with Chinese and ADNI cohorts [https://www.sciencedirect.com/science/article/pii/S2213158221003442]
- 9. Representation, Pattern Information, and Brain Signatures [https://pmc.ncbi.nlm.nih.gov/articles/PMC6296466/]
- 10. Toward a statistical validation of brain signatures as robust ... [https://pubmed.ncbi.nlm.nih.gov/36939069/]
- 11. Brain signatures indexing variation in internal processing ... [https://www.sciencedirect.com/science/article/pii/S2589004223018278]
- 12. A prospective protocol for remotely investigating brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542568/]
- 13. Topological signatures of brain dynamics: persistent ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1607941/full]
- 14. Overview of Challenges in Brain-based Predictive Modeling [https://www.sciencedirect.com/science/article/pii/S000632232501460X]
- 15. Task and resting state fMRI modelling of brain-behavior ... [https://www.sciencedirect.com/science/article/pii/S0006322325014878]
- 16. The Global Neurodegeneration Proteomics Consortium [https://www.nature.com/articles/s41591-025-03834-0]
- 17. Multi-cohort machine learning identifies predictors of ... [https://www.nature.com/articles/s41746-025-01862-1]
- 18. Multi-cohort cerebrospinal fluid proteomics identifies robust ... [https://www.sciencedirect.com/science/article/pii/S0896627325001321]
- 19. Integrated multi-cohort transcriptional meta-analysis of ... [https://actaneurocomms.biomedcentral.com/articles/10.1186/s40478-014-0093-y]
- 20. Multi-cohort cerebrospinal fluid proteomics identifies robust ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10896368/]
- 21. Characteristics of cohort data management systems (CDMS) [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619332/]
- 22. A data‐driven, multi‐domain brain gray matter signature as a powerful... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11584916/]
- 23. Comparison and aggregation of event sequences across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9020023/]
- 24. Alzheimer's Disease Neuroimaging Initiative (ADNI) [https://pmc.ncbi.nlm.nih.gov/articles/PMC2809036/]
- 25. Discovering subtypes with imaging signatures in the Motoric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505024/]
- 26. ADNI | Alzheimer's Disease Neuroimaging Initiative [https://adni.loni.usc.edu/]
- 27. ADNI Data [https://adni.loni.usc.edu/data-samples/adni-data/]
- 28. Explainable Machine Learning Models for Brain Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC11587041/]
- 29. Explainable machine learning for early detection of ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1672971/full]
- 30. Evidence‐based standardized sample handling protocol ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12481164/]
- 31. Multidimensional Visualization and AI-Driven Prediction Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561245/]
- 32. implications for microglia activation and sex differences - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12267417/]
- 33. Common genetic variation influencing human white matter ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8370718/]
- 34. Reliable Multimodal Brain Signatures Predict Mental ... [https://www.sciencedirect.com/science/article/pii/S2451902225000928]
- 35. Multimodal Integration of Plasma Biomarkers, MRI, and ... [https://www.sciencedirect.com/science/article/pii/S1053811925005531]
- 36. WAND: A multi-modal dataset integrating advanced MRI ... [https://www.nature.com/articles/s41597-024-04154-7]
- 37. Reproducible brain-wide association studies require ... [https://www.nature.com/articles/s41586-022-04492-9]
- 38. What You Get with Specific Sample Sizes in UX Problem ... [https://measuringu.com/specific-sample-sizes-in-problem-discovery-studies/]
- 39. The Extent and Consequences of P-Hacking in Science [https://pmc.ncbi.nlm.nih.gov/articles/PMC4359000/]
- 40. Controlling bias and inflation in epigenome ... - Genome Biology [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-016-1131-9]
- 41. Embracing cohort heterogeneity in clinical machine ... [https://www.nature.com/articles/s41598-023-35557-y]
- 42. Quantitative assessment of impact of technical and ... [https://www.sciencedirect.com/science/article/pii/S0010482525015008]
- 43. 14 Comparing quantitative data between individuals [https://bookdown.org/pkaldunn/SRM-Textbook/BetweenQuantData.html]
- 44. An integrated workflow to assess technical and biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5296239/]
- 45. Gene transcription, neurotransmitter, and neurocognition ... [https://www.nature.com/articles/s41467-025-63000-5]
- 46. Multi-Omics: Challenges and Solutions [https://bigomics.ch/blog/key-challenges-in-multi-omics-data-integration/]
- 47. Integrating Multi-Omics for Precision Medicine: 2025 Guide [https://lifebit.ai/blog/integrating-multi-modal-genomic-and-multi-omics-data-for-precision-medicine/]
- 48. Designing and interpreting 'multi-omic' experiments that may ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7477987/]
- 49. A multi-cohort validated OXPHOS signature predicts ... [https://pubmed.ncbi.nlm.nih.gov/40821817/]
- 50. A multi-cohort validated OXPHOS signature predicts ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1638824/full]
- 51. External validation of prognostic models: what, why, how, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7857818/]
- 52. Predictive overfitting immunological applications: Pitfalls and... in [https://pmc.ncbi.nlm.nih.gov/articles/PMC10498807/]
- 53. Understanding Overfitting: Strategies and Solutions [https://www.lyzr.ai/glossaries/overfitting/]
- 54. Decision Trees, Random Forests, and Overfitting – Machine ... [https://carpentries-incubator.github.io/ml4bio-workshop/04-trees-overfitting/index.html]
- 55. in Machine : key algorithms, applications... learning biological research [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-025-02424-3]
- 56. Multi-modal neuroimaging signatures predict cognitive ... [https://www.sciencedirect.com/science/article/abs/pii/S2211034823008799]
- 57. Bioinformatics Overfitting In [https://www.meegle.com/en_us/topics/overfitting/overfitting-in-bioinformatics]
- 58. Cross-Validation, Overfitting, and Validity [https://my-hdr-blogs.shaveensingh.com/article/cross-validation-and-overfitting/]
- 59. Characterizing changes to individual-specific brain ... [https://pubmed.ncbi.nlm.nih.gov/40671788/]
- 60. Characterizing changes to individual-specific brain ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1493855/full]
- 61. Frontiers | Interpretable machine learning for predicting early neurological deterioration in symptomatic intracranial atherosclerotic stenosis [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1667119/full]
- 62. Methods for Stratification and Validation Cohorts [https://pmc.ncbi.nlm.nih.gov/articles/PMC9144352/]
- 63. Robust and consistent biomarker candidates identification by ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-024-02578-0]
- 64. Verification, analytical validation, and clinical validation (V3) [https://www.nature.com/articles/s41746-020-0260-4]
- 65. Brain maps of general cognitive functioning [https://www.nature.com/articles/s41398-025-03617-8]
- 66. Heterogeneous, temporally consistent, and plastic brain ... [https://www.nature.com/articles/s41467-025-63967-1]
- 67. Multi-Cohort Federated Learning Shows Synergy in ... [https://link.springer.com/article/10.1007/s41666-025-00208-6]
- 68. AI improves consistency in regional brain volumes ... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2025.1588487/full]
- 69. Biological brain age prediction using machine learning on ... [https://elifesciences.org/articles/81067]
- 70. Recent advances in neuroimaging of Alzheimer's disease and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417339/]
- 71. Correlation between hippocampal volumes and medial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5341264/]
- 72. Memory Performance Correlates of Hippocampal Subfield ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2019.00259/full]
- 73. Steps to standardization and validation of hippocampal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3396131/]
- 74. Toward hippocampal volume measures on ultra-high field ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1238646/full]
- 75. Neuron脑影像机器学习: 表征、模式信息与大脑特征 [http://www.syfmri.com/ShowNews.asp?id=630]
- 76. 使用多模态机器学习方法探索精神疾病和额颞叶痴呆之间的 ... [https://blog.csdn.net/cc1609130201/article/details/129066670]
- 77. Key Updates in CONSORT 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439630/]
- 78. WO2023216293A1 - 预测痴呆症或轻度认知障碍的系统和方法 [https://patents.google.com/patent/WO2023216293A1/zh]
- 79. Assessing biomarkers for brain diseases: progress and gaps [https://pmc.ncbi.nlm.nih.gov/articles/PMC3706976/]
- 80. Eye movements as objective biomarkers: accelerating CNS ... [https://www.drugtargetreview.com/article/188266/eye-movements-as-objective-biomarkers-accelerating-cns-drug-development/]
- 81. CNS cell-derived exosome signatures as blood-based ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1426700/full]