Validating Virtual Reality Biomarkers for Mental Disorders: A New Frontier in Objective Diagnosis and Drug Development
This article explores the transformative potential of virtual reality (VR)-derived biomarkers in creating objective, biologically-grounded diagnostic tools for mental disorders.
Validating Virtual Reality Biomarkers for Mental Disorders: A New Frontier in Objective Diagnosis and Drug Development
Abstract
This article explores the transformative potential of virtual reality (VR)-derived biomarkers in creating objective, biologically-grounded diagnostic tools for mental disorders. Aimed at researchers, scientists, and drug development professionals, it synthesizes current evidence on the development, application, and validation of these digital biomarkers. The scope spans from foundational principles and methodological frameworks for data capture to the troubleshooting of implementation barriers and the critical validation of VR biomarkers against established standards like neuroimaging and clinical outcomes. By examining multimodal integration, AI-powered analytics, and the pathway to clinical adoption, this resource provides a comprehensive roadmap for leveraging VR to enhance precision in mental health diagnostics and therapeutic development.
The New Science of VR Biomarkers: Defining Digital Phenotypes for Mental Health
Virtual reality (VR) biomarkers are emerging as a transformative tool in mental health research and drug development, offering objective, quantifiable measures that overcome the limitations of traditional subjective assessments. By capturing rich behavioral, physiological, and neurophysiological data within standardized, immersive environments, VR biomarkers provide unprecedented insights into cognitive and emotional processes. This guide compares the performance of various VR biomarker paradigms against traditional methods, detailing experimental protocols, key findings, and essential research tools. The integration of VR with multimodal sensing and machine learning is establishing a new standard for validating digital biomarkers in mental disorders research, enabling more precise and translative outcomes for clinical trials and therapeutic development.
The Case for Objectivity: VR Biomarkers vs. Traditional Checklists
Traditional diagnostic approaches for mental disorders, such as symptom checklists and clinical interviews, are limited by their reliance on self-report, susceptibility to memory bias, and inherent subjectivity [1] [2]. These methods are unable to capture the fine-grained, real-time behavioral and physiological correlates of mental states. In contrast, VR biomarkers provide a novel pathway to objective assessment by creating controlled, ecologically valid environments where researchers can continuously and unobtrusively measure a user's responses.
Key Performance Advantages of VR Biomarkers:
- Objectivity & Quantification: VR biomarkers translate subjective experiences into quantifiable data points, such as hand movement speed, scanpath length, and physiological arousal, reducing reliance on introspection and clinician interpretation [3].
- Ecological Validity: VR environments can simulate complex, real-world scenarios (e.g., a food-ordering kiosk, a social interaction) that are more reflective of daily challenges than a questionnaire, thereby capturing more authentic behavioral signatures [1] [3].
- High-Density Data Capture: VR platforms enable the synchronous collection of multimodal data streams, including performance metrics, eye-tracking, electroencephalography (EEG), and heart rate variability (HRV), providing a holistic view of a participant's state [1].
- Enhanced Sensitivity for Early Detection: Studies have demonstrated that VR-derived biomarkers can detect subtle deficits associated with conditions like Mild Cognitive Impairment (MCI) with high specificity, often before they are apparent on traditional tests [3].
Comparative Performance Data: VR Biomarkers in Action
The following tables summarize quantitative data from key studies, comparing the performance of VR-based assessments against traditional methods and highlighting the diagnostic accuracy achieved through multimodal integration.
Table 1: Comparative Diagnostic Accuracy of VR vs. Traditional Biomarkers
| Condition Assessed | VR Biomarkers & Method | Traditional Method | Key Performance Metrics | Reference |
|---|---|---|---|---|
| Mild Cognitive Impairment (MCI) | Virtual kiosk test (hand movement, eye movement, errors, time) | Neuropsychological Tests (SNSB-C) & MRI | VR Only: 87.5% Sensitivity, 90% SpecificityMRI Only: 90.9% Sensitivity, 71.4% SpecificityVR + MRI (Multimodal): 94.4% Accuracy, 100% Sensitivity, 90.9% Specificity | [3] [4] |
| Adolescent Major Depressive Disorder (MDD) | VR emotional task with EEG, Eye-Tracking, & HRV | Clinical Diagnosis (DSM-5) & Self-Report Scales | SVM Model Classification: 81.7% Accuracy, 0.921 AUCKey Biomarkers: EEG theta/beta ratio, saccade count, fixation duration, HRV LF/HF ratio | [1] |
| Immersion & Task Difficulty | EEG during VR jigsaw puzzles (idle, easy, hard) | Post-Session Self-Report Questionnaires | Machine Learning Classification: 86-97% Accuracy for differentiating states (e.g., easy vs. hard) | [5] |
Table 2: Core Digital Phenotyping Features for Mental Health Monitoring [2]
| Device Category | Core Features (High Coverage & Importance) | Promising Additional Features |
|---|---|---|
| Actiwatch | Accelerometer, General Activity | Sleep (underused but important) |
| Smart Bands | Heart Rate, Steps, Sleep, Phone Usage | GPS, Electrodermal Activity (EDA), Skin Temperature |
| Smartwatches | Sleep, Heart Rate | Steps, Accelerometer (widely used but less decisive) |
Experimental Protocols for Key VR Biomarker Paradigms
VR Kiosk Test for Mild Cognitive Impairment (MCI)
This protocol is designed to detect subtle deficits in instrumental activities of daily living (IADLs), which are early indicators of MCI [3].
Objective: To classify participants as healthy controls or having MCI based on behavioral biomarkers collected during a simulated daily task. Participants: The study typically involves older adults (e.g., 54 participants, with 22 healthy controls and 32 with MCI), diagnosed according to a gold-standard neuropsychological test battery [3]. VR Apparatus: A head-mounted display (HMD) running a custom virtual environment that simulates a food-ordering kiosk. Procedure:
- The participant is immersed in the VR environment and given the task of ordering a specific food item using the virtual kiosk interface.
- The system automatically and continuously records four primary VR-derived biomarkers:
- Hand Movement Speed: Velocity and fluency of hand controllers while navigating the interface.
- Scanpath Length: Total distance of eye-gaze movement during task completion.
- Time to Completion: Total time taken to successfully complete the order.
- Number of Errors: Instances of incorrect selections or task deviations. Data Analysis: The collected biomarkers are used to train a machine learning model, such as a Support Vector Machine (SVM), to classify participants. Performance is validated against the clinical diagnosis [3].
Multimodal Framework for Adolescent Depression
This protocol uses a VR-based emotional task to elicit physiological responses indicative of Major Depressive Disorder (MDD) in adolescents [1].
Objective: To differentiate adolescents with MDD from healthy controls using synchronized EEG, eye-tracking, and HRV data. Participants: Case-control study involving adolescents (e.g., 51 with first-episode MDD and 64 healthy controls) [1]. Apparatus:
- VR Environment: A 10-minute immersive scenario, such as a "magical forest," featuring an interactive AI agent that conducts a structured dialogue about personal worries and hopes.
- Sensors: BIOPAC MP160 system or equivalent for EEG and ECG (for HRV), and a portable telemetric ophthalmoscope for eye-tracking. Data is synchronized using a platform like LabStreamingLayer (LSL) [1]. Procedure:
- Participants engage in the 10-minute VR emotional task, interacting with the AI agent.
- The following data are collected simultaneously in real-time:
- EEG: Spectral power in different frequency bands (e.g., theta, beta).
- Eye-Tracking: Saccade count, fixation duration, and pupillary response.
- HRV: Derived from ECG, specifically the Low Frequency/High Frequency (LF/HF) ratio. Data Analysis: Statistical analyses (e.g., ANCOVA) identify significant group differences in physiological metrics. A machine learning model (e.g., SVM) is then trained on these features to classify MDD status [1].
EEG Biomarkers of Immersion and Task Difficulty
This protocol investigates the use of EEG to objectively measure cognitive immersion and engagement in VR, moving beyond subjective questionnaires [5].
Objective: To classify a user's state (idle, easy task, hard task) in VR based on EEG signals. Participants: Typically, healthy adults (e.g., 14 participants) without neurological conditions [5]. VR Task: Participants complete a VR jigsaw puzzle with varying levels of difficulty, often manipulated by the number of puzzle pieces. EEG Recording: EEG data is continuously recorded from multiple channels (e.g., 3 or 9 central channels) while participants are in a baseline state (idle) and during the easy and hard puzzle conditions. Data Analysis & Machine Learning:
- Feature Extraction: Temporal, frequency-domain (power in delta, theta, alpha, beta bands), and non-linear features are extracted from the EEG signals.
- Model Training & Validation: Multiple machine learning algorithms (e.g., Stochastic Gradient Descent - SGD, Support Vector Classifier - SVC, Random Forest - RF) are trained and validated to classify the EEG data according to the three states.
- The high classification accuracy (86-97%) demonstrates the potential of EEG features as robust biomarkers for immersion level [5].
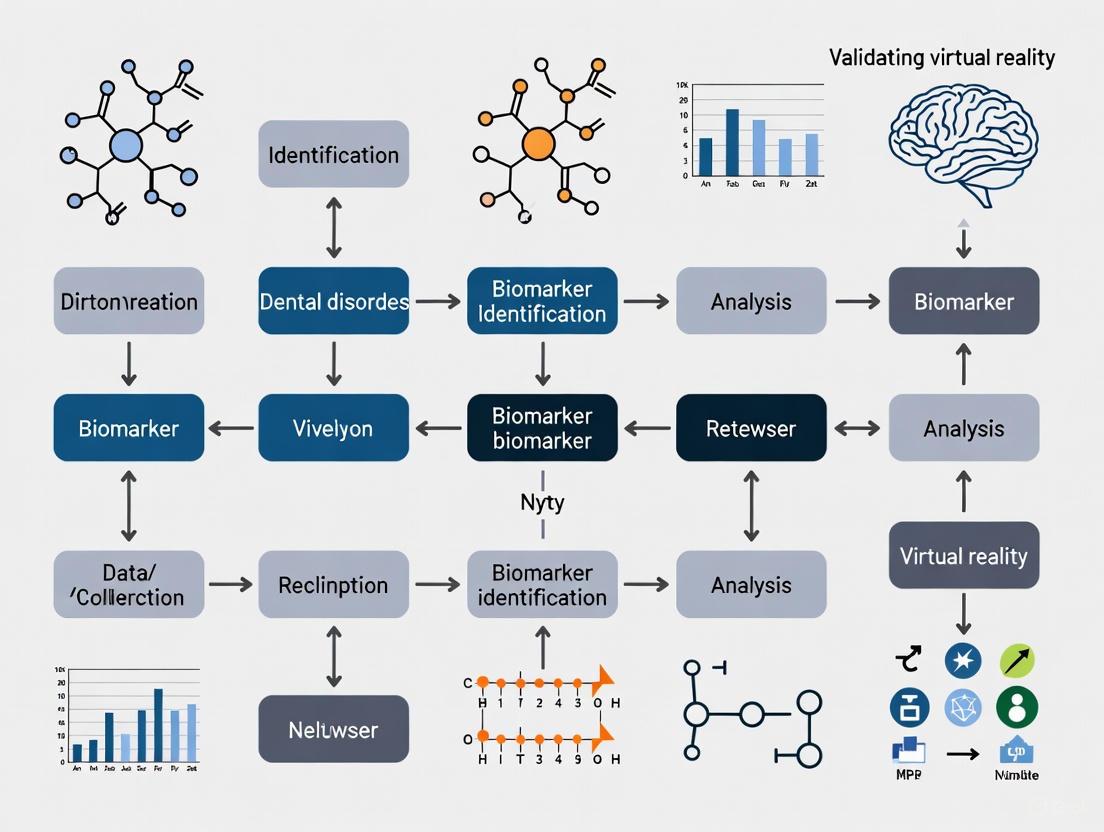
Visualizing the Workflow: From Data Collection to Biomarker Validation
The following diagram illustrates the standard experimental and analytical pipeline for developing and validating VR biomarkers.
Diagram Title: VR Biomarker Development Pipeline
The Scientist's Toolkit: Essential Research Reagents & Materials
Building a rigorous VR biomarker research program requires a suite of specialized hardware and software solutions. The following table details key components and their functions in typical experimental setups.
Table 3: Essential Research Toolkit for VR Biomarker Studies
| Tool Category | Specific Examples | Research Function & Application |
|---|---|---|
| VR Hardware | Head-Mounted Displays (HMDs) with integrated eye-tracking | Presents immersive environments; tracks gaze, pupillometry, and blink data for assessing attention and cognitive load [1]. |
| Physiological Data Acquisition Systems | BIOPAC MP160 system, portable EEG systems, See A8 ophthalmoscope | Records high-fidelity, synchronized physiological data (EEG, ECG, EDA) and eye movements as objective correlates of mental state [1]. |
| Data Synchronization Software | LabStreamingLayer (LSL) | Precisely time-aligns data streams from different sensors (EEG, ET, HRV) with events in the VR environment, which is critical for multimodal analysis [1]. |
| VR Development Platforms | Unity, Unreal Engine, A-Frame framework | Enables the creation of custom, ecologically valid virtual scenarios and tasks tailored to specific research questions (e.g., virtual kiosk, forest environment) [1] [3]. |
| Machine Learning Libraries | Scikit-learn (for SVM, Random Forest), TensorFlow, PyTorch | Used for feature selection, model training, and classification to identify biomarker patterns and build diagnostic or predictive models [5] [1] [3]. |
| Clinical Assessment Tools | Seoul Neuropsychological Screening Battery (SNSB), CES-D | Provides gold-standard clinical phenotyping for participant grouping and validation of VR biomarker findings against established metrics [1] [3]. |
The evidence demonstrates that VR biomarkers represent a significant advancement over subjective symptom checklists, providing the objectivity, ecological validity, and multivariate data required for modern mental health research and drug development. The integration of VR with multimodal sensing and machine learning creates a powerful platform for identifying robust digital signatures of disorders like MCI and depression with high accuracy. As the field matures, standardizing experimental protocols and reagent kits will be crucial for validating these biomarkers and translating them into tools that can reliably assess therapeutic efficacy in clinical trials, ultimately accelerating the development of new treatments.
Virtual Reality (VR) has evolved from an expensive novelty into a robust tool for clinical research and intervention [6]. Its ability to create controlled, immersive, and reproducible environments is particularly valuable for psychiatry and neuroscience, offering new avenues for therapy and the development of objective digital biomarkers for mental disorders [7] [3]. This guide compares the application of VR against traditional methods across key domains, supported by experimental data and detailed methodologies.
Comparative Efficacy of VR-Based Interventions
VR's therapeutic application spans multiple mental health conditions, primarily leveraging its capacity for controlled exposure and skill training. The table below summarizes its performance compared to traditional methods.
Table 1: Comparison of VR-Based Therapies vs. Traditional Methods
| Condition/Therapy | Key Finding | Comparative Outcome | Source Study Details |
|---|---|---|---|
| Social Anxiety Disorder (SAD) & Agoraphobia | No significant difference in symptom reduction between VR-CBT and traditional in-vivo CBT at post-treatment and 1-year follow-up. | Both groups showed significant improvements; VR-CBT offered a feasible, flexible alternative without compromising efficacy [8]. | Design: RCT, 177 participants.VR Intervention: 14 weekly group sessions using HMDs with 360° videos of anxiogenic situations (e.g., public speaking, crowded buses) [8]. |
| Psychosis Stigma in Professionals | Both VR and control groups showed improved attitudes and reduced stigma; no change in empathy. | VR intervention (simulating hallucinations) was not superior to control VR in outcomes, but had higher user satisfaction [9]. | Design: RCT, 180 mental health professionals.VR Intervention: Single ≤7-minute session using a smartphone-based HMD to simulate auditory and visual hallucinations in a home environment [9]. |
| Specific Phobias & PTSD | Effective as a medium for exposure therapy, especially when in-vivo exposure is impractical, dangerous, or costly [6] [10]. | Provides a safe, confidential, and controllable alternative to in-vivo or imaginal exposure, potentially improving patient access and adherence [10]. | Protocol: Virtual Reality Exposure Therapy (VRET) allows therapists to precisely control and tailor exposure stimuli based on a patient's fear hierarchy [6] [10]. |
VR in Biomarker Discovery and Cognitive Assessment
Beyond therapy, VR is proving instrumental in the objective assessment of cognitive and functional deficits, generating digital biomarkers that correlate with neurobiological changes.
Table 2: VR-Generated Biomarkers for Objective Assessment
| Assessment Target | VR-Derived Biomarkers | Performance vs. Traditional Methods | Source Study Details |
|---|---|---|---|
| Mild Cognitive Impairment (MCI) | Hand movement speed, scanpath length, time to completion, number of errors on a virtual kiosk test [3]. | SVM model using VR biomarkers alone achieved 90% specificity and 87.5% sensitivity in classifying MCI. A multimodal model combining VR and MRI biomarkers achieved 94.4% accuracy [3]. | Design: Validation study, 54 participants.VR Task: Virtual kiosk test for food ordering.Integration: VR biomarkers (high specificity) were combined with MRI biomarkers (high sensitivity) in a multimodal learning model for superior detection [3]. |
| Vestibular Dysfunction (post-mTBI) | Gaze stability, balance, and cognitive-motor integration metrics during military-relevant VR tasks. | Aims to correlate functional performance in VR with neurophysiological changes via rs-fMRI to support return-to-duty decisions [11]. | Design: Pilot study protocol (Praxis).VR Intervention: 4-week rehabilitation using VR and wearable sensors to deliver multisensory exercises. Outcome measures include functional performance and neuroimaging biomarkers [11]. |
| Mood Disorders | Data from wearables and smartphones: physical activity, sleep patterns, geolocation, voice analytics [12]. | Digital biomarkers offer continuous, longitudinal, and objective metrics, in contrast to intermittent self-reported clinical scales [12]. | Methodology: Passive and active data collection via consumer devices. Machine learning models analyze complex datasets to identify patterns related to symptom severity [12]. |
Detailed Experimental Protocols
To ensure reproducibility and critical evaluation, here are the methodologies from key cited experiments.
- Objective: To evaluate the effectiveness of a VR intervention on improving attitudes, empathy, and reducing stigma toward people with psychotic disorders.
- Study Design: Randomized Controlled Trial (RCT).
- Participants: 180 mental health care professionals (allied health staff, nurses, physicians).
- Intervention Group: Viewed a 7-minute VR scenario depicting a home environment with simulated auditory hallucinations (e.g., negative voices, laughing, crying) and visual distortions (e.g., floating words "die").
- Control Group: Viewed the same VR home environment without any hallucinations or distortions.
- Hardware: Smartphone device inserted into a VR headset equivalent to Google Cardboard.
- Outcome Measures: Standardized scales for attitudes, stigma, and empathy, administered at baseline, post-intervention, and 1-month follow-up.
- Objective: To integrate VR-derived and MRI biomarkers to enhance the early detection of Mild Cognitive Impairment (MCI).
- Study Design: Validation study.
- Participants: 54 adults (22 healthy controls, 32 with MCI).
- VR Biomarker Collection: Participants completed a "virtual kiosk test," where they performed a food-ordering task in a VR environment. Four biomarkers were extracted:
- Hand movement speed
- Scanpath length (eye movement)
- Time to completion
- Number of errors
- MRI Biomarker Collection: T1-weighted MRI scans were performed to collect 22 structural biomarkers from memory-associated brain regions.
- Data Integration: A Support Vector Machine (SVM) model was trained using the significant biomarkers from both modalities to classify participants as healthy or having MCI.
The workflow for this multimodal approach is outlined below.
The Scientist's Toolkit: Essential Research Reagents and Materials
This table details key solutions and technologies used in VR mental health research.
Table 3: Key Research Reagent Solutions in VR Mental Health Research
| Item/Technology | Function in Research | Specific Examples & Notes |
|---|---|---|
| Head-Mounted Display (HMD) | Creates an immersive virtual environment by occluding the outside world and displaying 3D computer-generated imagery [6]. | Ranges from high-end tethered devices (e.g., Oculus Rift) to cost-effective mobile solutions (e.g., Google Cardboard) [6] [9]. |
| VR Development Engine | Software platform used to create and render interactive, realistic virtual environments for therapy or assessment. | Unreal Engine [9] is used to create controlled scenarios with high visual fidelity. |
| Biometric Sensors | Capture objective physiological and behavioral data during VR sessions to quantify user response. | Eye-tracking within HMDs, hand motion controllers, and wearable devices (e.g., Actigraph, smart patches) to measure gait, heart rate, and electrodermal activity [11] [12] [3]. |
| Virtual Reality Exposure Therapy (VRET) Software | Provides pre-designed or customizable virtual environments for conducting exposure therapy. | Environments are tailored to specific phobias (e.g., heights, flying) or PTSD triggers, allowing graded exposure [6] [10]. |
| Data Analytics & Machine Learning Platform | Processes and analyzes the complex multimodal data (behavioral, physiological, neuroimaging) to identify digital biomarkers. | Used to build classification models (e.g., Support Vector Machines) that distinguish between clinical groups and healthy controls [12] [3]. |
Synthesis and Future Directions
The evidence confirms that VR is a validated medium for delivering therapeutic interventions, particularly exposure therapy, with efficacy comparable to traditional methods [8]. Its greater promise for research and drug development may lie in its capacity to generate objective, quantifiable digital biomarkers of functional impairment and cognitive decline [3]. The integration of VR with other data modalities like MRI, wearable sensors, and machine learning analytics is creating a new paradigm for validating biomarkers and assessing treatment efficacy in mental health [11] [12] [3]. Future work should focus on standardizing protocols, conducting large-scale studies, and integrating AI to further personalize and enhance interventions [10] [7].
Virtual reality (VR) has emerged as a powerful tool in mental disorders research, offering unprecedented opportunities for the development of objective biomarkers. By creating controlled, yet ecologically valid environments, VR enables the precise measurement of behavioral domains that are directly relevant to psychiatric pathology. This guide provides a comparative analysis of three key behavioral domains—eye-tracking, movement kinematics, and task performance—that are measured using VR technologies, with supporting experimental data and their validation status for mental disorders research.
Comparative Analysis of Key VR-Measured Behavioral Domains
The table below summarizes the core characteristics, measurement approaches, and evidence base for the three primary behavioral domains measurable via VR.
Table 1: Comparative Overview of Key VR-Measured Behavioral Domains
| Behavioral Domain | Key Measured Parameters | Primary VR Capabilities Utilized | Disorders with Strongest Evidence | Sample Classification Accuracy |
|---|---|---|---|---|
| Eye-Tracking | Fixations, saccades, smooth pursuit, scanpath length, pupillometry [13] [14] | Head-mounted display with integrated eye trackers, video oculography (VOG) [14] | Psychosis [15], ADHD [13] | 92% AUC (ADHD) [13]; 65% balanced accuracy (psychosis) [15] |
| Movement Kinematics | Hand movement speed, controller trajectory, navigation path efficiency, motor activity level [16] [4] | Motion controllers, hand tracking, positional tracking | MCI [4], ADHD [16] | 90% specificity (MCI) [4] |
| Task Performance | Errors (omission/commission), time to completion, tasks correctly performed, irrelevant actions [16] [13] [4] | Performance metrics within simulated functional tasks | ADHD [16] [13], MCI [4] | Higher % of irrelevant actions in ADHD [16] |
Detailed Experimental Protocols and Evidence
Eye-Tracking Biomarkers
Protocol: Smooth Pursuit Eye Movements (SPEM) for Psychosis
- Objective: To identify sensorimotor biomarkers for psychotic disorders using smooth pursuit eye movements [15].
- Methodology: Participants track a small moving object on a screen while eye movements are recorded. Key parameters include mean eye velocity, initial eye acceleration, and initiation latency [15].
- Analysis: Machine-learning models (multivariate pattern analysis) are trained on SPEM parameters to distinguish psychosis probands from healthy controls [15].
- Validation: Comprehensive external validation across multiple independent samples (B-SNIP, PARDIP, FOR2107) demonstrates robust classification with balanced accuracies ranging from 58% to 66% [15].
Protocol: Naturalistic Eye Tracking in ADHD (EPELI Task)
- Objective: To quantify attention and executive function deficits in children with ADHD using a lifelike VR task [13].
- Methodology: Participants perform a prospective memory game in VR (EPELI) with 13 scenarios of everyday chores, using a head-mounted display with a 90 Hz eye tracker [13].
- Analysis: Eye movement patterns are analyzed throughout the task, with a support vector machine classifier trained on this data [13].
- Validation: The classifier demonstrated excellent discrimination with 0.92 area under the curve (AUC), significantly outperforming traditional task performance measures [13].
Movement Kinematics Biomarkers
Protocol: Virtual Kiosk Test for Mild Cognitive Impairment (MCI)
- Objective: To capture behaviors associated with subtle deficits in instrumental activities of daily living for early MCI detection [4].
- Methodology: Participants interact with a virtual food-ordering kiosk while movement kinematics are tracked. Key parameters include hand movement speed and controller movement [4].
- Analysis: Comparison of kinematic biomarkers between healthy controls and MCI patients, with a support vector machine model achieving 90% specificity using VR-derived biomarkers alone [4].
- Integration: A multimodal approach combining VR-derived and MRI biomarkers achieved superior classification (94.4% accuracy, 100% sensitivity, 90.9% specificity) [4].
Task Performance Biomarkers
Protocol: Executive Performance in Everyday Living (EPELI) for ADHD
- Objective: To assess attention and executive function deficits in ecologically valid conditions that resemble situations where ADHD symptoms are manifested [16] [13].
- Methodology: Participants perform everyday chores in a virtual environment, with tasks including morning routines or returning from school, comprising 4-6 subtasks each [13].
- Performance Metrics: Percentage of irrelevant actions, navigation path length, number of correctly performed tasks, and amount of controller movement [16] [13].
- Findings: Children with ADHD showed higher percentages of irrelevant actions, longer navigation paths, more excessive actions, fewer correctly performed tasks, and greater controller movement compared to typically developing controls [16] [13].
Signaling Pathways and Experimental Workflows
The following diagram illustrates the integrated workflow from VR data acquisition to clinical biomarker validation, highlighting how multiple behavioral domains contribute to diagnostic insights.
VR Biomarker Development Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Solutions for VR Biomarker Studies
| Tool Category | Specific Examples | Research Function | Key Characteristics |
|---|---|---|---|
| VR Hardware with Integrated Eye Tracking | Tobii, Pupil Labs, Varjo, Fove [14] | Provides primary data acquisition for eye movement parameters | Uses Video Oculography (VOG); cameras mounted in HMD track eye orientation [14] |
| Behavioral Assessment Platforms | Nesplora Aquarium, EPELI, Virtual Kiosk Test [16] [13] [4] | Delivers standardized functional tasks in ecologically valid environments | Measures specific cognitive domains (attention, executive function, IADL) [16] [13] [4] |
| Motion Tracking Systems | VR controllers, hand tracking algorithms, positional tracking [16] [4] | Captures movement kinematics and motor activity | Quantifies hand movement speed, navigation efficiency, motor control [16] [4] |
| Machine Learning Frameworks | Support Vector Machines (SVM), Multivariate Pattern Analysis [13] [15] [4] | Analyzes complex multimodal data for classification | Identifies patterns distinguishing clinical groups from controls [13] [15] [4] |
VR-based measurement of eye-tracking, movement kinematics, and task performance represents a paradigm shift in mental disorders research, offering objective, quantifiable biomarkers with strong ecological validity. While eye-tracking currently shows the most robust classification accuracy for disorders like ADHD and psychosis, multimodal approaches that integrate multiple behavioral domains demonstrate superior predictive power. The field continues to evolve toward more sophisticated analytical approaches and standardized protocols that will further validate these digital biomarkers for both research and clinical applications.
The validation of virtual reality (VR) biomarkers for mental disorders research represents a paradigm shift in neuroscience and psychiatric diagnostics. Traditional diagnostic approaches often rely on subjective reports and clinical interviews, which lack biological grounding and are susceptible to observer bias [1]. VR technology, integrated with multimodal physiological sensing, offers a promising pathway for more objective diagnostics by creating standardized, immersive environments that can elicit ecologically valid neurophysiological responses [1] [17]. This guide systematically compares the performance of various VR-based neurophysiological assessment methodologies, providing researchers with experimental data and protocols for establishing validated biomarkers for mental health conditions. The core advantage of VR lies in its ability to seamlessly collect behavioral and physiological metrics—such as body movement, gaze patterns, and biosignals—without disrupting user engagement, thereby fostering deeper cognitive, social, and physical involvement that enhances the reliability of psychological assessments [1]. By synchronously capturing data within controlled yet naturalistic virtual environments, researchers can identify robust biomarkers of psychiatric conditions, transcending the limitations of traditional methods and potentially transforming early identification and intervention strategies for mental health [1].
Comparative Analysis of VR-Based Neurophysiological Biomarkers
Table 1: Comparative Performance of Neurophysiological Modalities in VR-Based Assessment
| Physiological Modality | Key Biomarkers Identified | Association with Mental Health Conditions | Supported by Experimental Evidence |
|---|---|---|---|
| EEG (Electroencephalography) | Higher theta/beta ratio [1]; Elevated beta/alpha ratio indicating high arousal [18]; Increased beta wave activity [18] | Associated with depression severity [1]; Differentiates emotional states in VR vs. real environments [18] | Case-control study with 115 adolescents [1]; Controlled comparison study of VR vs. real spaces [18] |
| HRV (Heart Rate Variability) | Elevated LF/HF ratio [1]; Transient increase in parasympathetic activity (pNN50) [18] | Significantly associated with depression severity [1]; Differentiates autonomic responses in VR environments [18] | Case-control study with 115 adolescents [1]; Pilot study on emotional equivalence [18] |
| Eye-Tracking (ET) | Reduced saccade counts; Longer fixation durations [1] | Robust biomarker for Major Depressive Disorder (MDD) in adolescents [1] | Case-control study with 115 adolescents [1] |
| Multimodal Integration (EEG+ET+HRV) | Combined biomarker profile; Machine learning classification features [1] | Achieved 81.7% classification accuracy for MDD with AUC of 0.921 [1] | SVM model trained on multimodal features from 115 participants [1] |
Table 2: Quantitative Experimental Results from Key VR Neurophysiology Studies
| Study Reference | Participant Population | VR Intervention/Task | Key Quantitative Findings | Statistical Significance |
|---|---|---|---|---|
| Wu et al. (2025) [1] | 51 MDD adolescents, 64 healthy controls | 10-minute VR-based emotional task with AI agent interaction | MDD group showed: EEG theta/beta ratio ↑, saccade counts ↓, fixation duration ↑, HRV LF/HF ratio ↑; SVM classification accuracy: 81.7% (AUC 0.921) | All group differences: p < 0.05 [1] |
| Emotional Equivalence Study (2025) [18] | Not specified | Comparison of identical spaces in VR vs. real world | Real-world: associated with comfort/preference; VR: evoked higher arousal impressions; EEG: elevated beta/alpha ratios in VR | Physiological measures showed consistent differences [18] |
| Cognitive Performance Study (2023) [19] | 41 older adults (mean age 62.8) | 4 Enhance VR games assessing memory, attention, flexibility | VR environments demonstrated high tolerance and usability; No significant correlation with traditional pen-and-paper tests | Hardware well-tolerated even by VR-naive participants [19] |
Detailed Experimental Protocols and Methodologies
VR-Based Emotional Task for Adolescent Depression Screening
The groundbreaking study by Wu et al. (2025) developed a comprehensive protocol for assessing major depressive disorder (MDD) in adolescents using VR-integrated multimodal sensing [1]. The experimental design involved:
- Participant Recruitment: 51 adolescents diagnosed with first-episode MDD according to DSM-5 criteria and 64 healthy controls recruited through a school-based screening program [1].
- VR Environment: A custom-developed immersive scenario using the A-Frame framework, featuring a magical forest lakeside panoramic background with an AI agent named "Xuyu" for interactive dialogue [1].
- Task Structure: A 10-minute structured interaction consisting of: (1) Introduction (1 minute), (2) Immersive Relaxation (5 minutes), (3) Supportive Interaction (3 minutes), and (4) Conclusion (1 minute) [1].
- Physiological Monitoring: Real-time data collection using the BIOPAC MP160 system for EEG, ECG, and ocular motility, with a See A8 portable telemetric ophthalmoscope for eye-tracking [1].
- Data Synchronization: LabStreamingLayer (LSL) technology for aligning multimodal physiological data with VR task events [1].
This protocol successfully identified robust physiological biomarkers, including significantly higher EEG theta/beta ratios, reduced saccade counts, longer fixation durations, and elevated HRV LF/HF ratios in adolescents with MDD compared to healthy controls [1].
Emotional Equivalence Protocol: VR vs. Real Environments
A critical methodological approach for validating VR biomarkers involves direct comparison with real-world environments [18]. The pilot investigation into emotional equivalence employed:
- Experimental Design: Construction of identically designed VR and real spaces to enable direct comparison of emotional responses [18].
- Assessment Methods: Combination of subjective evaluations (Semantic Differential method) and physiological indices (EEG and HRV) [18].
- Baseline Estimation: Implementation of two specialized methods for determining physiological baselines: the Pre-Stimulus Averaging Method and the Resting-State Prediction Method to account for habituation effects during VR viewing [20].
- Controlled Conditions: Careful matching of visual stimuli between VR and real conditions while controlling for non-visual environmental factors such as sound and scent [18].
This protocol revealed that real-world environments were associated with impressions of comfort and preference, whereas VR environments evoked impressions characterized by heightened arousal, with elevated beta wave activity and increased beta/alpha ratios observed in the VR condition [18].
Diagram 1: Experimental workflow for VR-real world emotional equivalence studies
Cognitive Assessment Protocols in Virtual Environments
VR-based cognitive assessment represents another significant application in mental health research. The Enhance VR study protocol demonstrates this approach [19]:
- Participant Profile: 41 older adults (mean age 62.8 years) without neurodegenerative or psychiatric disorders [19].
- Hardware: Meta Quest (Oculus VR) standalone headset with two controllers for interaction [19].
- VR Cognitive Tasks: Four specific gamified exercises based on validated neuropsychological principles:
- Magic Deck: Inspired by Paired Associates Learning test for memory assessment [19].
- Memory Wall: Motivated by Visual Pattern Test for short-term memory evaluation [19].
- Pizza Builder: Inspired by divided attention assessments requiring simultaneous task management [19].
- React: Based on Wisconsin Card Sorting Task and Stroop test for cognitive flexibility [19].
- Comparison Methodology: Random assignment to either traditional neuropsychological testing or VR assessment sessions on different days to compare assessment methodologies [19].
This protocol demonstrated that VR-based cognitive assessment was extremely well tolerated, intuitive, and accessible even to those with no prior VR experience, supporting the ecological validity of VR environments for neuropsychological evaluation [19].
Signaling Pathways and Neurophysiological Logical Framework
The relationship between VR stimulation, physiological responses, and clinical applications follows a logical pathway that can be mapped to validate VR biomarkers for mental health research.
Diagram 2: Neurophysiological pathways linking VR stimulation to clinical applications
The logical framework demonstrates how controlled VR stimuli elicit responses across both central and autonomic nervous systems, generating measurable biomarkers that can be leveraged for various clinical applications in mental health research [1] [18] [21]. The EEG theta/beta ratio has been specifically associated with depression severity, while HRV LF/HF ratios reflect autonomic dysregulation linked to psychiatric conditions [1]. Eye-tracking metrics provide behavioral indicators of attentional patterns characteristic of mental disorders [1].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Tools for VR Neurophysiology Studies
| Tool Category | Specific Products/Technologies | Key Functions | Research Applications |
|---|---|---|---|
| VR Hardware Platforms | Meta Quest (Oculus VR) [19]; HTC Vive [17]; Head-Mounted Displays (HMDs) [21] | Create immersive virtual environments; Enable user interaction through controllers | Cognitive assessment [19]; Mindfulness interventions [21]; Emotional task delivery [1] |
| Physiological Data Acquisition Systems | BIOPAC MP160 system [1]; Portable telemetric ophthalmoscope (See A8) [1] | Record EEG, ECG, ocular motility; Capture eye-tracking data | Multimodal sensing during VR tasks [1]; Real-time biosignal collection [1] |
| VR Development Frameworks | A-Frame framework [1]; Virtools Dev software [17] | Develop custom VR environments; Create interactive 3D scenarios | Building controlled experimental paradigms [1]; Designing ecological valid scenarios [17] |
| Data Synchronization Solutions | LabStreamingLayer (LSL) [1] | Align multimodal physiological data with VR events; Ensure temporal precision | Multimodal data integration [1]; Time-locked analysis of responses [1] |
| Analysis & Machine Learning Tools | Support Vector Machine (SVM) [1]; Statistical analysis packages (R, Python) | Classify MDD status based on features; Identify significant biomarker differences | Developing diagnostic models [1]; Analyzing physiological patterns [1] |
The integration of VR with multimodal physiological monitoring represents a transformative approach in mental health research, offering objective biomarkers that complement traditional subjective assessments. Experimental evidence demonstrates that VR-based paradigms can successfully identify robust neurophysiological signatures of mental health conditions, with EEG, HRV, and eye-tracking metrics showing consistent differentiation between clinical populations and healthy controls [1]. The strong classification performance of machine learning models applied to these multimodal features (81.7% accuracy for MDD with AUC of 0.921) underscores the clinical potential of this approach [1].
Future research directions should address several key challenges, including the need for standardized VR protocols specifically tailored for mental health assessment [1], refinement of baseline estimation methods for physiological data [20], and larger-scale validation studies across diverse populations. Additionally, further investigation is needed to establish the emotional equivalence between VR and real-world environments, as current research indicates measurable differences in arousal states and physiological responses [18]. As the field advances, the translation of these VR biomarker platforms into wearable or mobile systems promises to enhance the scalability and accessibility of objective mental health screening, potentially revolutionizing early detection and intervention strategies for psychiatric disorders [1].
The rising global prevalence of Alzheimer's disease underscores the critical need for accessible early screening of its preclinical stage, mild cognitive impairment (MCI). Virtual Kiosk Tests (VKTs) represent an emerging class of digital biomarkers that leverage immersive virtual reality (VR) to assess instrumental activities of daily living (IADL). This guide objectively compares the performance of VKTs against traditional screening tools and other biomarker-based approaches, presenting synthesized experimental data to validate VR-based biomarkers for mental disorders research. Evidence indicates that VKTs achieve high diagnostic accuracy, offer superior ecological validity, and integrate effectively into multimodal screening frameworks, presenting a compelling tool for researchers and drug development professionals.
Mild cognitive impairment (MCI), particularly the amnestic subtype (aMCI), is a transitional stage between healthy aging and Alzheimer's disease (AD), with approximately 80% of individuals eventually progressing to AD [22]. Early detection is paramount, as it represents a critical window for interventions that may slow progression or even restore cognitive function [23] [3]. Traditional screening tools face significant limitations:
- Brief Cognitive Tests: Tools like the Montreal Cognitive Assessment (MoCA) are common but can lack the sensitivity to detect subtle, early deficits [24] [25].
- Conventional Biomarkers: Neuroimaging (MRI, PET) and cerebrospinal fluid analysis, while valuable, are often expensive, invasive, and lack feasibility for widespread, repeated screening [23] [25].
- Neuropsychological Batteries: Although comprehensive, these are time-consuming and can suffer from issues like ceiling effects and poor ecological validity, meaning they poorly reflect real-world cognitive challenges [3] [24].
Virtual Kiosk Tests address these gaps by using immersive VR to simulate a common IADL—ordering food at a self-service kiosk. This approach captures ecologically valid behavioral data in a standardized, controlled environment [23].
Virtual Kiosk Test: Protocol & Measured Biomarkers
Core Experimental Protocol
The VKT methodology is standardized to ensure reproducibility and reliable data collection across participants. The following workflow outlines the key stages of a typical VKT experiment, from participant preparation to data analysis.
Participant Preparation: Participants are typically recruited from memory clinics and diagnosed according to established criteria (e.g., Petersen criteria) by experienced neurologists [23] [22]. Key inclusion criteria often include being over 50 years old and having normal sensory perception [23].
VR Setup: Participants sit on a chair for safety and use a head-mounted display (e.g., HTC Vive Pro Eye) and a hand controller. Eye movements are tracked via sensors in the HMD, and hand movements are tracked using base stations [23] [22].
Task Execution: Participants are instructed to memorize a complex order (e.g., "Order a shrimp burger, cheese sticks, and a Coca-Cola using a credit card with password 6289") [22]. They then perform the ordering task in the virtual environment, which involves multiple steps such as selecting food items, choosing a payment method, and entering a PIN [23] [22].
Key Digital Biomarkers Captured
The VKT generates quantitative, objective metrics across several behavioral domains:
1. Hand Movement Kinematics
- Hand Movement Speed: Slower average speed is indicative of MCI [23].
- 3D Trajectory Length: Longer, less efficient movement paths are associated with cognitive impairment [24].
2. Eye Movement Metrics
- Proportion of Fixation Duration: Lower percentage of time fixated on target menu items suggests attentional deficits [23].
- Scanpath Length: Longer total gaze distance indicates less efficient visual search strategies [22].
3. Task Performance Metrics
- Time to Completion: Longer total time to complete the task [23].
- Number of Errors: Higher error counts (e.g., incorrect selections) [23].
- Hesitation Latency: Delays in initiating actions, reflecting executive dysfunction [24].
Performance Comparison: VKTs vs. Alternative Modalities
The following tables synthesize quantitative data from recent studies, comparing the diagnostic performance of VKTs against other screening methods and biomarkers.
Table 1: Comparative Diagnostic Accuracy for MCI Detection
| Screening Method | Reported Accuracy | Reported Sensitivity | Reported Specificity | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| Virtual Kiosk Test (VKT) | 93.3% [23] | 100% [23] [3] | 90.9% [3] | High ecological validity, cost-effective, short test duration (5-15 mins) [23] | Requires VR equipment, potential for cybersickness |
| VKT + EEG-SSVEP | 98.38% [22] | - | - | Provides linked behavioral & neurological insight [22] | Complex setup, requires specialized EEG equipment & expertise |
| VKT + MRI Biomarkers | 94.4% [3] | 100% [3] | 90.9% [3] | Multimodal validation, links behavior to structural brain changes [3] | High cost of MRI, less accessible for routine screening |
| VR Stroop Test (VRST) | AUC: 0.981 [24] | - | - | Excellent discriminant power, high construct validity [24] | Assesses specific cognitive domain (executive function) |
| MoCA (Traditional Tool) | AUC: 0.962 [24] | Lower than VR [25] | Lower than VR [25] | Widespread use, fast administration [25] | Lower sensitivity for early MCI, lacks ecological validity [24] [25] |
| MRI Biomarkers (Unimodal) | - | 90.9% [3] | 71.4% [3] | High sensitivity, quantifies brain structure [3] | Low specificity, high cost, unsuitable for frequent monitoring [3] |
Table 2: Statistical Significance of Key VKT Biomarkers (MCI vs. Healthy Controls)
| Digital Biomarker | Statistical Result | P-Value | Cognitive Domain Assessed |
|---|---|---|---|
| Hand Movement Speed | t~49~ = 3.45 | P = .004 [23] | Psychomotor speed, executive function |
| Proportion of Fixation Duration | t~49~ = 2.69 | P = .04 [23] | Attention, visual search efficiency |
| Time to Completion | t~49~ = -3.44 | P = .004 [23] | Processing speed, task efficiency |
| Number of Errors | t~49~ = -3.77 | P = .001 [23] | Memory, executive function |
| 3D Hand Trajectory Length | Highest AUC = 0.981 [24] | P < .001 (implied) | Motor planning, executive control |
A meta-analysis of 29 studies on VR for MCI detection found that VR-based assessments have a pooled sensitivity of 0.883 and specificity of 0.887, confirming the robust performance of this approach across various implementations [25].
The Scientist's Toolkit: Essential Research Reagents & Materials
Implementing a Virtual Kiosk Test in a research setting requires specific hardware and software components. The following table details the essential solutions and their functions.
Table 3: Key Research Reagents and Solutions for VKT Implementation
| Item Name / Category | Example Model / Software | Primary Function in Protocol |
|---|---|---|
| Head-Mounted Display (HMD) | HTC Vive Pro Eye [23] [22] | Presents the virtual environment; integrated eye-tracking enables collection of gaze metrics. |
| Hand Motion Controller | HTC Vive Controller [22] [24] | Tracks hand movement kinematics (speed, trajectory) during task interaction. |
| Position Tracking System | HTC Vive Base Stations [23] [22] | Provides precise spatial tracking of the HMD and controller within the physical space. |
| Software & Game Engine | Unity [24] | Platform for developing, rendering, and running the interactive virtual kiosk environment. |
| Data Processing & Analysis | Custom Python/MATLAB scripts; SVM classifiers [23] [3] | For processing time-series data, extracting features, and building classification models. |
| Performance Validation | Seoul Neuropsychological Screening Battery (SNSB-C) [23] [3] | Gold-standard neuropsychological test used for participant diagnosis and correlational validation. |
Integration in a Multimodal Biomarker Framework
VKTs are most powerful when integrated into a broader biomarker strategy. Research shows that VKT performance correlates with both neurological and neuropsychological measures, establishing its construct validity.
- Correlation with Brain Structure: A multimodal study found a significant correlation between impaired VKT performance and brain atrophy in memory-related regions like the hippocampus and entorhinal cortex, measured via MRI [3]. This links behavioral deficits observed in VR to their underlying neurological substrates.
- Correlation with Neural Function: Integrating VKT with EEG-SSVEP has demonstrated a relationship between behavioral impairments and a compromised dorsal stream of the visual pathway, which governs behavioral responses to visual stimuli [22].
- Correlation with Cognitive Domains: VKT features (e.g., time to completion, errors) show significant correlations with standardized tests of executive function, attention, and memory [23] [24].
The following diagram illustrates the convergent validity of the VKT and its position within a multimodal assessment framework.
Discussion and Future Directions
Virtual Kiosk Tests demonstrate a compelling balance of high diagnostic accuracy, ecological validity, and practical feasibility for early MCI screening. The synthesized data shows that VKTs consistently outperform traditional brief cognitive screens and can serve as a specific, cost-effective tool for population-level screening prior to more invasive and expensive confirmatory biomarker tests [3] [25].
For researchers and drug development professionals, VKTs offer a reliable digital biomarker for enriching clinical trial cohorts with early MCI patients and for providing sensitive, objective outcome measures to track intervention effects. Future work should focus on standardizing protocols across sites, validating VKTs in more diverse populations, and further exploring their predictive value for conversion from MCI to Alzheimer's dementia. The integration of VKTs with other digital data streams, such as passive smartphone monitoring, presents a promising avenue for continuous, real-world cognitive assessment.
Building and Deploying VR Biomarker Assays: From Lab to Clinical Trial
Designing Ecologically Valid VR Environments for Specific Disorders
Virtual Reality (VR) has emerged as a transformative tool in mental health research and treatment development, particularly for its potential to create controlled yet ecologically valid assessment and intervention environments. Ecological validity refers to the extent to which laboratory findings generalize to real-world settings, encompassing both verisimilitude (the degree to which test demands resemble everyday life demands) and veridicality (the empirical relationship between test performance and real-world functioning) [26]. For researchers and pharmaceutical developers targeting specific disorders, designing VR environments with strong ecological validity is crucial for generating clinically meaningful biomarkers and treatment outcomes that translate beyond laboratory settings.
The tension between experimental control and real-world relevance has long challenged clinical neuroscience [26]. Traditional paper-and-pencil neuropsychological tests often assess cognitive constructs without clear connections to daily functioning [26]. VR technology offers a resolution to this dilemma by enabling precise stimulus control within simulations that closely mimic real-world challenges faced by people with mental disorders [27] [26]. This capacity for creating standardized yet ecologically relevant environments makes VR particularly valuable for developing digital biomarkers that can sensitively measure treatment effects in clinical trials.
Theoretical Framework: Core Principles of Ecologically Valid VR Design
Key Dimensions of Ecological Validity
| Dimension | Definition | Research Application | Clinical Relevance |
|---|---|---|---|
| Verisimilitude | Similarity between task demands in VR and everyday life [26] | Designing supermarket shopping tasks for ADHD assessment [27] | Predicts real-world functional capacity |
| Veridicality | Empirical relationship between VR performance and real-world functioning [26] | Correlating VR attention measures with academic performance [28] | Validates biomarkers for treatment outcome prediction |
| Personal Relevance | Match between VR scenario and patient-specific challenges | Customizing social scenarios for social anxiety disorder | Enhances engagement and treatment generalization |
| Dynamic Complexity | Incorporation of multi-sensory, unpredictable elements | Adding distractors to continuous performance tests [28] | Captures real-world cognitive challenges |
Critical Technical Elements for Enhancing Ecological Validity
Several technical and design elements collectively contribute to the ecological validity of VR environments for mental health applications:
Immersion Level: Higher immersion through head-mounted displays (HMDs) enhances the feeling of presence, though both immersive and non-immersive systems have applications depending on the target disorder and assessment goals [27]. HMDs were perceived as more immersive than cylindrical room-scale VR in audio-visual research, though both showed ecological validity for perceptual parameters [29].
Naturalistic Interaction: Interfaces that allow users to employ their own body movements (rather than keyboards or joysticks) facilitate more comparable performance between gamers and non-gamers, making assessments more applicable to broader populations [27].
Contextual Embedding: Placing cognitive tasks within emotionally engaging narratives or familiar real-world contexts enhances affective experience and social interactions, making responses more representative of real-world behavior [26].
Multi-sensory Integration: Incorporating visual, auditory, and even haptic cues that mirror real-world experiences strengthens the illusion of reality and elicits more naturalistic responses [29].
Disorder-Specific VR Environment Design: Applications and Evidence
Psychotic Disorders: Simulating Subjective Experiences
VR interventions for psychotic disorders have primarily focused on fostering empathy and reducing stigma among healthcare professionals, while also showing promise for assessment and rehabilitation.
A randomized controlled trial with 180 mental health professionals demonstrated that a VR intervention simulating auditory hallucinations (e.g., hearing voices saying "die" and "poison") and visual hallucinations (e.g., floating items, shadow-like figures) in a home environment significantly improved attitudes and reduced stigma toward people with psychotic disorders [9]. The intervention, delivered via head-mounted display and lasting approximately 7 minutes, presented increasing frequency of negative auditory content corresponding with visual hallucinations, culminating in suicidal ideation voices [9].
Experimental Protocol: The VR environment was constructed using Unreal Engine and based on systematic review of effective stigma reduction elements [9]. Clinical input and peer specialist feedback ensured authentic representation of psychotic experiences. The control group experienced the same virtual home environment without hallucination simulations.
ADHD and Attention Disorders: Environmental Distraction Modulation
VR continuous performance tests (CPTs) have addressed ecological validity limitations of traditional attention assessments by incorporating real-world distractors. The "Pay Attention!" program exemplifies this approach with four key design innovations [28]:
- Multiple Real-World Scenarios: Four familiar environments (room, library, outdoors, café) instead of artificial laboratory settings
- Graduated Difficulty Levels: Four distinct difficulty levels varying in distraction intensity, stimulus complexity, and inter-stimulus intervals
- Home-Based Assessment: Deployment in naturalistic home settings rather than clinical laboratories
- Extended Assessment Period: Multiple testing sessions over time to capture intra-individual variability
Experimental Protocol: A feasibility study with 20 Korean adults implemented 12 blocks of testing over two weeks. Each block presented CPT tasks within the different environmental contexts with varying distraction levels. Performance metrics (commission errors, omission errors, reaction time variability) were tracked alongside psychological assessments and EEG measurements [28].
The results demonstrated that higher commission errors specifically emerged in the "very high" difficulty level featuring complex stimuli and increased distraction. A significant correlation between overall distraction level and CPT accuracy validated the ecological relevance of the environmental manipulations [28].
Acquired Brain Injury: Activities of Daily Living Simulation
A systematic review of 70 studies on VR for acquired brain injury (ABI) revealed diverse ecological environments targeting real-world functioning [27]. The most common simulations included:
- 12 different kitchen environments for meal preparation tasks
- 11 supermarket scenarios for shopping and navigation challenges
- 10 shopping malls for complex wayfinding and purchasing
- 16 street environments for crossing safety and navigation
- 11 city contexts for large-scale spatial orientation
- 10 other everyday life scenarios for various daily activities
These environments primarily assessed and rehabilitated cognitive functions within the context of activities of daily living (ADLs), addressing the critical need for functional relevance in neurorehabilitation [27]. The ecological approach moves beyond construct-driven assessment to function-led evaluation that directly predicts real-world capabilities.
Quantitative Outcomes: Comparative Efficacy of VR Interventions
Performance Comparison Across Disorders and Environments
| Disorder | VR Environment Type | Key Outcome Measures | Effect Size/Performance | Comparison Condition |
|---|---|---|---|---|
| Psychotic Disorders | Home environment with hallucination simulations [9] | Attitudes, Stigma, Empathy | Significant improvements in attitudes and stigma (p<0.05) | VR control without hallucinations |
| ADHD | "Pay Attention!" with multi-level distractions [28] | Commission Errors, Omission Errors | Significantly higher commission errors at highest difficulty | Traditional CPT without ecological distractors |
| Acquired Brain Injury | Kitchen, supermarket, street scenarios [27] | Functional Independence Measures | Modest evidence for functional improvement | Traditional occupational therapy |
| Medical Education | Various anatomical and procedural trainers [30] | Examination Pass Rates | OR=1.85 (95% CI: 1.32-2.58) | Traditional education methods |
Ecological Validity Metrics Across VR Systems
| VR System Type | Perceptual Validity | Psychological Restoration | Physiological Response | Realism Rating |
|---|---|---|---|---|
| Head-Mounted Display (HMD) | High ecological validity [29] | Moderate accuracy vs. real-world [29] | Valid for EEG change metrics [29] | Higher immersion [29] |
| Cylindrical Room-Scale VR | High ecological validity [29] | Slightly better accuracy than HMD [29] | More accurate for EEG time-domain features [29] | Lower immersion [29] |
| Computer Screen VR | Moderate ecological validity [27] | Not systematically assessed | Limited physiological engagement | Lower presence [27] |
| CAVE Systems | Limited research available [29] | Limited research available | Limited research available | Limited research available |
Methodological Considerations for VR Biomarker Development
Experimental Design Workflow for VR Environment Validation
Research Reagent Solutions: Essential Materials for VR Experimentation
| Research Tool | Function | Example Application | Technical Specifications |
|---|---|---|---|
| Head-Mounted Displays (HMDs) | Create immersive visual experience | Hallucination simulation for psychosis [9] | Varying levels of immersion and field of view |
| Game Engines (Unreal Engine) | Develop interactive 3D environments | Creating home environment for psychosis simulation [9] | Real-time rendering capabilities |
| Physiological Monitors (EEG, HR) | Objective arousal and cognitive load measurement | Attention monitoring during VR CPT [28] | Synchronization with VR presentation |
| Virtual Environment Libraries | Standardized scenario repositories | Kitchen, supermarket, street scenarios for ABI [27] | Customization capacity for specific disorders |
| Cybersickness Assessment Tools | Measure VR-induced discomfort | Essential for ABI populations with higher susceptibility [27] | Multiple symptom dimensions |
The development of ecologically valid VR environments for specific disorders represents a promising pathway for creating clinically meaningful digital biomarkers in mental health research and pharmaceutical development. Current evidence demonstrates that VR can effectively bridge the gap between laboratory control and real-world relevance across multiple disorders, including psychotic disorders, ADHD, and acquired brain injury.
Key design principles emerging from the research include:
- Disorder-specific environmental relevance matching particular functional challenges
- Graduated difficulty and distraction levels to avoid ceiling and floor effects
- Multi-sensory integration enhancing realism and engagement
- Naturalistic interaction modalities reducing technological barriers
Future research should address current limitations, including standardization of outcome measures, development of normative profiles across different populations, and systematic assessment of cybersickness particularly in vulnerable clinical groups [27]. Additionally, further validation studies comparing VR measures with real-world functioning across different disorders will strengthen the ecological validity of these approaches.
For pharmaceutical researchers, VR environments offer the potential for sensitive, ecologically relevant biomarkers that can detect subtle treatment effects and predict real-world functional outcomes. The continued refinement of these virtual environments holds significant promise for enhancing the validity and clinical utility of mental health intervention research.
The quest for objective biomarkers in mental health research is increasingly turning to immersive technologies like virtual reality (VR) combined with sophisticated multimodal data fusion. This approach integrates diverse neurophysiological and behavioral data streams—eye-tracking, electroencephalography (EEG), heart rate variability (HRV), and motion data—to capture the complex dynamics of brain function and behavior that underlie psychiatric disorders [31]. In the era of big data, where vast amounts of information are generated at unprecedented rates, innovative data-driven fusion methods are essential for integrating diverse perspectives to extract meaningful insights and achieve a more comprehensive understanding of complex psychiatric conditions [32]. Traditional separate analysis of each data modality may only reveal partial insights or miss important correlations between different data types, whereas multimodal fusion enables researchers to uncover hidden patterns and relationships that would otherwise remain undetected [32].
The validation of VR biomarkers represents a paradigm shift from subjective symptom reporting toward biologically-grounded, objective diagnostic tools. This is particularly crucial in conditions like major depressive disorder (MDD), where current diagnostic approaches predominantly rely on symptom checklists and clinical interviews that lack biological grounding and are susceptible to subjectivity [31]. Empirical research indicates that over 50% of depression cases are either misdiagnosed or overlooked, significantly compromising treatment effectiveness [31]. Multimodal fusion approaches allow researchers to incorporate multiple factors including genetics, environment, cognition, and treatment outcomes across various brain disorders, potentially uncovering subtle abnormalities or biomarkers that may benefit targeted treatments and personalized medical interventions [32].
Experimental Approaches in Multimodal Data Collection
VR-Integrated Experimental Protocols
Recent research has pioneered sophisticated protocols for collecting multimodal data within controlled yet ecologically valid VR environments. One notable case-control study focused on adolescent depression screening developed a 10-minute VR-based emotional task where participants engaged in interactive dialogues with an AI agent named "Xuyu" while physiological data were collected in real-time [31]. The VR environment featured a panoramic magical forest landscape by a lakeside, creating a standardized yet immersive context for emotional exploration. During the session, participants discussed themes of personal worries, distress, and hopes for the future, providing a rich behavioral context for the simultaneously acquired physiological measurements [31].
Another innovative approach examined visuomotor integration using a complex aircraft identification scenario. This protocol collected simultaneous EEG (34 electrodes), functional near-infrared spectroscopy (fNIRS) with 44 channels covering frontal and parietal cortex, eye movements, and manual joystick responses [33]. The experiment consisted of six blocks, each containing both easy tasks (with fixed target positions) and hard tasks (with random target locations), allowing researchers to examine cognitive load and attentional processes across different difficulty levels. This comprehensive setup enabled the capture of implicit behaviors (eye movements) alongside explicit motor responses, providing unique insights into how cognitive processes unfold over time [33].
Cognitive Load Assessment Protocols
Research on cognitive load measurement has developed specialized reading protocols to examine how different types of cognitive load manifest in physiological signals. One study with 102 non-native English speakers investigated how background music (BGM) affects reading comprehension and cognitive processes [34]. Participants read English passages either with self-selected preferred BGM or in silence while researchers collected eye movement data, electrodermal activity (EDA), heart rate (HR), and heart rate variability (HRV). The study employed the triarchic model of cognitive load, examining:
- Extraneous load: Created by adding background music
- Intrinsic load: Manipulated through text complexity
- Germane load: Reflected by comprehension accuracy [34]
This approach allowed researchers to identify which physiological signals were most sensitive to different types of cognitive load, providing a framework for non-intrusive cognitive state monitoring during complex tasks.
Data Fusion Methodologies and Analytical Frameworks
Machine Learning Approaches for Diagnostic Classification
Sophisticated machine learning frameworks have demonstrated remarkable success in classifying psychiatric conditions based on multimodal data. In the adolescent depression study, researchers trained a support vector machine (SVM) model to classify MDD status based on selected features from EEG, eye-tracking, and HRV data [31]. The model achieved an impressive 81.7% classification accuracy with an area under the curve (AUC) of 0.921, significantly outperforming traditional diagnostic approaches. Key physiological features that drove classification accuracy included:
- EEG metrics: Higher theta/beta ratios in adolescents with MDD
- Eye-tracking measures: Reduced saccade counts and longer fixation durations
- HRV parameters: Elevated LF/HF ratios indicating autonomic nervous system dysregulation [31]
The theta/beta and LF/HF ratios both showed significant associations with depression severity, suggesting their potential as quantitative biomarkers for tracking symptom progression and treatment response.
Deep Graph Learning for Treatment Prediction
For treatment prediction, advanced deep learning approaches have emerged that can model the complex relationships between multimodal brain networks. One groundbreaking study analyzed resting-state fMRI and EEG connectivity data from 265 patients from the EMBARC study—130 treated with sertraline and 135 with placebo [35]. Researchers developed a novel deep learning framework using graph neural networks (GNNs) to integrate data-augmented connectivity and cross-modality correlations, aiming to predict individual symptom changes by revealing multimodal brain network signatures [35].
The model demonstrated promising prediction accuracy, with an R² value of 0.24 for sertraline and 0.20 for placebo, and exhibited potential in transferring predictions using only EEG data. Critical brain regions identified for predicting sertraline response included the inferior temporal gyrus (fMRI) and posterior cingulate cortex (EEG), while for placebo response, the precuneus (fMRI) and supplementary motor area (EEG) were particularly important [35]. This approach demonstrates how fusion of complementary neuroimaging modalities can uncover clinically meaningful biomarkers for predicting treatment outcomes.
Table 1: Performance Comparison of Multimodal Fusion Approaches
| Study Objective | Data Modalities | Fusion Method | Key Performance Metrics |
|---|---|---|---|
| Adolescent MDD Screening [31] | EEG, Eye-tracking, HRV | Support Vector Machine (SVM) | 81.7% classification accuracy, AUC: 0.921 |
| Antidepressant Treatment Prediction [35] | fMRI, EEG | Graph Neural Networks (GNN) | R² = 0.24 (sertraline), R² = 0.20 (placebo) |
| Cognitive Load Assessment [34] | Eye-tracking, EDA, HR, HRV | Multimodal Learning Analytics | EM predicted all 3 load types; HR/HRV predicted extraneous and germane load |
Multimodal Fusion Techniques
The field has developed various technical approaches for fusing multimodal data, each with distinct advantages and applications. Joint Independent Component Analysis (jICA) jointly analyzes multiple datasets by concatenating them along a certain dimension, based on the assumption that two or more features share the same mixing matrix and maximize independence among joint components [32]. Multimodal Canonical Correlation Analysis (mCCA) explores inter-subject relationships by identifying maximally correlated components across modalities, while mCCA + jICA combines both approaches to leverage their complementary strengths [32]. Emerging deep learning approaches directly handle high-dimensional raw data to extract individual variations by integrating multi-level dimensionality reduction and subject-level reconstruction techniques [32].
Key Physiological Biomarkers Across Modalities
EEG-Derived Biomarkers
Electroencephalography provides crucial information about brain electrical activity with millisecond temporal resolution, making it particularly valuable for capturing dynamic neural processes. Research has consistently identified distinctive EEG patterns associated with psychiatric conditions. In adolescent depression, significantly higher EEG theta/beta ratios have been observed in those with MDD compared to healthy controls [31]. This metric reflects an imbalance between cortical inhibition and arousal, potentially indicating regulatory deficits in depression. For antidepressant treatment prediction, studies have identified the posterior cingulate cortex as a critical region in EEG connectivity patterns that predict sertraline response [35]. The superior temporal resolution of EEG also enables the capture of event-related potentials (ERPs) that index specific cognitive processes such as attention, working memory, and error monitoring, which are frequently impaired across psychiatric disorders.
Eye-Tracking Biomarkers
Eye movement patterns provide a rich window into cognitive processes including attention, engagement, and information processing. Research has identified several robust oculometric biomarkers for psychiatric conditions. Adolescents with MDD demonstrate reduced saccade counts and longer fixation durations compared to healthy controls, potentially reflecting altered attentional allocation and processing speed [31]. In cognitive load assessment during reading tasks, measures such as fixation duration, saccade amplitude, and regression count have proven predictive of all three types of cognitive load—extraneous, intrinsic, and germane [34]. These eye movement patterns can indicate difficulties in lexical processing and post-lexical semantic integration, providing non-invasive markers of cognitive effort and processing efficiency.
HRV and Autonomic Nervous System Biomarkers
Heart rate variability offers valuable insights into autonomic nervous system regulation, which is frequently disrupted in psychiatric disorders. Research consistently shows elevated LF/HF ratios in adolescents with MDD, indicating sympathetic nervous system dominance and reduced parasympathetic modulation [31]. These HRV-derived metrics reflect autonomic dysregulation linked to depression severity and have shown significant associations with depression severity scores [31]. In cognitive load research, HR and HRV measures have demonstrated sensitivity to extraneous and germane cognitive load during reading tasks, providing objective physiological indices of cognitive resource allocation [34]. Additionally, electrodermal activity (EDA), particularly skin conductance response (SCR), captures phasic sympathetic nervous system activation that correlates with emotionally salient stimuli and cognitively demanding moments [34].
Table 2: Key Physiological Biomarkers Identified Through Multimodal Fusion
| Modality | Biomarker | Association with Mental States | Clinical/Research Utility |
|---|---|---|---|
| EEG | Theta/Beta Ratio [31] | Elevated in adolescent MDD | Potential indicator of cortical regulation imbalance |
| EEG | Posterior Cingulate Cortex Connectivity [35] | Predictive of sertraline response | Treatment prediction biomarker |
| Eye-Tracking | Saccade Count [31] | Reduced in adolescent MDD | Attentional allocation marker |
| Eye-Tracking | Fixation Duration [31] [34] | Prolonged in MDD; sensitive to cognitive load | Processing speed and effort indicator |
| HRV | LF/HF Ratio [31] | Elevated in adolescent MDD | Autonomic nervous system dysregulation marker |
| HRV | Heart Rate Variability [34] | Predictive of extraneous and germane cognitive load | Cognitive resource allocation index |
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing robust multimodal fusion research requires specialized equipment and analytical tools. Below is a comprehensive table of essential research reagents and solutions used in the featured studies:
Table 3: Essential Research Reagents and Solutions for Multimodal Studies
| Tool/Reagent | Specification/Model | Primary Function | Example Use Case |
|---|---|---|---|
| VR Development Framework | A-Frame framework [31] | Creates immersive web-based VR environments | Developing magical forest scenario for depression assessment |
| Physiological Data Acquisition | BIOPAC MP160 system [31] | Synchronized recording of EEG, ECG, and other physiological signals | Collecting multimodal data during VR emotional tasks |
| Portable Ophthalmoscope | See A8 telemetric ophthalmoscope [31] | Records ocular motility and eye movement data | Tracking gaze patterns during VR tasks |
| EEG Recording Systems | 34-electrode whole-brain EEG [33] | Captures electrical brain activity with millisecond resolution | Monitoring neural dynamics during visuomotor tasks |
| fNIRS Systems | 44-channel fNIRS covering frontal and parietal cortex [33] | Measures hemodynamic responses using near-infrared light | Assessing brain activation during cognitive tasks |
| Eye-Tracking Integration | Integrated with VR headset [31] | Records gaze patterns and pupillary responses within immersive environments | Monitoring attentional allocation during VR scenarios |
| Machine Learning Framework | Support Vector Machine (SVM) [31] | Classifies physiological patterns associated with clinical conditions | Differentiating MDD patients from healthy controls |
| Deep Learning Architecture | Graph Neural Networks (GNN) [35] | Models complex relationships in brain network data | Predicting antidepressant treatment outcomes |
Comparative Performance of Fusion Approaches
The integration of multiple data modalities consistently demonstrates superior performance compared to unimodal approaches across various applications. In mental health assessment, multimodal frameworks achieve significantly higher classification accuracy for conditions like depression compared to single-modality models [31]. For treatment prediction, the combination of fMRI's spatial precision with EEG's temporal resolution creates complementary information that enhances prediction accuracy for antidepressant outcomes [35]. In cognitive load assessment, different modalities show specificity for various load types—while eye movements predict all three types of cognitive load, HR/HRV measures specifically predict extraneous and germane load [34].
Future Directions and Clinical Translation
The field of multimodal data fusion in VR-based mental health assessment is rapidly evolving toward more sophisticated analytical approaches and broader clinical applications. Emerging trends include N-way multimodal fusion techniques that can simultaneously integrate more than two data modalities, deep learning approaches that automatically learn optimal feature representations from raw data, and increased focus on clinical translation of validated biomarkers into routine practice [32]. The integration of artificial intelligence with VR therapies, such as virtual therapists voiced by real people or AI-driven digital therapists, represents another promising direction for increasing accessibility to mental health interventions [36].
Significant challenges remain in standardizing protocols across research sites, ensuring reproducibility of findings, and addressing the computational demands of processing high-dimensional multimodal data. Furthermore, the ethical implementation of these technologies requires careful consideration of privacy concerns, algorithm transparency, and equitable access. Nevertheless, the compelling evidence from current research suggests that multimodal fusion of eye-tracking, EEG, HRV, and motion data within immersive VR environments will play an increasingly important role in establishing objectively validated biomarkers for mental disorders, ultimately advancing toward more personalized and effective mental healthcare.
The validation of virtual reality (VR) biomarkers for mental disorder research represents a frontier in computational psychiatry, demanding robust machine learning (ML) frameworks for pattern recognition. This guide objectively compares the performance of ML models in classifying Major Depressive Disorder (MDD) and Mild Cognitive Impairment (MCI), two conditions with overlapping symptomatology yet distinct underlying pathologies. While direct comparative studies on MDD and MCI are emerging, foundational research in Alzheimer's disease (AD) and MCI classification provides established methodologies and performance benchmarks relevant to this domain. ML models excel at identifying subtle patterns in complex, high-dimensional data, making them particularly suited for distinguishing between neurological and psychiatric conditions based on digital biomarkers [37] [38]. The integration of VR-based assessments—which can quantify behavioral markers such as movement, gaze patterns, and reaction times—generates rich datasets amenable to these analytical approaches [39]. This guide synthesizes experimental data and methodologies from peer-reviewed literature to compare the performance of leading ML algorithms, detail their experimental protocols, and provide resources for researchers and drug development professionals working to validate digital biomarkers for mental disorders.
Performance Comparison of Machine Learning Models
Machine learning models demonstrate varying capabilities in classifying cognitive and mental health disorders, with performance heavily dependent on data modality, feature selection, and model architecture. The tables below summarize quantitative performance metrics for models tackling classification tasks relevant to MDD and MCI.
Table 1: Performance of Traditional ML Models on Neurocognitive Classification Tasks
| Model | Task | Accuracy | F1-Score | Key Strengths | Reference |
|---|---|---|---|---|---|
| Random Forest (RF) | NC vs AD | 97.8% | 97.6% | Robust, balanced precision/recall, handles high-dimensional data | [40] |
| Support Vector Machine (SVM) | Multiclass (NC, MCI, AD) | 85.1% | 90.7% | High performance on selected features, effective in complex feature spaces | [40] |
| Logistic Regression (LR) | AD Prediction | ~96% | N/A | Strong baseline predictor, highly interpretable | [41] |
| XGBoost | Predictive Biomarker Identification | LOOCV Accuracy: 0.7-0.96 | N/A | Superior accuracy for ranking biomarker candidates | [42] |
Table 2: Performance of Advanced AI Models on Broader Biomarker and Classification Tasks
| Model / Approach | Application Domain | Key Metric / AUC | Key Strengths | Reference |
|---|---|---|---|---|
| Deep Learning (CNN) | Medical Image Analysis (AD) | N/A | Automatically extracts hierarchical features from images (MRI, PET) | [37] |
| Hybrid Models (CNN+RNN) | Time-series MRI Data | N/A | Captures spatial and temporal patterns for disease progression | [37] |
| AI for Digital Biomarkers | MCI Detection | Avg. AUC: 0.821 | Analyzes motor activity, eye tracking, speech | [38] |
| Vision Transformer (ViT) | Image Classification | N/A | Applies self-attention to image patches, identifies long-range dependencies | [37] |
Detailed Experimental Protocols and Methodologies
The high performance of ML models is contingent on rigorous experimental protocols. The following section details the methodologies commonly employed in studies that achieve state-of-the-art results.
Data Acquisition and Preprocessing
The foundation of any robust ML model is high-quality, well-curated data. Research in this field typically relies on large, publicly available datasets.
- Dataset Sourcing: Studies often use datasets like the Open Access Series of Imaging Studies (OASIS) or the National Alzheimer's Coordinating Center (NACC) dataset. One study utilized the NACC dataset, comprising 169,408 records and 1,024 features spanning demographic, clinical, and neuropsychological test data [40].
- Data Preprocessing: This involves several critical steps:
- Feature Reduction: To combat the "curse of dimensionality," techniques like feature selection are applied to reduce the initial feature set to the most clinically relevant variables, improving model generalizability and performance [40].
- Data Splitting: Data is typically partitioned into training, validation, and test sets to ensure unbiased evaluation of the model's performance on unseen data [41].
Model Training and Validation
A systematic approach to model training and validation is crucial for generating reliable, clinically applicable results.
- Model Selection and Training: Researchers often compare a suite of models, including Random Forest (RF), Support Vector Machine (SVM), k-Nearest Neighbors (KNN), and others. Models are trained on the preprocessed training set, with hyperparameters tuned via cross-validation [41] [40].
- Validation Techniques: Robust validation is key. Methods include:
- k-Fold Cross-Validation: The data is split into k subsets; the model is trained on k-1 folds and validated on the remaining fold, repeated k times.
- Leave-One-Out Cross-Validation (LOOCV): A special case of k-fold where k equals the number of samples, providing a nearly unbiased estimate but at high computational cost [42].
- External Validation: The gold standard is testing the final model on a completely independent, external dataset. However, this is underutilized, with one review noting only 2 of 86 AI models for digital biomarkers incorporated external validation [38].
The Role of Explainable AI (XAI)
For clinical adoption, model predictions must be interpretable. Explainable AI techniques are used to uncover the "black box" nature of complex models.
- SHAP (SHapley Additive exPlanations): This method quantifies the contribution of each feature to an individual prediction, providing both local and global interpretability. For instance, it can reveal that factors like MEMORY, JUDGMENT, and ORIENT are the most significant in determining AD risk [40].
- Rule-Extraction Algorithms: Methods like SIRUS (Stable and Interpretable Rule Set) or Class Association Rule (CAR) mining generate human-understandable "if-then" rules that elucidate the inter-relationships between key clinical factors involved in disease development [40].
Figure 1: End-to-end machine learning workflow for MDD and MCI classification, showing the pipeline from raw data to clinical insight.
Signaling Pathways and Logical Frameworks
Understanding the logical relationship between data sources, computational models, and clinical validation is key to building effective diagnostic tools.
A Multimodal Data Integration Framework
Effective classification of MDD and MCI often requires integrating diverse data types to capture the full complexity of the disorders.
- Structural Data: MRI provides detailed information on brain atrophy, where a 3-5% annual reduction in brain volume is a key indicator of AD progression, with the hippocampus showing up to 10-15% annual shrinkage [37].
- Functional Data: PET scans offer metabolic and functional insights, capturing changes in brain activity [37].
- Digital Biomarkers: VR and other digital devices provide objective, quantifiable data on behavior, including gait parameters, eye movement, and speech features, enabling real-world monitoring [38].
- Clinical & Genetic Data: Standard neuropsychological test results (e.g., CDR scores) and genetic risk factors provide additional layers of information for the model [40].
Figure 2: A multimodal data fusion framework for MDD and MCI classification, integrating diverse data sources for a holistic model.
This section catalogs key computational tools, datasets, and methodologies that form the backbone of ML research for MDD and MCI classification.
Table 3: Key Research Reagent Solutions for ML-Driven Classification
| Tool / Resource | Type | Function / Application | Relevance to MDD/MCI |
|---|---|---|---|
| OASIS Datasets | Neuroimaging Dataset | Provides MRI data, clinical, and demographic information for model training and validation. | Foundational dataset for benchmarking model performance on cognitive impairment tasks [41]. |
| NACC Dataset | Clinical Dataset | Large-scale dataset with detailed longitudinal clinical data for ~170k subjects. | Enables training of models on a wide array of clinical and cognitive features [40]. |
| SHAP (SHapley Additive exPlanations) | Explainable AI Library | Explains output of any ML model, quantifying feature importance for individual predictions. | Critical for interpreting model decisions and identifying key diagnostic features for clinicians [40]. |
| SIRUS Algorithm | Rule-Extraction Tool | Extracts stable, interpretable decision rules from random forest-like models. | Generates human-understandable "if-then" rules for clinical decision support [40]. |
| VR Eye Tracking & Motion Sensors | Digital Biomarker Hardware | Captures objective behavioral data (gaze, posture, movement) in controlled virtual environments. | Provides novel biomarkers for differentiating MDD (psychomotor slowing) from MCI (visuospatial deficits) [39] [38]. |
| Random Forest / XGBoost | Machine Learning Algorithm | Powerful, ensemble-based classifiers for structured/tabular data. | Top-performing models for classification tasks using clinical and biomarker data [42] [41] [40]. |
| Convolutional Neural Network (CNN) | Deep Learning Model | Specialized for image data; automatically learns hierarchical features from raw inputs. | Standard for analyzing structural neuroimaging data (MRI, PET) to identify atrophy patterns [37]. |
The integration of virtual reality (VR) in clinical research represents a paradigm shift from traditional, subjective endpoints towards dynamic, objective, and quantitative assessment. Framed within a broader thesis on validating VR biomarkers for mental disorders research, this guide explores how VR-based metrics are refining two cornerstone processes in clinical trials: patient stratification and measurement of intervention efficacy. The inherent capabilities of VR—creating controlled, repeatable, and immersive environments—enable the collection of rich behavioral and physiological data. These data streams serve as digital biomarkers, providing tools to identify more homogeneous patient subgroups and to detect nuanced, clinically meaningful responses to interventions with greater sensitivity than conventional scales [43] [44]. This objective comparison details how these technologies perform against established alternatives, providing researchers and drug development professionals with the experimental data and methodologies needed for informed adoption.
Comparative Efficacy: VR-Based Interventions vs. Standard Protocols
Evidence from recent clinical studies demonstrates the therapeutic potential of VR, though its performance against gold-standard treatments varies. The following tables summarize quantitative findings across different mental health conditions, highlighting where VR shows superiority, equivalence, or areas for development.
Table 1: Comparative Efficacy of VR-Based Interventions for Mental Health Conditions
| Condition | VR Intervention | Comparator | Key Efficacy Outcomes | Experimental Findings |
|---|---|---|---|---|
| Paranoia in Schizophrenia Spectrum Disorders [45] | VR-based Cognitive Behavioral Therapy for paranoia (VR-CBTp) | Standard CBTp (Gold Standard) | Primary Outcome: Ideas of Persecution (GPTS Scale).Secondary: Social self-reference, social anxiety, safety behaviors. | Non-significant superiority for VR-CBTp (Effect Estimate: +2%; 95% CI: -11% to +17%; Cohen's d = 0.04; P=0.77). VR-CBTp was non-inferior to the established gold standard. |
| Anxiety & Specific Phobias [44] | VR-based Exposure Therapy | In Vivo Exposure / Waitlist | Reduction in fear and anxiety symptoms measured via self-report questionnaires and physiological biomarkers. | Superior to waitlist controls, and often as effective as in vivo exposure. High patient preference for VR over in vivo (76% in one study). |
| Depression [46] | VR-based Acceptance and Commitment Therapy (ACT) | N/A (Pilot Study) | Therapeutic engagement, symptom reduction via clinical scales. | Pilot studies show feasibility and promising effects on engagement and emotional immersion. Larger-scale RCTs are needed for efficacy validation. |
| Psychological Distress in Oncology [47] | VR Relaxation Intervention | Standard Care (Single-Arm Trial) | Feasibility, distress, and anxiety symptoms (NCCN Distress Thermometer). | Established feasibility in a high-symptom burden population. Preliminary efficacy data supports its use for "scanxiety." |
Table 2: Performance of Biomarkers in VR-Based Exposure Therapy for Anxiety [44]
| Biomarker | Utility in Within-Session Change | Utility in Between-Session Change | Synchrony with Self-Report Questionnaires | Current Readiness for Clinical Trials |
|---|---|---|---|---|
| Heart Rate (HR) | Moderate (Positive in ~75% of instances) | Moderate (Positive in ~60% of instances) | Moderate | Moderate - Most consistently useful biomarker. |
| Skin Conductance Level (SCL) | Inconclusive | Inconclusive | High for group differences (~87%) | Low to Moderate - Good for group-level analysis. |
| Heart Rate Variability (HRV) | Limited Data | Limited Data | Inconclusive | Low - Requires more standardized research. |
| Respiratory Rate | Limited Data | Limited Data | Inconclusive | Low - Insufficient evidence. |
Experimental Protocols: Methodologies for VR Biomarker Research
Protocol for a Randomized Controlled Trial (RCT): VR-CBT for Paranoia
The "FaceYourFears" RCT provides a robust methodology for comparing a novel VR intervention against a gold-standard therapy [45].
- Study Design: Assessor-masked, randomized, parallel-group superiority trial.
- Participants: 254 adults with schizophrenia spectrum disorders and paranoia (Green Paranoid Thoughts Scale total score ≥40).
- Intervention Groups:
- Experimental Group: Received 10 sessions of VR-CBTp. Therapists used customizable VR environments to gradually expose patients to social situations that triggered paranoid anxiety, allowing for real-time cognitive restructuring and behavioral experiments [45].
- Active Comparator Group: Received 10 sessions of standard, symptom-specific CBTp.
- Outcome Measures:
- Primary Endpoint: Ideas of Persecution subscale of the Green Paranoid Thoughts Scale at treatment cessation.
- Secondary Endpoints: Ideas of social self-reference, social anxiety, safety behaviors, emotion recognition, and psychosocial functioning, assessed at baseline, endpoint, and 6-month follow-up.
- Key Findings: The trial established that VR-CBTp was not statistically superior to standard CBTp, but it was non-inferior with a high completion rate (81%), demonstrating its viability as an effective therapeutic modality [45].
The workflow below illustrates the participant journey and key assessment points in this RCT.
Protocol for a Feasibility Study: VR for Distress in Brain Tumor Patients
This phase 2 single-arm trial outlines a method for testing VR feasibility in a medically vulnerable population [47].
- Study Design: Single-arm, uncontrolled, pre-post test feasibility trial conducted remotely via telehealth.
- Participants: 120 primary brain tumor (PBT) patients with upcoming MRI scans, experiencing "scanxiety."
- Intervention: A 5-minute, remotely supervised VR relaxation session prior to MRI/clinic appointment. Patients could then use the VR system ad libitum for one month.
- Data Collection:
- Feasibility Metrics: Proportion of eligible patients who consent, complete the intervention, and have complete data; incidence of adverse effects; patient satisfaction.
- Preliminary Efficacy: Patient-reported outcomes (PROs) for distress and anxiety collected at baseline, immediately post-VR, at 1 week, and 4 weeks.
- Exploratory Biomarkers: Optional collection of salivary cortisol, DHEA-S, and alpha-amylase to correlate with PROs [47].
- Key Findings: The study was designed to establish feasibility and inform the design of future multicenter RCTs for oncology populations [47].
Analysis of VR Biomarkers: From Physiology to Behavior
Physiological Biomarkers in Anxiety Research
A systematic review of 27 studies (n=1046) provides the best available evidence on the utility of physiological biomarkers in VR-based exposure for anxiety [44].
- Heart Rate (HR): The most consistently useful biomarker. Evidence tentatively supports its use for detecting changes in anxiety within a single session (successful in ~75% of instances) and between sessions (successful in ~60% of instances). It shows moderate synchrony with self-reported anxiety levels [44].
- Skin Conductance Level (SCL): While less consistent for tracking change over time, SCL shows high synchrony with questionnaire data for distinguishing between groups (e.g., patients vs. controls; 87% of instances). This makes it valuable for stratifying patients based on physiological arousal [44].
- Conclusion: The review concludes that while promising, biomarkers cannot yet reliably distinguish differences in self-reported symptoms of anxiety in VR-based exposure treatments with high confidence. They are best used as complementary objective measures alongside PROs [44].
Neural and Behavioral Biomarkers
Beyond physiology, VR enables the capture of complex neural and behavioral signatures.
- EEG Biomarkers of Embodiment: Research into the Sense of Embodiment (SoE) in VR has identified potential electroencephalography (EEG) biomarkers. Studies show a significant increase in Beta and Gamma power over the occipital lobe during a virtual embodiment illusion, suggesting these frequency bands as candidates for objectively measuring this complex subjective experience [48].
- Digital Phenotyping: Smartphones and VR can generate behavioral metrics (e.g., movement patterns, reaction times, gaze tracking) that serve as digital phenotypes. In mental health, relapse detection in schizophrenia and symptom prediction in mood disorders have shown promising pilot results. However, the field lacks standardization in data processing, limiting generalizability [43].
The diagram below summarizes the relationship between VR stimuli, the resulting biomarker classes, and their clinical applications in trials.
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing VR biomarker research requires a suite of specialized hardware and software solutions. The table below details key components and their functions based on the cited experimental protocols.
Table 3: Essential Research Reagents for VR Biomarker Clinical Trials
| Tool Category | Specific Examples / Features | Primary Function in Research | Supporting Context |
|---|---|---|---|
| Immersive VR Hardware | Head-Mounted Display (HMD) with tracking sensors (e.g., Oculus Quest, HTC Vive). | Creates immersive 3D environments; tracks user movement and rotation in real-time for realistic interaction and data collection. | [47] [46] |
| Biometric Sensor Suites | ECG for Heart Rate (HR), Electrodermal Activity for Skin Conductance Level (SCL), EEG systems. | Provides objective, continuous physiological data (biomarkers) synchronized with VR events to quantify arousal and cognitive state. | [48] [44] |
| Software & VR Content | Customizable VR environments for exposure (e.g., crowded virtual spaces); Gamified therapeutic tasks. | Presents standardized, controlled stimuli for behavioral activation; enhances user engagement and adherence through interactive design. | [45] [46] |
| Data Integration Platforms | Systems for synchronizing biometric data streams, behavioral logging (gaze, movement), and patient-reported outcomes (PROs). | Enables multi-modal data analysis, correlating physiological, behavioral, and subjective measures for comprehensive biomarker identification. | [43] [48] |
Experimental Comparison of Digital Screening and Intervention Tools for Depression
This section objectively compares the performance of various technology-assisted methods for diagnosing and treating depression, focusing on a novel Virtual Reality (VR) framework for adolescent Major Depressive Disorder (MDD) screening.
Table 1: Performance Comparison of Digital Tools for Depression Management
| Methodology | Study Population | Key Metrics & Performance | Reported Advantages | Key Limitations |
|---|---|---|---|---|
| VR-based Multimodal Screening (SVM Model) [31] [1] [49] | 51 adolescents with MDD, 64 healthy controls (HC) | Accuracy: 81.7%AUC: 0.921 [31] [1] | Objective biomarkers; Integrated, immersive assessment [31] | Requires specialized VR and biosensing hardware |
| Passive Sensing (LightGBM Model) [50] | 28 college students | F1-score: 0.744Cohen κ: 0.474 [50] | Low-burden, real-world data collection [50] | Lower performance metrics; Relies on user-owned device consistency |
| Transcranial Magnetic Stimulation (TMS) [51] | 41 adolescents with MDD | Improved CDRS-R scores; Biomarker (ICF) guided dosing effective for 1-Hz TMS [51] | Non-pharmacological intervention; Biomarker-informed protocol [51] | Specialized medical equipment and clinical setting required |
| VR-based Cognitive Behavior Therapy [52] | 57 participants with MDD | Reduced depression scores; Significantly reduced suicidality [52] | Non-inferior to pharmacotherapy; Potential to reduce suicidality [52] | Explores treatment, not screening |
Detailed Experimental Protocols
VR-Based Multimodal Screening Framework
This protocol outlines the core methodology for the featured VR-based screening framework.
- Study Design and Participants: A case-control study was conducted involving 51 adolescents diagnosed with first-episode MDD and 64 healthy controls. All MDD diagnoses were confirmed according to DSM-5 criteria [31] [1].
- VR Task and Data Collection: Participants engaged in a 10-minute immersive VR emotional task involving interactive dialogues with an AI agent named "Xuyu" in a standardized virtual environment (a magical forest by a lakeside). During the task, the following physiological data were collected synchronously using a BIOPAC MP160 system and a See A8 portable telemetric ophthalmoscope [31] [1]:
- Electroencephalography (EEG): Brain activity data.
- Eye-Tracking (ET): Ocular motility data.
- Electrocardiogram (ECG): Data for deriving Heart Rate Variability (HRV).
- Data Analysis and Modeling: Key physiological differences between groups were identified via statistical analysis. A Support Vector Machine (SVM) model was then trained to classify MDD status based on the selected multimodal features [31] [1].
Passive Sensing with Machine Learning
This protocol describes an alternative approach using passive data collection from wearables and smartphones.
- Participants and Sensing: A diverse sample of 28 undergraduate students wore two devices (an Oura ring for sleep/physiology and a Samsung smartwatch for physiology/movement) and installed the AWARE software on their smartphones to collect passive data (e.g., screen time, call logs). Data were collected over 19-22 weeks [50].
- Outcome and Modeling: Participants completed the self-report Patient Health Questionnaire-9 (PHQ-9) weekly to measure depressive symptoms. A Light Gradient Boosting Machine (LightGBM) model was trained to classify participants as depressed or non-depressed based entirely on the passively sensed features [50].
Experimental Workflow and Biomarker Pathways
The following diagram illustrates the integrated workflow of the VR-based multimodal screening framework, from data acquisition to diagnostic classification.
VR Multimodal Screening Workflow
Biomarker-to-Diagnosis Signaling Pathway
This diagram maps the specific physiological biomarkers identified in the VR framework to their functional interpretations and their contribution to the final diagnostic output.
Biomarker Interpretation Pathway
Research Reagent Solutions
This table details the key materials and tools essential for implementing the featured VR-based multimodal screening framework.
Table 2: Essential Research Reagents and Materials for VR Biomarker Research
| Item Name | Function/Application | Specific Example/Details |
|---|---|---|
| BIOPAC MP160 System | A data acquisition system used for recording synchronized physiological signals including EEG and ECG (for HRV) [31] [1]. | Used to capture high-fidelity EEG, ECG, and other biosignals in real-time during the VR task [31] [1]. |
| See A8 Portable Telemetric Ophthalmoscope | A device for capturing eye-tracking data, which provides metrics on gaze, saccades, and fixations [31] [1]. | Employed to collect ocular motility data (saccade count, fixation duration) as behavioral biomarkers [31] [1]. |
| Virtual Reality Environment | The immersive, standardized context for presenting emotional stimuli and collecting user interaction data. | A custom-built magical forest lakeside scene using the A-Frame framework, integrated with an AI agent for dialogue [31] [1]. |
| Support Vector Machine (SVM) | A machine learning algorithm used for classification tasks, such as distinguishing between MDD and healthy individuals based on features [31] [1]. | The classifier trained on extracted EEG, ET, and HRV features, achieving an AUC of 0.921 [31] [1]. |
| Center for Epidemiologic Studies Depression Scale (CES-D) | A validated self-report scale used to assess depression severity and correlate with the identified physiological biomarkers [31] [1]. | The Chinese version was used to validate the association between physiological features (e.g., theta/beta ratio) and depression severity [31] [1]. |
Navigating the Roadblocks: Technical, Clinical, and User-Centric Challenges in VR Biomarker Development
Virtual reality (VR) holds transformative potential for mental health research and therapeutic interventions, offering controlled, immersive environments for exposure therapy, neurophysiological monitoring, and biomarker discovery [43] [7]. However, its adoption in clinical neuroscience and pharmaceutical development faces significant technical barriers. Cybersickness can disrupt experimental protocols and participant engagement [53] [54]. Hardware limitations constrain ecological validity and accessibility [55] [56], while the absence of data standards impedes reproducibility and the validation of digital biomarkers [43] [57]. This guide objectively compares current solutions and presents experimental data to help researchers select appropriate methodologies for integrating VR into mental disorders research.
Cybersickness: Measurement, Impact, and Mitigation
Cybersickness—characterized by symptoms like nausea, disorientation, and oculomotor discomfort—remains a primary barrier to reliable VR research. The sensory conflict theory suggests these symptoms arise from discrepancies between visual and vestibular system inputs [53] [54]. The table below summarizes quantitative findings from recent studies on cybersickness incidence and measurement.
Table 1: Measured Cybersickness Effects and Methodologies Across VR Studies
| Study Context | Primary Measurement Tool | Key Symptom Increases (Pre- to Post-VR) | Sample Size & Population | Reported Impact on Outcomes |
|---|---|---|---|---|
| Seated VR Walk (Venice Canals) [53] | Virtual Reality Sickness Questionnaire (VRSQ) | Eye strain (+0.66), General discomfort (+0.6), Headache (+0.43) | 30 healthy adults (age 20-25) | High flow state maintained (3.47-3.70/5) despite symptoms. |
| Therapeutic VR Applications [54] | Simulator Sickness Questionnaire (SSQ) | Disorientation (most frequent), Nausea, Oculomotor disturbances | 416 patients across 10 studies (mean age 24.54) | More frequent with head-mounted displays vs. desktop systems. |
| Game Session (VR vs. 2D) [56] | EEG Spectral Power & Theta/Beta Ratio | Theta/beta ratio indicated lower visual arousal in VR group in first session. | 28 adults (26-40 years) | VR group outperformed 2D in initial session; different neurophysiological engagement. |
Experimental Protocols for Cybersickness Assessment
Protocol Example: Evaluating a Seated VR Walk [53]
- Objective: To assess cybersickness symptoms and spatial presence during a passive VR experience for therapeutic potential.
- VR Setup: Meta Quest 2 headset displaying a 15-minute, 360° video walkthrough of the Venice Canals. Participants sat on a rotating chair in a silent room.
- Measures:
- Cybersickness: Virtual Reality Sickness Questionnaire (VRSQ) administered before and after the experience.
- Psychological Impact: International Positive and Negative Affect Schedule-Short Form (I-PANAS-SF), Spatial Presence Experience Scale (SPES), and Flow State Scale (FSS) post-experience.
- Key Findings: Despite statistically significant increases in eye strain, discomfort, and headache, participants reported a high flow state and a predominance of positive emotions, indicating the experience's overall benefit was not negated by cybersickness.
Hardware Limitations: Immersive vs. Standard Display
The choice between immersive head-mounted displays (HMDs) and standard 2D monitors involves trade-offs between ecological validity and practical constraints like cost, accessibility, and cybersickness risk.
Table 2: Performance Comparison: VR Head-Mounted Display vs. Standard 2D Monitor
| Performance Metric | VR HMD Group Findings [56] | Standard 2D Monitor Group Findings [56] | Interpretation & Implications |
|---|---|---|---|
| Behavioral Performance (DMTS Task) | Outperformed 2D group in the first session, maintained performance thereafter. | Increased performance across each session, eventually matching VR group in the third session. | VR may accelerate initial learning curve or engagement, but 2D can achieve similar performance with repeated exposure. |
| Neurophysiological Engagement (EEG) | Stronger and more synchronized neuronal activity in delta, theta, and gamma bands in the first session. | Less synchronized neuronal activity compared to the VR group in the first session. | Immersive VR elicits a different, potentially more intense, neurophysiological response, which is crucial for biomarker research. |
| Impact of Visual Arousal | Lower theta/beta2 ratio in parietal electrodes, suggesting less impact from visual arousals. | Higher ratio indicates greater impact from visual arousals. | VR may provide a more stable neural environment for assessment by dampening extraneous visual distractions. |
Experimental Protocol: VR vs. 2D Cognitive Training
Protocol Example: Three-Session DMTS Task Comparison [56]
- Objective: To compare cognitive performance and neurophysiological correlates between VR and 2D display environments across multiple sessions.
- Setup:
- VR Group: Oculus Rift CV1 goggles with a 270° field of view. Task was set in a detailed spaceship cabin.
- 2D Group: Standard LCD monitor with an approximate 17° field of view.
- Task: Participants performed an adapted Delay Match-To-Sample (DMTS) task, a working memory game, over three 25-minute sessions spaced days apart. EEG was recorded throughout.
- Measures: Behavioral performance (accuracy, reaction time) and EEG metrics (spectral power, phase locking value, spectral entropy).
- Key Findings: The VR environment provided an initial advantage in performance and distinct neural engagement, underscoring its utility for creating engaging, ecologically valid research environments.
Data Standardization and Biomarker Validation
A significant hurdle in VR research is the lack of standardized data collection and processing protocols, which undermines the validation of VR-based biomarkers and the reproducibility of studies [43] [57]. Research highlights variability in how digital phenotyping data from smartphones and VR is processed, making cross-study comparisons difficult [43].
The field is advancing with the integration of real-time biophysiological monitoring to create closed-loop, adaptive VR systems. These systems use biomarkers like heart rate (HR), electrodermal activity (EDA), and electroencephalography (EEG) to dynamically adjust the virtual environment based on the user's affective state [57]. This approach represents a frontier in precision psychiatry but requires standardized biomarkers and algorithms to be fully validated and widely adopted.
Experimental Protocol: Real-Time Adaptive VR Exposure Therapy
Protocol Example: Biofeedback-Enhanced VR for Anxiety [57]
- Objective: To use real-time physiological data to modulate a VR exposure therapy session for generalized anxiety disorder.
- Setup: VR environment displayed via HMD with integrated physiological monitoring.
- Measures & Adaptation:
- Physiological Inputs: Heart rate (HR) and electrodermal activity (EDA) are monitored in real-time.
- Adaptive Logic: A software algorithm analyzes the biosensor data to categorize the participant's anxiety level. Based on this classification, the system dynamically adjusts the intensity of the anxiety-provoking stimuli in the VR environment (e.g., the number of virtual people in a social anxiety scenario).
- Key Findings: Studies using such closed-loop systems show they are technically feasible and offer promising personalization benefits, potentially enhancing engagement and preventing emotional overload [57].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials and Tools for VR Mental Health Research
| Item Name | Function/Application in Research | Exemplar Use Case |
|---|---|---|
| Meta Quest 2 / Oculus Rift CV1 | Consumer-grade HMD for delivering immersive VR environments. | Used in seated VR walks [53] and cognitive task comparisons [56]. |
| Simulator Sickness Questionnaire (SSQ) | Standardized tool to quantify cybersickness symptoms. | Applied in systematic reviews of VR therapeutic applications [54]. |
| Virtual Reality Sickness Questionnaire (VRSQ) | Alternative to SSQ, designed specifically for VR contexts. | Measuring cybersickness in a seated VR immersion study [53]. |
| EEG with 21-electrode cap | Recording neurophysiological responses (e.g., spectral power, connectivity) during VR exposure. | Comparing neural engagement between VR and 2D displays [56]. |
| Electrodermal Activity (EDA) Sensor | Measuring sympathetic nervous system arousal via skin conductance. | Used as input for real-time adaptive VRET systems [57]. |
| Heart Rate (HR) Monitor | Tracking cardiac activity as a biomarker of emotional arousal and stress. | Integrated into biofeedback loops for adaptive VR interventions [57]. |
| I-PANAS-SF & Flow State Scale (FSS) | Assessing emotional response and optimal engagement states post-VR. | Evaluating the emotional impact of a virtual walk despite cybersickness [53]. |
Visualizing the Adaptive VR Research Workflow
The following diagram illustrates the logical flow and feedback loops in a real-time adaptive VR experiment for mental health research.
Real-Time Adaptive VR System with Biosensor Feedback
Overcoming the technical hurdles of cybersickness, hardware limitations, and data standardization is paramount for validating VR biomarkers in mental health research. Cybersickness is a prevalent issue but can be managed and measured with standardized tools like the VRSQ and SSQ, and its impact may not wholly negate therapeutic benefits [53] [54]. Hardware choices involve a critical trade-off; while HMDs offer superior ecological validity and can enhance initial engagement and neural responses, 2D setups remain viable for specific research questions [55] [56]. The most significant future advancement lies in standardizing data and leveraging real-time biophysiological markers to create adaptive, closed-loop VR systems. This approach promises a new generation of precise, individualized, and valid digital therapeutics for mental disorders [43] [57].
Virtual reality (VR) has emerged as a promising tool for mental health treatment, demonstrating effectiveness comparable to traditional in-vivo exposure therapy for conditions such as anxiety disorders, posttraumatic stress disorder (PTSD), and specific phobias [58] [59]. Despite robust evidence supporting its efficacy and technological advancements making VR more accessible, adoption in routine clinical practice remains remarkably low [58] [60]. A recent large-scale survey among Austrian clinical psychologists and psychotherapists revealed that only 10 out of 694 participants reported using therapeutic VR in their practice – a stark adoption rate of approximately 1.4% [58]. This clinical adoption paradox represents a critical implementation gap between VR's demonstrated potential and its real-world application, highlighting the urgent need to address the complex interplay of training deficits, methodological protocols, and therapist attitudes that hinder widespread integration into mental healthcare.
The validation of VR biomarkers for mental disorders research depends fundamentally on successful clinical implementation. Without therapist buy-in and standardized protocols, even the most promising digital biomarkers cannot be reliably collected or applied in real-world settings. This article examines the key barriers to VR adoption and presents evidence-based strategies to overcome them, focusing on the essential components of training, protocol development, and stakeholder engagement needed to advance the field.
Current State of VR Clinical Adoption and Research Quality
Documented Barriers to Clinical Implementation
Recent research has identified a complex constellation of barriers preventing therapists from adopting VR technology. A 2024 survey of 694 clinical psychologists and psychotherapists categorized these barriers into four primary themes, with notable differences between clinicians interested in VR and those with no interest [58]:
Table 1: Key Barriers to VR Adoption in Mental Health Practice
| Barrier Category | Specific Challenges | Prevalence Among Those Interested in VR | Prevalence Among Those Not Interested in VR |
|---|---|---|---|
| Professional Barriers | Lack of knowledge, training, time, personal reasons | Frequently cited | Less frequently cited |
| Financial Barriers | High costs, unfavorable cost-benefit ratio | Significant concern | Significant concern |
| Therapeutic Barriers | Concerns about "real" therapeutic relationship, clinical applicability | Commonly expressed | Primary concern: lack of perceived relevance/advantage |
| Technological Barriers | Immature technology, cybersickness, lack of equipment | Frequently mentioned | Less emphasized |
The same study found significant differences in interest toward therapeutic VR based on prior experience with the technology, employment status, professional training, and therapeutic orientation (with behavioral therapists showing more interest than psychodynamic, humanistic, or systemic therapists) [58]. Interestingly, aside from a small age effect, gender and professional experience did not significantly influence VR interest rates.
Methodological Challenges in VR Research
The clinical adoption of VR is further complicated by significant methodological limitations in the existing research literature. A comprehensive systematic review of 721 VR mental health studies revealed astonishing gaps in scientific robustness [60]:
Table 2: Comparison of Research Quality Metrics Between VR and General Mental Health Studies
| Research Quality Metric | VR Mental Health Studies | General Mental Health Studies |
|---|---|---|
| Randomization Rate | 44.4% | 86.4% |
| Blinding Implementation | 10.1% (2.2% double-blind) | 67.2% (45.6% double-blind) |
| Median Sample Size | 36 | 61-90 |
| Risk of Bias Composite Scores | >50% (significant limitations) | Lower overall risk |
These methodological deficiencies preclude firm conclusions about efficacy for many mental health conditions and contribute to clinician skepticism about VR's evidence base [60]. The field has been described as the "Wild West," with a focus on technical innovation rather than theoretical rationale and insufficient statistical power [60].
Strategies for Enhancing Clinical Adoption
Comprehensive Training and Support Systems
The knowledge and training gaps identified as primary barriers to VR adoption necessitate structured educational approaches. Successful implementation requires:
Interdisciplinary Training Programs: Developing curricula that bridge clinical expertise and technical knowledge, enabling mental health professionals to confidently operate VR systems while maintaining therapeutic integrity [61]. These programs should address both technical competencies (equipment operation, software navigation) and clinical adaptations (maintaining therapeutic alliance during immersion, integrating VR into treatment plans).
Peer Support and Lived Experience Integration: Incorporating peer research methods, where individuals with lived experience of mental health issues contribute to data collection and analysis, provides unique insights into patient perspectives and enhances treatment development [62]. This approach fosters more clinically relevant VR interventions and facilitates implementation.
Ongoing Technical Support: Establishing reliable support systems for troubleshooting technical issues is crucial for maintaining clinician confidence and preventing abandonment of VR technology due to frustration with operational challenges [61].
Standardized Protocols and Implementation Frameworks
The development and validation of practical protocols for VR implementation in psychological practice is essential for overcoming existing barriers [61]. A proposed four-stage framework includes:
Diagram 1: VR Implementation Framework
Equipment Selection: Considerations include immersion capabilities, space limitations, resource demands, and options for integration with other hardware [61]. Selection should be guided by clinical population needs rather than technological novelty.
Design and Development: Creating virtual environments requires interdisciplinary collaboration between clinicians, software developers, and end-users throughout development to ensure clinical relevance and usability [61].
Technology Integration: Combining VR with other assessment technologies (physiological monitoring, EEG, eye-tracking) enhances data collection but requires creative solutions as most commercial systems aren't designed for multi-technology combinations [61].
Clinical Implementation: Successful integration into healthcare systems depends on appropriateness, acceptability, and feasibility within specific clinical contexts [61]. This includes adapting to various settings from solo practices to community clinics and hospital wards.
Enhancing Technological Refinement and Personalization
Recent advances in VR platform sophistication demonstrate the importance of technological refinement for clinical adoption. A 2025 validation study comparing upgraded VR platforms found that technological improvements significantly enhanced user experience and sense of presence [63]. Key advancements included:
- Superior avatar realism (d = 0.574; p < 0.001)
- Enhanced voice realism (d = 1.035; p < 0.001)
- Improved lip synchronization (d = 0.693; p < 0.001)
- Heightened sense of presence (d = 0.520; p = 0.002)
- Better overall immersive experience (d = 0.756; p < 0.001)
These technological improvements were associated with increased participant engagement and potentially greater therapeutic effectiveness, addressing clinician concerns about VR's ability to facilitate genuine therapeutic experiences [63].
Addressing Financial and Systemic Barriers
The high costs of VR equipment and development present significant implementation barriers, particularly for individual practitioners and smaller clinics [58]. Strategic approaches to overcome these barriers include:
Multicenter Collaborations: Pooling resources across institutions enables more efficient sample size generation, enhanced reproducibility, and generalizability of findings while distributing financial burdens [60]. The successful completion of one of the few clinical VR multicenter studies to date on the Secret Garden paradigm demonstrates the feasibility of this approach [60].
Hybrid Funding Models: Developing funding instruments that support both technical development and clinical validation phases, addressing the current bias toward innovation at the expense of confirmatory trials [60].
Platform Standardization and Open-Access Resources: Creating shared, standardized VR applications reduces development costs and facilitates implementation across diverse clinical settings [60]. Recent initiatives to develop easy-to-use platforms that allow VR application generation without programming knowledge represent promising directions [60].
Implications for VR Biomarker Validation
The successful implementation of VR in clinical practice has profound implications for validating digital biomarkers in mental disorders research. Several key considerations emerge:
Multi-Modal Biomarker Integration
VR enables the simultaneous collection of multiple data streams during ecologically valid experiences, creating opportunities for comprehensive biomarker development [44]. Current evidence suggests:
- Heart rate shows promise for identifying anxiety changes within (75% of instances) and between sessions (60% of instances) [44]
- Skin conductance level demonstrates high synchrony with questionnaire results for between-group differences (87% of instances) [44]
- Behavioral metrics (eye-tracking, movement patterns, interaction decisions) provide additional objective measures of symptomatology [59]
However, biomarkers cannot yet reliably distinguish differences in self-reported anxiety symptoms in VR-based exposure treatments, indicating the need for further refinement of multi-modal assessment approaches [44].
Methodological Considerations for Biomarker Validation
Diagram 2: VR Biomarker Validation Workflow
The validation of VR-derived biomarkers requires addressing several methodological challenges:
Standardization of VR Environments: Inconsistent stimulus presentation across studies compromises biomarker reliability [16]. Developing validated, standardized VR paradigms for specific clinical populations is essential for generating comparable data across research sites.
Contextual Biomarker Interpretation: Understanding the relationship between biomarker modalities provides crucial situational context [64]. For example, interpreting heart rate reactivity requires simultaneous assessment of physical movement to distinguish anxiety from other causes of cardiovascular activation.
Representative Sampling: Historically, mental health research has suffered from limited generalizability due to unrepresentative samples [64]. VR studies must intentionally include historically underrepresented groups to ensure biomarkers generalize beyond narrow demographic profiles.
Table 3: Essential Research Reagent Solutions for VR Biomarker Validation
| Resource Category | Specific Tools/Platforms | Primary Function | Key Considerations |
|---|---|---|---|
| VR Hardware | HMDs (Oculus Rift, HTC Vive), CAVE systems | Create immersive environments | Balance between immersion and practicality; consider cybersickness mitigation |
| Biometric Sensors | ECG sensors, GSR devices, eye-tracking, motion capture | Capture physiological and behavioral data | Integration capabilities with VR systems; sampling rates; data synchronization |
| Software Platforms | Unity, Unreal Engine, specialized VR therapy platforms | Environment development and customization | Flexibility for clinical adaptation; compatibility with assessment tools |
| Data Integration Systems | LabStreamingLayer, custom API solutions | Synchronize multi-modal data streams | Handling temporal alignment across different data sources and formats |
| Analysis Tools | MATLAB, Python, R with specialized libraries | Process and analyze biomarker data | Development of standardized analytical pipelines for cross-study comparison |
The clinical adoption of VR in mental healthcare represents a complex challenge requiring coordinated efforts across multiple domains. Successful implementation depends on addressing fundamental barriers including knowledge gaps, financial constraints, methodological limitations in research, and technological refinement. The validation of VR-based biomarkers for mental disorders research is inextricably linked to these implementation challenges – without robust, standardized clinical protocols and therapist engagement, even the most promising digital biomarkers cannot be reliably collected or applied in real-world settings.
Future directions should prioritize the development of comprehensive training programs, standardized implementation protocols, enhanced technological platforms with greater personalization capabilities, and sustainable funding models that support both development and validation phases. Multicenter collaborations and increased involvement of end-users throughout the development process will be essential for creating VR interventions that are both clinically effective and practically implementable.
As the field advances, the parallel development of implementation frameworks and biomarker validation protocols will create a virtuous cycle – improved clinical adoption generates higher-quality data for biomarker refinement, which in turn enhances treatment personalization and effectiveness. By systematically addressing the critical needs for training, protocols, and therapist buy-in, the mental health field can realize the full potential of VR as both a therapeutic tool and a platform for advancing our understanding of mental disorders through digital biomarker discovery.
Within the advancing field of digital mental health, virtual reality (VR) is being rigorously validated as a tool for identifying digital biomarkers in mental disorders research. For researchers and clinicians, the primary focus has often been on clinical efficacy; however, the translation of these findings into reliable, scalable biomarkers is highly dependent on overcoming key patient-centered barriers. Autonomy, or the patient's control over the therapeutic experience; personalization, the tailoring of interventions to individual needs; and physical comfort, the mitigation of adverse effects like cybersickness, are not merely usability concerns but are fundamental to data integrity and biomarker reliability [10] [7]. This guide provides a comparative analysis of how contemporary VR frameworks and protocols are addressing these barriers, with direct implications for the consistency and validity of collected biometric data.
Comparative Analysis of VR Therapeutic Approaches
The table below summarizes quantitative data and design features from recent studies, illustrating how different VR modalities address patient-centered barriers and facilitate biomarker research [10] [46] [65].
Table 1: Comparison of VR-Based Therapeutic Approaches for Mental Health
| VR Intervention Type | Target Condition(s) | Reported Effect Size / Key Metric | Autonomy & Personalization Features | Physical Comfort & Tolerability Data |
|---|---|---|---|---|
| VR Exposure Therapy (VRET) [10] [66] | Specific phobias, PTSD, Social Anxiety | Large effect sizes (Cohen's d ~0.8) for phobias [66]; Moderate-to-large for PTSD (d ~0.6) [66] | Gradual, patient-controlled exposure hierarchy; customizable virtual scenarios [10] | Safe, confidential setting reduces initial anxiety; cybersickness noted as a challenge requiring management [10] |
| VR-based CBT [43] [65] | Performance Anxiety, Depression, Psychosis | Superior to waitlist controls; generally as effective as traditional CBT [43] | Interactive tasks; real-time biofeedback potential [46] | Immersive nature can enhance engagement, potentially offsetting discomfort [7] |
| VR-based ACT & DTx [46] | Depression | Structured, evidence-based protocol; evaluation metrics integrated for personalization [46] | Modularized sessions (6-12 mins); gamification and multimodal arts for engagement [46] | Shorter session durations may improve tolerability; structured design minimizes unpredictability |
| VR-based Mindfulness [67] | Stress, Anxiety, Depression | Meta-analyses show higher engagement and lower dropout vs. traditional methods [67] | Personalized, immersive environments (e.g., virtual beach) enhance focus and presence [67] | High immersion may deepen relaxation response, though formal comfort metrics are needed |
| VR Multimodal Assessment [1] | Adolescent Major Depressive Disorder (MDD) | Diagnostic accuracy of 81.7% (AUC 0.921) using SVM classifier [1] | Dynamic dialogue with AI agent ("Xuyu") within a standardized, immersive scenario [1] | Fixed 10-minute duration; controlled, consistent environment to ensure data reliability [1] |
Experimental Protocols for Biomarker Research
Protocol 1: VR Multimodal Biomarker Identification for Adolescent MDD
This case-control study protocol exemplifies the integration of patient-centered design with rigorous biomarker collection [1].
- Objective: To identify robust physiological biomarkers for Major Depressive Disorder (MDD) in adolescents using a synchronized, VR-based multimodal sensing platform.
- Population: 51 adolescents with first-episode MDD and 64 healthy controls [1].
- VR Task: A 10-minute immersive interaction in a "magical forest" with an AI agent ("Xuyu") that initiates structured conversations about personal worries and hopes [1].
- Data Acquisition & Biomarkers:
- Electroencephalography (EEG): Measured frontal alpha asymmetry and the theta/beta ratio, which was significantly associated with depression severity [1].
- Eye-Tracking (ET): Tracked saccade counts and fixation durations; adolescents with MDD showed reduced saccades and longer fixations [1].
- Heart Rate Variability (HRV): Collected ECG data; the LF/HF ratio was elevated in the MDD group and correlated with symptom severity [1].
- Personalization & Comfort: The VR environment was standardized to ensure experimental control and reproducibility, while the interactive AI agent provided a consistent yet engaging context for emotional expression, balancing ecological validity with data reliability [1].
Protocol 2: Structured Framework for VR Digital Therapeutics (DTx) Development
This development protocol provides a methodological roadmap for creating valid and engaging VR interventions, which is crucial for generating consistent biomarker data across sessions and individuals [46].
- Objective: To establish a standardized, five-phase methodology for translating evidence-based psychotherapy (Acceptance and Commitment Therapy) into an interactive VR-based Digital Therapeutic (DTx) for depression [46].
- Development Phases:
- Preliminary Research: Establishing the evidence base and conceptual roadmap via a Program Logic Model.
- Design: Modularizing the therapy protocol using a Session Structuring System (SSS) for macro (whole program) and micro (individual session) design.
- Development: Creating immersive VR sessions incorporating ACT metaphors, interactive tasks, and multisensory feedback.
- Advancement: Integrating gamification and multimodal arts strategies to enhance user engagement and adherence.
- Commercialization: Preparing for clinical validation and regulatory approval [46].
- Personalization & Data Collection: The framework explicitly integrates a data-driven evaluation framework, collecting real-time behavioral patterns and sensor-based data to enable comprehensive assessment and future personalization of interventions [46].
The workflow below illustrates the structured process of this development framework.
Conceptual Framework for Biomarker Detection
The Virtual Reality Analytics Map (VRAM) is a novel conceptual framework designed to systematically leverage VR for detecting symptoms of mental disorders [68]. It bridges psychological constructs with VR technology by mapping and quantifying behavioral domains through specific tasks, thereby capturing nuanced digital biomarkers [68]. The framework outlines a six-step process from defining target symptoms to data analysis, providing a standardized structure that enhances the reliability of biomarker research by ensuring that measurements are directly linked to theoretical constructs [68]. This structured approach directly supports the validation of VR biomarkers by providing a clear methodology for their identification and quantification.
The Scientist's Toolkit: Essential Research Reagents
For researchers designing experiments to validate VR biomarkers, the following tools and components are critical. This list synthesizes key hardware and software elements from the analyzed studies, with a focus on their function in generating reliable data while managing patient-centered barriers.
Table 2: Key Research Reagent Solutions for VR Biomarker Studies
| Research Reagent | Function in VR Research | Considerations for Barriers |
|---|---|---|
| Head-Mounted Display (HMD) [10] [7] | Primary hardware for delivering immersive 3D environments; fosters a sense of "presence". | HMD weight and design impact physical comfort; newer, lighter models can reduce cybersickness risk and improve adherence. |
| Biofeedback Sensors (EEG, ECG, ET) [1] | Captures physiological biomarkers (brain activity, heart rate variability, eye movement) in real-time. | Enables objective data collection independent of self-report, validating patient response within the VR environment. |
| Session Structuring System (SSS) [46] | A model for operationalizing therapy protocols into modular, timed VR sessions. | Standardizes intervention delivery, enhancing treatment fidelity and data comparability across subjects and sessions. |
| Gamification & Multimodal Arts [46] | Incorporates game-like elements and artistic modalities (visual, sound) into therapeutic content. | Boosts user engagement and motivation, potentially increasing adherence and the ecological validity of collected data. |
| Virtual Reality Analytics Map (VRAM) [68] | A conceptual framework for mapping psychological symptoms to quantifiable VR tasks and analytics. | Provides a systematic, hypothesis-driven approach for identifying and validating digital biomarkers of mental disorders. |
The integration of patient-centered design principles is no longer ancillary but integral to the validation of VR biomarkers in mental health research. Frameworks that explicitly address autonomy through user-controlled elements, personalization via adaptive protocols and multimodal data, and physical comfort through manageable session durations and hardware considerations are producing more reliable and valid datasets [10] [46] [1]. The comparative data and structured protocols outlined here provide a foundation for researchers to design studies where biomarker validity is reinforced by a positive and engaging patient experience, ultimately accelerating the development of objective diagnostics and personalized therapeutics in mental health.
The validation of virtual reality (VR) biomarkers for mental disorder research represents a frontier in precision psychiatry, offering unprecedented potential for objective assessment and therapeutic innovation. However, this potential is inextricably linked to critical ethical considerations surrounding data privacy, immersive technology implementation, and clinical supervision frameworks. As VR technologies rapidly advance from research settings to clinical applications, they generate complex datasets including behavioral, physiological, and neuroimaging data that require sophisticated analytical approaches and robust ethical safeguards. This guide examines the current landscape of VR biomarker validation through an ethical lens, comparing technological approaches, methodological frameworks, and implementation strategies to inform researchers, scientists, and drug development professionals working at this emerging intersection of technology and mental health.
The Current Landscape of VR in Mental Health
Virtual reality has demonstrated significant utility across multiple mental health domains, with applications expanding rapidly beyond initial exposure therapy paradigms. Current implementations span diagnostic assessment, therapeutic intervention, and treatment monitoring, leveraging VR's capacity to create controlled, replicable environments that elicit ecologically valid responses [68]. The Department of Veterans Affairs alone has deployed over 40 active use cases of augmented and virtual reality, utilizing approximately 3,500 VR headsets across more than 170 medical centers for conditions including PTSD, suicide prevention, and other mental health disorders [69].
The technological ecosystem for VR mental health applications includes multiple modalities, each with distinct implementation considerations:
Table 1: Virtual Reality Modalities in Mental Health Applications
| Modality | Key Characteristics | Primary Applications | Data Collection Capabilities |
|---|---|---|---|
| Virtual Reality (VR) | Fully immersive computer-generated environments viewed through head-mounted displays | Exposure therapy, neuropsychological assessment, avatar-based interventions | Behavioral tracking, eye-tracking, physiological monitoring, performance metrics |
| Augmented Reality (AR) | Digital elements overlaid onto physical environment in real-time | Phobia treatment, cognitive training, procedural guidance | Environmental interaction patterns, response to integrated stimuli |
| 360° Video Immersion | Pre-recorded spherical video content providing immersive environments | Empathy training, relaxation exercises, preliminary exposure | Viewing patterns, physiological responses, engagement metrics |
Ethical Frameworks for VR Implementation
The ethical implementation of VR technologies in mental health care requires balancing therapeutic potential against emerging risks. A scoping review of ethical issues in extended reality identified five core challenges: balancing beneficence and non-maleficence, preserving autonomy amid reality alteration, ensuring data privacy and confidentiality, establishing clinical liability and regulation, and fostering inclusiveness and equity in XR development [70]. These concerns are particularly salient in biomarker validation research, where sensitive data collection intersects with vulnerable populations.
Data Privacy and Security Considerations
Data privacy emerges as a paramount concern, especially as VR applications transition from clinical to home environments. Caitlin Rawlins of the Veterans Health Administration notes that when VR data is captured outside VA facilities, "it is no longer considered VA-owned data," creating significant ethical and regulatory challenges regarding data governance, access control, and patient awareness of data collection practices [69]. This distinction is crucial for biomarker research, as longitudinal data collection often extends beyond clinical settings.
The types of data collected through VR systems present unique privacy challenges:
Table 2: VR Data Types and Privacy Implications
| Data Category | Specific Data Collected | Privacy Implications | Biomarker Relevance |
|---|---|---|---|
| Behavioral Data | Movement patterns, reaction times, avoidance behaviors, interaction patterns | Potential identification through behavioral biometrics | Core component for diagnostic and prognostic biomarkers |
| Physiological Data | Heart rate, galvanic skin response, EEG patterns, eye tracking | Health information requiring HIPAA compliance | Correlates with emotional arousal, cognitive load, treatment response |
| Performance Data | Task accuracy, completion times, error patterns | May reveal cognitive deficits or mental health status | Quantitative metrics for cognitive assessment |
| Environmental Data | Home environment mapping, room layout, ambient sounds | Invasion of domestic privacy spaces | Contextual factors affecting biomarker validity |
VR Biomarker Validation: Methodological Approaches
The Virtual Reality Analytics Map (VRAM) Framework
The Virtual Reality Analytics Map (VRAM) provides a conceptual framework for detecting mental disorders using VR data, offering a systematic approach to biomarker validation [68]. This framework integrates psychological constructs with VR technology through a six-step process: (1) identifying target symptoms and psychological constructs, (2) selecting relevant behavioral domains, (3) designing VR tasks to quantify behaviors, (4) data collection and feature extraction, (5) analytical modeling, and (6) clinical validation. The VRAM framework exemplifies the methodological rigor required for biomarker development while highlighting the ethical necessity of transparent analytical approaches.
EEG Biomarkers of Sense of Embodiment
Research investigating EEG biomarkers of sense of embodiment (SoE) in VR environments demonstrates the complexity of validating neurophysiological correlates of subjective experiences. Studies have identified significant increases in Beta and Gamma power over the occipital lobe as potential EEG biomarkers for SoE, suggesting the occipital lobe's role in multisensory integration and sensorimotor synchronization [48]. This research exemplifies the multimodal approach required for biomarker validation, combining subjective measures (validated questionnaires) with objective neural correlates.
The experimental protocol for SoE biomarker investigation typically includes:
- Participant Preparation: Application of EEG electrodes according to the 10-20 system, impedance checking, and VR headset calibration
- Baseline Recording: Resting-state EEG in both physical and virtual environments
- Embodiment Induction: Synchronized visuomotor and visuotactile stimulation to induce ownership of virtual avatar
- Embodiment Disruption: Introduction of temporal or spatial incongruities in multisensory feedback
- Data Acquisition: Continuous EEG recording throughout conditions with event markers
- Subjective Measures: Administration of validated embodiment questionnaires (e.g., 16-item version by Peck and Gonzalez-Franco) following each condition
Experimental Protocols for VR Biomarker Validation
Protocol 1: VR-Based Fear Extinction Biomarkers
This protocol examines physiological and behavioral biomarkers during fear extinction learning in VR environments, relevant to anxiety disorders and PTSD research:
- Participant Screening: Recruit participants with specific phobia or PTSD diagnoses, excluding those with photosensitive epilepsy or severe motion sickness
- Fear Conditioning Phase: Pair neutral virtual stimuli (e.g., colored shapes) with mild aversive stimuli (e.g., mild electric shock or unpleasant sounds) in VR environment
- Extinction Learning: Repeatedly present conditioned stimuli without aversive consequences in novel VR contexts
- Data Collection:
- Physiological: Skin conductance response (SCR), heart rate variability (HRV), electromyography (EMG)
- Behavioral: Avoidance distance, reaction time, gaze avoidance
- Self-report: Subjective units of distress (SUDS) ratings collected at 60-second intervals
- Data Analysis: Compare physiological response patterns between successful versus unsuccessful extinction learners, examining potential biomarkers of treatment response
Protocol 2: Cognitive Biomarkers in Neurodegenerative Disorders
Adaptive Cognitive Assessments (ACAs) implemented through VR platforms offer novel approaches to detecting subtle cognitive changes in neurodegenerative disorders [71]. These systems utilize dynamic difficulty adaptation to individual performance, potentially reducing floor and ceiling effects that limit conventional assessments:
- Participant Cohorts: Patients with mild cognitive impairment, early Alzheimer's disease, and healthy controls
- VR Cognitive Tasks: Six distinct ACA instruments assessing working memory, information processing speed, short-term visuo-spatial memory, semantic recognition, executive functioning, and cognitive flexibility
- Adaptive Protocol: Initial 14 daily tests establishing individual performance baselines, followed by weekly testing sessions with continuous difficulty adaptation
- Data Collection: Performance metrics, difficulty progression, learning curves, and intra-individual variability
- Validation Measures: Correlation with standard neuropsychological batteries, MRI biomarkers, and cerebrospinal fluid biomarkers where available
Comparative Analysis of VR Assessment Approaches
Different VR methodological approaches offer distinct advantages and limitations for biomarker validation:
Table 3: Comparison of VR Biomarker Validation Approaches
| Approach | Key Features | Data Outputs | Validation Strength | Implementation Challenges |
|---|---|---|---|---|
| VRAM Framework [68] | Systematic mapping of psychological constructs to VR tasks | Behavioral metrics, performance scores | High construct validity, comprehensive assessment | Complex implementation, requires multidisciplinary expertise |
| EEG Biomarkers [48] | Direct neural activity measurement during VR experiences | Spectral power, event-related potentials, connectivity patterns | Objective neural correlates, high temporal resolution | Technical complexity, signal artifacts in VR environments |
| Adaptive Cognitive Assessments [71] | Dynamic difficulty adjustment based on performance | Difficulty progression, learning curves, performance variability | Reduced floor/ceiling effects, sensitive to subtle changes | Complex analytical requirements, limited normative data |
| Digital Phenotyping [43] | Passive behavioral monitoring through VR sensors | Movement patterns, interaction metrics, response latencies | Ecological validity, continuous assessment | Privacy concerns, data interpretation challenges |
Clinical Supervision and Implementation Frameworks
Ethical Implementation in Clinical Settings
The implementation of VR technologies in clinical settings requires careful consideration of supervision frameworks, particularly when deploying systems in non-clinical environments. Rawlins emphasizes that clinicians providing AR and VR tools for patients to use at home have a responsibility to ensure patients understand "what data is being collected, where it will be stored, who has access to it and what they are using it for" [69]. This transparency is essential for maintaining therapeutic alliance and ethical practice.
Case studies from long-term care settings in Canada and the Czech Republic highlight the importance of the "ABCDEF" framework for ethical VR implementation: Access, Balance, Connection, Diversity, Engagement and Freedom to say no [72]. These principles emphasize equitable access to VR benefits, balanced risk assessment, social connection preservation, cultural relevance, meaningful engagement, and respect for autonomy through the right to decline participation.
Safety Monitoring and Adverse Event Protocols
Clinical supervision of VR-based interventions requires specialized protocols for monitoring and addressing potential adverse effects:
- Cybersickness Assessment: Regular monitoring using standardized scales (e.g., Simulator Sickness Questionnaire) with session termination protocols for significant symptoms
- Emotional Distress Management: Real-time monitoring of distress indicators with clinician-controlled termination options and post-session debriefing procedures
- Reality Orientation: Structured procedures for reorientation to physical environment following immersive experiences, particularly important for patients with reality testing impairments
- Data Security Monitoring: Regular audits of data handling procedures, access logs, and encryption protocols to maintain privacy safeguards
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Essential Research Resources for VR Biomarker Validation
| Research Tool | Function | Example Applications | Implementation Considerations |
|---|---|---|---|
| VR Development Platforms (Unity, Unreal Engine) | Create controlled virtual environments with precise stimulus delivery | Custom environment development for specific disorder assessment | Requires programming expertise, hardware compatibility testing |
| Biometric Sensors (EEG, EDA, ECG, eye-tracking) | Capture physiological responses during VR experiences | Arousal monitoring, engagement assessment, emotional response quantification | Sensor integration challenges, signal artifact management |
| Data Analytics Platforms (Python, R, MATLAB) | Process multi-modal VR data streams and identify biomarker patterns | Machine learning analysis, feature extraction, statistical validation | Computational resources, specialized analytical expertise |
| Ethical Review Frameworks (Institutional Review Boards) | Ensure participant protection and ethical implementation | Protocol review, informed consent development, risk-benefit assessment | Evolving standards for immersive technology, privacy protection |
The validation of VR biomarkers for mental disorders represents a promising frontier in precision psychiatry, offering potential breakthroughs in objective assessment, treatment personalization, and therapeutic innovation. However, this potential must be balanced against significant ethical imperatives regarding data privacy, equitable access, and appropriate clinical supervision. As VR technologies continue to evolve and generate increasingly sophisticated biomarkers, the field must develop corresponding ethical frameworks that prioritize patient welfare while enabling scientific advancement.
Future research directions should include: (1) standardized protocols for multi-site biomarker validation studies, (2) development of ethical guidelines specific to VR-based assessment and treatment, (3) investigation of privacy-preserving analytical approaches for sensitive VR data, and (4) exploration of hybrid implementation models that balance technological innovation with human clinical oversight. By addressing these challenges through collaborative, multidisciplinary efforts, the field can realize the potential of VR biomarkers while maintaining the ethical standards essential to mental health research and practice.
Virtual reality (VR) demonstrates significant clinical potential for treating mental disorders, yet a critical challenge remains: how to maintain its therapeutic efficacy beyond initial novelty. For researchers and drug development professionals, the validation of digital biomarkers is inextricably linked to consistent, long-term user engagement. Without strategies to sustain participation, the data required for robust biomarker development becomes fragmented and unreliable. This guide compares current VR therapeutic applications and their associated experimental protocols, focusing on evidence relevant to sustaining user engagement and validating digital biomarkers for mental health research. The field is transitioning from proof-of-concept studies to the development of enduring, evidence-based interventions that can produce high-quality longitudinal data [43].
Comparative Analysis of VR Therapeutic Applications and Endurance
The utility of VR in mental healthcare spans multiple disorders, but the implementation strategies and evidence for long-term use vary considerably. The following table summarizes key applications, their supporting evidence, and specific engagement considerations relevant to longitudinal study design.
Table 1: Comparison of VR Therapeutic Applications and Sustained Engagement Potential
| Mental Health Condition | Therapeutic Application of VR | Reported Clinical Outcomes & Endurance | Engagement & Adherence Considerations for Long-Term Studies |
|---|---|---|---|
| Anxiety Disorders & Phobias | VR Exposure Therapy (VRET): Controlled, graded exposure to feared stimuli in safe, virtual environments [43] [73]. | Superior to waitlist/psychoeducation controls [43]. Sustained gains at 6-month follow-up in 9/11 survivor study [73]. | High initial engagement; long-term use may require progressively challenging scenarios to prevent habituation. |
| Psychosis & Schizophrenia | VR-CBT for delusions and hallucinations; social cognition training in controlled social settings [43] [7]. | Generally as effective as traditional CBT [43]. Feasible for improving social cognition [7]. | Requires careful titration of stress triggers. Personalization is key to maintaining engagement and tolerability. |
| Depression | Computerized CBT via "serious games" (e.g., Sparx); immersive behavioral activation [73] [7]. | Reduces symptoms in high-risk groups (e.g., students) [7]. | Game-based formats may enhance stickiness. Integrating motivational principles is critical for a condition characterized by anhedonia. |
| Neurodevelopmental Disorders (e.g., ASD) | Social skills training through simulated social interactions and scenarios [7]. | Shown to foster empathy and social cognition [7]. | Predictable, structured virtual environments can be inherently engaging for these populations. |
| Pain & Stress Management | Distraction therapy using immersive, relaxing environments; mindfulness and relaxation training [7] [74]. | Effective in mitigating pain, anxiety, and depression in serious illnesses [74]. | High utility for repeated use, as pain and stress are often chronic. Content variety is essential to prevent boredom. |
Experimental Protocols for Evaluating Engagement and Biomarkers
To validate VR biomarkers and therapeutic effects, rigorous, standardized experimental methodologies are required. Below are detailed protocols from key research areas.
Protocol for VR Exposure Therapy (VRET) in Anxiety Disorders
This protocol is adapted from studies on PTSD and specific phobias [43] [73].
- 1. Participant Screening & Baseline Assessment: Diagnose using structured clinical interviews (e.g., MINI). Establish baseline symptom severity (e.g., CAPS-5 for PTSD, SUDS for phobias).
- 2. Pre-Treatment Psychoeducation: Explain the rationale of exposure therapy, the VR technology, and the process of subjective units of distress (SUDS) scoring.
- 3. Constructing the Fear Hierarchy: Collaboratively develop a hierarchy of feared scenarios with the patient, ranked by SUDS.
- 4. Graded VR Exposure Sessions:
- Use a head-mounted display (HMD) to present scenarios.
- Begin with items low on the fear hierarchy.
- The patient remains in the scenario until SUDS decreases significantly (e.g., 50% reduction).
- Sessions are typically 30-60 minutes, repeated weekly.
- 5. Data Collection & Biomarker Sensing:
- Subjective Data: Continuous SUDS ratings during exposure.
- Behavioral Data: HMD tracking of head movement, avoidance behaviors (e.g., closing eyes).
- Physiological Data (Digital Phenotyping): Synchronized capture of heart rate (ECG), skin conductance (EDA), and respiration via wearable sensors [43].
- 6. Post-Session Processing & Homework: Discuss the experience, consolidate learning, and assign in-vivo exposure exercises if appropriate.
- 7. Long-Term Follow-Up: Re-administer clinical scales at post-treatment, 3-month, 6-month, and 12-month intervals to assess durability.
Protocol for EEG Biomarker Identification in VR Embodiment
This protocol is based on research identifying neural correlates of the Sense of Embodiment (SoE) [48].
- 1. Participant Preparation: Apply a high-density EEG cap (e.g., 64-channel). Measure electrode impedances to ensure signal quality.
- 2. Experimental Setup: Calibrate VR HMD and motion tracking systems. Set up a synchronized data acquisition system for EEG and VR events.
- 3. Experimental Paradigm:
- Baseline Block: Record resting-state EEG with eyes open and closed in a neutral virtual environment.
- Embodiment Induction Block: Use multisensory triggers (visuomotor, visuotactile) to induce a strong SoE toward a virtual avatar. For example, the participant sees the virtual hand moving in sync with their own and receives synchronous tactile feedback.
- Embodiment Disruption Block: Introduce spatial or temporal asynchrony between the participant's movements and the avatar's movements to disrupt SoE.
- 4. Subjective Measures: After each condition, administer a validated embodiment questionnaire (e.g., a 16-item SoE scale) to quantify the subjective experience [48].
- 5. EEG Data Preprocessing:
- Apply band-pass filtering (e.g., 0.5-70 Hz).
- Remove artifacts (eye blinks, muscle movement) using ICA or other algorithms.
- Segment data into epochs for each condition.
- 6. Feature Extraction & Analysis:
- Compute spectral power density in key frequency bands (Delta, Theta, Alpha, Beta, Gamma).
- Perform statistical comparisons (e.g., ANOVA) of power between conditions (Baseline vs. Induction vs. Disruption) across brain regions.
- Use source localization techniques to identify neural generators of significant effects.
- 7. Biomarker Validation: Correlate significant EEG features (e.g., increased Beta/Gamma power in the occipital lobe) with subjective questionnaire scores to validate the neural signature of SoE [48].
The following diagram illustrates the logical workflow and data integration of this experimental protocol.
Diagram 1: Experimental Workflow for VR-EEG Biomarker Identification
A Framework for Sustained Engagement and Biomarker Development
Long-term therapeutic effect requires moving beyond isolated interventions to a continuous care model. The following diagram outlines a strategic framework for achieving this, integrating key concepts from implementation science and digital phenotyping [43].
Diagram 2: Framework for Long-Term Engagement and Biomarker Validation
Key Framework Components:
- Just-in-Time Adaptive Interventions (JITAIs): These systems use passive sensor data (digital phenotyping) to detect moments of need and deliver micro-interventions precisely when they are most effective, moving away from fixed scheduling to a dynamic model [43].
- Blended Human Support: The "set-it-and-forget-it" model is ineffective. Integrating human support, such as digital navigators or clinicians, to guide users, troubleshoot technology, and provide encouragement is crucial for long-term adherence [43].
- Personalized Content: Leveraging user interaction data and preferences to adapt virtual environments and therapeutic challenges maintains relevance and counters monotony.
- Multi-Modal Data Fusion: Combining active (surveys), passive (sensors), and performance data creates a comprehensive picture of the user's state, which is fundamental for discovering robust digital biomarkers predictive of long-term outcomes [43] [75].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Materials and Technologies for VR Mental Health Research
| Item Category | Specific Examples & Functions | Relevance to Research & Biomarkers |
|---|---|---|
| VR Hardware Platforms | Head-Mounted Displays (HMDs) like Meta Quest Pro, HTC Vive, Varjo. Provide immersive visual/auditory stimulation and track head movement. | High-quality tracking is essential for measuring behavior (e.g., avoidance) and inducing embodiment. The platform choice affects generalizability. |
| Physiological Sensors | EEG Systems (high-density for neural correlates), EDA/GSR Sensors (for arousal), ECG Sensors (for heart rate variability), Eye-Tracking (integrated in HMDs). | The primary tools for digital phenotyping and objective biomarker discovery. Critical for validating subjective states like anxiety or embodiment [43] [48]. |
| Software & Development | Game Engines (Unity, Unreal Engine) for creating virtual environments; SDKs (e.g., OpenVR, LabStreamingLayer) for data synchronization. | Enables the creation of ecologically valid and customizable therapeutic scenarios. Precise time-sync of stimuli and data is non-negotiable for mechanistic studies. |
| Biometric Analysis Suites | Software for analyzing EEG (e.g., EEGLAB, BrainVision Analyzer), EDA (e.g., Ledalab), and motion data (custom scripts in Python/R). | Used to preprocess, clean, and extract features (e.g., spectral power, SCR peaks) from raw physiological signals for biomarker development. |
| Validated Clinical Scales | Self-report measures for specific constructs (e.g., Presence, Sense of Embodiment questionnaires, PHQ-9, GAD-7, PANSS) [48] [7]. | Provide the "ground truth" for validating digital biomarkers against established clinical and subjective metrics. |
Optimizing VR for long-term use requires a multifaceted approach that integrates engaging, personalized content with supportive human contact and adaptive, data-driven interventions. For the research community, the path to validating reliable VR biomarkers for mental disorders is parallel to the path of solving the engagement puzzle. Sustained use generates the rich, longitudinal data essential for discovering biomarkers that are not merely correlates of state, but predictors of therapeutic trajectory and long-term recovery. The future of the field hinges on building these enduring therapeutic ecosystems and leveraging them for rigorous scientific discovery.
Proving Efficacy: Validating VR Biomarkers Against Gold Standards and Multimodal Benchmarks
The validation of virtual reality (VR) biomarkers represents a pivotal advancement in mental disorders research, addressing critical limitations of traditional neuropsychological assessments. Current gold-standard diagnostic methods for conditions like mild cognitive impairment (MCI) and Alzheimer's disease (AD)—including comprehensive neuropsychological testing, amyloid PET imaging, and cerebrospinal fluid analysis—face significant practical constraints regarding cost, invasiveness, and ecological validity [25]. These challenges are particularly problematic for large-scale screening and early intervention, especially with the advent of disease-modifying treatments that show maximal efficacy in early disease stages [25].
VR technology offers a transformative approach by enabling the creation of ecologically valid testing environments that simulate real-world cognitive challenges while maintaining controlled laboratory conditions. Unlike traditional paper-and-pencil tests that may lack sensitivity to subtle cognitive changes, VR assessments can capture nuanced behavioral metrics including movement efficiency, hesitation latency, and error patterns during complex tasks [24]. However, for these digital biomarkers to achieve widespread adoption in both clinical research and drug development, they must demonstrate robust criterion validity through correlation with established biological and cognitive measures.
This guide systematically evaluates the experimental evidence establishing criterion validity for VR biomarkers through direct comparison with magnetic resonance imaging (MRI) biomarkers and standardized cognitive tests, providing researchers with validated protocols and performance benchmarks for implementation in mental disorders research.
Experimental Protocols for Establishing Criterion Validity
Multimodal Validation Integrating VR and MRI Biomarkers
Objective: To evaluate the relationship between VR-derived behavioral biomarkers and MRI-based structural biomarkers for early detection of mild cognitive impairment [4].
Participant Characteristics: The study enrolled 54 older adults, comprising 22 healthy controls (41%) and 32 patients with MCI (59%). Participants were typically aged 65-80 years, with comprehensive cognitive screening to confirm diagnostic status [4].
VR Assessment Protocol:
- Task: Virtual food-ordering kiosk test simulating instrumental activities of daily living
- Equipment: Immersive VR headset with motion-tracking controllers
- Primary Biomarkers:
- Hand movement speed (cm/sec)
- Visual scanpath length (pixels)
- Time to completion (seconds)
- Number of errors (count)
- Procedure: Participants completed the kiosk task in a single session, with all interactions recorded for subsequent behavioral analysis [4]
MRI Acquisition and Processing:
- Protocol: T1-weighted structural MRI scans
- Biomarkers: 22 cortical and subcortical volume measurements from both hemispheres
- Analysis: Automated segmentation and volumetry using FSL or FreeSurfer pipelines
- Correlation Analysis: ANCOVA models comparing biomarkers between groups, with age as a covariate [4]
Multimodal Integration: A support vector machine (SVM) model was trained using significant biomarkers from both modalities to classify MCI versus healthy controls [4].
VR Stroop Test Validation Against Established Cognitive Assessments
Objective: To develop and validate a novel VR-based Stroop Test (VRST) for detecting executive dysfunction in MCI [24].
Participant Characteristics: 413 older adults (224 healthy controls, 189 with MCI) recruited from senior and daycare centers in South Korea. MCI diagnosis followed Petersen criteria with comprehensive neuropsychological assessment [24].
VRST Protocol:
- Task: Clothing-sorting task with incongruent word-color stimuli (reverse Stroop paradigm)
- Equipment: HTC Vive Controller with desktop display (no head-mounted display to reduce cybersickness)
- Behavioral Metrics:
- Task completion time (seconds)
- 3D trajectory length of controller movement (units)
- Hesitation latency (response delay in seconds)
- Procedure: Participants completed three 2-minute trials with 30-second breaks after comprehensive tutorial [24]
Traditional Assessment Battery:
- Global Cognition: Korean version of Montreal Cognitive Assessment (MoCA-K)
- Inhibitory Control: Paper-based Stroop test
- Working Memory: Corsi Block Test (CBT)
- Motor Function: Box and Block Test and Grooved Pegboard Test (to control for baseline motor differences) [24]
Validation Analysis: Receiver operating characteristic (ROC) curves to assess discriminant power, with Spearman correlations between VRST outcomes and traditional measures [24].
Comparative Performance Data: VR Versus Established Modalities
Diagnostic Accuracy Across Assessment Modalities
Table 1: Comparison of Diagnostic Accuracy Between VR Biomarkers, MRI Biomarkers, and Traditional Cognitive Tests
| Assessment Modality | Specific Biomarker | Sensitivity (%) | Specificity (%) | Area Under Curve (AUC) | Research Context |
|---|---|---|---|---|---|
| VR Only | Hand movement speed | 87.5 | 90.0 | - | MCI detection [4] |
| VR Only | 3D trajectory length | - | - | 0.981 | MCI executive function [24] |
| VR Only | Hesitation latency | - | - | 0.967 | MCI executive function [24] |
| MRI Only | Structural volumetry | 90.9 | 71.4 | - | MCI detection [4] |
| Multimodal (VR+MRI) | SVM integrated model | 100 | 90.9 | - | MCI detection [4] |
| Traditional MoCA | Global cognitive score | - | - | 0.962 | MCI screening [24] |
| Meta-Analysis | Various VR assessments | 88.3 | 88.7 | - | MCI detection [25] |
Correlation Coefficients Between VR and Established Measures
Table 2: Correlation Strengths Between VR Biomarkers and Established Cognitive Tests
| VR Biomarker | Traditional Measure | Correlation Coefficient | Cognitive Domain | Significance |
|---|---|---|---|---|
| 3D trajectory length | MoCA-K | Significant correlation | Global cognition | P<0.001 [24] |
| Hesitation latency | Stroop test | Significant correlation | Inhibitory control | P<0.001 [24] |
| Completion time | Corsi Block Test | Significant correlation | Working memory | P<0.001 [24] |
| Hand movement speed | MRI volumetry | Significant correlation | Brain structure | P<0.05 [4] |
Visualization of Experimental Workflows and Validation Relationships
Multimodal Biomarker Validation Workflow
Diagram Title: Multimodal Biomarker Validation Workflow
VR Task Design Principles for Cognitive Assessment
Diagram Title: VR Task Design and Validation Principles
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Materials and Methods for VR Biomarker Validation Research
| Category | Specific Tool/Reagent | Research Function | Example Implementation |
|---|---|---|---|
| VR Hardware | HTC Vive Controller | Captures 3D movement kinematics | Tracking hand trajectory during VR Stroop test [24] |
| VR Software | Unity Engine with XR Interaction Toolkit | Enables virtual environment development | Implementing virtual kiosk and clothing-sorting tasks [24] |
| Neuroimaging | 3T MRI Scanner with T1-weighted sequences | Provides structural brain biomarkers | Quantifying cortical atrophy related to MCI [4] |
| Analysis Tools | Support Vector Machine (SVM) | Multimodal classifier integration | Combining VR and MRI biomarkers for MCI detection [4] |
| Statistical Software | R or Python with sci-kit learn | Statistical analysis and machine learning | Calculating ROC curves and correlation coefficients [4] [24] |
| Traditional Cognitive Tests | MoCA, Stroop Test, Corsi Block Test | Establishes criterion validity | Correlating VR biomarkers with standard measures [24] |
| Motor Control Assessments | Grooved Pegboard Test, Box and Block Test | Controls for baseline motor differences | Ensuring VR metrics reflect cognition not motor impairment [24] |
The established criterion validity between VR biomarkers and both neuroimaging findings and traditional cognitive tests positions virtual reality as a powerful tool in mental disorders research. The high sensitivity and specificity demonstrated by VR assessments, particularly when combined with other modalities through machine learning approaches, supports their utility for early detection and monitoring of cognitive decline [4] [24] [25].
For researchers and drug development professionals, these validated protocols offer practical frameworks for implementing VR biomarkers in both clinical trials and basic research. The strong correlation between VR performance metrics and established measures provides confidence that these digital biomarkers capture meaningful cognitive constructs while offering advantages in ecological validity, precise measurement, and participant engagement [76].
As the field advances, standardized validation protocols like those detailed here will be essential for establishing VR biomarkers as accepted endpoints in clinical trials and tools for screening and monitoring in both research and clinical practice.
The quest for objective biomarkers in mental disorders research is pivotal for advancing diagnostic precision and therapeutic monitoring. Within this context, Virtual Reality (VR) and Magnetic Resonance Imaging (MRI) emerge as two powerful technologies with distinct and complementary profiles. While MRI provides an unparalleled window into the brain's structure, VR offers a controlled platform for capturing ecologically valid behavioral data. This guide provides a comparative analysis of these tools, framing VR's high specificity as a complementary screening tool to MRI's high sensitivity, a synergy that can enhance early detection and validation in mental health research [77].
The following table summarizes the fundamental characteristics, primary applications, and core strengths of VR and MRI in a research context.
| Feature | Virtual Reality (VR) | Magnetic Resonance Imaging (MRI) |
|---|---|---|
| Core Function | Creates immersive, interactive simulated environments to elicit and measure behavior and physiological responses [10]. | Provides high-resolution, non-invasive imaging of anatomical brain structure and volume [77]. |
| Primary Data Type | Behavioral biomarkers (e.g., performance errors, hand/eye movement), physiological data (e.g., heart rate), and self-report [77]. | Structural biomarkers (e.g., cortical thickness, volume of specific brain regions like the hippocampus) [77]. |
| Key Strength in Context | High Specificity: Excels at distinguishing individuals with cognitive impairment from healthy controls based on functional performance [77]. | High Sensitivity: Excels at detecting the presence of subtle structural brain changes associated with conditions like Mild Cognitive Impairment (MCI) [77]. |
| Typical Application | Assessment of instrumental activities of daily living (IADLs), exposure therapy for anxiety disorders, and cognitive training [10] [77]. | Diagnosis and tracking of neurodegenerative diseases, localization of lesions, and research into brain-behavior relationships [77]. |
Quantitative Performance Comparison
A direct comparison of their classification performance for Mild Cognitive Impairment (MCI) highlights their complementary nature. The data below is derived from a study with 54 participants (22 healthy controls, 32 MCI patients) that used a virtual kiosk test for VR biomarkers and T1-weighted scans for MRI biomarkers [77].
| Biomarker Type | Sensitivity | Specificity | Key Performance Insight |
|---|---|---|---|
| VR-Derived Biomarkers [77] | 87.5% | 90% | Superior at correctly identifying healthy individuals (low false positive rate). |
| MRI Biomarkers [77] | 90.9% | 71.4% | Superior at correctly identifying those with the condition (low false negative rate). |
| Multimodal Model (VR + MRI) [77] | 100% | 90.9% | Integration achieves superior overall accuracy, leveraging the strengths of both. |
Detailed Experimental Protocols
Protocol for VR Biomarker Collection: The Virtual Kiosk Test
The virtual kiosk test is designed to assess cognitive impairment by analyzing behavioral data collected during a complex Instrumental Activity of Daily Living (IADL) [77].
- Objective: To distinguish patients with MCI from healthy controls using VR-derived biomarkers of hand movement, eye movement, and task performance [77].
- Setup: Participants wear a VR head-mounted display (HMD). The system runs on a laptop with a high-performance processor (e.g., Intel i7) and graphics card (e.g., NVIDIA GeForce RTX 3080) using Unity and VIVEPORT software [77].
- Task: Participants are immersed in a virtual environment and instructed to order menu items at a touch-screen kiosk. The task requires navigation, reading, selection, and payment, engaging multiple cognitive domains [77].
- Data Extraction: The system automatically collects four key VR-derived biomarkers:
- Hand Movement Speed: Quantifies motor agility and planning.
- Scanpath Length: Measures the efficiency of visual search.
- Time to Completion: Assesses overall task efficiency.
- Number of Errors: Captures deficits in attention and executive function [77].
- Analysis: A support vector machine (SVM) model is trained on these biomarkers to classify participants [77].
Protocol for MRI Biomarker Collection
This protocol focuses on quantifying structural brain changes for early MCI detection [77].
- Objective: To identify patients with MCI based on observable atrophy in brain structures, particularly in memory-associated regions [77].
- Image Acquisition: T1-weighted MRI scans are performed to obtain high-contrast images of brain anatomy [77].
- Region of Interest (ROI) Analysis: 22 biomarkers are collected from structures in both brain hemispheres, with a focus on the hippocampus and entorhinal cortex, which are critically involved in memory and are early sites of atrophy in Alzheimer's disease [77].
- Data Extraction: Biomarkers typically include the volume, cortical thickness, or density of these pre-specified ROIs [77].
- Analysis: Statistical models (e.g., Analysis of Covariance with age as a covariate) compare these measures between healthy controls and MCI patients. Significant biomarkers are then used to train classification models like SVM [77].
Conceptual Workflow for Multimodal Integration
The following diagram illustrates the logical workflow for integrating VR and MRI biomarkers, a process that leads to enhanced detection capabilities [77].
The Scientist's Toolkit: Essential Research Reagents and Materials
This table details key materials and solutions used in the featured multimodal experiment for MCI detection [77].
| Item Name | Function / Rationale |
|---|---|
| Immersive VR Head-Mounted Display (HMD) | Presents the virtual environment, blocking external distractions to create a controlled, ecologically valid testing space [77]. |
| Virtual Kiosk Software | Provides the standardized cognitive task (food ordering) designed to engage executive function, memory, and visuospatial skills for biomarker extraction [77]. |
| 3T MRI Scanner | Generates high-resolution T1-weighted structural images necessary for quantifying subtle volumetric changes in brain regions like the hippocampus [77]. |
| Eye & Hand Tracking System | Integrated into the VR HMD to collect precise, quantitative behavioral data (scanpath, movement speed) as functional biomarkers [77]. |
| Support Vector Machine (SVM) Model | A machine learning algorithm that integrates the VR and MRI biomarker data to perform the final classification of participants, demonstrating the added value of multimodal integration [77]. |
The detection of Mild Cognitive Impairment (MCI) stands as a critical frontier in neuropsychiatry, representing the transitional stage between expected age-related cognitive decline and the more serious onset of dementia. Accurate early detection of MCI is paramount for enabling timely intervention and potentially slowing disease progression. Traditional diagnostic approaches, which often rely on unimodal data such as structural neuroimaging or standalone cognitive tests, frequently struggle with sensitivity and specificity limitations. In response to these challenges, multimodal integration has emerged as a transformative methodology that synergistically combines diverse data streams—from neuroimaging and physiological sensing to immersive behavioral analysis—to achieve unprecedented diagnostic accuracy. This paradigm shift is particularly evident in the validation of virtual reality (VR) biomarkers, which provide ecologically valid, objective measures of cognitive and behavioral function within standardized environments.
Framed within the broader thesis of validating digital biomarkers for mental disorders research, this guide objectively compares the performance of unimodal versus multimodal approaches, with specific emphasis on VR-enabled platforms. For researchers and drug development professionals, these technological advances offer not only enhanced diagnostic precision but also novel endpoints for clinical trials. By moving beyond traditional subjective rating scales to objective, frequently collected digital measures, multimodal frameworks are poised to accelerate therapeutic development and personalize intervention strategies.
Performance Comparison: Multimodal vs. Traditional Approaches
Quantitative Performance Metrics Across Methodologies
Table 1: Comparative performance of unimodal and multimodal approaches in MCI and related disorder classification
| Methodology | Data Modalities | Accuracy | Sensitivity | Specificity | Balanced Accuracy | AUC |
|---|---|---|---|---|---|---|
| Traditional CNN (MRI-only) | Structural MRI | - | - | - | - | - |
| ECAResNet269 (Multimodal MRI) | 2D grid sMRI (10 slices) | - | - | - | 63% (Baseline) | - |
| ECAResNet269 + Imbalance Mitigation | 2D grid sMRI + Class balancing | - | CN: 78%, MCI: 76%, AD: 69% | - | 74% | - |
| FusionNet | MRI + PET + CT | 94% | 93% | - | - | - |
| VR Multimodal Framework (MDD) | EEG + ET + HRV | 81.7% | - | - | - | 0.921 |
| VR Assessment (Panic Disorder) | HRV + Behavioral metrics | 85% | - | - | - | - |
Note: CN = Cognitively Normal; AD = Alzheimer's Disease; AUC = Area Under Curve; MDD = Major Depressive Disorder. Performance metrics for MCI classification specifically vary based on dataset and implementation. The ECAResNet269 model with imbalance mitigation shows strong sensitivity across all classes, including MCI [78]. The VR Multimodal Framework, while tested for MDD, demonstrates the power of combining physiological sensors for high classification accuracy [1].
Key Performance Insights
Impact of Class Imbalance Mitigation: The performance leap in the ECAResNet269 model—from 63% to 74% balanced accuracy after implementing combined SMOTE, cost-sensitive learning, and focal loss approaches—highlights a critical consideration for real-world MCI detection where data imbalance is common [78].
Multimodal Superiority in Neuroimaging: FusionNet's 94% accuracy in AD classification, achieved through integrated analysis of MRI, PET, and CT scans, demonstrates that multi-modal imaging provides complementary information that significantly outperforms single-modality approaches [79].
VR-Enhanced Diagnostic Accuracy: The 85% accuracy achieved by combining VR-based and clinical data for panic disorder classification surpasses models using only clinical (77%) or only VR data (75%), validating that VR biomarkers add unique, predictive information beyond conventional measures [80].
Experimental Protocols: Methodologies for Multimodal Validation
VR-Based Multimodal Framework for Adolescent MDD
Table 2: Key research reagents and experimental components for VR-based multimodal assessment
| Research Reagent / Component | Function / Rationale | Implementation Example |
|---|---|---|
| Custom VR Environment (A-Frame) | Provides standardized, immersive emotional task scenario | Magical forest lakeside panorama with AI agent "Xuyu" |
| BIOPAC MP160 System | Acquires synchronized physiological data (EEG, ECG) | Records EEG, ocular motility, and ECG signals |
| See A8 Portable Telemetric Ophthalmoscope | Tracks eye movement metrics | Captures saccade counts and fixation durations |
| Claude API | Enables dynamic therapeutic dialogue | Generates AI agent responses for interactive emotional exploration |
| LabStreamingLayer (LSL) | Synchronizes multimodal data streams | Aligns EEG, ET, and HRV timestamps for integrated analysis |
| Support Vector Machine (SVM) Model | Classifies MDD status based on selected features | Uses RFECV for feature selection; trained on physiological differences |
Experimental Protocol:
This case-control study recruited 51 adolescents with first-episode MDD and 64 healthy controls, all undergoing a 10-minute VR-based emotional task [1]. The VR environment consisted of a panoramic magical forest by a lakeside with an AI agent named "Xuyu" that initiated conversations around personal worries and future hopes using a standardized script. During the immersion, the system simultaneously collected electroencephalography (EEG), eye-tracking (ET), and heart rate variability (HRV) data in real-time, synchronized via LabStreamingLayer.
Key physiological differences were identified through statistical analysis, including significantly higher EEG theta/beta ratios, reduced saccade counts, longer fixation durations, and elevated HRV LF/HF ratios in the MDD group. A support vector machine (SVM) model was then trained using recursive feature elimination with cross-validation (RFECV) to classify MDD status based on the selected features. The model achieved 81.7% classification accuracy with an AUC of 0.921, demonstrating strong diagnostic performance [1].
Diagram 1: Experimental workflow for VR-based multimodal assessment of MDD [1]
Multimodal Deep Learning for Alzheimer's Disease Classification
Experimental Protocol:
This comprehensive study systematically compared ten deep learning architectures for Alzheimer's disease classification using structural MRI data [78]. The research utilized T1-weighted MRI scans comprising 14,983 2D grid images derived from 1,346 unique patients from the Alzheimer's Disease Neuroimaging Initiative (ADNI) database.
The methodology employed a novel 2D coronal-10 slicing approach for sMRI, where ten coronal brain slices spaced 2mm apart were arranged in 512 × 512-pixel grids. This technique preserved anatomical relationships while significantly reducing computational demands, retaining 96% of diagnostic information compared to 3D approaches while providing 4.2× faster processing.
To prevent data leakage, patient-level data splitting was implemented, ensuring all images from a single subject were exclusively assigned to one data partition. The study compared traditional CNNs (including ECAResNet269), Vision Transformers, and Capsule Networks. Class imbalance mitigation strategies were critically evaluated, including combined SMOTE, cost-sensitive learning, and focal loss approaches.
ECAResNet269 achieved the highest balanced accuracy (63% at baseline, improving to 74% with imbalance mitigation), with clinically relevant performance across dementia (38% sensitivity/77% specificity), MCI (72% sensitivity/66% specificity), and healthy controls (44% sensitivity/90% specificity) [78]. Notably, pretrained CNN architectures substantially outperformed more advanced methods—Vision Transformer and Capsule Networks showed complete classification failure in this application.
Technological Implementation: Pathways to Multimodal Integration
Multimodal Fusion Architectures in Mental Health
Table 3: Multimodal data types and their clinical relevance in mental health assessment
| Data Modality | Typical Sources | Salient Features | Clinical Relevance for MCI/Neuropsychiatric Disorders |
|---|---|---|---|
| Text | Therapy transcripts, Clinical notes | Lexical affect, Semantic coherence, Syntactic complexity | Cognitive decline screening through language impairment detection |
| Audio | Structured interviews, Spontaneous speech | Prosody (F0, intensity), Speech rate, Voice quality | Depression screening, Cognitive load assessment |
| Video | Clinical assessments, Webcam recordings | Facial action units, Gaze patterns, Head pose, Psychomotor retardation | Emotion recognition, Disease severity rating |
| Physiology | Wearables (PPG, EDA), EEG/ERP, Eye-tracking | Heart rate variability, EEG power bands, Pupillary response, Skin conductance | Objective indices of autonomic/central nervous system activity |
| Neuroimaging | MRI, PET, CT | Brain atrophy, Amyloid-beta deposition, Metabolic activity | Structural and functional brain changes associated with MCI/AD |
The integration of these heterogeneous data streams presents both opportunities and challenges. As identified in a comprehensive survey of multimodal machine learning in mental health, optimal fusion strategies must navigate fragmented data silos, inconsistent annotation schemes, algorithmic bias, and privacy constraints [81]. The field is increasingly moving toward transformer-based fusion architectures that can effectively model complex interactions between modalities, though their success depends on sufficient training data and appropriate regularization to prevent overfitting.
Diagram 2: Multimodal fusion architecture for enhanced MCI detection [78] [81] [79]
Emerging Approaches: Multimodal LLMs and Generative AI
The field is rapidly advancing with the emergence of Multimodal Large Language Models (MLLMs), which extend traditional text-only LLMs by integrating and jointly processing multiple input modalities such as speech, images, video, and physiological signals [82]. These models represent a layered architecture comprising three core modules: a modality encoder that transforms raw signals into vector embeddings, a modality interface that aligns these embeddings into a unified space, and a language model backbone that performs cross-modal reasoning.
For mental health applications, MLLMs offer the potential to interpret emotional states from both spoken language and facial expressions, analyze behavioral patterns from video and physiological data, and generate comprehensive clinical assessments from heterogeneous data sources [82]. While most current applications remain exploratory, they demonstrate the potential for MLLMs to provide more nuanced understanding of mental health conditions by capturing complementary aspects of disorders that may be missed when analyzing modalities in isolation.
The evidence comprehensively demonstrates that multimodal integration consistently achieves superior accuracy in MCI detection and related neuropsychiatric assessments compared to unimodal approaches. The synergistic combination of VR environments with physiological sensing, the fusion of multiple neuroimaging modalities, and the application of advanced machine learning architectures collectively represent a paradigm shift in mental health diagnostics and biomarker validation.
For researchers and drug development professionals, these advancements offer two critical benefits: first, enhanced precision in early detection and stratification of patient populations; second, the development of more sensitive, objective endpoints for clinical trials that can capture treatment effects more efficiently than traditional rating scales. The validation of VR biomarkers, in particular, provides ecologically valid measures of real-world functioning that directly translate to clinically meaningful outcomes.
As the field progresses, key challenges remain in standardizing data collection protocols, ensuring demographic fairness in algorithmic performance, and establishing regulatory pathways for novel digital biomarkers. Nevertheless, the consistent demonstration of superior accuracy through multimodal integration confirms its indispensable role in the future of mental health research and therapeutic development.
The integration of virtual reality (VR) into mental health research and clinical trials represents a paradigm shift in how psychiatric disorders are assessed and treated. By 2025, VR has evolved from a technological demonstration to a validated trial engine capable of standardizing complex tasks, compressing onboarding processes, and unlocking endpoints that clinics struggle to capture consistently [83]. The fundamental advantage of VR technology lies in its ability to convert multi-step instructions into timed, spatially constrained tasks with real-time coaching, thereby yielding lower variance and cleaner audit trails than traditional paper or video-based assessments [83]. However, this promising technology faces a significant validation challenge: ensuring that VR-captured biomarkers perform reliably across diverse demographic groups and cultural contexts.
The validation of VR biomarkers for mental disorders extends beyond mere technical verification—it requires demonstrating that these digital signatures maintain their psychometric properties across different ages, genders, ethnicities, and cultural backgrounds. Research has revealed that performance in immersive VR environments is closely related to age, gender, and frequency of playing video games [84]. This introduces potential biases that must be addressed through rigorous cross-cultural and demographic validation protocols. Without such validation, VR-based assessments risk generating findings that lack generalizability, potentially exacerbating healthcare disparities rather than alleviating them.
This review examines the current state of cross-cultural and demographic validation methodologies for VR biomarkers in mental health research. By comparing validation approaches across different technological platforms and populations, we aim to provide researchers with evidence-based frameworks for establishing the generalizability of their findings. The subsequent sections will analyze quantitative validation data, detail experimental protocols, and provide practical resources for implementing comprehensive validation strategies in VR mental health research.
Comparative Analysis of VR Biomarker Validation Across Platforms and Populations
Performance Variation Across Demographic Groups
Table 1: Demographic Factors Influencing VR Performance Metrics
| Demographic Variable | Effect Size | Impact on VR Performance | Clinical Implications |
|---|---|---|---|
| Age | 11.09, p < 0.001 [84] | Younger participants demonstrate significantly higher performance scores | Age-matched norms essential for accurate assessment |
| Gender | 11.09, p < 0.001 [84] | Identifying as male associated with higher scores | Gender balancing crucial in validation cohorts |
| Video Game Experience | 18.96, p < 0.001 [84] | Higher frequency of play predicts better performance | Prior gaming experience must be recorded and controlled |
| Prior VR Comfort Level | 6.29, p = 0.003 [84] | Self-perceived comfort more predictive than prior experience | Pre-assessment acclimation may reduce bias |
| Professional Background | N/A [84] | Nurses showed higher scores than physicians in multivariate analysis | Occupational factors may influence performance |
The demographic variations highlighted in Table 1 present both challenges and opportunities for VR biomarker validation. Notably, self-perceived comfort with VR technology demonstrated greater predictive power for performance outcomes than actual prior VR experience [84]. This suggests that psychological factors may play a crucial role in VR assessment validity, particularly in cross-cultural contexts where technology acceptance patterns may vary significantly. The finding that NASA Task Load Index scores trended downward while System Usability Index scores trended upward with increasing performance further underscores the importance of user experience factors in validation protocols [84].
Cross-Cultural Validation Status of VR Assessment Platforms
Table 2: Validation Metrics Across Cultural Contexts and Device Types
| VR Application Domain | Current Validation Status | Key Validated Populations | Identified Gaps |
|---|---|---|---|
| VR Perimetry (Visual Field Testing) | FDA/CE marked devices show promising agreement with HFA in moderate-severe glaucoma [85] | Primarily Western populations; limited pediatric validation | Performance in early-stage disease often suboptimal; limited non-Western validation [85] |
| VR Exposure Therapy with Biofeedback | Technically feasible with promising personalization benefits [57] | Overrepresentation of anxiety disorders in Western clinical populations | Small sample sizes, methodological variability, limited population diversity [57] |
| VR Mental Health Applications | Demonstrated efficacy for specific phobias, PTSD, anxiety disorders [10] [7] | Expanding from anxiety disorders to diverse clinical populations | Lack of standardized protocols, limited long-term outcome measures [7] |
| VR Neurocognitive Assessment | Test standardization and repeatability advantages [83] | Early validation across limited demographic bands | Learning effects without alternate forms; limited cross-cultural normative data [83] |
The validation landscape reveals significant disparities in geographic and demographic representation. While certain applications like VR perimetry have achieved regulatory approval for specific use cases, their validation often remains limited to Western populations and moderate to severe disease stages [85]. Similarly, VR exposure therapy with biofeedback shows technical feasibility but suffers from an overrepresentation of anxiety disorders and limited population diversity in validation studies [57]. These gaps highlight the critical need for more inclusive validation frameworks that account for cultural variations in symptom expression, technology acceptance, and behavioral response patterns.
Experimental Protocols for Cross-Cultural and Demographic Validation
Comprehensive Validation Workflow
The following diagram illustrates a systematic approach to cross-cultural and demographic validation of VR biomarkers for mental health research:
VR Biomarker Validation Workflow illustrates the comprehensive process required for robust validation of virtual reality biomarkers across diverse populations, incorporating both cross-cultural and demographic considerations at each stage.
Key Methodological Components
Context of Use Definition
The validation process must begin with precise specification of the VR biomarker's intended context of use. This includes declaring specific headset models, tracking modes (inside-out vs. external), minimum lighting requirements, and firmware versions across all study sites [83]. For psychological endpoints, researchers must specify forms to mitigate learning effects and establish appropriate washout periods between assessments. This precise specification is particularly crucial in cross-cultural research where technical infrastructure may vary significantly between regions.
Population Stratification and Sampling
Stratified sampling frameworks must deliberately oversubscribe underrepresented demographic groups to ensure adequate statistical power for subgroup analyses. Research indicates that performance during immersive VR experiences varies significantly by age (F=11.09, p<0.001), gender (F=11.09, p<0.001), and frequency of playing video games (F=18.96, p<0.001) [84]. These factors must be systematically addressed in recruitment strategies to avoid validation biases. Additionally, cultural background variables including technology acceptance patterns, subjective norms, and perceived enjoyment should be incorporated into sampling frameworks [86].
Cross-Cultural Protocol Adaptation
Beyond simple translation of instructions, comprehensive cultural adaptation requires modifying VR content to ensure ecological validity across different cultural contexts. This includes adjusting virtual environments, social scenarios, and emotional cues to align with culturally specific expressions of psychological distress. Studies of technology acceptance have found that variables such as perceived enjoyment and immersion act as crucial antecedents to adoption behaviors, with significant cultural variations in their relative importance [86]. These factors must be considered when adapting VR biomarkers for different cultural contexts.
Equivalence Testing and Statistical Validation
Statistical validation must include tests of measurement invariance across demographic and cultural groups. This involves confirming configural (same factor structure), metric (equivalent factor loadings), and scalar (equivalent intercepts) invariance using structural equation modeling approaches. Bland-Altman agreement analyses against reference standards should be reported separately for different demographic subgroups, and test-retest reliability must be established across these groups [83]. For VR applications incorporating physiological monitoring, researchers should establish equivalent measurement properties for biomarkers such as heart rate, electrodermal activity, and electroencephalography across different ethnic groups, as physiological responses to stressors may vary culturally [57].
Table 3: Key Research Reagent Solutions for VR Biomarker Validation
| Tool Category | Specific Examples | Function in Validation | Implementation Considerations |
|---|---|---|---|
| VR Hardware Platforms | Oculus Quest 2, HTC Vive, Windows Mixed Reality [84] | Provide standardized stimulus delivery across sites | Freeze firmware versions; document tracking specifications [83] |
| Biophysiological Monitoring Systems | ECG/HRV sensors, EDA, EEG headsets [57] | Objective physiological correlation with VR biomarkers | Synchronization protocols; cultural norms regarding physical contact |
| Cultural Adaptation Frameworks | TRAPD (Translation, Review, Adjudication, Pretest, Documentation) | Ensure linguistic and conceptual equivalence | Involve native speakers with mental health expertise |
| Technology Acceptance Measures | Extended TAM models incorporating immersion, enjoyment [86] | Assess cultural variability in VR adoption drivers | Adapt for specific cultural contexts and demographic groups |
| Statistical Equivalence Packages | R lavaan, Mplus, SEM packages | Test measurement invariance across groups | Plan sufficient sample sizes for multi-group analyses |
| Standardized Clinical Reference Measures | HAM-D, PANSS, CAPS culturally adapted versions [7] | Establish criterion validity against gold standards | Use properly validated local versions of reference scales |
The resources outlined in Table 3 represent the essential components for establishing cross-cultural validity of VR biomarkers in mental health research. Particularly critical are the technology acceptance measures, as research has demonstrated that Perceived Usefulness and Perceived Enjoyment serve as primary direct drivers of intention to use VR technologies, with Immersion and Content Quality acting as crucial antecedents [86]. These factors vary significantly across cultural contexts and must be properly assessed and controlled in validation studies.
Analytical Framework for Generalizability Assessment
Demographic Influence Pathways
The following diagram maps the key demographic factors that influence VR biomarker measurements and must be accounted for in validation studies:
Demographic Influence Pathways maps the key demographic and psychological factors that significantly influence virtual reality biomarker measurements, based on empirical research findings. Asterisks (*) denote statistically significant relationships (p<0.001) identified in validation studies.
Implementation Roadmap for Validation Studies
Based on current evidence and technological capabilities, a phased approach to VR biomarker validation is recommended:
2025: Foundation Building – Deploy VR for low-risk applications such as eConsent processes, site start-up tours, and rater training to establish technical infrastructure and preliminary validation data across diverse populations [83]. Measure activation time, deviation rates, and source data verification hours per site as preliminary metrics of cross-site consistency.
2026: Expanded Demographic Validation – Shift task-based endpoints such as neurocognitive tests, motor function assessments, and exposure therapy adjuncts to home-based VR with scheduled tele-supervision [83]. Pre-register rescue pathways for participants who experience motion sickness or demonstrate failed tracking, with particular attention to age-related and cultural variations in adverse effect prevalence.
2027: Comprehensive Generalizability – Promote validated VR-captured measures from secondary to primary endpoints, supported by robust agreement and repeatability datasets across diverse demographic groups and cultural contexts [83]. Establish comprehensive normative databases that account for age, gender, technological experience, and cultural background.
The validation of VR biomarkers for mental disorders must evolve beyond technical verification to encompass comprehensive demographic and cultural validation. Current evidence indicates significant variations in VR performance across age, gender, and gaming experience groups [84], while cross-cultural validation remains limited by small sample sizes and methodological heterogeneity [57] [85]. Future validation efforts must prioritize inclusive sampling frameworks, systematic testing of measurement invariance, and culturally sensitive adaptation of VR content. By addressing these challenges, researchers can unlock the full potential of VR biomarkers to generate globally generalizable findings that advance mental health research and treatment across diverse populations.
Navigating the regulatory landscape is a critical step in translating innovative diagnostic tools from the laboratory to the clinic. For researchers developing novel approaches, such as virtual reality (VR) biomarkers for mental disorders, understanding the distinct pathways of the U.S. Food and Drug Administration (FDA) and the European Union's In Vitro Diagnostic Regulation (IVDR) is essential. This guide provides a structured comparison of these two frameworks to aid in strategic planning for global market access.
Regulatory Frameworks and Classification Systems
The FDA and IVDR operate under different foundational frameworks and classify devices based on distinct, risk-based logic.
In the United States, the FDA regulates In Vitro Diagnostic (IVD) devices as a category of medical devices under the Federal Food, Drug, and Cosmetic Act [87]. The classification is a three-tiered system:
- Class I: Low to moderate risk, subject to general controls.
- Class II: Moderate to high risk, typically requiring a 510(k) premarket notification to demonstrate substantial equivalence to a predicate device.
- Class III: High-risk devices, which require a Premarket Approval (PMA) application to demonstrate safety and effectiveness [87] [88] [89]. Most IVDs fall under Class I or II [90].
In the European Union, IVDs are regulated under the In Vitro Diagnostic Regulation (IVDR - EU 2017/746), a distinct framework from the Medical Device Regulation (MDR) [91]. The IVDR uses a four-tiered classification system based on the device's intended purpose and the inherent risks to patients and public health:
- Class A: Lowest risk (e.g., general lab equipment).
- Class B: Low to moderate risk.
- Class C: Moderate to high risk.
- Class D: Highest risk (e.g., tests for life-threatening infectious diseases) [91] [90] [89].
A pivotal difference is the scope of oversight. Under the previous EU directive, most IVDs could be self-certified. The IVDR has dramatically expanded the scope, requiring that 80-90% of IVDs now undergo review by a Notified Body, an independent organization designated by an EU member state to assess conformity [91] [90]. This shift makes the EU pathway more comparable to the FDA in terms of rigor for most devices.
Table 1: Comparison of Regulatory Frameworks and Classification
| Aspect | U.S. FDA | EU IVDR |
|---|---|---|
| Governing Law | Federal Food, Drug, and Cosmetic Act [87] | Regulation (EU) 2017/746 [91] |
| Regulatory Authority | FDA (Centralized) [91] | Notified Bodies (Decentralized) [91] |
| Classification System | Class I, II, III (based on risk to patient) [89] | Class A, B, C, D (based on patient/public health risk) [91] |
| Notified Body Review | Not applicable | Required for ~80-90% of IVDs (Classes B, C, D) [90] |
Premarket Approval Pathways
The journey to market differs significantly between the two regions, primarily in the required submission types and the role of predicate devices.
FDA Pathways
- 510(k) (Premarket Notification): This is the most common pathway for Class II devices and some Class I devices. A 510(k) submission must demonstrate that the new device is "substantially equivalent" (SE) to a legally marketed predicate device in terms of intended use and technological characteristics [87] [88]. The review focuses heavily on analytical performance (e.g., accuracy, precision, sensitivity) compared to the predicate [87].
- De Novo Classification: This pathway is for novel, low-to-moderate-risk devices for which no predicate exists. Once classified through De Novo, such devices can serve as predicates for future 510(k) submissions [87] [88].
- Premarket Approval (PMA): Required for all Class III devices, this is the most stringent pathway. It demands comprehensive scientific evidence to provide reasonable assurance of the device's safety and effectiveness, typically generated through clinical investigations [87] [88].
IVDR Pathways
Under the IVDR, there is no direct equivalent to the FDA's 510(k). Instead, for all devices except some Class A products, manufacturers must undergo a conformity assessment with a Notified Body [91] [90]. This process involves a detailed review of the device's Technical Documentation, which must prove conformity with the General Safety and Performance Requirements (GSPRs). A cornerstone of the IVDR is the Performance Evaluation Report, which consolidates evidence on scientific validity, analytical performance, and clinical performance [90]. Unlike the FDA's predicate-based system, the IVDR emphasizes a device's own performance data and its alignment with the "state of the art" [90].
Table 2: Comparison of Premarket Submission and Evidence Requirements
| Aspect | U.S. FDA | EU IVDR |
|---|---|---|
| Common Submission Types | 510(k), De Novo, PMA [88] | Technical Documentation Review by Notified Body [90] |
| Basis for Market Access | Substantial Equivalence to a predicate (510(k)) or Safety & Effectiveness (PMA/De Novo) [88] | Conformity with General Safety and Performance Requirements [91] |
| Clinical Evidence | Required for Class III and some Class II; level depends on risk [90] [89] | Performance Evaluation Report required for all classes; level of clinical evidence scales with risk [90] |
| Use of Predicate Devices | Central to the 510(k) pathway [88] | Not permitted; assessment is based on the device's own data and state of the art [90] |
Biomarker Qualification and Evidence Generation
For novel tools like VR biomarkers, the regulatory approach to validation and evidence generation is paramount. The FDA has a structured Biomarker Qualification Program for drug development tools. This collaborative, multi-stage process allows the FDA to evaluate a biomarker for a specific Context of Use (COU) [92]. A qualified biomarker provides a publicly available tool that any drug developer can use in regulatory submissions for that COU. The process involves submitting a Letter of Intent, a detailed Qualification Plan, and finally a Full Qualification Package of supporting evidence [92].
While the IVDR does not have an identically named program, its requirements for clinical evidence and performance evaluation serve a similar function for IVDs. The regulation demands robust evidence of scientific validity, analytical performance, and clinical performance, which must be maintained and updated throughout the device's lifecycle via Post-Market Performance Follow-up (PMPF) [90].
The experimental protocols for validating a VR biomarker, as seen in recent research, illustrate the type of evidence required. For instance, a 2025 study on adolescent Major Depressive Disorder (MDD) used a case-control design involving 51 patients and 64 healthy controls [1]. Participants underwent a 10-minute VR emotional task while multimodal data (EEG, eye-tracking, HRV) was collected [1]. Statistical analysis identified key physiological differences, and a Support Vector Machine (SVM) model was trained, achieving an 81.7% classification accuracy [1]. Similarly, a study on Panic Disorder used a 6-month longitudinal design with a Virtual Reality Assessment of Panic Disorder (VRA-PD) that collected self-reported anxiety and HRV data [80]. A machine-learning model (CatBoost) integrating VR and clinical data achieved 85% accuracy in predicting early treatment response [80]. These methodologies highlight the trend toward ecologically valid, data-driven biomarker validation.
Biomarker Qualification Process
Post-Market Surveillance and Lifecycle Management
Obligations continue after a device reaches the market, and here the two systems diverge in their requirements.
FDA Requirements: The U.S. operates a largely reactive post-market surveillance system. Manufacturers must report device malfunctions and serious injuries or deaths through Medical Device Reporting (MDR) under 21 CFR 803 [91]. While quality system records and complaint handling are required, there is no mandatory requirement for periodic summary reports for most devices [91] [90].
IVDR Requirements: The EU system is more proactive and structured. All manufacturers must have a Post-Market Surveillance (PMS) Plan [91] [89].
- For Class A and B devices, a Post-Market Surveillance Report (PMSR) is required.
- For the higher-risk Class C and D devices, a Periodic Safety Update Report (PSUR) must be generated, which acts as a periodic summary of the device's safety and performance based on post-market data [90] [89].
- The IVDR also mandates Post-Market Performance Follow-up (PMPF) to actively update the performance evaluation with real-world data [90]. This reinforces the IVDR's emphasis on continuous evidence generation throughout the device's lifecycle.
Table 3: Comparison of Post-Market and Quality System Requirements
| Aspect | U.S. FDA | EU IVDR |
|---|---|---|
| Adverse Event Reporting | Medical Device Reporting (MDR) [91] | Vigilance reporting via EUDAMED [91] |
| Periodic Reporting | Not generally required [90] | PSUR for Class C/D, PMSR for Class A/B [90] |
| Performance Follow-up | Monitored through complaints and CAPA [93] | Post-Market Performance Follow-up (PMPF) required [90] |
| Quality Management System | 21 CFR Part 820 (QSR), aligning with ISO 13485 via QMSR [93] [91] | ISO 13485:2016 certification (mandatory) [91] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Translating a VR biomarker from a research concept into a regulatory-ready tool requires a suite of specialized technologies and materials. The following toolkit details essential components, drawing from validated experimental protocols in digital mental health research [1] [80].
Table 4: Essential Research Toolkit for VR Biomarker Development
| Tool/Reagent | Function in Research & Development |
|---|---|
| Immersive VR Platform | Creates standardized, ecologically valid environments to elicit and measure behavioral and physiological responses in a controlled manner [1] [80]. |
| Multimodal Biosignal Sensors (EEG, ECG, ET) | Collects objective physiological data (brain activity, heart rate variability, ocular motility) for identifying digital biomarkers correlated with mental states [1] [80]. |
| Data Synchronization Software (e.g., LSL) | Ensures precise temporal alignment between stimuli presented in the VR environment and the recorded physiological and behavioral data streams [1]. |
| Clinical Assessment Scales | Validated questionnaires (e.g., CES-D, PDSS) provide the clinical ground truth for training and validating machine learning models against standardized diagnostic criteria [1] [80]. |
| Machine Learning Frameworks | Enables the development of classification or predictive models (e.g., SVM, CatBoost) to identify patterns in multimodal data and define the biomarker signature [1] [80]. |
VR Biomarker Validation Workflow
Strategic Considerations for Global Development
A harmonized strategy is key to efficient global development. Researchers should note that while the FDA and IVDR are distinct, they are gradually aligning, particularly in Quality Management Systems (QMS). The FDA's move toward the Quality Management System Regulation (QMSR), which harmonizes 21 CFR Part 820 with ISO 13485, reduces divergence with the EU, where ISO 13485 certification is mandatory [93] [91].
Building a QMS that meets both FDA QSR and ISO 13485 requirements from the outset is a foundational step. Furthermore, creating a core "unified" technical file that contains all necessary evidence allows for more efficient adaptation for FDA submissions (e.g., 510(k)) and EU Technical Documentation for Notified Body review [91]. Engaging with regulators early via the FDA's Pre-Submission process is highly encouraged for novel devices to gain feedback on proposed testing strategies [87].
Conclusion
The validation of VR biomarkers marks a paradigm shift towards objective, quantitative, and ecologically valid assessment in mental health. The synthesis of evidence confirms that VR-derived metrics, particularly when fused with multimodal data and analyzed with machine learning, achieve diagnostic accuracy comparable to or even surpassing traditional methods. Key takeaways include the critical importance of multimodal integration, the need to address user-centric and technical barriers for clinical implementation, and the robust validation of these digital tools against gold-standard biomarkers. Future directions must focus on large-scale longitudinal studies to confirm long-term predictive value, the development of standardized protocols to ensure reproducibility, and the deep integration of VR biomarkers into the drug development pipeline to optimize patient stratification and treatment efficacy measurement. For biomedical research, this heralds a new era of precision psychiatry, enabling earlier intervention, more personalized therapeutic strategies, and a faster, more reliable path to bringing effective treatments to patients.
References
- 1. A virtual reality-based multimodal framework for adolescent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12484203/]
- 2. Key Features of Digital Phenotyping for Monitoring Mental ... [https://www.jmir.org/2025/1/e77331]
- 3. Integrating Biomarkers From Virtual Reality and Magnetic ... [https://www.jmir.org/2024/1/e54538/]
- 4. Integrating Biomarkers From Virtual Reality and Magnetic ... [https://www.sciencedirect.com/science/article/pii/S1438887124001845]
- 5. Biomarkers of Immersion in Virtual Reality Based on Features ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11119742/]
- 6. Clinical Virtual Reality: Emerging Opportunities for Psychiatry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6493092/]
- 7. Exploring the potential of virtual reality (VR) in mental ... [https://link.springer.com/article/10.1007/s10055-025-01181-6]
- 8. Group Cognitive Behavioral Therapy With Virtual Reality ... [https://mental.jmir.org/2025/1/e73815]
- 9. Impact of a Virtual Reality Intervention on Stigma, Empathy ... [https://mental.jmir.org/2025/1/e66925]
- 10. Virtual Reality: Challenges and Perspectives in Mental Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593772/]
- 11. A virtual reality system for delivery of military-specific ... [https://pubmed.ncbi.nlm.nih.gov/40470496/]
- 12. The implementation of digital biomarkers in the diagnosis, ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1595243/full]
- 13. Eye movement behavior in a real-world virtual reality task ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9700686/]
- 14. Eye Tracking in Virtual Reality: a Broad Review of ... [https://link.springer.com/article/10.1007/s10055-022-00738-z]
- 15. Evidence from comprehensive independent validation ... [https://www.nature.com/articles/s41598-024-64487-6]
- 16. Use of Virtual Reality in Psychiatric Diagnostic Assessments [https://pmc.ncbi.nlm.nih.gov/articles/PMC8918631/]
- 17. Impact of Virtual Reality Cognitive and Motor Exercises on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10002333/]
- 18. A Pilot Study on Emotional Equivalence Between VR and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12251632/]
- 19. Evaluating cognitive performance using virtual reality ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2023.1153145/full]
- 20. A Study on Baseline Estimation Methods for Emotion ... [https://www.sciencedirect.com/science/article/pii/S1877050925029965]
- 21. Psychological and physiological health outcomes of virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11526413/]
- 22. Correlation Study between Virtual Kiosk Test and EEG ... [https://www.mdpi.com/1424-8220/24/11/3543]
- 23. Digital Marker for Early Screening of Mild Cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10625097/]
- 24. Detection of mild cognitive impairment using a virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12335173/]
- 25. Innovations in dementia screening: a systematic review ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2025.1606562/full]
- 26. Virtual Reality for Enhanced Ecological Validity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4675850/]
- 27. Frontiers | Ecologically valid virtual reality-based technologies for assessment and rehabilitation of acquired brain injury: a systematic review [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2023.1233346/full]
- 28. Advancing ecological validity and clinical utility in virtual reality-based continuous performance test: exploring the effects of task difficulty and environmental distractors - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10832060/]
- 29. Ecological validity of VR experiments for psychological and ... [https://www.sciencedirect.com/science/article/abs/pii/S0360132325002495]
- 30. The comparison of teaching efficiency between virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7940910/]
- 31. A virtual reality-based multimodal framework for adolescent ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1655554/full]
- 32. Data-driven multimodal fusion: approaches and applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10734907/]
- 33. Simultaneous Dataset of Brain, Eye and Hand during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11785794/]
- 34. Using eye movements, electrodermal activities, and heart ... [https://www.nature.com/articles/s41598-025-03052-1]
- 35. Deep graph learning of multimodal brain networks defines ... [https://www.nature.com/articles/s41380-025-02974-6]
- 36. How virtual reality therapy is shaping mental health [https://www.nature.com/immersive/d41591-024-00032-2/index.html]
- 37. Alzheimer’s disease detection using deep learning and machine learning: a review | Artificial Intelligence Review [https://link.springer.com/article/10.1007/s10462-025-11258-y]
- 38. Alzheimer's disease digital biomarkers multidimensional ... [https://www.nature.com/articles/s41746-025-01640-z]
- 39. A Bibliometric Study of the Evidence About Applying Virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399854/]
- 40. An explainable machine learning approach for Alzheimer’s disease classification | Scientific Reports [https://www.nature.com/articles/s41598-024-51985-w]
- 41. Evaluation of machine learning models for the prediction of Alzheimer's: In search of the best performance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11850780/]
- 42. MarkerPredict: predicting clinically relevant ... [https://www.nature.com/articles/s41540-025-00603-0]
- 43. The evolving field of digital mental health: current evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079407/]
- 44. Biomarkers in exposure-based treatment of anxiety ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2024.1355082/full]
- 45. Virtual reality-based versus standard cognitive behavioral ... [https://www.nature.com/articles/s41591-025-03880-8]
- 46. Developing interactive VR-based digital therapeutics for ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1554394/full]
- 47. Study protocol for a phase 2 clinical trial - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10030076/]
- 48. Identifying EEG biomarkers of sense of embodiment in ... [https://www.frontiersin.org/journals/neuroergonomics/articles/10.3389/fnrgo.2025.1572851/full]
- 49. A virtual reality-based multimodal for framework ... adolescent [https://pubmed.ncbi.nlm.nih.gov/41040947/]
- 50. JMIR Formative Research - Detection of Depressive Symptoms in... [https://formative.jmir.org/2025/1/e67964]
- 51. A Dose-Finding, Biomarker Validation, and Effectiveness ... [https://pubmed.ncbi.nlm.nih.gov/39245178/]
- 52. Virtual Reality-Based Cognitive Behavior Therapy for Major ... [https://eymj.org/DOIx.php?id=10.3349/ymj.2024.0002]
- 53. Understanding Cybersickness and Presence in Seated VR [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027998/]
- 54. Cybersickness. A systematic literature review of adverse ... [https://www.sciencedirect.com/science/article/pii/S0213485322000664]
- 55. A quantitative comparison of virtual and physical ... [https://www.nature.com/articles/s41598-024-55253-9]
- 56. Performance of game sessions in VR vs standard 2D monitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11534712/]
- 57. Real-Time Applications of Biophysiological Markers in ... [https://www.mdpi.com/2673-7426/5/3/48]
- 58. Barriers to adopting therapeutic virtual reality - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11958971/]
- 59. Virtual reality as a clinical tool in mental health research and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7366939/]
- 60. Clinical adoption of virtual reality in mental health is ... [https://www.nature.com/articles/s44184-024-00069-8]
- 61. Considerations and practical protocols for using virtual ... [https://link.springer.com/article/10.3758/s13428-021-01543-3]
- 62. Automated Virtual Reality Cognitive Therapy for People ... [https://www.sciencedirect.com/org/science/article/pii/S1929074821001086]
- 63. Validation of an Upgraded Virtual Reality Platform ... [https://www.mdpi.com/2673-7426/5/1/4]
- 64. The State of Digital Biomarkers in Mental Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC11584197/]
- 65. Comparative Efficacy of Virtual Reality–Assisted Cognitive ... [https://www.researchprotocols.org/2025/1/e66112]
- 66. Virtual Reality in Mental Health | Research Update 2025 [https://huntingtonbeachmentalhealth.com/virtual-reality-in-mental-health-research-update-2025/]
- 67. The Effectiveness of Virtual Reality–Based Mindfulness ... [https://www.researchprotocols.org/2025/1/e68231]
- 68. Virtual reality analytics map (VRAM): A conceptual ... [https://www.sciencedirect.com/science/article/pii/S0732118X24000552]
- 69. In-home clinical uses of immersive tech will raise data ... [https://www.nextgov.com/emerging-tech/2025/09/-home-clinical-uses-immersive-tech-will-raise-data-privacy-questions-va-official-says/408021/]
- 70. What Are the Ethical Issues Surrounding Extended Reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561320/]
- 71. Biomarkers of Alzheimer's disease modification using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500584/]
- 72. Ethical considerations in implementing virtual reality ... [https://www.sciencedirect.com/science/article/pii/S2352552525000337]
- 73. The application of metaverse in mental health [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1463494/full]
- 74. Using Virtual Reality to Improve Outcomes Related ... [https://www.jmir.org/2025/1/e54452/]
- 75. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 76. A scoping review of remote and unsupervised digital ... [https://www.nature.com/articles/s41746-025-01583-5]
- 77. Integrating Biomarkers From Virtual Reality and Magnetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11063880/]
- 78. Comparative analysis of multiple deep learning models ... [https://www.nature.com/articles/s41598-025-27914-w]
- 79. Multi-Modal Fusion and Longitudinal Analysis for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11941453/]
- 80. Simulated virtual reality experiences for predicting early ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1684001/full]
- 81. Multimodal Machine Learning in Mental Health: A Survey ... [https://arxiv.org/html/2407.16804v2]
- 82. Generative multimodal large language models in mental ... [https://journals.plos.org/mentalhealth/article?id=10.1371/journal.pmen.0000488]
- 83. Virtual Reality Clinical Trials: Step Inside the Future of ... [https://ccrps.org/clinical-research-blog/virtual-reality-clinical-trials-step-inside-the-future-of-medicine-2025]
- 84. Relationship between demographic and social variables and ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-05180-0]
- 85. Evaluating the Clinical Validity of Commercially Available ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551044/]
- 86. A Validated Model of VR Acceptance to Inform Design in ... [https://www.mdpi.com/2571-9408/8/12/503]
- 87. Overview of IVD Regulation [https://www.fda.gov/medical-devices/ivd-regulatory-assistance/overview-ivd-regulation]
- 88. Step 3: Pathway to Approval [https://www.fda.gov/patients/device-development-process/step-3-pathway-approval]
- 89. IVDs – A Comparison of Requirements between the US and EU [https://blog.pqegroup.com/medical-device/ivds-a-comparison-of-requirements-between-the-us-and-eu]
- 90. A Comparison of IVDR to FDA IVD Regulatory Submission ... [https://www.rqmplus.com/blog/a-comparison-of-ivdr-to-fda-ivd-regulatory-submission-requirements/]
- 91. How Do You Comply with EU MDR/IVDR vs. U.S. FDA ... [https://avendium.com/2025/10/31/how-do-you-comply-with-eu-mdr-ivdr-vs-u-s-fda-regulations/]
- 92. About Biomarkers and Qualification [https://www.fda.gov/drugs/biomarker-qualification-program/about-biomarkers-and-qualification]
- 93. FDA medical device inspections in 2025: What we're ... [https://www.hoganlovells.com/en/publications/fda-medical-device-inspections-in-2025]