Active Sensing in Virtual Reality: Transforming Biomedical Research and Drug Discovery
This article explores the transformative role of Virtual Reality (VR) as an active sensing platform in biomedical research and drug development.
Active Sensing in Virtual Reality: Transforming Biomedical Research and Drug Discovery
Abstract
This article explores the transformative role of Virtual Reality (VR) as an active sensing platform in biomedical research and drug development. Targeting researchers, scientists, and pharmaceutical professionals, it details how VR enables the interactive exploration and manipulation of complex biological systems. The scope spans from foundational principles of VR-enabled active sensing to its methodological applications in molecular visualization and clinical trial optimization. It also addresses critical challenges in model fidelity and data integration, and provides a framework for validating VR systems against traditional methods, offering a comprehensive guide to leveraging immersive technologies for scientific advancement.
What is VR-Enabled Active Sensing? Core Principles for Scientific Inquiry
Defining Active Sensing in Virtual Environments
Active sensing represents a fundamental framework for understanding how intelligent agents strategically control their sensors to extract task-relevant information from their environment. In virtual environments, this process becomes both measurable and manipulable, offering unprecedented opportunities for research and application. This technical guide examines the core principles, mechanisms, and implementations of active sensing within virtual reality systems, with particular emphasis on applications in pharmaceutical research and drug development. By synthesizing computational theories with practical implementations, we provide researchers with a comprehensive framework for leveraging active sensing paradigms in virtual environments to advance scientific discovery.
Active sensing describes the closed-loop process whereby an agent directs its sensors to efficiently gather and process task-relevant information [1]. Unlike passive sensing, where information is received without deliberate sensor manipulation, active sensing involves strategic movements specifically designed to reduce uncertainty about environmental variables or system states. This paradigm has profound implications for virtual reality (VR) applications, where sensorimotor contingencies can be precisely controlled and measured.
The theoretical foundation of active sensing rests upon two complementary processes: perception, through which sensory information is processed to form inferences about the world, and action, through which agents select optimal sampling strategies to acquire useful information [1]. In virtual environments, this closed loop enables researchers to study and exploit the symbiotic relationship between movement and information gain under controlled conditions. The integration of active sensing principles with VR technologies is particularly transformative for domains requiring visualization and manipulation of complex 3D data, such as structure-based drug design [2] [3].
Theoretical Framework
Computational Foundations
Active sensing can be formally described as an approximation to the general problem of exploration in reinforcement learning frameworks [1]. The process involves an ideal observer that extracts task-relevant information from sensory inputs, and an ideal planner that specifies actions leading to the most informative observations [1].
The mathematical formulation centers on the Bayesian ideal observer, which performs inference about environmental states using Bayes' rule:
ℙ(x|z₀:t,M) ∝ ℙ(z₀:t|x,M)ℙ(x|M)
where x represents environmental states, z₀:t represents sensory inputs from time 0 to t, and M represents the internal model of the environment and sensory apparatus [1].
Information Maximization Principle
A fundamental proxy for evaluating action selection in active sensing is Shannon information, which quantifies the expected reduction in uncertainty about state x:
ℐ(x,zₜ₊₁|a) = ℋ(x|z₀:t,M) - ⟨⟨ℋ(x|z₀:t₊₁,M)⟩ℙ(zₜ₊₁|a,x,M)⟩ℙ(x|z₀:t,M)
where ℋ(x) represents the entropy of the probability distribution ℙ(x), quantifying uncertainty about x [1]. The information-maximizing ideal planner simply selects the action a that maximizes this information gain:
aₜ₊₁ = argmaxₐ ℐ(x,zₜ₊₁|a)
This formalization provides a principled approach to understanding how virtual agents can optimize their sensing strategies to extract maximal information from their environments.
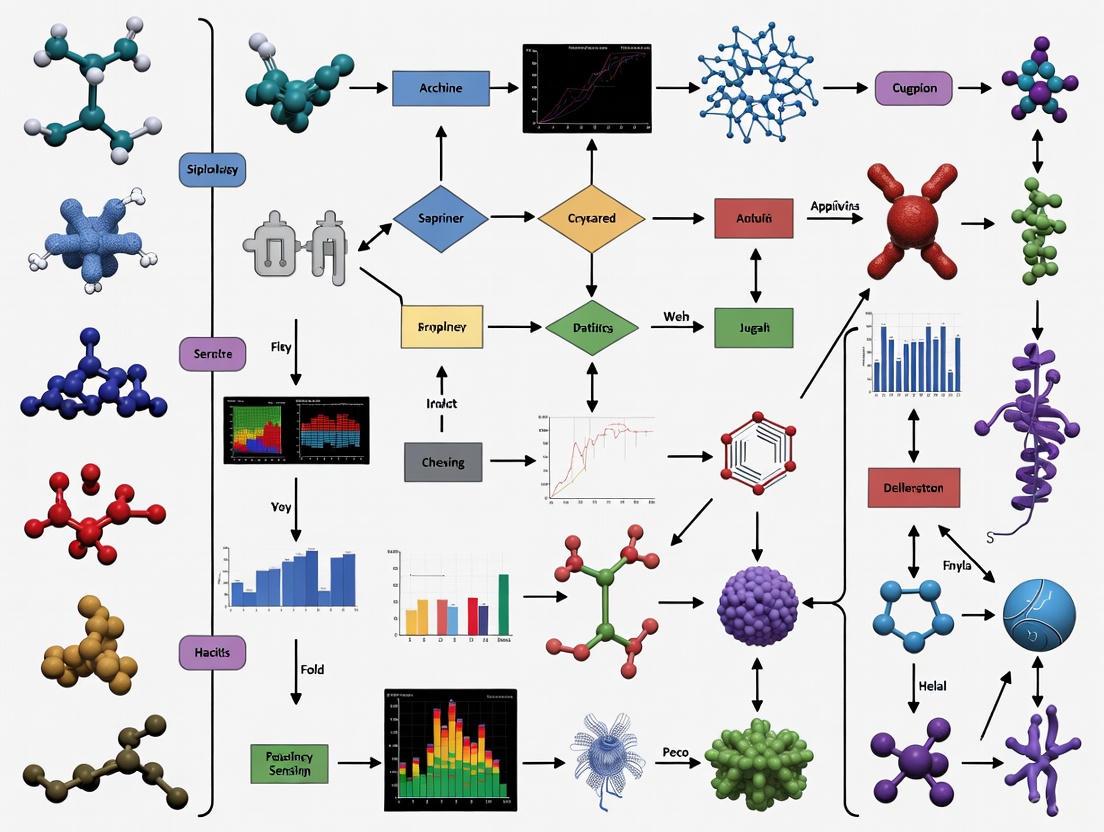
Figure 1: Active Sensing Closed-Loop Framework. This diagram illustrates the fundamental perception-action cycle underlying active sensing, where beliefs inform actions that modify sensory inputs.
Active Sensing in Virtual Reality Systems
Implementation in Immersive Environments
Virtual reality implementations of active sensing leverage head-mounted displays (HMDs) and motion tracking systems to create controlled sensorimotor loops [4]. Multi-user VR platforms further extend these capabilities by enabling collaborative active sensing scenarios, where multiple agents can simultaneously gather and share information within shared virtual spaces [5]. These platforms have proven particularly valuable in industrial contexts, where they facilitate intuitive exploration of complex data structures [4].
In pharmaceutical applications, VR enables researchers to visualize and manipulate molecular structures in three dimensions, engaging in active sensing behaviors such as rotating protein-ligand complexes, examining binding sites from multiple viewpoints, and simulating molecular dynamics through controlled movements [2] [3]. This immersive interaction paradigm transforms how scientists extract information from complex biochemical data.
Levels of Interaction in Drug Design
Three distinct levels of interaction characterize active sensing applications in structure-based drug design within virtual environments [2] [3]:
Level 1: Visualization and Inspection - Researchers manipulate viewpoint and orientation to examine molecular structures from optimal angles, employing natural head and hand movements to resolve spatial ambiguities.
Level 2: Molecular Manipulation - Users directly manipulate molecular components through gesture-based controls, testing hypotheses about binding affinities and structural compatibilities through purposeful sensorimotor engagement.
Level 3: Dynamic Simulation Control - Experts actively control parameters of molecular dynamics simulations, strategically sampling conformational spaces to identify stable binding configurations and reaction pathways.
Table 1: Active Sensing Interaction Levels in VR Drug Design
| Interaction Level | Primary Sensing Actions | Information Gained | Technical Requirements |
|---|---|---|---|
| Visualization & Inspection | Viewpoint manipulation, rotation, zoom | Spatial relationships, molecular geometry | 3D visualization, head tracking |
| Molecular Manipulation | Direct manipulation, docking, positioning | Binding compatibility, steric constraints | Hand tracking, haptic feedback |
| Dynamic Simulation Control | Parameter adjustment, sampling strategy | Energy landscapes, kinetic properties | Real-time simulation, interactive rendering |
Experimental Protocols and Methodologies
BOUNDS Computational Pipeline
The BOUNDS (Bounding Observability for Uncertain Nonlinear Dynamic Systems) pipeline provides a empirical methodology for quantifying how sensor movement contributes to estimation performance in active sensing scenarios [6]. This approach is particularly valuable for analyzing active sensing in virtual environments, where state trajectories can be precisely recorded and analyzed.
Protocol Implementation:
State Trajectory Collection - Record time-series state trajectories (X̃) comprising sequences of observed state vectors (x̃ₖ) that describe agent/sensor movement and environmental variables in the virtual environment [6].
Model Definition - Define a model incorporating: (i) inputs controlling locomotion, (ii) basic physical properties, and (iii) sensory dynamics representing what the agent measures [6].
Observability Matrix Calculation - Compute the empirical observability matrix (O) for nonlinear systems using measured or simulated state trajectories [6].
Fisher Information Matrix Computation - Calculate the Fisher information matrix (F) associated with O to account for sensor noise properties [6].
Cramér-Rao Bound Application - Apply the Cramér-Rao bound under rank-deficient conditions to quantify observability with meaningful units [6].
Active Sensing Motif Identification - Iterate the pipeline along dynamic state trajectories to identify patterns of sensor movement that increase information for individual state variables [6].
Figure 2: BOUNDS Computational Pipeline. This workflow illustrates the empirical process for quantifying observability and identifying active sensing patterns in virtual environments.
Systematic Evaluation Framework
Comprehensive assessment of human factors in VR active sensing environments requires standardized methodologies [4]. A systematic literature review approach based on PRISMA 2020 guidelines can identify and categorize key evaluation metrics and experimental designs [4].
Experimental Design Protocol:
Research Question Formulation - Define specific questions addressing how human factors influence and are influenced by active sensing in VR environments [4].
Search Strategy Implementation - Execute structured searches across electronic databases using tailored search equations combining terms for: (i) virtual reality/VR, (ii) industry 4.0/5.0 context, (iii) human factors/cognition/UX, and (iv) evaluation/assessment [4].
Study Selection - Apply inclusion/exclusion criteria focusing on peer-reviewed journal articles within appropriate timeframes relevant to current VR technological capabilities [4].
Data Extraction and Synthesis - Extract data on human factors, metrics, and experimental outcomes, then synthesize to identify patterns and relationships [4].
Quality Assessment - Evaluate selected studies for potential biases and methodological limitations [4].
Applications in Pharmaceutical Research
Molecular Visualization and Manipulation
Virtual reality active sensing systems enable researchers to visualize and manipulate complex molecular structures in immersive 4D environments [2] [3]. This capability transforms structure-based drug design by allowing intuitive exploration of protein-ligand complexes through natural sensorimotor interactions [2]. Case studies in COVID-19 research have demonstrated VR's potential for rapid molecular structure analysis, where researchers actively sensed structural features of viral proteins to identify potential drug targets [2] [3].
The active sensing paradigm in molecular visualization allows researchers to employ embodied cognition strategies, using physical movements to resolve spatial ambiguities that remain opaque in traditional 2D representations. This approach leverages human spatial reasoning capabilities to solve complex structural biological problems through strategic viewpoint control and molecular manipulation [2].
Industrial Perspectives and Implementation Challenges
Conversations with pharmaceutical industry experts reveal cautious optimism about VR's potential in drug discovery, while highlighting significant implementation challenges [2] [3]. Key barriers include integration with existing workflows, hardware ergonomics, and establishing synergistic relationships between VR and expanding artificial intelligence tools [2].
Industry professionals identify active sensing interfaces as particularly promising for collaborative drug design sessions, where multi-user VR environments enable research teams to collectively explore molecular interactions and formulate structural hypotheses [3]. However, widespread adoption requires addressing technical challenges related to simulation fidelity, interaction precision, and seamless integration with computational chemistry pipelines [2] [3].
Table 2: Active Sensing Applications in Pharmaceutical Research
| Application Domain | Active Sensing Actions | Research Impact | Implementation Status |
|---|---|---|---|
| Protein-Ligand Docking | Molecular rotation, binding site exploration | Improved understanding of binding mechanisms | Research validation |
| Structure-Based Drug Design | Conformational sampling, interactive modification | Accelerated lead optimization | Early adoption |
| COVID-19 Research | Spike protein analysis, binding site identification | Rapid target identification | Case studies demonstrated |
| Collaborative Drug Design | Multi-user molecular inspection, shared perspective control | Enhanced team-based problem solving | Prototype development |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Active Sensing in Virtual Environments
| Tool Category | Specific Solutions | Function in Active Sensing Research |
|---|---|---|
| VR Hardware Platforms | Meta Quest, HTC Vive, Sony PlayStation VR | Provide immersive display and tracking capabilities for sensorimotor loops [4] |
| Multi-User VR Platforms | Custom collaborative environments | Enable shared active sensing experiences for team-based research [5] |
| Molecular Visualization Software | Custom VR-enabled molecular viewers | Facilitate 3D manipulation of chemical structures [2] [3] |
| Observability Analysis Tools | BOUNDS/pybounds Python package | Quantify information gain from sensor movements [6] |
| Motion Tracking Systems | Inside-out tracking, lighthouse systems | Capture precise movement data for sensing action analysis [4] |
| Data Analysis Frameworks | Fisher information calculators, Bayesian estimators | Process sensor data and quantify information extraction [1] [6] |
Future Directions and Research Opportunities
The convergence of active sensing principles with virtual reality technologies presents numerous research opportunities across scientific domains. In pharmaceutical research, developing more sophisticated molecular manipulation interfaces that provide haptic feedback and physicochemical simulation capabilities represents a promising direction [2]. Integration with artificial intelligence systems creates opportunities for hybrid intelligence approaches, where human active sensing strategies complement machine learning algorithms in analyzing complex biological data [2] [3].
Advancements in hardware ergonomics and display technologies will address current limitations in resolution, field of view, and comfort, enabling longer, more productive active sensing sessions [4]. Standardized assessment frameworks for evaluating human factors in VR active sensing environments will facilitate more systematic research and application development [4].
From a computational perspective, extending the BOUNDS framework to handle increasingly complex state estimation problems will expand applications in virtual environment design and analysis [6]. The Augmented Information Kalman Filter (AI-KF) approach, which combines data-driven state estimation with model-based filtering, demonstrates how active sensing principles can be implemented in practical estimation algorithms [6].
As these technologies mature, active sensing in virtual environments is poised to transform research methodologies across scientific disciplines, particularly in complex 3D data analysis domains like drug discovery, structural biology, and materials science [2] [3].
The study of human perception and behavior has long relied on passive observation paradigms, where data is collected from subjects reacting to static, laboratory-controlled stimuli. This whitepaper delineates a fundamental paradigm shift toward interactive manipulation, enabled by advanced virtual reality (VR) technologies and sophisticated sensing techniques. Within VR environments, participants are no mere observers but active agents whose sensing and manipulation behaviors can be tracked, quantified, and analyzed in real-time. This shift is critically examined through its application in affective computing and immersive analytics, demonstrating enhanced ecological validity, richer data acquisition, and the emergence of novel experimental frameworks for researchers and drug development professionals.
Traditional research methodologies in neuroscience and psychology have been dominated by passive induction paradigms. In these settings, subjects are exposed to stimuli—such as images or videos on a screen—while their physiological responses are measured. While controlled, this approach lacks ecological validity; the induced emotional changes differ significantly from the active, self-generated emotions experienced in real-world scenarios [7]. This limitation poses a significant challenge for fields like drug development, where understanding genuine human responses is paramount.
The integration of Virtual Reality (VR) marks a transition to active induction paradigms. VR provides a highly immersive and realistic virtual environment, allowing for the assessment of emotional experiences and behaviors in a more naturalistic context [7]. This evolution from passive observation to interactive manipulation represents a profound methodological shift. It moves the subject from a reactive entity to an active participant who can sense, manipulate, and alter a virtual environment, thereby generating a richer, more complex, and ecologically valid dataset for analysis. This whitepaper explores the technical underpinnings, experimental evidence, and practical implementations of this shift.
Theoretical Foundations: From Passive to Active Paradigms
The distinction between passive and active research paradigms is foundational to this discussion.
Passive Observation Paradigms: Characterized by a one-directional flow of information. The laboratory environment presents a stimulus, and the researcher measures the subject's response using tools like Electroencephalography (EEG) or functional Magnetic Resonance Imaging (fMRI). This method is often critiqued for its weak induction effects and its disconnection from the complexities of real-life situations [7]. The data acquired, while precise, may not fully capture the dynamism of natural human behavior.
Interactive Manipulation Paradigms: Founded on the principles of active sensing, where perception is guided by action. In a VR environment, participants use motor actions to control sensing apparatuses. For instance, they might turn their heads to look around a virtual space or use haptic controllers to manipulate virtual objects. This process generates a closed-loop feedback system between the participant and the environment [8]. This paradigm provides a highly immersive experience, evoking emotions and behaviors more naturally and authentically [7]. It allows researchers to study not just the final response, but the entire process of sensory-guided motor planning and execution.
Experimental Evidence: Quantitative Comparisons
The superiority of active, VR-based paradigms is supported by empirical evidence across multiple domains. The table below summarizes key quantitative findings from comparative studies.
Table 1: Quantitative Comparison of Passive vs. Active VR Research Paradigms
| Research Domain | Experimental Task | Key Metric | Passive Paradigm Result | Active VR Paradigm Result | Significance & Context |
|---|---|---|---|---|---|
| EEG Emotion Recognition [7] | Emotion classification using EEG signals | Classification Performance | High performance on lab-collected data, but lacks ecological validity and transferability. | Robust classification performance; model (EmoSTT) transferred well between different emotion elicitation paradigms. | The VR-based active paradigm provides data that leads to more generalizable and robust computational models. |
| Graph Data Analytics [9] | Cluster search task in a graph | Task Efficiency & Error Rate | Efficient manipulation on 2D touch displays, but limited by display space and lack of immersion. | More efficient task performance with user-controlled transformation; lower error rates with constant transformation. | User-controlled manipulation in immersive 3D space enhanced task efficiency, demonstrating the value of interactive exploration. |
| Crowd Dynamics Research [5] | Study of pedestrian movement patterns | Data Validity & Control | Field observations (video) have high external validity but lack control and are difficult to quantify. | Controlled experiments with high external validity; enables study of dangerous scenarios safely. | VR provides an optimal balance between experimental control and ecological validity for complex behavioral studies. |
Detailed Experimental Protocol: EEG-Based Emotion Recognition in VR
The following protocol outlines the methodology for conducting an active paradigm emotion recognition study, as exemplified in the research by Beihang University [7].
1. Objective: To collect electroencephalography (EEG) data correlated with emotional states elicited within an immersive Virtual Reality environment.
2. Materials and Reagents: - VR Head-Mounted Display (HMD): A high-fidelity HMD (e.g., Meta Quest 3, Apple Vision Pro) capable of rendering immersive videos. - EEG Acquisition System: A multi-channel EEG system with a compatible electrode cap (e.g., 32 or 64 channels). - Stimuli: A curated set of 360-degree VR videos designed to elicit specific emotional states (e.g., joy, fear, calmness). - Software: VR presentation software, EEG recording software, and data analysis platforms (e.g., Python with MNE, EEGLAB).
3. Experimental Procedure: - Step 1: Participant Preparation. Recruit participants according to the approved ethical guidelines. After obtaining informed consent, fit the participant with the EEG electrode cap, ensuring impedances are below 5 kΩ. Then, equip the participant with the VR HMD. - Step 2: Baseline Recording. Record a 5-minute resting-state EEG with eyes open and closed in a neutral VR environment (e.g., a plain, virtual room). - Step 3: VR Stimulus Presentation. Present the series of VR videos to the participant in a randomized or counterbalanced order. Each video segment should be followed by a self-assessment manikin (SAM) questionnaire where the participant rates their emotional experience. - Step 4: Data Synchronization. Ensure precise synchronization between the EEG data stream, the VR stimulus markers (e.g., start/end of each video), and the behavioral responses from the questionnaire. - Step 5: Data Preprocessing. Process the raw EEG data, which includes: - Filtering (e.g., 0.5-50 Hz bandpass, 50/60 Hz notch filter). - Bad channel removal and interpolation. - Ocular and muscular artifact correction using algorithms like Independent Component Analysis (ICA). - Epoching the data into 1-second segments. - Step 6: Feature Extraction. For each epoch, apply the Short-Time Fourier Transform (STFT) to compute frequency-domain features. Extract Differential Entropy (DE) features from the five standard frequency bands: δ (1-3Hz), θ (4-7Hz), α (8-13Hz), β (14-30Hz), and γ (31-50Hz) [7]. - Step 7: Model Training and Analysis. The DE features (shape: N samples × T time frames × C channels × F frequency bands) are used to train a spatial and temporal Transformer model (EmoSTT) to decode emotional states, comparing its performance against models trained on passive paradigm data.
Technical Implementation: Enabling Technologies
The shift to interactive manipulation is powered by advances in several key technological areas.
Haptic Sensing and Feedback
Haptic interaction is a cornerstone of active manipulation, comprising two main functions:
- Haptic Sensing: Artificial tactile sensors gather information from physical contact. Based on mechanisms like piezoresistive, capacitive, and piezoelectric effects, these sensors can detect force, pressure distribution, and even identify textures [8]. In VR, they are used for gesture recognition and touch identification, translating real-world actions into virtual commands.
- Haptic Feedback: This is the reverse process, where devices stimulate the skin to evoke tactile sensations. Techniques include:
- Mechanical Vibration: Actuators provide vibrotactile feedback, targeting Meissner corpuscles (FA-I, 10-50 Hz) for light contact and texture, and Pacinian corpuscles (FA-II, 200-300 Hz) for high-frequency vibrations [8].
- Dielectric Elastomer Actuators (DEAs): These soft actuators can produce controllable deformations to simulate touch.
- Electrotactile (ET) Display: Uses electrical currents to stimulate nerve endings directly, creating tactile feelings.
Table 2: The Scientist's Toolkit - Key Research Reagent Solutions
| Item Name | Function / Application in Research |
|---|---|
| High-Density EEG System | Records electrical brain activity with high temporal resolution, essential for capturing neural correlates of active tasks in VR [7]. |
| Video-Based See-Through HMD | Provides the immersive VR/AR environment; video pass-through allows for seamless blending of real and virtual elements (Cross-Reality) [9]. |
| Haptic Sensing Glove | Equipped with tactile sensor arrays to capture hand gestures, touch force, and manipulation kinematics for virtual object interaction [8]. |
| Galvanic Skin Response (GSR) Sensor | Measures electrodermal activity as a proxy for physiological arousal and stress, often used in conjunction with VR behavioral analysis [10]. |
| Eye-Tracking Module (Integrated in HMD) | Monitors gaze direction and pupillometry, providing insights into visual attention and cognitive load during interactive tasks [10]. |
| Spatial-Temporal Transformer Model (EmoSTT) | A deep learning architecture specifically designed to model both the temporal dynamics and spatial relationships of physiological signals like EEG for robust state classification [7]. |
Sensor Fusion and Lightweight Sensing Architectures
A key development is the move away from complex, multi-sensor setups to more streamlined architectures. The Sensor-Assisted Unity Architecture exemplifies this: it uses VR as the primary sensing platform for behavioral analysis (e.g., head movement, interaction logs) and supplements it with a minimal number of physiological sensors, such as a GSR sensor [10]. This approach reduces system complexity and cost while maintaining high data quality by focusing on the most informative signals.
Data Visualization and Transformation
Interactive manipulation also extends to data exploration. Research shows that transforming 2D data visualizations into 3D Augmented Reality (AR) space can enhance understanding. Parameters such as transformation methods (e.g., user-controlled vs. constant), node transformation order, and visual interconnection (e.g., using "ghost" visuals of the original 2D view) are critical for helping users build a coherent mental model of their data when shifting from a 2D display to an interactive 3D manipulation space [9].
Visualization of Core Workflows
The following diagrams, generated with Graphviz, illustrate the core logical and workflow relationships described in this whitepaper.
Active Sensing Research Paradigm
Diagram 1: Active sensing research paradigm workflow.
Sensor-Assisted VR Architecture
Diagram 2: Sensor-assisted VR architecture for data collection.
Virtual Reality (VR) has transcended its origins in entertainment to become a pivotal tool in scientific research, particularly in the field of active sensing, which is fundamental to pharmaceutical development. Active sensing describes the purposeful acquisition of sensory information to guide behavior. In the context of drug discovery, researchers act as active sensors, using their expertise to probe and understand the three-dimensional (3D) interaction between drug molecules and their biological targets. VR technologies directly augment this human-centered research process. This whitepaper details how three key technological enablers—haptic feedback, motion tracking, and real-time rendering—create immersive, interactive environments that empower scientists to conduct research intuitively and with unprecedented spatial understanding. By bridging the gap between abstract data and tangible experience, these technologies are revolutionizing the design and discovery of new therapeutic compounds.
Haptic Feedback: Conveying Molecular Interactions
Haptic feedback technology aims to replicate the sense of touch, providing critical tactile and force feedback that is essential for a researcher interacting with virtual molecular models. This transforms the drug design process from a visual exercise into a multi-sensory experience.
Technological Foundations and Recent Advances
Most commercial haptic technologies are limited to simple vibrations, which fall short of conveying the complex forces involved in molecular docking. The sense of touch in human skin involves different mechanoreceptors sensitive to pressure, vibration, and stretching. Reproducing this sophistication requires precise control over the type, magnitude, and timing of stimuli [11].
A significant recent advancement is the development of a compact, wireless haptic actuator with Full Freedom of Motion (FOM). This device can apply forces in any direction—pushing, twisting, and sliding—against the skin, rather than merely poking it. By combining these actuators into arrays, the technology can reproduce sensations as varied as pinching, stretching, and tapping [11]. These devices include an accelerometer to track orientation and movement, enabling context-aware haptic feedback. For instance, the friction of a virtual finger moving across different molecular surfaces can be simulated by altering the direction and speed of the actuator's movement [11].
Application in Pharmaceutical Active Sensing
In active sensing research, advanced haptics allows a scientist to "feel" the interaction between a drug candidate and a protein binding pocket. The repulsive forces from steric clashes, the attractive forces of hydrogen bonds, or the smooth sliding along a hydrophobic patch can be rendered as tangible sensations. This provides an intuitive understanding of molecular fit and stability that is difficult to glean from a 2D screen, dramatically enhancing the researcher's role as an active sensor in the virtual environment [11].
Table 1: Quantitative Data for Advanced Haptic Actuators
| Parameter | Specification / Capability | Research Implication |
|---|---|---|
| Form Factor | Compact, millimeter-scale, wearable [11] | Can be placed anywhere on the body or integrated into gloves. |
| Actuation Type | Full Freedom of Motion (FOM) [11] | Simulates push, pull, twist, and slide forces for complex texture and force feedback. |
| Force Control | Precise control via magnetic field interaction with a tiny magnet [11] | Enables fine manipulation of virtual molecular objects. |
| Sensory Engagement | Engages multiple mechanoreceptors (pressure, vibration, stretch) [11] | Creates a nuanced and realistic sense of touch for molecular interactions. |
| Connectivity | Wireless, Bluetooth [11] | Allows for unencumbered movement in a VR space. |
Motion Tracking: Capturing and Translating Researcher Movement
Precise motion tracking is the cornerstone of immersion, ensuring that a researcher's physical movements are accurately mirrored by their virtual avatar or hands. This creates a direct, one-to-one correspondence between human action and virtual reaction, which is critical for precise manipulation of 3D molecular structures.
Tracking Modalities and Performance Metrics
Multiple technological approaches exist for motion tracking, each with distinct advantages:
- Inside-Out Tracking (HMD-Based): Used in headsets like Meta Quest and HTC Vive, this method relies on cameras and sensors on the headset itself to map the environment and track movement. It offers a good balance of ease of use, display quality, and affordability, making it accessible for research labs [12].
- Outside-In Tracking (External Sensor-Based): Systems like OptiTrack use external cameras placed around a room to track reflective or active LED markers. This provides superior, sub-millimeter accuracy and ultra-low latency, which is essential for applications requiring the highest precision. These systems are also "drift-free," meaning their calibration does not degrade over time, unlike some IMU-based systems [13].
- Inertial Measurement Unit (IMU) Tracking: Systems like SlimeVR full-body trackers use onboard IMUs (Inertial Measurement Units) to track their own rotation without external cameras or base stations. While susceptible to yaw drift over time, this drift can be easily reset with a gesture or keypress [14].
- Camera-Based AI Tracking: Solutions like Driver4VR leverage the power of artificial intelligence and a standard smartphone or webcam to infer body pose through deep learning, providing an accessible entry point for full-body tracking [15] [16].
Table 2: Comparative Analysis of Motion Tracking Technologies
| Tracking Technology | Accuracy & Latency | Key Advantage | Best-Suited Research Application |
|---|---|---|---|
| Inside-Out (HMD) | Moderate accuracy, low latency [12] | Ease of setup and use; wireless freedom [12] | Collaborative molecular visualization; routine drug design ideation [17] |
| Outside-In (Optical) | Sub-millimeter accuracy, very low latency [13] | High precision for complex manipulations; drift-free [13] | Detailed molecular docking studies; high-fidelity simulation and training |
| IMU-Based (e.g., SlimeVR) | Rotation-only tracking; susceptible to drift [14] | No external hardware required; not susceptible to occlusion [14] | Supplementary tracking for body posture in large-scale virtual labs |
| Camera/AI (e.g., Driver4VR) | Lower accuracy, higher latency | Very low cost; utilizes existing hardware (phone/webcam) [15] | Prototyping and exploring full-body tracking applications |
Experimental Protocol: Molecular Docking with Interactive Manipulation
The following workflow, derived from published studies, outlines how precise motion tracking is utilized in a drug design experiment using Interactive Molecular Dynamics in VR (iMD-VR) [18].
Diagram 1: Motion tracking workflow for iMD-VR.
Methodology:
- System Setup: The researcher dons a VR headset (e.g., Meta Quest) with hand controllers, and the tracking system (either inside-out or outside-in) is calibrated [17] [18].
- Environment Loading: The target protein (e.g., influenza neuraminidase) and drug molecule are loaded into the iMD-VR software, which renders them as 3D objects in the virtual space [18].
- Docking Procedure: The researcher uses physically tracked hand movements to grab the virtual drug molecule, position it near the protein's binding site, and manipulate it in 3D space. The tracking system relays the precise position and rotation of the researcher's hands to the software in real time [18].
- Interaction and Analysis: The researcher can push, pull, and rotate the drug to find the optimal binding conformation. The software provides real-time computational feedback on binding energies and molecular forces [18]. This entire unbinding and rebinding process can be achieved interactively in under five minutes of real time [18].
Real-Time Rendering: Visualizing Complex Data in 3D
Real-time rendering is the computational process of generating photorealistic or scientifically accurate 3D imagery instantaneously as the user interacts with the environment. For active sensing in drug discovery, it transforms complex molecular data into visual forms that researchers can intuitively explore and understand.
Technology and Impact on Spatial Awareness
Modern VR systems leverage powerful graphics processing units (GPUs) to render high-fidelity virtual worlds with high-resolution textures, dynamic lighting, and high frame rates essential for user comfort and immersion [19]. Standalone headsets like the Meta Quest 3 have been crucial in making this technology accessible, offering sufficient processing power to visualize multiple protein structures simultaneously without a tethered PC [17].
The primary value for pharmaceutical research lies in enhancing spatial awareness. Traditional methods rely on 2D screens, physical models, or imagination to comprehend 3D molecular interactions. Real-time rendering places the scientist inside the structure, allowing them to walk around a protein, look into active sites, and perceive depth and spatial relationships directly. This has been shown to help chemists create "better" drugs by improving their understanding of the spatial arrangement between molecules and their targets [17]. Studies using software like Nanome on Meta Quest headsets have demonstrated that after a short orientation, design teams can independently build and manipulate immersive molecular models [17].
Research Reagent Solutions: Essential Materials for VR-Enabled Drug Design
The following table details key hardware and software "reagents" required to establish a VR-based active sensing platform for pharmaceutical research.
Table 3: Key Research Reagents for VR-Enabled Drug Design
| Item Name | Function / Application | Example in Use |
|---|---|---|
| Standalone VR Headset | Provides the immersive visual interface and onboard processing for untethered operation. | Meta Quest series used for collaborative molecular design with Nanome software [17]. |
| Interactive MD-VR Software | Enables real-time manipulation and simulation of molecules with physics-based feedback. | University of Bristol's iMD-VR for docking drugs into proteins like HIV protease [18]. |
| Collaborative VR Platform | Allows multiple researchers in different locations to share and manipulate the same virtual models. | Nanome software used by LifeArc to bring chemists from London and Lithuania together in a virtual lab [17]. |
| Haptic Feedback Actuators | Provides tactile sensation to simulate molecular forces like repulsion and bond formation. | Northwestern University's FOM actuators to simulate the feeling of touching different molecular surfaces [11]. |
| Precision Tracking System | Captures user movement with high accuracy for precise manipulation of virtual objects. | OptiTrack systems for sub-millimeter tracking in research requiring the highest precision [13]. |
Integrated Experimental Protocol: A Collaborative Drug Design Session
This protocol synthesizes the three enabling technologies into a single, cohesive workflow for a collaborative drug design session, based on the documented practices of organizations like LifeArc [17].
Diagram 2: Collaborative drug design workflow.
Methodology:
- Session Initiation: Multiple researchers from different geographical locations don their VR headsets and join a shared virtual room using a platform like Nanome. Their movements are tracked, and their avatars are represented in the space [17].
- Data Integration and Rendering: The target protein structure and relevant molecular data (e.g., from assays or computational models) are loaded and rendered in 3D in the center of the virtual space. Real-time rendering ensures all participants see the model from their own perspective [17].
- Collaborative Ideation and Manipulation: One researcher ("Driver") takes control of a drug molecule. Using precise motion tracking, they grab and position the molecule into the protein's binding site. Other participants can observe from the same viewpoint and provide real-time verbal feedback or use virtual annotations to suggest modifications [17].
- Multi-Sensory Feedback Loop: As the drug is manipulated, real-time simulation calculations run in the background. The rendering engine visually updates the model, while haptic actuators (if available) provide force feedback based on molecular interactions. This creates a tight loop where the researcher's active sensing is guided by immediate visual and tactile cues [18].
- Output and Iteration: Promising molecular designs are saved directly from the virtual session. The team can rapidly iterate on designs, with changes incorporated and visualized in real-time, significantly accelerating the ideation process compared to traditional methods [17]. This integrated approach has been reported to yield a 10-fold gain in efficiency for method transfer and design tasks [20].
Haptic feedback, motion tracking, and real-time rendering are not isolated technologies; they are deeply interconnected enablers of a new paradigm for active sensing in pharmaceutical research. Together, they create a synthetic environment where the intricate, 3D nature of molecular interactions can be perceived, manipulated, and understood with human intuition and skill. By effectively placing the scientist inside the data, these technologies enhance spatial awareness, enable true collaborative exploration, and dramatically accelerate the iterative process of drug design. As these technologies continue to advance—becoming more affordable, higher-fidelity, and more deeply integrated with computational simulation—their role in unlocking new therapeutic discoveries will only grow more critical.
The ability to comprehend complex, multi-dimensional data is paramount in fields such as drug development and active sensing research. Traditional visualization methods often fall short in conveying the intricate spatial relationships inherent in such datasets. Immersive technologies, particularly Virtual Reality (VR) and Mixed Reality (MR), are emerging as transformative tools that leverage the human brain's innate capacities for spatial reasoning to overcome these limitations. Framed within the broader context of active sensing—where an agent selectively gathers sensory information to guide its actions in an environment—immersive visualization creates a closed-loop system. In this system, researchers can actively explore data, and their movements and decisions within the virtual space in turn shape the information they perceive [21]. This article details the theoretical foundations, supported by empirical evidence and experimental protocols, that explain how immersion fundamentally enhances the spatial understanding of complex data.
Theoretical Foundations of Immersive Spatial Understanding
The efficacy of immersive visualization is rooted in several interconnected cognitive and technological principles.
Multimodal Perception and Interaction
Immersive visualization utilizes VR, MR, and interactive devices to create a novel visual environment that integrates multimodal perception and interaction [21]. Unlike traditional screens, immersive environments engage multiple sensory channels—visual, auditory, and sometimes haptic—in a coordinated manner. This multisensory input is crucial for building robust mental models of complex data, as it mirrors the way humans naturally perceive and interact with the physical world. The integration of perception and action allows researchers to actively sense their data environment, testing hypotheses through physical navigation and manipulation rather than passive observation [21].
Ecological Validity and Embodied Cognition
A core strength of immersive environments is their high ecological validity; they can present complex data within a context that closely mimics real-world scenarios or effectively represents abstract data spaces [22]. This is closely tied to the theory of embodied cognition, which posits that cognitive processes are deeply rooted in the body's interactions with the world. In an immersive setting, a researcher's physical movements—such as walking around a molecular structure or using hand gestures to manipulate a dataset—facilitate deeper cognitive engagement and understanding. This embodied experience is a direct analogue to active sensing, where perception is guided by action [23].
Enhanced Spatial Memory Encoding
Spatial memory, the cognitive ability to retain and recall the configuration of one's surroundings, is fundamental to navigation and environmental awareness [23]. Research indicates that immersive technologies are particularly effective at engaging the hippocampus and entorhinal cortex, brain regions critical for spatial memory and among the first affected in neurodegenerative diseases like Alzheimer's [23]. By presenting data in a full 3D, navigable space, immersion promotes the same neural mechanisms used for real-world navigation, leading to more durable and accessible memory traces of the data's spatial layout [23].
Empirical Evidence and Quantitative Data
The theoretical principles are supported by a growing body of empirical evidence. The table below summarizes key findings from recent research on the application of immersive technologies to spatial tasks.
Table 1: Empirical Evidence for Immersion in Spatial Understanding
| Study Focus | Technology Used | Key Spatial Metric | Reported Outcome | Citation |
|---|---|---|---|---|
| Spatial Memory Assessment | Immersive VR (HMD) | Path Integration, Object-Location Memory | Higher diagnostic sensitivity for Mild Cognitive Impairment (MCI) than traditional paper-and-pencil tests. | [23] |
| User Comfort & Behaviour | Immersive Virtual Office | Sense of Presence, Realism | Excellent self-reported sense of presence and realism, supporting ecological validity. | [22] |
| Framework for Behavioural Research | VR Frameworks (EVE, Landmarks, etc.) | Data Reproducibility & Experiment Control | DEAR principle (Design, Experiment, Analyse, Reproduce) improves standardization. | [24] |
| Museum Immersive Experience | VR in Cultural Institutions | Perceived Usefulness, Ease of Use | Core technical indicators (from Technology Acceptance Model) are primary drivers of user engagement. | [25] |
Furthermore, studies have successfully captured the impact of environmental variables on human performance within immersive settings, demonstrating the criterion validity of VR. For instance, an experiment with 52 subjects in a virtual office showed that the system could properly capture the statistically significant influence of different temperature setpoints on thermal comfort votes and adaptive behavior [22].
Experimental Protocols for Immersive Data Visualization
To ensure the validity and reliability of research conducted in immersive environments, a structured experimental framework is essential. The following protocol, synthesizing best practices from the literature, can be adapted for studies on spatial data understanding.
Pre-Experimental Phase: Design and Preparation
- Hypothesis and Variable Definition: Clearly define the research question. The independent variable could be the level of immersion (e.g., desktop 3D vs. fully immersive VR). Dependent variables should measure spatial understanding, such as:
- Content and Ecological Validity: Develop the virtual environment and data representation. For active sensing research, this could be a 3D point cloud from LIDAR scans or a complex molecular structure. Expert review should be used to establish content validity, ensuring the environment accurately represents the target domain [22].
- Pilot Testing: Conduct small-scale trials to calibrate the experiment, identify technical issues, and ensure that tasks are neither too easy nor too difficult.
Experimental Execution: Data Collection
- Participant Briefing and Training: Inform participants about the procedure and obtain consent. Provide a standardized training session within the VR environment to familiarize them with the controls and interface, minimizing the impact of the learning curve on task performance [24].
- Experimental Task: Guide participants through the core task. An example workflow for a drug development context is visualized below.
Diagram 1: Experimental Workflow for an Immersive Drug Discovery Study
- Data Recording: Automatically and systematically log all relevant data. This includes the dependent variables, but also process metrics like head and hand tracking data, gaze paths, and interaction logs, which can provide rich insights into the user's cognitive and active sensing strategies [24].
Post-Experiment: Analysis and Reproducibility
- Data Analysis: Apply statistical tests to evaluate the hypothesis. For complex data, machine learning techniques can be used to analyze behavioral patterns [23].
- Ensuring Reproducibility: Adhere to the DEAR (Design, Experiment, Analyse, Reproduce) principle. This involves documenting all aspects of the experiment, from the framework and software version to the specific parameters of the virtual environment, and making the experimental setup scriptable to allow for exact replication [24].
The Scientist's Toolkit: Essential Research Reagents and Materials
Conducting rigorous immersive visualization research requires both hardware and software components. The following table details key items and their functions.
Table 2: Essential Research Reagents and Materials for Immersive Visualization
| Item Name | Category | Function & Application in Research |
|---|---|---|
| Head-Mounted Display (HMD) | Hardware | Provides the visual and auditory immersive experience. Application: The primary device for presenting the virtual data environment to the user. Examples include Oculus, VIVE. [24] |
| Motion Tracking System | Hardware | Tracks the user's head, hand, and potentially full-body position in real-time. Application: Enables embodied interaction and active sensing, allowing researchers to physically navigate and manipulate data. [21] |
| VR Experiment Framework (e.g., EVE, UXF) | Software | Provides pre-determined features and templates for creating, running, and managing experiments in VR. Application: Standardizes experimental procedures, manages participants, and facilitates data collection, enhancing internal validity and reproducibility. [24] |
| Game Engine (e.g., Unity, Unreal) | Software | The development platform used to create the 3D virtual environment and data visualizations. Application: Allows for the rendering of complex data structures and the programming of interactive elements and logic. [24] |
| Data Logging Module | Software | A customized or framework-integrated tool for recording participant data. Application: Systematically captures all dependent variables (accuracy, time) and process metrics (trajectories, gaze) for subsequent analysis. [22] [24] |
The theoretical basis for how immersion enhances spatial understanding of complex data is built upon a powerful convergence of cognitive science and technology. By leveraging multimodal perception, embodied cognition, and ecological validity, immersive environments transform abstract data into spatial experiences that the human brain is exquisitely adapted to understand. This creates a direct pipeline to the neural substrates of spatial memory, making it a potent tool for tasks ranging from analyzing molecular interactions in drug development to interpreting 3D sensor data in active sensing research. While challenges such as cybersickness and standardization remain, the rigorous application of structured experimental protocols and frameworks ensures that this promising field will continue to yield valid, reproducible, and profound insights into complex data.
VR in Action: Methodologies for Drug Target Visualization and Simulation
Molecular Docking and Drug-Target Interaction Analysis in VR
Active sensing research, particularly in the context of drug discovery, involves the proactive exploration of biological systems to understand how potential therapeutics interact with their targets. Virtual Reality (VR) is transforming this field by providing an immersive, three-dimensional spatial context for visualizing and manipulating complex molecular and biological data. This paradigm shift moves researchers from passive observation to active, intuitive exploration within a computational space, dramatically accelerating the process of hypothesis generation and testing [26]. The core of this approach lies in using VR to simulate a hypothetical reality where researchers can confront scenarios driven by interactions between their scientific intuition and the digital environment, much like pilots training in flight simulators [26]. This guide details the technical integration of molecular docking, drug-target interaction (DTI) prediction, and VR, framing them as essential components of an advanced active sensing framework for modern pharmaceutical research.
Recent Advances in Computational Prediction Methods
Molecular Docking Techniques
Molecular docking is a fundamental structure-based method that predicts the orientation and conformation of a small molecule (ligand) when bound to a target macromolecule (receptor). Recent advances have significantly enhanced their accuracy and efficiency in predicting drug-target interactions [27].
Key Advancements include:
- Fragment-Based Docking: This technique breaks down complex molecules into smaller fragments for docking, improving the sampling of binding sites and the identification of key interactions.
- Covalent Docking: These methods predict interactions between drugs and protein residues that form covalent bonds, opening new opportunities for targeting challenging drug-resistant mutations [27].
- Handling Protein Flexibility: Improved sampling techniques and sophisticated algorithms have increased the efficiency and precision of simulations, allowing researchers to investigate conformational changes and protein flexibility during the drug-binding process [27].
- Virtual Screening: This approach leverages docking to rapidly evaluate massive libraries of compounds against a target, streamlining the initial hit-finding phase [27].
Popular algorithms such as Vina, Glide, and AutoDock continue to be refined, offering enhanced performance. However, it is crucial to remember that molecular docking alone is insufficient to ensure the safety and efficacy of a drug candidate. While it excels at predicting binding affinity and interaction, it does not account for pharmacokinetics, toxicity, off-target effects, or in vivo behavior. Experimental validation through molecular dynamics (MD) simulation, ADMET profiling, and in vitro/in vivo studies remains essential [27].
Drug-Target Interaction (DTI) Prediction
While docking relies on 3D structures, broader DTI prediction methods use various data types to identify potential interactions. Accurate DTI prediction is an essential step in drug discovery, and in silico approaches mitigate the high costs, low success rates, and extensive timelines of traditional development [28].
Table 1: Categories of In Silico DTI Prediction Methods
| Method Category | Description | Key Strengths | Common Limitations |
|---|---|---|---|
| Structure-Based [29] | Uses 3D structures of target proteins (e.g., from X-ray crystallography, Cryo-EM, or AlphaFold) to predict interactions. | Provides atomic-level insight into binding modes; facilitates lead optimization. | Computational resource-intensive; requires a known or reliably predicted 3D structure. |
| Ligand-Based [29] | Compares a candidate ligand to known active ligands for a target (e.g., using QSAR). | Effective when target structure is unknown but active ligands are available. | Predictive power limited by the number and diversity of known ligands. |
| Network-Based [29] | Constructs heterogeneous networks from diverse data (chemical, genomic, pharmacological) and uses topological information. | Does not require structural data; can integrate multiple data types for novel predictions. | Can be a "black box"; performance depends on network quality and completeness. |
| Machine Learning-Based [29] | Uses ML models to learn latent features from drug and target data (e.g., SMILES strings, protein sequences). | Can handle large-scale data; strong predictive performance with sufficient labeled data. | Often relies on large, high-quality labeled datasets; can suffer from "cold start" problems with new entities. |
Recent state-of-the-art frameworks, such as DTIAM, unify the prediction of DTI, drug-target binding affinity (DTA), and the critical mechanism of action (MoA)—distinguishing between activation and inhibition [29]. DTIAM and similar advanced models leverage self-supervised learning from large amounts of unlabeled data (molecular graphs and protein sequences) to learn meaningful representations, which dramatically improves generalization performance, especially in "cold start" scenarios involving novel drugs or targets [29].
Integrating VR into the Drug Discovery Workflow
Virtual Reality acts as a powerful unifying layer, bringing the computational methods described above into an interactive, intuitive, and collaborative environment. The VRID (Virtual Reality Inspired Drugs) concept formalizes this approach, positioning VR as a vein for novel drug discoveries [26].
Table 2: VR Applications in the Drug Discovery Pipeline
| Discovery Stage | Role of Virtual Reality | Quantitative Impact |
|---|---|---|
| Target Identification | Serves as a hypothesis generator by providing a system-level theoretical framework to explore dynamics and test "what-if" scenarios [26]. | Allows theoretical testing of hundreds of treatment combinations and doses in silico [26]. |
| Lead Generation & Screening | Provides a 3D spatial platform to screen and visualize lead compounds, tuning parameters like potency and selectivity interactively [26]. | Shortens lead generation and screening phases by predicting therapeutic efficacy and biological activity before wet-lab experiments. |
| Pharmacokinetics/Pharmacodynamics (PK/PD) | Models drug absorption, distribution, metabolism, and excretion (ADME) in a dynamic 3D space for different delivery systems [26]. | Serves as an additional layer to mathematical PK/PD models, guiding treatment strategy and dosage predictions. |
| Precision Medicine | Builds patient-specific simulations from individual data (e.g., MRI) to tailor optimal treatment protocols [26]. | Moves beyond "one-size-fits-all"; e.g., eBrain modeling indicated combinatorial approaches could reduce single drug doses, lowering side-effect likelihood [26]. |
A proof-of-concept for VRID is eBrain, a VR platform that models drug administration to the brain. For instance, eBrain can upload a patient's MRI, simulate the infusion of a drug (e.g., intranasal insulin for Alzheimer's), and visualize its diffusion through brain tissue and subsequent activation of neurons [26]. This allows for the in silico testing of hundreds of doses and combination treatments to identify the most efficacious and cost-effective approach for a specific patient profile [26].
Experimental Protocols for VR-Enhanced Analysis
Protocol 1: VR-Enabled Molecular Docking and Analysis
This protocol integrates traditional docking workflows with an immersive VR layer for enhanced visualization and interaction.
1. System Setup and Preparation: * Hardware: Utilize a standalone VR headset (e.g., Meta Quest 3) or a PC-connected system. For full sensory immersion, consider haptic feedback gloves or suits to "feel" molecular forces and surfaces [19]. * Software: Employ a molecular visualization package with VR capability (e.g., molecular viewers extended for VR) coupled with standard docking software (Vina, Glide, AutoDock). * Data Preparation: Prepare the protein target by removing water molecules, adding hydrogen atoms, and defining the binding site grid, as per standard docking procedure.
2. Immersive Docking and Visualization: * Import the prepared protein structure and pre-docked ligand poses into the VR environment. * Don the VR headset to enter the molecular-scale space. Physically walk around the protein target to inspect the binding pocket from all angles. * Manually manipulate and re-dock ligands using hand controllers, leveraging intuitive human spatial reasoning to explore binding modes that might be missed by automated algorithms alone. * Use the VR interface to toggle visualization of key interactions, such as hydrogen bonds, hydrophobic contacts, and pi-stacking, overlaid directly within the 3D space.
3. Analysis and Hypothesis Generation: * Compare multiple docked poses side-by-side in the virtual space to assess their stability and interaction networks critically. * Annotate observations directly in the VR environment using virtual markers or voice notes. * Collaboratively analyze the scene with remote colleagues in a multi-user VR session, discussing the viability of different binding hypotheses in real-time [19].
Protocol 2: Validating DTI Predictions Using a VR Simulation Platform
This protocol uses a VR simulation platform like eBrain to validate and contextualize DTI predictions from a model like DTIAM.
1. Data Input and Model Integration: * Input: Feed the results from a DTIAM prediction—including the predicted interaction, binding affinity, and MoA (activation/inhibition)—into the VR platform. * Contextualization: The VR platform (e.g., eBrain) maps this drug-target interaction onto a broader physiological context. For a neurological target, this means simulating the relevant brain region based on a standard or patient-specific MRI atlas [26].
2. System-Level Simulation: * The platform simulates the pharmacokinetics of the drug, modeling its route of administration (e.g., intranasal, intravenous), diffusion through tissues, and uptake by cells [26]. * It then visualizes the pharmacodynamic effect—the activation or inhibition of the target pathway—within the virtual tissue environment. For example, the propagation of a neural signal in the substantia nigra could be simulated and visually represented [26].
3. Outcome Analysis and Iteration: * Observe the system-level outcome of the drug's action, such as changes in network activity or biomarker levels. * Analyze the simulation to predict efficacy and potential side-effects based on the drug's distribution and MoA in the full physiological context. * Iteratively adjust drug parameters (e.g., dose, formulation) in the VR model and re-run the simulation to theoretically optimize the treatment protocol before moving to experimental validation [26].
Visualization of Workflows and Signaling Pathways
The following diagrams, created using Graphviz DOT language, illustrate the core logical workflows and relationships described in this guide.
VR Enhanced Drug Discovery Workflow
DTIAM Model Architecture
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Research Reagents and Solutions for VR-Enhanced Drug Discovery
| Item | Function & Role in Research |
|---|---|
| VR Simulation Platform (e.g., eBrain) | Models drug administration, diffusion, uptake, and effect within a physiological system (e.g., the brain), allowing for system-level testing of treatments in silico [26]. |
| Standalone VR Headset (e.g., Meta Quest 3) | Provides an accessible, high-performance, wireless portal into the virtual molecular environment, enabling widespread adoption in labs [19]. |
| Multi-sensory Haptic Technology | Haptic gloves and suits provide tactile feedback, allowing researchers to "feel" molecular surfaces, forces, and textures, which is critical for assessing interactions in fields like gaming and training [19]. |
| Self-Supervised Learning Model (e.g., DTIAM) | A unified computational framework that learns from unlabeled data to predict drug-target interactions, binding affinity, and mechanism of action, particularly powerful for cold-start problems [29]. |
| Advanced Docking Software (Vina, Glide, AutoDock) | The computational engine for predicting the atomic-level binding pose and orientation of a small molecule within a target protein's binding site [27]. |
| Scientific Illustration Tool (e.g., BioRender) | Creates clear, standardized visual protocols and pathway diagrams to document findings, communicate complex concepts, and ensure consistency across research teams [30] [31]. |
Building Patient-Specific 3D Disease Models for Personalized Medicine
The paradigm of drug development and therapeutic intervention is shifting from a one-size-fits-all approach to a more tailored strategy, enabled by the creation of patient-specific three-dimensional (3D) disease models. These advanced ex vivo systems aim to recapitulate the complex architecture and cellular crosstalk of human tissues, providing a powerful platform for personalized drug screening and disease mechanism investigation [32]. The convergence of tissue engineering, 3D bioprinting, and patient-derived cellular materials has facilitated the development of biomimetic environments that more accurately predict individual patient responses to therapies. Furthermore, the integration of these physical models with immersive virtual reality (VR) technologies is opening new frontiers for researchers to visualize, manipulate, and understand disease biology within spatially complex microenvironments, thereby enhancing the utility of these models in active sensing research [33]. This technical guide examines the current state of patient-specific 3D disease models, with a focus on their construction, validation, and integration with VR for advanced analysis in personalized medicine.
Technical Foundations of 3D Disease Models
Core Bioprinting Technologies
The fabrication of patient-specific 3D models relies heavily on additive manufacturing approaches that enable precise spatial patterning of cellular and acellular components [34].
- Inkjet Bioprinting: This non-contact technology utilizes thermal or piezoelectric mechanisms to deposit bioink droplets. It is characterized by its high speed and capability for multi-material printing, enabling the generation of heterogeneous tissues. A key limitation is the potential for nozzle clogging and reduced cell viability due to shear stress, restricting bioink cell density to below 5 × 10^6 cells/mL [32].
- Extrusion Bioprinting: This method employs pneumatic or mechanical dispensing systems to continuously deposit bioink filaments. It is one of the most prevalent techniques in tissue engineering due to its ability to handle a wide range of biomaterial viscosities and achieve high cell densities. Challenges include limited printing resolution (typically in the hundreds of microns) and potential nozzle obstruction [32].
- Laser-Assisted Bioprinting: This technology uses laser energy to transfer bioink from a donor layer to a substrate. It offers high resolution and is gentle on cells, but its complexity and cost have limited its widespread adoption compared to other modalities [32].
Table 1: Comparison of Major 3D Bioprinting Technologies
| Technology | Mechanism | Resolution | Advantages | Limitations |
|---|---|---|---|---|
| Inkjet Bioprinting | Thermal/Piezoelectric droplet deposition | Single cell scale | High speed, multi-material capability, non-contact | Low cell density, potential heat/shear stress |
| Extrusion Bioprinting | Continuous filament deposition | ~100 μm | High cell density, wide biomaterial compatibility | Lower resolution, nozzle clogging risk |
| Laser-Assisted Bioprinting | Laser-induced forward transfer | High (cell scale) | High resolution, high cell viability | High cost, complex setup, lower throughput |
Essential Biomaterials and Microenvironment
The biomaterials used in 3D disease models, often hydrogel-based, are critical as they must biomimic the native extracellular matrix (ECM) to support physiological cell behavior [34].
Key Hydrogel Properties:
- Biocompatibility: The material must support cell viability, proliferation, and function without inducing cytotoxicity [34].
- Biomimicry: The hydrogel should replicate the biochemical and biophysical properties of the target tissue's native ECM, including presentation of adhesion ligands and appropriate mechanical stiffness [34] [35].
- Tunable Mechanical Properties: The stiffness, viscosity, and elasticity of the hydrogel can be modulated to match the pathological tissue of interest [34].
- Degradability: The scaffold should degrade at a rate commensurate with new tissue formation, allowing for remodeling [32].
The Scientist's Toolkit: Key Research Reagents for 3D Disease Modeling
Table 2: Essential reagents and materials for constructing patient-specific 3D disease models.
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| Patient-Derived Cells (e.g., cancer cells, hiPSCs) | Provides the patient-specific genetic and phenotypic foundation for the model. | Source (primary vs. immortalized), culture stability, need for stromal components [32] [35]. |
| Decellularized ECM (dECM) | Provides a tissue-specific biochemical scaffold that preserves native ECM composition and signaling cues. | Source tissue, decellularization efficiency, batch-to-batch variability [34]. |
| Synthetic Hydrogels (e.g., PEG, Pluronics) | Provides a defined, tunable scaffold with controllable mechanical and biochemical properties. | Functionalization for cell adhesion, degradation kinetics, biocompatibility [34]. |
| Natural Hydrogels (e.g., Collagen, Matrigel, Alginate, GelMA) | Offers innate bioactivity and cell adhesion motifs; widely used for high-fidelity cell culture. | Lot-to-lot variability (especially Matrigel), immuneogenicity, mechanical weakness [34]. |
| Crosslinking Agents | Induces gelation of hydrogel precursors to form stable 3D structures (e.g., ionic, UV, enzymatic). | Cytotoxicity, crosslinking speed, homogeneity of the resulting gel [32]. |
| Soluble Factors (e.g., Growth Factors, Cytokines) | Directs cell differentiation, maintains phenotype, and recreates key signaling pathways of the TME. | Stability in culture, concentration gradients, cost [35]. |
Application-Specific Model Design
Modeling the Tumor Microenvironment
3D bioprinted cancer models are at the forefront of personalized oncology, designed to capture the intricate interplay between malignant cells and the tumor microenvironment (TME) [32]. Key design considerations include:
- Incorporating Stromal Components: Faithful models integrate cancer-associated fibroblasts (CAFs), endothelial cells, and immune cells to replicate the pro-tumorigenic signaling and drug resistance mechanisms conferred by the TME [34] [35].
- Recreating Gradients: The TME is characterized by gradients of oxygen, nutrients, and cytokines. Bioprinting allows for the spatial patterning of these factors to mimic the core vs. periphery conditions of a tumor, which is crucial for studying drug penetration and efficacy [32] [35].
- Vascularization: A major challenge is incorporating functional vasculature. Strategies include co-printing endothelial cells with supportive pericytes and using sacrificial bioinks to create perfusable channels, which are essential for modeling metastatic spread and delivering therapeutics [32].
Diagram 1: Workflow for building a 3D bioprinted patient-specific tumor model.
Recapitulating the Bone Marrow Niche in Hematologic Malignancies
For diseases like multiple myeloma (MM), the bone marrow (BM) niche is a master regulator of disease progression and drug resistance. Patient-derived 3D MM models seek to recreate this complex ensemble [35].
- Cellular Complexity: A faithful MM model must include, besides the malignant plasma cells, BM stromal cells (BMSCs), adipocytes, endothelial cells, osteoclasts, and immune cells. The crosstalk between these cells, mediated by adhesion molecules and soluble factors, is a critical therapeutic target [35].
- Biomaterial Strategy: Hydrogels for MM models must support the growth of both adherent (stromal) and non-adherent (myeloma) cell populations. Fibrin and hyaluronic acid-based hydrogels have shown promise in maintaining these co-cultures and preserving patient-specific drug response profiles [35].
Integration with Virtual Reality for Analysis and Visualization
The complex, multi-parametric data generated by 3D disease models can be more intuitively understood and analyzed through immersive VR technologies. This integration is pivotal for active sensing research, where scientists can actively probe and interact with the model in a simulated space.
- Surgical Planning and Visualization: VR platforms, such as Medical Imaging XR (MIXR), allow clinicians and researchers to visualize medical imaging data (CT, MRI) in augmented reality on common devices like smartphones. Workflows like "VR-prep" optimize DICOM files for rapid AR visualization, significantly improving the confidence of clinicians in using these models for diagnostics and preoperative planning [36].
- Enhanced Collaborative Analysis: Metaverse platforms enable multidisciplinary teams to collaborate in shared virtual spaces to review 3D anatomical models and plan treatments. This facilitates a more holistic understanding of patient-specific disease geometry and the spatial relationship between tissues [33].
- Interactive Medical Education and Training: VR is revolutionizing medical education by providing immersive, interactive learning experiences. For instance, VR anatomy training has been shown to increase knowledge retention by up to 63% and user engagement by up to 72%, enabling students and researchers to deeply understand the structural context of the diseases they are modeling [19] [37].
Diagram 2: VR integration for analyzing 3D model data.
Detailed Experimental Workflow: A Case Study
This protocol outlines the steps for creating a patient-specific, bioprinted breast cancer model for personalized drug screening, as adapted from recent literature [34] [32].
Protocol: Bioprinting a Vascularized Breast Tumor Model
Objective: To fabricate a 3D breast cancer model containing patient-derived cancer cells and an endothelial network for assessing drug response.
Materials:
- Cells: Patient-derived breast cancer cells (BCCs), Human Umbilical Vein Endothelial Cells (HUVECs), Cancer-Associated Fibroblasts (CAFs) isolated from the same tumor [34].
- Bioinks:
- Tumor Bioink: Gelatin methacrylate (GelMA) supplemented with patient-derived dECM, loaded with BCCs and CAFs.
- Vascular Bioink: Glycidyl methacrylate-hyaluronic acid (GMHA) loaded with HUVECs.
- Bioprinter: Extrusion-based bioprinter equipped with a multi-cartridge printhead and a UV crosslinking module.
Method:
- Pre-bioprinting:
- Cell Expansion: Expand patient-derived BCCs, CAFs, and HUVECs in 2D culture using appropriate media.
- Bioink Preparation: Mix GelMA with digested tumor dECM at a ratio of 4:1. Resuspend the pellet of BCCs and CAFs (at a 5:1 ratio) in the GelMA/dECM blend to a final density of 10 × 10^6 cells/mL. Keep on ice.
- Prepare the vascular bioink by dissolving GMHA and loading HUVECs at a density of 15 × 10^6 cells/mL.
Bioprinting Process:
- Load the tumor and vascular bioinks into separate sterile cartridges mounted on the bioprinter.
- Set the printing parameters: Nozzle diameter: 250 μm (tumor), 150 μm (vascular); Pressure: 18-22 kPa (tumor), 12-15 kPa (vascular); Print speed: 8 mm/s; Print bed temperature: 15°C.
- Using a computer-aided design (CAD) model, co-print the tumor and vascular bioinks in a concentric pattern. The tumor bioink forms the core, while the vascular bioink is printed as an surrounding network.
- Apply UV light (365 nm, 5 mW/cm²) for 60 seconds after each layer is deposited to achieve partial crosslinking.
Post-bioprinting:
- After the construct is complete, immerse it in cell culture medium and incubate at 37°C, 5% CO₂.
- Culture the model for up to 21 days, with medium changes every 2-3 days. The endothelial network will typically form lumen-like structures within 7-14 days.
Drug Screening Application:
- On day 7 post-bioprinting, treat the model with a panel of anti-cancer drugs (e.g., chemotherapeutics, targeted therapies) at clinically relevant concentrations.
- After 72-96 hours of exposure, assess viability using assays like AlamarBlue or Calcein-AM/Ethidium homodimer-1 live/dead staining. Confocal microscopy and immunohistochemistry can be used to evaluate morphological changes, endothelial integrity, and specific protein markers.
Patient-specific 3D disease models represent a transformative technology in personalized medicine, moving beyond the limitations of traditional 2D cultures and animal models. The synergy between advanced biomanufacturing techniques like 3D bioprinting and cutting-edge visualization tools like virtual reality creates a powerful feedback loop. This integration allows researchers not only to build more physiologically relevant models of human disease but also to actively sense, probe, and interpret the complex biological phenomena within them in an intuitive and collaborative manner. As these technologies continue to mature and become more accessible, they hold the promise of accelerating the development of truly personalized therapeutic strategies, ultimately improving patient outcomes across a spectrum of diseases.
Simulating Drug Penetration and Cellular Response in Virtual Tissues
The integration of virtual reality (VR) and computational modeling is revolutionizing active sensing research in drug development. By simulating drug penetration and cellular responses in virtual tissues, researchers can visualize and analyze biological processes in immersive, dynamic environments. This approach leverages in silico models—such as virtual patients, AI-driven virtual cells, and digital twins—to predict drug efficacy, optimize dosing, and reduce reliance on traditional laboratory experiments [38] [39] [40]. Framed within a broader thesis on VR's role in active sensing, this whitepaper explores methodologies, tools, and experimental protocols for simulating tissue-level drug behavior.
Computational Frameworks for Virtual Tissue Simulation
Virtual tissue models integrate multi-scale data to simulate drug transport and cellular dynamics. Key frameworks include:
- Agent-Based Models (ABMs): Simulate individual cell interactions (e.g., tumor-immune dynamics) and drug effects using stochastic rules [39].
- AI Virtual Cells (AIVCs): Combine artificial intelligence (AI) with multi-modal data (e.g., static architecture and dynamic perturbation states) to predict cellular responses to drugs [41].
- Physiologically Based Pharmacokinetic (PBPK) Modeling: Quantifies drug absorption, distribution, metabolism, and excretion (ADME) across tissue compartments [38].
- Digital Twins: Virtual replicas of human patients, updated with real-time clinical data to simulate personalized treatment outcomes [39].
These frameworks rely on three data pillars for accuracy:
- A Priori Knowledge: Existing biological mechanisms from literature [41].
- Static Architecture: Spatial cellular structures from cryo-electron microscopy or spatial omics [41].
- Dynamic States: Time-resolved data from perturbations (e.g., CRISPR, drug treatments) [41].
Table 1: Quantitative Parameters for Multi-Scale Virtual Tissue Models
| Model Component | Key Parameters | Data Sources |
|---|---|---|
| Tissue Penetration | Diffusion coefficients, capillary permeability | Mass spectrometry, imaging [41] |
| Cellular Response | Protein expression, metabolic rates | Perturbation proteomics, transcriptomics [41] |
| Virtual Patient Cohorts | Demographic variability, genetic markers | Real-world data, biobanks [39] [40] |
Virtual Reality as an Active Sensing Tool
VR transforms virtual tissues into interactive, immersive environments for active sensing—enabling researchers to "sense" and manipulate molecular interactions in 3D. Applications include:
- Visualizing Drug Diffusion: VR platforms render simulated drug permeation through tissue layers, highlighting barriers like dense extracellular matrix [42].
- Real-Time Feedback Loops: Closed-loop systems integrate VR with robotic experiments, where AI identifies knowledge gaps and designs new perturbations [41].
- Ethical Safeguards: Protocols like the "3 C's" (Context, Control, Choice) ensure user safety in immersive settings [42].
Experimental Protocols for Virtual Tissue Assays
Protocol 1: Simulating Antibody-Drug Conjugate (ADC) Efficacy
Objective: Predict payload efficacy and resistance mechanisms [40]. Workflow:
- Input Setup:
- Load virtual patient data (e.g., multi-omics profiles from Champions Oncology [40]).
- Define ADC parameters (antibody affinity, linker stability, payload cytotoxicity).
- Simulation Execution:
- Output Analysis:
- Calculate combination synergy scores.
- Identify biomarkers of sensitivity/resistance.
Protocol 2: Closed-Loop Active Learning for Perturbation Screening
Objective: Optimize drug combinations using AI-guided experiments [41]. Workflow:
- Data Integration: Feed static (e.g., spatial proteomics) and dynamic (e.g., live-cell imaging) data into an AIVC.
- AI-Driven Hypothesis Generation: Train models to predict understudied phosphorylation events.
- Robotic Validation: Execute automated CRISPR or small-molecule perturbations.
- Model Refinement: Update simulations with experimental outcomes.
Visualization of Signaling Pathways and Workflows
Diagram 1: Virtual Tissue Simulation Workflow
Title: Virtual Tissue Simulation and Feedback Loop
Diagram 2: Signaling Pathway Integration in AIVCs
Title: Drug-Induced Signaling in Virtual Cells
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for Virtual Tissue Experiments
| Tool/Platform | Function | Application Example |
|---|---|---|
| Turbine Virtual Lab [40] | Simulates cell behavior and therapy responses using AI. | ADC payload selection via in silico screening. |
| AIVC Framework [41] | Integrates multi-omics data to predict drug efficacy and synergy. | Simulating S. cerevisiae response to perturbations. |
| Champions Oncology Data [40] | Provides patient-derived xenograft models for virtual patient cohorts. | Enriching virtual libraries with real-world tumor data. |
| Closed-Loop Robotics [41] | Automates perturbations for model validation. | High-throughput phosphoproteomics in response to drugs. |
Virtual tissue simulation, enhanced by VR and AI, offers a paradigm shift in active sensing research. By adopting protocols for virtual patients, AIVCs, and digital twins, researchers can accelerate drug development while ensuring ethical and scalable methodologies. Future work will focus on standardizing model validation and integrating VR-driven active sensing into regulatory decision-making [38] [39] [41].
Optimizing Clinical Trial Design through Immersive Patient Engagement Modules
The integration of Virtual Reality (VR) into clinical trial design represents a paradigm shift from traditional data collection methods toward immersive, patient-centered approaches framed within active sensing research. This framework posits that perception is not a passive reception of stimuli but an active process of hypothesis testing through goal-directed exploration. VR serves as the ideal medium to structure and measure this exploration, creating controlled sensory environments where patient engagement becomes a rich, quantifiable dataset. By modulating sensory inputs and tracking behavioral outputs, VR transforms patients from passive subjects into active participants whose interactions provide direct insight into cognitive, motor, and emotional processes. This technical guide examines how immersive patient engagement modules leverage active sensing principles to optimize clinical trials through enhanced data quality, patient retention, and ecological validity.
Therapeutic Mechanisms and Clinical Applications
How VR Modules Alleviate Patient Burdens
Immersive VR interventions function through multiple therapeutic mechanisms that align with active sensing principles. By engaging attentional resources and providing multisensory stimulation, VR directly modulates pain perception through the gate control theory [43]. Furthermore, the creation of presence—the psychological state of "being there" in the virtual environment—facilitates emotional regulation and reduces anxiety by transporting patients from stressful clinical settings to calming virtual environments [43]. These mechanisms are particularly valuable in managing procedural pain, anticipatory anxiety, and treatment-related distress commonly experienced in clinical trial participation.
Evidence for Clinical Efficacy Across Specialties
Recent evidence demonstrates the practical benefits of VR across therapeutic areas, supporting its role in enhancing trial outcomes:
- Oncology Settings: VR interventions have shown promising effects in reducing anxiety and pain during radiotherapy sessions and supporting patient education through engaging, immersive experiences [43].
- Radiology Applications: Findings have been less consistent, likely due to shorter procedure durations limiting VR's effectiveness, highlighting the importance of tailoring immersive interventions to specific clinical contexts [43].
- Neurological Assessments: VR enables precise standardization of neurocognitive batteries and motor function tasks, capturing nuanced metrics like latency, accuracy, dwell time, and error types with superior consistency to traditional methods [44].
Table 1: Clinical Evidence for VR Across Medical Specialties
| Therapeutic Area | Primary Application | Reported Benefits | Evidence Level |
|---|---|---|---|
| Oncology | Radiotherapy distress reduction | Reduced anxiety and pain during sessions | Multiple clinical studies [43] |
| Neurology | Neurocognitive assessment | Test standardization; improved repeatability | Validation studies [44] |
| Surgical Training | Crisis management simulation | Enhanced decision-making skills | Clinical trial (NCT04451590) [45] |
| Chronic Pain | Pain modulation | Analgesic sparing endpoints | Clinical trials [44] |
Implementation Framework: The BUILD REALITY Model
Design Phase: Foundational Considerations
Successful implementation of VR modules begins with rigorous planning and design. The BUILD REALITY framework provides a systematic approach comprising twelve distinct phases [45]:
- Begin with a needs assessment: Conduct thorough stakeholder engagement including end users, content experts, and technical specialists to identify unmet needs that VR can specifically address [45].
- Use the needs assessment to set objectives: Align objectives with educational evaluation models like the Kirkpatrick model, focusing on reaction, learning, behavior, and results [45].
- Identify the best VR modality: Select appropriate immersion levels and hardware based on use case requirements, choosing between screen-based VR (low-medium immersion) versus stand-alone headsets (medium-high immersion) [45].
- Leverage learning theory: Ground VR environments in established pedagogical frameworks like constructivism and self-regulated learning to maximize educational effectiveness [45].
- Define and support cocreation: Establish interprofessional teams including software developers, animators, human factors specialists, and clinicians to collaboratively achieve project outcomes [45].
- Recreate diversity and accessibility: Intentionally design for diverse participant populations through various avatars, virtual patients, and accessibility considerations [45].
Implementation Phase: From Testing to Integration
The implementation phase focuses on practical deployment and evaluation:
- Educate users with prebriefing: Ensure participants understand VR operation and intervention goals through comprehensive orientation sessions [45].
- Adapt and test iteratively: Conduct pilot testing with both learners and educators to refine the VR environment based on real-world feedback [45].
- Look for VR simulation champions: Identify and empower advocates who can promote adoption within their clinical or research teams [45].
- Identify barriers: Proactively address technical, logistical, and human factor obstacles to implementation [45].
- Test the impact: Evaluate the VR tool against predefined objectives and metrics to demonstrate value [45].
- Amplify VR integration: Strategically incorporate successful VR modules within broader clinical trial curricula and protocols [45].
Table 2: VR Modality Selection Guide Based on Trial Requirements
| Modality | Immersion Level | Hardware Examples | Best For | Cost Consideration |
|---|---|---|---|---|
| Screen-Based VR | Low-medium | Computer monitors, smartphones, Google Cardboard | Patient education, cognitive tasks | Low cost [45] |
| Stand-Alone VR | Medium-high | Oculus Quest, Pico 4, HTC Vive Pro | Motor function assessment, complex simulations | Medium-high cost [45] |
Experimental Protocol for VR Clinical Trials
Protocol Design and Validation Methodology
Implementing robust VR trials requires meticulous methodological planning. The following protocol provides a framework for rigorous validation:
Hybrid Decentralized RCT Design:
- Maintain biosamples and imaging in clinic settings while shifting task-based endpoints (motor rehab, neurocognitive tests) to VR-administered assessments in home environments [44].
- Incorporate tele-supervised windows for safety monitoring during remote sessions [44].
- Justify sample size using lower variance expected from standardized VR tasks compared to traditional measures [44].
Endpoint Validation Approach:
- For novel VR-captured endpoints, begin with context-of-use specification including headset models, tracking mode, minimum lighting requirements, and firmware versions [44].
- Establish validation through Bland-Altman agreement studies against reference standard tools [44].
- Conduct test-retest reliability assessments with appropriate calibration cohorts [44].
- Implement washout periods for cognitive tasks to mitigate learning effects [44].
Data Quality and Safety Considerations:
- Set minimum tracking confidence thresholds and room-scale boundaries in the study protocol [44].
- Implement pose calibration at every assessment session to maintain data consistency [44].
- Version-freeze VR applications and content packs per site activation, treating updates as controlled amendments [44].
- Embed tele-supervised windows for tasks with non-trivial risk (e.g., balance/vestibular assessments) [44].
Data Collection Strategy: Daily vs. Intermittent Assessment
Pilot studies comparing daily versus weekly PRO data collection in VR interventions reveal distinct advantages for frequent assessment:
- Weekly assessments demonstrate benefits including reduced participant burden, higher completion rates through spaced push notifications, and HIPAA-compliant survey administration [46].
- Daily assessments capture nuanced symptom patterns missed by intermittent evaluation, including early intervention effects, plateaus, and "double-bottom" effects in symptom trajectories [46].
- In-device data capture enables momentary assessment that minimizes recall bias through visual analog scales administered immediately pre- and post-VR intervention [46].
VR Clinical Trial Implementation Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential VR Research Components for Clinical Trials
| Component Category | Specific Examples | Function in Research | Technical Considerations |
|---|---|---|---|
| Hardware Platforms | Meta Quest 2, HTC Vive Pro, Pico 4 | Delivery of immersive experiences; data capture | Stand-alone vs. PC-based; inside-out vs. external tracking [45] [46] |
| Software Development Kits | Unity XR Toolkit, Oculus Integration, OpenXR | Creation of custom assessment environments | Cross-platform compatibility; biometric integration capabilities |
| Data Capture Modules | Eye-tracking, motion capture, performance metrics | Quantification of participant responses and behaviors | Sampling rate; data privacy protocols; export formats [44] |
| Assessment Libraries | Neurocognitive batteries, motor tasks, PRO collections | Standardized outcome measurement | Validation status; learning effects; alternate forms [44] |
| Analytical Tools | Behavioral analytics platforms, statistical packages | Interpretation of complex multimodal datasets | Data visualization; normative databases; signal processing |
Implementation Roadmap and Future Directions
A phased implementation approach ensures systematic adoption of VR modules in clinical trials:
- 2025: Low-Risk Productivity Applications: Deploy VR for electronic consent processes, site start-up tours, rater training, and in-clinic SOP overlays. Measure outcomes through activation time, deviation rates, and source data verification hours [44].
- 2026: Home-Based Task Assessment: Shift appropriate endpoints (rehabilitation exercises, inhaler technique, neurocognitive tests) to home-based VR administration with scheduled tele-supervision. Pre-register rescue pathways for motion sensitivity and technical failures [44].
- 2027: Validated VR Endpoints: Promote rigorously validated VR-captured measures from secondary to primary endpoint status, supported by comprehensive agreement and repeatability datasets [44].
Active Sensing Framework in VR Trials
The integration of immersive patient engagement modules represents the future of patient-centered clinical trial design. By applying active sensing principles through carefully designed VR environments, researchers can obtain richer, more ecologically valid data while simultaneously enhancing participant experience. The structured implementation approach outlined in this guide provides a pathway for leveraging these innovative technologies to advance clinical research methodologies and therapeutic development.
The field of molecular research is undergoing a transformative shift with the integration of Artificial Intelligence (AI) and Virtual Reality (VR). These technologies are creating powerful platforms for collaborative molecular exploration, fundamentally changing how researchers visualize, manipulate, and understand complex biological systems. Within the context of active sensing research—where understanding molecular interaction dynamics is paramount—AI-driven VR tools provide an unprecedented capacity for intuitive, immersive investigation. They bridge the gap between computational data and human intuition, allowing scientists to "actively sense" and interrogate molecular structures in a shared, interactive 3D space [2]. This case study examines the technical foundations, applications, and experimental protocols of these platforms, highlighting their role in accelerating drug discovery and biochemical research.
Technological Foundations of AI-VR Integration
The synergy between AI and VR creates a feedback loop that enhances both human understanding and computational efficiency. AI algorithms, particularly in deep learning, rapidly process vast chemical spaces and predict molecular behavior, while VR interfaces render this data into an intuitive, manipulable 3D format [47] [48].
- Immersive Visualization: VR enables researchers to step inside structural data, visualizing and manipulating protein-ligand complexes in three dimensions. This goes beyond static 3D models by incorporating a spatial and temporal component (4D), allowing researchers to observe molecular dynamics and conformational changes in real-time [2].
- AI-Accelerated Screening: AI platforms can screen billions of chemical compounds to predict binding affinities and poses. When integrated with VR, these hits can be visually explored and rationally optimized, closing the loop between computational prediction and human design intuition [47] [49]. For instance, the RosettaVS platform employs a physics-based force field and active learning to efficiently triage billions of compounds, achieving high enrichment factors in virtual screens [47].
- Collaborative Environments: Modern VR platforms support multi-user sessions, enabling geographically dispersed research teams to collaboratively interact with the same molecular structures simultaneously. This shared exploration is vital for hypothesis generation and interdisciplinary problem-solving [50].
Table 1: Core Components of an AI-Driven VR Molecular Exploration Platform
| Component | Function | Example Tools/Technologies |
|---|---|---|
| VR Rendering Engine | Generates immersive 3D environment from structural data | Unity 3D, NarupaXR, UCSF ChimeraX [50] |
| AI/Docking Backend | Predicts binding poses, affinities, and synthesizability | RosettaVS, ROCS X, AlphaFold, Orion Platform [47] [49] |
| Force Field Engine | Calculates molecular dynamics and energy minimization | RosettaGenFF-VS, NVIDIA BioNeMo [47] [51] |
| Collaboration Server | Synchronizes state and interactions across multiple users | Custom NarupaXR server infrastructure [50] |
Quantitative Performance and Applications
The efficacy of AI-driven VR platforms is demonstrated by quantifiable successes in real-world drug discovery projects. These platforms are not merely visualization tools but are integral to active sensing workflows, where researcher interaction directly guides the exploration of chemical space.
In a landmark application, an AI-accelerated virtual screening platform (OpenVS) was used to screen multi-billion compound libraries against two unrelated targets: a ubiquitin ligase (KLHDC2) and a sodium channel (NaV1.7). The screen identified seven hits for KLHDC2 (a 14% hit rate) and four hits for NaV1.7 (a 44% hit rate), all with single-digit micromolar binding affinity. This entire screening process was completed in under seven days, a task that would be prohibitively time-consuming with traditional methods [47]. The subsequent validation of a KLHDC2-ligand complex via X-ray crystallography confirmed the accuracy of the predicted docking pose, underscoring the method's precision [47].
Another breakthrough comes from Cadence's ROCS X, an AI-enabled search technology that allows scientists to conduct 3D shape and electrostatic searches across trillions of drug-like molecules. This represents a performance increase of at least three orders of magnitude over previous approaches. In a validation with Treeline Biosciences, this technology led to the discovery of over 150 synthesizable, novel drug candidates across multiple projects [49].
Table 2: Performance Metrics of AI-VR Enabled Discovery Platforms
| Platform / Application | Key Metric | Result |
|---|---|---|
| OpenVS Platform [47] | Screening Time (Billion-compound library) | < 7 days |
| OpenVS Platform [47] | Hit Rate (NaV1.7 target) | 44% |
| RosettaVS Scoring [47] | Enrichment Factor (Top 1%) | 16.72 (outperformed 2nd best: 11.9) |
| ROCS X Search [49] | Database Scale | Trillions of molecules |
| ROCS X Validation [49] | Novel Compounds Identified | >150 synthesizable candidates |
Experimental Protocol for Collaborative VR Docking Analysis
The following detailed protocol outlines a typical workflow for using an AI-driven VR platform to analyze and validate molecular docking poses, a common task in active sensing research. This protocol is adapted from methodologies described for systems like NarupaXR and RosettaVS [47] [50].
Preparation of the Target Structure and Compound Library
- Target Preparation: Obtain a high-resolution 3D structure of the target protein (e.g., from X-ray crystallography, cryo-EM, or AI-based prediction tools like AlphaFold). Prepare the structure by adding hydrogen atoms, assigning protonation states, and optimizing side-chain conformers using a tool like RosettaRelax or Schrödinger's Protein Preparation Wizard.
- Library Curation: Select a chemical compound library for screening. This can range from focused libraries of a few thousand molecules to ultra-large libraries of billions of compounds, such as those available from Enamine or ZINC [47].
- AI-Powered Pre-screening: To reduce computational load, use an AI-accelerated docking platform like OpenVS or ROCS X to perform an initial screen.
- The platform employs active learning, where a target-specific neural network is trained on-the-fly to predict binding affinity, prioritizing only the most promising compounds for full physics-based docking [47].
- The output is a ranked list of top-hit compounds with their predicted binding poses and affinity scores.
VR Setup and Collaborative Session Initiation
- Hardware Configuration:
- VR Headsets: One HTC Vive or Vive Pro headset with controllers per researcher [50].
- Computational Server: A central server acting as the "force field engine," equipped with a high-performance GPU (e.g., NVIDIA 1080Ti or higher) and a multi-core CPU [50].
- Networking: An 8-port Gigabit Ethernet switch and LAN cables to connect all user PCs and the server for a synchronized, multi-user experience [50].
- Software Launch:
- Researchers launch the VR front-end application (e.g., NarupaXR).
- The session host launches the server application, which loads the target protein structure and the list of pre-screened hit compounds with their docked poses.
- Users connect their VR clients to the server's IP address, joining a shared virtual space.
Immersive Analysis and Collaborative Discussion
- Visualization of the Complex: Each researcher loads a protein-ligand complex from the pre-screened hit list. The system displays the protein as a surface or cartoon, with the ligand as a detailed ball-and-stick model.
- Pose Analysis and Interaction Mapping:
- Researchers can freely walk around and "fly through" the protein's binding pocket.
- Using VR controllers, they can manipulate the ligand pose—translating, rotating, and examining key interactions such as hydrogen bonds, hydrophobic contacts, and pi-stacking.
- The system can visually highlight these interactions, and calculate interaction energies in real-time.
- Collaborative Rationalization:
- Researchers can discuss findings in real-time via integrated audio.
- They can point to specific residues or interactions, or "pass" a ligand to another user for a second opinion.
- This collaborative sensing allows the team to quickly triage false positives from the AI screen and select the most promising candidates for synthesis based on both quantitative scores and qualitative, visual assessment.
Post-VR Validation and Iteration
- Candidate Selection: The team selects a shortlist of compounds based on the VR session.
- Synthesis and Experimental Testing: The selected compounds are sourced or synthesized and subjected to in vitro binding assays (e.g., SPR, ITC) and functional assays to confirm biological activity.
- Iterative Redesign: If necessary, the crystal structure of a confirmed hit is solved. This experimental structure is then fed back into the VR platform, allowing researchers to analyze the true binding mode and use the intuitive interface to design next-generation compounds with improved properties, thus closing the design-make-test-analyze cycle [47].
AI-VR Drug Discovery Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key hardware and software components required to establish an AI-driven VR molecular exploration platform.
Table 3: Essential Research Reagents and Materials for AI-VR Molecular Exploration
| Item Name | Type | Function / Explanation |
|---|---|---|
| HTC Vive/Pro Headset & Controllers | Hardware | Provides the immersive VR interface, allowing researchers to see, point to, and manipulate molecular structures in 3D space [50]. |
| Computational Server (NVIDIA GPU) | Hardware | Acts as the central "force field engine" for running AI/docking calculations (e.g., RosettaVS) and synchronizing the multi-user VR environment [50]. |
| NarupaXR Software | Software | A VR front-end application designed for education and research, allowing observation and interaction with molecular dynamics simulations in a collaborative setting [50]. |
| RosettaVS Software Suite | Software | An open-source, physics-based virtual screening platform used for accurate prediction of docking poses and binding affinities for billions of compounds [47]. |
| ROCS X (Cadence) | Software | An AI-enabled 3D search tool for performing shape and electrostatic similarity searches across trillions of molecules to identify novel chemical matter [49]. |
| Steam & SteamVR | Software | A common platform required to launch and manage the VR hardware and runtime environment [50]. |
| Orion Molecular Design Platform | Software | The underlying platform that integrates components like OMEGA conformer generation and ROCS for end-to-end molecular design and screening [49]. |
AI-driven VR platforms represent a paradigm shift in molecular exploration and active sensing research. By merging the computational power of AI with the intuitive, collaborative nature of VR, these systems enable a deeper, more efficient understanding of molecular interactions. Quantitative results from platforms like OpenVS and ROCS X demonstrate tangible accelerations in lead discovery, achieving hit rates and timelines that are unattainable with conventional methods. As hardware ergonomics improve and integration with AI and data workflows deepens, these collaborative virtual laboratories are poised to become indispensable tools, reshaping the landscape of drug discovery and structural biology [2] [48].
Overcoming Technical and Practical Hurdles in VR Research Systems
The creation of high-fidelity virtual models of biological systems represents a transformative approach in biomedical research and drug development, particularly within the context of virtual reality (VR) for understanding active sensing. Active sensing research investigates how organisms selectively gather sensory information to guide behavior, a process that requires dynamic, interactive simulation environments. Virtual reality serves as an ideal platform for this research by enabling researchers to visualize and manipulate complex biological systems in three-dimensional space, creating embodied experiences that mirror the exploratory nature of biological sensing itself [52].
The concept of model fidelity in this context extends beyond visual realism to encompass the accurate representation of biological characteristics, including viscoelastic, anisotropic, and nonlinear properties of tissues [53]. As noted in recent systematic reviews, VR possesses significant potential for educational and research applications, though current implementations often prioritize usability over comprehensive biological accuracy [54]. This technical guide addresses this gap by providing detailed methodologies for creating virtual biological models that maintain scientific precision while leveraging VR's capacity for immersive, interactive exploration—a combination essential for advancing active sensing research.
Core Components of Biological Fidelity in Virtual Modeling
Essential Biological Characteristics for Virtual Tissue Modeling
Achieving high fidelity in virtual biological models requires incorporating specific mechanical and biological properties that govern tissue behavior in real-world environments. These characteristics must be mathematically represented and computationally optimized for real-time interaction in VR environments.
Table 1: Essential Biological Characteristics for Virtual Tissue Modeling
| Biological Characteristic | Technical Definition | Implementation in Virtual Models | Research Significance |
|---|---|---|---|
| Viscoelasticity | Time-dependent mechanical response combining viscous fluid and elastic solid properties | Implement relaxation functions and time-dependent deformation algorithms | Critical for simulating tissue response to sustained forces during surgical simulation |
| Anisotropy | Direction-dependent mechanical properties based on tissue microstructure | Use tensor-based mathematics with directional variation parameters | Essential for accurately modeling fibrous tissues like muscle and connective tissue |
| Nonlinearity | Non-proportional relationship between stress and strain in biological tissues | Employ hyperelastic material models (e.g., Ogden, Mooney-Rivlin) | Enables realistic simulation of large deformations beyond linear elastic ranges |
| Viscoplasticity | Permanent deformation after load removal when yield point is exceeded | Implement yield criteria and plastic flow rules | Particularly important for simulating pathological tissue states and surgical resection [53] |
Recent research has highlighted that most existing virtual tissue models lack these unique biological characteristics, limiting their utility in research and training applications. The introduction of viscoplasticity to virtual liver models, for instance, has shown significant improvements in simulating diseased liver resection processes where tissues undergo excessive deformation and permanent shape changes [53].
Multi-Modal Sensory Integration for Active Sensing
Active sensing research in VR environments depends on multi-sensory feedback that engages multiple perceptual channels simultaneously. This approach creates a more comprehensive embodied experience that mirrors biological sensing processes in real organisms.
- Visual Fidelity: High-resolution texture mapping and biologically accurate color representation using specialized palettes optimized for VR displays [55]
- Haptic Feedback: Force feedback systems like the PHANTOM OMNI manual controller that provide resistance corresponding to tissue density and composition [53]
- Proprioceptive Alignment: Accurate spatial mapping between virtual tissue manipulation and real-world motor movements to enhance embodiment in the VR experience
- Temporal Synchronization: Precise coordination between visual, haptic, and auditory feedback to avoid sensory dissonance that disrupts presence
The integration of these sensory modalities creates the conditions for presence—the psychological sensation of "being there" in the virtual environment—which has been shown to significantly enhance learning outcomes and research validity in VR-based biological simulations [56].
Quantitative Framework for Evaluating Model Fidelity
Metrics for Assessing Virtual Biological Model Accuracy
A standardized quantitative framework is essential for objectively evaluating the fidelity of virtual biological models. This framework must encompass both technical performance metrics and biological accuracy measurements.
Table 2: Quantitative Metrics for Evaluating Virtual Biological Model Fidelity
| Metric Category | Specific Metrics | Target Values | Measurement Methods |
|---|---|---|---|
| Technical Performance | Frame rate (>90 Hz), Latency (<20 ms), Computational load | Maintain real-time interaction without visual artifacts | Performance profiling, motion-to-photon latency measurement |
| Visual Accuracy | Texture resolution (≥4K), Color depth, Geometric precision | Sub-millimeter spatial accuracy for surgical applications | Photogrammetric analysis, expert visual assessment |
| Mechanical Accuracy | Stress-strain correlation (R² ≥ 0.85), Relaxation time constants | <15% deviation from ex vivo tissue measurements | Mechanical testing comparison, material parameter optimization |
| Behavioral Validity | Expert acceptance rate (>90%), Face validity scores | Significant improvement over previous models (p < 0.05) | Expert surveys, structured evaluation protocols |
Experimental validation of a high-fidelity virtual liver model demonstrated that incorporating biological characteristics enhanced visual perception ability while improving deformation accuracy and fidelity across all measured parameters [53]. The implementation of this model using 3DMax2020 and OpenGL4.6 established a platform for ongoing refinement of these quantitative metrics.
Experimental Protocols for Model Development and Validation
Protocol for Developing High-Fidelity Virtual Tissue Models
This detailed protocol provides a methodological framework for creating validated virtual biological models with emphasis on mechanical biological accuracy.
Workflow for Virtual Model Development
Protocol for Physiological Presence Assessment in VR Biological Environments
The following protocol assesses the sense of presence in VR biological environments, a crucial factor for active sensing research applications.
Physiological Presence Assessment Protocol
Implementation Framework for VR Biological Simulations
Technical Implementation Workflow
The implementation of high-fidelity biological models in VR environments requires a structured technical workflow that balances computational efficiency with biological accuracy.
Data Acquisition and Processing
- Collect high-resolution medical imaging data (micro-CT, MRI) at appropriate spatial resolutions for the target biological system
- Perform mechanical testing on ex vivo tissue samples to establish baseline material properties
- Compile literature values for biological materials to supplement experimental data
Geometric Model Construction
- Segment anatomical structures from medical imaging data using semi-automated algorithms
- Generate surface meshes with optimized polygon counts for real-time rendering
- Apply smoothing and decimation algorithms to maintain anatomical accuracy while reducing computational load
Material Property Assignment
- Implement constitutive models that incorporate viscoelastic, anisotropic, and nonlinear characteristics
- Assign region-specific material properties based on anatomical differentiation
- Optimize computational implementation for stable real-time simulation
VR Integration and Optimization
- Implement model within VR rendering environment (e.g., OpenGL 4.6, Unity, Unreal Engine)
- Integrate with haptic feedback devices to provide appropriate force feedback
- Optimize rendering pipeline to maintain target frame rates without visual artifacts
Recent implementations have demonstrated the effectiveness of this workflow, with a virtual liver model showing significant improvements in deformation accuracy and fidelity when biological characteristics were incorporated [53].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Solutions for Virtual Biological Modeling
| Category | Specific Tool/Resource | Function/Purpose | Implementation Notes |
|---|---|---|---|
| Modeling Software | 3DMax2020, Blender, Maya | 3D geometry reconstruction and mesh optimization | 3DMax2020 was successfully implemented in virtual liver modeling [53] |
| VR Development Platforms | OpenGL 4.6, Unity, Unreal Engine | Real-time rendering and interaction implementation | OpenGL 4.6 provides low-level control for specialized biological visualization |
| Haptic Interfaces | PHANTOM OMNI, HapticVR controllers | Force feedback during virtual tissue manipulation | Provides kinesthetic feedback essential for active sensing research |
| Physiological Monitoring | EEG, EDA, ECG, eye-tracking | Assessment of presence and cognitive engagement during VR experience | Critical for validating user experience in active sensing applications [52] |
| Biomechanical Simulation | SOFA, FEBio, ArtiSynth | Implementation of soft tissue deformation physics | Open-source frameworks that can be customized for specific biological systems |
Discussion: Applications in Active Sensing Research and Drug Development
The development of high-fidelity virtual models of biological systems has profound implications for active sensing research and pharmaceutical development. In active sensing research, these models provide simulated environments where researchers can study how biological organisms selectively acquire sensory information to guide motor behavior and decision-making processes. The embodied experience of VR creates unique opportunities to investigate sensorimotor integration in ways not possible with traditional experimental paradigms.
In drug development, high-fidelity virtual models enable researchers to simulate drug interactions at tissue and organ levels, providing insights into therapeutic effects and potential adverse reactions before proceeding to costly clinical trials. The incorporation of accurate biological characteristics allows for more predictive modeling of drug distribution, metabolism, and site-specific actions.
The measured decrease in questionnaire use and growing preference for physiological markers to define presence in VR [52] underscores the importance of objective validation methods for these applications. As the field advances, the integration of artificial intelligence, particularly deep learning approaches, offers promising avenues for refining these models and enhancing their predictive capabilities across research and development applications.
Creating high-fidelity virtual models of biological systems requires meticulous attention to both technical implementation and biological accuracy. By incorporating essential characteristics including viscoelasticity, anisotropy, nonlinearity, and viscoplasticity, researchers can develop virtual representations that faithfully emulate biological system behavior. These models provide valuable platforms for active sensing research and drug development when validated through comprehensive assessment protocols that include technical performance metrics, mechanical accuracy measurements, and physiological presence evaluation.
Future developments in this field will likely focus on increasing model complexity through multi-scale approaches that connect molecular, cellular, tissue, and organ-level phenomena. Additionally, the integration of machine learning methods for parameter optimization and real-time adaptation holds significant promise for creating virtual biological systems that not only replicate known behaviors but also predict novel responses to interventions. As these technologies mature, they will increasingly serve as essential tools for advancing our understanding of biological systems and accelerating the development of therapeutic interventions.
Virtual Reality (VR) has transcended its origins in gaming to become a critical tool for scientific research, particularly in the field of active sensing. Active sensing research investigates how organisms dynamically acquire and process sensory information to guide behavior and decision-making. VR provides an unparalleled platform for this research by allowing scientists to construct highly controlled, yet complex, sensory environments in which subject behavior can be precisely tracked and measured [57]. The core advantage lies in the ability to present multi-sensory stimuli within a fully interactive framework, enabling the study of perception and action loops in ways that are impossible in the real world. This capability is transforming research into crowd dynamics, neural mechanisms of navigation, and clinical interventions for sensory processing disorders.
However, the power of VR in active sensing research is gated by a fundamental technical hurdle: the effective integration of complex, often massive, datasets into the immersive environment. The process of importing, rendering, and enabling real-time interaction with this data presents a unique set of challenges that span computational, technical, and conceptual domains. This paper details these challenges, provides structured methodologies for overcoming them, and outlines the essential tools for researchers aiming to leverage VR for active sensing studies.
Data Typology and Integration Challenges
The first step in managing data integration is understanding the nature of the data itself. Complex datasets for VR can be broadly categorized, each presenting distinct integration challenges.
Table 1: Data Types and Associated Integration Challenges
| Data Type | Description | Primary VR Integration Challenges |
|---|---|---|
| Tracking & Motion Data [57] | Quantitative continuous data from motion capture, eye-tracking, and positional sensors. | High-frequency data streams; latency; synchronization of multiple data sources; real-time processing for feedback. |
| Environmental & Scene Data [19] | 3D models, textures, and spatial audio that define the virtual world. | Large file sizes (high-poly models, 4K textures); rendering performance bottlenecks; ensuring realism and interactivity. |
| Behavioral & Quantitative Data [58] | Numerical data from experiments, such as response times, physiological measures (heart rate, GSR), and survey results. | Mapping abstract numerical data to intuitive visual metaphors; enabling filtering and multi-variable analysis within VR. |
| Categorical & Qualitative Data [59] | Non-numerical data such as participant groupings, survey responses, or coded behaviors. | Visually representing categories without cluttering the environment; creating logical data hierarchies for user exploration. |
The challenges in Table 1 manifest in several critical technical areas. Computational Performance is paramount; VR requires a consistent high frame rate (often 90Hz or more) to prevent user discomfort [19]. Importing dense 3D models or large point clouds can cause significant frame rate drops. Data Synchronization is another major hurdle, especially in multi-user VR studies [57]. Aligning timestamps for motion tracking, physiological data, and in-world events across a network requires precision timing protocols. Finally, User Interface (UI) and Interaction Design for data representation is a significant challenge. Presenting complex quantitative data tables or 2D graphs within a 3D space must be done thoughtfully to avoid breaking immersion or causing cognitive overload [58].
Experimental Protocols for VR Data Integration
To ensure reproducible and valid results in active sensing research, a structured experimental protocol for data handling is essential. The following methodology provides a robust framework.
Protocol: Multi-User Behavioral and Motion Data Integration
1. Objective: To integrate real-time motion tracking and behavioral data from multiple participants into a shared VR environment for the study of collective crowd behavior [57].
2. Materials and Setup:
- VR Platform: A standalone VR headset (e.g., Meta Quest 3) [19].
- Tracking System: Inside-out tracking capabilities of the headset, supplemented with external base stations for higher precision if needed.
- Network Infrastructure: A dedicated local wireless network with low latency and high bandwidth.
- Data Server: A central server running synchronization software to aggregate data streams.
3. Procedure:
- Step 1: Data Acquisition and Pre-processing
- Record participant trajectories and body movements using the VR system's native tracking.
- Apply noise-filtering algorithms to the raw tracking data.
- Simultaneously, log discrete behavioral actions (e.g., button presses, gaze selection) as quantitative discrete event data [59].
- Step 2: Data Streaming and Synchronization
- Transmit each participant's processed tracking data (position, rotation) as continuous UDP packets to the central server to minimize latency.
- Send behavioral event data and physiological data (if used) as timestamped TCP packets to ensure reliability.
- The server applies a global clock and buffers incoming data packets to correct for network jitter before broadcasting a unified world state to all clients.
- Step 3: In-World Data Representation and Rendering
- Represent each participant as a simplified, rigged avatar model to maintain performance with multiple users.
- Visualize collective motion patterns (e.g., flow fields, density maps) as semi-transparent overlays on the virtual environment, which can be toggled by the researcher.
- Step 4: Data Recording and Export
- Record the synchronized global state at a fixed frequency (e.g., 30Hz) for post-hoc analysis.
- Export data in a structured format (e.g., JSON or CSV) containing fields for
timestamp,user_id,3d_position,avatar_pose, andbehavioral_events.
The following workflow diagram illustrates this multi-step protocol for integrating data into a VR environment for research.
Visualization and Workflow for Complex Data
Effectively visualizing integrated data is crucial for researcher insight. The choice of visualization must be matched to the data type and the research question.
Table 2: Data Visualization Techniques for VR Environments
| Research Data Type | Recommended VR Visualization | Benefit for Active Sensing Research |
|---|---|---|
| Quantitative Continuous [58] (e.g., Walking speed, Heart rate) | Interactive 3D Line Graphs; Color-mapped Heatmaps on avatars or paths. | Allows for correlation of physiological/behavioral metrics with spatial position and movement in real-time. |
| Quantitative Discrete [59] (e.g., Choice counts, Survey scores) | Animated 3D Bar Charts; Floating data tags attached to objects of interest. | Provides immediate, spatial understanding of frequency and distribution of participant choices or actions. |
| Categorical / Qualitative [59] (e.g., Participant group, Behavior type) | Distinctly colored avatars or objects; Spatial zoning with different textures/themes. | Enables rapid visual identification of different participant groups and their interaction patterns. |
The process of going from raw data to an immersive insight can be broken down into a logical workflow, which helps in identifying and isolating potential integration challenges at each stage.
The Scientist's Toolkit: Research Reagent Solutions
Building a successful VR active sensing lab requires a combination of hardware, software, and data management "reagents." The following table details these essential components.
Table 3: Essential Research Reagents for VR Data Integration
| Category | Item | Function |
|---|---|---|
| Hardware | Standalone VR Headset (e.g., Meta Quest 3) [19] | Provides an all-in-one platform for presenting the immersive environment and tracking user head and hand movements. |
| Hardware | Haptic Feedback Gloves/Suits [19] | Adds a critical layer of tactile realism, essential for studies on active touch and object manipulation. |
| Software | Game Engine (Unity / Unreal Engine) [60] | The core development environment for building the VR experience, importing 3D assets, and scripting interactions. |
| Software | NVIDIA Omniverse [60] | A collaborative platform that simplifies the integration of complex 3D datasets and models from various sources. |
| Software | Data Visualization Plugins (e.g., ChartXpo) [58] | Specialized tools within game engines to help create standard and advanced graphs (bar charts, scatter plots) in 3D space. |
| Data Management | WebXR/WebVR [60] | A set of web standards that allows for the delivery of VR experiences directly in a browser, simplifying data distribution and participant access. |
| Data Management | Real-time Synchronization Middleware | Custom or commercial software that handles the networking and time-alignment of data from multiple clients and sensors. |
The integration of complex datasets into VR environments remains a formidable challenge, yet overcoming it is the key to unlocking profound new capabilities in active sensing research. The challenges of performance, synchronization, and visualization are significant but can be systematically addressed through the structured protocols, appropriate visual mapping, and dedicated toolkits outlined in this guide. As VR hardware continues to become more accessible and powerful, and as software tools like AI-driven content creation and robust multi-user platforms evolve, the process of data integration will become increasingly streamlined [19] [60]. This progression will firmly establish VR not merely as a visualization tool, but as a fundamental instrument for the generation of scientific insight, enabling researchers to step inside their data and interact with complex systems in ways previously confined to the realm of imagination.
The emergence of fully immersive virtual reality (VR) represents a paradigm shift for research in active sensing—the process by which organisms selectively gather sensory information to guide motor actions and perceptual decisions. However, a significant barrier impedes the seamless integration of VR into experimental frameworks: cybersickness and visual discomfort. These phenomena directly disrupt the very active sensing processes that researchers aim to study, as symptoms like oculomotor disturbances, disorientation, and general discomfort can alter naturalistic sensory sampling behaviors [61]. The sensory conflict theory provides the dominant explanation for this challenge, positing that cybersickness arises from mismatches between visual motion cues processed by the eyes and the vestibular and proprioceptive signals indicating a stationary body [62] [63]. For researchers investigating active sensing, this conflict contaminates the natural sensorimotor loop, making VR an invaluable yet problematic tool that must be carefully managed to preserve the ecological validity of findings.
Quantitative Characterization of Cybersickness
Understanding the prevalence, severity, and underlying mechanisms of cybersickness is crucial for designing robust VR experiments in active sensing research. The following tables consolidate key quantitative findings from recent studies to inform experimental design and protocol development.
Table 1: Prevalence and Severity of Cybersickness Symptoms
| Symptom Category | Specific Symptoms | Prevalence/Increase | Measurement Scale/Notes |
|---|---|---|---|
| General Cybersickness | Nausea, disorientation, general discomfort | 40-70% of users [63]; ~80% after 10 min [62] | Cybersickness Questionnaire (CSQ), Simulator Sickness Questionnaire (SSQ) |
| Oculomotor Disturbances | Eye strain, headache, visual fatigue | Most frequently documented [61]; Eye strain +0.66 [62] | VRSQ (Virtual Reality Sickness Questionnaire) |
| Disorientation | Dizziness, imbalance | Common [61]; General discomfort +0.6 [62] | VRSQ, SSQ |
| Visual Fatigue | Eye fatigue, focusing issues | Blink frequency up to 52/min indicates severe fatigue [64] | Pupil diameter change, subjective ratings |
Table 2: Technical and User Factors Influencing Symptom Severity
| Factor Category | Specific Factor | Impact on Cybersickness/Discomfort | Supporting Evidence |
|---|---|---|---|
| Hardware Factors | Low Refresh Rate (<90Hz) | Increased motion blur and lag [63] | User reports, SSQ scores |
| High Latency Tracking | Delays cause sensory conflict [63] | User reports, SSQ scores | |
| Incorrect瞳距 (IPD) | Increased visual fatigue and discomfort [65] [66] | Objective eye-tracking, subjective feedback | |
| Content & Interaction Factors | High Visual Flow & Complexity | Overwhelms brain, precipitating sickness [63] | SSQ scores |
| Controller-based Locomotion | Higher sickness vs. gaze-based interaction [67] | Controlled experiments | |
| High Eye-Tracking Interaction Frequency | Increased visual fatigue at high (>0.8Hz) and low (<0.6Hz) frequencies [64] | Pupil diameter change, blink rate |
The following diagram illustrates the primary mechanism and contributing factors of cybersickness, contextualized within the active sensing loop.
Diagram: Cybersickness disrupts the active sensing loop via sensory conflict.
Experimental Protocols for Assessment and Mitigation
To ensure the validity of active sensing research in VR, rigorous protocols are needed to quantify and mitigate cybersickness. The following methodologies provide a framework for robust data collection.
Protocol 1: Quantifying Cybersickness in Seated VR Exposure
This protocol, adapted from a study investigating a virtual walk, is suitable for experiments where seated immersion is part of the active sensing paradigm [62].
- Objective: To assess the spatial presence and impact of an immersive VR experience on symptoms of cybersickness, emotions, and participant engagement.
- Participants: 30 healthy individuals (or as required by power analysis), with prior VR experience documented.
- Apparatus:
- Headset: Meta Quest 2 or equivalent with refresh rate ≥90Hz.
- Content: A 15-minute, passive 360° video tour (e.g., Venice Canals) with ambient audio.
- Seating: A rotating chair to facilitate gentle, unrestricted head and body movement.
- Procedure:
- Pre-Test: Participants complete the Virtual Reality Sickness Questionnaire (VRSQ) and the International Positive and Negative Affect Schedule-Short Form (I-PANAS-SF).
- Exposure: Participants experience the 15-minute virtual walk while seated on the rotating chair in a quiet, controlled environment.
- Post-Test: Participants immediately re-complete the VRSQ and I-PANAS-SF. They then complete the Spatial Presence Experience Scale (SPES) and the Flow State Scale (FSS).
- Data Analysis: Calculate pre-post differences in VRSQ and I-PANAS-SF scores. Use SPES and FSS to correlate presence and engagement with symptom severity.
Protocol 2: Evaluating Visual Guides for Sickness Reduction
This protocol tests an active content-creation strategy to mitigate sensory conflict, crucial for maintaining natural active sensing behaviors during locomotion-based tasks [67].
- Objective: To analyze the correlation between a visual guide (crosshair) and the reduction of VR sickness in a First-Person Shooter (FPS) game context.
- Participants: 32 individuals minimum (e.g., 23 male, 9 female), aged 20s, with no prior HMD VR experience and no history of hearing or balance disorders.
- Apparatus:
- Headset: HTC VIVE or equivalent.
- Controller: Xbox One Wireless Controller or equivalent.
- Content: A custom VR FPS game set in a space environment to induce multi-axis movement.
- Procedure:
- Pre-Test: Participants complete a preliminary SSQ (M1) to baseline motion sickness.
- Training: A preliminary experiment (M2) teaches participants HMD and controller operation.
- Experimental Scenarios: Participants are exposed to eight 60-second scenarios (S1-S8) in a counterbalanced order. Variables include:
- Visual guide: On/Off.
- Visual guide size: 0%, 10%, 30%, 50% of aspect ratio.
- Visual guide position: None, Head-tracking (H), Game controller (G), H & G.
- Game controller: On/Off.
- Post-Scenario Assessment: After each scenario, participants complete the SSQ. Rest videos are shown between scenarios to reset symptoms.
- Data Analysis: A paired t-test is used to compare SSQ scores across scenarios with and without the visual guide, and for different sizes and positions.
Protocol 3: Measuring Visual Fatigue from Eye-Tracking Interaction
This protocol is essential for studies integrating eye-tracking as an input method, as it directly measures the impact of interaction frequency on visual fatigue, a key component of active sensing [64].
- Objective: To investigate whether the frequency of eye movement interaction in VR causes user visual fatigue.
- Participants: 25 participants.
- Apparatus:
- Headset: HMD with a built-in eye-tracker (e.g., HTC VIVE Pro Eye).
- Software: A VR scene with visual targets appearing at controlled frequencies.
- Procedure:
- Frequency Exposure: Each participant undergoes a 20-minute experiment for each of the 8 interaction frequencies set between 0.2 Hz and 1.6 Hz.
- Data Collection:
- Objective: The HMD's built-in eye-tracker continuously captures pupil diameter and blink data.
- Subjective: Every minute, participants provide a subjective evaluation using a five-level fatigue scale.
- Data Processing: Pupil diameter data is processed with linear interpolation and noise reduction (e.g., Savitzky-Golay filter, Median filter).
- Data Analysis:
- The relative change rate of pupil diameter is calculated to reflect fatigue.
- Spearman correlation analysis explores the link between subjective comfort scores and blink frequency.
- Kruskal-Wallis tests analyze the relationship between blink frequency and interaction frequency.
The Researcher's Toolkit: Essential Reagents and Materials
For researchers replicating or building upon the aforementioned experimental protocols, the following table details key hardware, software, and assessment tools.
Table 3: Key Research Reagents and Experimental Materials
| Item Name/Type | Specification/Function | Experimental Role & Rationale |
|---|---|---|
| Head-Mounted Display (HMD) | High-refresh rate (≥90Hz), low persistence display, low latency tracking, 6DoF [63]. | Core apparatus for delivering fully immersive VR. High refresh rates and low latency are critical for minimizing sensory conflict. |
| Eye-Tracking Module | Integrated into HMD; samples pupil diameter and blink frequency at high rate (e.g., >60Hz) [64]. | Provides objective, continuous data on oculomotor activity and visual fatigue, crucial for quantifying a key aspect of active sensing. |
| Motion Controllers | 6DoF controllers (e.g., HTC VIVE Wands, Xbox One Wireless Controller) [67]. | Enables natural interaction within the VE, allowing for the study of embodied active sensing. |
| Simulator Sickness Questionnaire (SSQ) | 16-item questionnaire; scores nausea, oculomotor, disorientation subscales [62] [67]. | The gold-standard subjective metric for quantifying cybersickness severity and comparing across studies. |
| Virtual Reality Sickness Questionnaire (VRSQ) | Adapted from SSQ, focuses on 9 symptoms relevant to HMDs [62]. | A targeted tool for subjective cybersickness assessment in modern HMD-based VR. |
| Visual Guide (Crosshair) | 2D image (e.g., white circle, 1px line), size/position variable [67]. | An experimental visual reagent that acts as a rest frame to stabilize gaze and reduce vection-induced sensory conflict. |
| 3D Virtual Environment | Customizable 3D environment, preferably over 360° images [63]. | Provides a stable, grounded spatial reference for users, reducing disorientation and presence disruption compared to 2D backgrounds. |
Mitigating cybersickness and visual discomfort is not merely a technical challenge for improving user comfort; it is a fundamental prerequisite for conducting valid and reliable active sensing research within virtual environments. The sensory conflicts that underlie these symptoms directly corrupt the naturalistic feedback loops between sensation and action that are the focus of study. By adopting the rigorous assessment protocols—ranging from seated exposure tests to advanced eye-tracking fatigue measures—and implementing the technical mitigations detailed in this guide, researchers can create VR experiences that minimize artifactual interference. The successful integration of these strategies will enable the full potential of VR as a tool for unraveling the complexities of active sensing, leading to more robust findings in neuroscience, psychology, and beyond.
Virtual reality (VR) technology is fundamentally transforming research into active sensing—the process by which organisms voluntarily move sensory organs to explore their environment. In fields from neuroscience to drug development, VR enables the creation of controlled, immersive environments where researchers can study complex behaviors like the active touch of a rodent's whiskers or a human's fingertip exploration of textures [68]. This controlled setting is vital for isolating variables and understanding the neural mechanisms that underlie sensory perception. However, the specialized hardware required for this research—including head-mounted displays (HMDs), motion tracking systems, and custom tactile interfaces—often creates significant financial and technical barriers for many laboratories [54]. These barriers can limit participation in cutting-edge science and slow the pace of innovation. This guide details these challenges and presents actionable strategies, from leveraging open-source hardware to adopting cost-effective experimental designs, to democratize access to VR technology and fuel advancement in active sensing research.
Technical and Financial Hurdles in Research-Grade VR
The implementation of VR in active sensing research is fraught with specific, high-cost challenges. Understanding these bottlenecks is the first step toward developing effective strategies to overcome them.
- High-Fidelity Sensory Interfaces: Research into active touch requires tactile stimulators that can deliver precise, high-resolution feedback in sync with a user's movements. Specialized equipment, such as piezo-electric Braille element arrays used to simulate virtual textures, is complex and costly to develop and procure [68].
- Motion Tracking and Latency: A core component of active sensing research is the precise, real-time tracking of sensory organs (e.g., hands, fingers, or whiskers). This requires high-speed, low-latency tracking systems to update the virtual environment instantly based on user movement. Any perceptible delay can break immersion and invalidate behavioral data [57].
- Computational and Data Costs: Generating realistic virtual environments and processing the vast amounts of data from motion tracking and neurophysiological recordings (e.g., fMRI, MEG, EEG) demands substantial computational power. Furthermore, ensuring these complex systems are compatible with neuroimaging environments requires additional engineering and shielding, adding to the cost and complexity [68].
- Proprietary Lock-In: The VR market is dominated by proprietary architectures and software platforms. This can lead to vendor lock-in, where labs become dependent on a single company for updates, support, and compatible software tools, stifling customization and inflating long-term costs [69].
Table 1: Cost Analysis of Proprietary vs. Emerging Open-Source VR Hardware Approaches
| Component | Proprietary Solution | Open-Source / Custom Alternative | Key Trade-Offs |
|---|---|---|---|
| AI/Compute Chip | NVIDIA GPUs (e.g., H100/H200) [69] | RISC-V based processors (e.g., Tenstorrent, SiFive) [69] | Lower licensing cost & high customizability vs. potentially lower initial performance |
| Tactile Stimulator | Commercial haptic interfaces | Custom-built piezo-electric piston matrix [68] | High upfront development time vs. tailored functionality for specific research needs |
| Platform Software | Licensed, closed-source SDKs | Community-driven, open-source platforms | Less vendor lock-in and greater transparency vs. potentially less polished user experience |
Strategic Pathways to Improved Accessibility
Several promising strategies are emerging to directly address the cost and accessibility challenges of research-grade VR.
The Open-Source Hardware Revolution
A paradigm shift is underway with the rise of open-source hardware, which is particularly impactful in the realm of AI-specific chips. Instruction set architectures (ISAs) like RISC-V are royalty-free and modular, allowing developers to tailor chips to specific AI and VR workloads without exorbitant licensing fees [69].
- Technical Advantages: RISC-V's modularity allows for custom instructions and domain-specific accelerators, which is crucial for the diverse workloads in AI-driven VR research. Its scalable vector processing extension is ideal for the data-parallel tasks fundamental to deep learning and real-time environment rendering [69].
- Cost and Flexibility: Open-source designs dramatically lower the barrier to entry for custom silicon development. As noted by industry experts, AI processors are simpler than commonly perceived and do not require billions to develop, making open-source alternatives a viable path for specialized research applications [69].
Leveraging Budget-Conscious VR Modalities
While fully immersive VR with head-mounted displays is powerful, researchers can often gather high-quality data using more accessible and affordable forms of VR.
- Cinematic VR (Cine-VR): This approach uses 360-degree video filmed with cameras like the Insta360 Pro 2, presented via affordable HMDs like the Oculus Go [70]. Cine-VR is highly effective for role-playing and clinical encounter simulations, as it provides a strong sense of presence and emotional connection at a fraction of the cost of a fully computer-generated environment [70].
- Semi-Immersive VR: For some research questions, a semi-immersive setup—such as displaying a 360-degree environment on a standard high-resolution monitor—can be sufficient. This approach avoids the cost of HMDs and the technical challenges of multi-user, fully immersive platforms while still providing a controlled visual context for behavioral studies [57].
Practical Guidelines for MEG/fMRI Compatibility
A significant portion of active sensing research requires correlating behavior with neural activity. Custom, cost-effective hardware must be compatible with neuroimaging techniques. The tactile VR system developed by [68] provides an excellent model:
- Low-Noise Design: Using a resistive touchpad with a reduced input voltage (50 mV instead of 5V) and incorporating galvanic decoupling and low-pass filters significantly reduces electromagnetic artifacts that corrupt sensitive MEG signals [68].
- Synchronized Control: Operating the control unit at a fixed frequency (e.g., 600 Hz) confines electrical noise to specific, predictable harmonics, making it easier to filter out during data analysis without masking the neural signals of interest [68].
Experimental Design for Resource Efficiency
Well-designed experiments can maximize data yield without requiring the most expensive hardware.
- Within-Subject Designs: Where possible, use experimental designs where participants experience all conditions. This reduces between-subject variability and allows for robust findings with smaller sample sizes.
- Focus on Key Metrics: Instead of striving for the highest possible graphical fidelity, focus on the key sensory or behavioral metrics that answer the research question. For instance, in active touch, the precise delivery of vibrotactile patterns is more critical than hyper-realistic visual rendering [68].
Detailed Experimental Protocol: A Case Study in Active Touch
The following protocol, based on the tactile virtual reality system described in [68], provides a concrete example of implementing a cost-effective, neuroimaging-compatible VR setup for active somatosensation research.
Objective: To investigate the neural correlates of active versus passive tactile perception using MEG.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function/Description | Example/Specification |
|---|---|---|
| Piezo-Electric Stimulator | Delivers spatial-tactile patterns to the fingertip. | 4x4 matrix of pistons (1mm diameter); e.g., Metec AG Braille elements [68]. |
| Resistive Touchpad | Tracks the position of the scanning probe in 2D space. | KEYTEC KTT-191LAM, modified for low magnetic noise [68]. |
| Control Units | Interfaces between computer, touchpad, and stimulator; updates stimulation at high frequency. | Custom in-house built touchpad and piezo control units [68]. |
| Scanning Probe | Handheld device housing the piezo tactile stimulator. | Custom body designed to be held comfortably with the probing finger placed on the piston matrix [68]. |
| MEG/EEG System | Records neuromagnetic/brain activity with high temporal resolution. | A whole-head MEG system housed in a magnetically shielded room. |
Procedure:
- Setup: Place the touchpad control unit and piezo-electric control unit outside the MEG shielded room. Connect them to the stimulation computer via USB. Use twisted, low magnetic noise wires to connect the control units to the touchpad and scanning probe inside the MEG room.
- Calibration: Calibrate the system to map coordinates on the touchpad to specific activation patterns of the piston matrix.
- Participant Preparation: Seat the participant in the MEG chair. Place the touchpad on their lap or a nearby stand. Instruct them on how to hold the scanning probe and place their index fingertip on the piston matrix.
- Task Conditions:
- Active Condition: Participants actively move the scanning probe across the touchpad in a specified pattern (e.g., back-and-forth scanning). The piston matrix stimulates the fingertip based on the probe's position, simulating a virtual texture (e.g., a grating).
- Passive Condition: The participant's hand remains stationary. The scanning probe is mechanically moved by the experimenter (or a robot) along the same path, delivering an identical sequence of tactile stimulation to the fingertip.
- Data Recording: Simultaneously record MEG data and the trigger signals from the control unit marking the onset of each stimulation sequence and the position data from the touchpad.
Diagram 1: Active touch workflow
The integration of VR into active sensing research offers unparalleled opportunities to decode the brain's interaction with the environment. While significant hardware and cost barriers exist, they are not insurmountable. The strategic adoption of open-source hardware principles, the clever use of cost-effective VR modalities like cine-VR, and the meticulous design of compatible, low-noise experimental apparatus provide a clear roadmap to improved accessibility. By embracing these strategies, the research community can democratize access to these powerful tools, ensuring that a wider range of scientists and labs can contribute to the burgeoning field of active sensing, ultimately accelerating progress in neuroscience, psychology, and drug development.
Ensuring Data Privacy and Ethical Use of Patient-Specific Models
The integration of patient-specific models in healthcare research, particularly within immersive technologies like virtual reality (VR), is transforming the understanding of active sensing and its role in human perception. These computational models, which simulate individual patient physiology, genetics, or neural processes, enable unprecedented personalization in drug development and therapeutic interventions. However, this powerful approach introduces significant ethical complexities regarding data privacy, patient autonomy, and algorithmic fairness [71] [38]. As researchers increasingly utilize VR to study active sensing—the process by which organisms voluntarily control sensory inputs through motor activity—the handling of sensitive neural and behavioral data requires rigorous ethical frameworks. This technical guide examines core principles and methodologies for ensuring ethical compliance and robust privacy protection when working with patient-specific models in research environments bridging VR, active sensing, and therapeutic development.
Core Ethical Principles and Privacy Challenges
Foundational Ethical Frameworks
The ethical development and deployment of patient-specific models in healthcare research rests upon several core principles that must be balanced against technological innovation. Patient autonomy stands as a primary concern, emphasizing the right of individuals to control their personal health information and its applications [72]. This principle necessitates transparent consent processes that clearly communicate how patient data will be used in model development, including potential secondary applications. Justice and equity require researchers to actively identify and mitigate biases that may be inherent in training data or algorithmic processes, ensuring models do not perpetuate or exacerbate healthcare disparities across demographic groups [71]. The principle of beneficence obligates researchers to maximize the benefits of patient-specific models while minimizing potential harms through robust privacy protections and security measures. Finally, transparency and accountability demand clear documentation of model development processes, data handling procedures, and decision-making pathways to maintain research integrity and public trust [71] [73].
Specific Privacy Risks in Patient-Specific Modeling
Patient-specific models introduce unique privacy vulnerabilities that extend beyond conventional health data concerns. The identifiability risk represents a significant challenge, as even anonymized datasets may contain sufficient unique characteristics to allow re-identification when combined with other data sources [73]. Model inversion attacks present another serious threat, wherein malicious actors exploit access to model outputs to reconstruct sensitive training data, potentially revealing confidential patient information [73]. The generational capacity of advanced AI models introduces additional vulnerabilities, as they may inadvertently memorize and reproduce protected health information (PHI) from their training datasets in seemingly novel outputs [73]. Furthermore, the complex data ecosystems supporting patient-specific modeling often involve transferring sensitive information across institutions or to cloud-based platforms, creating multiple potential points of unauthorized access or breach [71] [73].
Table 1: Privacy Risks and Mitigation Strategies in Patient-Specific Modeling
| Risk Category | Specific Vulnerabilities | Potential Impact | Recommended Mitigations |
|---|---|---|---|
| Data Processing | Unauthorized access during transfer; Inadequate de-identification | Privacy breaches; Regulatory violations | Encryption (in transit/at rest); Data anonymization; Secure APIs |
| Model Development | Model inversion attacks; Membership inference; Data memorization | Reconstruction of training data; PHI leakage | Differential privacy; Federated learning; Homomorphic encryption |
| Consent Management | Inadequate informed consent; Scope creep in data usage | Ethical violations; Erosion of trust | Dynamic consent models; Clear usage boundaries; Patient portals |
| Regulatory Compliance | Cross-jurisdictional conflicts; Rapid technological evolution | Legal penalties; Implementation delays | Privacy-by-design; Regular audits; Regulatory alignment |
Regulatory Requirements and Compliance Frameworks
Major Privacy Regulations
Researchers developing patient-specific models must navigate a complex landscape of privacy regulations that vary by jurisdiction. The Health Insurance Portability and Accountability Act (HIPAA) establishes standards for protecting sensitive patient data in the United States, requiring appropriate safeguards for protected health information and limiting its use without patient authorization [71] [74]. The General Data Protection Regulation (GDPR) in the European Union imposes stringent requirements for data processing, including lawful basis for processing, data minimization, and the right to erasure, with special provisions for health data as a "special category" of personal information [74]. Additionally, the California Consumer Privacy Act (CCPA) grants California residents rights over their personal information, including knowledge of what data is collected and how it is used, and the right to opt out of its sale [74]. Compliance with these frameworks requires implementing technical and organizational measures such as data encryption, access controls, and comprehensive audit trails to monitor data access and usage [71] [74].
Emerging Regulatory Guidance for AI in Healthcare
Regulatory bodies are increasingly developing specific frameworks to address the unique challenges posed by AI and machine learning in healthcare contexts. The FDA's approach to model-informed drug development acknowledges the value of computational modeling while emphasizing the need for robust validation [38]. Emerging standards like the American Society of Mechanical Engineers (ASME) Verification and Validation 40 (V&V40) and the International Council for Harmonization (ICH) M15 guidance establish best practices for model development, validation, and submission [38]. For reporting standards, the TRIPOD-LLM statement extends traditional prediction model guidelines to address the unique challenges of large language models in biomedical and healthcare applications [73]. These evolving frameworks increasingly emphasize the importance of demonstrating real-world clinical efficacy rather than merely technical proficiency on historical datasets [71] [38].
Technical Safeguards and Privacy-Enhancing Technologies
Data Protection Methodologies
Implementing robust technical safeguards is essential for protecting patient privacy throughout the model development lifecycle. Data anonymization techniques remove directly identifiable information from datasets, while de-identification processes eliminate or obscure identifying characteristics to prevent re-identification [71] [74]. Advanced encryption methods should be applied to protect data both in transit and at rest, with regular updates to encryption protocols to address emerging cyber threats [71] [74]. Strict access control policies based on role-based permissions ensure that researchers and developers only access information relevant to their specific functions, reducing the risk of internal data exposure [74]. Additionally, privacy-by-design approaches integrate privacy considerations from the initial stages of system design rather than as an afterthought, creating more fundamentally secure architectures [71] [74].
Advanced Privacy-Preserving Computation Techniques
Several advanced computational techniques enable model development while minimizing privacy risks. Federated learning allows model training across decentralized devices or servers holding local data samples without exchanging the data itself, thus maintaining data locality and reducing privacy risks [73]. Differential privacy adds carefully calibrated mathematical noise to query results or model parameters, providing strong mathematical guarantees against privacy breaches while preserving data utility [73]. Homomorphic encryption enables computation on encrypted data without needing to decrypt it first, allowing sensitive health information to remain protected throughout the analytical process [73]. These techniques can be combined in layered approaches to create comprehensive privacy protection frameworks suitable for different research contexts and sensitivity levels.
Diagram 1: Privacy-preserving technical approaches for patient-specific models.
Experimental Protocols for Ethical Patient-Specific Modeling
Data Collection and Informed Consent Framework
Establishing ethical data collection practices requires structured protocols that prioritize patient autonomy and transparency. The consent process must provide clear, comprehensive information about how patient data will be used in model development, including potential secondary applications and any third-party sharing [73] [72]. Researchers should implement dynamic consent models that allow patients to adjust their preferences over time rather than relying on single-point authorization [72]. Data minimization principles should guide collection practices, limiting data acquisition to only what is strictly necessary for the intended research purpose [74]. Documentation should include detailed records of consent procedures, data provenance, and any transformations applied to original datasets. Regular ethics reviews should evaluate collection protocols to identify potential vulnerabilities or ethical concerns before implementation [73].
Model Validation and Bias Assessment Protocols
Robust validation methodologies are essential for ensuring patient-specific models perform equitably across diverse populations. Comprehensive auditing should evaluate models for potential biases related to demographic factors, socioeconomic status, or healthcare access disparities [71]. Representative sampling techniques ensure training datasets adequately reflect the target population demographics, reducing the risk of performance disparities across subgroups [71]. Continuous monitoring processes should track model performance in real-world applications to identify degradation or emerging biases not apparent during initial development [71]. Transparency documentation should clearly outline model limitations, known performance characteristics across subgroups, and potential failure modes to guide appropriate clinical or research use [71] [38].
Table 2: Experimental Protocol Framework for Ethical Patient-Specific Modeling
| Research Phase | Core Ethical Considerations | Required Documentation | Validation Metrics |
|---|---|---|---|
| Study Design | Ethical review approval; Patient burden assessment; Inclusion criteria | IRB approval; Protocol specification; Data management plan | Representativeness score; Power analysis; Privacy impact assessment |
| Data Collection | Informed consent; Data minimization; Cultural appropriateness | Consent records; Data provenance; Privacy safeguards | Consent comprehension; Data quality; Demographic diversity |
| Model Development | Algorithmic fairness; Transparency; Privacy preservation | Bias audit results; Model architecture decisions; Privacy techniques applied | Performance equity; Privacy loss quantification; Feature importance |
| Validation & Testing | Clinical relevance; Generalizability; Error analysis | Validation protocols; Failure mode analysis; Subgroup performance | Real-world accuracy; Demographic parity; Model calibration |
| Deployment & Monitoring | Ongoing surveillance; Update procedures; Incident response | Monitoring plan; Update protocols; User feedback mechanisms | Performance drift; Adverse event reports; User satisfaction |
VR-Specific Considerations for Active Sensing Research
Privacy Implications in VR and Active Sensing Applications
Virtual reality platforms used in active sensing research present unique privacy challenges that require specialized approaches. Biometric data collection in VR environments extends beyond conventional health information to include detailed movement patterns, gaze tracking, physiological responses, and interaction behaviors that may serve as identifiable biomarkers [52] [75]. The immersive nature of VR creates rich datasets of unconscious behaviors and reactions that users may not even be aware they are revealing, raising questions about what constitutes informed consent for such nuanced data collection [52]. Environmental context captured through VR applications may inadvertently record information about a user's physical surroundings, creating additional privacy concerns beyond the intended research data [75]. Furthermore, the multimodal data streams typical in VR research (combining physiological, behavioral, and environmental data) create heightened re-identification risks even when individual data sources are anonymized [52] [75].
Ethical VR Experimental Design for Active Sensing Studies
Designing ethically sound VR research protocols requires addressing the unique aspects of immersive technologies while maintaining scientific rigor. Comprehensive consent procedures should specifically address the types of data collected in VR environments, including biometric, behavioral, and environmental information, with clear explanations of how this data will be used, stored, and protected [75]. Privacy-preserving sensor data handling should implement techniques such as on-device processing where feasible, minimizing raw data transmission and storage [75]. User control mechanisms should provide participants with clear options to pause, stop, or review data collection during VR experiments, acknowledging the potentially disorienting nature of immersive experiences [75] [76]. Data retention policies should establish specific timelines for different categories of VR-collected data, with explicit procedures for secure deletion at the end of the retention period [75]. These specialized considerations complement general ethical research practices to address the unique challenges of VR-based active sensing studies.
Diagram 2: VR data handling workflow for active sensing research.
Implementation Checklist and Research Reagent Solutions
Ethical Implementation Checklist
- Regulatory Compliance: Verify alignment with HIPAA, GDPR, and other relevant regulations; Document compliance measures [71] [74]
- Informed Consent: Implement comprehensive consent procedures specifically addressing model development and data reuse; Consider dynamic consent frameworks [73] [72]
- Privacy by Design: Integrate privacy-enhancing technologies from project inception; Conduct privacy impact assessment [71] [74]
- Bias Mitigation: Audit training data for representativeness; Test model performance across demographic subgroups [71]
- Transparency Documentation: Create detailed model cards specifying intended use, limitations, and performance characteristics [71] [38]
- Security Safeguards: Implement encryption, access controls, and regular security audits; Develop breach response plan [71] [74]
- Ongoing Monitoring: Establish procedures for continuous evaluation of model performance and privacy protection [71]
- Stakeholder Engagement: Include patient representatives in ethical review processes; Solicit diverse perspective [72]
Research Reagent Solutions for Ethical Implementation
Table 3: Essential Research Reagents for Ethical Patient-Specific Modeling
| Tool Category | Specific Solutions | Primary Function | Ethical Application |
|---|---|---|---|
| Data Anonymization | ARX Privacy Tool; Amnesia; Differential privacy libraries | De-identification; k-anonymity implementation; Noise injection | Protects patient privacy while maintaining data utility for research |
| Bias Detection | AI Fairness 360; Fairlearn; Aequitas | Algorithmic fairness assessment; Disparity measurement | Identifies and mitigates discriminatory patterns in models and data |
| Secure Computation | PySyft; OpenMined; Microsoft SEAL | Federated learning; Homomorphic encryption; Secure multi-party computation | Enables collaborative model training without sharing raw patient data |
| Consent Management | Dynamic consent platforms; Blockchain-based systems | Consent tracking; Preference management; Patient engagement | Supports ongoing patient autonomy and participation preferences |
| Model Transparency | SHAP; LIME; Model cards | Interpretability; Feature importance; Documentation | Enhances understanding of model behavior and limitations |
| VR-Specific Tools | VR privacy frameworks; Biometric data handlers | Specialized anonymization; Secure sensor data processing | Addresses unique privacy challenges in immersive research environments |
Benchmarking VR: Validating Outcomes Against Traditional Research Methods
The integration of virtual reality (VR) into experimental science represents a paradigm shift in how researchers approach complex biological and chemical investigations. This transition is particularly relevant in the field of active sensing research, where understanding dynamic, multi-dimensional interactions is paramount. As wet-lab experimentation faces constraints related to cost, waste, and accessibility, VR offers a complementary approach that enables immersive visualization and manipulation of complex molecular structures [2]. This technical guide provides a systematic framework for quantifying the efficacy of VR versus traditional wet-lab experimentation through defined metrics, standardized protocols, and comparative analysis, providing researchers with evidence-based methodologies for evaluating these complementary approaches.
Quantitative Metrics for Comparative Analysis
A rigorous comparison between VR and wet-lab experimentation requires quantifying performance across multiple dimensions. The tables below synthesize key efficacy indicators identified from empirical studies.
Table 1: Core Performance Metrics in Skill Transfer Studies
| Metric Category | Specific Measurable Parameters | Application Context | Superior Modality (Evidence) |
|---|---|---|---|
| Technical Proficiency | Circularity, Size, Centering of surgical maneuvers [77] | Surgical Training (Capsulorhexis) | VR Training [77] |
| Procedure-specific scoring systems (e.g., 0-10 scale) [77] | Surgical Training | VR Training (Score: +3.67 vs. +0.33) [77] | |
| Operational Efficiency | Procedure Time [78] | Surgical Training | VR Training [78] |
| Consistency & Error Control | Standard Deviation of Performance Scores [77] | Surgical Training | VR Training (Lower SD: 1.3 vs. 2.1) [77] |
| Rate of Intraoperative Complications [78] | Surgical Training | VR Training [78] |
Table 2: System Efficiency and Accessibility Metrics
| Metric Category | Specific Measurable Parameters | Wet-Lab Characteristic | VR Characteristic |
|---|---|---|---|
| Resource Utilization | Material Waste (e.g., tubes, containers, substrates) [79] | High (Single-use items) | Minimal (Digital process) [79] |
| Scalability & User Capacity [79] | Limited by physical space and equipment | Virtually unlimited [79] | |
| Process & Analytics | Traceability of Process Steps [79] | Limited (Often only end-product analysis) | Comprehensive (Step-by-step recording) [79] |
| User Engagement | Psychological Engagement & Focus Levels [80] | Variable | Quantifiably Higher [80] |
Experimental Protocols for Efficacy Measurement
Protocol 1: Structured Skill Transfer in Surgical Training
This protocol is adapted from a randomized, controlled study investigating VR training for ophthalmological surgery [77].
- Objective: To determine if structured VR training improves subsequent wet-lab performance of a specific surgical task (capsulorhexis) compared to a control group with no VR training.
- Participants: Medical students and surgical residents with no prior expert-level experience in the procedure. They are randomly assigned to VR training or control groups.
- Pre-Test: All participants perform the target task (e.g., three capsulorhexis attempts) in a wet-lab setting using porcine eyes. Performances are recorded.
- Intervention: The VR training group completes multiple structured training sessions on a high-fidelity simulator (e.g., EYESi). Training involves:
- Basic skill tasks and procedure-specific tasks of increasing difficulty.
- Preset, objective performance goals that must be met for each task before progression.
- Control: The control group receives no supplemental training between the pre- and post-test.
- Post-Test: All participants repeat the wet-lab task under identical conditions to the pre-test.
- Data Collection & Analysis:
- Blinded Assessment: Recorded performances from pre- and post-tests are assessed by a masked observer using a predefined scoring system.
- Primary Outcome: The intra-individual difference in the average overall performance score between the first and second wet-lab session.
- Statistical Comparison: The improvement scores of the VR training group are statistically compared to those of the control group.
Protocol 2: Molecular Biology Laboratory Simulation
This protocol is based on pioneering projects developing VR for molecular biology wet-lab training [79].
- Objective: To evaluate the efficacy of a VR wet-lab in accurately teaching standard molecular biology techniques and protocols compared to traditional training.
- Participants: Two cohorts of trainees: one trained exclusively in a VR wet-lab environment, the other via traditional, supervised practice in a physical lab.
- VR Simulation: The VR environment ("Wet-Lab-VR") realistically recreates the lab, allowing users to interact with tubes, pipettes, and equipment. Its core is a software infrastructure that simulates biochemical processes and molecular biological reactions in real-time based on user actions [79].
- Intervention: Both groups learn and practice a standard protocol, such as polymerase chain reaction (PCR) or plasmid digestion.
- Experimental Workflow:
- Cohort 1 (VR): Performs the protocol repeatedly in the VR environment, receiving automated feedback.
- Cohort 2 (Traditional): Performs the protocol in a physical lab under supervisor guidance.
- Outcome Measures:
- Final Product Accuracy: The success rate of the experimental procedure in both groups.
- Process Efficiency: Time to completion and material waste.
- Skill Assessment: Evaluation of technique by an expert, blinded to the training method.
- Error Analysis: For the VR group, the system's recorded step-by-step data is analyzed to identify common error points [79].
Diagram 1: Skill Transfer Experiment Workflow
The Scientist's Toolkit: Research Reagent Solutions
The transition to VR-based experimentation relies on a suite of specialized hardware and software tools that constitute the modern researcher's toolkit.
Table 3: Essential Components for VR and Wet-Lab Experimentation
| Tool Category | Specific Tool / Solution | Function & Application |
|---|---|---|
| VR Hardware Platforms | Head-Mounted Display (HMD) (e.g., Meta Quest 2, HTC VIVE) [81] | Provides visual and aural immersion in the virtual environment; the primary hardware for VR experiences. |
| Context-Aware Sensors | Eye Tracker [81] | Tracks user's gaze and pupil movement, providing data for attention and cognitive load analysis. |
| Electroencephalogram (EEG) Headset (e.g., Emotiv Insight) [80] | Monitors brain activity to assess cognitive states like engagement, stress, and relaxation. | |
| Physiological Sensors (Pulse, Respiration, GSR) [81] | Measures autonomic nervous system responses (heart rate, breathing, skin conductance) for emotional state inference. | |
| Software & Simulation Engines | Unity Game Engine [81] | A core development platform for creating interactive, 3D VR applications and simulations. |
| Data Collection Framework (e.g., ManySense VR) [81] | A reusable software framework that unifies data collection from diverse sensors for context-aware VR applications. | |
| Traditional Wet-Lab Materials | Organic Animal Tissues (e.g., Porcine Eyes) [77] | Provides a realistic biological substrate for practicing surgical skills in a controlled wet-lab setting. |
| Plastic Tubes, Pipettes, Substrates [79] | Standard consumables for molecular biology procedures; their digital counterparts are used in VR simulations. |
Context-Awareness and Embodiment in VR
A significant advantage of VR is its capacity for context-awareness, which moves beyond one-size-fits-all experiences to enable personalized, adaptive experimentation. A reusable data collection framework, such as ManySense VR, allows for the unified gathering of data from diverse sources including eye trackers, EEG, and other physiological sensors [81]. This multi-modal data enables the VR system to infer the user's cognitive and emotional state, such as engagement levels, which have been shown to be higher in immersive applications [80].
This context-awareness is crucial for achieving a strong sense of embodiment—the "ensemble of sensations that arise in conjunction with being inside, having, and controlling a body" in VR [81]. High-quality embodiment requires accurate tracking of the user's body beyond the head and hands, often achieved through inverse kinematics (IK) and data from additional sensors [81]. For active sensing research, a strong sense of embodiment allows researchers to intuitively manipulate molecular structures in 3D space, facilitating a deeper understanding of spatial relationships and interactions [2].
Diagram 2: Context-Aware VR System Architecture
Application in Drug Design and Substance Use Research
The quantitative benefits of VR are finding concrete applications in complex fields like drug design and substance use disorder (SUD) research. In structure-based drug design, VR enables researchers to visualize and manipulate complex 3D molecular structures immersively, allowing for intuitive exploration of protein-ligand interactions in real-time [2]. This capability complements the growing suite of AI tools by providing a spatial and visual context for computational predictions.
In SUD therapy, VR has shown efficacy as a tool for exposure-based interventions. Studies have utilized immersive VR to create controlled environments where cravings can be safely induced and managed. A systematic review indicated that VR is effective at reducing substance use and cravings, particularly for nicotine use disorders, though findings on its impact on co-occurring mood and anxiety symptoms were mixed [82]. This therapeutic application demonstrates a different facet of efficacy, where the key metric is not technical skill transfer but the successful management of physiological and psychological responses in a clinically relevant context.
The quantification of efficacy between VR and wet-lab experimentation reveals a nuanced landscape. For training procedural and surgical skills, VR demonstrates clear, measurable benefits in improving technical performance, consistency, and patient safety while reducing resource consumption and waste [77] [79] [78]. The integration of context-aware sensors and embodiment technologies further enhances the VR experience by providing a personalized and deeply immersive environment that fosters high user engagement [81] [80]. For applications in drug design and behavioral therapy, VR offers unique capabilities for spatial molecular manipulation and controlled clinical intervention that are difficult to replicate in traditional settings [82] [2]. Ultimately, VR does not necessarily seek to replace wet-lab experimentation but to serve as a powerful, complementary tool within the scientific method. The future of experimental science lies in leveraging the respective strengths of both physical and virtual realms to accelerate discovery, enhance education, and improve therapeutic outcomes.
Analyzing Cost and Time Efficiency in Preclinical Research Phases
The preclinical research phase represents a critical bottleneck in the journey from scientific discovery to therapeutic application, characterized by escalating costs, extended timelines, and high failure rates. Traditional preclinical methodologies face significant challenges in translating basic research findings into clinically relevant outcomes, with attrition rates exceeding 95% for certain drug classes and development cycles spanning 3-6 years before clinical testing can commence. Within this challenging landscape, innovative technologies are emerging to enhance research efficiency, with virtual reality (VR) positioned to revolutionize how scientists interact with complex biological data.
The integration of VR into preclinical workflows aligns with a broader industry shift toward digital transformation in life sciences. As pharmaceutical and biotechnology companies seek to optimize resource allocation and compress development timelines, virtual reality technologies offer unprecedented capabilities for data visualization, protocol simulation, and collaborative analysis. This technical guide examines how VR-enabled active sensing research can address persistent inefficiencies in preclinical phases through enhanced spatial understanding, iterative experimental design, and reduced reliance on physical resources, ultimately bridging the gap between fundamental research and clinical application.
The Current Preclinical Research Landscape
Market Dynamics and Efficiency Challenges
The global preclinical Contract Research Organization (CRO) market, valued at approximately $6.4 billion in 2024 and projected to reach $11.3 billion by 2033, reflects the growing reliance on specialized outsourcing to manage complex research requirements [83]. This expansion is driven by several persistent challenges in internal research operations:
- Rising drug development costs compel organizations to seek more efficient preclinical models
- Regulatory complexities require more comprehensive data packages before clinical transition
- Chronic disease burden necessitates more sophisticated research approaches for complex conditions
- Specialized expertise requirements increasingly favor outsourcing to dedicated CRO providers
North America currently dominates the preclinical CRO landscape with a 47.5% market share in 2024, followed by rapidly growing Asia Pacific markets offering cost-effective alternatives [83]. This geographic distribution highlights how efficiency pressures are reshaping global research strategies, with organizations increasingly seeking regional advantages in cost structures and specialized capabilities.
Traditional Preclinical Workflow Limitations
Conventional preclinical research methodologies exhibit several systemic inefficiencies that prolong timelines and increase costs:
- Sequential testing protocols that extend project durations through linear dependencies
- Physical model limitations requiring resource-intensive maintenance and replication
- Spatial comprehension challenges in complex biological systems leading to design flaws
- Protocol optimization bottlenecks requiring multiple iterative physical experiments
- Data fragmentation across specialized teams and experimental systems
These limitations are particularly pronounced in complex research areas such as neurological disorders, oncology, and metabolic diseases, where biological complexity translates directly to extended preclinical timelines and higher costs. The transition toward targeted therapies and personalized medicine approaches further exacerbates these challenges, as traditional one-size-fits-all preclinical models struggle to accommodate increasingly specific research questions.
Virtual Reality as an Efficiency Catalyst
Technical Foundations of VR in Preclinical Research
Virtual reality technology enables a paradigm shift in preclinical research through several core capabilities:
- Immersive visualization of complex biological systems with spatial context preservation
- Real-time interaction with simulated experimental environments and parameters
- Multi-sensory integration combining visual, haptic, and auditory feedback
- Collaborative virtual workspaces enabling distributed expert participation
- Dynamic simulation of biological processes and experimental outcomes
Advanced VR systems incorporate head-mounted displays (HMDs) with head-tracking systems, haptic feedback devices, and manipulation interfaces that collectively create immersive research environments [84]. These systems transform abstract data into spatially coherent models that researchers can manipulate with intuitive gestures and actions, significantly enhancing comprehension of complex biological relationships.
The efficacy of VR in research applications stems from its alignment with dual-code theory, which posits that information processing through both visual and verbal channels creates multiple representations that strengthen neural connections and improve recall [85]. This cognitive advantage translates directly to research efficiency through enhanced pattern recognition, improved experimental design, and more effective knowledge transfer between team members.
Quantitative Efficiency Gains from VR Implementation
Table 1: Documented Efficiency Improvements from VR Implementation in Preclinical Research
| Efficiency Metric | Traditional Methods | VR-Enhanced Approach | Improvement | Source |
|---|---|---|---|---|
| Procedural accuracy | Baseline | VR training | 42% improvement | [86] |
| Training time | Conventional methods | VR platform | 38% reduction | [86] |
| Error rates | Standard training | VR with haptic feedback | 45% reduction | [86] |
| Skill retention | Control group | VR training group | Significant gains | [86] |
| Trainee confidence | Baseline assessment | Post-VR training | 48% increase | [86] |
| Knowledge retention | Traditional learning | VR medical training | 63% improvement | [19] |
| User engagement | Conventional training | VR training | 72% improvement | [19] |
| Task completion time | Standard simulation | VR simulation | 30-50% faster | [87] |
The efficiency gains demonstrated in Table 1 reflect fundamental advantages in how VR facilitates research processes. Beyond these quantitative metrics, VR implementation generates significant qualitative improvements in research quality, including enhanced spatial understanding of biological systems, more effective identification of experimental design flaws, and accelerated troubleshooting of methodological approaches.
VR-Enabled Active Sensing Research Applications
Virtual reality creates unique opportunities for advancing active sensing research through several specialized applications:
- Spatial mapping of signaling pathways within realistic cellular environments
- Dynamic simulation of ligand-receptor interactions with real-time parameter adjustment
- Virtual exploration of anatomical structures relevant to drug distribution and metabolism
- Simulated electrophysiological experiments with visualized signal propagation
- Interactive molecular docking studies with haptic feedback for binding affinity assessment
These applications leverage VR's capacity to render abstract biological concepts as tangible, interactive objects, thereby enhancing researcher intuition about complex systems. The integration of AI-driven adaptive learning with VR environments further personalizes these experiences to individual researcher needs and knowledge gaps, creating optimized learning and experimentation pathways [86].
Experimental Protocols and Methodologies
Protocol 1: VR-Enhanced Pharmacokinetic-Pharmacodynamic (PK-PD) Modeling
This protocol demonstrates how VR can accelerate the development and refinement of PK-PD models, a critical component of preclinical drug evaluation.
Objective: To reduce iteration cycles in PK-PD model development by 40% through immersive visualization and manipulation of model parameters.
Materials and Reagents:
- VR Simulation Platform: High-fidelity PK-PD modeling software compatible with VR interfaces
- Data Integration Module: System for importing experimental data from in vitro and in vivo studies
- Haptic Feedback Devices: Controllers providing resistance and tactile feedback during parameter adjustment
- Multi-User Collaboration Interface: Virtual workspace for simultaneous expert review and modification
Methodology:
- Data Upload and Preprocessing: Import existing PK-PD data from preliminary studies into the VR environment
- Model Visualization: Render current PK-PD model as an interactive 3D structure within immersive environment
- Parameter Manipulation: Adjust model parameters using intuitive hand gestures and haptic feedback
- Scenario Testing: Simulate drug behavior under varying physiological conditions and dosing regimens
- Collaborative Refinement: Multiple experts simultaneously review and adjust model components in virtual workspace
- Validation Cycling: Compare model predictions against experimental data with real-time visual highlighting of discrepancies
Outcome Measures:
- Time to model convergence
- Number of iteration cycles required for satisfactory prediction accuracy
- Inter-expert agreement on model validity
- Computational resources required compared to traditional methods
This protocol demonstrates how VR transforms abstract mathematical modeling into an intuitive, collaborative process, significantly reducing the cognitive load associated with complex parameter optimization and accelerating model development timelines.
Protocol 2: VR-Based High-Content Screening (HCS) Optimization
High-content screening generates massive multidimensional datasets that challenge traditional analysis methods. This protocol applies VR to enhance pattern recognition and assay optimization.
Objective: To improve HCS assay design efficiency and data interpretation accuracy through immersive data exploration.
Materials and Reagents:
- VR Data Visualization Suite: Software for converting HCS data into interactive 3D visualizations
- Motion Tracking System: Precise tracking of researcher movements and gestures within VR environment
- Virtual Laboratory Interface: Simulation of physical laboratory environment with available reagents and equipment
- Statistical Analysis Module: Integrated tools for real-time statistical evaluation within VR environment
Methodology:
- Data Import: Transfer HCS data from image analysis systems to VR platform
- Multidimensional Visualization: Render complex cellular phenotypes as interactive 3D objects within tissue context
- Pattern Recognition Training: Use AI-guided highlighting of subtle phenotypic patterns potentially missed in 2D review
- Assay Parameter Adjustment: Virtually modify assay conditions and immediately visualize potential impacts on data quality
- Hit Selection Refinement: Manipulate selection criteria with real-time visualization of how changes affect candidate identification
- Collaborative Review: Multiple researchers simultaneously examine data patterns and reach consensus on findings
Outcome Measures:
- False positive/false negative rates in hit identification
- Time required for comprehensive data review
- Inter-reviewer consistency in pattern recognition
- Assay optimization cycle times
This approach addresses a critical bottleneck in high-content screening by transforming massive datasets into navigable biological landscapes, enabling researchers to identify subtle patterns and relationships that might escape conventional analysis.
Visualization of VR-Enhanced Preclinical Workflows
Figure 1: Comparative Workflow: Traditional vs. VR-Enhanced Preclinical Research
Essential Research Reagent Solutions for VR-Enhanced Preclinical Research
Table 2: Key Research Reagent Solutions for VR-Enhanced Preclinical Studies
| Reagent/Technology | Function in VR-Enhanced Research | Efficiency Contribution |
|---|---|---|
| Patient-Derived Xenograft (PDX) Models | Provide clinically relevant tumor models for virtual simulation | High predictive accuracy in oncology studies; 61% market share in 2025 [88] |
| Bioanalysis and DMPK Study Platforms | Generate pharmacokinetic data for virtual absorption, distribution, metabolism, and excretion (ADME) modeling | 35.6% share of preclinical CRO services; essential for regulatory submissions [88] |
| AI-Enhanced Haptic Feedback Systems | Provide tactile sensation during virtual procedures and manipulations | 45% reduction in error rates; critical for procedural skill transfer [86] |
| Multi-User VR Collaboration Platforms | Enable simultaneous researcher interaction in shared virtual laboratory spaces | Facilitate distributed expertise application; reduce collaboration delays |
| Small Animal Model Datasets | Provide foundational data for virtual model construction and validation | 58% of animal model market; cost-effective research basis [88] |
| High-Fidelity 3D Anatomical Models | Create realistic virtual environments for surgical and procedural training | 42% improvement in procedural accuracy; enhanced spatial understanding [86] |
| Adaptive Learning Algorithms | Personalize VR training content based on individual performance metrics | 38% reduction in training time; optimized skill acquisition [86] |
The reagents and technologies detailed in Table 2 represent the infrastructure foundation for effective VR-enhanced preclinical research. These solutions bridge the physical and virtual research domains, ensuring that simulations maintain biological relevance while leveraging the efficiency advantages of virtual environments.
Implementation Framework and Future Directions
Strategic Implementation Pathway
Successful integration of VR technologies into preclinical research operations requires a structured approach:
Phase 1: Infrastructure Assessment (Weeks 1-4)
- Audit existing research workflows to identify key inefficiencies
- Evaluate current computational resources and VR compatibility
- Identify pilot projects with high potential for VR-enabled improvement
- Establish cross-functional implementation team with research and technical expertise
Phase 2: Technology Acquisition and Customization (Weeks 5-12)
- Select VR platforms aligned with specific research needs
- Develop or procure domain-specific content and simulations
- Integrate with existing data systems and research platforms
- Establish baseline metrics for pre-implementation performance
Phase 3: Staff Training and Change Management (Weeks 13-16)
- Implement phased training programs with competency benchmarks
- Establish super-user program for early technology adopters
- Develop standardized operating procedures for VR-enhanced workflows
- Create feedback mechanisms for continuous improvement
Phase 4: Full Integration and Optimization (Weeks 17-24+)
- Expand VR implementation across additional research domains
- Refine processes based on performance metrics and user feedback
- Develop advanced applications leveraging accumulated experience
- Establish centers of excellence for ongoing innovation
This implementation pathway emphasizes measurable outcomes at each phase, ensuring that VR integration delivers tangible efficiency improvements rather than functioning as merely decorative technology.
Emerging Trends and Future Applications
The convergence of VR with other transformative technologies promises continued efficiency gains in preclinical research:
- AI-integrated VR environments that adapt in real-time to researcher actions and queries, creating personalized research assistants within immersive spaces [19]
- Multi-sensory VR systems incorporating olfactory and gustatory feedback for more comprehensive simulation of biological environments [89]
- Blockchain-secured collaborative networks enabling secure sharing of proprietary research models and data within virtual workspaces
- Extended reality (XR) continuum seamlessly blending physical and virtual research environments through mixed reality interfaces
- Quantum computing-enhanced simulations enabling real-time modeling of extraordinarily complex biological systems within VR environments
These advancing capabilities will further compress preclinical timelines while enhancing research quality, ultimately accelerating the delivery of innovative therapies to patients.
Virtual reality technologies represent a paradigm-shifting approach to addressing persistent efficiency challenges in preclinical research phases. Through immersive visualization, intuitive interaction with complex data, and enhanced collaborative capabilities, VR-enabled workflows demonstrably improve both the speed and quality of preclinical research. Documented outcomes include protocol optimization time reduced by 38%, procedural accuracy improved by 42%, and error rates decreased by 45% [86], representing meaningful advances in a field where incremental improvements traditionally dominate.
The integration of VR into preclinical research operations requires strategic investment and organizational commitment, but the demonstrated returns in accelerated timelines, enhanced data comprehension, and reduced physical resource requirements justify this investment. As these technologies continue evolving alongside complementary advances in artificial intelligence, sensor technologies, and computational power, VR promises to become an increasingly central component of efficient, effective preclinical research ecosystems. Research organizations that strategically embrace these technologies position themselves to achieve significant competitive advantages in the increasingly challenging landscape of therapeutic development.
The U.S. Food and Drug Administration (FDA) recognizes augmented reality (AR) and virtual reality (VR), collectively part of medical extended reality (XR), as transformative technologies with the potential to fundamentally change healthcare delivery [90]. The FDA defines AR as "a real-world augmented experience with overlaying or mixing simulated digital imagery with the real world," often through a smartphone or head-mounted display. In contrast, VR is defined as "a virtual world immersive experience" that typically uses a headset to completely replace the user's surroundings with a simulated environment [91]. For developers and researchers, particularly in the field of active sensing where precise spatial interaction and data visualization are paramount, understanding the FDA's regulatory framework is essential for translating innovative concepts into clinically validated tools.
The FDA's Digital Health Center of Excellence (DHCE) is leading the effort to create a tailored regulatory approach for digital health technologies, aiming to provide efficient oversight while maintaining standards for safety and effectiveness [92]. For VR tools, this involves a risk-based classification system and specific pathways for premarket review. The growing body of FDA-cleared devices provides a roadmap for the types of technological applications and validation methodologies the agency deems acceptable for clinical use.
FDA-Cleared VR Medical Devices: Current Market Landscape
The FDA maintains a published list of AR/VR medical devices that have received marketing authorization, providing valuable insight into the current regulatory landscape [91]. This list serves as a critical transparency tool for developers, healthcare providers, and researchers, illustrating the scope of approved applications and the types of technical claims that have successfully navigated the regulatory process.
Quantitative Analysis of Authorized VR Devices
As of recent updates, the FDA has authorized over 90 medical devices incorporating AR/VR technologies [93] [94]. The earliest submissions were cleared in 2015, indicating a relatively recent but rapidly expanding regulatory acceptance. The distribution of these devices across medical specialties and regulatory pathways reveals important patterns for developers.
Table 1: FDA Authorization Statistics for AR/VR Medical Devices
| Analysis Category | Statistical Breakdown | Key Insights |
|---|---|---|
| Total Authorized Devices | 92 devices [94] | Demonstrates substantial and growing clinical adoption |
| Review Panel Distribution | Radiology (37%), Orthopedics (27%), Neurology (18%) [94] | Certain specialties show more advanced regulatory acceptance |
| Regulatory Pathways | Predominantly 510(k) clearance; some De Novo classifications [94] | Most devices demonstrate substantial equivalence to existing technologies |
Representative Examples of Cleared VR Devices
The diversity of FDA-cleared VR devices illustrates the technology's application across multiple clinical domains, from surgical navigation to pain management and diagnostic visualization.
Table 2: Representative Examples of FDA-Cleared VR Medical Devices
| Device Name | Manufacturer | FDA Review Panel | Primary Clinical Application |
|---|---|---|---|
| xvision Spine System | Augmedics Ltd. | Neurology | Surgical navigation using AR overlay for spinal procedures [91] |
| RelieVRx | AppliedVR | Neurology | VR-based therapeutic for chronic pain management [91] |
| Ceevra Reveal 3+ | Ceevra, Inc. | Radiology | 3D visualization of radiological data for surgical planning [91] [95] |
| VSI HoloMedicine | apoQlar medical GmbH | Radiology | Immersive 3D visualization of medical images for preoperative planning [95] |
| Smileyscope System | Smileyscope Holding Inc. | Physical Medicine | VR therapy for procedural pain and anxiety reduction [91] |
FDA Regulatory Pathways for VR Medical Devices
Premarket Submission Pathways
VR medical devices are regulated according to the same risk-based framework as other medical devices, with three primary pathways to market:
- 510(k) Premarket Notification: Most VR devices pursue this pathway, requiring demonstration of substantial equivalence to a legally marketed predicate device [94]. This pathway is typically appropriate for Class II devices with established predicates, such as many surgical navigation systems based on existing navigational technologies.
- De Novo Classification: For novel VR devices with no predicate, but with low-to-moderate risk profiles, the De Novo pathway provides a route to market classification [94]. This creates a new regulatory classification that can serve as a predicate for future devices.
- Premarket Approval (PMA): The most rigorous pathway, required for Class III devices, which typically include VR technologies addressing critical or life-sustaining functions [94]. This requires demonstration of reasonable assurance of safety and effectiveness based on valid scientific evidence.
The FDA's Q-Submission Program allows developers to request feedback on proposed device development and testing strategies before formal submission, a valuable mechanism for navigating novel regulatory questions posed by innovative VR technologies [96].
Benefits and Risks Framework
The FDA evaluates VR devices through a benefit-risk assessment that considers both the novel capabilities and unique challenges of immersive technologies [91].
Probable Benefits recognized by the FDA include:
- Increased healthcare access through remote delivery of care
- Improved procedural preparation through enhanced visualization
- Reduced invasiveness of interventions through precise navigation
- Accelerated diagnostic processes via immersive data interpretation
Identified Risks requiring mitigation include:
- Cybersickness (vestibular-ocular conflict causing nausea)
- Physical discomfort (neck strain from head-mounted displays)
- Human factors concerns (distraction in clinical environments)
- Cybersecurity and privacy vulnerabilities
- Potential for diagnostic error from display inaccuracies
For active sensing research applications, particular attention must be paid to validating the spatial accuracy of VR representations and establishing the clinical validity of any diagnostic or monitoring functions derived from sensor data.
Experimental Protocols for VR Device Validation
Protocol for Spatial Accuracy Validation
Spatial accuracy is fundamental for VR tools used in surgical navigation, diagnostic imaging, and active sensing research. The following protocol outlines key validation methodology:
Objective: To quantify the spatial accuracy of VR-rendered anatomical structures against ground truth physical space or reference standard imaging.
Materials and Equipment:
- VR medical device under evaluation (e.g., xvision Spine System [91])
- Anatomical phantoms with known dimensions and radiological properties
- Tracking system capable of sub-millimeter accuracy (e.g., optical or electromagnetic tracking)
- Reference standard (CT/MRI datasets with verified spatial fidelity)
- Statistical analysis software
Procedure:
- Phantom Registration: Align the VR coordinate system with the physical phantom using fiducial markers or surface registration.
- Target Selection: Identify multiple target points within the phantom (≥20 points recommended) distributed throughout the working volume.
- Coordinate Measurement: Record the 3D coordinates of each target point in both the VR environment and the physical reference system.
- Data Analysis: Calculate the target registration error (TRE) for each point as the Euclidean distance between VR-measured and ground truth positions.
- Statistical Analysis: Compute mean TRE, standard deviation, and root mean square error across all targets. Establish accuracy thresholds based on clinical requirements (e.g., <2mm for spinal procedures [91]).
Validation Metrics:
- Accuracy: Mean and distribution of registration errors across the operational volume
- Precision: Consistency of repeated measurements on the same targets
- Robustness: Performance under simulated clinical conditions (e.g., ambient lighting, operator movement)
This validation approach directly supports FDA submissions by providing quantifiable evidence of technical performance, a key component of the safety and effectiveness determination [91].
Protocol for Clinical Efficacy in Therapeutic Applications
For VR devices with therapeutic claims (e.g., pain management, rehabilitation), clinical studies must demonstrate measurable patient benefits.
Objective: To evaluate the clinical efficacy of a VR therapeutic intervention compared to standard care or sham control.
Study Design: Randomized controlled trial with appropriate blinding and control conditions.
Materials and Equipment:
- VR therapeutic system (e.g., RelieVRx for chronic pain [91])
- Validated outcome measures specific to the clinical condition
- Physiological monitoring equipment (as appropriate)
- Data collection and management system
Procedure:
- Participant Recruitment: Enroll subjects meeting specific inclusion/exclusion criteria, with sample size determined by power analysis.
- Randomization: Assign participants to intervention or control groups using concealed allocation.
- Intervention Protocol: Administer the VR therapy according to a standardized protocol, documenting session duration, frequency, and content.
- Outcome Assessment: Collect primary and secondary endpoints at baseline, during intervention, and at follow-up intervals using validated instruments.
- Statistical Analysis: Compare outcomes between groups using appropriate statistical methods, accounting for potential confounders.
Endpoint Selection:
- Primary Endpoints: Direct measures of the targeted clinical benefit (e.g., pain intensity scales, functional measures)
- Secondary Endpoints: Patient-reported outcomes, medication usage, quality of life measures
- Safety Endpoints: Incidence of adverse events (cybersickness, discomfort, etc.)
The FDA's authorization of RelieVRx through the de novo pathway establishes a precedent for the type and rigor of clinical evidence required for VR-based therapeutics [91] [94].
Visualization of Regulatory Pathways
The journey from concept to FDA authorization involves multiple stages and decision points. The following diagram illustrates the key regulatory pathway for VR medical devices:
The Researcher's Toolkit: Essential Components for VR Medical Device Development
Successful development and regulatory approval of VR medical tools requires specific components and methodologies. The following table outlines essential elements for creating clinically valid VR systems for active sensing and other medical applications.
Table 3: Research Reagent Solutions for VR Medical Device Development
| Component Category | Specific Examples | Function in Development | Regulatory Considerations |
|---|---|---|---|
| Tracking Systems | Optical tracking, Electromagnetic sensors, Inertial measurement units (IMUs) | Spatial localization of user and instruments for AR overlay and interaction | Accuracy validation against ground truth; robustness in clinical environments [91] |
| Display Technologies | Head-mounted displays (HMDs), See-through displays, Holographic projectors | Visual presentation of virtual content and sensor data | Resolution, contrast, latency, and ergonomic factors affecting clinical usability [91] |
| Validation Phantoms | 3D-printed anatomical models, Fiducial marker arrays, Custom calibration targets | Quantitative assessment of spatial accuracy and system performance | Traceability to reference standards; representation of clinical anatomy [95] |
| Software Platforms | 3D rendering engines, DICOM processing libraries, Surgical planning software | Core functionality for medical image processing and visualization | Software validation, cybersecurity protections, and interoperability testing [97] [96] |
| Data Integration | PACS interfaces, EHR connectivity, Sensor data pipelines | Integration with clinical workflow and existing healthcare infrastructure | Data integrity, privacy safeguards, and reliability under clinical conditions [98] |
The FDA's approach to VR medical devices continues to evolve as the technology advances and clinical evidence accumulates. Recent initiatives like the Regulatory Accelerator for digital health devices demonstrate the agency's commitment to streamlining development processes while maintaining appropriate oversight [99]. For researchers in active sensing and related fields, understanding this regulatory landscape is not merely a compliance exercise but an opportunity to design more effective validation strategies from the earliest stages of development.
The growing list of FDA-cleared devices establishes important precedents for the technical requirements and clinical evidence needed for market authorization. As VR technologies increasingly incorporate artificial intelligence, haptic feedback, and more sophisticated sensing capabilities, the regulatory framework will continue to adapt. Researchers and developers who engage early with regulatory requirements through the FDA's Q-Submission program and other feedback mechanisms will be best positioned to translate innovative VR concepts into clinically impactful tools that meet the FDA's standards for safety and effectiveness.
Comparative Analysis of VR Platforms for Specific Biomedical Applications
Virtual reality (VR) technology has emerged as a transformative force in biomedical fields, creating new paradigms for medical training, surgical simulation, rehabilitation, and therapeutic interventions. The global healthcare VR market is projected to grow from approximately $4 billion in 2024 to over $46 billion by 2032, reflecting its rapidly expanding adoption [98] [100]. This growth is driven by VR's unique ability to create immersive, controlled environments that enhance learning, improve patient outcomes, and reduce healthcare costs. For researchers investigating active sensing—the process by which organisms selectively gather information from their environment to guide behavior—VR provides unprecedented experimental control over sensory inputs and motor outputs within ecologically valid scenarios [101]. This technical review analyzes current VR platforms through the lens of their biomedical applications, with particular emphasis on their utility for active sensing research and drug development.
Current VR Landscape in Healthcare
Classification of VR Technologies
Extended Reality (XR) encompasses a spectrum of technologies that differ in their immersion levels and integration of virtual and real-world elements Table 1.
Table 1: XR Technology Classification in Healthcare
| Technology | Definition | Key Characteristics | Primary Healthcare Applications |
|---|---|---|---|
| Virtual Reality (VR) | Fully immersive digital environment replacing real-world perception | Complete visual isolation; head-mounted displays; positional tracking | Surgical simulation, medical education, exposure therapy, pain management |
| Augmented Reality (AR) | Digital content overlaid onto real-world environment | See-through displays; context-aware information; real-world anchor | Surgical navigation, medical imaging overlay, anatomy learning |
| Mixed Reality (MR) | Seamless blending of virtual and real-world elements | Interactive digital objects anchored to real environment; spatial understanding | Surgical planning, complex procedure guidance, collaborative diagnosis |
Virtual Reality creates fully synthetic environments that completely replace the user's visual field, providing high levels of experimental control ideal for studying perception-action cycles in active sensing [102]. Augmented Reality enhances real-world perception by overlaying digital information, while Mixed Reality enables interactive digital objects to coexist with the physical environment [102]. The healthcare sector has demonstrated particularly strong adoption, with 84% of healthcare professionals believing AR/VR will positively change the industry [98].
Dominant VR Hardware Platforms
Table 2: VR Hardware Platforms for Biomedical Applications
| Device | Type | Key Features | Biomedical Applications | Limitations |
|---|---|---|---|---|
| Meta Quest 3 | Standalone | Color pass-through cameras, Snapdragon XR2 Gen 2 processor | Surgical training, patient education, rehabilitation therapy | Short battery life, lacks eye-tracking [103] |
| Apple Vision Pro | Standalone | High-resolution displays, eye/hand tracking, no controllers needed | Medical visualization, precise surgical planning, data analysis | High cost, front-heavy design, limited battery [103] |
| HTC Vive Pro 2 | PC-tethered | High resolution (2448×2448 per eye), requires base stations | Research applications requiring high fidelity, visual perception studies | Expensive, requires external tracking hardware [103] |
| Sony PlayStation VR2 | Console-tethered | Eye tracking, haptic feedback, 110° field of view | Therapeutic gaming, motor rehabilitation, patient engagement | Limited to PS5 ecosystem, not enterprise-focused [103] |
Hardware selection critically influences research capabilities in active sensing studies. Standalone headsets like the Meta Quest 3 offer mobility and accessibility, while PC-tethered systems like the HTC Vive Pro 2 provide superior graphical fidelity essential for visual psychophysics research [103]. Emerging technologies such as haptic feedback systems and eye-tracking are becoming increasingly important for creating multi-sensory environments that more accurately simulate naturalistic active sensing behaviors [19].
Analysis of VR Software Platforms for Biomedical Applications
Medical Training and Simulation Platforms
Table 3: VR Platforms for Medical Training and Simulation
| Platform | Primary Application | Key Features | Evidence Base | Technical Requirements |
|---|---|---|---|---|
| SimX | Medical simulation training | Largest library of medical scenarios; multiplayer collaboration; pediatric cardiac critical care | 22% less time and 40% lower cost vs traditional simulation; higher performance scores [104] | VR headsets; network connectivity for collaborative features |
| zSpace with BodyViz | Anatomy education | 3D anatomy visualization from real medical imaging; no headset required; virtual dissection | Increased knowledge retention; addresses cadaver lab shortages [100] | zSpace AR/VR laptop; stylus interaction |
| Oxford Medical Simulation | Clinical decision making | Interactive patient scenarios; immediate feedback and assessment | Improved diagnostic accuracy and patient communication skills [104] [105] | VR headsets; institutional licensing |
VR medical training platforms demonstrate significant advantages over traditional methods. Studies show that VR simulation education takes 22% less time and costs 40% less than traditional high-fidelity simulation while producing better performance outcomes [104]. At Purdue Global, VR training helped increase national nursing exam pass rates by 10-15% while supporting over 4,000 graduate nurses [105]. These platforms provide controlled environments where healthcare professionals can practice complex procedures and encounter rare clinical scenarios without patient risk, making them particularly valuable for studying how medical experts actively gather and integrate diagnostic information [105].
Therapeutic and Clinical Application Platforms
Table 4: VR Platforms for Therapeutic Applications
| Platform | Clinical Focus | Methodology | Evidence Outcomes | Integration Capabilities |
|---|---|---|---|---|
| Novobeing | Stress, anxiety, and pain management | Controller-free design; clinically tested methods; user-friendly interface | Validated reduction in stress, anxiety, and pain metrics [104] | Minimal training required; fits existing clinical workflows |
| XRHealth | Chronic pain, anxiety, cognitive rehabilitation | Telehealth VR therapy; distraction techniques; mindfulness exercises | Reduced patient-reported pain; improved cognitive function [104] | EHR integration; remote monitoring capabilities |
| Oxford Medical Simulation (Therapy) | Mental health treatment | Combines VR with cognitive behavioral therapy (CBT) | Clinically validated for mental health applications [104] | Home-based treatment model |
Therapeutic VR platforms leverage immersive environments to create controlled therapeutic contexts. For active sensing research, these platforms offer methodologies to investigate how altered sensory environments affect perceptual processes and behavioral adaptations. XRHealth's distraction techniques for pain management, for instance, provide insight into how redirected attention modulates pain perception—a form of sensory gating relevant to active sensing mechanisms [104]. These platforms demonstrate the clinical translation of basic research on how organisms selectively allocate sensory resources.
Experimental Protocols and Methodologies
Protocol: Assessing Surgical Skill Acquisition Using VR Simulation
Objective: To quantify the efficacy of VR simulation training for developing surgical motor skills and decision-making capabilities.
Materials:
- VR surgical simulator (e.g., Osso VR, PrecisionOS)
- HMD with motion tracking (e.g., Meta Quest 3)
- Performance metrics software
- Control group (traditional training) and experimental group (VR training)
Procedure:
- Baseline Assessment: All participants complete initial skill assessment using standardized tasks
- Training Phase:
- Experimental group: 3×60-minute VR training sessions weekly for 4 weeks
- Control group: Traditional surgical training equivalent time
- Skill Transfer Evaluation: Participants perform actual surgical procedures on cadavers or simulated tissue
- Metrics Collection:
- Procedure completion time
- Error rates and critical incidents
- Economy of motion (path length)
- Expert-rated performance scores
Data Analysis: Compare pre-post improvement between groups using ANOVA; correlate VR metrics with real-world performance [105].
This protocol exemplifies how VR creates controlled environments to study the development of active sensing skills in complex motor tasks, revealing how practitioners learn to efficiently gather visual and haptic information to guide surgical actions.
Protocol: VR-Based Exposure Therapy for Anxiety Disorders
Objective: To evaluate the efficacy of graduated exposure in VR environments for treating specific phobias.
Materials:
- Therapeutic VR platform (e.g., Oxford Medical Simulation)
- HMD with biofeedback sensors
- Subjective Units of Distress Scale (SUDS)
- Physiological monitoring (heart rate, GSR)
Procedure:
- Baseline Assessment: Establish individual anxiety hierarchy and baseline physiological measures
- Graduated Exposure:
- Session 1: Introduce minimal anxiety-provoking stimuli in VR
- Subsequent sessions: Gradually increase stimulus intensity based on patient tolerance
- Each session: 45-60 minutes, 2× weekly for 8 weeks
- In-Session Monitoring: Continuous SUDS ratings and physiological recording
- Generalization Assessment: Measure real-world approach behaviors post-treatment
Data Analysis: Compare pre-post treatment metrics using paired t-tests; analyze correlation between physiological and subjective measures [104].
This protocol demonstrates how VR enables precise control over sensory stimuli to study how organisms gradually adapt their defensive behaviors through controlled exposure to threat-relevant cues—a process fundamentally dependent on modifications to active sensing strategies.
Visualization of VR Experimental Workflows
Diagram 1: VR Experimental Design Workflow. This workflow outlines the systematic process for designing and implementing VR-based biomedical research studies, highlighting critical decision points from platform selection through data interpretation.
Diagram 2: VR System Architecture for Biomedical Research. This architecture illustrates the integration of hardware and software components in a typical VR biomedical research system, highlighting key data collection points relevant to active sensing studies.
Research Reagent Solutions: Essential Materials for VR Biomedical Research
Table 5: Essential Research Materials for VR Biomedical Studies
| Category | Specific Items | Function/Application | Example Products/Platforms |
|---|---|---|---|
| Hardware Platforms | Standalone HMDs, PC-tethered HMDs, AR glasses | Provide visual immersion and tracking capabilities | Meta Quest 3, Apple Vision Pro, HTC Vive Pro 2 [103] |
| Tracking Systems | Inside-out tracking, eye-tracking, hand-tracking, body tracking | Capture movement and attention data for behavior analysis | Meta Quest built-in tracking, Apple Vision Pro eye tracking [103] |
| Software Development | Game engines, VR development frameworks, 3D modeling tools | Create custom experimental environments and stimuli | Unity 3D, Unreal Engine, WebXR [106] |
| Biometric Sensors | EEG headsets, GSR sensors, heart rate monitors, EMG | Collect physiological data correlated with VR experiences | Muse EEG, Empatica E4, Polar H10 [101] |
| Analysis Tools | Behavior analysis software, statistical packages, visualization tools | Process and interpret multimodal VR research data | Noldus Observer, MATLAB, R, Python [101] |
Emerging Trends and Future Directions
AI and LLM Integration with VR
The convergence of large language models (LLMs) with VR technologies represents a significant frontier in biomedical applications. LLM-empowered VR can transform medical education through interactive learning platforms and address complex healthcare challenges using comprehensive solutions [107]. This integration enhances the quality of training, decision-making, and patient engagement, establishing intelligent virtual environments that can dynamically adapt to user actions and provide personalized feedback—a crucial capability for studying how active sensing strategies evolve with experience [107].
Multi-Sensory and Haptic Technologies
Future VR platforms are increasingly incorporating multi-sensory feedback, including advanced haptic systems that enable users to feel touch, pressure, and texture within virtual environments [19]. These technologies are particularly valuable for creating more ecologically valid experimental paradigms for active sensing research, where haptic feedback often guides subsequent information-gathering behaviors. Haptic gloves, suits, and specialized controllers are becoming more affordable and sophisticated, adding critical layers of realism to virtual simulations [19].
Telemedicine and Remote Collaboration
VR technologies are increasingly supporting remote healthcare delivery and collaboration. Platforms like XRHealth bring VR therapy directly to patients' homes, increasing accessibility while maintaining treatment efficacy [104]. For research, this enables larger-scale studies with more diverse participant populations, addressing recruitment limitations that often constrain biomedical research. Remote collaboration features also allow experts to guide procedures and training across geographical boundaries, creating new paradigms for distributed healthcare and research [105].
VR platforms have matured beyond speculative technology into essential tools with demonstrated efficacy across diverse biomedical applications. For active sensing research, these platforms provide unprecedented experimental control while maintaining ecological validity, enabling precise investigation of how organisms gather and utilize sensory information to guide behavior. The comparative analysis presented here reveals specialized platforms optimized for distinct biomedical applications, from surgical skill acquisition to therapeutic interventions. As VR hardware becomes more accessible and software platforms more sophisticated, these technologies will increasingly support both basic research into perceptual-motor processes and their clinical applications. Future developments in AI integration, multi-sensory interfaces, and remote collaboration will further enhance VR's utility as an experimental and therapeutic platform, solidifying its role in advancing biomedical research and healthcare delivery.
Establishing Standardized Protocols for Validation in Virtual Environments
Virtual reality (VR) has emerged as a transformative tool for active sensing research, enabling controlled, immersive, and reproducible studies of perception and behavior. In the context of active sensing—where organisms voluntarily control sensory inputs through movement—VR provides unparalleled experimental control over stimulus presentation and interactive scenarios. However, the validity of findings from these virtual environments hinges on the establishment and adherence to rigorous, standardized validation protocols. Without such standards, results may lack reliability, generalizability, and scientific rigor, ultimately undermining the potential of VR to advance our understanding of sensory-motor loops.
The adoption of international performance standards is no longer optional but essential for credible research outcomes. These standards provide measurable benchmarks for critical parameters including visual performance, user safety, and experimental reproducibility. For drug development professionals and neuroscientists studying active sensing mechanisms, standardized validation ensures that VR-based behavioral measurements accurately reflect biological processes rather than technological artifacts. This technical guide establishes a comprehensive framework for validating virtual environments, with specific application to active sensing research where sensory feedback is contingent upon self-generated movement.
Core Validation Metrics and International Standards
Validation of virtual environments for research requires compliance with internationally recognized standards that address visual performance, user safety, and data quality. The table below summarizes the critical parameters, their research implications, and relevant international standards.
Table 1: Essential Validation Metrics for Virtual Research Environments
| Validation Category | Specific Metric | Research Impact | Applicable Standards |
|---|---|---|---|
| Visual Performance | Spatial Resolution | Determines acuity for visual tasks; critical for stimulus discrimination in perception studies | IEC 63145-20-10 [108] |
| Contrast Ratio | Affects detection thresholds; fundamental for visual psychophysics | IEC 63145-20-10 [108] | |
| Field of View | Impacts spatial awareness and immersion; crucial for ecological validity | IEC 63145-22-20 [108] | |
| Color Gamut | Important for color discrimination tasks and emotional response studies | IEC 63145-20-10 [108] | |
| User Safety & Comfort | Real Scene Visibility | Affects collision risk during movement-based tasks | ANSI 8400 [108] |
| Visually Induced Motion Sickness (VIMS) | Can confound behavioral data and increase dropout rates | ISO 9241-394 [108] | |
| Vergence-Accommodation Conflict | Causes visual fatigue during prolonged experiments | ISO 9241-392 [108] | |
| Flicker Frequency | Risk of photosensitive seizures; safety critical | ISO 9241-391 [108] | |
| Data Quality | Motion-to-Photon Latency | Critical for motor control studies and temporal precision | ANSI 8400 [108] |
| Tracking Accuracy | Determines spatial precision of movement data | Instrument-specific calibration | |
| Inter-pupillary Distance Alignment | Affects depth perception and binocular vision tasks | ANSI 8400 [108] |
These metrics establish the technical foundation upon which valid experimental protocols can be built. For active sensing research specifically, parameters such as motion-to-photon latency and tracking accuracy are particularly crucial as they directly impact the fidelity of sensory-motor contingency—the core mechanism underlying active sensing behaviors.
Experimental Protocol Framework for VR Validation
The DEAR Principle for Comprehensive Experimentation
A systematic approach to VR experimentation requires implementation of the Design, Experiment, Analyse, and Reproduce (DEAR) principle [24]. This framework ensures methodological rigor throughout the experimental lifecycle:
Design Phase: Develop experimental protocols using validated VR frameworks that provide predefined features for common research tasks. Specify hardware models, tracking modes, minimum lighting conditions, and firmware versions in the experimental protocol to ensure consistency [44].
Experiment Phase: Implement standardized calibration procedures before each testing session. This includes pose calibration, IPD adjustment, and environment mapping to establish consistent baseline conditions across participants and sessions [44].
Analyse Phase: Employ automated data processing pipelines that record both performance metrics (reaction times, accuracy) and process metrics (head movement, gaze tracking) to enable comprehensive analysis of active sensing behaviors [24].
Reproduce Phase: Document all technical parameters, software versions, and experimental conditions using standardized checklists. Version-freeze applications and content packs per site activation to maintain consistency across longitudinal studies [44].
Protocol for Validating VR-Based Perimetry Against Gold Standards
The validation of VR-based assessment tools against established clinical standards illustrates a robust validation approach. The following protocol, adapted from visual field testing validation, provides a template for establishing clinical-grade measurements in virtual environments:
Table 2: Validation Protocol for VR-Based Sensory Assessment Tools
| Protocol Phase | Key Procedures | Validation Metrics | Acceptance Criteria |
|---|---|---|---|
| Device Calibration | Luminance calibration using photometer; Spatial mapping of display coordinates; Contrast validation across intensity levels | Gamma correction values; Geometric distortion measurements; Contrast linearity | <10% deviation from reference standards; Consistent performance across display areas [109] |
| Participant Preparation | Standardized instructions & training; IPD measurement & adjustment; Refractive error correction | Task comprehension; Lens alignment confirmation; Visual acuity measurement | >95% comprehension on practice trials; Optimal lens alignment for visual clarity [109] [108] |
| Testing Procedure | Randomized stimulus presentation; Attention monitoring with catch trials; Environmental condition control; Breaks to prevent fatigue | False positive/negative rates; Test-retest reliability; Completion rate; Session duration | <15% false positive rate; ICC > 0.8 for test-retest; >90% completion rate [109] |
| Data Analysis | Agreement analysis with Bland-Altman plots; Correlation coefficients with reference standard; Spatial analysis of deviation patterns | Mean difference (bias); 95% limits of agreement; Correlation coefficients (r); Pattern standard deviation | Bias not significantly different from zero; Narrow limits of agreement; r > 0.7 for key metrics [109] |
This comprehensive validation approach has demonstrated promising results, with devices such as Heru, Olleyes VisuALL, and the Advanced Vision Analyzer showing clinically acceptable agreement with gold standard measures like the Humphrey Field Analyzer, particularly in moderate to advanced deficit detection [109].
Visualization of Validation Workflows
VR Validation Protocol Workflow
Active Sensing Research Application
Successful implementation of VR validation protocols requires specific technical resources and methodological assets. The following table catalogues essential components for establishing a validated virtual research environment.
Table 3: Essential Research Reagents and Resources for VR Validation
| Resource Category | Specific Tool/Resource | Primary Function | Validation Application |
|---|---|---|---|
| Hardware Standards | Photometer/Spectroradiometer | Display luminance & color accuracy | Calibration verification per IEC 63145-20-10 [108] |
| Motion Tracking Validation System | Positional tracking accuracy | Latency measurement per ANSI 8400 [108] | |
| Eye Tracking Validation Kit | Gaze position accuracy | Attention monitoring in perceptual tasks [109] | |
| Software Frameworks | EVE Framework | Experimental design & data management | Implementation of DEAR principle [24] |
| RosettaVS | Virtual screening & molecular docking | Drug discovery applications [47] | |
| OpenVS Platform | AI-accelerated compound screening | Large-scale virtual screening [47] | |
| Methodological Resources | ISO 9241-392 | Stereoscopic image comfort guidelines | Mitigating visual fatigue [108] |
| CASF2016 Dataset | Virtual screening benchmark | Method validation [47] | |
| PRISMA Guidelines | Systematic review methodology | Evidence synthesis [109] |
These resources provide the technical foundation for implementing the validation protocols outlined in this guide. Selection of appropriate tools should be guided by specific research questions and the active sensing paradigms under investigation.
Establishing standardized validation protocols for virtual environments represents a fundamental requirement for advancing active sensing research. The frameworks, metrics, and methodologies presented in this technical guide provide researchers with concrete tools for implementing rigorous validation procedures that ensure scientific credibility and reproducibility. As VR technology continues to evolve, maintaining adherence to international standards while adapting to new technological capabilities will remain essential for producing valid, impactful research in the understanding of active sensing mechanisms and their applications in drug development and clinical practice.
Conclusion
Virtual Reality has unequivocally evolved from a visualization tool into a powerful active sensing platform that is reshaping biomedical research and drug discovery. By enabling researchers to actively interrogate and manipulate complex biological systems, VR enhances intuition, accelerates hypothesis testing, and personalizes therapeutic development. The integration of AI and the establishment of robust validation frameworks will be pivotal in overcoming current fidelity and accessibility challenges. Future directions point towards fully immersive, collaborative virtual laboratories, the widespread adoption of VR in regulatory decision-making, and its central role in realizing the full potential of personalized medicine. For researchers and drug development professionals, mastering these tools is no longer optional but essential for driving the next wave of scientific innovation.
References
- 1. Theoretical perspectives on active sensing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6116896/]
- 2. Virtual reality in drug design: Benefits, applications and ... [https://www.sciencedirect.com/science/article/pii/S0959440X25000624]
- 3. Virtual reality in drug design: Benefits, applications and ... [https://pubmed.ncbi.nlm.nih.gov/40199042/]
- 4. Assessing Human Factors in Virtual Reality Environments ... [https://www.mdpi.com/2078-2489/16/1/35]
- 5. How New Technologies Can Boost Research on Crowd ... [https://www.frontiersin.org/journals/robotics-and-ai/articles/10.3389/frobt.2018.00082/full]
- 6. Discovering and exploiting active sensing motifs for ... [https://arxiv.org/html/2511.08766v1]
- 7. Frontiers | A spatial and temporal transformer-based EEG emotion... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1517273/full]
- 8. Haptic Sensing and Feedback Techniques toward Virtual Reality [https://pmc.ncbi.nlm.nih.gov/articles/PMC10964227/]
- 9. Transforming graph data visualisations from 2D displays ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2023.1155628/full]
- 10. Virtual Reality and Sensing Techniques for Human [https://www.mdpi.com/journal/sensors/special_issues/A03YMB9GX6]
- 11. Feeling the future: New wearable tech simulates realistic touch [https://news.northwestern.edu/stories/2025/03/feeling-the-future-new-wearable-device-mimics-the-complexity-of-human-touch]
- 12. Virtual Reality in Pharmacy: Opportunities for Clinical, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6487969/]
- 13. Motion Capture for Virtual Reality - vr tracking [https://optitrack.com/applications/virtual-reality]
- 14. SlimeVR Full-Body Trackers - SlimeVR Official [https://slimevr.dev/]
- 15. Driver4VR: Full Body Tracking - Apps on Google Play [https://play.google.com/store/apps/details?id=com.franklydog.driver4vr&hl=en_US]
- 16. Driver4VR - Full Body Tracking VRChat, Kinect, Smartphone [https://www.driver4vr.com/]
- 17. LifeArc use VR/MR to supercharge drug design [https://forwork.meta.com/case-studies/lifearc-vr-drug-design/]
- 18. VR could be used to design new drugs, say researchers [https://www.drugtargetreview.com/news/57192/virtual-reality-could-be-used-to-design-new-drugs-say-researchers/]
- 19. Virtual Reality Trends of 2025: Future of VR Technology [https://hqsoftwarelab.com/blog/virtual-reality-trends/]
- 20. Mixed Reality Meets Pharmaceutical Development [https://www.sciencedirect.com/science/article/abs/pii/S0022354917306160]
- 21. A survey of immersive visualization: Focus on perception ... [https://www.sciencedirect.com/science/article/pii/S2468502X23000499]
- 22. Development and application of an experimental ... [https://www.sciencedirect.com/science/article/pii/S235271022300459X]
- 23. Immersive Technologies Targeting Spatial Memory Decline [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466985/]
- 24. The design, experiment, analyse, and reproduce principle ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2023.1069423/full]
- 25. Identifying key factors influencing immersive experiences ... [https://www.nature.com/articles/s41598-025-15628-y]
- 26. Virtual Reality Inspired Drugs (VRID): the Future Arena of Drug ... [https://link.springer.com/article/10.1007/s42399-019-00117-x]
- 27. Recent Advances in Molecular Docking Techniques [https://pubmed.ncbi.nlm.nih.gov/40696555/]
- 28. In silico methods for drug-target interaction prediction [https://www.sciencedirect.com/science/article/pii/S2667237525002206]
- 29. DTIAM: a unified framework for predicting drug-target ... [https://www.nature.com/articles/s41467-025-57828-0]
- 30. Tips for Illustrating Biological Pathways [https://www.biorender.com/learn/drawing-biological-pathways]
- 31. Graphic Protocols [https://www.biorender.com/features/graphic-protocols]
- 32. Advances and Challenges in 3D Bioprinted Cancer Models: Opportunities for Personalized Medicine and Tissue Engineering [https://www.mdpi.com/2073-4360/17/7/948]
- 33. a global mixed-methods study of VR, metaverse, and 3D ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1632528/full]
- 34. Recent Advances in Hydrogel-Based 3D Disease Modeling and Drug Screening Platforms | SpringerLink [https://link.springer.com/chapter/10.1007/5584_2025_851]
- 35. Patient-Derived Multiple Myeloma 3D Models for Personalized Medicine—Are We There Yet? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9657251/]
- 36. VR-prep improves visualization of medical data in ... [https://www.nature.com/articles/s41598-025-26856-7]
- 37. Immersive virtual reality based on head-mounted display in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613627/]
- 38. Are virtual models ready to transform early-phase drug ... [https://www.drugdiscoverynews.com/are-virtual-models-ready-to-transform-early-phase-drug-development-16618]
- 39. Virtual Patients in Clinical Trials for Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12228009/]
- 40. Turbine Launches the World's First Virtual Lab Using Cell ... [https://turbine.ai/news/virtual-lab-launch-2025/]
- 41. Grow AI virtual cells: three data pillars and closed-loop ... [https://www.nature.com/articles/s41422-025-01101-y]
- 42. A neuroscientist develops safety protocols for immersive ... [https://www.scu.edu/news-and-events/feature-stories/2025-feature-stories/stories/a-neuroscientist-develops-safety-protocols-for-immersive-technology.html]
- 43. A Mixed Scoping and Narrative Review of Immersive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428699/]
- 44. Virtual Reality Clinical Trials: Step Inside the Future of ... [https://ccrps.org/clinical-research-blog/virtual-reality-clinical-trials-step-inside-the-future-of-medicine-2025]
- 45. Creating a Successful Virtual Reality–Based Medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9975916/]
- 46. Virtual Reality Interventions of Daily Versus Weekly Data ... [https://formative.jmir.org/2025/1/e73506]
- 47. An artificial intelligence accelerated virtual screening ... [https://www.nature.com/articles/s41467-024-52061-7]
- 48. The Rise of AI-Driven Virtual Laboratories in Modern Science [https://www.expertmarketresearch.com/healthcare-articles/ai-virtual-labs-transforming-scientific-research]
- 49. Cadence Unveils AI-Driven ROCS X AI-Enabled Molecular ... [https://finance.yahoo.com/news/cadence-unveils-ai-driven-rocs-130000373.html]
- 50. Immersive Molecular Dynamics in Virtual Reality [https://pmc.ncbi.nlm.nih.gov/articles/PMC8321342/]
- 51. Drug Discovery Industry Roundup with Barry Bunin [https://www.collaborativedrug.com/cdd-blog/drug-discovery-industry-roundup-with-barry-bunin-november-24-2025]
- 52. Assessing virtual reality presence through physiological ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1530770/full]
- 53. A high-fidelity virtual liver model incorporating biological ... [https://www.sciencedirect.com/science/article/pii/S2405844023101861]
- 54. A systematic review of immersive virtual reality applications ... [https://www.sciencedirect.com/science/article/pii/S0360131519303276]
- 55. Virtual Reality Color Scheme - Palettes - SchemeColor.com [https://www.schemecolor.com/virtual-reality.php]
- 56. Research on the impact of immersive virtual reality ... [https://link.springer.com/article/10.1007/s10055-025-01153-w]
- 57. Virtual Sensing and Virtual Reality: How New Technologies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7806084/]
- 58. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 59. 5.6 Data Visualization [https://web.stevenson.edu/mbranson/m4tp/version1/greenhouse-gas-math-topic-data-visualization.html]
- 60. Virtual Reality Trends in 2025: Exploring the Future of VR! - Flam [https://flamapp.ai/blog/virtual-reality-trends]
- 61. Cybersickness and discomfort from head-mounted displays ... [https://www.sciencedirect.com/science/article/pii/S1471595325001325]
- 62. Understanding Cybersickness and Presence in Seated VR [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027998/]
- 63. VR Motion Sickness: Common Causes and Prevention ... [https://arborxr.com/blog/vr-motion-sickness]
- 64. 虚拟现实中眼动交互频率对视觉疲劳影响的研究 [http://www.txxb.com.cn/CN/10.11996/JG.j.2095-302X.2024030528]
- 65. VR/AR临床实验设计中的注意事项 - GoldenGrape's Blog [https://goldengrape.github.io/posts/ophthalmology/vr-ar-exp/]
- 66. VR晕动症是什么?该如何克服? [https://cn.pimax.com/blogs/news/vr%E6%99%95%E5%8A%A8%E7%97%87%E6%98%AF%E4%BB%80%E4%B9%88-%E8%AF%A5%E5%A6%82%E4%BD%95%E5%85%8B%E6%9C%8D]
- 67. Using Visual Guides to Reduce Virtual Reality Sickness in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8323020/]
- 68. A Tactile Virtual Reality for the Study of Active ... [https://www.frontiersin.org/journals/integrative-neuroscience/articles/10.3389/fnint.2020.00005/full]
- 69. AI’s Silicon Revolution: Open-Source Hardware Demolishes Barriers, Unleashing Unprecedented Innovation | FinancialContent [https://markets.financialcontent.com/stocks/article/tokenring-2025-10-29-ais-silicon-revolution-open-source-hardware-demolishes-barriers-unleashing-unprecedented-innovation]
- 70. Perspectives of 360-Degree Cinematic Virtual Reality [https://pmc.ncbi.nlm.nih.gov/articles/PMC9107048/]
- 71. Ethics of AI in Healthcare: Addressing Privacy, Bias & Trust ... [https://www.alation.com/blog/ethics-of-ai-in-healthcare-privacy-bias-trust-2025/]
- 72. Patient consent for the secondary use of health data in ... [https://www.sciencedirect.com/science/article/pii/S1386505625000899]
- 73. Considerations for Patient Privacy of Large Language ... [https://www.jmir.org/2025/1/e76571]
- 74. Data Privacy & AI Ethics Best Practices - TrustCommunity [https://community.trustcloud.ai/docs/grc-launchpad/grc-101/governance/data-privacy-and-ai-ethical-considerations-and-best-practices/]
- 75. Non-Invasive BCI-VR Applied Protocols as Intervention ... [https://www.mdpi.com/1424-8220/25/5/1342]
- 76. Developing interactive VR-based digital therapeutics for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12174457/]
- 77. Virtual reality training improves wet - lab performance of capsulorhexis... [https://pubmed.ncbi.nlm.nih.gov/19172289/]
- 78. Virtual reality simulation and real-life training programs for cataract... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-06245-w]
- 79. SRH University accompanies pioneering project: EXIST start-up grant... [https://www.srh-university.de/en/folder/news/2025/04-25/srh-university-accompanies-pioneering-project-exist-start-up-grant-for-virtual-reality-laboratory-training/]
- 80. An evaluation of intelligent and immersive digital ... [https://www.sciencedirect.com/science/article/pii/S2215016124002012]
- 81. Data Collection Framework for Context-Aware Virtual Reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9228658/]
- 82. A Systematic Review of Virtual Reality Therapies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10557052/]
- 83. Preclinical CRO Trends and Forecast Report 2025 [https://finance.yahoo.com/news/preclinical-cro-trends-forecast-report-114900451.html]
- 84. Application of virtual reality technology in clinical medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC5622235/]
- 85. Virtual reality and preclinical medical education [https://link.springer.com/article/10.1007/s44217-025-00628-x]
- 86. Innovating medical education using a cost effective and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277400/]
- 87. Five Predictions for Clinical Research in 2025 [https://www.muralhealth.com/blog/five-predictions-for-clinical-research-in-2025]
- 88. Preclinical CRO Market Size, Trends & Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/preclinical-cro-market]
- 89. Top 5 Virtual Reality Trends of 2025 — The Future of VR [https://program-ace.com/blog/virtual-reality-trends/]
- 90. Augmented Reality and Virtual Reality Medical Devices [https://www.fda.gov/medical-devices/digital-health-center-excellence/augmented-reality-and-virtual-reality-medical-devices-questions-consider]
- 91. Augmented Reality and Virtual Reality in Medical Devices [https://www.fda.gov/medical-devices/digital-health-center-excellence/augmented-reality-and-virtual-reality-medical-devices]
- 92. Digital Health Center of Excellence [https://www.fda.gov/medical-devices/digital-health-center-excellence]
- 93. FDA Lists 90+ AR/VR Medical Devices Approved Between ... [https://medtechspectrum.com/news/57/24542/fda-lists-90-ar-vr-medical-devices-approved-between-20152025-cementing-a-decade-of-immersive-tech-in-clinical-care.html]
- 94. FDA's Latest Lists for Digital Health Technologies [https://www.thefdalawblog.com/2025/07/fdas-latest-lists-for-digital-health-technologies/]
- 95. Cleared Virtual Reality Technologies in Radiology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12228893/]
- 96. May 2025 Medical Device Regulations: USA, EU, Asia & More [https://www.vistaar.ai/blog/medical-devices-usa-europe-asia-and-row-regulatory-news-may-2025/]
- 97. Guidances with Digital Health Content [https://www.fda.gov/medical-devices/digital-health-center-excellence/guidances-digital-health-content]
- 98. AR/VR's Potential in Health Care [https://itif.org/publications/2025/06/02/arvrs-potential-in-health-care/]
- 99. FDA Launches Regulatory Accelerator for Digital Health ... [https://community.hlth.com/insights/news/fda-launches-regulatory-accelerator-for-digital-health-devices-2025-08-26]
- 100. AR/VR is Revolutionizing Medical Education & Training ... [https://www.globenewswire.com/news-release/2025/10/28/3175527/0/en/AR-VR-is-Revolutionizing-Medical-Education-Training-While-Transforming-Healthcare-Industry.html]
- 101. Current status of virtual reality researches at healthcare [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1411075/full]
- 102. Current applications and future perspectives of extended ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12185561/]
- 103. The Best VR Headsets We've Tested for 2025 [https://www.pcmag.com/picks/the-best-vr-headsets]
- 104. Best VR Platforms for Medical Practice: 2025 [https://www.novobeing.com/blog/best-vr-platforms-for-medical-practice-2025]
- 105. How VR healthcare technology is changing the field [https://forwork.meta.com/blog/virtual-reality-new-healthcare-technology/]
- 106. Virtual Reality Guide 2025: Complete VR Technology ... [https://treeview.studio/blog/virtual-reality-complete-guide]
- 107. Urgent needs, opportunities and challenges of virtual ... [https://www.sciencedirect.com/science/article/pii/S2096579625000476]
- 108. Visual performance standards for virtual and augmented ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1575870/full]
- 109. Evaluating the Clinical Validity of Commercially Available ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551044/]