Addiction: A Disease of Self-Control
How neuroscience is revolutionizing our understanding of substance use disorders
The Battle Within: Why Addiction Isn't About Willpower
Imagine craving something so intensely that it drowns out all other thoughts—food, family, even survival itself.
This isn't a matter of weak character or poor morals; it's the daily reality for those struggling with addiction, a complex brain disorder that hijacks the very mechanisms of self-control we take for granted.
For decades, society viewed addiction through a moral lens, dismissing those affected as lacking willpower. However, groundbreaking scientific research has revolutionized our understanding, revealing addiction as a chronic medical condition that alters brain function, particularly in regions responsible for decision-making, impulse control, and reward processing 9 .
Did You Know?
Addiction affects the brain's reward system, motivation, memory, and related circuitry to such an extent that it leads to biological, psychological, social, and spiritual manifestations.
The Brain's Control Center: Anatomy of Self-Regulation
Prefrontal Cortex: Your Brain's Brake System
At the forefront of self-control is the prefrontal cortex (PFC), the brain's executive center responsible for decision-making, impulse control, and evaluating long-term consequences.
In addiction, this brain region undergoes significant changes. Neuroimaging studies reveal that people with substance use disorders show physical changes in areas of the brain critical to judgment, decision-making, learning and memory, and behavior control 1 .
Reward System: Hijacked by Substances
The brain's reward system, primarily involving dopamine pathways, reinforces behaviors essential for survival like eating and social interaction.
Drugs of abuse hijack this system, producing dopamine releases that are 2 to 10 times greater than those produced by natural rewards 1 . This leads to a state where the individual needs the substance just to feel "normal," while simultaneously experiencing reduced capacity for self-control.

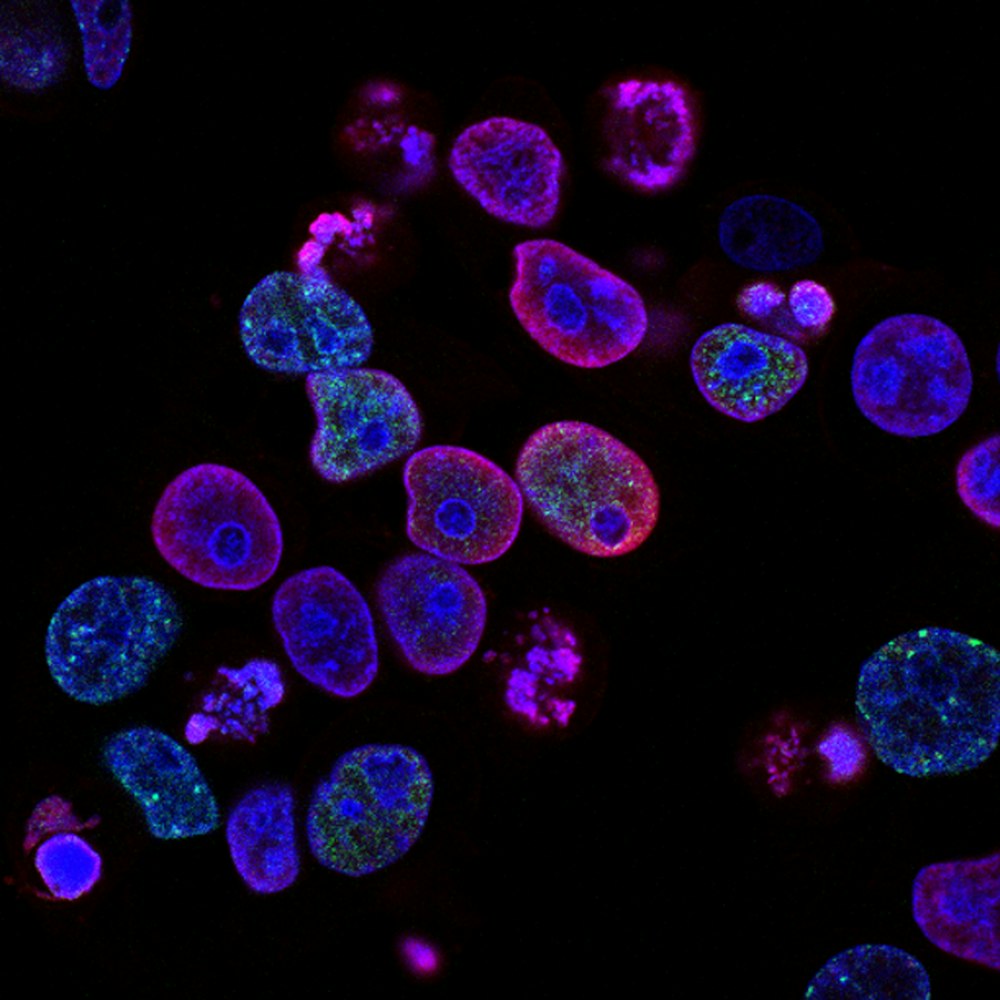
The prefrontal cortex (blue) and reward system (red) work together to regulate self-control
The Dual-System Theory: Brakes vs. Acceleration
Modern theories of self-control describe a dual-system model that helps explain why addiction creates such profound internal conflict.
The Impulsive System
This automatic, reflexive system seeks immediate reward and pleasure. It's driven by emotions, cravings, and immediate stimuli.
Balance disrupted in addiction
The Reflective System
This deliberate, thoughtful system regulates impulses and considers long-term consequences. It's essentially our capacity for self-regulation.
Risk and Protective Factors for Addiction
| Risk Factors | Protective Factors |
|---|---|
| Aggressive behavior in childhood | Self-efficacy (belief in self-control) |
| Lack of parental supervision | Parental monitoring and support |
| Drug experimentation | Positive relationships |
| Availability of drugs at school | Good grades |
| Community poverty | Neighborhood resources |
Key Experiment: Self-Regulation in Recovery
Methodology: Studying Self-Control in Sober Living Homes
A groundbreaking study examined the relationship between self-regulation and abstinence maintenance among adults in recovery residing in Oxford Houses—self-governed, communal living homes across the United States 7 .
The research involved 606 participants (407 men, 199 women) with a mean age of 38.5 years, all recovering from substance abuse disorders.
Results and Analysis: The Self-Control/Recovery Connection
The findings revealed a significant positive relationship between self-regulation scores and length of abstinence. The component related to impulsivity control showed a stronger relationship with abstinence maintenance than general self-regulation.
Study Results
Self-Regulation Components and Their Correlation with Abstinence
| Self-Regulation Component | Relationship with Abstinence Length | Statistical Significance |
|---|---|---|
| Overall Self-Regulation | Positive correlation | p < 0.05 |
| Impulsivity Control | Strong positive correlation | p < 0.01 |
| General Self-Discipline | Moderate positive correlation | p < 0.05 |
Scientific Importance
This study provided crucial evidence that self-regulation capacity—particularly impulse control—plays a vital role in maintaining recovery. The findings suggest that treatments specifically targeting impulsivity might be more effective than those focusing solely on general self-discipline.
Research Reagent Toolkit: Essential Tools
fMRI
Functional Magnetic Resonance Imaging
Measures brain activity by detecting changes in blood flow to map regions involved in craving and self-control.
DASE Scale
Drug Abstinence Self-Efficacy Scale
Assesses confidence in resisting drug use in specific situations to predict relapse risk and treatment outcomes.
SRI-25
Self-Regulation Inventory
Evaluates self-control capacity across multiple domains and compares self-regulation between different groups.
EMA
Ecological Momentary Assessment
Collects real-time data on cravings and emotions to study self-control fluctuations in natural environments.
Delay Discounting Tasks
Measures preference for immediate vs. delayed rewards to quantify impulsivity in substance users.
Genetic Testing
Identifies genetic markers associated with addiction vulnerability and treatment response.
Treatment Innovations: Restoring Self-Control
Pharmacological Approaches
GLP-1 receptor agonists (e.g., semaglutide), originally developed for diabetes and obesity, have demonstrated surprising effects on substance cravings. These medications appear to influence dopaminergic pathways in the brain, reducing the rewarding effects of substances 8 .
Neuromodulation Techniques
Transcranial Magnetic Stimulation (TMS) targets specific areas of the prefrontal cortex to rebalance neurological circuits disrupted by addiction. By stimulating these regions, TMS may enhance impulse control and reduce compulsive drug-seeking behavior 8 .
Behavioral Strategies
Mindfulness-Oriented Recovery Enhancement (MORE) blends mindfulness training, cognitive-behavioral therapy, and positive psychology to help individuals shift their focus from temporary relief provided by substances to more meaningful, sustainable sources of well-being 8 .
Technology-Assisted Interventions
Virtual recovery platforms and AI-powered tools are making support more accessible than ever. These technologies provide real-time interventions when self-control resources are depleted, offering immediate coping strategies 2 .
Social and Environmental Support
Creating supportive environments is crucial for recovery. This includes addressing social determinants of health like housing stability, employment, and social connections 2 .
Treatment Effectiveness Comparison
Recovery Capital Components
Conclusion: Beyond Willpower - A New Understanding of Addiction
The science is clear: addiction is far more complex than simply lacking willpower.
It's a chronic brain disorder that disrupts the very mechanisms of self-control we rely on to make healthy decisions. Through groundbreaking research, we've learned how addictive substances alter brain function, particularly in regions responsible for impulse control, decision-making, and reward processing.
The promising news is that the same neuroplasticity that makes the brain susceptible to addiction also enables it to heal, especially when internal and external conditions support recovery 5 . Effective treatments are evolving beyond traditional approaches to include innovative strategies that specifically target self-control mechanisms.
Perhaps most importantly, our evolving understanding of addiction as a disease of self-control helps reduce the stigma that has long surrounded substance use disorders. By recognizing addiction as a medical condition rather than a moral failing, we can create more compassionate, effective approaches to prevention, treatment, and recovery support.
Key Takeaway
Addiction is a treatable medical condition that affects brain circuits involved in reward, stress, and self-control. Recovery involves retraining these circuits and building environments that support self-regulation.
This article was based on scientific research and contributed by the National Institute on Drug Abuse (NIDA) - Advancing recovery research through science and innovation 5 .