Advanced Strategies for Mitigating Motion Artifacts in Diffusion Tensor Imaging: From Acquisition to Analysis
Motion artifacts present a significant challenge in Diffusion Tensor Imaging (DTI), potentially compromising data integrity and leading to biased quantitative measures in both research and clinical settings.
Advanced Strategies for Mitigating Motion Artifacts in Diffusion Tensor Imaging: From Acquisition to Analysis
Abstract
Motion artifacts present a significant challenge in Diffusion Tensor Imaging (DTI), potentially compromising data integrity and leading to biased quantitative measures in both research and clinical settings. This article provides a comprehensive overview of current strategies for mitigating these artifacts, addressing the entire pipeline from data acquisition to processing. We explore the foundational characteristics of head motion, evaluate the efficacy of modern preprocessing tools and novel motion-compensated acquisition sequences, and offer practical troubleshooting guidance. Furthermore, we discuss validation methodologies and comparative analyses of correction techniques, emphasizing their critical importance for ensuring reproducible and reliable DTI outcomes in neuroscience research and drug development.
Understanding the Motion Problem: Characterizing Head Motion and Its Impact on DTI Data
Head motion during diffusion tensor imaging (DTI) is a significant source of artifact that can bias quantitative measures of brain microstructure and structural connectivity. Effective motion mitigation is therefore critical for ensuring data quality and the validity of research conclusions. This technical support resource provides troubleshooting guides and frequently asked questions (FAQs) to assist researchers in quantifying, understanding, and addressing head motion within their experimental paradigms, framed within the broader context of mitigating motion artifacts in DTI research.
Frequently Asked Questions (FAQs)
1. What are the typical magnitude and direction of head motion in a large, diverse population? Based on a characterization of head motion across 13 cohorts comprising 16,995 imaging sessions, researchers can expect the following general patterns [1]:
- Magnitude: Subjects typically move at a rate of 1–2 mm/min [1].
- Primary Directions: The most common motion is observed as translation in the anterior–posterior direction and rotation around the right–left axis [1].
Table 1: Characterizing Head Motion in a Large Cohort
| Metric | Typical Value | Details |
|---|---|---|
| Mean Displacement | 1-2 mm/min | Average movement per minute of scan time [1] |
| Most Common Translation | Anterior-Posterior | Direction of most frequent linear movement [1] |
| Most Common Rotation | Around Right-Left Axis | Direction of most frequent rotational movement [1] |
| Sample Size | 16,995 sessions | From 13 different cohorts [1] |
| Age Range | 0.1 - 100 years | Spanning the entire human lifespan [1] |
2. Do state-of-the-art preprocessing pipelines effectively mitigate motion-induced biases? Yes, modern preprocessing pipelines have shown significant efficacy. Evidence from large-scale analyses indicates that these pipelines can effectively mitigate motion to the point where biases in quantitative measures of microstructure and connectivity are not detectable with current analysis techniques [1]. These pipelines typically integrate tools for global head motion correction, eddy current distortion correction, outlier detection and replacement, and susceptibility-induced distortion correction [1].
3. Are there inherent differences in the brain's structural connectivity between individuals who move more versus those who move less? Analysis of scan-rescan data from the same subjects suggests that there are no apparent differences in microstructure or macrostructural connections between participants who exhibit high motion and those who exhibit low motion [1]. This indicates that observed differences in data quality are likely due to motion artifacts rather than underlying neuroanatomical differences.
4. What acquisition-based techniques can mitigate artifacts from continuous motion? Emerging proof-of-principle studies demonstrate that using motion-compensating diffusion gradients can significantly reduce artifacts. In one study, standard (M0) gradients led to signal dropout in up to 44% of images during continuous motion. In contrast, second-order motion-compensated (M2) gradients resulted in 0% of images being corrupted by signal dropout under the same conditions, producing DTI parameters consistent with motion-free reference data [2] [3].
Table 2: Comparison of Motion Compensation Techniques
| Technique | Description | Key Finding / Efficacy |
|---|---|---|
| Standard (M0) Gradients | Traditional Stejskal-Tanner diffusion gradients [2] | Up to 44% of DW images corrupted by signal dropout during continuous motion [2] |
| 1st-Order (M1) Compensated | Nulls zeroth and first-order gradient moments [2] | Reduced visual signal dropout to 7% of images; further reduced to 1% with retrospective correction [2] |
| 2nd-Order (M2) Compensated | Nulls zeroth, first, and second-order gradient moments [2] | 0% of images showed substantial signal dropout during continuous motion [2] |
| Retrospective Correction (e.g., FSL eddy) | Software-based post-processing for motion and eddy currents [1] | Effective in large cohorts when combined with outlier replacement [1]; may be insufficient for extreme motion corrupting >15% of DW images [2] |
Troubleshooting Guides
Problem: Data Corruption from Continuous Head Motion
Symptoms: Significant signal dropout in diffusion-weighted images; implausible values in derived DTI metrics (e.g., elevated fractional anisotropy or diffusivity); failure of registration algorithms.
Solutions:
- Prospective Correction: Consider implementing motion-compensated diffusion gradient schemes (M1 or M2) in your acquisition protocol. These are designed to refocus moving spins and have been shown to be highly effective in preventing signal dropout during continuous motion [2] [3].
- Robust Preprocessing: Ensure your preprocessing pipeline includes a comprehensive toolset. The combination of FSL's
topupandeddyis considered state-of-the-art. Crucially, runeddywith its outlier detection and replacement feature (-repolflag) to identify and correct for signal dropouts [1]. - Hardware Tracking: For the highest accuracy, use external motion tracking. Marker-based optical systems (e.g., Polaris Vicra) or markerless systems using depth cameras can provide high-frequency motion estimates. One robust registration method for camera data was shown to outperform vendor-supplied methods and correlate well with image-based quality metrics [4] [5].
Problem: Quantifying Motion in a Study Cohort
Challenge: You need to describe and report the amount of head motion in your dataset for inclusion as a covariate in statistical models or for quality control.
Standardized Methodology:
- Use Preprocessing Outputs: After running
eddy(FSL), you will obtain two key files [1]:eddy_movement_rms: Contains the root-mean-square (RMS) movement per volume, both relative to the first volume and relative to the previous volume.eddy_parameters: A text file with six columns (three translations and three rotations) detailing the rigid-body movement parameters for each volume.
- Derive Summary Metrics: From these files, you can calculate:
- Relative mean displacement (mm).
- Maximum translation and rotation.
- Mean displacement normalized by scan duration (mm/min).
- Consider Data-Driven Alternatives: In the absence of external tracking, data-driven deep learning methods are being developed. For example, the DL-HMC++ framework uses a cross-attention mechanism on PET raw data to predict rigid head motion with high accuracy, demonstrating generalization across scanners and radiotracers [5].
Experimental Protocols for Key Studies
- Objective: To characterize the magnitude and direction of head motion across multiple populations and investigate the efficacy of preprocessing pipelines.
- Datasets: 13 consortium datasets (e.g., ADNI, BLSA, OASIS) totaling 16,995 imaging sessions. Included cognitively normal, cognitively impaired, and developmentally delayed participants across the lifespan (0.1-100 years).
- Preprocessing: All data were processed with the
PreQualpipeline, which includestopupfor susceptibility distortion correction andeddyfor eddy current and motion correction. Theeddycommand was run with the-repolflag for outlier replacement. - Motion Quantification: Motion descriptors (translations, rotations, RMS displacement) were derived from the
eddy_movement_rmsandeddy_parametersoutput files.
- Objective: To test the feasibility of motion-compensated diffusion gradients for DTI during continuous head motion.
- Subjects: Five healthy volunteers.
- Acquisition: Scanned on a 3T Siemens Prisma. DTI data acquired with standard (M0), first-order (M1), and second-order (M2) motion-compensated gradients. For each, datasets were acquired with and without continuous, deliberate head motion.
- Analysis:
- Visual assessment of signal dropout in DW images.
- Processing with
eddy(with and without extreme motion correction). - Calculation of DTI parameter maps (FA, MD, etc.) using
dtifit. - Voxelwise comparison of DTI parameters from motion-corrupted data to a motion-free reference.
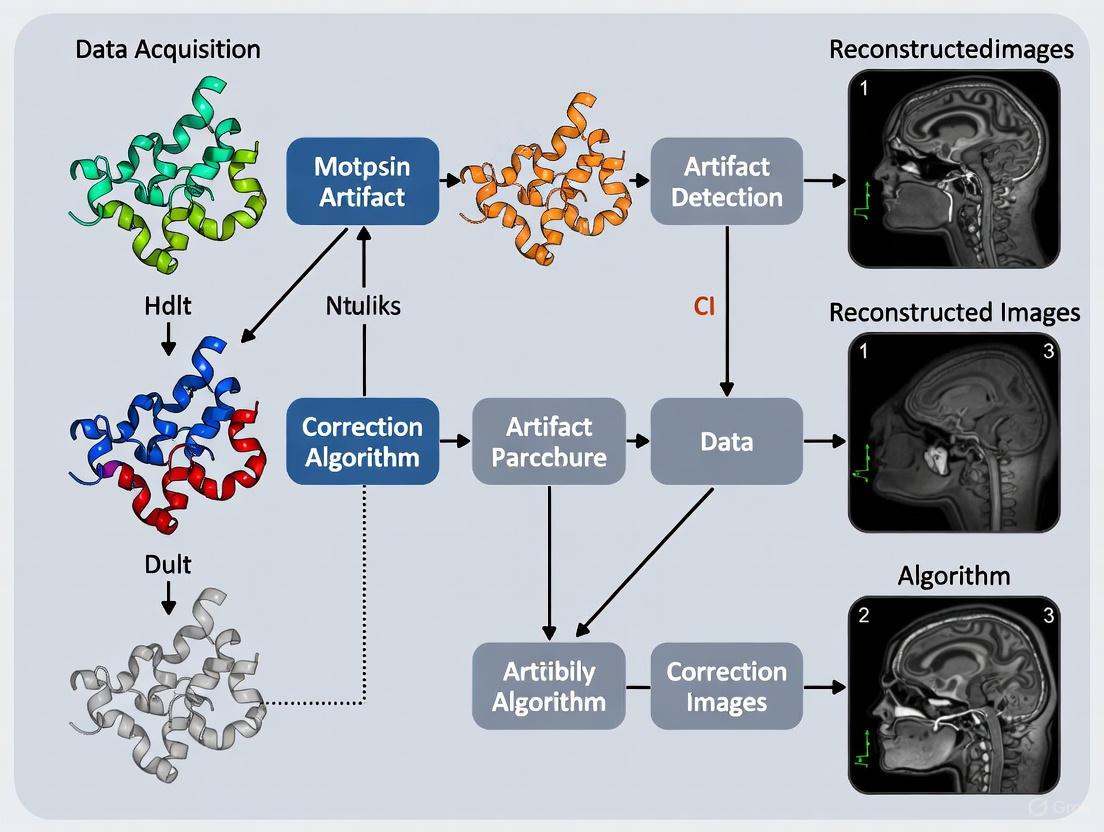
Workflow Visualization
The Scientist's Toolkit: Key Research Reagents & Solutions
Table 3: Essential Materials and Software for Motion Mitigation Research
| Item Name | Type | Function / Application |
|---|---|---|
| FSL (FMRIB Software Library) | Software Library | Provides the topup and eddy tools for comprehensive retrospective correction of susceptibility distortions, eddy currents, and motion in DTI data [1]. |
| PreQual Pipeline | Software Pipeline | An end-to-end diffusion preprocessing pipeline that automates the use of topup and eddy for robust and reproducible results [1]. |
| Motion-Compensated Diffusion Gradients (M1/M2) | Pulse Sequence | Acquisition-based gradient schemes that null higher-order gradient moments to reduce phase accumulation in moving spins, thereby mitigating signal dropout [2] [3]. |
| External Optical Motion Tracking (e.g., Polaris Vicra) | Hardware | Provides gold-standard, high-frequency measurement of rigid head motion for validation or direct use in motion correction frameworks [5]. |
| DL-HMC++ | Deep Learning Model | A supervised deep learning framework with a cross-attention mechanism for estimating rigid head motion directly from PET raw data, eliminating the need for external hardware [5]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary motion-induced artifacts in Diffusion Tensor Imaging (DTI)? The three most common motion-induced artifacts in DTI are signal dropout, misalignment, and erroneous signal attenuation. Signal dropout refers to partial or complete signal loss in voxels due to residual dephasing during strong diffusion encoding gradients. Misalignment occurs when head motion causes spatial inconsistencies between acquired slices or volumes. Erroneous signal attenuation involves incorrect measurement of diffusion strength due to motion-induced phase errors, leading to inaccurate tensor calculations [6] [7].
Q2: Why is DTI particularly sensitive to patient motion? DTI is highly motion-sensitive because it uses large amplitude and long duration diffusion gradients to encode microscopic water motion. Even minor head movements during these encoding periods can cause significant phase changes and signal loss. Furthermore, advanced DTI applications often require long scan times with many diffusion directions, increasing the likelihood of voluntary or involuntary motion [6] [8].
Q3: What is the difference between prospective and retrospective motion correction? Prospective motion correction methods compensate for motion in real-time during image acquisition using external tracking devices or navigator echoes to adjust scan geometry. Retrospective methods operate on already-acquired data using volume realignment and other post-processing algorithms without requiring hardware modifications [7] [9].
Q4: Can motion artifacts affect quantitative DTI measures like Fractional Anisotropy (FA)? Yes, motion artifacts can significantly bias quantitative DTI measures. Motion-induced signal loss and misregistration can lead to inaccurate estimation of diffusion tensors, resulting in erroneous FA values and other derived metrics such as mean diffusivity (MD), potentially compromising clinical and research conclusions [6] [7] [8].
Troubleshooting Guide: Identifying and Addressing Motion Artifacts
Artifact Identification Table
| Artifact Type | Visual Appearance | Primary Cause | Affected DTI Metrics |
|---|---|---|---|
| Signal Dropout | Focal dark regions or complete signal voids in diffusion-weighted images | Motion during diffusion encoding gradients causing residual dephasing within voxels | All tensor metrics, particularly biased toward lower FA |
| Slice Misalignment | Discontinuities between slices, geometric distortions, blurring | Bulk head motion between slice acquisitions causing inconsistent slice excitation | Altered tensor orientation, reduced reliability across slices |
| Erroneous Attenuation | Inhomogeneous signal intensity across similar tissue types | Motion-induced phase errors and gradient moment imbalance during encoding | Inaccurate apparent diffusion coefficient (ADC) calculations |
| Ghosting | Duplicate anatomical features along the phase-encoding direction | Periodic motion during the EPI readout train | General image quality degradation, noise in all metrics |
Motion Correction Method Comparison
| Method Category | Specific Techniques | Key Advantages | Key Limitations |
|---|---|---|---|
| Prospective Correction | Optical tracking (e.g., MPT system) [6], Sequence-embedded navigators (e.g., PROMO) [9] | Corrects through-plane motion, prevents data corruption | Requires specialized hardware, complex implementation |
| Retrospective Correction | Volume realignment [7], Eddy current correction (e.g., FSL eddy) [10], Volume rejection | No hardware requirements, applicable to existing data | Cannot fully correct through-plane motion, may introduce smoothing |
| Deep Learning Approaches | Self-supervised denoising (SSDLFT) [11], Generative models (GANs, diffusion models) [9] | Can work with limited training data, handles complex artifacts | Risk of visual distortions, limited generalizability across scanners |
| Sequence-Based Solutions | Moment-restoring gradient blips [6], Twice-refocused spin-echo sequences [6] | Addresses fundamental cause of signal dropout | May increase minimum echo time, specific to certain artifact types |
Experimental Protocols for Motion Mitigation
Protocol 1: Real-Time Motion Correction with Gradient Moment Restoration
This protocol combines prospective slice tracking with restoration of gradient moment balance to prevent signal loss [6].
Materials and Equipment:
- MRI scanner with sequence programming capability
- Optical motion tracking system (e.g., Moiré Phase Tracking)
- Head coil with camera access
- Motion tracking target (attaches to forehead)
Procedure:
- Attach motion tracking target securely to subject's forehead.
- Set up tracking system to provide head pose data at high frame rate (≥80 Hz).
- Modify standard DW-EPI sequence to include:
- Real-time updates of slice position and orientation before each RF pulse and readout.
- Storage of all rotation data between excitation and readout.
- Calculation of motion-induced gradient moment imbalance using:
M→(t) ≡ ∫₀ᵗ R^−1(t′)G→(t′)dt′[6] - Insertion of brief gradient blip immediately prior to signal readout to restore moment balance.
- For through-plane motion, ensure gradient moment satisfies:
MzΔz < 3.79γ⁻¹to prevent 50% signal loss. - For in-plane motion, ensure gradient moment satisfies:
MiΔxi < 0.5γ⁻¹to prevent sudden signal loss.
Protocol 2: Retrospective Correction with Automated Quality Control
This protocol uses post-processing approaches to identify and correct motion artifacts without specialized hardware [7] [10].
Materials and Equipment:
- DTI dataset with multiple b=0 volumes interspersed throughout acquisition
- Processing tools: FSL, DTIPrep, or QIT quantitative imaging toolkit
- Computational resources for image registration and tensor fitting
Procedure:
- Data Acquisition:
- Acquire multiple b=0 volumes (minimum 5) interspersed throughout DTI acquisition.
- Use acceleration techniques (e.g., GRAPPA) to maintain reasonable scan times.
Quality Control and Preprocessing:
- Run automated QC using DTIPrep to identify corrupted volumes based on:
- Interlace correlation values between slices
- Gradient-wise motion parameters
- Signal-to-noise thresholds
- Select optimal calibration weights from b=0 volumes with least motion.
- Run automated QC using DTIPrep to identify corrupted volumes based on:
Motion Correction:
- Perform 3D rigid-body realignment using all diffusion volumes.
- Apply importance weighting to prioritize well-aligned volumes.
- Implement phase correction and complex averaging to reduce Rician noise.
- For severe motion, apply b-matrix reorientation to account for head rotations.
Validation:
- Compare tensor metrics before and after correction.
- Check for improved consistency in FA values across the dataset.
- Verify anatomical plausibility of resulting fiber tractography.
Research Reagent Solutions
| Tool/Category | Specific Examples | Primary Function | Implementation Considerations |
|---|---|---|---|
| Quality Control Software | DTIPrep [12], QIT [10] | Automated detection of motion-corrupted volumes | DTIPrep requires careful threshold setting; gradient check may need disabling for high b-value data [12] |
| Processing Toolkits | FSL [10], DTI-TK [10], DTIplayground [12] | Retrospective correction and tensor calculation | FSL eddy corrects for eddy currents and motion simultaneously; GPU acceleration available |
| Motion Tracking Systems | Optical tracking (MPT) [6], Camera-based systems | Real-time head pose measurement for prospective correction | Require MR-compatible cameras; ~30 ms lag time typical; need secure attachment to subject |
| Deep Learning Frameworks | SSDLFT [11], SuperDTI [11], DeepDTI [11] | Denoising and artifact reduction using neural networks | SSDLFT reduces need for large training datasets; requires substantial computational resources |
Visual Guide to Motion Artifact Mechanisms and Correction
Motion-Induced Signal Loss Mechanism
Integrated Motion Correction Workflow
Frequently Asked Questions (FAQs)
Q1: What is the fundamental impact of head motion on DTI scalar metrics? Head motion during diffusion MRI acquisition introduces a positive bias in both Fractional Anisotropy (FA) and Mean Diffusivity (MD) values [13]. This effect is observed across different analysis pipelines, including tract-based spatial statistics (TBSS), voxelwise, and region of interest (ROI) analyses [13]. The bias is typically greater for MD than for FA [13].
Q2: Can modern preprocessing pipelines fully eliminate motion-induced bias? Recent evidence suggests that state-of-the-art preprocessing pipelines can effectively mitigate motion to the point where biases become undetectable with current analysis techniques [1]. These pipelines incorporate tools for susceptibility distortion correction, eddy-current correction, and outlier replacement [1]. Studies analyzing scan-rescan data from the same subjects found no detectable differences in microstructure or connectivity between high-motion and low-motion scans after comprehensive preprocessing [1].
Q3: How does motion correction methodology affect the accuracy of DTI metrics? Combining denoising with B-matrix Spatial Distribution (BSD) correction significantly improves the accuracy of both FA and MD measures, as well as overall tractography quality [14]. Research demonstrates that these approaches are complementary—denoising reduces random errors while BSD correction addresses systematic errors associated with nonuniformity of magnetic field gradients [14].
Q4: What are the challenges when comparing DTI metrics across different methodologies? Substantial differences in FA measurements can occur between different tractography methods [15]. Studies comparing manual DTI-based methods with AI-based approaches (like TractSeg) found poor-to-moderate agreement in FA values across most white matter tracts [15]. This highlights that FA values derived from different methodologies are not directly interchangeable without appropriate standardization [15].
Q5: How can multi-scanner variability in DTI metrics be addressed? Harmonization algorithms such as NeuroCombat and LongCombat effectively reduce both intra- and inter-scanner variability in diffusion metrics [16]. These methods minimize scanner-specific effects while preserving biological variability, making them particularly valuable for multi-site studies [16].
Troubleshooting Guides
Identifying and Quantifying Head Motion in DTI Data
Problem: Suspected head motion contamination in DTI metrics, manifested as unexpected FA or MD values.
Investigation Protocol:
- Extract Motion Parameters: Calculate relative mean displacement (mm) from preprocessing outputs (e.g., FSL's EDDY output) [1].
- Characterize Motion Patterns: quantify translation in anterior-posterior, left-right, and inferior-superior directions, plus rotations around these axes [1].
- Establish Reference Values: Note that healthy subjects typically move 1-2 mm/min, with most motion occurring as translation in the anterior-posterior direction and rotation around the right-left axis [1].
- Compare to Norms: Motion exceeding 2 mm/min or three standard deviations above your cohort mean warrants careful inspection [13].
Resolution Steps:
- Implement comprehensive preprocessing with integrated distortion correction and outlier replacement [1].
- For extreme motion, consider excluding subjects with displacement >3 standard deviations from your cohort mean [13].
- Document motion metrics as part of your quality assurance protocol to enable covariance analysis [13].
Addressing Systematic Errors in DTI Metrics
Problem: Systematic errors and noise disrupting accurate visualization of white matter anatomy.
Investigation Protocol:
- Identify Error Sources: Determine whether errors stem from random noise or systematic gradient nonuniformity [14].
- Evaluate Current Pipeline: Assess which corrections your preprocessing currently implements.
Resolution Steps:
- Implement a combined approach of denoising AND BSD correction [14].
- For phantom data, prioritize BSD correction, which has substantially greater effect on improving DTI metric accuracy in controlled conditions [14].
- For in vivo data, apply both denoising and BSD correction to address both random and systematic errors [14].
- Validate improvements in specific brain structures including corpus callosum, internal capsule, putamen, and thalamus [14].
Managing Scanner-Related Variability in Multi-Site Studies
Problem: Inconsistent DTI metrics across different scanners or sites, complicating pooled analysis.
Investigation Protocol:
- Quantify Variability: Measure intra-scanner and inter-scanner variability using a healthy control cohort if available [16].
- Identify Sources: Determine whether variability stems from hardware differences, acquisition parameters, or reconstruction algorithms [16].
Resolution Steps:
- Apply ComBat-based harmonization (NeuroCombat for cross-sectional studies, LongCombat for longitudinal studies) [16].
- Implement harmonization at either the ROI or voxel level, depending on your research question [16].
- Include biological covariates (age, sex) in the harmonization model to preserve relevant biological variability [16].
- Validate that harmonization reduces variability to levels comparable to scan-rescan variability within the same scanner [16].
Interpreting Unexpected FA Increases in Pathological Populations
Problem: Observing increased FA values in patient populations where decreases are typically expected.
Investigation Protocol:
- Rule Out Motion Artifact: Ensure observed increases are not attributable to differential motion between patients and controls [13].
- Consider Biological Plausibility: Evaluate whether increases might reflect compensatory mechanisms rather than pathology [17].
- Employ Advanced Modeling: Consider whether free-water correction might reveal different patterns [18].
Resolution Steps:
- Document and compare motion parameters between groups as a standard quality control measure [13].
- For neurodegenerative populations, consider that increased FA and magnetic susceptibility in regions like the cerebral peduncle may represent early biomarkers of phenoconversion [17].
- Implement free-water correction to eliminate partial volume effects from enlarged perivascular spaces, particularly in populations with morphological abnormalities [18].
Quantitative Data Tables
Table 1: Motion-Induced Bias in DTI Metrics Across Analysis Pipelines
| Analysis Pipeline | FA Bias Direction | MD Bias Direction | Relative Effect Size | Key References |
|---|---|---|---|---|
| Tract-Based Spatial Statistics (TBSS) | Positive | Positive | Greater for MD | [13] |
| Voxelwise Analysis | Positive | Positive | Greater for MD | [13] |
| Region of Interest (ROI) | Positive | Positive | Greater for MD | [13] |
Table 2: Effectiveness of Motion Correction Approaches
| Correction Method | FA Improvement | MD Improvement | Tractography Quality | Key References |
|---|---|---|---|---|
| Denoising Only | Significant | Significant | Moderate Improvement | [14] |
| BSD Correction Only | Significant | Significant | Moderate Improvement | [14] |
| Denoising + BSD Correction | Most Significant | Most Significant | Greatest Improvement | [14] |
| Modern Preprocessing Pipelines | Bias Effectively Eliminated | Bias Effectively Eliminated | High Quality | [1] |
Table 3: Harmonization Methods for Multi-Scanner Studies
| Harmonization Method | Study Type | Variability Reduction | Preserves Biological Variance | Key References |
|---|---|---|---|---|
| NeuroCombat | Cross-sectional | Effective intra- and inter-scanner | Yes, with appropriate covariates | [16] |
| LongCombat | Longitudinal | Effective intra- and inter-scanner | Yes, accounts for within-subject correlation | [16] |
Experimental Protocols
Protocol for Evaluating Motion Correction Efficacy
Purpose: To quantitatively assess the effectiveness of different motion correction approaches in improving DTI metric accuracy [14].
Materials:
- DTI data from a single subject scanned multiple times or a multi-subject cohort (≥40 participants recommended) [14]
- Corresponding phantom data acquired with the same sequence [14]
- Processing environment with denoising and BSD correction capabilities [14]
Methodology:
- Data Acquisition: Acquire DTI data using your standard protocol, ensuring consistent parameters between in vivo and phantom scans [14].
- Processing Configurations: Process each dataset using six configurations:
- Raw data without correction
- Denoising only
- Full preprocessing without BSD correction
- Each of the above with added BSD correction [14]
- Metric Evaluation: Quantify FA and MD values in specific structures: corpus callosum, internal capsule, putamen, and thalamus [14].
- Quality Assessment: Perform both visual and quantitative evaluation of tractography results [14].
Validation:
- Compare results across processing configurations [14]
- Use phantom data to establish ground truth comparisons [14]
- Focus on structures known to be sensitive to motion artifacts [14]
Protocol for Multi-Scanner Harmonization Validation
Purpose: To validate the effectiveness of harmonization methods for reducing intra- and inter-scanner variability in DTI metrics [16].
Materials:
- Cohort of healthy participants (≥38 recommended) scanned on multiple scanners on the same day [16]
- Multi-shell dMRI protocol optimized for diffusion kurtosis imaging [16]
- Structural T1-weighted images [16]
- Harmonization software (NeuroCombat/LongCombat) [16]
Methodology:
- Data Collection: Scan all participants on two different scanners using identical protocols [16].
- Preprocessing: Perform standard preprocessing including motion correction, eddy-current correction, and distortion correction [16].
- Metric Extraction: Calculate diffusion metrics (FA, MD, AD, RD) for both voxel-wise and ROI-based analyses [16].
- Harmonization Application: Apply NeuroCombat and LongCombat algorithms to the diffusion metric maps [16].
- Variability Quantification: Calculate intra-scanner and inter-scanner variability before and after harmonization [16].
Validation:
- Compare variability measures pre- and post-harmonization [16]
- Target: Achieve variability levels comparable to scan-rescan variability within the same scanner [16]
- Ensure biological variability related to age and sex is preserved [16]
Workflow Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Tools for DTI Artifact Mitigation
| Tool/Technique | Primary Function | Application Context | Key Considerations |
|---|---|---|---|
| FSL EDDY with --repol | Motion correction with outlier replacement | All DTI studies requiring motion correction | Effectively mitigates motion to undetectable levels when properly implemented [1] |
| B-matrix Spatial Distribution (BSD) Correction | Corrects systematic errors from gradient nonuniformity | Studies requiring high precision in FA/MD measurements | Complementary to denoising; substantially improves phantom data accuracy [14] |
| Free-Water Correction | Eliminates partial volume effects from extracellular fluid | Populations with atrophy or enlarged perivascular spaces | Reveals microstructural differences masked by free-water contamination [18] |
| NeuroCombat/LongCombat | Harmonizes multi-scanner data | Multi-site studies and clinical trials | Reduces scanner variability to scan-rescan levels; preserves biological signals [16] |
| Denoising Algorithms | Reduces random noise in DTI data | All DTI applications, especially low-SNR data | Works synergistically with BSD correction to improve tractography quality [14] |
FAQs: Understanding Motion in DTI and Its Complex Correlates
FAQ 1: How do age and developmental stage affect a subject's propensity for motion during DTI? Motion in DTI studies is strongly correlated with age, following a U-shaped curve across the lifespan. Pediatric populations, around age 7, are particularly prone to incidental motion during scanning, presenting a significant challenge for data acquisition [19]. Similarly, studies involving older adults, especially those in late middle-age to older adulthood (ages 54-92), must account for age as a primary factor. While in these cohorts age is more strongly linked to alterations in white matter microstructure itself, the increased prevalence of conditions causing discomfort or restlessness can indirectly influence motion [20]. In contrast, compliant healthy adults typically represent the most stable demographic for motion-free DTI.
FAQ 2: Are certain clinical populations more susceptible to motion, and how does this interact with their underlying neuropathology? Yes, motion susceptibility is significantly elevated in specific clinical populations. Patients with neurological conditions such as Parkinson's disease (PD), stroke, or other neurodegenerative disorders often have difficulty remaining still due to motor symptoms, tremor, or cognitive impairment [2]. This is particularly problematic because DTI is a powerful tool for investigating the microstructural changes in these very conditions, such as studying the substantia nigra in PD or white matter tracts post-stroke [21]. Furthermore, research on populations with Down syndrome (DS) highlights a critical confound: the neuropathology of interest (e.g., Alzheimer's disease-related amyloid accumulation) is longitudinally correlated with changes in DTI metrics, making it crucial to disentangle true microstructural changes from motion-induced artifacts [22].
FAQ 3: What is the impact of cognitive status on scan quality? Cognitive status is a major determinant of scan quality. Subjects with Mild Cognitive Impairment (MCI) or dementia, including those with Down syndrome (DS), may have reduced comprehension of instructions, increased anxiety, or physical agitation, all of which elevate the risk of motion [22] [2]. For instance, in studies of adults with DS, cognitive status is a key variable, and researchers must employ specific strategies to accommodate participants, as standard DTI protocols are often unsuitable for populations prone to movement [22]. The resulting artifacts can obscure the subtle white matter differences these studies aim to detect.
FAQ 4: Why are traditional DTI sequences so vulnerable to motion artifacts? Traditional DTI sequences use Stejskal-Tanner (M0) diffusion gradients. These gradients are sensitive to any macroscopic head motion because moving spins accumulate non-zero residual phase when these gradients are applied. This leads to severe signal dropout and corrupted image data [2]. The problem is exacerbated by the use of single-shot Echo Planar Imaging (EPI), which is highly susceptible to geometric distortions and ghosting artifacts from even minor subject movement [19] [23].
FAQ 5: What are the most effective strategies for mitigating motion artifacts in vulnerable populations? A multi-pronged approach is most effective, combining acquisition and processing strategies:
- Prospective Motion Correction (vNav): Real-time tracking of head motion with navigators to update the scanner's gradient coordinates during data acquisition, preventing artifacts at the source [19] [24].
- Motion-Compensated Gradient Schemes: Using first-order (M1) or second-order (M2) motion-compensated diffusion gradients that nullify phase accumulation from velocity and acceleration, making the sequence inherently robust to continuous motion [2].
- Retrospective Correction: Post-processing with software like FSL or TORTOISE to correct for motion and eddy current distortions. For extreme motion, combining prospective navigation with retrospective correction yields the best results [2] [19].
- Sequence Optimization: Incorporating dummy gradients and optimized navigator echoes to reduce eddy current-induced distortions and N/2 ghosting artifacts, which is particularly beneficial at higher field strengths [23].
Troubleshooting Guides
Guide 1: Diagnosing and Quantifying Motion Corruption
Problem: Suspected motion corruption in DTI dataset, leading to unreliable fractional anisotropy (FA) and mean diffusivity (MD) maps.
Solution:
- Visual Inspection: Scroll through the diffusion-weighted images (DWI) dynamically. Look for images with obvious signal dropout, geometric misalignment, or "ghosting" duplicates of the brain [2].
- Quantitative Assessment:
- Use tools like
eddyin FSL to generate a report on the number of corrupted slices or volumes [2]. - Calculate the mean squared displacement between consecutive volumes. Sudden large displacements indicate abrupt motion.
- Use tools like
- Parameter Map Analysis: Generate initial FA and MD maps. Unusually high or low values, or a "patchy" appearance in white matter, can indicate residual motion artifacts after processing. Compare the values to established norms for the population; for example, in healthy aging, FA decreases and MD increases, but in a non-linear, region-specific pattern [25].
Table 1: Common Motion Artifacts and Their Signatures
| Artifact Type | Visual Signature in DWI | Impact on DTI Metrics |
|---|---|---|
| Signal Dropout | Dark, blurry, or missing slices in individual volumes [2] | Spurious increases in MD and RD; decreases in FA [2] |
| Ghosting | Duplicate, faint images of the brain shifted along the phase-encode direction [23] | Inaccurate tensor estimation, leading to noisy FA/MD maps |
| Eddy Current Distortion | Shearing and stretching of the brain image, varying by diffusion direction [19] [23] | Misalignment between volumes, causing errors in tractography |
Guide 2: Selecting a Motion Correction Pipeline
Problem: Choosing an appropriate processing pipeline for a dataset with known motion, particularly from a vulnerable population.
Solution: The optimal pipeline depends on the severity and nature of the motion.
Table 2: Motion Correction Pipeline Performance Comparison
| Pipeline Strategy | Best For | Procedure | Advantages | Limitations |
|---|---|---|---|---|
Retrospective Only (e.g., FSL's eddy) |
Datasets with mild, intermittent motion [19] | Post-hoc volume alignment and outlier replacement [2] | Widely available; no special acquisition required | Struggles with severe, continuous motion; can introduce smoothing [2] [19] |
| Prospective Only (vNav) | Populations where some motion is anticipated | Real-time motion tracking and scanner adjustment during scan [19] [24] | Prevents artifacts at source; improves raw image quality | May not be available on all scanners; does not correct for between-volume motion |
| Combined (vNav + Retrospective) | High-motion populations (e.g., children, patients with PD) [19] | Acquire with vNav, then process with TORTOISE or FSL | Highest sensitivity and specificity in tractography; best overall correction [19] | More complex workflow; longer processing times |
| Motion-Compensated Gradients (M1/M2) | Continuous, gross motion (e.g., tremor, unable to suppress movement) [2] | Use M1/M2 sequence instead of standard M0 during acquisition | Inherently robust to motion; 0% signal dropout reported in studies with continuous motion [2] | May require custom sequence implementation; potentially longer TE |
Decision Workflow for Motion Mitigation
Experimental Protocols & Supporting Data
Protocol 1: Implementing Motion-Compensated DTI Acquisition
This protocol is adapted from studies demonstrating the efficacy of second-order (M2) motion-compensated gradients during continuous head motion [2].
Methodology:
- Scanner: 3T Siemens Prisma.
- Sequence: Diffusion-prepared Echo Planar Imaging (EPI).
- Key Parameters: TR/TE = 12600/89 ms; FOV = 220 × 220 mm²; 2 mm isotropic voxels; 60 slices; 30 directions at b=1000 s/mm², 4 b=0 volumes.
- Experimental Groups: For validation, scan subjects under two conditions:
- No Motion: Instruct the subject to remain still.
- Continuous Motion: Subject performs periodic head rotation (e.g., 20°, 1 Hz).
- Diffusion Gradients: Acquire data using standard (M0), first-order (M1), and second-order (M2) motion-compensated schemes in the same session [2].
- Processing: Process all datasets using FSL's
eddy(with and without outlier replacement) anddtifitto generate FA, MD, AD, and RD maps.
Key Findings:
- In the presence of continuous motion, 44% of images acquired with standard M0 gradients were corrupted by signal dropout.
- Under the same motion conditions, M2 gradients reduced corrupted images to 0% [2].
- DTI parameters from motion-M2 data were consistent with reference no-motion data, whereas motion-M0 data showed significant deviations even after retrospective correction [2].
Protocol 2: Longitudinal DTI in a Vulnerable Clinical Population (Down Syndrome)
This protocol details a longitudinal study design that investigates the correlation between amyloid burden and white matter change in adults with DS, a population where motion and pathology are key considerations [22].
Methodology:
- Participants: 35 adults with DS (age range 25-57), including individuals classified as cognitively stable (CS), with mild cognitive impairment (MCI-DS), or with dementia.
- Imaging Timepoints: Baseline and follow-up at approximately 3.7 years.
- Multimodal Imaging:
- DTI: Acquired on a 3T GE Signa 750. Parameters: 2.0 mm³ isotropic resolution, TR/TE = 7800/60.4 ms, b=0,1000 s/mm² (48 directions).
- Amyloid PET: [C-11]PiB PET on a Siemens ECAT HR+ scanner to measure Aβ burden (Centiloid values).
- Analysis: Use tract-based spatial statistics (TBSS) to analyze DTI metrics (FA, MD). Perform permutation analysis to test for correlation between the rates of change in DTI and amyloid PET.
Key Findings:
- The rates of change for all DTI metrics and amyloid burden were significantly related [22].
- Significant changes were observed in widespread white matter, including the corpus callosum, corona radiata, and long-association fibers [22].
- This study highlights the importance of longitudinal design to track intra-individual change and control for population heterogeneity.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Motion-Resilient DTI Research
| Tool / Resource | Function | Example Use-Case |
|---|---|---|
| Motion-Compensated Diffusion Gradients (M1/M2) | Acquisition sequences that nullify phase accumulation from head velocity/acceleration, preventing signal dropout [2]. | Imaging patients with Parkinson's tremor or restless children. |
| Prospective Motion Correction (vNav) | A 3D-EPI navigator that tracks head position in real-time and updates scan coordinates [19] [24]. | Preventing motion artifacts in any anxious or movement-prone subject during longer scans. |
| FSL (FMRIB Software Library) | A comprehensive software library for MRI analysis, including the eddy tool for retrospective motion and eddy current correction [2] [19]. |
Standard processing and correction of DTI data, including outlier replacement. |
| TORTOISE | A software package for retrospective correction of DTI distortions, particularly effective for eddy currents and EPI distortions [19]. | Advanced processing, especially when combined with prospective correction for highest quality. |
| Optimized Navigator Echoes & Dummy Gradients | Sequence modifications that better capture phase errors and pre-emphasize gradients to reduce eddy currents [23]. | Improving image quality and geometric accuracy at high field strengths (e.g., 7T). |
Motion Mitigation Strategy Map
Motion Mitigation in Practice: Acquisition and Processing Techniques
FAQs: Understanding Navigator Echoes
What is a navigator echo and what is its primary function in DTI? A navigator echo is an additional radio-frequency (RF) pulse used to dynamically track anatomic motion in real-time during an MRI scan [26]. In the context of Diffusion Tensor Imaging (DTI), its primary function is to monitor and correct for subject motion, such as head movement, which is a fundamental source of artifact due to the long acquisition times of DTI sequences [19] [27]. This prospective (real-time) correction helps to prevent spatial misregistration, blurring, and errors in the computation of the diffusion tensor [27].
How does a navigator echo track motion? A navigator pulse, which can be a spin echo or gradient echo, is prescribed over a specific anatomic region, such as the diaphragm or part of the brain [26]. It creates a column of excited spins, often called a "pencil beam." The signal returned from this column is reconstructed and displayed in an M-mode format, showing the position of the tissue boundary over time [26]. Automated software detects this motion, and the information is used to either trigger data acquisition only during a specific part of the motion cycle (e.g., respiration) or to dynamically adjust the location of the imaging slices to follow the moving anatomy, a process known as "slice tracking" or "slice following" [26].
What are the key differences between prospective and retrospective motion correction?
- Prospective Correction (e.g., with Navigator Echoes): Correction occurs in real-time during data acquisition. The scanning geometry (e.g., slice position and orientation) is updated to compensate for subject motion as it happens [19] [27]. This method directly addresses spin-history effects and intra-volume motion and ensures the applied diffusion encoding (b-matrix) aligns correctly with the anatomy [27].
- Retrospective Correction: Correction is applied after the scan is complete during data processing. It typically involves volume-to-volume or slice-to-volume registration algorithms (e.g., in software packages like FSL or TORTOISE) [19]. While it can correct for spatial misregistration, it cannot fully account for spin-history effects or the corruption of the b-matrix due to motion occurring during the acquisition [27].
Can prospective and retrospective correction be used together? Yes, research indicates that a combination of both methods is highly effective. One study found that using navigator-based prospective correction alongside retrospective processing with TORTOISE resulted in the best match with anatomical white matter maps [19]. The inclusion of retrospective correction improved ellipsoid fits and the sensitivity and specificity of group tractography results, even for data that had already been acquired with prospective correction [19].
What are "leading" and "trailing" navigators?
- A leading navigator is acquired before data acquisition to determine the initial position of the anatomy and is required for slice tracking [26].
- A trailing navigator is acquired after data acquisition. It is used to verify that the anatomy returned to the same position. If the position difference between the leading and trailing navigators exceeds a set threshold, the data can be discarded and reacquired [26].
Troubleshooting Guides
Issue: Poor Quality of Navigator Signal
Problem: The navigator signal is weak or noisy, leading to unreliable motion tracking.
| Potential Cause | Recommended Action |
|---|---|
| Incorrect navigator placement | Reposition the navigator beam over a well-defined tissue boundary (e.g., the dome of the liver for diaphragmatic motion). Using a "pencil beam" from two intersecting bands can improve accuracy [26]. |
| Suboptimal navigator parameters | Adjust the navigator beam width (typically 1-2 cm) and spatial resolution (approx. 1 mm along the beam) [26]. For 2D spiral RF-navigators, consider adjusting the flip angle and number of cycles to balance pulse duration and artifacts [26]. |
| Hardware/Coil selection | Ensure the body coil or a dedicated parallel imaging coil is properly assigned and functioning for navigator detection [26]. |
Issue: Inconsistent Gating or Tracking Performance
Problem: The system fails to consistently acquire data within the desired motion window, or slice tracking is erratic.
| Potential Cause | Recommended Action |
|---|---|
| Drifting gating levels | Enable automatic detection schemes on the scanner to continuously monitor and update the expiration level throughout the scan [26]. |
| Inconsistent respiratory pattern (in patients) | Set a wider gating tolerance window (typically 3-6 mm) to accommodate natural variation [26]. For brain imaging, consider alternative tracking methods like optical motion correction for more direct head movement tracking [27]. |
| Inadequate tracking algorithm | Verify that the software is correctly detecting the peaks and troughs of the motion signal. Manually adjust the detection thresholds if necessary [26]. |
Issue: Persistent Motion Artifacts in Final DTI Images
Problem: Even with navigator echoes enabled, the resulting fractional anisotropy (FA) maps or tractography still show artifacts suggestive of motion.
| Potential Cause | Recommended Action |
|---|---|
| Intra-volume motion | Navigator echoes may not fully correct for motion that occurs during the acquisition of a single volume. Consider complementary techniques like prospective optical motion correction, which can update the scan plane with very low latency [27]. |
| Inadequate combination with other corrections | Ensure that the data processing pipeline includes concurrent correction for other DTI artifacts, such as eddy currents and EPI distortion, in addition to the prospective motion data [19]. |
| Limitations of navigator correction | Recognize that navigator echoes primarily correct for rigid-body motion in the plane of the navigator. For complex motion or studies requiring high precision, a multi-modal approach (prospective + retrospective) is recommended [19]. |
Experimental Protocols & Data
Protocol: Implementing Navigator Echoes for DTI
Aim: To acquire DTI data with real-time prospective motion correction using volumetric navigator echoes (vNavs).
Methodology:
- Pulse Sequence: A standard twice-refocused spin-echo EPI diffusion sequence is modified to incorporate a 3D, multishot EPI navigator echo immediately after the acquisition of each diffusion-weighted volume [19].
- Navigator Acquisition: The navigator is not diffusion-weighted and has a short acquisition time (e.g., 526 ms) [19]. It is co-registered to a reference navigator from the first volume to calculate motion parameters (rotation and translation).
- Real-Time Update: Before the start of the next diffusion volume, the sequence receives the motion parameters. The scanner's gradient and RF systems are updated in real-time to adjust the slice position and orientation, compensating for the measured motion [19].
- Data Acquisition: The subsequent diffusion volume is acquired with the updated geometry, ensuring it is aligned with the moving anatomy.
This protocol was used in a pediatric study, a population prone to motion, and demonstrated improved outcomes when combined with retrospective processing [19].
Quantitative Data on Motion Correction Efficacy
Table 1: Comparison of Motion Correction Method Combinations in a Pediatric Cohort [19] This table summarizes the relative performance of different processing pipelines for DTI data, as measured by the match to anatomical white matter maps.
| Prospective Acquisition Correction | Retrospective Processing Package | Relative Performance (Match to WM Anatomy) |
|---|---|---|
| Standard DTI (no navigator) | FSL | Baseline |
| Navigator-enabled DTI (vNav) | FSL | Improved |
| Standard DTI (no navigator) | TORTOISE | Improved |
| Navigator-enabled DTI (vNav) | TORTOISE | Highest |
Table 2: Key Technical Specifications of Different Motion Tracking Technologies Note: Data synthesized from multiple sources. [26] [19] [27]
| Tracking Technology | Typical Accuracy | Key Advantages | Key Limitations |
|---|---|---|---|
| Navigator Echoes (vNav) | Sub-millimeter and sub-degree [19] | Integrated into the MRI pulse sequence; does not require external hardware. | Latency of one TR; primarily tracks a single direction or volume; can be affected by SNR. |
| Optical Tracking | < 1 mm and < 1° [27] | Very low latency; independent of MRI sequence; tracks rigid head motion directly. | Requires MR-compatible camera and a marker attached to the patient; setup and cross-calibration needed. |
Workflow Diagrams
Diagram 1: Navigator Echo Prospective Motion Correction Workflow
Diagram 2: Combined Prospective & Retrospective Correction
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for DTI Motion Correction
| Item | Function in Research |
|---|---|
| Navigator-Enabled Pulse Sequence | A modified MRI pulse sequence (e.g., a twice-refocused SE-EPI with integrated vNav) that permits the acquisition of navigator echoes for real-time motion tracking and correction [19]. |
| Retrospective Processing Software (TORTOISE) | A software package for post-processing DTI data. It is used to apply retrospective motion, eddy current, and EPI distortion correction, and has been shown to be effective even on data acquired with prospective correction [19]. |
| Retrospective Processing Software (FSL) | A comprehensive library of tools for FMRI, MRI, and DTI brain image analysis. Its eddy tool is commonly used for retrospective correction of eddy currents and motion [19]. |
| Optical Motion Tracking System | An external, camera-based system that tracks head movement via a marker on the subject. It provides very low-latency motion data for prospective correction, independent of the MRI sequence [27]. |
| Phantom for Validation | A stable, non-biological object used to validate the accuracy and precision of the motion correction pipeline without the confounding variable of live subject motion [19]. |
This guide provides troubleshooting and FAQs for using FSL's EDDY and TOPUP tools, specifically within the context of mitigating motion and distortion artifacts in diffusion tensor imaging (DTI) research.
Frequently Asked Questions (FAQs)
Q1: What are the primary causes of artifacts that EDDY and TOPUP are designed to correct?
TOPUP corrects for susceptibility-induced distortions, which are caused by the object (e.g., the head) disrupting the main magnetic field, leading to a spatially varying off-resonance field. This results in image distortions, particularly severe in Echo-Planar Imaging (EPI) sequences used in DTI due to the long time during which the off-resonance field can translate into a phase difference [28]. EDDY corrects for eddy current-induced distortions and subject movement. Eddy currents are induced in conductive parts of the scanner gantry by the rapid switching of strong diffusion encoding gradients, creating off-resonance fields that distort each diffusion volume differently. Subject movement during the long DTI acquisition further misaligns volumes [29].
Q2: My data was not acquired on the "whole-sphere" for diffusion directions. Can I still use EDDY effectively?
Yes, you can. While it is helpful for EDDY's internal Gaussian Process model if data is acquired on the whole-sphere (as this results in a prediction target in undistorted space), it is not a strict requirement. If your data was sampled on a half-sphere, you can simply add the --repol flag to the EDDY command line. This option enables the replacement of outlier slices, which is particularly beneficial in this scenario [29].
Q3: The subject moved between my two phase-encoded b0 acquisitions. Will this affect the TOPUP field estimation?
TOPUP features an internal movement model that allows it to simultaneously estimate the off-resonance field and any rigid-body movement between the two input volumes. This means it can typically handle subject movement gracefully. Methods without such a model may inaccurately attribute differences caused by movement to the off-resonance field, producing a poor and potentially misleading estimate [30].
Q4: I have old data and cannot find the total readout time for my acquisition. What should I use in the acqparams.txt file?
If the output of TOPUP and EDDY will only be used within the FSL ecosystem (i.e., with applytopup or eddy), you can use an arbitrary but reasonable value, such as 0.05 or 0.1. The critical factor for correction is the consistency of the scaling between displacement and Hz across tools, not the absolute value. The correction will still be accurate even if the readout time is not exact [30].
Troubleshooting Common Issues
Issue 1: EDDY fails or runs exceptionally slowly due to high memory usage.
- Explanation: EDDY is computationally intensive and memory hungry. A rule of thumb for its memory requirement is 8 × m × nx × ny × nz bytes, where m is the number of volumes, and nx, ny, nz are the matrix dimensions [31].
- Solution: Ensure your system has sufficient RAM. If possible, run EDDY on a high-performance computing node with ample memory.
Issue 2: Poor quality brain mask leads to suboptimal EDDY results.
- Explanation: EDDY uses a mask to define the brain region for processing. An inaccurate mask (e.g., including non-brain tissue or excluding parts of the brain) can severely degrade the correction quality [31] [32].
- Solution: Always visually inspect the mask generated from the high-fidelity b0 image (from TOPUP) using
fsleyesorfslview. Manually adjust the BET parameters (e.g.,-ffor fractional intensity threshold) to optimize brain extraction before running EDDY [32].
Issue 3: Incorrect parameters in the acqparams.txt file.
- Explanation: The phase-encoding direction and total readout time must be accurately specified for both TOPUP and EDDY to work correctly. An error here will result in an incorrect distortion correction [33] [30].
- Solution: Use the
dcm2niixconverter, which often generates a.jsonfile alongside the NIfTI image. This file may contain a"TotalReadoutTime"field. Alternatively, calculate it from the DICOM protocol using the formula:ReadoutTime = EchoSpacing * (EPI_Factor - 1)[30]. The table below provides common examples.
Table: Examples of acqparams.txt Entries for Different Phase-Encoding Directions
| Phase Encoding Direction | Phase Encoding Vector | Total Readout Time (s) |
|---|---|---|
| Anterior → Posterior (A>>P) | 0 -1 0 | 0.095 |
| Posterior → Anterior (P>>A) | 0 1 0 | 0.095 |
| Right → Left (R>>L) | 1 0 0 | 0.122 |
| Left → Right (L>>R) | -1 0 0 | 0.122 |
Issue 4: Outlier slices and signal dropout remain after standard EDDY correction.
- Explanation: When a subject moves during diffusion encoding, it can cause complete or partial signal dropout in entire slices. After motion correction, these can appear as diagonal bands in the data, biasing parameter estimation [31].
- Solution: Use the
--repoloption in EDDY. This flag enables outlier detection and replacement by predicting the missing signal using a Gaussian Process, effectively mitigating this specific artifact [31].
Experimental Protocols and Workflows
Integrated TOPUP and EDDY Processing Pipeline
The following workflow details the standard protocol for jointly using TOPUP and EDDY to correct DTI data [31] [32].
Diagram Title: Integrated TOPUP and EDDY Processing Workflow
Key Configuration Parameters
Table: Essential Parameters for Running TOPUP and EDDY
| Tool | Parameter | Typical Value / File | Purpose |
|---|---|---|---|
| TOPUP | --imain |
AP_PA_b0.nii.gz |
Input 4D image of b0 volumes with different PE directions. |
--datain |
acqparams.txt |
Text file specifying PE vector and readout time for each volume in --imain. |
|
--config |
b02b0.cnf |
Pre-defined configuration file with parameters optimized for registering b0 images. | |
--out |
my_topup_results |
Base name for output files containing the estimated field. | |
| EDDY | --imain |
data.nii.gz |
The main 4D input diffusion data to be corrected. |
--mask |
my_hifi_b0_brain_mask.nii.gz |
Brain mask generated from the high-fidelity b0 output from TOPUP. | |
--index |
index.txt |
Text file mapping each volume in --imain to a row in acqparams.txt. |
|
--topup |
my_topup_results |
Base name of the TOPUP results (for applying the susceptibility correction). | |
--acqp |
acqparams.txt |
The same acquisition parameters file used for TOPUP. | |
--bvecs/--bvals |
bvecs, bvals |
Files containing the diffusion gradient directions and b-values. | |
--repol |
(Flag) | Recommended: Enables detection and replacement of outlier slices. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Resources for DTI Preprocessing with FSL
| Item | Function / Purpose |
|---|---|
| FSL Installation | The software library containing the TOPUP and EDDY executables. Essential for all processing steps. |
| Diffusion Dataset | 4D NIfTI file(s) of DWI data. Must include volumes with at least two different phase-encoding directions (e.g., A>>P and P>>A) for accurate TOPUP estimation [31] [32]. |
| b-values File (.bval) | A text file listing the b-value for each volume in the diffusion dataset. Required by EDDY for modeling the diffusion signal. |
| b-vectors File (.bvec) | A text file listing the diffusion gradient direction vector for each volume. EDDY uses this and can output a rotated version (*.rotated_bvecs) to maintain consistency after motion correction [31]. |
| Acquisition Parameters File (acqparams.txt) | A text file defining the phase-encoding vector and total readout time for each volume input to TOPUP and EDDY. Critical for accurate distortion modeling [31] [30]. |
| Index File (index.txt) | A text file with one entry per diffusion volume, indicating which line of acqparams.txt describes its acquisition. Links the full dataset to the acquisition parameters [31]. |
| Brain Mask | A binary 3D image defining the brain region. Generated from the undistorted b0 output of TOPUP using BET. Cruishes processing speed and accuracy of EDDY by restricting calculations to the brain [31] [32]. |
Frequently Asked Questions (FAQs)
Q1: What are M1 and M2 motion-compensated diffusion gradients? M1 and M2 are advanced diffusion gradient schemes designed to nullify the effects of subject motion during Diffusion Tensor Imaging (DTI). The standard Stejskal-Tanner (M0) gradient only nulls the zeroth-order gradient moment, making it sensitive to any tissue movement. First-order (M1) motion-compensated gradients null both the zeroth and first-order moments, making them robust to spins moving at a constant velocity. Second-order (M2) gradients null the zeroth, first, and second-order moments, providing compensation for spins experiencing constant acceleration [2] [3].
Q2: In which research applications are these schemes most crucial? These motion-compensated schemes are particularly valuable in populations where movement is involuntary, frequent, or continuous. This includes:
- Pediatric studies: Where children may have difficulty remaining still [34].
- Neurological disorders: Research involving patients with Parkinson's disease, stroke, or other conditions causing tremors or involuntary motions [2] [35].
- Cardiac diffusion imaging (cDTI): Where the inherent motion of the beating heart has traditionally made DTI exceedingly difficult [2] [36].
- Any study where subject cooperation is limited and the use of sedation is undesirable.
Q3: What is the main practical benefit of using M2 gradients over standard M0 gradients? The primary benefit is the significant reduction of signal dropout in the acquired diffusion-weighted images during motion. In a proof-of-principle study, continuous head motion corrupted up to 44% of images acquired with standard M0 gradients. In contrast, 0% of the images acquired with M2 gradients were corrupted by signal dropout under the same motion conditions [2] [3].
Q4: Can I combine motion-compensated gradients with retrospective software correction? Yes, these methods can be complementary. However, the same study showed that for severe motion (corrupting >15% of DW images), retrospective software corrections applied to M0 data failed to produce consistent DTI parameters. Meanwhile, M2 data alone, even without advanced retrospective correction, yielded parameters consistent with motion-free reference data [2]. This suggests that M2 gradients address the motion problem at the acquisition level, providing a more robust foundation.
Q5: Do M1/M2 gradients compromise image quality when no motion is present? No. Research confirms that in the absence of motion, DTI parameters (like Fractional Anisotropy and Mean Diffusivity) calculated from M0, M1, and M2 data are consistent with each other. This indicates that using these advanced schemes does not introduce biases or degrade data quality in motion-free scenarios [2].
Troubleshooting Guide
| Problem | Possible Cause | Solution |
|---|---|---|
| Persistent ghosting/geometric distortions in DWI. | Eddy currents induced by strong, switched diffusion gradients, especially problematic at high field strengths (e.g., 7T). | Consider sequences with optimized navigator echoes (e.g., Nav2) placed after diffusion gradients and the use of dummy diffusion gradients to precondition the gradients and mitigate eddy currents [23]. |
| Blurring or artifacts in multishot DTI acquisitions. | Shot-to-shot phase variations due to physiological motion (e.g., cardiac pulsation, respiration). | Implement a navigator-based prospective motion correction that tracks head position and updates the imaging coordinate system in real-time [34]. |
| Residual motion artifacts despite using M1 gradients. | M1 gradients are only immune to constant velocity. Complex motion (e.g., acceleration) in patients can still cause artifacts. | Upgrade to M2 motion-compensated gradients, which are designed to null the effects of acceleration, providing a higher level of motion immunity [2] [3]. |
| Low signal-to-noise ratio (SNR) in DTI data. | General challenge in DWI; motion compensation does not directly address intrinsic SNR limitations. | Employ parallel imaging (e.g., SENSE, GRAPPA) and simultaneous multi-slice (SMS) acquisition techniques to improve SNR efficiency and reduce scan time [37]. |
Quantitative Performance Data
The following table summarizes key quantitative findings from a study directly comparing M0, M1, and M2 diffusion gradient schemes during continuous head motion [2] [3].
Table 1: Comparison of Motion Compensation Gradient Performance During Continuous Head Motion
| Metric | Standard M0 Gradients | First-Order (M1) Gradients | Second-Order (M2) Gradients |
|---|---|---|---|
| Theoretical Compensation | Zeroth-order moment (position) | Zeroth & First-order moments (position & velocity) | Zeroth, First, & Second-order moments (position, velocity, & acceleration) |
| % of Corrupted DW Images (Study 0) | 44% | 7% | 0% |
| % of Corrupted DW Images (Study 2) | 39% | Not Acquired | 0% |
| Consistency of DTI parameters with reference (no-motion) data | Poor (parameters elevated) | Good (after retrospective correction) | Excellent (consistent without specialized correction) |
| Efficacy of Retrospective Motion Correction (e.g., FSL eddy) | Ineffective when >15% of images are corrupted | Improved correction; reduced dropout to 1% | Not required for parameter consistency |
Experimental Protocols
Protocol: Validating M2 Motion-Compensated Brain DTI
This protocol is adapted from a published proof-of-principle study demonstrating the feasibility of M2 gradients for brain DTI during gross motion [2] [3].
1. Hardware and Software Setup
- Scanner: Clinical 3T MRI system (e.g., Siemens Prisma).
- Coil: A 32-channel head coil.
- Sequence: Diffusion-prepared echo-planar imaging (EPI) with integrated M0, M1, and M2 motion-compensating diffusion gradient schemes [2].
- Software: Post-processing pipeline including FSL (for
eddymotion correction anddtifitfor tensor fitting) and ANTs for image registration [2].
2. Key Acquisition Parameters
- TR/TE: 12600/89 ms
- Field of View (FOV): 220 x 220 mm²
- Matrix: 110 x 110
- Spatial Resolution: 2 mm isotropic voxels (60 slices)
- Diffusion Weighting: 30 volumes at b=1000 s/mm², 4 volumes at b=0
- Acquisition Time: ~7 minutes 46 seconds per scheme (M0, M1, M2)
3. Subject and Motion Paradigm
- Subjects: Scan healthy volunteers under two conditions:
- No-Motion Condition: Subject instructed to remain still.
- Motion Condition: Subject performs continuous head motion, such as approximately 20° periodic rotation around the spine axis at a frequency of ~1 Hz.
- Data Acquisition: Acquire full DTI datasets for each gradient scheme (M0, M1, M2) in both motion and no-motion conditions.
4. Data Processing and Analysis
- Preprocessing: Correct all datasets for motion and eddy current artifacts using
eddyin FSL. - Tensor Fitting: Generate Fractional Anisotropy (FA), Mean Diffusivity (MD), Longitudinal Diffusivity (LD), and Transverse Diffusivity (TD) maps using
dtifit. - Analysis:
- Visual Inspection: Qualitatively assess signal dropout in individual diffusion-weighted images.
- Voxelwise Comparison: Coregister all parameter maps to a common space and compute density plots of per-voxel differences between motion-corrected and reference (no-motion M0) data.
- Quantitative Validation: Compare the consistency of DTI parameters derived from motion-M0, motion-M1, and motion-M2 data against the reference.
Visual Workflow: Motion Compensation Strategy Selection
The following diagram illustrates the logical decision process for selecting a motion mitigation strategy in DTI research, based on the nature of the expected motion.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential "Reagents" for Motion-Compensated DTI Experiments
| Item | Function in the Experiment |
|---|---|
| M1/M2 Motion-Compensated Gradient Sequences | The core pulse sequence modification that nulls first and second-order gradient moments to make the acquisition inherently robust to tissue motion [2] [3]. |
| Prospective Motion Correction (Navigators) | Short, volumetric navigator pulses (e.g., 3D-EPI) acquire real-time head pose data. This information is used to update the imaging FOV and gradient orientation during the scan, maintaining anatomical consistency [34]. |
| Eddy Current Mitigation Toolkit | A combination of dummy diffusion gradients and strategically placed navigator echoes (e.g., Nav2) to precondition the scanner's gradients and correct for phase errors induced by eddy currents, crucial for high-field DTI [23]. |
| Post-Processing Software (FSL, ANTs) | Software packages for retrospective correction, tensor fitting, and image registration. They are used for quantitative comparison of DTI parameters (FA, MD) between different gradient schemes [2] [34]. |
| Advanced Diffusion Models (IVIM, DKI) | Multi-compartment diffusion models (e.g., Intravoxel Incoherent Motion, Diffusion Kurtosis Imaging) that can be combined with motion-compensated acquisitions to probe more complex microstructural properties beyond the standard tensor model [37]. |
Diffusion Tensor Imaging (DTI) is a valuable neuroimaging technique for assessing white matter connectivity and integrity non-invasively. However, its accuracy is compromised by several physical artifacts, primarily caused by eddy currents and magnetic susceptibility (B0) effects. These artifacts manifest as geometric distortions, image blurring, and misregistration between diffusion-weighted images, leading to significant errors in derived diffusion metrics like Fractional Anisotropy (FA) and in fiber tractography results. This guide provides troubleshooting and methodologies for integrated correction of these concomitant distortions within the broader context of mitigating artifacts in DTI research [38] [8].
Frequently Asked Questions (FAQs)
1. What are the main sources of distortion in DTI data?
The primary sources are eddy currents and B0 inhomogeneity. Eddy currents are induced by the rapid switching of strong diffusion-weighting gradients, causing image stretching or shearing that varies with the diffusion direction (d) and time (t): B0eddy(x, t, d). Magnetic susceptibility artifacts (B0) arise from static field inhomogeneities at tissue-air interfaces (e.g., near the sinuses), causing geometric distortions that are spatial but constant in time: B0susc(x). Both artifacts are exacerbated by the use of Echo-Planar Imaging (EPI), a common DTI acquisition sequence [38] [39].
2. Why can't I use a single, static B0 map to correct all my diffusion volumes?
A static B0 map, typically acquired without diffusion weighting, accurately models B0susc(x) but does not account for the additional, dynamic magnetic field distortions created by B0eddy(x, t, d) when diffusion gradients are applied. Using only a static map leaves eddy-current-induced distortions uncorrected, which can be substantial and vary across different diffusion-weighted images [40].
3. My data has severe signal dropout from subject motion. What are my options? Beyond prospective methods like physical restraint, two key approaches exist:
- Retrospective Correction with Outlier Replacement: Software like FSL's
eddycan detect and replace corrupted slices or volumes [2]. - Motion-Compensated Gradient Schemes: Using first-order (M1) or second-order (M2) motion-compensated diffusion gradients can inherently reduce phase accumulation from bulk head motion, dramatically decreasing signal dropout. Studies show M2 gradients can reduce the number of corrupted images from 44% to 0% during continuous motion [2].
4. Are there acquisition strategies that correct for both distortion types simultaneously?
Yes, advanced sequences are designed for this purpose. The RPG-MUSE technique integrates Reversed Polarity Gradients (RPG) into a multi-shot EPI acquisition. By alternating the phase-encoding direction between shots, it allows for the inherent estimation of a combined distortion map (ΔB) that includes both B0susc and B0eddy for each diffusion volume, without increasing scan time [40].
5. What software tools are available for distortion correction? Several established software packages offer processing pipelines. The table below summarizes key tools and their capabilities [41].
Table 1: Software Tools for DTI Processing and Artifact Correction
| Software Package | Pre-processing | Tensor Estimation | Fiber Tracking | Registration |
|---|---|---|---|---|
| FSL | Yes | Yes | Yes | Yes |
| Camino | Yes | Yes | Yes | Yes |
| DTI-TK | Yes | Yes | ||
| AIR | Yes | Yes | ||
| JIST | Yes | Yes | Yes | |
| TORTOISE | Yes | Yes |
Detailed Experimental Protocols
Protocol 1: Dynamic B0 and Eddy Current Mapping and Correction
This protocol measures the exact spatial, temporal, and diffusion-direction dependence of the artifact-inducing magnetic fields [38].
1. Objective: To dynamically measure and correct for B0susc(x) and B0eddy(x, t, d).
2. Materials and Methods:
- Phantom: A standardized MRI phantom.
- Pulse Sequence: Multiecho spin-echo pulse sequence.
- Key Acquisition Parameters:
- Acquire a series of diffusion-weighted asymmetric spin-echo images at different time points (τ₁, ..., τₘ) spanning the DTI readout window (
T_acq). - Acquire data for each diffusion-weighting (DW) direction (
d) used in the main DTI scan. - For
B0eddymapping, perform this on the phantom once per DTI protocol. ForB0suscmapping, perform in vivo without diffusion-weighting.
- Acquire a series of diffusion-weighted asymmetric spin-echo images at different time points (τ₁, ..., τₘ) spanning the DTI readout window (
3. Data Processing Steps:
- Dynamic B0eddy Mapping (Phantom):
- For each time point
τ_mand DW directiond, fit the phase images from multiple echoes to the equation:φ(x,t,d) = φ₀(x,τ_m,d) + γB0eddy(x,τ_m,d)t[38]. - Subtract a non-diffusion-weighted B0 map of the phantom to isolate the eddy-current-induced field.
- Fit the resulting
B0eddymaps with a third-order polynomial function in space and extrapolate.
- For each time point
- Static B0susc Mapping (In Vivo):
- Using the same sequence without diffusion-weighting, fit all echoes to
φ(x,t) = φ₀(x) + γB0susc(x)tto derive a high-resolution static field map [38].
- Using the same sequence without diffusion-weighting, fit all echoes to
- Dynamic Image Correction:
- For each time point
t_nin the DTI EPI acquisition (corresponding to each k-space line) and each DW directiond, calculate the total phase error:φ(x,t_n,d) = γ ∫_{TE}^{t_n} [B0susc(x) + B0eddy(x,t,d)] dt[38]. - Multiply the uncorrected DTI image by
exp[-iφ(x, t_n, d)]. - Fourier transform each of these N images to k-space, extract the corresponding k-space line from each to form a new, corrected k-space, and then inverse Fourier transform to get the final corrected image [38].
- For each time point
Protocol 2: Correction Using Phase-Encoding Reversal (COVIPER)
This method corrects for vibration-induced artifacts, which are a specific type of eddy-current-related effect, by combining data from two phase-encoding directions [42].
1. Objective: To mitigate signal dropout in DWI caused by scanner vibration.
2. Materials and Methods:
- Pulse Sequence: A DTI sequence capable of acquiring data with reversed phase-encoding directions (blip-up/blip-down).
- Key Acquisition Parameters:
- Acquire two complete DTI datasets with identical parameters except for the phase-encoding (PE) direction (e.g., Anterior-Posterior "blip-up" and Posterior-Anterior "blip-down") [42].
3. Data Processing Steps:
- Preprocessing: Correct both datasets for motion and eddy currents (e.g., using FSL's
eddy). Correct for susceptibility-induced geometric distortion using a voxel displacement map derived from a B0 field map [42]. - Tensor Fit Error Calculation: Calculate the diffusion tensor (
D) and the residual error of the tensor fit (ε) for both the blip-up and blip-down datasets independently [42]. - Weighted Combination: For each voxel, combine the apparent diffusion coefficients (ADCs) from the two datasets using a local weighted-sum approach. The weighting
w(r)is a Lorentzian function of the normalized tensor-fit errorx(r)[42]:ADC_combined(r) = w_up(r) * ADC_up(r) + w_down(r) * ADC_down(r)w(r) = 1 / (1 + x²(r))wherex(r) = ||ε(r)|| / normalization_factor
The workflow for an integrated correction pipeline combining multiple techniques is illustrated below.
Diagram 1: Integrated DTI Correction
Comparison of Correction Methods
Table 2: Summary of DTI Distortion Correction Methods
| Method | Key Principle | Corrects B0 | Corrects Eddy Currents | Advantages | Limitations |
|---|---|---|---|---|---|
| Dynamic B0 Mapping [38] | Directly measures B0eddy(t,d) and B0susc via field mapping. |
Yes | Yes (time-varying) | High fidelity; models temporal variation. | Requires specialized acquisition; longer setup. |
| Reversed PE (RPG-MUSE) [40] | Alternates phase-encode direction to estimate combined ΔB map. |
Yes | Yes | No scan time penalty; dynamic correction. | Requires multi-shot EPI sequence. |
| Non-linear Registration [39] | Warps DTI (B0) volume to match undistorted anatomical (e.g., T1) volume. | Yes | No (assumes static) | Uses standard sequences; no extra scan time. | Does not correct eddy currents; registration challenges. |
| Motion-Compensated Gradients [2] | Uses M1/M2 gradients to null phase accumulation from motion. | No | Mitigates effects | Dramatically reduces signal dropout from motion. | May require sequence programming; not for all scanners. |
| Post-processing (FSL eddy) [2] | Affine registration of DWIs to B0 image. | No | Yes (assumes static) | Widely available; standard in many pipelines. | Assumes eddy currents are constant during readout. |
The Scientist's Toolkit
Table 3: Essential Research Reagents and Solutions for DTI Artifact Correction
| Item | Function / Explanation |
|---|---|
| MRI Phantom | A standardized object used to characterize scanner-specific eddy current fields (B0eddy) for a given protocol, allowing for prospective correction [38]. |
| FSL Software Library | A comprehensive software library containing topup (for susceptibility correction) and eddy (for eddy current and motion correction), which are industry standards [2] [41]. |
| B0 Field Mapping Sequence | A specialized MRI pulse sequence (e.g., dual-echo gradient echo) used to acquire a voxel displacement map, which is essential for quantifying and correcting B0 inhomogeneity [42]. |
| Motion-Compensated Diffusion Gradients | Modified gradient waveforms (e.g., M2) that null first and second-order gradient moments, reducing phase accumulation from bulk motion and thus minimizing signal dropout [2]. |
| Reversed Phase-Encoding (RPG) Data | Paired datasets (blip-up/blip-down) that encode opposite spatial distortions, enabling highly accurate estimation of the total distortion field when combined [42] [40]. |
Optimizing the DTI Pipeline: Best Practices for Data Quality and Reliability
Troubleshooting Guides and FAQs
FAQ: Motion Artifact Correction Fundamentals
Q1: What are the primary sources of artifacts in diffusion MRI data?
Diffusion MRI data are susceptible to a range of artifacts more than many other common MRI techniques. The primary sources include:
- Image distortions due to magnetic field (B0) inhomogeneities caused by the subject's head (susceptibility artifacts).
- Image distortions due to eddy currents caused by rapid switching of diffusion-encoding gradients.
- Subject movement, which changes the location of the object within the field of view.
- Signal dropout caused by bulk motion (subject movement or cardiac pulsation) during the diffusion encoding part of the imaging sequence [43].
Q2: What is the difference between inter-volume and intra-volume motion, and why does it matter for correction?
- Inter-volume motion occurs between the acquisition of entire diffusion-weighted volumes. Most conventional motion correction methods only address this type of movement.
- Intra-volume motion occurs during the acquisition of a single volume, that is, between the acquisition of individual slices. Traditional methods assume the subject remains still during this time, which is often an approximation [44]. The distinction matters because intra-volume motion cannot be corrected by simple volume-to-volume alignment. Ignoring it leads to residual artifacts even after "perfect" inter-volume motion correction, reducing the accuracy of derived parameters like Fractional Anisotropy (FA) [44].
Q3: How can I automatically assess the quality of my diffusion data, particularly for color Fractional Anisotropy (CFA) maps?
Automated assessment can be performed by analyzing the color cast in CFA images. In a properly acquired dataset without significant motion, the colors in the CFA map (representing the primary diffusion direction) should be heterogeneous. A dominant, unnatural tint across the entire image (a color cast) indicates potential motion corruption. This can be quantified by calculating distribution statistics of the 2D histogram in a color-opponent space like CIELAB [45].
Troubleshooting Guide: Common Preprocessing Problems
Q1: My dataset has severe signal dropout in several slices. What strategies can I use?
A framework integrating outlier detection and replacement can be highly effective [43].
- Detection: Identify slices affected by significant signal loss. This can be achieved without relying on a specific biophysical model by comparing a generative model of the data to the observed slices.
- Replacement: Once detected, replace the corrupted slices with a non-parametric prediction. This prediction is a linear combination of angularly neighboring measurements in q-space for the same anatomical slice.
- Efficacy: This method shows high sensitivity and specificity. When the affected slices constitute no more than 10% of the total data, it can almost completely correct the deleterious effects on standard metrics like FA and Mean Diffusivity (MD) [43].
Q2: After standard volume-based motion correction, I still see motion artifacts. What is the likely cause and solution?
The likely cause is intra-volume motion. Standard volume-based correction cannot address movement that happens between slice acquisitions within a single volume [44]. Solution: Implement a slice-to-volume motion correction framework. This models movement as a piecewise continuous function over time, effectively performing motion correction at the temporal resolution of slice acquisition rather than volume acquisition. Studies show this approach significantly increases the fidelity of scalar parameters like FA and improves alignment with data from a subject lying still [44].
Q3: For my fetal or neonatal DTI study, the 3D volumes are heavily corrupted by inter-slice motion. How can I reconstruct a usable 3D volume?
Slice-to-Volume Reconstruction (SVR) is designed specifically for this challenge.
- Process: This technique treats the stack of acquired 2D slices as multiple, low-resolution samplings of an underlying high-resolution 3D volume. It solves an inverse problem to reconstruct this volume.
- Robustness: For best results, use a robust M-estimation framework that minimizes an error norm function between the model-generated slices and the acquired slices. This makes the process less sensitive to motion-corrupted slices and mis-registrations that inevitably occur [46].
- Advanced Methods: Emerging techniques use Implicit Neural Representations (INRs) to model the 3D volume as a continuous function, simultaneously addressing motion correction, outlier handling, and super-resolution reconstruction in a unified framework [47].
Table 1: Performance Comparison of Motion Correction Pipelines (Based on [19])
| Motion Correction Pipeline | Data Acquisition Method | Key Finding | Impact on Tractography |
|---|---|---|---|
| FSL (Retrospective) | Standard (no navigator) | Improved ellipsoid fits over uncorrected data. | Increased sensitivity and specificity of group tractographic results. |
| TORTOISE (Retrospective) | Standard (no navigator) | Improved ellipsoid fits over uncorrected data. | Increased sensitivity and specificity of group tractographic results. |
| Prospective (vNav) + FSL | Navigated (real-time correction) | Further improvement in ellipsoid fits and WM map matches. | Highest sensitivity and specificity in group results among tested FSL pipelines. |
| Prospective (vNav) + TORTOISE | Navigated (real-time correction) | Highest match with anatomical white matter maps throughout the brain. | Highest sensitivity and specificity in group results among all tested pipelines. |
Table 2: Efficacy of Outlier Detection and Replacement (Based on [43])
| Metric | Performance Finding | Notes / Constraints |
|---|---|---|
| Outlier Detection | High sensitivity and specificity achieved. | Method is non-parametric and integrated with distortion correction. |
| Correction of FA/MD | Deleterious effects on FA and MD "almost completely corrected." | Effective as long as corrupted slices constitute ≤10% of total data. |
| Replacement Data | Uses a non-parametric prediction from angularly neighboring q-space measurements. | Prediction contains no "new information" but minimizes impact on downstream analysis. |
Experimental Protocols
Protocol 1: Integrated Framework for Distortion, Motion, and Dropout Correction
This protocol is adapted from methods designed for comprehensive correction of dMRI artifacts [43] [44].
- Data Acquisition: Acquire diffusion data with pairs of volumes that have opposite phase-encoding directions (e.g., AP-PA). This is crucial for subsequent distortion correction.
- Outlier Detection:
- Model the expected image based on a generative model (e.g., a Gaussian process) using all non-outlier data.
- Compare each acquired slice to this model.
- Label a slice as an outlier if the discrepancy exceeds a defined threshold based on a robust summary statistic.
- Outlier Replacement:
- Replace the identified outlier slices with a non-parametric prediction.
- This prediction, ( \hat{yi}(xi|y{-i}) ), is an estimate of the corrupted data point ( yi ) conditioned on all other non-outlier data points ( y_{-i} ) in q-space.
- Joint Correction:
- Within a single framework, estimate and correct for susceptibility-induced distortions and eddy current-induced distortions.
- Simultaneously, estimate subject movement. For full efficacy, this should model intra-volume movement as a piecewise continuous function over time (slice-to-volume registration) rather than assuming one rigid transformation per volume [44].
- Output: A fully corrected set of diffusion-weighted images ready for tensor estimation or other modeling.
Protocol 2: Robust Super-Resolution Slice-to-Volume Reconstruction
This protocol is for creating high-resolution 3D volumes from motion-corrupted 2D slices, common in fetal and neonatal imaging [46].
- Data Acquisition: Acquire multiple stacks of fast (e.g., SSFSE) 2D slices in different orientations (e.g., axial, coronal, sagittal). These slices have high in-plane resolution but are thick and suffer from inter-slice motion.
- Formulate the Acquisition Model: Model the relationship between the desired high-resolution volume ( x ) and the acquired slices ( yk ) as:
( yk = Dk Bk Sk Mk x + vk )
where:
- ( Mk ) is the 3D rigid transformation for slice ( k ).
- ( Sk ) is the slice selection operator.
- ( Bk ) represents the blurring due to the slice profile.
- ( Dk ) is the downsampling operator.
- ( vk ) is noise.
- Reconstruction as Inverse Problem: Solve for the underlying volume ( x ) by minimizing the error between the model-generated slices and the actually acquired slices.
- Robust Error Norm Minimization: Use a robust M-estimator (e.g., Lorentzian, Geman-McClure) instead of a standard least-squares (l2-norm) minimizer. This reduces the influence of severe outliers (mis-registered or corrupted slices) on the final reconstruction.
- Reconstruction: Iterate between estimating the slice transformations ( M_k ) and updating the high-resolution volume ( x ) until convergence.
Workflow and Signaling Pathway Diagrams
Diagram 1: Comprehensive dMRI Artifact Correction Pipeline
Integrated Correction Workflow
Diagram 2: Slice-to-Volume Reconstruction with Robust M-Estimation
Robust SVR Iteration Process
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Software Tools for Motion Artifact Mitigation
| Tool / Solution Name | Type | Primary Function | Key Application / Note |
|---|---|---|---|
FSL eddy [43] [19] |
Software Tool | Joint correction of eddy currents, movement, and signal dropout. | Widely adopted; integrates outlier detection and replacement. |
| TORTOISE [19] | Software Tool | Retrospective correction for motion, eddy currents, and EPI distortion. | Often used in comparison studies; shows high performance when combined with prospective correction. |
| Prospective Motion Correction (vNav) [19] | Acquisition Sequence / Technique | Real-time motion tracking and correction during data acquisition. | Uses a 3D EPI navigator to update scanner coordinates; reduces motion before post-processing. |
| SLOMOCO (mSLOMOCO) [48] | Software Pipeline | Intravolume motion correction for fMRI/2D EPI data. | Addresses slice-level motion and spin-history effects; can be adapted for dMRI. |
| Robust Super-Resolution SVR [46] | Algorithmic Framework | Reconstructs high-resolution 3D volumes from motion-corrupted 2D slices. | Essential for fetal and neonatal imaging; uses robust M-estimation to handle outliers. |
| Implicit Neural Representations (INRs / NeSVoR) [47] | Emerging Methodology | Continuous representation for SVR; jointly learns motion correction and SR. | Reduces reconstruction time; promising for severe motion cases; active research area. |
| Color Cast Analysis [45] | Quality Assessment Metric | Automated quality assessment of CFA images to detect motion. | Provides a quantitative, objective measure for data quality assurance. |
Diffusion Tensor Imaging (DTI) is an invaluable tool for presurgical planning and the early detection of neurodegenerative diseases, as it enables the reconstruction of white matter pathways and provides enhanced insights into brain connectivity [14]. However, its utility is significantly hindered by two fundamental types of errors: stochastic errors from noise and systematic errors from imperfections in the magnetic field gradients and artifacts [14] [49]. These errors disrupt the visualization of critical anatomical details necessary for understanding brain function and disorders.
Individually, denoising and systematic error correction provide partial solutions. The true breakthrough in data quality emerges when these techniques are combined synergistically. This approach simultaneously addresses both random and systematic error sources, leading to more accurate and biologically relevant DTI metrics and tractography [14] [49]. This technical support center guide provides researchers with the practical knowledge to implement this powerful combined approach.
Frequently Asked Questions (FAQs)
Q1: Why should I combine denoising with systematic error correction instead of using just one method?
These techniques target different, complementary sources of error. Denoising methods primarily reduce random, stochastic noise (e.g., thermal noise) [50] [51], while systematic error corrections, like the B-matrix Spatial Distribution (BSD) method, address physical imperfections in the MRI scanner's gradient fields [14] [49]. Using only one leaves the other error source unchecked. Research shows that their combined use leads to significant improvements in Fractional Anisotropy (FA) and Mean Diffusivity (MD) measures, as well as overall tractography quality, that are greater than either method alone can provide [14].
Q2: Will denoising alter or remove genuine biological signals from my data?
A primary goal of modern denoising algorithms is to preserve structural information while removing noise. Methods like Structure-Adaptive Sparse Denoising (SASD) are explicitly designed to achieve a good trade-off between image smoothness and the preservation of fine structures and edges [50]. Furthermore, a 2025 study on glaucoma patients found that while denoising improved image quality and reduced residuals in model fitting, it had a limited impact on the core tractometry metrics used to distinguish patients from controls, suggesting it does not fundamentally alter the key biological signals of interest [51].
Q3: In what order should I apply these preprocessing steps?
The established effective order is to first apply denoising, then correct for other artifacts like Gibbs ringing, and finally apply systematic error correction such as the BSD method [49]. This sequence allows the BSD method to work on data where stochastic noise has already been reduced, thereby improving its effectiveness in correcting gradient-related biases [14] [49].
Q4: Can these techniques correct for severe motion artifacts?
While denoising and BSD correction improve general data quality, they are not a complete solution for severe subject motion. For motion artifacts, specialized methods are required. Deep learning models like Res-MoCoDiff, which use efficient diffusion processes to correct motion corruption, have shown superior performance in removing motion artifacts while preserving fine structural details [52]. Furthermore, understanding motion-sampling interactions through frameworks like motion-sampling plots is crucial for predicting and mitigating these artifacts [53].
Q5: What is the practical impact on my tractography results?
Correcting systematic errors leads to more accurate fiber pathways. One study demonstrated that the direction of the first eigenvector—which dictates tractography direction—differed by an average of 10 degrees after applying denoising, Gibbs ringing removal, and BSD correction, compared to data that only had denoising and Gibbs ringing removal [49]. This indicates a substantial improvement in the accuracy of tracked neural pathways solely attributable to the correction of systematic gradient errors.
Troubleshooting Guides
Guide 1: Addressing Inaccurate Fractional Anisotropy (FA) Values
Problem: FA values in isotropic phantoms are significantly above zero, or show unrealistic variations across different brain regions.
Solution: This is a classic sign of unresolved systematic errors.
- Apply a robust denoising method. Local PCA has been shown to deliver the lowest FA in isotropic phantoms, outperforming other methods like non-local means or simple Gaussian blurring [49].
- Incorporate Gibbs ringing removal. The Gibbs phenomenon can artificially inflate DTI metrics. Removing it is a crucial step before final tensor calculation [49].
- Implement BSD correction. This step calibrates the diffusion gradient field, which is a major source of systematic bias. Studies on isotropic phantoms show that the combination of denoising and BSD correction can lead to a dramatic decrease in FA (e.g., up to -90%), bringing it much closer to the expected ground truth [49].
Guide 2: Improving Fiber Tractography Quality and Consistency
Problem: Tractography results show unnaturally short fibers, poor density, or biologically implausible directions.
Solution: Enhance the fidelity of the underlying diffusion tensor field.
- Ensure high-quality denoising. Use a structure-adaptive method like SASD, which preserves edges and fine structures crucial for tracking pathways through complex regions [50].
- Verify the preprocessing pipeline. Follow the sequence: Denoising → Gibbs ringing removal → BSD correction [49]. This pipeline has been proven to improve fiber tract density, length, and direction.
- Quantitatively check the first eigenvector. As reported, the first eigenvector direction can shift significantly after full preprocessing. This change directly translates to more anatomically accurate fiber tracking [49].
Guide 3: Managing Residual Motion Artifacts Post-Correction
Problem: Despite denoising and BSD correction, images still show ghosting or blurring from subject motion.
Solution: Integrate a dedicated motion correction tool.
- Consider image-domain deep learning models. If raw k-space data is unavailable, models like Res-MoCoDiff operate directly on magnitude images. They are designed as efficient, "off-the-shelf" solutions that can be integrated into clinical workflows without scanner-specific modifications [52].
- Evaluate the correction performance. Use quantitative metrics such as Peak Signal-to-Noise Ratio (PSNR), Structural Similarity Index Measure (SSIM), and Normalized Mean Squared Error (NMSE) to validate the effectiveness of the motion correction [52] [54].
- Understand the artifact source. Use frameworks like motion-sampling plots to predict the severity and nature of artifacts based on the interaction between the specific head motion and the k-space sampling trajectory used in your acquisition [53].
Experimental Protocols & Workflows
Protocol 1: Combined Preprocessing for DTI Metric Accuracy
This protocol is designed to maximize the accuracy of quantitative DTI metrics like FA and MD.
Step-by-Step Methodology:
- Data Acquisition: Acquire DWI data using a standard single-shot EPI sequence with multiple diffusion-encoding directions. Include multiple b=0 s/mm² volumes.
- Initial Denoising: Apply a patch-based denoising algorithm.
- Gibbs Ringing Removal: Use a dedicated algorithm (e.g., local subvoxel-shifts method) to suppress ringing artifacts at tissue interfaces [49].
- Standard Preprocessing: Correct for eddy currents and subject motion using a tool like FSL's EDDY [51].
- Systematic Error Correction (BSD): Apply the B-matrix Spatial Distribution method.
- Action: This involves replacing the single, vendor-supplied B-matrix with a spatially distributed B-matrix that is unique for each voxel, accounting for the non-uniformity of the magnetic field gradients [14] [55].
- Requirement: This step requires a prior calibration of the gradient field using a phantom [55].
- Tensor Fitting & Analysis: Recompute the diffusion tensor and derived metrics (FA, MD, eigenvectors) using the corrected B-matrices.
The workflow for this protocol is summarized in the diagram below:
Protocol 2: An Integrated Pipeline for High-Fidelity Tractography
This protocol builds on the previous one, optimizing the steps specifically for superior fiber tracking results.
Step-by-Step Methodology:
- Follow Steps 1-5 of Protocol 1. The combination of denoising and BSD correction is critical for producing an accurate tensor field [14] [49].
- Probabilistic Tractography: Use a probabilistic algorithm (e.g., implemented in FSL or MRTrix3) to generate streamlines from the corrected diffusion data.
- Automated Fiber Quantification (AFQ): Use the AFQ toolbox to automatically identify specific white matter tracts (e.g., optic radiations, corpus callosum) and compute tract profiles [51].
- Tract Profile Analysis: Analyze tissue properties (FA, MD, ICVF) at 100 equidistant nodes along the cleaned tract to create a tract profile [51].
The logical relationship of this pipeline is as follows:
The tables below consolidate key quantitative findings from recent studies, providing a clear overview of the performance gains achieved by combining denoising and systematic error correction.
Table 1: Impact on DTI Metrics in an Isotropic Phantom (Ground Truth: FA=0) [49]
| Preprocessing Method | Average FA Value | Reduction vs. Standard Method |
|---|---|---|
| Standard DTI (sDTI) | 0.0562 | Baseline |
| sDTI + Denoising + Gibbs Removal | ~0.0141 | ~75% |
| BSD + Denoising | ~0.0052 | ~90% |
Table 2: Impact on In-Vivo Human Brain Tractography [49]
| Preprocessing Scenario | Change in 1st Eigenvector Direction |
|---|---|
| Standard DTI vs. Standard DTI + Denoising + Gibbs + BSD | 56° |
| Standard DTI + Denoising + Gibbs vs. + BSD | 10° |
Table 3: Performance of a Deep Learning Motion Correction Model (Res-MoCoDiff) [52]
| Metric | Performance (Minor Distortions) |
|---|---|
| PSNR | 41.91 ± 2.94 dB |
| Inference Speed | 0.37 seconds per batch |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Tools for Advanced DTI Processing
| Item / Solution | Function | Example / Note |
|---|---|---|
| Local PCA Denoising | Reduces stochastic noise in DWI data while preserving structural information. | Identified as a top performer for minimizing FA bias in isotropic phantoms [49]. |
| BSD-DTI 2.0 Software | Calibrates the B-matrix to correct for systematic errors from gradient field non-uniformity. | Home-build software (NMR LaTiS, AGH-UST); requires gradient field calibration [55]. |
| Res-MoCoDiff Model | An efficient deep learning model for correcting motion artifacts in the image domain. | Operates on magnitude images; reduces inference time dramatically vs. conventional DDPMs [52]. |
| Isotropic & Anisotropic Phantoms | Used for scanner calibration and validation of DTI metrics. | Essential for pre-calibrating gradient fields for the BSD method [49] [55]. |
| Patch-Based Joint Reconstruction (PB-SENSE) | Accelerates acquisition by exploiting correlations across diffusion directions. | Enables high-quality images from highly undersampled data (acceleration factor of 5) [56]. |
Frequently Asked Questions (FAQs)
FAQ 1: Why is pediatric DTI data particularly challenging to acquire and analyze? Pediatric brains are not simply smaller adult brains; they are undergoing profound, non-linear developmental changes in both structure and function [57]. This inherent biological variability is compounded by practical challenges. Young children are often unable to remain still for prolonged scans, making the data highly susceptible to motion artifacts. Furthermore, the lack of large, high-quality, annotated pediatric imaging datasets makes it difficult to develop and validate robust AI models and analytical pipelines that are specific to this population [58].
FAQ 2: What does an "older-looking brain" or positive Brain Age Gap (BAG) indicate in a child? In children and adolescents, a brain-predicted age that is higher than chronological age (a positive BAG) is generally interpreted as a sign of accelerated brain maturation [57]. Studies have linked an older BAG in youth to certain conditions, including depression, psychosis, and general psychopathology [57]. However, interpreting BAG requires caution, as it is a global summary metric that may average out complex, region-specific developmental patterns [57].
FAQ 3: Is there a single best method for correcting motion artifacts in DTI? No, there is no single "winner" for motion correction [59] [19]. Evidence suggests that an integrated approach is most effective. Combining prospective motion correction (real-time tracking during data acquisition) with retrospective correction (using software like FSL or TORTOISE after data collection) provides the best results [19]. The optimal pipeline can also depend on your specific scanner capabilities and research question.
FAQ 4: Can I use a DTI protocol designed for adults on pediatric patients? It is not recommended. Pediatric DTI requires specifically designed protocols that account for a trade-off between scanning time, diffusion strength, and the number of diffusion directions [60]. Adult protocols may lead to biased results. Best practices for children include using opposite phase-encoding directions to correct for distortions and creating population-specific templates for improved image registration [60].
Troubleshooting Guides
Guide 1: Mitigating Head Motion Artifacts
Head motion is a primary source of artifact in DTI, and its effects can be more pronounced in pediatric and patient cohorts [61]. The following integrated strategy addresses this issue at multiple stages.
Step 1: Acquisition - Minimize Motion at the Source
- Reduce Scan Time: Shorten sequences to match the patient's ability to lie still. For young children, this may be critical.
- Use Prospective Motion Correction: If available, use a navigated (vNav) DTI sequence that tracks head position in real-time and updates the scanner gradients to correct for motion during the scan [19].
- Acquire Multiple b=0 Volumes: Intersperse several non-diffusion weighted (b=0) volumes throughout the acquisition. These serve as robust reference volumes for post-processing correction [7].
Step 2: Reconstruction - Apply Retrospective Corrections
- 3D Rigid-Body Realignment: Use tools like FSL's
eddy_corrector TORTOISE to align all diffusion-weighted volumes to a reference b=0 volume, correcting for rigid head motion [19] [7]. - Volume Rejection: For large motions, implement a criterion to identify and discard severely corrupted volumes before tensor fitting [7].
- b-Matrix Reorientation (Rotation): When the head rotates, the orientation of the diffusion gradients relative to the brain tissue changes. Correcting the b-matrix accordingly is essential for accurate tensor estimation [7].
- 3D Rigid-Body Realignment: Use tools like FSL's
Step 3: Quantification - Report Motion Metrics
- It is not common practice but is highly recommended to quantify and report head motion parameters for each subject [61]. This allows you to check for systematic differences in motion between patient and control groups, which could bias your results. Tools like FSL's
eddy_correctoutput displacement and rotation parameters that can be summarized per subject [61].
- It is not common practice but is highly recommended to quantify and report head motion parameters for each subject [61]. This allows you to check for systematic differences in motion between patient and control groups, which could bias your results. Tools like FSL's
The workflow below summarizes this multi-stage correction pipeline:
Guide 2: Correcting Vibration and Distortion Artifacts
Beyond patient motion, DTI is susceptible to system-level artifacts from gradient vibrations and magnetic field inhomogeneities [42] [62].
Symptom: Localized signal-loss patterns in diffusion-weighted images.
- Cause & Solution: This is often a vibration artifact caused by strong diffusion gradients exciting mechanical resonances in the scanner [42].
- Acquisition: Acquire two datasets with reversed phase-encoding (PE) directions (blip-up/blip-down).
- Correction: Use a method like COVIPER which combines the blip-up and blip-down images. It weights the contribution of each image at every voxel based on the local error of the diffusion tensor fit, effectively recovering signal lost in one of the acquisitions [42].
- Cause & Solution: This is often a vibration artifact caused by strong diffusion gradients exciting mechanical resonances in the scanner [42].
Symptom: Geometric stretching or compression of the brain image, often in the frontal regions.
- Cause & Solution: This is EPI distortion due to magnetic field (B0) inhomogeneities [62].
- Acquisition with Fieldmap: Acquire a fieldmap (e.g., a dual-echo gradient echo sequence) that directly measures the B0 field. Tools like FSL's
FUGUEcan then use this map to unwarp the distorted DTI data [62]. - Acquisition without Fieldmap: If a fieldmap is unavailable, the blip-up/blip-down method is again the best practice. Use FSL's
TOPUPtool to estimate the distortion field from the two opposing PE datasets and then apply the correction [62].
- Acquisition with Fieldmap: Acquire a fieldmap (e.g., a dual-echo gradient echo sequence) that directly measures the B0 field. Tools like FSL's
- Cause & Solution: This is EPI distortion due to magnetic field (B0) inhomogeneities [62].
The following workflow integrates the correction of these specific artifacts:
Comparison of DTI Analysis Methods
The table below summarizes different DTI analysis strategies evaluated by the OPTIMAL study for use in clinical trials, highlighting their performance in predicting dementia conversion across different cohorts [59].
Table 1: Performance of Different DTI Analysis Strategies in Predicting Dementia Conversion
| Analysis Method | Description | Key Strengths | Predicts Dementia in Severe SVD? | Predicts Dementia in Mild SVD? | Predicts Dementia in MCI? |
|---|---|---|---|---|---|
| MD Median | Conventional histogram measure of mean diffusivity in white matter. | Simple, widely understood metric. | Yes [59] | Not Specified | Yes [59] |
| PC1 | First principal component derived from multiple conventional DTI histogram measures. | Combines information from multiple DTI parameters for potentially better prediction. | Yes [59] | Yes [59] | Yes [59] |
| PSMD | Peak Width of Skeletonized Mean Diffusivity. | Fully automated, sensitive to white matter damage, good for large datasets. | Yes [59] | Yes [59] | Yes [59] |
| DSEG θ | Diffusion Tensor Image Segmentation, a unitary score for whole cerebrum changes. | Semi-automated, provides a single score for global change. | Yes [59] | Not Specified | Yes [59] |
| G-eff | Global Efficiency, a measure of brain network integrity from tractography. | Reflects the overall efficiency of the brain's structural connectivity network. | Yes [59] | Yes [59] | No [59] |
Note: SVD = Cerebral Small Vessel Disease; MCI = Mild Cognitive Impairment. "Not Specified" indicates the source did not explicitly report performance for that cohort [59].
Experimental Protocols
Protocol 1: DTI Acquisition for a Pediatric Cohort
This protocol is adapted from studies specifically designed for school-aged children, including those born preterm [60].
1. Scanner Setup:
- Sequence: Single-shot spin-echo EPI.
- Diffusion Encoding: Use a twice-refocused spin-echo diffusion scheme to minimize eddy current artifacts [19].
- Phase-Encoding: Acquire data in two separate runs with reversed phase-encoding directions (e.g., Anterior-Posterior and Posterior-Anterior). This is crucial for subsequent distortion correction with
TOPUP[60]. - Directions & Weighting: A minimum of 20-30 isotropically distributed diffusion directions with a b-value of 1000 s/mm² is recommended. Include multiple (e.g., 5) b=0 volumes interspersed throughout the acquisition [63] [7].
2. Motion Management Strategy:
- If available, enable prospective motion correction (vNav) to track and correct for head motion in real-time [19].
- Keep scanning time as short as possible to accommodate the child's attention and ability to remain still.
3. Data Preprocessing Pipeline:
- Step 1: Distortion Correction. Use FSL's
TOPUPto estimate the susceptibility-induced distortion field from the blip-up/blip-down data [60]. - Step 2: Motion & Eddy Current Correction. Use FSL's
eddy_correctoreddytool to correct for head motion and eddy current-induced distortions, incorporating the output fromTOPUP[60]. - Step 3: Tensor Fitting. Fit the diffusion tensor model to the corrected data to generate maps of fractional anisotropy (FA), mean diffusivity (MD), axial diffusivity (AD), and radial diffusivity (RD).
- Step 1: Distortion Correction. Use FSL's
4. Spatial Normalization & Analysis:
- Create a Study-Specific Template. For a pediatric population, a study-specific template generated from your own data can provide a better registration target than an adult atlas brain [60].
- Nonlinear Registration. Use tools like
TBSS(Tract-Based Spatial Statistics) or advanced tensor-based registration to align each subject's FA map to the study-specific template for voxel-wise group comparisons [60].
The Scientist's Toolkit
Table 2: Essential Software and Analytical Tools for DTI Research
| Tool Name | Primary Function | Brief Description & Role in Mitigating Artifacts |
|---|---|---|
| FSL | Comprehensive MRI data analysis suite. | Its tools TOPUP and eddy are industry standards for correcting EPI distortions and eddy currents, especially when using blip-up/blip-down data [19] [62]. |
| TORTOISE | Diffusion MRI preprocessing and analysis. | Provides an alternative pipeline for rigorous correction of motion, eddy currents, and EPI distortions. Studies show it can be highly effective, particularly when combined with prospective correction [19]. |
| Phase-Encoding Reversal (Blip-Up/Blip-Down) | Data acquisition strategy. | Not a software tool per se, but a critical acquisition protocol. It provides the raw data necessary for TOPUP and COVIPER to correct for EPI distortions and vibration artifacts [42] [60]. |
| Prospective Motion Correction (vNav) | Real-time motion correction during acquisition. | A sequence-based tool that tracks head motion and updates the scanner's coordinate system during the scan, proactively reducing motion artifacts before they are embedded in the data [19]. |
| COVIPER | Retrospective vibration artifact correction. | A specialized method that combines blip-up and blip-down images, weighted by local tensor-fit error, to recover signal loss caused by scanner vibration [42]. |
Frequently Asked Questions
Q1: What are the most common causes and appearances of motion artifacts in DWI/DTI? Motion artifacts in diffusion MRI primarily arise from head motion during the acquisition of diffusion-weighted volumes. This occurs because DTI sequences are highly sensitive to any movement due to the strong diffusion gradients employed [2] [64]. Common manifestations include:
- Signal Dropout: Sudden, severe movements can lead to complete signal loss in parts of the image, appearing as dark slices or patches [2] [65].
- Ghosting: Periodic motion, such as from pulsation or tremor, causes replicated copies of the brain structure along the phase-encoding direction [64] [66].
- Blurring: Slow, continuous drifts during acquisition can result in a general loss of image sharpness [64].
- Eddy Current Distortions: Motion can interact with imaging gradients, causing geometric distortions in the images [65].
Q2: Why is rigorous quality control especially critical for developmental or clinical populations? Head motion is often systematic and correlated with the population being studied. For instance, children, neonates, and patients with certain neurological disorders are more likely to move during a scan [2] [67] [68]. If not accounted for, this can introduce a systematic bias into the research findings. A spurious group difference might be observed that is actually driven by different levels of motion artifact rather than true underlying biology [69] [68]. One study found that including poor-quality data significantly attenuated the correlation between diffusion metrics and age in an adolescent cohort [68].
Q3: Can I still use data where a large number of DWI volumes are corrupted? Yes, but it requires specialized methods. Traditional processing can fail if a high percentage (e.g., 44% [2]) of volumes are corrupted. However, advanced techniques are being developed for this scenario:
- Deep Learning-Based Estimation: One approach uses a hierarchical convolutional neural network (H-CNN) to estimate diffusion parameters directly, demonstrating stable performance even when 70-90% of the data was rejected due to motion [69].
- Motion-Compensated Acquisition: Using second-order motion-compensated (M2) diffusion gradients at the acquisition stage can prevent signal dropout entirely, making the data robust to continuous motion [2].
Q4: What are the key automated metrics for quantifying DWI data quality? Automated quality control is essential for objective and high-throughput processing. Key metrics include [68]:
- Temporal Signal-to-Noise Ratio (TSNR): Best at differentiating poor data from good/excellent data.
- Voxel Intensity Outlier Count (e.g., MAXVOX): Identifies volumes with severe, localized artifacts and helps differentiate good from excellent data.
- Mean Relative Motion (MOTION): Quantifies the average head displacement across all volumes.
Troubleshooting Guides
Issue 1: Identifying and Classifying Motion Artifacts
Problem: You suspect motion corruption in your DWI dataset and need to systematically identify its type and severity.
Solution:
- Visual Inspection: Begin by visually inspecting your DWI volumes in a gradient-by-gradient and slice-by-slice manner. Look for the classic signs of signal dropout, ghosting, and blurring [65].
- Automated Quality Metrics: Run your data through an automated QC pipeline to calculate quantitative metrics. The following table summarizes the optimal thresholds for classifying data quality based on a large developmental study [68]:
Table 1: Automated Quality Metric Thresholds for DWI Data Classification
| Quality Classification | Key Differentiating Metric | Optimal Threshold | Primary Use |
|---|---|---|---|
| Poor | Temporal Signal-to-Noise Ratio (TSNR) | TSNR < Threshold* | Identify data with severe artifacts for exclusion or aggressive correction. |
| Good vs. Excellent | Maximum Voxel Outlier Count (MAXVOX) | MAXVOX > Threshold* | Differentiate between acceptable and high-quality data. |
Note: Specific threshold values are dataset-dependent and should be derived from a representative training sample [68].
- Use QC Tools: Leverage open-source tools like DTIPrep [65] [68], which pipelines checks for intensity artifacts, eddy current distortions, and motion.
Issue 2: Correcting for Residual Motion Effects in Parameter Estimation
Problem: After volumetric realignment, your derived diffusion metrics (like FA or MD) still show a dependence on the level of subject motion.
Solution: This indicates residual motion effects that require more advanced correction techniques.
Table 2: Methods for Mitigating Residual Motion Effects
| Method Category | Description | Key Advantage | Example |
|---|---|---|---|
| Data Rejection & Robust Fitting | Identifies and removes corrupted volumes before tensor fitting using iteratively reweighted least squares (IRLLS). | Reduces bias from severe outliers. | Standard in many pipelines; see [65]. |
| Deep Learning Estimation | Uses a neural network to estimate diffusion parameters directly, bypassing traditional model-fitting. | Minimal sensitivity to motion; performs well even with high data rejection rates [69]. | Hierarchical CNN (H-CNN) [69]. |
| Motion-Compensated Acquisition | Uses modified gradient waveforms (M1, M2) that are nulled to specific orders of motion (velocity, acceleration). | Prospectively mitigates signal dropout at the source [2]. | Second-order motion-compensated (M2) gradients [2]. |
| Deep Learning Image Reconstruction | Applies a deep learning model to reconstruct cleaner images from the raw k-space or image data. | Can enhance SNR and reduce artifacts without changing acquisition time [70]. | Vendor-provided solutions like AIR Recon DL [70]. |
Experimental Protocol for H-CNN-Based Correction [69]:
- Data Preparation: Acquire DWI data using your standard protocol. Apply any standard volumetric motion correction and eddy-current correction.
- Motion Assessment & Rejection: Use an automated tool (e.g., based on outlier detection) to identify and flag motion-corrupted DWI volumes.
- Model Application: Input the surviving DWI volumes into the pre-trained Hierarchical Convolutional Neural Network (H-CNN). The architecture is designed to learn spatial hierarchies of features from the brain data.
- Parameter Estimation: The H-CNN outputs the estimated diffusion parameter maps (e.g., for DKI or DTI), which have been shown to be more stable and less biased by residual motion compared to traditional methods like IRLLS.
Issue 3: Establishing a Reliable QC Protocol for a Vulnerable Population
Problem: You are designing a DTI study for a population prone to motion (e.g., neonates, young children) and need a protocol to ensure data integrity.
Solution:
- Acquisition Strategy:
- Segment the Acquisition: Divide a high-direction-count sequence (e.g., 96 directions) into 3-4 shorter segments [67]. This allows for a break or reacquisition if one segment is ruined by motion.
- Consider Motion-Compensated Gradients: If available, use M2-type diffusion gradients to inherently reduce signal dropout from motion [2].
- Quality Control Pipeline:
- Automated QC on Each Segment: Run each acquired segment through an automated QC tool (like DTIPrep) to check for severe artifacts immediately after acquisition [67].
- Standardize Direction Count: From each quality-passed segment, extract a standardized number of diffusion directions (e.g., 25) that are evenly distributed to ensure robust tensor estimation [67].
- Check for Residual Motion Bias: After processing, verify that your final diffusion metrics (FA, MD) do not show significant correlations with quantitative motion parameters (e.g., mean framewise displacement) [67].
The Scientist's Toolkit
Table 3: Key Research Reagents and Tools for DTI Motion Mitigation
| Item Name | Function/Brief Explanation | Example Use Case |
|---|---|---|
| DTIPrep | An open-source tool that automates a comprehensive QC pipeline for DWI data, checking for artifacts and correcting for eddy currents and motion [65]. | Standardized, high-throughput quality control for large-scale or multi-site studies [68]. |
| FSL eddy | A widely used tool for correcting for eddy currents and subject movement in DWI data. It includes options for outlier replacement to address severe signal dropout [2]. | Standard post-processing correction in most DTI studies. |
| Motion-Compensated Diffusion Gradients | Modified gradient waveforms (e.g., M1, M2) that are nulled to the 1st and 2nd-order moments of motion, reducing phase errors in moving spins [2]. | Imaging continuously moving subjects, such as in pediatric or certain patient populations [2]. |
| Hierarchical CNN (H-CNN) | A deep learning model for estimating diffusion parameters that is less sensitive to the biasing effects of residual motion after data rejection [69]. | Obtaining reliable parameter maps from datasets where a large number of DWI volumes had to be discarded. |
| AIR Recon DL | A vendor-provided, deep learning-based image reconstruction algorithm that can improve SNR and reduce noise in reconstructed images, including DTI [70]. | Enhancing image quality and the sensitivity to detect subtle white matter differences in clinical research [70]. |
Workflow Diagram
The following diagram illustrates a robust workflow for DTI data acquisition and processing that integrates multiple quality control and motion mitigation strategies.
Validating Correction Methods and Comparing Clinical Efficacy
Troubleshooting Guides and FAQs
FAQ 1: Why do we need phantoms for DTI, and what can they be used for? Diffusion phantoms serve as a stable, ground-truth reference to validate the stability and repeatability of diffusion MRI measurements over time. They are essential for:
- Technical Validation: Isolating and quantifying technical sources of variability, such as scanner-related noise or gradient coil heating, without the confounding influence of physiological factors present in human subjects [71].
- Multi-Scanner Harmonization: Assessing and mitigating differences in DTI metrics (like FA and MD) that arise from using different scanner models, software versions, or manufacturers in multi-center trials [72] [73].
- Protocol and Model Assessment: Providing a known standard to evaluate the performance and reproducibility of different diffusion models (e.g., DTI, DKI, NODDI) and analysis pipelines [71].
FAQ 2: Our multi-center study shows significant differences in DTI metrics between sites. Is this due to the scanners? It is a distinct possibility. Significant cross-scanner differences in DTI metrics like fractional anisotropy (FA) and longitudinal diffusivity (LD) have been documented, even when using harmonized protocols. One study found significant differences in these metrics between GE and Siemens scanners [72]. Furthermore, parameters like the signal-to-noise floor ratio (SNFR) can vary significantly between scanner models and are critical to assess when comparing studies from different platforms [72]. Implementing a phantom-based quality assurance program, like monthly ACR phantom scans, can help monitor this inter-scanner variability [73].
FAQ 3: What is the best way to correct for motion artifacts in DTI data? A combined approach is often most effective. Research indicates that using both prospective (real-time) motion correction during data acquisition and retrospective correction during data processing provides the most robust results [19].
- Prospective Correction: Uses real-time motion tracking (e.g., with volumetric navigators) to update scan parameters during acquisition, preventing motion from occurring in the first place [19].
- Retrospective Correction: Uses computational algorithms (e.g., in software like FSL or TORTOISE) to correct for motion and distortions after the data has been collected. This should include correction for eddy currents and EPI distortion [19]. For populations prone to motion, such as children, behavioral interventions like allowing them to watch movies during the scan can also significantly reduce head motion [74].
FAQ 4: How reproducible are DTI measurements in a multi-center setting? When protocols are harmonized, DTI measurements can show good reproducibility. Evidence from large multi-center studies indicates:
- Scan-Rescan Repeatability: Excellent intra-scanner repeatability for DTI metrics within the same scanner [72].
- Inter-Scanner Variability: Cross-scanner coefficients of variation (CV) for DTI metrics in white matter regions can be kept low (e.g., below 5.7% in one study) [72] [73]. For example, one multi-scanner analysis reported mean inter-scanner CV of 4.5% for FA and 5.4% for MD [73]. These values provide a benchmark for expected technical variability in multi-center trials.
FAQ 5: What are the key steps in processing DTI data to minimize artifacts? A robust processing pipeline is crucial. Key steps include [75]:
- Signal Drift Correction: Correcting for slow scanner-induced signal changes over time.
- Gibbs Ringing Correction: Removing truncation artifacts from the images.
- Eddy Current & Motion Correction: Correcting for geometric distortions and subject movement.
- EPI Distortion Correction: Using methods based on magnetic field maps or reverse phase-encoded images to correct for susceptibility-induced distortions. It is recommended to perform these steps in a specific order, with signal drift correction occurring before sorting the diffusion volumes by their b-values [75].
Experimental Protocols & Benchmarking Data
Protocol 1: Phantom Validation for Diffusion Metric Stability
This protocol outlines the use of a fiber-ring diffusion phantom to establish the baseline repeatability of diffusion metrics [71].
Methodology:
- Phantom: A dedicated diffusion phantom mimicking restricted anisotropic diffusion in white matter [71].
- Acquisition: The phantom is scanned repeatedly using a multi-shell HARDI protocol.
- Long-term repeatability: Scan the phantom on four different days over two months.
- Short-term consistency: Perform eight consecutive scans without stopping to assess the impact of gradient coil heating.
- Analysis: For each scan, extract DTI (FA, MD), DKI (MK, AK), and NODDI metrics from a defined Region of Interest (ROI) within the phantom's fiber ring. Calculate the Coefficient of Variation (CoV) across repeated scans to assess repeatability.
Results: Table 1: Reproducibility of DTI, DKI, and NODDI metrics in a fiber phantom across multiple scans [71].
| Metric | Description | Coefficient of Variation (CoV) across 4 days | Coefficient of Variation (CoV) across 8 consecutive scans |
|---|---|---|---|
| FA | Fractional Anisotropy | 1.03% | 0.54% |
| MD | Mean Diffusivity | 2.34% | 0.61% |
| MK (MSDKI) | Mean Kurtosis (Mean Signal DKI) | < 5% | < 5% |
| ODI | Orientation Dispersion Index | < 5% | Not Reported |
Protocol 2: Multi-Scanner Scan-Rescan Reproducibility
This protocol assesses the inter- and intra-scanner variability of DTI metrics, which is critical for multi-center clinical trials [72] [73].
Methodology:
- Subjects: One healthy volunteer (a "human phantom") scanned on multiple scanners (e.g., 27 scanners across different sites), with each session including a scan-rescan [72] [73].
- Acquisition: A harmonized DTI or HARDI protocol is implemented across all scanners. In one study, this included 64 diffusion-weighting directions (b=700 s/mm²) and 8 b=0 volumes [72].
- Analysis: DTI metrics (FA, MD, LD, TD) are calculated within specific white matter structures (e.g., pyramidal tracts). Intra- and inter-scanner Coefficients of Variation (CV) are computed for these metrics.
Results: Table 2: Inter- and intra-scanner reproducibility of DTI metrics from multi-center studies [72] [73].
| Study | Metric | Inter-Scanner CV (across scanners) | Intra-Scanner CV (scan-rescan on same scanner) |
|---|---|---|---|
| SPRINT-MS (27 scanners) | FA (Pyramidal Tract) | < 5.7% (Cross-scanner CV for all metrics) | No significant difference between scan and rescan |
| TACERN (7 scanners) | FA (White Matter) | 4.5% | 2.5% |
| TACERN (7 scanners) | MD (White Matter) | 5.4% | 1.5% |
Protocol 3: Combined Prospective and Retrospective Motion Correction
This protocol evaluates the efficacy of combining different motion correction strategies to improve data quality in challenging populations [19].
Methodology:
- Subjects: Populations prone to motion (e.g., pediatric subjects).
- Acquisition:
- Standard DTI: Acquired with a twice-refocused spin-echo EPI sequence.
- Navigated DTI (vNav): The same sequence modified with a 3D EPI navigator to track and prospectively correct for head motion in real-time after each diffusion volume [19].
- Processing: Data from both acquisitions are processed with and without additional retrospective motion, eddy current, and EPI distortion correction using software like FSL or TORTOISE [19].
- Analysis: Compare the quality of ellipsoid fits, white matter maps, and probabilistic tractography results across the different processing pipelines.
Key Finding: The inclusion of both prospective and retrospective motion correction with EPI distortion correction provides the most sensitive and specific tractography results, which is particularly important for studying subject populations that are prone to motion [19].
Workflow Visualization
Phantom Validation and Data Processing Workflow
DTI Data Processing with Motion Correction
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential materials and tools for DTI validation and artifact mitigation studies.
| Item | Function & Application |
|---|---|
| ACR Phantom | A standardized phantom for routine quality control of MRI scanners, used to monitor signal intensity and uniformity across sites and over time [73]. |
| Anisotropic Diffusion Phantom | A specialized phantom (e.g., with fiber rings) designed to mimic the restricted diffusion properties of white matter, providing a ground truth for validating DTI, DKI, and NODDI metrics [71]. |
| Human Phantom | A healthy volunteer repeatedly scanned on all study scanners to characterize the normal biological and technical variability of quantitative MRI measures in living tissue [73]. |
| Prospective Motion Correction (vNav) | A pulse sequence modification that uses real-time motion tracking (navigators) to update scan coordinates during acquisition, effectively preventing motion artifacts [19]. |
| Retrospective Correction Software (FSL, TORTOISE) | Computational tools for post-processing correction of subject motion, eddy current-induced distortions, and EPI distortions in diffusion data [19]. |
| Behavioral Motion Reduction | Non-invasive interventions, such as allowing movie watching during scans, which have been shown to significantly reduce head motion in younger children [74]. |
Within the context of mitigating motion artifacts in diffusion tensor imaging (DTI) research, the selection of a data preprocessing pipeline is a critical decision. Motion artifacts can severely compromise the integrity of DTI data, leading to inaccurate estimation of key microstructural metrics such as fractional anisotropy (FA) and mean diffusivity (MD). This technical support guide compares the performance of widely used processing pipelines, including FSL, TORTOISE, and DSI Studio, providing troubleshooting guidance and FAQs to help researchers, scientists, and drug development professionals optimize their DTI analyses.
FAQs and Troubleshooting Guides
How does the choice of preprocessing pipeline affect my final DTI metrics?
Different pipelines, even when applied to the same raw data, can produce significantly different quantitative outputs. This variability is a major concern for the reproducibility of studies, particularly in clinical settings.
- Problem: Large, clinically important variability in diffusion parameter estimates from peripheral nerves depending on the software used for preprocessing [76] [77].
- Evidence: A comparative study on upper limb DTI data found that when compared to FSL's TOPUP & eddy pipeline:
- Troubleshooting Guide:
- Symptom: Your FA values seem inconsistent with the literature or visual inspection of the data.
- Solution: Do not directly compare DTI metric values obtained from different preprocessing pipelines. If comparing your results to another study, ensure you know which preprocessing pipeline was used. For longitudinal studies within the same subjects, always use the same pipeline for all time points.
- Prevention: State the preprocessing pipeline (including software and version) explicitly in your methods section. Consider trying multiple pipelines on a subset of your data to understand the direction and magnitude of the bias introduced.
Table: Comparison of DTI Metric Variations Between Preprocessing Pipelines (vs. FSL TOPUP & eddy)
| Pipeline | Effect on Fractional Anisotropy (FA) | Effect on Radial Diffusivity (RD) |
|---|---|---|
| DSI Studio | 2% Lower | 6% Higher |
| TORTOISE | 6% Lower | 13% Higher |
Source: Adapted from Wade et al. [76] [77]
Which pipeline offers the best geometric correction for distortion artifacts?
While all major pipelines improve geometric fidelity, their performance in correcting distortions may be more comparable than their effect on quantitative metrics.
- Problem: Single-shot EPI, a common DTI acquisition method, is prone to geometric and intensity distortions due to susceptibility effects and eddy currents [77].
- Evidence: A study evaluating distortion correction in the upper limb found that preprocessing improved the geometric similarity of DTI data to structural T1-weighted images by about 1%. However, there were no meaningful differences between the Sörenson-Dice similarity coefficients achieved by FSL, TORTOISE, or DSI Studio [76] [77]. This suggests that while all pipelines improve geometric accuracy, the choice between them may not be based on this factor alone.
- Troubleshooting Guide:
- Symptom: Your diffusion images appear warped or misaligned with the anatomical reference.
- Solution: Any of the major pipelines (FSL, TORTOISE) will provide a baseline level of distortion correction. The choice can then be based on other factors, such as quantitative bias, workflow integration, or comfort with the software.
I am working with non-brain data. Are these pipelines still suitable?
Pipelines like FSL and TORTOISE were primarily developed for brain imaging, and their application to other body parts, like the spinal cord or peripheral nerves, requires careful consideration.
- Problem: The performance of pipelines optimized for the brain may not fully translate to other anatomical regions, which present unique challenges like severe metal artifacts from implants [78].
- Evidence: Studies have successfully applied specialized acquisition sequences (like reduced FOV with phase-segmented EPI) to obtain DTI in the lumbar spinal cord and near cervical spine metal implants, followed by processing with standard pipelines [78] [79]. However, the comparison study on upper limb data confirmed that pipeline choice introduces significant variability in nerve metrics [76].
- Troubleshooting Guide:
- Symptom: Poor quality corrections or failed processing runs for non-brain DTI data.
- Solution: Ensure your data is converted to a compatible format (e.g., NIfTI). For body parts with significant metal implants, investigate specialized acquisition sequences to minimize artifacts at the source [78]. Acknowledge the potential for increased uncertainty in quantitative metrics in your research conclusions.
What are the key practical differences between FSL and TORTOISE?
The choice between pipelines often involves trade-offs between quantitative accuracy, computational demand, and ease of use.
- Problem: Researchers need to select a pipeline that is not only accurate but also feasible to implement within their computational environment and expertise.
- Evidence: While a direct comparison of computational speed between FSL and TORTOISE was not provided in the results, other motion correction methods highlight that speed can vary significantly between algorithms [80]. Furthermore, TORTOISE is noted for its strong theoretical foundation in correcting for spatial systematic errors related to gradient nonlinearities [81] [82].
- Troubleshooting Guide:
- Symptom: Uncertainty about which pipeline to adopt for a new study.
- Solution: Consider the following practical aspects:
- FSL (TOPUP & eddy): Very widely adopted, making it a de facto standard. Well-integrated into many neuroimaging workflows. Has both command-line and graphical interfaces.
- TORTOISE: Known for its high accuracy in distortion correction, implementing advanced methods like DR-BUDDI for blip-up/blip-down data [81]. It can be more computationally intensive and has a steeper learning curve. Note that as of 2025, support has migrated to TORTOISEV4 on GitHub, and users are encouraged to use the new version [81].
Table: Practical Considerations for FSL and TORTOISE
| Feature | FSL | TORTOISE |
|---|---|---|
| Primary Strength | Widespread adoption, integrated workflow | Advanced distortion correction, high accuracy [81] |
| Key Tool | TOPUP & eddy | DR-BUDDI, DIFF_PREP [81] |
| Current Version | FSL (ongoing) | TORTOISEV4 [81] |
| Access | Requires registration; free for academic use | Free; available on GitHub [81] |
Experimental Protocols from Key Cited Studies
To ensure reproducibility, below is a summary of the methodology from a key comparative study.
Protocol: Comparison of Preprocessing Pipelines in Upper Limb DTI [76] [77]
Data Acquisition:
- Scanner: 3T MAGNETOM Prisma.
- Sequence: Single-shot EPI.
- Acquisition: Data acquired in blip-up and blip-down phase-encoding directions to enable distortion correction.
- Subjects: 13 healthy volunteers.
Data Preprocessing:
- Denoising: Raw data were first denoised.
- Concatenation & Correction: Data were then processed through four independent pipelines:
- (i) FSL's TOPUP & eddy
- (ii) FSL's TOPUP only
- (iii) DSI Studio
- (iv) TORTOISE
Analysis:
- Geometric Fidelity: The Sörenson-Dice coefficient was used to measure the similarity between corrected b=0 images and matched T1-weighted anatomical images.
- DTI Metrics: Fractional Anisotropy (FA), Radial Diffusivity (RD), Axial Diffusivity (AD), and Mean Diffusivity (MD) were extracted from regions of interest (ROIs) drawn around the median, radial, and ulnar nerves.
- Statistical Comparison: Metrics were compared between pipelines using mixed-effects linear regression.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Software and Computational Tools for DTI Preprocessing
| Item Name | Function/Brief Explanation | Relevance to Motion Artifact Mitigation |
|---|---|---|
| FSL | A comprehensive library of analysis tools for MRI data. Its TOPUP and eddy tools are the gold standard for many for distortion and eddy-current correction. |
Corrects for distortions and eddy currents induced by motion and hardware imperfections. |
| TORTOISE | Software package specializing in improved correction of EPI distortions and motion in diffusion MRI. | Its DR-BUDDI tool is designed for highly accurate correction using pairs of data with opposite phase encoding [81]. |
| DSI Studio | A software tool for diffusion MRI analysis, providing an all-in-one platform for reconstruction, processing, and tractography. | Offers an integrated and often user-friendly pipeline for processing, including motion and distortion correction. |
| Blip-Up/Blip-Down Data | A data acquisition strategy where images are collected with two opposite phase-encoding directions. | This data is a prerequisite for powerful distortion correction algorithms like FSL's TOPUP and TORTOISE's DR_BUDDI [81] [76]. |
| Reduced FOV (rFOV) Sequences | Acquisition sequences (e.g., ZOOMit, FOCUS) that limit the field of view to the region of interest. | Reduces susceptibility artifacts and blurring, which is particularly useful in areas like the spinal cord and can minimize artifacts that complicate motion correction [78] [79]. |
Workflow and Pipeline Relationship Diagrams
FAQ: Troubleshooting Guides for Motion Artifacts in DTI
Q1: How can I determine if observed microstructural differences are biologically real or caused by motion artifacts?
To assess biological plausibility, you must systematically evaluate the pattern and nature of the findings. Real microstructural changes typically follow known neuroanatomical patterns and are consistent across multiple diffusion metrics. For example, genuine age-related changes show a specific trajectory: a negative relationship between age and intracellular isotropic signal fraction, fiber density, and cross-section, while extracellular signal fraction increases with age [83]. If your "movers" group shows deviations from established neurobiological patterns that cannot be explained by known physiological processes, motion artifacts should be suspected. Furthermore, biologically plausible findings will demonstrate consistent lateralization patterns and follow white matter tract anatomy rather than exhibiting random, scattered abnormalities that correlate with motion severity but not neuroanatomy.
Q2: What acquisition strategies can prevent motion artifacts from being mistaken for biological findings?
Implement motion-compensated diffusion gradients, which have demonstrated significant efficacy in preserving data quality during subject movement. First-order (M1) and particularly second-order (M2) motion-compensating diffusion gradients can dramatically reduce signal dropout—from 44% of images with standard (M0) sequences to 0% with M2 gradients during continuous gross head motion [3]. Additionally, incorporate multiple interspersed T2-weighted (b=0) volumes throughout your acquisition. These can be used for robust GRAPPA and Nyquist ghost calibration, selecting the optimal weights from the set of b=0 scans to reduce calibration errors due to motion [7]. For clinical populations prone to movement, consider using a GRAPPA-accelerated EPI sequence with an acceleration factor of R=3, which provides single-shot robustness with parallel imaging benefits [7].
Q3: What processing methods can correct for motion artifacts after acquisition?
Several advanced processing approaches can mitigate motion artifacts:
- Retrospective motion correction with 3D rigid-body realignment and importance weighting: This approach effectively reduces inter-volume motion artifacts and can be combined with volume rejection methods to discard severely corrupted volumes [7].
- AI-based correction with Res-MoCoDiff: This efficient denoising diffusion probabilistic model uses a residual-guided approach and requires only four reverse diffusion steps, substantially reducing processing time (0.37 seconds per batch of two image slices) while maintaining high fidelity (PSNR up to 41.91±2.94 dB for minor distortions) [84].
- Non-linear registration for susceptibility artifacts: Approaches using Bézier functions and simultaneous perturbation stochastic approximation (SPSA) optimization can correct spatial distortions in DTI data, particularly crucial when integrating fiber tract data into stereotactic systems for surgical guidance [39].
Q4: How do I validate that my motion correction methods are working effectively?
Employ quantitative quality metrics before and after correction processing. Compare quantitative DTI parameters (FA, MD) between motion-corrected data and a reference dataset acquired without motion. Studies show that without proper correction, DTI parameters from motion-corrupted data are significantly elevated compared to reference data, and conventional retrospective corrections often fail when more than 15% of diffusion-weighted images are corrupted [3]. Additionally, implement qualitative assessment of specific artifact patterns: look for signal "drop-outs" (caused by motion during diffusion preparation), ghosting (from motion between volumes), and aliasing (from motion during calibration scans) [7]. Effective correction should reduce these specific artifacts while preserving anatomical detail.
Q5: What are the key indicators that my results may be compromised by motion artifacts?
Several red flags suggest possible motion contamination:
- Inconsistent lateralization: While healthy brains show natural lateral differences in microstructure [83], motion artifacts often create asymmetries that don't correspond to established neuroanatomical patterns.
- Abnormal metric relationships: Genuine microstructural changes typically affect multiple diffusion metrics in biologically consistent ways (e.g., increased extracellular signal fraction with age) [83]. Motion artifacts often produce discordant metric changes.
- Spatial patterns correlating with susceptibility regions: Artifacts frequently appear at tissue interfaces with different magnetic susceptibility (skull base, brainstem, frontal lobe) [39].
- Statistical outliers in data quality metrics: Abnormally high variance in DTI parameters or inconsistent fiber tracking results compared to established norms.
Experimental Protocols for Motion Mitigation
Protocol 1: Prospective Motion Compensation with Advanced Diffusion Gradients
This protocol utilizes motion-compensating diffusion gradients to minimize artifacts during data acquisition [3].
Materials: 3T MRI scanner with programable diffusion gradient capabilities, 8-channel head coil, motion-compensated diffusion sequence (M1 and M2 gradients).
Procedure:
- Implement first-order (M1) and second-order (M2) motion-compensating diffusion gradients previously developed for cardiac DTI for brain imaging.
- Acquire DTI data with 25 isotropically distributed diffusion directions with b=1000 s/mm².
- Include 5 T2-weighted (b=0) images interspersed throughout the acquisition.
- Use identical sequence parameters (FOV = 20-24 cm, acquisition matrix = 128×128, 3 mm slice thickness) for standard (M0), M1, and M2 acquisitions.
- For validation, acquire data in the same subjects with and without intentional head motion.
- Process data using identical reconstruction pipelines for all gradient types.
- Compare DTI parameters (FA, MD) and rates of image corruption between gradient types.
Validation: Quantitative comparison of DTI parameters should show consistency between M0, M1, and M2 data in the absence of motion. During motion, M2 data should show significantly fewer corrupted images (<5% vs. up to 44% with M0) and DTI parameters consistent with motion-free reference data [3].
Protocol 2: Res-MoCoDiff AI-Based Motion Correction
This protocol implements an efficient diffusion model for retrospective motion correction of acquired DTI data [84].
Materials: Motion-corrupted DTI datasets, computational resources with GPU acceleration, Res-MoCoDiff implementation, reference motion-free datasets for validation.
Procedure:
- Prepare motion-corrupted DTI datasets and corresponding motion-free reference data if available.
- Implement the Res-MoCoDiff architecture with U-net backbone and Swin Transformer blocks replacing attention layers.
- Train the model using a combined ℓ1+ℓ2 loss function to promote image sharpness and reduce pixel-level errors.
- Apply the novel residual error shifting mechanism during the forward diffusion process to incorporate information from motion-corrupted images.
- Perform the reverse diffusion process with only four steps for computational efficiency.
- Validate correction quality using quantitative metrics (PSNR, SSIM, NMSE) across minor, moderate, and heavy distortion levels.
- Compare against conventional methods (cycleGAN, Pix2pix) for benchmarking.
Validation: Corrected images should achieve PSNR values up to 41.91±2.94 dB for minor distortions, with the highest SSIM and lowest NMSE values across all distortion levels. Processing time should average 0.37 seconds per batch of two image slices [84].
Quantitative Data on Motion Artifact Impact and Correction Efficacy
Table 1: Impact of Motion on DTI Data Quality and Correction Performance
| Metric | Standard DTI (M0) with Motion | Motion-Compensated DTI (M2) | AI Correction (Res-MoCoDiff) |
|---|---|---|---|
| Percentage of Corrupted DW Images | Up to 44% [3] | 0% [3] | N/A (post-processing) |
| Signal Dropout | Severe [3] | Minimal [3] | Eliminated [84] |
| DTI Parameter Reliability | Elevated values vs. reference [3] | Consistent with reference [3] | High fidelity to reference [84] |
| Processing Time | N/A | N/A | 0.37 sec per 2 slices [84] |
| PSNR Improvement | N/A | N/A | Up to 41.91±2.94 dB [84] |
| Effectiveness with >15% Corruption | Poor (retrospective correction fails) [3] | Maintains effectiveness [3] | Maintains effectiveness [84] |
Table 2: Normal Age-Related Microstructural Changes vs. Motion Artifact Patterns
| Characteristic | Biologically Plausible Change | Motion Artifact Indicator |
|---|---|---|
| Extracellular Signal Fraction | Increases with age [83] | Random spatial distribution |
| Intracellular Isotropic Signal | Decreases with age [83] | Inconsistent across sessions |
| Fiber Density/Cross-section | Decreases with age [83] | Abnormal regional patterns |
| Spatial Pattern | Follows white matter anatomy [83] | Concentrated at susceptibility interfaces [39] |
| Laterality | Consistent hemispheric differences [83] | Inconsistent asymmetries |
| Relationship to Motion Severity | None | Direct correlation |
Research Reagent Solutions
Table 3: Essential Tools for Motion-Resilient DTI Research
| Resource | Function | Application Context |
|---|---|---|
| Motion-Compensating Diffusion Gradients (M1/M2) | Reduces signal dropout during acquisition by compensating for subject movement [3] | Prospective motion correction during scanning |
| Res-MoCoDiff Algorithm | AI-based retrospective correction using efficient diffusion models [84] | Post-processing of motion-corrupted data |
| Non-linear Registration with Bézier Functions | Corrects spatial distortions from susceptibility artifacts [39] | Preprocessing for tractography and surgical planning |
| GRAPPA-Accelerated EPI Sequence | Provides motion-insensitive acquisition with parallel imaging [7] | Pediatric and clinical populations |
| 3T-CSD Model | Advanced microstructural mapping to establish normal trajectories [83] | Biological plausibility assessment |
| Retrospective Motion Correction with Importance Weighting | 3D rigid-body realignment with volume rejection [7] | Standard preprocessing pipeline |
Decision Pathway for Assessing Biological Plausibility
Motion Artifact Correction Workflow
FAQs: Motion Artifacts in DTI Research
Q1: What are the most common causes and impacts of motion artifacts in DTI data? Motion artifacts are a major confounding factor in DTI studies. They occur when a subject moves their head during the scan, leading to misalignment of diffusion volumes and causing individual voxels to be exposed to unintended diffusion encoding gradients [34]. This results in signal dropouts and can significantly bias key DTI metrics. Specifically, motion contamination has been shown to more severely affect connectivity strength when measured by mean tract Fractional Anisotropy (FA) compared to streamline count [85]. These artifacts can lead to inaccurate tractography and false conclusions in both clinical and research settings.
Q2: What is the difference between retrospective and prospective motion correction?
- Retrospective Motion Correction: This is a computational method applied after data acquisition. It relies on coregistering the misaligned diffusion volumes. A limitation is that it cannot fully correct for the effects of through-plane motion on the local history of magnetization and is susceptible to distortion from partial voluming, which can negatively bias DTI parameters [34].
- Prospective Motion Correction: This method actively tracks head position in real-time during the scan, often using a short, non-diffusion-weighted 3D-EPI navigator pulse. The scanner then immediately updates both the spatial encoding and the diffusion encoding gradients to maintain consistent alignment with the anatomy. Studies show this approach leads to smaller changes in FA values and reduces spurious tractographic changes compared to retrospective methods [34].
Q3: Which preprocessing steps are most effective in reducing motion-related confounds? A comprehensive analysis of 240 preprocessing pipelines found that the choice of strategy dramatically influences motion contamination. The most effective approach includes:
- Outlier Replacement: Identifying and replacing corrupted data points.
- Within-Slice Volume Correction: Correcting for motion that occurs even during the acquisition of a single slice [85]. Pipelines incorporating these advanced motion-correction tools showed a significant reduction in cross-subject correlations between head motion and structural connectivity strength [85].
Q4: How can I validate the effectiveness of my motion correction protocol? It is recommended to:
- Correlate Motion Parameters with Output Metrics: Calculate the correlation between estimated head motion parameters and key DTI outcomes (e.g., mean FA, connectivity strength). A strong correlation indicates residual motion contamination [85].
- Use a Stationary Phantom: Scanning a structured, stationary phantom (e.g., a pineapple) can help isolate and evaluate the artifacts introduced by the correction algorithms themselves, in the absence of real motion [34].
Q5: Are there specific challenges for DTI in pediatric or patient populations? Yes, populations that may have difficulty remaining still (e.g., young children, patients with neurodegenerative diseases) present a particular challenge. In such cases, prospective motion correction with reacquisition capabilities is highly beneficial. One study used a navigated sequence that could reacquire a fixed number of corrupted diffusion volumes immediately after motion exceeded a threshold, ensuring data integrity without significantly prolonging scan times [34].
Experimental Protocols for Motion Mitigation
Protocol 1: Prospective Motion Correction with Navigator Pulse
This protocol is adapted from a study on pediatric DTI [34].
1. Sequence Parameters:
- Pulse Sequence: A twice-refocused 2D diffusion pulse sequence to minimize eddy currents.
- Navigator: A 3D-EPI navigator (duration 526 msec) is acquired after each diffusion volume. It is not diffusion-weighted to ensure accurate coregistration.
- Key Parameters: TR ~10,000 ms, TE ~86 ms, resolution 2x2x2 mm³, 30 non-collinear diffusion directions at b=1000 s/mm², and 4 non-diffusion-weighted (B0) acquisitions.
- Real-time Correction: The motion estimates from the navigator are used to update the spatial and diffusion encoding gradients in real-time.
- Reacquisition: The sequence is set to reacquire a maximum of 5 diffusion volumes if motion exceeds a predefined threshold.
2. Subject Preparation:
- Use foam padding around the head to minimize motion.
- For young children, conduct mock scanner training to practice lying still.
3. Data Processing:
- Following navigated scanning, standard processing steps (e.g., eddy current correction, outlier rejection) can be applied within existing pipelines.
Protocol 2: Advanced Preprocessing Pipeline for Structural Connectomics
This protocol is derived from a large-scale analysis of preprocessing choices [85].
1. Data Acquisition:
- Acquire DTI data using a standard single-shot EPI sequence with multiple diffusion directions.
2. Preprocessing Pipeline Choices:
- Explicit Head Motion Correction: Utilize a tool that incorporates outlier replacement and within-slice motion correction.
- Tractography Propagation: Choose an algorithm (e.g., deterministic or probabilistic).
- Track Seeding & Termination: Define seeding method (e.g., whole brain) and termination constraints (e.g., FA threshold, curvature threshold).
- Connectome Edge Weighting: Prefer streamline count for connectivity strength, as it was found to be less susceptible to motion effects than mean tract FA [85].
- Parcellation: Register tracts to a standard brain atlas to define network nodes.
3. Validation:
- For each subject, calculate a framewise displacement metric from the motion parameters.
- Statistically assess the correlation between this motion metric and the final structural connectivity matrices to ensure confounds have been mitigated.
Workflow Visualization
The following diagram illustrates the decision-making process for addressing motion artifacts in a DTI research pipeline, integrating both prospective and retrospective correction strategies.
Research Reagent Solutions
The table below details key computational "reagents" and tools essential for DTI analysis, with a focus on mitigating motion artifacts.
| Research Reagent / Tool | Function in DTI Analysis |
|---|---|
| 3D-EPI Navigator (vNav) [34] | A short, non-diffusion-weighted volumetric pulse used for real-time head tracking and prospective motion correction during data acquisition. |
| Outlier Replacement Algorithms [85] | Identifies and replaces signal corruptions (e.g., from sudden motion) in the raw diffusion data before tensor fitting. |
| Within-Slice Motion Correction [85] | A sophisticated correction method that addresses motion occurring during the acquisition of a single slice, not just between volumes. |
| Spinal Cord Toolbox [86] | A software toolbox used for processing spinal cord DTI data, including extraction of B0 images and calculation of Fractional Anisotropy (FA) maps. |
| FSL (FMRIB Software Library) [34] | A comprehensive library of MRI analysis tools, including FLIRT for image registration, which can be used for retrospective motion correction in DTI. |
| Fractional Anisotropy (FA) [8] [87] | A scalar metric ranging from 0 (isotropic) to 1 (anisotropic) that quantifies the directionality of water diffusion, sensitive to white matter integrity. |
| Mean Diffusivity (MD) / Apparent Diffusion Coefficient (ADC) [8] [87] | A measure of the overall magnitude of water diffusion, which increases in conditions like edema or necrosis. |
Conclusion
The mitigation of motion artifacts in DTI requires a comprehensive, multi-faceted approach that spans the entire data lifecycle. Foundational research has thoroughly characterized motion patterns, while methodological advances in both prospective acquisition and retrospective processing have proven highly effective at reducing biases in quantitative DTI metrics. The integration of complementary techniques, such as denoising with systematic error correction and the combination of prospective and retrospective methods, yields the most robust results. Looking forward, the validation of these pipelines ensures their reliability for sensitive clinical applications, including early detection of neurodegenerative diseases and presurgical planning. Future directions should focus on the development and widespread adoption of even more robust motion-compensated sequences, the standardization of processing protocols across consortiums, and the continued validation of DTI biomarkers in therapeutic development, ultimately enhancing the precision and diagnostic power of neuroimaging in research and clinical practice.
References
- 1. Head Motion in Diffusion Magnetic Resonance Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC11814480/]
- 2. Facilitating diffusion tensor imaging of the brain during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10872734/]
- 3. Facilitating diffusion tensor imaging of the brain during ... [https://pubmed.ncbi.nlm.nih.gov/38073070/]
- 4. Quantifying MR head motion in the Rhineland Study - PubMed [https://pubmed.ncbi.nlm.nih.gov/37209757/]
- 5. PET Head Motion Estimation Using Supervised Deep ... [https://arxiv.org/html/2510.12758v1]
- 6. Prevention of Motion-Induced Signal Loss in Diffusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4420624/]
- 7. Diffusion tensor imaging (DTI) with retrospective motion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3443529/]
- 8. Diffusion Tensor Imaging - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK537361/]
- 9. Systematic Review and Meta-analysis of AI-driven MRI ... [https://arxiv.org/html/2509.05071v1]
- 10. Workflow Tutorial - Quantitative Imaging Toolkit [https://cabeen.io/qitwiki/workflow/]
- 11. Accelerated diffusion tensor imaging with self-supervision ... [https://www.nature.com/articles/s41598-025-96459-9]
- 12. DWI/DTI Quality Control Tool: DTIPrep: open-discussion [https://www.nitrc.org/forum/forum.php?set=custom&forum_id=1188&style=nested&max_rows=75]
- 13. Head injury or head motion? Assessment and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6869898/]
- 14. Reduction of systematic errors in diffusion tensor imaging ... [https://www.sciencedirect.com/science/article/pii/S0010482525008546]
- 15. Manual vs. AI-Based Tractography: Assessing Fractional ... [https://www.medrxiv.org/content/10.1101/2025.04.25.25326403v1.full]
- 16. Harmonization of diffusion MRI on healthy subjects using ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1591169/full]
- 17. Susceptibility and diffusion MRI biomarkers predict ... [https://www.nature.com/articles/s41531-025-01174-x]
- 18. Diffusion tensor imaging with free‐water correction reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11703597/]
- 19. Assessing the performance of different DTI motion correction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5118068/]
- 20. Tract Specificity of Age Effects on Diffusion Tensor Imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8006297/]
- 21. Diffusion tensor imaging technique for studying brain ... [https://www.sciencedirect.com/science/article/pii/S0208521625000385]
- 22. Longitudinal diffusion tensor imaging correlates with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333877/]
- 23. Reducing Eddy Current Artifacts With Dummy Gradients ... [https://i-mri.org/DOIx.php?id=10.13104/imri.2025.0013]
- 24. DTI with Prospective Motion Correction & Reacquisition in ... [https://archive.ismrm.org/2011/4592.html]
- 25. Age-Related Alterations in DTI Metrics in the Human Brain ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2021.682109/full]
- 26. Navigator echoes - Questions and Answers in MRI [https://mriquestions.com/navigator-echoes.html]
- 27. Real-time Optical Motion Correction for Diffusion Tensor Imaging - PMC [https://ncbi.nlm.nih.gov/pmc/articles/PMC3139706]
- 28. TOPUP - FSL - FMRIB Software Library [https://fsl.fmrib.ox.ac.uk/fsl/docs/diffusion/topup/index.html]
- 29. EDDY - FSL - FMRIB Software Library [https://fsl.fmrib.ox.ac.uk/fsl/docs/diffusion/eddy/index.html]
- 30. Frequently asked questions about TOPUP [https://fsl.fmrib.ox.ac.uk/fsl/docs/diffusion/topup/FAQ/index.html]
- 31. eddy/UsersGuide [https://web.mit.edu/fsl_v5.0.10/fsl/doc/wiki/eddy(2f)UsersGuide.html]
- 32. FSL topup and eddy | Behavior and Neuroimaging Core User ... [https://docs.ccv.brown.edu/bnc-user-manual/analysis-pipelines/diffusion-weighted-imaging-dwi-analysis/fsl-topup-and-eddy]
- 33. topup/TopupUsersGuide [https://web.mit.edu/fsl_v5.0.10/fsl/doc/wiki/topup(2f)TopupUsersGuide.html]
- 34. Motion Artifact Reduction in Pediatric Diffusion Tensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4269573/]
- 35. Correction of Motion-Affected MRI Images via ... [https://archive.ismrm.org/2025/3980.html]
- 36. Cardiac diffusion-weighted and tensor imaging: A ... [https://www.sciencedirect.com/science/article/pii/S1097664724011360]
- 37. Diffusion Encoding Methods in MRI: Perspectives and ... [https://i-mri.org/DOIx.php?id=10.13104/imri.2022.26.4.208]
- 38. Dynamic Correction of Artifacts due to Susceptibility Effects ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3138839/]
- 39. Correction of susceptibility artifacts in diffusion tensor data ... [https://www.sciencedirect.com/science/article/abs/pii/S1361841507000540]
- 40. Simultaneous and Inherent Correction of B0 and Eddy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6631373/]
- 41. DTI Processing - Software Tools - Diffusion Imaging [https://www.diffusion-imaging.com/2013/03/list-of-software-tools-for-dti.html]
- 42. Correction of vibration artifacts in DTI using phase-encoding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3569871/]
- 43. Incorporating outlier detection and replacement into a non- ... [https://www.sciencedirect.com/science/article/abs/pii/S1053811916303068]
- 44. Towards a comprehensive framework for movement and ... [https://www.sciencedirect.com/science/article/pii/S1053811917301945]
- 45. Automated Assessment of the Quality of Diffusion Tensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4169879/]
- 46. Robust Super-resolution Volume Reconstruction from Slice ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3694441/]
- 47. Meta-learning Slice-to-Volume Reconstruction in Fetal ... [https://arxiv.org/html/2505.09565v1]
- 48. Estimation and Removal of Residual Motion Artifact in ... [https://apertureneuro.org/article/123369-estimation-and-removal-of-residual-motion-artifact-in-retrospectively-motion-corrected-fmri-data-a-comparison-of-intervolume-and-intravolume-motion-u]
- 49. The effect of elimination of gibbs ringing, noise and systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11217413/]
- 50. Structure-adaptive sparse denoising for diffusion-tensor MRI [https://www.sciencedirect.com/science/article/abs/pii/S1361841513000078]
- 51. Evaluating the impact of denoising diffusion MRI data on ... [https://www.nature.com/articles/s41598-025-10947-6]
- 52. MRI motion correction via efficient residual-guided ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12083705/]
- 53. An Exploration of Motion-Sampling Interactions in 3D MRI ... [https://pubmed.ncbi.nlm.nih.gov/41204061/]
- 54. A Physics-Informed Deep Learning Method for Correcting ... [https://archive.ismrm.org/2025/3844.html]
- 55. BSD DTI is a method to reduce systematic errors observed ... [https://cds.ismrm.org/protected/22MProceedings/PDFfiles/2818.html]
- 56. Accelerating multi-directional diffusion MRI through patch- ... [https://www.sciencedirect.com/science/article/pii/S1053811925004161]
- 57. Current challenges and future directions for brain age ... [https://www.nature.com/articles/s41467-025-63222-7]
- 58. The Role of Artificial Intelligence in Pediatric Neuroradiology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468975/]
- 59. Determining the OPTIMAL DTI analysis method for application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9421487/]
- 60. A protocol for the analysis of DTI data collected from young ... [https://www.sciencedirect.com/science/article/pii/S2215016120300972]
- 61. A guide to quantifying head motion in DTI studies [https://www.diffusion-imaging.com/2015/11/a-guide-to-quantifying-head-motion-in.html]
- 62. DTI Processing - Distortion Correction - Diffusion Imaging [https://www.diffusion-imaging.com/2012/03/dti-preprocessing-distortion-correction.html]
- 63. DTI - Diffusion Tensor Imaging [https://mriquestions.com/dti-tensor-imaging.html]
- 64. Motion Artefacts in MRI: a Complex Problem with Many Partial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4517972/]
- 65. Quality Control of Diffusion Weighted Images - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3864968/]
- 66. Basic Theory of Motion Artifacts in MRI [https://cds.ismrm.org/protected/21MProceedings/PDFfiles/E5763.html]
- 67. Test-retest reliability of Diffusion Tensor Imaging metrics in ... [https://www.sciencedirect.com/science/article/abs/pii/S1053811919303532]
- 68. The Impact of Quality Assurance Assessment on Diffusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4753778/]
- 69. Deep learning-based method for reducing residual motion ... [https://pubmed.ncbi.nlm.nih.gov/33058279/]
- 70. Deep learning-based image reconstruction benefits ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1607130/full]
- 71. Assessment of a diffusion phantom for quality assurance in ... [https://www.nature.com/articles/s41598-025-12777-y]
- 72. Scan-rescan repeatability and cross-scanner comparability of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6138530/]
- 73. Reproducibility of Structural and Diffusion Tensor Imaging ... [https://www.frontiersin.org/journals/integrative-neuroscience/articles/10.3389/fnint.2019.00024/full]
- 74. Behavioral interventions for reducing head motion during ... [https://www.sciencedirect.com/science/article/pii/S1053811918300235]
- 75. Diffusion MRI Data Processing and Analysis: A Practical ... [https://link.springer.com/protocol/10.1007/978-1-0716-4260-3_10]
- 76. Comparison of distortion correction preprocessing ... [https://pubmed.ncbi.nlm.nih.gov/37831659]
- 77. Comparison of distortion correction preprocessing ... [https://www.bohrium.com/paper-details/comparison-of-distortion-correction-preprocessing-pipelines-for-dti-in-the-upper-limb/920501144147460272-6181]
- 78. Metal Artifact Reduction Around Cervical Spine Implant Using... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10841892/]
- 79. Comparing single-shot EPI and 2D-navigated, multi ... [https://www.sciencedirect.com/science/article/pii/S0730725X25001298]
- 80. Toward optimal inline respiratory motion correction for in vivo ... [https://pubmed.ncbi.nlm.nih.gov/40065566/]
- 81. Home | TORTOISE group [https://tortoise.nibib.nih.gov/]
- 82. Diagnostic performance of a multi-shell DTI protocol and its ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1618582/full]
- 83. Diffusion MRI Microstructure Markers of Changes in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616505/]
- 84. Res-MoCoDiff: residual-guided diffusion models for motion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532098/]
- 85. The efficacy of different preprocessing steps in reducing ... [https://www.sciencedirect.com/science/article/pii/S1053811920307382]
- 86. A Deep-Learning-Based Diffusion Tensor Imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384042/]
- 87. Review article Diffusion Tensor Imaging of the Brain [https://www.sciencedirect.com/science/article/pii/S1878747923006530]