Beyond Single Studies: A Framework for Replicable Consensus Models in Biomedical Validation Cohorts
This article provides a comprehensive guide for researchers and drug development professionals on ensuring the replicability of consensus prediction models across diverse validation cohorts.
Beyond Single Studies: A Framework for Replicable Consensus Models in Biomedical Validation Cohorts
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on ensuring the replicability of consensus prediction models across diverse validation cohorts. It explores the foundational principles of the replication crisis in science, presents methodological frameworks for building robust multi-model ensembles, addresses common troubleshooting and optimization challenges, and establishes rigorous standards for external validation and comparative performance analysis. Drawing on recent advances in machine learning and lessons from large-scale replication projects, the content offers practical strategies to enhance the reliability, generalizability, and clinical applicability of predictive models in biomedical research.
The Replicability Crisis and the Critical Need for Consensus Models
Defining Replicability and Reproducibility in Computational Biomedicine
In computational biomedicine, where research increasingly informs regulatory and clinical decisions, the precise concepts of reproducibility and replicability form the bedrock of scientific credibility. While often used interchangeably in general discourse, these terms represent distinct validation stages in the scientific process. Reproducibility refers to obtaining consistent results using the same input data, computational steps, methods, and conditions of analysis, essentially verifying that the original analysis was conducted correctly. Replicability refers to obtaining consistent results across studies aimed at answering the same scientific question, each of which has obtained its own data [1].
The importance of this distinction has been formally recognized by major scientific bodies. At the request of Congress, the National Academies of Sciences, Engineering, and Medicine (NASEM) conducted a study to evaluate these issues, highlighting that reproducibility is computationally focused, while replicability addresses the robustness of scientific findings [2] [1]. This guide explores these concepts within computational biomedicine, providing a framework for researchers, scientists, and drug development professionals to enhance the rigor of their work.
Defining the Framework: Reproducibility vs. Replicability
Terminological Challenges and Consensus
The scientific community has historically used the terms "reproducibility" and "replicability" in inconsistent and even contradictory ways across disciplines [2]. As identified in the NASEM report, this confusion primarily stems from three distinct usage patterns:
- Usage A: The terms are used with no distinction between them.
- Usage B1: "Reproducibility" refers to using the original researcher's data and code to regenerate results, while "replicability" refers to a researcher collecting new data to arrive at the same scientific findings.
- Usage B2: "Reproducibility" refers to independent researchers arriving at the same results using their own data and methods, while "replicability" refers to a different team arriving at the same results using the original author's artifacts [2].
The NASEM report provides clarity by establishing standardized definitions, which are adopted throughout this guide and summarized in the table below.
Comparative Definitions
| Concept | Core Definition | Key Question | Primary Goal | Typical Inputs |
|---|---|---|---|---|
| Reproducibility | Obtaining consistent computational results using the same input data, computational steps, methods, code, and conditions of analysis [1]. | "Can we exactly recompute the reported results from the same data and code?" | Verify the computational integrity and transparency of the original analysis [3]. | Original data + original code/methods |
| Replicability | Obtaining consistent results across studies aimed at the same scientific question, each of which has obtained its own data [1]. | "Do the findings hold up when tested on new data or in a different context?" | Confirm the robustness, generalizability, and validity of the scientific finding [3]. | New data + similar methods |
This relationship is foundational. Reproducibility is a prerequisite for replicability; if a result cannot be reproduced, there is little basis for evaluating its validity through replication [4].
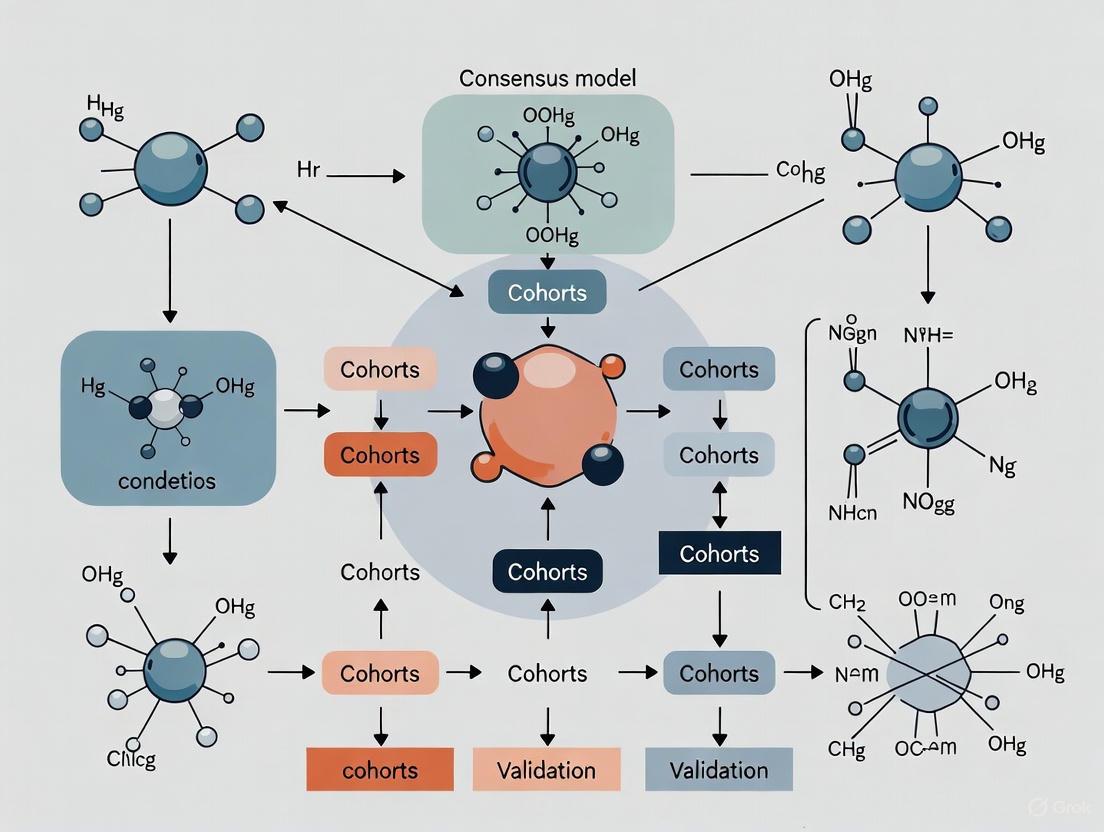
The Reproducibility and Replicability Workflow
The following diagram illustrates the typical sequential workflow for validating computational findings, from initial discovery through reproduction and replication, highlighting the distinct inputs and goals at each stage.
Case Study: Replicability in Brain Signature Research
Experimental Protocol and Methodology
A 2023 study on "brain signatures of cognition" provides a robust example of replicability in computational biomedicine [5]. The researchers aimed to develop and validate a data-driven method for identifying key brain regions associated with specific cognitive functions.
The experimental workflow involved a multi-cohort, cross-validation design, which can be broken down into the following key stages:
- Discovery of Consensus Signatures: In each of two independent discovery cohorts, researchers repeatedly (40 times) randomly selected subsets of 400 participants. For each subset, they computed associations between regional brain gray matter thickness and two behavioral domains: neuropsychological and everyday cognition memory. They then generated spatial overlap frequency maps from these iterations and defined the most frequently associated regions as "consensus" signature masks [5].
- Validation of Replicability: The core of the replicability test was performed using completely separate validation datasets that were not used in the discovery phase. The researchers evaluated whether the consensus signature models derived in the discovery phase showed consistent model fits and maintained their explanatory power for predicting behavioral outcomes in the new cohorts. The analysis compared the performance of these data-driven signature models against other theory-based models [5].
Key Quantitative Findings
The study successfully demonstrated a high degree of replicability, a critical step for establishing these brain signatures as robust measures.
| Validation Metric | Finding | Implication for Replicability |
|---|---|---|
| Spatial Convergence | Convergent consensus signature regions were identified across cohorts [5]. | The brain-behavior relationships identified were not flukes of a single sample. |
| Model Fit Correlation | Consensus signature model fits were "highly correlated" across 50 random subsets of each validation cohort [5]. | The predictive model itself was stable and reliable when applied to new data from similar populations. |
| Explanatory Power | Signature models "outperformed other commonly used measures" in full-cohort comparisons [5]. | The replicable models provided a superior explanation of the cognitive outcomes compared to existing approaches. |
This study exemplifies the "replicability consensus model fits validation cohorts research" context, moving beyond a single discovery dataset to demonstrate that the findings are stable and generalizable.
Case Study: Reproducibility in Real-World Evidence
Experimental Protocol and Methodology
A large-scale 2022 study in Nature Communications systematically evaluated the reproducibility of 150 real-world evidence (RWE) studies used to inform regulatory and coverage decisions [4]. These studies analyze clinical practice data to assess the effects of medical products.
The reproduction protocol was designed to be independent and blinded:
- Study Identification: A systematic, random sample of 250 RWE studies fitting pre-specified parameters was identified.
- Independent Reproduction: For 150 of these studies, researchers independently attempted to reproduce the study population and primary outcome findings. This was done using the same underlying healthcare databases as the original authors.
- Method Application: The reproduction team applied the methods described in the original papers, appendices, and other public materials.
- Blinded Assumptions: When study parameters were not fully reported, the reproduction team made informed assumptions while blinded to the original study's findings to avoid bias [4].
Key Quantitative Findings on Reproducibility
The results provide a unique, large-scale insight into the state of reproducibility in the field.
| Reproduction Aspect | Result | Interpretation |
|---|---|---|
| Overall Effect Size Correlation | Original and reproduction effect sizes were strongly correlated (Pearson’s r = 0.85) [4]. | Indicates a generally strong but imperfect level of reproducibility across a large number of studies. |
| Relative Effect Magnitude | Median relative effect (e.g., HR~original~/HR~reproduction~) = 1.0 [IQR: 0.9, 1.1], Range: [0.3, 2.1] [4]. | The central tendency was excellent, but a subset of results showed significant divergence. |
| Population Size Reproduction | Relative sample size (original/reproduction) median = 0.9 [IQR: 0.7, 1.3] [4]. | For 21% of studies, the reproduced cohort size was less than half or more than double the original, highlighting reporting ambiguities. |
| Clarity of Reporting | The median number of methodological categories requiring assumptions was 4 out of 6 for comparative studies [4]. | Incomplete reporting of key parameters (e.g., exposure duration algorithms, covariate definitions) was the primary barrier to perfect reproducibility. |
The Scientist's Toolkit: Essential Research Reagents for R&R
Achieving reproducibility and replicability requires more than just careful analysis; it depends on a ecosystem of tools and practices. The table below details key "research reagent solutions" essential for robust computational research in biomedicine.
| Tool Category | Specific Examples & Functions | Role in Enhancing R&R |
|---|---|---|
| Data & Model Standards | MIBBI (Minimum Information for Biological and Biomedical Investigations) checklists [6], BioPAX (pathway data), PSI-MI (proteomics) [6]. | Standardizes data and model reporting, enabling other researchers to understand, reuse, and replicate the components of a study. |
| Version-Controlled Code & Data | Public sharing of analysis code and data via repositories (e.g., GitHub, Zenodo) [2] [6]. | The fundamental requirement for reproducibility, allowing others to verify the computational analysis. |
| Declarative Modeling Languages | Standardized model description languages (e.g., SBML, CellML) [6]. | Facilitates model sharing and reuse across different simulation platforms, aiding both reproducibility and replicability. |
| Workflow Management Systems | Galaxy [6], Workflow4Ever project [6]. | Captures and shares the entire analytical pipeline, reducing "in-house script" ambiguity and ensuring reproducibility. |
| Software Ontologies | Software Ontology (SWO) for describing software tasks and data flows [6]. | Helps clarify if the same scientific question is being asked when different software tools are used, supporting replicability. |
In computational biomedicine, reproducibility (using the same data and methods) and replicability (using new data and similar methods) are not interchangeable concepts but are complementary pillars of rigorous and credible science. The consensus, as detailed by the National Academies, provides a clear framework for the field [2] [1]. As evidenced by the case studies, achieving these standards requires a concerted effort involving precise methodology, transparent reporting, and the adoption of shared tools and practices. For researchers and drug development professionals, rigorously demonstrating both reproducibility and replicability is paramount for building a reliable evidence base that can confidently inform clinical and regulatory decisions.
The credibility of scientific research across various disciplines has been fundamentally challenged by what is now known as the "replicability crisis." This crisis emerged from numerous high-profile failures to reproduce landmark studies, particularly in psychology and medicine, prompting a systemic reevaluation of research practices. In response, the scientific community has initiated large-scale, collaborative projects specifically designed to empirically assess the reproducibility and robustness of published findings. These projects systematically re-test key findings using predefined methodologies, often in larger, more diverse samples, and with greater statistical power than the original studies. The emergence of these projects represents a paradigm shift toward prioritizing transparency, rigor, and self-correction in science. This guide objectively compares the protocols and outcomes of major replication efforts across psychology and medicine, framing the results within a broader thesis on replicability consensus model fits validation cohorts research. For researchers and drug development professionals, understanding these findings is crucial for designing robust studies, interpreting the published literature, and developing reproducible and useful measures for modeling complex biological and behavioral domains [7].
Comparative Analysis of Large-Scale Replication Projects
Large-scale replication initiatives have now been conducted across multiple scientific fields, providing a quantitative basis for comparing replicability. The table below summarizes the objectives and key findings from several major projects.
Table 1: Overview of Large-Scale Replication Projects
| Project Name | Field/Topic | Key Finding/Objective | Status |
|---|---|---|---|
| Reproducibility Project: Psychology [8] | Psychology | A large-scale collaboration to replicate 100 experimental and correlational studies published in three psychology journals. | Completed |
| Many Labs 1-5 [8] | Psychology | A series of projects investigating the variability in replicability of specific effects across different samples and settings. | Completed |
| Reproducibility Project: Cancer [8] | Medicine (Preclinical) | Focused on replicating important results from preclinical cancer biology studies. | Completed |
| REPEAT Initiative [4] [8] | Healthcare (RWE) | A systematic evaluation of the reproducibility of real-world evidence (RWE) studies used to inform regulatory and coverage decisions. | Completed |
| CORE [8] | Judgment and Decision Making | Replication studies in the field of judgment and decision-making. | Ongoing |
| Many Babies 1 [8] | Developmental Psychology | A collaborative effort to replicate foundational findings in infant cognition and development. | Ongoing |
| Sports Sciences Replications [8] | Sports Sciences | A centre dedicated to replicating findings in the field of sports science. | Ongoing |
The outcomes of these projects reveal a spectrum of replicability. In the Reproducibility Project: Psychology, only 36% of the replications yielded significant results, and the effect sizes of the replicated studies were on average half the magnitude of the original effects [8]. This contrasts with findings from the REPEAT Initiative in healthcare, which demonstrated a stronger correlation between original and reproduced results. In REPEAT, which reproduced 150 RWE studies, the original and reproduction effect sizes were positively correlated (Pearson’s correlation = 0.85). The median relative magnitude of effect (e.g., hazard ratio~original~/hazard ratio~reproduction~) was 1.0, with an interquartile range of [0.9, 1.1] [4]. This suggests that while the majority of RWE results were closely reproduced, a subset showed significant divergence, underscoring that reproducibility is not guaranteed even in data-rich observational fields.
Detailed Experimental Protocols from Key Replication Efforts
Protocol: The "REPEAT Initiative" for Real-World Evidence Validation
The REPEAT Initiative provides a rigorous methodology for assessing the reproducibility of RWE studies, which are critical for regulatory and coverage decisions in drug development [4].
- Aim: To evaluate the independent reproducibility of 150 published RWE studies using the same healthcare databases as the original investigators.
- Experimental Workflow:
- Systematic Sampling: A large, random sample of RWE studies fitting pre-specified parameters was systematically identified.
- Blinded Reproduction: Reproduction teams, blinded to the original studies' results, attempted to reconstruct the study population and analyze the primary outcome by applying the methods described in the original publications and appendices.
- Assumption Logging: For study parameters that were not explicitly reported (e.g., detailed algorithms for defining exposure duration or covariate measurement), the reproduction team documented and made informed assumptions. This process directly tested the clarity of reporting.
- Outcome Comparison: The reproduced population sizes, baseline characteristics, and outcome effect sizes (e.g., hazard ratios) were quantitatively compared to the original published results.
- Key Metrics:
- Relative sample size (original/reproduction).
- Difference in prevalence of baseline characteristics (original—reproduction).
- Relative magnitude of effect (e.g., hazard ratio~original~/hazard ratio~reproduction~).
The following diagram illustrates the core workflow of the REPEAT Initiative's validation process.
Protocol: Brain Signature Validation using Consensus Model Fits in Validation Cohorts
Research in neuroscience has developed sophisticated methods for creating and validating brain signatures of cognition, which serve as a prime example of replicability consensus model fits validation cohorts research [7].
- Aim: To derive and validate robust, data-driven brain signatures (e.g., of episodic memory) that replicate across independent cohorts, moving beyond theory-driven approaches.
- Experimental Workflow:
- Discovery in Multiple Subsets: In discovery cohorts (e.g., n=578 from UCD and n=831 from ADNI 3), regional brain gray matter thickness associations with a behavioral outcome (e.g., neuropsychological memory) are computed not once, but in 40 randomly selected discovery subsets of size 400. This step leverages multiple discovery set generation to enhance robustness.
- Consensus Mask Generation: Spatial overlap frequency maps are generated from these multiple discovery runs. Regions that are consistently selected as significant across the majority of subsets are defined as a "consensus" signature mask.
- Validation in Separate Cohorts: The derived consensus signature is then applied to completely separate validation cohorts (e.g., n=348 from UCD and n=435 from ADNI 1) that were not used in the discovery phase.
- Model Fit Evaluation: The replicability of the consensus model's fit to the behavioral outcome is evaluated in 50 random subsets of each validation cohort. Its explanatory power is compared against competing theory-based models.
- Key Metrics:
- Spatial convergence of consensus signature regions.
- Correlation of consensus signature model fits across validation subsets.
- Explanatory power (e.g., R²) compared to other models.
The multi-cohort, multi-validation design of this protocol is captured in the diagram below.
The Scientist's Toolkit: Essential Reagents for Replication Research
Successful replication and validation research relies on a set of key "reagents" or resources beyond traditional laboratory materials. The following table details these essential components for researchers designing or executing replication studies.
Table 2: Key Research Reagent Solutions for Replication and Validation Studies
| Item/Resource | Function in Replication Research | Example Use Case |
|---|---|---|
| Validation Cohorts | Independent datasets, separate from discovery cohorts, used to test the robustness and generalizability of a model or finding. | Used in brain signature research to evaluate if a model derived in one population predicts outcomes in another [7]. |
| High-Quality Healthcare Databases | Large, longitudinal datasets from clinical practice used to generate and test Real-World Evidence (RWE). | The REPEAT Initiative used such databases to reproduce study findings on treatment effects [4]. |
| Consensus Model Fits | A statistical approach that aggregates results from multiple models or subsets to create a more robust and reproducible final model. | Used to define robust brain signatures by aggregating features consistently associated with an outcome across many discovery subsets [7]. |
| Standardized Reporting Guidelines | Frameworks (e.g., CONSORT, STROBE) that improve methodological transparency by ensuring all critical design and analytic parameters are reported. | Lack of adherence to such guidelines was a key factor leading to irreproducible RWE studies, as critical parameters were missing [4]. |
| Pre-registration Platforms | Public repositories (e.g., OSF, ClinicalTrials.gov) where research hypotheses and analysis plans are documented prior to data collection. | Mitigates bias and distinguishes confirmatory from exploratory research, a core practice in many large-scale replication projects [8]. |
Quantitative Results from Replication Validations
The outcomes of large-scale replication projects provide hard data on the state of reproducibility. The following table synthesizes key quantitative results from major efforts, offering a clear comparison of replicability across fields.
Table 3: Quantitative Outcomes from Major Replication Projects
| Project | Primary Quantitative Outcome | Result Summary | Implication |
|---|---|---|---|
| REPEAT Initiative (RWE) [4] | Correlation between original and reproduced effect sizes. | Pearson’s correlation = 0.85. | Strong positive relationship with room for improvement. |
| REPEAT Initiative (RWE) [4] | Relative magnitude of effect (Original/Reproduction). | Median: 1.0; IQR: [0.9, 1.1]; Range: [0.3, 2.1]. | Majority of results closely reproduced, but a subset diverged significantly. |
| REPEAT Initiative (RWE) [4] | Relative sample size (Original/Reproduction). | Median: 0.9 (Comparative), 0.9 (Descriptive); IQR: [0.7, 1.3]. | For 21% of studies, reproduction size was <½ or >2x original, indicating population definition challenges. |
| Brain Signature Validation [7] | Correlation of consensus model fits in validation subsets. | Model fits were "highly correlated" across 50 random validation subsets. | High replicability of the validated model's performance was achieved. |
| Brain Signature Validation [7] | Model performance vs. theory-based models. | Signature models "outperformed other commonly used measures" in explanatory power. | Data-driven, validated models can provide more complete accounts of brain-behavior associations. |
The collective evidence from large-scale replication projects underscores a critical message: reproducibility is achievable but not automatic. It is a measurable outcome that depends critically on methodological rigor, transparent reporting, and the use of robust validation frameworks. The higher correlation and closer effect size alignment observed in the REPEAT Initiative, compared to earlier psychology projects, may reflect both the nature of the data and an evolving scientific culture increasingly attuned to these issues. The successful application of consensus model fits and independent validation cohorts in neuroscience illustrates a proactive methodological shift designed to build replicability directly into the discovery process.
For the research community, the path forward is clear. Prioritizing transparent reporting of all methodological parameters, from cohort entry definitions to analytic code, is non-negotiable for enabling independent reproducibility [4]. Embracing practices like pre-registration and data sharing, as seen in the projects listed on the Replication Hub [8], is essential. Furthermore, adopting sophisticated validation architectures, such as consensus modeling and hold-out validation cohorts, will help ensure that the measures and models we develop are not only statistically significant but also reproducible and useful across different populations and settings [7]. For drug development professionals, these lessons are directly applicable to the evaluation of RWE and biomarker validation, ensuring that the evidence base for regulatory and coverage decisions is as robust and reliable as possible.
In the pursuit of accurate predictive models, researchers and drug development professionals often find that a model that performs exceptionally well in initial studies fails catastrophically when applied to new data. This replication crisis stems primarily from two intertwined pitfalls: overfitting and sample-specific bias. Overfitting occurs when a model learns not only the underlying signal in the training data but also the noise and irrelevant details, rendering it incapable of generalizing to new datasets [9] [10]. Sample-specific bias arises when training data is not representative of the broader population, often due to limited sample size, demographic skew, or non-standardized data collection protocols [9] [11]. This guide objectively compares the performance of single, complex models against consensus and validated approaches, demonstrating through experimental data why rigorous validation frameworks are non-negotiable for replicable science.
Defining the Problem: Overfitting and Bias Explained
An overfit model is characterized by high accuracy on training data but poor performance on new, unseen data [9] [12]. This undesirable machine learning behavior is often driven by high model complexity relative to the amount of training data, noisy data, or training for too long on a single sample set [9].
The companion issue, sample-specific bias, introduces systematic errors. For instance, a model predicting academic performance trained primarily on one demographic may fail for other groups [9]. Similarly, an AI game agent might exploit a glitch in its specific training environment, a creative but fragile solution that fails in a corrected setting [10]. This underscores that a model can fail not just on random data, but on data from a slightly different distribution, which is common in real-world applications.
The Bias-Variance Tradeoff
The classical understanding of this problem is framed by the bias-variance tradeoff [10] [12].
- High Bias (Underfitting): The model is too simple to capture the underlying patterns in the data, leading to inaccurate predictions on both training and test data [9] [12].
- High Variance (Overfitting): The model is too complex, capturing noise in the training data and resulting in accurate predictions for training data but poor performance on new data [9] [12].
The conventional solution is to find a "sweet spot" between bias and variance [9] [10]. However, modern machine learning, particularly deep learning, has revealed phenomena that challenge this classical view, such as complex models that generalize well despite interpolating training data, suggesting our understanding of overfitting is still evolving [10].
Experimental Evidence: Case Studies of Model Failure and Success
The following case studies from recent biomedical research illustrate the severe consequences of overfitting and bias, and how rigorous validation protocols can mitigate them.
Case Study 1: Predicting Complications in Acute Leukemia
This study developed a model to predict severe complications in patients with acute leukemia, explicitly addressing overfitting risks through a robust validation framework [11].
Experimental Protocol:
- Objective: To develop and externally validate a machine-learning model for predicting severe complications within 90 days of induction chemotherapy [11].
- Data Cohorts: Retrospective electronic health record data from three tertiary haematology centres (2013–2024). The derivation cohort had 2,009 patients, and the external validation cohort had 861 patients [11].
- Predictor Selection: 42 candidate predictors were selected based on literature review and clinical relevance. Data preprocessing included multiple imputation for missing values, Winsorization of outliers, and correlation filtering to remove highly correlated features (|ρ| > 0.80) [11].
- Model Training: Five algorithms (Elastic-Net, Random Forest, XGBoost, LightGBM, and a multilayer perceptron) were trained using nested 5-fold cross-validation to tune hyperparameters and evaluate performance without overfitting the validation set [11].
- Validation Strategy: The model was tested on a temporally and geographically distinct external validation cohort, following TRIPOD-AI and PROBAST-AI guidelines [11].
Table 1: Performance of Machine Learning Models for Leukemia Complication Prediction
| Model | Derivation AUROC (Mean ± SD) | External Validation AUROC (95% CI) | Calibration Slope |
|---|---|---|---|
| LightGBM | 0.824 ± 0.008 | 0.801 (0.774–0.827) | 0.97 |
| XGBoost | Not Reported | 0.785 (0.757–0.813) | Not Reported |
| Random Forest | Not Reported | 0.776 (0.747–0.805) | Not Reported |
| Elastic-Net | Not Reported | 0.759 (0.729–0.789) | Not Reported |
| Multilayer Perceptron | Not Reported | 0.758 (0.728–0.788) | Not Reported |
The LightGBM model demonstrated the best performance, maintaining robust discrimination in external validation. Its excellent calibration (slope close to 1.0) indicates that its predicted probabilities closely match the observed outcomes, a critical feature for clinical decision-making [11]. The use of external validation, rather than just internal cross-validation, provided a true test of its generalizability.
Case Study 2: A Simplified Frailty Assessment Tool
This study developed a machine learning-based frailty tool, highlighting the importance of feature selection and multi-cohort validation to ensure simplicity and generalizability [13].
Experimental Protocol:
- Objective: To develop a clinically feasible frailty assessment tool that balances predictive accuracy with implementation simplicity [13].
- Data Cohorts: Multi-cohort study using data from NHANES (n=3,480), CHARLS (n=16,792), CHNS (n=6,035), and SYSU3 CKD (n=2,264) [13].
- Feature Selection: A systematic process using five complementary algorithms (LASSO, VSURF, Boruta, varSelRF, and RFE) was applied to 75 potential variables. Intersection analysis identified a minimal set of 8 core features consistently selected by all algorithms [13].
- Model Training: 12 machine learning algorithms were evaluated. The best-performing model was selected based on performance across training, internal validation, and external validation datasets [13].
- Validation Strategy: The model was externally validated on three independent cohorts for predicting frailty diagnosis, chronic kidney disease progression, cardiovascular events, and all-cause mortality [13].
Table 2: Performance of XGBoost Frailty Model Across Cohorts and Outcomes
| Validation Cohort | Outcome | AUROC (95% CI) | Comparison vs. Traditional Indices (p-value) |
|---|---|---|---|
| NHANES (Training) | Frailty Diagnosis | 0.963 (0.951–0.975) | Not Applicable |
| NHANES (Internal) | Frailty Diagnosis | 0.940 (0.924–0.956) | Not Applicable |
| CHARLS (External) | Frailty Diagnosis | 0.850 (0.832–0.868) | Not Applicable |
| SYSU3 CKD | CKD Progression | 0.916 | < 0.001 |
| SYSU3 CKD | Cardiovascular Events | 0.789 | < 0.001 |
| SYSU3 CKD | All-Cause Mortality | 0.767 (Time-dependent) | < 0.001 |
The XGBoost model, built on only 8 readily available clinical parameters, significantly outperformed traditional frailty indices across multiple health outcomes [13]. This demonstrates that rigorous feature selection can create simple, generalizable models without sacrificing predictive power. The decline in AUROC from training to external validation underscores the necessity of testing models on independent data.
The Validation Toolkit: Methodologies to Ensure Replicability
Detecting and preventing overfitting requires a systematic approach to model validation. Below are key techniques and their workflows.
Core Validation Techniques
- K-Fold Cross-Validation: This method partitions the dataset into K equally sized subsets (folds). The model is trained on K-1 folds and validated on the remaining fold. This process is repeated K times, with each fold used exactly once as the validation set. The final performance is averaged across all iterations [9] [14] [12].
- Hold-Out Validation with a Test Set: The dataset is split into training, validation, and test sets. The model is trained on the training set, its hyperparameters are tuned on the validation set, and its final performance is evaluated exactly once on the held-out test set [15].
- External Validation: The ultimate test of a model's generalizability is its performance on data collected from a different source, location, or time period, ideally as part of a multi-cohort study [11] [13].
- Regularization: Techniques like L1 (Lasso) and L2 (Ridge) regularization add a penalty term to the model's loss function, discouraging it from becoming overly complex and relying too heavily on any single feature [9] [10] [12].
- Ensembling: Methods like bagging (e.g., Random Forest) and boosting (e.g., XGBoost, LightGBM) combine predictions from multiple weaker models to create a more robust and accurate final model that is less prone to overfitting [9] [10].
The following workflow diagram illustrates how these techniques are integrated into a robust model development pipeline.
Key Performance Metrics for Validation
A comprehensive model assessment requires evaluating multiple aspects of performance [16].
Table 3: Key Metrics for Model Validation
| Aspect | Metric | Interpretation |
|---|---|---|
| Overall Performance | Brier Score | Measures the average squared difference between predicted probabilities and actual outcomes. Closer to 0 is better [16]. |
| Discrimination | Area Under the ROC Curve (AUC/AUROC) | Measures the model's ability to distinguish between classes. 0.5 = random, 1.0 = perfect discrimination [11] [16]. |
| Discrimination | Area Under the Precision-Recall Curve (AUPRC) | Particularly informative for imbalanced datasets, as it focuses on the performance of the positive (usually minority) class [11]. |
| Calibration | Calibration Slope & Intercept | Assesses the agreement between predicted probabilities and observed frequencies. A slope of 1 and intercept of 0 indicate perfect calibration [11] [16]. |
| Clinical Utility | Decision Curve Analysis (DCA) | Quantifies the net benefit of using the model for clinical decision-making across a range of probability thresholds [11] [17] [16]. |
The Scientist's Toolkit: Research Reagent Solutions
The following tools and reagents are essential for building and validating predictive models that stand up to the demands of replicable research.
Table 4: Essential Research Reagents and Tools
| Item | Function | Example Tools & Notes |
|---|---|---|
| Programming Environment | Provides the foundational language and libraries for data manipulation, model development, and analysis. | R (version 4.4.2) [17], Python with scikit-learn [15]. |
| Machine Learning Algorithms | The core models used to learn patterns from data. Comparing multiple algorithms is crucial. | LightGBM [11], XGBoost [13], Random Forest [11], Elastic-Net regression [11] [17]. |
| Feature Selection Algorithms | Identify the most predictive variables, reducing model complexity and overfitting potential. | LASSO regression [17], Boruta algorithm, Recursive Feature Elimination (RFE) [13]. |
| Model Validation Platforms | Tools that streamline the process of model comparison, validation, and visualization. | DataRobot [18], Scikit-learn, TensorFlow [14]. |
| Explainability Frameworks | Techniques to interpret "black-box" models, building trust and providing biological insights. | SHapley Additive exPlanations (SHAP) [11]. |
Key Insights and Best Practices for Robust Models
The evidence overwhelmingly shows that a single model developed and validated on a single dataset is highly likely to fail in practice. The path to replicable models requires a consensus on rigorous validation.
- Prioritize External Validation: Internal validation via cross-validation is necessary but insufficient. Models must be tested on externally held-out cohorts, preferably from different institutions or time periods, to prove their generalizability [11] [13].
- Embrace Simplicity with Rigor: A model with fewer, well-selected features is often more robust and clinically translatable than a complex model with hundreds of variables. Employ systematic feature selection to avoid overfitting [13].
- Report Comprehensive Metrics: Go beyond the AUROC. A model must also be well-calibrated (its predictions must match reality) and provide a net clinical benefit, as shown by decision curve analysis [11] [16].
- Utilize Ensemble Methods: For complex problems, ensemble methods like gradient boosting (XGBoost, LightGBM) often provide superior and more robust performance compared to single models by reducing variance [11] [13].
- Adopt a Validation-First Mindset: The validation strategy should be designed before model development begins, incorporating techniques like nested cross-validation to prevent over-optimism and data leakage [11] [14].
In conclusion, the failure of single models is not an inevitability but a consequence of inadequate validation. By adopting a consensus framework that demands external validation, transparent reporting, and a focus on clinical utility, researchers can build predictive tools that truly replicate and deliver on their promise in drug development and beyond.
In scientific research and forecasting, a multi-model ensemble (MME) is a technique that combines the outputs of multiple, independent models to produce a single, more robust prediction or projection. The fundamental thesis is that a consensus drawn from diverse models is more likely to capture the underlying truth and generalize effectively to new data, such as validation cohorts, than any single "best" model. This guide explores the theoretical and empirical basis for this consensus, comparing the performance of ensemble means against individual models across diverse fields including hydrology, climate science, and healthcare.
Theoretical Foundations of Ensemble Robustness
The enhanced robustness of MMEs is not merely an empirical observation but is grounded in well-established statistical and theoretical principles.
- The Wisdom of Crowds: The core idea is that the aggregation of information from a group of independent, diverse, and decentralized models often yields a more accurate and stable estimate than that of any single member. In the context of climate science, this means that different models, with their unique structural representations of physical processes, sample the uncertainties in our understanding of the climate system [19].
- Error Cancellation: Individual models often contain specific biases and errors. When models are independent, their errors are frequently uncorrelated. By averaging model outputs, these individual biases can partially cancel each other out, leading to an ensemble mean with a lower overall error than the average error of the constituent models [20].
- Structural Uncertainty Quantification: A key source of uncertainty in predictions is "structural uncertainty," which arises from the different ways processes can be represented in a model. A multi-model ensemble directly samples this structural uncertainty. Relying on a single model ignores this uncertainty, while an MME provides a distribution of plausible outcomes, offering a more honest representation of forecast confidence [19].
Empirical Evidence: Cross-Domain Performance Comparison
Quantitative evidence from multiple scientific disciplines consistently demonstrates the superior performance and robustness of multi-model ensembles when validated on independent data.
Table 1: Performance of Multi-Model Ensembles Across Disciplines
| Field of Study | Ensemble Method | Performance Metric | Ensemble Result | Individual Model Results | Key Finding |
|---|---|---|---|---|---|
| Hydrology [20] | Arithmetic Mean (44 models) | Accuracy & Robustness | More accurate and robust; smaller performance degradation in validation | Performance degraded more significantly, especially with climate change | MME showed greater robustness to changing climate conditions between calibration and validation periods. |
| Climate Simulation [21] | Bayesian Model Averaging (5 models) | Kling-Gupta Efficiency (KGE) | Precipitation: 0.82Tmax: 0.65Tmin: 0.82 | Arithmetic Mean KGE:Precipitation: 0.59Tmax: 0.28Tmin: 0.45 | Performance-weighted ensemble (BMA) significantly outperformed simple averaging. |
| Colorectal Cancer Detection [22] | Stacked Ensemble (cfDNA fragmentomics) | Area Under Curve (AUC) | Validation AUC: 0.926 | N/A | The ensemble achieved high sensitivity across all cancer stages (Stage I: 94.4%, Stage IV: 100%). |
| ICU Readmission Prediction [23] | Custom Ensemble (iREAD) | AUROC (Internal Validation) | 48-hr Readmission: 0.771 | Outperformed all traditional scoring systems and conventional machine learning models (p<0.001) | Demonstrated superior generalizability in external validation cohorts. |
Experimental Protocols for Ensemble Construction
The process of building and validating a robust multi-model ensemble follows a systematic workflow. The diagram below outlines the key stages, from model selection to final validation.
The following protocols detail the critical methodologies cited in the research:
- Protocol 1: Large-Sample Hydrological Ensemble Testing - This evaluation of 44 conceptual hydrological models across 582 river basins highlights the importance of scale. The models were calibrated on a period (1980-1990) and validated on a much later period (2013-2014) with a long gap in between. This "differential split-sample" test was designed to stress-test model robustness under a changing climate. The key performance metric was the degradation in prediction accuracy between the calibration and validation periods, with the MME showing significantly less degradation than any single model [20].
- Protocol 2: Multi-Criteria Climate Model Ranking and Weighting - This study used a Multi-Criteria Decision-Making (MCDM) technique, TOPSIS, to rank 19 CMIP6 climate models. The models were evaluated against ERA5 reanalysis data using seven different error metrics (e.g., Kling-Gupta Efficiency, normalized root mean squared error) for different seasons and variables. This comprehensive ranking ensured that the final ensemble of top models was not biased by a single performance metric. The ensemble mean was then calculated using both a simple Arithmetic Mean (AM) and a performance-weighted Bayesian Model Averaging (BMA), with BMA demonstrating superior skill [21].
- Protocol 3: Stacked Ensemble for Medical Diagnosis - In this clinical study, a stacked ensemble model was built by integrating three distinct fragmentomics features from cell-free DNA using a machine learning meta-learner. The model was trained on a multi-center cohort and then validated on a completely independent cohort of patients. This rigorous validation on unseen data from different hospitals was critical to demonstrating that the model's high accuracy (AUC of 0.926) was generalizable and not a product of overfitting to the training data [22].
The Scientist's Toolkit: Essential Reagents for Ensemble Research
Table 2: Key Analytical Tools and Resources for Ensemble Modeling
| Tool/Resource Name | Function in Ensemble Research | Field of Application |
|---|---|---|
| MARRMoT Toolbox [20] | Provides 46 modular conceptual hydrological models for consistently testing and comparing a wide range of model structures. | Hydrology, Rainfall-Runoff Modeling |
| CAMELS Dataset [20] | A large-sample dataset providing standardized meteorological forcing and runoff data for hundreds of basins, enabling robust large-sample studies. | Hydrology, Environmental Science |
| CMIP6 Data Portal [21] | The primary repository for a vast suite of global climate model outputs, forming the basis for most modern climate multi-model ensembles. | Climate Science, Meteorology |
| ERA5 Reanalysis Data [21] | A high-quality, globally complete climate dataset that serves as a common benchmark ("observed data") for evaluating and weighting climate models. | Climate Science, Geophysics |
| TOPSIS Method [21] | A multi-criteria decision-making technique used to rank models based on their performance across multiple, often conflicting, error metrics. | General Model Evaluation |
| Bayesian Model Averaging (BMA) [21] | A sophisticated ensemble method that assigns weights to individual models based on their probabilistic likelihood and historical performance. | Climate, Statistics, Machine Learning |
| SHAP (SHapley Additive exPlanations) [24] | An interpretable machine learning method used to explain the output of an ensemble model by quantifying the contribution of each input feature. | Machine Learning, Healthcare AI |
Advanced Ensemble Methodologies
Beyond simple averaging, advanced techniques are being developed to further enhance the robustness and adaptability of ensembles, particularly for complex, non-stationary systems.
- Dynamic Weighting with Reinforcement Learning: Unlike ensembles with static weights, this approach uses reinforcement learning (e.g., the soft actor-critic framework) to dynamically adjust the contribution of each base model in response to changing environmental conditions. This has shown significant promise in ocean wave forecasting, where the optimal model mix can change with sea state, leading to more accurate and stable predictions than any single model or static ensemble [25].
- Addressing Model Dependence: A critical theoretical challenge is that models within an ensemble are often not fully independent, as they share literature, ideas, and code. The presence of these "model families" can bias the ensemble if not accounted for. Research emphasizes that quantifying this dependence and using weighting or sub-selection strategies that consider both model performance and independence is key to a sound interpretation of ensemble projections [19].
The consensus derived from multi-model ensembles provides a more robust and reliable foundation for scientific prediction and decision-making than single-model approaches. The theoretical basis—rooted in error cancellation and structural uncertainty quantification—is strongly supported by empirical evidence across hydrology, climate science, and clinical research. The critical factor for success is a rigorous validation protocol that tests the ensemble on independent data, ensuring that the observed robustness translates to real-world generalizability. As ensemble methods evolve with techniques like dynamic weighting and sophisticated dependence-aware averaging, their role in enhancing the replicability and reliability of scientific models will only grow.
In the evolving landscape of scientific research, particularly within drug development and biomedical sciences, the validation of findings through replication has become a cornerstone of credibility and progress. Replication serves as the critical process through which the scientific community verifies the reliability and validity of reported findings, ensuring that research built upon these foundations is sound. A nuanced understanding of replication reveals three distinct methodologies: direct, conceptual, and computational replication. Each approach serves unique functions in the scientific ecosystem, from verifying basic reliability to exploring the boundary conditions of findings and leveraging in silico technologies for validation.
The ongoing "replication crisis" in various scientific fields has heightened awareness of the importance of robust replication practices. Within this context, direct replication focuses on assessing reliability through repetition, conceptual replication explores the generality of findings across varied operationalizations, and computational replication emerges as a transformative approach leveraging virtual models and simulations. This guide provides an objective comparison of these replication methodologies, their experimental protocols, and their application within modern research paradigms, particularly focusing on the validation of consensus models and cohorts in biomedical research.
Defining the Replication Landscape
Direct Replication
Direct replication (sometimes termed "exact" or "close" replication) involves repeating a study using the same methods, procedures, and measurements as the original investigation [26]. The primary function is to assess the reliability of the original findings by determining whether they can be consistently reproduced under identical conditions [27]. While a purely "exact" replication may be theoretically impossible due to inevitable contextual differences, researchers strive to maintain the same operationalizations of variables and experimental procedures [26].
A key insight from recent literature is that direct replication serves functions beyond mere reliability checking. It can uncover important contextualities inherent in research findings, leading to a richer understanding of what results truly imply [27]. For instance, identical numerical results in direct replications may sometimes mask differential effects of biases across different data sources, highlighting the risk of asymmetric evaluation in scientific assessment [27].
Conceptual Replication
Conceptual replication tests the same fundamental hypothesis or theory as the original study but employs different methodological approaches to operationalize the key variables [26]. This form of replication aims to determine whether a finding holds across varied measurements, populations, or contexts, thereby assessing its generality and robustness.
Where direct replication seeks to answer "Can this finding be reproduced under the same conditions?", conceptual replication asks "Does this phenomenon manifest across different operationalizations and contexts?" This approach is particularly valuable for addressing concerns about systematic error that might affect both the original and direct replication attempts [26]. By deliberately sampling for heterogeneity in methods, conceptual replication can reveal whether a finding represents a general principle or is limited to specific methodological conditions.
Computational Replication
Computational replication represents a paradigm shift in verification methodologies, leveraging computer simulations, virtual models, and artificial intelligence to validate research findings. In biomedical contexts, this approach includes in silico trials that use "individualized computer simulation used in the development or regulatory evaluation of a medicinal product, device, or intervention" [28]. This methodology is rapidly evolving from a supplemental technique to a central pillar of biomedical research, alongside traditional in vivo, in vitro, and ex vivo approaches [29].
The rise of computational replication is facilitated by advances in AI, high-performance computing, and regulatory science. The FDA's 2025 announcement phasing out mandatory animal testing for many drug types signals a paradigm shift toward in silico methodologies [29]. Computational replication enables researchers to simulate thousands of virtual patients, test interventions across diverse demographic profiles, and model biological systems with astonishing granularity, all while reducing ethical concerns and resource requirements associated with traditional methods.
Comparative Analysis of Replication Methodologies
Table 1: Comparison of Replication Types Across Key Dimensions
| Dimension | Direct Replication | Conceptual Replication | Computational Replication |
|---|---|---|---|
| Primary Goal | Assess reliability through identical repetition | Test generality across varied operationalizations | Validate through simulation and modeling |
| Methodological Approach | Same procedures, measurements, and analyses | Different methods testing same theoretical construct | Computer simulations, digital twins, AI models |
| Key Strength | Identifies false positives and methodological artifacts | Establishes robustness and theoretical validity | Enables rapid, scalable, cost-effective validation |
| Limitations | Susceptible to same systematic errors as original | Difficult to interpret failures; may test different constructs | Model validity dependent on input data and assumptions |
| Resource Requirements | Moderate to high (new data collection often needed) | High (requires developing new methodologies) | High initial investment, lower marginal costs |
| Typical Timeframe | Medium-term | Long-term | Rapid once models are established |
| Regulatory Acceptance | Well-established | Well-established | Growing rapidly (FDA, EMA) |
| Role in Consensus Model Validation | Tests reliability of original findings | Explores boundary conditions and generalizability | Enables validation across virtual cohorts |
Table 2: Quantitative Comparison of Replication Impact and Outcomes
| Performance Metric | Direct Replication | Conceptual Replication | Computational Replication |
|---|---|---|---|
| Estimated Overturn Rate | 3.5-11% of studies [30] | Not systematically quantified | Varies by model accuracy |
| Citation Impact After Failure | ~35% reduction after few years [30] | Dependent on clarity of conceptual linkage | Not yet established |
| Typical Cost Range | Similar to original study | Often exceeds original study | $3.76B global market (2023) [31] |
| Time Efficiency | Similar to original study | Often exceeds original study | VICTRE study: 1.75 vs. 4 years [28] |
| Downstream Attention Averted | Up to 35% of citations [30] | Potentially broader impact | Prevents futile research directions earlier |
Experimental Protocols and Methodologies
Protocol for Direct Replication
A rigorous direct replication requires meticulous attention to methodological fidelity while acknowledging inevitable contextual differences:
Protocol Verification: Obtain and thoroughly review the original study materials, including methods, measures, procedures, and analysis plans. When available, examine original data and code to identify potential ambiguities in the reported methodology.
Contextual Transparency: Document all aspects of the replication context that may differ from the original study, including laboratory environment, researcher backgrounds, participant populations, and temporal factors. As Satyanarayan et al. note, design elements of visualizations (and by extension, all methodological elements) can influence viewer assumptions about source and trustworthiness [32].
Implementation Fidelity: Execute the study following the original procedures as closely as possible while maintaining ethical standards. This includes using the same inclusion/exclusion criteria, experimental materials, equipment specifications, and data collection procedures.
Analytical Consistency: Apply the original analytical approach, including statistical methods, data transformation procedures, and outcome metrics. Preregister any additional analyses to distinguish confirmatory from exploratory work.
Reporting Standards: Clearly report all deviations from the original protocol and discuss their potential impact on findings. The replication report should enable readers to understand both the methodological similarities and differences relative to the original study.
Protocol for Conceptual Replication
Conceptual replication requires careful translation of theoretical constructs into alternative operationalizations:
Construct Mapping: Clearly identify the theoretical constructs examined in the original study and develop alternative methods for operationalizing these constructs. This requires deep theoretical understanding to ensure the new operationalizations adequately capture the same underlying phenomenon.
Methodological Diversity: Design studies that vary key methodological features while maintaining conceptual equivalence. This might include using different measurement instruments, participant populations, experimental contexts, or data collection modalities.
Falsifiability Considerations: Define clear criteria for what would constitute successful versus unsuccessful replication. Unlike direct replication where success is typically defined as obtaining statistically similar effects, conceptual replication success may involve demonstrating similar patterns across methodologically diverse contexts.
Convergent Validation: Incorporate multiple methodological variations within a single research program or across collaborating labs to establish a pattern of convergent findings. As Feest argues, systematic error remains a concern in replication, necessitating thoughtful design [26].
Interpretive Framework: Develop a framework for interpreting both consistent and inconsistent findings across methodological variations. Inconsistencies may reveal theoretically important boundary conditions rather than simple replication failures.
Protocol for Computational Replication
Computational replication, particularly using in silico trials, follows a distinct protocol focused on model development and validation:
Figure 1: Computational Replication Workflow for In Silico Trials
Data Integration and Model Development: Collect and integrate diverse real-world data sources to inform model parameters. This includes clinical trial data, electronic health records, biomedical literature, and omics data. Develop mechanistic or AI-driven models that accurately represent the biological system or intervention being studied.
Virtual Cohort Generation: Create in silico cohorts that reflect the demographic, physiological, and pathological diversity of target populations. The EU-Horizon funded SIMCor project, for example, has developed statistical web applications specifically for validating virtual cohorts against real datasets [28].
Simulation Execution: Run multiple iterations of the virtual experiment across the simulated cohort to assess outcomes under varied conditions. This may include testing different dosing regimens, patient characteristics, or treatment protocols.
Validation Against Empirical Data: Compare simulation outputs with real-world evidence from traditional studies. Use statistical techniques to quantify the concordance between virtual and actual outcomes. The SIMCor tool provides implemented statistical techniques for comparing virtual cohorts with real datasets [28].
Regulatory Documentation: Prepare comprehensive documentation of model assumptions, parameters, validation procedures, and results for regulatory submission. Agencies like the FDA and EMA increasingly accept in silico evidence, particularly through Model-Informed Drug Development (MIDD) programs [29] [31].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Research Reagent Solutions for Replication Studies
| Tool Category | Specific Solutions | Function in Replication | Applicable Replication Types |
|---|---|---|---|
| Statistical Platforms | R-statistical environment with Shiny [28] | Validates virtual cohorts and analyzes in-silico trials | Computational |
| Simulation Software | BIOVIA, SIMULIA [31] | Virtual device testing and biological modeling | Computational |
| Digital Twin Platforms | Unlearn.ai, InSilicoTrials Technologies [29] [31] | Creates virtual patient replicas for simulation | Computational |
| Toxicity Prediction | DeepTox, ProTox-3.0, ADMETlab [29] | Predicts drug toxicity and off-target effects | Computational, Direct |
| Protein Structure Prediction | AlphaFold [29] | Predicts protein folding for target validation | Conceptual, Computational |
| Validation Frameworks | Good Simulation Practice (GSP) | Standardizes model evaluation procedures | Computational |
| Data Visualization Tools | ColorBrewer, Tableau | Ensures accessible, interpretable results reporting | All types |
| Protocol Registration | OSF, ClinicalTrials.gov | Ensures transparency and reduces publication bias | All types |
Analysis of Quantitative Data and Outcomes
Success Rates and Impact Metrics
Recent meta-scientific research provides quantitative insights into replication outcomes across fields. Analysis of 110 replication reports from the Institute for Replication found that computational reproduction and robustness checks fully overturned a paper's conclusions approximately 3.5% of the time and substantially weakened them another 16.5% of the time [30]. When considering both fully overturned cases and half of the weakened cases, the estimated rate of genuine unreliability across the literature reaches approximately 11% [30].
The impact of failed replications on subsequent citation patterns reveals important information about scientific self-correction. Evidence suggests that failed replications lead to a ~10% reduction in citations in the first year after publication, stabilizing at a ~35% reduction after a few years [30]. This citation impact is crucial for calculating the return on investment of replication studies, as averted citations to flawed research represent saved resources that might otherwise have been wasted on fruitless research directions.
Economic Considerations in Replication
The economic case for replication funding hinges on comparing the costs of replication against the potential savings from averting research based on flawed findings. When targeted at recent, influential studies, replication can provide large returns, sometimes paying for itself many times over [30]. Analysis suggests that a well-calibrated replication program could productively spend about 1.4% of the NIH's annual budget before hitting negative returns relative to funding new science [30].
The economic advantage of computational replication is particularly striking. The VICTRE study demonstrated that in silico trials required only one-third of the resources and approximately 1.75 years compared to 4 years for a conventional trial [28]. The global in-silico clinical trials market, valued at USD 3.76 billion in 2023 and projected to reach USD 6.39 billion by 2033, reflects growing recognition of these efficiency gains [31].
Figure 2: Decision Framework for Selecting Replication Approaches
The contemporary research landscape demands a strategic approach to replication that leverages the complementary strengths of direct, conceptual, and computational methodologies. Direct replication remains essential for verifying the reliability of influential findings, particularly those informing policy or clinical practice. Conceptual replication provides critical insights into the generality and boundary conditions of phenomena. Computational replication offers transformative potential for accelerating validation while reducing costs and ethical concerns.
The most robust research programs strategically integrate these approaches, recognizing that they address different but complementary questions about scientific claims. Direct replication asks "Can we trust this specific finding?" Conceptual replication asks "How general is this phenomenon?" Computational replication asks "Can we model and predict this system?" Together, they form a comprehensive framework for establishing scientific credibility.
As computational methods continue to advance and gain regulatory acceptance, their role in the replication ecosystem will likely expand. However, rather than replacing traditional approaches, in silico methodologies will increasingly complement them, creating hybrid models of scientific validation that leverage the strengths of each paradigm. The researchers and drug development professionals who master this integrated approach will be best positioned to produce reliable, impactful science in the decades ahead.
Building Robust Consensus Models: From Data Curation to Implementation
High-dimensional data presents a significant challenge in biomedical research, particularly in genomics, transcriptomics, and clinical biomarker discovery. The selection of relevant features from thousands of potential variables is critical for building robust, interpretable, and clinically applicable predictive models. Within the context of replicability consensus model fits validation cohorts research, the choice of feature selection methodology directly impacts a model's ability to generalize beyond the initial discovery dataset and maintain predictive performance in independent validation cohorts.
This guide provides an objective comparison of three prominent feature selection approaches—LASSO regression, Random Forest-based selection, and the Boruta algorithm—examining their theoretical foundations, practical performance, and suitability for different research scenarios. Each method represents a distinct philosophical approach to the feature selection problem: LASSO employs embedded regularization within a linear framework, Random Forests use ensemble-based importance metrics, and Boruta implements a wrapper approach with statistical testing against random shadows. Understanding their comparative strengths and limitations is essential for constructing models that not only perform well initially but also maintain their predictive power across diverse populations and experimental conditions, thereby advancing replicable scientific discovery.
Methodological Foundations: Three Approaches to Feature Selection
LASSO (Least Absolute Shrinkage and Selection Operator)
LASSO regression operates as an embedded feature selection method that performs both variable selection and regularization through L1-penalization. By adding a penalty equal to the absolute value of the magnitude of coefficients, LASSO shrinks less important feature coefficients to zero, effectively removing them from the model [33] [34]. This results in a sparse, interpretable model that is particularly valuable when researchers hypothesize that only a subset of features has genuine predictive power. The method assumes linear relationships between features and outcomes and requires careful hyperparameter tuning (λ) to control the strength of regularization.
Random Forest Feature Importance
Random Forest algorithms provide feature importance measures through an embedded approach that calculates the mean decrease in impurity (Gini importance) across all trees in the ensemble [35]. Each time a split in a tree is based on a particular feature, the impurity decrease is recorded and averaged over all trees in the forest. Features that consistently provide larger decreases in impurity are deemed more important. This method naturally captures non-linear relationships and interactions without explicit specification, making it valuable for complex biological systems where linear assumptions may not hold.
Boruta Algorithm
The Boruta algorithm is a robust wrapper method built around Random Forest classification that identifies all relevant features—not just the most prominent ones [33] [36]. It works by creating shuffled copies of all original features (shadow features), training a Random Forest classifier on the extended dataset, and then comparing the importance of original features to the maximum importance of shadow features. Features with importance significantly greater than their shadow counterparts are deemed important, while those significantly less are rejected. This iterative process continues until all features are confirmed or rejected, or a predetermined limit is reached [36].
Performance Comparison Across Biomedical Applications
Table 1: Comparative Performance of Feature Selection Methods Across Different Biomedical Domains
| Application Domain | LASSO Performance | Random Forest Performance | Boruta Performance | Best Performing Model | Key Performance Metrics |
|---|---|---|---|---|---|
| Stroke Risk Prediction in Hypertension [33] | AUC: 0.716 | AUC: 0.626 | AUC: 0.716 | LASSO and Boruta (tie) | Area Under Curve (AUC) of ROC |
| Asthma Risk Prediction [34] | AUC: 0.66 | N/R | AUC: 0.64 | LASSO | Area Under Curve (AUC) of ROC |
| COVID-19 Mortality Prediction [35] | N/R | Accuracy: 0.89 with Hybrid Boruta | Accuracy: 0.89 (Hybrid Boruta-VI + RF) | Hybrid Boruta-VI + Random Forest | Accuracy, F1-score: 0.76, AUC: 0.95 |
| Diabetes Prediction [37] | N/R | N/R | Accuracy: 85.16% with LightGBM | Boruta + LightGBM | Accuracy, F1-score: 85.41%, 54.96% reduction in training time |
| DNA Methylation-based Telomere Length Estimation [38] | Moderate performance with prior feature selection | Variable performance | N/R | PCA + Elastic Net | Correlation: 0.295 on test set |
Table 2: Characteristics and Trade-offs of Feature Selection Methods
| Characteristic | LASSO | Random Forest Feature Importance | Boruta |
|---|---|---|---|
| Selection Type | Embedded | Embedded | Wrapper |
| Primary Strength | Produces sparse, interpretable models; handles correlated features | Captures non-linear relationships and interactions | Identifies all relevant features; robust against random fluctuations |
| Key Limitation | Assumes linear relationships; sensitive to hyperparameter tuning | May miss features weakly relevant individually; bias toward high-cardinality features | Computationally intensive; may select weakly relevant features |
| Interpretability | High (clear coefficient magnitudes) | Moderate (importance scores) | Moderate (binary important/not important) |
| Computational Load | Low to Moderate | Moderate | High (iterative process with multiple RF runs) |
| Stability | Moderate | Moderate to High | High (statistical testing against shadows) |
| Handling of Non-linearity | Poor (without explicit feature engineering) | Excellent | Excellent |
| Implementation Complexity | Low | Low to Moderate | Moderate |
Experimental Protocols and Workflows
Standard Boruta Implementation Protocol
The Boruta algorithm follows a meticulously defined iterative process to distinguish relevant features from noise [36]:
- Shadow Feature Creation: Duplicate all features in the dataset, shuffle their values to break correlations with the outcome, and prefix them with "shadow" for identification.
- Random Forest Training: Train a Random Forest classifier on the extended dataset containing both original and shadow features.
- Importance Comparison: Calculate the Z-score of importance for each original and shadow feature. Establish a threshold using the maximum importance score among shadow features.
- Statistical Testing: Perform a two-sided test of equality for each unassigned feature comparing its importance to the shadow maximum.
- Feature Classification:
- Features with importance significantly higher than the threshold are tagged as 'important'
- Features with importance significantly lower are deemed 'unimportant' and removed from consideration
- Iteration: Remove all shadow features and repeat the process until importance is assigned to all features or a predetermined iteration limit is reached.
LASSO Regression Protocol for Feature Selection
LASSO implementation follows a standardized workflow [33] [34]:
- Data Preprocessing: Standardize or normalize all features to ensure penalty terms are equally applied. For positive indicators, divide each value by the maximum value (X′ = X/max). For negative indicators, divide the minimum value by each observation (X′ = min/X).
- Parameter Tuning: Use k-fold cross-validation (typically 5- or 10-fold) to determine the optimal regularization parameter (λ) that minimizes cross-validation error.
- Model Fitting: Apply LASSO regression with the optimal λ to the entire training set, which will naturally shrink coefficients of less relevant features to zero.
- Feature Selection: Retain only features with non-zero coefficients in the final model.
- Validation: Assess model performance on held-out test data using AUC, accuracy, or other domain-appropriate metrics.
Hybrid Boruta-LASSO Workflow
Recent studies have explored combining Boruta and LASSO in sequential workflows [33]:
- Initial Feature Screening: Apply Boruta algorithm to identify a subset of potentially relevant features, removing clearly irrelevant variables.
- Secondary Regularization: Apply LASSO regression to the Boruta-selected feature subset for further refinement and coefficient shrinkage.
- Performance Validation: Evaluate the hybrid approach against individual methods using nested cross-validation or independent test sets.
Essential Research Reagents and Computational Tools
Table 3: Essential Research Reagents and Computational Tools for Feature Selection Implementation
| Tool/Resource | Function/Purpose | Implementation Examples |
|---|---|---|
| R Statistical Software | Primary environment for statistical computing and model implementation | glmnet package for LASSO [33] [34], Boruta package for Boruta algorithm [33] [36] |
| Python Scikit-learn | Machine learning library for model development and evaluation | LassoCV for LASSO, RandomForestClassifier for ensemble methods [35] |
| SHAP (SHapley Additive exPlanations) | Model interpretation framework for consistent feature importance values | TreeExplainer for Random Forest and Boruta interpretations [36] [37] |
| MLR3 Framework | Comprehensive machine learning framework for standardized evaluations | mlr3filters for filter-based feature selection methods [35] |
| Custom BorutaShap Implementation | Python implementation combining Boruta with SHAP importance | Enhanced feature selection with more consistent importance metrics [36] |
| Cross-Validation Frameworks | Robust performance estimation and hyperparameter tuning | k-fold (typically 5- or 10-fold) cross-validation for parameter optimization [33] [37] |
Discussion: Implications for Replicability and Validation Research
The comparative analysis of LASSO, Random Forest, and Boruta feature selection methods reveals critical considerations for researchers focused on replicability consensus model fits validation cohorts. Each method offers distinct advantages that may be appropriate for different research contexts within biomedical applications.
LASSO regression demonstrates strong performance in multiple clinical prediction tasks (AUC 0.716 for stroke risk, 0.66 for asthma) while providing sparse, interpretable models [33] [34]. Its linear framework produces coefficients that are directly interpretable as feature effects, facilitating biological interpretation and clinical translation. However, this linear assumption may limit its performance in capturing complex non-linear relationships prevalent in biological systems.
Random Forest-based feature importance, particularly when implemented through the Boruta algorithm, excels at identifying features involved in complex interactions without requiring a priori specification of these relationships. The superior performance of Boruta with LightGBM for diabetes prediction (85.16% accuracy) and Hybrid Boruta-VI with Random Forest for COVID-19 mortality prediction (AUC 0.95) demonstrates its capability in challenging prediction tasks [35] [37].
For replicability research, the stability of feature selection across study populations is paramount. Boruta's statistical testing against random shadows provides theoretical advantages for stability, though at increased computational cost. The hybrid Boruta-LASSO approach represents a promising direction, potentially leveraging Boruta's comprehensive screening followed by LASSO's regularization to produce sparse, stable feature sets [33].
Researchers should select feature selection methods aligned with their specific replicability goals: LASSO for interpretable linear models, Random Forest for capturing complexity, and Boruta for comprehensive feature identification. In all cases, validation across independent cohorts remains essential for establishing true replicability, as performance on training data may not generalize to diverse populations.
Multi-cohort studies have become a cornerstone of modern epidemiological and clinical research, enabling investigators to overcome the limitations of individual studies by increasing statistical power, enhancing generalizability, and addressing research questions that cannot be answered by single populations [39]. The integration of data from diverse geographic locations and populations allows researchers to explore rare exposures, understand gene-environment interactions, and investigate health disparities across different demographic groups [39]. However, the process of sourcing and harmonizing data from multiple cohorts presents significant methodological challenges that must be carefully addressed to ensure valid and reliable research findings.
The fundamental value of multi-cohort integration lies in its ability to generate more substantial clinical evidence by augmenting sample sizes, particularly critical for studying rare diseases or subgroup analyses where individual cohorts lack sufficient statistical power [40]. Furthermore, integrated databases provide the capability to examine questions when there is little heterogeneity in an exposure of interest within a single population or when investigating complex interactions between exposures and environmental factors [39]. Despite these clear benefits, researchers face substantial obstacles in harmonizing data collected across different studies with variable protocols, measurement tools, data structures, and terminologies [41].
This guide examines current methodologies for multi-cohort data harmonization, compares predominant approaches through experimental data, and provides practical frameworks for researchers embarking on such investigations, with particular emphasis on validation within the context of replicability consensus models.
Methodological Frameworks for Cohort Harmonization
Data Harmonization Approaches: Prospective vs. Retrospective
Data harmonization—the process of integrating data from separate sources into a single analyzable dataset—generally follows one of two temporal approaches, each with distinct advantages and limitations [39].
Prospective harmonization occurs before or during data collection and involves planning for future data integration by implementing common protocols, standardized instruments, and consistent variable definitions across participating cohorts. The Living in Full Health (LIFE) project and Cancer Prevention Project of Philadelphia (CAP3) integration exemplifies this approach, where working groups including epidemiologists, psychologists, and laboratory scientists collaboratively selected questions to form the basis of shared questionnaire instruments [39]. This forward-looking strategy typically results in higher quality harmonization with less information loss but requires early coordination and agreement among collaborating teams.
Retemporary harmonization occurs after data collection is complete and involves mapping existing variables from different cohorts to a common framework. This approach offers greater flexibility for integrating existing datasets but often involves compromises in variable comparability. As noted in harmonization research, "harmonisation is not an exact science," but sufficient comparability across datasets can be achieved with relatively little loss of informativeness [41]. The harmonization of neurodegeneration-related variables across four diverse population cohorts demonstrated that direct mapping was possible for 51% of variables, while others required algorithmic transformations or standardization procedures [41].
Technical Implementation: ETL Processes and Data Models
The technical implementation of data harmonization typically follows an Extraction, Transformation, and Load (ETL) process, which can be implemented using various data models and technical infrastructures [39] [40].
Table 1: Common Data Models for Cohort Harmonization
| Data Model | Primary Application | Key Features | Implementation Examples |
|---|---|---|---|
| C-Surv | Population cohorts | Four-level acyclic taxonomy; 18 data themes | DPUK, Dementias Platform Australia, ADDI Workbench |
| OMOP CDM | Electronic health records | Standardized clinical data structure | OHDSI community, Alzheimer's Disease cohorts |
| REDCap | Research data collection | HIPAA-compliant web application | LIFE-CAP3 integration, clinical research cohorts |
The ETL process begins with extraction of source data from participating cohorts, often facilitated by Application Programming Interfaces (APIs) in platforms like REDCap [39]. The transformation phase involves mapping variables to a common schema through direct mapping, algorithmic transformation, or standardization. In the LIFE-CAP3 integration, this involved creating a mapping table with source variables, destination variables, value recoding specifications, and inclusion flags [39]. Finally, the load phase transfers the harmonized data into a unified database, with automated processes running on scheduled intervals to update the integrated dataset as new data becomes available [39].
Quality assurance procedures are critical throughout the ETL pipeline, including routine cross-checks between source and harmonized data, logging of integration jobs, and prevention of direct data entry into the harmonized database to maintain integrity [39].
Diagram 1: Data Harmonization Workflow. This diagram illustrates the sequential phases of the data harmonization process, from initial preparation through ETL implementation to quality assurance.
Comparative Analysis of Harmonization Methodologies
Experimental Protocols and Performance Metrics
To objectively evaluate harmonization approaches, we examined several recent implementations across different research domains, analyzing their methodologies, variable coverage, and output quality.
Table 2: Multi-Cohort Harmonization Performance Comparison
| Study/Initiative | Cohorts Integrated | Variables Harmonized | Coverage Rate | Harmonization Strategy |
|---|---|---|---|---|
| LIFE-CAP3 Integration [39] | 2 (LIFE Jamaica, CAP3 US) | 23 questionnaire forms | 74% (>50% variables mapped) | Prospective, ETL with REDCap |
| Neurodegeneration Variables [41] | 4 diverse populations | 124 variables | 93% (complete/close correspondence) | Simple calibration, algorithmic transformation, z-standardization |
| AD Cohorts Harmonization [40] | Multiple international | 172 clinical concepts | Not specified | OMOP CDM-based, knowledge-driven |
| Frailty Assessment ML [13] | 4 (NHANES, CHARLS, CHNS, SYSU3) | 75 potential → 8 core features | Robust across cohorts | Feature selection + machine learning |
The LIFE-CAP3 integration demonstrated that prospective harmonization achieved good coverage, with 17 of 23 (74%) questionnaire forms successfully harmonizing more than 50% of their variables [39]. This approach leveraged REDCap's API capabilities to create an automated weekly harmonization process, with quality checks ensuring data consistency between source and integrated datasets.
In contrast, the neurodegeneration variable harmonization across four cohorts employed retrospective methods, achieving complete or close correspondence for 111 of 120 variables (93%) found in the datasets [41]. The remaining variables required marginal loss of granularity but remained harmonizable. This implementation utilized three primary strategies: simple calibration for direct mappings, algorithmic transformation for non-clinical questionnaire responses, and z-score standardization for cognitive performance measures [41].
Machine Learning Approaches for Feature Harmonization
An emerging approach utilizes machine learning for feature selection and harmonization, particularly valuable when integrating highly heterogeneous datasets. The frailty assessment development study systematically applied five feature selection algorithms (LASSO regression, VSURF, Boruta, varSelRF, and RFE) to 75 potential variables, identifying a minimal set of eight clinically available parameters that demonstrated robust predictive power across cohorts [13].
This methodology employed comparative evaluation of 12 machine learning algorithms, with Extreme Gradient Boosting (XGBoost) exhibiting superior performance across training, internal validation, and external validation datasets [13]. The resulting model significantly outperformed traditional frailty indices in predicting chronic kidney disease progression, cardiovascular events, and mortality, demonstrating the value of optimized variable selection in multi-cohort frameworks.
Validation in Replicability Consensus Models
External Validation Frameworks
Robust validation across multiple cohorts is essential for establishing replicability and generalizability of research findings. Multi-cohort benchmarking serves as a powerful tool for external validation of analytical models, particularly for artificial intelligence algorithms [42].
The chest radiography AI validation study exemplifies this approach, utilizing three clinically relevant cohorts that differed in patient positioning, reference standards, and reader expertise [42]. This design enabled comprehensive assessment of algorithm performance across diverse clinical scenarios, revealing variations that were not apparent in single-cohort validation. For instance, the "Infiltration" classifier performance was highly dependent on patient positioning, performing best in upright CXRs and worst in supine CXRs [42].
Similarly, the frailty assessment tool was validated through a multi-cohort design including NHANES, CHARLS, CHNS, and SYSU3 CKD cohorts, each contributing distinct populations and healthcare contexts [13]. This strategy enhances model generalizability and follows established practices for clinical prediction models.
Measuring Harmonization Success and Comparability
Evaluating harmonization success requires assessment of both technical execution and scientific utility. The LIFE-CAP3 integration evaluated their process by examining variable coverage and conducting preliminary analyses comparing age-adjusted prevalence of health conditions across cohorts, demonstrating regional differences that could inform disease hypotheses in the Black Diaspora [39].
The neurodegeneration harmonization project assessed utility by examining variable representation across cohorts, finding distribution varied from 34 variables common to all cohorts to 46 variables present in only one cohort [41]. This reflects the diversity of scientific purposes underlying the source datasets and highlights the importance of transparent documentation of harmonization limitations.
Diagram 2: Multi-Cohort Validation Framework. This diagram illustrates the comprehensive validation approach for harmonized data models, incorporating internal, external, and clinical validation components.
Research Reagent Solutions for Multi-Cohort Studies
Successful implementation of multi-cohort research requires careful selection of technical tools and methodological approaches. The following table summarizes key "research reagents" – essential tools and methodologies – for conducting multi-cohort investigations.
Table 3: Essential Research Reagents for Multi-Cohort Studies
| Tool/Methodology | Function | Implementation Examples | Considerations |
|---|---|---|---|
| REDCap API | Automated data extraction and integration | LIFE-CAP3 harmonization [39] | HIPAA/GDPR compliant; requires technical implementation |
| C-Surv Data Model | Standardized variable taxonomy | Neurodegeneration harmonization [41] | Optimized for cohort data; less complex than OMOP |
| OMOP CDM | Harmonization of EHR datasets | Alzheimer's Disease cohorts [40] | Complex but comprehensive for clinical data |
| Feature Selection Algorithms | Identification of core variables across cohorts | Frailty assessment development [13] | Reduces dimensionality; maintains predictive power |
| XGBoost Algorithm | Machine learning with high cross-cohort performance | Frailty prediction model [13] | Superior performance in multi-cohort validation |
| Multi-Cohort Benchmarking | External validation of models/algortihms | CheXNet radiography AI [42] | Reveals confounders not apparent in single cohorts |
| Simple Calibration | Direct mapping of equivalent variables | Neurodegeneration harmonization [41] | Preserves original data structure when possible |
| Algorithmic Transformation | Harmonization of differently coded variables | Lifestyle factors harmonization [41] | Enables inclusion of similar constructs with different assessment methods |
| Z-Score Standardization | Normalization of continuous measures | Cognitive performance scores [41] | Facilitates comparison of differently scaled measures |
Multi-cohort study designs represent a powerful approach for advancing scientific understanding of health and disease across diverse populations. The comparative analysis presented herein demonstrates that successful harmonization requires careful selection of appropriate methodologies based on research questions, data types, and available resources.
Prospective harmonization approaches, such as implemented in the LIFE-CAP3 integration, offer advantages in data quality but require early collaboration and standardized protocols [39]. Retrospective harmonization methods, while sometimes necessitating compromises in variable granularity, can achieve sufficient comparability to enable meaningful cross-cohort analyses [41]. Emerging machine learning approaches show promise for identifying optimal variable sets that maintain predictive power across diverse populations while minimizing measurement burden [13].
Validation across multiple cohorts remains essential for establishing true replicability, as demonstrated by the external benchmarking approaches that reveal performance variations not apparent in single-cohort assessments [42]. As multi-cohort research continues to evolve, ongoing development of standardized tools, transparent methodologies, and validation frameworks will further enhance our ability to generate robust and generalizable evidence from diverse populations.
Ensemble algorithms have become foundational tools in data science, particularly for building predictive models in research and drug development. Among the most prominent are Random Forest (RF), eXtreme Gradient Boosting (XGBoost), and Light Gradient Boosting Machine (LightGBM). The selection of an appropriate algorithm is critical for developing models that are not only high-performing but also computationally efficient and replicable across validation cohorts. This guide provides an objective, data-driven comparison of these three algorithms, focusing on their architectural differences, performance metrics, and suitability for various research tasks. We frame this comparison within the critical context of replicable research, emphasizing methodologies that ensure model robustness and generalizability through proper validation.
This section breaks down the fundamental characteristics and learning approaches of each algorithm.
Core Characteristics
- Random Forest: An ensemble of bagged decision trees. It builds multiple trees independently, each on a random subset of the data and features, and aggregates their predictions (e.g., by majority vote for classification or averaging for regression). This parallelism reduces variance and mitigates overfitting.
- XGBoost: A highly optimized implementation of gradient boosting. It builds trees sequentially, where each new tree learns to correct the errors made by the previous ensemble of trees. It incorporates regularization (L1 and L2) to control model complexity and prevent overfitting [43].
- LightGBM: Another gradient-boosting framework developed by Microsoft, focused on speed and efficiency. It uses two novel techniques—Gradient-based One-Side Sampling (GOSS) and Exclusive Feature Bundling (EFB)—to achieve faster training and lower memory usage while often maintaining, or even improving, accuracy [43].
Structural Growth Policies
A key difference lies in how the trees are constructed, which impacts both performance and computational cost.
Diagram 1: A comparison of level-wise (XGBoost/Random Forest) versus leaf-wise (LightGBM) tree growth strategies.
- Level-Wise Growth (XGBoost/Random Forest): The tree expands one complete level at a time. This approach is more conservative, can be efficiently parallelized, and helps control overfitting, potentially leading to more robust models [43].
- Leaf-Wise Growth (LightGBM): The tree expands by splitting the leaf that results in the largest reduction in loss. This can create asymmetrical, deeper trees that often achieve higher accuracy but are more prone to overfitting on small datasets if not properly regularized (e.g., using the
max_depthparameter) [43].
Performance Comparison and Experimental Data
Empirical evidence from recent studies across various domains allows for a quantitative comparison.
Quantitative Performance Metrics
Table 1: Comparative performance of XGBoost, LightGBM, and Random Forest across different studies.
| Domain / Study | Primary Metric | XGBoost Performance | LightGBM Performance | Random Forest Performance | Validation Notes |
|---|---|---|---|---|---|
| Acute Leukemia Complications [11] | AUROC (External Validation) | Not the best performer | 0.801 (95% CI: 0.774–0.827) | Among other tested algorithms | LightGBM achieved highest AUROC in derivation (0.824) and maintained it in external validation. |
| Frailty Assessment [13] | AUC (Internal Validation) | 0.940 (95% CI: 0.924–0.956) | Not the best performer | Evaluated among 12 algorithms | XGBoost demonstrated superior performance in predicting frailty, CKD progression, and mortality. |
| HPC Strength Prediction [44] | RMSE (Augmented Data) | 5.67 | 5.82 | Not the top performer | On the original dataset, their performance was very close (XGBoost: 11.44, LightGBM: 11.20). |
| General Trait [43] | Training Speed | Fast on CPU | Faster on GPU / similar data | Moderate | LightGBM is often significantly faster due to histogram-based methods and GOSS. |
| General Trait [43] | Model Robustness | High | High (with tuning) | High | Random Forest and XGBoost are often considered very robust. LightGBM may require careful tuning to avoid overfitting. |
Key Performance Insights
- Performance is Context-Dependent: No single algorithm dominates all scenarios. In the acute leukemia study, LightGBM was superior [11], while XGBoost excelled in the multi-cohort frailty assessment [13]. For predicting concrete strength, their performance was remarkably similar, with the winner depending on data preprocessing [44].
- The Speed-Accuracy Trade-off: LightGBM's primary advantage is training speed, often being significantly faster than XGBoost, especially on large datasets [43]. However, this does not always translate to better accuracy, and XGBoost can sometimes produce more robust models [43].
- Robustness of Random Forest: While sometimes outperformed in accuracy by boosting methods, Random Forest remains a strong, highly robust baseline. It is less prone to overfitting and is known for providing reliable, interpretable feature importance measures [45].
Experimental Protocols for Replicable Model Validation
To ensure model validity and replicability, research must adhere to rigorous experimental protocols. The following workflow outlines a standardized process for model development and validation, as exemplified by high-quality studies [11] [13] [45].
Diagram 2: A standardized workflow for developing and validating ensemble models to ensure replicability.
Detailed Methodological Components
Data Preprocessing: High-quality studies explicitly report handling of missing data (e.g., multiple imputation [11]), outliers (e.g., Winsorization [11]), and scaling. This is critical for reproducibility and reducing bias.
Feature Selection: Using systematic methods to identify predictors minimizes overfitting and improves model interpretability. Common techniques include:
Model Training with Hyperparameter Tuning: Optimizing hyperparameters is essential for maximizing performance.
- Frameworks like Optuna with Tree-structured Parzen Estimator can efficiently search the hyperparameter space [44].
- Nested cross-validation is the gold standard for providing an unbiased performance estimate while tuning hyperparameters [11].
- Addressing class imbalance through techniques like up-sampling the minority class or using algorithm-specific weighting (e.g.,
scale_pos_weightin XGBoost/LightGBM) is crucial for predictive accuracy on underrepresented classes [11].
Comprehensive Model Validation: Going beyond a simple train-test split is paramount for replicability.
- External Validation: The strongest validation tests the model on a completely held-out cohort from a different time period or institution [11]. This assesses true generalizability.
- Evaluation Metrics: Beyond Area Under the Receiver Operating Characteristic Curve (AUROC), researchers should report the Area Under the Precision-Recall Curve (AUPRC - especially for imbalanced data), and calibration metrics (slope, intercept) to ensure predicted probabilities match observed event rates [11].
Model Interpretation: Using tools like SHapley Additive exPlanations (SHAP) is critical for moving from a "black box" to an interpretable model. SHAP provides consistent feature importance scores and illustrates the direction and magnitude of each feature's effect on the prediction, fostering trust and clinical insight [11] [44].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key software tools and libraries for implementing ensemble algorithms in a research context.
| Tool / Reagent | Type | Primary Function | Relevance to Replicability |
|---|---|---|---|
| Optuna [44] | Software Framework | Hyperparameter optimization | Automates and documents the search for optimal model parameters, ensuring the process is systematic and reproducible. |
| SHAP [11] [44] | Interpretation Library | Model explainability | Provides a unified framework to interpret model predictions, which is essential for validating model logic and building trust for clinical use. |
| SMOGN [44] | Data Preprocessing Method | Handles imbalanced data | Combines over-sampling and under-sampling to generate balanced datasets, improving model performance on minority classes. |
| TRIPOD-AI / PROBAST-AI [11] [45] | Reporting Guideline & Risk of Bias Tool | Research methodology | Adherence to these guidelines ensures transparent and complete reporting, reduces risk of bias, and facilitates peer review and replication. |
| CopulaGAN/CTGAN [46] | Data Augmentation Model | Generates synthetic tabular data | Addresses data scarcity, a common limitation in research, by creating realistic synthetic data for model training and testing. |
| Cholesky Decomposition [47] | Statistical Method | Enforces correlation structures | A method used in synthetic data generation to preserve realistic inter-variable relationships found in real-world populations. |
The choice between Random Forest, XGBoost, and LightGBM is not a matter of identifying a universally superior algorithm, but rather of selecting the right tool for a specific research problem. Consider the following:
- Choose LightGBM when dealing with very large datasets where training speed and computational efficiency are paramount, and when you can dedicate effort to regularization to prevent overfitting.
- Choose XGBoost when you need a robust, highly accurate model and have sufficient computational resources. Its strong community, excellent documentation, and consistent performance make it a default choice for many competition winners and researchers.
- Choose Random Forest as a reliable baseline model. It is quick to train, highly robust, and less prone to overfitting, providing a strong benchmark against which to compare more complex boosting algorithms.
Ultimately, the validity of any model is determined not just by the algorithm selected, but by the rigor of the entire development and validation process. Employing robust experimental protocols—including proper data preprocessing, external validation, and model interpretation—is the most critical factor in achieving replicable, scientifically sound results that hold up across diverse patient cohorts.
Handling Class Imbalance and Missing Data in Multi-Source Datasets
In translational research, particularly in drug development, the analysis of multi-source datasets presents critical challenges that directly impact the validity and replicability of scientific findings. Class imbalance and missing data represent two pervasive issues that, if unaddressed, can severely compromise the performance of predictive models and the consensus when these models are applied to external validation cohorts. The replicability crisis in machine learning-based research often stems from improper handling of these data fundamental issues, leading to models that fail to generalize beyond their initial training data. This guide provides a systematic comparison of contemporary methodologies for addressing these challenges, with a specific focus on ensuring that model fits maintain their performance and consensus across diverse patient populations—a crucial requirement for regulatory science and robust drug development.
Comparative Analysis of Class Imbalance Handling Techniques
Class imbalance arises when one or more classes in a dataset are significantly underrepresented compared to others, a common scenario in medical research where disease cases may be rare compared to controls. This imbalance can bias machine learning models toward the majority class, reducing their sensitivity to detect the critical minority class. The following sections compare the primary strategies for mitigating this bias.
Data-Level Strategies: Resampling and Augmentation
Data-level methods modify the dataset itself to achieve better class balance before model training.
Oversampling Techniques: These methods increase the representation of the minority class.
- Random Oversampling: Involves randomly duplicating existing samples from the minority class until class sizes are balanced. While simple, it can lead to overfitting as it replicates the same samples without introducing new information [48].
- SMOTE (Synthetic Minority Oversampling Technique): Generates synthetic data points by interpolating between existing minority class samples and their nearest neighbors. This approach creates "new" examples that resemble the minority class, reducing the risk of overfitting present in simple duplication [49] [50].
- Advanced SMOTE Variants: More sophisticated implementations include Borderline-SMOTE (which focuses on generating samples near the class boundary), SVM-SMOTE (using support vectors to identify critical areas for sample generation), and K-Means SMOTE (which applies clustering before oversampling to align synthetic data with natural data structures) [48].
- GAN-Based Oversampling: Uses Generative Adversarial Networks conditioned on class labels to create realistic and diverse synthetic samples, particularly valuable for high-dimensional data like medical images or complex biomarkers [48].
Undersampling Techniques: These methods reduce the size of the majority class to balance the distribution.
- Random Undersampling: Randomly removes samples from the majority class. This approach risks discarding potentially useful information and can lead to underfitting [50].
- Tomek Links: Identifies and removes majority class samples that are each other's nearest neighbors with minority class samples, effectively cleaning the decision boundary [50] [48].
- Edited Nearest Neighbors (ENN): Removes samples from the majority class that are misclassified by their k-nearest neighbors, eliminating noisy and overlapping samples to create cleaner decision boundaries [48].
- Cluster-Based Undersampling: Uses clustering algorithms (e.g., k-means) to identify representative samples from the majority class, reducing redundancy while retaining critical patterns and preserving data diversity [50] [48].
Domain-Specific Data Synthesis: For non-tabular data common in multi-source studies, specialized augmentation approaches are required.
- Image Data: Augmentation techniques include rotation, cropping, flipping, brightness/contrast adjustment, and noise addition [50] [51].
- Text Data: Methods include synonym replacement, sentence simplification, back-translation (translating to another language and back), and word/sentence order shuffling [50] [51].
Table 1: Comparison of Data-Level Methods for Handling Class Imbalance
| Method | Mechanism | Best-Suited Data Types | Advantages | Limitations |
|---|---|---|---|---|
| Random Oversampling | Duplicates minority samples | Structured/tabular data | Simple to implement; No information loss from majority class | High risk of overfitting |
| SMOTE | Generates synthetic minority samples | Structured/tabular data | Reduces overfitting compared to random oversampling | May increase class overlap; Creates unrealistic samples |
| Borderline-SMOTE | Focuses on boundary samples | Structured/tabular data | Improves definition of decision boundaries | Complex parameter tuning |
| GAN-Based Oversampling | Generates samples via adversarial training | Image, text, time-series data | Creates highly realistic, diverse samples | Computationally intensive; Complex implementation |
| Random Undersampling | Removes majority samples | Large structured datasets | Reduces dataset size and training time | Discards potentially useful information |
| Tomek Links | Removes boundary majority samples | Structured data with clear separation | Cleans overlap between classes | Does not reduce imbalance significantly |
| Cluster-Based Undersampling | Selects representative majority samples | Structured data with clusters | Preserves overall data distribution | Quality depends on clustering performance |
| Image Augmentation | Applies transformations to images | Image data | Significantly expands dataset size | May not preserve label integrity if excessive |
| Text Back-Translation | Translates to other languages and back | Text/NLP data | Preserves meaning while varying expression | Depends on translation quality |
Algorithm-Level Strategies: Cost-Sensitive Learning
Algorithm-level approaches modify the learning process itself to account for class imbalance without changing the data distribution.
- Weighted Loss Functions: Assign higher weights to minority classes in the loss function calculation, increasing their influence on model updates. The weight for class c is often calculated as wc = N/nc, where N is the total number of samples and n_c is the number of samples in class c [48] [51].
- Focal Loss: Specifically designed for extreme class imbalance, Focal Loss down-weights easy-to-classify samples and focuses training on hard examples. The formula is L = -α(1-pt)^γ log(pt), where α balances class contributions, and γ focuses training on hard samples [50] [48].
- Ensemble Methods with Imbalance Adjustments: Combine multiple models with built-in mechanisms to handle imbalance.
- EasyEnsemble: Uses ensemble learning with multiple undersampled datasets, creating several balanced subsets by undersampling the majority class and training a classifier on each [49] [50].
- BalanceCascade: Uses a cascade of classifiers where correctly classified majority samples are removed in subsequent iterations [50].
- RUSBoost: Combines random undersampling with boosting algorithms [49] [48].
- SMOTEBoost: Integrates SMOTE oversampling directly into the boosting algorithm at each iteration [48].
Table 2: Algorithm-Level Approaches for Class Imbalance
| Method | Implementation | Theoretical Basis | Compatibility with Models |
|---|---|---|---|
| Weighted Loss Functions | Class weights in loss calculation | Cost-sensitive learning | Most models (LR, SVM, NN, XGBoost) |
| Focal Loss | Modifies cross-entropy to focus on hard examples | Hard example mining | Deep neural networks primarily |
| EasyEnsemble | Multiple balanced bootstrap samples + ensemble | Bagging + undersampling | Any base classifier |
| RUSBoost | Random undersampling + AdaBoost | Boosting + undersampling | Decision trees as base learners |
| SMOTEBoost | SMOTE + AdaBoost | Boosting + oversampling | Decision trees as base learners |
Evaluation Metrics for Imbalanced Data
Choosing appropriate evaluation metrics is critical when assessing models trained on imbalanced data, as standard accuracy can be profoundly misleading.
- Threshold-Dependent Metrics:
- Precision and Recall: Precision measures the proportion of correctly identified positive samples out of all samples predicted as positive (TP/(TP+FP)), while recall measures the proportion of actual positives correctly identified (TP/(TP+FN)) [48].
- F1-Score: The harmonic mean of precision and recall, providing a single metric that balances both concerns (2·Precision·Recall/(Precision+Recall)) [48].
- Threshold-Independent Metrics:
- AUC-ROC (Area Under the Receiver Operating Characteristic Curve): Plots the true positive rate against the false positive rate at various classification thresholds.
- AUC-PR (Area Under the Precision-Recall Curve): Plots precision against recall and is often more informative than ROC for imbalanced datasets as it avoids dilution by the dominant majority class [48].
- Alternative Comprehensive Metrics:
- Matthew's Correlation Coefficient (MCC): A balanced measure that considers all four confusion matrix categories, particularly robust for imbalanced datasets [48].
- Cohen's Kappa: Measures agreement between predicted and actual labels, adjusted for chance, effectively accounting for class imbalance [48].
Methodologies for Handling Missing Data in Multi-Source Studies
Missing data represents a ubiquitous challenge in multi-source datasets, where different data collection protocols, measurement technologies, and processing pipelines result in inconsistent data completeness across sources.
Missing Data Mechanisms and Assessment
Understanding the nature of missingness is essential for selecting appropriate handling methods.
- Missing Completely at Random (MCAR): The probability of missingness is unrelated to both observed and unobserved data.
- Missing at Random (MAR): The probability of missingness may depend on observed data but not on unobserved data.
- Missing Not at Random (MNAR): The probability of missingness depends on the unobserved values themselves.
Technical Approaches for Missing Data
- Deletion Methods:
- Listwise Deletion: Removes entire records with any missing values. This approach is simple but can introduce significant bias, particularly if data are not MCAR.
- Pairwise Deletion: Uses all available data for each specific analysis, but can lead to inconsistent sample sizes across analyses.
- Single Imputation Methods:
- Mean/Median/Mode Imputation: Replaces missing values with central tendency measures. While simple, this approach distorts distributions and underestimates variance.
- Regression Imputation: Uses predictive models to estimate missing values based on other variables, preserving relationships but still potentially underestimating uncertainty.
- Multiple Imputation:
- MICE (Multiple Imputation by Chained Equations): Creates multiple complete datasets by iteratively imputing missing values using appropriate models for each variable, analyzes each dataset separately, and pools results. This approach accounts for imputation uncertainty and provides more valid statistical inferences.
- Advanced Approaches:
- Matrix Completion Methods: Techniques like Singular Value Decomposition (SVD) imputation that leverage low-rank assumptions to recover missing values.
- Deep Learning Approaches: Autoencoders and other neural network architectures that can learn complex patterns to inform imputation.
Table 3: Comparison of Missing Data Handling Methods
| Method | Handling Mechanism | Assumed Mechanism | Advantages | Limitations |
|---|---|---|---|---|
| Listwise Deletion | Removes incomplete cases | MCAR | Simple implementation; No imputation bias | Inefficient; Potentially large information loss |
| Mean/Median Imputation | Replaces with central tendency | MCAR | Preserves sample size; Simple | Distorts distribution; Underestimates variance |
| k-NN Imputation | Uses similar cases' values | MAR | Data-driven; Adaptable to patterns | Computationally intensive; Choice of k critical |
| MICE | Multiple regression-based imputations | MAR | Accounts for imputation uncertainty; Flexible | Computationally intensive; Complex implementation |
| Matrix Factorization | Low-rank matrix completion | MAR | Effective for high-dimensional data | Algorithmically complex; Tuning sensitive |
| Deep Learning Imputation | Neural network-based prediction | MAR, MNAR | Captures complex patterns | High computational demand; Large data requirements |
Experimental Protocols for Method Validation
Benchmarking Protocol for Class Imbalance Methods
To objectively compare the performance of different class imbalance handling techniques, researchers should implement the following experimental protocol:
- Dataset Selection and Preparation: Curate multiple datasets with varying levels of class imbalance (e.g., 10:1, 50:1, 100:1 ratio). For replicability studies, include both the original dataset and external validation cohorts with potentially different distributions.
- Baseline Establishment: Train standard classifiers (e.g., Logistic Regression, Random Forest, XGBoost) on the unmodified imbalanced data as a performance baseline.
- Method Implementation: Apply various imbalance handling techniques:
- Data-level: Random oversampling, SMOTE, cluster-based undersampling
- Algorithm-level: Class weights, focal loss, ensemble methods
- Hybrid: SMOTE+ENN, RUSBoost
- Model Training and Validation: Use stratified k-fold cross-validation (e.g., k=5 or 10) with strict separation between training and validation sets to prevent data leakage.
- Performance Assessment: Evaluate using multiple metrics appropriate for imbalance (F1-score, AUC-PR, MCC) in addition to standard metrics.
- Statistical Significance Testing: Apply appropriate statistical tests (e.g., paired t-tests, Wilcoxon signed-rank tests) to determine if performance differences are significant.
- Replicability Assessment: Test the best-performing models on external validation cohorts to assess generalizability and consensus across populations.
Validation Protocol for Missing Data Methods
For evaluating missing data handling techniques:
- Data Preparation: Start with a complete dataset and introduce missingness under different mechanisms (MCAR, MAR, MNAR) at varying rates (e.g., 10%, 30%, 50%).
- Method Application: Apply different missing data handling techniques:
- Deletion methods (listwise, pairwise)
- Single imputation (mean, regression, k-NN)
- Multiple imputation (MICE)
- Advanced methods (matrix factorization, deep learning)
- Performance Evaluation: Compare the reconstructed datasets to the original complete data using:
- Value accuracy: RMSE between imputed and actual values
- Distribution preservation: Statistical tests comparing distributions
- Model performance: Impact on downstream analytical tasks
- Robustness Testing: Evaluate method performance across different missingness patterns and proportions.
Visualization of Methodologies
Workflow for Handling Multi-Source Data Challenges
Replicability Validation Framework
Table 4: Essential Tools for Handling Class Imbalance and Missing Data
| Tool/Resource | Type | Primary Function | Application Context |
|---|---|---|---|
| Imbalanced-Learn | Python library | Provides resampling techniques | Implementing SMOTE, undersampling, ensemble methods for tabular data [49] |
| Scikit-Learn | Python library | Machine learning with class weights | Implementing cost-sensitive learning and evaluation metrics [48] |
| XGBoost/LightGBM | Algorithm | Gradient boosting with scaleposweight | Native handling of imbalance through parameter tuning [49] |
| MICE Algorithm | Statistical method | Multiple imputation for missing data | Handling MAR missingness in structured data [48] |
| Autoencoders | Neural network architecture | Dimensionality reduction and imputation | Complex missing data imputation for high-dimensional data [48] |
| Focal Loss | Loss function | Handles extreme class imbalance | Deep learning models for computer vision, medical imaging [50] [48] |
| Data Augmentation | Technique | Expands minority class representation | Image, text, and time-series data in domain-specific applications [50] [51] |
| Stratified K-Fold | Validation method | Maintains class distribution in splits | Robust evaluation on imbalanced datasets [48] |
Addressing class imbalance and missing data in multi-source datasets is not merely a technical preprocessing step but a fundamental requirement for building models that achieve consensus across validation cohorts. Our comparison reveals that no single method dominates across all scenarios—the optimal approach depends on the specific data characteristics, missingness mechanisms, and analytical goals. For class imbalance, strong classifiers like XGBoost with appropriate class weights often provide a robust baseline, while data-level methods may offer additional benefits for weaker learners or extremely skewed distributions [49]. For missing data, multiple imputation techniques generally provide the most statistically sound approach, particularly under MAR assumptions.
Critically, the replicability crisis in predictive modeling can be substantially mitigated through rigorous attention to these fundamental data challenges. By implementing the systematic comparison protocols and validation frameworks outlined in this guide, researchers in drug development and translational science can enhance the generalizability of their models, ultimately leading to more reliable and consensus-driven findings that hold across diverse patient populations. The path to replicability begins with acknowledging and properly addressing these ubiquitous data challenges in multi-source studies.
Implementing Nested Cross-Validation to Prevent Optimism Bias
In the pursuit of robust and generalizable predictive models, researchers in fields such as drug development and neuroscience face a critical challenge: the accurate estimation of a model's performance on independent data. Standard validation approaches often produce optimistically biased performance estimates because the same data is used for both model tuning and evaluation, leading to overfitting and reduced replicability across validation cohorts [52] [53]. This bias fundamentally undermines the replicability consensus model fits validation cohorts research, as models that appear high-performing during development may fail when applied to new populations or datasets.
Nested cross-validation (CV) has emerged as a rigorous validation framework specifically designed to mitigate this optimism bias. By structurally separating hyperparameter tuning from model evaluation, it provides a less biased estimate of generalization error, which is crucial for building trust in predictive models intended for real-world applications [52] [54]. This guide objectively compares nested CV against alternative methods, providing the experimental data and protocols necessary for researchers to make informed validation choices.
Understanding Nested Cross-Validation and Its Necessity
The Architectural Framework
Nested CV employs a two-layer hierarchical structure to prevent information leakage between the model selection and performance evaluation phases:
- Outer Loop: Functions as the evaluation layer. The data is split into multiple training and testing folds. The model, configured with its optimal hyperparameters (determined from the inner loop), is trained on the outer training fold and its performance is assessed on the outer testing fold. The average performance across all outer folds provides the final, unbiased estimate of generalization error [52].
- Inner Loop: Functions as the tuning layer. Within each outer training fold, a separate cross-validation process is performed. This inner loop is dedicated exclusively to hyperparameter optimization and model selection, identifying the best configuration based on its performance across the inner folds [52] [54].
This separation of duties ensures that the data used to assess the final model's performance never influences the selection of its hyperparameters, thereby preventing optimism bias [52].
The Problem of Optimism Bias in Standard Validation
Standard, or "flat," cross-validation uses a single data-splitting procedure to simultaneously tune hyperparameters and estimate future performance. This approach introduces optimistic bias because the performance metric is maximized on the same data that guides the tuning process, causing the model to overfit to the specific dataset [54] [55]. The model's performance estimate is therefore not a true reflection of its ability to generalize.
Empirical evidence highlights this concern. A scikit-learn example comparing nested and non-nested CV on the Iris dataset found that the non-nested approach produced an overly optimistic score, with an average performance bias of 0.007581 [54]. In healthcare predictive modeling, non-nested methods exhibited higher levels of optimistic bias—approximately 1% to 2% for the area under the receiver operating characteristic curve (AUROC) and 5% to 9% for the area under the precision-recall curve (AUPR) [52]. This bias can lead to the selection of suboptimal models and diminish replicability in validation cohorts.
Comparative Analysis of Cross-Validation Methods
Performance and Bias Comparison
The table below summarizes a quantitative comparison between nested CV and standard flat CV, synthesizing findings from multiple experimental studies.
Table 1: Quantitative comparison of nested and flat cross-validation performance
| Study Context | Metric | Nested CV | Flat CV | Note |
|---|---|---|---|---|
| Iris Dataset (SVM) [54] | Average Score Difference | Baseline | +0.007581 | Flat CV shows optimistic bias |
| Healthcare Modeling [52] | AUROC Bias | Baseline | +1% to 2% | Higher optimistic bias for flat CV |
| Healthcare Modeling [52] | AUPR Bias | Baseline | +5% to 9% | Higher optimistic bias for flat CV |
| 115 Binary Datasets [55] | Algorithm Selection | Reference | Comparable | Flat CV selected similar-quality algorithms |
A key study on 115 real-life binary datasets concluded that while flat CV produces a biased performance estimate, the practical impact on algorithm selection may be limited. The research found that flat CV generally selected algorithms of similar quality to nested CV, provided the learning algorithms had relatively few hyperparameters to optimize [55]. This suggests that for routine model selection without the need for a perfectly unbiased error estimate, the computationally cheaper flat CV can be a viable option.
Consensus Nested Cross-Validation: A Focus on Feature Stability
An advanced variant called Consensus Nested Cross-Validation (cnCV) addresses optimism bias with a focus on feature selection. Unlike standard nested CV, which selects features based on the best inner-fold classification accuracy, cnCV selects features that are stable and consistent across inner folds [56].
Table 2: Comparison of standard nCV and consensus nCV (cnCV)
| Aspect | Standard Nested CV (nCV) | Consensus Nested CV (cnCV) |
|---|---|---|
| Primary Goal | Minimize inner-fold prediction error | Identify features common across inner folds |
| Inner Loop Activity | Trains classifiers for feature/model selection | Performs feature selection only (no classifiers) |
| Computational Cost | High | Lower (no inner-loop classifier training) |
| Feature Set | Can include more irrelevant features (false positives) | More parsimonious, with fewer false positives |
| Reported Accuracy | Similar training/validation accuracy to cnCV [56] | Similar accuracy to nCV and private evaporative cooling [56] |
This method has been shown to achieve similar training and validation accuracy to standard nested CV but with shorter run times and a more parsimonious set of features, reducing false positives [56]. This makes cnCV particularly valuable in domains like bioinformatics and biomarker discovery, where interpretability and feature stability are paramount for replicability.
Experimental Protocols for Robust Validation
Implementation Workflow for Nested Cross-Validation
The following diagram illustrates the procedural workflow for implementing nested cross-validation, showing the interaction between the outer and inner loops.
Code Implementation Protocol
The Python code below provides a concrete starting point for implementing a nested cross-validation framework, adapted from a foundational example [52].
For a real-world application in drug development, a study predicting drug release from polymeric long-acting injectables employed a nested CV strategy. The outer loop reserved 20% of drug-polymer groups for testing, while the inner loop used group k-fold (k=10) cross-validation on the remaining 80% for hyperparameter tuning via a random grid search. This process was repeated ten times to ensure robust performance estimation [57].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key computational tools and concepts for implementing robust validation
| Tool/Concept | Function/Purpose | Example Use Case |
|---|---|---|
| Scikit-learn [54] | Python ML library providing CV splitters & GridSearchCV | Implementing inner & outer loops, hyperparameter tuning |
| TimeSeriesSplit [52] | Cross-validation iterator for time-dependent data | Prevents data leakage in temporal studies (e.g., patient records) |
| ReliefF Algorithm [56] | Feature selection method detecting interactions & main effects | Identifying stable, consensus features in cnCV |
| Hyperparameter Grid [54] | Defined set of parameters to search over (e.g., C, gamma for SVM) | Systematically exploring model configuration space in the inner loop |
| Stratified CV [53] | Ensures relative class frequencies are preserved in each fold | Critical for validation with imbalanced datasets (e.g., rare diseases) |
Nested cross-validation is a powerful methodological tool for mitigating optimism bias and advancing the goal of replicable model fits across validation cohorts. While it comes with a higher computational cost, its ability to provide a realistic and unbiased estimate of generalization error is invaluable, especially in high-stakes fields like drug development and clinical neuroscience [52] [57]. For research where the primary goal is a definitive performance estimate, nested CV is the gold standard. However, evidence suggests that for routine model selection with simple classifiers, flat CV may be a sufficient and efficient alternative [55]. The choice of method should therefore be guided by the specific research objectives, the required rigor of performance estimation, and the computational resources available.
In modern computational research, particularly in drug development and biomedical sciences, the path from raw data to a validated model output is fraught with challenges that can compromise replicability. A robust, well-documented workflow is not merely a convenience but a fundamental requirement for producing models that yield consistent results across independent validation cohorts. Replicability—the ability of independent investigators to recreate the computational process and achieve consistent results using the same data and methodology—serves as the bedrock of scientific credibility in an era increasingly dependent on machine learning and complex data analysis [13].
This guide provides a comprehensive, step-by-step framework for constructing a practical workflow that embeds replicability into every stage, from initial data ingestion to final model validation. By adopting the structured approach outlined here, researchers and drug development professionals can create transparent, methodical processes that stand up to rigorous scrutiny across multiple cohorts and experimental conditions, thereby addressing the current crisis of replicability in computational sciences.
The complete workflow from data ingestion to model output represents an integrated system where each component directly influences the reliability and replicability of the final output. The entire process can be visualized as a structured pipeline with critical feedback mechanisms.
Figure 1: End-to-End Workflow from Data Ingestion to Replicability Consensus
This integrated framework emphasizes critical feedback loops where validation results inform earlier stages of the pipeline, enabling continuous refinement and ensuring the final model achieves replicability consensus across multiple validation cohorts.
Stage 1: Data Ingestion Architecture
Strategic Approaches and Modern Tools
Data ingestion forms the foundational layer of the entire analytical workflow, comprising the processes designed to capture, collect, and import data from diverse source systems into a centralized repository where it can be stored and analyzed [58]. The architecture of this ingestion layer directly influences all subsequent stages and ultimately determines the reliability of model outputs.
Modern data ingestion has evolved significantly from traditional batch processing to incorporate real-time streaming paradigms that enable immediate analysis and response [58]. Contemporary frameworks support both structured and unstructured data at scale, accommodating the variety and velocity of data generated in scientific research and drug development environments. The selection of appropriate ingestion strategies—whether batch processing for large volumetric datasets or real-time streaming for time-sensitive applications—represents a critical design decision with profound implications for workflow efficiency and model performance.
Table 1: Data Ingestion Tools Comparison for Research Environments
| Tool | Primary Use Case | Supported Patterns | Scalability | Integration Capabilities |
|---|---|---|---|---|
| Apache Kafka | High-throughput real-time streaming | Streaming, Event-driven | Distributed, horizontal scaling | Extensive API ecosystem, cloud-native |
| Apache NiFi | Visual data flow management | Both batch and streaming | Horizontal clustering | REST API, extensible processor framework |
| AWS Glue | Cloud-native ETL workflows | Primarily batch with streaming options | Managed serverless auto-scaling | Native AWS services, JDBC connections |
| Google Cloud Dataflow | Unified batch/stream processing | Both batch and streaming | Managed auto-scaling | GCP ecosystem, Apache Beam compatible |
| Rivery | Complete data ingestion framework | Both batch and streaming | Volume-based scaling | Reverse ELT, alerting, multi-source support |
Implementation Protocol
Implementing a robust data ingestion architecture requires methodical planning and execution. The following protocol ensures a comprehensive approach:
Source Identification and Characterization: Systematically catalog all data sources, noting their structure (structured, semi-structured, unstructured), volume, velocity, and connectivity requirements. Research environments typically encompass experimental instrument outputs, electronic lab notebooks, clinical databases, and literature mining streams [58].
Ingestion Pattern Selection: Determine the appropriate processing pattern for each data source based on analytical requirements. Batch processing is ideal for large-scale historical data where immediate analysis is unnecessary, while streaming is essential for time-sensitive applications requiring real-time insights [58].
Tool Configuration and Deployment: Based on the selected patterns and organizational constraints, implement the chosen ingestion tools. For streaming platforms like Apache Kafka, this involves configuring topics, partitions, and replication factors. For ETL services like AWS Glue, this requires defining jobs, data sources, and transformation logic [58].
Scalability and Security Implementation: Configure auto-scaling mechanisms to handle variable data loads and implement comprehensive security measures including encryption in transit and at rest, access controls, and authentication protocols to protect sensitive research data [58].
Stage 2: Data Validation Processes
Validation Typology and Error Prevention
Data validation comprises the systematic processes and checks that ensure data accuracy, consistency, and adherence to predefined quality standards before it progresses through the analytical pipeline [59]. In scientific contexts where model replicability is paramount, rigorous validation is non-negotiable, as erroneous or inconsistent data inevitably compromises analytical outcomes and prevents consensus across validation cohorts.
A comprehensive validation strategy implements checks at multiple stages of the data lifecycle, each serving distinct protective functions. Pre-entry validation establishes initial quality standards before data enters systems, entry validation provides real-time feedback during data input, and post-entry validation maintains quality controls over existing datasets [59]. This multi-layered approach creates defensive barriers against data quality degradation throughout the analytical workflow.
Table 2: Data Validation Types and Research Applications
| Validation Type | Implementation Stage | Primary Research Benefit | Example Techniques |
|---|---|---|---|
| Pre-entry Validation | Before data entry | Prevents obviously incorrect data entry | Required field enforcement, data type checks, format validation |
| Entry Validation | During data input | Reduces entry errors with immediate feedback | Drop-down menus, range checking, uniqueness verification |
| Post-entry Validation | After data storage | Maintains long-term data integrity across cohorts | Data cleansing, referential integrity checks, periodic rule validation |
Validation Protocol and Error Handling
The data validation process follows a systematic four-stage methodology that transforms raw input into verified, analysis-ready data:
Data Entry and Collection: The initial stage involves gathering data from various sources, which may include automated instrument feeds, manual data entry, or imports from existing systems. Before validation, data may undergo preliminary cleansing to remove duplicates and standardize formats [59].
Validation Rule Definition: This critical stage establishes the specific criteria that define valid data for a given research context. These rules encompass data type checks (ensuring values match expected formats), range checks (verifying numerical data falls within acceptable limits), format checks (validating structures like email addresses or sample identifiers), and referential integrity checks (ensuring relational consistency between connected datasets) [59].
Rule Application and Assessment: The defined validation rules are systematically applied to the dataset, with each data element evaluated against the established criteria. Data satisfying all requirements is classified as valid and progresses through the pipeline, while records failing validation checks are flagged for further handling [59].
Error Resolution: The final stage addresses invalid data through either prompting users for correction or implementing automated correction routines where possible. This stage includes comprehensive logging of validation outcomes and error types to inform process improvements and provide audit trails for replicability assessment [59].
Stage 3: Feature Engineering and Model Development
Feature Selection Methodologies
Feature engineering represents the critical transformation of raw validated data into predictive variables that effectively power analytical models. In replicability-focused research, this process must be both systematic and well-documented to ensure consistent application across training and validation cohorts.
Research demonstrates that sophisticated feature selection approaches significantly enhance model generalizability while reducing complexity. A recent multi-cohort frailty assessment study employed five complementary feature selection algorithms—LASSO regression, VSURF, Boruta, varSelRF, and Recursive Feature Elimination—applied to 75 potential variables to identify a minimal set of just eight clinically available parameters with robust predictive power [13]. This rigorous methodology ensured that only the most informative features progressed to model development, directly contributing to the model's performance across independent validation cohorts.
Multi-Algorithm Model Development
The model development phase requires comparative evaluation of multiple algorithmic approaches to identify the optimal technique for a given research problem. The frailty assessment study exemplifies this process, with systematic evaluation of 12 machine learning approaches across four categories: ensemble learning models (XGBoost, Random Forest, C5.0, AdaBoost, GBM), neural network approaches (Neural Network, Multi-layer Perceptron), distance and boundary-based models (Support Vector Machine), and regression models (Logistic Regression) [13].
This comprehensive comparative analysis determined that the Extreme Gradient Boosting (XGBoost) algorithm delivered superior performance across training, internal validation, and external validation datasets while maintaining clinical feasibility—a crucial consideration for practical implementation [13]. The selection of clinically feasible features alongside the optimal algorithm creates models that balance predictive accuracy with practical implementation requirements.
Stage 4: Model Validation and Replicability Assessment
Multi-Cohort Validation Framework
Model validation constitutes the most critical phase for establishing replicability consensus, moving beyond simple performance metrics on training data to demonstrate generalizability across independent populations. A robust validation framework incorporates both internal and external validation components, with external validation representing the gold standard for assessing model transportability.
Internal validation employs techniques such as cross-validation or bootstrap resampling on the development dataset to provide preliminary estimates of model performance while guarding against overfitting. External validation, however, tests the model on completely independent datasets collected by different research teams, often across diverse geographic locations or healthcare systems, providing authentic assessment of real-world performance [13]. The frailty assessment model exemplifies this approach, with development in the NHANES cohort followed by external validation in the CHARLS, CHNS, and SYSU3 CKD cohorts, demonstrating consistent performance across diverse populations and healthcare environments [13].
Performance Metrics and Replicability Protocols
Comprehensive model validation requires assessment across multiple performance dimensions using standardized metrics. The experimental protocol should include:
Discrimination Assessment: Evaluate the model's ability to distinguish between outcome states using Area Under the Receiver Operating Characteristic Curve (AUC), with 95% confidence intervals calculated through bootstrapping. The frailty model demonstrated AUC values of 0.940 (95% CI: 0.924-0.956) in internal validation and 0.850 (95% CI: 0.832-0.868) in external validation [13].
Comparative Performance Analysis: Benchmark new models against existing standards using statistical tests for significance. The frailty model significantly outperformed traditional indices for predicting CKD progression (AUC 0.916 vs. 0.701, p < 0.001), cardiovascular events (AUC 0.789 vs. 0.708, p < 0.001), and mortality [13].
Clinical Calibration Assessment: Evaluate how well predicted probabilities match observed outcomes across the risk spectrum using calibration plots and statistics.
Feature Importance Interpretation: Employ model interpretation techniques like SHAP (SHapley Additive exPlanations) analysis to provide transparent insights into prediction drivers, facilitating clinical understanding and trust [13].
Visualization of the Complete Workflow
The integrated relationship between workflow components and validation cohorts can be visualized as a system with explicit inputs, processes, and outputs, emphasizing the critical replication feedback loop.
Figure 2: Multi-Cohort Validation Framework with Replicability Feedback
This visualization illustrates how the Input-Process-Output model functions within a multi-cohort validation framework, with development and validation cohorts providing essential feedback that drives the replicability consensus essential for scientifically rigorous model outputs.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagent Solutions for Replicable Workflows
| Reagent Category | Specific Examples | Function in Workflow | Implementation Considerations |
|---|---|---|---|
| Data Ingestion Tools | Apache Kafka, Apache NiFi, AWS Glue | Collect, transport, and initially process raw data from source systems | Scalability, support for both batch and streaming, integration capabilities [58] |
| Validation Frameworks | Custom rule engines, Great Expectations | Enforce data quality standards through predefined checks and constraints | Support for multiple validation types (pre-entry, entry, post-entry) [59] |
| Feature Selection Algorithms | LASSO, VSURF, Boruta, varSelRF, RFE | Identify most predictive variables while reducing dimensionality | Employ multiple complementary algorithms for robust selection [13] |
| Machine Learning Algorithms | XGBoost, Random Forest, Neural Networks | Develop predictive models from engineered features | Comparative evaluation of multiple algorithms essential [13] |
| Model Interpretation Tools | SHAP, LIME | Provide transparent insights into model predictions and feature importance | Critical for building clinical trust and understanding model behavior [13] |
| Validation Cohorts | NHANES, CHARLS, CHNS, SYSU3 CKD | Provide independent datasets for external model validation | Diversity of cohorts essential for assessing generalizability [13] |
The practical workflow from data ingestion to model output represents a methodical journey where each stage systematically contributes to the ultimate goal of replicability consensus. By implementing robust data ingestion architectures, rigorous multi-stage validation processes, systematic feature engineering, and comprehensive multi-cohort validation, researchers can create models that transcend their development environments and demonstrate consistent performance across diverse populations. This structured approach, documented with sufficient transparency to enable independent replication, represents the path forward for computationally-driven scientific disciplines, particularly in drug development and biomedical research where decisions based on model outputs have profound real-world consequences.
Diagnosing and Solving Common Replicability Failures
Identifying and Mitigating Dataset Shift Between Development and Validation Cohorts
In the pursuit of replicable scientific findings, particularly in healthcare and clinical drug development, the stability of machine learning (ML) model performance across different patient cohorts is paramount. Dataset shift, a phenomenon where the data distribution used for model development differs from the data encountered during validation and real-world deployment, presents a fundamental challenge to this stability [60]. It can lead to performance degradation, thereby threatening the validity and generalizability of research conclusions [61] [62]. This guide objectively compares the current methodologies for identifying and mitigating dataset shift, framing them within the broader thesis of achieving a replicability consensus where models maintain their performance when validated on independent cohorts.
The core of the problem lies in the mismatch between training and deployment environments. As detailed by Sparrow (2025), dataset shift can arise from technological changes (e.g., updates to electronic health record software), population changes (e.g., shifts in hospital patient demographics), and behavioral changes (e.g., new disease patterns) [60]. A recent systematic review underscores that temporal shift and concept drift are among the most commonly encountered types in health prediction models [61] [62]. For researchers and drug development professionals, proactively managing dataset shift is not merely a technical exercise but a critical component of ensuring that predictive models are robust, equitable, and reliable in supporting clinical decisions.
Types of Dataset Shift and Their Impact
Understanding the specific type of dataset shift is the first step toward its mitigation. Shift can manifest in the input data (covariates), the output labels, or the relationship between them.
- Covariate Shift: This occurs when the distribution of input features (e.g., patient age, biomarker levels) changes between development and validation cohorts, while the conditional probability of the output given the input remains unchanged. For example, a model trained on a population with a specific average age may underperform when applied to a significantly older or younger population.
- Prevalence Shift: Also known as label shift, this happens when the overall prevalence of the outcome of interest changes. A model predicting a rare disease outcome trained on a general population will face prevalence shift if deployed in a specialist clinic where the disease is more common.
- Concept Drift: This refers to a change in the fundamental relationship between the input variables and the target outcome. The same set of clinical features might lead to a different diagnosis over time due to evolving disease definitions or the emergence of new disease subtypes.
The table below summarizes these key types of dataset shift.
Table 1: Key Types of Dataset Shift in Clinical Research
| Shift Type | Definition | Example in Clinical Research |
|---|---|---|
| Covariate Shift | Change in the distribution of input features (X) | Model trained on data from urban hospitals is applied to rural populations with different demographic characteristics [60]. |
| Prevalence Shift | Change in the distribution of output labels (Y) | A frailty prediction model developed for a general elderly population is used in a diabetic sub-population where frailty is 3-5 times more prevalent [63]. |
| Concept Drift | Change in the relationship between inputs and outputs (P(Y|X)) | The diagnostic criteria for a disease are updated, altering the clinical meaning of certain feature combinations [61]. |
| Mixed Shifts | Simultaneous occurrence of multiple shift types | A model experiences both a change in patient demographics (covariate shift) and disease prevalence over time (prevalence shift) [64]. |
Comparative Analysis of Shift Identification and Mitigation Strategies
A systematic review of 32 studies on machine learning for health predictions provides a comprehensive overview of the current landscape of strategies [61] [62]. The following table synthesizes the experimental findings from the literature, comparing the most prominent techniques for detecting and correcting dataset shift.
Table 2: Comparison of Dataset Shift Identification and Mitigation Strategies
| Method Category | Specific Technique | Reported Performance / Experimental Data | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Shift Identification | Model-based Performance Monitoring | Most frequent detection strategy; tracks performance metrics (e.g., AUC, accuracy) drop over time or across sites [61] [62]. | Directly linked to model utility; easy to interpret. | Reactive; indicates a problem only after performance has degraded. |
| Statistical Tests (e.g., Two-sample tests) | Used to detect distributional differences in input features between cohorts [62]. | Proactive; can alert to potential issues before performance loss. | Does not directly measure impact on model performance; can be sensitive to sample size. | |
| Unsupervised Framework (e.g., with self-supervised encoders) | Effectively distinguishes prevalence, covariate, and mixed shifts across chest radiography, mammography, and retinal images [64]. | Identifies the precise type of shift, which is critical for selecting mitigation strategies. | Primarily demonstrated on imaging data; applicability to tabular clinical data requires further validation. | |
| Shift Mitigation | Model Retraining | Predominant correction approach; can restore model performance when applied with new data [61] [65]. | Directly addresses the root cause of performance decay; can incorporate latest data patterns. | Computationally burdensome; requires continuous data collection and labeling [61] [60]. |
| Feature Engineering / Recalibration | Used to adjust model inputs or outputs to align with the new data distribution [61] [62]. | Less resource-intensive than full retraining; can be effective for specific shift types. | May not be sufficient for severe concept drift; can introduce new biases if not carefully applied. | |
| Domain Adaptation & Distribution Alignment | Includes techniques to learn domain-invariant feature representations [62]. | Aims to create a single, robust model that performs well across multiple domains or time periods. | Algorithmic complexity can be high; interpretability of the resulting model may be reduced. |
Experimental Insights from Clinical Case Studies
Recent clinical ML studies highlight the real-world impact of these strategies. For instance, a study predicting short-term progression to end-stage renal disease (ESRD) in patients with stage 4 chronic kidney disease demonstrated the importance of external validation as a form of shift identification. The XGBoost model experienced a drop in AUC from 0.93 on the internal development cohort to 0.85 on the external validation cohort, clearly indicating the presence of a dataset shift [65]. This performance drop, despite using similar eligibility criteria, underscores the hidden distributional differences that can exist between institutions.
In medical imaging, Roschewitz et al. (2024) proposed an automated identification framework that leverages self-supervised encoders and model outputs. Their experimental results across three imaging modalities showed that this method could reliably distinguish between prevalence shift, covariate shift, and mixed shifts, providing a more nuanced diagnosis of the problem than mere performance monitoring [64].
Experimental Protocols for Shift Assessment
For researchers aiming to implement the strategies discussed, the following workflow provides a detailed, actionable protocol for assessing dataset shift.
Detailed Methodology
Data Distribution Analysis: Conduct statistical hypothesis tests (e.g., Kolmogorov-Smirnov test for continuous features, Chi-square test for categorical features) to compare the distributions of key input variables between the development and validation cohorts [62]. This proactively identifies covariate shift before model deployment.
Model Performance Check: Deploy the trained model on the validation cohort and calculate standard performance metrics (e.g., Area Under the Curve (AUC), Accuracy, F1-score). Compare these metrics directly with the performance on the development cohort. A statistically significant drop indicates a problem requiring intervention [61] [65].
Shift Type Diagnosis: Use specialized frameworks to diagnose the specific type of shift. For imaging data, the method proposed by Roschewitz et al. can distinguish prevalence, covariate, and mixed shifts [64]. For tabular data, analyzing performance across subgroups and comparing prior and posterior label distributions can provide similar insights.
Mitigation Action: Based on the diagnosis, select and apply a mitigation strategy.
- For covariate shift, consider importance weighting or domain adaptation [62].
- For prevalence shift, recalibrate the model's output probabilities on the new cohort.
- For concept drift or mixed shifts, model retraining on a combined dataset from both cohorts is often the most reliable solution [61] [65].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key computational and methodological "reagents" essential for conducting rigorous dataset shift research.
Table 3: Essential Research Tools for Dataset Shift Analysis
| Tool / Solution | Function | Application Context |
|---|---|---|
| Two-Sample Statistical Tests | Quantifies the probability that two sets of data (development vs. validation) are drawn from the same distribution. | Identifying covariate shift by comparing feature distributions [62]. |
| Self-Supervised Encoders | A type of neural network that learns meaningful data representations without labeled data, sensitive to subtle input changes. | Detecting and diagnosing subtle covariate shifts in complex data like medical images [64]. |
| SHAP (SHapley Additive exPlanations) | A method for interpreting model predictions, quantifying the contribution of each feature to a single prediction. | Model debugging and understanding how feature importance changes between cohorts, indicating potential concept drift [63] [65]. |
| XGBoost (eXtreme Gradient Boosting) | A powerful, scalable machine learning algorithm based on gradient boosted decision trees. | Serves as a high-performance benchmark model in comparative studies, as seen in the ESRD prediction study [65]. |
| Domain Adaptation Algorithms | A class of algorithms designed to align feature distributions from different domains (e.g., development vs. validation cohort). | Mitigating covariate shift by learning domain-invariant representations [62]. |
The path to a replicability consensus in clinical ML model development is inextricably linked to the effective management of dataset shift. As evidenced by the comparative data, no single method has emerged as a universally superior solution; rather, the choice depends on the specific type of shift encountered and the available computational resources [61] [62]. The scientific community must move beyond single-cohort validation and adopt a proactive, continuous monitoring paradigm. This involves standardized reporting of model performance on external cohorts, subgroup analyses to ensure equitable performance, and the development of more sophisticated, automated tools for shift identification and diagnosis [64] [61]. By integrating these practices into the core of the research workflow, researchers and drug developers can build more robust and reliable models, thereby strengthening the foundation of evidence-based medicine.
Addressing the Small Sample Size Problem in Niche Biomedical Applications
In niche biomedical research—such as studies on rare diseases, specialized animal models, or detailed mechanistic investigations—researchers frequently face the formidable challenge of extremely small sample sizes. These constraints often arise due to ethical considerations, financial limitations, or the sheer scarcity of available subjects [66]. While small sample sizes present significant statistical hurdles, including reduced power and increased vulnerability to type-I errors, this guide compares several modern methodological solutions that enable robust scientific inference even with limited data [66] [67]. Framed within the critical context of replicability and validation across independent cohorts, we objectively evaluate the performance of these approaches to guide researchers and drug development professionals in selecting optimal strategies for their specific applications.
Comparative Analysis of Methodological Solutions
The table below summarizes the core characteristics, performance data, and ideal use cases for four key methodologies addressing the small sample size problem.
| Methodology | Core Principle | Reported Performance/Data | Key Advantages | Limitations & Considerations |
|---|---|---|---|---|
| Randomization-Based Max-T Test [66] | Approximates the distribution of a maximum t-statistic via randomization, avoiding parametric assumptions. | Accurate type-I error control with ( ni < 20 ); outperforms bootstrap methods which require ( ni \geq 50 ). | Does not rely on multivariate normality; robust to variance heterogeneity and small ( n ). | Computationally intensive; complex implementation in high-dimensional designs. |
| Replicable Brain Signature Models [5] | Derives consensus brain regions from multiple discovery subsets; validates in independent cohorts. | High replicability of model fits (( r > 0.9 ) in 50 validation subsets); outperformed theory-based models. | Creates robust, generalizable measures; mitigates overfitting via cross-cohort validation. | Requires large initial datasets to create discovery subsets and independent cohorts for validation. |
| Cross-Cohort Replicable Functional Connectivity [68] | Employs feature selection and machine learning to identify connectivity patterns replicable across independent cohorts. | Identified 23 replicable FCs; distinguished patients from controls with 82.7-90.2% accuracy across 3 cohorts. | Individual-level prediction; identifies stable biomarkers despite cohort heterogeneity. | Complex pipeline integrating feature selection and machine learning. |
| Bayesian Methods [67] | Incorporates prior knowledge or data into analysis via Bayes' theorem, updating beliefs with new data. | Enables complex model testing even with small ( n ); implemented with R syntax for accessibility. | Reduces effective sample size needed; provides intuitive probabilistic results (credible intervals). | Requires careful specification of prior distributions; results can be sensitive to prior choice. |
Detailed Experimental Protocols
Protocol for Randomization-Based Max-T Test
This protocol is designed for high-dimensional, small-sample-size designs, such as those with repeated measures or multiple endpoints [66].
Step 1: Hypothesis and Contrast Formulation Define the global null hypothesis of no effect across all endpoints or time points. Formulate a set of pre-specified contrasts (e.g., pairwise comparisons between groups) using a contrast matrix. The test statistic is the maximum absolute value of the t-statistics derived from these contrasts (the max-T statistic) [66].
Step 2: Data Randomization Under the assumption that the global null hypothesis is true, randomly shuffle the group labels of the entire dataset. This process creates a new, permuted dataset where any systematic differences between groups are due only to chance.
Step 3: Null Distribution Construction For each randomization, recalculate the max-T statistic. Repeat this randomization process a large number of times (e.g., 10,000 iterations) to build a comprehensive empirical distribution of the max-T statistic under the null hypothesis.
Step 4: Inference Compare the original, observed max-T statistic from the actual data to the constructed empirical null distribution. The family-wise error rate (FWER)-controlled p-value is calculated as the proportion of permutations in which the randomized max-T statistic exceeds the observed value [66].
Protocol for Cross-Cohort Replicable Functional Connectivity
This protocol outlines the process for identifying brain connectivity patterns that predict symptoms and replicate across independent validation cohorts, as demonstrated in schizophrenia research [68].
Step 1: Data Acquisition and Preprocessing Acquire resting-state functional MRI (rs-fMRI) data from at least two independent cohorts. Preprocess all data using a standardized pipeline, which typically includes realignment, normalization, and spatial smoothing. Extract whole-brain functional connectivity (FC) matrices for each subject.
Step 2: Individualized Predictive Modeling Within a discovery cohort, employ a machine learning model that integrates feature selection (e.g., to identify the most predictive FCs) with a regression or classification algorithm. Train this model to predict a continuous clinical score (e.g., positive or negative symptoms) from the FC matrix for each subject.
Step 3: Identification of Replicable Features Run the model on multiple random subsets of the discovery cohort. For each analysis, rank the features (FCs) by their importance in the prediction. Define "replicable FCs" as those that consistently appear within the top 80% of important features across these subsets and, crucially, in analogous analyses in the independent validation cohort(s) [68].
Step 4: Validation of Diagnostic and Predictive Utility Test the final set of replicable FCs in a separate validation cohort using a simple model (e.g., a back-propagation neural network) to confirm their ability to distinguish between clinical groups and predict symptom severity.
Visual Workflow of a Replicability Pipeline
The following diagram illustrates the logical flow for establishing a replicable finding, integrating principles from the validation cohort and cross-cohort methodologies discussed above.
The Scientist's Toolkit: Research Reagent Solutions
This table details essential materials and their functions for conducting rigorous small-sample studies, with a focus on reproducibility and validation.
| Reagent/Resource | Function in Research | Specific Role in Addressing Small n |
|---|---|---|
| Validated Behavioral/Cognitive Batteries [68] | Standardized tools to assess clinical symptoms and cognitive function. | Ensures consistent, reliable measurement of phenotypes across different cohorts, which is critical for pooling data or cross-validating results. Examples: PANSS, MCCB. |
| Preprocessed Cohort Datasets [68] | Independent, pre-collected datasets from studies like COBRE, FBIRN, and BSNIP. | Serve as essential validation cohorts to test the generalizability of findings from a small initial discovery sample. |
| Reporting Guidelines (e.g., CONSORT, STROBE) [69] | Checklists and frameworks for reporting study design and results. | Promotes transparency and completeness of reporting, allowing for better assessment of potential biases and feasibility of replication. |
| Raw Data & Associated Metadata [70] | The original, unprocessed data and detailed information on experimental conditions. | Enables re-analysis and meta-analytic techniques, which can combine raw data from several small studies to increase overall statistical power. |
| R Statistical Software & Syntax [67] | Open-source environment for statistical computing and graphics. | Provides implementations of specialized methods (e.g., Bayesian models, randomization tests) tailored for small sample size analysis, as detailed in resources like "Small Sample Size Solutions." |
Poor calibration, where a model's predicted probabilities systematically deviate from observed outcome frequencies, is a critical failure point that can undermine the real-world application of predictive models. This guide examines methodologies to diagnose, evaluate, and correct for poor calibration, a cornerstone for ensuring that research findings are reproducible and valid across different validation cohorts.
Experimental Protocols for Calibration Assessment
Protocol for A-Calibration and D-Calibration in Survival Analysis
A-calibration and D-calibration are goodness-of-fit tests designed specifically for censored survival data.
- Core Principle: Both methods use the Probability Integral Transform (PIT), which states that if a model's predicted survival function is correct, the transformed survival times will follow a standard uniform distribution. The tests check for deviations from this uniform distribution [71].
- Handling Censoring: This is the key difference between the two methods.
- D-Calibration: Uses an imputation approach. For a censored observation, it distributes its contribution evenly across the time intervals where its unobserved true event time might lie. This reliance on imputation under the null hypothesis can make the test conservative and reduce its statistical power [71].
- A-Calibration: Uses Akritas's goodness-of-fit test, which is designed for censored data. It estimates the censoring distribution directly from the data, avoiding imputation. This typically results in superior power to detect miscalibration, especially under moderate to heavy censoring [71].
- Test Statistic: Both methods ultimately use a Pearson’s goodness-of-fit test statistic, which compares observed and expected counts of PIT residuals in predefined intervals and follows a chi-square distribution under the null hypothesis of good calibration [71].
Protocol for Linear Re-calibration
This is a common and straightforward method to correct for systematic over- or underestimation, often used when applying a model to a new population.
- Core Principle: A simple linear model is fit to adjust the original model's predictions to better align with the observed outcomes in a new dataset [72].
- Procedure:
- Obtain the model's predictions on a held-out calibration dataset.
- Fit a linear regression model where the outcome is the observed result (or a transformation of it) and the predictor is the model's original prediction.
- The fitted slope and intercept from this regression become the calibration parameters.
- Case Study Example: When applying the Deeplasia bone age assessment AI to a Georgian population, researchers found it systematically overestimated bone age. They created a population-specific version, Deeplasia-GE, by fitting sex-specific linear regressions on a training set of 121 images. The calibration successfully reduced the signed mean difference from +5.35 months to +0.58 months in boys, and from +2.85 months to -0.03 months in girls [72].
Protocol for Independent Reproduction and Validation
This protocol assesses whether a published model's findings can be independently reproduced and validated.
- Core Principle: An independent team attempts to recreate the study population and reproduce the primary outcome findings using the same database and methods described in the original publication [4].
- Procedure:
- Systematic Identification: A large, random sample of published real-world evidence (RWE) studies is identified.
- Blinded Reproductions: For each study, analysts, blinded to the original results, attempt to reconstruct the study cohort by applying the reported inclusion/exclusion criteria, definitions for exposure, outcome, and covariates.
- Analysis of Reporting Clarity: The clarity of reporting for key study parameters (e.g., cohort entry date, algorithms for exposure duration, covariate definitions) is systematically evaluated.
- Comparison: The reproduced population size, baseline characteristics, and outcome effect sizes are compared to the original publication [4].
Comparative Performance Data
The following tables summarize quantitative data from experiments that evaluated and compared different calibration approaches.
Table 1: Comparison of A-Calibration vs. D-Calibration in Survival Analysis [71]
| Feature | A-Calibration | D-Calibration |
|---|---|---|
| Statistical Power | Similar or superior power in all cases | Lower power, especially with higher censoring |
| Sensitivity to Censoring | Robust | Highly sensitive |
| Handling of Censored Data | Akritas's test; estimates censoring distribution | Imputation approach under the null hypothesis |
| Key Advantage | Better power without disadvantages identified | Historical importance; simple concept |
Table 2: Impact of Linear Re-calibration on Model Performance [72]
| Performance Metric | Uncalibrated Deeplasia | Calibrated Deeplasia-GE |
|---|---|---|
| Mean Absolute Difference (MAD) | 6.57 months | 5.69 months |
| Root Mean Squared Error (RMSE) | 8.76 months | 7.37 months |
| Signed Mean Difference (SMD) - Males | +5.35 months | +0.58 months |
| Signed Mean Difference (SMD) - Females | +2.85 months | -0.03 months |
Table 3: Reproducibility of Real-World Evidence (RWE) Studies [4]
| Reproduction Aspect | Median & Interquartile Range (IQR) | Findings |
|---|---|---|
| Relative Effect Size | 1.0 [0.9, 1.1] (HR~original~/HR~reproduction~) | Strong correlation (r=0.85) but room for improvement |
| Relative Sample Size | 0.9 [0.7, 1.3] (Original/Reproduction) | 21% of studies had >2x or <0.5x sample size in reproduction |
| Baseline Characteristic Prevalence | 0.0% [-1.7%, 2.6%] (Original - Reproduction) | 17% of characteristics had >10% absolute difference |
Workflow Diagrams
Calibration Assessment and Workflow
A-Calibration Methodology
The Scientist's Toolkit
Table 4: Essential Reagents for Calibration Research
| Tool / Reagent | Function in Calibration Research |
|---|---|
| Independent Validation Cohort | A dataset not used in model development, essential for testing model performance and calibration in new data [73]. |
| Goodness-of-Fit Tests (A/D-Calibration) | Statistical tests to quantitatively assess whether a model's predictions match observed outcomes across the data distribution [71]. |
| Calibration Plots | Visual tools to display the relationship between predicted probabilities and observed event frequencies, helping to diagnose the type of miscalibration. |
| Linear Re-calibration Model | A simple statistical model (slope & intercept) used to correct for systematic over- or under-prediction in a new population [72]. |
| Reporting Guidelines (e.g., TRIPOD) | Checklists to ensure complete and transparent reporting of model development and validation, which is fundamental for reproducibility [73]. |
| Bayesian Hierarchical Modeling (BHM) | An advanced statistical approach that can reduce calibration uncertainty by pooling information across multiple data points or similar calibration curves [74]. |
Optimizing Hyperparameters for Generalizability Rather Than Single-Dataset Performance
In the pursuit of high-performing machine learning (ML) models, researchers and practitioners often focus intensely on optimizing hyperparameters to maximize performance on a single dataset. However, this narrow focus can lead to models that fail to generalize beyond their original development context, particularly in critical fields like healthcare and drug development. Model generalizability—the ability of a model to maintain performance on new, independent data from different distributions or settings—has emerged as a fundamental challenge for real-world ML deployment [75]. The replication crisis affecting many scientific domains extends to machine learning, where models exhibiting exceptional performance on internal validation often disappoint when applied to external cohorts or different healthcare institutions.
This guide examines hyperparameter optimization (HPO) strategies specifically designed to enhance model generalizability rather than single-dataset performance. We compare mainstream HPO techniques through the lens of generalizability, present experimental evidence from healthcare applications, and provide practical methodologies for developing models that maintain performance across diverse populations and settings. By framing HPO within the broader thesis of replicability and consensus model fits for validation cohorts, we aim to equip researchers with tools to build more robust, reliable ML systems for scientific and clinical applications.
Hyperparameter Optimization Techniques: A Generalizability Perspective
Hyperparameters are configuration variables that control the machine learning training process itself, set before the model learns from data [76]. Unlike model parameters learned during training, hyperparameters govern aspects such as model complexity, learning rate, regularization strength, and architecture decisions. Hyperparameter optimization is the process of finding the optimal set of these configuration variables to minimize a predefined loss function, typically measured via cross-validation [76].
The choice of HPO methodology significantly influences not only a model's performance but also its ability to generalize to new data. Below we compare prominent HPO techniques with specific attention to their implications for model generalizability:
Table 1: Hyperparameter Optimization Techniques and Their Generalizability Properties
| Technique | Mechanism | Generalizability Strengths | Generalizability Risks | Computational Cost |
|---|---|---|---|---|
| Grid Search [76] [77] | Exhaustive search over predefined parameter grid | Simple, reproducible, covers space systematically | High risk of overfitting to validation set; curse of dimensionality | Very high (grows exponentially with dimensions) |
| Random Search [76] [77] | Random sampling from parameter distributions | Better for high-dimensional spaces; less overfitting tendency | May miss optimal regions; results can vary between runs | Moderate to high (controlled by number of iterations) |
| Bayesian Optimization [76] [78] | Probabilistic model guides search toward promising parameters | Efficient exploration/exploitation balance; fewer evaluations needed | Model mismatch can misdirect search; can overfit validation scheme | Low to moderate (overhead of maintaining model) |
| Gradient-based Optimization [76] | Computes gradients of hyperparameters via differentiation | Suitable for many hyperparameters; direct optimization | Limited to continuous, differentiable hyperparameters; complex implementation | Low (leverages gradient information) |
| Evolutionary Algorithms [76] | Population-based search inspired by natural selection | Robust to noisy evaluations; discovers diverse solutions | Can require many function evaluations; convergence can be slow | High (requires large population sizes) |
| Population-based Training [76] | Joint optimization of weights and hyperparameters during training | Adaptive schedules; efficient resource use | Complex implementation; can be unstable | Moderate (parallelizable) |
| Early Stopping Methods [76] | Allocates resources to promising configurations | Resource-efficient; good for large search spaces | May prune potentially good configurations early | Low (avoids full training of poor configurations) |
The relationship between these optimization techniques and generalizability is mediated by several key mechanisms. Techniques that efficiently explore the hyperparameter space without overfitting the validation procedure tend to produce more generalizable models. Bayesian optimization often achieves superior generalizability by balancing exploration of uncertain regions with exploitation of known promising areas, typically requiring fewer evaluations than grid or random search [76] [78]. Similarly, early stopping-based approaches like Hyperband or ASHA promote generalizability by efficiently allocating computational resources to the most promising configurations without over-optimizing to a single dataset [76].
Experimental Evidence: HPO for Generalizability in Healthcare Applications
Case Study 1: Predicting Complications in Acute Leukemia
A 2025 study developed machine learning models to predict severe complications in patients with acute leukemia, explicitly addressing generalizability through rigorous validation methodologies [11].
Experimental Protocol:
- Objective: Predict severe complications within 90 days after induction chemotherapy
- Dataset: 2,870 patients from three tertiary haematology centres (derivation n=2,009; external validation n=861)
- Predictors: 42 candidate variables including demographics, comorbidity indices, laboratory values, disease biology, and treatment logistics
- Preprocessing: Multiple imputation for missing values, Winsorised z-scaling, correlation filtering
- Algorithms Compared: Elastic-Net, Random Forest, XGBoost, LightGBM, multilayer perceptron
- HPO Methodology: Nested 5-fold cross-validation with Bayesian hyperparameter optimization (50 iterations)
- Validation Approach: External temporal-geographical validation on completely separate centre
Results and Generalizability Findings: The LightGBM model achieved the highest performance in both derivation (AUROC 0.824 ± 0.008) and, crucially, maintained robust performance on external validation (AUROC 0.801), demonstrating successful generalizability [11]. The researchers attributed this generalizability to several HPO and modeling choices: (1) using nested rather than simple cross-validation to reduce overfitting, (2) applying appropriate regularization through hyperparameter tuning, and (3) utilizing Bayesian optimization which efficiently explored the hyperparameter space without over-optimizing to the derivation set.
Table 2: Performance Comparison Across Algorithms in Leukemia Complications Prediction
| Algorithm | Derivation AUROC | External Validation AUROC | AUPRC | Calibration Slope |
|---|---|---|---|---|
| LightGBM | 0.824 ± 0.008 | 0.801 | 0.628 | 0.97 |
| XGBoost | 0.817 ± 0.009 | 0.794 | 0.615 | 0.95 |
| Random Forest | 0.806 ± 0.010 | 0.785 | 0.601 | 0.92 |
| Elastic-Net | 0.791 ± 0.012 | 0.776 | 0.587 | 0.98 |
| Multilayer Perceptron | 0.812 ± 0.011 | 0.782 | 0.594 | 0.89 |
Case Study 2: Multi-site COVID-19 Screening
A 2022 multi-site study investigated ML model generalizability for COVID-19 screening across four NHS Hospital Trusts, providing critical insights into customization approaches for improving cross-site performance [75].
Experimental Protocol:
- Objective: Screen emergency admissions for COVID-19 across different healthcare settings
- Dataset: Electronic health record data from four UK NHS Trusts
- Approaches Compared:
- Ready-made model applied "as-is"
- Decision threshold adjustment using site-specific data
- Finetuning via transfer learning using site-specific data
- Validation: Strict separation between source and target sites with independent preprocessing
Generalizability Findings: The study revealed substantial performance degradation when models were applied "as-is" to new hospital sites without customization [75]. However, two adaptation techniques significantly improved generalizability: (1) readjusting decision thresholds using site-specific data, and (2) finetuning models via transfer learning. The transfer learning approach achieved the best results (mean AUROCs between 0.870 and 0.925), demonstrating that limited site-specific customization can dramatically improve cross-site performance without requiring retraining from scratch or sharing sensitive data between institutions.
Case Study 3: Frailty Assessment Tool Development
A 2025 multi-cohort study developed a simplified frailty assessment tool using machine learning and validated it across four independent cohorts, providing insights into feature selection and HPO for generalizability [13].
Experimental Protocol:
- Objective: Develop a clinically feasible frailty assessment tool with generalizability across populations
- Datasets: NHANES (n=3,480), CHARLS (n=16,792), CHNS (n=6,035), SYSU3 CKD (n=2,264)
- Feature Selection: Five complementary algorithms (LASSO, VSURF, Boruta, varSelRF, RFE) to identify minimal predictive feature set
- Algorithms: 12 ML approaches across ensemble methods, neural networks, distance-based models, and regression
- HPO Approach: Systematic hyperparameter tuning with cross-validation
Results and Generalizability Findings: The study identified just eight readily available clinical parameters that maintained robust predictive power across diverse populations [13]. The XGBoost algorithm demonstrated superior generalizability across training (AUC 0.963), internal validation (AUC 0.940), and external validation (AUC 0.850) datasets. This performance consistency across heterogeneous cohorts highlights how parsimonious model design combined with appropriate HPO can enhance generalizability. The intersection of multiple feature selection methods identified a core set of stable predictors less susceptible to site-specific variations.
Methodological Pitfalls in HPO That Undermine Generalizability
Several common methodological errors during hyperparameter optimization can create overoptimistic performance estimates and undermine model generalizability:
Violation of Independence Assumption
Applying preprocessing techniques such as oversampling or data augmentation before splitting data into training, validation, and test sets creates data leakage that artificially inflates perceived performance [79]. One study demonstrated that improper oversampling before data splitting artificially inflated F1 scores by 71.2% for predicting local recurrence in head and neck cancer, and by 46.0% for distinguishing histopathologic patterns in lung cancer [79]. Similarly, distributing data points from the same patient across training, validation, and test sets artificially improved F1 scores by 21.8% [79]. These practices violate the fundamental independence assumption required for proper validation and produce models that fail to generalize.
Inappropriate Performance Metrics and Baselines
Relying on inappropriate performance metrics or comparisons during HPO can misguide the optimization process [79]. For instance, using accuracy with imbalanced datasets can lead to selecting hyperparameters that achieve high accuracy by simply predicting the majority class. Similarly, failing to compare against appropriate baseline models during HPO can create the illusion of performance where none exists. Metrics should be chosen to reflect the real-world application context and class imbalances.
Batch Effects and Domain Shift
Batch effects—systematic technical differences between datasets—can severely impact generalizability but are rarely considered during HPO [79]. One study demonstrated that a pneumonia detection model achieving an F1 score of 98.7% on the original data correctly classified only 3.86% of samples from a new dataset of healthy patients due to batch effects [79]. Hyperparameters optimized without considering potential domain shift yield models that overfit to technical artifacts rather than learning biologically or clinically relevant patterns.
Diagram 1: HPO Practices Impact on Model Generalizability. Proper practices (green) promote generalizability while pitfalls (red) undermine it.
Best Practices for HPO Targeting Generalizability
Validation Strategies for Robust HPO
Nested Cross-Validation: Implement nested rather than simple cross-validation, where an inner loop performs HPO and an outer loop provides performance estimation [11]. This prevents overfitting the validation scheme and provides more realistic performance estimates.
External Validation: Whenever possible, reserve completely external datasets—from different institutions, geographical locations, or time periods—for final model evaluation after HPO [11] [13]. This represents the gold standard for assessing generalizability.
Multi-site Validation: For healthcare applications, validate across multiple clinical sites with independent preprocessing to simulate real-world deployment conditions [75].
HPO Techniques Conducive to Generalizability
Bayesian Optimization: For most scenarios, Bayesian optimization provides the best balance between efficiency and generalizability by modeling the objective function and focusing evaluations on promising regions [76] [78].
Regularization-focused Search: Allocate substantial hyperparameter search budget to regularization parameters (dropout rates, L1/L2 penalties) rather than focusing exclusively on capacity parameters [76].
Early Stopping Methods: Utilize early stopping-based HPO methods like Hyperband or ASHA for large search spaces, as they efficiently allocate resources without over-optimizing poor configurations [76].
Diagram 2: HPO Workflow for Generalizable Models. The workflow emphasizes nested data splitting, appropriate HPO technique selection, and rigorous external validation.
Table 3: Essential Research Reagents and Tools for Generalizable HPO
| Tool/Resource | Function | Implementation Considerations |
|---|---|---|
| Bayesian Optimization Frameworks (e.g., Scikit-optimize, Optuna) | Efficient hyperparameter search using probabilistic models | Choose based on parameter types (continuous, discrete, categorical) and parallelization needs |
| Nested Cross-Validation Implementation | Proper validation design preventing overfitting | Computationally expensive but necessary for unbiased performance estimation |
| Multiple Imputation Methods | Handling missing data without leakage | Implement after data splitting; use chained equations for complex missingness patterns |
| Feature Selection Stability Analysis | Identifying robust predictors across datasets | Use multiple complementary algorithms (LASSO, RFE, Boruta) and intersect results |
| Domain Adaptation Techniques | Adjusting models to new distributions | Particularly important for healthcare applications across different institutions |
| Model Interpretation Tools (e.g., SHAP, LIME) | Explaining predictions and building trust | Critical for clinical adoption; provides validation of biological plausibility |
| Transfer Learning Capabilities | Fine-tuning pre-trained models on new data | Effective for neural networks; requires careful learning rate selection |
Optimizing hyperparameters for generalizability rather than single-dataset performance requires a fundamental shift in methodology and mindset. The techniques and evidence presented demonstrate that generalizability is not an afterthought but must be embedded throughout the HPO process—from experimental design through validation. The replication crisis in machine learning necessitates rigorous approaches that prioritize performance consistency across diverse populations and settings, particularly in high-stakes fields like healthcare and drug development.
Successful HPO for generalizability incorporates several key principles: (1) strict separation between training, validation, and test sets with independent preprocessing; (2) appropriate HPO techniques like Bayesian optimization that balance exploration and exploitation; (3) comprehensive external validation across multiple sites and populations; and (4) methodological vigilance against pitfalls like data leakage and batch effects. By adopting these practices, researchers can develop models that not only perform well in controlled experiments but maintain their effectiveness in real-world applications, ultimately advancing the reliability and utility of machine learning in scientific discovery and clinical practice.
Feature mismatch represents a critical challenge in the development and validation of predictive models, particularly in biomedical research and drug development. This phenomenon occurs when the variables or data structures available in external validation cohorts differ substantially from those used in the original model development, potentially compromising model performance, generalizability, and real-world applicability. The expanding use of machine learning and complex statistical models in clinical decision-making has heightened the importance of addressing feature mismatch, as it directly impacts the replicability and trustworthiness of predictive algorithms across diverse populations and healthcare settings.
Within the broader context of replicability consensus model fits validation cohorts research, feature mismatch presents both a methodological and practical obstacle. When models developed on one dataset fail to generalize because of missing or differently measured variables in new populations, the entire evidence generation process is undermined. Recent systematic assessments of real-world evidence studies have demonstrated that incomplete reporting of key study parameters and variable definitions affects a substantial proportion of research, with one large-scale reproducibility evaluation finding that reproduction teams needed to make assumptions about unreported methodological details in the majority of studies analyzed [4]. This underscores the pervasive nature of feature description gaps that contribute to mismatch challenges.
The consequences of unaddressed feature mismatch can be significant, ranging from reduced predictive accuracy to complete model failure when critical predictors are unavailable in new settings. In clinical applications, this can directly impact patient care and resource allocation decisions that rely on accurate risk stratification. Therefore, developing robust strategies to anticipate, prevent, and mitigate feature mismatch is essential for advancing replicable predictive modeling in biomedical research.
Comparative Analysis of Feature Mismatch Solutions
Multiple approaches have emerged to address feature mismatch in predictive modeling, each with distinct strengths, limitations, and implementation requirements. The table below summarizes the primary strategies, their underlying methodologies, and key performance considerations based on current research and implementation studies.
Table 1: Comparative Analysis of Feature Mismatch Solution Strategies
| Solution Strategy | Methodological Approach | Data Requirements | Implementation Complexity | Best-Suited Scenarios |
|---|---|---|---|---|
| Variable Harmonization | Standardizing variable definitions across cohorts through unified data dictionaries and transformation rules | Original raw data or sufficient metadata for mapping | Moderate | Prospective studies with collaborating institutions; legacy datasets with similar measurements |
| Imputation Methods | Estimating missing features using statistical (MICE) or machine learning approaches | Partial feature availability or correlated variables | Low to High | Datasets with sporadic missingness; strongly correlated predictor availability |
| Feature Selection Prioritization | Identifying robust core feature sets resistant to cohort heterogeneity through stability measures | Multiple datasets with varying variable availability | Low to Moderate | Resource-limited settings; rapid model deployment across diverse settings |
| Consensus Modeling | Developing ensemble predictions across multiple algorithms and feature subsets | Multiple datasets or resampled versions of original data | High | Complex phenotypes; high-stakes predictions requiring maximal robustness |
| Transfer Learning | Using pre-trained models adapted to new cohorts with limited feature overlap | Large source dataset; smaller target dataset with different features | High | Imaging, omics, and complex data types; substantial source data available |
Among these approaches, consensus modeling has demonstrated particular promise for addressing feature mismatch while maintaining predictive performance. In the First EUOS/SLAS joint compound solubility challenge, a consensus model based on 28 individual approaches achieved superior performance by combining diverse models calculated using both descriptor-based and representation learning methods [80]. This ensemble approach effectively decreased both bias and variance inherent in individual models, highlighting the power of methodological diversity in overcoming dataset inconsistencies. The winning model specifically leveraged a combination of traditional descriptor-based methods with advanced Transformer CNN architectures, illustrating how integrating heterogeneous modeling approaches can compensate for feature-level discrepancies across validation cohorts.
Similarly, research on variable and feature selection strategies for clinical prediction models has emphasized the importance of methodical predictor selection. A comprehensive simulation study protocol registered with the Open Science Framework aims to compare multiple variable selection methodologies, including both traditional statistical approaches (e.g., p-value based selection, AIC) and machine learning techniques (e.g., random forests, LASSO, Boruta algorithm) [81]. This planned evaluation across both classical regression and machine learning paradigms will provide critical evidence for selecting the most robust variable selection strategies when facing potential feature mismatch across development and validation settings.
Experimental Protocols for Feature Mismatch Methodologies
Variable Harmonization Protocol
The variable harmonization process begins with a systematic mapping exercise to identify corresponding variables across cohorts. This protocol was implemented in a large-scale cancer prediction algorithm development study that successfully integrated data from over 7.4 million patients across multiple UK databases [82]. The methodology involved:
- Creating a unified data dictionary specifying all variables, their definitions, measurement units, coding schemes, and permissible values before data extraction
- Implementing cross-walking procedures for transforming similar but not identical measurements into common metrics using predetermined transformation rules
- Establishing quality control checks to verify harmonization success through summary statistics and distribution comparisons across cohorts
This approach enabled the development of models that maintained high discrimination (c-statistics >0.87 for most cancers) across validation cohorts despite inherent database differences [82]. The protocol emphasizes proactive harmonization rather than retrospective adjustments, significantly reducing feature mismatch during external validation.
Consensus Modeling with Heterogeneous Features
The consensus modeling protocol follows a structured process to integrate predictions from multiple models with different feature sets, as demonstrated in the EUOS/SLAS solubility challenge [80]:
- Develop multiple base models using different algorithms and feature subsets that capture complementary aspects of the prediction task
- Train each model on available features in the development cohort, allowing for variation in feature availability across models
- Generate predictions from each model on the validation cohort using whichever features are available for that specific model
- Combine predictions using weighted averaging based on each model's performance in internal validation, with weights optimized to maximize ensemble performance
This protocol explicitly accommodates feature mismatch by not requiring identical feature availability across all model components. Instead, it leverages the strengths of diverse feature representations to create a robust composite prediction. In the solubility challenge, this approach outperformed all individual models, demonstrating the power of consensus methods to overcome limitations of individual feature sets [80].
Visualization of Strategic Approaches
The following diagram illustrates the comprehensive strategic framework for addressing feature mismatch, from problem identification through solution implementation and validation:
Strategic Framework for Addressing Feature Mismatch
The visualization outlines the systematic process for addressing feature mismatch, beginning with comprehensive data assessment to characterize the nature and extent of the problem, followed by strategic solution selection based on the specific mismatch context, and concluding with rigorous performance validation using appropriate metrics.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Essential Research Reagents and Computational Tools for Feature Mismatch Research
| Tool/Reagent | Specific Function | Application Context | Implementation Examples |
|---|---|---|---|
| Multiple Imputation by Chained Equations (MICE) | Handles missing data by creating multiple plausible imputations | Missing feature scenarios in validation cohorts | R mice package; Python fancyimpute |
| LASSO Regularization | Automated feature selection while preventing overfitting | High-dimensional data with correlated predictors | R glmnet; Python scikit-learn |
| Boruta Algorithm | Wrapper method for all-relevant feature selection using random forests | Identifying robust features stable across cohorts | R Boruta package |
| SHapley Additive exPlanations (SHAP) | Interprets model predictions and feature importance | Understanding feature contributions in complex models | Python shap library |
| TRIPOD Statement | Reporting guideline for prediction model studies | Ensuring transparent methodology description | 33-item checklist for model development and validation |
| Consensus Model Ensembles | Combines predictions from multiple algorithms | Leveraging complementary feature strengths | Weighted averaging; stacking methods |
These tools form the foundation for implementing the strategies discussed throughout this article. Their selection should be guided by the specific feature mismatch context, available computational resources, and the intended application environment for the predictive model.
Addressing feature mismatch is not merely a technical challenge but a fundamental requirement for enhancing the replicability and real-world applicability of predictive models in biomedical research. The strategies outlined—from careful variable harmonization to sophisticated consensus modeling—provide a toolkit for researchers confronting the common scenario of validation cohorts lacking key variables. The experimental evidence demonstrates that proactive approach to feature management, rather than retrospective adjustments, yields superior model performance across diverse validation settings.
The integration of these approaches within a consensus framework offers particular promise, as evidenced by performance in competitive challenges and large-scale healthcare applications [82] [80]. As the field moves toward more transparent and reproducible research practices, the systematic addressing of feature mismatch will play an increasingly important role in validating predictive algorithms that can truly inform clinical and drug development decisions across diverse populations and healthcare settings.
Computational reproducibility is fundamental to scientific research, ensuring that findings are reliable, valid, and generalizable [83]. In public health and biomedical research, reproducibility is crucial for informing policy decisions, developing effective interventions, and improving health outcomes [83]. The ideal of computationally reproducible research dictates that "an article about computational science in a scientific publication is not the scholarship itself, it is merely advertising of the scholarship. The actual scholarship is the complete software development environment and the complete set of instructions which generated the figures" [84]. Despite this ideal, empirical evidence reveals a significant reproducibility crisis. Analysis of 296 R projects from the Open Science Framework (OSF) revealed that only 25.87% completed successfully without error when executed in reconstructed computational environments [84]. This comprehensive guide examines the current evidence, compares best practices, and provides actionable protocols for enhancing computational reproducibility.
Quantitative Evidence: The State of Computational Reproducibility
Empirical studies consistently demonstrate substantial challenges in computational reproducibility across research domains. The following table summarizes key findings from recent large-scale assessments:
Table 1: Empirical Evidence of Computational Reproducibility Challenges
| Study Focus | Sample Size | Success Rate | Primary Barriers Identified |
|---|---|---|---|
| R Projects on OSF [84] | 264 projects | 25.87% | Undeclared dependencies (98.8% lacked dependency files), invalid file paths, system-level issues |
| Harvard Dataverse R Files [84] | Not specified | 26% (74% failed) | Missing dependencies, environment configuration issues |
| Jupyter Notebooks [84] | Not specified | 11.6%-24% | Environment issues, missing dependencies |
| Manual Reproduction Attempts [84] | 30 papers | <80% (≥20% partially reproducible) | Incomplete code, missing documentation |
The scarcity of explicit dependency documentation is particularly striking. Analysis of OSF R projects found that 98.8% lacked any formal dependency descriptions, such as DESCRIPTION files (0.8%), Dockerfile (0.4%), or environment configuration files (0%) [84]. This deficiency represents the most significant barrier to successful computational reproduction.
Best Practices Comparison: Framework for Reproducible Research
Effective computational reproducibility requires implementing structured practices throughout the research workflow. The following table compares essential practices across computational environments:
Table 2: Comparative Analysis of Computational Reproducibility Practices
| Practice Category | Specific Tools/Approaches | Implementation Benefits | Evidence Support |
|---|---|---|---|
| Project Organization | RStudio Projects; code/, data/, figures/ folders [85] |
Isolated environments, standardized structure | Foundational for 25.87% of successful executions [84] |
| Dependency Management | {here} package; avoid setwd() [85]; renv.lock, sessionInfo() [84] |
Portable paths, explicit dependency tracking | 98.8% of failed projects lacked these [84] |
| Environment Containerization | Docker, Code Ocean, MyBinder [86] [84] | Consistent computational environments across systems | Automated pipeline increased execution success [84] |
| Code Documentation | Google R Style Guide [85]; README files; comments [87] | Enhanced understandability and reuse | Critical for interdisciplinary collaboration [86] |
| Version Control & Sharing | Git; GitHub with Zenodo/GitHub integration [88]; FAIR principles [89] | Track changes, enable citation, ensure persistence | Required by publishers and funders [86] [88] |
Research demonstrates that combining multiple practices creates synergistic benefits. For instance, containerization technologies like Docker create consistent and isolated environments across different systems, while version control tracks changes to code and data over time [84] [83]. The integration of these approaches addresses both environment consistency and change management.
Experimental Protocols for Validation Studies
Automated Reproducibility Assessment Pipeline
Recent research has developed sophisticated methodologies for assessing computational reproducibility at scale. The following workflow illustrates the automated pipeline used to evaluate R projects from the Open Science Framework:
Diagram 1: Automated reproducibility assessment pipeline
This protocol employs static dataflow analysis (flowR) to automatically extract dependencies from R scripts, generates appropriate Docker configuration files, builds containerized environments using repo2docker, executes the code in isolated environments, and publishes the resulting environments for community validation [84]. This approach successfully reconstructed computational environments directly from project source code, enabling systematic assessment of reproducibility barriers.
Machine Learning Model Validation Framework
Research employing machine learning approaches demonstrates rigorous validation methodologies that align with reproducibility principles. The following workflow illustrates a multi-cohort validation framework for clinical prediction models:
Diagram 2: Machine learning model validation framework
This protocol incorporates data preprocessing with multiple imputation for missing values, Winsorised z-scaling, and correlation filtering [11]. Model development utilizes nested cross-validation with Bayesian hyperparameter optimization, while validation follows TRIPOD-AI and PROBAST-AI recommendations through internal, external, and subgroup analyses [11] [13]. The implementation of standardized evaluation metrics (AUROC, calibration, decision-curve analysis) enables consistent comparison across studies and facilitates replication.
Research Reagent Solutions: Essential Tools for Reproducible Research
Implementing computational reproducibility requires specific tools and platforms that address different aspects of the research workflow. The following table details essential solutions:
Table 3: Research Reagent Solutions for Computational Reproducibility
| Tool Category | Specific Solutions | Function & Application | Evidence Base |
|---|---|---|---|
| Environment Management | Docker, Code Ocean, renv | Containerization for consistent computational environments | Automated containerization enabled 25.87% execution success [84] |
| Version Control Systems | Git, GitHub, SVN | Track changes to code and data over time | Recommended for transparency and collaboration [83] |
| Reproducibility Platforms | MyBinder, Zenodo, Figshare | Share executable environments with permanent identifiers | MyBinder enables easy verification by others [84] |
| Documentation Tools | README files, CodeMeta.json, CITATION.cff | Provide human- and machine-readable metadata | Essential for FAIR compliance and citability [87] |
| Statistical Programming | R/Python with specific packages ({here}, sessionInfo) | Implement reproducible analytical workflows | {here} package avoids setwd() dependency [85] |
These tools collectively address the primary failure modes identified in reproducibility research. Environment management systems solve dependency declaration problems, version control addresses code evolution tracking, and reproducibility platforms provide persistent access to research materials.
The empirical evidence clearly demonstrates that computational reproducibility remains a significant challenge, with success rates below 26% for R-based research projects [84]. The primary barriers include undeclared dependencies, invalid file paths, and insufficient documentation of computational environments. Successful reproducibility requires implementing integrated practices including project organization, dependency management, environment containerization, and comprehensive documentation. The experimental protocols and research reagents outlined in this guide provide actionable pathways for researchers to enhance the reproducibility of their computational work. As computational methods become increasingly central to scientific advancement, embracing these practices is essential for producing reliable, valid, and impactful research.
Proving Generalizability: Rigorous Validation Across Diverse Cohorts
External validation is a cornerstone of robust predictive model development, serving as the ultimate test of a model's generalizability and clinical utility. Moving beyond internal validation, it assesses how a model performs on data originating from different populations, time periods, or healthcare settings. This process is fundamental to the replicability consensus model, which posits that a model's true value is not determined by its performance on its development data but by its consistent performance across heterogeneous, independent cohorts. The design of an external validation study—specifically, the strategy for splitting data—directly influences the credibility of the performance estimates and dictates the model's readiness for real-world deployment. This guide objectively compares the three primary split strategies—temporal, geographic, and institutional—by examining their experimental protocols, performance outcomes, and implications for researchers and drug development professionals.
Comparative Analysis of External Validation Split Strategies
The following table synthesizes experimental data and methodological characteristics from recent studies to provide a direct comparison of the three core external validation strategies.
Table 1: Comparative Analysis of External Validation Split Strategies
| Split Strategy | Core Experimental Protocol | Typical Performance Metrics Reported | Reported Impact on Model Performance (from Literature) | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| Temporal Validation | Model developed on data from time period T1 (e.g., 2015-2017); validated on data from a subsequent, mutually exclusive period T2 (e.g., 2018-2019) from the same institution(s) [90]. | - Calibration Slope & Intercept [91]- Expected Calibration Error (ECE) [91]- Area Under Curve (AUC) [90]- Brier Score [91] | Logistic Regression: Often retains a calibration slope close to 1.0 under temporal drift [91].Gradient-Boosted Trees (GBDT): Can achieve lower Brier scores and ECE than regression, but may show greater slope variation [91].Example: AUC drop from 0.732 (training) to 0.703 (internal temporal validation) observed in a radiomics study [92]. | Tests model resilience to temporal drift (e.g., evolving clinical practices, changing disease definitions). Logistically simpler to implement within a single center. | Does not assess geographic or cross-site generalizability. Performance can be optimistic compared to fully external tests. |
| Geographic/ Institutional Validation | Model developed on data from one or more institutions/regions (e.g., US SEER database); validated on data from a completely separate institution or country (e.g., a hospital in China) [90]. | - C-index [90]- AUC for 3, 5, 10-year overall survival [90]- Net Benefit from Decision Curve Analysis (DCA) [91] | General Trend: All model types can experience significant performance degradation.Example: A cervical cancer nomogram showed strong internal performance (C-index: 0.885) and maintained it externally, though with a slight decrease (C-index: 0.872) [90].Deep Neural Networks (DNNs): Frequently underestimate risk for high-risk deciles in new populations [91]. | Provides the strongest test of generalizability across different patient demographics, equipment, and treatment protocols. Essential for confirming broad applicability. | Most logistically challenging and costly to acquire data. Highest risk of performance decay, potentially necessitating model recalibration or retraining. |
| Hybrid Validation (Temporal + Geographic) | Model is developed on a multi-source dataset and validated on data from a different institution and a later time period. This represents the most rigorous validation tier [91]. | - All metrics from temporal and geographic splits.- Emphasis on calibration and decision utility post-recalibration. | Foundation Models: Show sample-efficient adaptation in low-label regimes but often require local recalibration to achieve ECE ≤ 0.03 and positive net benefit [91].Recalibration: Critical for utility; net benefit increases only when ECE is maintained ≤ 0.03 [91]. | Most realistic simulation of real-world deployment scenarios. Offers the most conservative and trustworthy performance estimate. | Extreme logistical complexity. Often reveals the need for site-specific or periodic model updating before deployment. |
Detailed Experimental Protocols for Key Studies
The comparative data in Table 1 is derived from structured experimental protocols. Below are the detailed methodologies for two cited studies that exemplify rigorous external validation.
Protocol 1: Cervical Cancer Survival Nomogram (Geographic/Institutional Split)
This study developed a nomogram to predict overall survival (OS) in cervical cancer patients, with a primary geographic/institutional validation [90].
- Data Sourcing and Cohorts:
- Training & Internal Validation Cohort: 13,592 patient records were obtained from the Surveillance, Epidemiology, and End Results (SEER) database in the United States (2000-2020). These were randomly split 7:3 into a training cohort (TC, n=9,514) and an internal validation cohort (IVC, n=4,078) [90].
- External Validation Cohort (EVC): 318 patients were sourced from Yangming Hospital Affiliated to Ningbo University in China (2008-2020), representing a distinct geographic and institutional population [90].
- Predictor and Outcome Definition:
- Predictors: Univariate and multivariate Cox regression identified six key predictors: age, tumor grade, FIGO 2018 stage, tumor size, lymph node metastasis (LNM), and lymphovascular space invasion (LVSI). The model was visualized as a nomogram [90].
- Outcome: The primary endpoint was overall survival (OS), with predictions for 3-year, 5-year, and 10-year OS [90].
- Validation and Analysis:
- Performance Assessment: The model's discrimination was evaluated using the Concordance Index (C-index) and time-dependent Area Under the Receiver Operating Characteristic Curve (AUC). Calibration was assessed with calibration plots, and clinical utility was evaluated with Decision Curve Analysis (DCA) [90].
- Results: The model demonstrated strong performance, with the external validation cohort showing a C-index of 0.872 (95% CI: 0.829–0.915) and AUCs of 0.892, 0.896, and 0.903 for 3, 5, and 10-year OS, respectively, confirming its geographic transportability [90].
Protocol 2: Chronic-Disease Risk Model Comparison (Temporal & Geographic Shifts)
This narrative review synthesized evidence from 2019-2025 on how various model classes calibrate and transport under shift conditions [91].
- Study Design and Data Synthesis:
- Method: A narrative synthesis of comparative studies was conducted. Searches were performed on PubMed, Scopus, and arXiv for studies comparing classical regression, tree-based methods, deep neural networks (DNNs), and foundation models [91].
- Focus: The analysis specifically focused on studies reporting calibration metrics (ECE, calibration slope/intercept, Brier score), transportability via temporal or site-based validation, and decision utility (net benefit) [91].
- Model Training and Validation Strategy:
- Temporal Shift: Models were trained on data from one time period (e.g., 2015-2017) and validated on a later hold-out set from the same institutions (e.g., 2018-2019) [91].
- Geographic/Site Shift: Models were developed on data from one set of hospitals or a national registry and then validated on data from entirely different healthcare systems or countries [91].
- Key Metrics and Comparative Findings:
- Performance Metrics: Primary outcomes included Expected Calibration Error (ECE), calibration slope, Brier score, and net benefit from Decision Curve Analysis [91].
- Model Class Comparison: The review found that modern tree-based methods often achieved lower Brier scores and ECE than logistic regression, but logistic regression often retained a calibration slope closer to 1.0 under temporal drift. DNNs frequently exhibited miscalibration, underestimating risk for high-risk patients in new settings. Foundation models showed promise in low-label regimes but typically required local recalibration to achieve optimal calibration and net benefit [91].
Visualizing External Validation Workflows
The following diagram illustrates the logical workflow and decision points in designing a rigorous external validation study, incorporating elements from the cited research.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key resources and methodological components essential for conducting the types of external validation studies featured in this guide.
Table 2: Research Reagent Solutions for External Validation Studies
| Item Name | Function/Application in External Validation |
|---|---|
| SEER (Surveillance, Epidemiology, and End Results) Database | A comprehensive cancer registry in the United States frequently used as a large-scale, population-based source for developing training cohorts and conducting internal validation [90]. |
| Institutional Electronic Health Record (EHR) Systems | Source of localized patient data for creating external validation cohorts, enabling tests of geographic and institutional generalizability [90] [91]. |
| R/Python Statistical Software (e.g., R 4.3.2) | Primary environments for performing statistical analyses, including Cox regression, model development, and calculating performance metrics like the C-index and AUC [90]. |
| Calibration Metrics (ECE, Slope, Intercept) | Statistical tools to quantify the agreement between predicted probabilities and observed outcomes. Critical for evaluating model reliability under shift conditions [91]. |
| Decision Curve Analysis (DCA) | A methodological tool to evaluate the clinical utility and net benefit of a model across different probability thresholds, informing decision-making in deployment [90] [91]. |
| ITK-SNAP / PyRadiomics | Software tools used in radiomics studies for manual tumor segmentation (ITK-SNAP) and automated extraction of quantitative imaging features (PyRadiomics) from medical scans [92]. |
| Foundation Model Backbones | Pre-trained deep learning models (e.g., transformer architectures) that can be fine-tuned with limited task-specific data, offering potential in low-label regimes across sites [91]. |
In the evolving landscape of clinical prediction models (CPMs), the pursuit of replicability and generalizability across validation cohorts has intensified the focus on comprehensive performance assessment. While the Area Under the Receiver Operating Characteristic Curve (AUROC) has long been the dominant metric for evaluating diagnostic and prognostic models, a growing consensus recognizes that discrimination alone provides an incomplete picture of real-world usefulness [93]. A model with exceptional AUROC can still produce systematically miscalibrated predictions that mislead clinical decision-making, while a well-calibrated model with modest discrimination may offer substantial clinical utility when applied appropriately [94]. This guide examines the complementary roles of AUROC, calibration, and clinical utility metrics, providing researchers and drug development professionals with experimental frameworks for robust model evaluation and comparison.
The challenge of model replication across diverse populations underscores the necessity of this multi-faceted approach. Recent evidence demonstrates substantial heterogeneity in AUROC values when CPMs are validated externally, with one analysis of 469 cardiovascular prediction models revealing that performance in new settings remains highly uncertain even after multiple validations [95]. This instability necessitates evaluation frameworks that extend beyond discrimination to encompass calibration accuracy and net benefit across clinically relevant decision thresholds, particularly for models intended to inform patient care across diverse healthcare systems and patient populations.
Metric Deep Dive: Definitions, Methods, and Interpretation
AUROC: The Discrimination Metric
Definition and Interpretation: The Area Under the Receiver Operating Characteristic (ROC) Curve quantifies a model's ability to distinguish between two outcome classes (e.g., diseased vs. non-diseased) across all possible classification thresholds [96]. The ROC curve plots the true positive rate (sensitivity) against the false positive rate (1-specificity), with the AUROC representing the probability that a randomly selected positive case will receive a higher predicted probability than a randomly selected negative case [97]. An AUROC of 1.0 represents perfect discrimination, 0.5 indicates discrimination no better than chance, and values below 0.5 suggest worse than random performance.
Experimental Protocols for Evaluation:
- Calculation Methods: AUROC can be calculated parametrically under binormal distribution assumptions or nonparametrically using Wilcoxon statistics, with the latter being more practical for non-Gaussian data or small sample sizes [97].
- Validation Procedures: Internal validation via bootstrapping (e.g., 2000 iterations) provides optimism-corrected estimates, while external validation across geographically or temporally distinct cohorts assesses generalizability [98] [95].
- Performance Interpretation: AUROC values of 0.7-0.8 are typically considered acceptable, 0.8-0.9 excellent, and >0.9 outstanding, though these benchmarks vary by clinical context and baseline prevalence [11].
Table 1: AUROC Performance Interpretation Guide
| AUROC Range | Discrimination Performance | Clinical Context Example |
|---|---|---|
| 0.5 | No discrimination | Random classifier |
| 0.7-0.8 | Acceptable | Prolonged opioid use prediction model [98] |
| 0.8-0.9 | Excellent | Severe complications in acute leukemia [11] |
| >0.9 | Outstanding | Best-performing deterioration models [99] |
Limitations and Stability Concerns: AUROC has notable limitations, including insensitivity to predicted probability scale and vulnerability to performance instability across populations. A 2025 analysis of 469 CPMs with 1,603 external validations found substantial between-study heterogeneity (τ = 0.055), meaning the 95% prediction interval for a model's AUROC in a new setting has a width of at least ±0.1, regardless of how many previous validations have been conducted [95]. This inherent uncertainty necessitates complementary metrics for comprehensive model assessment.
Calibration: The Accuracy of Predictions
Definition and Interpretation: Calibration measures the agreement between predicted probabilities and observed outcomes, answering "When a model predicts a 70% risk, does the event occur 70% of the time?" [94]. A perfectly calibrated model demonstrates that among all cases receiving a predicted probability of P%, exactly P% experience the outcome. Poor calibration can persist even with excellent discrimination, creating potentially harmful scenarios where risk predictions systematically over- or underestimate true probabilities [94].
Experimental Protocols for Evaluation:
- Calibration Plots: Visualize the relationship between predicted probabilities (x-axis) and observed outcomes (y-axis) with a smoothing curve or binned aggregates. Perfect calibration follows the 45-degree diagonal [94].
- Statistical Measures: The calibration slope assesses whether predictions are too extreme (slope <1) or too conservative (slope >1), while the calibration-in-the-large evaluates whether predictions are systematically over- or under-estimated [11].
- Brier Score: Decomposes into calibration and refinement components, with lower scores (closer to 0) indicating better overall accuracy [98] [94].
Table 2: Calibration Assessment Methods
| Method | Calculation | Interpretation | Application Example |
|---|---|---|---|
| Calibration Plot | Predicted vs. observed probabilities by deciles | Deviation from diagonal indicates miscalibration | Visual inspection of curve [94] |
| Brier Score | Mean squared difference between predictions and outcomes | 0 = perfect, 1 = worst; Lower is better | 0.011-0.012 for clinical deterioration models [99] |
| Calibration Slope/Intercept | Logistic regression of outcome on log-odds of predictions | Slope=1, intercept=0 indicates perfect calibration | Slope=0.97, intercept=-0.03 in leukemia model [11] |
Calibration Techniques: For ill-calibrated models, methods like isotonic regression or Platt scaling can transform outputs to improve calibration. A comparison of variant-scoring methods demonstrated that isotonic regression significantly improved Brier scores across multiple algorithms, with ready-to-use implementations available in libraries like scikit-learn [94].
Clinical Utility: The Impact on Decision-Making
Definition and Interpretation: Clinical utility measures the value of a prediction model for guiding clinical decisions, incorporating the consequences of true and false predictions and accounting for patient preferences regarding trade-offs between benefits and harms [93]. Unlike AUROC and calibration, clinical utility explicitly acknowledges that the value of a prediction depends on how it will be used to inform actions with different benefit-harm tradeoffs.
Experimental Protocols for Evaluation:
- Decision Curve Analysis (DCA): Quantifies net benefit across a range of clinically reasonable probability thresholds, enabling comparison against "treat all" and "treat none" strategies [98] [100] [11].
- Standardized Net Benefit (SNB): Extends traditional DCA by facilitating fairness assessments through net benefit comparisons across patient subgroups, helping ensure equitable utility across diverse populations [98].
- Threshold Probability Selection: Incorporates clinical context by evaluating net benefit at decision thresholds relevant to specific clinical scenarios (e.g., 10-40% for intervention in acute leukemia complications) [11].
Application in Practice: A 2025 study of prolonged opioid use prediction demonstrated how clinical utility analysis reveals systematic shifts in net benefit across threshold probabilities and patient subgroups, highlighting how models with similar discrimination may differ substantially in their practical value [98]. Similarly, traumatic brain injury prognosis research has incorporated DCA to evaluate net benefit across different threshold probabilities, addressing a critical gap in applying outcome prediction tools in Indian settings [100].
Integrated Evaluation Frameworks and Experimental Comparisons
Multi-Stage Validation Frameworks
Comprehensive model evaluation requires integrated assessment across multiple validation stages. A 2025 study proposed a 3-phase evaluation framework for prediction models [98]:
- Internal Validation: Assess performance on development data with optimism correction via bootstrapping.
- External Validation: Evaluate transportability to completely independent datasets.
- Retraining and Subgroup Analysis: Retrain models on external data and conduct detailed subgroup evaluations across demographic, clinical vulnerability, risk, and comorbidity categories.
This framework explicitly evaluates fairness as performance parity across subgroups and incorporates clinical utility through standardized net benefit analysis, addressing the critical gap between fairness assessment and real-world decision-making [98].
Algorithm Performance Comparisons
The choice between traditional statistical methods and machine learning approaches depends heavily on dataset characteristics and modeling objectives. A 2025 viewpoint synthesizing comparative studies concluded that no single algorithm universally outperforms others across all clinical prediction tasks [93]. Key findings include:
Table 3: Algorithm Comparison Based on Dataset Characteristics
| Dataset Characteristic | Recommended Approach | Evidence |
|---|---|---|
| Small sample size, linear relationships | Statistical logistic regression | More stable with limited data [93] |
| Large sample size, complex interactions | Machine learning (XGBoost, LightGBM) | Superior for capturing nonlinear patterns [11] [93] |
| High-cardinality categorical variables | Categorical Boosting | Built-in encoding without extensive preprocessing [93] |
| Structured tabular data with known predictors | Penalized logistic regression | Comparable performance to complex ML [93] |
| Missing data handling required | LightGBM | Native handling of missing values [11] |
Experimental evidence from acute leukemia complication prediction demonstrated that LightGBM achieved AUROC of 0.824 in derivation and 0.801 in external validation while maintaining excellent calibration, outperforming both traditional regression and other machine learning algorithms [11]. Similarly, multimodal deep learning approaches for clinical deterioration prediction showed that combining structured data with clinical note embeddings achieved the highest area under the precision-recall curve (0.208), though performance was similar to structured-only models [99].
Practical Implementation Guide
Research Reagent Solutions for Model Evaluation
Table 4: Essential Tools for Comprehensive Model Assessment
| Tool Category | Specific Solutions | Function | Implementation Example |
|---|---|---|---|
| Statistical Analysis | R metafor package [95] | Random-effects meta-analysis of AUROC across validations | Quantifying heterogeneity in performance across sites |
| Machine Learning | Scikit-learn calibration suite [94] | Recalibration of predicted probabilities | Isotonic regression for ill-calibrated classifiers |
| Deep Learning | Apache cTAKES [99] | Processing clinical notes for multimodal models | Extracting concept unique identifiers from unstructured text |
| Model Interpretation | SHAP (SHapley Additive exPlanations) [11] | Explaining black-box model predictions | Identifying top predictors in LightGBM leukemia model |
| Clinical Utility | Decision curve analysis [98] [100] [11] | Quantifying net benefit across decision thresholds | Evaluating clinical value over probability thresholds |
Reporting Standards and Guidelines
Adherence to reporting guidelines enhances reproducibility and critical appraisal. The TRIPOD+AI (Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis + Artificial Intelligence) statement provides comprehensive guidance for reporting prediction model studies [100] [11]. Key recommendations include:
- Explicit reporting of calibration performance, not just discrimination [94]
- Clear documentation of hyperparameter tuning strategies and feature selection methods [93]
- Assessment of clinical utility through decision curve analysis rather than relying solely on statistical metrics [98] [93]
- Evaluation of fairness and performance across clinically relevant subgroups [98]
Visualization of Comprehensive Model Evaluation Workflow
The following diagram illustrates the integrated evaluation process encompassing all three critical metrics:
Model Evaluation Workflow
Relationship Between Evaluation Metrics
The interrelationship between the three core metrics can be visualized as follows:
Metric Interrelationships
Robust evaluation of clinical prediction models requires integrated assessment of AUROC, calibration, and clinical utility—three complementary metrics that collectively provide a comprehensive picture of model performance and practical value. The increasing emphasis on replicability and generalizability across validation cohorts demands moving beyond the traditional focus on discrimination alone. Researchers and drug development professionals should adopt multi-stage validation frameworks that incorporate internal and external validation, subgroup analyses for fairness assessment, and clinical utility evaluation through decision curve analysis. By implementing these comprehensive evaluation strategies and adhering to rigorous reporting standards, the field can advance toward more replicable, generalizable, and clinically useful prediction models that ultimately enhance patient care across diverse populations and healthcare settings.
The demonstration of superior performance for any new predictive model is a scientific process, not merely a marketing exercise. Within rigorous research contexts, particularly in fields like drug development and healthcare, this process is framed by a broader thesis on replicability consensus—the principle that model fits must be consistently validated across distinct and independent cohorts [11] [101]. Relying on a single, optimized dataset risks models that are brittle, overfitted, and clinically useless. True validation is demonstrated when a model developed on a derivation cohort maintains its performance on a separate external validation cohort, proving its generalizability and robustness [11]. This article details the experimental protocols and quantitative comparisons necessary to objectively benchmark a new model against traditional alternatives within this critical framework.
Experimental Protocols for Benchmarking
A robust benchmarking study requires a meticulously designed methodology to ensure that performance comparisons are fair, reproducible, and scientifically valid.
Cohort Selection and Data Preprocessing
The foundation of any replicable model is a clearly defined study population. The process begins with the application of strict inclusion and exclusion criteria to a broad data source, such as an electronic health record (EHR) database [101]. The eligible patients are then typically split into a derivation cohort (e.g., 70% of the data) for model training and an external validation cohort (e.g., the remaining 30%) for final testing. This external cohort should ideally come from a different temporal period or geographical location to rigorously test generalizability [11].
Data preprocessing is critical for minimizing bias:
- Handling Missing Data: Variables with a high degree of missingness (e.g., >15%) are often excluded. For remaining variables, sophisticated techniques like Multiple Imputation by Chained Equations (MICE) are used to estimate missing values [11].
- Data Scaling and Filtering: Continuous variables are often Winsorized (e.g., at the 1st and 99th percentiles) to reduce the impact of extreme outliers, and then z-scored. Highly correlated predictors (e.g., |ρ| > 0.80) are filtered to reduce multicollinearity [11].
Model Selection and Training
The benchmarking process should include a diverse set of algorithms to ensure a comprehensive comparison. A typical protocol evaluates both traditional and modern machine learning (ML) approaches. As exemplified in recent literature, this often includes:
- Traditional Statistical Models: Penalised logistic regression (e.g., Elastic-Net).
- Classical Machine Learning: Random Forest, Support Vector Machines.
- Advanced Gradient Boosting: Extreme Gradient Boosting (XGBoost), Light Gradient-Boosting Machine (LightGBM).
- Neural Networks: Multilayer perceptrons (MLPs) [11] [101].
To ensure a fair comparison and avoid overfitting, model training should employ a nested cross-validation framework. An inner loop is used for hyperparameter optimisation (e.g., via Bayesian methods), while an outer loop provides an unbiased estimate of model performance on the derivation data [11].
Evaluation Metrics and Validation Framework
Moving beyond simple accuracy is essential for a meaningful benchmark, especially for imbalanced datasets common in healthcare. The key is to evaluate models based on a suite of metrics that capture different aspects of performance [11] [101]:
- Discrimination: The model's ability to separate classes, measured by the Area Under the Receiver Operating Characteristic Curve (AUROC) and the Area Under the Precision-Recall Curve (AUPRC).
- Calibration: The agreement between predicted probabilities and observed outcomes, assessed via calibration slopes, intercepts, and Hosmer-Lemeshow tests.
- Clinical Utility: The net benefit of using the model for clinical decision-making, evaluated via Decision-Curve Analysis (DCA).
This entire workflow, from cohort definition to model evaluation, can be visualized as a structured pipeline.
Figure 1: Experimental workflow for robust model benchmarking and validation.
Performance Comparison: Quantitative Data
The ultimate test of a new model is its head-to-head performance against established benchmarks in the external validation cohort. The following table summarizes key quantitative results from a representative study that developed a multi-task prediction model, showcasing how such a comparison should be presented [101].
Table 1: Performance comparison of a multi-task Random Forest model against a traditional logistic regression benchmark in external validation [101].
| Prediction Task | Benchmark Model (Logistic Regression AUROC) | New Model (Random Forest AUROC) | Performance Improvement (ΔAUROC) |
|---|---|---|---|
| Acute Kidney Injury (AKI) | 0.781 | 0.906 | +0.125 |
| Disease Severity | 0.742 | 0.856 | +0.114 |
| Need for Renal Replacement Therapy | 0.769 | 0.852 | +0.083 |
| In-Hospital Mortality | 0.754 | 0.832 | +0.078 |
Beyond discrimination, a model's calibration is crucial for clinical use. A well-calibrated model ensures that a predicted risk of 20% corresponds to an observed event rate of 20%. In one study, the LightGBM model showed excellent calibration in validation, with a slope of 0.97 and an intercept of -0.03, indicating almost perfect agreement between predictions and observations [11].
Finally, Decision-Curve Analysis (DCA) quantifies clinical utility. A superior model demonstrates a higher "net benefit" across a range of clinically reasonable probability thresholds. For instance, a model might enable targeted interventions for 14 additional high-risk patients per 100 at a 20% decision threshold compared to traditional "treat-all" or "treat-none" strategies [11].
The Replicability Consensus Validation Framework
Adherence to consensus guidelines is what separates a credible validation study from a simple performance report. The TRIPOD-AI (Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis) statement provides a checklist specifically designed for reporting AI prediction models, ensuring all critical aspects of the study are transparently documented [11]. Furthermore, the PROBAST-AI (Prediction model Risk Of Bias Assessment Tool) is used to assess the risk of bias and applicability of the developed models, guiding researchers in designing methodologically sound studies [11].
A key component of this framework is the use of Explainable AI (XAI) techniques, such as SHapley Additive exPlanations (SHAP), to interpret model outputs. SHAP provides insight into which features are most influential for a given prediction, transforming a "black box" model into a tool that can be understood and trusted by clinicians [11] [101]. For example, in a model predicting complications in acute leukemia, CRP, absolute neutrophil count, and cytogenetic risk were identified as top predictors, with SHAP plots revealing their monotonic effects on risk [11]. This interpretability is a critical step towards building consensus and facilitating adoption.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key resources and methodologies essential for conducting a rigorous benchmarking study.
Table 2: Essential resources and methodologies for model benchmarking and validation.
| Item / Methodology | Function & Application |
|---|---|
| TRIPOD-AI Checklist | A reporting guideline that ensures transparent and complete reporting of prediction model studies, enhancing reproducibility and critical appraisal [11]. |
| SHAP (SHapley Additive exPlanations) | An explainable AI (XAI) method that quantifies the contribution of each feature to an individual prediction, improving model interpretability and trust [11] [101]. |
| Nested Cross-Validation | A resampling procedure used to evaluate model performance and tune hyperparameters without leaking data, providing an almost unbiased performance estimate [11]. |
| Decision-Curve Analysis (DCA) | A method to evaluate the clinical utility of a prediction model by quantifying the net benefit against standard strategies across different probability thresholds [11]. |
| Electronic Health Record (EHR) Databases (e.g., MIMIC-IV, eICU-CRD) | Large, de-identified clinical datasets used as sources for derivation and internal validation cohorts in healthcare prediction research [101]. |
Demonstrating superior performance in a scientifically rigorous manner requires a commitment to the principles of replicability consensus. This involves a meticulous experimental protocol that includes external validation in distinct cohorts, comparison against relevant traditional models using a comprehensive set of metrics, and adherence to established reporting guidelines like TRIPOD-AI. By employing this robust framework and leveraging modern tools for interpretation and clinical utility analysis, researchers can provide compelling, objective evidence of a model's value and take a critical step towards its successful translation into practice.
Multi-cohort validation has emerged as a cornerstone methodology for establishing the robustness, generalizability, and clinical applicability of predictive models in medical research. Unlike single-center validation, which risks model overfitting to local population characteristics, multi-cohort validation tests model performance across diverse geographical, demographic, and clinical settings, providing a more rigorous assessment of real-world utility [102] [103]. This approach is particularly crucial in oncology and other complex disease areas where patient heterogeneity, treatment protocols, and healthcare systems can significantly impact model performance.
The transition toward multi-cohort validation represents a paradigm shift in predictive model development, addressing widespread concerns about reproducibility and translational potential. Studies demonstrate that models evaluated solely on their development data frequently exhibit performance degradation when applied to new populations due to spectrum bias, differing outcome prevalences, and population-specific predictor-outcome relationships [104] [103]. Multi-cohort validation directly addresses these limitations by quantifying performance heterogeneity across settings and identifying contexts where model recalibration or refinement is necessary before clinical implementation.
Recent Exemplars of Multi-Cohort Validation
Cisplatin-Associated Acute Kidney Injury (C-AKI) Prediction Models
A 2025 external validation study compared two C-AKI prediction models originally developed for US populations in a Japanese cohort of 1,684 patients [104]. The research evaluated models by Motwani et al. (2018) and Gupta et al. (2024) for predicting C-AKI (defined as ≥0.3 mg/dL creatinine increase or ≥1.5-fold rise) and severe C-AKI (≥2.0-fold increase or renal replacement therapy). Both models demonstrated similar discriminatory performance for general C-AKI (AUROC: 0.616 vs. 0.613, p=0.84), but the Gupta model showed superior performance for predicting severe C-AKI (AUROC: 0.674 vs. 0.594, p=0.02) [104]. Despite this discriminatory ability, both models exhibited significant miscalibration in the Japanese population, necessitating recalibration to improve accuracy. After recalibration, decision curve analysis confirmed greater net benefit, particularly for the Gupta model in severe C-AKI prediction [104].
Table 1: Performance Metrics of C-AKI Prediction Models in Multi-Cohort Validation
| Model | Target Population | C-AKI Definition | AUROC (General C-AKI) | AUROC (Severe C-AKI) | Calibration Performance |
|---|---|---|---|---|---|
| Motwani et al. (2018) | US (development) | ≥0.3 mg/dL creatinine increase in 14 days | 0.613 | 0.594 | Poor in Japanese cohort, improved after recalibration |
| Gupta et al. (2024) | US (development) | ≥2.0-fold creatinine increase or RRT in 14 days | 0.616 | 0.674 | Poor in Japanese cohort, improved after recalibration |
Machine Learning Model for Postoperative Complications
A 2025 study developed and externally validated a tree-based multitask learning model to simultaneously predict three postoperative complications—acute kidney injury (AKI), postoperative respiratory failure (PRF), and in-hospital mortality—using just 16 preoperative variables [105]. The model was derived from 66,152 cases and validated on two independent cohorts (13,285 and 2,813 cases). The multitask gradient boosting machine (MT-GBM) demonstrated robust performance across all complications in external validation, with AUROCs of 0.789-0.863 for AKI, 0.911-0.925 for PRF, and 0.849-0.913 for mortality [105]. This approach outperformed single-task models and traditional ASA classification, highlighting the advantage of leveraging shared representations across related outcomes. The model maintained strong calibration across institutions with varying case mixes and demonstrated clinical utility across decision thresholds.
Simplified Frailty Assessment Using Machine Learning
A multi-cohort study leveraging data from NHANES, CHARLS, CHNS, and SYSU3 CKD cohorts developed a parsimonious frailty assessment tool using extreme gradient boosting (XGBoost) [13]. Through systematic feature selection from 75 potential variables, researchers identified just eight clinically accessible parameters: age, sex, BMI, pulse pressure, creatinine, hemoglobin, and difficulties with meal preparation and lifting/carrying. The model achieved excellent discrimination in training (AUC 0.963), internal validation (AUC 0.940), and external validation (AUC 0.850) [13]. This simplified approach significantly outperformed traditional frailty indices in predicting clinically relevant endpoints, including CKD progression (AUC 0.916 vs. 0.701, p<0.001), cardiovascular events (AUC 0.789 vs. 0.708, p<0.001), and mortality. The integration of SHAP analysis provided transparent model interpretation, addressing the "black box" limitation common in machine learning approaches.
Table 2: Machine Learning Models with Multi-Cohort Validation
| Model | Medical Application | Algorithm | Cohorts (Sample Size) | Key Performance Metrics |
|---|---|---|---|---|
| Multitask Postoperative Complication Prediction | Preoperative risk assessment | MT-GBM (Multitask Gradient Boosting) | Derivation: 66,152; Validation A: 13,285; Validation B: 2,813 | AKI AUROC: 0.789-0.863; PRF AUROC: 0.911-0.925; Mortality AUROC: 0.849-0.913 |
| Simplified Frailty Assessment | Frailty diagnosis and outcome prediction | XGBoost | NHANES: 3,480; CHARLS: 16,792; CHNS: 6,035; SYSU3 CKD: 2,264 | Training AUC: 0.963; Internal validation AUC: 0.940; External validation AUC: 0.850 |
| Acute Leukemia Complication Prediction | Severe complications after induction chemotherapy | LightGBM | Derivation: 2,009; External validation: 861 | Derivation AUROC: 0.824±0.008; Validation AUROC: 0.801 (0.774-0.827) |
Molecular Signatures with Multi-Cohort Validation
In oncology, multi-cohort validation has been extensively applied to molecular signatures. For hepatocellular carcinoma (HCC), a four-gene signature (HCC4) was developed and validated across 20 independent cohorts comprising over 1,300 patients [106]. The signature demonstrated significant prognostic value for overall survival, recurrence, tumor volume doubling time, and response to transarterial chemoembolization (TACE) and immunotherapy. Similarly, in bladder cancer, a four-gene anoikis-based signature (Ascore) was validated across multiple cohorts, including TCGA-BLCA, IMvigor210, and two institutional cohorts [107]. The Ascore signature achieved an AUC of 0.803 for prognostic prediction using circulating tumor cells and an impressive AUC of 0.913 for predicting immunotherapy response in a neoadjuvant anti-PD-1 cohort, surpassing PD-L1 expression (AUC=0.662) as a biomarker [107].
Experimental Protocols for Multi-Cohort Validation
Standardized Validation Workflow
The experimental workflow for multi-cohort validation typically follows a structured process to ensure methodological rigor and comparability across datasets. The workflow can be visualized as follows:
Cohort Identification and Data Harmonization
The initial phase involves identifying appropriate validation cohorts that represent the target population and clinical settings where the model will be applied. Key considerations include population diversity (demographic, genetic, clinical), data completeness, and outcome definitions [102]. Successful multi-cohort studies employ rigorous data harmonization protocols to ensure variable definitions are consistent across datasets. For example, the C-AKI validation study explicitly reconciled different AKI definitions between the original models (Motwani: ≥0.3 mg/dL increase; Gupta: ≥2.0-fold increase) by evaluating both thresholds in their cohort [104]. Similarly, the frailty assessment study utilized a modified Fried phenotype consistently across NHANES and CHARLS cohorts while acknowledging adaptations necessary for different data collection methodologies [13].
Statistical Evaluation Framework
Comprehensive model evaluation in multi-cohort validation encompasses three key domains: discrimination, calibration, and clinical utility [104] [103].
Discrimination evaluates how well models distinguish between patients who do and do not experience the outcome, typically assessed using the Area Under the Receiver Operating Characteristic Curve (AUROC). The C-AKI study compared AUROCs between models using bootstrap methods to determine statistical significance [104].
Calibration measures the agreement between predicted probabilities and observed outcomes. Poor calibration indicates the need for model recalibration before clinical application. The C-AKI study employed calibration plots and metrics like calibration-in-the-large to quantify miscalibration [104]. Both the Motwani and Gupta models required recalibration despite adequate discrimination, highlighting how performance across these domains can diverge across populations.
Clinical utility assesses the net benefit of using the model for clinical decision-making across various probability thresholds. Decision curve analysis (DCA) compares model-based decisions against default strategies of treating all or no patients [104] [105]. The postoperative complication model demonstrated superior net benefit compared to ASA classification, particularly at lower threshold probabilities relevant for preventive interventions [105].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Multi-Cohort Validation Studies
| Category | Specific Tools/Platforms | Application in Validation Studies |
|---|---|---|
| Statistical Analysis Platforms | R Statistical Software, Python | Data harmonization, model recalibration, performance evaluation [104] |
| Machine Learning Libraries | XGBoost, LightGBM, scikit-learn | Developing and comparing prediction algorithms [11] [13] |
| Model Interpretation Tools | SHAP (SHapley Additive exPlanations) | Explaining model predictions and feature importance [11] [13] |
| Genomic Analysis Tools | RT-PCR platforms, RNA-Seq pipelines | Validating gene signatures across cohorts [106] [107] |
| Data Harmonization Tools | OMOP Common Data Model, REDCap | Standardizing variable definitions across cohorts [102] |
| Validation Reporting Guidelines | TRIPOD+AI checklist | Ensuring comprehensive reporting of validation studies [103] |
Multi-cohort validation represents a critical methodology for establishing the generalizability and clinical applicability of prediction models. Recent exemplars across diverse medical domains demonstrate consistent patterns: even well-performing models typically require population-specific recalibration, simple models with carefully selected variables can achieve robust performance across settings, and machine learning approaches can maintain utility across heterogeneous populations when properly validated [104] [105] [13].
The evolving standard for clinical prediction models emphasizes external validation across multiple cohorts representing diverse populations and clinical settings before implementation. This approach directly addresses the reproducibility crisis in predictive modeling and provides a more realistic assessment of real-world performance. Future directions include developing standardized protocols for cross-cohort data harmonization, establishing benchmarks for acceptable performance heterogeneity across populations, and integrating algorithmic fairness assessments into multi-cohort validation frameworks [103]. As these methodologies mature, multi-cohort validation will play an increasingly central role in translating predictive models from research tools to clinically impactful decision-support systems.
In the era of data-driven healthcare, the ability of a predictive model to perform accurately across diverse populations and clinical settings—a property known as transportability—has emerged as a critical validation requirement. Transportability represents a metric of external validity that assesses the extent to which results from a source population can be generalized to a distinct target population [108]. For researchers, scientists, and drug development professionals, establishing model transportability is no longer optional but essential for regulatory acceptance, health technology assessment (HTA), and equitable clinical implementation.
The need for transportability assessment stems from fundamental challenges in modern healthcare research. High-quality local real-world evidence is not always available to researchers, and conducting additional randomized controlled trials (RCTs) or extensive local observational studies is often unethical or infeasible [108]. Transportability methods enable researchers to fulfill evidence requirements without duplicative research, thereby accelerating data access and potentially improving patient access to therapies [108]. The emerging consensus across recent studies indicates that transportability methods represent a promising approach to address evidence gaps in settings with limited data and infrastructure [109].
This article examines the current landscape of transportability assessment through a systematic analysis of experimental data, methodological protocols, and validation frameworks. By objectively comparing approaches and their performance across diverse populations, we aim to establish a replicability consensus for model validation that can inform future research and clinical implementation strategies.
Current Research on Transportability Assessment
Evidence from Systematic Reviews
Recent systematic reviews reveal that transportability methodology is rapidly evolving but not yet widely adopted in practice. A 2024 targeted literature review identified only six studies that transported an effect estimate of clinical effectiveness or safety to a target real-world population from 458 unique records screened [109]. These studies were all published between 2021-2023, focused primarily on US/Canada contexts, and covered various therapeutic areas, indicating this is an emerging but not yet mature field.
A broader 2025 landscape analysis published in Annals of Epidemiology identified 68 publications describing transportability and generalizability analyses conducted with 83 unique source-target dataset pairs and reporting 99 distinct analyses [110]. This review found that the majority of source and target datasets were collected in the US (75.9% and 71.1%, respectively), highlighting significant geographical limitations in current research. These methods were most often applied to transport RCT findings to observational studies (45.8%) or to another RCT (24.1%) [110].
The same review noted several innovative applications of transportability analysis beyond standard uses, including identifying effect modifiers and calibrating measurements within an RCT [110]. Methodologically, approaches that used weights and individual-level patient data were most common (56.5% and 96.4%, respectively) [110]. Reporting quality varied substantially across studies, indicating a need for more standardized reporting frameworks.
Performance Comparison of Transportability Methods
Table 1: Performance Comparison of Transportability Approaches Across Studies
| Study Focus | Transportability Method | Performance Metrics | Key Findings | Limitations |
|---|---|---|---|---|
| Cognitive Impairment Prediction [111] | Causal vs. Anti-causal Prediction | Calibration differences, AUC | Models predicting with causes of outcome showed better transportability than those predicting with consequences (calibration differences: 0.02-0.15 vs. 0.08-0.32) | Inconsistent AUC trends across external settings |
| Frailty Assessment [13] | Multi-cohort XGBoost Validation | AUC across training and validation cohorts | Robust performance across training (AUC 0.963), internal validation (AUC 0.940), and external validation (AUC 0.850) datasets | Limited to specific clinical domain (frailty) |
| Acute Kidney Injury Prediction [112] | Gradient Boosting with Survival Framework | AUROC, AUPRC | Cross-site performance deterioration observed: temporal validation AUROC 0.76 for any AKI, 0.81 for moderate-to-severe AKI | Performance variability across healthcare systems |
| Acute Liver Failure Classification [113] | Multi-Algorithm Consensus Clustering | Subtype validation across databases | Identified three distinct ALF subtypes with differential treatment responses maintained across five international databases | Requires multiple databases for validation |
The experimental data reveal that model transportability is achievable but consistently challenging. The study on cognitive impairment prediction demonstrated that models using causes of the outcome (causal prediction) were significantly more transportable than those using consequences (anti-causal prediction), particularly when measured by calibration differences [111]. This finding underscores the importance of causal reasoning in developing transportable models.
Similarly, the frailty assessment study showed that a simplified model with only eight readily available clinical parameters could maintain robust performance across multiple international cohorts (NHANES, CHARLS, CHNS, SYSU3 CKD), achieving an AUC of 0.850 in external validation [13]. This suggests that model simplicity and careful feature selection may enhance transportability.
The acute kidney injury prediction study provided crucial insights into cross-site performance, demonstrating that performance deterioration is likely when moving between healthcare systems [112]. The heterogeneity of risk factors across populations was identified as the primary cause, emphasizing that no matter how accurate an AI model is at its source hospital, its adoptability at target hospitals cannot be assumed.
Methodological Frameworks for Transportability Assessment
Core Transportability Methods
Table 2: Methodological Approaches to Transportability Assessment
| Method Category | Key Principles | Implementation Requirements | Strengths | Weaknesses |
|---|---|---|---|---|
| Weighting Methods [109] [108] | Inverse odds of sampling weights to align source and target populations | Identification of effect modifiers; individual-level data from both populations | Intuitive approach; does not require outcome modeling | Sensitive to misspecification of weight model |
| Outcome Regression Methods [109] [108] | Develop predictive model in source population, apply to target population | Rich covariate data from source; covariate data from target | Flexible modeling approach; can incorporate complex relationships | Sensitive to model misspecification; requires correct functional form |
| Doubly-Robust Methods [109] | Combine weighting and outcome regression approaches | Both weighting and outcome models; individual-level data | Double robustness: consistent if either model is correct | More computationally intensive |
| Causal Graph Approaches [111] | Use DAGs to identify stable causal relationships | Domain knowledge for DAG construction; testing of conditional independences | Incorporates causal knowledge for more stable predictions | Requires substantial domain expertise |
Experimental Protocols for Transportability Assessment
Causal Graph Development for Cognitive Impairment Prediction
The protocol for assessing transportability of cognitive impairment prediction models illustrates a sophisticated approach combining causal reasoning with empirical validation [111]. The methodology followed these key steps:
DAG Creation: Researchers reviewed scientific literature to identify causal relationships between variables associated with cognitive impairment. They created an initial DAG, then tested its fit to the Alzheimer's Disease Neuroimaging Initiative (ADNI) dataset using conditional independence testing with the 'dagitty' R package [111].
Structural Equation Modeling (SEM): The team fitted SEMs using three imputed ADNI datasets to quantify the causal relationships specified in their DAG. The 'lavaan' R package was employed with weighted least squares estimates for numeric endogenous variables [111].
Semi-Synthetic Data Generation: Using SEM parameter estimates, researchers generated six semi-synthetic datasets with 10,000 individuals each (training, internal validation, and four external validation sets). External validation sets implemented interventions on variables to reflect different populations [111].
Intervention Scenarios: The team created four external validation scenarios: (1) younger mean age (73⇒35 years); (2) intermediate age reduction (73⇒65 years); (3) lower APOE ε4 prevalence (46.9%⇒5.0%); and (4) altered mechanism for tau-protein generation [111].
Model Evaluation: Multiple algorithms (logistic regression, lasso, random forest, GBM) were applied to predict cognitive state. Transportability was measured by performance differences between internal and external settings using both calibration metrics and AUC [111].
This experimental design enabled rigorous assessment of how different types of predictors (causes vs. consequences) affected transportability under controlled distribution shifts.
Multi-Cohort Validation for Frailty Assessment
The frailty assessment study demonstrated a comprehensive multi-cohort validation approach [13]:
Multi-Cohort Design: Researchers leveraged four independent cohorts (NHANES, CHARLS, CHNS, SYSU3 CKD) for model development and validation, selecting NHANES as the primary training dataset due to its comprehensive variable collection.
Systematic Feature Selection: Through systematic application of five complementary feature selection algorithms (LASSO, VSURF, Boruta, varSelRF, RFE) to 75 potential variables, researchers identified a minimal set of eight clinically available parameters.
Algorithm Comparison: The team evaluated 12 machine learning algorithms across four categories (ensemble learning, neural networks, distance-based models, regression models) to determine the optimal modeling approach.
Multi-Level Validation: The model was validated for predicting not only frailty diagnosis but also clinically relevant outcomes including chronic kidney disease progression, cardiovascular events, and all-cause mortality.
This protocol emphasized both predictive performance and clinical practicality, addressing a common limitation in machine learning healthcare applications.
Diagram 1: Transportability Assessment Workflow. This diagram illustrates the comprehensive process for evaluating model transportability, from problem identification through implementation decision.
Key Considerations for Transportability Assessment
Identifiability Assumptions and Limitations
Transportability methods rely on several key identifiability assumptions that must be met to produce valid results [109]:
Internal Validity of Original Study: The estimated effect must equal the true effect in the source population, requiring conditional exchangeability, consistency, positivity of treatment, no interference, and correct model specification.
Conditional Exchangeability Over Selection: Individuals in study and target populations with the same baseline characteristics must have the same potential outcomes under treatment and no treatment.
Positivity of Selection: There must be a non-zero probability of being in the original study population in every stratum of effect modifiers needed to ensure conditional exchangeability.
In practice, several limitations can impact the comparability of transported data [108]:
- Variability in treatment patterns influenced by differing clinical guidelines, medication availability, and reimbursement statuses
- Population differences across regions shaped by demographic, lifestyle, socioeconomic, and epidemiological factors
- Differences in data quality, completeness, and transparency affecting accuracy and reliability
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Transportability Research
| Tool Category | Specific Solutions | Function in Transportability Assessment | Example Implementations |
|---|---|---|---|
| Causal Inference Frameworks | Directed Acyclic Graphs (DAGs) | Map assumed causal relationships between variables and identify effect modifiers | DAGitty R package [111] |
| Structural Equation Modeling | SEM with Maximum Likelihood Estimation | Quantify causal relationships and generate synthetic data for validation | lavaan R package [111] |
| Weighting Methods | Inverse Odds of Sampling Weights | Reweight source population to match target population characteristics | Multiple R packages (survey, WeightIt) |
| Machine Learning Algorithms | XGBoost, Random Forest, LASSO | Develop predictive models with complex interactions while managing overfitting | XGBoost, glmnet, randomForest R packages [13] |
| Interpretability Tools | SHAP (Shapley Additive Explanations) | Provide transparent insights into model predictions and feature importance | SHAP Python library [13] [112] |
| Performance Assessment | Calibration Plots, AUC, Decision Curve Analysis | Evaluate model discrimination, calibration, and clinical utility | Various R/Python validation packages |
Diagram 2: Causal and Methodological Relationships in Transportability. This diagram illustrates the key factors influencing transportability assessment and their relationships.
The experimental evidence and methodological review presented in this analysis demonstrate that model transportability across demographics and healthcare systems is achievable but requires rigorous assessment frameworks. The current research consensus indicates that causal approaches to prediction, multi-cohort validation designs, and transparent reporting are essential components of robust transportability assessment.
The findings reveal several critical priorities for future research. First, there is a need for greater methodological standardization and transparency in reporting transportability analyses [109] [110]. Second, researchers should prioritize the identification and measurement of effect modifiers that differ between source and target populations [109]. Third, the field would benefit from increased attention to calibration performance rather than relying solely on discrimination metrics like AUC [111].
For drug development professionals and researchers, the implications are clear: transportability assessment cannot be an afterthought but must be integrated throughout model development and validation. As regulatory and HTA bodies increasingly recognize the value of real-world evidence [109], establishing robust transportability frameworks will be essential for justifying the use of models across diverse populations and healthcare systems.
The replicability consensus emerging from current research emphasizes that transportability is not merely a statistical challenge but a multidisciplinary endeavor requiring domain expertise, causal reasoning, and pragmatic validation across multiple cohorts. By adopting the methodologies and frameworks presented here, researchers can enhance the transportability of their models, ultimately contributing to more equitable and effective healthcare applications.
The Role of SHAP and Interpretability in Building Trust for Clinical Adoption
The integration of Artificial Intelligence (AI) and Machine Learning (ML) into clinical decision-making and drug development represents a transformative shift in healthcare. However, the "black-box" nature of many high-performing algorithms has been identified as a critical barrier to their widespread clinical adoption [114]. Explainable AI (XAI) aims to bridge this gap by making the decision-making processes of ML models transparent, understandable, and trustworthy for clinicians, researchers, and regulators [115]. Within the XAI toolkit, SHapley Additive exPlanations (SHAP) has emerged as a leading method for explaining model predictions [116]. This guide provides a comparative analysis of SHAP's role in building trust for clinical AI, focusing on its performance against other explanation paradigms within a framework that prioritizes replicability and validation across diverse patient cohorts.
Theoretical Foundations of SHAP
SHAP is a unified measure of feature importance rooted in cooperative game theory, specifically leveraging Shapley values [116]. It provides a mathematically fair distribution of the "payout" (i.e., a model's prediction) among the "players" (i.e., the input features) [116].
Core Principles and Calculation
The fundamental properties that make Shapley values suitable for model explanation are:
- Efficiency: The sum of the SHAP values for all features equals the model's output, ensuring a complete explanation.
- Symmetry: If two features contribute equally to all possible combinations of features, they receive the same Shapley value.
- Dummy (Null Player): A feature that does not change the predicted value, regardless of which other features it is combined with, receives a Shapley value of zero.
- Additivity: The Shapley value for a combination of games is the sum of the Shapley values for the individual games.
The SHAP value for a feature (i) is calculated using the following formula, which considers the marginal contribution of the feature across all possible subsets of features (S):
[\phii = \sum{S \subseteq N \setminus {i}} \frac{|S|! (|N| - |S| - 1)!}{|N|!} (V(S \cup {i}) - V(S))]
Where (N) is the set of all features, and (V(S)) is the prediction for a subset of features (S) [116].
From Game Theory to Clinical Predictions
In an ML context, the "game" is the model's prediction for a single instance, and the "players" are the instance's feature values. SHAP quantifies how much each feature value contributes to pushing the final prediction away from the base value (the average model output over the training dataset) [115]. This allows clinicians to see not just which factors were important, but the direction and magnitude of their influence on a case-by-case basis (local interpretability) or across the entire model (global interpretability) [116].
Comparative Analysis of Explanation Methods in Clinical Settings
While several XAI methods exist, their utility varies significantly in clinical contexts. The table below compares SHAP against other prominent techniques.
Table 1: Comparison of Explainable AI (XAI) Methods in Clinical Applications
| Method | Type | Scope | Clinical Interpretability | Key Strengths | Key Limitations in Clinical Settings |
|---|---|---|---|---|---|
| SHAP (SHapley Additive exPlanations) [116] [115] | Feature-based, Model-agnostic | Local & Global | High (Provides quantitative feature impact) | Unified framework, solid theoretical foundation, local & global explanations | Computationally expensive; explanations may lack clinical context without augmentation [114] |
| LIME (Local Interpretable Model-agnostic Explanations) [114] | Feature-based, Model-agnostic | Local | Moderate | Creates locally faithful explanations | Instability in explanations; perturbations may create unrealistic clinical data [117] |
| Grad-CAM (Gradient-weighted Class Activation Mapping) [117] | Model-specific (Neural Networks) | Local | Moderate to High for imaging | Provides spatial explanations for image-based models; fast computation | Limited to specific model architectures; less suitable for non-image tabular data [117] |
| Saliency Maps [117] | Model-specific (Neural Networks) | Local | Low to Moderate for imaging | Simple visualization of influential input regions | Can be unstable and provide overly broad, uninformative explanations [117] |
| Inherently Interpretable Models (e.g., Logistic Regression, Decision Trees) | Self-explaining | Local & Global | Variable | Model structure itself is transparent | Often trade-off exists between model complexity/predictive performance and interpretability [116] |
Experimental Evidence: SHAP vs. Clinician-Friendly Explanations
A critical study directly compared how different explanation formats influence clinicians' acceptance, trust, and decision-making [114]. In a controlled experiment, surgeons and physicians were presented with AI recommendations for perioperative blood transfusion in three formats:
- Results Only (RO): The AI's prediction without any explanation.
- Results with SHAP (RS): The AI's prediction accompanied by a standard SHAP plot.
- Results with SHAP and Clinical Explanation (RSC): The AI's prediction with a SHAP plot and a supplementary explanation written in clinical terms.
The study quantitatively measured the Weight of Advice (WOA), which reflects the degree to which clinicians adjusted their decisions based on the AI advice. The results, summarized below, provide a powerful comparison of real-world effectiveness.
Table 2: Quantitative Impact of Explanation Type on Clinical Acceptance and Trust [114]
| Metric | Results Only (RO) | Results with SHAP (RS) | Results with SHAP + Clinical Explanation (RSC) | Statistical Significance (p-value) |
|---|---|---|---|---|
| Weight of Advice (WOA) - Acceptance | 0.50 (SD=0.35) | 0.61 (SD=0.33) | 0.73 (SD=0.26) | < 0.001 |
| Trust in AI Explanation (Scale Score) | 25.75 (SD=4.50) | 28.89 (SD=3.72) | 30.98 (SD=3.55) | < 0.001 |
| Explanation Satisfaction (Scale Score) | 18.63 (SD=7.20) | 26.97 (SD=5.69) | 31.89 (SD=5.14) | < 0.001 |
| System Usability Scale (SUS) Score | 60.32 (SD=15.76) | 68.53 (SD=14.68) | 72.74 (SD=11.71) | < 0.001 |
Key Insight: While SHAP alone (RS) significantly improved all metrics over providing no explanation (RO), the combination of SHAP and a clinical explanation (RSC) yielded the highest levels of acceptance, trust, and satisfaction [114]. This demonstrates that SHAP is a powerful component, but not a standalone solution, for building clinical trust. Its value is maximized when it is integrated with and translated into domain-specific clinical knowledge.
Experimental Protocols for Evaluating Explainable AI
To ensure replicability and robust validation of XAI methods in clinical research, standardized evaluation protocols are essential. Below are detailed methodologies for key experiments cited in this guide.
Protocol: Comparing Explanation Formats for Clinical Decision-Making
This protocol is based on the experimental design used to generate the data in Table 2 [114].
- Objective: To evaluate the impact of different AI explanation formats on clinicians' acceptance, trust, and satisfaction.
- Study Design: Randomized, counterbalanced study using clinical vignettes.
- Participants: 63 surgeons and physicians with experience in prescribing blood products prior to surgery.
- Intervention: Participants made decisions on six clinical vignettes before and after receiving AI advice. They were randomly assigned to one of three explanation method groups: RO, RS, or RSC.
- Primary Outcome Measure: Weight of Advice (WOA), calculated as
(Post-advice estimate - Pre-advice estimate) / (AI advice - Pre-advice estimate). This measures the degree of advice adoption. - Secondary Outcome Measures: Validated questionnaire scores for Trust in AI Explanation, Explanation Satisfaction, and the System Usability Scale (SUS).
- Analysis: Friedman test with Conover post-hoc analysis for comparing outcomes across the three groups. Correlation analysis between acceptance, trust, satisfaction, and usability scores.
Protocol: Developing and Validating an Interpretable ML Model with SHAP
This protocol summarizes a common workflow for creating interpretable clinical prediction models, as seen in multiple studies [118] [119] [120].
- Objective: To develop a robust, interpretable ML model for a clinical prediction task (e.g., intrinsic capacity decline, cardiovascular risk, cancer treatment recommendation).
- Data Sourcing: Use data from a large-scale database (e.g., SEER database for oncology [120] [121]) for model development. Secure an external validation cohort from a geographically or demographically distinct population [118] [121].
- Data Preprocessing: Handle missing data using techniques like K-Nearest Neighbors (KNN) imputation [119]. Split the development data into training and test sets (e.g., 70:30).
- Model Development and Selection: Train multiple ML algorithms (e.g., Support Vector Machine, Random Forest, XGBoost, LightGBM). Evaluate models based on discrimination (Area Under the ROC Curve - AUC), calibration (Brier score), and clinical utility (Decision Curve Analysis). Select the best-performing model.
- Model Interpretation with SHAP:
- Calculate SHAP values for the entire validation set.
- Generate summary plots (beeswarm or bar plots) to visualize global feature importance.
- Generate local explanation plots (force or waterfall plots) to explain individual predictions.
- Correlate SHAP-derived insights with established clinical knowledge to validate model logic.
- Validation: The final model's performance and interpretability must be confirmed on the held-out external validation cohort to ensure generalizability and replicability.
Visualizing the Workflow for Trustworthy Clinical AI
The following diagram illustrates the integrated workflow for developing and deploying a trustworthy clinical AI model, from data preparation to clinical decision support, emphasizing the critical role of SHAP and clinical explanation.
Diagram Title: Pathway to Clinically Trustworthy AI
The Scientist's Toolkit: Essential Reagents for Interpretable ML Research
The following table details key software and methodological "reagents" required for implementing SHAP and building interpretable ML models in clinical and translational science.
Table 3: Essential Research Reagents for Interpretable ML with SHAP
| Tool / Reagent | Type | Primary Function | Relevance to Research |
|---|---|---|---|
| SHAP Python Library [116] | Software Library | Computes Shapley values for any ML model. | Core reagent for generating local and global explanations; model-agnostic. |
| TreeSHAP [116] | Algorithm Variant | Efficiently computes approximate SHAP values for tree-based models (e.g., Random Forest, XGBoost). | Drastically reduces computation time for complex models, making SHAP feasible on large clinical datasets. |
| LIME (Local Interpretable Model-agnostic Explanations) [114] | Software Library | Creates local surrogate models to explain individual predictions. | Useful as a comparative method to benchmark SHAP's explanations. |
| Streamlit [119] | Web Application Framework | Creates interactive web applications for displaying model predictions and explanations. | Enables building user-friendly CDSS prototypes for clinician testing and feedback. |
| scikit-survival / RandomForestSRC [121] | Software Library | Implements ML models for survival analysis (e.g., Random Survival Forest). | Essential for developing prognostic models in oncology and chronic disease. |
| External Validation Cohort [118] [120] [121] | Methodological Component | A dataset from a different population used to test model generalizability. | Critical for assessing replicability and the true performance of the model and its explanations beyond the development data. |
The journey toward widespread clinical adoption of AI hinges on trust, which is built through transparency and interpretability. SHAP has established itself as a cornerstone technology in this endeavor, providing a mathematically robust and flexible framework for explaining complex model predictions. The experimental evidence clearly shows that while SHAP significantly enhances clinician acceptance and trust over opaque models, its effectiveness is maximized when its outputs are translated into clinician-friendly explanations. For researchers and drug development professionals, the path forward involves a commitment to a rigorous workflow that integrates robust model development, thorough validation using external cohorts, SHAP-based interpretation, and finally, the crucial step of contextualizing explanations within the clinical domain. This integrated approach is the key to developing replicable, validated, and ultimately, trustworthy AI tools for medicine.
Conclusion
The path to clinically impactful predictive models in biomedicine requires a fundamental shift from single-study successes to replicable, consensus-based approaches. By embracing multi-cohort validation frameworks, rigorous methodological standards, and transparent reporting, researchers can build models that genuinely generalize across diverse populations and clinical settings. Future directions must prioritize prospective implementation studies, the development of standardized reporting guidelines for model replicability, and greater integration of biological plausibility into computational frameworks. Ultimately, this replicability-first approach will accelerate the translation of predictive models into tools that reliably improve patient care and drug development outcomes.
References
- 1. Reproducibility and Replicability in Science: Report Highlights [https://hdsr.mitpress.mit.edu/pub/nas-report-highlights]
- 2. Understanding Reproducibility and Replicability - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK547546/]
- 3. A Quick Guide to Reproducibility and Replicability in ... [https://researcher.life/blog/article/a-quick-guide-to-reproducibility-and-replicability-in-research/]
- 4. Reproducibility of real-world evidence studies using ... [https://www.nature.com/articles/s41467-022-32310-3]
- 5. Toward a statistical validation of brain signatures as robust ... [https://pubmed.ncbi.nlm.nih.gov/36939069/]
- 6. Where next for the reproducibility agenda in computational ... [https://bmcsystbiol.biomedcentral.com/articles/10.1186/s12918-016-0288-x]
- 7. Toward a statistical validation of brain signatures as robust ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10171525/]
- 8. List of Large-Scale Replication Projects [https://forrt.org/replication-hub/large-scale-replication-projects/]
- 9. Overfitting in Machine Learning Explained [https://aws.amazon.com/what-is/overfitting/]
- 10. 4 – The Overfitting Iceberg [https://blog.ml.cmu.edu/2020/08/31/4-overfitting/]
- 11. Construction and validation of a risk prediction model for ... [https://www.nature.com/articles/s41598-025-24478-7]
- 12. Overfitting in Machine Learning Explained [https://encord.com/blog/overfitting-in-machine-learning/]
- 13. Development and multi-cohort validation of a machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357463/]
- 14. AI Model Validation: Best Practices for Accuracy & Reliability [https://galileo.ai/blog/best-practices-for-ai-model-validation-in-machine-learning]
- 15. Model Validation Techniques | TDS Archive [https://medium.com/data-science/model-validation-techniques-explained-a-visual-guide-with-code-examples-eb13bbdc8f88]
- 16. Assessing the performance of prediction models: a framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3575184/]
- 17. Construction and validation of a prediction model for 90 ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1627789/full]
- 18. Compare models [https://docs.datarobot.com/en/docs/workbench/wb-experiment/manage-experiments/wb-model-compare.html]
- 19. Model dependence in multi-model climate ensembles ... [https://esd.copernicus.org/articles/10/91/2019/]
- 20. How Robust Is a Multi-Model Ensemble Mean of ... [https://www.mdpi.com/2073-4441/14/18/2852]
- 21. Optimizing the multi-model ensemble of CMIP6 GCMs for ... [https://www.nature.com/articles/s41598-025-96446-0]
- 22. A multi-center study for colorectal cancer early detection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574013/]
- 23. Articles Multicenter validation of a machine learning model ... [https://www.sciencedirect.com/science/article/pii/S2589537025000446]
- 24. Development of a Multi-Model Ensemble Tool for Early ... [https://sciety-discovery.elifesciences.org/articles/by?article_doi=10.1101/2025.11.06.25339737]
- 25. Reinforcement learning-based multi-model ensemble for ... [https://www.frontiersin.org/journals/marine-science/articles/10.3389/fmars.2025.1534622/full]
- 26. Explicating Exact versus Conceptual Replication | Erkenntnis [https://link.springer.com/article/10.1007/s10670-021-00464-z]
- 27. The function of conducting a direct replication may be ... [https://www.sciencedirect.com/science/article/pii/S0895435625001180]
- 28. An open source statistical web application for validation ... [https://www.nature.com/articles/s41598-025-99720-3]
- 29. In Silico Research Is Rewriting the Rules of Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12070237/]
- 30. How Much Should We Spend on Scientific Replication? [https://ifp.org/how-much-should-we-spend-on-replication/]
- 31. In-Silico Clinical Trials Market Set to Reach USD 6.39 ... [https://www.prnewswire.com/news-releases/in-silico-clinical-trials-market-set-to-reach-usd-6-39-billion-by-2033-as-pharma-and-medtech-accelerate-digital-first-validation-ai-modeling--virtual-patient-simulations-302627526.html]
- 32. Charts can be social artifacts that communicate more than ... [https://news.mit.edu/2025/charts-can-be-social-artifacts-communicate-more-than-data-1022]
- 33. Lasso regression model, random forest model, Boruta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12129492/]
- 34. LASSO regression and Boruta algorithm to explore the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12065745/]
- 35. Comparative analysis of feature selection techniques for ... [https://www.nature.com/articles/s41598-024-69209-6]
- 36. Is this the Best Feature Selection Algorithm “BorutaShap”? [https://medium.com/analytics-vidhya/is-this-the-best-feature-selection-algorithm-borutashap-8bc238aa1677]
- 37. Diabetes Prediction Using Feature Selection Algorithms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563305/]
- 38. A comparison of feature selection methodologies and learning ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05282-4]
- 39. Harmonization and integration of data from prospective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109133/]
- 40. A methodology for cohort harmonisation in multicentre ... [https://www.sciencedirect.com/science/article/pii/S2352914821002343]
- 41. Evaluating the harmonisation potential of diverse cohort ... [https://link.springer.com/article/10.1007/s10654-023-00997-3]
- 42. Clinically focused multi-cohort benchmarking as a tool for ... [https://www.nature.com/articles/s41598-022-16514-7]
- 43. XGBoost vs LightGBM: How Are They Different [https://neptune.ai/blog/xgboost-vs-lightgbm]
- 44. Optimizing LightGBM and XGBoost Algorithms for ... [https://link.springer.com/article/10.1007/s13369-025-10217-7]
- 45. Methodological and reporting quality of machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12034563/]
- 46. Advancing LightGBM with data augmentation for predicting ... [https://www.nature.com/articles/s41529-025-00673-9]
- 47. Generating Realistic Synthetic Patient Cohorts: Enforcing ... [https://www.mdpi.com/1999-4893/18/8/475]
- 48. Imbalanced Data | Peter Lorenz - GitHub Pages [https://lorenz-peter.github.io/blog/2025/imbalanced-data/]
- 49. Should You Use Imbalanced-Learn in 2025? [https://www.blog.trainindata.com/should-you-use-imbalanced-learn-in-2025/]
- 50. 解决类别不平衡问题的方法综述原创 [https://blog.csdn.net/vivian_ll/article/details/105201120]
- 51. 技术分析:计算机视觉与机器学习等领域不平衡数据处理综述 [https://m.ofweek.com/ai/2021-04/ART-201716-11000-30492326.html]
- 52. Secrets of time series modeling: Nested cross-validation [https://www.datasciencecentral.com/secrets-of-time-series-modeling-nested-cross-validation/]
- 53. Practical Considerations and Applied Examples of Cross ... [https://ai.jmir.org/2023/1/e49023]
- 54. Nested versus non-nested cross-validation [https://scikit-learn.org/stable/auto_examples/model_selection/plot_nested_cross_validation_iris.html]
- 55. Nested cross-validation when selecting classifiers is ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417421006540]
- 56. Consensus features nested cross-validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7776094/]
- 57. Machine learning models to accelerate the design of ... [https://www.nature.com/articles/s41467-022-35343-w]
- 58. Data Ingestion Architecture: Complete Guide [https://rivery.io/data-learning-center/data-ingestion-architecture-guide/]
- 59. Data Validation: Processes, Benefits & Types (2025) [https://atlan.com/what-is-data-validation/]
- 60. A moving target in AI-assisted decision-making: dataset ... [https://link.springer.com/article/10.1007/s10676-025-09829-2]
- 61. Strategies for detecting and mitigating dataset shift in ... [https://pubmed.ncbi.nlm.nih.gov/40876698/]
- 62. Strategies for detecting and mitigating dataset shift in ... [https://www.sciencedirect.com/science/article/abs/pii/S1532046425001315]
- 63. Development and validation of a machine learning-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12410600/]
- 64. Automatic dataset shift identification to support safe ... [https://arxiv.org/abs/2411.07940]
- 65. Machine learning models for predicting short-term ... [https://www.nature.com/articles/s41598-025-23037-4]
- 66. Small sample sizes: A big data problem in high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8008424/]
- 67. Small Sample Size Solutions [https://library.oapen.org/handle/20.500.12657/22385]
- 68. Cross‐cohort replicable resting‐state functional connectivity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11083889/]
- 69. A Beginner's Guide: Study Design in Biomedical Research [https://guides.library.uwindsor.ca/c.php?g=744598&p=5386743]
- 70. Best practices for data management and sharing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11380994/]
- 71. A-calibration: assessment of prediction models for survival ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542389/]
- 72. Population-specific calibration and validation of an open- ... [https://www.nature.com/articles/s41598-025-20148-w]
- 73. Development and Spatial External Validation of a ... [https://www.jmir.org/2025/1/e71257]
- 74. Rethinking calibration as a statistical estimation problem to ... [https://pubmed.ncbi.nlm.nih.gov/40903110/]
- 75. Machine learning generalizability across healthcare settings [https://www.nature.com/articles/s41746-022-00614-9]
- 76. Hyperparameter optimization [https://en.wikipedia.org/wiki/Hyperparameter_optimization]
- 77. “Hyperparameter Tuning” In Data Science | by Rajat Sharma [https://medium.com/pythoneers/hyperparameter-tuning-in-data-science-ad1a03d830b9]
- 78. Hyperparameter optimization of machine learning models ... [https://www.sciencedirect.com/science/article/pii/S2666827025000441]
- 79. Generalizability of Machine Learning Models: Quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9885377/]
- 80. The openOCHEM consensus model is the best-performing ... [https://www.sciencedirect.com/science/article/pii/S2472555224000066]
- 81. Comparing variable and feature selection strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12316309/]
- 82. Development and external validation of prediction ... [https://www.nature.com/articles/s41467-025-57990-5]
- 83. in Public Health Research Reproducibility [https://www.numberanalytics.com/blog/reproducibility-in-public-health-research]
- 84. of R Computational Supplements on OSF Reproducibility Code [https://arxiv.org/html/2505.21590v1]
- 85. · GitHub Code Reproducibility Good Practices [https://gist.github.com/sergiouribe/d01b4a11c44905f2232ce93c539bdd7a]
- 86. Supporting open science practices: Why sharing your code ... [https://www.springernature.com/gp/researchers/the-researchers-source/open-science-blogpost/open-science-sharing-code/27793060]
- 87. Best practices in writing and sharing code - Code Sharing [https://libguides.chapman.edu/code_sharing/best_practices]
- 88. Best Practices for Data Sharing and Archiving [https://library.weill.cornell.edu/research-support/research-data-management-retention-and-sharing/best-practices-data-sharing-and]
- 89. Code Sharing in Healthcare Research: A Practical Guide ... [https://arxiv.org/abs/2510.19279]
- 90. Development and Internal-External Validation Models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12267828/]
- 91. From Logistic Regression to Foundation Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611635/]
- 92. Development and external validation of a radiomics model for ... [https://insightsimaging.springeropen.com/articles/10.1186/s13244-022-01361-x]
- 93. Beyond Comparing Machine Learning and Logistic ... [https://www.jmir.org/2025/1/e77721]
- 94. Calibrating variant-scoring methods for clinical decision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8023678/]
- 95. Instability of the AUROC of Clinical Prediction Models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11806515/]
- 96. Evaluating Risk Prediction with ROC Curves [https://www.publichealth.columbia.edu/research/population-health-methods/evaluating-risk-prediction-roc-curves]
- 97. Methods of determining optimal cut-point of diagnostic ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02198-2]
- 98. Evaluating the impact of data biases on algorithmic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483547/]
- 99. Comparison of Multimodal Deep Learning Approaches for ... [https://www.jmir.org/2025/1/e75340]
- 100. Development, validation and clinical utility of prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12496054/]
- 101. Development and validation of an interpretable multi-task ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12396465/]
- 102. Methods for Stratification and Validation Cohorts [https://pmc.ncbi.nlm.nih.gov/articles/PMC9144352/]
- 103. Clinical prediction models using machine learning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506039/]
- 104. External validation and comparison of clinical prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482746/]
- 105. Multicenter validation of a scalable, interpretable, multitask ... [https://www.nature.com/articles/s41746-025-01949-9]
- 106. Multi-cohort validation study of a four-gene signature for ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482523011599]
- 107. Multi-cohort validation of Ascore: an anoikis-based prognostic ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-01945-9]
- 108. Can Data Transportability Connect Patients to Therapies ... [https://www.costellomedical.com/what-we-do/evidence-development/real-world-evidence/data-transportability-in-real-world-evidence/]
- 109. Use of transportability methods for real-world evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11542082/]
- 110. Systematic review of applied transportability and ... [https://www.sciencedirect.com/science/article/pii/S1047279725000420]
- 111. Assessing the transportability of clinical prediction models for ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-02003-6]
- 112. Cross-site transportability of an explainable artificial ... [https://www.nature.com/articles/s41467-020-19551-w]
- 113. Multi-algorithm consensus classification identifies three ... [https://www.sciencedirect.com/science/article/pii/S2090123225004266]
- 114. Comparison of SHAP and clinician friendly explanations ... [https://www.nature.com/articles/s41746-025-01958-8]
- 115. AI in Drug Discovery: The Role of SHAP in Pharmacology [https://www.reprocell.com/blog/biopta/ai-in-drug-discovery-the-role-of-shap-in-pharmacology]
- 116. Practical guide to SHAP analysis: Explaining supervised ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11513550/]
- 117. A Comparison of SHAP and Grad-CAM in Human Activity ... [https://arxiv.org/html/2412.16003v2]
- 118. Development and validation of an interpretable machine ... [https://www.sciencedirect.com/science/article/pii/S0531556525002529]
- 119. Comparative analysis of explainable machine learning ... [https://www.sciencedirect.com/science/article/pii/S2666521225000900]
- 120. Development and external validation of interpretable ... [https://pubmed.ncbi.nlm.nih.gov/41124941/]
- 121. Interpretable machine learning models to predict survival in ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1665383/full]