Geographic Mobility in Pediatric and Geriatric Populations: Implications for Clinical Research and Drug Development
This article examines the distinct drivers of high geographic mobility in pediatric and older adult populations and their critical implications for biomedical research.
Geographic Mobility in Pediatric and Geriatric Populations: Implications for Clinical Research and Drug Development
Abstract
This article examines the distinct drivers of high geographic mobility in pediatric and older adult populations and their critical implications for biomedical research. For older adults, mobility is primarily driven by health declines, such as cardiovascular events, and the need for informal caregiving, often resulting in relocations closer to adult children. For children, mobility is often linked to parental life course events. These patterns present significant methodological challenges for longitudinal studies, clinical trial retention, and pharmacovigilance systems, which can be addressed through targeted recruitment, dynamic follow-up protocols, and digital health technologies. A comparative analysis of mobility triggers and their impact on healthcare engagement reveals the necessity for tailored, life-course-informed research strategies to ensure representative sampling and data integrity in drug development.
Understanding the Core Drivers of Mobility in Vulnerable Populations
Late-life mobility, a critical area of gerontological research, is predominantly driven by health triggers and the ensuing need for care. This whitepaper synthesizes quantitative evidence from longitudinal cohort and population register studies to delineate the specific health events that precipitate residential moves among older adults. Framed within the broader context of life-course mobility, where both young adults and older individuals constitute high-mover populations, this analysis details the experimental methodologies used to establish causality and pattern. The findings underscore that health-driven mobility is a strategic adaptation to disability, fundamentally shaping intergenerational living arrangements and care networks.
Population aging necessitates a deeper understanding of the mechanisms behind late-life mobility. While young adults move primarily for education, employment, and family formation [1], older adults experience a distinct mobility resurgence driven by different triggers. The life course exhibits a pronounced peak in residential mobility in early adulthood (ages 20-30), a period of stabilization, and then a second, significant phase of mobility in later life linked to health transitions [2]. This paper positions late-life mobility not as a random event, but as a strategic adaptation to changing capacities and care needs, a process that can be rigorously quantified and modeled.
Understanding these patterns is vital for multiple stakeholders. For researchers, it clarifies confounding factors in longitudinal studies where residential mobility can introduce selection bias or exposure misclassification [3] [4]. For drug development and health services professionals, it highlights critical periods of intervention and the need for therapies that can delay disability and thus alter the trajectory of care needs and subsequent relocation.
Quantitative Evidence: Health Events as Predictors of Residential Moves
Robust, longitudinal data from multiple large-scale studies consistently demonstrates a strong association between specific health triggers and increased mobility in older populations. The following tables summarize key quantitative findings.
Table 1: Health Triggers and Associated Mobility Outcomes in Older Adults
| Health Trigger | Population Studied | Mobility Outcome | Measured Effect | Citation |
|---|---|---|---|---|
| Severe Health Problems (Parents ≥80 years) | Swedish Population Registers | Parent moves closer to child | Increased likelihood | [1] |
| Severe Health Problems (Parents ≥80 years) | Swedish Population Registers | Parent moves to institution | Increased likelihood | [1] |
| First Cardiovascular Event (Stroke, Heart Attack, CHF) | U.S. Health and Retirement Study (HRS) | Child moves closer to parent | 1.55x increased probability (Relative Risk Ratio) | [5] |
| First Cardiovascular Event (Stroke, Heart Attack, CHF) | U.S. Health and Retirement Study (HRS) | Parent and child move in together | 1.61x increased probability (Relative Risk Ratio) | [5] |
| Self-Rated Poor Health | Atherosclerosis Risk in Communities (ARIC) Cohort | Short-distance move | Significant positive association | [3] [4] |
| Physical Limitations | Atherosclerosis Risk in Communities (ARIC) Cohort | Short-distance move | Significant positive association | [3] [4] |
Table 2: Moderating Factors in Health-Triggered Mobility
| Moderating Factor | Effect on Mobility Probability | Context |
|---|---|---|
| Child's Gender | Older mothers are more likely to move closer to a daughter than a son [1]. | Intergenerational moves |
| Parent's Marital Status | The effect of a cardiovascular event is stronger for spouseless older parents [5]. | Moves following a health crisis |
| Location of Other Children | Children are more likely to move closer to a parent if a sibling already lives nearby [1]. | Moves following a health crisis |
| Move Distance | Poor health and physical limitations are more strongly associated with short-distance moves than long-distance moves [3] [4]. | General late-life mobility |
Methodological Protocols: Establishing Causal Inference
Establishing that health triggers cause mobility, rather than merely correlate with it, requires sophisticated longitudinal study designs and statistical models. The following protocols are derived from the cited seminal research.
Protocol: Analyzing Intergenerational Moves in Response to Health Shocks
This protocol is based on the study of cardiovascular events using the Health and Retirement Study (HRS) [5].
- Objective: To determine if a discrete, severe health event causes changes in intergenerational residential proximity.
- Data Source: Longitudinal, nationally representative surveys (e.g., HRS) with biennial interviews. Must include modules on health history, residential addresses of respondents and their children, and family structure.
- Sample Selection:
- Restrict baseline sample to respondents living in the community, above a certain age (e.g., 55+), without a history of the specific health condition under study (e.g., CVD).
- Include only respondents with at least one non-coresident child at baseline to ensure the possibility of a proximity-enhancing move.
- Key Variables:
- Independent Variable: Incident health event (e.g., first-ever stroke, heart attack, or congestive heart failure), confirmed in a follow-up wave.
- Dependent Variable: Change in residential proximity between baseline and follow-up, categorized as: (a) child moves closer to parent, (b) parent and child move in together, (c) no change, (d) move further apart.
- Covariates: Age, gender, race/ethnicity, education, marital status, income, baseline functional limitations, and number of children.
- Statistical Analysis: Multinomial logistic regression to model the likelihood of each proximity change category as a function of the health event, adjusting for covariates. Results are expressed as relative risk ratios.
Protocol: Predicting Movers vs. Non-Movers in an Aging Cohort
This protocol is based on analyses of the Atherosclerosis Risk in Communities (ARIC) cohort [3] [4].
- Objective: To characterize movers and identify predictors of short- and long-distance moves in a middle-aged and early-retirement cohort.
- Data Source: Established longitudinal cohort (e.g., ARIC) with geocoded residential addresses at multiple visits and extensive covariate data.
- Move Identification:
- Geocode all participant addresses at sequential study visits.
- Calculate pairwise distances between consecutive addresses.
- Classify participants as: Non-movers, Short-distance movers (within county), or Long-distance movers (outside county).
- Predictor Variables: Collect data from six categories: sociodemographic characteristics, health and psychosocial factors, incident life "triggers" (e.g., retirement, widowhood), characteristics of the physical home, and neighborhood-level characteristics.
- Statistical Analysis: Use best-subset selection algorithms to identify the most important predictors of moving. Crucially, include interaction terms between predictors (e.g., age and health status) to improve model fit and uncover substantive relationships. Compare the characteristics of short-distance and long-distance movers to non-movers.
The logical workflow for investigating health-triggered mobility, from study design to analysis, is summarized below.
The Scientist's Toolkit: Research Reagents & Essential Materials
For researchers investigating late-life mobility, the following "research reagents" are critical resources.
Table 3: Essential Resources for Research on Late-Life Mobility
| Research Resource | Type | Function & Application | Example |
|---|---|---|---|
| Linked Population & Health Registers | Data Source | Provides complete, longitudinal data on an entire population for residential moves, health diagnoses, and family linkages, minimizing selection bias. | Swedish Administrative Registers [1] |
| Longitudinal Cohort Studies | Data Source | Provides deep, rich data on health, socioeconomic, and psychosocial variables linked to residential history over time. | Health and Retirement Study (HRS) [5], Atherosclerosis Risk in Communities (ARIC) [3] |
| Geocoded Address Histories | Data / Method | Enables precise, objective calculation of move distances and classification of move type (short vs. long distance). | ARIC study geocoding [3] |
| Multinomial Logistic Regression | Statistical Model | Models the likelihood of falling into one of multiple unordered mobility categories (e.g., move closer, move in, no change) based on health triggers. | HRS analysis of proximity changes [5] |
| Best-Subset Selection Algorithms | Statistical Method | Identifies the most important predictors of moving from a large set of variables, including meaningful interactions. | ARIC analysis of mover characteristics [4] |
The evidence is conclusive: health triggers and the associated care needs are a primary driver of mobility in later life. This movement is a non-random, strategic adaptation characterized by proximity-enhancing relocations to adult children, particularly daughters, and transitions to institutional care. The phenomenon is distinct from the mobility of younger populations in its triggers but similar in its role as a key life-course adaptation.
For the research and drug development community, these findings have profound implications:
- Clinical Trial Design: Recruitment and retention strategies must account for the high mobility of older populations following health events to prevent attrition bias.
- Endpoint Selection: Functional mobility and independence (ADLs/IADLs) are critical endpoints, as their decline is a direct precursor to life-altering relocations.
- Health Economics: The full cost of diseases like CVD and stroke must include the significant social and economic impacts of resultant residential moves and changes in caregiving. Future research should leverage emerging technologies and linked data to further elucidate the mechanisms linking specific disease pathways to mobility decisions, ultimately informing interventions that support healthy aging in place.
This whitepaper examines the dynamics of informal support networks, focusing on the migratory patterns of children and older adults as high-mover populations in response to health and familial crises. Within the context of a broader thesis on high-mobility populations, this analysis synthesizes quantitative data and qualitative research to elucidate the critical roles undertaken by daughters and siblings. The findings demonstrate that informal care structures significantly influence residential decisions, with quantitative models revealing increased relocation probabilities following cardiovascular events and qualitative studies highlighting the undervalued contributions of young siblings in psychiatric care contexts. This paper provides methodologies, data visualizations, and analytical frameworks to guide future research and inform policy decisions aimed at supporting these essential care networks.
The mobility patterns of children and older adults represent a critical area of demographic research, particularly concerning the formation and maintenance of informal support networks. Informal support networks, comprising family members who provide unpaid care and assistance, serve as a primary source of caregiving during health crises and developmental challenges [6] [5]. This paper frames its investigation within the broader thesis that children and older adults constitute high-mover populations due to their heightened dependency on these familial structures.
Among older adults, health declines—particularly unexpected cardiovascular events—act as powerful catalysts for residential relocation, either bringing adult children closer to parents or parents closer to children [5]. Conversely, among children, the presence of a sibling with significant health needs creates a unique caregiving dynamic that shapes family systems and developmental outcomes [6]. Within these networks, daughters disproportionately assume caregiving roles for aging parents, while siblings of children with psychiatric disorders often provide substantial emotional and practical support despite their own developmental needs [6] [5].
This whitepaper provides researchers, scientists, and drug development professionals with a technical analysis of these phenomena, emphasizing quantitative methodologies, experimental protocols, and visualization tools to advance understanding of how informal support networks influence population mobility and health outcomes.
Quantitative Analysis of Support-Driven Mobility
Cardiovascular Events and Proximity Changes
Analysis of longitudinal data from the Health and Retirement Study (HRS) reveals a significant association between the onset of cardiovascular disease (CVD) and changes in intergenerational residential proximity. The following table summarizes key quantitative findings from a nationally representative study of older adults in the United States [5].
Table 1: Impact of First Cardiovascular Event on Residential Proximity to Adult Children
| Variable | Baseline Probability (No CVD) | Post-CVD Probability | Relative Risk Ratio | Statistical Significance |
|---|---|---|---|---|
| Move In Together | 1.2% | 1.9% | 1.61 | p < 0.05 |
| Move Closer | 4.1% | 6.4% | 1.55 | p < 0.05 |
| Any Proximity Increase | 5.3% | 8.3% | 1.57 | p < 0.05 |
The data demonstrates that a first cardiovascular event increases the two-year predicted probability of children and parents moving closer together, with specific subgroups showing heightened responsiveness [5]:
- Spouseless older adults: Those without a spouse were significantly more likely to experience proximity changes with adult children following CVD onset, highlighting the substitution effect between spousal and child caregiving.
- Daughter availability: Families with at least one daughter showed greater responsiveness to CVD events, confirming the predominant role of daughters in providing informal care support.
- Stroke survivors: Compared to other cardiovascular conditions (myocardial infarction, congestive heart failure), stroke—which often results in more severe long-term disability—triggered more substantial residential adjustments.
Sibling Impact and Emotional Adaptation
Qualitative research on siblings of children with psychiatric disorders reveals substantial impacts, though these effects often resist simple quantification. The following table synthesizes findings from hermeneutic phenomenological analysis of interviews with 13 siblings aged 8-15 [6].
Table 2: Impacts and Support Needs of Siblings of Children with Psychiatric Disorders
| Impact Domain | Manifestation | Support Need | Preferred Support Modality |
|---|---|---|---|
| Emotional Conflict | Guilt, resentment, ambivalence about family adaptation to sibling's needs | Personalized attention from parents; acknowledgment of personal struggles | Informal, conversational support rather than structured therapy |
| Social Functioning | Restricted social activities; concerns about explaining sibling's condition to peers | Peer connection with others in similar situations; normalization of experience | Play-based interactions; casual group settings |
| Family Dynamics | Perceived inequity in parental attention; responsibility for sibling care | Involvement in care process; age-appropriate information about sibling's condition | Family inclusion in treatment planning; shared activities |
| Identity Development | Defining self in relation to sibling's needs; increased maturity and empathy | Recognition of individual strengths and achievements outside caregiving role | Mentoring relationships; opportunities for personal achievement |
Methodological Approaches
Longitudinal Analysis of Residential Proximity
Study Design and Population: The investigation into cardiovascular events and proximity changes employed a longitudinal design using waves from the Health and Retirement Study (2004, 2006, 2008) [5]. The baseline sample included respondents who were: (1) aged 55+ in 2004; (2) living in the community; (3) interviewed in 2004 and 2006/2008; (4) without CVD history as of 2004; and (5) had no co-resident child but at least one non-coresident child in the prior interview.
Key Variables and Measurement:
- Cardiovascular events: Included new onset of stroke, myocardial infarction, or congestive heart failure between survey waves, identified through self-report.
- Residential proximity: Measured using geographic information on children's residences, categorized as: (1) same household; (2) <1 mile; (3) 1-10 miles; (4) 10-100 miles; (5) 100+ miles; (6) unknown.
- Covariates: Included age, gender, race, education, income, wealth, marital status, number of children, baseline health conditions, and functional limitations.
Analytical Approach: Multinomial logistic regression models estimated the association between incident CVD and changes in proximity, adjusting for covariates. Models specifically tested interaction effects for spouseless individuals and those with daughters.
Hermeneutic Phenomenology in Sibling Research
Qualitative Methodology: The investigation of siblings' experiences employed a hermeneutic phenomenological framework to interpret the meaning of lived experiences [6]. This approach recognizes that personal narratives provide access to how individuals evaluate life conditions and ascribe meaning to them.
Data Collection Protocol:
- Participant Recruitment: Purposive sampling of children (ages 8-16) with siblings diagnosed with psychiatric disorders, recruited through a child psychiatric day clinic.
- Interview Protocol: Unstructured interviews conducted in chosen locations to build trust, beginning with neutral questions before exploring sibling relationships. Sessions lasted ≤60 minutes.
- Ethical Considerations: Project approval by Medical Ethical Commission; written informed consent from participants and parents.
Analytical Process: The hermeneutic analysis proceeded through three distinct phases [6]:
- Naïve Reading: Initial reading of interview transcripts to develop preliminary understanding.
- Structural Analysis: Identification of recurring structures and coding of text into "meaning units." Comparison of individual "sub-themes" across interviews to identify shared "main themes."
- Validated Interpretation: Continuous validation of meaning units, subthemes, and main themes through circular refinement against previous analytical stages.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Resources for Support Network Research
| Research Tool | Function | Application Example | Technical Specifications |
|---|---|---|---|
| Health and Retirement Study (HRS) | Nationally representative longitudinal dataset | Tracking residential proximity changes before/after health events | Biennial survey; demographic, economic, health data; geographic child locations |
| Hermeneutic Phenomenological Framework | Qualitative analysis of lived experiences | Interpreting meaning in siblings' narratives of family life | Three-phase approach: naïve reading, structural analysis, validated interpretation |
| Multinomial Logistic Regression | Statistical modeling of categorical outcomes | Predicting probability of proximity change categories post-CVD | Handles nominal dependent variables; estimates relative risk ratios |
| ACT Rules for Color Contrast | Ensuring visual accessibility in research dissemination | Creating compliant data visualizations and diagrams | Minimum 4.5:1 contrast ratio for normal text; 3:1 for large text [7] [8] [9] |
| Open DOT Language | Standardized graph visualization | Diagramming methodological workflows and conceptual models | Text-based graph description; compatible with Graphviz tools |
The investigation of informal support networks reveals consistent patterns in the mobility behaviors of children and older adults as high-mover populations. Quantitative evidence demonstrates that health shocks, particularly cardiovascular events, systematically trigger residential realignments within families, with daughters assuming disproportionate caregiving responsibilities. Qualitative findings illuminate the complex emotional landscapes of siblings providing support to brothers and sisters with psychiatric disorders, highlighting their need for acknowledgment and age-appropriate inclusion rather than formalized support structures.
These findings carry significant implications for researchers, healthcare professionals, and policy makers seeking to understand and support these critical care networks. Future research should continue to develop integrated methodologies that bridge quantitative and qualitative approaches, creating more comprehensive models of how informal support networks shape population mobility and wellbeing across the lifespan.
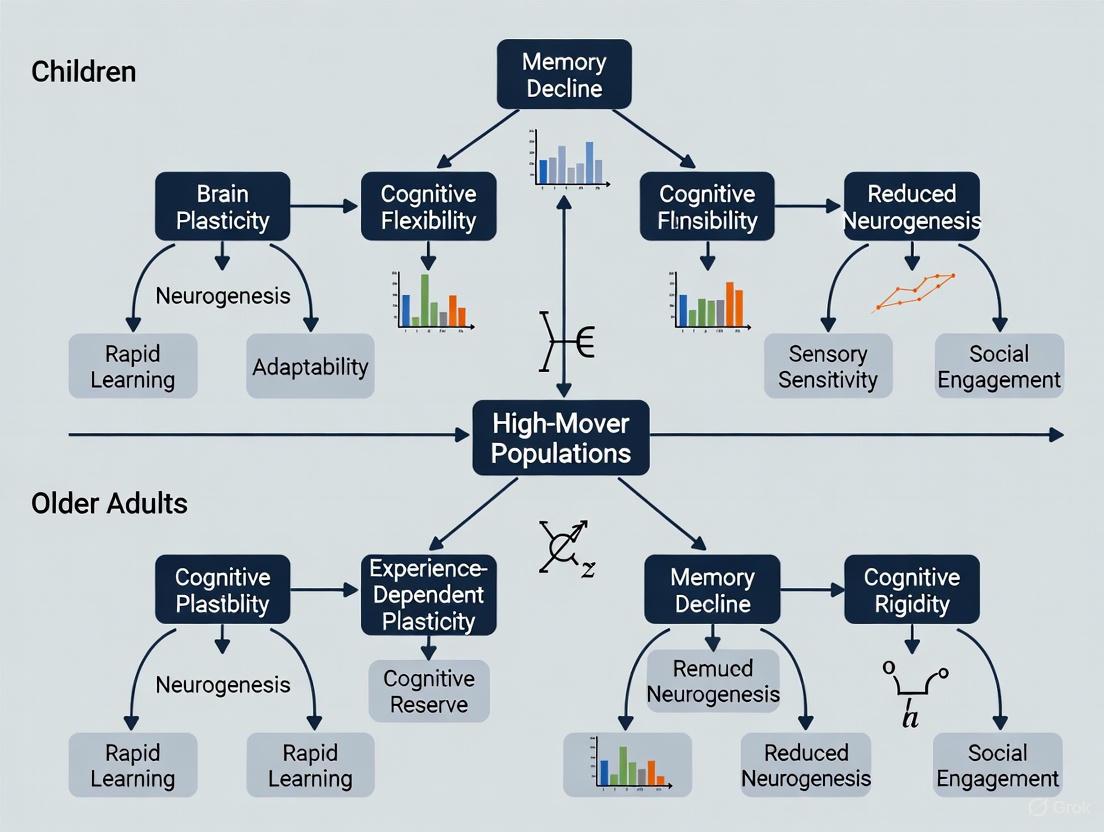
This technical guide examines pediatric and older adult populations as high-mobility groups within life course theory. While children experience mobility primarily through parental decisions shaped by educational opportunities, health considerations, and socioeconomic factors, older adults typically move in response to health declines and care needs. Analyzing data from longitudinal studies and population registers, this whitepaper identifies key drivers across life stages and demonstrates how early-life mobility patterns establish trajectories with long-term consequences for health, educational attainment, and socioeconomic status. The structural dynamics creating high mobility in these populations provide critical insights for researchers and policy professionals addressing intergenerational health and social stratification.
Life course perspective provides the fundamental theoretical framework for understanding why children and older adults constitute high-mobility populations. This approach conceptualizes human development as a lifelong process shaped by historical and social contexts, with earlier life events establishing trajectories that influence subsequent outcomes [10]. Within this framework, mobility represents not merely geographical relocation but a manifestation of broader social and biological processes that unfold across distinct developmental periods.
The life course principle of timing recognizes that the impact of transitions and events depends on when they occur in a person's life. For children, mobility decisions are predominantly made by parents and reflect complex calculations balancing perceived opportunities against constraints. These decisions often cluster around key transition points in educational systems, creating predictable mobility patterns around school entry ages [10]. In contrast, older adult mobility frequently responds to health triggers such as new limitations in activities of daily living (ADLs) or instrumental activities of daily living (IADLs), widowhood, or the need for specialized care [11] [12].
Both populations experience decreased autonomy in mobility decisions compared to working-age adults—children due to developmental dependence, and older adults due to health-related dependencies. This shared structural position as dependent populations creates parallel methodological challenges for researchers studying mobility patterns and their consequences.
Pediatric Mobility: Parental Decisions and Educational Trajectories
Quantitative Patterns in Pediatric Mobility Drivers
Table 1: Primary Drivers of Pediatric Mobility Based on Longitudinal Studies
| Driver Category | Specific Factors | Data Source | Impact Measurement |
|---|---|---|---|
| Educational Opportunities | School quality, Academic tracking, Special programs | British National Child Development Study [10] | Strong influence on occupational skill qualifications in mid-adulthood |
| Health Considerations | Persistent poor health, Prenatal exposures, Chronic conditions | British National Child Development Study [10] | 30%+ reduction in educational performance; effects largely explained by early academic achievement |
| Family Structure | Parental resources, Sibling configuration, Caregiver availability | National Health and Aging Trends Study [11] | 90% of children live with familial caregivers when needed |
| Socioeconomic Status | Income, Parental education, Occupational status | Life course mobility models [10] | Compensatory (resource buffer) vs. exacerbation (loss of advantage) patterns |
Mechanisms Linking Early Health to Mobility and Attainment
Childhood health limitations significantly influence long-term educational and occupational outcomes through multiple pathways. The British National Child Development Study followed a cohort from birth through middle age, demonstrating that poor health before and during education predicts lower occupational skill qualifications in mid-adulthood [10]. These associations are particularly strong for children in persistently poor health rather than those with transient conditions.
The explanatory mechanism operates primarily through academic performance early in children's educational careers. Performance differentials emerge before the first important educational transition points, suggesting that health-related cognitive and non-cognitive skill development establishes trajectories that influence subsequent placement in educational tracks [10]. The relationship between specific prenatal exposures (e.g., maternal smoking) and mid-adulthood qualifications demonstrates particular persistence even after accounting for early academic performance.
Table 2: Methodological Approaches for Studying Pediatric Mobility and Outcomes
| Method Type | Data Collection Approach | Analytical Technique | Key Strengths |
|---|---|---|---|
| Longitudinal Cohort | Follow cohorts from birth through adulthood (e.g., British NCDS) | Life course models, Path analysis, Structural equation modeling | Captures temporal ordering; establishes causality |
| Administrative Register | Link health, education, and tax records | Fixed effects models, Regression discontinuity | Large sample sizes; minimal recall bias |
| Time Use Surveys | 24-hour activity diaries (e.g., American Time Use Survey) | Time budget analysis, Sequence analysis | Captures daily routines; reveals trade-offs |
Methodological Framework: Experimental Protocols for Mobility Research
Longitudinal Cohort Study Protocol
Objective: To examine the relationship between childhood health, educational mobility, and long-term socioeconomic attainment.
Population: Nationally representative birth cohort (e.g., British National Child Development Study with participants born in 1958) [10].
Data Collection Waves:
- Baseline: Prenatal period (maternal health behaviors, socioeconomic indicators)
- Childhood Assessments: Ages 7, 11, 16 (health limitations, cognitive testing, teacher evaluations)
- Early Adulthood: Age 23 (educational qualifications, first occupation)
- Mid-Life: Age 42 (occupational skill qualifications, income, health status)
Key Variables:
- Independent Variables: Persistent poor health (defined as health limitations at multiple assessment points), prenatal exposures (maternal smoking), socioeconomic background
- Mediating Variables: Academic performance at ages 7, 11, and 16; educational track placement; school absence
- Outcome Variables: Occupational skill qualifications in mid-adulthood coded using standardized classification
Analytical Approach: Path analysis with maximum likelihood estimation to test direct and indirect effects of childhood health on adult qualifications, controlling for socioeconomic background and testing for moderation effects.
Geographic Mobility and Caregiving Study Protocol
Objective: To quantify travel behavior changes among family caregivers of older adults.
Data Source: American Time Use Survey (ATUS) extracts covering a 9-year period, with daily time diaries from approximately 13,000 respondents including caregivers and non-caregivers [13].
Caregiver Identification: Respondents self-identifying as providing unpaid care for aging family members in the past 3-6 months.
Time Use Coding:
- Primary activities (e.g., direct care, medical care coordination)
- Travel time associated with care activities
- Simultaneous activities (e.g., care provision during travel)
Analytical Approach: Multivariate regression models controlling for employment status, household structure, race/ethnicity, and day of week, with separate models for male and female caregivers to test for gender differences in travel burdens.
Research workflow for life course mobility studies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Resources for Life Course Mobility Studies
| Resource Category | Specific Instrument/Data Source | Application in Mobility Research |
|---|---|---|
| Longitudinal Cohort Data | British National Child Development Study (NCDS) [10] | Tracking health-education linkages from birth to midlife |
| Time Use Surveys | American Time Use Survey (ATUS) [13] | Quantifying care-related travel burdens and time poverty |
| Health Assessment Tools | Activities of Daily Living (ADLs)/Instrumental ADLs scales [11] | Measuring functional limitations triggering mobility events |
| Administrative Registers | Swedish Population Registers [1] | Large-sample analysis of geographic mobility patterns |
| Mobility Metrics | Life-Space Mobility (LSM) assessment [12] | Evaluating mobility across different environmental zones |
| Geospatial Tools | Global Human Settlement Layer (GHSL) [14] | Harmonized definition of urban areas for cross-national comparison |
Older Adult Mobility: Health and Care Dynamics
Quantitative Patterns in Older Adult Mobility
Health triggers represent the primary driver of mobility in older populations, with distinct patterns emerging by severity of limitation. Analysis of Swedish register data demonstrates that severe health problems increase the likelihood of parents relocating closer to children or into institutions by 40-60%, but show no significant association with children moving closer to parents [1]. This asymmetry reflects the complex negotiation of care needs within family systems.
Gender patterning significantly structures older adult mobility, with mothers more likely to move toward daughters or toward distant children who have at least one sibling living nearby [1]. This reflects the well-documented gender division of care labor, where daughters provide more care, particularly for activities of daily living [11].
Table 4: Mobility Triggers and Patterns in Older Adults (80+)
| Mobility Type | Primary Triggers | Likelihood with Severe Health Problems | Gender Patterns |
|---|---|---|---|
| Parent Moves to Child | Widowhood, ADL limitations, Cognitive decline | 40-60% increase [1] | Mothers move toward daughters; relies on sibling proximity |
| Institutional Relocation | Multiple ADL limitations, High care needs, Cognitive impairment | Stronger than geographic convergence [1] | Women overrepresented due to longevity and higher disability rates |
| Child Moves to Parent | Parent health crises, Lack of local support, Only child status | No significant association [1] | Limited gender differentiation |
Conceptual Framework of Late-Life Mobility
Determinants of older adult mobility decisions
Integration and Implications for Research and Policy
The parallel high-mobility status of children and older adults reflects their shared structural position as dependent populations whose mobility decisions are made within constraints imposed by others' assessments of their needs and capabilities. For researchers and drug development professionals, this intersection presents several critical considerations:
Methodological implications include the need for longitudinal designs that capture mobility events in relation to key transition points, whether educational transitions for children or health transitions for older adults. The explanatory mechanisms differ substantially between these populations—while pediatric mobility influences outcomes primarily through educational opportunity structures, older adult mobility responds to declining functional capacity and care availability.
Intervention leverage points also differ across life stages. For children, policies addressing early identification of health and developmental limitations can mitigate negative educational consequences [10]. For older adults, supporting "aging in place" through assistive technologies and home modifications can reduce disruptive relocations while maintaining quality of life [12]. Both populations benefit from approaches that recognize mobility as embedded within family systems rather than individual decisions.
Future research should develop integrated models that track how early-life mobility experiences establish trajectories influencing later-life mobility patterns, creating potential pathways of cumulative advantage or disadvantage across the life course.
Socioeconomic and Geographic Disparities in Relocation Patterns
The study of relocation patterns represents a critical area of demographic research, particularly concerning two high-mover populations: children and older adults. While these groups exhibit elevated mobility rates, the underlying drivers, implications, and socioeconomic mediators differ substantially. Children typically move as dependents within family units responding to economic opportunities, housing adjustments, and community resources [15]. Older adults experience mobility driven by retirement transitions, health needs, and caregiving requirements [16]. Understanding the distinct relocation patterns of these demographics is essential for policymakers, urban planners, and public health professionals addressing the consequences of geographic mobility. This technical guide examines the socioeconomic and geographic disparities shaping relocation patterns, employing rigorous methodological frameworks to analyze moving behaviors and their impacts across the life course. The complex interplay between economic constraints, social policies, and developmental needs creates distinctive mobility signatures for these populations, requiring sophisticated analytical approaches to disentangle competing influences on relocation decisions.
Theoretical Frameworks for Understanding Relocation Disparities
Economic Migration Theories
Traditional economic models frame migration decisions as rational calculations weighing expected benefits against costs [17]. These models prioritize employment opportunities, earnings differentials, and housing costs as primary drivers. Within this framework, families with children often relocate to optimize human capital development and long-term economic prospects [15], while older adults may move to maximize retirement resources or access age-specific amenities [16]. The declining geographic mobility observed across all age groups in recent decades suggests structural changes in these economic calculations, potentially due to dual-earner household constraints, housing market transformations, or regional convergence in wage premiums [17].
Life Course Perspective
The life course perspective provides a developmental framework for understanding age-graded mobility patterns. Transition points such as family formation, child-rearing, and retirement create mobility susceptibilities through changing housing needs and social obligations. For children, mobility is often involuntary and linked to parental socioeconomic status, with profound implications for developmental outcomes and opportunity structures [15]. Older adults face mobility decisions shaped by accumulating health limitations, changing social networks, and caregiving availability [16]. The life course approach emphasizes how historical context, such as pandemic disruptions or economic recessions, shapes these mobility transitions differently across birth cohorts.
Intersectional Inequality Framework
An intersectional framework acknowledges that relocation patterns reflect compounded advantages and disadvantages across multiple social axes [18]. Disparities emerge through intersecting identities of age, race, socioeconomic status, and migration history. This framework is particularly relevant for understanding the heightened vulnerabilities of certain subpopulations, such as migrant children [19] or economically disadvantaged older adults [20]. Research demonstrates how structural inequities in healthcare access, neighborhood opportunity, and social protection create systematically different mobility constraints and outcomes across population segments [18] [15].
Methodology for Analyzing Relocation Patterns
Table 1: Primary Data Sources for Analyzing Relocation Patterns
| Data Source | Population Coverage | Key Mobility Metrics | Strengths | Limitations |
|---|---|---|---|---|
| Current Population Survey (CPS) [17] | U.S. households | Annual state-to-state migration rates; demographic and labor force characteristics | Large sample size; detailed demographic and economic variables | Does not capture reasons for move; limited contextual data |
| CDC WONDER Database [20] | U.S. mortality records | Geographic and demographic mortality variations | Detailed cause-of-death data; longitudinal tracking | Limited to mortality outcomes; no direct mobility measures |
| Redfin Platform Data [21] | Online home searchers | Anticipated migration through search patterns; housing cost data | Real-time behavioral data; geographic specificity | Selection bias toward housing-market participants |
| UN Migration Stock Data [19] | International migrants | Global migrant stocks by age and destination | Comparative international framework; child-specific estimates | Limited socioeconomic characteristics; infrequent updates |
Statistical Modeling Approaches
Multivariate regression models represent the primary analytical method for identifying factors predicting migration decisions. The standard protocol involves specifying a model with migration status as the dependent variable and a vector of independent variables capturing demographic characteristics, economic incentives, and geographic attributes [17] [21]. Model specification should control for age, marital status, labor force participation, homeownership, and parental status, with special attention to interaction effects capturing differential responses across subpopulations [17].
For temporal analysis of migration trends, researchers employ joinpoint regression to identify significant change points in time series data [20]. This method fits a series of connected straight lines to the migration rate data, testing whether each joinpoint (where trends change) is statistically significant. The protocol involves calculating Annual Percentage Changes (APCs) for each segment and overall Average Annual Percentage Changes (AAPCs) to quantify trend magnitudes.
Spatial analysis techniques incorporate geographic information systems to map migration flows and identify clustering of mobility patterns. These approaches are particularly valuable for detecting regional disparities and neighborhood-level effects on relocation decisions [21]. Spatial regression models can test whether migration patterns in proximate locations demonstrate autocorrelation, requiring specialized estimation techniques.
Experimental Workflow for Migration Analysis
The following diagram illustrates the systematic research workflow for analyzing relocation patterns:
Relocation Patterns in Child Populations
Demographic Trends and Disparities
Child relocation patterns reflect family responses to economic opportunities and constraints. Recent data indicates nearly 1 million additional children experiencing poverty following the reduction of pandemic-era social investments, exacerbating mobility-related stresses [15]. The Child Opportunity Index reveals stark disparities in neighborhood resources, with approximately 60% of Black, Hispanic, and American Indian/Alaska Native children residing in lower-opportunity neighborhoods [15]. These geographic disparities in childhood resources create unequal developmental contexts with lifelong consequences for health, education, and economic mobility.
International child migration represents another significant dimension of relocation patterns. In 2020, 36 million children were international migrants, with 34 million refugees and asylum seekers forcibly displaced from their countries—half of them children [19]. The global migrant child population has increased by 50% since 1990, rising from 24 million to 36 million, creating urgent needs for specialized protection policies and integration services [19].
Socioeconomic Mediators of Child Mobility
Table 2: Socioeconomic Factors Influencing Child Relocation Patterns
| Factor | Impact on Mobility | Evidence | Disparity Dimensions |
|---|---|---|---|
| Neighborhood Opportunity | Families with resources move to higher-opportunity areas; constrained families remain in disadvantaged neighborhoods | 60% of Black, Hispanic, and American Indian children live in low-opportunity neighborhoods [15] | Racial/ethnic and socioeconomic disparities in access to high-opportunity areas |
| Housing Costs | High housing costs reduce mobility; families with children prioritize housing size and quality | Housing restrictions lowered U.S. GDP growth by 36% (1964-2009) [17] | Low-income families face severe constraints in high-opportunity areas |
| Child Care Accessibility | Families locate near relatives for child care; availability influences employment-related moves | Women living near parents experienced smaller earnings drops after having children [17] | Geographic variation in child care costs and availability |
| Parental Education | Highly educated parents cluster in cities with better schools and amenities | Geographic sorting by education with highly educated in large cities [17] | Intergenerational transmission of advantage through residential sorting |
Economic instability represents a powerful driver of child mobility, with families responding to employment shocks, housing cost pressures, and changing household composition. The end of pandemic-era child care funding has created a "funding cliff," exacerbating affordability challenges for working parents [15]. These economic pressures produce distinctive mobility patterns, including doubled-up households, frequent residential moves, and homelessness—each with documented negative consequences for child development and educational continuity.
Relocation Patterns in Older Adult Populations
Demographic Trends and Disparities
Older adult mobility reflects complex negotiations between health needs, economic resources, and social connections. America's rapidly aging population faces distinctive challenges, including increasing caregiving gaps as the traditional caregiver population (ages 45-64) shrinks relative to the oldest-old cohort [16]. By 2040, the caregiver ratio is projected to fall to 3:1 (from 6:1 in 2025), creating potential mobility pressures as older adults seek supportive environments [16].
Health disparities significantly shape later-life mobility patterns. Mortality from malnutrition and gastrointestinal cancers among older adults demonstrates striking racial and geographic variation, with Black or African American individuals experiencing rates of 5.3 per 100,000 compared to lower rates among other groups [20]. Alaska (7.1) and the Western United States (7.0) show the highest regional mortality rates, while nonmetropolitan areas consistently exceed metropolitan areas in age-adjusted mortality (4.0 vs. 3.3) [20]. These health gradients create distinctive mobility patterns as older adults seek appropriate medical care and support services.
Socioeconomic Mediators of Older Adult Mobility
Table 3: Socioeconomic Factors Influencing Older Adult Relocation Patterns
| Factor | Impact on Mobility | Evidence | Disparity Dimensions |
|---|---|---|---|
| Caregiving Availability | Older adults move closer to family care; or to facilities when family unavailable | 69% of older adults receive only informal care; 5% receive only formal care [16] | Childless older adults rely more on siblings and other relatives |
| Health Infrastructure | Mobility toward areas with better healthcare services; away from underserved areas | Mortality from malnutrition/GI cancer rising since 2013 (APC: 11.6) [20] | Rural-urban disparities in healthcare access and outcomes |
| Housing Affordability | Constrained mobility despite changing needs; aging in place without appropriate modifications | Households less responsive to housing costs; prefer to stay [17] | Low-income older adults face worst housing-cost burdens |
| Social Isolation | Mobility decisions influenced by social network preservation; relocation can disrupt ties | Socially isolated older adults face greater risk of early death, dementia, heart disease [16] | Black Americans, poverty populations, sexual/gender minorities experience higher isolation |
The dramatic growth of Medicare Advantage plans (enrolling 54% of older adults in 2024, up from 19% in 2007) has created new constraints on mobility through network restrictions and service area limitations [16]. Simultaneously, family caregiving demands have intensified, with time spent assisting older adults with dementia increasing by almost 50% between 2011 and 2022 (from 21 to 31 hours weekly) [16]. These competing pressures—institutional constraints versus family resources—create complex mobility decisions for older households.
Research Reagents and Analytical Tools
Table 4: Essential Research Materials for Studying Relocation Patterns
| Research Tool | Function | Application Example | Technical Specifications |
|---|---|---|---|
| Current Population Survey (CPS) | Provides annual migration flows with demographic and economic covariates | Analyzing declining interstate migration trends by age, marital status, and labor force participation [17] | Annual sample size ~50,000 households; includes geographic mobility supplement |
| CDC WONDER Database | Analyzes mortality trends by geographic and demographic characteristics | Tracking malnutrition and GI cancer mortality disparities by region and race [20] | Underlying cause-of-death data with multiple demographic stratifiers |
| Joinpoint Regression Software | Identifies significant trend change points in temporal data | Determining when mortality trends reversed from decline to increase [20] | National Cancer Institute software; tests up to 3 joinpoints |
| Child Opportunity Index | Measures neighborhood resources affecting child development | Documenting racial/ethnic disparities in access to high-opportunity neighborhoods [15] | Composite index of 29 indicators across education, health, environment domains |
| Redfin Platform Data | Captures housing search behavior indicating anticipated migration | Analyzing factors influencing planned moves across metropolitan areas [21] | Search data from major real estate platform; geographic and temporal variation |
Advanced research approaches incorporate biomarker data, wearable sensors, and geographic information systems to capture multidimensional influences on mobility behavior [16]. Biomarker collection through blood and other medical tests offers insights into physiological processes linking stress, environmental conditions, and relocation decisions. Wearable devices can track social interactions and physical mobility, providing real-time behavioral data to complement traditional survey measures. These methodological innovations enable more precise measurement of the mechanisms connecting socioeconomic status, geographic context, and relocation outcomes.
Socioeconomic and geographic disparities in relocation patterns for children and older adults reflect structural inequities with profound implications for health, economic security, and intergenerational mobility. Children's mobility is largely involuntary, embedding them in opportunity structures with lasting developmental consequences [15]. Older adults face mobility decisions constrained by accumulating health limitations, caregiving availability, and fixed incomes [16]. Both populations demonstrate heightened vulnerability to policy shocks, economic downturns, and environmental disruptions, requiring targeted interventions to address their distinctive needs.
Research indicates promising policy directions, including strengthened social protection systems, investment in community infrastructure, and anticipatory governance approaches that recognize the intersecting dimensions of demographic disadvantage [18]. For children, expanding access to high-opportunity neighborhoods through housing assistance and community investment may mitigate relocation-driven disparities [15]. For older adults, developing comprehensive long-term care systems while supporting family caregivers may create more sustainable mobility options [16]. Future research should prioritize longitudinal designs that capture mobility trajectories across the life course, integrate biological and social determinants, and evaluate policy interventions addressing the structural drivers of relocation disparities.
Research Design and Pharmacovigilance in Dynamic Populations
Designing Robust Longitudinal Studies with Mobile Cohorts
Longitudinal studies, which employ continuous or repeated measures to follow particular individuals over prolonged periods of time—often years or decades—provide invaluable insights into developmental trajectories, health outcomes, and the long-term effects of interventions. [22] However, their implementation faces particular methodological challenges when studying high-mover populations, such as children and older adults, who experience frequent residential transitions or inherent instability in their living situations.
For children, factors including family dynamics, parental career changes, economic pressures, and housing instability can create frequent relocations. [23] Among older adults, transitions may be driven by health declines, financial constraints, moving to be closer to family support, or entering care facilities. [24] These mobility patterns threaten longitudinal research through attrition bias and interrupted data collection, potentially compromising the validity of findings. This guide provides technical methodologies for maintaining robust data collection with these mobile cohorts.
Core Methodological Framework
Defining Longitudinal Study Designs
Longitudinal research employs continuous or repeated measures to follow individuals over prolonged periods, enabling researchers to identify and relate events to particular exposures, establish sequences of events, and follow change over time within particular individuals. [22] Several design variants exist:
- Prospective Cohort Studies: Same participants followed over time, with data collected before relevant outcomes occur. [22]
- Repeated Cross-Sectional Studies: Different participants sampled from the same population at each time point. [22]
- Linked Panel Studies: Data collected for other purposes is linked to form individual-specific datasets. [22]
Table 1: Advantages and Disadvantages of Longitudinal Designs
| Advantages | Disadvantages |
|---|---|
| Establish sequence of events | Participant attrition and loss to follow-up |
| Track individual change over time | Difficulty separating reciprocal exposure-outcome impact |
| Reduce recall bias through prospective data collection | Increased temporal and financial demands |
| Account for cohort, period, and age effects | Requires robust infrastructure to withstand time challenges |
Special Considerations for Mobile Cohorts
Mobile populations present unique methodological challenges that require specialized approaches:
- Infrastructure Stability: The research infrastructure must maintain consistent data collection methods across multiple geographic locations and withstand the test of time. [22]
- Remote Engagement: Technologies must enable continued follow-up despite participant relocation, requiring flexible, location-independent assessment methods. [24]
- Standardized Protocols: Data collection and recording methods must be identical across study sites and consistent over time to maintain data integrity. [22]
- Unique Identification Systems: All information pertaining to particular individuals must be linked through robust coding systems that persist despite location changes. [22]
Implementation Strategies for Mobile Cohorts
Digital Data Collection Framework
Modern longitudinal studies increasingly leverage digital technologies to maintain contact with mobile participants, though this introduces considerations regarding the digital divide—disparities in digital technology access, usage, and outcomes. [24]
Table 2: Operationalizing Digital Data Collection
| Component | Implementation Method | Mobile Cohort Consideration |
|---|---|---|
| Digital Access | Provision of tablets/smartphones with data plans | Addresses access gaps prevalent among lower socioeconomic groups [24] |
| e-Communication | Health portals, messaging platforms, virtual visits | Requires training to overcome usage gaps, particularly among older adults [24] |
| Cognitive Support | Digital literacy training, simplified interfaces | Mitigates self-efficacy gaps in information seeking [24] |
| Remote Monitoring | Wearable sensors, mobile health apps | Enables continuous data collection despite geographic mobility |
Research indicates that while digital access gaps are decreasing over time (OR = 0.86, 95% CI = 0.78, 0.94), disparities persist particularly among older adults with lower education and income, and those identifying as Hispanic. [24] These patterns must be considered when implementing digital frameworks with mobile cohorts.
Retention Protocols for High-Mover Populations
Successful longitudinal studies with mobile cohorts implement systematic retention strategies:
- Preemptive Location Tracking: Collect multiple contact methods (email, phone, addresses of close relatives) at baseline and update regularly.
- Minimized Participant Burden: Streamline data collection procedures and offer flexible assessment scheduling to maintain participation during transitions.
- Maintained Engagement: Regular, low-stakes contact between major assessment waves (newsletters, holiday cards, small incentives).
- Exit Interviews: Conduct detailed interviews with participants leaving the study to understand reasons for attrition and improve protocols. [22]
Data Analysis Considerations
Statistical Approaches for Longitudinal Data
Analyzing longitudinal data requires specialized statistical approaches that account for the correlated nature of repeated measurements within individuals. Common methods include:
- Mixed-Effect Regression Models (MRM): Focus on individual change over time while accounting for variation in timing of measures and missing data. [22]
- Generalized Estimating Equation (GEE) Models: Rely on independence of individuals within populations to focus primarily on regression data. [22]
- Multivariate Analysis of Variance (MANOVA): Compares means across groups but sacrifices individual-specific data. [22]
A critical consideration is avoiding repeated hypothesis testing as would be applied to cross-sectional studies, as this leads to underutilization of data, underestimation of variability, and increased likelihood of Type II errors. [22]
Handling Missing Data from Mobile Cohorts
With mobile populations, missing data is inevitable and requires sophisticated handling:
- Missing Data Mechanism Analysis: Determine whether data is missing completely at random (MCAR), at random (MAR), or not at random (MNAR).
- Multiple Imputation Techniques: Create several complete datasets by imputing missing values, analyzing each, then combining results.
- Sensitivity Analyses: Test how different assumptions about missing data affect study conclusions.
Table 3: Bayesian Synthesis Approach for Multi-Cohort Data (Example) [25]
| Research Phase | Methodological Action | Outcome for Mobile Cohorts |
|---|---|---|
| Individual Cohort Analysis | Evaluate competing hypotheses within each cohort using appropriate statistical models | Maintains cohort-specific context while preparing for synthesis |
| Evidence Aggregation | Apply Bayesian methods to synthesize findings across diverse cohorts | Enables robust conclusions supported by all data sources despite mobility |
| Robustness Assessment | Test whether conclusions hold across all measurement approaches and cohorts | Provides confidence in findings despite missing data patterns |
The Bayesian research synthesis approach has been successfully demonstrated in multi-cohort developmental studies, such as research on self-control development during adolescence that aggregated evidence across three Dutch cohorts with different measures to arrive at robust conclusions. [25]
Case Study: Framingham Heart Study Adaptations
The Framingham Heart Study, initiated in 1948, represents the quintessential longitudinal study that has evolved methodologies to maintain engagement with a mobile population. [22] Originally following 5,209 subjects from Framingham, Massachusetts, the study faced challenges of geographical mobility over its decades-long duration.
Key adaptations for mobility management included:
- Multi-Generational Recruitment: Engaging children and grandchildren of original participants to maintain family linkages despite geographic dispersal.
- Decentralized Assessment Sites: Establishing satellite data collection centers to accommodate participant movement beyond the original community.
- Periodic Intensive Follow-Ups: Implementing focused tracking efforts to re-establish contact with lost participants at regular intervals.
- Flexible Data Collection Modalities: Evolving from purely in-person assessments to incorporate mail, telephone, and eventually digital data collection.
Essential Research Toolkit
Table 4: Research Reagent Solutions for Mobile Cohort Studies
| Tool Category | Specific Solutions | Function in Mobile Context |
|---|---|---|
| Participant Tracking Systems | REDCap (Research Electronic Data Capture), custom CRM databases | Maintain contact information across geographic transitions |
| Digital Assessment Platforms | Tablet-based surveys, mobile health apps, web-based cognitive tests | Enable continuous data collection despite location changes |
| Remote Sensing Technologies | Wearable activity monitors, smartphone sensors, GPS trackers | Passively capture data without requiring participant location |
| Communication Tools | Secure messaging platforms, virtual meeting software, automated reminder systems | Maintain engagement through preferred communication channels |
| Data Integration Systems | API-based data pipelines, cloud storage solutions, blockchain for data integrity | Aggregate data from multiple sources and locations securely |
Designing robust longitudinal studies for mobile cohorts requires intentional methodological planning from inception through analysis. By implementing flexible digital frameworks, proactive retention strategies, and appropriate statistical approaches that account for mobility-related challenges, researchers can maintain data integrity and generate valid findings even with high-mover populations like children and older adults. The strategic integration of technology, methodological rigor, and participant-centered protocols enables successful longitudinal investigation despite the inherent mobility of these populations.
Mitigating Attrition and Loss to Follow-up in Clinical Trials
Attrition, or loss to follow-up, presents a significant threat to the integrity and validity of longitudinal clinical research. It negatively affects statistical power, disrupts the random composition of groups, and can produce unwanted bias that compromises both internal and external validity [26]. The problem is particularly acute for special populations, including children and older adults, who experience unique challenges that make them high-attrition populations in clinical research. This technical guide examines the specific factors contributing to attrition in these vulnerable groups and provides evidence-based methodologies for mitigating these challenges throughout the clinical trial lifecycle.
For children, study participation inherently involves complex dynamics between the child, caregivers, and research staff. In pediatric traumatic brain injury (TBI) research, completers had significantly higher primary caregiver education and family income than non-completers, highlighting how socioeconomic factors indirectly impact a child's ability to remain in studies [26]. For older adults, a longitudinal aging study found attrition was most likely to occur in participants who were older, male, inactive, socially isolated, and cognitively impaired [27]. Understanding these population-specific vulnerabilities is essential for designing retention strategies that address the fundamental causes of attrition.
Quantifying the Attrition Challenge: Comparative Data Across Populations
Table 1: Attrition Rates Across Different Clinical Trial Populations
| Population | Attrition Rate | Time Frame | Key Predictors of Attrition |
|---|---|---|---|
| Pediatric TBI [26] | 20-60% | Long-term follow-up | Lower caregiver education, lower family income, higher injury severity |
| Older Adults [28] | Up to 40% | 2-year follow-up | Age, smoking, frailty, lower education, racial minority status |
| Postmenopausal Women [28] | 30.2% | 6-year follow-up | Age, smoking, frailty, lower educational level, race, hospitalization, poorer quality of life |
| Pediatric Obesity [29] | 33-51% | 12-month follow-up | Lower parental education, less structured home environment, lower treatment success |
| Neonatal Research [30] | 11% | 12-month follow-up | Less maternal education, more people in household, public insurance |
Table 2: Comparative Predictors of Attrition in Pediatric vs. Geriatric Populations
| Factor Category | Pediatric Populations | Geriatric Populations |
|---|---|---|
| Socioeconomic | Lower parental education [26] [30], Lower family income [26], Public insurance [30] | Lower educational level [28] [27], Lower socioeconomic status [28] |
| Clinical | Higher injury severity [26], Less success during treatment [29] | Cognitive impairment [27], Frailty [28], Worse self-rated health [27], Polypharmacy [28] |
| Social/Environmental | More people in household [30], Less structured eating environment [29] | Social isolation [27], Leaving house less often [27], No engagement in social activities [27] |
| Behavioral | Not significant in most studies | Smoking [28], No physical activity [27] |
Methodological Framework for Understanding Attrition
Statistical Considerations and Impact Analysis
The statistical implications of attrition extend beyond simple sample size reduction. Attrition disrupts the random composition of groups, potentially introducing confounding influences and threatening both internal validity (through disruption of group randomization) and external validity (by making data less generalizable) [26] [29]. The fragility of trial results due to patients lost to follow-up can be quantified using specialized statistical measures. The LTFU-aware fragility index is a recently developed metric that determines the number of lost patients who must have outcomes different than expected based on the observed patients to reverse statistical significance [31]. This approach allows researchers to rigorously explore how the outcomes of patients lost to follow-up could potentially alter trial conclusions.
Population-Specific Vulnerability Assessment
Children and older adults share similar vulnerabilities despite being at opposite ends of the age spectrum. Both groups often depend on caregivers for participation, face unique physiological considerations, and experience barriers related to autonomy and communication. For pediatric populations, the burden of participation falls on both the child and caregivers, with socioeconomic factors creating substantial barriers to ongoing engagement [26] [29]. For older adults, physiological changes, comorbidities, and social isolation create distinct challenges for trial participation and retention [27] [32].
Historical context and trust issues significantly impact participation in special populations. Older adults from minority communities may harbor mistrust rooted in historical unethical research practices, while parents of pediatric participants may struggle with logistical and financial burdens that disproportionately affect retention in lower-income households [33]. Understanding these contextual factors is essential for designing effective retention strategies.
Experimental Protocols and Methodologies for Retention
Retention Strategies for Pediatric Populations
Effective retention in pediatric trials requires addressing both the child's needs and caregiver barriers. In a pediatric traumatic brain injury study, researchers provided all participating families with high-speed Internet access for the first 6 months and a desktop computer to address potential disparities in Internet access and utilization [26]. This technological support was complemented by financial compensation for time spent completing assessments ($10, $50, and $35 for the 6-, 12-, and 18-month follow-ups, respectively).
In neonatal research, implementing intensive tracking measures and maintaining consistency of study procedures have shown success in improving participant retention [30]. Research coordinators in the Prematurity and Respiratory Outcomes Program (PROP) study estimated the likelihood of attrition before discharge and used this assessment to target additional support to high-risk families. The study also employed structured satisfaction surveys to identify and address family concerns early in the participation process [30].
Retention Strategies for Older Adult Populations
Retention of older adults requires addressing physical, cognitive, and social barriers to participation. Decentralized clinical trial (DCT) elements show particular promise for this population, with 74% of older adults preferring remote participation options over in-person clinic visits [32]. Implementing frontier sites at local pharmacies and clinics in community-accessible locations can significantly reduce transportation challenges.
Social isolation is a critical factor in older adult attrition. Studies show that participants not living with another study participant, those with limited social activities, and those who leave the house less frequently are at higher risk of attrition [27]. Addressing these factors through regular social contact from research staff, incorporating study activities into social routines, and creating opportunities for social connection within the trial context can improve retention.
Engagement strategies must also account for technological access and literacy among older adults. While digital solutions offer convenience, they must be implemented with appropriate support for participants with limited digital experience. This may include telephone-based alternatives, in-person technology assistance, and simplified digital interfaces designed for older users [32].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Tools for Attrition Mitigation
| Tool Category | Specific Solution | Function/Application | Evidence |
|---|---|---|---|
| Participant Tracking | Intensive tracking protocols | Identify at-risk participants early for targeted intervention | [26] [30] |
| Multiple contact methods (phone, email, mail) | Maintain communication channels for hard-to-reach participants | [28] [30] | |
| Data Collection | Decentralized clinical trial (DCT) technologies | Reduce participant burden through remote data collection | [32] |
| Wearable devices and remote monitoring | Capture objective data without requiring site visits | [32] | |
| Participant Support | Financial compensation structures | Offset participation costs and acknowledge participant time | [26] [29] |
| Technology provision (internet, devices) | Address digital divide and access disparities | [26] [32] | |
| Analytical Tools | LTFU-aware fragility indices | Quantify robustness of trial results to missing data | [31] |
| Multiple imputation techniques | Handle missing data statistically to reduce bias | [28] [31] |
Integrated Retention Workflow and Implementation Framework
Mitigating attrition in clinical trials requires a sophisticated, multi-faceted approach that addresses the unique challenges faced by high-attrition populations such as children and older adults. The evidence demonstrates that successful retention strategies must begin at study design and continue through implementation, monitoring, and analysis phases. By understanding the population-specific factors that contribute to attrition—from socioeconomic barriers in pediatric populations to social isolation and physical limitations in older adults—researchers can develop targeted interventions that maintain participant engagement throughout the trial lifecycle. The integration of technological solutions, appropriate statistical methods for handling missing data, and proactive relationship-building creates a comprehensive framework for reducing attrition and ensuring the validity and generalizability of clinical trial results across all populations.
Pharmacovigilance, defined as the science and activities relating to the detection, assessment, understanding, and prevention of adverse drug reactions (ADRs), represents a critical component of post-marketing drug safety surveillance [34]. Within this domain, the persistent challenge of underreporting disproportionately affects vulnerable populations, particularly children and older adults, who constitute high-risk populations for several physiological and methodological reasons. These groups experience unique pharmacological challenges; pediatric patients often receive drugs prescribed off-label or unlicensed due to their exclusion from clinical trials, while older adults experience age-related physiological changes and polypharmacy that increase their susceptibility to ADRs [35] [34] [36].
The convergence of limited clinical trial data for special populations and systemic underreporting creates significant gaps in drug safety profiles. Underreporting is a pervasive issue worldwide, with estimates suggesting that over 94% of ADRs go unreported by healthcare professionals [37]. This whitepaper examines the particular challenges of ADR underreporting in mobile health and rural contexts, framed within the broader thesis of pediatric and geriatric vulnerabilities, and proposes structured methodologies and technological solutions to enhance pharmacovigilance systems for these demographically and geographically underserved subgroups.
Physiological and Methodological Vulnerabilities in High-Risk Populations
Pediatric Vulnerabilities
Children are not merely "small adults" from a pharmacological perspective. Their dynamic physiological development significantly alters drug pharmacokinetics and pharmacodynamics. Key factors contributing to their classification as a high-risk population include:
- Off-label and Unlicensed Prescribing: Pediatric medication use frequently occurs outside the specifications of the marketing authorization due to the exclusion of children from clinical trials [35] [38].
- Developing Physiological Systems: Immature metabolic enzymes, renal excretion mechanisms, and changing body composition ratios result in unpredictable drug distribution and elimination patterns [34].
- Atypical ADR Presentations: Adverse reactions in children may manifest differently than in adults, often with non-specific symptoms that are easily misattributed to common childhood illnesses [35].
Geriatric Vulnerabilities
The aging process introduces another set of complex pharmacological challenges that extend beyond chronological age:
- Polypharmacy: Older adults frequently manage multiple chronic conditions, leading to the concurrent use of five or more medications. This dramatically increases the risk of drug-drug interactions and cumulative ADRs [36].
- Age-Related Physiological Changes: Reduced hepatic metabolism, declining renal function, altered body composition (increased fat-to-muscle ratio), and changes in gastrointestinal absorption collectively alter drug effects [36].
- Frailty as a Better Predictor: Contemporary research suggests that frailty status, more than age alone, better predicts ADR risk. Frail older patients are twice as likely to experience ADRs compared to non-frail patients, yet this parameter is rarely captured in current pharmacovigilance systems [39].
- Atypical Presentations: ADRs in older adults often present with non-specific geriatric syndromes such as falls, confusion, delirium, or functional decline, which are frequently misattributed to aging or comorbid conditions rather than medication effects [36].
Quantitative Assessment of Underreporting Challenges
The following tables synthesize empirical data on the scope and nature of underreporting across different contexts and populations.
Table 1: Documented Underreporting Rates and Primary Barriers in Different Settings
| Setting/Population | Underreporting Rate/Level | Primary Identified Barriers | Citation |
|---|---|---|---|
| Healthcare Professionals (General) | >94% of ADRs unreported | Lack of time, uncertainty about causation, complacency, perception that only serious ADRs need reporting | [37] |
| Pediatricians (Netherlands) | 19% had never reported an ADR | Prior knowledge of ADR (61%), uncertainty if symptom was ADR, lack of severity, time constraints | [35] [38] |
| Patients/Consumers (General) | Represents only ~9% of total reports | Ignorance of reporting systems, complacency, lethargy, low health literacy | [37] |
| Rural Settings (Mozambique) | Qualitative reporting challenges | Poor telecommunications, transportation limitations, remote location, low education levels | [40] |
Table 2: Effectiveness of Mobile Health Applications in Enhancing ADR Reporting
| Mobile Application | Region/Country | Key Efficacy Findings | Statistical Significance |
|---|---|---|---|
| MedWatcher | United States | High VigiGrade completeness score (averaging 0.80); 55.9% well-documented | N/R |
| My eReport France | France | High clinical quality score in ClinDoc tool; 36% well-documented | p = 0.002 |
| WEB-RADR (Yellow Card) | United Kingdom | Better reporting rates among patients compared to conventional methods | p < 0.01 |
| ADR Reporting App | India | Significantly better completeness score than paper-based systems | p < 0.001 |
| Med Safety | 13 African countries | Missing information: 0% (vs. 29.6% for paper-based CIOMS forms) | N/R |
Experimental Protocols and Methodologies for Addressing Underreporting
Protocol 1: Implementing Spontaneous Reporting in Resource-Limited Rural Settings
Background: Based on the Mozambique study, this protocol outlines a framework for establishing spontaneous reporting systems in rural districts with infrastructure challenges [40].
Methodology:
- Training Program Development:
- Conduct intensive training sessions for all levels of healthcare workers (including those with basic training)
- Utilize standardized ADR reporting forms ("yellow card" system)
- Focus on ADR diagnosis, treatment, and reporting procedures
- Training duration: 1-2 days with refresher sessions
Implementation Framework:
- Identify and appoint focal persons in each district to facilitate communication with the National Pharmacovigilance Unit (NPU)
- Establish routine quality-assurance site visits (monthly initially, then quarterly)
- Implement supportive supervision to identify and clarify problems in form completion and submission
- Develop simplified reporting forms with visual aids for low-literacy settings
Infrastructure Assessment:
- Evaluate telecommunications infrastructure (mobile network coverage, internet access)
- Assess transportation availability for form collection and supervision
- Implement hybrid paper-digital systems where infrastructure is limited
Outcome Measures:
- Number of ADR reports received per month
- Quality of reports (completeness, causality assessment)
- Diversity of reporters across healthcare worker categories
- Time from ADR identification to report submission
Protocol 2: Systematic Evaluation of Mobile Health Applications for ADR Reporting
Background: This protocol derives from the systematic review of mobile applications for ADR reporting, providing a standardized methodology for assessing efficacy [41].
Methodology:
- Application Selection Criteria:
- Include apps with both iOS and Android compatibility
- Select apps integrated with national pharmacovigilance systems
- Prioritize apps with user-centered design tailored to local contexts
- Ensure multi-language support where appropriate
Study Design:
- Implement randomized controlled trials or interrupted time-series analyses
- Recruit diverse participant groups (healthcare professionals, patients, caregivers)
- Establish control groups using conventional reporting methods (paper-based, web forms)
Evaluation Metrics:
- Reporting Rates: Number of ADR reports per 1000 population or per healthcare facility
- Report Quality: Assessed using standardized tools (VigiGrade, ClinDoc)
- Completeness: Percentage of reports with all mandatory fields completed
- User Experience: System Usability Scale (SUS) scores and satisfaction surveys
Statistical Analysis:
- Employ multivariable logistic regression to identify factors associated with willingness to use apps
- Use Wilcoxon two-sample tests or Kolmogorov-Smirnov tests for completeness scores
- Calculate adjusted odds ratios (AOR) with 95% confidence intervals for predictive factors
Implementation Considerations:
- Assess connectivity requirements for low-resource settings
- Provide basic computer and mHealth-related training to users
- Ensure data privacy and security compliance
- Plan for scalability and interoperability with existing health information systems
Visualization of Pharmacovigilance System Relationships and Workflows
Diagram 1: Pharmacovigilance ecosystem relationships showing how special populations and rural settings face multiple barriers leading to underreporting, and how interventions can mitigate these challenges.
Diagram 2: Comprehensive ADR reporting workflow from identification through signal detection, showing multiple entry points for different reporting contexts and modalities.
Table 3: Key Research Reagents and Resources for Pharmacovigilance Studies
| Tool/Resource | Type | Primary Function | Application Example |
|---|---|---|---|
| VigiBase | International Database | WHO global ICSR database; aggregates reports from >140 countries | Signal detection for rare ADRs across diverse populations [34] |
| EudraVigilance | Regulatory Database | EU system for managing ADR reports; supports signal detection | Monitoring post-authorization safety within EU member states [34] |
| FAERS | Regulatory Database | FDA Adverse Event Reporting System; US post-marketing surveillance | Data mining for drug safety signals in US population [34] |
| MedDRA | Terminology | Medical Dictionary for Regulatory Activities; standardized terminology | Coding ADR terms for consistent analysis across reports [42] |
| VigiGrade | Assessment Tool | WHO tool for assessing completeness of ADR reports | Quality assessment in mobile app efficacy studies [41] |
| Disproportionality Analysis Methods | Statistical | Algorithms (ROR, PRR, BCPNN) to identify drug-ADR associations | Signal detection in large spontaneous reporting databases [34] |
| mERA Checklist | Assessment Framework | mHealth Evidence Reporting and Assessment | Evaluating quality and completeness of mHealth intervention studies [41] |
| AXIS Tool | Assessment Framework | Appraisal tool for Cross-Sectional Studies | Quality assessment of observational pharmacovigilance studies [37] |
Addressing underreporting in mobile and rural subgroups requires a multifaceted approach that acknowledges the unique vulnerabilities of pediatric and geriatric populations while implementing context-appropriate solutions. The evidence indicates that technological innovations, particularly mobile health applications, demonstrate significant promise in improving both the quantity and quality of ADR reports. However, their effectiveness depends on addressing fundamental barriers including knowledge gaps, attitudinal factors, and infrastructural limitations.
Future pharmacovigilance strategies should incorporate frailty measures alongside chronological age for geriatric risk stratification, develop pediatric-specific ADR lexicons to improve recognition, and implement adaptive mobile solutions that function in low-connectivity environments. Furthermore, successful implementation requires basic digital literacy training for healthcare professionals and patients, integration with existing health information systems, and context-specific adaptations for rural and resource-limited settings.
By recognizing children and older adults as distinct high-risk populations with unique pharmacovigilance needs, and by tailoring reporting systems to overcome geographical and technological barriers, we can significantly strengthen global drug safety surveillance and protect our most vulnerable patients from preventable medication-related harm.
Leveraging Real-World Data and Digital Health Technologies for Dynamic Tracking
The integration of Real-World Evidence (RWE) and Digital Health Technologies (DHT) is transforming the landscape of clinical research and public health surveillance. This technical guide explores how these tools enable dynamic tracking of high-mobility populations, with a specific focus on the factors driving mobility in children and older adult demographics. For researchers and drug development professionals, leveraging these technologies provides unprecedented insights into patient experiences outside controlled clinical settings, enabling more responsive and personalized healthcare interventions. The following sections provide a detailed examination of mobility drivers, technical frameworks for data collection, and methodological protocols for effective implementation.
Population mobility presents significant challenges for continuous health monitoring and longitudinal research. Children and older adults represent particularly dynamic demographic groups due to distinct life-stage events and dependencies.
Mobility in Older Adults
Research indicates that the transition to the "fourth age" (typically between 80-85 years) is marked by diminished capacity for self-care and increased need for support systems [1]. This life stage, characterized by health deterioration and potential partner loss, often triggers geographic convergence—proximity-enhancing moves between older parents and their adult children [1]. These relocations are structured by:
- Severe health problems leading to parental moves toward children or into institutional care
- Children's gender, with daughters more likely to be caregivers
- Location of other family members, creating clustering effects that reinforce migration patterns [1]
The "Sandwich Generation" Dynamic
Nearly a quarter (23%) of U.S. adults, predominantly Gen Xers in their 40s, belong to the "Sandwich Generation"—simultaneously supporting young children and aging parents [43]. This caregiving dynamic creates complex mobility patterns:
- 54% of adults in their 40s have a living parent age 65+ plus a child under 18 or financially dependent young adult
- Those with higher education (30% with Bachelor's degrees) are more likely to be in this situation
- Geographic separation from native support systems necessitates mobility to provide care [43]
Digital Health Technologies for Data Capture
DHT encompasses tools that monitor health in real-time outside conventional clinical settings, facilitating continuous data collection from mobile populations [44]. These technologies are particularly valuable for capturing data from individuals who cannot easily communicate their experiences or who frequently change locations.
Table 1: Digital Health Technology Categories and Applications
| Technology Category | Specific Examples | Data Capture Capabilities | Population Applications |
|---|---|---|---|
| Wearable Devices | Smart watches, fitness trackers | Step count, heart rate, blood pressure, blood oxygen, ECG, sleep patterns | Older adults with mobility issues, children with chronic conditions |
| Mobile Applications (mHealth) | BetterHelp, patient education apps | Symptom tracking, medication adherence, cognitive behavioral therapy, patient-reported outcomes | Sandwich generation caregivers, managing multiple family health needs |
| Electronic Medical Records (EMRs) | Hospital EMR systems, integrated health networks | Medical history, medications, lab results, immunizations, progress notes | Continuity of care during relocations, provider transitions |
| Telemedicine Platforms | Video consultation, secure messaging | Virtual clinical assessments, remote monitoring, specialist consultations | Rural populations, homebound elderly, reducing travel burden |
These technologies enable collection of real-world data (RWD) during daily activities regardless of location (home, school, workplace), reducing participant burden in clinical trials and improving recruitment and retention rates [44].
Real-World Evidence Frameworks
RWE refers to clinical evidence derived from analyzing RWD regarding the usage and potential benefits or risks of medical products [44]. Unlike data from randomized controlled trials conducted in controlled environments, RWE reflects actual product performance in diverse real-world settings, capturing a wider range of patient experiences and outcomes.
Table 2: Real-World Data Sources and Research Applications
| RWD Source | Data Characteristics | Research Applications | Mobility Considerations |
|---|---|---|---|
| Claims and Billing Data | Healthcare utilization, costs, economic outcomes | Health economics research, treatment pattern analysis | Tracking care continuity across geographic regions |
| Patient Registries | Disease-specific data, long-term outcomes | Comparative effectiveness research, post-market surveillance | Monitoring health outcomes despite location changes |
| Pharmacy Data | Prescription fulfillment, medication adherence | Drug utilization studies, adherence pattern analysis | Identifying lapses in care during transitional periods |
| Social Media and Patient Forums | Patient experiences, side effects, outcomes | Patient perspective analysis, adverse event detection | Capturing experiential data from distributed populations |
The integration of RWE is particularly valuable for understanding how treatments perform across different care settings and geographic locations, providing crucial insights for drug development and regulatory decision-making [44].
Methodological Framework for Dynamic Tracking
Experimental Protocol for Mobility-Integrated Health Research
Objective: To establish a robust methodology for tracking health outcomes in high-mobility populations using DHT and RWE.
Population Recruitment Criteria:
- Older adults (80+ years) with recent health transitions
- Adult children (40-60 years) with caregiving responsibilities for both parents and children
- Children and young adults with frequent residential changes
Data Collection Workflow:
- Baseline Assessment: Comprehensive health evaluation, socioeconomic factors, family structure mapping
- DHT Deployment: Provision of wearable devices and mobile applications based on population needs
- Continuous Monitoring: Passive data collection through DHT, active patient-reported outcomes
- Geographic Tracking: Documentation of location changes, care transitions, and support network modifications
- Data Integration: Synthesis of DHT data with EMR, claims, and registry information
Analysis Framework:
- Multivariate regression models controlling for socioeconomic confounders
- Time-series analysis of health outcomes pre- and post-relocation
- Network analysis of care provision patterns across geographic distances
Research Reagent Solutions
Table 3: Essential Research Materials and Digital Tools
| Research Component | Specific Solution | Function/Application |
|---|---|---|
| Activity Monitoring | Axivity AX3 Accelerometer | Objective measurement of physical activity patterns in free-living environments |
| Geolocation Tracking | GPS-enabled Smartphones | Precise location monitoring with participant privacy safeguards |
| Physiological Monitoring | Empatica E4 Wristband | Continuous capture of heart rate variability, electrodermal activity, and movement |
| Data Integration Platform | REDCap (Research Electronic Data Capture) | Secure web-based application for managing heterogeneous research datasets |
| Biometric Authentication | Duo Mobile two-factor authentication | Secure participant access to digital platforms while maintaining data integrity |
| Continuous Glucose Monitoring | Dexcom G7 CGM System | Real-time glucose monitoring for metabolic studies in ambulatory populations |
Visualization of Research Framework
Dynamic Tracking Workflow
Data Integration Architecture
Analytical Considerations for Mobile Populations
Research involving high-mobility demographics requires specialized methodological approaches to address unique challenges in study design and interpretation.
Quantitative Thresholds for Effective Monitoring
Table 4: Socioeconomic Indicators and Research Implications
| Indicator | Impact on Data Quality | Threshold for Reliability | Research Implications |
|---|---|---|---|
| Total Population | Affects correlation between search volume and health events | >11.08 million urban population | Larger urban size indicates higher accuracy in digital estimation |
| GRP Per Capita | Influences technology adoption and data completeness | >120,700 local currency | Higher economic development supports more robust DHT implementation |
| Education Level | Impacts engagement with digital tools and data quality | >38.13% with high school diploma or higher | Higher education correlates with better protocol adherence |
These thresholds, derived from search-engine-based estimation models, highlight the importance of considering urban socioeconomic indicators when designing studies involving mobile populations [45].
Methodological Protocols for Mobility Events
Protocol 1: Health Impact Assessment of Relocation Events
- Pre-Move Baseline: Comprehensive health assessment 30 days prior to relocation
- Transition Monitoring: Intensive data collection during moving period (7 days before to 14 days after)
- Post-Relocation Adjustment: Extended observation for 90 days to capture stabilization effects
- Control Group: Matched participants without relocation events
Protocol 2: Caregiver Burden Assessment in Sandwich Generation
- Multidimensional Metrics: Financial strain, time allocation, emotional stress, health impacts
- Longitudinal Design: Quarterly assessments over 24-month period
- Dyadic Approach: Parallel data collection from caregiver and care recipient
- Geographic Component: Distance calculations between caregiver and care recipient residences
The convergence of Real-World Evidence and Digital Health Technologies creates unprecedented opportunities for dynamic health tracking in traditionally challenging mobile populations. By implementing the methodological frameworks, technical protocols, and analytical approaches outlined in this guide, researchers and drug development professionals can overcome the historical limitations of studying children and older adults during transitional life stages. This integrated approach enables more responsive, personalized, and effective healthcare interventions that account for the complex reality of human mobility across the lifespan.
Strategies for Enhancing Participant Retention and Data Quality
Adaptive recruitment represents a paradigm shift in clinical trial methodology, leveraging real-time data to optimize patient enrollment strategies. This approach is particularly critical when studying high-mover populations such as children and older adults, whose geographic mobility patterns directly impact trial retention, data completeness, and ultimately, trial validity. This technical guide examines the intersection of dynamic recruitment frameworks and population mobility, providing clinical researchers with methodologies to identify stable subgroups, anticipate relocation triggers, and implement adaptive strategies that maintain statistical power amid participant attrition. We present quantitative models of mobility drivers, Bayesian approaches for subgroup stability prediction, and practical protocols for minimizing missing data in longitudinal studies of geographically unstable populations.
The structural integrity of longitudinal clinical trials is fundamentally threatened by participant attrition, a risk magnified when studying populations with inherent geographic instability. Children and older adults represent two demographically distinct yet similarly mobile groups whose life transitions—including parental relocation, college attendance, health deterioration, and retirement—create substantial methodological challenges for research requiring sustained engagement [1] [46]. Understanding the drivers and patterns of this mobility is not merely a methodological concern but a prerequisite for valid trial design in precision medicine.
Traditional fixed-design trials often fail to account for the dynamic nature of these populations, leading to biased estimates, reduced statistical power, and compromised generalizability. Adaptive recruitment strategies offer a framework for proactively managing these challenges by continuously monitoring participant stability indicators and reallocating resources to subgroups with higher retention potential [47]. This whitepaper establishes the theoretical foundation for why children and older adults exhibit high-mobility characteristics, provides quantitative models for predicting stability, and presents technical protocols for implementing adaptive recruitment within master protocols capable of evaluating multiple subgroups simultaneously.
Quantitative Analysis of Mobility Drivers in High-Risk Populations
Understanding the specific factors that drive mobility in children and older adults provides the predictive foundation for adaptive recruitment strategies. The quantitative data below summarizes evidence-based drivers from longitudinal studies.
Table 1: Primary Mobility Drivers in Older Adult Populations
| Driver Category | Specific Factor | Effect Size | Population Specificity |
|---|---|---|---|
| Health Status | First cardiovascular event | RRR = 1.61 for co-residence [5] | Adults 65+ with no prior CVD history |
| Health Status | Severe health problems | Increased likelihood of moving to institutions [1] | Parents aged 80+ |
| Social Support | Spouseless status | Significantly increased moving probability [5] | Older adults post-health event |
| Social Support | Presence of daughters | RRR = 1.55 for children moving closer [1] [5] | Parents with adult children |
| Socioeconomic | Long-term care insurance | Reduced likelihood of moving closer to children [46] | Adults 69+ with faraway children |
| Residential History | Homeownership | Reduced proximity-moving probability [46] | Seniors in long-term residences |
Table 2: Mobility Patterns in Intergenerational Contexts
| Mobility Pattern | Population | Frequency | Key Triggers |
|---|---|---|---|
| Child moves closer to parent | Adult children | 1.6x more likely than parent moves [46] | Parent health decline, low child income (<$35k) |
| Parent moves closer to child | Older parents | More likely with daughters [1] | Widowhood, severe health problems, living alone |
| Transition to institutional care | Older adults | Increased with severe health issues [1] | Diminished self-care capacity, cognitive decline |
| Geographic convergence | Families | 14% over 4-year period [46] | CV events, functional disability, spousal loss |
The data reveals that health transitions serve as primary mobility catalysts, with cardiovascular events increasing the two-year predicted probability of children and parents moving closer by 61% and 55% respectively [5]. This effect is moderated by social factors—notably, spouseless older adults with daughters demonstrate significantly higher moving probabilities following health events [5]. For researchers, these quantifiable relationships enable predictive modeling of attrition risk based on baseline participant characteristics.
Methodological Framework for Adaptive Recruitment
Bayesian Information Borrowing for Subgroup Stability
Adaptive recruitment in high-mover populations requires sophisticated statistical approaches that balance recruitment efficiency with subgroup retention potential. Bayesian information-borrowing methods provide a flexible framework for leveraging information across multiple subgroups within a master protocol, allowing for dynamic resource allocation based on accumulating data [48].
The fundamental challenge lies in distinguishing between fully exchangeable subgroups (where borrowing strength is statistically appropriate) and partially exchangeable or unique subgroups (where excessive borrowing may mask important differences). Bayesian hierarchical modeling (BHM) addresses this by constructing a multilevel model where subgroup-specific parameters are treated as random samples drawn from a common population distribution, resulting in shrinkage toward a common mean [48]. This approach is particularly valuable when recruiting across diverse geographic regions with varying mobility patterns.
For early-phase trials, Bayesian clustering methods enable identification of subgroups with similar mobility-risk profiles, while Bayesian model averaging (BMA) or selection (BMS) approaches allow researchers to simultaneously evaluate multiple candidate models of mobility drivers [48]. These techniques improve the precision of stability predictions, particularly when historical data on participant mobility exists.
Experimental Protocols for Mobility Risk Assessment
Implementing adaptive recruitment requires standardized assessment protocols for evaluating mobility risk at enrollment and throughout trial participation. The following methodological sequence provides a framework for systematic stability evaluation:
Protocol 1: Baseline Mobility Risk Stratification
- Objective: Categorize enrollment candidates by predicted geographic stability throughout trial duration
- Data Collection: Administer standardized instrument capturing (1) historical residence duration, (2) anticipated life transitions, (3) social support network density, and (4) socioeconomic indicators
- Scoring Algorithm: Apply weighted scoring system where scores >0.67 indicate high stability, 0.33-0.67 moderate stability, and <0.33 high mobility risk
- Validation: Cross-validate with historical mobility data from similar populations where available [46] [5]
Protocol 2: Dynamic Stability Monitoring
- Objective: Detect emerging mobility triggers during trial participation
- Procedure: Implement quarterly trigger assessments evaluating (1) health status changes, (2) caregiver availability modifications, (3) employment transitions, and (4) housing stability
- Technology Integration: Utilize electronic health record data linkages for automatic flagging of hospitalization events or new clinical diagnoses known to precipitate moves [5]
- Response Protocol: Escalate high-risk participants to retention intervention pathway
Protocol 3: Adaptive Site Resource Allocation
- Objective: Dynamically redistribute recruitment targets based on site-level retention performance
- Methodology: Apply Bayesian hierarchical model to borrow information across sites while preserving site-specific effect estimation [48]
- Decision Rules: Pre-specify rules for reducing enrollment at sites with retention rates falling below pre-defined thresholds and reallocating to higher-performing sites
- Timing: Conduct interim assessments at 25%, 50%, and 75% of target enrollment
Technical Implementation: The Scientist's Toolkit
Successfully implementing adaptive recruitment strategies requires specialized methodological tools and analytical approaches. The table below details essential components of the technical infrastructure needed for mobility-informed trial design.
Table 3: Research Reagent Solutions for Adaptive Recruitment
| Tool Category | Specific Solution | Technical Function | Application Context |
|---|---|---|---|
| Statistical Methods | Bayesian Hierarchical Modeling (BHM) | Enables information borrowing across subgroups while accounting for heterogeneity [48] | Master protocols with multiple population subgroups |
| Statistical Methods | Bayesian Model Averaging (BMA) | Averages across multiple candidate models of mobility drivers | Early-phase trials with limited prior data |
| Data Sources | Population Register Data | Provides historical mobility patterns and validation benchmarks [1] | Retrospective mobility risk model development |
| Data Sources | Electronic Health Records (EHR) | Enables real-time detection of health triggers for mobility [49] | Dynamic stability monitoring during trial participation |
| Design Frameworks | Multi-Arm Multi-Stage (MAMS) | Allows for early stopping of recruitment for unstable subgroups [47] | Trials targeting multiple geographic regions |
| Design Frameworks | Response-Adaptive Randomization (RAR) | Adjusts allocation probabilities based to favor stable subgroups [47] | Resource optimization within active trials |
Case Study Implementation: Cardiovascular Event Recovery Trial
To illustrate the practical application of these principles, consider a phase III trial examining functional recovery interventions following first cardiovascular events in adults 65+. This population demonstrates particularly high mobility risk following health shocks, with documented relocation probabilities increasing significantly post-event [5].
Adaptive Recruitment Strategy:
- Pre-screening: Identify candidates with recent MI, stroke, or CHF without prior CVD history
- Stability scoring: Apply weighted algorithm incorporating marital status, child proximity, gender of nearest child, and homeownership status
- Stratified enrollment: Oversample participants with stability scores >0.67 while maintaining minimum enrollment from high-risk subgroups for generalizability
- Dynamic monitoring: Implement monthly health status reviews with automatic triggers for new disability diagnoses
- Site performance: Reallocate enrollment targets quarterly based on site-specific retention metrics
Implementation Framework: The trial employs a Bayesian hierarchical model to borrow information across clinical sites regarding the relationship between participant characteristics and study completion. This approach allows sites with smaller enrollment to benefit from stability patterns observed in larger sites while maintaining ability to detect site-specific effects [48]. Response-adaptive randomization further optimizes resource allocation by increasing enrollment probabilities for demographic subgroups demonstrating higher retention rates after interim analyses.
Retention Safeguards: For participants identified as high mobility risk, the protocol implements preemptive retention strategies including telehealth options, flexible visit windows around anticipated transitions, and engagement of family members in visit planning. These measures reduce missing data from geographic moves without compromising protocol adherence.
Adaptive recruitment represents a methodological imperative for clinical research involving children and older adults—populations whose life course transitions create inherent geographic instability. By integrating quantitative mobility predictors, Bayesian statistical methods, and dynamic resource allocation, researchers can preemptively address attrition threats that compromise trial validity. The technical frameworks presented in this whitepaper provide actionable roadmaps for implementing these approaches across therapeutic areas, ultimately strengthening the evidence base for precision medicine interventions in high-mover populations. As the clinical research paradigm shifts toward more flexible, efficient designs, adaptive recruitment strategies will play an increasingly vital role in generating reliable evidence for vulnerable populations most in need of novel therapeutics.
Developing Flexible and Remote Follow-Up Protocols
The development of effective clinical follow-up protocols is fundamentally challenged by the unique characteristics of high-mover populations—groups experiencing frequent geographical or care-setting transitions. Children and older adults represent two such populations where traditional in-person clinical monitoring often proves inadequate. Research indicates that nearly 70-90% of older adults experience some degree of dysphagia (swallowing difficulties), while as many as 25-45% of typically developing children and up to 80% of those with developmental disabilities exhibit feeding disorders that complicate medication administration [50]. These physiological challenges, combined with frequent transitions between home, school, hospital, and care facilities, render these populations particularly difficult to monitor through conventional clinical visits.
The concept of "high-mover" status extends beyond mere geographical mobility to encompass transitions across developmental stages, care environments, and health statuses. Children progress through rapidly evolving physiological and cognitive developmental stages, while older adults often navigate complex care transitions and deteriorating physiological conditions. These dynamics create significant barriers to consistent medication adherence and treatment monitoring, with studies showing that polypharmacy (concurrently taking more than five medications) has high prevalence among older adults, creating additional compliance challenges [50]. This whitepaper establishes a technical framework for developing flexible remote follow-up protocols that address these unique mobility challenges while maintaining scientific rigor in data collection.
Quantitative Foundations: Comparative Analysis of Pediatric and Geriatric Challenges
Table 1: Patient-Centered Factors Affecting Clinical Protocol Acceptability
| Factor | Pediatric Population | Geriatric Population |
|---|---|---|
| Age Ranges | 0-18 years; subdivided by developmental stage [50] | >65 years; frailty often more significant than chronological age [50] |
| Health Conditions | Single conditions more common than comorbidities [50] | Multi-morbidities common; highly prevalent diseases affect medication handling [50] |
| Swallowing Ability | Developing swallow function; maturation generally complete by 6 years [50] | Dysphagia affects 70-90% of population; age-related neuromuscular decline [50] |
| Therapy Duration | Both acute and long-term treatments required [50] | Long-term treatments common; acceptability affected by treatment outcomes [50] |
| Medication Burden | Single medications more common due to acute illness prevalence [50] | Polypharmacy highly prevalent; affects dosage form preference [50] |
| Administration Responsibility | Usually assisted by caregivers [50] | Mixed: independent living vs. caregiver-assisted [50] |
| Administration Environments | Home, nursery, school, hospital [50] | Home, residential home, nursing home, hospital [50] |
Table 2: Key Elements of Remote Follow-Up Protocols for High-Mover Populations
| Protocol Element | Technical Requirements | Pediatric Adaptations | Geriatric Adaptations |
|---|---|---|---|
| Communication Framework | Defined tools, protocols, and response times [51] | Age-appropriate communication methods; parental interfaces | Accommodating for visual, hearing, or cognitive impairments |
| Performance Metrics | SMART goals; outcome-based tracking [51] | Developmental milestone integration | Functional status assessments; frailty measures |
| Data Collection Technology | Secure platforms; multi-factor authentication [51] | Taste-masked formulations; mini-tablets [52] | Dysphagia-adapted formulations; compliance packaging |
| Flexibility Structure | 4-6 overlapping core hours with adjustable schedules [51] | School and activity schedule integration | Medical appointment coordination; caregiver availability |
| Compliance Monitoring | Quantitative observation methods [53] | Play-based engagement; caregiver reporting | Simplified interfaces; automated reminders |
Remote Monitoring Methodologies: Technical Protocols for High-Mover Populations
Quantitative Observation Framework for Remote Data Collection
Remote follow-up protocols require rigorous quantitative observation methods to ensure data reliability across diverse environments. Quantitative observation constitutes a research method involving the collection and analysis of numerical data about people, objects, or events, measuring specific variables such as frequency, duration, or intensity [53]. This approach provides objective, reliable data that can be analyzed statistically, allowing for precise measurement and comparison of variables across populations and settings [53].
The technical implementation involves:
Standardized Metric Development: Create consistent measurement protocols for physiological parameters, behavioral observations, and adherence metrics that remain valid across different environments where children and older adults receive care.
Technology-Assisted Data Capture: Implement secure digital platforms that facilitate real-time data collection while maintaining compliance with healthcare privacy regulations. These systems must accommodate varying levels of technical proficiency among patients and caregivers.
Multi-Source Data Integration: Establish protocols for combining patient-reported outcomes, caregiver observations, and automated sensor data to create comprehensive assessment pictures despite environmental transitions.
Experimental Protocol for Medication Adherence Monitoring
Table 3: Research Reagent Solutions for Adherence Monitoring
| Research Tool | Technical Specification | Application Function |
|---|---|---|
| Electronic Monitoring Caps | Embedded sensors recording opening events | Objective adherence measurement without direct observation |
| Taste-Masking Excipients | Child-safe flavor compounds | Improve palatability and acceptance of pediatric formulations [52] |
| Orodispersible Tablets | Fast-dissolving polymer matrices | Avoid swallowing difficulties in both populations [52] |
| Multi-Compartment Adherence Aids | Time-organized medication containers | Support complex medication regimens in older adults [50] |
| Biorelevant Dissolution Media | Simulated pediatric and geriatric GI fluids | Predict oral dosage form performance in specific populations [52] |
Experimental Objective: To evaluate the effectiveness of a remote monitoring protocol in improving medication adherence among high-mover pediatric and geriatric populations.
Methodology:
- Participant Stratification: Recruit matched cohorts of pediatric (n=150) and geriatric (n=150) participants with documented high mobility patterns across care settings.
- Intervention Protocol: Implement a comprehensive remote monitoring system incorporating:
- Electronic adherence monitoring technology
- Automated reminder systems tailored to population-specific needs
- Video conferencing for virtual follow-ups scheduled during core overlapping hours [51]
- Secure digital platforms for caregiver and provider communication
- Data Collection Points: Establish standardized intervals for quantitative data collection including:
- Adherence rates (primary outcome)
- Treatment-related morbidity
- Quality of life measures
- Healthcare utilization
- Participant and caregiver satisfaction
- Analysis Framework: Employ statistical methods including t-tests for group mean comparisons and regression analysis to evaluate predictive relationships between remote monitoring elements and adherence outcomes [54].
Implementation Framework: Technological and Protocol Considerations
Digital Infrastructure Requirements
Effective remote follow-up protocols require robust technological infrastructure that addresses the unique needs of high-mover populations. Implementation should include:
Communication Tools: Defined platforms for messaging, video calls, and file sharing with established response time expectations (e.g., 2-4 hours during work hours) [51]. Platforms must comply with healthcare data security standards while remaining accessible to populations with varying technical abilities.
Data Security Measures: Multi-factor authentication, VPN protection, and endpoint security on all devices handling patient information [51]. These measures are particularly crucial when monitoring occurs across multiple insecure environments such as schools, public spaces, or various care facilities.
Interoperability Standards: Systems capable of integrating with electronic health records, pharmacy databases, and caregiver communication platforms to create seamless information flow despite patient mobility.
Adaptive Protocol Design
Remote follow-up protocols must incorporate structured flexibility to accommodate the dynamic nature of high-mover populations:
Core Flexibility Model: Implement 4-6 overlapping core hours for collaborative care coordination while allowing adjustable schedules to accommodate appointments, school activities, and varying care routines [51].
Stratified Communication Hierarchy: Establish clear guidelines for communication urgency levels, using instant messaging for urgent matters while relying on asynchronous tools for routine updates [51].
Environment-Specific Assessment Tools: Develop validated evaluation instruments that maintain reliability across different settings where assessments may occur, accounting for environmental variables that may influence results.
Diagram 1: Remote Protocol Architecture for High-Mover Populations
The development of flexible remote follow-up protocols represents a methodological imperative for researching high-mover populations such as children and older adults. By implementing structured yet adaptable frameworks that incorporate quantitative observation methods, robust technological infrastructure, and population-specific accommodations, researchers can overcome traditional barriers to studying these clinically challenging populations. The technical guidelines presented in this whitepaper provide a foundation for generating reliable, generalizable evidence regarding therapeutic interventions across the human lifespan, ultimately advancing the science of pediatric and geriatric pharmacotherapy and improving clinical outcomes for these vulnerable populations.
Future protocol innovations should focus on advancing real-time data analytics, developing more sophisticated adherence monitoring technologies, and creating even more adaptable assessment frameworks that maintain scientific rigor while accommodating the inherent mobility of these populations across diverse care environments and developmental trajectories.
The study of population mobility reveals that children and older adults represent distinctly significant, yet often overlooked, high-mover demographic groups. Research indicates that older adults' residential mobility is frequently driven by transitions in health status and care needs, particularly as they enter the "fourth age" (typically between 80-85 years) marked by diminished capacity for self-care and increased dependency [1]. This life stage, characterized by multiple chronic disabilities and degenerative illnesses, creates compelling needs for geographic convergence with potential caregivers, primarily adult children [1]. Simultaneously, highly mobile artisanal and small-scale gold mining (ASGM) populations demonstrate another facet of population mobility, with individuals typically spending 2-3 months in mining camps with temporary stays at logistical sites for supplies, medical care, and family visits [55]. Understanding these patterns is crucial for developing effective community-engaged research and intervention strategies that address the unique challenges of maintaining trust and continuity with transient populations.
The theoretical framework for understanding older adult mobility is partially explained by Lin and Rogerson's three-stage developmental model of intergenerational proximity and life-cycle mobility, where the final stage involves "geographic convergence" in response to parents' increasing need for healthcare, sometimes compounded by partner loss [1]. Similarly, Litwak and Longino's classic model describes later-life mobility where older parents move to the vicinity of adult children as potential caregivers or to residential care facilities [1]. These theoretical constructs help explain why health declines trigger residential adjustments that fundamentally alter family geographic configurations.
Theoretical Foundations of Trust-Building in Mobile Communities
Core Principles of Community-Engaged Research
Building trust within mobile populations requires a fundamental shift from traditional research paradigms to community-engaged research (CEnR) approaches. Whereas traditional models position investigators as sole decision-makers who recruit "subjects," CEnR recognizes community members as active partners who co-identify needs, co-design methods, share decisions, and help interpret and disseminate results [56]. This transition represents both an ethical imperative and a practical strategy that improves research quality, relevance, and real-world impact.
Trust operates as a measurable construct that predicts behavior in community-engaged research. Validated instruments like the Perceptions of Research Trustworthiness Scale clarify specific dimensions driving trust, including honesty, respect, fairness, and competence [56]. Research demonstrates that trust grows when communities see their priorities shape decisions, when benefits flow back locally, and when partners are compensated and credited for their expertise. During the COVID-19 pandemic, for instance, community advisory mechanisms embedded in community health centers strengthened equitable access to testing and services for populations facing disparities, demonstrating that trust translates directly into improved outcomes through broader reach and faster uptake of evidence-based resources [56].
The Trust-Building Continuum in Mobile Populations
Community engagement is conceptualized as a continuum of participation, ranging from minimal involvement to substantive collaboration [55]. This spectrum typically includes phases of informing, consulting, collaborating, participating, and community leadership. For mobile populations like the ASGM communities, this continuum acknowledges the dynamic nature of engagement, adaptable to different circumstances and settings [55]. The community-based model sits at the foundation of this continuum and relies on collaborative approaches with non-academic partners in creating knowledge to understand social and cultural dynamics, integrating this knowledge with action to improve health outcomes.
Table 1: Core Principles of Ethical Community Engagement in Research with Mobile Populations
| Principle | Key Components | Application to Mobile Populations |
|---|---|---|
| Shared Governance | Clear roles, timely feedback loops, transparent decision rights, fair compensation, facilitated diverse voices | Establish community advisory boards with real influence over protocols; formalize through memoranda of collaboration |
| Equity by Design | Teams reflecting community demographics; accessible data sharing; co-created consent materials; mutual benefit | Ensure materials accommodate literacy levels and language preferences (e.g., Brazilian Portuguese for ASGM communities) |
| Accountability Through Evaluation | Monitor partnership quality; track perceived respect, influence, capacity gains, sustained collaboration | Use simple tools to monitor trust over time; adjust engagement strategies based on community feedback |
| Capacity Building | Training for both researchers and community partners; shadowing opportunities; joint ethics training | Provide research ethics training for community partners; cultural competency training for researchers |
| Sustainability Planning | Identify what remains after funding ends; standing advisory groups; community-owned data assets | Plan for continuity to counter "helicopter research" patterns that erode trust in transient communities |
Methodological Framework: Community-Based Models for Engagement
Community-Based Intervention Design
The Curema project, implemented among mobile ASGM populations in the Guiana Shield region, exemplifies an effective community-based model for engaging hard-to-reach populations [55]. This project employs several crucial design elements that enable successful engagement with transient groups. The multi-actor partnership approach brings together diverse stakeholders to address complex health challenges like malaria elimination. This is complemented by structured pre-post intervention studies and monitoring systems that track engagement and outcomes. Perhaps most critically, the model emphasizes strategic site selection, establishing seven bases in logistical sites serving the ASGM community along border areas rather than attempting direct entry to gold mining sites [55]. These neutral spaces allow community members to be approached without the risk of police pursuit linked to their activities or migratory status, creating essential psychological safety for engagement.
The recruitment and involvement of community members as field workers represents another cornerstone of this approach, leveraging existing social networks and cultural knowledge to build bridges between researchers and the community [55]. This is supported by participatory development of Information, Education, and Communication (IEC) strategies created through iterative and collaborative consultative processes. The entire model rests on a foundation of ongoing trust-building through site visits that demonstrate commitment and presence, essential elements for working with populations often characterized by suspicion toward external authorities [55].
Experimental Protocols for Community Engagement
Implementing successful community engagement with mobile populations requires structured methodological approaches with clearly defined protocols:
Protocol 1: Establishing Community Advisory Structures
- Begin with mapping existing community leadership and decision-making networks
- Recruit advisory board members who represent diverse sub-groups within the mobile population
- Formalize roles, compensation, and decision rights through memoranda of collaboration
- Establish regular meeting schedules with transparent reporting mechanisms
- Integrate advisory boards into governance structures with genuine influence over protocol decisions, recruitment materials, and return-of-results plans [56]
Protocol 2: Participatory Development of Culturally-Sensitive Materials
- Conduct initial listening sessions to understand community priorities and communication preferences
- Convene co-design workshops with community representatives to draft initial materials
- Iteratively refine materials through focus groups and cognitive testing
- Produce final versions in appropriate languages and literacy levels (e.g., Brazilian Portuguese for ASGM communities) [55]
- Train community members to deliver educational content using these materials
Protocol 3: Trust and Partnership Monitoring
- Administer validated trust measures like the Perceptions of Research Trustworthiness Scale at baseline [56]
- Track partnership quality indicators (perceived respect, influence on decisions, clarity of roles) at regular intervals
- Conduct periodic qualitative assessments through structured interviews or focus groups
- Use collected data to make real-time adjustments to engagement strategies
- Share monitoring results with community partners through accessible formats
The following workflow diagram illustrates the iterative process of engaging mobile populations, from initial contact through sustainable partnership:
Data Management and Analysis in Mobile Population Research
Quantitative Data Management Framework
Research with mobile populations generates complex quantitative data requiring careful management and analysis. The fundamentals of data management begin with meticulous checking for errors and missing values upon entry into datasets [57]. Variables must then be clearly defined and coded systematically as part of comprehensive data management protocols. For research involving mobile populations like older adults or ASGM communities, this often involves creating specialized coding frameworks to capture mobility patterns, temporary residences, and multiple contact points that characterize transient groups.
The analysis of quantitative data in mobile population research typically employs both descriptive and inferential statistics. Descriptive statistics summarize variables in a dataset to show what is typical for a sample, including measures of central tendency (mean, median, mode), measures of spread (standard deviation), and parameter estimation measures (confidence intervals) [57]. Inferential statistics help test hypotheses about whether a hypothesized effect, relationship, or difference is likely true, producing P values that must be accompanied by measures of magnitude (effect sizes) to interpret how small or large the effect, relationship, or difference appears [57]. For research with mobile populations, these analytical approaches must often account for clustered data patterns and repeated measures due to the transient nature of these groups.
Effective Data Presentation Strategies
Clear data presentation is essential for conveying findings about mobile populations to diverse audiences. Tables represent a crucial component of research papers, providing richer insight into study participants and main research findings than text alone can deliver [58]. Effective tables should be designed with clear headings for rows and columns and careful consideration of format, typically featuring more rows than columns since reading down a table is generally easier than reading across it [58].
Table 2: Mobility Triggers and Family Responses in Older Adult Populations
| Mobility Trigger | Population Characteristics | Likelihood of Move | Direction of Move | Key Influencing Factors |
|---|---|---|---|---|
| First Cardiovascular Event | Adults 55+ with no prior CVD history | 61% increased probability of children moving closer [5] | Children move toward parents | Spouseless status; having a daughter |
| Severe Health Problems | Parents aged 80+ with severe health issues | Increased likelihood of parent relocations | Parents move toward children or institutions | Daughter proximity; sibling clustering |
| Transition to "Fourth Age" | Adults 80-85+ with diminished self-care capacity | High probability of residential adjustment | Toward children or care facilities | Gender differences in health conditions |
| Stroke Diagnosis | Older adults with new stroke diagnosis | Higher than MI or CHF | Both directions | Severe long-term disability requiring care |
| Myocardial Infarction | Older adults with heart attack | Less significant than stroke | Variable | Potential for return to function after rehab |
Table presentation guidelines recommend that titles should enable readers to understand content without reference to the rest of the article, including information on study, time, and place [58]. Footnotes should be used judiciously to explain abbreviations or symbols or to list confounding factors for which adjustment has been made in the analysis. For research with mobile populations, tables often need to capture complex mobility patterns, multiple time points, and various residential arrangements that characterize these groups.
Case Study: The Curema Project with ASGM Populations
Intervention Design and Implementation
The Curema project represents an exemplary community-based intervention targeting malaria elimination among highly mobile ASGM populations in the Guiana Shield region [55]. This project addresses the emergence of Plasmodium vivax as a dominant malaria strain (approximately 80% in the region), which poses particular challenges due to P. vivax hypnozoites causing relapses that require specific treatment regimens for radical cure [55]. The project combines three coordinated actions: targeted drug administration (TDA) against P. vivax; Malakit delivery and user training with improved education tools; and comprehensive health education activities to eliminate malaria.
The targeted drug administration component involves providing full P. vivax treatment to adult asymptomatic individuals suspected of carrying P. vivax hypnozoites, based on specific eligibility criteria related to the participant's medical history [55]. To ensure safety, prior Glucose-6-Phosphate Dehydrogenase (G6PD) deficiency screening and pregnancy tests are performed, along with questions about previous adverse drug reactions and other clinical data. A commitment to a 14-day follow-up is mandatory through either in-person visits, phone calls, or a mobile application, demonstrating adaptive strategies for maintaining connection with a highly mobile population [55].
Engagement Strategies for Hard-to-Reach Populations
The Curema project's engagement approach specifically addresses the challenges of working with mobile, often hidden populations. The project focuses interventions on strategically located logistical sites rather than attempting to access remote and often illegal mining sites directly [55]. These neutral spaces include three cities (Oiapoque, Albina, Paramaribo) and four informal inland settlements (Ilha Bela, Ampoema, Ronaldo, Yawpassi) where community members can be approached without immediate risk of police pursuit related to their activities or migratory status.
The project recognizes that the ASGM community, while appearing as a single entity from external perspectives, actually consists of multiple sub-groups or distinct communities of identity [55]. In French Guiana, over 95% of individuals working in mining sites are of Brazilian origin, with Brazilian Portuguese serving as the predominant common language despite diverse origins existing within the population [55]. Women constitute 15-30% of the ASGM population, primarily working in the mining services sector. This nuanced understanding of community composition enables more targeted and effective engagement strategies.
Table 3: Research Reagent Solutions for Community-Based Studies with Mobile Populations
| Research Tool | Primary Function | Application in Mobile Populations |
|---|---|---|
| Perceptions of Research Trustworthiness Scale | Measures specific dimensions driving trust (honesty, respect, fairness, competence) | Track trust over time; identify gaps; align engagement strategies with community values [56] |
| Community Advisory Boards | Shared governance; community input into research design and implementation | Ensure research addresses community priorities; improve cultural appropriateness of methods [56] |
| Memorandum of Collaboration | Formalizes roles, rights, compensation, and decision rights | Establishes clear expectations between researchers and community partners; prevents exploitation [56] |
| Malakit Distribution | Self-test and self-treatment kits for malaria with user training | Enables healthcare access for remote populations with limited formal healthcare access [55] |
| Targeted Drug Administration | Provides full P. vivax treatment to asymptomatic individuals | Addresses specific health needs (malaria hypnozoites) in hard-to-reach populations [55] |
| Information, Education, Communication Materials | Culturally-sensitive educational tools developed through collaborative processes | Ensure health messages are understood and adopted across literacy levels and languages [55] |
Implementation Tools and Visualizations
Strategic Engagement Workflow
The following diagram illustrates the strategic decision-making process for engaging mobile populations based on community characteristics and mobility patterns:
Best Practices Checklist for Researchers
Based on successful engagement models with both older adult and ASGM mobile populations, researchers should implement the following best practices:
- Co-define problems and success metrics beginning with listening sessions that capture community priorities and lived realities
- Establish community advisory structures with genuine authority rather than token representation, ensuring they are resourced, compensated, and integrated into governance
- Codify roles, rights, and compensation through memoranda of collaboration that specify decision rights, conflict resolution processes, and credit sharing
- Share data early and in accessible formats by returning interim findings to partners on a schedule they help define, using dashboards or plain-language briefs
- Measure trust and partnership quality systematically using simple tools to monitor trust over time and identify which engagement actions matter most
- Invest in shared capacity building through training for both researchers and community partners on research ethics, methods, and cultural context
- Plan for sustainability from the outset by identifying what can remain after funding ends, such as standing advisory groups or community-owned data assets [56]
Understanding the distinct mobility patterns of children and older adults provides crucial insights for developing effective community-engaged approaches with these populations. Research demonstrates that older adults' mobility is primarily health-driven, with cardiovascular events increasing the two-year predicted probability of children and parents moving closer together by 61% and 55% respectively [5]. These moves are particularly likely when the older person experiencing the health event is spouseless or has a daughter, reflecting gendered caregiving patterns well-established in the literature [1]. Simultaneously, the mobility patterns of populations like the ASGM communities are driven by economic necessity and characterized by circular migration between mining sites and logistical settlements [55].
Building trust with these diverse mobile populations requires adapting engagement strategies to their specific circumstances, constraints, and communication preferences. For older adults, this may involve accommodating physical and cognitive limitations, while for ASGM populations it requires acknowledging legal vulnerabilities and migration patterns. In both cases, the fundamental principles of community-engaged research apply: beginning with community-identified priorities, sharing power and resources equitably, building capacity on all sides, and committing to sustained partnerships that extend beyond individual research projects. By implementing these evidence-based approaches, researchers can develop more effective, ethical, and sustainable interventions that truly meet the needs of mobile populations while advancing scientific understanding of mobility patterns and their implications for health and well-being.
Data Linkage and Integration Techniques to Compensate for Mobility Gaps
Understanding human mobility is fundamental to societal research, influencing urban planning, public health, and economic development [59]. Within this domain, the mobility patterns of two demographic groups—children and older adults—present unique challenges and necessitate specialized research approaches. These groups exhibit distinct mobility characteristics shaped by biological, social, and environmental constraints, making them "high-mover" populations in specific contexts. For older adults, mobility is not merely a functional requirement but a crucial component of well-being, enabling social participation and access to essential services [60]. However, aging often brings functional declines and increased dependency on both informal networks (like family) and formal care systems, which profoundly shapes their mobility geographies [61]. Similarly, childhood mobility, often involuntary due to family decisions, can have long-term consequences; research indicates that frequent residential moves during childhood are associated with poorer mental and physical health outcomes in later life [62].
Studying these populations is complicated by significant mobility gaps—discrepancies between potential, desired, and actual movement. Traditional single-method approaches, such as surveys or GPS tracking alone, often fail to capture the full complexity of these mobility patterns. For instance, GPS data might reveal where and when movement occurs, but cannot explain the why—the motivations, constraints, and perceptions behind travel choices [60]. This paper provides an in-depth technical guide to data linkage and integration techniques designed to compensate for these mobility gaps, offering researchers robust methodologies for generating a more holistic understanding of movement in vulnerable populations.
Understanding Mobility Gaps in High-Mover Populations
The Nature and Causes of Mobility Gaps
Mobility gaps refer to the disparities and limitations in the movement patterns of a population. For children and older adults, these gaps arise from a constellation of factors:
- Physical and Developmental Constraints: Older adults experience functional declines that impose capacity constraints on daily travel behaviors [63]. Children's mobility is largely dictated by their developmental stage and parental supervision.
- Social and Care Networks: The mobility of older adults is heavily influenced by their social networks. The provision of informal care is facilitated by geographic proximity, often triggering relocations (e.g., moving closer to adult children) when health deteriorates [1] [61].
- Economic and Environmental Factors: High costs of living can force "boomerang" moves, where adult children return to their parents' homes, altering the mobility patterns of both generations [64]. Urban-rural differences also play a significant role; older adults in urban areas spend more time on leisure trips, while those in rural areas may face isolation due to reduced transportation resources [63].
Consequences of Unaddressed Mobility Gaps
Failure to adequately measure and understand these gaps has real-world implications. For older adults, it can lead to social isolation, reduced access to healthcare, and diminished quality of life [61]. For children, frequent, involuntary moves are linked to long-term negative health outcomes [62]. From a research perspective, relying on a single data source can lead to biased or incomplete findings. For example, one study found that self-reported travel diaries and GPS-tracked data often revealed different mobility geographies for the same individual, highlighting the critical need for methodological integration [60].
A comprehensive mobility study begins with a careful selection of data sources. Each source possesses unique strengths and weaknesses, making it suitable for capturing different facets of mobility. The following table summarizes the key data sources available to researchers.
Table 1: Key Data Sources for Human Mobility Research
| Data Source | Key Characteristics | Strengths | Limitations |
|---|---|---|---|
| Census & Surveys [59] | Traditional, government-collected data on population characteristics and travel. | High population coverage; includes trip purpose; reliable for long-term trends. | Infrequent collection (5-10 years); high cost; cannot capture real-time dynamics. |
| Call Detail Records (CDRs) [59] | Passively collected mobile phone data from service providers. | High temporal frequency; large sample sizes; reveals broad movement patterns. | Spatially coarse (tower-dependent); demographic biases (under-represents children/elderly); privacy concerns. |
| Time-Use Diaries [65] [63] | Self-reported diaries of daily activities and travel. | High activity context; accurate time expenditure; low participant barriers. | Relies on memory and participant diligence; can be burdensome. |
| GPS Tracking [60] | High-precision, passive location tracking via GPS devices. | High spatial and temporal accuracy; objective movement paths. | Does not capture motivation; battery life; privacy issues; data volume complexity. |
| Qualitative Interviews [60] | In-depth, open-ended interviews about mobility experiences. | Reveals perceptions, motivations, and lived experiences. | Small sample sizes; not generalizable; time-intensive to collect and analyze. |
Core Integration Techniques and Methodological Approaches
To overcome the limitations of individual data sources, researchers employ a variety of linkage and integration techniques. The choice of method depends on the research question and the types of gaps being addressed.
The Mixed-Methods Triangulation Approach
This approach combines quantitative and qualitative data to not only validate findings but also to provide complementary layers of understanding. A seminal study by Meijering and Weitkamp (2016) demonstrates a robust protocol for this integration [60].
Table 2: Mixed-Methods Protocol for Mobility Research
| Method | Implementation | Role in Integration |
|---|---|---|
| GPS Tracking | Participants wear GPS devices for a defined period (e.g., 7 days) to record precise movement paths. | Provides objective, high-resolution data on revealed mobility (actual movements). |
| Travel Diaries | Participants concurrently fill out diaries, noting trip purposes, transportation modes, and companions. | Adds context to GPS data; explains the purpose and mode of travel that GPS cannot. |
| In-depth Interviews | Post-tracking interviews explore participants' perceptions of their mobility, satisfaction, and constraints. | Explains the reasoning and experience behind the patterns observed in the GPS and diary data. |
Workflow Diagram: The following diagram visualizes the sequential and integrative nature of this mixed-methods approach.
This integration proved powerful in a study of older Dutch adults, revealing discrepancies between self-reported and GPS-measured mobility and providing deep insight into how social schedules and personal motivations shape daily movement [60].
Data Linkage for Life-Course Analysis
Understanding the long-term impact of mobility, such as how childhood moves affect health in old age, requires linking data across the life course. The REGARDS study provides a exemplary model [62].
Experimental Protocol:
- Data Collection: A large cohort of older adults is recruited. Baseline data includes current health metrics (e.g., SF-12 for mental and physical health) and a detailed "Places You Have Lived" questionnaire, which retrospectively collects residential history from birth.
- Supplementary Data: A follow-up mailed questionnaire collects data on childhood socioeconomic status (e.g., mother's education), adverse childhood experiences (ACEs), and childhood social support.
- Data Linkage and Analysis: Researchers create a linked dataset for each participant, connecting:
- The exposure variable (number of childhood moves from the residential history).
- The outcome variable (current physical and mental health scores).
- Covariates and moderators (demographics, childhood SES, ACEs, social support).
- Statistical Modeling: Linear regression models are used to test the association between childhood moves and older adult health, while interaction terms assess how this relationship is modified by factors like race and childhood adversity.
This linked-data approach allowed researchers to discover that the negative health effects of frequent childhood moves were worse for Black individuals and those with low childhood SES [62].
Geospatial Integration of Activity Spaces
This technique involves linking individual mobility data with geospatial information systems (GIS) to understand how the built environment influences movement. Research on older adults' daily mobility across ten countries effectively used this method [63].
Methodology:
- Mobility Data Extraction: Time-use diaries from the Multinational Time Use Study (MTUS) were used to extract the time spent by non-working older adults on non-work trips (leisure and housework), including the mode of transport.
- Geospatial Context: The MTUS data provided the crucial variable of whether the respondent lived in an urban or rural area.
- Integrated Analysis: Researchers analyzed the relationship between urbanity and mobility patterns, controlling for sociodemographic factors. This integration revealed that urban older adults spent significantly more time on leisure trips than their rural counterparts, a finding critical for urban planning and public health policy [63].
The Researcher's Toolkit: Essential Reagents and Materials
Successful data linkage requires a suite of conceptual and technical tools. The following table details key "research reagents" for designing a mobility study.
Table 3: Essential Research Reagents for Mobility Studies
| Tool / Reagent | Function in Research | Application Notes |
|---|---|---|
| Harmonized Time-Use Diaries [63] | Standardized instrument for collecting self-reported activity and travel data across populations. | Gold standard for behavioral data; reduces barriers for older adult participation [65]. Must be carefully designed for the target population (e.g., simple language for children). |
| GPS Data Logger | Hardware for passively collecting high-fidelity location data. | Prefer devices with long battery life and simple operation to minimize participant burden. Smartphone apps can be a viable alternative. |
| GIS (Geographic Information System) | Software platform for visualizing, managing, and analyzing spatial data. | Used to link mobility paths (from GPS/diaries) with map data (land use, transport networks) to define "activity spaces." |
| Validated Health & Well-being Scales | Standardized questionnaires to measure outcomes of interest (e.g., SF-12 [62]). | Allows for the linkage of mobility patterns to health outcomes. Crucial for establishing the impact of mobility gaps. |
| Interview & Coding Protocols [60] | Structured guides for conducting and analyzing qualitative interviews. | Ensures consistency in qualitative data collection. Thematic analysis is typically used to code transcripts and identify key themes. |
Compensating for mobility gaps in the study of children and older adults is a complex but achievable goal. As this guide outlines, no single data source is sufficient. A strategic combination of methods—linking the objective precision of GPS with the contextual richness of diaries, the explanatory power of interviews, and the macro-perspective of census data—is essential. The techniques of mixed-methods triangulation, life-course data linkage, and geospatial integration provide a robust framework for generating a multi-layered, nuanced understanding of why and how these populations move. By adopting these integrated approaches, researchers, public health professionals, and policymakers can develop more effective, evidence-based strategies to support mobility, thereby enhancing health, well-being, and social participation across the entire lifespan.
Comparative Analysis and Validation of Mobility-Associated Outcomes
The frequent relocation of pediatric and geriatric populations represents a significant area of study within public health and life course epidemiology. While both groups exhibit high rates of mobility, the underlying triggers, consequences, and research approaches differ substantially. For older adults, mobility often refers to physical movement capacity, the decline of which is a key hallmark of functional aging with strong prognostic value for disability and survival [66]. Conversely, for children, mobility typically refers to residential relocation, which can disrupt social networks and environmental stability during critical developmental periods [62] [67]. This whitepaper provides a comparative analysis of mobility triggers across these populations, examining distinct methodological approaches for studying mobility-related outcomes and their implications for health research and intervention development.
Understanding why these groups are high-mover populations requires a life course perspective. The roots of mobility loss in late life can only be understood in the context of life course epidemiology, which studies long-term biological, behavioral, and psychosocial processes linking adult health and disease risk to physical or social exposures acting during gestation, childhood, adolescence, or earlier adult life [66]. Similarly, childhood residential mobility has demonstrated long-term health implications extending into older adulthood [62]. This analysis frames mobility triggers within this broader context to inform targeted research and intervention strategies.
Pediatric Mobility Triggers and Consequences
Primary Triggers of Residential Mobility
Childhood residential mobility is predominantly driven by external socioeconomic factors and family dynamics rather than individual choice. Housing instability represents a central trigger, with rent-burdened households (those spending over 30% of income on housing) at higher risk for eviction and subsequent relocation [62]. Family structure changes, including parental separation, divorce, or remarriage, frequently necessitate residential moves [62]. Employment-related factors, such as parental job loss or new employment opportunities, account for approximately 21% of moves [62]. Additionally, economic precarity and social instability often create circumstances where moves are not fully voluntary, particularly for low-income families [62].
Health Consequences and Modifying Factors
Frequent childhood moves are associated with negative long-term health outcomes, with effects potentially persisting into older adulthood. Meta-analytic data reveals the association between moving and health is more often negative than positive, with moving most strongly associated with externalizing problem behaviors [68]. Research from the REGARDS study shows that each additional childhood move predicts poorer mental health component scores (β = -0.10, SE = 0.05, p = 0.03) and physical health component scores (β = -0.25, SE = 0.06, p < 0.0001) in older adulthood [62].
Critical moderating factors influence the strength of these associations. The age during moving appears significant, with moves during ages 10-18 having particularly lasting effects into adulthood [68]. The frequency of moves demonstrates a dose-response relationship, where impact increases with each additional move [68]. Racial and socioeconomic disparities are evident, with Black individuals, those with low childhood socioeconomic status, and those experiencing high adverse childhood experiences showing synergistic negative effects on older adult health [62]. Individual differences in personality also moderate outcomes, with introverted or neurotic children experiencing poorer well-being outcomes after frequent moves compared to extraverted children [67].
Table 1: Health Outcomes Associated with Childhood Residential Mobility
| Outcome Domain | Short-Term Effects | Long-Term Effects (into Adulthood) |
|---|---|---|
| Mental Health | Poorer childhood adjustment [62] | Greater risk of depressed affect, attempted suicide [62] |
| Physical Health | Poorer childhood health [62] | Poorer physical health component scores in older adulthood [62] |
| Social Functioning | Loss of friends, school changes [62] | Fewer quality social relationships in adulthood [67] |
| Behavioral Outcomes | Poorer self-regulation [62] | Smoking and alcoholism [62] |
Geriatric Mobility Triggers and Consequences
Multifactorial Triggers of Late-Life Mobility
Geriatric mobility triggers encompass both physical functional decline and environmental mismatches, creating a complex interplay of push and pull factors. Physical function decline represents a primary trigger, with mobility loss in older persons typically resulting from multiple impairments in the central nervous system, muscles, joints, and energetic and sensory physiological systems [66]. The exhaustion of compensatory mechanisms often precipitates overt mobility limitations, as natural selection has built the "engine" of mobility with great robustness, redundancy, and functional reserve that can mask early decline [66].
Environmental press theory suggests that community-level factors create push and pull dynamics that influence relocation. Urban environmental stressors such as noise, heavy traffic, high crime levels, and deprivation may push older adults to move away from their residences [69]. Conversely, lack of local services in rural areas presents known barriers for older people to remain living independently in their communities [69]. Research from the Cognitive Function and Ageing Study indicates that urban/rural contexts and area deprivation are significantly associated with relocation at older age [69].
Table 2: Relocation Patterns in Older Adults (Age 65+)
| Relocation Factor | Findings | Data Source |
|---|---|---|
| Overall Relocation Rate | 27.3% moved over 10 years [69] | Cognitive Function and Ageing Study (n=2,424) |
| Age Trend | Relocation increased from 24.6% (age 74-79) to 36.7% (age 90+) [69] | Cognitive Function and Ageing Study |
| Socioeconomic Pattern | Higher probability of moving with low education and low social class [69] | Cognitive Function and Ageing Study |
| Deprivation Association | Likelihood of relocation increased from least to most deprived areas (OR: 2.0, 95% CI: 1.4, 2.8) [69] | Cognitive Function and Ageing Study |
Physiological Aspects of Mobility Decline
Age-related mobility loss follows distinct patterns across joint systems and physiological domains. Research demonstrates that mobility decline is joint-specific, with shoulder mobility decreasing from 13.9% of total flexibility score at age 28 to only 5.2% by age 85 in males, while elbow and knee mobility are relatively preserved [70]. This specificity may relate to distinct routine usage patterns of major body joints throughout life [70].
The trajectory of mobility decline varies based on the challenging nature of the task. While usual pace walking speed remains relatively stable until age 65-70, more challenging tasks like fast-paced walking or long-distance walking show decline much earlier in adulthood [66]. This pattern suggests that early decline in mobility is detectable through appropriate assessment methods and may guide preventive strategies targeted to at-risk individuals [66].
Methodological Approaches: Measuring Mobility Across Populations
Assessing Pediatric Residential Mobility
Research on childhood mobility employs methodological approaches focused on documenting relocation frequency, reasons for moves, and contextual factors. The "Places You Have Lived Questionnaire" used in the REGARDS study exemplifies a comprehensive approach, documenting city, state, and age at the time of move for each location participants lived for at least one year from birth until study enrollment [62]. This method allows for precise quantification of move frequency during critical developmental periods.
Statistical approaches must account for significant confounding variables when examining health outcomes. Key confounders include parental socioeconomic status, parental marital status, ethnicity, and co-occurring childhood adversities [68]. Studies typically employ linear regression models adjusting for these factors, with additional analyses exploring interactions by race, childhood SES, and adverse childhood experiences [62].
Assessing Geriatric Mobility and Function
Geriatric mobility assessment encompasses both physical performance measures and relocation documentation. Standardized physical performance measures include walking speed tests (over 4 meters usual and fast pace, and 400 meters as fast as possible), chair rise tests, and balance assessments [66]. These measures track overall health status and predict adverse health outcomes including disability, nursing home admission, and mortality [66].
For relocation documentation, studies like the Cognitive Function and Ageing Study map participant postcodes to enumeration districts and link them to deprivation scores and rural/urban classifications [69]. Multilevel logistic regression examines the influence of both individual (age, gender, education, social class) and community-level (rural/urban categories, area deprivation) factors on relocation over time [69].
Biomarker Applications Across Populations
Biomarker research approaches differ substantially between pediatric and geriatric populations, reflecting their distinct mobility contexts.
Table 3: Biomarker Applications in Mobility Research
| Application Area | Pediatric Context | Geriatric Context |
|---|---|---|
| Primary Focus | Point-of-care biomarkers for acute conditions (sepsis, trauma) [71] | Biomarkers of chronic age-related processes [72] |
| Key Biomarkers | Procalcitonin, CRP for infection; S100B, GFAP for traumatic brain injury [71] | p-tau217 (Alzheimer's), NfL (neurodegeneration), GFAP, IL-6 (inflammation) [72] |
| Methodological Considerations | Age-dependent variations in biomarker performance [71] | Multipathway panels assessing multiple age-related processes simultaneously [72] |
Experimental Protocols and Research Tools
Protocol for Assessing Age-Related Mobility Change
The InCHIANTI study protocol provides a robust methodology for tracking mobility change across the life course. This longitudinal study conducted assessments at baseline, 3-, 6-, 9-, and 14-year follow-ups, employing mixed effect models with inverse probability weighting to address selective attrition [66]. The protocol includes:
Walking Speed Assessments:
- 4-meter walk at usual speed
- 4-meter walk at fast speed
- 400-meter walk as fast as possible
Data Collection Frequency: Repeated measures every 3-6 years to capture trajectory of change
Statistical Analysis: Calculation of average rates of change in walking speed per year of aging by sex and age groups, allowing identification of critical periods of decline [66]
This approach reveals that decline in challenging mobility tasks (400-meter walk) becomes evident in participants as young as 20-25 years, while usual pace walking only declines after age 65-70 [66].
Protocol for Joint-Specific Mobility Assessment
The Flexitest protocol provides a comprehensive method for assessing age-related mobility loss across joint systems. This assessment tool evaluates passive range of motion in 20 body movements across seven joints [70]:
Assessment Areas:
- Ankle: dorsal and plantar flexion (2 movements)
- Knee: flexion and extension (2 movements)
- Hip: flexion, extension, adduction, abduction (4 movements)
- Trunk: anterior and lateral flexion, extension (3 movements)
- Wrist: flexion and extension (2 movements)
- Elbow: flexion and extension (2 movements)
- Shoulder: posterior abduction, posterior adduction, posterior extension, lateral and medial rotations (5 movements)
Scoring System: Each movement scored 0-4 based on standardized evaluation maps, with composite scores calculated for each joint and overall flexibility (Flexindex)
Standardization: No warm-up allowed before assessment; experienced evaluators required (intraclass correlation coefficients 0.78-0.99 for movements) [70]
This protocol has demonstrated that age-related mobility loss is joint-specific, with shoulder and trunk mobility declining more rapidly than elbow and knee mobility [70].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Mobility Studies
| Reagent/Instrument | Application | Function in Research |
|---|---|---|
| Point-of-Care Biomarker Assays (PCT, CRP, S100B) [71] | Pediatric emergency care | Rapid diagnosis of acute conditions affecting mobility |
| Multidomain Biomarker Panels (p-tau217, NfL, GFAP, IL-6, GDF-15) [72] | Geriatric cognitive and functional decline | Assessing multiple pathological age-related processes simultaneously |
| Flexitest Evaluation Maps [70] | Joint-specific mobility assessment | Standardized scoring of passive range of motion across 20 movements |
| Wearable Devices [72] | Physical activity monitoring | Objective measurement of mobility and activity patterns in free-living environments |
| GIS Mapping Systems [69] | Residential mobility studies | Linking postcodes to deprivation scores and rural/urban classifications |
Conceptual Frameworks and Pathways
Childhood Residential Mobility and Long-Term Health Pathway
The following diagram illustrates the conceptual pathway through which childhood residential mobility influences long-term health outcomes, based on findings from longitudinal studies:
Childhood Mobility Health Pathway
Geriatric Mobility Decline and Relocation Pathway
The following diagram illustrates the multifactorial pathway leading to mobility decline and relocation in older adults:
Geriatric Mobility Decline Pathway
This comparative analysis reveals that while pediatric and geriatric populations are both considered "high-mover" groups, the nature, triggers, and consequences of their mobility differ fundamentally. Children experience primarily residential mobility driven by external family and socioeconomic factors, with effects modulated by personality and social support. Older adults experience primarily physical mobility decline driven by physiological changes and environmental mismatches, with effects influenced by socioeconomic resources and community characteristics.
Understanding these distinctions has profound implications for research methodology and intervention development. Life course epidemiological approaches that connect early life experiences with late-life outcomes are essential for fully understanding mobility patterns and their health consequences [66]. Future research should prioritize longitudinal studies that track both residential and physical mobility from childhood through older adulthood, employing multidisciplinary methods that capture biological, psychological, and social dimensions of mobility across the lifespan.
For researchers and drug development professionals, these findings highlight the need for distinct assessment approaches and intervention strategies tailored to the specific mobility contexts of each population. Interventions supporting housing stability for families represent potential policies that support older adults' health decades later [62], while multidimensional approaches addressing physical, cognitive, and social domains show promise for promoting functional mobility in aging populations [72].
Validating Safety Signals in Mobile vs. Non-Mobile Subpopulations
In pharmacovigilance, the systematic process of detecting, assessing, and understanding safety signals is fundamental to protecting patient health. This process becomes particularly critical for specific subpopulations—notably children and older adults—who constitute "high-mover" populations in the context of drug safety research. These groups experience dynamic physiological changes that significantly alter drug pharmacokinetics and pharmacodynamics, creating moving targets for safety monitoring [73] [74].
Older adults, especially those over 80, often experience age-related physiological changes that lead to substantial differences in how their bodies process medications compared to the general population [73]. This population frequently presents with multiple comorbidities and polypharmacy, increasing the risk of adverse drug reactions (ADRs) and drug-drug interactions [73] [74]. Similarly, children undergo continuous physiological development that affects drug metabolism, making them uniquely vulnerable to ADRs [75]. Despite these heightened risks, both populations remain substantially underrepresented in pre-market clinical trials, creating significant evidence gaps that must be addressed through robust post-marketing surveillance [73] [75].
This whitepaper provides a technical guide for validating safety signals within these high-mover populations, detailing specialized methodologies, data integration strategies, and analytical frameworks essential for accurate risk characterization.
The Scientific and Regulatory Imperative
The disproportionate vulnerability of pediatric and geriatric populations to adverse drug reactions necessitates specialized signal validation approaches. For older adults, the "silver tsunami" demographic shift means that by 2034, adults over 65 are projected to outnumber children in the United States for the first time in history [74]. This population not only uses medications at higher rates but also experiences age-related changes in pharmacokinetics and pharmacodynamics that increase susceptibility to drug toxicity [74].
Children, often described as "therapeutic orphans," face similar challenges in drug development and safety monitoring [75]. Pediatric drug development suffers from chronic underfunding, ethical concerns, and complex regulatory frameworks, resulting in limited therapeutic options that are often used off-label without adequate evidence from well-controlled trials [75]. The physiological differences between children and adults, and between children of different age groups, mean that safety signals identified in adult populations cannot be extrapolated to pediatric populations without rigorous validation [76] [75].
Regulatory agencies worldwide recognize these challenges. The European Medicines Agency (EMA), the U.S. Food and Drug Administration (FDA), and other international bodies have established frameworks requiring specialized signal management for vulnerable populations [77]. The EMA's Good Pharmacovigilance Practices (GVP) Module IX specifically addresses signal management, while the FDA mandates rigorous post-marketing surveillance and risk evaluation strategies [78] [77].
Table 1: Characteristics of High-Mover Populations in Pharmacovigilance
| Characteristic | Pediatric Population | Geriatric Population |
|---|---|---|
| Physiological Status | Rapid development affecting drug metabolism & response | Age-related decline in organ function affecting drug clearance |
| Clinical Trial Representation | Vastly underrepresented; considered "therapeutic orphans" [75] | Significantly underrepresented, especially those >80 years [73] |
| Medication Use Pattern | Often off-label use due to lack of pediatric formulations [75] | High prevalence of polypharmacy and comorbidities [73] [74] |
| Key Safety Concerns | Unique ADR profiles; long-term effects on development [76] [75] | Increased vulnerability to ADRs and drug-drug interactions [74] |
Effective signal validation for high-mover populations requires leveraging multiple complementary data sources, each with distinct strengths and limitations.
Spontaneous Reporting Databases (SRDs)
SRDs represent the cornerstone of traditional pharmacovigilance, collecting voluntary reports of suspected adverse reactions from healthcare professionals, patients, and manufacturers [79]. These databases are particularly valuable for early signal detection and rare event identification. Key global SRDs include:
- VigiBase: The WHO global database containing over 38 million individual case safety reports (ICSRs) from more than 150 countries [79]
- FDA Adverse Event Reporting System (FAERS): Contains over 29.6 million drug-focused ICSRs from the United States and other countries [79]
- EudraVigilance: The European database managed by the EMA, containing over 25 million ICSRs [79] [77]
While SRDs offer extensive coverage and rapid signal detection capabilities, they suffer from limitations including under-reporting, reporting biases, and variable data quality [79]. These limitations are particularly pronounced for high-mover populations, where comorbidities and polypharmacy can complicate causality assessment.
Longitudinal Healthcare Databases (LHDs)
LHDs provide comprehensive patient data over extended time periods, offering valuable context for signal validation [79]. These include:
- Electronic Health Records (EHRs): Contain detailed clinical information including medical history, prescriptions, diagnostic results, and treatment outcomes [79]
- Claims Databases: Focus on billing and healthcare utilization data, providing extensive longitudinal records [79]
- Patient and Disease Registries: Collect specific information for populations defined by particular conditions or exposures [79]
LHDs enable researchers to establish temporal relationships between drug exposure and outcomes, control for confounding factors, and study real-world drug utilization patterns—all critical for validating signals in high-mover populations [79].
Table 2: Comparison of Primary Data Sources for Signal Validation
| Data Source | Primary Strengths | Key Limitations | Utility for High-Mover Populations |
|---|---|---|---|
| Spontaneous Reporting Databases (SRDs) | Early detection of rare events; global coverage; regulatory mandate [79] [77] | Under-reporting; missing denominators; reporting biases [79] | Initial signal detection; identifying unusual ADR patterns [76] |
| Longitudinal Healthcare Databases (LHDs) | Rich clinical context; longitudinal follow-up; population-based data [79] | Variable data quality; fragmented records; coding inconsistencies [79] | Signal confirmation; assessing risk factors & confounders [79] |
| Scientific Literature | Detailed case narratives; mechanistic insights [80] [81] | Publication bias; non-systematic coverage [81] | Identifying potential biological plausibility [81] |
Methodological Framework for Signal Validation
Signal Detection Methods
Initial signal detection typically employs disproportionality analysis, which identifies unexpected reporting frequencies of specific drug-event combinations compared to background rates [80] [81] [76]. Key statistical measures include:
- Proportional Reporting Ratio (PRR): Compares the rate of a specific adverse event for one drug to that of all other drugs in the database [80] [81] [76]
- Reporting Odds Ratio (ROR): Assesses the odds of a drug-event pair compared to all other combinations [80] [81] [76]
- Bayesian Methods: Including the Bayesian Confidence Propagation Neural Network (BCPNN) and Multi-item Gamma Poisson Shrinker (MGPS), which use shrinkage to stabilize estimates for rare events [81] [82]
These quantitative approaches are particularly valuable for scanning large datasets efficiently, but they require subsequent clinical validation to distinguish true signals from statistical artifacts [81].
Signal Validation and Assessment
Once a statistical signal is detected, comprehensive validation is essential—particularly for high-mover populations where multiple confounding factors may be present. The validation process includes:
- Clinical Review of Case Narratives: Detailed assessment of individual case safety reports (ICSRs) to evaluate temporal relationships, dechallenge/rechallenge information, alternative explanations, and biological plausibility [80] [81]
- Causality Assessment: Application of standardized algorithms (e.g., WHO-UMC criteria, Naranjo scale) to evaluate the likelihood of a causal relationship between drug and event [80] [79]
- Data Source Triangulation: Corroborating findings across multiple data sources (SRDs, LHDs, literature) to strengthen signal credibility [79]
For high-mover populations, special attention must be paid to age-specific physiological factors, comorbidities, concomitant medications, and appropriate outcome definitions [73] [76] [75].
Advanced and Emerging Methods
Artificial intelligence (AI) and machine learning (ML) are revolutionizing signal validation, particularly for complex populations [82]. These advanced methods include:
- Natural Language Processing (NLP): Extracting relevant safety information from unstructured clinical notes, social media, and scientific literature [80] [82]
- Knowledge Graphs: Representing complex relationships between drugs, adverse events, and patient characteristics to identify hidden patterns [82]
- Multi-task Deep Learning: Simultaneously analyzing multiple drug-ADR interactions to improve detection accuracy [82]
These technologies can achieve impressive performance metrics, with some deep learning models achieving Area Under the Curve (AUC) values of 0.96 for classifying drug-ADR interactions [82]. However, they require careful validation and oversight to address potential biases, particularly for vulnerable populations that may be underrepresented in training data [82].
Experimental Protocols for Targeted Validation
When validating safety signals in high-mover populations, specific methodological considerations must be addressed to ensure accurate and reliable results.
Disproportionality Analysis for Subpopulation Focus
The following protocol outlines a robust approach for conducting disproportionality analysis specifically targeted at pediatric or geriatric populations:
Data Extraction: Extract reports for the drug of interest and the specific adverse event from databases like FAERS or VigiBase, filtering for the target subpopulation (e.g., children 0-17 years or adults ≥65 years) [76]
Case Selection: Apply stringent inclusion criteria, ensuring accurate age classification and excluding reports with missing critical data (e.g., age, gender, event date) [76]
Reference Group Definition: Create appropriate reference groups by including all other drugs and adverse events for the same subpopulation to calculate expected reporting rates [76]
Statistical Analysis: Calculate multiple disproportionality measures (ROR, PRR) with 95% confidence intervals to assess signal strength [76]
Sensitivity Analysis: Conduct stratified analyses by gender, age subgroups (e.g., 0-1 years, 2-11 years, 12-17 years for pediatrics), and geographic region to evaluate consistency [76]
This approach was successfully implemented in a recent study comparing ibuprofen safety signals in children versus adults, which identified distinct toxicity profiles, including a novel signal of decreased white blood cell count specifically in children (ROR = 12.72, PRR = 12.63) [76].
Integration of Spontaneous Reports and Longitudinal Data
A protocol for integrating SRDs and LHDs provides a comprehensive approach to signal validation:
Signal Detection in SRDs: Identify potential signals using quantitative methods in spontaneous reporting databases [79]
Cohort Definition in LHDs: Define exposed and comparator cohorts in longitudinal databases, matching for key confounders (e.g., comorbidities, concomitant medications) particularly relevant to the subpopulation [79]
Outcome Assessment: Apply validated algorithms to identify adverse events in LHDs, using appropriate washout periods and follow-up windows [79]
Analysis: Calculate incidence rates and relative risks, adjusting for residual confounding using advanced methods like propensity score stratification or disease risk scores [79]
Triangulation: Synthesize evidence from both sources, assessing consistency while accounting for the inherent limitations of each data source [79]
This integrated approach leverages the complementary strengths of different data sources, providing a more robust evidence base for regulatory decision-making [79].
Table 3: Research Reagent Solutions for Signal Validation Studies
| Research Tool | Function | Application in High-Mover Populations |
|---|---|---|
| MedDRA (Medical Dictionary for Regulatory Activities) | Standardized terminology for adverse event coding [81] | Enables consistent coding across populations; SMQs (Standardized MedDRA Queries) group related terms [81] |
| WHO-UMC Causality Assessment Criteria | Standardized system for evaluating case-level causality [80] [79] | Provides consistent framework for assessing drug-Event relationship in complex cases with polypharmacy [80] |
| Disproportionality Analysis Algorithms (PRR, ROR, BCPNN) | Statistical methods for identifying unexpected reporting patterns [80] [81] | Initial signal detection in subpopulations; requires careful interpretation due to confounding [76] |
| Electronic Health Record Systems with API Access | Sources of rich, longitudinal clinical data [79] | Enables study of real-world drug use and outcomes in routine care settings [79] |
| AI-Powered Signal Management Platforms | Automated processing and prioritization of potential signals [78] [82] | Handles large data volumes; can be trained to recognize subpopulation-specific patterns [82] |
Analytical Considerations for High-Mover Populations
Age-Appropriate Methodological Adjustments
Validating signals in high-mover populations requires specific methodological adjustments to account for their unique characteristics:
- Age Stratification: For pediatric populations, implement finer age categories (e.g., neonates, infants, children, adolescents) to account for developmental differences in drug metabolism and response [75]
- Comorbidity Adjustment: For older adults, comprehensively capture and adjust for burden of comorbidities using validated measures such as the Charlson Comorbidity Index [73] [74]
- Polypharmacy Assessment: Systematically document and account for concomitant medications, particularly in geriatric populations where complex medication regimens are common [73] [74]
- Outcome Definition: Employ age-appropriate definitions for adverse events, recognizing that clinical presentations may differ significantly from adult populations [76] [75]
Managing Data Limitations
Data sources for high-mover populations present specific challenges that must be addressed during signal validation:
- Underrepresentation in Databases: Actively monitor for and address potential selection biases arising from the systematic underrepresentation of these populations in certain data sources [73] [75]
- Confounding by Indication: Carefully control for confounding by indication, particularly in older adults with multiple conditions where drug exposure may be correlated with underlying disease severity [79]
- Validation of Case Ascertainment: Implement robust validation studies for case ascertainment algorithms in LHDs, particularly for outcomes that may be coded differently in pediatric versus adult populations [79]
Validating safety signals in mobile versus non-mobile subpopulations represents both a significant challenge and moral imperative in pharmacovigilance. Children and older adults, as high-mover populations with dynamically changing physiology and unique vulnerability to adverse drug reactions, require specialized approaches throughout the signal management process. Through the integrated use of complementary data sources, application of robust statistical and epidemiological methods, implementation of age-appropriate analytical frameworks, and adoption of emerging technologies like artificial intelligence, researchers can overcome the inherent challenges in characterizing safety signals for these populations. A systematic, rigorous approach to signal validation for high-mover populations is essential for closing the current evidence gaps and ensuring the safe use of medications across all age groups.
Within the broader investigation of why children and older adults constitute high-mover populations, this whitepaper examines a critical consequence of this mobility: its impact on healthcare access and patient outcomes. Residential mobility is a life-course process with distinct drivers at different ages; the moves of older adults are often linked to declining health and the need for care, while children typically move as part of family units responding to socioeconomic factors [1] [3]. Understanding the healthcare implications for these groups is paramount for public health officials, drug development professionals seeking to understand real-world efficacy, and researchers designing robust cohort studies.
This technical guide synthesizes current evidence on how moving influences a patient's interaction with the healthcare system and their subsequent health. It delves into the methodological frameworks used to disentangle this relationship, presents key quantitative findings on utilization and mortality, and provides a scientific toolkit for researchers in this field. The central thesis is that moving acts as a natural experiment, revealing how place-based supply-side factors and individual patient demand characteristics independently and jointly shape healthcare utilization and outcomes, with varying effects across age and socioeconomic groups.
Drivers of Mobility in High-Mover Populations
The decision to relocate is influenced by a distinct set of factors for different age groups. Understanding these drivers is essential for interpreting the associated healthcare patterns.
Older Adults
For older adults, particularly those transitioning to the "fourth age" (typically over 80), mobility is heavily driven by health and care needs [1].
- Health Triggers: Severe health problems are a primary catalyst for relocation. This manifests in two key ways: an increased likelihood of geographic convergence (moving closer to an adult child or having a child move closer) and a greater probability of moving into an institutionalized care facility [1]. The effect of health issues is stronger for the parent moving closer to a child than for a child moving closer to the parent [1].
- Social and Familial Structures: Older mothers are more likely to move towards daughters or towards distant children who have at least one sibling living nearby, reflecting gendered patterns of care provision [1]. The presence of a local sibling network also increases the likelihood of a distant child moving closer to an aging parent [1].
General Adult Population
While not the focus of this paper, understanding movers in the general adult population provides context. A study of middle-aged and early-retirement adults found that movers differ systematically from non-movers. Predictors of moving include sociodemographic characteristics, health and psychosocial factors, incident life "triggers" (e.g., divorce, retirement), and area-level characteristics [3]. Furthermore, the characteristics of those who complete short-distance moves differ from those who undertake long-distance moves, suggesting varying motivations (e.g., health needs vs. job opportunities) [3].
Table 1: Key Drivers of Residential Moves in Older Adults
| Driver Category | Specific Factor | Impact on Mobility |
|---|---|---|
| Health Status | Severe health problems | Strongly associated with moves closer to children and transitions to institutional care [1]. |
| Functional limitations | A predictor of residential moves, often motivating a shift to more accessible housing or care settings [3]. | |
| Familial Networks | Gender of adult children | Older parents are more likely to move closer to daughters, who are more likely to provide care [1]. |
| Proximity of sibling network | Increases the probability of geographic convergence between a distant child and an aging parent [1]. | |
| Socioeconomic Status | Income and Education | Influences the ability to move and the type of destination (e.g., quality of housing or care facility) [3]. |
Methodological Frameworks for Studying Mover Effects
A primary challenge in this research area is untangling the effect of a person's health characteristics from the effect of the place they live. Individuals are not randomly assigned to locations; those who move may be systematically different from those who do not. Several advanced methodological approaches have been developed to address this selection bias.
The "Mover Design" for Estimating Place Effects
A core method, exemplified by Finkelstein et al. (2021), uses outcomes of migrants to separately identify the effects of health capital and current location ("place effects") on mortality [83].
Core Protocol:
- Sample Definition: The analysis focuses on a population of movers (e.g., elderly Medicare beneficiaries). This controls for the initial selection bias of who chooses to move [83].
- Model Specification: Log mortality is modeled as an additive function of age, place effects, and health capital. This relies on two key assumptions:
- Statistical Control: Mortality differences among movers to different destinations are analyzed while controlling for their origin locations and a rich vector of pre-move health measures from claims data (e.g., diagnoses, utilization) [83].
- Selection on Unobservables Adjustment: A novel strategy uses the correlation between movers' choice of destination and their observed health capital to adjust for potential correlation with unobserved health capital. The correlation between origin locations and residual post-move mortality provides an additional moment to gauge the importance of unobservables [83].
This design effectively compares two individuals from the same origin (e.g., Boston), one of whom moved to a low-mortality area (e.g., Minneapolis) and the other to a high-mortality area (e.g., Houston), to estimate the causal effect of the destination on mortality [83].
Mandatory Mover Designs
An alternative, powerful approach harnesses the mandatory migration of specific populations, such as military personnel and their dependents. This design virtually eliminates the issue of selection bias, as moves are not motivated by health or preference [84].
Core Protocol:
- Sample Definition: Analyze healthcare utilization data for a closed system like the U.S. Military Health System for active-duty personnel and their families (ages 5-64) who are subject to mandatory relocation [84].
- Variation Analysis: Compare utilization patterns across different locations of care. Since patient demand characteristics are largely held constant (due to the mandatory nature of moves), the remaining regional variation is attributed to supply-side "place effects" [84].
- Estimation: This methodology has shown that place or supply effects explain as much as 80% of the overall regional variation in utilization within this system [84].
The following diagram illustrates the core analytical logic used in mover studies to isolate the effect of place from the effect of person-specific characteristics.
Key Findings on Utilization, Mortality, and Place
Applying these rigorous methodologies has yielded robust evidence on how moving and place shape healthcare and health.
The Impact of Moving on Healthcare Utilization
Moving exposes individuals to a new set of supply-side factors, which can dramatically alter their care patterns.
- Place Effects Explain Half of Regional Variation: A study of cross-region migration in Norway found that place factors account for approximately 50% of the difference in healthcare utilization between high- and low-utilization regions. The other half reflects persistent patient demand characteristics [85].
- Socioeconomic Status Modifies Place Effects: The impact of place on utilization is not uniform. The Norwegian study found striking heterogeneity: place factors accounted for 75% of the regional utilization difference for high school dropouts, 40% for high school graduates, and had a negligible impact for patients with a college degree [85]. This suggests that patients with higher socioeconomic status are better able to navigate and overcome local supply-side constraints.
- Extreme Place Effects in Salaried Systems: Research on the U.S. Military Health System—where physicians are salaried and financial barriers are low—found that supply-side "place effects" explain up to 80% of regional variation in utilization. This indicates that factors like local physician practice styles and beliefs are powerful drivers of care patterns, independent of patient health or financial incentives [84].
The Impact of Moving on Mortality and Life Expectancy
Where one lives in later life has a profound and causal impact on mortality risk.
- Substantial Effects on Life Expectancy: Analysis of elderly Medicare movers shows that current location has a large impact on mortality. Moving from a 10th-percentile location to a 90th-percentile location in terms of favorable place effects would increase life expectancy at age 65 by 1.1 years [83].
- Relative Importance of Place vs. Health Capital: While significant, equalizing place effects across areas would reduce the cross-sectional variation in life expectancy by only about 15%. In contrast, equalizing health capital (the persistent effects of genetics and past health behaviors) across areas would reduce variation by about 70% [83]. This underscores that an individual's accumulated health is the dominant long-term factor, but place effects are powerful short-term determinants.
- Correlates of Favorable Mortality Effects: Areas with more favorable place effects on life expectancy tend to have higher quality and quantity of healthcare, less extreme climates, lower crime rates, and higher socioeconomic status [83]. The correlation between an area's healthcare utilization and its impact on life expectancy contrasts with the well-known Dartmouth Atlas findings, highlighting the importance of mover designs in isolating causal effects [83].
Table 2: Quantitative Impact of Location on Healthcare and Mortality Based on Mover Studies
| Metric | Population | Finding | Source |
|---|---|---|---|
| Life Expectancy Impact | Elderly Medicare Movers | Moving from a 10th to a 90th percentile location increases life expectancy at age 65 by 1.1 years. | [83] |
| Variation Explained by Place | Elderly Medicare Movers | Equalizing place effects would reduce cross-sectional life expectancy variation by 15%. | [83] |
| Healthcare Utilization | Norwegian Migrants | Place factors account for 50% of the difference in utilization between high- and low-use regions. | [85] |
| Healthcare Utilization (SES) | Norwegian Migrants (Low SES) | Place effects account for 75% of regional utilization differences for high school dropouts. | [85] |
| Healthcare Utilization (System) | U.S. Military Health System | Supply-side place effects explain up to 80% of regional utilization variation. | [84] |
The Scientist's Toolkit: Research Reagent Solutions
Researchers investigating healthcare access and outcomes among movers rely on a suite of "reagent solutions"—key data sources, methodological approaches, and variables. The table below details these essential components.
Table 3: Essential Research Components for Studying Mover Populations
| Tool / Reagent | Function / Definition | Application in Mover Studies |
|---|---|---|
| Administrative Health Data | Comprehensive, longitudinal data on healthcare encounters, diagnoses, procedures, and prescriptions. | Serves as the primary source for measuring pre- and post-move health capital, utilization outcomes, and mortality. (e.g., Medicare claims, Norwegian Patient Registry) [83] [85]. |
| Geocoded Residential Histories | Longitudinal records of participant addresses, standardized and converted to geographic coordinates (latitude/longitude). | Used to identify residential moves (using pairwise distance calculations between timepoints) and assign individuals to specific geographic units of analysis [3]. |
| Commuting Zones (CZs) | A geographic unit aggregating counties to approximate local labor markets. | A standard analytic geography used to define "places" or healthcare markets when studying regional variation in the U.S. [83]. |
| Pre-Move Health Capital Vector | A rich set of health measures derived from claims data (e.g., diagnoses, Elixhauser comorbidities, spending) for a period prior to a move. | A critical set of control variables used to account for observable health differences between individuals who choose different destinations, reducing selection bias [83]. |
| Mandatory Mover Sample | A sub-population whose moves are mandated by an external authority (e.g., military personnel). | An instrumental variable that mitigates selection bias by creating a scenario where movement is quasi-random with respect to health preferences [84]. |
Implications for Research and Drug Development
The findings from mover studies have significant implications for epidemiological research, public policy, and the drug development industry.
- Mitigating Bias in Cohort Studies: In long-term epidemiological studies, participants who move may be systematically different from those who remain, leading to selection bias. Furthermore, using only baseline addresses to assign environmental exposures can result in significant exposure misclassification for movers. Understanding predictors of mobility helps researchers quantify and adjust for these biases [3].
- Informing "Care at Home" Strategies: The COVID-19 pandemic catalyzed a shift toward home-based care, with estimates suggesting up to $265 billion in Medicare care services could shift to the home by 2025 [86]. Research on movers and geographic access informs this transition, highlighting the importance of supplementing virtual care with remote monitoring and social supports to ensure equitable outcomes, especially for older movers who may be relocating for care [86].
- Contextualizing Real-World Evidence (RWE) and Clinical Trials: For drug development professionals, the geographic variation in practice styles and utilization uncovered by these studies is critical. A drug's real-world effectiveness and observed side-effect profiles may vary significantly based on local treatment patterns and access to follow-up care [85] [84]. When analyzing RWE or selecting clinical trial sites, companies must account for these place-based practice patterns, as they can influence measured adherence, companion treatments, and outcomes. The mover effect paradigm provides a framework for understanding and controlling for these geographic confounders.
The following diagram synthesizes the key factors that influence healthcare outcomes for mobile populations, illustrating the interaction between individual characteristics and the features of their new location.
The study of geographic mobility, particularly concerning child and older adult populations, provides critical insights into the interplay between state institutions, family dynamics, and life-course transitions. Within comparative sociological research, understanding why these demographic groups exhibit high mobility rates necessitates examining how different welfare systems shape, facilitate, or constrain their relocation patterns. This technical guide examines the complex relationships between welfare state typologies, educational and social policies, and the resultant mobility patterns observed across nations. Framed within a broader thesis on the high mobility of children and older adults, this analysis synthesizes methodological approaches, empirical findings, and theoretical frameworks to elucidate how institutional structures mediate life-course transitions for these populations. The focus extends beyond mere descriptive patterns to investigate the mechanisms through which state policies either ameliorate or exacerbate the dependencies that often drive mobility at the beginnings and endings of the life course.
Theoretical Foundations: Welfare Regimes and Mobility
Welfare State Typologies and Their Mobility Implications
Comparative stratification research has established that welfare states systematically influence mobility patterns through their institutional configurations. Esping-Andersen's classic typology—social democratic, conservative-corporatist, and liberal welfare regimes—provides a foundational framework for understanding cross-national variations [87]. Research indicates that socialist and social democratic welfare regimes consistently foster a weaker association between occupational origins and destinations, creating more open mobility structures compared to liberal, corporatist, or mixed regimes [87]. This has profound implications for how children's future life chances are shaped by their family backgrounds across different policy environments.
The mechanism underlying this relationship operates through both educational and social policy channels. Nations with better-educated labor forces tend to exhibit weaker origin-destination associations, suggesting that educational expansion serves as a potential equalizing mechanism [87]. However, the relationship is nuanced by welfare context: the tendency for educational access to lower the origin-destination association is most pronounced in liberal welfare settings where the association would otherwise be greatest [87]. This interaction effect highlights the complex interplay between educational and social policies in structuring mobility regimes.
Life-Course Perspectives on High-Mover Populations
Children and older adults emerge as high-mover populations due to their specific vulnerability to dependency relationships within welfare systems. For children, mobility is primarily passive, reflecting family responses to institutional incentives and constraints. As census data indicates, children (1-15 years) represent a substantial proportion of movers (4.62 million annually in the U.S.), predominantly relocating for family and housing reasons [88]. Their mobility patterns fundamentally reflect how welfare systems mediate the intergenerational transmission of advantage through educational access, housing policies, and income support mechanisms.
For older adults, mobility patterns reflect different dependencies, primarily driven by health transitions and care needs. The transition to the "fourth age" (typically between 80-85 years) marks a critical period where diminished capacity for self-care creates dependencies on both formal care systems and informal family networks [1]. This life-course stage is characterized by increased mobility responses to health deterioration, including relocations closer to children, moves into institutional care, or rarely, having children move closer [1]. Gender differences further structure these patterns, with women often enduring multiple chronic disabilities while men experience more fatal conditions, creating divergent mobility pathways in later life [1].
Methodological Approaches
Quantitative Strategies for Comparing Mobility Patterns
Cross-national mobility research employs sophisticated statistical approaches to isolate welfare effects from other contextual factors. The log-multiplicative layer effects model (often called "unidiff") represents the standard analytical framework for comparing variation among countries in the association between origins and destinations [87]. This model formally estimates the association between origin class (i), destination class (j), and nation (k) using the following structure:
log Fijk = λ + λiO + λjD + λijOD + ϕkψijk
Where ϕk parameters indicate the relative strength of the origin-destination association in nation k compared to other nations [87]. This approach allows researchers to test whether substantive national differences in relative mobility rates exist while accounting for differences in marginal distributions.
For analyzing older adult mobility, researchers increasingly employ multinomial logistic regression models to assess the relationship between parents' health issues and different types of relocations [1]. This approach effectively captures the multiple, mutually exclusive mobility outcomes common in later life: moving closer to children, transitioning to institutional care, or remaining in place. Swedish register data studies exemplify this methodology, controlling for location-specific capital, sociodemographic characteristics, and urbanization levels to isolate welfare effects [1].
Comparative mobility research faces significant data challenges, particularly regarding cross-national equivalence. The International Social Survey Programme (ISSP) inequality module has emerged as a valuable data source, with specifically designed comparability across nations that reduces methodological artifacts [87]. For health and aging-related mobility, the Survey of Health, Ageing and Retirement in Europe (SHARE) and the English Longitudinal Study of Ageing (ELSA) provide comprehensive, longitudinal data on individuals aged 50+ across multiple welfare contexts [89].
Methodological protocols must explicitly address occupational coding consistency, sample representativeness, and measurement equivalence to ensure valid comparisons. The International Standard Classification of Occupations (ISCO) provides the foundational taxonomy, but implementation varies significantly across national contexts [87]. Recent advances in harmonization protocols, such as those developed by Ganzeboom et al. (1996), have improved comparability but require careful implementation [87].
Empirical Patterns: Welfare Systems and Mobility Outcomes
Educational Policy Regimes and Child Mobility
The relationship between educational systems and child mobility operates through both direct and indirect pathways. Nations characterized by comprehensive educational systems with minimal tracking tend to exhibit weaker associations between social origins and educational attainment, reducing the reproduction of inequality through generational mobility [87]. However, evidence suggests that educational expansion alone does not necessarily produce greater equality of opportunity, as privileged families often find new ways to transmit advantages even within expanded systems [87].
Table 1: Educational Policy Dimensions and Child Mobility Patterns
| Policy Dimension | Social Democratic Regime | Liberal Regime | Conservative Regime |
|---|---|---|---|
| Educational Access | Universal with strong public subsidy | Mixed public-private with significant cost barriers | Tracked system with early selection |
| Origin-Destination Association | Weaker | Stronger | Moderate to Strong |
| Child Mobility Pattern | Family mobility less determinative of outcomes | Family mobility crucial for accessing opportunity | Mobility patterns reflect educational tracking |
| Compensatory Mechanisms | Strong public institutions reduce family dependency | Market-based solutions amplify family resource effects | Family resources mediate institutional selection |
The interaction between educational policy and welfare regime type produces distinctive mobility patterns for children. In social democratic contexts, the state assumes greater responsibility for equalizing opportunities, reducing the pressure for strategic mobility to access quality education [87]. Conversely, in liberal regimes, where the origin-destination association is typically strongest, geographic mobility becomes increasingly strategic as families seek to position children in superior educational markets [87]. This explains the high mobility observed among children in liberal welfare contexts, where housing-related moves (2.17 million annually for 1-15 year olds in the U.S.) often reflect educational positioning strategies [88].
Care Regimes and Older Adult Mobility
Welfare systems fundamentally structure older adult mobility through their varied approaches to long-term care provision, pension systems, and intergenerational responsibility. Research across European contexts demonstrates that the marginal utility of consumption changes with health status, creating distinct mobility patterns based on welfare system type [89]. Specifically, individuals in countries with lower public spending on long-term care (<1% of GDP) experience a greater drop in marginal utility when cognitive impairment occurs compared to those in high-spending countries (>2% of GDP) [89].
Table 2: Care Regimes and Older Adult Mobility Responses to Health Decline
| Mobility Response | Social Democratic Model | Liberal Model | Family-Based Model |
|---|---|---|---|
| Relocation to Institutional Care | High likelihood; state-supported | Market-dependent; resource-stratified | Low availability; familial last resort |
| Moving Closer to Children | Less common; formal care替代 | Moderate; reflects care gaps | Primary strategy; cultural expectation |
| Children Moving Closer | Rare; state assumes care role | Occasional; constrained by labor markets | Common; filial obligation |
| Health-Mobility Relationship | Formalized transitions at high care needs | Resource-mediated access to optimal care | Direct relationship; familial capacity determinant |
The Swedish case exemplifies the social democratic pattern, where severe health problems among older parents increase the likelihood of either moving closer to children or transitioning to institutional care, but show no significant association with children moving closer [1]. This reflects a state-substituted care model where formal institutions replace familial care obligations. In contrast, research from India illustrates a family-based model, where adult son migration creates significant caregiving gaps for left-behind parents, resulting in poorer health outcomes, higher chronic morbidity, and increased psychological distress [90]. This contrast highlights how welfare systems mediate the relationship between family structure, mobility, and wellbeing in later life.
Analytical Framework Diagram
Welfare Systems and Mobility Relationships
Research Reagents Toolkit
Table 3: Essential Methodological Resources for Comparative Mobility Research
| Research Resource | Primary Function | Application Context |
|---|---|---|
| ISSP Inequality Module | Cross-national comparable data on occupational mobility | Testing hypotheses about welfare state effects on origin-destination association |
| SHARE/ELSA Surveys | Longitudinal data on health, aging, and retirement | Analyzing health-related mobility in later life across welfare contexts |
| Log-Multiplicative Layer Effects Models | Statistical estimation of cross-national variation in mobility associations | Quantifying relative openness of different welfare regimes |
| EGP/ISCO Occupational Classification | Standardized coding of occupational origins and destinations | Ensuring comparability of mobility measures across national contexts |
| Multinomial Logistic Regression | Modeling multiple categorical mobility outcomes | Analyzing distinct relocation types in older adult populations |
| Welfare Regime Typology | Theoretical classification of state-market-family relationships | Contextualizing mobility patterns within institutional frameworks |
Cross-national analysis of mobility patterns reveals the profound imprint of welfare systems on life-course transitions, particularly for the high-mover populations of children and older adults. The evidence consistently demonstrates that social democratic regimes, characterized by comprehensive educational access and extensive care systems, produce more open mobility structures and more institutionalized responses to dependency needs. In contrast, liberal and family-based regimes intensify the role of private resources and familial obligations in structuring mobility, often reinforcing existing inequalities. Future research should develop more integrated analytical frameworks that simultaneously examine child and older adult mobility within unified welfare regime typologies, particularly as demographic aging and educational expansion continue to reshape dependency relationships across the life course. The methodological toolkit outlined here provides a foundation for such comparative investigations, emphasizing both statistical rigor and theoretical nuance in unpacking the complex relationships between welfare institutions and geographic mobility.
Conclusion
The high mobility of pediatric and older adult populations is not a random demographic phenomenon but is driven by predictable, life-course-specific triggers. For drug development and clinical research, this mobility directly impacts trial integrity, data completeness, and the generalizability of safety and efficacy findings. Success in this landscape requires a paradigm shift from static to dynamic research models that incorporate mobility risk into their core design. Future efforts must focus on developing more agile, technology-enabled frameworks for participant tracking, alongside regulatory guidance that acknowledges and accommodates population mobility. By proactively integrating these considerations, the biomedical research community can enhance the validity, equity, and impact of clinical studies for these critical, and often moving, populations.
References
- 1. Geographic mobility among older people and their adult children [https://pmc.ncbi.nlm.nih.gov/articles/PMC8072412/]
- 2. The complex life course of mobility: Quantitative description ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10426073/]
- 3. Characteristics of movers and predictors of residential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9004423/]
- 4. Characteristics of movers and predictors of residential ... [https://www.sciencedirect.com/science/article/abs/pii/S1353829222000326]
- 5. Older Adults' Residential Proximity to Their Children [https://pmc.ncbi.nlm.nih.gov/articles/PMC4817072/]
- 6. The importance of informal support and a listening ear [https://pmc.ncbi.nlm.nih.gov/articles/PMC10540488/]
- 7. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 8. Elements must meet minimum color contrast ratio thresholds [https://dequeuniversity.com/rules/axe/4.8/color-contrast]
- 9. Color contrast - Accessibility - MDN Web Docs - Mozilla [https://developer.mozilla.org/en-US/docs/Web/Accessibility/Guides/Understanding_WCAG/Perceivable/Color_contrast]
- 10. A Life Course Perspective on Child Health, Academic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3893027/]
- 11. Family Structures and Support Strategies in the Older ... [https://aspe.hhs.gov/reports/family-structures-support-strategies-older-population-implications-baby-boomers-issue-brief-0]
- 12. Challenges and opportunity in mobility among older adults [https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-023-04106-7]
- 13. the travel burdens of family caregivers in an aging America [https://link.springer.com/article/10.1007/s11116-025-10630-9]
- 14. Urbanization - Our World in Data [https://ourworldindata.org/urbanization]
- 15. 8 Trends to Know About Children and Families for 2025 [https://www.childtrends.org/publications/8-trends-children-and-families-2025]
- 16. 7 Trends Reshaping the Health and Lifespans of America's ... [https://www.prb.org/resources/seven-trends-reshaping-the-health-and-lifespans-of-americas-rapidly-aging-population/]
- 17. Why Is Geographic Mobility Declining? | Richmond Fed [https://www.richmondfed.org/publications/research/economic_brief/2025/eb_25-19]
- 18. Intersecting impacts of ageing, migration, and socioeconomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593769/]
- 19. Child Migration - UNICEF Data [https://data.unicef.org/topic/child-migration-and-displacement/migration/]
- 20. A comprehensive longitudinal Centers for Disease Control ... [https://pubmed.ncbi.nlm.nih.gov/41117070/]
- 21. Factors influencing anticipated migration patterns across ... [https://link.springer.com/article/10.1007/s44243-025-00053-6]
- 22. Longitudinal studies - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4669300/]
- 23. Children in an ageing society - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1117089/]
- 24. Digital divide as a determinant of health in the U.S. older ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11662839/]
- 25. Robust longitudinal multi-cohort results: The development ... [https://www.sciencedirect.com/science/article/pii/S1878929320300657]
- 26. Factors Influencing Attrition in a Multisite, Randomized, Clinical Trial Following Traumatic Brain Injury in Adolescence - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4465204/]
- 27. Predictors of attrition in a longitudinal population-based ... [https://www.sciencedirect.com/science/article/pii/S1041610224035324]
- 28. Exploring participant attrition in a longitudinal follow-up of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10373724/]
- 29. Loss to follow-up in a randomized controlled trial study for pediatric weight management (EPOC) - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5109701/]
- 30. Patient, Family, and Center-Based Factors Associated with Attrition in Neonatal Clinical Research: A Prospective Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6657796/]
- 31. On clinical trial fragility due to patients lost to follow up [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-021-01446-z]
- 32. Age Diversity In Clinical Trials Considerations For ... [https://www.clinicalleader.com/doc/age-diversity-in-clinical-trials-considerations-for-improving-older-adult-representation-0001]
- 33. Inclusion of special populations in clinical research [https://pmc.ncbi.nlm.nih.gov/articles/PMC6410628/]
- 34. Opportunities and challenges of pharmacovigilance in special ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10540608/]
- 35. Exploring Challenges in Pediatric Pharmacovigilance in ... [https://pubmed.ncbi.nlm.nih.gov/40753519/]
- 36. Pharmacovigilance in Older Adults is a Lifeline for Safer ... [https://drug-card.io/blog/pharmacovigilance-in-older-adults-is-a-lifeline-for-safer-aging/]
- 37. Factors associated with underreporting of adverse drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10682061/]
- 38. Uncovering the Hidden Hurdles: Exploring Challenges in ... [https://link.springer.com/article/10.1007/s40264-025-01593-y]
- 39. Looking beyond age to understand adverse reaction risk in ... [https://uppsalareports.org/articles/looking-beyond-age-to-understand-adverse-reaction-risk-in-older-patients/]
- 40. Spontaneous adverse drug reaction reporting in rural ... [https://pubmed.ncbi.nlm.nih.gov/18759510/]
- 41. Effectiveness of mobile applications in enhancing adverse ... [https://bmcdigitalhealth.biomedcentral.com/articles/10.1186/s44247-025-00153-9]
- 42. Social media and pharmacovigilance: A review of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4594734/]
- 43. The Sandwich Generation: Stuck Between Aging Parents ... [https://mylifesite.net/blog/post/the-sandwich-generation-stuck-between-aging-parents-young-children]
- 44. Harnessing digital health technologies and real-world ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12290384/]
- 45. Quantitative analysis of the impact of various urban ... [https://www.sciencedirect.com/science/article/pii/S2468042722000227]
- 46. Children of Aging Parents Are Often Nearby, Study Finds [https://archive.nytimes.com/newoldage.blogs.nytimes.com/2012/09/13/children-of-aging-parents-are-often-nearby-study-finds/]
- 47. Adaptive designs in clinical trials: why use them, and how to ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-018-1017-7]
- 48. Adaptive Bayesian information borrowing methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11132956/]
- 49. Use of big data in drug development for precision medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC6613936/]
- 50. Patient-Centered Pharmaceutical Design to Improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4210646/]
- 51. Best Practices for Remote Work Policies in 2025 [https://www.remotelytalents.com/blog/best-practices-for-remote-work-policies-in-2025]
- 52. Drug Delivery Formulations and Devices Tailored for ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2021.782635/full]
- 53. Quantitative Observation: Everything You Need To Know [https://www.surveylab.com/blog/quantitative-observation/]
- 54. Comparative Analysis: Mastering Techniques for Effective ... [https://www.storytellingwithcharts.com/blog/a-comparative-analysis-mastering-techniques-for-effective-data-comparison/]
- 55. a community-based intervention for malaria elimination in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11420009/]
- 56. Building Trust in Community-Engaged Research [https://about.citiprogram.org/blog/from-participant-to-partner-building-trust-in-community-engaged-research/]
- 57. An Overview of the Fundamentals of Data Management ... [https://www.sciencedirect.com/science/article/pii/S0749208123000293]
- 58. Getting started with tables - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5357815/]
- 59. A review of human mobility: Linking data, models, and real- ... [https://link.springer.com/article/10.1007/s42001-025-00414-7]
- 60. Developing a mixed-methods approach to understand ... [https://www.sciencedirect.com/science/article/abs/pii/S027795361630288X]
- 61. Examining the social networks of older adults receiving ... [https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-023-04190-9]
- 62. Childhood Residential Mobility and Mental and Physical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10394967/]
- 63. The daily mobility of older adults: Urban/rural differences in ... [https://link.springer.com/article/10.1007/s00168-022-01192-0]
- 64. The adult 'boomerang kids' moving home to their parents [https://www.bbc.com/worklife/article/20220208-the-adult-boomerang-kids-moving-home-to-their-parents]
- 65. Methodological Insights from Older Adults' Activity Diaries [https://www.sciencedirect.com/science/article/pii/S0277953625010573]
- 66. Age-Related Change in Mobility: Perspectives From Life ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4978365/]
- 67. Moving repeatedly in childhood associated with poorer ... [https://www.apa.org/news/press/releases/2010/06/moving-well-being]
- 68. Childhood residential mobility and health outcomes [https://www.sciencedirect.com/science/article/pii/S1353829221001465]
- 69. Relocation at older age: results from the Cognitive Function ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4552011/]
- 70. Age-related mobility loss is joint-specific: an analysis from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3824991/]
- 71. Point-of-Care Biomarkers in Pediatric Emergency Medicine [https://link.springer.com/article/10.1007/s40746-025-00332-w]
- 72. Multi-pathway blood biomarkers to target and monitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12092390/]
- 73. Drug Research and Development for Adults Across the Older Age Span ... [https://www.ncbi.nlm.nih.gov/books/NBK575965/]
- 74. On the perspective of an aging population and its potential impact on ... [https://www.sciencedirect.com/science/article/pii/S1056871922000314]
- 75. Breaking the silence: challenges and opportunities in pediatric drug ... [https://www.nature.com/articles/s41390-025-03923-3]
- 76. Comparison of safety signals for ibuprofen in children and ... [https://pubmed.ncbi.nlm.nih.gov/40288559/]
- 77. Signal management | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/human-regulatory-overview/post-authorisation/pharmacovigilance-post-authorisation/signal-management]
- 78. What Is Pharmacovigilance? A 2025 Guide for Pharma ... [https://www.vitrana.com/what-is-pharmacovigilance-a-2025-guide-for-pharma-leaders/]
- 79. Interplay of Spontaneous Reporting and Longitudinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12334467/]
- 80. Signal Detection in Pharmacovigilance;2025 Guide [https://pharmuni.com/2025/11/19/signal-detection-in-pharmacovigilance-methods-steps-and-types-of-signals/]
- 81. Signal Detection & Management Mastery in ... [https://ccrps.org/clinical-research-blog/signal-detection-amp-management-mastery-in-pharmacovigilance]
- 82. Artificial intelligence in pharmacovigilance: advancing drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317250/]
- 83. Place-Based Drivers of Mortality: Evidence from Migration [https://pmc.ncbi.nlm.nih.gov/articles/PMC8653912/]
- 84. Place-Based Variation in Health Care: Evidence from ... [https://www.nber.org/papers/w34204]
- 85. Regional variation in health care utilization and mortality [https://www.sciencedirect.com/science/article/pii/S0167629619303819]
- 86. From facility to home: How healthcare could shift by 2025 [https://www.mckinsey.com/industries/healthcare/our-insights/from-facility-to-home-how-healthcare-could-shift-by-2025]
- 87. Welfare states and social mobility: How educational and ... [https://www.sciencedirect.com/science/article/abs/pii/S0276562406000503]
- 88. Who Relocates Most by Age, Income & Family? [https://murphymovers.com/blog/2025/august/who-moves-the-most-surprising-moving-stats-by-age-income-family-status/]
- 89. An Empirical Analysis of Health-Dependent Utility on SHARE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9559118/]
- 90. Impact of adult son migration on the health wellbeing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455820/]