Mapping the Mind-Behavior Link: A Guide to DT-MRI Fiber Tracking for Research and Drug Development
Diffusion-Tensor Magnetic Resonance Imaging (DT-MRI) fiber tracking has emerged as a powerful, non-invasive tool for visualizing the brain's structural connectivity, providing critical insights for behavioral studies and clinical drug development.
Mapping the Mind-Behavior Link: A Guide to DT-MRI Fiber Tracking for Research and Drug Development
Abstract
Diffusion-Tensor Magnetic Resonance Imaging (DT-MRI) fiber tracking has emerged as a powerful, non-invasive tool for visualizing the brain's structural connectivity, providing critical insights for behavioral studies and clinical drug development. This article explores the foundational principles of DT-MRI, detailing how it maps white matter pathways by measuring the directional diffusion of water. It delves into methodological applications, from investigating neurological disorders like autism to its role in clinical trials for assessing drug efficacy. The content also addresses key technical challenges and optimization strategies, such as mitigating CSF partial volume effects with FLAIR-DTI and improving signal-to-noise. Finally, it examines the validation of DT-MRI against other neuroscientific methods and its growing use as a biomarker in pharmaceutical research, offering a comprehensive resource for scientists and drug development professionals.
The Neural Blueprint: Understanding DT-MRI Fundamentals and Its Role in Behavioral Neuroscience
Diffusion Tensor Magnetic Resonance Imaging (DT-MRI) leverages the inherent anisotropic diffusion of water molecules in neural tissues to non-invasively map the brain's structural connectivity. Within the tightly packed, myelinated axons of white matter, the movement of water is restricted across the fibers but occurs relatively freely along the axonal length [1] [2]. This direction-dependent water mobility is known as anisotropic diffusion. DT-MRI captures this phenomenon, allowing researchers to infer the orientation, integrity, and trajectory of white matter tracts [3] [4]. In behavioral studies research, this provides a powerful tool to investigate the microstructural neural pathways that underlie behavior, cognitive functions, and the effects of pharmacological interventions, linking brain structure directly to function.
Key Quantitative DTI Metrics for Behavioral Research
DTI provides several quantitative metrics that serve as sensitive probes of white matter microstructure. These metrics are crucial for comparing patient groups, tracking disease progression, or assessing treatment effects in behavioral and drug development studies.
Table 1: Key DTI Scalar Metrics and Their Interpretation
| Metric | Full Name | Biological/Structural Correlation | Application in Behavioral Research |
|---|---|---|---|
| FA (Fractional Anisotropy) | Fractional Anisotropy | Degree of directionality of water diffusion; reflects axonal density, myelination, and fiber coherence [3] [2]. | A primary indicator of white matter integrity; reductions correlate with cognitive deficits in TBI [2], MS [5], and aging. |
| MD (Mean Diffusivity) | Mean Diffusivity | The overall magnitude of water diffusion, inversely related to cellular density [3] [2]. | Increased MD suggests edema, necrosis, or reduced tissue density; useful in early stroke detection and neurodegenerative studies [3] [2]. |
| AD (Axial Diffusivity) | Axial Diffusivity | The rate of diffusion parallel to the primary axon direction [2]. | Positively correlates with brain maturation; decreases may indicate axonal damage or degeneration [2]. |
| RD (Radial Diffusivity) | Radial Diffusivity | The rate of diffusion perpendicular to the primary axon direction [2]. | Increased RD is a marker of demyelination pathologies, as in multiple sclerosis [2]. |
Table 2: Example DTI Metric Values in Health and Pathology
| Brain Region / Condition | FA Value (Approx.) | MD Value (x 10⁻³ mm²/s) | Notes |
|---|---|---|---|
| Adult Corpus Callosum | ~0.7-0.8 [5] | ~0.7-0.9 [5] | Highly anisotropic due to coherently packed fibers. |
| Isotropic CSF | ~0 | ~3.0 | Free, unrestricted diffusion [3]. |
| Normal Brain Parenchyma | Varies by region | ~1.95-2.2 [3] | Relative uniformity in healthy white/gray matter. |
| Multiple Sclerosis (Lesion) | Decreased [5] | Increased [5] | Reflects loss of structural integrity and demyelination. |
| Traumatic Brain Injury | Decreased [2] | Increased [2] | Indicates axonal injury and edema. |
Experimental Protocol for DTI Acquisition and Analysis
This protocol outlines a standardized methodology for acquiring and processing DTI data suitable for multi-site behavioral studies, incorporating best practices for data quality.
Data Acquisition Protocol
Scanner Settings:
- Pulse Sequence: Single-shot spin-echo echo-planar imaging (EPI) is standard.
- Diffusion Weighting: Use a minimum of 30 diffusion-encoding directions to ensure robust tensor estimation [2] [6]. For more complex modeling, 64 or more directions are recommended.
- b-values: A b-value of 700-1000 s/mm² is standard for single-shell acquisition. Multi-shell protocols (e.g., b=700, 2000 s/mm²) enhance sensitivity to different tissue compartments [7].
- Number of b=0 images: Acquire at least 4-8 non-diffusion-weighted (b=0) volumes interspersed throughout the acquisition for accurate reference [7].
- Spatial Resolution: Isotropic voxels of 2.0-2.5 mm are typical. Higher resolution improves specificity but reduces signal-to-noise ratio (SNR) [2].
- Echo Time (TE): Use the minimum possible TE to maximize SNR. Note that DTI metrics like FA and MD can be TE-dependent [7].
Data Preprocessing Workflow
Preprocessing is critical for mitigating artifacts and ensuring data quality. The following workflow should be applied using software like FSL, MRtrix3, or similar.
Tensor Fitting and Tractography
- Tensor Model Fitting: The diffusion tensor is calculated at each voxel by solving the Stejskal-Tanner equation using a least-squares or robust fitting method [3] [4]. This generates maps of FA, MD, AD, and RD.
- Tractography: Deterministic or probabilistic algorithms are used to reconstruct white matter pathways. Streamlines are initiated from seed points and propagated based on the principal diffusion direction (the major eigenvector of the tensor) [4]. For behavioral studies, tractography of specific pathways (e.g., corpus callosum, superior longitudinal fasciculus) is common.
Advanced Methodologies and Considerations
Protocol Optimization for Clinical Trials
For multi-site pharmaceutical trials, protocol harmonization is essential.
- Spatial Error Correction: Gradient field inhomogeneities can introduce systematic errors. Methods like the B-matrix Spatial Distribution (BSD-DTI) can correct these, improving metric accuracy and cross-site comparability [5].
- Accelerated Acquisitions: Deep learning methods, such as the Self-Supervised Deep Learning with Fine-Tuning (SSDLFT) framework, can generate high-quality tensor maps from a reduced number of DWIs, cutting acquisition time and mitigating motion artifacts [6].
- The "Human Phantom": Scanning a single healthy subject across all scanners in a trial establishes a scaling factor, enabling direct comparison of DTI metrics from different hardware [2].
Multi-Parametric Diffusion Imaging
Conventional DTI is limited in regions of complex fiber architecture (e.g., crossing fibers). Advanced models provide more biological specificity.
- Multi-TE DTI: Acquiring data at multiple echo times helps disentangle diffusion effects from T2 relaxation, reducing bias in microstructural parameters [7].
- Beyond the Tensor: Techniques like Neurite Orientation Dispersion and Density Imaging (NODDI) or diffusion spectrum imaging (DSI) model crossing fibers more effectively and provide estimates of intracellular volume fraction and orientation dispersion [7].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagents and Computational Tools for DTI Analysis
| Tool/Resource | Category | Function/Brief Explanation | Example Software/Package |
|---|---|---|---|
| Preprocessing Pipelines | Software | Implements the core preprocessing workflow for artifact correction and data preparation. | FSL (TOPUP, EDDY) [7], MRtrix3 (dwidenoise) [7] |
| Tensor Fitting Toolbox | Software | Fits the diffusion tensor model to preprocessed DWI data to generate FA, MD, AD, and RD maps. | FSL (DTIFIT) [7], Dipy (Python) |
| Tractography Algorithm | Software | Reconstructs 3D white matter pathways from tensor fields for connectivity analysis. | FSL (PROBTRACKX), MRtrix3 (tckgen) [4] |
| Anatomical Atlas | Data | Provides reference regions of interest (ROIs) for automated segmentation and quantitative analysis. | JHU White Matter Atlas [7], AAL Atlas |
| Deep Learning Framework | Software | Enables advanced denoising and acceleration of DTI acquisitions, reducing scan times. | TensorFlow, PyTorch (for SSDLFT) [6] |
| B-matrix Spatial Distribution (BSD) | Method/Algorithm | Corrects for spatial systematic errors in diffusion measurements caused by gradient nonuniformities. | Custom implementation [5] |
Diffusion Tensor Imaging (DTI) is a magnetic resonance imaging (MRI) technique that utilizes the phenomenon of water diffusion as a natural source of contrast to investigate the microstructure of biological tissues [5]. In the nervous system, the microstructure of white matter dictates the directionality of water diffusion; water molecules preferentially diffuse along the length of axons rather than across them, a property known as anisotropic diffusion [8]. DTI quantifies this directional water diffusion to infer the organization of white matter tracts in vivo.
The primary mathematical construct in DTI is the diffusion tensor, a 3x3 matrix that is calculated for each image voxel from a series of diffusion-weighted images. From this tensor, several scalar metrics can be derived, each reflecting different microstructural properties [9]. Fractional Anisotropy (FA) represents the degree of directional preference of water diffusion, with values ranging from 0 (perfectly isotropic) to 1 (perfectly anisotropic). Mean Diffusivity (MD) reflects the overall magnitude of diffusion, independent of direction. Axial Diffusivity (AD) measures diffusion parallel to the primary axon orientation, while Radial Diffusivity (RD) measures diffusion perpendicular to the axonal fibers [9]. These metrics provide the foundation for quantitative analysis of white matter integrity.
DTI-based tractography extends this principle by using the directional information from the diffusion tensor to reconstruct the trajectories of white matter pathways throughout the brain [10]. By following the principal direction of diffusion from voxel to voxel, these algorithms can generate three-dimensional reconstructions of neuronal fiber bundles, enabling researchers to visualize and quantify the brain's structural connectivity [11]. This process has become an indispensable tool in both clinical and research settings, particularly for studying how connectivity shapes brain function, development, and cognition [10].
Key DTI Metrics and Their Biological Significance
The quantitative metrics derived from DTI provide crucial information about the microstructural properties of white matter tracts. Understanding the biological correlates of these metrics is essential for proper interpretation of tractography results in behavioral research.
Table 1: Key DTI Metrics and Their Biological Correlates
| DTI Metric | Description | Biological Significance | Interpretation in Pathologies |
|---|---|---|---|
| Fractional Anisotropy (FA) | Degree of directional preference of water diffusion [9] | Axonal integrity, myelination, and fiber density [9] | Decreased in various neurological conditions [9] |
| Mean Diffusivity (MD) | Overall magnitude of water diffusion [9] | Membrane density, cellularity [9] | Increases with edema, necrosis; decreases with cellularity [9] |
| Axial Diffusivity (AD) | Diffusion parallel to the axonal fibers [9] | Axonal integrity [9] | Decreases with axonal damage [9] |
| Radial Diffusivity (RD) | Diffusion perpendicular to the axonal fibers [9] | Myelin integrity [9] | Increases with myelin damage [9] |
These DTI scalars are particularly valuable in behavioral studies as they provide sensitive measures of microstructural changes that may underlie cognitive functions or behavioral deficits. For instance, decreased FA in the corticospinal tract has been investigated as a potential biomarker in amyotrophic lateral sclerosis, while alterations in multiple DTI parameters have been documented in conditions such as multiple sclerosis, Parkinson's disease, and Alzheimer's dementia [9]. It is important to note that while FA is highly sensitive to microstructural changes, it lacks specificity; therefore, the combined use of multiple DTI scalars (AD, RD, MD) is recommended for more comprehensive characterization of white matter microstructure [9].
Tractography Process: From Data Acquisition to 3D Model
The journey from raw MRI signals to a three-dimensional tractography model involves a multi-stage processing pipeline, each step requiring careful consideration to ensure accurate and biologically plausible results.
Data Acquisition and Preprocessing
The foundation of reliable tractography lies in high-quality diffusion-weighted data acquisition. A typical research-grade protocol uses a multi-shell acquisition scheme with a minimum of 30 diffusion encoding directions distributed across multiple b-values (e.g., b=0 s/mm² and b=800-1000 s/mm²) [11] [12]. The acquisition should be optimized to maximize signal-to-noise ratio while minimizing artifacts. Critical parameters include echo time (TE), repetition time (TR), field of view (FOV), and voxel size, with contemporary studies often employing voxel dimensions of approximately 2.5 mm isotropic or smaller [11].
Preprocessing is crucial for correcting various artifacts that can compromise data quality. Essential preprocessing steps include:
- Motion Correction: Compensation for subject movement during acquisition using rigid body registration [11] [13].
- Eddy Current Correction: Addressing distortions induced by rapidly switching diffusion gradients [11].
- Susceptibility Distortion Correction: Correcting for geometric distortions caused by magnetic field inhomogeneities, often using reverse phase-encoded images and tools like FSL's TOPUP [11] [14].
- B-matrix Spatial Distribution (BSD) Correction: Accounting for spatial systematic errors in diffusion measurements caused by gradient field inhomogeneities [5].
Following these corrections, the diffusion tensor is calculated at each voxel, and DTI-derived metrics (FA, MD, AD, RD) are computed for subsequent analysis.
Fiber Tracking Algorithms and Reconstruction
Fiber tracking algorithms use the directional information from the diffusion tensor to reconstruct continuous pathways through the white matter. The most common approaches include deterministic and probabilistic methods. Deterministic algorithms, such as Fiber Assignment by Continuous Tracking (FACT), follow the principal diffusion direction at each voxel in a continuous path [8]. These algorithms typically employ stopping criteria based on FA thresholds (commonly 0.15-0.2) and maximum allowable curvature between successive points (typically 45-60 degrees) to prevent biologically implausible trajectories [11] [13].
In practice, tractography often employs region-of-interest (ROI) approaches to reconstruct specific white matter pathways. For example, reconstructing the Frontal Aslant Tract (FAT) may involve placing ROIs in the Superior Frontal Gyrus (SFG) and pars opercularis of the Inferior Frontal Gyrus (IFG) [11]. The accuracy of the reconstructed pathways depends heavily on the appropriate selection of these anatomical landmarks.
Visualization and Interpretation
Effective visualization of tractography results is essential for both qualitative assessment and quantitative analysis. Streamlines, which are continuous curves following the direction of the vector field, are the most common visualization method [10]. These are often displayed as illuminated streamtubes with color encoding based on direction (red for left-right, green for anterior-posterior, blue for superior-inferior) or based on quantitative scalar values such as FA [15].
When creating visualizations for publication or clinical interpretation, careful attention must be paid to color map selection. perceptually uniform color maps with high overall lightness contrast are recommended to ensure accurate representation of data and accessibility for individuals with color vision deficiencies [15]. The rainbow color palette should be avoided due to its non-uniform color gradient and potential for misleading interpretation [15].
Experimental Protocols for DTI Tractography
Protocol 1: Standardized DTI Acquisition for Behavioral Studies
This protocol outlines a standardized approach for DTI data acquisition suitable for investigating white matter correlates of behavior.
Materials and Equipment:
- 3T MRI scanner with high-performance gradient system
- Multi-channel head coil (32-channel or higher recommended)
- Compatible DTI acquisition sequence (typically spin-echo EPI)
- Physiological monitoring equipment (cardiac and respiratory monitoring)
- Head stabilization equipment (foam padding, tape)
Acquisition Parameters:
- Pulse Sequence: Spin-echo echo-planar imaging (SE-EPI)
- Diffusion Directions: Minimum 30 non-collinear directions
- b-values: b=0 s/mm² (non-diffusion weighted) and b=800-1000 s/mm²
- Field of View: 224×224 mm (adjusted to head size)
- Matrix Size: 96×96 (reconstructed to 128×128)
- Slice Thickness: 2.5 mm isotropic voxels
- Repetition Time/Echo Time: TR=3232 ms, TE=85 ms (minimized)
- Parallel Imaging: SENSE factor=2-3
- Number of Averages: 2 for improved signal-to-noise ratio
Procedure:
- Position the subject supine on the scanner bed with head securely stabilized.
- Align the anterior commissure-posterior commissure (AC-PC) line with the laser positioning system.
- Perform automated shimming to optimize magnetic field homogeneity.
- Acquire localizer scans and plan the DTI volume to cover the entire brain.
- Run the DTI acquisition sequence, monitoring for subject motion.
- Acquire reverse phase-encoded b=0 images for distortion correction.
Quality Control:
- Visually inspect raw DWI for artifacts (ghosting, signal dropouts)
- Calculate signal-to-noise ratio (SNR) in the b=0 images
- Check for excessive motion using framewise displacement metrics
Protocol 2: Tract-Specific Analysis of the Frontal Aslant Tract
This protocol provides a detailed methodology for reconstructing and analyzing the Frontal Aslant Tract (FAT), a pathway relevant to language and executive functions, using DSI Studio software [11].
Table 2: Quantitative Characteristics of the Frontal Aslant Tract (FAT) [11]
| Parameter | Left Hemisphere | Right Hemisphere | Age-Related Changes |
|---|---|---|---|
| Streamline Count | Higher (left dominance) [11] | Lower [11] | Not specified |
| Fiber Volume | Larger (left dominance) [11] | Smaller [11] | Not specified |
| Mean FA | Not specified | Not specified | Lower in patients >55 years [11] |
| Mean MD | Not specified | Not specified | Higher in patients >55 years [11] |
| Optimal ROI | SFG to IFG pars opercularis [11] | SFG to IFG pars opercularis [11] | Not applicable |
Materials and Software:
- DSI Studio (http://dsi-studio.labsolver.org)
- Preprocessed DTI data in NIFTI format
- ICBM152 adult brain anatomical atlas (embedded in DSI Studio)
Fiber Tracking Parameters:
- Tracking Algorithm: Deterministic fiber tracking
- Method: Generalized Q-Sampling Imaging (GQI)
- Angular Threshold: 60 degrees
- FA Threshold: Determined automatically by software
- Step Size: 1.25 mm
- Maximum Length: 400 mm
- Minimum Length: 30 mm
- Streamline Count: 20,000
- Pruning: 2 iterations of topology-informed pruning
Reconstruction Procedure:
- Import preprocessed DWI data into DSI Studio and reconstruct diffusion data using GQI.
- Navigate to the "Tractography" tab and select "ROI-based tracking."
- For FAT reconstruction, define the first ROI in the Superior Frontal Gyrus (SFG) using the ICBM152 atlas.
- Define the second ROI in the pars opercularis of the Inferior Frontal Gyrus (IFG).
- Execute the tracking algorithm and apply pruning to remove false connections.
- Visually inspect the resulting tract for anatomical accuracy.
- Export quantitative metrics (streamline count, mean length, volume, FA, MD) for statistical analysis.
Validation Steps:
- Verify that the reconstructed FAT follows the known anatomical trajectory between SFG and IFG.
- Confirm the absence of streamlines extending into adjacent tracts (corticospinal tract, fronto-striatal tracts).
- Ensure reproducibility by repeating the tracking with slight variations in ROI placement.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of DTI tractography requires both specialized software tools and careful attention to methodological details. The following table summarizes key resources for conducting tractography research.
Table 3: Essential Software Tools for DTI Tractography Research
| Tool Name | Primary Function | Key Features | Platform Compatibility |
|---|---|---|---|
| DSI Studio [14] | Comprehensive diffusion MRI analysis | Deterministic & probabilistic tracking, multiple diffusion models (DTI, GQI), connectome mapping | Windows, macOS, Linux |
| FSL TBSS [9] | Voxel-based analysis of DTI data | Skeleton-based cross-subject alignment, group statistics, multiple DTI scalars | Windows, macOS, Linux |
| MRtrix [9] | Advanced diffusion MRI analysis | Fiber orientation distribution estimation, anatomically constrained tractography, fixel-based analysis | Windows, macOS, Linux |
| FreeSurfer TRACULA [9] | Automated probabilistic tractography | Reconstruction of 18 major pathways using prior anatomical information | Windows, macOS, Linux |
| DTI Studio [9] | Basic DTI processing and tracking | Fiber tracking with FACT algorithm, eddy-current correction, color mapping | Windows |
When selecting and using these tools, researchers should consider that different software packages can produce varying results due to differences in underlying algorithms and methodologies. A comparative study of four DTI software packages found substantial inter-rater agreement but poor between-software agreement for quantitative DTI metrics, highlighting the importance of consistent tool usage throughout a study [12].
Applications in Behavioral Research and Methodological Considerations
DTI tractography offers powerful applications for behavioral neuroscience and clinical research, particularly for investigating the structural correlates of cognitive functions and behavioral deficits. The technique has been successfully applied to study neural pathways in various domains.
In language research, tractography has been used to delineate the Frontal Aslant Tract (FAT), which connects the superior and inferior frontal gyri. This pathway plays crucial roles in verbal fluency, sentence formation, and lexical decision-making [11]. Damage to the FAT is associated with deficits in speech output and difficulties in recognizing the meaning of homophonic words, highlighting its importance in language processing [11]. Studies have consistently shown left-hemisphere dominance of the FAT, characterized by higher streamline counts and fiber volumes in the left hemisphere compared to the right [11].
When applying tractography in behavioral studies, several methodological considerations are essential:
- Cross-Scanner Compatibility: DTI metrics show limited comparability across different scanners and protocols due to dependence on MRI hardware and sequence-specific parameters [5].
- Spatial Error Correction: Implementation of B-matrix Spatial Distribution (BSD-DTI) correction is recommended to address spatial systematic errors in diffusion measurements [5].
- Age Matching: Age-related changes in DTI metrics (increased MD, decreased FA in older individuals) necessitate careful age-matching in case-control studies [11].
- Multi-Modal Validation: Where possible, tractography results should be validated with complementary techniques, such as intraoperative electrical stimulation in clinical populations or histology in experimental models [14].
With appropriate methodological rigor, DTI tractography serves as a powerful approach for investigating the structural basis of behavior, potentially contributing to the development of biomarkers for neurological and psychiatric conditions and enhancing our understanding of brain-behavior relationships.
Diffusion Tensor Imaging (DTI) is an advanced magnetic resonance imaging (MRI) modality that leverages the Brownian motion of water molecules to non-invasively visualize and quantify the brain's white matter architecture [2]. By measuring the directionality and magnitude of water diffusion, DTI provides unique insights into the microstructure of neural pathways. The core principle underpinning DTI is that in organized tissues like white matter tracts, water diffusion is anisotropic, meaning it moves more freely in directions parallel to the axonal fibers rather than perpendicular to them [2]. This directional preference allows researchers to infer the location, orientation, and integrity of major white matter pathways, creating a virtual map of the brain's structural connectivity. In behavioral studies, this is paramount, as behavior emerges from complex interactions between distributed brain networks, all communicating via these white matter highways. Understanding the link between the structural integrity of these pathways and their functional behavioral outcomes is a key objective in modern neuroscience and drug development research.
Key Quantitative Metrics in DTI Analysis
DTI provides several quantitative metrics that serve as indirect biomarkers of white matter microstructural integrity. These metrics are derived from the diffusion tensor and are sensitive to various pathological and developmental changes.
Fractional Anisotropy (FA) is a scalar value between 0 and 1 that reflects the degree of directional preference of water diffusion [2]. A value of 0 represents perfectly isotropic diffusion (equal in all directions), while a value close to 1 indicates highly anisotropic diffusion (primarily along one axis). Reduced FA in a white matter tract is often interpreted as a sign of microstructural disorganization, which can be caused by axonal damage, demyelination, or decreased fiber density [2]. It is highly sensitive to changes but can be nonspecific to the exact underlying cause.
Mean Diffusivity (MD) or Apparent Diffusion Coefficient (ADC), quantifies the overall magnitude of water diffusion, irrespective of direction [2]. It is influenced by cellular density and the presence of barriers to diffusion. Increased MD is often associated with edema, necrosis, or overall tissue breakdown, where water movement becomes less restricted.
To provide a clearer understanding, the following table summarizes these primary DTI metrics, their biological correlates, and how they are interpreted in behavioral research:
Table 1: Key Quantitative DTI Metrics for Behavioral Studies
| Metric | Description | Biological Correlate | Interpretation in Behavior Studies |
|---|---|---|---|
| Fractional Anisotropy (FA) | Degree of directionality of water diffusion [2] | Axonal membrane integrity, myelination, fiber density [2] | Decrease may indicate white matter disorganization linked to cognitive or motor deficits [2] |
| Mean Diffusivity (MD) / Apparent Diffusion Coefficient (ADC) | Overall magnitude of water diffusion [2] | Cellularity, membrane density, viability [2] | Increase often suggests edema, inflammation, or tissue loss |
| Axial Diffusivity (AD) | Rate of diffusion parallel to the primary axon orientation [2] | Axonal integrity and damage [2] | Decrease may reflect axonal injury |
| Radial Diffusivity (RD) | Rate of diffusion perpendicular to the primary axon orientation [2] | Myelin integrity [2] | Increase is strongly associated with demyelination |
These metrics allow researchers to move beyond simple anatomy and form quantitative hypotheses about how specific structural properties of white matter tracts underpin individual differences in behavior, symptom severity, or treatment response.
Automated White Matter Tract Segmentation Methods
A critical step in DTI analysis is white matter tract segmentation, the process of identifying and delineating specific white matter bundles from whole-brain tractography data. While manual dissection by experts is considered the gold standard, it is time-consuming and subject to operator bias [16]. Consequently, automated methods have been developed to standardize and accelerate this process. A systematic review of the literature from 2013 to 2023 identified 59 key studies, which can be broadly categorized into five main approaches [16].
The following table summarizes these automated methods, their underlying principles, and key characteristics:
Table 2: Categories of Automated White Matter Tract Segmentation Methods
| Method Category | Proportion of Studies | Core Principle | Key Characteristics |
|---|---|---|---|
| Direct Voxel-Based | 27% | Uses voxel-wise diffusion metrics (e.g., FA, MD) to classify tracts without explicit streamlines [16] | Fast; good for population studies; may struggle with complex crossing fibers [16] |
| Streamline-Based Clustering | 25% | Groups whole-brain tractography streamlines based on similarity in their geometric or spatial properties [16] | Data-driven; useful for exploring tractography data; cluster interpretation can be challenging [16] |
| Streamline-Based Classification | 20% | Assigns whole-brain tractography streamlines to predefined tract labels using a classifier [16] | Requires a training atlas; can be highly accurate for known tracts [16] |
| Atlas-Based | 14% | Applies a pre-existing anatomical atlas to new subject data, often via registration [16] | Straightforward; efficient; accuracy depends on registration quality to the atlas [16] |
| Hybrid | 14% | Combines elements from two or more of the above categories to leverage their strengths [16] | Aims to improve robustness and accuracy; can be more complex to implement [16] |
The choice of method depends on the research question, the available computational resources, and the need for either a pre-defined tract of interest or a more exploratory, data-driven approach. Hybrid methods are increasingly popular as they seek to overcome the limitations of any single approach.
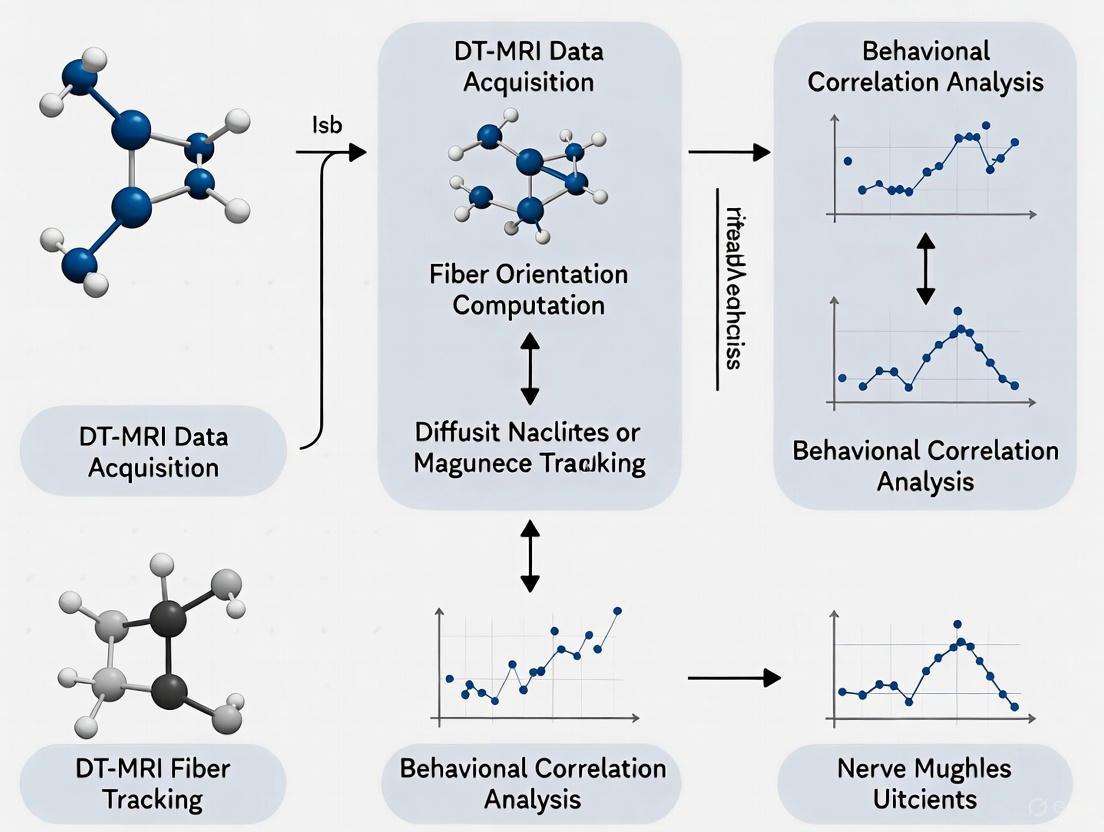
The workflow for automating tract segmentation typically involves a multi-stage process that integrates several of these concepts, as illustrated below:
Diagram 1: Automated Tract Segmentation Workflow
Experimental Protocol: DTI Data Acquisition and Preprocessing
This protocol outlines a standardized pipeline for acquiring and preparing DTI data for subsequent tract segmentation and analysis in a behavioral research context.
Equipment and Reagents
Table 3: Research Reagent Solutions and Essential Materials for DTI Studies
| Item | Function/Description | Example/Note |
|---|---|---|
| MRI Scanner | Acquisition of diffusion-weighted images. | 3T MRI scanner recommended for optimal balance of signal-to-noise and resolution [2]. |
| Head Coil | Signal reception from the brain. | Use a multi-channel head coil (e.g., 32-channel) for improved image quality. |
| Data Processing Server | Running computationally intensive preprocessing and analysis. | Linux-based system recommended; requires sufficient RAM and CPU cores. |
| dMRI Processing Software | Data preprocessing and analysis. | FSL (FMRIB Software Library), MRtrix3, or DSI Studio. |
| T1-weighted MPRAGE Sequence | Provides high-resolution anatomical reference. | Used for co-registration and spatial normalization. |
| Diffusion Phantoms | Quality control and cross-scanner harmonization. | "Human phantoms" can be used to compare metrics across different scanners [2]. |
Step-by-Step Procedure
1. Participant Preparation and Data Acquisition: - Safety Screening: Conduct a standard MRI safety screening for all participants. - Head Stabilization: Use foam padding to minimize head motion and instruct the participant to remain still. Explain that the procedure will involve loud knocking noises. - Sequence Parameters: Acquire diffusion-weighted images using a spin-echo echo-planar imaging (EPI) sequence. Typical parameters include: - b-values: A minimum of two b-values are required. Use a low b-value (e.g., b=0 s/mm²) and at least one high b-value (e.g., b=1000 s/mm²). Higher b-values increase sensitivity to diffusion but reduce signal-to-noise. - Diffusion Directions: Acquire diffusion gradients in at least 6 non-collinear directions, though more directions (e.g., 33, 64) significantly improve the accuracy of the tensor estimation and the reliability of subsequent tractography [2]. - Other Parameters: Isotropic voxel size of ~2 mm, TR/TE optimized for the specific scanner and sequence.
2. Data Preprocessing:
- Data Conversion: Convert raw scanner data from DICOM format to a more processing-friendly format (e.g., NIfTI) using tools like dcm2niix [17].
- Noise and Artifact Correction:
- Eddy Current Correction: Correct for distortions and subject movements using tools like eddy in FSL.
- B0 Field Distortion Correction: Use acquired B0 field maps or reverse phase-encoded b=0 images with tools like topup in FSL to correct for susceptibility-induced distortions.
- Skull Stripping: Remove non-brain tissue from the images using tools like BET (Brain Extraction Tool) in FSL.
- Tensor Estimation: Fit a diffusion tensor model to each voxel to generate maps of FA, MD, AD, and RD.
Experimental Protocol: Tract-Specific Analysis and Behavioral Correlation
This protocol details the steps for segmenting a specific white matter tract and statistically linking its microstructural properties to behavioral measures.
The Scientist's Toolkit
- Software for Tract Segmentation: Depending on the chosen method (see Table 2), tools like
TRACULA(atlas-based),AFQ(Atlas-Based Fiber Quantification), or custom scripts inMRtrix3orDSI Studiocan be used. - Statistical Software: Platforms like R, Python (with Pandas, Scipy, Statsmodels), SPSS, or MATLAB for performing correlation and regression analyses.
- Behavioral Assessment Battery: Standardized tests selected based on the hypothesis. For example:
- Executive Function: Trail Making Test (TMT), Stroop Test.
- Memory: California Verbal Learning Test (CVLT), Wechsler Memory Scale (WMS).
- Processing Speed: Digit Symbol Coding Test.
Step-by-Step Procedure
1. Tract Segmentation: - Method Selection: Choose an automated segmentation method appropriate for your tract of interest (e.g., Atlas-Based for well-known tracts like the Corpus Callosum or Corticospinal Tract). - Execution: Run the selected segmentation algorithm on your preprocessed DTI data. For instance, using an atlas-based method involves non-linearly registering the individual's FA map to a standard template, then applying the pre-defined tract atlas in the template space back to the native individual space. - Quality Control: Visually inspect the resulting segmented tracts for each subject to ensure anatomical plausibility. Exclude subjects with poor segmentation results.
2. Metric Extraction: - For each successfully segmented tract, extract the mean or median values of the DTI metrics (FA, MD, etc.) across all voxels or streamlines within that tract. This provides a single, summary measure of microstructural integrity for each tract per participant.
3. Behavioral Data Preparation: - Score the raw data from the behavioral assessments according to their standardized manuals. This typically results in summary scores (e.g., time to completion, number of errors, standardized T-scores).
4. Statistical Analysis: - Data Screening: Check all variables for normality and the presence of outliers. Apply transformations if necessary. - Correlational Analysis: Perform Pearson or Spearman correlations between the tract-specific DTI metric (e.g., FA of the Arcuate Fasciculus) and the behavioral score (e.g., verbal fluency score). - Multiple Regression: To control for potential confounds such as age, sex, or overall brain volume, perform a multiple regression analysis with the behavioral score as the dependent variable and the DTI metric and covariates as independent variables.
The logical flow of this analytical phase, from segmented tracts to statistical inference, is summarized in the following diagram:
Diagram 2: From Tract Segmentation to Behavioral Correlation
Application in Drug Development and Behavioral Research
DTI serves as a powerful tool for providing objective, quantifiable biomarkers in clinical trials for neurological and psychiatric disorders. In the context of drug development, it can be applied in several key areas:
- Target Engagement: Demonstrating that an investigational drug intended to promote remyelination (e.g., for Multiple Sclerosis) actually produces a biological effect on its intended target. A successful drug might manifest as a significant decrease in Radial Diffusivity (RD) in relevant tracts, indicating improved myelin integrity [2].
- Patient Stratification: DTI metrics can be used to identify patient subgroups with specific patterns of white matter pathology. This enables enrollment of a more homogeneous population in a clinical trial, potentially increasing the trial's sensitivity to detect a drug effect.
- Monitoring Progression and Treatment Response: DTI can be used as a secondary or exploratory endpoint to track the natural progression of a disease or the efficacy of an intervention over time. For example, in a traumatic brain injury (TBI) trial, a drug that slows neurodegeneration might result in the stabilization of FA values in the corpus callosum over time, whereas the placebo group might show a decline [2].
- Linking Mechanism to Behavior: The ultimate goal is to connect a drug's biological action to a meaningful functional outcome. A compelling finding would be a statistically significant correlation between a drug-induced change in a DTI metric (e.g., an increase in FA in the Uncinate Fasciculus) and an improvement on a behavioral test (e.g., a reduction in negative symptoms in schizophrenia) [2]. This triad of evidence—drug effect on biomarker, drug effect on behavior, and correlation between biomarker and behavior—provides strong support for the treatment's mechanism of action.
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition characterized by persistent challenges in social communication and interaction, as well as restricted and repetitive patterns of behavior [18]. The neurobiological basis of ASD is increasingly understood as a disorder of neural connectivity, with growing evidence from diffusion tensor magnetic resonance imaging (DT-MRI) revealing consistent abnormalities in the brain's white matter architecture [19] [20]. This case study explores how DT-MRI fiber tracking techniques have uncovered specific fiber pathway abnormalities in ASD, with particular focus on pathways critical for social functioning.
The investigation of neural connectivity in ASD has evolved from initial observations of paradoxical cognitive profiles, where individuals might exhibit excellent rote memory while struggling with complex information processing [19]. This profile suggested impairments in distributed neural networks rather than isolated brain regions. White matter tracts serve as the brain's communication highways, enabling efficient information transfer between distant brain regions [19]. DT-MRI provides a non-invasive window into the microstructure of these tracts, allowing researchers to identify and characterize connectivity abnormalities that may underlie core ASD symptoms.
DT-MRI Principles and Relevance to ASD
Fundamental DT-MRI Metrics
Diffusion Tensor Imaging (DT-MRI) measures the directional dependence of water molecule diffusion in biological tissues [19]. In organized white matter tracts, water diffusion is restricted perpendicular to the axonal fibers due to structural barriers like cell membranes and myelin sheaths. This directional dependence, called diffusion anisotropy, forms the basis for inferring microstructural properties of white matter pathways [19].
Key DT-MRI metrics include:
- Fractional Anisotropy (FA): Quantifies the degree of directional water diffusion (0 = perfectly isotropic, 1 = perfectly anisotropic). Higher FA typically indicates more coherently organized fiber tracts [19].
- Mean Diffusivity (MD): Represents the overall magnitude of water diffusion, sensitive to cellular density and integrity [19].
- Axial Diffusivity (AD): Measures water diffusion parallel to the primary fiber orientation [19].
- Radial Diffusivity (RD): Quantifies diffusion perpendicular to the main fiber direction, sensitive to myelination and axonal membrane integrity [19].
DT-MRI Application to ASD Pathophysiology
In ASD research, DT-MRI has proven particularly valuable because it can detect microstructural alterations that may not be visible with conventional structural MRI [21]. The technique's sensitivity to axonal organization and myelination patterns makes it ideal for investigating the "underconnectivity" theory of ASD, which proposes reduced coordination between different brain regions as a core feature of the condition [20].
Studies applying DT-MRI to ASD have consistently identified a pattern of decreased FA accompanied by increased RD across multiple white matter tracts, suggesting potential disruptions in myelination or axonal organization [19] [18]. These findings align with histological studies reporting abnormal minicolumnar organization in the brains of individuals with ASD, which would necessarily affect white matter connectivity patterns [19] [20].
Key Findings: Fiber Pathway Abnormalities in ASD
Consistent Regional Abnormalities
Comprehensive reviews of DT-MRI studies in ASD have identified consistent white matter abnormalities across multiple brain regions, though the specific pattern may vary by age and clinical presentation [19] [18]. The most consistently affected tracts include:
Table 1: Consistently Identified White Matter Abnormalities in ASD
| Brain Region/Tract | Primary DT-MRI Findings | Functional Correlates |
|---|---|---|
| Corpus Callosum | Decreased FA, Increased RD [19] [22] | Interhemispheric communication; motor skills and complex information processing [19] |
| Cingulum Bundles | Decreased FA, Increased MD [19] | Executive function, emotional regulation [19] |
| Temporal Lobe Tracts | Decreased FA, Altered AD/RD [19] | Social functioning, face processing [19] [20] |
| Frontal Projection Fibers | Variable FA changes [18] | Higher-order cognition, planning |
A recent study of 90 children with ASD (aged 1-6 years) found distinctive lateralization patterns, with higher FA values in the right genu of corpus callosum, splenium of corpus callosum, and superior temporal gyrus compared to the left side [22]. This altered lateralization may reflect aberrant neurodevelopmental trajectories in ASD.
Face Processing Pathway Abnormalities
A focused investigation of white matter pathways involved in face processing provides a compelling case study of ASD-related connectivity abnormalities. The hippocampo-fusiform (HF) and amygdalo-fusiform (AF) pathways, which connect medial temporal lobe structures with the fusiform face area, show distinctive abnormalities in ASD [20] [23].
In high-functioning adolescents and adults with ASD, these pathways demonstrate normal size and shape but abnormal microstructure, characterized by:
- Reduced across-fiber diffusivity (D-min) in the right HF pathway
- Increased across-fiber diffusivity in left HF and bilateral AF pathways
- Loss of typical lateralization compared to controls [20] [23]
These microstructural abnormalities correlate with behavioral measures, as individuals with lower Benton face recognition scores showed more pronounced right HF pathway alterations [20] [23]. This structure-function relationship strengthens the evidence for clinically meaningful connectivity disturbances in ASD.
Developmental Trajectory Considerations
The manifestation of white matter abnormalities in ASD appears to follow a distinct developmental course. While children with ASD often show more prominent alterations, adults with ASD typically demonstrate less pronounced differences compared to neurotypical individuals [18]. This pattern suggests possible compensatory mechanisms or continued brain maturation that may partially normalize white matter organization in adulthood [18].
Table 2: Age-Related Patterns in ASD White Matter Organization
| Age Group | Characteristic DT-MRI Findings | Interpretation |
|---|---|---|
| Infants/Toddlers (1-3 years) | Emerging alterations in corpus callosum and projection fibers [22] | Early deviation from typical developmental trajectory |
| Children (3-11 years) | Prominent decreases in FA across multiple tracts [19] [18] | Peak expression of connectivity differences |
| Adolescents (12-18 years) | Continued alterations, though potentially less pronounced than in childhood [18] | Possible onset of normalization processes |
| Adults (18+ years) | Less prominent differences, regional specificity [18] | Maturation, compensation, or selective persistence |
Experimental Protocols and Methodologies
DT-MRI Data Acquisition Protocol
Standardized acquisition parameters are essential for reproducible DT-MRI findings in ASD research. The following protocol summarizes parameters from multiple studies:
Scanner Requirements: 3T MRI system with multi-channel head coil [22] [24] Sequence: Pulsed-gradient spin-echo echo-planar imaging (PGSE EPI) Key Parameters:
- TR/TE: ~9000/90 ms [22]
- b-values: 0, 1000 s/mm² [22]
- Diffusion directions: 15-64 directions [22] [25]
- Spatial resolution: 1.5-2.5 mm isotropic [22] [25]
- Parallel imaging: SENSE or GRAPPA with acceleration factor 2-4
Quality Control Measures:
- Real-time monitoring for motion artifacts
- Phantom calibration scans for multi-site consistency [26]
- Visual inspection of raw diffusion-weighted images [25]
Fiber Tracking and Analysis Protocol
For investigating specific pathways like the HF and AF pathways, the following analytical approach has been employed:
- Preprocessing:
- Correction for eddy currents and head motion
- Brain extraction (BET from FSL) [25]
- B-matrix spatial distribution correction for gradient nonlinearities (BSD-DTI) [24]
- Tensor Calculation:
- Voxel-wise diffusion tensor estimation
- Generation of FA, MD, AD, and RD maps
- Fiber Tracking:
- Seed region placement in hippocampus, amygdala, and fusiform gyrus [20]
- Deterministic or probabilistic tracking algorithms
- Exclusion of fibers with unrealistic curvature
- Quantitative Analysis:
- Extraction of DT-MRI metrics along fiber pathways
- Statistical comparison between ASD and control groups
- Correlation with behavioral measures (e.g., face recognition scores) [20]
Multi-Site Harmonization Protocol
For multi-site studies, essential for adequate sample sizes in ASD research, data harmonization is critical:
- Pre-acquisition Harmonization:
- Use of same-vendor scanners with standardized protocols [26]
- Traveling phantom studies to characterize cross-site differences [26]
- Post-processing Harmonization:
- Application of ComBat or similar harmonization methods [26]
- Covariate adjustment for site effects while preserving biological variability
- Validation of harmonization effectiveness
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for DT-MRI ASD Research
| Resource Category | Specific Tools/Resources | Primary Function |
|---|---|---|
| MRI Acquisition | 3T MRI systems with multi-channel head coils [22] | High-quality diffusion data acquisition |
| Pulse Sequences | Multi-shell diffusion-weighted sequences [24] [25] | Comprehensive diffusion characterization |
| Analysis Software | FSL, ANTs, Automated Fiber Quantification [26] [27] | Data processing, normalization, fiber tracking |
| Harmonization Tools | ComBat, T-ComBat algorithms [26] | Multi-site data harmonization |
| Quality Control | BSD-DTI correction [24] | Correction of gradient nonlinearities |
| Genetic Analysis | Polygenic scoring methods [25] | Investigation of genetic-structural relationships |
Implications for Research and Therapeutics
The consistent identification of white matter abnormalities in ASD has significant implications for both basic research and clinical applications. From a research perspective, these findings validate network-based approaches to understanding ASD pathophysiology and provide potential biomarkers for tracking disease progression or treatment response [19] [18].
For drug development, DT-MRI metrics could serve as objective outcome measures in clinical trials, particularly for interventions targeting neural connectivity or myelination [19]. The ability to quantify microstructural changes in specific pathways provides a more sensitive assessment tool than behavioral measures alone.
Emerging evidence suggests that white matter alterations in ASD may be a target for emerging interventions, including pharmacological, behavioral, and neuromodulation approaches [19]. The regional specificity of findings (e.g., involvement of face processing pathways in individuals with social perception deficits) opens possibilities for personalized intervention strategies targeting an individual's specific connectivity profile.
DT-MRI fiber tracking has revealed consistent and clinically meaningful abnormalities in the white matter architecture of individuals with ASD. The most robust findings include decreased fractional anisotropy in tracts such as the corpus callosum, cingulum bundles, and temporal lobe pathways, often accompanied by increased radial diffusivity, suggesting potential disruptions in myelination or axonal organization.
The case study of face processing pathways demonstrates how specific fiber pathway abnormalities can be linked to particular behavioral profiles in ASD. Future research directions include:
- Longitudinal studies to clarify developmental trajectories
- Multi-modal integration with functional MRI and genetic data
- Refined harmonization methods for multi-site studies
- Investigation of how white matter alterations relate to heterogeneous clinical presentations in ASD
These findings establish DT-MRI as an essential tool for unraveling the neurobiological underpinnings of ASD and developing targeted interventions for this complex neurodevelopmental condition.
From Theory to Practice: Methodological Approaches and Real-World Applications in Research and Trials
Diffusion Tensor Imaging (DTI) tractography has revolutionized the ability to map white matter pathways in vivo, providing critical insights into neural connectivity underlying complex cognitive functions. This document details the application of DTI tractography to investigate the hippocampo-fusiform (HF) and amygdalo-fusiform (AF) pathways, two distinct white matter bundles interconnecting the mid-fusiform cortex with the hippocampus and amygdala, respectively [28]. These pathways are hypothesized to form a critical neuroanatomical substrate for face processing, linking regions involved in high-order visual perception with those mediating emotional salience and memory consolidation [28] [29]. The integrity of these pathways is of significant interest in behavioral studies and drug development research for conditions like autism spectrum disorder and Alzheimer's disease, where face-processing deficits and aberrant functional connectivity are prominent features [28] [29].
Experimental Protocols & Methodologies
Key DTI Acquisition Parameters
The following parameters, derived from foundational studies, are critical for successful pathway reconstruction [28] [11].
Table 1: DTI Acquisition Protocol for HF/AF Pathway Tracking
| Parameter | Specification | Rationale |
|---|---|---|
| Scanner Field Strength | 1.5T or 3.0T [28] [11] | Higher field strength (3T) provides a better signal-to-noise ratio. |
| Diffusion Encoding Directions | 23 or more [30] [11] | Improved angular resolution for accurate tensor estimation. |
| b-values | ~850 - 1000 s/mm² [28] [30] | Optimizes sensitivity to water diffusion in tissue. |
| Slice Thickness | 2.0 - 2.5 mm [28] [30] | Balances spatial resolution with adequate signal. |
| Number of Averages | 4-10 repeats [28] | Averages multiple scans to enhance signal-to-noise ratio. |
Fiber Tracking and Pathway Selection Protocol
A robust, unbiased tracking approach is essential for probing previously under-described pathways like the HF and AF.
- Whole-Brain Tractography: Initiate tracking from a 1mm cubic grid of seed points throughout the brain. This avoids a priori assumptions about the pathway's location [28].
- Deterministic Tracking Algorithm: Utilize a deterministic streamlines algorithm (e.g., fourth-order Runge-Kutta integration) [30].
- Stopping Criteria: Halt tracking when fractional anisotropy (FA) falls below a threshold of 0.15–0.20 or the turning angle between steps exceeds 30–50 degrees [28] [30].
- Pathway Selection via Spatial Volumes: Use large, anatomically defined spatial selection volumes (SSVs) to isolate the HF and AF pathways from the whole-brain track dataset [28].
- Fusiform SSV: Place an ellipsoidal SSV in the mid-fusiform gyrus, superior to the lateral occipitotemporal sulcus.
- Anteromedial Temporal SSV: Place a second SSV encompassing the amygdala and hippocampal head.
- Boolean Selection: Select only tracks that pass through both the fusiform and the anteromedial temporal SSVs.
- Exclusion: Remove tracks that pass posterior to the mid-fusiform region to prevent inclusion of unrelated visual pathways [28].
- Quality Control: Manually exclude spurious tracts that project to subcortical structures like the cerebellum or thalamus, or that exhibit biologically implausible trajectories (e.g., crossing the midsagittal plane twice) [30].
Quantitative Analysis of Diffusion Metrics
Extract the following microstructural properties from the segmented HF and AF pathways to infer axonal integrity and organization [28] [30].
Table 2: Key Quantitative Diffusion Metrics
| Metric | Description | Biological Interpretation |
|---|---|---|
| Fractional Anisotropy (FA) | Degree of directional water diffusion (0 = isotropic, 1 = anisotropic) | Indicator of white matter integrity; reflects axonal density, myelination, and coherence. |
| Axial Diffusivity (D-ax or D-max) | Rate of water diffusion parallel to the primary axon direction. | Often interpreted as axonal integrity. |
| Radial Diffusivity (D-rad or D-min) | Rate of water diffusion perpendicular to the primary axon direction. | Often inversely related to myelination; higher values may suggest demyelination. |
| Mean Diffusivity (MD) | Overall magnitude of water diffusion, averaged over all directions. | General indicator of cellularity and edema. |
Application Notes: Key Findings and Data
Studies applying the above protocol have yielded consistent quantitative findings on the HF and AF pathways in healthy and clinical populations.
Table 3: Representative Quantitative Data from HF/AF Pathway Studies
| Study Population | Pathway | Key Finding | Reported Values / Effect |
|---|---|---|---|
| Healthy Controls (n=15) [28] | HF & AF | Left-Hemisphere Lateralization | Consistently larger cross-sectional area, higher FA, and lower radial diffusivity (D-min) on the left. |
| Autism Spectrum Disorder (n=17) [29] | Right HF | Abnormally Low Radial Diffusivity (D-min) | Suggested higher axonal packing density or smaller axon diameters, correlating with lower face recognition scores. |
| Autism Spectrum Disorder (n=17) [29] | Left HF & AF | Abnormally High Axial & Radial Diffusivity | Suggested axonal loss or decreased myelination, consistent with a general "under-connectivity" model. |
| Healthy Controls (n=68) [11] | Frontal Aslant Tract (FAT) | Age-Related Microstructural Changes | Higher MD and lower FA in patients >55 years vs. younger patients, demonstrating protocol sensitivity to aging. |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Tools for dMRI Tractography Research
| Tool / "Reagent" | Function / Purpose | Examples & Notes |
|---|---|---|
| dMRI Preprocessing Software | Corrects raw dMRI data for distortions, motion, and eddy currents. | FSL's eddy tool [11], DSI Studio preprocessing modules. |
| Tractography Software Suite | Reconstructs diffusion tensors, performs fiber tracking, and allows visualization. | DSI Studio [11], mrDiffusion, CINCH [30]. |
| Deterministic Tracking Algorithm | Generates streamlines by following the primary diffusion direction step-by-step. | Default algorithm in DSI Studio; used with Runge-Kutta integration [30]. |
| Brain Atlas & ROI Templates | Provides standardized anatomical references for defining seed and target regions. | ICBM152 atlas (built into DSI Studio) [11], Mayo Clinic 3D Brain Atlas [28]. |
| Spatial Selection Volumes (SSVs) | Virtual 3D shapes used to select specific pathways from whole-brain tractograms. | Used in unbiased tracking to isolate pathways without constraining their expected location [28]. |
Visualizing the Experimental Workflow and Anatomy
The following diagrams, generated with Graphviz, illustrate the core experimental workflow and the anatomical relationships of the pathways studied.
Diagram 1: DTI tractography workflow for HF/AF pathways.
Diagram 2: Anatomical schematic of the AF and HF pathways.
Diffusion Tensor Imaging (DTI) is a powerful magnetic resonance imaging (MRI) technique that enables non-invasive investigation of macroscopic axonal organization in nervous system tissues by measuring the directional diffusion of water molecules [31]. Within behavioral neuroscience research, DT-MRI fiber tracking has become an indispensable tool for probing the structural connectivity that underpins behavior, linking neural pathways to cognitive functions and their alterations. The accuracy of this fiber tracking is profoundly influenced by data acquisition parameters, with parallel imaging techniques and slice thickness representing two critical factors that determine the balance between scan time, signal-to-noise ratio (SNR), and spatial resolution. Parallel imaging accelerates data acquisition by using spatial information from multi-channel radiofrequency coils to undersample k-space, while slice thickness directly impacts the precision of tractography reconstructions in the through-plane direction [32] [33]. This Application Note provides detailed protocols and evidence-based recommendations for optimizing these parameters specifically for DT-MRI studies of nerve fiber architecture in behavioral research contexts.
Optimized Acquisition Parameters for DT-MRI Fiber Tracking
Extensive optimization studies have established that high-quality DT-MRI data sufficient for detailed brain fiber tracking can be acquired in clinically feasible scan times by strategically leveraging the SNR advantages of high-field scanners and multi-channel coils. The following table summarizes key parameter combinations and their performance characteristics, based on empirical findings from 3T systems with an 8-channel phased-array head coil [32].
Table 1: Optimized DT-MRI Acquisition Parameters for Brain Fiber Tracking at 3T
| Parameter | Recommended Value | Alternative Ranges | Impact on Tracking Quality |
|---|---|---|---|
| Slice Thickness | 2 mm | 2-3 mm | Enables high-resolution tracking; thinner slices reduce partial volume effects but require higher SNR. |
| b-value | 700 s/mm² | 600-1000 s/mm² | Balances diffusion weighting and signal attenuation; lower values may insufficiently contrast oriented structures. |
| MPG Directions | 6 | 6-32 | Minimum for tensor calculation; more directions improve angular resolution at cost of scan time. |
| Number of Averages | 1 | 1-2 | Feasible due to high intrinsic SNR from parallel imaging; no averaging enables ultra-fast acquisitions. |
| Parallel Imaging Factor | 2-3 (e.g., GRAPPA) | 2-4 | Accelerates acquisition; higher factors reduce SNR and require robust reconstruction. |
| Approximate Scan Time | < 2 minutes | 2-8 minutes | Enables clinical throughput and reduces motion artifact risk in behavioral studies. |
The optimization evidence indicates that with a 2 mm slice thickness, a b-factor of 700 s/mm², 6 motion probing gradient (MPG) directions, and a single average (no signal averaging), DT-MRI data of sufficient quality for robust fiber tracking of major white matter tracts like the pyramidal tract and trigeminal nerve can be obtained in under two minutes [32]. This parameter set represents a sweet spot for many behavioral studies where participant compliance, throughput, and motion minimization are practical concerns.
Experimental Protocol for DT-MRI with Parallel Imaging
Pre-Scanning Preparation and Hardware Requirements
- Scanner and Coils: This protocol is optimized for a 3T MRI scanner equipped with an 8-channel or higher-count phased-array head coil. The high-field strength and multi-channel coil array are prerequisites for achieving the necessary SNR for high-resolution imaging with parallel imaging acceleration [34].
- Subject Stabilization: Use comfortable but firm foam padding to minimize head motion. For behavioral studies involving potential patient populations, consider using a vacuum-bag system for superior immobilization. Provide subjects with earplugs and headphones for hearing protection.
- Cardiac Gating (if applicable): For spinal cord or high-resolution brainstem imaging, implement pulse oximetry-based cardiac gating to mitigate pulsation artifacts.
Step-by-Step Acquisition Protocol
- Localizer and Shimming: Acquire a rapid three-plane localizer scan. Perform automated and, if available, higher-order shimming over the region of interest (e.g., whole brain or specific tract volume) to maximize magnetic field (B0) homogeneity, which is critical for echo-planar imaging (EPI)-based DTI.
- Structural Reference Scan: Acquire a high-resolution 3D T1-weighted anatomical scan (e.g., MPRAGE or SPGR). This will serve as an anatomical reference for fiber tracking and analysis.
- Parameters: Voxel size = 1x1x1 mm³, TR/TI/TE = ~2300/900/3 ms, parallel imaging factor (e.g., SENSE or GRAPPA) = 2.
- DTI Sequence Setup: Use a single-shot spin-echo EPI sequence with dual-spin echo preparation to minimize eddy current-induced distortions.
- Geometry: Match the orientation to the anatomical scan. Set slice thickness to 2 mm with no gap. Use an in-plane resolution of 2x2 mm² or finer (e.g., 1.8x1.8 mm²).
- Diffusion Encoding: Set the b-value to 700 s/mm². Acquire a minimum of 6 non-collinear diffusion-encoding directions [32]. For more sophisticated analysis (e.g., crossing fibers), increase directions to 32 or 64, accepting a longer scan time.
- Parallel Imaging: Enable parallel imaging (e.g., GRAPPA or SENSE) with an acceleration factor of R=2 or 3. Ensure the integrated auto-calibration signal (ACS) lines are acquired for kernel calibration [33].
- Other Parameters: Typical values: TR = ~8000 ms, TE = ~80 ms, bandwidth = ~1500 Hz/pixel, and a single average (NEX=1).
- Non-Diffusion-Weighted (b=0) Volume: Acquire at least one volume without diffusion weighting (b=0 s/mm²). This volume serves as a reference for motion correction and tensor calculation.
Quality Control and Post-Processing Workflow
- Online QC: Visually inspect the raw DICOM images immediately after acquisition for significant ghosting, signal dropouts, or motion artifacts.
- Data Preprocessing: Process the data using a dedicated DTI software toolkit (e.g., FSL, DSI Studio, or Tortoise). Standard steps include:
- Eddy Current Correction: Correct for distortions and subject motion using the b=0 volume as a reference.
- Skull Stripping: Remove non-brain tissue from the diffusion-weighted images.
- Tensor Calculation: Fit a diffusion tensor model to the data at each voxel to derive quantitative maps: Fractional Anisotropy (FA), Mean Diffusivity (MD), Axial Diffusivity (AD), and Radial Diffusivity (RD).
- Fiber Tracking: Perform deterministic or probabilistic tractography on the processed data, seeding from regions of interest defined on the FA map or based on the co-registered T1-weighted anatomy.
Diagram Title: DT-MRI Acquisition and Processing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for DT-MRI Research in Behavioral Studies
| Tool / Reagent | Category | Function in Research | Example Solutions |
|---|---|---|---|
| High-Field MRI Scanner | Hardware | Provides the main magnetic field (B0); higher fields (3T, 7T) yield greater SNR, enabling higher spatial resolution. | Siemens Prisma, Philips Ingenia, GE Discovery |
| Multi-Channel Phased-Array Coil | Hardware | Receives the MR signal; more elements enable higher acceleration in parallel imaging and improve SNR. | 32-channel, 64-channel head coils |
| Parallel Imaging Software | Software | Reconstructs full images from undersampled k-space data, reducing scan time. | GRAPPA [33], SENSE, RAKI [33] |
| Diffusion MRI Sequence | Software | Pulse sequence that applies diffusion-sensitizing gradients. Must support EPI and parallel imaging. | Single-shot spin-echo EPI |
| Phantom for QA | Reagent | An object with known diffusion properties used to validate scanner performance and protocol stability. | Isotropic diffusion phantoms, anisotropic fiber phantoms |
| DTI Processing Toolkit | Software | Suite of algorithms for correcting artifacts, calculating tensors, and performing tractography. | FSL, DSI Studio, Tortoise, MRtrix3 |
Advanced Considerations and Future Directions
Mitigating Artifacts and Harmonization
A primary challenge in multi-site behavioral studies is the variability in DT-MRI data introduced by differences in scanner hardware and acquisition protocols. This can be addressed through:
- Prospective Harmonization: Standardizing acquisition protocols across all study sites before data collection begins is the most effective strategy [35]. This includes using identical scanner models, coil types, and sequence parameters where possible.
- Retrospective Harmonization: When prospective control is not feasible, image-level or feature-level harmonization techniques can be applied. Deep learning-based methods, such as scan-specific networks trained on auto-calibration signal (ACS) data, can help reduce structured residual artifacts in reconstructed images [33] [35]. The recently proposed COrrelation-Based Residual Artifact Index (COBRAI) provides a useful metric for quantifying these artifacts during model selection and optimization [33].
The Role of Emerging Technologies
- Digital Twins: In drug development and advanced research, patient-specific digital twins—virtual representations of an individual's neuroanatomy and connectivity—are emerging as powerful tools. Optimized DT-MRI protocols provide the critical structural connectivity data that informs these models, enabling in-silico testing of hypotheses and interventions without risk to subjects [36] [37].
- Advanced Reconstruction: Deep learning-based reconstruction, such as the optimized three-layer residual linear CNN with complex implementation mentioned in search results, is showing promise in providing robust reconstructions from highly accelerated data, even with limited training data [33]. This could further push the boundaries of acquisition speed and resolution in behavioral DT-MRI studies.
Diagram Title: Resolving the SNR Trade-off in DT-MRI
This application note details the implementation and advantages of Fluid-Attenuated Inversion Recovery Diffusion Tensor Imaging (FLAIR-DTI) for accurate fiber tracking in periventricular white matter regions. Within behavioral neuroscience and drug development research, precise reconstruction of neural pathways is paramount for correlating structural connectivity with cognitive phenotypes and treatment outcomes. Conventional DTI faces significant challenges in periventricular zones due to cerebrospinal fluid (CSF) partial volume effects, which contaminate diffusion measurements and compromise tractography fidelity. FLAIR-DTI addresses this limitation by suppressing the CSF signal, thereby providing more accurate microstructural metrics. This document provides a comprehensive technical overview, quantitative comparisons, and detailed experimental protocols for integrating FLAIR-DTI into research on white matter degeneration in aging and neuropsychiatric disorders.
The Problem of CSF Contamination in Conventional DTI
The periventricular white matter is a critical area containing major fiber bundles such as the corpus callosum, corona radiata, and optic radiations. However, its proximity to the lateral ventricles makes it particularly susceptible to signal contamination from CSF on conventional DTI.
Key Limitations of Conventional DTI:
- CSF Partial Volume Effects: CSF has a high diffusion coefficient (~3.0 × 10⁻³ mm²/s) and is largely isotropic. When a DTI voxel contains both brain tissue and CSF, the measured diffusion becomes a weighted average, leading to an overestimation of the apparent diffusion coefficient (ADC) by 15-30% and a concomitant underestimation of fractional anisotropy (FA) [38].
- Compromised Tractography: The reduction in perceived anisotropy due to CSF contamination can cause algorithms to prematurely terminate fiber tracking in periventricular regions. This results in an underestimation of fiber bundle volume and a false representation of structural connectivity [38] [39].
- Reduced Sensitivity in Behavioral Studies: In longitudinal studies of aging, cognitive decline, or drug efficacy, these inaccuracies can obscure genuine microstructural changes and their correlations with behavioral data.
The FLAIR-DTI Solution: Principles and Advantages
The FLAIR-DTI sequence integrates a fluid-attenuating inversion recovery pulse with a diffusion-weighted echo-planar imaging readout. The FLAIR component nulls the signal from CSF by applying an inversion pulse with a long inversion time (TI, typically ~2300 ms), timed so that the longitudinal magnetization of CSF is at its null point when data acquisition begins [38].
Quantified Advantages of FLAIR-DTI:
Table 1: Quantitative Comparison of Conventional DTI vs. FLAIR-DTI in Periventricular White Matter
| Parameter | Conventional DTI | FLAIR-DTI | Experimental Basis |
|---|---|---|---|
| CSF Signal Contamination | Significant | Effectively suppressed | [38] |
| FA Measurement Accuracy | Underestimated in periventricular regions | Significantly improved | [38] [39] |
| Fiber Tract Volume (Periventricular) | Baseline | 17% greater on average | [38] |
| Tractography Reliability | Lower near ventricles/sulci | Higher, with continuous fibers in callosum & corona radiata | [38] |
| Key Trade-off | Higher Signal-to-Noise Ratio (SNR) | Lower intrinsic SNR, longer acquisition time | [38] |
The data confirms that despite a lower SNR, the benefit of eliminating CSF contamination results in a net positive gain for tractography, particularly in the regions most relevant to the study of aging and neurodegenerative disease [40] [38] [39].
Experimental Protocols for FLAIR-DTI
Image Acquisition Protocol
The following protocol is adapted from established methods and can be implemented on a clinical 3T scanner [38] [41].
Table 2: Example FLAIR-DTI Acquisition Parameters for a 3T Scanner
| Parameter | Specification | Notes |
|---|---|---|
| Sequence | Spin-echo echo-planar imaging (SE-EPI) with FLAIR prep | Use a twice-refocused spin-echo to reduce eddy currents |
| Field Strength | 3T | Also validated at 1.5T |
| Inversion Time (TI) | 2300 ms | Critical for effective CSF nulling |
| Repetition Time (TR) | ≥ 9000 ms | Must be sufficiently long due to inversion recovery |
| Echo Time (TE) | ~100-120 ms | Minimize to improve SNR |
| Diffusion Directions | 45-64 | Higher angular resolution improves tractography |
| b-value | 1000 s/mm² | Standard value for DTI; a reference b=0 image is also acquired |
| Voxel Size | 2.0 mm isotropic | Balance between resolution and SNR |
| Parallel Imaging | GRAPPA or ASSET (acceleration factor 2) | Reduces acquisition time and EPI distortions |
Implementation Note: To acquire gapless slices without cross-talk from the inversion pulses, the acquisition is often performed in two interleaved steps: first for odd-numbered slices and then for even-numbered slices, which doubles the scan time [38].
Data Processing and Tractography Workflow
The processing pipeline involves co-registration, tensor calculation, and tractography, with careful attention to handling FLAIR-DTI data.
Diagram 1: FLAIR-DTI Data Processing and Tractography Workflow.
Key Processing Steps:
Preprocessing: Utilize tools from FSL or similar packages. Critical steps include:
- Eddy current correction and subject motion correction are essential for DTI.
- Skull extraction to remove non-brain tissue.
- Co-registration of DTI data with structural images (T1-weighted, FLAIR) for anatomical context [41].
Tensor and Metric Calculation: Calculate the diffusion tensor on a voxel-by-voxel basis. Derive scalar maps of FA, MD, axial diffusivity (AD), and radial diffusivity (RD) [38] [41].
Tractography:
- Algorithm Selection: Both deterministic (e.g., tensor deflection, FACT) and probabilistic algorithms can be used. Probabilistic methods may better handle regions of fiber complexity or crossing [38] [42].
- Seeding Strategy: For periventricular tracts, seed points can be placed manually in regions like the corpus callosum or optic radiations, or a global seeding approach can be used to reconstruct the whole-brain connectome.
- Tracking Parameters: Standard thresholds include FA > 0.2 and an angular threshold of <18° between adjacent voxels to prevent biologically implausible turns [38].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for FLAIR-DTI Studies
| Item/Category | Function/Application | Example Specifications |
|---|---|---|
| MRI Scanner | Image acquisition platform. | 3T preferred for superior SNR; sequences validated on Siemens, GE, Philips systems. |
| Multi-channel Head Coil | Signal reception. | 32-channel or higher for improved SNR and parallel imaging. |
| Diffusion Phantoms | Quality control and sequence validation. | Phantoms with known diffusion properties to calibrate scanners. |
| Image Processing Software | Data analysis and tractography. | FSL, FreeSurfer, DSI Studio, SPM; in-house scripts for custom analysis. |
| T2/FLAIR Hyperintensity Segmentation Tool | Quantification of white matter lesion load. | Lesion Segmentation Toolbox (LST) for SPM, requires T1 and FLAIR inputs [41]. |
| Statistical Analysis Package | Correlating imaging metrics with behavioral/drug response data. | R, Python, SPSS, MATLAB. |
Application in Behavioral and Drug Development Research
Integrating FLAIR-DTI into a research pipeline provides a more sensitive tool for investigating brain-behavior relationships and treatment effects.
Use Case 1: Aging and Cognitive Decline
- Protocol: Longitudinal study design with FLAIR-DTI at baseline and follow-up (e.g., 2-4 years). Participants should include cognitively normal elders and those with Mild Cognitive Impairment (MCI) [40].
- Analysis: Track the conversion of normal-appearing white matter (NAWM) to white matter hyperintensities (WMH). Voxel-based analysis can model the risk of conversion as a function of baseline FA and FLAIR intensity.
- Outcome: Studies show that lower baseline FA and higher baseline FLAIR intensity in NAWM are independently associated with an increased risk of converting to WMH. This demonstrates that FLAIR and DTI provide complementary information for understanding the continuous process of white matter degeneration in aging [40] [39].
Use Case 2: Monitoring Drug Efficacy in White Matter Diseases
- Protocol: Double-blind, placebo-controlled trial in diseases like Multiple Sclerosis (MS). Acquire FLAIR-DTI at baseline and post-treatment.
- Analysis: Beyond lesion count, use FLAIR-DTI to quantify:
- Outcome: More accurate measurement of drug effects on axonal integrity and myelin repair, as DTI metrics are sensitive to demyelination and axonal loss [41].
FLAIR-DTI is a critical methodological advancement for behavioral neuroscience and pharmaceutical research, effectively mitigating the confounding influence of CSF in periventricular white matter tractography. The protocol, which entails a specific acquisition sequence and a rigorous processing pipeline, yields a 17% increase in reliably tracked fiber volume in these regions. By providing more accurate measurements of microstructural integrity, it enhances the sensitivity of studies investigating the links between white matter pathology, cognitive function, and therapeutic intervention. Its application is particularly warranted in longitudinal studies of aging, cerebrovascular disease, and neuroinflammatory conditions where periventricular white matter integrity is a key biomarker.
Diffusion Tensor Magnetic Resonance Imaging (DT-MRI or DTI) is a non-invasive medical imaging technique that quantifies the microstructural integrity and organization of tissues by measuring the direction and magnitude of water molecule diffusion. The technique has emerged as a powerful biomarker in neurological research and drug development because it can reveal subtle changes in tissue architecture long before macroscopic changes become apparent on conventional imaging. Water diffusion in biological tissues is constrained by cellular membranes, myelin sheaths, and other microstructural elements, making diffusion measurements highly sensitive to pathological changes. In the context of preclinical and early-phase clinical trials for conditions affecting the nervous system, DT-MRI provides valuable quantitative metrics that can serve as objective endpoints for treatment efficacy.
The fundamental principle underlying DT-MRI is that in organized tissues such as white matter tracts, water diffusion is directionally dependent (anisotropic), preferentially moving parallel to axon bundles rather than perpendicular to them. This directional preference is quantitatively captured through the diffusion tensor, a 3x3 matrix that is calculated from multiple diffusion-weighted measurements. From this tensor, various scalar metrics can be derived, each providing different insights into tissue microstructure. The most commonly used metric is fractional anisotropy (FA), which represents the degree of directional preference of water diffusion and serves as a marker for axonal integrity and myelination [9].
Key DT-MRI Metrics and Their Biological Significance
DT-MRI generates several quantitative parameters that serve as sensitive biomarkers for detecting microstructural changes in neural tissues in response to experimental therapies or disease progression.
Table 1: Key DT-MRI Scalar Metrics and Their Biological Significance
| Metric | Full Name | Biological Significance | Interpretation in Pathology |
|---|---|---|---|
| FA | Fractional Anisotropy | Degree of directional water diffusion; marker of axonal integrity and myelination | Decreased FA suggests white matter disruption, as seen in ALS, MS, and SCI [9] |
| ADC | Apparent Diffusion Coefficient | Overall magnitude of water diffusion | Increased ADC indicates vasogenic edema, cellular necrosis; decreased ADC suggests cytotoxic edema [45] [9] |
| AD | Axial Diffusivity | Water diffusion parallel to axonal fibers | Decreased AD suggests axonal injury [9] |
| RD | Radial Diffusivity | Water diffusion perpendicular to axonal fibers | Increased RD suggests myelin damage [9] |
| MD | Mean Diffusivity | Overall average diffusion | Increased MD indicates edema, decreased cellularity [9] |
| MO | Mode of Anisotropy | Shape of diffusion tensor (linear vs. planar) | Helps characterize complex fiber configurations [9] |
These quantitative metrics enable researchers to track longitudinal changes in tissue microstructure with high sensitivity. For example, in a clinical study of spinal cord injury (SCI) patients treated with umbilical cord mesenchymal stem cell (UC-MSC) transplantation, DT-MRI revealed statistically significant microstructural improvements. Researchers observed an increased FA value (from 0.42 ± 0.05 to 0.51 ± 0.06) and decreased ADC value (from 1.15 ± 0.13 × 10⁻³ mm²/s to 0.98 ± 0.11 × 10⁻³ mm²/s) in the experimental group compared to controls, suggesting enhanced structural integrity of spinal cord tissues following treatment [45]. These quantitative changes correlated with clinical improvements in sensory and motor function, supporting DT-MRI's role as a validated biomarker.
Experimental Protocols for DT-MRI in Research
Preclinical Animal Model Protocol
For preclinical studies using animal models of neurological disorders, the following optimized DT-MRI acquisition protocol is recommended:
Animal Preparation:
- Implement appropriate anesthetic regimen (e.g., isoflurane maintenance at 1.5-2% in oxygen)
- Utilize physiological monitoring throughout scanning (respiratory rate, temperature, blood oxygenation)
- Maintain normothermia using a heated water pad or air warming system
- Position animal in dedicated stereotaxic head holder to minimize motion artifacts
Image Acquisition:
- Use high-field preclinical scanner (7T or higher recommended for enhanced SNR)
- Employ single-shot echo-planar imaging (SS-EPI) sequence for motion insensitivity
- Set key parameters: TR = 5000 ms, TE = 25 ms, matrix size = 128 × 128, FOV = 25 × 25 mm
- Acquire 30-40 contiguous slices at 0.5 mm thickness for full brain coverage
- Apply diffusion encoding in 30-60 non-collinear directions with b-value = 1000 s/mm²
- Include multiple non-diffusion-weighted volumes (b = 0 s/mm²) for reference
- Implement cardiac and respiratory gating to minimize pulsation artifacts
Quality Control:
- Conduct daily phantom scans to monitor gradient performance and SNR
- Visually inspect raw diffusion-weighted images for artifacts before proceeding with analysis
- Monitor animal physiology throughout acquisition session
Human Clinical Trial Protocol
For Phase I/II clinical trials involving human participants, the following DT-MRI protocol provides robust data for biomarker assessment:
Participant Preparation and Positioning:
- Screen participants for MRI contraindications (metallic implants, pacemakers, etc.)
- Use foam padding and head restraints to minimize head motion
- Instruct participants to remain still during acquisition
- Position phased-array head coil for optimal signal reception
Sequence Optimization:
- Utilize single-shot echo-planar imaging on 3T clinical scanner
- Implement parallel imaging (acceleration factor R = 2) to reduce EPI distortions
- Apply key parameters: TR = 8000 ms, TE = 80 ms, matrix size = 128 × 128, FOV = 240 × 240 mm
- Acquire 60-70 axial slices at 2-2.5 mm thickness for full brain coverage
- Apply diffusion encoding in 30-64 non-collinear directions with b-value = 1000 s/mm²
- Include at least 7 non-diffusion-weighted (b = 0 s/mm²) volumes
- Implement fat suppression techniques to minimize chemical shift artifacts
Advanced Considerations:
- For spinal cord imaging, use cardiac gating to reduce pulsation artifacts [46]
- Consider reduced FOV techniques for regions with susceptibility artifacts
- For multicenter trials, implement rigorous quality assurance protocols including standardized phantom scans
Table 2: DT-MRI Acquisition Parameters for Different Research Applications
| Parameter | Preclinical (Rodent) | Human Brain | Human Spinal Cord |
|---|---|---|---|
| Magnetic Field Strength | 7T-11T | 3T | 3T |
| Diffusion Directions | 30-60 | 30-64 | 30-64 |
| b-value (s/mm²) | 1000 | 1000 | 800-1000 |
| Non-Diffusion Volumes (b=0) | 5-10 | 7-10 | 7-10 |
| Spatial Resolution | 0.2 × 0.2 × 0.5 mm | 2 × 2 × 2 mm | 1.5 × 1.5 × 3 mm |
| Parallel Imaging | Not applicable | Factor 2 | Factor 2 |
| Cardiac Gating | Optional | Optional | Recommended [46] |
Data Processing and Analysis Workflow
Processing DT-MRI data requires multiple computational steps to transform raw diffusion-weighted images into meaningful quantitative biomarkers. The following workflow represents current best practices for clinical trial applications:
Processing Steps Description
Preprocessing:
- Eddy current correction: Compensates for distortions caused by diffusion-sensitizing gradients using registration-based methods [46]
- Motion correction: Realigns diffusion-weighted volumes to a reference volume to account for subject motion
- Denoising: Implements algorithms to remove random noise while preserving signal integrity
- Artifact removal: Identifies and corrects for various artifacts including susceptibility distortions and physiological noise
Tensor Reconstruction and Metric Calculation: After preprocessing, the diffusion tensor is calculated for each voxel using linear or nonlinear fitting algorithms. From the tensor, quantitative scalar maps (FA, MD, AD, RD) are derived for subsequent analysis.
Fiber Tractography: Tractography algorithms reconstruct white matter pathways by following the principal diffusion direction between voxels. Both deterministic and probabilistic approaches are used, with the choice depending on the specific research question and data quality.
Quantitative Analysis Approaches
Table 3: DT-MRI Data Analysis Methods for Clinical Trials
| Method | Description | Use Case | Software Tools |
|---|---|---|---|
| ROI-Based Analysis | Places regions of interest on specific white matter tracts | Hypothesis-driven studies of particular pathways | DTI Studio, DSI Studio [9] [12] |
| Tract-Based Spatial Statistics (TBSS) | Voxel-wise analysis projected onto group mean FA skeleton | Whole-brain analysis without a priori hypotheses | FSL TBSS [9] |
| Tract-Specific Analysis | Quantifies metrics along specific fiber bundles | Assessing particular tracts of interest | TRACULA, DSI Studio [9] |
| Connectometry | Analyzes structural connectivity patterns | Investigating brain network alterations | DSI Studio [9] |
Each analysis method offers distinct advantages. ROI-based analysis provides high reliability for specific tracts but requires a priori hypotheses. TBSS enables comprehensive whole-brain analysis without smoothing artifacts but may miss smaller tracts. Tract-specific analysis balances these approaches by quantifying metrics along anatomically defined pathways.
Successful implementation of DT-MRI in preclinical and clinical trials requires access to specialized software tools and analytical resources.
Table 4: Essential DT-MRI Software Tools for Research
| Tool Name | Primary Function | Platform | Key Features |
|---|---|---|---|
| DTI Studio | DTI computation and fiber tracking | Windows | Eddy-current correction, tensor calculation, color mapping [9] |
| DSI Studio | Advanced diffusion MRI analysis | Windows, macOS, Linux | Deterministic fiber tracking, connectometry analysis [9] [12] |
| FSL TBSS | Voxel-based analysis of FA data | macOS, Linux | Projection onto mean FA skeleton, group statistics [9] |
| TRACULA | Automated tract reconstruction | macOS, Linux | Reconstruction of 18 major white matter pathways [9] |
| MRtrix | Advanced tractography | Windows, macOS, Linux | Fiber orientation distributions, fixel-based analysis [9] |
Application in Clinical Trials: Case Examples
Spinal Cord Injury Trial
A 2021 clinical study demonstrated DT-MRI's utility as a biomarker in a trial evaluating umbilical cord mesenchymal stem cell (UC-MSC) transplantation for spinal cord injury (SCI). The study employed DT-MRI to detect microstructural changes in the spinal cord before and after treatment [45].
Methodology:
- Seven SCI patients received UC-MSC transplantation plus comprehensive rehabilitation
- Control group received rehabilitation only
- DT-MRI acquired at baseline, 2 months, and 6 months post-treatment
- ROI analysis performed at lesion site and normal-appearing cord
- FA and ADC values quantified and correlated with ASIA sensory/motor scores
Results: The experimental group showed statistically significant microstructural improvements on DT-MRI:
- FA values increased from 0.42 ± 0.05 to 0.51 ± 0.06
- ADC values decreased from (1.15 ± 0.13) × 10⁻³ mm²/s to (0.98 ± 0.11) × 10⁻³ mm²/s
- Differences in ADC and FA values at the lesion layer were significantly greater than in normal-appearing cord
- DT-MRI changes correlated with clinical improvements in light touch, acupuncture sensation, and motor scores
This study demonstrated DT-MRI's sensitivity to detect treatment-induced microstructural changes that preceded clinical improvement, supporting its role as a predictive biomarker in regenerative therapy trials.
Amyotrophic Lateral Sclerosis (ALS) Applications
DT-MRI has been extensively studied as a potential biomarker in ALS clinical trials. Multiple meta-analyses have consistently identified reduced FA in the corticospinal tracts of ALS patients, correlating with disease severity and progression [9]. A retrospective multicenter study of 253 ALS patients revealed FA reductions not only in motor pathways but also in extra-motor regions including the frontal lobe and brainstem, suggesting DT-MRI's utility for tracking disease spread [9].
Implementation Considerations for Clinical Trials
Technical Optimization
Successful implementation of DT-MRI in clinical trials requires careful attention to technical factors that impact data quality and reproducibility:
Magnetic Field Strength: While 3T scanners provide sufficient SNR for most clinical applications, 7T scanners offer enhanced resolution for preclinical studies and specialized clinical research. Higher fields increase SNR but also exacerbate susceptibility artifacts, requiring additional compensation strategies [46].
Gradient Performance: High-performance gradients enable stronger diffusion weighting at shorter TE, improving SNR and reducing geometric distortions. Modern scanners with 40-80 mT/m maximal gradient amplitude and 150-200 mT/m/ms slew rates provide excellent DTI capability while remaining within safety limits for peripheral nerve stimulation [46].
Multi-channel Coils and Parallel Imaging: Multi-channel phased-array head coils significantly improve SNR compared to standard birdcage coils. Parallel imaging techniques such as SENSE or GRAPPA reduce EPI distortions and allow shorter echo trains, but require careful calibration to avoid noise amplification [46].
Artifact Mitigation Strategies
Eddy Current Artifacts: Caused by residual magnetic fields from rapidly switched diffusion gradients, leading to image scaling, shifting, or shearing. Compensation strategies include:
- Bipolar diffusion gradient designs that cancel eddy currents
- Twice-refocused spin-echo sequences that break up eddy current formation time
- Post-processing registration-based correction algorithms [46]
Physiological Motion Artifacts: Cardiac and respiratory pulsations can cause phase encode inconsistencies in EPI readouts. Mitigation approaches include:
- Cardiac gating for spinal cord and brainstem imaging
- Prospective acquisition correction (PACE) techniques
- Post-processing regression of physiological noise [46]
Susceptibility Artifacts: Magnetic field inhomogeneities near air-tissue interfaces cause geometric distortions and signal dropout. Reduction strategies include:
- Reduced FOV imaging techniques
- Increased bandwidth in phase-encode direction
- Z-shim compensation methods for specific regions [46]
DT-MRI has matured into a robust imaging biomarker that provides sensitive, quantitative measures of tissue microstructure with particular relevance for clinical trials targeting neurological disorders. The technique's ability to detect subtle treatment effects before clinical manifestations appear makes it especially valuable in early-phase trials where objective biomarkers of biological activity are essential. As standardization improves and analytical methods become more sophisticated, DT-MRI is poised to play an increasingly important role in accelerating therapeutic development for conditions affecting white matter integrity and neural connectivity.
Navigating Technical Challenges: Strategies for Optimizing DT-MRI Data Quality and Tractography
Diffusion Tensor Imaging (DTI) is a pivotal magnetic resonance imaging technique for non-invasively investigating the microstructure of white matter in the human brain, providing in vivo insights into neural connectivity through metrics such as fractional anisotropy (FA) and mean diffusivity (MD) [47] [48]. A significant confound in accurate DTI quantification, particularly in regions adjacent to cerebral ventricles, is the partial volume effect caused by cerebrospinal fluid (CSF) [49]. CSF has a high diffusion coefficient and exhibits isotropic diffusion, which when averaged within a voxel containing brain tissue, leads to an overestimation of MD and an underestimation of FA [49] [50]. This contamination compromises the integrity of tractography, often causing premature termination of reconstructed white matter pathways near CSF interfaces [51].
The Fluid-Attenuated Inversion Recovery (FLAIR) technique, when incorporated with DTI, effectively suppresses the CSF signal by using an inversion recovery pulse timed to null the CSF signal [51]. While FLAIR-DTI successfully mitigates CSF partial volume effects, it introduces a critical trade-off: the inversion recovery preparation reduces the signal-to-noise ratio (SNR) and lengthens the scan time, which can increase vulnerability to motion artifacts [49] [51]. This application note explores this fundamental SNR trade-off, provides a quantitative comparison of CSF suppression methods, and details practical protocols for implementing FLAIR-DTI in research focused on behavioral and substance abuse studies, where accurate periventricular and cortical tractography is paramount.
Quantitative Comparison of CSF Suppression Techniques
The following tables summarize the performance characteristics and quantitative findings for different DTI acquisition strategies aimed at mitigating CSF contamination.
Table 1: Performance Characteristics of DTI Acquisition Techniques for CSF Suppression
| Technique | Primary Mechanism | Key Advantages | Key Limitations/Disadvantages |
|---|---|---|---|
| Conventional DTI | Single shell, high b-value acquisition [49] | Higher baseline SNR; Shorter acquisition time [49] [51] | Significant CSF partial volume effects in periventricular and cortical areas [49] [51] |
| FLAIR-DTI | Inversion recovery pulse to null CSF signal [51] | Effective elimination of CSF partial volume effects [49] [51] | 33% reduction in SNR; Longer TR/scan time; Limited slice coverage [51] |
| Combined DTI (e.g., FLAIR b=0) | FLAIR preparation for low-b images only; conventional for high-b [49] | Higher SNR and shorter scan time vs. FLAIR-DTI; effective CSF suppression [49] | More complex acquisition protocol [49] |
| Free Water Elimination (FWE) DTI | Bi-tensor computational model separating tissue and CSF signals [51] | No SNR penalty; No volumetric coverage limitations; Does not require sequence modification [51] | Requires two b-values; Computational post-processing; Assumes known CSF diffusivity [51] |
Table 2: Quantitative Differences in Diffusion Metrics and Tractography Outcomes
| Parameter | Finding | Technique Comparison | Implication |
|---|---|---|---|
| SNR | FLAIR-DTI reduces SNR by ~33% compared to conventional DTI [51]. | FWE-DTI showed only an 11% SNR reduction [51]. | FLAIR-DTI's lower SNR can downgrade fiber tracking results [49]. |
| Tract Volume (Fornix) | FLAIR and FWE-DTI produce more complete fornix reconstructions than conventional DTI [51]. | FWE-DTI tract volumes were significantly larger than FLAIR-DTI (p < 0.0005) [51]. | FLAIR-DTI's lower SNR may limit the extent of tractography in vulnerable regions. |
| Mean Diffusivity (MD) in GM | Standard DKI overestimates MD in gray matter due to CSF [50]. | FLAIR-DKI reduces MD in gray matter by 19% to 52% [50]. | Confirms significant CSF contamination in cortical GM, corrected by suppression. |
| Fractional Anisotropy (FA) | CSF contamination causes underestimation of FA [49]. | FLAIR preparation can increase measured FA in contaminated regions [49] [50]. | Improves accuracy of microstructural assessment in periventricular WM and GM. |
| Scan Time | FLAIR preparation increases repetition time (TR) [51]. | For similar resolution, FLAIR-DTI may require >2x longer scan time than conventional DTI [50]. | Reduces clinical feasibility, increases motion artifact risk [49]. |
Experimental Protocols for Behavioral Research
This section provides detailed methodologies for implementing and evaluating CSF-suppressed DTI in a research setting, with a focus on applications in substance abuse and behavioral neuroscience.
Protocol 1: FLAIR-DTI Acquisition for Periventricular Tract Integrity
This protocol is optimized for studying tracts like the fornix and corpus callosum, which are often implicated in chronic substance abuse [48].
- 1. MRI System Setup: Utilize a 3 Tesla MRI scanner equipped with a high-channel count head coil (e.g., 32-channel) to maximize baseline SNR [51] [48].
- 2. Sequence Parameters:
- Pulse Sequence: Spin-echo echo-planar imaging (SE-EPI) with FLAIR preparation [51] [50].
- Inversion Time (TI): Set to null CSF, typically ~2000-2300 ms [51] [52].
- Diffusion Encoding: Use a single shell with b=1000 s/mm² and at least 30 encoding directions to ensure robust tensor estimation [51] [48].
- b=0 Images: Acquire 6-10 non-diffusion weighted volumes with the FLAIR preparation [51].
- Spatial Resolution: Isotropic voxels of 2.0-2.5 mm [51]. Thinner slices (e.g., 3mm) are particularly beneficial for FLAIR-DTI to mitigate SNR limitations [49].
- Other Parameters: TR = ~10000 ms (lengthened due to TI), TE = minimum possible (e.g., ~63-110 ms), parallel imaging acceleration factor (e.g., GRAPPA or ASSET R=2) to reduce TE and TR [51] [52] [50].
- 3. Quality Control:
- Gibbs Ringing: Inspect MD maps for ringing artifacts near the lateral ventricles, which are reduced by FLAIR [52].
- Signal Drop-out: Ensure FLAIR inversion is effective across the brain volume.
Protocol 2: Free Water Elimination DTI Acquisition
This protocol is recommended for studies where scan time and SNR are primary concerns, such as in longitudinal studies or those with clinical populations [51].
- 1. MRI System Setup: Same as Protocol 1.
- 2. Sequence Parameters:
- Pulse Sequence: Standard SE-EPI without FLAIR preparation.
- Diffusion Encoding: Two-shell acquisition is mandatory [51].
- Shell 1: b = 500 s/mm²
- Shell 2: b = 1500 s/mm²
- Use matching encoding directions for both shells. A total of 40-80 encoding directions split across shells is recommended [51].
- b=0 Images: Acquire 6-10 volumes.
- Spatial Resolution: Isotropic 2.5 mm voxels [51].
- Other Parameters: TR = ~6000 ms, TE = minimum possible, parallel imaging acceleration factor R=2 [51].
- 3. Data Processing:
- Perform standard preprocessing: motion and eddy-current correction, gradient direction correction, and brain extraction [51].
- Fit the FWE DTI model (Equation 1 in [51]) using specialized software (e.g., custom Matlab scripts) to separate the tissue tensor from the free water (CSF) component.
- Use the corrected tissue tensor for all subsequent tractography and metric analysis (FA, MD) in software like Camino or FSL [51].
Protocol 3: Evaluating CSF Suppression Efficacy
A standardized workflow for comparing the performance of different acquisition methods.
- 1. Subject Cohort: Recruit 10 or more healthy volunteers. Scanning the same subjects with multiple protocols is ideal for within-subject comparisons [51].
- 2. Data Acquisition: Acquire datasets for Conventional DTI, FLAIR-DTI, and FWE-DTI on the same scanner, matching spatial resolution and coverage as much as possible [51].
- 3. Region of Interest (ROI) Analysis:
- Manually delineate ROIs in regions with high CSF contamination (e.g., fornix, genu of corpus callosum, cortical gray matter) and in deep white matter (e.g., posterior limb of internal capsule) as a control [50].
- Extract mean FA, MD, AD, and RD for each ROI and each acquisition type.
- 4. Tractography Analysis:
- 5. Statistical Comparison:
Diagram 1: A decision workflow for selecting the appropriate DTI acquisition protocol based on study priorities, guiding researchers towards optimal SNR and CSF suppression balance.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Essential Tools for Advanced DTI Research
| Item/Category | Specification/Example | Primary Function in FLAIR-DTI Research |
|---|---|---|
| High-Field MRI Scanner | 3 Tesla (3T) or higher [51] [48] | Provides the high baseline SNR necessary to offset the penalties introduced by FLAIR preparation. |
| Multi-Channel Head Coil | 32-channel receive coil [51] | Further improves SNR and enables parallel imaging, reducing acquisition time and minimizing artifacts. |
| Diffusion Phantoms | Isotropic water phantoms (FA ≈ 0) [53] | Essential for quality control, protocol optimization, and calibration of diffusion metrics across scanning sessions. |
| Processing Software Suite | FSL, Camino, ExploreDTI, DSI Studio, custom Matlab scripts [51] [52] [12] | Used for data preprocessing (motion correction), tensor fitting (including FWE modeling), and fiber tractography. |
| Bi-tensor Model Algorithm | Free Water Elimination (FWE) DTI model [51] | Computational tool to separate CSF and tissue diffusion signals from standard DTI data, mitigating partial volume effects without SNR loss. |
| Standardized ROI Atlas | JHU White Matter Atlas, AAL | Provides anatomically defined regions of interest for consistent quantification of diffusion metrics across subjects and studies. |
Application in Behavioral & Drug Development Research
In behavioral neuroscience, particularly in substance abuse research, accurate DTI is critical as microstructural white matter alterations are a consistent finding. For instance, chronic alcohol and opiate use are associated with reduced white matter coherence, often most prominent in anterior regions like the genu of the corpus callosum [48]. The anterior-posterior gradient of age-related white matter degradation also mirrors the patterns of vulnerability in substance abuse, underscoring the need for precise measurement in these regions [54].
FLAIR-DTI and FWE-DTI directly address the methodological limitations that have plagued this field. Many earlier studies used 1.5T scanners, low-direction DTI, and were confounded by polydrug use [48]. The implementation of advanced CSF-suppressed DTI protocols allows for:
- Improved Specificity: By isolating tissue-specific microstructural changes from CSF contamination, researchers can more confidently attribute differences in FA or MD to alterations in axonal integrity or myelination, rather than to hydration or atrophy-related CSF space enlargement [50].
- Enhanced Tractography: Reliable reconstruction of tracts like the fornix, which is critical for memory and often affected in addiction, becomes feasible [51]. This improves the validity of tract-based analyses.
- Objective Biomarkers in Clinical Trials: In CNS drug development, functional imaging biomarkers are increasingly used to provide objective data on drug effects on brain structure and function [55]. Robust DTI metrics, free from CSF contamination, can serve as sensitive biomarkers for tracking drug efficacy in modifying white matter integrity in conditions like alcohol use disorder or cognitive decline.
Diagram 2: The logical pathway from the core problem of CSF contamination to its solutions and the subsequent benefits for research applications, highlighting the role of these techniques in generating more reliable biomarkers.
The trade-off between effective CSF suppression and preserved SNR in FLAIR-DTI represents a central consideration in modern diffusion imaging. While FLAIR-DTI remains a robust method for eliminating CSF partial volume effects, its significant SNR penalty and prolonged scan time can be prohibitive. The emergence of FWE-DTI offers a powerful alternative, overcoming CSF contamination computationally without the inherent SNR and coverage limitations of FLAIR. For researchers employing DT-MRI in behavioral and drug development studies, the choice between these techniques should be guided by the specific experimental priorities: FLAIR-DTI for maximal CSF suppression when SNR is sufficient, and FWE-DTI for studies where efficiency, SNR preservation, and whole-brain coverage are critical. The implementation of the detailed protocols and quantitative comparisons provided herein will empower researchers to make informed decisions, ultimately leading to more accurate and reliable characterization of white matter microstructure in health and disease.
Diffusion Tensor Magnetic Resonance Imaging (DT-MRI) is an indispensable tool for non-invasive investigation of white matter architecture in behavioral neuroscience. However, its application in longitudinal and multi-site studies, which are central to understanding the neural correlates of behavior and drug efficacy, is hampered by significant artifacts. Thermal noise and subject motion can corrupt the delicate diffusion signal, leading to biased tensor estimations and unreliable tractography. This document provides advanced application notes and detailed protocols for denoising and motion compensation, specifically tailored for researchers employing DT-MRI for nerve fiber tracking in behavioral and drug development contexts. Implementing these techniques is crucial for ensuring the reproducibility and cross-sectional validity of microstructural findings.
Advanced Denoising Techniques for DT-MRI
Image denoising is a critical preprocessing step that mitigates the impact of thermal noise on diffusion-weighted images (DWIs), leading to more accurate and biologically plausible estimates of tensor-derived metrics.
Denoising Methodologies and Quantitative Impact
The following table summarizes the performance characteristics of established and emerging denoising methods, as evidenced by recent research.
Table 1: Comparison of Advanced DT-MRI Denoising Techniques
| Method | Underlying Principle | Key Performance Findings | Impact on Reproducibility |
|---|---|---|---|
| MPPCA [56] [57] | Marchenko-Pastur Principal Component Analysis to define and remove noise components. | - Improved visual quality of DTI/DKI maps.- Reduced outliers in kurtosis metrics.- Limited impact on case-control tractometry differences in glaucoma [56]. | - Reduces test-retest variability of kurtosis indices from 15-20% to 5-10% [57].- Enhances cross-scanner and cross-protocol reproducibility. |
| Patch2Self [56] | Self-supervised learning using a J-invariant framework to learn random fluctuations from the 4D data itself. | - Reduces residuals in voxelwise model fitting.- Increases the estimated Signal-to-Noise Ratio (SNR) [56]. | Specific reproducibility metrics not reported in the reviewed studies, though improved SNR suggests potential benefits. |
| Structure-Adaptive Sparse Denoising (SASD) [58] | Groups similar 3D patches using a modified structure-similarity index and performs Wiener shrinkage in a transform domain. | - Outperforms BLS-GSM and FOE in preserving fine structures and edges in simulated cardiac DWIs.- Maintains structural integrity better than non-adaptive methods [58]. | Implicitly improved through superior detail preservation, facilitating more consistent tensor estimation. |
| Deep Learning (DnCNN) [59] | A denoising convolutional neural network trained to identify and remove the spatial distribution of noise. | - Enables 2x acceleration of cardiac DT-MRI by reducing averages while preserving SNR and metrics like FA and MD.- Preserved group differences (e.g., in obesity) lost in non-denoised accelerated data [59]. | Improves statistical power for group comparisons in low-SNR scenarios by enabling faster acquisitions with maintained quality. |
Experimental Protocol: MPPCA Denoising for Multi-Site Studies
This protocol is designed to enhance the reproducibility of DTI and DKI metrics, making it ideal for large-scale behavioral studies across multiple scanners.
- Objective: To apply MPPCA denoising to multi-shell dMRI data to reduce test-retest variability and improve cross-scanner harmonization.
- Materials:
- Multi-shell dMRI data (e.g., b=0, 1000, 2000 s/mm²).
- Software: MRtrix3 (for MPPCA) or DIPY.
- Procedure:
- Data Preparation: Ensure dMRI data is in a compatible format (e.g., NIfTI). No other preprocessing (like eddy-current correction) should be performed prior to denoising.
- Denoising Execution:
- Using MRtrix3: Execute the command
dwidenoise input.nii.gz output_denoised.nii.gz -noise noise_map.nii.gz. This command processes theinput.nii.gzfile and generates both the denoised data (output_denoised.nii.gz) and a noise map (noise_map.nii.gz).
- Using MRtrix3: Execute the command
- Data Integrity Check: Visually inspect the denoised images against the original to confirm noise reduction without excessive smoothing of anatomical details.
- Subsequent Processing: Proceed with standard preprocessing steps (e.g., eddy-current and motion correction) using the denoised data as input.
- Harmonization (Optional): If combining data from multiple scanners or protocols, apply harmonization tools (e.g., ComBat) to the denoised scalar maps (FA, MD) to further reduce site-specific biases [57].
Diagram 1: MPPCA Denoising and Harmonization Workflow
Motion Compensation Techniques for DT-MRI
Subject motion is a paramount challenge, particularly in behavioral studies involving populations with limited compliance (e.g., pediatric, geriatric, or psychiatric cohorts). Motion compensation is essential to avoid spurious findings related to movement rather than underlying biology.
Motion Compensation Strategies
The field has moved beyond simple prospective gating to more sophisticated integrated approaches.
- Prospective Motion Correction: These techniques adjust the imaging plane in real-time to track tissue motion.
- Slice Tracking (MNav-CoS): A novel prospective method that uses a navigator to track and correct for cardiac through-plane motion during free breathing. It performs comparably to multiple breath-holds but offers significant time-saving benefits, making longer, more detailed cDTI acquisitions feasible in a clinical context [60].
- Motion-Compensated Diffusion Gradients: The design of the diffusion-sensitizing gradients themselves can be optimized to reduce signal dropout from motion.
- Optimized Diffusion‐Weighting Gradient Waveform Design (ODGD): This approach designs motion-compensated gradient waveforms. The use of high-performance gradients (Gmax=200 mT/m) allows for shorter echo times (TE), boosting SNR by 30.4% for Gaussian diffusion and 45.3% for non-Gaussian diffusion in the liver, compared to standard gradients [61]. This principle is directly transferable to neural applications.
- Post-Processing and Unsupervised Reconstruction: For free-breathing, ungated acquisitions, computational methods can recover a motion-free state.
- Low-Rank Diffeomorphic Motion Model (DMoCo): This advanced, unsupervised algorithm models the image volume at each cardiac/respiratory phase as a diffeomorphic (smooth and invertible) deformation of a single static template. A low-rank model for the velocity fields provides a compact representation, enabling high-quality motion-compensated reconstruction from extremely undersampled data (e.g., ~100x), which drastically reduces acquisition times [62].
Experimental Protocol: Motion-Compensated Cardiac DT-MRI with Deep Learning
This protocol illustrates a comprehensive integration of acquisition and post-processing for motion compensation.
- Objective: To acquire in vivo cardiac DT-MRI data with a reduced number of averages using a motion-compensated sequence, and recover image quality using a Deep Learning denoiser.
- Materials:
- 3T MRI System with high-performance gradients.
- Second-order motion-compensated spin-echo EPI sequence.
- Denoising Convolutional Neural Network (DnCNN) trained on acquired noise images.
- Procedure:
- Data Acquisition: Acquire DT-MRI data of the left ventricle under free-breathing conditions. Use a second-order motion-compensated sequence (M2) with ECG triggering and respiratory motion correction.
- Multi-Average Data Synthesis: Reconstruct the DT-MRI data at different average levels for comparison: 8-Average (8Av) as a reference standard, 4-Average (4Av), and 2-Average (2Av).
- Deep Learning Denoising: Apply the pre-trained DnCNN to the 4Av and 2Av datasets to generate 4AvDnCNN and 2AvDnCNN datasets.
- Quantitative Analysis:
- Calculate Signal-to-Noise Ratio (SNR) and Structural Similarity Index (SSIM) for all datasets against the 8Av reference.
- Compute DT-MRI parameters: Mean Diffusivity (MD), Fractional Anisotropy (FA), and Helix Angle Transmurality (HAT).
- Validation: Statistically compare the denoised accelerated data (4AvDnCNN, 2AvDnCNN) to the 8Av reference to confirm no significant difference in image quality or parameter quantification. Verify that known group differences (e.g., between cohorts with and without obesity) are preserved in the denoised, accelerated data [59].
Diagram 2: Motion-Compensated Cardiac DT-MRI with DnCNN
The Scientist's Toolkit: Research Reagent Solutions
This section details the essential software and computational tools required to implement the described techniques.
Table 2: Essential Research Tools for Advanced DT-MRI Processing
| Tool Name | Type/Category | Primary Function in DT-MRI Analysis |
|---|---|---|
| MRtrix3 [56] | Software Library | Provides command-line tools for state-of-the-art dMRI processing, including the dwidenoise command for MPPCA denoising and advanced tractography. |
| DIPY [56] | Software Library | A Python-based library for the analysis of dMRI data. It includes implementations of various denoising algorithms, including Patch2Self. |
| Denoising Convolutional Neural Network (DnCNN) [59] | Deep Learning Model | A residual deep learning model trained to identify and remove non-Gaussian noise from diffusion-weighted images, enabling scan acceleration. |
| FSL [56] | Software Library | A comprehensive library of MRI analysis tools. Its TOPUP and EDDY tools are the gold standard for susceptibility-induced and eddy-current distortion correction. |
| Optimized Diffusion Gradient Waveforms [61] | Pulse Sequence Design | Custom-designed diffusion-gradient waveforms that are motion-compensated and leverage high-performance gradient systems to minimize TE and maximize SNR. |
| Low-Rank Diffeomorphic Model (DMoCo) [62] | Computational Algorithm | An unsupervised motion-compensated reconstruction algorithm for representing a family of image deformations compactly, enabling recovery from highly undersampled data. |
Diffusion Tensor Magnetic Resonance Imaging (DT-MRI) serves as a powerful, non-invasive method for studying the structural organization of white matter in the brain, providing invaluable insights for behavioral studies and CNS drug development research [63] [47]. This application note details the comprehensive data processing pipeline that transforms raw diffusion-weighted images into detailed 3D tractograms, enabling researchers to investigate structural connectivity and its relationship to behavior, cognition, and pathological states. The ability to delineate axonal nerve fiber bundles indirectly through water diffusion behavior makes this technology particularly valuable for tracking neurological changes in response to pharmacological interventions or behavioral manipulations [63] [55]. Within drug development, this pipeline offers objective data on drug effects within the living brain, potentially improving the probability of success in identifying useful treatments for CNS diseases across all clinical phases [55]. The protocols outlined herein provide a standardized framework for generating reproducible, quantifiable metrics of white matter integrity and connectivity.
Background and Principles
Physical Principles of Diffusion MRI
Diffusion MRI measures the random motion (Brownian motion) of water molecules within biological tissues [63]. In oriented structures such as bundles of axonal fibers, tissue barriers restrict water diffusion, making it greater along the axis parallel to the main direction of axons than perpendicular to it [47]. This directional dependence is known as anisotropy. The diffusion tensor model describes this anisotropic diffusion at each voxel location on a regular lattice, providing a volumetric average of the directional properties of diffusion within each imaging element [63]. The presence and organization of white matter fiber bundles can thus be inferred from the behavior of water molecules adjacent to the neural tissue.
Key Diffusion Metrics
Diffusion MRI data can be processed to yield several quantitative metrics that reflect microstructural properties of white matter. These metrics are typically derived from the diffusion tensor and its eigenvalues (λ₁, λ₂, λ₃), which represent the magnitude of diffusion in the principal directions.
Table 1: Key Diffusion Tensor Imaging Metrics and Their Interpretations
| Metric | Full Name | Biological Interpretation | Changes in Pathology |
|---|---|---|---|
| FA | Fractional Anisotropy | Overall integrity/coherence of white matter structures; nonspecifically associated with axonal integrity [64] [47] | Decreases: demyelination, inflammation, edema, axonal loss [64] |
| AD | Axial Diffusivity | Diffusion along the primary axon direction; nonspecifically associated with axonal density [64] [47] | Decreases: axonal loss [64] |
| RD | Radial Diffusivity | Diffusion perpendicular to axons; nonspecifically associated with myelination [64] [47] | Increases: demyelination [64] |
| MD | Mean Diffusivity | Overall magnitude of water diffusion; associated with edema and cell infiltration [64] [47] | Increases: vasogenic edema; Decreases: cytotoxic edema [64] |
| QA | Quantitative Anisotropy | Anisotropy measure less affected by edema; associated with axonal density [64] | Decreases: axonal loss [64] |
Different neurological conditions manifest distinct patterns of change across these metrics. For instance, acute axonal injury with inflammation (e.g., stroke <3 months, TBI <3 months) typically presents with decreased FA, increased RD, increased MD, and elevated ISO (isotropy measure), while axonal loss without inflammation (e.g., ALS, Huntington's Disease) shows decreased FA, decreased AD, increased RD, and decreased QA [64].
Comprehensive Processing Pipeline
The transformation of raw diffusion-weighted images to 3D tractograms involves a multi-stage process that can be conceptually divided into four major phases: data acquisition, preprocessing, tensor estimation and analysis, and fiber tracking.
Data Acquisition Protocol
The foundation of any successful DT-MRI study lies in appropriate data acquisition. The following protocol outlines key parameters for robust diffusion data collection.
Table 2: Example Acquisition Parameters for Preclinical and Human Studies
| Parameter | Preclinical Example [65] | Human Study Example [66] | Notes |
|---|---|---|---|
| Field Strength | 9.4 Tesla | 1.5 Tesla or 3 Tesla | Higher fields improve SNR but increase artifacts |
| Sequence | Dual-spin-echo EPI | Single-shot EPI | Multi-shot reduces distortions but is motion-sensitive |
| b-values | 1000, 2000 s/mm² (multi-shell) | 1000 s/mm² (single-shell) | Multiple b-values enable advanced models |
| Gradient Directions | 32 (b=1000), 56 (b=2000) | 64 uniformly distributed | More directions improve tensor estimation |
| b=0 Images | 10 (5 per shell) | 1 | Multiple b=0 improves registration |
| Voxel Size | 130×130×130 µm³ | 2×2×2 mm³ | Isotropic voxels preferred for tractography |
| TE/TR | 35.84/3000 ms | ~98/11000 ms | Minimize TE to maximize SNR |
Experimental Protocol: Data Acquisition
- Subject Preparation: Anesthetize subjects (preclinical) with appropriate agents (e.g., 1.5-3% isoflurane in oxygen). For human studies, ensure proper head fixation with padding to minimize motion [65].
- Sequence Selection: Use a diffusion-weighted spin-echo EPI sequence with dual diffusion weightings for more comprehensive microstructural characterization [65].
- Parameter Optimization: Adjust TE to the minimum possible while maintaining adequate diffusion weighting. Use partial Fourier acquisition (e.g., GRAPPA factor 2) to reduce scan time while preserving spatial resolution [66].
- Multiple Acquisitions: Acquire multiple b=0 images throughout the scan session to facilitate motion correction and serve as registration targets.
- Quality Assessment: Monitor respiration and physiological parameters throughout acquisition. Reconstruct a subset of data in real-time to identify significant motion or artifacts requiring repeat acquisition.
Image Preprocessing and Denoising
Raw diffusion-weighted images are corrupted by various noise sources and artifacts that must be addressed before tensor estimation. Voltage variations in the receiving coil of the MRI machine due to thermal noise represent a major source of signal degradation, typically modeled as additive zero-mean Gaussian noise [63].
Experimental Protocol: Image Preprocessing
- Denoising: Apply a weighted Total Variation (TV)-norm minimization formulation specifically tuned for smoothing vector-valued diffusion data [63]. This approach outperforms smoothing after tensor calculation as it preserves edges while reducing noise in homogeneous regions.
- Eddy Current Correction: Use registration-based methods to correct for distortions and misalignments between diffusion-weighted images caused by eddy currents induced by strong diffusion gradients.
- Head Motion Correction: Implement rigid body registration to align all diffusion-weighted images to a reference volume (typically an average b=0 image).
- EPI Distortion Correction: Apply field mapping or reverse phase-encoding techniques to correct for susceptibility-induced distortions common in EPI sequences [67].
- Gradient Direction Adjustment: Reorient the gradient vectors according to any rotational component of the transformation applied during motion correction.
Tensor Estimation and Analysis
Following preprocessing, the diffusion tensor is estimated at each voxel, typically using a linear least-squares fit to the log-transformed signal intensities [63]. The tensor is then diagonalized to obtain eigenvalues and eigenvectors that describe the magnitude and direction of diffusion in the principal directions.
Experimental Protocol: Tensor Estimation
- Tensor Calculation: For each voxel, solve the linear system:
ln(S/S₀) = -bĝᵀDĝ, where S is the diffusion-weighted signal, S₀ is the non-diffusion-weighted signal, b is the diffusion weighting factor, ĝ is the gradient direction unit vector, and D is the diffusion tensor [63]. - Eigenanalysis: Perform diagonalization of the diffusion tensor D to obtain three eigenvalues (λ₁, λ₂, λ₃) and corresponding eigenvectors (ε₁, ε₂, ε₃). The principal eigenvector (ε₁) corresponds to the dominant diffusion direction.
- Metric Calculation: Compute scalar diffusion metrics for each voxel:
- FA = √(3/2) * √((λ₁-λ)² + (λ₂-λ)² + (λ₃-λ)²) / √(λ₁² + λ₂² + λ₃²), where λ = (λ₁+λ₂+λ₃)/3
- MD = (λ₁ + λ₂ + λ₃)/3
- AD = λ₁
- RD = (λ₂ + λ₃)/2
- Quality Validation: Inspect eigenvalue maps for physically plausible values (positive eigenvalues) and check FA maps for appropriate contrast between white matter, gray matter, and CSF.
Fiber Tracking and Tractography
Neuronal fiber tracking follows a two-stage process: (a) computing the dominant eigenvector field from the regularized diffusion tensor field, and (b) estimating regularized streamlines as the desired fiber tracts [63].
Experimental Protocol: Deterministic Fiber Tracking
- Seed Point Definition: Select seeding strategy based on research question:
- Aponeurosis-based (APO) seeding: Places seeds at muscle-aponeurosis boundaries for mechanically relevant structural properties [68]
- Voxel-based (VXL) seeding: Regularly spaced seeds throughout the muscle volume for comprehensive coverage [68]
- Edge (EDGE) seeding: Places seeds one voxel internal to muscle boundaries [68]
- Streamline Propagation: Use deterministic tracking based on the principal diffusion direction:
- Employ a step size of approximately 1/10 of the voxel size in diffusion space [66]
- Apply Euler integration:
posᵢ₊₁ = posᵢ + step_size * ε₁(posᵢ)
- Termination Criteria: Halt streamline propagation when:
- FA falls below a threshold (typically 0.1-0.2)
- The tracking angle between consecutive steps exceeds a maximum (typically 30-45°)
- The streamline exits the defined mask (white matter or specific ROI)
- Tract Filtering: Remove spurious or anatomically implausible streamlines through manual cleaning or automated methods based on length, endpoints, or trajectory.
Determining Appropriate Streamline Counts
The number of streamlines generated significantly impacts the reproducibility of tractography results. Required streamline counts vary substantially based on anatomical tract, image resolution, number of diffusion directions, and desired reliability level [69].
Experimental Protocol: Streamline Count Optimization
- Reliability Assessment: Automatically estimate the number of streamlines required to achieve reliable microstructural measurements using methods that assess reproducibility [69].
- Prospective Seeding: Implement prospective methods that cease streamline generation when stability criteria are met rather than using arbitrary counts [69].
- Validation: Repeatedly generate tractograms with calculated streamline numbers to verify actual reproducibility meets target thresholds [69].
Advanced Applications: Tractometry and Quantitative Analysis
Tractometry represents an advanced analytical approach that combines tractography with quantitative analysis of microstructural properties along specific white matter pathways [66] [70]. This method is particularly valuable for detecting subtle, localized changes in white matter integrity that may correlate with behavioral measures or treatment response.
Experimental Protocol: Tractometry Analysis
- Bundle Segmentation: Isolate specific tracts of interest (e.g., optic radiation, corpus callosum) through manual dissection or automated methods.
- Tract Cleaning: Remove spurious or anatomically implausible streamlines to ensure a clean bundle representation.
- Parameter Sampling: Resample each streamline to a fixed number of equidistant points (typically 50-100) and compute diffusion metrics at each point.
- Tract Profile Generation: Create group average profiles of diffusion metrics along the length of the bundle to identify regions of significant difference.
- Statistical Analysis: Implement point-wise statistical testing along the tract profile, correcting for multiple comparisons using methods like threshold-free cluster enhancement.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Tool/Resource | Function/Purpose | Implementation Notes |
|---|---|---|
| Diffusion MRI Sequences (EPI, RESOLVE) [68] [65] | Data acquisition with diffusion weighting | Multi-shell acquisition provides more comprehensive microstructural information |
| Denoising Algorithms (Weighted TV-norm) [63] | Noise reduction in raw DWI data | Applying before tensor estimation improves accuracy of derived metrics |
| Tensor Estimation Libraries | Calculation of diffusion tensors from DWI | Linear least-squares fitting is most common approach |
| Deterministic Tracking Algorithms [63] [68] | Streamline propagation from seed points | Euler integration with fractional step size improves angular resolution |
| Tractometry Software [66] [70] | Quantitative analysis along specific tracts | Enables detection of localized changes in white matter integrity |
| Visualization Tools (Streamtubes, LIC, Particles) [63] | 3D representation of fiber tracts | Particle-based visualization allows real-time interaction without preprocessing |
The processing pipeline from raw diffusion-weighted images to 3D tractograms represents a sophisticated methodology for investigating white matter architecture in vivo. When implemented with careful attention to each processing stage—from appropriate data acquisition through rigorous tensor estimation to reproducible fiber tracking—this pipeline provides powerful insights into structural connectivity relevant to behavioral studies and CNS drug development. The standardization of these protocols across research groups will enhance reproducibility and enable more meaningful comparisons across studies, ultimately advancing our understanding of brain structure-function relationships in health and disease.
Diffusion Tensor Magnetic Resonance Imaging (DT-MRI) provides a non-invasive means to investigate white matter architecture and neural connectivity in the living brain. Within behavioral studies research and central nervous system (CNS) drug development, DT-MRI offers a powerful tool for identifying microstructural correlates of behavior and assessing the impact of therapeutic interventions on neural pathways. The reliability of these findings is critically dependent on the careful optimization of acquisition parameters and analysis techniques. This application note provides detailed protocols for selecting b-values, gradient encoding schemes, and fiber tracking algorithms, with a specific focus on applications in behavioral and pharmacological research.
Optimizing Acquisition Parameters
B-Value Selection
The b-value, determining the strength and timing of diffusion-sensitizing gradients, directly influences the sensitivity of DT-MRI to water diffusion. Optimal selection is crucial for balancing signal-to-noise ratio (SNR) with sensitivity to microstructural features.
Table 1: B-Value Optimization for DT-MRI
| Parameter | Recommended Protocol | Physiological Rationale | Impact on Quantitative Metrics |
|---|---|---|---|
| Low b-values | Exclude b-values ≤ 100 s/mm² [71] | Minimizes contamination from perfusion effects in capillaries [71] | Reduces overestimation of ADC; improves accuracy of diffusion metrics [71] |
| High b-values | Include b-values ≥ 1000 s/mm² [71] | Increases sensitivity to restricted diffusion within axonal structures | Provides robust ADC calculation; reduces noise bias in tensor estimation |
| Optimal Combination | Use 2-3 b-values from the set: b=500, 1000, 1300 s/mm² [71] | Balances diffusion weighting and signal attenuation for monoexponential modeling | Yields smallest deviation from biexponential reference models [71] |
| Number of b-values | Minimum 2 (b=0 and b=800), but more are beneficial [11] | Enables calculation of the diffusion tensor at each voxel | Under-sampling leads to inaccurate tensor estimation and noisy maps |
The selection of b-values must also consider the specific application. For instance, in a study focusing on the Frontal Aslant Tract (FAT), a b-value of 800 s/mm² was effectively used alongside a b=0 volume [11].
Gradient Encoding Directions
The number and spatial distribution of gradient encoding directions determine the accuracy and precision of the diffusion tensor estimation.
Table 2: Gradient Direction Scheme Optimization
| Number of Directions | Recommended Scheme | Angular Resolution & Tensor Accuracy | Practical Considerations |
|---|---|---|---|
| 6 Directions | Icosahedron scheme [72] | Optimum for 6 directions; functionally equivalent to numerically optimized solutions (MV, MF, ME) [72] | Heuristic schemes based on cube geometry (vertices, face centers) are suboptimal [72] |
| >6 Directions | Regular polyhedra or numerically optimized solutions (ME, MF, MV) [72] | Improved signal-to-noise and robustness to motion artifacts | No significant advantage beyond 6 directions if an optimum encoding scheme is used [72] |
| Common Practice | 15 directions (medium resolution) [11] | Balances scan time with adequate sampling for deterministic tractography | A medium directional resolution with b=800 was sufficient for FAT tracking [11] |
Protocol for Preprocessing and Data Quality Control
Prior to tensor estimation and fiber tracking, diffusion-weighted images must be preprocessed to correct for artifacts. The following protocol, adapted from a clinical tractography study [11], ensures data integrity.
Experimental Protocol 1: DWI Preprocessing for Tractography
Objective: To correct for common artifacts in DWI data to ensure robust tensor estimation and fiber tracking.
Materials:
- Diffusion-weighted images (DWI) in DICOM or NIfTI format.
- Processing software (e.g., DSI Studio, FSL).
Methodology:
- Data Conversion: Convert raw DICOM files to a processing-friendly format (e.g., NIfTI).
- Artifact Correction:
- Execute
eddy_currentcorrection (e.g., using FSL'seddytool) to remove motion artifacts and eddy current-induced distortions [11].
- Execute
- Brain Masking: Apply a brain mask to remove non-brain tissue from the analysis.
- Tensor Reconstruction: Reconstruct the diffusion tensor or other models (e.g., using Generalized Q-Sampling Imaging in DSI Studio) [11].
- Quality Control:
- Visually inspect corrected images for residual artifacts.
- Check the quality of derived fractional anisotropy (FA) and mean diffusivity (MD) maps for homogeneity and expected contrast.
Fiber Tracking Algorithms and Parameter Selection
Fiber tracking, or tractography, is the process of reconstructing neural pathways from diffusion tensor data. The choice of algorithm and its parameters dictates the biological validity of the results.
Figure 1: A standardized workflow for fiber tractography, from data input to final tract output, incorporating critical steps like parameter setting and pruning.
Experimental Protocol 2: Region of Interest (ROI)-Based Tractography of the Frontal Aslant Tract
Objective: To reliably reconstruct the Frontal Aslant Tract (FAT) using an anatomically constrained ROI-based approach.
Materials:
- Preprocessed DWI data.
- Tractography software (e.g., DSI Studio).
- Brain anatomical atlas (e.g., ICBM152).
Methodology [11]:
- ROI Definition: Define ROIs based on anatomical landmarks in standard space (e.g., using the ICBM152 atlas).
- ROI 1: Superior Frontal Gyrus (SFG).
- Endpoint 1: Inferior Frontal Gyrus, pars opercularis.
- Alternative:
- ROI 2: Supplementary Motor Area (SMA).
- Endpoint 2: Inferior Frontal Gyrus, pars triangularis.
- Algorithm Configuration: Use a deterministic tracking algorithm [11]. Configure key parameters:
- Tract Generation: Run the tracking algorithm between the specified ROI and endpoint.
- Post-processing: Apply topology-informed pruning (e.g., 2 iterations) to remove false-positive streamlines [11].
- Quantification: Extract quantitative metrics for the reconstructed FAT, including:
- Streamline count.
- Mean fiber length.
- Tract volume.
- Mean Fractional Anisotropy (FA) and Mean Diffusivity (MD) of the tract.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for DT-MRI Studies
| Item | Function/Application | Example/Note |
|---|---|---|
| MRI Scanner | Data acquisition. | Preferable 3.0 T for higher signal-to-noise ratio [11]. |
| Head Coil | Signal reception. | 32-channel head coil for improved image quality [11]. |
| Processing Software | Image analysis, tensor calculation, tractography. | DSI Studio, FSL, NordicICE [71] [11]. |
| Anatomical Atlas | Anatomical reference for ROI placement. | ICBM152 adult brain atlas [11]. |
| Denoising Algorithm | Improves signal-to-noise ratio prior to tensor calculation. | Weighted TV-norm minimization [73]. |
Application in CNS Drug Development
In CNS drug development, DT-MRI serves as a pharmacodynamic biomarker to objectively demonstrate the biological impact of a therapeutic intervention on brain structure [74] [55] [75]. For example, a drug aimed at promoting neuroprotection or remyelination might be expected to increase FA or decrease MD in specific white matter tracts. This objective measurement can provide evidence of target engagement and biological activity in early-phase trials, helping to guide go/no-go decisions and dose selection [74] [55]. The optimized protocols outlined herein are essential for ensuring that such imaging biomarkers are reproducible, sensitive to change, and capable of being standardized across multiple clinical trial sites.
Establishing Credibility: Validating DT-MRI Findings and Comparing it to Other Neuroscientific Methods
Diffusion Tensor Imaging (DTI) has emerged as a pivotal magnetic resonance imaging (MRI) technique for investigating the microstructural integrity of white matter in vivo. By measuring the direction and magnitude of water molecule diffusion in neural tissues, DTI provides quantitative metrics that are sensitive to subtle pathological changes often undetectable by conventional imaging [5]. These measurements, including fractional anisotropy (FA), mean diffusivity (MD), axial diffusivity (AD), and radial diffusivity (RD), serve as proxies for tissue organization, myelination, and axonal density [76]. The core premise of this application note is that these microstructural properties form the biological foundation for cognitive functions. By establishing robust correlations between DTI-derived metrics and behavioral performance across neurological conditions, researchers and drug development professionals can identify objective, non-invasive biomarkers for tracking disease progression and therapeutic efficacy. This document provides a structured framework for designing studies and analyzing data to link microstructural changes to cognitive outcomes.
Quantitative Evidence: Linking DTI Metrics to Cognitive Performance
Substantial evidence demonstrates significant correlations between DTI metrics and performance on standardized cognitive tests. The table below summarizes key findings from recent meta-analyses and clinical studies, highlighting the most consistent relationships.
Table 1: Correlations Between DTI Metrics and Cognitive Test Performance
| Cognitive Domain | Cognitive Test | Relevant Brain Region | DTI Metric | Correlation Coefficient (r) | Population | Source |
|---|---|---|---|---|---|---|
| Processing Speed | Symbol Digit Modalities Test (SDMT) | Corpus Callosum | FA | r = 0.54 [0.40, 0.66] | Multiple Sclerosis | [77] |
| Processing Speed | Symbol Digit Modalities Test (SDMT) | Corpus Callosum | MD | r = -0.48 [-0.61, -0.33] | Multiple Sclerosis | [77] |
| Processing Speed | Symbol Digit Modalities Test (SDMT) | Whole White Matter | FA | r = 0.39 [0.24, 0.52] | Multiple Sclerosis | [77] |
| Learning & Memory | California Verbal Learning Test (CVLT) | Fornix | FA | r = 0.35 [0.12, 0.54] | Multiple Sclerosis | [77] |
| Learning & Memory | California Verbal Learning Test (CVLT) | Fornix | MD | r = -0.35 [-0.49, -0.19] | Multiple Sclerosis | [77] |
| Global Cognition | Mini-Mental State Exam (MMSE) | Whole Brain White Matter | FA | r = 0.285* | Elderly | [78] |
| Global Cognition | Modified Mini-Mental State (3MS) | Whole Brain White Matter | FA | r = 0.315* | Elderly | [78] |
*Correlation coefficients for MMSE and 3MS are derived from the study's reported Spearman's rho values for the relationship between FA and cognitive scores.
Key Insights from the Data
- Direction of Correlation: The data reveals a fundamental pattern: higher FA and lower MD are consistently associated with better cognitive performance. This is because high FA indicates coherently bundled, well-myelinated axons, facilitating efficient neural transmission, while low MD indicates restricted water diffusion, reflective of dense, intact cellular structures [76] [77].
- Region-Specificity: The strength of the correlation varies by brain region. The corpus callosum, a critical hub for interhemispheric communication, shows one of the strongest associations with processing speed [77]. The fornix, a key limbic system structure, is specifically linked to memory function [77].
- Clinical Applicability: These relationships hold across different populations, including people with multiple sclerosis (MS) and cognitively normal elderly individuals, suggesting DTI's broad utility as a biomarker for cognitive status in both neurodegenerative and neuroinflammatory conditions [78] [77].
Experimental Protocols for DTI in Behavioral Correlation Studies
Protocol 1: Clinical Study Design for Cognitive Correlation
This protocol outlines the steps for a cross-sectional or longitudinal study investigating the relationship between white matter microstructure and cognitive performance.
A. Participant Characterization and Recruitment
- Cohort Definition: Recruit well-characterized cohorts (e.g., patients with a specific neurological condition and matched healthy controls). For example, a study on MS may enroll patients with relapsing-remitting MS and low Expanded Disability Status Scale (EDSS) scores to investigate early changes [5].
- Sample Size: Justify sample size using power analysis based on expected effect sizes (e.g., correlation coefficients from Table 1). Meta-analyses suggest that samples of ~50 patients per group can reveal significant effects [5] [77].
- Exclusion Criteria: Standardize exclusion criteria, typically including contraindications for MRI, major psychiatric comorbidities, other neurological disorders, and use of medications that significantly impact cognitive function [5] [79].
B. Multimodal Data Acquisition
- Cognitive Assessment: Administer a standardized neuropsychological battery targeting key domains. Essential tests include:
- MRI Acquisition:
- Structural Imaging: Acquire high-resolution 3D T1-weighted (for anatomical parcellation) and T2-weighted/FLAIR images (for lesion detection, e.g., white matter hyperintensity volume) [78].
- DTI Protocol: Use a multi-shell diffusion-weighted sequence on a 3T scanner for optimal data quality.
C. Data Processing and Analysis Pipeline The following workflow diagram outlines the key steps from raw data to statistical correlation.
Diagram 1: DTI-Behavior Correlation Workflow
- Preprocessing: Process DTI data using tools like FSL or MRtrix3. Steps include eddy current correction and head motion correction to minimize artifacts [81].
- Spatial Error Correction: Apply advanced correction methods like the B-matrix Spatial Distribution (BSD-DTI) to mitigate spatial systematic errors induced by gradient field inhomogeneities, which is critical for metric accuracy and cross-protocol comparability [5].
- Region of Interest (ROI) Analysis: Co-register FA/MD maps to a standard brain atlas (e.g., JHU ICBM-DTI-81). Extract mean metric values from predefined ROIs (e.g., corpus callosum, fornix, whole white matter) [77]. For comprehensive analysis, segmentation into 95 ROIs can be performed [5].
- Statistical Analysis: Perform multiple linear regression analyses with cognitive test scores as the dependent variable and DTI metrics as independent variables, while controlling for confounders like age, sex, and education [78] [77].
Protocol 2: Technical Validation and Fiber Tracking Optimization
For studies focusing on nerve fiber tracking specifically, validating and optimizing the tractography pipeline is essential.
A. Tractography Algorithm Selection and Setup
- Algorithm Choice: Select a fiber tracking algorithm suitable for the research question. Probabilistic algorithms (e.g., iFOD2 in MRtrix3) are often preferred for complex fiber architectures [81]. For cranial nerves, the Unscented Kalman Filter (UKF) method, which can model one or two fibers per voxel, has shown high success rates [80].
- Seeding and Termination: Define seed regions accurately. For whole-brain connectomics, seed throughout the white matter. For specific tracts (e.g., facial nerve), manual ROI placement by an expert is required [80]. Termination criteria typically include an FA cutoff (e.g., 0.1-0.2) and a maximum turning angle between steps (e.g., 45°) [81].
B. Optimization and Validation Framework
- Multi-Objective Optimization (MOO): Use a data-driven framework to optimize tracking parameters (e.g., maximum angle, cutoff, minlength) rather than relying on default settings. Employ algorithms like the non-dominated sorting genetic algorithm II (NSGA-II) to find parameters that balance sensitivity and specificity [81].
- Reference Standard Validation: When possible, validate tractography results against a histological ground truth, such as neural tracer data from the same species, which provides definitive evidence of structural connectivity [81].
- Performance Metrics: Evaluate tracking performance using metrics like True Positive Rate (TPR), False Positive Rate (FPR), distance-weighted coverage of axonal tracts, and fiber length [81].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for DTI Studies
| Item | Function/Application | Specification Notes |
|---|---|---|
| 3T MRI Scanner | High-field magnetic resonance imaging for data acquisition. | Essential for high signal-to-noise ratio (SNR) DTI. Multi-channel head coils improve data quality. |
| Diffusion MRI Sequence | Pulse sequence for acquiring diffusion-weighted volumes. | Multi-shell sequences (multiple b-values) are recommended for advanced modeling [5]. |
| FSL (FMRIB Software Library) | Comprehensive software suite for DTI processing and analysis. | Used for eddy current correction, tensor fitting, TBSS, and atlas-based segmentation [78]. |
| MRtrix3 | Advanced software platform for diffusion MRI analysis. | Specializes in probabilistic tractography (e.g., iFOD2 algorithm) and multi-shell data processing [81]. |
| BSD-DTI Phantom/Algorithm | Corrects spatial systematic errors in diffusion measurements. | Critical for ensuring accuracy and comparability of DTI metrics across scanners and protocols [5]. |
| Standardized Cognitive Batteries | Assessment of behavioral correlates (e.g., processing speed, memory). | Tests like the SDMT and CVLT have validated correlations with DTI metrics [77]. |
| Brain Parcellation Atlas | Reference for automated ROI segmentation. | Atlases like the JHU ICBM-DTI-81 provide standardized white matter labels for consistent analysis. |
DTI provides a powerful, non-invasive window into the brain's microstructural architecture, enabling researchers to establish robust, quantitative links between tissue integrity and cognitive performance. The protocols and data summarized here offer a roadmap for designing rigorous studies that can identify sensitive biomarkers for neurological diseases and drug development. By adhering to optimized acquisition protocols, implementing rigorous corrections for spatial errors, and employing validated tractography methods, scientists can reliably use DTI to decode the structural underpinnings of behavior. Future advancements in multi-shell modeling, such as NODDI, and large-scale, open-data projects will further refine our ability to map the complex relationship between brain structure and cognitive function.
Understanding the complex relationship between brain structure, function, and behavior is a fundamental goal of neuroscience research. For over a century, the lesion method—correlating focal brain damage with specific cognitive deficits—has provided foundational insights into brain-behavior relationships [82]. While invaluable, this method is inherently limited by its dependence on naturally occurring lesions. The advent of advanced neuroimaging techniques has dynamically transformed this field, offering non-invasive ways to study both brain structure and function in vivo. Among these, Diffusion Tensor Magnetic Resonance Imaging (DT-MRI or DTI) and functional Magnetic Resonance Imaging (fMRI) have emerged as particularly powerful tools [83].
DT-MRI and fMRI provide complementary information about the brain's organization. DT-MRI excels at visualizing the white matter architecture and structural connectivity by measuring the directionality of water diffusion within neural tracts [2] [70]. In contrast, fMRI maps brain activity by detecting hemodynamic changes associated with neural firing, primarily within grey matter [82] [83]. Used in conjunction with the established principles of the lesion method, this multi-modal approach provides a more comprehensive understanding of the neural substrates of behavior. This is especially critical in behavioral studies research and drug development, where pinpointing both the functional nodes and their structural connections can illuminate mechanisms of action and treatment efficacy [84].
This article details how DT-MRI complements fMRI and the lesion method, providing structured data comparisons, detailed experimental protocols, and visualization tools to guide researchers in integrating these techniques.
Comparative Analysis of Neuroimaging Techniques
The following table summarizes the core technical and application-based characteristics of DT-MRI, fMRI, and the Lesion Method, highlighting their complementary roles.
Table 1: Gold Standard Comparison of DT-MRI, fMRI, and the Lesion Method
| Feature | DT-MRI (Diffusion Tensor Imaging) | fMRI (Functional MRI) | Lesion Method |
|---|---|---|---|
| What it Measures | Directionality and magnitude of water diffusion (anisotropy) in white matter tracts [2]. | Blood-oxygen-level-dependent (BOLD) signal, reflecting hemodynamic changes linked to neural activity [82] [83]. | Focal neurological or cognitive deficits resulting from brain damage. |
| Primary Application | Mapping structural connectivity, white matter integrity, and nerve fiber tracking (tractography) [2] [85]. | Localizing task-evoked or resting-state brain function and functional networks [82] [83]. | Establishing causal brain-behavior relationships and essential brain areas for a function [82]. |
| Key Metrics | Fractional Anisotropy (FA), Mean Diffusivity (MD), Axial/Radial Diffusivity [2]. | BOLD signal percent change, functional connectivity coefficients [86]. | Location and extent of lesion, correlated with neuropsychological test scores. |
| Spatial Resolution | High (millimeter-scale for tract topography) [70]. | High (millimeter-scale for localizing cortical activation) [83]. | Variable (depends on imaging modality used to define the lesion). |
| Temporal Resolution | Low (static snapshot of structure) [2]. | Medium (seconds, limited by hemodynamic response) [82] [87]. | Not applicable (chronic deficit). |
| Strengths | Non-invasive white matter mapping; sensitive to microstructural changes [2] [85]. | Non-invasive whole-brain functional mapping; excellent for network analysis [86] [83]. | Provides causal, not just correlational, evidence for function [82]. |
| Limitations | Lower specificity; cannot resolve crossing fibers well without advanced models [2] [70]. | Indirect measure of neural activity; confounded by noise (e.g., motion) [82] [83]. | Dependent on rare and naturally occurring lesion patterns; lesions are often not anatomically precise. |
Table 2: Quantitative DTI Metrics for Assessing White Matter Integrity in Behavioral Studies
| DTI Metric | Biological Interpretation | Change Associated with Pathology/Disruption | Example Behavioral Correlation |
|---|---|---|---|
| Fractional Anisotropy (FA) | Degree of directional water diffusion; reflects fiber density, myelination, and coherence [2]. | Decrease indicates loss of microstructural organization (e.g., axonal damage) [2] [85]. | Reduced FA in uncinate fasciculus correlated with verbal memory deficits in temporal lobe epilepsy [85]. |
| Mean Diffusivity (MD) / Apparent Diffusion Coefficient (ADC) | Overall magnitude of water diffusion; reflects cellularity and membrane density [2]. | Increase indicates edema, necrosis, or broader tissue damage [2]. | Increased MD in optic radiation associated with visual field loss in glaucoma [70]. |
| Axial Diffusivity (AD) | Rate of diffusion parallel to the primary axon direction [2]. | Increase may indicate axonal degeneration; decrease may indicate acute axonal injury [2]. | Altered AD in white matter tracts during brain maturation [2]. |
| Radial Diffusivity (RD) | Rate of diffusion perpendicular to the primary axon direction [2]. | Increase is associated with demyelination pathology [2]. | Increased RD in corpus callosum in traumatic brain injury [2]. |
Integrated Experimental Protocols
The power of these methods is fully realized when they are integrated into a coherent research workflow. The following protocols outline how to combine them for a comprehensive behavioral study.
Protocol 1: Multi-Modal Imaging for Pre-Surgical Mapping in Tumor Patients
Application Note: This protocol leverages DT-MRI and fMRI to guide surgical planning and predict post-operative outcomes, directly extending the logic of the lesion method by proactively mapping critical circuits [88].
- Participant Preparation & Clinical Assessment:
- fMRI Data Acquisition for Functional Localization:
- Imaging Parameters: Use a 3T MRI scanner. Acquire T1-weighted anatomical images with 1 mm isotropic resolution. For fMRI, use a T2*-weighted single-shot EPI sequence (TR: 2000 ms, TE: 30 ms, flip angle: 90°, voxel size: 2.5 mm isotropic) [88].
- Task Paradigms: Administer block-design paradigms to localize eloquent cortex.
- Motor: Repetitive fist-clenching.
- Sensory: Brush stimulation of the hand.
- Language: Verb generation or word repetition tasks [88].
- Analysis: Preprocess data (motion correction, normalization). Use general linear model (GLM) analysis to generate statistical maps of activation. Threshold maps to identify significant clusters of task-related activity.
- DTI Data Acquisition for Structural Connectivity:
- Imaging Parameters: On the same scanner, acquire diffusion-weighted images using a spin-echo EPI sequence (TR: 8000 ms, TE: 100 ms, voxel size: 2 mm isotropic). Use at least 30 diffusion-encoding directions with a b-value of 1000 s/mm², plus one b=0 volume [85] [88].
- Tractography Analysis:
- Preprocess data (eddy-current correction, motion correction).
- Reconstruct the diffusion tensor and calculate FA and MD maps.
- Seed Region of Interest (ROI) Placement: Use active clusters from the fMRI analysis as ROIs for deterministic or probabilistic tractography [88]. Alternatively, use anatomical landmarks to reconstruct known tracts (e.g., arcuate fasciculus for language, corticospinal tract for motor function).
- Quantification: Calculate mean FA, MD, AD, and RD within the reconstructed tracts of interest.
- Data Integration & Surgical Planning:
- Fuse the T1 anatomical, fMRI activation maps, and DTI tractography models into a single 3D dataset for neuronavigation.
- Plan the surgical trajectory to maximize lesion resection while avoiding the identified eloquent functional cortices (fMRI) and critical white matter pathways (DTI) [88].
- Outcome Correlation:
- Conduct post-operative neurological and neuropsychological assessments at 1, 6, and 12 months.
- Correlate the extent of resection and the integrity of preserved tracts (as measured by DTI metrics) with post-operative functional outcomes [88].
Protocol 2: Investigating Network Disruption in Neurodegenerative Disease
Application Note: This protocol uses the "natural lesion model" of neurodegenerative diseases to study how functional and structural connectivity breakdowns underlie behavioral symptoms like memory loss [84] [85].
- Cohort Selection:
- Recruit patient groups (e.g., Alzheimer's disease, Mild Cognitive Impairment) and age-matched healthy controls. All participants undergo thorough clinical and neuropsychological characterization.
- Multi-Modal Data Acquisition:
- Anatomical Scan: Acquire a high-resolution 3D T1-weighted image (e.g., MPRAGE sequence).
- Resting-State fMRI (rs-fMRI): Acquire a 10-minute T2*-weighted EPI scan while participants fixate on a cross (TR: 2000 ms, eyes open). Instruct participants to remain awake and still.
- DTI Scan: Acquire diffusion-weighted images using parameters similar to Protocol 1, with a higher number of directions (e.g., 60-90) for improved accuracy [2].
- Data Analysis:
- rs-fMRI Processing: Preprocess data (slice-timing correction, motion correction, normalization, band-pass filtering). Perform independent component analysis (ICA) or seed-based correlation analysis to identify resting-state networks (e.g., Default Mode Network). Calculate functional connectivity matrices [86].
- DTI Processing & Tractometry: Reconstruct major white matter tracts (e.g., cingulum, fornix, uncinate fasciculus) using tractography. Use a tractometry approach, sampling DTI metrics (FA, MD) at multiple equidistant points along each tract to create a detailed profile of microstructural integrity [70] [85].
- Statistical Modeling & Correlation with Behavior:
- Compare functional connectivity strength and tract-specific DTI metrics between patient and control groups using ANOVA or general linear models.
- Build multiple regression models to determine whether functional connectivity strength and white matter integrity (DTI metrics) independently or interactively predict scores on memory or cognitive tests [85].
Visualization of Method Synergy
The complementary relationship between DT-MRI, fMRI, and the Lesion Method can be visualized as an integrated workflow for behavioral research.
Diagram 1: Integrated workflow showing synergy between methods.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Integrated DT-MRI/fMRI Studies
| Item / Solution | Function / Application in Research |
|---|---|
| High-Angular Resolution Diffusion Imaging (HARDI) Phantoms | Calibration and validation of DTI scanners and tractography algorithms to ensure measurement accuracy across study sites and time [70]. |
| fMRI Task Paradigm Software (e.g., E-Prime, PsychoPy) | Precisely present sensory, motor, and cognitive stimuli during fMRI scans to reliably evoke and measure brain activity [88]. |
| Neuropsychological Assessment Batteries (e.g., WMS-IV) | Provide standardized, quantitative measures of behavioral output (e.g., memory performance) for correlation with imaging metrics [85]. |
| Multi-Modal Imaging Analysis Suites (e.g., FSL, FreeSurfer, SPM) | Integrated software platforms for processing and co-registering T1, fMRI, and DTI data, enabling voxel-based analysis and tract-based spatial statistics [86]. |
| Biophysical Diffusion Models (e.g., NODDI, DKI) | Advanced models that provide more specific microstructural indices (e.g., neurite density, orientation dispersion) beyond standard DTI metrics, enhancing biological interpretation [70]. |
Diffusion Tensor Magnetic Resonance Imaging (DT-MRI) provides non-invasive, quantitative measures of white matter microstructure, making it a potent candidate for a surrogate endpoint in clinical trials for neurological disorders. Its application in nerve fiber tracking is critical for behavioral studies research, where correlating structural connectivity with cognitive and clinical outcomes is paramount. This document details the regulatory framework, key metrics, and advanced methodologies for employing DT-MRI as a surrogate endpoint. It provides structured protocols for data acquisition, analysis, and validation, specifically contextualized within research on white matter pathways. Designed for researchers and drug development professionals, these application notes aim to standardize practices and facilitate the acceptance of DT-MRI biomarkers in regulatory decision-making.
Within clinical development, a surrogate endpoint is a biomarker intended to substitute for a clinical endpoint, predicting clinical benefit (or harm, or lack of benefit or harm) on the basis of epidemiologic, therapeutic, pathophysiologic, or other scientific evidence [89]. The U.S. Food and Drug Administration (FDA) grants accelerated approval for drugs treating serious conditions that address an unmet medical need based on an effect on a surrogate endpoint that is "reasonably likely to predict clinical benefit" [89]. This pathway is codified in the FDA's Clinical Trial Imaging Endpoint Process Standards Guidance, which mandates rigorous standardization across image acquisition, display, archiving, and interpretation to ensure data quality and reliability [90].
The rationale for developing DT-MRI as a surrogate endpoint stems from its unique ability to quantify in vivo the microstructural integrity of cerebral white matter, which is often compromised in neurological and psychiatric disorders. Tractography, a computational technique that reconstructs white matter tracts from DT-MRI data, allows for the specific assessment of pathways relevant to behavioral functions [70] [91]. Confirmation of clinical benefit is subsequently required through post-marketing studies verifying the effect on a clinically relevant outcome, such as cognitive function or patient-reported quality of life [89]. This framework creates a powerful opportunity to accelerate the development of therapies for conditions where traditional clinical endpoints take years to measure.
Key DT-MRI Metrics for Quantitative Tractography
DT-MRI derives its sensitivity from characterizing the directionally dependent diffusion of water molecules. In organized white matter, water diffuses more freely along the axis of fibers than perpendicular to them, a property known as anisotropy. The diffusion tensor model yields several quantitative parameters that serve as potential biomarkers for white matter integrity [92] [91].
Table 1: Key DT-MRI Scalar Metrics for Assessing White Matter Integrity
| Metric | Full Name | Biological Interpretation | Direction of Change in Injury/Disease |
|---|---|---|---|
| FA | Fractional Anisotropy | Degree of directional restriction of water diffusion; reflects fiber density, axonal diameter, and myelination. | Decrease [70] [91] |
| MD | Mean Diffusivity | Overall magnitude of water diffusion; inversely related to tissue density. | Increase [70] [91] |
| AD | Axial Diffusivity | Rate of diffusion parallel to the primary axon direction. | Variable (may decrease with axonal injury) [70] |
| RD | Radial Diffusivity | Rate of diffusion perpendicular to the primary axon direction; often associated with demyelination. | Increase [70] |
These scalar metrics can be analyzed on a voxel-wise basis or, more powerfully, extracted along specific white matter pathways using tractography. Tractometry refers to the method of quantifying microstructural properties within specific fiber bundles reconstructed via tractography, providing a direct link between a pathway's integrity and its function [70]. This tract-specific approach is essential for behavioral research, as it allows for the correlation of damage in specific neural circuits to deficits in specific cognitive or behavioral domains.
Advanced Diffusion Models and Regulatory-Grade Biomarkers
While standard DT-MRI metrics like FA and MD are widely used, advanced diffusion models can provide more biologically specific information, strengthening the case for a surrogate endpoint.
Table 2: Advanced dMRI Models for Enhanced Biomarker Specificity
| Technique | Description | Key Parameters | Advantage for Surrogate Endpoint Development |
|---|---|---|---|
| DKI | Diffusion Kurtosis Imaging | Mean Kurtosis (MK) | Captures non-Gaussian water diffusion, providing enhanced sensitivity to microstructural complexity in neural tissue [70]. |
| NODDI | Neurite Orientation Dispersion and Density Imaging | Neurite Density Index (NDI), Orientation Dispersion Index (ODI) | Differentiates between contributions from axonal density and fiber dispersion, offering more specific biological interpretation [70]. |
| FBA | Fixel-Based Analysis | Fiber Density (FD), Fiber Cross-Section (FC) | Resolves complex fiber crossings and quantifies distinct fiber populations within a voxel, preventing misinterpretation in areas of crossing fibers [70]. |
The convergence of these advanced imaging techniques with artificial intelligence is further refining tractography accuracy. Deep learning frameworks are now being employed to improve the reconstruction of white matter streamlines, integrating spatial and anatomical information to reduce false-positive connections and enhance the reliability of tract-based metrics [93]. For a surrogate endpoint to be accepted by regulators, the underlying methodology must be standardized and reproducible. The Imaging Review Charter (IRC) is a critical document that details the imaging methodology, reader qualifications, and quality control processes to ensure this consistency across all trial sites [90].
Experimental Protocol: DT-MRI Tractometry for Behavioral Studies
This protocol provides a detailed methodology for employing DT-MRI tractometry in a research setting aimed at validating imaging biomarkers for behavioral correlation.
Materials and Reagents
Table 3: Research Reagent Solutions and Essential Materials
| Item/Category | Specification/Function |
|---|---|
| MRI Scanner | 3T MRI system recommended for superior signal-to-noise ratio [94]. |
| Head Coil | Multi-channel phased-array head coil for high-resolution data acquisition. |
| Diffusion MRI Sequence | Single-shot echo-planar imaging (EPI) sequence. |
| Gradient Directions | Minimum of 30 diffusion-encoding directions to robustly estimate the tensor. |
| b-values | Typically b=0 s/mm² (non-diffusion-weighted) and b=1000 s/mm² [92]. |
| Phantom | Imaging phantom for ongoing scanner calibration and quality assurance [90] [94]. |
| Analysis Software | DTI-dedicated software packages (e.g., DTIStudio, FSL, MedINRIA) for tensor calculation, tractography, and metric quantification [91]. |
Data Acquisition and Preprocessing
- Subject Positioning and Stabilization: Position the subject in the scanner and use foam padding to minimize head movement. Instruct the subject to remain still throughout the scan.
- Sequence Execution: Acquire the diffusion-weighted data using the specified parameters. The acquisition should include:
- One or more volumes without diffusion weighting (b=0 s/mm²).
- Multiple volumes with diffusion sensitization applied along the predefined non-collinear directions [92].
- Data Preprocessing: Process the raw DICOM data using a standardized pipeline, which should include:
- Noise Reduction: Apply methods to mitigate noise in the raw diffusion images.
- Artifact Correction: Correct for eddy currents and subject motion.
- Tensor Calculation: Reconstruct the diffusion tensor model for each voxel, deriving the eigenvalues (λ1, λ2, λ3) and eigenvectors [92] [91].
- Metric Map Generation: Compute scalar maps (FA, MD, AD, RD) from the tensor data.
Tractography and Tractometry Analysis
- Whole-Brain Tractography: Generate a whole-brain tractography model. This can be done using deterministic or probabilistic algorithms, resulting in a set of streamlines representing the white matter architecture [91].
- Tract-of-Interest (TOI) Selection: Isolate specific tracts relevant to the behavioral domain under study (e.g., optic radiation for visual studies, cingulum bundle for memory and emotion, arcuate fasciculus for language). This involves segmenting and cleaning the tract to remove spurious or anatomically implausible streamlines [70] [91].
- Quantitative Tractometry:
- Extract the microstructural scalar values (e.g., FA, MD) from all streamlines within the cleaned TOI.
- Calculate summary statistics (e.g., mean, standard deviation) for each metric within the entire TOI.
- Alternatively, create a "tract profile" by sampling the metric at multiple equidistant nodes along the trajectory of the tract, allowing for the detection of localized changes [70].
Correlation with Behavioral and Clinical Measures
Statistically correlate the tractometry metrics (e.g., mean FA in the cingulum bundle) with behavioral test scores (e.g., results from a processing speed task or a memory recall test). This correlation is the foundational evidence demonstrating that the DT-MRI biomarker is "reasonably likely to predict" a clinically relevant functional outcome [91] [89].
The following diagram illustrates the logical workflow and decision points in the regulatory pathway for a DT-MRI surrogate endpoint, from initial discovery through post-marketing confirmation.
Visualization and Data Interpretation
Effective visualization of multiparametric DT-MRI data is crucial for interpretation and presentation. While grayscale maps are conventional, tri-variate color-coded visualization can merge information from three spatially aligned parameter maps (e.g., FA, MD, NDI) into a single, perceptually uniform image [95]. This method uses the CIELAB color space to ensure Euclidean distances in signal intensity correspond linearly to perceived color differences, allowing human observers to extract complex information more efficiently than from sequential grayscale images [95]. In a diagnostic setting, such color-coded visualization has been shown to achieve diagnostic performance comparable to conventional radiological evaluation [95].
The diagram below outlines the core experimental workflow for a DT-MRI tractometry study, from data acquisition to the final statistical analysis correlating imaging findings with behavior.
DT-MRI has evolved beyond a pure research tool into a strong candidate for a surrogate endpoint in regulatory decision-making for neurological and psychiatric disorders. Its power lies in the ability to provide specific, quantitative, and non-invasive measures of white matter integrity through tractography and tractometry, directly linking brain structure to behavioral and clinical outcomes. Successfully navigating the regulatory pathway requires meticulous attention to standardization, validation, and the demonstration of a clear link between the DT-MRI biomarker and clinically meaningful endpoints. As advanced models and AI-driven tractography continue to improve the specificity and accuracy of these measurements, the case for DT-MRI's role in accelerating the development of effective therapies will only grow stronger.
Diffusion Tensor Magnetic Resonance Imaging (DT-MRI or DTI) has established itself as a pivotal neuroimaging technique for investigating the microstructural architecture of the brain's white matter in vivo. In the specific context of behavioral studies research and drug development, DTI provides a non-invasive window into the integrity and organization of neural fiber pathways, which serve as the structural foundation for brain function and, consequently, behavior. The core principle of DTI rests upon measuring the directionality of water diffusion within biological tissues. In cerebral white matter, water molecules diffuse more readily along the long axis of densely packed, myelinated axons than across them, a property known as anisotropy. By quantifying this directional preference, DTI infers the orientation and microstructural integrity of white matter tracts, enabling researchers to reconstruct the brain's wiring diagram through a process called tractography [9] [2] [96].
For scientists investigating the neural substrates of behavior or the impact of pharmacological agents on the brain, DTI offers a unique biomarker-sensitive tool. Changes in white matter microstructure, whether due to learning, disease, or treatment, can be detected and quantified, providing insights that complement functional imaging and behavioral assays. This application note provides a clear-eyed view of DTI's capabilities and constraints, equipping researchers with the knowledge to effectively integrate this modality into their experimental paradigms.
Core Technical Principles and Quantitative Scalars
At the heart of DTI is the diffusion tensor, a 3x3 matrix mathematically representing the magnitude and direction of water diffusion within each voxel. From this tensor, several key quantitative scalars are derived, each sensitive to different microstructural properties [9] [2].
Table 1: Key DTI-Derived Quantitative Scalars and Their Biological Correlates
| Scalar | Full Name | Biological Interpretation | Significance in Behavioral Research |
|---|---|---|---|
| FA | Fractional Anisotropy | Degree of directional water diffusion; marker of axonal integrity and fiber density [9]. | A reduction often suggests microstructural disruption, potentially correlating with cognitive or behavioral deficits. |
| MD | Mean Diffusivity | Overall magnitude of water diffusion, inverse measure of membrane density [9]. | Increased MD may indicate edema, necrosis, or decreased cellularity. |
| AD | Axial Diffusivity | Diffusion rate parallel to the primary axon direction [9]. | Putatively associated with axonal injury; decreases may reflect axonal damage. |
| RD | Radial Diffusivity | Diffusion rate perpendicular to the primary axon direction [9]. | Putatively associated with myelin integrity; increases may suggest demyelination. |
These scalars provide a multi-faceted profile of white matter health. For instance, a behavioral study might find that poor performance on a cognitive task is correlated with reduced FA and increased RD in the frontal white matter, suggesting that myelin integrity in that region is critical for the task [9]. It is crucial to note that while these scalars are highly sensitive to microstructural changes, they are not highly specific; their interpretation is strengthened when used in combination and in conjunction with other experimental data [9].
Comparative Analysis with Other Imaging Modalities
DTI occupies a specific niche within the broader neuroimaging toolkit. Its strengths are pronounced in certain areas, while other modalities outperform it in others.
Table 2: DT-MRI Versus Other Prevalent Neuroimaging Modalities
| Modality | Primary Strength | Primary Limitation vs. DTI | Ideal Application Context |
|---|---|---|---|
| DT-MRI | Directly assesses white matter microstructure and structural connectivity via tractography [9] [2]. | Less specific to underlying biology (e.g., cannot distinguish axonal loss from demyelination without AD/RD) [9] [97]. | Mapping neural pathways, assessing microstructural integrity in traumatic brain injury, neurodegenerative diseases [9] [2]. |
| Structural T1/T2 MRI | Excellent anatomical detail for visualizing gray matter and gross white matter anatomy. | Insensitive to microstructural organization and directionality of white matter tracts [98]. | Volumetric studies, detecting gross lesions, cortical thickness measurement. |
| fMRI | Maps brain function by measuring blood-oxygen-level-dependent (BOLD) signals. | Provides indirect, hemodynamic correlate of neural activity, not structural connection [99]. | Identifying brain regions involved in specific tasks or states. |
| Diffusion Microstructure Imaging (DMI) | Higher specificity by modeling multiple tissue compartments (intra-axonal, extra-axonal, CSF) [97]. | More complex acquisition and modeling, less established in clinical practice. | Differentiating tumor types, quantifying specific axonal pathologies [97]. |
A critical limitation of DTI is its inability to resolve complex fiber configurations, such as crossing, kissing, or fanning fibers, within a single voxel. The standard tensor model assumes a single primary fiber orientation per voxel, leading to inaccurate tractography in regions with complex architecture [63] [96]. Advanced techniques like High Angular Resolution Diffusion Imaging (HARDI) and Diffusion Spectrum Imaging (DSI) were developed to overcome this limitation, providing a more nuanced view of the neural landscape at the cost of longer acquisition times [100] [98].
Experimental Protocols for Nerve Fiber Tracking
Data Acquisition Protocol
A robust DTI acquisition is the foundation of valid tractography. The following protocol outlines key parameters for a human behavioral study on a 3T scanner.
Objective: To acquire high-quality diffusion-weighted data for whole-brain tractography and microstructural analysis. Primary Output: A diffusion dataset suitable for tensor fitting and probabilistic or deterministic tractography.
Step-by-Step Methodology:
- Sequence: Use a single-shot spin-echo echo-planar imaging (EPI) sequence for its motion robustness [96].
- Diffusion Gradients: Apply diffusion-sensitizing gradients in at least 64 distinct directions to reliably estimate fiber orientation in complex white matter. A higher number of directions (e.g., 90+) improves accuracy but increases scan time [2].
- b-value: Select a b-value of 700-1000 s/mm². This provides an optimal balance between diffusion contrast and signal-to-noise ratio (SNR) [96].
- Isotropic Voxels: Acquire data with isotropic (or near-isotropic) voxels (e.g., 2.0 x 2.0 x 2.0 mm³) to minimize directional bias in tractography.
- Cardiac Gating: If feasible, employ cardiac gating to reduce pulsation artifacts from brainstem and major vessels [96].
- Multiple b=0 Volumes: Acquire several (e.g., 8-10) non-diffusion-weighted (b=0) volumes for improved registration and signal averaging.
Data Processing and Tractography Workflow
Post-processing transforms raw diffusion data into interpretable tractography and scalar maps. The workflow below is implemented using standard software tools like FSL, MRtrix, or DSI Studio [9].
Diagram 1: DTI data processing and analysis workflow.
Detailed Steps:
- Preprocessing: This critical first step involves correcting for distortions and artifacts.
- Eddy Current Correction: Correct for distortions induced by the rapid switching of diffusion gradients using tools like
eddy_correct(FSL) [9]. - Head Motion Correction: Realign all diffusion-weighted volumes to a reference b=0 image to mitigate the effects of subject movement.
- Denoising: Employ algorithms to improve the signal-to-noise ratio, which is crucial for reliable tensor estimation and tractography [63].
- Eddy Current Correction: Correct for distortions induced by the rapid switching of diffusion gradients using tools like
- Tensor Fitting & Scalar Map Generation: Fit the diffusion tensor model to the preprocessed data at each voxel. From the fitted tensors, compute voxel-wise maps of FA, MD, AD, and RD [9] [96].
- Tractography: Reconstruct white matter pathways.
- Deterministic: Algorithms like FACT propagate streamlines based on the principal diffusion direction, moving to the next voxel if the direction is consistent. This method is fast but can fail in regions of complex fiber geometry [9] [101].
- Probabilistic: These algorithms (e.g., in FSL's ProbtrackX) model the uncertainty in fiber orientation at each voxel, generating a distribution of possible pathways. They are more robust to crossing fibers but can produce "false positive" streamlines [101].
- Analysis:
- Tract-Based Spatial Statistics (TBSS): A voxel-wise approach that projects all subjects' FA data onto a mean FA skeleton, mitigating alignment issues and providing a powerful framework for group comparisons [9].
- Region-of-Interest (ROI) Analysis: Manually or automatically place ROIs on specific white matter tracts to extract mean scalar values for correlation with behavioral measures (e.g., symptom severity, drug dosage) [2] [101].
The Scientist's Toolkit: Essential Research Reagents & Software
Successful implementation of a DTI study in behavioral research relies on a suite of specialized software tools and analytical methods.
Table 3: Essential Software Tools for DTI Analysis
| Tool / "Reagent" | Primary Function | Key Utility in Behavioral Research | Access |
|---|---|---|---|
| FSL (TBSS) | Voxel-based cross-subject analysis of FA and other scalar maps [9]. | Gold-standard for unbiased group comparisons (e.g., patients vs. controls). | https://fsl.fmrib.ox.ac.uk/fsl/ |
| MRtrix3 | Advanced tractography using constrained spherical deconvolution to handle crossing fibers [9]. | More accurate reconstruction of complex pathways linked to behavior. | http://www.mrtrix.org/ |
| DSI Studio | Integrated platform for DTI and DSI reconstruction, tractography, and connectometry [9]. | User-friendly interface for rapid tractography and visualization. | http://dsi-studio.labsolver.org/ |
| FreeSurfer (TRACULA) | Fully automated reconstruction of 18 major white matter pathways [9]. | Eliminates manual ROI placement, ensuring reproducibility in large-scale studies. | https://surfer.nmr.mgh.harvard.edu/ |
| Deterministic Tractography | Streamline tracking assuming a single fiber orientation per voxel [101]. | Fast, intuitive visualization of major tracts; useful for surgical planning. | (Implemented in most platforms) |
| Probabilistic Tractography | Tracking that models uncertainty in fiber orientation [101]. | More accurate for connecting regions through complex white matter. | (Implemented in most platforms) |
The following diagram outlines the decision-making logic for selecting an appropriate analysis pathway based on the research question.
Diagram 2: Decision pathway for DTI analysis methods.
DT-MRI is a powerful, non-invasive tool that provides unparalleled insights into the structural connectivity of the living brain, making it invaluable for behavioral neuroscience and drug development. Its strengths in visualizing white matter architecture and quantifying microstructural integrity are tempered by limitations, including low biological specificity and difficulty resolving crossing fibers. The future of diffusion imaging in behavioral research lies in the adoption of more sophisticated models like Diffusion Microstructure Imaging (DMI) and HARDI, which promise greater specificity by disentangling different tissue compartments [97] [98]. Furthermore, the integration of DTI with other modalities, such as fMRI and genetics, in large-scale, longitudinal, and rigorously designed studies is essential to move beyond correlations and toward a causal understanding of how white matter structure shapes behavior and responds to therapeutic intervention [99].
Conclusion
DT-MRI fiber tracking has fundamentally advanced our ability to explore the structural underpinnings of behavior, offering unparalleled in vivo mapping of the brain's connective networks. Its application in disorders like autism demonstrates its power to link specific microstructural abnormalities, such as changes in axon packing density or myelination, with behavioral deficits. For drug development, DT-MRI presents a promising tool for providing objective, imaging-based biomarkers that can help demonstrate drug efficacy on the nervous system, particularly in early-phase trials. Future directions will likely focus on standardizing these methodologies for multi-centre clinical trials, further validating DT-MRI parameters as surrogate endpoints, and integrating them with other functional and molecular imaging techniques to build a more complete, multi-modal understanding of brain function and the impact of therapeutic interventions.
References
- 1. The basis of anisotropic water diffusion in the nervous system [https://pubmed.ncbi.nlm.nih.gov/12489094/]
- 2. Diffusion Tensor Imaging - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK537361/]
- 3. An introduction to diffusion tensor image analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3163395/]
- 4. Processing and visualization for diffusion tensor MRI [https://www.sciencedirect.com/science/article/abs/pii/S1361841502000531]
- 5. Diagnostic performance of a multi-shell DTI protocol and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12340240/]
- 6. Accelerated diffusion tensor imaging with self-supervision ... [https://www.nature.com/articles/s41598-025-96459-9]
- 7. Multi-TE Diffusion MRI Dataset for Exploring Combined ... [https://www.nature.com/articles/s41597-025-05544-1]
- 8. Diffusion Tensor Imaging 101 [https://www.diffusion-imaging.com/2009/05/diffusion-tensor-imaging-101.html]
- 9. Current Clinical Applications of Diffusion-Tensor Imaging in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5897194/]
- 10. A taxonomic guide to diffusion MRI tractography visualization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11631367/]
- 11. A comparison of diffusion tensor imaging tractography ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1543032/full]
- 12. Fiber tracking: A qualitative and quantitative comparison ... [https://www.sciencedirect.com/science/article/pii/S235204771630020X]
- 13. Quantitative assessment of DTI-based muscle fiber tracking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2632726/]
- 14. DSI-Studio: Tractography Software for Diffusion MRI, Fiber ... [https://dsi-studio.labsolver.org/]
- 15. Color Maps: Facilitating the Clinical Impact of Quantitative MRI [https://pmc.ncbi.nlm.nih.gov/articles/PMC11896930/]
- 16. A systematic review of automated methods to perform white ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1376570/full]
- 17. DICOM Standard Status [https://www.dclunie.com/dicom-status/status.html]
- 18. Exploring the Autistic Brain: A Systematic Review of Diffusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384897/]
- 19. Diffusion Tensor Imaging in Autism Spectrum Disorder [https://pmc.ncbi.nlm.nih.gov/articles/PMC3474893/]
- 20. Neuronal fiber pathway abnormalities in autism: An initial MRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3298449/]
- 21. Studying Autism Spectrum Disorder with Structural and ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2016.00211/full]
- 22. Characteristic parameter analysis of magnetic resonance ... [https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-025-05771-w]
- 23. Neuronal Fiber Pathway Abnormalities in Autism - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/18954474/]
- 24. Diagnostic performance of a multi-shell DTI protocol and its ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1618582/full]
- 25. Autism common variants associated with white matter ... [https://www.nature.com/articles/s41398-025-03252-3]
- 26. Evaluating Transferability of ComBat Harmonization ... [https://link.springer.com/article/10.1007/s10439-025-03886-w]
- 27. Altered white matter connectivity of ventral language ... [https://www.sciencedirect.com/science/article/pii/S1053811924002246]
- 28. MRI diffusion tensor tracking of a new amygdalo-fusiform and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2720528/]
- 29. Neuronal fiber pathway abnormalities in autism [https://www.cambridge.org/core/journals/journal-of-the-international-neuropsychological-society/article/neuronal-fiber-pathway-abnormalities-in-autism-an-initial-mri-diffusion-tensor-tracking-study-of-hippocampofusiform-and-amygdalofusiform-pathways/3167A352D49A042EC1EA91201CC43B97]
- 30. Using Diffusion Tensor Imaging and Fiber Tracking to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2852641/]
- 31. Principles of Diffusion Tensor Imaging and Its Applications ... [https://www.sciencedirect.com/science/article/pii/S0896627306006349]
- 32. Optimization of diffusion-tensor MR imaging data ... [https://pubmed.ncbi.nlm.nih.gov/14625784/]
- 33. Insights on Scan‐Specific Deep‐Learning Strategies for Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183417/]
- 34. Current Status and Future Perspectives of Magnetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3586777/]
- 35. Harmonization in Magnetic Resonance Imaging: A Survey ... [https://arxiv.org/html/2507.16962v1]
- 36. Enhancing randomized clinical trials with digital twins [https://www.nature.com/articles/s41540-025-00592-0]
- 37. Digital Twin Technology In Radiology | Journal of Imaging ... [https://link.springer.com/article/10.1007/s10278-025-01597-1]
- 38. FLAIR Diffusion-Tensor MR Tractography - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7976478/]
- 39. Characterization of white matter degeneration in elderly ... [https://www.sciencedirect.com/science/article/abs/pii/S1053811909001426]
- 40. FLAIR and Diffusion MRI Signals Are Independent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3710440/]
- 41. Advanced Analysis of Diffusion Tensor Imaging Along With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8138061/]
- 42. Methods of diffusion MRI tractography for localization of the ... [https://www.sciencedirect.com/science/article/pii/S2213158223001857]
- 43. Application of advanced diffusion MRI based tractometry of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12133882/]
- 44. Neurite orientation dispersion and density imaging in ... [https://www.sciencedirect.com/science/article/pii/S2211034825000677]
- 45. Study of the Diffusion Tensor Imaging for Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8686231/]
- 46. Diffusion Tensor MR Imaging and Fiber Tractography [https://pmc.ncbi.nlm.nih.gov/articles/PMC8128579/]
- 47. Substance Abuse and White Matter: Findings, Limitations, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6440853/]
- 48. Substance abuse and white matter: Findings, limitations ... [https://www.sciencedirect.com/science/article/abs/pii/S0376871618304939]
- 49. Diffusion tensor imaging with cerebrospinal fluid ... [https://www.sciencedirect.com/science/article/abs/pii/S0720048X10000124]
- 50. Effect of CSF Suppression for Diffusional Kurtosis Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC3538115/]
- 51. A Comparison with Conventional and FLAIR DTI Acquisitions [https://pmc.ncbi.nlm.nih.gov/articles/PMC4615277/]
- 52. Oscillating Gradient Spin-Echo Diffusion Tensor Imaging of ... [https://cds.ismrm.org/protected/19MProceedings/PDFfiles/3493.html]
- 53. A Framework for Quality Control and Parameter Optimization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2185542/]
- 54. Quantitative fiber tracking of lateral and interhemispheric white ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2815144/]
- 55. Use of functional imaging across clinical phases in CNS ... [https://www.nature.com/articles/tp201343]
- 56. Evaluating the impact of denoising diffusion MRI data on ... [https://www.nature.com/articles/s41598-025-10947-6]
- 57. Denoising Improves Cross-Scanner and Cross-Protocol Test ... [https://pubmed.ncbi.nlm.nih.gov/40051327/]
- 58. Structure-adaptive sparse denoising for diffusion-tensor MRI [https://www.sciencedirect.com/science/article/abs/pii/S1361841513000078]
- 59. Accelerated in Vivo Cardiac Diffusion-Tensor MRI Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8259662/]
- 60. Comparison of cardiac diffusion MRI using multiple ... [https://pubmed.ncbi.nlm.nih.gov/40953222/]
- 61. Motion-compensated Diffusion MRI of Liver Using High- ... [https://archive.ismrm.org/2025/0669.html]
- 62. Motion-compensated cardiac MRI using low-rank ... [https://arxiv.org/html/2505.03149v1]
- 63. DT-MRI denoising and neuronal fiber tracking [https://www.sciencedirect.com/science/article/abs/pii/S1361841503001014]
- 64. Diffusion metrics provided by DSI Studio [https://dsi-studio.labsolver.org/doc/how_to_interpret_dmri.html]
- 65. Diffusion MRI acquisition [https://bio-protocol.org/exchange/minidetail?id=17772673&type=30]
- 66. Visualization, Interaction and Tractometry [https://pmc.ncbi.nlm.nih.gov/articles/PMC5483435/]
- 67. Advanced Body Diffusion: Acquisition & Reconstruction [https://www.ismrm.org/25/program-files/O-28.htm]
- 68. A Comparison of Skeletal Muscle Diffusion Tensor Imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12529087/]
- 69. How many streamlines are required for reliable ... [https://www.sciencedirect.com/science/article/pii/S1053811920301336]
- 70. Application of advanced diffusion MRI based tractometry ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1577991/full]
- 71. Low b-values in apparent diffusion coefficient calculations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553313/]
- 72. Comparison of gradient encoding schemes for diffusion-tensor MRI [https://pubmed.ncbi.nlm.nih.gov/11329200/]
- 73. DT-MRI denoising and neuronal fiber tracking - PubMed [https://pubmed.ncbi.nlm.nih.gov/15063860/]
- 74. The role of fMRI in drug development - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5931333/]
- 75. Magnetic Resonance Imaging (MRI) In Drug Development [https://www.ddw-online.com/magnetic-resonance-imaging-mri-in-drug-development-683-201512/]
- 76. MRI Fiber Tracking May Be Potential Biomarker of ... [https://smanewstoday.com/news/mri-fiber-tracking-may-be-potential-biomarker-sma-course-response-therapy/]
- 77. A systematic review and meta-analysis [https://pubmed.ncbi.nlm.nih.gov/39798200/]
- 78. Exploring the relationship between cognitive performance ... [https://pubmed.ncbi.nlm.nih.gov/41124430/]
- 79. Cognitive implications of white matter microstructural ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1503599/full]
- 80. Facial nerve tractography using diffusion MRI: A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11458140/]
- 81. Optimization and validation of diffusion MRI-based fiber ... [https://www.nature.com/articles/s41598-020-78284-4]
- 82. Functional Imaging and Related Techniques - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3225087/]
- 83. Exploring the Frontiers of Neuroimaging: A Review ... [https://www.mdpi.com/2075-1729/13/7/1472]
- 84. Advanced Imaging Techniques (PET, fMRI, DTI) in Early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245986/]
- 85. Diffusion tensor imaging with tractography to predict ... [https://www.sciencedirect.com/science/article/abs/pii/S0967586825004990]
- 86. A Comparison of Static and Dynamic Functional ... [https://www.nature.com/articles/s41598-019-42090-4]
- 87. Brain Imaging: SPECT, fMRI, & QEEG and what they ... [https://www.neurocaregroup.com/news-insights/brain-imaging-what-they-uncover]
- 88. Functional Magnetic Resonance Imaging and Diffusion ... [https://www.mdpi.com/2076-3425/13/11/1574]
- 89. Proposed study designs for approval based on a surrogate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11514055/]
- 90. Clinical Trial Imaging Endpoints for Regulatory Compliance [https://collectiveminds.health/articles/clinical-trial-imaging-endpoints-for-regulatory-compliance-a-comprehensive-guide]
- 91. Quantitative Tractography Metrics of White Matter Integrity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2745947/]
- 92. Diffusion Tensor Magnetic Resonance Imaging Strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5992900/]
- 93. Deep learning-based diffusion MRI tractography [https://www.sciencedirect.com/science/article/pii/S1053811925003179]
- 94. ADNI | MRI [https://adni.loni.usc.edu/data-samples/adni-data/neuroimaging/mri/]
- 95. Color-coded visualization of magnetic resonance imaging ... [https://www.nature.com/articles/srep41107]
- 96. Diffusion Tensor Imaging and Its Application to ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2853779/]
- 97. A systematic review of diffusion microstructure imaging (DMI) [https://www.sciencedirect.com/science/article/pii/S2666459325000587]
- 98. Comparative Study of MRI Modality Embeddings for ... [https://www.mdpi.com/2673-4591/112/1/57]
- 99. Current limitations and future directions in MRI studies of child ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4029914/]
- 100. Diffusion-weighted magnetic resonance imaging [https://en.wikipedia.org/wiki/Diffusion-weighted_magnetic_resonance_imaging]
- 101. Brainstem Diffusion Tensor Tractography and Clinical ... [https://www.frontiersin.org/journals/pain-research/articles/10.3389/fpain.2022.840328/full]