Neuroplasticity in Behavioral Adaptation and Optimal Performance: Mechanisms, Applications, and Therapeutic Frontiers
This article synthesizes current research on neuroplasticity to provide a comprehensive framework for understanding its role in behavioral adaptation and the pursuit of optimal performance.
Neuroplasticity in Behavioral Adaptation and Optimal Performance: Mechanisms, Applications, and Therapeutic Frontiers
Abstract
This article synthesizes current research on neuroplasticity to provide a comprehensive framework for understanding its role in behavioral adaptation and the pursuit of optimal performance. Targeting researchers, scientists, and drug development professionals, it explores foundational mechanisms, from synaptic remodeling and neurogenesis to large-scale network reorganization. It critically evaluates innovative methodologies—including neuromodulation, cognitive remediation, and biomarker-guided interventions—for harnessing plasticity. The review also addresses significant challenges such as maladaptive plasticity and recovery plateaus, while presenting validation strategies through advanced neuroimaging and case studies. Finally, it discusses the translational implications of these findings for developing next-generation therapeutic interventions and precision medicine approaches in neurology and psychiatry.
The Core Mechanisms of Neuroplasticity: From Synapses to Systems
Neuroplasticity is fundamentally defined as the ability of the nervous system to change its activity in response to intrinsic or extrinsic stimuli by reorganizing its structure, functions, or connections [1]. This dynamic capacity, which persists throughout the lifespan, allows the brain to adapt following injuries, learn new skills, consolidate memories, and adjust to environmental changes [2]. The concept of a plastic brain stands in stark contrast to the early, rigid view of the brain as a static organ. Research has now firmly established that the brain exhibits a remarkable capacity for functional and structural change, a property central to behavioral adaptation and the pursuit of optimal performance [3]. This whitepaper provides a technical guide to the core mechanisms, experimental methodologies, and key research tools in neuroplasticity research, framed within the context of behavioral adaptation and optimal performance.
Core Mechanisms of Neuroplasticity
Neuroplasticity manifests through two primary, interconnected biological mechanisms: structural plasticity, which involves physical changes to neuronal connections and brain anatomy, and functional plasticity, which involves changes in the efficiency and strength of synaptic communication and network dynamics [2] [1].
Structural Neuroplasticity
Structural plasticity refers to the brain's ability to change its physical architecture. This includes:
- Synaptic Plasticity: The experience-dependent long-lasting change in the strength of neuronal connections, most famously exemplified by long-term potentiation (LTP). LTP, first discovered by Bliss and Lomo in 1973, describes the persistent strengthening of synapses based on recent patterns of activity, forming a fundamental cellular model for learning and memory [1].
- Morphological Changes: Alterations in neuronal morphology, such as increased dendritic spines, modified dendritic branching, and the formation of new synapses [3].
- Adult Neurogenesis: The generation of new neurons in the adult brain. While conclusively demonstrated in the hippocampus and olfactory bulb of small mammals, its extent and functional significance in humans remain an active area of investigation and debate [2] [1].
Functional Reorganization
Functional plasticity involves the reassignment of neural resources to support adaptation, particularly after injury. Key concepts include:
- Vicariation and Equipotentiality: Vicariation occurs when a brain region takes on a new, unrelated function, while equipotentiality suggests that if damage occurs early in life, other brain areas have the potential to assume lost functions. Modern neuroimaging shows the brain employs a combination of both, with the remaining hemisphere reorganizing to restore function after procedures like hemispherectomy [1].
- Diaschisis: A concept where damage to one part of the brain causes a loss of function in a distant, but connected, area due to the loss of excitatory input. This can be observed as hypoperfusion in the ipsilateral thalamus following a middle cerebral artery stroke [1].
- Map Expansion: The phenomenon where the cortical representation of a frequently used body part expands at the expense of less-used areas, demonstrating the experience-dependent nature of functional organization [2].
Table 1: Key Concepts in Functional Reorganization After Brain Injury
| Concept | Definition | Clinical/Experimental Example |
|---|---|---|
| Vicariation | A brain region overtakes a new function that it was not originally responsible for. | Reorganization of the supplemental motor area to control motor function after a primary motor cortex stroke [1]. |
| Equipotentiality | The capacity of certain brain areas, particularly in the young brain, to assume the functions of a damaged region. | Functional recovery after unilateral brain injury in childhood, where the remaining hemisphere supports development [1]. |
| Diaschisis | Loss of function in a brain region remote from, but connected to, the site of primary damage. | Hypoperfusion of the ipsilateral thalamus observed after an acute middle cerebral artery (MCA) stroke [1]. |
Quantitative Frameworks and Research Data
A key application of neuroplasticity research involves developing interventions to enhance brain performance and resilience. Physical exercise serves as a powerful, non-pharmacological modulator of brain plasticity, with its effects quantifiable across different exercise modalities.
Table 2: Neuroplasticity Outcomes Modulated by Physical Exercise Parameters
| Exercise Modality | Intensity | Duration | Key Neuroplastic Effects on Brain Networks |
|---|---|---|---|
| Cardiovascular | Light-to-Moderate (57-76% HRmax) | Long-Term (≥1 year) | Increased functional connectivity in the Default Mode and Salience Networks [4]. |
| Strength | Vigorous (70-<85% 1RM) | Short-Term (<1 year) | Functional changes in the Central Executive and Visuospatial Networks [4]. |
| Mixed Exercise | Light-to-Moderate | Long-Term (≥1 year) | Structural and functional changes in the Sensorimotor Network [4]. |
The timeline of neuroplastic changes following neural injury occurs in distinct, overlapping phases, which can be quantified and targeted for therapeutic intervention.
Table 3: Temporal Phases of Neuroplasticity After Injury
| Phase | Timeline | Primary Neuroplastic Events |
|---|---|---|
| Acute | First 48 hours | Initial cell death and loss of cortical pathways; recruitment of secondary neuronal networks to maintain function [1]. |
| Subacute | Following weeks | Shift in cortical pathways from inhibitory to excitatory; synaptic plasticity and formation of new connections [1]. |
| Chronic | Weeks to months | Axonal sprouting and further structural reorganization of brain networks around the site of damage [1]. |
Experimental Protocols and Methodologies
Protocol: Investigating Experience-Dependent Plasticity Using an Enriched Environment Paradigm
This protocol is used to study how complex sensory, cognitive, and motor stimulation drive structural and functional plasticity in animal models, relevant to research on optimal performance and cognitive reserve [3].
- Subject Housing: Randomly assign subjects (e.g., rodent models) to either an Enriched Environment (EE) or a Standard Environment (SE) control group.
- Environmental Design:
- EE Condition: A large cage containing a variety of changing stimuli such as running wheels, tunnels, ladders, and novel objects of different textures and shapes. Social housing is standard.
- SE Condition: A standard laboratory cage with standard bedding, food, and water but no additional complex stimuli.
- Intervention Duration: The intervention typically lasts for several weeks to months, with objects in the EE being rearranged and replaced regularly to maintain novelty.
- Tissue Preparation and Analysis:
- Perfuse and fix the brains transcardially.
- Section brain regions of interest (e.g., hippocampus, cerebral cortex).
- Employ staining techniques such as Golgi-Cox impregnation to visualize and quantify dendritic branching and spine density.
- Use immunohistochemistry for markers like c-Fos to map neuronal activity or BrdU/DCX to assess adult neurogenesis.
- Behavioral Correlates: Conduct behavioral tests (e.g., Morris water maze, novel object recognition) at the end of the environmental exposure period to correlate neuroplastic changes with cognitive performance.
Protocol: Functional MRI (fMRI) in Studying Neuroplasticity in Post-Stroke Aphasia
This protocol assesses functional reorganization of language networks in the human brain after injury, a key area for understanding vicariation and diaschisis [5].
- Participant Selection: Recruit a cohort of individuals with post-stroke aphasia and age-matched neurologically normal controls.
- Task Design: Develop a block-design or event-related fMRI paradigm. Tasks should engage core language processes (e.g., auditory comprehension, semantic decision, verbal fluency) and include a low-level control task (e.g., tone discrimination, rest) for contrast.
- Data Acquisition: Acquire high-resolution T1-weighted anatomical images and T2*-weighted BOLD fMRI images on a 3T MRI scanner.
- Preprocessing: Preprocess data using standard pipelines (e.g., SPM, FSL) including realignment, slice-time correction, normalization to standard space (e.g., MNI), and smoothing.
- Statistical Analysis:
- Model the BOLD response for each condition at the single-subject level.
- Perform second-level group analyses to identify:
- Between-Group Differences: Regions showing significantly different activation in patients vs. controls.
- Correlation with Behavior: Regions where activation magnitude correlates with language performance scores in the aphasia group.
- Critical Methodological Considerations:
- Control for Task Performance: Match task difficulty or use performance as a covariate to avoid confounds from differing effort or ability [5].
- Contrast Validity: Ensure the task contrast effectively isolates language-specific activation in control subjects [5].
- Multiple Comparisons Correction: Apply appropriate family-wise error (FWE) or false discovery rate (FDR) correction to statistical maps [5].
The Scientist's Toolkit: Key Research Reagent Solutions
Cutting-edge research in neuroplasticity relies on a suite of sophisticated tools and reagents to probe the molecular, cellular, and systems-level mechanisms of brain adaptation.
Table 4: Essential Research Tools and Reagents in Neuroplasticity Research
| Research Tool/Reagent | Primary Function/Application |
|---|---|
| Bruker timsTOF Ultra 2 Mass Spectrometer | A state-of-the-art instrument for single-cell proteomic and lipidomic analysis, enabling the precise quantification of proteins and lipids within individual neurons to study aging and cognitive decline [6]. |
| Patch-seq | An integrated technique that combines patch-clamp electrophysiology (to record neuronal electrical activity), immunohistochemistry (to locate proteins), and single-cell RNA sequencing (to profile gene expression) to comprehensively characterize individual neurons [6]. |
| Phosphospecific Antibodies | Antibodies that target phosphorylated epitopes on proteins (e.g., NMDA receptor subunits, CREB) to study activity-dependent signaling cascades and synaptic plasticity mechanisms like LTP [2]. |
| Neuromodulators (Dopamine Agonists/Antagonists) | Pharmacological agents used to manipulate dopaminergic and other neuromodulatory systems, which are known to positively influence synaptic plasticity and learning [1]. |
| Activity-Dependent Biomarkers (c-Fos, Arc) | Endogenous proteins whose expression is rapidly upregulated in neurons following activation. Their detection via immunohistochemistry or in situ hybridization allows for functional mapping of neural circuits engaged by specific experiences or behaviors [3]. |
| BrdU (Bromodeoxyuridine) | A thymidine analog that incorporates into the DNA of dividing cells. It is used in conjunction with cell-specific markers (e.g., NeuN, DCX) to label and track the birth, migration, and fate of new neurons in the process of adult neurogenesis [3]. |
Signaling Pathways and Experimental Workflows
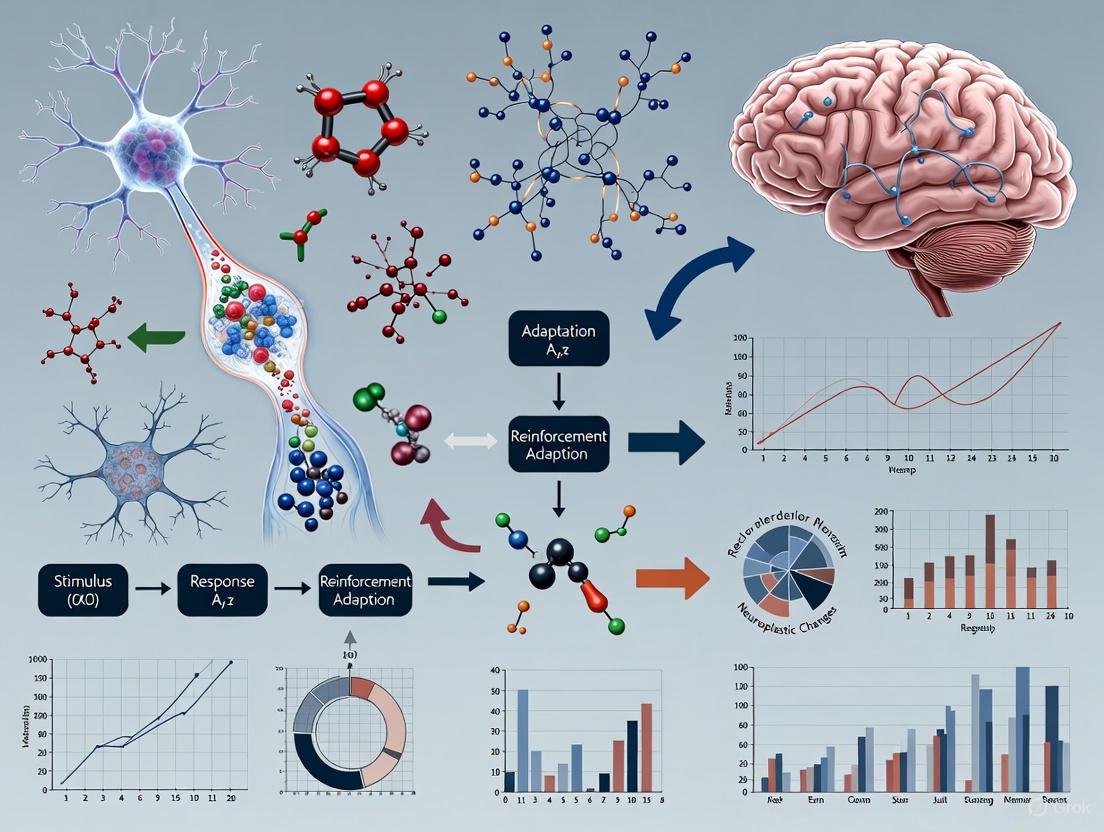
The following diagrams, generated using Graphviz DOT language, illustrate core concepts and experimental workflows in neuroplasticity research. The color palette and contrast ratios adhere to the specified technical requirements.
Hebbian Synaptic Plasticity Pathway
Functional Reorganization Post-Stroke
Single-Cell Plasticity Analysis Workflow
Neuroplasticity, the biological capacity of the brain to reorganize its neural connections in response to environmental stimuli, experience, learning, and injury, serves as the fundamental substrate for behavioral adaptation and optimal performance [7]. This adaptive capability encompasses a range of cellular and molecular mechanisms, including changes in synaptic strength and connectivity, the formation of new synapses, alterations in the structure and function of neurons, and the generation of new neurons [7]. For researchers and drug development professionals, understanding these core mechanisms—synaptic plasticity, dendritic remodeling, and neurogenesis—is paramount for developing interventions that enhance brain function and promote resilience across the lifespan. This technical guide synthesizes current research on these foundational processes, framing them within the broader thesis of neuroplasticity's role in enabling organisms to achieve optimal performance in dynamic environments, a concept explored in adaptive neurobiological plasticity research [3] [8].
Synaptic Plasticity: Mechanisms of Information Storage
Synaptic plasticity refers to the activity-dependent modification of the strength and efficacy of synaptic transmission. This dynamic process is widely regarded as the primary cellular mechanism underlying learning and memory [9] [7].
Key Molecular Mechanisms
Long-Term Potentiation (LTP) and Long-Term Depression (LTD) represent the most extensively studied forms of functional synaptic plasticity. LTP is a persistent strengthening of synapses based on recent patterns of activity, whereas LTD is a persistent weakening of synapses [7]. The induction of these processes often involves NMDA receptor activation, leading to calcium influx that triggers divergent intracellular signaling cascades [9]. Expression mechanisms include:
- AMPA receptor trafficking: LTP often involves the insertion of additional AMPA receptors into the postsynaptic density, while LTD involves their internalization [9].
- Phosphorylation/dephosphorylation cycles: Key enzymes include Ca²⁺/calmodulin-dependent protein kinase II (CaMKII), which promotes AMPA receptor insertion during LTP, and protein phosphatases that facilitate AMPA receptor removal during LTD [9].
- Structural modifications: Changes in synapse size and shape often accompany long-lasting plasticity [10].
Table 1: Quantitative Profiles of Dendritic Spine Subtypes Observed In Vivo
| Spine Subtype | Relative Stability | Morphological Characteristics | Functional Correlates |
|---|---|---|---|
| Filopodia | Highly dynamic (appear/disappear in ~10 min) [10] | Long, thin protrusions without bulbous heads [10] | Predominant in early postnatal life; exploratory function [10] |
| Thin Spines | Moderately dynamic (can persist days) [10] | Small heads with long, thin necks [10] | Potential transitional state; can form functional synapses [10] |
| Mushroom Spines | Highly stable (can persist months to years) [10] | Large heads with variably lengthed necks [10] | Considered "memory spines" with stable synaptic connections [10] |
| Stubby Spines | Moderately stable | Originally described as lacking necks; STED microscopy reveals very short necks [10] | May represent active mushroom spines with shortened necks [10] |
Experimental Protocols for Synaptic Plasticity Research
In Vivo Two-Photon Microscopy for Spine Imaging:
- Animal Preparation: Utilize transgenic mice (e.g., Thy1-GFP) or deliver fluorophores via viral transmission, in utero electroporation, or single-cell electroporation for controlled neuronal labeling [10].
- Cranial Window Surgery: Either perform a craniotomy followed by implantation of a transparent window or use a less invasive thinned-skull technique where the skull is carefully shaved to approximately 20μm thickness [10].
- Image Acquisition: Image the same dendritic segments repeatedly over days to months using two-photon microscopy [10].
- Data Analysis: Quantify spine density, morphology, formation, and elimination rates across experimental conditions [10].
Electrophysiological Assessment of LTP/LTD:
- Slice Preparation: Prepare acute hippocampal or cortical brain slices (300-400μm thick) from rodents.
- Stimulation and Recording: Place a stimulating electrode in afferent pathways and a recording electrode in the postsynaptic region.
- Baseline Recording: Measure field excitatory postsynaptic potentials (fEPSPs) for at least 20 minutes to establish stable baseline transmission.
- Induction Protocol: Apply high-frequency stimulation (e.g., 100Hz tetanus) for LTP or low-frequency stimulation (e.g., 1Hz for 15 minutes) for LTD.
- Monitoring: Record fEPSPs for at least 60 minutes post-induction to quantify the magnitude and persistence of plasticity [9].
Dendritic Remodeling: Structural Adaptation of Neural Circuits
Dendritic spines are small protrusions studding neuronal dendrites that constitute the postsynaptic sites of most excitatory synapses in the mammalian brain [10]. Their structural plasticity represents a critical interface between experience and neural circuit modification.
Spine Dynamics and Behavioral Adaptation
Dendritic spines are highly dynamic structures whose turnover and stabilization are modulated by neuronal activity, experience, and developmental age [10]. In vivo imaging studies reveal that spine dynamics follow specific patterns across development and different cortical regions:
Table 2: In Vivo Spine Stability Across Development and Brain Regions
| Brain Region | Animal Age | Stability Measurement | Key Findings | Citation |
|---|---|---|---|---|
| Visual Cortex, Layer 5 | P30 | 73% stable over 30 days | Spines become more stable from juvenile to adult ages | [10] |
| Visual Cortex, Layer 5 | 4 months | 96% stable over 30 days | Significant stabilization in adulthood | [10] |
| Somatosensory Cortex, Layer 5 | P16-25 | 35% stable over ≥8 days | Developmental increase in stability | [10] |
| Somatosensory Cortex, Layer 5 | P175-225 | 73% stable over ≥8 days | Progressive stabilization through adolescence | [10] |
| Barrel Cortex, Layer 5 | P30 | 60% stable over 22 months | Subset of spines can last throughout life | [10] |
| Barrel Cortex, Layer 5 | 4-6 months | 74% stable over 18 months | Increased stability in adulthood | [10] |
Experimental Protocols for Dendritic Spine Analysis
Long-Term In Vivo Spine Imaging Protocol:
- Animal Model Selection: Use Thy1-GFP-M or similar transgenic mice expressing fluorescent proteins in sparse neuronal populations [10].
- Surgical Preparation: Implement either thinned-skull or cranial window approach based on experimental needs. Thinned-skull is less invasive but requires re-thinning for long-term studies; cranial windows allow longer imaging durations but may cause initial inflammation [10].
- Baseline Imaging: Collect high-resolution z-stacks of labeled dendritic segments using two-photon microscopy.
- Experimental Manipulation: After baseline imaging, introduce experimental variables such as sensory deprivation, motor learning tasks, or pharmacological treatments [10].
- Longitudinal Imaging: Re-image the exact same dendritic segments at multiple time points (hours to months apart) using vascular landmarks and branch patterns for relocation.
- Morphological Classification: Categorize spines based on established morphological criteria (filopodia, thin, stubby, mushroom) and track their fate over time [10].
Correlative Light and Electron Microscopy (CLEM):
- Perform in vivo two-photon imaging of spines as described above.
- Transcardially perfuse animal with fixative following final imaging session.
- Process brain tissue for EM analysis using standard protocols.
- Relocate the previously imaged dendritic segments using distinctive landmarks.
- Correlate spine dynamics observed in vivo with ultrastructural features such as postsynaptic density size, presynaptic bouton characteristics, and mitochondrial content [10].
Neurogenesis: Adding New Neurons to Existing Circuits
Neurogenesis refers to the process of generating new functional neurons from neural precursor cells. While most prolific during development, this process continues in specific regions of the adult brain, contributing to neural plasticity throughout the lifespan [7].
Developmental and Adult Neurogenesis
Developmental Neurogenesis occurs primarily during embryonic and early postnatal stages, involving the proliferation, migration, and differentiation of neural precursor cells from the ventricular zone [7]. Key stages include:
- Neural tube formation around embryonic day 30 in humans
- Interkinetic nuclear migration of neural stem cells between weeks 4-5 of human gestation
- Neurogenesis onset around gestational week 5 with asymmetric division of radial glial cells
- Synaptogenesis beginning approximately at human gestational week 27, continuing postnatally with a peak synapse density around age two followed by synaptic pruning [7]
Adult Neurogenesis persists in two main neurogenic niches: the subventricular zone (SVZ) lining the lateral ventricles and the subgranular zone (SGZ) of the hippocampal dentate gyrus [7]. The process involves highly regulated stages of cell proliferation, neuronal fate specification, migration, maturation, and functional integration into existing circuits [7].
Experimental Protocols for Neurogenesis Research
Labeling and Tracking Adult-Born Neurons:
- Thymidine Analog Administration: Inject animals with bromodeoxyuridine (BrdU) or other thymidine analogs to label dividing cells.
- Perfusion and Tissue Collection: Sacrifice animals at multiple time points post-injection (hours for proliferation, days for fate specification, weeks for maturation and integration).
- Immunohistochemical Processing: Use antibodies against BrdU combined with cell-type-specific markers (e.g., NeuN for mature neurons, GFAP for astrocytes, DCX for immature neurons).
- Quantification: Employ stereological counting methods (e.g., optical fractionator) to obtain unbiased estimates of cell numbers in neurogenic regions.
Functional Manipulation of Neurogenesis:
- Genetic Ablation Models: Use transgenic approaches (e.g., thymidine kinase models) to specifically ablate dividing neural precursor cells.
- Optogenetic/Chemogenetic Manipulation: Express light-sensitive or designer receptor exclusively activated by designer drug (DREADD) proteins in adult-born neurons to selectively activate or inhibit their activity.
- Behavioral Assessment: Evaluate cognitive functions (particularly hippocampus-dependent tasks such as pattern separation) following manipulation of adult neurogenesis.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Research Reagent Solutions for Neuroplasticity Studies
| Reagent/Method | Function/Application | Key Examples/Notes |
|---|---|---|
| Thy1-GFP Transgenic Mice | Sparse neuronal labeling for in vivo imaging | Enables longitudinal tracking of dendritic spines in specific neuronal populations [10] |
| Two-Photon Microscopy | High-resolution live imaging in intact brain | Allows repeated imaging of the same neuronal structures over time with minimal phototoxicity [10] |
| BrdU (Bromodeoxyuridine) | Thymidine analog for labeling dividing cells | Used to birth-date newborn cells and track their fate in neurogenesis studies [7] |
| Cell-Type-Specific Markers | Identification of neural cell types | Sox2, Nestin (neural stem cells); DCX, βIII-tubulin (immature neurons); NeuN (mature neurons) [7] |
| Viral Vector Systems | Targeted gene delivery | AAVs, lentiviruses for gene overexpression, knockdown, or expression of fluorescent reporters [10] |
| Electrophysiology Setup | Functional assessment of synaptic transmission | Extracellular field recordings for LTP/LTD; patch-clamp for detailed biophysical analysis [9] |
| STED Microscopy | Superresolution imaging | Reveals spine ultrastructural details (e.g., short necks of stubby spines) beyond diffraction limit [10] |
The cellular and molecular mechanisms of synaptic plasticity, dendritic remodeling, and neurogenesis represent complementary adaptive strategies the brain employs to optimize performance in dynamic environments. Synaptic plasticity provides the mechanism for rapid information storage, dendritic remodeling enables structural circuit adaptation, and neurogenesis introduces new computational elements into existing networks. Research in adaptive neurobiological plasticity suggests that interventions such as environmental enrichment, which enhances behavioral affordances, can harness these mechanisms to promote cognitive reserve and resilience [3]. For drug development professionals, understanding these foundational processes and their methodological assessment provides critical insights for developing targeted therapies that enhance neuroplasticity to maintain optimal brain function across the lifespan and in neurological disorders.
The central nervous system's (CNS) limited regenerative capacity presents a significant challenge in treating neurodegenerative diseases, traumatic injuries, and stroke-related damage. Within this context, neuroplasticity—the brain's ability to reorganize its structure and function—provides the fundamental framework for behavioral adaptation and functional recovery. The efficacy of this plastic response is not solely governed by neurons but is critically orchestrated by a suite of non-neuronal cells that create permissive microenvironments for repair. Glial cells, once considered merely supportive "neural glue," are now recognized as active participants in neural circuit formation, plasticity, and regeneration [11] [12]. Similarly, neural stem cells (NSCs) and oligodendrocytes play indispensable roles in replenishing cellular components and restoring efficient neural communication. Understanding the precise mechanisms by which these cellular players contribute to neural repair is paramount for developing targeted therapeutic strategies that optimize the brain's innate capacity for self-renewal and functional adaptation, ultimately enhancing behavioral outcomes and cognitive performance following neurological insult.
This technical review synthesizes contemporary research on the roles of glial cells, neural stem cells, and oligodendrocytes in neural repair mechanisms, framing their functions within the broader context of neuroplasticity-driven recovery. We provide detailed experimental methodologies, quantitative analyses of cellular responses, and visualization of key signaling pathways to serve as a comprehensive resource for researchers and drug development professionals working at the frontier of regenerative neurology.
Glial Cells: Master Regulators of the Neural Milieu
Astrocytes: Dual Roles in Synaptic Homeostasis and Scar Formation
Astrocytes, a predominant glial cell type, exhibit functional duality in neural repair processes. They are integral to synaptic homeostasis, regulating extracellular neurotransmitter levels, particularly glutamate, via excitatory amino acid transporters (EAATs) to prevent excitotoxicity [13]. Furthermore, astrocytes release gliotransmitters such as ATP and D-serine, which are essential for synaptic plasticity and memory encoding [13]. Following injury, however, astrocytes undergo reactive astrogliosis, forming glial scars that initially seal the lesion site but subsequently release chondroitin sulfate proteoglycans (CSPGs) that inhibit axonal regeneration [11].
Table 1: Astrocyte Functions and Associated Molecular Markers in Neural Repair
| Function | Mechanism | Key Molecular Players | Impact on Repair |
|---|---|---|---|
| Synaptic Homeostasis | Glutamate uptake, gliotransmitter release | EAATs, D-serine, ATP [13] | Prevents excitotoxicity, supports plasticity |
| Metabolic Support | Lactate shuttle via Aquapor-4 (AQP4) channels | AQP4, MCT1 [11] [13] | Provides energy substrate for neurons |
| Edema Regulation | Cellular volume regulation at blood-brain barrier | TRPV4 channels, AQP4 [11] | Modulates severity of cerebral edema during ischemia |
| Scar Formation | Reactive gliosis, CSPG secretion | GFAP, CSPGs [11] | Barriers lesion site but inhibits regeneration |
Microglia: Immune Surveillance and Synaptic Remodeling
As the resident immune cells of the CNS, microglia are pivotal in responding to injury by clearing cellular debris and modulating neuroinflammation [11]. They exhibit remarkable plasticity, transitioning between pro-inflammatory (M1) and anti-inflammatory, regenerative (M2) phenotypes. Beyond their immune functions, microglia contribute to activity-dependent synaptic pruning, a process crucial for circuit refinement during learning and recovery [13]. Dysregulation of this pruning function is implicated in neurodegenerative diseases; for instance, excessive synaptic elimination by microglia can contribute to memory loss in Alzheimer's disease pathology [13].
Recent single-cell transcriptomic analyses have revealed significant heterogeneity within microglial populations, with distinct subtypes emerging in different pathological contexts [11]. This functional diversity presents both a challenge and an opportunity for therapeutic intervention, as selectively modulating specific microglial subpopulations could promote beneficial phagocytic activity while curbing detrimental inflammatory responses.
Neural Stem Cells: Engines of Regeneration and Paracrine Signaling
Neural stem cells (NSCs), residing in niches such as the subventricular zone (SVZ) and subgranular zone (SGZ) of the hippocampus, hold immense therapeutic potential due to their ability to differentiate into neurons, astrocytes, and oligodendrocytes [14]. The regenerative capacity of endogenous NSCs is often insufficient for complete functional restoration, particularly in the inhibitory microenvironment of the injured and aging brain [14]. Consequently, therapeutic strategies have evolved to include NSC transplantation. A 2025 study demonstrated that transplanted human induced pluripotent stem cell-derived neural progenitor cells (hiPSC-NPCs) survived for over five weeks in stroke-injured mouse brains, primarily differentiating into GABAergic and glutamatergic neurons and promoting functional recovery [15].
The mechanism of action for NSC therapies is increasingly attributed to potent paracrine effects rather than direct cell replacement alone. NSCs secrete extracellular vesicles (EVs) containing bioactive molecules—including miRNAs, proteins, and lipids—that modulate neuroinflammation, promote neurogenesis, and restore cellular bioenergetics [14]. These EVs represent a promising cell-free therapeutic modality, circumventing challenges associated with direct cell transplantation, such as tumorigenesis and immune rejection.
Experimental Protocol: Assessing NSC Graft-Host Integration
The following methodology outlines the key procedures for evaluating the survival, integration, and therapeutic efficacy of transplanted NSCs, as utilized in recent groundbreaking research [15].
- 1. Cell Preparation: Differentiate human iPSCs into neural progenitor cells (NPCs) under xeno-free, GMP-compliant conditions. Characterize NPCs via immunocytochemistry for canonical markers (Nestin, Pax6) and confirm the absence of pluripotency markers (Nanog).
- 2. Animal Model & Surgery: Subject mice to photothrombotic stroke induction in the sensorimotor cortex. Confirm stroke success by Laser-Doppler Imaging (LDI), expecting a 60-70% reduction in cerebral blood flow.
- 3. Cell Transplantation: At 7 days post-injury (dpi), stereotactically inject NPCs expressing a dual-reporter (rFluc-eGFP) into the peri-infarct region. Control groups receive a vehicle injection.
- 4. Graft Monitoring: Track cell survival longitudinally over 35 days using in vivo bioluminescence imaging. Quantify signal intensity to monitor graft viability and expansion.
- 5. Histological Analysis: At endpoint (e.g., 43 dpi), perform immunohistochemistry on brain sections using antibodies against Human Nuclei (HuNu) to demarcate graft location and size. Additional staining for neuronal (βIII-Tubulin) and astrocytic (S100β, GFAP) markers assesses differentiation.
- 6. Functional Assessment: Evaluate motor recovery using deep learning-based gait analysis and fine-motor tests. Compare performance between NPC-treated and vehicle-treated groups over time.
- 7. Molecular Profiling: Conduct single-nucleus RNA sequencing (snRNA-seq) on grafted cells and surrounding host tissue to characterize neuronal subtypes formed and analyze graft-host crosstalk signaling pathways.
Diagram 1: Experimental workflow for evaluating neural stem cell therapy in a stroke model.
Oligodendrocytes: Restoring Conduction and Metabolic Support
Oligodendrocytes (OLs) are the myelinating cells of the CNS, essential for saltatory conduction and axonal integrity. A single oligodendrocyte can myelinate up to 50 axonal segments, significantly enhancing the speed and efficiency of action potential propagation [12]. Following demyelinating injuries or diseases such as multiple sclerosis (MS), OLs facilitate repair through remyelination, a process driven by the differentiation of oligodendrocyte precursor cells (OPCs) resident in the adult CNS [12].
Beyond insulation, OLs provide critical metabolic support to axons. They uptake glucose via monocarboxylate transporter 1 (MCT1) and convert it to lactate, which is shuttled to axons to meet their high energy demands [12]. Disruption of this metabolic coupling, as evidenced by MCT1 knockout models, leads to axonal degeneration and motor deficits, underscoring its necessity for long-term axonal survival [12]. Furthermore, OLs contribute to neural plasticity; learning and motor skill acquisition stimulate OPC differentiation and adaptive changes in myelin, a process termed "myelin plasticity" [12] [13].
Table 2: Oligodendrocyte Lineage Functions in Homeostasis and Repair
| Cell Type | Primary Function | Key Markers | Role in Repair |
|---|---|---|---|
| Oligodendrocyte Precursor Cell (OPC) | Proliferation, migration, surveillance | NG2, PDGFRα [11] | Recruited to site of injury, source of new OLs |
| Mature Oligodendrocyte | Myelination, metabolic support | MBP, PLP, MCT1 [12] | Forms new myelin sheaths (remyelination), supports axonal health |
| Myelin Sheath | Axonal insulation, saltatory conduction | Lipids (70%), MBP, PLP [12] | Restores conduction velocity, protects axon |
Signaling Pathways Mediating Cellular Crosstalk in Repair
The functional recovery of the nervous system is not the result of isolated cellular actions but is driven by intricate molecular crosstalk between grafted NSCs, endogenous glia, and host neurons. snRNA-seq data from a 2025 transplantation study revealed that graft-derived GABAergic neurons engage with host tissue through several key signaling pathways: Neurexin (NRXN), Neuregulin (NRG), Neural Cell Adhesion Molecule (NCAM), and SLIT pathways [15]. These interactions are hypothesized to underpin observed therapeutic effects, such as reduced inflammation, enhanced angiogenesis, and structural repair.
Concurrently, astrocytic signaling involving channels like Transient Receptor Potential Vanilloid 4 (TRPV4) and Aquaporin-4 (AQP4) plays a critical role in cellular volume regulation, influencing the onset and severity of cerebral edema during ischemic events [11]. Research using knockout models has demonstrated that the deletion of these channels alters the expression of glutamate receptors and other ion channels, impacting the brain's response to injury beyond direct volume control [11].
Diagram 2: Molecular graft-host crosstalk via key signaling pathways driving neural repair.
The Scientist's Toolkit: Essential Reagents and Models
Table 3: Research Reagent Solutions for Neural Repair Studies
| Reagent / Model | Category | Specific Example / Target | Research Application |
|---|---|---|---|
| hiPSC-derived NPCs | Cell Source | Xeno-free, GMP-compliant differentiation [15] | Cell therapy, graft-host interaction studies |
| Reporter Constructs | Tracking | rFluc-eGFP dual reporter [15] | Longitudinal monitoring of graft survival and migration |
| snRNA-seq | Profiling | 10x Genomics Platform | Unbiased characterization of graft/host cell types and pathways |
| Photothrombotic Stroke Model | Animal Model | Focal ischemia in sensorimotor cortex [15] | Preclinical testing of repair therapies |
| Optogenetics | Modulation | Channelrhodopsin (Opsins) in glia [11] | Precise control of glial cell activity to study function |
| Senolytic Compounds | Therapeutics | Senescence-targeting drugs [11] | Clear senescent cells to improve cognition post-injury |
| Clemastine | Remyelination Drug | M1 muscarinic receptor antagonist [13] | Promote OPC differentiation and remyelination |
| Anti-GFAP / Iba1 / HuNu | Antibodies | Cell-specific markers [11] [15] | Histological identification of astrocytes, microglia, and human grafts |
The intricate interplay between glial cells, neural stem cells, and oligodendrocytes forms the bedrock of the CNS's reparative response, directly influencing the neuroplasticity that underlies behavioral adaptation and functional recovery. Astrocytes and microglia perform complex, dual roles that can either support or hinder repair, while oligodendrocytes extend their function beyond mere insulation to include vital metabolic and plastic support. The emergence of NSC-derived therapies, particularly those leveraging paracrine effects via extracellular vesicles, represents a paradigm shift in regenerative strategies.
Future research must prioritize resolving the contextual signals that determine whether glial responses are beneficial or detrimental. Advancing the clinical translation of these cellular players will require refinements in targeted delivery, such as optimized nanoparticles for glial modulation [11], and safety-enhanced cell grafts. By deepening our understanding of these key cellular players and their complex interactions, we can pioneer novel, effective treatments that harness the brain's innate plastic potential to restore function after neurological injury and disease.
Neuroplasticity, the brain's remarkable capacity to change its structure and function in response to experience, represents a fundamental property of the nervous system that enables adaptation, learning, and memory formation [16]. This dynamic process operates along a spectrum of functional outcomes, yielding either beneficial adaptive plasticity or detrimental maladaptive plasticity with significant implications for behavioral outcomes. Adaptive plasticity refers to neural changes that enhance an organism's fit to its environment, improving function and supporting recovery after injury [17] [18]. In contrast, maladaptive plasticity describes neural reorganization that disrupts function, potentially leading to pathological states and behavioral impairments [19] [20]. This dichotomy mirrors concepts in evolutionary biology, where phenotypic plasticity—the ability of a single genotype to produce different phenotypes in different environments—can be locally adaptive, maladaptive, or neutral [21]. Understanding the mechanisms that determine whether plastic changes yield adaptive or maladaptive outcomes is crucial for developing targeted interventions for neurological and psychiatric disorders.
The distinction between these plasticity outcomes extends beyond simple beneficial versus harmful changes. As demonstrated in evolutionary biology, the adaptive value of plasticity depends critically on the nature of the trait being measured and its relationship to fitness [21]. Similarly, in neuroscience, the same plastic mechanism may produce adaptive outcomes in one context and maladaptive consequences in another, depending on environmental factors, timing, and neural circuitry involved. This whitepaper examines the mechanisms, manifestations, and experimental approaches for distinguishing these two faces of neuroplasticity, with particular emphasis on implications for drug development and therapeutic interventions.
Fundamental Mechanisms: Structural and Functional Bases
Forms of Neuroplasticity
Neuroplasticity encompasses multiple mechanisms operating at different spatial and temporal scales. Structural neuroplasticity refers to physical changes in neural circuits, including the growth of new dendritic spines, axonal sprouting, synaptic formation, and even neurogenesis—the generation of new functional neurons primarily in the subventricular zone and hippocampal dentate gyrus [16]. These structural changes provide the physical foundation for long-term neural reorganization. In contrast, functional neuroplasticity involves changes in the strength, efficiency, and synchrony of synaptic connections without immediate structural alterations [16]. This includes mechanisms such as long-term potentiation (LTP), which strengthens synaptic connections through repeated stimulation, and long-term depression (LTD), which weakens less-used connections [16]. Both forms work in concert to enable the brain's dynamic adaptation to experience, injury, and environmental demands.
The process of adaptive plasticity follows a characteristic sequence of events. Initially, the brain undergoes chemical changes, increasing or decreasing neurotransmitter release to facilitate short-term learning [17]. With sustained activity, these chemical changes lead to structural modifications as new connections form between neurons that weren't previously linked [17]. Finally, functional changes occur as entire networks of brain activity reorganize, making the learned action more efficient and automatic [17]. This progression from chemical to structural to functional change exemplifies how repeated experience physically sculpts the brain's organization, as dramatically demonstrated by London taxi drivers who develop enlarged hippocampi—a brain region critical for spatial navigation—after memorizing the city's complex street layout [17].
Molecular Mediators of Plasticity
At the molecular level, neuroplasticity involves complex signaling pathways and molecular determinants. Delta-type ionotropic glutamate receptors (GluDs) play a crucial role in synaptic formation and signaling between neurons [22]. These proteins house charged particles that help bind neurotransmitters, facilitating interneuronal communication at synapses [22]. Mutations in GluD proteins are implicated in psychiatric conditions including anxiety and schizophrenia, with underactivity associated with schizophrenia and hyperactivity linked to cerebellar ataxia [22]. Other critical molecular players include brain-derived neurotrophic factor (BDNF), which supports neuronal survival and differentiation, and immediate early genes (IEGs) that act as rapid-response elements in synaptic plasticity [23]. The mammalian target of rapamycin (mTOR) pathway serves as a central regulator of protein synthesis-dependent plasticity, with increased phosphorylated mTOR in serotonergic spinally projecting neurons observed in neuropathic pain models [19].
Table 1: Key Molecular Determinants of Plasticity Outcomes
| Molecule/Pathway | Function in Plasticity | Associated Outcomes |
|---|---|---|
| GluD receptors | Synapse formation, neuronal signaling | Cerebellar ataxia (hyperactivity), schizophrenia (hypoactivity) |
| mTOR pathway | Protein synthesis, synaptic growth | Neuropathic pain (maladaptive), learning (adaptive) |
| BDNF/TrkB signaling | Neuronal survival, differentiation | Adaptive learning and memory |
| Immediate Early Genes (IEGs) | Rapid genomic response to stimulation | Required for classic psychedelic neuroplasticity |
| Matrix Metalloproteinases (MMPs) | Extracellular matrix remodeling | Neuropathic pain development |
Maladaptive Plasticity: Mechanisms and Pathological Consequences
Neuropathic Pain and Central Sensitization
Maladaptive plasticity manifests prominently in neuropathic pain conditions, where injury to the sensory nervous system triggers plastic changes that paradoxically amplify pain signaling rather than restoring normal function [19]. This condition affects 4-8% of the population and presents with allodynia (pain from normally non-painful stimuli), hyperalgesia (heightened pain response), and spontaneous pain [19]. The maladaptive changes occur along the entire sensory pathway, from peripheral nociceptors to central processing regions. In the peripheral nervous system, upregulation of transient receptor potential cation channel subfamily V member 1 (TRPV1) channels lowers activation thresholds, increasing sensitivity to thermal and chemical stimuli [19]. Central sensitization involves structural and functional changes in the spinal cord and brain, including microglial activation, increased expression of toll-like receptors (TLR2 and TLR4), and enhanced synaptic efficacy in pain-processing pathways [19].
The anterior cingulate cortex (ACC), a brain region involved in pain perception, exhibits maladaptive plasticity through upregulation of acetylcholinesterase (AChE) following nerve injury [19]. This change contributes to the affective component of chronic pain. Similarly, the descending pain modulatory system in the rostral ventromedial medulla (RVM) shows increased phosphorylation of mTOR in serotonergic neurons after spared nerve injury, enhancing excitatory synaptic transmission and intrinsic neuronal excitability that maintains pain states [19]. Administration of rapamycin, an mTOR inhibitor, reverses these changes and produces analgesic effects, highlighting the potential for targeting maladaptive plasticity therapeutically [19].
Phantom Limb Phenomena and Cortical Reorganization
Another striking example of maladaptive plasticity occurs in phantom limb pain, where amputation leads to persistent perceptions of the missing limb, often accompanied by painful sensations [20]. This phenomenon results from extensive cortical reorganization in the primary somatosensory cortex, wherein areas that previously received input from the amputated limb become responsive to stimulation from adjacent body regions [20]. The degree of cortical reorganization correlates with the intensity of phantom pain, demonstrating a direct relationship between maladaptive neural rewiring and pathological perception. Functional neuroimaging studies reveal that the cortical representation of the face (immediately adjacent to the hand representation in the somatosensory homunculus) expands into the territory previously occupied by the amputated hand, such that touching the face is perceived as sensation in the missing hand [20].
Maladaptive plasticity also underlies tinnitus, where hearing loss triggers compensatory changes in central auditory pathways that generate phantom auditory perceptions [20]. Similarly, in dystonia, repetitive movements lead to abnormal sensorimotor integration and loss of inhibitory control, resulting in sustained muscle contractions and abnormal postures [20]. These examples share a common theme: initial injury or altered input triggers plastic mechanisms that normally support adaptation, but in these cases, the reorganization produces pathological outcomes that impair rather than improve function.
Adaptive Plasticity: Mechanisms and Beneficial Outcomes
Learning, Memory, and Skill Acquisition
Adaptive plasticity serves as the neural foundation for learning and memory across the lifespan [16]. The process follows a well-defined sequence beginning with chemical changes that support short-term memory, progressing to structural changes that establish new neural connections, and culminating in functional changes that make the learned skill automatic and efficient [17]. Myelination—the addition of protective sheathing around nerve fibers—plays a crucial role in this process by increasing the speed and efficiency of neural signaling [17]. With repeated practice, myelin accumulates around frequently used circuits, making skilled performance increasingly automatic. This process explains why London taxi drivers develop enlarged hippocampi and why blind individuals reading Braille show expansion in tactile processing regions [17].
The developmental period represents a time of exceptionally high adaptive plasticity, characterized by rapid synaptogenesis followed by experience-dependent pruning that refines neural circuits [16]. During critical periods, environmental input powerfully shapes neural organization, allowing children to acquire language and other skills with remarkable efficiency [16]. Though plasticity decreases with age, the adult brain retains significant capacity for adaptive change, as demonstrated by recovery from brain injury where undamaged regions can take over functions from affected areas [18]. Engaging in targeted therapy and rehabilitation can enhance this adaptive plasticity, promoting better functional outcomes [18].
Cross-Modal Reorganization and Compensation
Adaptive plasticity enables remarkable cross-modal reorganization in sensory systems, where loss of one modality triggers compensatory enhancement in remaining senses [20]. Blind individuals demonstrate expansion of visual cortical areas that become responsive to auditory and tactile stimuli, leading to genuine perceptual enhancements in hearing acuity and tactile discrimination [20]. These changes support improved Braille reading and auditory localization abilities. Similarly, deaf individuals show enhanced peripheral visual processing and motion detection in visual cortex, adapting to rely more heavily on visual information for communication and spatial awareness [20]. These cross-modal changes reflect the brain's inherent capacity to reallocate computational resources based on environmental demands and available inputs.
The potential for adaptive plasticity is influenced by multiple factors including age, overall health, genetic background, and environmental enrichment [16]. Physical activity, cognitive engagement, and environmental complexity have been shown to enhance neurogenesis and synaptic plasticity, particularly in the hippocampus where new neurons contribute to learning and memory processes [16]. Non-pharmacological lifestyle interventions leveraging these principles can promote adaptive plasticity and maintain cognitive function throughout the lifespan, potentially counteracting age-related neurodegenerative processes [16].
Experimental Approaches and Methodologies
Assessing Plasticity in Model Systems
Research into neuroplasticity employs diverse methodological approaches across multiple model systems. Reciprocal transplant experiments, borrowed from evolutionary biology, provide powerful insights into adaptive potential by transplanting individuals between different environments and measuring resulting trait changes [21]. However, interpreting these experiments requires careful consideration of whether measured traits are locally adaptive or simply correlated with fitness, as fitness-correlated traits may show flat reaction norms despite significant adaptive plasticity in unobserved traits [21]. In marine isopod studies, for instance, reciprocal transplantation between high- and low-salinity environments revealed that flat reaction norms for survival and growth likely reflected phenotypic buffering rather than absence of plasticity, demonstrating the importance of measuring multiple traits with known relationships to fitness [21].
Table 2: Experimental Approaches for Studying Neuroplasticity
| Methodology | Application | Key Insights |
|---|---|---|
| Reciprocal transplant designs | Assessing genotype-environment interactions | Distinguishing adaptive from neutral plasticity |
| Cryo-electron microscopy | Structural analysis of synaptic proteins | Revealing GluD receptor activation mechanisms |
| Genetic and pharmacological tools | Manipulating specific plasticity pathways | Establishing causal roles (e.g., mTOR in pain) |
| Reaction norm analysis | Quantifying phenotypic responses | Differentiating types of plasticity outcomes |
| Functional neuroimaging | Mapping cortical reorganization | Correlating neural changes with behavior |
In laboratory settings, in silico simulations of evolution demonstrate how adaptive plasticity can emerge even when selected against in individual environments [24]. These models incorporate linear reaction norms to simulate how populations evolve plastic responses to temporal environmental heterogeneity [24]. The simulations reveal that limited genetic change per environment (low "learning rate") actually promotes the evolution of adaptive plasticity by preventing populations from completely adapting to each current environment before the next environmental shift [24]. This explains how adaptive plasticity can evolve without lineage selection or individual-level selection for plasticity, occurring instead as a by-product of inefficient short-term natural selection [24].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Plasticity Studies
| Reagent/Tool | Function/Application | Example Use |
|---|---|---|
| Tabernanthalog (TBG) | Nonhallucinogenic psychoplastogen | Promoting neuroplasticity without IEG activation |
| Bromodeoxyuridine (BrdU) | Thymidine analog for birth-dating cells | Identifying newly generated neurons |
| Rapamycin | mTOR pathway inhibitor | Reversing maladaptive plasticity in pain models |
| TRPV1 modulators | Targeting peripheral sensitization | Investigating neuropathic pain mechanisms |
| Genetic tools (Cre-Lox, RNAi) | Cell-specific manipulation | Dissecting circuit-specific plasticity mechanisms |
| Cryo-EM technologies | High-resolution structural biology | Characterizing synaptic protein structures |
Advanced genetic and pharmacological tools enable precise manipulation of plasticity mechanisms. For example, tabernanthalog (TBG), a nonhallucinogenic psychoplastogen, promotes cortical neuroplasticity through 5-HT2A, TrkB, mTOR, and AMPA receptor activation but without inducing immediate early gene activation or the glutamate burst associated with classic psychedelics [23]. This dissociation of neuroplastic effects from hallucinogenic properties highlights the potential for developing safer plasticity-promoting therapeutics. Similarly, region-specific manipulation of mTOR signaling using rapamycin or genetic approaches has demonstrated the pathway's critical role in maladaptive plasticity underlying neuropathic pain [19]. Toll-like receptor (TLR) antagonists and matrix metalloproteinase (MMP) inhibitors provide additional tools for targeting specific aspects of maladaptive plasticity in neurological disorders.
Signaling Pathways and Neural Circuits
The molecular pathways governing neuroplasticity outcomes involve sophisticated signaling networks that integrate environmental information with neural responses. The following diagram illustrates key pathways differentiating adaptive and maladaptive plasticity:
Diagram 1: Signaling pathways differentiating adaptive and maladaptive plasticity. Note the overlapping molecular players (GluD receptors, psychoplastogens) that can influence both pathways, with outcomes determined by regulation and context.
The experimental workflow for investigating these pathways combines multiple approaches, as illustrated below:
Diagram 2: Integrated experimental workflow for investigating plasticity mechanisms, combining molecular, structural, functional, and behavioral approaches.
Therapeutic Implications and Future Directions
Targeting Plasticity in Drug Development
Understanding the duality of plasticity opens promising avenues for therapeutic intervention. Psychoplastogens—compounds that promote rapid neuroplasticity—represent an emerging class of therapeutics with potential for treating psychiatric and neurological disorders [23]. Tabernanthalog (TBG), a nonhallucinogenic psychoplastogen, promotes cortical neuroplasticity through 5-HT2A, TrkB, mTOR, and AMPA receptor activation but without inducing immediate early gene activation or the glutamate burst associated with classic psychedelics [23]. This dissociation of neuroplastic effects from hallucinogenic properties enables development of potentially safer, more scalable alternatives to psychedelics for conditions including depression, addiction, and possibly neurodegenerative disorders.
Drugs targeting GluD receptors offer another promising direction, as these proteins directly regulate synapse function and are implicated in schizophrenia, anxiety, and cerebellar ataxia [22]. In schizophrenia, where GluDs are underactive, drugs that enhance GluD activity might restore synaptic function, while in cerebellar ataxia, where GluDs become hyperactive, blockers could normalize signaling [22]. Similarly, targeting mTOR signaling with rapamycin analogs shows potential for normalizing maladaptive plasticity in neuropathic pain [19]. The key therapeutic challenge lies in developing interventions that selectively enhance adaptive plasticity while suppressing maladaptive changes, requiring exquisite temporal and spatial precision.
Timing, Context, and Individual Factors
Therapeutic harnessing of neuroplasticity must account for critical periods and individual differences in plasticity capacity. During development, heightened plasticity enables rapid learning but also creates vulnerability to adverse experiences that can produce maladaptive outcomes [16]. In adulthood, plasticity becomes more constrained but remains modifiable through targeted interventions. Factors including age, genetics, environmental context, and neurological history all influence an individual's plastic potential [18]. Successful interventions will likely require personalized approaches that consider these variables while strategically timing interventions to coincide with periods of heightened plasticity.
Future research directions should focus on identifying biomarkers of plasticity outcomes to predict individual responses to plasticity-targeting interventions. Developing circuit-specific modulators will enable more precise targeting of pathological plasticity while sparing adaptive processes. Combining pharmacological and experiential approaches may yield synergistic benefits, as drugs that enhance plasticity potential could increase the effectiveness of behavioral therapies and rehabilitation. Finally, exploring how principles of evolutionary biology inform neuroplasticity may reveal novel therapeutic strategies for steering plastic changes toward adaptive outcomes [24] [20].
Neuroplasticity embodies a fundamental double-edged sword in neural function and behavioral outcomes. The same mechanisms that enable learning, memory, and recovery from injury can, when dysregulated, produce pathological states including chronic pain, tinnitus, and movement disorders. Distinguishing adaptive from maladaptive plasticity requires integrated analysis across molecular, structural, functional, and behavioral levels, with careful consideration of environmental context and individual differences. Current research is unraveling the complex signaling pathways and circuit mechanisms that determine plasticity outcomes, paving the way for innovative therapeutics that can selectively enhance adaptive plasticity while suppressing maladaptive consequences. As our understanding of these processes deepens, we move closer to precisely harnessing the brain's remarkable plastic capacity to treat neurological and psychiatric disorders, ultimately improving behavioral outcomes and quality of life for affected individuals.
The traditional view of the brain as a static organ with fixed circuitry has been fundamentally overturned. Research now reveals a highly dynamic system capable of large-scale reorganization throughout life, a process central to behavioral adaptation and optimal performance. Large-scale neural network reorganization refers to the brain's capacity to reconfigure its functional and structural connectivity in response to experience, learning, or injury. This whitepaper synthesizes cutting-edge research on the mechanisms, measurement, and functional implications of these reorganizational processes, providing a scientific framework for researchers and drug development professionals exploring the neural basis of adaptive behavior.
Underpinning this capacity for reorganization is neuroplasticity—the brain's biological ability to change its structure and function. Once believed limited to early development, neuroplasticity operates across multiple scales, from molecular and synaptic changes to system-level network reconfiguration [25]. This dynamic architecture enables the brain to maintain stability while retaining the flexibility necessary for learning new skills, recovering from injury, and adapting to changing environments—foundational requirements for optimal behavioral performance [26].
Mechanisms of Large-Scale Reorganization
The brain employs distinct biological mechanisms to achieve reorganization across different spatial and temporal scales. Understanding these processes provides critical insights for developing interventions aimed at modulating neural plasticity.
Synaptic and Structural Plasticity
At the most fundamental level, synaptic plasticity enables experience-dependent strengthening or weakening of connections between neurons. Long-term potentiation (LTP), a persistently strengthened synaptic connection based on recent activity patterns, remains the most studied cellular model for learning and memory [25]. LTP exhibits several critical properties:
- State-dependence: Requires simultaneous activation of sending and receiving neurons within approximately 100 milliseconds
- Input specificity: Strengthening of one synapse does not affect other inactive synapses on the same neuron
- Associativity: Strong activation of nearby pathways can help weak stimulation trigger LTP [25]
Recent research has revealed that spontaneous and experience-driven (evoked) synaptic transmissions originate from distinct synaptic sites with separate developmental timelines and regulatory rules, enabling the brain to maintain stable background activity while refining behaviorally relevant pathways [26].
Beyond synaptic strength changes, structural plasticity involves physical remodeling of neuronal connections. Studies using two-photon microscopy reveal that dendritic spines—tiny protrusions that receive synaptic inputs—can form or disappear at rates of 5-10% weekly during normal experience, increasing dramatically during intense learning or after injury [25]. After retinal lesions, up to 90% of spines in the affected visual cortex area may reorganize during recovery.
System-Level Reorganization
Large-scale reorganization extends beyond local circuits to encompass entire brain systems. Following spinal cord injuries in non-human primates, the deafferented hand region of the primary somatosensory cortex (area 3b) undergoes remarkable reorganization, with face inputs expanding into the hand territory over distances of 7-14 mm [27]. Crucially, this cortical reorganization reflects changes at the brainstem level, as selective inactivation of the reorganized cuneate nucleus eliminates observed face expansion in area 3b [27].
Table 1: Mechanisms of Large-Scale Neural Reorganization
| Mechanism | Spatial Scale | Temporal Scale | Functional Role |
|---|---|---|---|
| Synaptic Plasticity (LTP/LTD) | Microns (individual synapses) | Milliseconds to hours | Learning and memory formation |
| Structural Remodeling (dendritic spines) | Microns to millimeters | Days to weeks | Circuit refinement and experience-dependent adaptation |
| Neurogenesis | Local circuits | Weeks to months | Learning capacity and pattern separation |
| Cortical Reorganization | Millimeters to centimeters | Weeks to years | Functional recovery after injury and skill acquisition |
| Network Topological Reconfiguration | Whole-brain systems | Seconds to minutes | Adaptive information processing for changing task demands |
Behavioral Timescale Synaptic Plasticity (BTSP)
Recent research has identified Behavioral Timescale Synaptic Plasticity (BTSP) as a distinctive mechanism enabling rapid, one-shot learning. Unlike traditional spike-timing-dependent plasticity, BTSP:
- Does not depend on firing of the postsynaptic neuron
- Is gated by stochastic synaptic input from the entorhinal cortex
- Is effective after single or few trials (one-shot learning)
- Depends on preceding synaptic weight values
- Operates on time scales of seconds, suitable for episodic memory formation [28]
This mechanism creates content-addressable memory with binary synapses, enabling efficient memory storage and recall while reproducing the repulsion effect observed in human memory, where traces for similar items are actively separated to enable differential processing [28].
Experimental Paradigms and Measurement Approaches
Tracking Reorganization with Brain-Computer Interfaces
Brain-computer interface (BCI) paradigms provide exceptional experimental leverage for studying neural reorganization by establishing explicit, controlled mappings between neural activity and behavior. In landmark non-human primate studies, researchers tracked reorganization throughout motor skill learning spanning several weeks [29].
Table 2: Distinct Timescales of Neural Reorganization in Motor Learning
| Learning Phase | Behavioral Improvement | Neural Reorganization Process | Timescale |
|---|---|---|---|
| Fast Learning | Reduction of directional errors | Global reorganization of neural recruitment common to all neurons | Minutes to hours (hundreds of trials) |
| Slow Learning | Increased movement efficiency | Local changes in individual neuron tuning properties | Weeks (tens of thousands of trials) |
Experimental Protocol: Monkeys performed a center-out cursor task using a BCI that linearly mapped firing rates of primary motor cortex neurons to cursor velocity. Researchers implemented a perturbation by rotating the "pushing directions" of neuron subsets, then tracked how neural tuning properties changed throughout learning. Decoding parameters were estimated through calibration sessions using a coadaptive procedure, with spikes binned into 33-ms intervals, converted to firing rates, normalized, and smoothed with a boxcar filter over previous five time bins [29].
Network Topology Analysis in Sensory Cortex
Research investigating how primary visual cortex (V1) reorganizes during multimodal stimulation demonstrates how sensory systems reconfigure their functional connectivity based on processing demands. Using in vivo two-photon calcium imaging in awake mice, scientists recorded population activity in V1 during unimodal visual and bimodal visuotactile stimulation [30].
Experimental Protocol:
- Animal Preparation: Adult C57BL/6J mice (6-8 weeks) received AAV9-hSyn-GCaMP6f viral vector injections into V1 for calcium indicator expression
- Imaging: Two-photon microscopy recorded hundreds of neurons simultaneously in awake mice during stimulation
- Stimulation Paradigm: Unimodal (visual gratings) and bimodal (visual gratings + whisker deflection) stimuli
- Network Construction: Functional connectivity networks built from fluorescence time series
- Quantitative Analysis: Graph-theoretical metrics computed including betweenness centrality, closeness centrality, degree centrality, global efficiency, and modularity [30]
Findings revealed that unimodal visual processing relies on hub-centric, modular architectures, while cross-modal input promotes globally integrated, distributed networks with higher connectivity efficiency. This topological reconfiguration represents an adaptive mechanism for balancing local specialization with global integration based on sensory context [30].
Causal Intervention Approaches
Establishing causal relationships in neural reorganization requires direct intervention methods. Research on somatosensory reorganization after spinal cord injury employed selective neural inactivation to identify critical sites of plasticity [27].
Experimental Protocol:
- Animal Model: Macaque monkeys with unilateral dorsal column lesions at cervical levels (C4/C5)
- Chronic Preparation: Cortical and brainstem mapping 14-36 months post-lesion
- Neural Inactivation:
- Cortical Test: Lidocaine (4%) infusion into normal chin representation of area 3b
- Brainstem Test: Lidocaine injection into reorganized cuneate nucleus at multiple sites (2-4μl per site at 4μl/min)
- Simultaneous Recording: Multiunit activity recorded in both area 3b and brainstem nuclei during tactile stimulation (1Hz, 10ms skin contact) [27]
Results demonstrated that inactivation of the reorganized cuneate nucleus—but not the original cortical face representation—eliminated expanded chin responses in deafferented cortex, establishing brainstem plasticity as the substrate for large-scale cortical reorganization [27].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Neural Reorganization Studies
| Reagent/Technology | Function | Example Application |
|---|---|---|
| AAV9-hSyn-GCaMP6f | Genetically-encoded calcium indicator for neuronal activity visualization | Monitoring population activity in mouse primary visual cortex during multimodal stimulation [30] |
| Tungsten Microelectrodes | Extracellular recording of single or multiunit activity | Mapping somatotopic organization in primate somatosensory cortex and brainstem nuclei [27] |
| Lidocaine HCl (4%) | Sodium channel blocker for reversible neural inactivation | Causal testing of plasticity sites in cortical and brainstem structures [27] |
| Two-Photon Microscopy | High-resolution imaging of neuronal population activity | Recording hundreds of neurons simultaneously in awake, behaving mice [30] |
| Utah Multielectrode Arrays | Chronic recording from neuronal populations | Tracking motor cortex reorganization during long-term BCI learning [29] |
| Chubbuck Vibratory Stimulator | Precise tactile stimulation with controlled parameters | Mapping receptive fields in somatosensory pathways [27] |
Theoretical Frameworks: Prospective Configuration
The prospective configuration model offers a fundamentally different principle for understanding how the brain solves credit assignment problems during learning. Unlike backpropagation—which modifies weights first, leading to subsequent changes in neural activity—prospective configuration first infers the pattern of neural activity that should result from learning, then modifies synaptic weights to consolidate this change [31].
This mechanism naturally emerges from energy-based networks (including Hopfield networks and predictive coding networks), where neural activity and weights represent movable parts in a dynamical system that minimizes an energy function. The model reproduces surprising patterns of neural activity and behavior observed in diverse learning experiments while enabling more efficient learning in contexts faced by biological organisms, including continual learning and rapidly changing environments [31].
Implications for Therapeutic Development
Understanding large-scale neural reorganization provides crucial insights for developing interventions targeting neurological and psychiatric conditions. Abnormalities in synaptic signaling and plasticity mechanisms have been implicated in autism, Alzheimer's disease, and substance use disorders [26]. The separation of spontaneous and evoked transmission sites reveals potential therapeutic targets for modulating specific aspects of neural signaling without disrupting overall system function.
The BRAIN Initiative has identified advancing human neuroscience and developing innovative technologies to understand and treat brain disorders as key priorities [32]. Research consenting humans undergoing diagnostic brain monitoring or receiving neurotechnology for clinical applications provides extraordinary opportunities to understand human-specific reorganization mechanisms and test novel interventions [32].
Future directions include leveraging knowledge of large-scale reorganization to develop:
- Targeted neuromodulation approaches that guide adaptive plasticity while minimizing maladaptive reorganization
- Pharmacological agents that enhance beneficial plasticity mechanisms at specific organizational levels
- Rehabilitation protocols that optimally engage endogenous plasticity mechanisms through carefully timed intervention schedules
- Brain-computer interfaces that harness reorganization capacity to restore function after neurological injury
The dynamic, multi-scale nature of neural reorganization presents both challenges and opportunities for therapeutic development, requiring approaches that consider interactions across molecular, cellular, circuit, and system levels.
Harnessing Neuroplasticity: Research Methods and Therapeutic Applications
Neuroplasticity, the nervous system's capacity to reorganize itself in response to experience and injury, serves as the fundamental biological substrate for behavioral adaptation and optimal performance [3] [33]. This dynamic process spans multiple spatial and temporal scales, from molecular and synaptic changes to large-scale network reorganization [32] [34]. Understanding these mechanisms is crucial for developing interventions to enhance cognitive function, promote resilience, and facilitate recovery from neurological disorders. The assessment of neuroplastic change requires sophisticated technologies that can capture the brain's structural and functional dynamics non-invasively in humans. Functional magnetic resonance imaging (fMRI), electroencephalography (EEG), magnetoencephalography (MEG), and associated biomarkers now provide unprecedented windows into these processes, enabling researchers to quantify how neural circuits adapt throughout the lifespan [32] [33] [35].
Within the context of behavioral adaptation and optimal performance research, tracking neuroplastic changes is essential for understanding how individuals acquire skills, adapt to challenging environments, and maintain cognitive function. The BRAIN Initiative has identified the analysis of circuits of interacting neurons as particularly rich in opportunity, with potential for revolutionary advances in understanding how dynamic patterns of neural activity are transformed into cognition, emotion, perception, and action [32]. Continuous and real-time neural modifications in concert with dynamic environmental contexts provide opportunities for targeted interventions for maintaining healthy brain functions throughout the lifespan [3]. This technical guide provides a comprehensive overview of advanced assessment techniques for tracking these plastic changes, with specific emphasis on their application to optimal performance research.
fMRI Methodologies for Tracking Plastic Change
Fundamental Principles and Applications
Functional MRI measures brain activity by detecting changes in blood oxygenation and flow, providing an indirect marker of neural activity with high spatial resolution. This technique enables researchers to map neural circuits and observe how they reorganize in response to experience, training, or intervention [32] [36]. For plasticity research, fMRI can capture both rapid and long-term changes in brain function, including alterations in network connectivity, expansion or contraction of cortical representations, and shifts in activation patterns associated with skill acquisition [32].
The value of fMRI in neuroplasticity research lies in its ability to generate circuit diagrams that vary in resolution from synapses to the whole brain, enabling an understanding of the relationship between neuronal structure and function [32]. Advanced fMRI techniques now allow researchers to produce a dynamic picture of the functioning brain through large-scale monitoring of neural activity, capturing how circuits interact at the speed of thought [32]. When integrated with other modalities, fMRI provides a comprehensive view of how experience shapes brain organization across multiple spatial and temporal scales.
Experimental Protocols for Plasticity Assessment
Task-Based fMRI Protocol for Skill Acquisition:
- Experimental Design: Implement block or event-related designs with appropriate baseline conditions. For motor skill acquisition, use sequential finger tapping tasks; for cognitive training, employ working memory or attentional tasks.
- Scanning Parameters: Acquire T1-weighted structural images (MPRAGE sequence, 1mm isotropic resolution) and T2*-weighted functional images (EPI sequence, 2-3mm isotropic resolution, TR=2000ms, TE=30ms).
- Longitudinal Assessment: Conduct scanning sessions at baseline, immediately after training initiation, and at regular intervals throughout the training period (e.g., 1 week, 4 weeks, 3 months).
- Data Analysis: Preprocess data (motion correction, normalization, smoothing), then perform statistical analysis (GLM) to identify training-related activation changes. Include connectivity analyses (psychophysiological interactions, seed-based correlation) to detect network reorganization.
Resting-State fMRI Protocol for Network Plasticity:
- Data Acquisition: Acquire 10 minutes of resting-state data (eyes open, fixating on crosshair) using standard fMRI parameters.
- Analysis Pipeline: Preprocess data including nuisance regression (motion, CSF, white matter signals). Perform independent components analysis (ICA) to identify networks, or seed-based correlation to examine specific network connectivity.
- Longitudinal Tracking: Compare functional connectivity metrics across timepoints to identify plasticity-induced network changes.
Table 1: fMRI Metrics for Tracking Neuroplastic Change
| Metric | Description | Plasticity Correlation | Optimal Performance Link |
|---|---|---|---|
| BOLD Signal Amplitude | Magnitude of activation during task performance | Decreases with automaticity; increases with challenge | Efficient neural processing |
| Network Connectivity | Strength of functional coupling between brain regions | Increases with integrated processing | Enhanced coordination of distributed systems |
| Regional Homogeneity | Temporal similarity of neighboring voxels | Increases with specialization | Refined local processing |
| Graph Theory Metrics | Topological properties of brain networks | Shift toward more efficient organization | Global efficiency, modularity |
EEG and MEG Approaches to Plasticity Assessment
Technical Foundations and Applications
EEG and MEG provide direct measures of neural electrical activity with exceptional temporal resolution, capturing neural dynamics at the millisecond scale essential for understanding the rapid temporal features of neuroplastic change [33] [35]. EEG measures electrical potentials at the scalp surface, while MEG detects the magnetic fields generated by neuronal currents, with each modality offering complementary advantages for plasticity research. These techniques are particularly valuable for tracking the temporal evolution of plastic changes, capturing how neural assemblies reconfigure their communication patterns in response to experience, training, or clinical intervention [33].
Recent advances in EEG analysis have established EEG entropy as a theoretically appealing and emerging candidate biomarker of neural complexity that reflects the flexible information processing underpinning adaptive self-regulation [35]. Converging research indicates that neural complexity, quantified by entropy measures, reflects the flexible information processing that underpins adaptive self-regulation, with diminished neural complexity observed in emotional dysregulation and anxiety, while interventions like mindfulness may work by restoring it [35]. This approach moves beyond static, resting-state analysis to capture the brain's flexible response to challenges, providing a powerful and ecologically valid marker of regulatory capacity essential for optimal performance [35].
Experimental Protocols for EEG/MEG Plasticity Assessment
EEG Protocol for Learning-Induced Plasticity:
- Experimental Setup: Apply 64-128 channel EEG cap according to 10-20 system, impedance <5 kΩ. For MEG, use whole-head system in magnetically shielded room.
- Task Paradigm: Implement oddball, working memory, or cognitive control tasks with sufficient trials (≥50 per condition) for reliable ERP components.
- Data Acquisition: Sample at 1000 Hz with appropriate filters (e.g., 0.1-100 Hz). Include event markers synchronized with stimulus presentation.
- Analysis Pipeline: Preprocess data (filtering, artifact removal, ICA for ocular correction). Extract ERPs (P300, N200, MMN) or compute time-frequency representations (ERD/ERS). Calculate entropy metrics (Sample Entropy, Multiscale Entropy) for specific frequency bands.
Resting-State EEG Protocol for Brain State Plasticity:
- Data Collection: Acquire 5 minutes eyes-open and 5 minutes eyes-closed resting-state data.
- Spectral Analysis: Compute power spectral density for standard frequency bands (delta, theta, alpha, beta, gamma).
- Complexity Measures: Calculate entropy values and functional connectivity metrics (phase locking value, weighted phase lag index) to assess network dynamics.
- Longitudinal Assessment: Track changes in these metrics across training or intervention periods.
Table 2: EEG/MEG Biomarkers of Neuroplasticity
| Biomarker | Description | Plasticity Manifestation | Performance Correlation |
|---|---|---|---|
| Event-Related Potentials | Time-locked electrical responses to stimuli | Altered amplitude/latency with learning | Processing efficiency, automaticity |
| Spectral Power | Oscillatory activity in frequency bands | Band-specific shifts with expertise | Cognitive state regulation |
| EEG Entropy | Complexity of neural signal dynamics | Increased with adaptive capacity | Emotional regulation, resilience [35] |
| Coherence/Connectivity | Synchronization between brain regions | Enhanced integration with training | Network efficiency, cognitive flexibility |
Multimodal Integration and Biomarker Validation
Integrated Methodologies for Comprehensive Assessment
The most powerful approaches to tracking plastic change involve integrating multiple neuroimaging modalities to capitalize on their complementary strengths [32] [36]. Simultaneous EEG-fMRI recording captures both the high temporal resolution of electrical activity and the high spatial resolution of hemodynamic changes, providing a more complete picture of brain dynamics during plastic reorganization [33]. MEG can be combined with structural connectivity data from diffusion tensor imaging to understand how white matter pathways constrain functional plasticity. These integrated approaches reflect the BRAIN Initiative's emphasis on combining technologies to discover how dynamic patterns of neural activity are transformed into cognition, emotion, perception, and action [32].
The integration of neuroimaging with behavioral measures is equally important for establishing the functional consequences of plastic changes. Measures of skill acquisition, cognitive performance, and emotional regulation provide critical validation for neural biomarkers of plasticity [3] [35]. Research on optimal performance indicates that strategic tactics, such as effective coping strategies, can mitigate runaway stress responses and preserve adaptive neural and cognitive performance, with individual variability in stress and resilience responses affected by many factors, including genetic, experiential and neurobiological influences [3].
Experimental Protocol for Multimodal Plasticity Assessment
Multimodal Protocol for Intervention Studies:
- Baseline Assessment: Collect structural MRI (T1, DTI), resting-state fMRI, task-based fMRI, high-density EEG, and comprehensive neuropsychological testing.
- Intervention Period: Implement targeted training (cognitive, motor, or mindfulness-based) with duration sufficient to induce plastic changes (typically 4-12 weeks).
- Intermediate Assessment: Conduct brief EEG sessions weekly to track temporal dynamics of plasticity.
- Post-Intervention Assessment: Repeat full multimodal assessment immediately after training completion.
- Follow-Up: Repeat assessment after a no-contact period (e.g., 3-6 months) to evaluate persistence.
Figure 1. Workflow for multimodal assessment of neuroplastic change, illustrating the integration of longitudinal measurements across temporal scales and imaging modalities.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Neuroplasticity Research
| Resource Category | Specific Tools/Techniques | Research Application | Performance Utility |
|---|---|---|---|
| Neuroimaging Analysis Packages | FSL, SPM, AFNI, FreeSurfer, BrainVoyager | Preprocessing, statistical analysis, visualization of fMRI data | Enables reproducible analysis pipelines [36] |
| EEG/MEG Analysis Tools | EEGLAB, FieldTrip, MNE-Python, Brainstorm | Signal processing, source localization, connectivity analysis | Quantifies neural dynamics and complexity [35] |
| Programming Environments | R, Python, MATLAB | Statistical analysis, custom algorithm development, figure generation | Facilitates reproducible visualizations and analyses [36] |
| Visualization Software | SurfIce, PyCortex, Connectome Workbench | 3D rendering of brain data, creation of publication-quality figures | Enables programmatic and reproducible visualization [36] |
| Experimental Presentation Platforms | Presentation, E-Prime, PsychToolbox | Precise stimulus delivery and response collection | Ensures experimental control and timing accuracy |
Data Visualization and Reproducibility in Plasticity Research
The visualization of neuroimaging data forms the centerpiece of the interpretation and communication of scientific results, and is a cornerstone for data quality control [36]. Code-based brain visualization tools allow researchers to generate reproducible, publication-ready figures directly within programming environments such as R, Python and MATLAB, providing significant advantages in replicability, flexibility, and integration over GUI-based tools [36]. This approach is particularly valuable in plasticity research, where subtle changes in brain organization must be reliably detected and communicated across longitudinal studies.
The adoption of programmatic visualization methods enables researchers to maintain precise control over visualization settings, such as color schemes, thresholds, and visual orientations, which streamlines the scientific workflow when generating multiple figures or modifying visualizations in response to reviewer requests [36]. This capacity for exact replication of figures via code has marked advantages beyond open science practices, particularly for tracking subtle neuroplastic changes across multiple timepoints and analysis approaches.
Figure 2. Reproducible workflow for neuroplasticity data visualization, highlighting the critical role of code-based approaches in ensuring transparent and replicable research outcomes.
Advanced assessment techniques using fMRI, EEG/MEG, and associated biomarkers provide powerful tools for tracking plastic changes in the human brain, offering unprecedented insights into the neural mechanisms underlying behavioral adaptation and optimal performance. The integration of these multimodal approaches, combined with rigorous experimental designs and reproducible analysis methods, enables researchers to capture the dynamic reorganization of neural circuits across multiple spatial and temporal scales. Future research will benefit from emerging technologies that provide even greater resolution and specificity, including advances in high-density EEG, ultra-high field MRI, and wearable neuroimaging systems that can capture brain plasticity in real-world environments [32] [35].
The continued development and validation of biomarkers for neuroplasticity will transform how we assess and enhance mental function, providing objective indicators of the brain's adaptive capacity [35]. This interdisciplinary approach, integrating methods from neuroscience, psychology, engineering, and computational science, promises to bridge the gap between subjective experience and objective physiology, ultimately advancing our understanding of how the brain adapts to support optimal performance throughout the lifespan [32] [3] [35]. As these technologies mature, they will enable more personalized interventions to enhance cognitive function, promote resilience, and facilitate recovery from neurological disorders, fulfilling the promise of neuroplasticity research to improve human potential and well-being.
The brain's capacity for functional and structural reorganization, known as neuroplasticity, forms the foundational premise for developing non-pharmacological interventions in cognitive health and psychiatric rehabilitation [37]. This capacity enables the nervous system to modify its organization in response to altered environmental demands, ranging from molecular changes at the synapse to large-scale cortical map reorganization [37]. Once considered a static organ, the brain is now recognized as highly malleable, continuously shaped by behavioral experiences throughout the lifespan [37]. Neuroplasticity manifests adaptively in processes like skill acquisition and memory formation, but can also occur maladaptively in conditions such as phantom limb pain, tinnitus, and addictive behaviors [37]. Understanding these dual aspects is crucial for developing targeted interventions.
This technical review examines three evidence-based approaches for inducing neuroplastic change: targeted learning, cognitive remediation, and physical activity. These behavioral and experiential inducers represent powerful tools for enhancing cognitive function, treating neurological and psychiatric conditions, and optimizing performance in healthy populations. We synthesize current scientific evidence, detail experimental methodologies, and identify molecular mechanisms through which these interventions exert their effects, providing researchers and drug development professionals with a comprehensive resource for integrating these approaches into therapeutic development pipelines.
Neuroplasticity: Mechanisms and Measurement
Molecular Foundations of Neural Adaptation
At the molecular level, neuroplasticity is mediated by neurotrophic factors that promote neuronal survival, differentiation, and synaptic strengthening. Key mediators include:
- Brain-Derived Neurotrophic Factor (BDNF): Regulates synaptic plasticity, supports neuronal survival, and is crucial for learning and memory processes [38].
- Glial Cell Line-Derived Neurotrophic Factor (GDNF): Promotes dopamine neuron survival and supports synaptic function [38].
- Nerve Growth Factor (NGF): Essential for growth, maintenance, and survival of neurons [38].
- Tropomyosin-related receptor kinase B (TrkB): The primary receptor for BDNF, activation triggers intracellular signaling cascades that promote neuronal growth and plasticity [38].
Physical exercise and cognitive training have been shown to upregulate these neurotrophic factors, creating a molecular environment conducive to neural reorganization and circuit optimization [38].
Assessment Methodologies
Advances in neurotechnology enable precise quantification of neuroplastic changes at multiple scales:
- Neuroimaging: Structural and functional MRI detect exercise-induced changes in hippocampal volume, cortical thickness, and network connectivity [37] [39].
- Molecular assays: ELISA, immunoblotting, and RT-PCR measure exercise-induced changes in neurotrophic factor levels and receptor expression in both human and animal models [38].
- Behavioral testing: Cognitive batteries (e.g., MCCB, WAIS) assess functional outcomes across domains including attention, memory, and executive function [39].
Physical Exercise as a Neuroplasticity Inducer
Mechanistic Pathways
Physical exercise induces neuroplasticity through multiple biological pathways that converge to enhance brain structure and function. The signaling cascade begins with exercise-induced molecular changes that ultimately translate to improved cognitive performance.
Figure 1: Exercise-Induced Neuroplasticity Signaling Pathways
Empirical Evidence and Outcomes
Substantial evidence from both animal and human studies demonstrates the efficacy of physical exercise for enhancing cognitive function across multiple domains and populations.
Table 1: Effects of Physical Exercise on Cognitive Domains in Schizophrenia Spectrum Disorders [39]
| Cognitive Domain | Effect Size | Statistical Significance | Population | Exercise Modality |
|---|---|---|---|---|
| Global Cognition | Moderate to Large | p < 0.001 | SCZ (10 studies, n=385) | Aerobic, Supervised |
| Working Memory | 34% Improvement | p < 0.05 | SCZ (659 participants) | Aerobic & Strength |
| Attention | Significant | p < 0.009 | SCZ (122 studies, n=7,231) | Various |
| Executive Function | Significant | p = 0.013 | SCZ (122 studies, n=7,231) | Various |
| Social Cognition | Significant | p < 0.05 | SCZ (10 studies, n=385) | Aerobic |
| Verbal Memory | 34% Improvement | p < 0.05 | Psychosis (17 trials, n=659) | Various |
Table 2: Neurobiological Effects of Physical Exercise [37] [38]
| Outcome Measure | Effect Size/Change | Assessment Method | Experimental Model |
|---|---|---|---|
| Hippocampal Volume | 12% Increase | Structural MRI | Human (SCZ) |
| BDNF Expression | Significant Increase | ELISA, Immunoblotting | Human & Animal |
| Neurogenesis | Increased Rate | Immunofluorescence | Animal (Rat) |
| Cortical Thickness | Increased | Structural MRI | Human |
| Spatial Memory | Significant Improvement | Behavioral Tasks | Animal (Rat) |
Standardized Experimental Protocols
Well-defined exercise protocols are essential for consistent research outcomes and therapeutic application.
Table 3: Standardized Physical Exercise Protocols in Research [38]
| Protocol Parameter | Animal Model (Rat) | Human Clinical Application |
|---|---|---|
| Duration | 4-8 weeks | 12 weeks to 6 months |
| Frequency | 4-5 sessions/week | 3-5 sessions/week |
| Intensity | Progressive: 2-18 m/min | Moderate to vigorous (50-80% HRmax) |
| Session Length | 30-60 minutes | 30-60 minutes |
| Modality | Treadmill, voluntary wheel | Aerobic, resistance, yoga |
| Progression | Gradual speed/duration increase | Progressive overload |
Detailed Treadmill Protocol (Rat Model) [38]:
- Habituation Phase: 1-week adaptation with daily 3-5 minute sessions at low speed (2-8 m/min)
- Progressive Training: Gradually increase duration to 60 minutes and speed to 10-18 m/min
- Maintenance: Stable intensity and duration for remainder of protocol
- Control Procedures: Sedentary animals placed on stationary treadmill to control for handling stress
Human Aerobic Exercise Protocol [39]:
- Baseline Assessment: Cardiorespiratory fitness testing, cognitive assessment
- Progressive Regimen: Begin at 50% HRmax for 20 minutes, progressively increase to 80% HRmax for 45-60 minutes
- Supervision: Direct supervision by exercise physiologists to ensure compliance and safety
- Adherence Monitoring: Session attendance, heart rate monitoring, exercise logs
Cognitive Remediation and Targeted Learning
Principles and Mechanisms
Cognitive remediation (CR) refers to behavioral training-based interventions that target specific cognitive processes through structured practice. The effectiveness of CR stems from its ability to harness experience-dependent neuroplasticity through carefully designed learning paradigms [40]. Targeted learning engages specific neural networks through focused cognitive challenges, inducing plastic changes in the engaged circuits [37].
The three attention systems model provides a framework for understanding how cognitive training produces behavioral benefits [40]:
- Alerting network: Maintains readiness for incoming stimuli
- Orienting network: Selects specific sensory information
- Executive network: Monitors and resolves conflict in thoughts and actions
CR produces the strongest effects when targeting the executive network, which shows high plasticity in response to targeted training [40].
Evidence Base and Applications
Cognitive remediation has demonstrated efficacy across multiple psychiatric and neurological conditions:
- Schizophrenia: CR produces moderate improvements in cognitive function with better outcomes when integrated into comprehensive psychiatric rehabilitation [39].
- ADHD: Attention training can improve executive function, potentially serving as an adjunct or alternative to pharmacological treatment [40].
- Age-related cognitive decline: Cognitive training can enhance memory and executive function in older adults [37].
Key limitations in the field include overstated claims of far transfer effects by commercial brain training programs and methodological challenges in controlling for placebo effects [40]. The most effective approaches integrate CR with other evidence-based treatments rather than administering it in isolation [39].
Integrated Interventions and Synergistic Effects
Combined Physical and Cognitive Training
Emerging evidence suggests that combining physical exercise with cognitive remediation produces superior outcomes compared to either intervention alone:
- Animal studies: Environmental enrichment combined with voluntary wheel running produces greater increases in neurogenesis and improved spatial memory compared to either intervention alone [37].
- Human studies: Integrated physical and cognitive training provides superior benefits and quicker improvements compared to cognitive remediation alone in schizophrenia [39].
- Proposed mechanism: Physical exercise creates a neuroplastic-ready brain state by upregulating BDNF, which then amplifies the effects of subsequent cognitive training on synaptic strengthening and circuit reorganization [37].
Experimental Support for Synergistic Effects
Research demonstrates that combined interventions leverage complementary mechanisms:
- Temporal sequencing: Animal studies suggest cognitive stimulation during or immediately following physical exercise maximizes synergistic effects [37].
- Dose-response relationship: Higher intensity and longer duration protocols generally produce larger effects, with supervised exercise showing advantages over unsupervised regimens [39].
- Neurobiological basis: Combined interventions produce greater increases in hippocampal volume, cortical thickness, and neurotrophic factor expression compared to single-modality approaches [37] [39].
Research Applications and Methodological Considerations
The Scientist's Toolkit
Table 4: Essential Research Reagents and Materials
| Item | Function/Application | Example Use Cases |
|---|---|---|
| Open-field treadmill | Controlled aerobic exercise | Rat exercise studies [38] |
| Voluntary running wheel | Naturalistic exercise behavior | Mouse voluntary exercise models [38] |
| ELISA kits | Quantify BDNF, GDNF, NGF levels | Measure neurotrophic response [38] |
| Anti-BDNF antibodies | Immunohistochemistry, Western blot | Localize BDNF expression [38] |
| MRI/FMRI systems | Structural and functional brain imaging | Human hippocampal volume measurement [37] [39] |
| Cognitive batteries (MCCB, WAIS) | Standardized cognitive assessment | Pre/post intervention cognitive testing [39] |
| RNA extraction kits | Gene expression analysis | BDNF, TrkB mRNA quantification [38] |
Experimental Workflow
A standardized methodology ensures reproducible assessment of behavioral inducers on neuroplasticity outcomes.
Figure 2: Experimental Workflow for Neuroplasticity Intervention Studies
Methodological Challenges and Solutions
Research in behavioral induction of neuroplasticity faces several methodological challenges:
- Blinding difficulties: Participants are typically aware of their assignment in exercise trials, potentially introducing expectancy effects.
- Optimal dosing: The precise parameters for exercise intensity, duration, and cognitive training progression require further refinement.
- Individual differences: Factors such as age, genetics, baseline fitness, and cognitive status moderate response to interventions.
- Long-term adherence: Maintaining participation over extended periods remains challenging, particularly for unsupervised interventions.
Behavioral and experiential inducers represent powerful, evidence-based approaches for harnessing neuroplasticity to enhance cognitive function and treat neurological and psychiatric conditions. The research evidence demonstrates that physical exercise, cognitive remediation, and targeted learning produce significant structural and functional changes in the brain through mechanisms involving neurotrophic factor signaling, neurogenesis, and synaptic plasticity.
Future research directions should focus on:
- Precision medicine approaches: Identifying biomarkers that predict individual response to specific interventions
- Optimal protocol parameters: Refining intensity, duration, and timing of interventions for maximal effect
- Combination therapies: Developing optimized protocols that integrate behavioral interventions with pharmacological approaches
- Technology-enabled delivery: Leveraging digital health platforms to increase accessibility and adherence
- Long-term sustainability: Determining strategies for maintaining benefits beyond the intervention period
For drug development professionals, these behavioral interventions offer complementary approaches that may enhance pharmacological efficacy or reduce required dosages. The continued elucidation of their mechanisms provides novel targets for therapeutic development while the interventions themselves represent valuable adjuncts or alternatives to conventional treatments.
Neuromodulation technologies represent a revolutionary approach in neuroscience for modulating neural activity to study and enhance brain function. These technologies, which include Transcranial Magnetic Stimulation (TMS), Transcranial Direct Current Stimulation (tDCS), Trigeminal Nerve Stimulation (TLNS), and Brain-Computer Interfaces (BCIs), operate on the fundamental principle of inducing neuroplasticity—the brain's ability to reorganize its structure, function, and connections in response to experience and stimulation [34] [41]. Within the context of behavioral adaptation and optimal performance research, these tools provide a means to directly influence the neural mechanisms that underlie learning, skill acquisition, and cognitive enhancement. By promoting targeted neuroplastic changes, neuromodulation technologies offer unprecedented opportunities to optimize human performance and facilitate recovery from neurological conditions, thereby bridging the gap between fundamental neuroscience and applied clinical interventions [42] [43].
The significance of these technologies is further underscored by rapid market growth and scientific interest. The U.S. neurological device market was valued at over $7.6 billion in 2024 and is projected to reach nearly $10 billion by 2031, reflecting a compound annual growth rate of 3.8% [44]. A bibliometric analysis of the field from 2014 to 2024 identified 1,348 relevant publications, with the most significant growth occurring between 2020 and 2021, indicating accelerating research interest and technological development [45]. This expansion is driven by continuous advancements in stimulation precision, device portability, and the integration of artificial intelligence to create personalized treatment protocols [44] [46].
Technical Specifications of Neuromodulation Technologies
Table 1: Comparative Technical Specifications of Major Neuromodulation Technologies
| Parameter | TMS/rTMS | tDCS | TLNS | BCIs |
|---|---|---|---|---|
| Stimulation Mechanism | Electromagnetic induction | Weak direct current (1-2 mA) | Electrical stimulation of trigeminal nerve | Signal acquisition, feature extraction, translation |
| Spatial Resolution | Moderate (cm range) | Low (diffuse) | High (specific nerve branches) | Varies with invasiveness: High (invasive) to Low (non-invasive) |
| Temporal Resolution | High (milliseconds) | Low (minutes to hours after stimulation) | Medium | High (real-time processing) |
| Depth of Penetration | Cortical (up to 2 cm) [46] | Superficial cortical | Peripheral to central projections | Full cortical access (invasive) or superficial (non-invasive) |
| Primary Applications | Depression, stroke rehab, chronic pain [46] [45] | Motor recovery, cognitive enhancement, chronic pain [41] [47] | Epilepsy, attention modulation | Motor restoration for paralysis, communication aids [42] [48] |
| Invasiveness | Non-invasive | Non-invasive | Non-invasive or minimally invasive | Non-invasive to fully invasive [48] |
| Key Stimulation Parameters | Frequency (1-20 Hz), intensity (% motor threshold), pulse patterns (theta-burst) [46] | Current intensity (1-2 mA), electrode montage, duration (10-30 min) [41] | Electrode placement, frequency, current intensity | Signal-to-noise ratio, number of electrodes, decoding algorithms [42] |
| Neuroplastic Effects | LTP/LTD-like effects, modulation of cortical excitability [46] | Modulation of resting membrane potential, changes in cortical excitability [41] [43] | Regulation of cortical excitability via brainstem nuclei | Promotion of use-dependent plasticity through neurofeedback [42] |
Emerging Technical Trends
The field of neuromodulation is rapidly evolving toward greater precision and personalization. Closed-loop systems represent a particularly promising direction, combining real-time neural activity monitoring with adaptive stimulation parameters. These systems can detect pathological activity patterns and deliver precisely timed interventions, potentially enhancing therapeutic efficacy while reducing side effects [49] [44]. The integration of artificial intelligence and machine learning algorithms further refines these approaches by enabling patient-specific protocol optimization and outcome prediction [46]. Additionally, advancements in miniaturization and portability are expanding access to neuromodulation beyond traditional clinical settings, allowing for longer treatment durations and more naturalistic study of neural function [46].
Mechanisms of Action and Neuroplasticity
Neuromodulation technologies induce behavioral adaptation and support optimal performance primarily through the promotion of adaptive neuroplasticity—the brain's ability to reorganize its structure and function in response to experience [34] [41]. The specific mechanisms vary by technology but share common pathways involving modulation of neural excitability, synaptic strength, and network connectivity.
At the cellular level, techniques like TMS and tDCS influence cortical excitability through distinct yet complementary mechanisms. TMS generates brief, intense magnetic pulses that induce electrical currents in targeted cortical regions, leading to neuronal depolarization. Depending on stimulation parameters, TMS can produce long-term potentiation (LTP)-like or long-term depression (LTD)-like effects, thereby strengthening or weakening specific neural pathways [46]. In contrast, tDCS applies weak direct currents that modulate the resting membrane potential of neurons, making them more or less likely to fire in response to natural signals. Anodal stimulation typically depolarizes neurons (increasing excitability), while cathodal stimulation hyperpolarizes them (decreasing excitability) [41] [43].
These cellular changes manifest at the systems level as alterations in functional connectivity within and between neural networks. For instance, BCIs promote plasticity through use-dependent reinforcement, where successful performance of a desired mental command is rewarded with positive feedback, strengthening the underlying neural representations [42]. Similarly, when combined with physical or cognitive training, neuromodulation techniques can enhance consolidation of learning by optimizing brain states for skill acquisition [43].
A critical consideration in neuromodulation is the concept of the hormetic dose-response, a biphasic model where low-level challenges confer beneficial adaptations while excessive stimulation causes detrimental effects [43]. This principle emphasizes the importance of identifying optimal stimulation parameters for each individual to promote adaptive plasticity without overwhelming neural circuits.
Figure 1: Neuroplasticity Mechanisms of Neuromodulation Technologies. This diagram illustrates how various neuromodulation techniques engage cellular and systems-level mechanisms to promote functional outcomes through neuroplastic adaptation.
Experimental Protocols and Methodologies
Protocol Design Considerations
Designing effective neuromodulation experiments requires careful consideration of multiple parameters that influence neuroplastic outcomes. The hormetic principle is critical—researchers must identify stimulation intensities that provide sufficient challenge to induce adaptation without causing neural exhaustion or maladaptive changes [43]. Other key considerations include stimulation location (target brain region or nerve pathway), session duration and frequency, and concurrent behavioral training. Individual factors such as genetic polymorphisms, baseline neural excitability, and pathological characteristics also significantly influence response to neuromodulation and should be accounted for in study design [43].
Table 2: Standardized Experimental Protocols for Neuromodulation Technologies
| Technology | Protocol Type | Parameters | Session Structure | Target Population | Primary Outcome Measures |
|---|---|---|---|---|---|
| rTMS | Theta-Burst Stimulation (iTBS) | 50 Hz triplets, 5 Hz burst frequency, 2s on/8s off, 600 pulses total, 80% motor threshold [46] | 1 session/day, 3-5 days/week for 4-6 weeks | Depression, stroke rehabilitation | HAMD, motor function scales, neurophysiological measures (MEP) |
| rTMS | Low-Frequency (LF-rTMS) | 1 Hz, 90-120% motor threshold, 15-20 min sessions, 1200 pulses/session [46] | 1 session/day, 5 days/week for 2-4 weeks | Chronic pain, epilepsy | VAS pain scales, seizure frequency, fMRI connectivity |
| tDCS | Anodal Motor Cortex Stimulation | 1-2 mA, 35 cm² electrodes, 20-30 min, anode over M1, cathode contralateral supraorbital [41] | 1 session/day, 5-10 sessions over 2 weeks | Stroke motor recovery | Fugl-Meyer Assessment, Jebsen-Taylor Hand Function Test |
| tDCS | Bifrontal Stimulation | 2 mA, 35 cm² electrodes, 30 min, anode over F3, cathode over F4 | 1 session/day, 10-15 sessions over 2-3 weeks | Major depression, cognitive enhancement | HAMD, cognitive battery tests, EEG biomarkers |
| BCI | Motor Imagery Training | Graz BCI protocol, CSP for feature extraction, LDA classification, 2-4 classes [42] | 2-3 sessions/week, 45-60 min, 4-8 weeks | Spinal cord injury, stroke | BCI accuracy, Fitts' law test, SCPs |
| BCI | P300 Speller | Visual oddball paradigm, 5-20 Hz flashing, stepwise linear discriminant analysis | 2-3 sessions/week, 30-45 min, 4-12 weeks | ALS, locked-in syndrome | Characters per minute, accuracy rate, P300 amplitude |
Integration with Behavioral Paradigms
The timing of neuromodulation relative to behavioral training is critical for optimizing outcomes. Online approaches (stimulation during training) can enhance immediate performance by optimizing brain states for learning, while offline approaches (stimulation before or after training) may strengthen memory consolidation [43]. For example, applying tDCS during motor practice enhances skill acquisition, whereas stimulation after practice strengthens retention. Similarly, BCIs inherently combine neural modulation with task performance through closed-loop feedback, creating tight coupling between brain activity and behavioral reinforcement [42].
Figure 2: Experimental Workflow for Neuromodulation Studies. This diagram outlines the standard methodology for conducting neuromodulation research, from participant screening through data analysis, highlighting key decision points.
The Scientist's Toolkit: Research Reagents and Materials
Table 3: Essential Research Materials and Equipment for Neuromodulation Studies
| Category | Item | Specifications | Research Function |
|---|---|---|---|
| Stimulation Equipment | TMS Device with Cooled Coil | 1.5-2.5 T magnetic field, 10-20 μH coil inductance, 5000-10,000 A current [46] | Generation of precise magnetic pulses for cortical stimulation |
| Stimulation Equipment | tDCS/tACS Device | Constant current (1-2 mA), low impedance monitoring, programmable waveform | Delivery of weak electrical currents for cortical modulation |
| Stimulation Equipment | BCI System | EEG amplifiers (≥16 channels), signal processing unit, feedback display | Acquisition and translation of neural signals for device control |
| Electrodes & Interfaces | EEG Electrodes | Ag/AgCl, sintered silver, or gold-coated; passive or active | Recording electrical brain activity with optimal signal quality |
| Electrodes & Interfaces | tDCS Electrodes | Conductive rubber or metal with saline-soaked sponges (35 cm²) | Safe current delivery with minimized skin irritation |
| Electrodes & Interfaces | Utah Array / Microelectrodes | 96-256 channels, biocompatible materials (silicon, platinum, iridium) | High-resolution neural recording and stimulation in invasive BCIs |
| Localization & Targeting | Neuronavigation System | MRI/CT co-registration, infrared or electromagnetic tracking, 3D reconstruction | Precise targeting of brain regions for TMS and tDCS |
| Localization & Targeting | EMG System | Surface or needle electrodes, amplifiers, filters (10-500 Hz) | Recording motor evoked potentials (MEPs) for TMS outcome measures |
| Software & Analysis | Signal Processing Toolbox | MATLAB with EEGLAB, FieldTrip, or BCILAB; Python with MNE | Analysis of neural signals, feature extraction, and classification |
| Software & Analysis | Computational Modeling Software | SIMNIBS, ROAST, finite element method (FEM) tools | Prediction of current flow and optimization of stimulation parameters |
Applications in Behavioral Adaptation and Performance Optimization
Clinical Applications
Neuromodulation technologies show particular promise in enhancing recovery from neurological injury by promoting adaptive plasticity. In stroke rehabilitation, tDCS combined with constraint-induced movement therapy significantly improves upper extremity function by rebalancing interhemispheric competition and enhancing use-dependent plasticity [41]. Similarly, BCIs for motor restoration create closed-loop systems where attempted movements generate sensory feedback, strengthening residual neural connections and promoting functional recovery [42]. For chronic neuropathic pain—a condition characterized by maladaptive plasticity—noninvasive neuromodulation techniques like rTMS and tDCS can reverse central sensitization and restore normal pain processing [47]. These approaches target the prefrontal cortex, primary motor cortex, and other regions involved in the pain matrix, inducing analgesic effects through top-down modulation of pain pathways.
Cognitive and Performance Enhancement
Beyond clinical applications, neuromodulation technologies are increasingly explored for enhancing cognitive performance in healthy individuals. tDCS applied to prefrontal regions can improve working memory, attention, and executive functions by optimizing neuronal excitability during cognitive tasks [43]. The timing of stimulation appears critical, with effects being most pronounced when applied during or immediately before task performance. Similarly, BCIs utilizing neurofeedback paradigms enable users to learn voluntary regulation of brain activity patterns associated with optimal performance states, potentially enhancing focus and cognitive control [48]. These applications raise important ethical considerations regarding cognitive enhancement, necessitating careful oversight and regulation.
The field of neuromodulation is rapidly advancing toward more precise, adaptive, and personalized approaches. Closed-loop systems that monitor neural activity and adjust stimulation parameters in real time represent a particularly promising direction, potentially enhancing efficacy while minimizing side effects [49] [44]. The integration of artificial intelligence and machine learning will further refine these approaches by enabling prediction of individual response patterns and optimization of stimulation parameters [46]. Additionally, miniaturization of devices and the development of wearable neuromodulation technologies will expand applications beyond laboratory and clinical settings, allowing for chronic use in natural environments [48].
As these technologies evolve, several challenges must be addressed. Standardization of protocols across research sites remains limited, complicating comparison of results and replication of findings [45]. The biological mechanisms underlying the effects of neuromodulation, particularly long-term neuroplastic changes, require further elucidation [43]. Additionally, ethical considerations surrounding cognitive enhancement, neural privacy, and equitable access to emerging technologies demand ongoing attention and dialogue [48].
In conclusion, TMS, tDCS, TLNS, and BCIs represent powerful tools for studying and enhancing neuroplasticity to promote behavioral adaptation and optimal performance. By directly modulating neural activity, these technologies offer unprecedented opportunities to understand and influence the brain's remarkable capacity for change. As research continues to refine these approaches and elucidate their mechanisms, neuromodulation holds great promise for advancing both fundamental neuroscience and clinical applications in neurology and psychiatry.
The brain's capacity for neuroplasticity—its ability to reorganize itself by forming new neural connections throughout life—serves as the fundamental biological substrate for behavioral adaptation and optimal performance. This dynamic process encompasses synaptic strengthening and weakening, cortical remapping, and neurogenesis, enabling learning, memory formation, and recovery from injury [25]. Within the context of behavioral adaptation research, targeting neuroplasticity pharmacologically offers a promising avenue for enhancing cognitive flexibility, emotional regulation, and skill acquisition. The imperative for novel pharmacological agents stems from the limitations of current neuropsychiatric therapeutics, which often fail to address core plasticity deficits underlying these conditions [50]. This whitepaper delineates strategic molecular targets and corresponding experimental methodologies for developing compounds designed to enhance neuroplasticity, thereby facilitating superior behavioral outcomes and performance optimization.
Neuroplasticity Fundamentals and Pharmacological Rationale
Neuroplasticity operates through several core mechanisms: synaptic plasticity (e.g., long-term potentiation (LTP) and long-term depression (LTD)), structural plasticity (changes in dendritic spines and neurite outgrowth), and cellular plasticity (including adult neurogenesis) [25] [51]. At the molecular level, these processes are governed by complex signaling cascades often initiated by glutamate receptor activation, particularly N-methyl-D-aspartate (NMDA) receptors, leading to calcium influx and downstream activation of pathways involving proteins like brain-derived neurotrophic factor (BDNF) [50] [51].
The rationale for pharmacological intervention is twofold. First, in pathological states such as depression, chronic stress contributes to neuronal atrophy and synaptic depression in prefrontal and hippocampal regions, effectively creating a deficit of neuroplasticity [50]. Second, even in healthy systems, the targeted enhancement of plasticity can theoretically accelerate learning and adaptive behavioral change. The core hypothesis is that pharmacological agents can induce a state of heightened plasticity, creating a "window of opportunity" during which cognitive training or behavioral interventions can be more effectively solidified into lasting neural circuits [50]. This synergy between drug-based and experience-dependent plasticity is the cornerstone of next-generation approaches to enhancing performance and treating neuropsychiatric disorders.
Strategic Molecular Targets and Drug Development Candidates
The following table summarizes high-priority molecular targets for pharmacological leverage of neuroplasticity, their mechanisms of action, and key developmental considerations.
Table 1: Strategic Targets for Plasticity-Enhancing Drug Development
| Molecular Target | Therapeutic Mechanism | Representative Agents | Development Status & Key Challenges |
|---|---|---|---|
| NMDA Receptor | NMDA receptor antagonism (e.g., by ketamine) triggers rapid, robust synaptogenesis and reverses stress-induced synaptic deficits [50]. | Ketamine, D-Cycloserine [50] | Rapid antidepressant efficacy proven in RCTs; challenges include transient effect duration and potential for abuse and neurotoxicity with long-term use [50]. |
| BDNF/Tropomyosin receptor kinase B (TrkB) Signaling | Enhancement of BDNF signaling promotes neuronal survival, synaptogenesis, and supports long-term maintenance of plasticity [50]. | (Positive modulators under investigation) | A key downstream mediator of ketamine's effects; challenge lies in developing blood-brain-barrier-penetrant peptides or small-molecule positive modulators [50]. |
| Metabotropic Glutamate Receptors (mGluRs) | Modulation of synaptic glutamate transmission can fine-tune plasticity induction without the pro-excitotoxic risk of direct ionotropic receptor targeting [51]. | (Various negative allosteric modulators in development) | Offers a more nuanced control over glutamatergic signaling; target validation is ongoing for depression and Fragile X syndrome [51]. |
| Muscarinic Acetylcholine Receptors | Antagonism of specific muscarinic receptor subtypes (e.g., M1) may facilitate LTP and enhance cognitive function [51]. | Scopolamine | Scopolamine shows rapid antidepressant effects; the challenge is to achieve subtype selectivity to avoid peripheral anticholinergic side effects [51]. |
Experimental Protocols for Evaluating Plasticity-Enhancing Compounds
Robust preclinical evaluation is critical for validating candidate compounds. The following protocols are essential components of a drug development pipeline.
In Vitro Long-Term Potentiation (LTP) Induction and Pharmacological Interference
This protocol assesses a compound's direct impact on synaptic strengthening in brain tissue slices [51].
- Preparation: Prepare transverse hippocampal slices (400 μm thickness) from rodents (e.g., Sprague-Dawley rats) using a vibratome in ice-cold, oxygenated (95% O₂ / 5% CO₂) artificial cerebrospinal fluid (aCSF).
- Recording: Maintain slices in an interface chamber at 28-30°C for ≥1 hour recovery. Place a stimulating electrode in the Schaffer collateral pathway and a recording electrode in the stratum radiatum of the CA1 region.
- Baseline Recording: Deliver test stimuli every 30 seconds to evoke a field excitatory postsynaptic potential (fEPSP). Adjust stimulation intensity to obtain an fEPSP slope that is 30-40% of the maximum response. Record a stable baseline for at least 20 minutes.
- Compound Application: Apply the candidate drug to the aCSF perfusion system. Include a control group with vehicle application.
- LTP Induction: After 20 minutes of drug perfusion, induce LTP using a high-frequency stimulation (HFS) protocol (e.g., 1x 100 Hz tetanus for 1 second, or 4x 100 Hz trains separated by 5 minutes).
- Post-Tetanic Recording: Continue recording fEPSPs for at least 60 minutes post-tetanus. Monitor the change in fEPSP slope as a percentage of the baseline average.
- Data Analysis: Compare the magnitude and persistence of LTP (fEPSP slope 50-60 minutes post-tetanus) between drug-treated and vehicle-control slices using ANOVA. A significant enhancement indicates a pro-plasticity effect [51].
In Vivo Assessment of Structural Plasticity using Two-Photon Microscopy
This protocol evaluates a compound's ability to induce structural changes in dendritic spines in the living brain [51].
- Surgery: Express a fluorescent protein (e.g., GFP) under a neuronal promoter in the neurons of interest (e.g., medial prefrontal cortex) in Thy1-GFP transgenic mice or via viral vector injection.
- Cranial Window Implantation: Implant a chronic cranial window over the transfected region to allow for repeated optical imaging.
- Baseline Imaging: Acquire high-resolution image stacks of apical dendritic tufts using a two-photon microscope. Identify and map a set of dendritic segments for longitudinal tracking.
- Drug Administration: Systemically administer the candidate compound or vehicle.
- Post-Treatment Imaging: Re-image the same dendritic segments at designated time points (e.g., 4, 24, and 72 hours post-injection).
- Image Analysis: Blind the analysis. For each time point, count the number of existing, newly formed, and eliminated dendritic spines. Spine density and turnover rate are calculated. A significant increase in spine formation or net density post-drug administration indicates enhanced structural plasticity [51].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Plasticity Studies
| Reagent / Material | Function and Application in Plasticity Research |
|---|---|
| Ketamine Hydrochloride | NMDA receptor antagonist; used as a positive control to induce rapid synaptogenesis and study downstream plasticity mechanisms in vitro and in vivo [50]. |
| BDNF (Human, Recombinant) | The native neurotrophin; applied in cell culture or infused in vivo to study its direct effects on neuronal survival, dendritic arborization, and synaptic potentiation [50]. |
| ANOVA Statistical Test | Used to compare means across multiple experimental groups (e.g., drug dose-response effects on LTP magnitude or spine density) [52]. |
| Two-Photon Microscope | Enables high-resolution, deep-tissue imaging of neuronal structure in live animals, crucial for longitudinal studies of dendritic spine dynamics [51]. |
| Nerve Growth Factor (NGF) | A classic neurotrophin; used to study neuronal differentiation, neurite outgrowth, and survival in primary neuronal cultures, relevant to structural plasticity [53]. |
Visualizing Core Signaling Pathways
The following diagrams illustrate key signaling pathways involved in pharmacological enhancement of neuroplasticity.
NMDA Receptor-Dependent Synaptic Plasticity
Neurotrophic Signaling and Neuronal Growth
The brain's remarkable capacity for neuroplasticity—the ability to reorganize its structure, functions, and connections in response to experience and injury—serves as the fundamental biological mechanism underlying rehabilitation across neurological disorders. Research over recent decades has debunked the historical belief that the adult brain is largely static, revealing instead that continuous real-time neural modifications occur throughout the lifespan in dynamic interaction with environmental contexts [3]. This understanding has revolutionized approaches to neurological rehabilitation, shifting therapeutic paradigms from merely compensating for lost functions to actively harnessing inherent neuroplastic potential for restoration and optimization of neural performance.
The concept of optimal performance in neural contexts refers to the ability to achieve desired outcomes in goal-directed tasks, a capacity that becomes compromised following neurological injury or disorder [3]. Successful rehabilitation requires carefully targeted interventions that leverage multiple manifestations of neuroplasticity, including but not limited to altered morphology (e.g., increased dendritic spines, modified dendritic branching), enhanced neurophysiological functions such as Long-Term Potentiation, modified neural networks, and in specific regions, adult neurogenesis [3]. This whitepaper examines four distinct neurological conditions—stroke, traumatic brain injury (TBI), schizophrenia, and spinal cord injury (SCI)—as case studies in applying neuroplasticity principles to optimize behavioral adaptation and functional recovery.
Stroke Rehabilitation: Quantitative Imaging Biomarkers and Motivation Factors
Stroke remains a leading cause of long-term disability worldwide, with approximately 15 million people experiencing cerebrovascular accidents annually [54]. Successful rehabilitation depends on both physiological mechanisms of recovery and psychological factors that influence engagement in therapeutic activities.
Quantitative Collateral Assessment with Color-Coded Multiphase CTA
Recent advances in neuroimaging have enabled more precise characterization of post-stroke neurovascular plasticity, particularly through color-coded multiphase computed tomography angiography (cmCTA). This technique employs color-coding to visually depict temporal dynamics of collateral blood flow, offering quantitative parameters that predict functional outcomes [55].
Table 1: cmCTA Parameters for Predicting Functional Outcomes in Acute Ischemic Stroke
| Parameter | Definition | Measurement Approach | Predictive Value (AUC) |
|---|---|---|---|
| Delayed Vessel Ratio (DVR) | Proportion of vessels with delayed enhancement (green/blue on cmCTA) | Semi-automatic delineation in ACA and ASPECT regions | 0.81-0.90 for functional independence and excellent recovery |
| Collateral Ratio (CR) | Ratio of enhanced vessel volume on occluded side to healthy side | Phase-specific calculation from cmCTA maps | Correlates with functional outcomes (p < 0.001) |
| Deep Venous Outflow (DVO) | Assessment of deep venous collateral circulation | 6-point scale evaluation | 0.88 for predicting functional independence |
| Superficial Venous Outflow (SVO) | Assessment of superficial venous drainage | 6-point scale evaluation | Correlates with better outcomes (p < 0.001) |
The cmCTA imaging protocol involves three-phase scanning: peak arterial phase, peak venous phase (10-second delay after arterial phase), and late venous phase (8-second delay after venous phase). Tube voltage is maintained at 100 kV throughout, with slice thickness varying between 0.625mm for arterial phase and 1.25mm for venous phases [55]. Reconstruction utilizes specialized software (e.g., FastStroke, GE Healthcare) to generate maximum intensity projection ColorViz maps with 35mm thickness and 100% color saturation.
Multidimensional Factors Influencing Rehabilitation Motivation
Beyond physiological factors, successful stroke recovery depends critically on patient engagement, which is influenced by multiple dimensions of motivation. A recent scoping review of 23 studies identified key factors that influence rehabilitation motivation [54]:
Table 2: Factors Influencing Stroke Rehabilitation Motivation
| Factor Category | Specific Elements | Impact on Rehabilitation |
|---|---|---|
| Intrinsic Drivers | Self-efficacy, depressive states, cognitive capacity | Positive correlation with motivation and adherence |
| Extrinsic Supports | Familial support, social support, therapeutic alliance | Enhanced continuity and engagement |
| Disease Characteristics | Stroke severity, functional deficits, fatigue | Negative correlation with motivation |
| Intervention Strategies | Cognitive-behavioral therapy, gamified rehabilitation, goal setting | Improved adherence and outcomes |
| Economic Considerations | Financial pressure, rehabilitation costs, insurance coverage | Impacts access and duration of care |
The methodology for assessing rehabilitation motivation typically involves mixed-methods approaches, including standardized scales for self-efficacy (e.g., Stroke Self-Efficacy Questionnaire), depression assessments (e.g., Patient Health Questionnaire-9), motivation scales specifically validated for stroke populations, and qualitative interviews to capture lived experiences. Interventions targeting motivation enhancement include cognitive-behavioral approaches that address maladaptive beliefs about recovery, gamification elements to increase engagement, and family education programs to improve support systems [54].
Traumatic Brain Injury: Extended Early Rehabilitation Protocols
Traumatic brain injury represents a leading cause of disability worldwide, with over 64 million individuals affected annually by moderate-to-severe TBI [56]. Rehabilitation approaches have evolved significantly, with recent evidence supporting the efficacy of extended early intervention protocols.
Prospective Study on Extended Early Rehabilitation
A recent prospective experimental study involving 124 patients with moderate and severe TBI demonstrated the superiority of extended early rehabilitation protocols [57]. The study employed rigorous methodology with patients randomly divided into experimental and control groups:
- Experimental Group: Received kinesitherapy seven days weekly, twice daily for 45-minute sessions (90 minutes total daily)
- Control Group: Received standard kinesitherapy seven days weekly, twice daily for 30-minute sessions (60 minutes total daily)
Both groups followed identical kinesitherapy implementation plans, including positioning, anti-decubitus programs, passive and actively assisted exercises to maintain and increase range of motion, and respiratory kinesitherapy. Inclusion criteria required hemodynamic stability (heart rate 60-130/minute, mean arterial pressure 60-100 mm Hg, peripheral oxygen saturation >88%) with careful monitoring for intolerance signs necessitating session termination [57].
Table 3: Outcomes of Extended vs. Standard Early TBI Rehabilitation
| Outcome Measure | Experimental Group (n=62) | Control Group (n=62) | P-value |
|---|---|---|---|
| Tracheostomy at Hospital Discharge | 6 | 16 | 0.019 |
| Nasogastric Tube at ICU Discharge | 33 | 45 | 0.026 |
| Decubitus Ulcers at ICU Discharge | 0 | 4 | 0.042 |
| Diapers at Hospital Discharge | 29 | 40 | 0.047 |
| Urinary Catheter at Hospital Discharge | 38 | 48 | 0.051 |
| Mortality | 5 | 5 | NS |
| Rehabilitation Interruptions | 5 | 6 | NS |
The safety profile of extended early rehabilitation was favorable, with no statistically significant difference in adverse events between groups. This finding addresses historical concerns about early mobilization in critically ill TBI patients [57].
Integrated Rehabilitation Framework for Moderate-to-Severe TBI
Comprehensive TBI rehabilitation requires a multidisciplinary approach addressing the diverse physical, cognitive, behavioral, and psychosocial impairments that follow injury [56]. Current evidence supports an integrated framework incorporating:
- Restitutional Strategies: Direct restoration of lost functions through targeted exercises
- Compensatory Approaches: Teaching alternative methods to accomplish tasks
- Adaptive Techniques: Adjusting to new ways of living with residual limitations
Emerging technological innovations showing promise in TBI rehabilitation include virtual reality systems for immersive task-specific training, robotics for repetitive movement practice, brain-computer interfaces for severe motor deficits, and tele-rehabilitation to expand access to specialized care [56]. The integration of neurogaming and dual-task training provides simultaneous physical and cognitive challenges, enhancing engagement and promoting neuroplasticity through enriched environmental interactions.
Schizophrenia: Targeting Cognitive Symptoms Through Novel Mechanisms
While traditionally conceptualized as a psychiatric disorder, schizophrenia involves fundamental disruptions in neurodevelopment and neural circuitry that respond to principles of neuroplasticity. Current treatment approaches are expanding beyond dopamine-centric models to address particularly challenging cognitive symptoms.
GABAergic Dysfunction and Developmental Trajectory
Recent research has identified specific abnormalities in GABAergic projection neurons as a key mechanism underlying cognitive symptoms in schizophrenia [58]. Utilizing a mouse model with 15q13.3 microdeletion syndrome (associated with schizophrenia in humans), investigators tracked brain development from fetal stages to adulthood, discovering that dramatic functional changes occur late in brain development, specifically during the transition from childhood to adolescence.
The experimental approach involved:
- Genetic Modeling: Mice with 15q13.3 microdeletion to mimic human genetic vulnerability
- Longitudinal Monitoring: Tracking brain development across developmental stages
- Sleep as Behavioral Marker: Utilizing sleep disruptions as measurable behavioral output
- Cell-Specific Manipulation: Using chemogenetics to selectively modulate specific neuron populations
Notably, researchers demonstrated that until a specific developmental point, brain compensation maintains relatively normal function despite underlying abnormalities. This period may represent a critical treatment window where interventions could prevent functional impairment [58].
Experimental Therapeutic Approach
The investigation employed chemogenetic techniques (DREADDs - Designer Receptors Exclusively Activated by Designer Drugs) to selectively modulate the activity of identified overactive GABAergic projection neurons. When researchers reduced activity of these specific cells, sleep patterns in the test animals began to resemble those of healthy mice, suggesting potential for targeted symptom alleviation [58].
This approach represents a significant departure from conventional antipsychotic medications, which broadly affect dopamine or serotonin systems and often produce substantial side effects while providing limited benefit for cognitive symptoms. The precision of targeting specific malfunctioning cell types offers potential for more effective interventions with reduced adverse effects.
Spinal Cord Injury: Neuroinflammation Modulation and Regenerative Approaches
Spinal cord injury involves complex secondary injury processes that extend beyond initial mechanical damage, creating barriers to neural repair while simultaneously offering multiple intervention targets for neuroplasticity-based recovery.
Poliumoside and PI3K/AKT/mTOR Signaling Pathway
Recent research has identified poliumoside as a promising compound for modulating the destructive neuroinflammatory cascade following SCI [59]. The experimental methodology involved:
- SCI Modeling: Standardized contusion or compression injury models in rodents
- Compound Administration: Poliumoside delivery via systematic injection protocols
- Molecular Pathway Analysis: Assessment of PI3K/AKT/mTOR pathway activation through Western blot, immunohistochemistry, and RNA sequencing
- Functional Assessment: Behavioral tests (e.g., Basso Mouse Scale, CatWalk gait analysis) to quantify functional recovery
- Histological Validation: Tissue analysis to evaluate lesion volume, axonal sprouting, and glial scar formation
The mechanism of action involves poliumoside activation of the PI3K/AKT/mTOR pathway, which subsequently inhibits excessive microglial activation and reduces production of pro-inflammatory cytokines (TNF-α, IL-1β, IL-6), while simultaneously promoting antioxidant enzyme expression to combat oxidative stress [59].
Emerging Regenerative Strategies
The field of SCI research is rapidly advancing beyond neuroprotection toward truly regenerative approaches. Current investigational strategies include [59]:
- Cell Therapies: Stem cell transplantation to replace lost neural cells and create permissive environments for regeneration
- Biomaterials: Engineered scaffolds that provide physical guidance and molecular cues for axonal growth
- Neurotechnology: Brain-computer interfaces and electrical stimulation systems to bypass injury sites and restore communication between brain and periphery
- Combinatorial Approaches: Integrated protocols that simultaneously address multiple aspects of the injury cascade
These approaches recognize that successful recovery requires both modulation of the inhibitory post-injury environment and enhancement of the intrinsic growth capacity of damaged neurons.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Cross-disciplinary research in neurological disorders utilizes specialized reagents and methodologies to investigate and manipulate neuroplasticity mechanisms.
Table 4: Essential Research Reagents for Neuroplasticity and Rehabilitation Research
| Reagent/Method | Application | Function in Research |
|---|---|---|
| Chemogenetics (DREADDs) | Schizophrenia models [58] | Selective modulation of specific neuron populations |
| Color-Coded Multiphase CTA | Stroke imaging [55] | Visualization and quantification of collateral blood flow dynamics |
| Poliumoside | Spinal cord injury [59] | Activation of PI3K/AKT/mTOR pathway to reduce neuroinflammation |
| Glasgow Coma Scale | TBI assessment [57] | Standardized neurological evaluation of consciousness level |
| Functional Independence Measure | TBI outcomes [56] | Assessment of disability and monitoring rehabilitation progress |
| 15q13.3 Microdeletion Model | Schizophrenia research [58] | Genetic modeling of neurodevelopmental disorder vulnerability |
| Modified Rankin Scale | Stroke outcomes [55] | Functional outcome measurement after neurological injury |
| Dual-Task Training Paradigms | TBI rehabilitation [56] | Simultaneous cognitive and motor training to enhance engagement |
These case studies across four distinct neurological conditions reveal convergent principles in harnessing neuroplasticity for optimal behavioral adaptation and functional recovery. First, the timing of intervention is critical, with early targeted rehabilitation demonstrating superior outcomes across conditions, though different disorders may have distinct optimal windows for intervention. Second, successful approaches increasingly employ precision targeting of specific neural mechanisms rather than broad neuromodulation. Third, quantitative biomarkers are essential for both prognosis and tracking treatment response. Finally, multidimensional factors—from molecular pathways to psychological motivation—must be addressed simultaneously for optimal outcomes.
The future of neurorehabilitation lies in increasingly personalized approaches that integrate cutting-edge neurotechnologies with fundamental principles of neural adaptation, all while addressing the unique combination of physiological, psychological, and social factors that influence each individual's recovery trajectory. As research continues to elucidate the complex mechanisms governing neuroplasticity, rehabilitation paradigms will increasingly shift from compensatory approaches to true restoration of function through targeted manipulation of the brain's inherent adaptive capacity.
Overcoming Plateaus and Challenges in Neuroplasticity Induction
Identifying and Breaking Through Recovery Plateaus in Chronic Conditions
Recovery plateaus present a significant challenge in the rehabilitation of chronic neurological conditions, representing a critical juncture where functional progress stabilizes despite ongoing intervention. This technical review examines the neurobiological underpinnings of these plateaus within the context of adaptive neuroplasticity and optimal performance research. We synthesize evidence from preclinical and clinical studies to elucidate mechanisms involving metabolic constraints, maladaptive plasticity, and network reorganization failures. The article provides comprehensive experimental protocols for plateau identification and intervention, detailed signaling pathways, and reagent solutions for translational research. By integrating advanced imaging, computational modeling, and targeted interventions, researchers can develop precision approaches to reactivate neuroplastic potential beyond apparent recovery limits. This synthesis offers a framework for pharmaceutical and device development professionals to advance therapeutic strategies that overcome stabilization barriers in chronic recovery trajectories.
Neurobiological Foundations of Recovery Plateaus
Defining the Recovery Plateau Phenomenon
The recovery plateau represents a period of significantly slowed or stalled functional improvement despite continued rehabilitation efforts. In stroke recovery, motor recovery typically plateaus between 3-6 months post-injury, with over 50% of survivors exhibiting persistent hemiparesis at 6-month follow-up [60]. This stabilization occurs despite the brain's inherent neuroplastic capacity, suggesting a complex interaction between internal constraints and external therapeutic factors. The plateau should not be interpreted as the absolute limit of recovery potential, but rather as a transition between different phases of neuroplastic response [61].
From a neuroplasticity perspective, plateaus may reflect a transition from the subacute recovery phase (3-6 months), characterized by heightened plasticity, to the chronic phase (beyond 6 months), where different mechanisms govern neural adaptation [61]. The traditional clinical interpretation that recovery "maxes out" approximately one year post-injury is being reconsidered, as evidence demonstrates that directed effort and targeted interventions can spark neuroplastic change and functional gains well beyond this timeframe [61].
Mechanisms Underlying Neuroplastic Plateaus
Multiple intersecting biological processes contribute to the recovery plateau phenomenon in chronic conditions:
Metabolic and Growth Factor Depletion: The initial post-injury period is characterized by a surge in growth factors and inflammatory mediators that create a permissive environment for plasticity. Over time, this neurochemical milieu normalizes, reducing the priming for structural changes [62]. The reduction in brain-derived neurotrophic factor (BDNF) and other trophic factors may particularly impact synaptic strengthening and network reorganization [61].
Maladaptive Plasticity: Not all neuroplastic changes support functional recovery. Maladaptive plasticity can manifest as chronic pain, spasticity, or learned non-use of affected limbs, creating neural pathways that actively interfere with recovery [61]. These patterns become reinforced through repetition and neural efficiency, making them increasingly difficult to modify.
Network Stabilization and Homeostatic Regulation: As neural circuits establish new patterns of activation, homeostatic mechanisms work to stabilize these networks, reducing their responsivity to further modification [3]. This stabilization represents a potential adaptive mechanism that becomes maladaptive in the context of ongoing recovery needs.
Gliotic Barrier Formation: Following traumatic brain injury, reactive gliosis and gliotic scar tissue formation creates both physical and chemical barriers to axonal sprouting and regeneration [62]. While initially protective, this scarring can limit long-term structural reorganization.
Table 1. Primary Neurobiological Factors Contributing to Recovery Plateaus
| Factor Category | Specific Mechanisms | Impact on Recovery |
|---|---|---|
| Molecular Environment | Reduced growth factor expression (BDNF, NGF, GDNF); Increased inhibitory factors (Nogo-A, MAG) | Decreased synaptic strengthening and axonal sprouting capacity |
| Structural Barriers | Gliotic scar formation; Reduced dendritic branching in specific regions; Decreased synaptogenesis | Physical and chemical barriers to neural reorganization |
| Network Dynamics | Established maladaptive pathways; Homeostatic regulation of circuit excitability; Reduced network flexibility | Stabilization of suboptimal functional patterns; Resistance to reorganization |
| Metabolic Changes | Reduced angiogenesis in chronic phase; Altered cerebral blood flow distribution; Mitochondrial dysfunction | Limited energy supply to support plastic changes |
Quantitative Assessment and Detection Methodologies
Functional and Structural Imaging Protocols
Advanced neuroimaging techniques provide critical windows into the neuroplastic changes associated with recovery plateaus, offering biomarkers for plateau detection and intervention monitoring:
Functional MRI (fMRI) Experimental Protocol:
- Subject Preparation: Participants should refrain from caffeine, nicotine, and strenuous exercise for 4 hours prior to scanning. For motor task paradigms, ensure affected limbs are properly positioned for comfortable movement within scanner constraints.
- Task Paradigm Design: Implement block designs with alternating 30-second activation and 30-second rest periods. For upper extremity motor assessment, use finger-tapping or hand-closing movements paced at 1Hz with visual or auditory metronome guidance.
- Data Acquisition Parameters: Acquire T2*-weighted echoplanar images with TR=2000ms, TE=30ms, flip angle=75°, matrix size=64×64, FOV=220mm, slice thickness=3-4mm. Include high-resolution T1-weighted anatomical scans (MPRAGE sequence) for spatial normalization.
- Analysis Pipeline: Preprocess data with motion correction, spatial smoothing (6mm FWHM kernel), and temporal filtering. Use general linear model (GLM) analysis with hemodynamic response function modeling to identify activation patterns. Compare bilateral activation in motor networks, with increased contralesional activation often indicating compensatory patterns that may contribute to plateaus [62].
Diffusion Tensor Imaging (DTI) for White Matter Integrity:
- Acquisition Protocol: Use single-shot echoplanar imaging with 30-64 diffusion directions, b-value=1000 s/mm², and at least one b=0 image. Spatial resolution of 2×2×2mm provides balance between signal-to-noise and resolution.
- Tract-Based Spatial Statistics (TBSS): Perform whole-brain skeletonization of white matter tracts with FA threshold typically set at 0.2. Focus on corticospinal tract integrity as primary biomarker for motor recovery potential.
- Longitudinal Analysis: Register serial scans to baseline using nonlinear registration. Calculate changes in fractional anisotropy (FA), mean diffusivity (MD), radial diffusivity (RD), and axial diffusivity (AD) in regions of interest. Plateaus often correlate with stabilization of white matter metrics after initial post-injury changes [62].
Table 2. Quantitative Metrics for Plateau Identification and Monitoring
| Assessment Domain | Specific Metrics | Plateau Indicators |
|---|---|---|
| Functional Imaging (fMRI) | Laterality Index; Activation cluster volume; Network connectivity strength | Stabilization of laterality index; Reduced expansion of activation clusters; Decreased cross-hemispheric connectivity |
| Structural Imaging (DTI) | Fractional Anisotropy (FA); Mean Diffusivity (MD); Tract volume | Minimal change in FA (<2% over 3 months); Stabilization of MD values; Lack of tract reorganization |
| Neurophysiological (TMS) | Motor Evoked Potential amplitude; Cortical Silent Period; Intracortical inhibition/facilitation | Consistent MEP thresholds; Minimal change in cortical map topography; Stable interhemispheric inhibition balance |
| Behavioral Performance | Fugl-Meyer Assessment (stroke); Gait speed; Nine-Hole Peg Test; Functional Independence Measure | <5% change in primary measures over 4-week period with continued intervention |
Mathematical Modeling of Recovery Trajectories
Precision rehabilitation approaches increasingly incorporate mathematical modeling to predict and identify recovery plateaus, enabling more personalized intervention timing:
Recovery Trajectory Modeling Equation:
Where:
F(t)= Functional ability at time tB= Baseline function (pre-intervention)R= Individual recovery potential (genetic, age, comorbidity factors)α= Therapy efficacy coefficient (type, intensity, timing)T= Therapy intensity (hours/week)λ= Recovery plateau rate (determines steepness of plateau onset)t= Time since intervention initiation [63]
Parameter Estimation Protocol:
- Collect longitudinal functional assessment data at minimum of 5 timepoints
- Use nonlinear least squares optimization to fit model parameters
- Calculate confidence intervals for parameter estimates via bootstrapping (1000 iterations)
- Identify impending plateaus when recovery acceleration (second derivative) approaches zero while maintaining intervention intensity
Clinical Implementation Workflow:
- Baseline assessment establishes
Bparameter - Initial 2-3 weeks of intervention data used to estimate
R,α, and initialλ - Weekly updates to model parameters with new assessment data
- Alert triggered when projected recovery gain falls below 5% for upcoming month
- Intervention modification when plateau parameters identified [63]
- Baseline assessment establishes
Experimental Protocols for Plateau Mechanism Investigation
Preclinical Models of Recovery Plateau and Intervention
Animal models provide controlled conditions for investigating specific mechanisms of recovery plateaus and testing intervention strategies:
Photothrombotic Stroke Model for Motor Recovery Studies:
- Animal Preparation: Adult Sprague-Dawley rats (250-300g) or C57BL/6 mice (20-25g) anesthetized with isoflurane (4% induction, 1.5-2% maintenance in 70% N₂O/30% O₂). Maintain body temperature at 37°C using feedback-controlled heating pad.
- Lesion Induction: Inject Rose Bengal dye (20mg/kg intraperitoneal) followed after 5 minutes by focal illumination of skull surface over forelimb motor cortex (2mm anterior, 2.2mm lateral to bregma) with cold white light (150W) for 15 minutes through 3mm diameter aperture.
- Postoperative Care: Administer saline (1mL subcutaneous) for hydration and buprenorphine (0.05mg/kg) for analgesia. Monitor animals until fully recovered from anesthesia.
- Rehabilitation Protocol: Initiate constraint-induced movement therapy 7 days post-lesion by placing restrictive cast on unaffected limb for 6 hours daily, 5 days/week. During restraint period, animals perform skilled reaching tasks (single-pellet retrieval) and walking tasks (ladder rung walking) with affected limb.
- Plateau Induction: Continue intensive training for 4-6 weeks until performance stabilizes at <5% improvement over 2-week period, establishing preclinical plateau model [60].
Environmental Enrichment Neuroplasticity Protocol:
- Enriched Environment Setup: Large cage (60×50×40cm) containing various objects of different textures, sizes, and complexities. Include running wheels, tunnels, nesting material, and manipulable objects. Change object configuration 2-3 times weekly to maintain novelty.
- Control Conditions: Standard housing in typical laboratory cages with same bedding material but without additional enrichment objects.
- Exposure Protocol: Place animals in enriched environment for 6 hours daily, 5 days/week for intervention duration. Control animals remain in standard housing with equivalent human handling.
- Assessment Timeline: Conduct behavioral testing (motor function, cognitive performance) at baseline, weekly during intervention, and at protocol conclusion. Perform histological analysis (dendritic branching, synaptogenesis, neurogenesis) upon sacrifice [3] [64].
Human Neuroplasticity Training and Assessment Protocols
Constraint-Induced Movement Therapy (CIMT) Protocol:
- Candidate Selection: Upper extremity hemiparesis with minimum 20° wrist extension and 10° finger extension. Minimum Motor Criteria, but substantial real-world limb non-use.
- Restraint Application: Place mitt or sling on less-affected arm for up to 90% of waking hours (approximately 14 hours/day) during 2-week intervention period.
- Shaping Tasks: Structured practice involving 10-15 tasks of increasing difficulty with gradually changing performance criteria. Tasks include reaching, grasping, manipulation, and release actions. Provide immediate feedback and reinforcement.
- Transfer Package: Strategies to facilitate transfer of clinical gains to real-world settings, including behavioral contracts, home diaries, problem-solving discussions, and home practice assignments.
- Measurement: Administer Wolf Motor Function Test, Motor Activity Log, and Actual Amount of Use Test at baseline, post-treatment, and 4-month follow-up to assess plateau breakthrough [61].
Non-Invasive Brain Stimulation with Motor Training:
- Stimulation Parameters: Apply transcranial direct current stimulation (tDCS) using 1-2mA current for 20 minutes via 5×7cm electrodes. Position anode over ipsilesional primary motor cortex (C3/C4 according to 10-20 EEG system) and cathode over contralateral supraorbital region.
- Combined Therapy: Initiate physical or occupational therapy immediately following stimulation during the putative window of enhanced cortical excitability. Focus on task-specific practice with high repetition (300-400 movements/session).
- Dosing Regimen: Administer stimulation 3-5 times/week for 4-6 weeks. Include sham-controlled conditions in research protocols with identical setup but only 30 seconds of stimulation at beginning and end.
- Outcome Measures: Use transcranial magnetic stimulation to map cortical representation of target muscles, Jebsen-Taylor Hand Function Test for functional assessment, and fMRI for network activation patterns [61].
Signaling Pathways in Neuroplasticity and Plateau Mechanisms
Understanding the molecular signaling pathways that govern neuroplasticity provides targets for interventions aimed at breaking through recovery plateaus in chronic conditions.
Key Molecular Pathways in Plateau Persistence
The signaling architecture illustrated above represents validated targets for therapeutic intervention to reactivate plasticity beyond recovery plateaus:
BDNF-TrkB Signaling Cascade: This pathway demonstrates activity-dependent potentiation that frequently diminishes during plateau phases. Downstream effectors include:
- PI3K/Akt Pathway: Promotes neuronal survival and synaptic strengthening through regulation of protein synthesis and metabolic support
- MEK/ERK Pathway: Regulates gene expression through transcription factor phosphorylation including CREB, driving long-term structural adaptations
- PLCγ Pathway: Modulates synaptic function through IP3-mediated calcium release and PKC activation [62] [61]
Growth Inhibitory Signaling: Chronic phases show persistent expression of myelin-associated inhibitors that maintain plateau states:
- Nogo-A Signaling: Through NgR1/p75/LINGO-1 or PirB receptors activates RhoA/ROCK pathway, leading to actin cytoskeleton reorganization and growth cone collapse
- Semaphorin Signaling: Class 3 and 4 semaphorins contribute to inhibitory signaling through plexin and neuropilin receptors
- Wnt Signaling: Developmental pathways re-emerge in chronic phases, potentially limiting structural plasticity [62]
Interventional Targets: Pharmacological and activity-based approaches target these pathways:
- BDNF Potentiation: Aerobic exercise, specific motor skill training, and pharmacological TrkB agonists enhance this pathway
- Growth Inhibition Blockade: Anti-Nogo-A antibodies, ROCK inhibitors, and chondroitinase ABC to modify inhibitory extracellular matrix
- Neuromodulation: tDCS and TMS may modulate these molecular pathways through membrane potential changes and network activity alterations [3] [61]
Research Reagent Solutions for Neuroplasticity Studies
Table 3. Essential Research Reagents for Investigating Recovery Plateaus
| Reagent Category | Specific Examples | Research Application | Experimental Considerations |
|---|---|---|---|
| Cell Division & Lineage Tracing Markers | BrdU, 3H-thymidine, 14C, EdU | Identification of newborn cells and tracking of cell fate | Timing critical for specific developmental stages; Dose optimization required for different species [62] |
| Immunohistochemistry Antibodies | Doublecortin (DCX), NeuN, GFAP, Iba1, PSD-95, Synapsin I | Identification of specific cell types and synaptic structures | Antigen retrieval methods vary by fixation protocol; Multiple labeling requires host species compatibility [62] |
| Activity-Dependent Reporters | c-Fos, Arc, pERK, pCREB | Mapping neuronal activation patterns post-stimulation | Timecourse critical (early-immediate vs. late genes); Combination with behavioral paradigms essential [64] |
| Viral Vector Tools | AAV-Cre, AAV-DREADDs, Channelrhodopsin, Retrograde tracers | Circuit mapping and targeted manipulation | Serotype selection affects tropism and spread; Promoter choice determines cell-type specificity [60] |
| Growth Factors & Modulators | Recombinant BDNF, NT-3, Nogo-A inhibitors, Chondroitinase ABC | Testing therapeutic interventions for plasticity enhancement | Delivery method critical (osmotic pumps, bolus injection, engineered cells); Stability varies by formulation [61] |
| Calcium Indicators | GCaMP, Oregon Green BAPTA, Fura-2 | Real-time monitoring of neuronal activity in vitro and in vivo | Genetically encoded vs. synthetic tradeoffs; Photostability considerations for longitudinal studies [3] |
Strategic Intervention Approaches for Plateau Breakthrough
Principles of Targeted Intervention Timing
Breaking through recovery plateaus requires strategic timing and combination of interventions based on individual neuroplasticity states:
Pre-plateau Intervention: Implement intensive, task-specific training during the initial recovery phase (first 3 months) to maximize the natural surge in growth factors and permissive environment for plasticity. This "window of opportunity" establishes stronger initial foundations that may elevate the eventual plateau level [61].
Plateau Phase Intervention: When progress stabilizes despite continued conventional therapy, introduce novelty and increased challenge to reactivate plasticity mechanisms. This includes complex skill acquisition, dual-task training, or varying environmental contexts to engage broader neural networks [3] [64].
Combination Therapy Approaches: Pair behavioral interventions with biological or technological approaches to create synergistic effects:
- Physical Activity + Cognitive Engagement: Aerobic exercise increases BDNF and other growth factors, creating a molecular environment more responsive to subsequent skill learning [61].
- Non-Invasive Stimulation + Task-Specific Training: tDCS or TMS applied immediately before motor training can enhance use-dependent plasticity through modulation of cortical excitability and neurotransmitter systems [61].
- Pharmacological + Behavioral Pairing: Medications that enhance neurotransmitter systems (dopaminergic, noradrenergic, cholinergic) paired with appropriately timed rehabilitation can amplify plastic responses [62].
Environmental and Behavioral Optimization
The environmental context significantly influences neuroplastic potential, particularly during plateau phases where conventional approaches show diminished returns:
Environmental Enrichment Protocols: Implement complex housing or therapy environments with varied physical, cognitive, and social stimuli. Naturalistic environments appear particularly effective, with studies showing rats housed with natural stimuli (dirt, rocks, sticks) showed approximately 50% more interaction with environmental objects compared to those with artificial enrichment [3].
Affordance-Rich Environments: Design environments that invite active exploration and interaction based on Gibson's theory of affordances. These environments expand behavioral repertoires by providing opportunities for diverse actions and problem-solving, engaging broader neural networks [3] [64].
Stress Optimization: Moderate, controllable stress can enhance plasticity through noradrenergic activation and optimal cortisol/DHEA ratios, while chronic uncontrollable stress inhibits recovery. Special-forces military training research shows optimal DHEA levels correlate with superior performance in extreme challenge tasks, suggesting hormonal milieu optimization strategies [3].
Recovery plateaus in chronic conditions represent dynamic neurobiological states rather than fixed endpoints in the rehabilitation process. The integration of advanced assessment technologies, computational modeling of recovery trajectories, and targeted multi-modal interventions offers promising approaches to reactivate neuroplastic potential beyond apparent stabilization. Future research directions should prioritize:
- Biomarker Development: Identifying reliable molecular, imaging, and neurophysiological biomarkers that predict impending plateaus and responsivity to specific interventions
- Personalized Timing Algorithms: Developing individual-specific models to optimize intervention timing based on unique recovery trajectories and plastic potential
- Multi-system Interventions: Designing integrated approaches that simultaneously target molecular, circuit, behavioral, and environmental factors
- Translation of Preclinical Findings: Accelerating the application of identified mechanisms from animal models to human therapeutic development
By reconceptualizing recovery plateaus as modifiable neurobiological states rather than absolute recovery limits, researchers and clinicians can develop more effective strategies to optimize functional outcomes throughout the chronic phase of neurological conditions.
Counteracting Maladaptive Plasticity in Stress, Addiction, and Chronic Pain
Neuroplasticity, the nervous system's capacity to change its structure and function in response to experience, serves as the fundamental biological substrate for learning, memory, and behavioral adaptation [65]. While this remarkable adaptability enables optimal performance in changing environments, it possesses a crucial duality—the very same mechanisms that facilitate adaptive learning can, under specific conditions, become drivers of pathology [3]. Maladaptive plasticity refers to persistent, detrimental changes in neural circuits that reinforce dysfunctional states rather than promote healthy adaptation. In conditions such as chronic stress, substance addiction, and persistent pain, the brain undergoes a series of neurobiological alterations that strengthen negative circuits, creating self-perpetuating cycles of illness [66] [67]. Understanding these shared mechanisms provides a critical foundation for developing targeted interventions that can redirect plasticity toward adaptive outcomes, a core objective in contemporary behavioral adaptation and optimal performance research.
This whitepaper examines the overlapping neurobiological mechanisms underlying maladaptive plasticity across stress, addiction, and chronic pain pathologies. We synthesize current research on interventions capable of countering these detrimental changes, with particular emphasis on transdiagnostic approaches that target shared pathways. For researchers and drug development professionals, we present structured experimental data, detailed methodologies, and essential research tools to advance this promising frontier in clinical neuroscience.
Neurobiological Foundations of Maladaptation
Shared Neural Circuits and Mechanisms
Maladaptive processes in stress, addiction, and chronic pain converge on several key brain regions and molecular pathways. The prefrontal cortex (PFC), a hub for executive control and emotional regulation, exhibits significant structural and functional impairment across all three conditions [68]. Chronic stress exposure induces dendritic atrophy and spine loss in the medial PFC, particularly affecting pyramidal neurons in layers II/III and V/VI [68]. These structural changes correlate with functional deficits in cognitive control, which similarly manifest in addiction (as impaired inhibitory control) and chronic pain (as catastrophizing and attention biases) [66] [68] [67].
The overlap between chronic pain and addiction is particularly striking at the neurocircuitry level. Both conditions involve dysregulation of the brain's reward pathways, including the nucleus accumbens and ventral tegmental area, leading to shared symptomatology such as anhedonia, compulsive seeking (of pain relief or drugs), and stress dysregulation [67]. Neurobiological models attribute these shared features to reward deficiency, impaired inhibitory control, incentive sensitization, aberrant learning, and anti-reward allostatic neuroadaptations [67].
The following diagram illustrates the core neurobiological mechanisms common to these conditions:
Figure 1: Shared Neurobiological Mechanisms of Maladaptive Plasticity. Key brain regions and systems commonly affected across chronic stress, addiction, and chronic pain conditions, illustrating the transdiagnostic nature of these adaptations. NAcc = nucleus accumbens; VTA = ventral tegmental area; HPA = hypothalamic-pituitary-adrenal.
The Maladaptive Cycle of Pain and Stress
Chronic pain and stress exhibit particularly strong mutually reinforcing dynamics, creating a "vicious cycle" that perpetuates both conditions [66]. Pain activates physiological stress responses, while stress modulates pain perception through overlapping physiological, cognitive, and behavioral mechanisms [66]. This cycle is driven by three primary overlapping mechanisms: (1) maladaptive neuroplasticity, neuroendocrine dysfunction, and chronic inflammation; (2) cognitive-behavioral patterns including fear avoidance, hypervigilance, and catastrophizing; and (3) social, lifestyle, and environmental influences such as socioeconomic status and lack of social support [66]. This complex interplay results in allostatic load—the cumulative "wear-and-tear" on physiological systems that occurs with repeated attempts to adapt to stressors [66].
Quantitative Evidence: Epidemiological and Clinical Data
The high co-occurrence of conditions driven by maladaptive plasticity underscores their shared neurobiological foundations. Recent epidemiological data reveals the striking prevalence of these overlapping disorders, particularly highlighting the relationship between chronic pain and psychological symptoms.
Table 1: Population Prevalence of Co-Occurring Chronic Pain and Anxiety/Depression Symptoms in US Adults (2019 NHIS Data, n=31,997) [69]
| Population Group | Prevalence | Estimated US Adults | Key Characteristics |
|---|---|---|---|
| US Adults with Co-Occurring Conditions | 4.9% | ~12 million | Experience both chronic pain and anxiety/depression symptoms |
| Chronic Pain Subgroup with A/D | 23.9% | - | Nearly 1 in 4 adults with chronic pain has clinically significant anxiety/depression |
| A/D Subgroup with Chronic Pain | 55.6% | - | Majority of adults with anxiety/depression experience co-occurring chronic pain |
| General Population without Chronic Pain | 4.9% | - | Baseline prevalence of anxiety/depression without chronic pain |
Table 2: Functional Limitations Associated with Co-Occurring Chronic Pain and Anxiety/Depression [69]
| Functional Domain | Co-Occurring Conditions | Chronic Pain Alone | A/D Symptoms Alone |
|---|---|---|---|
| Work Limited by Health | 69.4% | - | - |
| Difficulty Doing Errands Alone | 43.7% | - | - |
| Difficulty in Social Activities | 55.7% | - | - |
| Comparative Functional Impact | Highest | Intermediate | Lower |
These data highlight the profound functional consequences of co-occurring conditions and emphasize the need for integrated treatment approaches that target shared mechanisms rather than isolated symptoms.
Intervention Strategies: Redirecting Plasticity Toward Adaptation
Non-Invasive Neuromodulation Approaches
Non-invasive neuromodulation techniques represent a promising frontier for directly modulating maladaptive neural plasticity. These approaches target specific brain regions to restore normal excitability and connectivity patterns in dysfunctional circuits.
Table 3: Non-Invasive Neuromodulation Techniques for Counteracting Maladaptive Plasticity [70] [71]
| Technique | Mechanism of Action | Target Brain Regions | Evidence in Conditions |
|---|---|---|---|
| rTMS (repetitive Transcranial Magnetic Stimulation) | Modulates cortical excitability through electromagnetic induction; LF-rTMS decreases while HF-rTMS increases excitability | DLPFC, M1, ACC | Chronic pain, depression, addiction |
| tDCS (transcranial Direct Current Stimulation) | Weak direct current alters neuronal membrane polarization; anodal increases while cathodal decreases excitability | DLPFC, M1, OFC | Neuropathic pain, craving reduction, cognitive enhancement |
| tACS (transcranial Alternating Current Stimulation) | Entrains endogenous neural oscillations to specific frequencies | Prefrontal-thalamic circuits | Memory consolidation, cognitive control |
| tUS (transcranial Ultrasound Stimulation) | Low-intensity focused ultrasound mechanically modulates neural membranes | Deep brain structures (e.g., insula, thalamus) | Preclinical pain models, mood regulation |
Experimental Protocol: Standard rTMS Application for Chronic Pain [71]
- Patient Assessment: Confirm diagnosis of chronic neuropathic pain using IASP diagnostic criteria.
- Target Localization: Identify the primary motor cortex (M1) hand area using the 10-20 EEG system (C3/C4 position) or neuronavigation.
- Motor Threshold Determination: Establish resting motor threshold (rMT) by applying single pulses to M1 and determining the minimum intensity that elicits a visible twitch in the contralateral abductor pollicis brevis muscle in 50% of trials.
- Stimulation Parameters:
- Frequency: 10 Hz
- Intensity: 80-90% of rMT
- Trains: 50 pulses per train
- Inter-train interval: 20-30 seconds
- Total pulses per session: 1000-2000
- Session frequency: 5 sessions per week for 2-6 weeks
- Outcome Assessment: Utilize standardized pain scales (VAS, NPSI) pre-, post-, and at follow-up intervals (1, 3, 6 months).
Pharmacological and Lifestyle Interventions
Pharmacological approaches aim to restore neurochemical balance and create permissive conditions for adaptive plasticity. Meanwhile, lifestyle interventions leverage the brain's inherent capacity for change through natural environmental modifications.
Table 4: Pharmacological and Lifestyle Interventions to Promote Adaptive Plasticity [70] [68]
| Intervention Category | Specific Approach | Proposed Mechanism | Evidence Level |
|---|---|---|---|
| Pharmacological | Fluoxetine (SSRI) | Enhances plasticity in adult visual cortex; promotes motor recovery when paired with physiotherapy | Preclinical/Clinical |
| Pharmacological | D-Cycloserine (NMDA partial agonist) | Facilitates extinction learning in exposure-based therapies | Clinical trials |
| Dietary/Lifestyle | Intermittent Fasting (16-24 hour periods) | Reduces inflammation, oxidative stress; increases synaptic plasticity and neurogenesis | Preclinical/Early Clinical |
| Dietary/Lifestyle | Glucose Supplementation | Enhances learning and memory processes; provides energy substrate for neural plasticity | Controlled studies |
| Environmental | Enriched Environments | Increases dendritic branching, neurogenesis; enhances cognitive reserve | Strong Preclinical |
Experimental Protocol: Intermittent Fasting Regimen for Plasticity Enhancement [70]
- Participant Screening: Exclude children, pregnant women, individuals with diabetes, eating disorders, or history of myocardial infarction.
- Protocol Options:
- 16-hour daily fast: Restrict all caloric intake to an 8-hour window each day (e.g., 12:00-20:00)
- 24-hour twice-weekly fast: Complete water-only fast for 24 hours on two non-consecutive days per week
- Hydration Protocol: Encourage adequate water intake during fasting periods (35-40 mL/kg/day).
- Monitoring Parameters:
- Weight and body composition (weekly)
- Vital signs (daily during initial adaptation)
- Subjective reports of energy, headaches, hunger
- Cognitive performance measures (pre/post intervention)
- Intervention Duration: Minimum 4 weeks to assess initial adaptation; 12 weeks for full plasticity assessment.
The following diagram illustrates how these diverse interventions target specific components of the maladaptive plasticity cycle:
Figure 2: Intervention Strategies Targeting Maladaptive Plasticity. Multiple approaches can redirect plasticity toward adaptive outcomes through distinct but complementary neurobiological mechanisms.
Transdiagnostic Psychological Approaches
Cognitive-behavioral therapy (CBT) and other psychological interventions directly target maladaptive learning processes that maintain pathological states. A transdiagnostic approach addressing shared mechanisms across chronic pain, depression, and anxiety has demonstrated particular efficacy [65]. This approach explicitly targets critical shared mechanisms such as catastrophizing, kinesiophobia, emotional dysregulation, and avoidance behaviors [65]. Interdisciplinary pain management programs that integrate rehabilitation physicians, psychologists, physiotherapists, and occupational therapists have shown success in improving cognitive, emotional, and physical function outcomes by simultaneously addressing these maladaptive patterns [65].
Notably, CBT has been shown to not only improve pain coping but also reverse central sensitization, with decreased pain catastrophizing significantly associated with this reversal process [65]. Neuroimaging evidence confirms that CBT can increase prefrontal cortex gray matter in patients with chronic pain, demonstrating the direct impact of psychological interventions on brain structure [65].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 5: Key Research Reagent Solutions for Neuroplasticity Research
| Reagent/Method | Primary Application | Function in Research | Example Use Cases |
|---|---|---|---|
| D-cycloserine | NMDA receptor partial agonist | Facilitates extinction learning and synaptic plasticity | Enhancing exposure therapy efficacy in anxiety disorders |
| Fluoxetine (SSRI) | Selective serotonin reuptake inhibitor | Promotes neuroplasticity in adult cortex | Improving motor recovery after stroke when paired with physiotherapy |
| PHQ-8 & GAD-7 | Validated clinical scales | Screening and assessment of depression and anxiety symptoms | Population surveillance of co-occurring pain and A/D symptoms |
| IASP Diagnostic Criteria | Standardized pain classification | Consistent phenotyping of chronic pain populations | Ensuring sample homogeneity in clinical trials |
| Neuronavigation Systems | Brain stimulation targeting | Precision localization of rTMS/tDCS targets | Optimizing non-invasive neuromodulation protocols |
| Dendritic Spine Morphometry | Structural plasticity analysis | Quantifying changes in synaptic architecture | Assessing interventional effects on neuronal connectivity |
The converging evidence across disciplines reveals that maladaptive neuroplasticity represents a common pathway through which stress, addiction, and chronic pain become entrenched and self-perpetuating. The shared neurobiological mechanisms underlying these conditions present both a challenge and an opportunity—while they contribute to diagnostic complexity and comorbidity, they also offer promising transdiagnostic targets for intervention.
Future research directions should focus on personalized approaches that match specific interventions to individual neurobiological signatures. Emerging evidence suggests that baseline brain states may determine suitability for different interventions, with some individuals responding better to hypnosis and others to mindfulness meditation for pain management [65]. The ideal future of treatment lies in identifying unique neurological signatures of an individual's condition and using algorithms to match this signature to the intervention most likely to be beneficial [65].
For drug development professionals, this landscape suggests promising avenues for compounds that directly target plasticity mechanisms rather than merely symptom management. The integration of neuromodulation technologies with pharmacological approaches and psychological interventions represents a particularly promising frontier. By creating optimal conditions for adaptive plasticity through combined approaches, we may ultimately disrupt the vicious cycles of maladaptation and restore the brain's inherent capacity for healthy adaptation and optimal performance.
Neuroplasticity, defined as the ability of the nervous system to change its activity in response to intrinsic or extrinsic stimuli by reorganizing its structure, functions, or connections, provides the fundamental biological substrate for behavioral adaptation and optimal performance [1]. In the context of a broader thesis on the role of neuroplasticity in behavioral adaptation, this technical guide examines the precise parameter optimization required to harness these adaptive capacities effectively. The functional outcomes of neuroplastic processes can be beneficial (restoration of function after injury), neutral, or negative, with specific parameter combinations determining the direction and magnitude of these effects [1]. For researchers and drug development professionals, understanding how to manipulate intensity, timing, and personalization parameters represents a critical pathway for enhancing cognitive reserve, neural reserve, and ultimately, optimal performance outcomes across clinical and non-clinical populations [3].
The following sections provide a comprehensive analysis of evidence-based protocols for parameter optimization, with structured quantitative data, experimental methodologies, and visualization tools to support research design and therapeutic development. By integrating foundational mechanisms with emerging biomarkers and technologies, this whitepaper establishes a rigorous framework for intervention design rooted in the temporal, intensity, and individual-specific dimensions of neuroplastic change.
Intensity: Calibrating the Neuroplastic Challenge
Intervention intensity must be calibrated to exceed the threshold required to trigger neuroplastic mechanisms while avoiding maladaptive stress responses that can impede optimal outcomes. The relationship between intensity and neuroplastic response follows a non-linear function, with insufficient challenge failing to elicit changes and excessive intensity potentially activating counterproductive stress pathways [3].
Quantitative Parameters for Intensity Optimization
Table 1: Evidence-Based Intensity Parameters for Neuroplastic Interventions
| Intervention Domain | Low Intensity | Moderate Intensity | High Intensity | Neuroplastic Correlates |
|---|---|---|---|---|
| Aerobic Exercise [3] [72] | 30-40% HRR, 2-3 days/week | 50-65% HRR, 4-5 days/week | 70-85% HRR, 5-6 days/week | ↑BDNF, ↑angiogenesis, ↑synaptogenesis |
| Cognitive Training [73] | Familiar tasks, 30 min, 2x/week | Novel challenges, 60 min, 3x/week | Complex integration, 90+ min, 4-5x/week | ↑dendritic arborization, ↑LTP, network efficiency |
| Motor Skill Acquisition [1] [73] | Simple repetitions, 45 min sessions | Progressive complexity, 60-75 min sessions | Variable contexts, 90+ min sessions | Cortical reorganization, ↑motor map representation |
| Environmental Enrichment [3] | Limited novel objects, minimal social interaction | Rotating novel objects, consistent social interaction | Complex habitat, varied social partners | ↑neurogenesis, ↑synaptic density, ↑cognitive reserve |
HRR = Heart Rate Reserve; BDNF = Brain-Derived Neurotrophic Factor; LTP = Long-Term Potentiation
Experimental Protocol: Intensity Progression for Motor Recovery
For researchers investigating post-stroke motor recovery, the following protocol exemplifies intensity progression parameters validated in rehabilitation settings [1] [73]:
- Weeks 1-2: Moderate-intensity parameters with 60-minute sessions of task-specific training, 5 days/week, focusing on proper movement patterns with 300-400 repetitions per session.
- Weeks 3-6: High-intensity parameters with 90-minute sessions, 5 days/week, incorporating variable practice conditions and complex skill integration with 500-700 repetitions per session.
- Progression Criteria: Increase intensity when movement quality reaches >80% accuracy and patient fatigue remains manageable (RPE <6/10).
- Biomarker Monitoring: Serum BDNF, GDF-10, and endostatin levels at baseline, 2, 4, and 6 weeks to correlate intensity with molecular markers of neuroplasticity [74].
The critical mechanism underlying intensity effects involves the relationship between challenge level and synaptic strengthening. As summarized by Hebb's axiom that "neurons that fire together, wire together," repetition alone is insufficient—the task must be sufficiently challenging to trigger synaptic modulation [73]. Activities that are difficult and challenging elicit changes in the neural network, whereas familiar, automatic, or easy tasks do not provide adequate stimulus for plasticity [73].
Timing: Temporal Dynamics of Intervention Efficacy
The temporal parameters of interventions—including onset, duration, frequency, and interval structure—profoundly influence neuroplastic outcomes. Research indicates that the brain undergoes distinct phases of reorganization after injury or challenge initiation, creating critical periods during which specific interventions show enhanced efficacy [1].
Phasic Neuroplasticity: Post-Injury Timeline
Table 2: Temporal Windows for Targeted Intervention Following Neural Insult
| Time Post-Injury | Primary Neural Events | Recommended Intervention Focus | Rationale |
|---|---|---|---|
| First 48 hours [1] | Cell death, loss of cortical pathways, activation of secondary networks | Very gentle stimulation, environmental modification | Prevents neural shock, supports endogenous protective mechanisms |
| Following Weeks [1] | Shift from inhibitory to excitatory cortical pathways, synaptic plasticity, new connection formation | Intensive, repetitive, task-specific training | Capitalizes on heightened plasticity state during synaptic reorganization |
| Weeks to Months [1] | Axonal sprouting, continued reorganization around damaged areas | Complex skill integration, variable context training | Supports consolidation of new circuits and connection refinement |
Biomarker Timing in Experimental Protocols
Cutting-edge research has identified temporal biomarkers that can guide intervention timing in both clinical and research settings. In a recent prospective, multicenter study of stroke rehabilitation, specific molecular markers demonstrated time-dependent relationships with functional outcomes [74]:
- Baseline Assessment: Blood collection for endostatin, GDF-10, uPA, and uPAR levels before rehabilitation initiation.
- Acute Phase (0-1 month): Serial biomarker measurement at 2-week intervals; decreased endostatin or increased GDF-10 during this period predicted greater sensorimotor improvements.
- Subacute Phase (1-3 months): Monthly monitoring; GDF-10 and uPAR levels inversely correlated with functional scores.
- Consolidation Phase (3-6 months): Quarterly assessment; biomarker stabilization indicated treatment response plateau.
The following workflow diagram illustrates the experimental protocol for timing biomarker assessment in neuroplasticity research:
Advanced neuroimaging research further reveals that neuroplasticity involves not just spatial but temporal modulation of neural activity. Ultrafast fMRI (ufMRI) studies demonstrate that induced neuroplasticity modulates temporal properties in entire neural pathways, suggesting timing parameters should address both intervention scheduling and the temporal dynamics of neural processing [75].
Personalization: Individualized Biomarkers and Signatures
The third critical parameter for optimizing neuroplastic interventions involves personalization based on individual genetic, biological, and experiential factors. Research indicates substantial individual variability in neuroplastic responses, necessitating customized approaches rather than one-size-fits-all protocols [3].
Molecular Biomarkers for Personalized Protocols
The emergence of blood-based biomarkers enables unprecedented personalization of neuroplastic interventions. Recent research has identified several molecules with significant predictive value for rehabilitation outcomes [74]:
- GDF-10 (Growth and Differentiation Factor 10): Higher baseline values associated with unfavorable sensorimotor scores during follow-up; increased levels during first month of rehabilitation predict greater functional improvements.
- Endostatin: Significantly increased at baseline after stroke; decreased levels during first month of rehabilitation correlate with sensorimotor improvements.
- uPAR (Urokinase-Type Plasminogen Activator Receptor): Highest baseline values related to unfavorable Fugl-Meyer Assessment and Medical Research Council scores throughout follow-up.
These biomarkers enable researchers and clinicians to stratify participants according to likely treatment response and adjust intervention parameters accordingly. For example, individuals with high baseline uPAR might receive more intensive or longer-duration interventions to overcome predicted resistance to standard protocols.
Environmental and Contextual Personalization
Beyond molecular signatures, optimal intervention personalization incorporates environmental and experiential factors. Research in animal models demonstrates that environmental complexity significantly influences neuroplastic outcomes, but these effects are modulated by individual behavioral interactions with the environment [3]. Notably, the relationship between environments and neuroplasticity responses is far from simplistic—with behavioral interactions, as well as exposure to novelty, playing critical roles in both adaptive and maladaptive plasticity [3].
The following diagram illustrates key signaling pathways involved in neuroplasticity that serve as targets for personalized interventions:
Individual differences in stress resilience further modulate neuroplastic responses. Research with special-forces military trainees revealed that plasma dehydroepiandrosterone (DHEA) positively correlates with superior performance in extreme challenge tasks, highlighting the importance of the neuroendocrine environment in determining optimal intensity parameters [3].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Neuroplasticity Intervention Studies
| Reagent/Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Molecular Biomarkers [74] | GDF-10, Endostatin, uPAR, uPA ELISA Kits | Patient stratification, treatment response monitoring | Quantify neuroplasticity-associated molecules in serum/plasma to personalize interventions |
| Neuroimaging Tools [75] | Ultrafast fMRI (ufMRI) | Mapping temporal neural dynamics | Detect neuroplasticity-induced timing modulations in global brain circuits |
| Synaptic Plasticity Assays [1] | Long-Term Potentiation (LTP) electrophysiology | Measuring synaptic strength changes | Quantify cellular correlate of learning and memory in ex vivo preparations |
| Genetic Tools [32] | Cell-type specific promoters, Cre-lox systems | Targeted manipulation of neural circuits | Enable precise intervention in specific cell populations to test causal mechanisms |
| Behavioral Assessment [74] | Fugl-Meyer Assessment, Barthel Index, CAHAI | Functional outcome measurement | Standardized quantification of sensorimotor recovery and daily living function |
| Environmental Enrichment [3] | Naturalistic habitats, novel object rotations | Environmental intervention studies | Standardize complex environments to study experience-dependent plasticity |
Integrated Experimental Protocol: Combining Parameters for Optimal Outcomes
This section provides a detailed methodology for a comprehensive research protocol integrating intensity, timing, and personalization parameters, suitable for implementation in both preclinical and clinical settings.
Phase 1: Biomarker Profiling and Stratification (Week 0)
- Participant Characterization: Comprehensive assessment including molecular profiling (GDF-10, endostatin, uPAR), functional baseline measures (Fugl-Meyer Assessment, Barthel Index), and neuroimaging (ufMRI where available).
- Stratification: Assign participants to intervention tracks based on biomarker profiles—high GDF-10/uPAR levels may indicate need for modified intensity progression.
Phase 2: Intensity-Modulated Intervention (Weeks 1-8)
- Progressive Intensity Algorithm: Begin with moderate intensity (60-minute sessions, 4 days/week) with progression criteria based on both performance metrics (80% movement accuracy) and biomarker response (favorable GDF-10 trends).
- Control Parameters: Monitor stress biomarkers (cortisol, DHEA) to ensure intensity remains in optimal zone—avoiding both insufficient challenge and excessive stress response.
Phase 3: Temporal Optimization (Weeks 4-12)
- Critical Period Capitalization: Increase session frequency to 5 days/week during weeks 4-6 to align with peak synaptic reorganization phase.
- Complexity Integration: Introduce variable context training and complex skill integration during weeks 7-12 to support circuit consolidation.
Phase 4: Long-Term Consolidation (Months 4-6)
- Maintenance Parameters: Reduce frequency to 3 days/week while maintaining challenge level through progressive task difficulty.
- Outcome Assessment: Comprehensive functional, biomarker, and neuroimaging evaluation at month 6 to quantify intervention efficacy.
This integrated approach exemplifies the synergy achievable through careful parameter optimization, providing a template for researchers designing neuroplasticity-based interventions across diverse populations and applications.
The optimization of intensity, timing, and personalization parameters represents the frontier of neuroplasticity research with profound implications for both basic science and clinical application. By integrating quantitative intensity parameters, temporal dynamics of neural reorganization, and individualized biomarker profiles, researchers can design interventions that precisely target neuroplastic mechanisms for optimal behavioral adaptation. The tools and protocols outlined in this technical guide provide a foundation for advancing this field, with particular relevance for drug development professionals working on neurological and psychiatric disorders where harnessing neuroplasticity is increasingly central to therapeutic success.
As the field evolves, emerging technologies—including ultrafast fMRI for mapping temporal dynamics [75], advanced molecular biomarkers for personalization [74], and sophisticated behavioral paradigms for intensity calibration—will further enhance our ability to precisely modulate the brain's remarkable capacity for change. Through continued refinement of these parameters within the context of a comprehensive understanding of neuroplasticity mechanisms, researchers move closer to the goal of truly optimized interventions for enhancing human performance and resilience across the lifespan.
Neuroplasticity, the nervous system's capacity to adapt its structure and function in response to experience, forms the foundational mechanism for behavioral adaptation and optimal performance. This dynamic process, which involves synaptic remodeling, neurogenesis, and large-scale network reorganization, enables the brain to maintain cognitive agility throughout the lifespan [25] [1]. While neuroplasticity mechanisms operate continuously, their efficacy and direction are profoundly influenced by modifiable lifestyle factors. This whitepaper synthesizes current evidence from human and preclinical studies to elucidate how sleep, stress management, and environmental exposures modulate neuroplasticity at molecular, systems, and behavioral levels, providing researchers and drug development professionals with a mechanistic framework for developing plasticity-targeted interventions.
The clinical and functional relevance of neuroplasticity extends across diverse domains. It supports cognitive flexibility, enabling task switching and problem-solving in dynamic environments [25]. It underlies skill acquisition, as demonstrated by structural changes in the hippocampus of London taxi drivers and musicians [25]. Critically, neuroplasticity enables functional recovery after neural injury, such as when undamaged brain regions assume functions from damaged areas following stroke [25] [1]. However, neuroplasticity operates as a double-edged sword—when maladaptive, it can reinforce pathological states such as chronic stress responses or addiction [4]. Understanding how lifestyle factors influence this balance provides crucial insights for optimizing brain health and developing novel therapeutic approaches.
Sleep and Neuroplasticity
Molecular and Cellular Mechanisms
Sleep facilitates neuroplasticity through multiple synergistic mechanisms operating at molecular and circuit levels. During sleep, the brain engages in memory consolidation, a process whereby labile short-term memories are stabilized into long-term storage [76]. This process involves the reactivation of hippocampal-neocortical circuits, gradually strengthening recently formed memory traces [76]. Simultaneously, sleep enables synaptic homeostasis, renormalizing synaptic strength that has been potentiated during waking experiences, thereby maintaining neural circuits within their dynamic operating range [77].
At the molecular level, the medial prefrontal cortex (mPFC) molecular clock plays a pivotal role in mediating sleep-dependent plasticity. Core clock genes, including Bmal1, Per, and Cry, oscillate in expression across sleep-wake cycles and regulate markers of glutamatergic plasticity such as Homer1a and synaptic AMPAR expression [77]. Disruption of this molecular clock in CaMK2a-expressing excitatory neurons abolishes both the behavioral and molecular (Homer1a) responses to sleep deprivation, demonstrating its essential role in sleep homeostasis [77]. Sleep deprivation experiments reveal that these molecular oscillations are crucial for maintaining optimal synaptic function and emotional regulation.
Table 1: Molecular Markers of Sleep-Related Neuroplasticity
| Marker | Function | Response to Sleep Deprivation | Research Significance |
|---|---|---|---|
| Homer1a | Synaptic protein regulating glutamatergic signaling | Blunted induction after SD in stress-susceptible mice [77] | Key mediator of SD's antidepressant effects |
| AMPAR | Glutamate receptors mediating fast excitatory transmission | Disrupted day-night oscillation in mPFC [77] | Indicator of synaptic strength and plasticity |
| BDNF | Neurotrophin supporting neuronal survival and plasticity | Decreased with sleep restriction [76] | Links sleep quality to structural plasticity |
| P300 | Event-related potential component | Prolonged latency after SD [78] | Objective measure of cognitive processing efficiency |
Cognitive and Behavioral Consequences
Sleep deprivation produces measurable deficits across multiple cognitive domains, particularly affecting attention, executive function, and memory processing. Electroencephalographic studies demonstrate that sleep deprivation significantly prolongs P300 latency, indicating slower cognitive processing speed, and increases reaction time, especially in acute sleep deprivation conditions [78]. The P300 component, occurring approximately 300ms after stimulus presentation, reflects neural activity related to attention allocation and working memory updating, making it a sensitive marker of sleep-related cognitive impairment [78].
Chronic sleep restriction produces distinct adaptive changes. Individuals with prolonged night shift histories show smaller increases in reaction time following sleep deprivation compared to acutely sleep-deprived individuals, suggesting compensatory neural mechanisms develop over time [78]. However, this apparent adaptation may come at the cost of chronic cognitive impairment, as evidenced by persistent baseline deficits in the chronic sleep deprivation group [78]. These findings highlight the brain's capacity for metaplasticity—the ability to adapt its own plasticity mechanisms—in response to sustained sleep pattern alterations.
Table 2: Cognitive Measures Affected by Sleep Deprivation
| Cognitive Domain | Measurement Tool | Acute SD Effect | Chronic SD Effect |
|---|---|---|---|
| Processing Speed | P300 Latency | Significant prolongation [78] | Moderate prolongation |
| Attention | Reaction Time (Oddball) | Increase of 83.69 ms [78] | Minor increase (6.54 ms) [78] |
| Working Memory | 2-back Task Performance | Decreased accuracy, compensatory activation [78] | Not reported |
| Executive Function | Cognitive Failures Questionnaire | Significant increase in errors [79] | Sustained elevation in errors |
Experimental Protocols for Sleep Research
P300 Measurement Protocol (adapted from Frontiers in Neuroscience study [78]):
- Participants: Healthy adults screened via polysomnography and exclusion of psychiatric/neurological conditions, substance abuse, and hearing impairment
- Apparatus: High-density electroencephalography (EEG) system using the oddball paradigm
- Stimuli: Auditory tones with standard (frequent) and target (infrequent) stimuli presented in random sequence
- Procedure: Baseline recording followed by sleep deprivation intervention (24-hour total sleep deprivation for acute group; chronic sleep restriction for chronic group) and post-intervention recording
- Parameters: P300 amplitude and latency at electrode sites Pz, Cz, Fz; subjective reaction time to target stimuli
- Analysis: ERP averaging time-locked to target stimuli; statistical comparison via ANOVA with factors of group and sleep condition
Sleep Deprivation in Mouse Models (adapted from Nature Communications protocol [77]):
- Subjects: Wild-type C57BL/6J and conditional Bmal1 knockout mice (both sexes, 8+ weeks old)
- Apparatus: Standard housing with 12-hour light-dark cycle (light phase corresponding to rest period for mice)
- SD Method: Gentle handling technique for 6 hours starting at light phase onset (ZT00)
- Behavioral Tests: Tail suspension test and forced swim test conducted at ZT06 by blinded experimenters
- Molecular Analysis: qRT-PCR for circadian gene expression; immunohistochemistry for Homer1a and synaptic markers
- Pharmacological Manipulation: REV-ERB agonist SR10067 (30 mg/kg, i.p.) to test clock manipulation effects
Stress Management and Neural Adaptation
Neuroendocrine Mechanisms
The relationship between stress and neuroplasticity follows an inverted U-shaped curve, whereby moderate stress enhances plasticity mechanisms while chronic or severe stress produces maladaptive changes. Acute stress activates the hypothalamic-pituitary-adrenal (HPA) axis, releasing cortisol which temporarily enhances memory consolidation through interactions with glucocorticoid receptors in the hippocampus and prefrontal cortex [80]. However, chronic stress leads to glucocorticoid receptor dysregulation, resulting in dendritic atrophy in hippocampal and prefrontal regions, and reduced neurogenesis—structural changes associated with cognitive impairment and emotional dysregulation [80].
Epigenetic mechanisms mediate the long-lasting effects of stress on neural circuitry. Early-life stress produces persistent changes in DNA methylation at promoter regions of genes critical for stress regulation, including glucocorticoid receptors and brain-derived neurotrophic factor (BDNF) [80]. These epigenetic modifications alter transcriptional potential, creating a predisposition toward heightened stress reactivity that persists throughout the lifespan. The timing of stress exposure is critical, with sensitive periods of epigenetic maturation during early development presenting particular vulnerability to programming effects [80].
Therapeutic Approaches and Mechanisms
Mindfulness meditation and related contemplative practices produce measurable changes in brain structure and function consistent with enhanced neuroplasticity. Regular meditation practice increases gray matter density in prefrontal regions supporting executive function and in insular regions involved in interoceptive awareness [76]. These structural changes correlate with improved emotional regulation and reduced amygdala reactivity to negative stimuli, demonstrating the potential for directed mental training to sculpt neural circuitry.
Pharmacological approaches targeting stress-related plasticity deficits represent an active area of drug development. Rapid-acting antidepressants like ketamine produce their effects in part by modulating stress-disrupted plasticity mechanisms. Ketamine downregulates negative clock loop genes (Per, Cry) in the mPFC, opposing the effects of stress and restoring synaptic homeostasis [77]. This interaction between circadian regulation and synaptic plasticity pathways offers novel targets for therapeutic intervention in stress-related disorders.
Diagram 1: Stress-Neuroplasticity Interactions and Intervention Targets. This pathway illustrates how acute and chronic stress differentially impact neuroplasticity through neuroendocrine and epigenetic mechanisms, and identifies key points for therapeutic intervention.
Environmental Enrichment and Physical Activity
Structural and Functional Network Plasticity
Physical exercise induces coordinated structural and functional changes across multiple brain networks. Cardiovascular training promotes neurogenesis in the hippocampal dentate gyrus, with approximately 700-1,500 new neurons generated daily in active individuals [25] [4]. This structural remodeling is mediated by exercise-induced increases in brain-derived neurotrophic factor (BDNF), which supports neuronal survival, differentiation, and synaptic formation [4] [76]. Different exercise modalities produce distinct patterns of network engagement: cardiovascular training preferentially enhances connectivity in the default mode network, strength training modulates the salience network, and mixed training approaches engage visuospatial networks [4].
Environmental complexity drives experience-dependent plasticity through mechanisms of synaptic competition. Novel stimuli and skill learning activate NMDA receptor-dependent long-term potentiation (LTP), strengthening actively engaged synapses while less active connections are pruned [25]. This selective stabilization follows Hebbian principles, where neurons that "fire together, wire together." Learning complex real-world skills, such as London taxi drivers navigating city routes or musicians mastering instruments, produces measurable expansion of relevant cortical regions, demonstrating that sustained environmental engagement drives macroscopic structural reorganization [25].
Exercise Parameters and Plasticity Optimization
The neuroplastic benefits of exercise follow dose-response relationships influenced by type, intensity, and duration. Moderate-to-vigorous intensity aerobic exercise (64-91% VO₂max) produces the most robust BDNF increases and hippocampal growth, with optimal effects observed at approximately 150 minutes per week [4] [76]. Strength training (70-85% 1 RM) preferentially improves executive function through frontal lobe mechanisms, while mixed exercise regimens that combine cardiovascular, resistance, and coordinative challenges produce the most widespread network effects [4].
Table 3: Exercise Parameters for Targeted Neuroplastic Outcomes
| Exercise Type | Intensity Parameters | Primary Neural Effects | Key Brain Networks |
|---|---|---|---|
| Cardiovascular | 64-91% VO₂max or 76-96% HRmax [4] | ↑ Hippocampal volume, ↑ BDNF, ↑ neurogenesis [4] [76] | Default Mode Network, Hippocampal Network |
| Strength Training | 70-85% 1 RM [4] | ↑ Frontal executive function, ↓ age-related atrophy | Salience Network, Frontal-Parietal Network |
| High-Intensity Interval Training | >91% VO₂max intervals [4] | Rapid BDNF release, enhanced connectivity | Multiple Network Integration |
| Mixed Exercise | Combination of modalities [4] | Widespread structural and functional benefits | Sensorimotor, Visuospatial, Executive Networks |
Long-term exercise adherence produces cumulative protective effects, increasing cognitive reserve and resilience to age-related decline. Regular physical activity attenuates normal age-related decreases in cortical volume and white matter integrity, particularly in prefrontal and hippocampal regions [4]. This structural preservation translates to reduced risk of neurodegenerative conditions, with physically active individuals demonstrating approximately 30-50% lower incidence of Alzheimer's disease and other dementias [81].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Neuroplasticity Investigation
| Reagent/Category | Research Application | Function/Mechanism | Example Use Cases |
|---|---|---|---|
| AAV-CaMKIIa-HI.GFP-Cre (Addgene #105551) [77] | Cell-type specific manipulation | Cre recombinase delivery to excitatory neurons | Conditional Bmal1 knockout in mPFC glutamatergic neurons [77] |
| AAV-CaMKIIa-EGFP (Addgene #50469) [77] | Control vector for neural transduction | GFP expression in excitatory neurons | Control for viral delivery in plasticity studies [77] |
| Ketamine Hydrochloride (Sigma-Aldrich) [77] | Rapid antidepressant modeling | NMDA receptor antagonism, synaptic plasticity modulation | Comparison with sleep deprivation effects on mPFC clock genes [77] |
| SR10067 (REV-ERB agonist) (Tocris) [77] | Circadian clock manipulation | Nuclear receptor agonist, negative clock loop enhancement | Testing clock repression effects on SD antidepressant actions [77] |
| Pittsburgh Sleep Quality Index (PSQI) [79] | Sleep quality assessment | Validated self-report measure of sleep patterns and disturbances | Correlating sleep quality with cognitive performance [79] |
| Cognitive Failures Questionnaire (CFQ) [79] | Cognitive assessment | Self-report measure of everyday cognitive errors | Quantifying brain fog and attention lapses [79] |
| High-Density EEG Systems [78] | Neural dynamics recording | Millisecond-temporal resolution of brain activity | P300 measurement during oddball tasks [78] |
| fMRI/SMRI [4] | Brain network mapping | Structural and functional connectivity assessment | Exercise-induced changes in network connectivity [4] |
Integrated Plasticity Regulation
The lifestyle factors discussed—sleep, stress management, and environmental enrichment—operate through shared molecular pathways that converge on final common mechanisms of neuroplasticity. BDNF signaling represents a key integration point, as it is enhanced by exercise, sleep, and cognitive stimulation, while being suppressed by chronic stress and sleep disruption [4] [76]. Similarly, circadian regulation interfaces with each domain, as the molecular clock in mPFC neurons influences sleep architecture, stress reactivity, and the timing of environmental engagement [77].
These interactive effects highlight the importance of a multidimensional approach to optimizing neuroplasticity. Combined interventions produce synergistic benefits, as demonstrated by the enhanced cognitive outcomes when physical activity, sleep hygiene, and stress reduction are implemented together [76]. Future research should focus on identifying optimal combinations and timing of lifestyle interventions to maximize plasticity outcomes across different populations and neural systems.
Diagram 2: Integrated Lifestyle Regulation of Neuroplasticity. This systems view illustrates how multiple lifestyle factors converge on shared molecular mechanisms to produce coordinated effects on structural, functional, and cognitive aspects of neuroplasticity.
Lifestyle factors represent powerful, non-pharmacological modulators of neuroplasticity with profound implications for behavioral adaptation and optimal performance. Sleep, stress management, and environmental engagement operate through distinct yet complementary mechanisms to shape neural structure and function across molecular, cellular, and systems levels. The evidence synthesized in this whitepaper provides a rigorous scientific foundation for developing targeted interventions to optimize neuroplastic outcomes in both healthy and clinical populations.
For drug development professionals, understanding these lifestyle-plasticity interactions offers crucial insights for contextualizing pharmacological effects and identifying novel therapeutic targets. The molecular interfaces between lifestyle factors and neuroplasticity mechanisms—particularly circadian regulation of synaptic plasticity, stress-mediated epigenetic programming, and exercise-induced neurotrophic signaling—represent promising avenues for future therapeutic development. Integrating lifestyle optimization with targeted pharmacotherapy may yield synergistic benefits for enhancing cognitive function, promoting resilience, and supporting recovery from neural injury across the lifespan.
Individual variability in response to stimuli, injury, or therapeutic intervention represents a fundamental challenge and opportunity in biomedical science. This variability arises from a complex interplay of genetic makeup, anatomical structure, and pathological history, which collectively influence an organism's functional output. Understanding these influences is paramount within the broader context of neuroplasticity—the nervous system's inherent capacity to reorganize itself in response to experience, injury, or disease to facilitate behavioral adaptation and optimal performance. This whitepaper provides a technical guide to the key sources of individual variability, detailing the quantitative genetic frameworks, molecular mechanisms, and experimental methodologies essential for researchers and drug development professionals working to predict, personalize, and optimize outcomes.
Genetic Foundations of Variability
The genetic blueprint is a primary source of individual variation, influencing everything from baseline anatomy to dynamic physiological responses.
Quantitative Genetic Framework
Quantitative genetics provides the statistical foundation for analyzing complex traits that vary continuously among individuals and are influenced by many genes and environmental factors [82]. The core model partitions the observed (phenotypic) variance (VP) into its constituent parts:
- VA: Additive genetic variance (variance in breeding values)
- VD: Dominance genetic variance
- VI: Epistatic variance (gene-gene interactions)
- VE: Environmental variance
A critical parameter is heritability (h²), defined as the proportion of phenotypic variance attributable to genetic factors: h² = VA/VP. It is widely used, though often misunderstood, for predicting responses to artificial and natural selection [82].
Table 1: Key Parameters in Quantitative Genetics
| Parameter | Symbol | Definition | Research Application |
|---|---|---|---|
| Phenotypic Variance | VP | Total observed variance in a trait | Describes the total variability in a population. |
| Additive Genetic Variance | VA | Variance due to additive allele effects | Predicts response to selection (Breeder's Equation). |
| Heritability | h² | VA/VP | Estimates the proportion of phenotypic variance due to additive genetic effects. |
| Selection Differential | S | Difference between population mean and mean of selected parents | Measures the intensity of selection applied. |
The infinitesimal model is a key assumption, positing that traits are controlled by an infinite number of unlinked genes, each with an infinitesimally small effect, allowing prediction of selection response over generations from base population parameters [82].
Molecular Mechanisms and Pharmacogenomics
At the molecular level, genetic variation modulates protein function and gene expression, leading to variable responses. Pharmacogenomics is the study of how genetic variants influence individual responses to drugs [83].
Table 2: Examples of Genetic Variants Influencing Drug Response
| Gene | Drug | Variant Impact | Clinical Consequence |
|---|---|---|---|
| CYP2D6 | Codeine, Tamoxifen | Loss-of-function alleles impair bioactivation [83]. | Poor metabolizers: Reduced efficacy of the prodrug. |
| CYP2C19 | Clopidogrel | Loss-of-function alleles impair bioactivation [83]. | Poor metabolizers: Reduced antiplatelet effect, increased cardiovascular risk. |
| VKORC1 | Warfarin | Polymorphisms affect enzyme activity [83]. | Altered dose requirements for stable anticoagulation. |
| SLCO1B1 | Simvastatin | Polymorphism reduces hepatic uptake [83]. | Increased risk of statin-induced myopathy. |
| Androgen Receptor | - | CAG repeat length polymorphism [84]. | Fewer repeats (≤19) associated with higher prostate weight. |
A "high-risk pharmacokinetics" scenario occurs when a drug is metabolized by a single pathway. If this pathway is compromised by genetic variation or drug interactions, it can lead to extreme variability in drug concentrations and effects [83]. Furthermore, allele frequencies of pharmacogenetically important variants can differ significantly across populations, contributing to "pharmacoethnicity" [85]. For instance, the frequency of the CYP3A5*3 loss-of-function variant is much higher in Caucasians (~0.85) than in African Americans (~0.55), contributing to population-differentiated responses to drugs like tacrolimus [83] [85].
Anatomical and Structural Variability
Genetic influences manifest in anatomical structure, which exhibits significant natural variation that impacts function and response.
Genetic Influence on Anatomy
Genetic instructions encoded in DNA orchestrate the development, structure, and function of organs and tissues. Variations in DNA sequence, such as single nucleotide polymorphisms (SNPs) and structural variants, contribute to anatomical diversity, including differences in organ size, shape, and structural configurations [86]. For example, a study on age-related prostate changes found a negative correlation between prostate weight and the number of CAG repeats in the androgen receptor gene (r = -0.32, P=0.003), and an association between the CYP17 A2A2 genotype and a higher stromal ratio (P=0.016) [84].
Cerebral Anatomical Variability
The human brain exhibits remarkable anatomical variability, particularly in sulcal and gyral patterns. This variability is developmentally determined, with primary sulci (e.g., Sylvian fissure, Rolandic sulcus) appearing early and showing less variability than tertiary sulci that develop later in gestation [87]. This has profound implications for intersubject registration and normalization in neuroimaging. In standard stereotactic space (e.g., Talairach space), the variability of the Rolandic sulcus can be as large as 12-20 mm, highlighting the challenge of precise localization across individuals [87]. Probabilistic atlases have revealed asymmetries, such as a left-hemisphere prominence of the paracingulate sulcus, which may be linked to language function [87].
Neuroplasticity as the Dynamic Interface
Neuroplasticity—the brain's ability to reorganize itself by forming new neural connections throughout life—serves as the central mechanism through which genetic, anatomical, and pathological factors are integrated to produce behavioral adaptation and influence response outcomes [25].
Mechanisms of Adaptive Neuroplasticity
Neuroplasticity operates through several biological mechanisms that allow the brain to adapt, learn, and recover:
- Synaptic Plasticity: The ability of synapses to strengthen or weaken over time. Long-term potentiation (LTP) is a widely studied form of synaptic plasticity that is considered a cellular model for learning and memory. LTP involves NMDA receptor activation, calcium influx, and biochemical cascades that lead to an increase in neurotransmitter receptors and structural changes in dendritic spines [25].
- Neurogenesis: The formation of new neurons, which continues in certain brain regions (e.g., the hippocampus) throughout life, contributing to learning and memory. The hippocampus creates an estimated 700 to 1,500 new neurons each day [25].
- Structural Remodeling: Physical changes in brain circuits, including the formation or disappearance of dendritic spines and the reshaping of axonal boutons. During intense learning or after injury, spine turnover rates can increase dramatically—up to 90% in some models of cortical reorganization [25].
Maladaptive Plasticity in Pathology
While often beneficial, neuroplastic changes can also be maladaptive. Severe stress or trauma can disrupt normal plastic processes, leading to the loss of synapses and contributing to conditions like PTSD and depression [25]. Similarly, chronic pain and some movement disorders can be perpetuated by maladaptive reorganization of neural circuits. The direction of plasticity—adaptive or maladaptive—is determined by the context, timing, and nature of the influencing stimuli.
Methodological Toolkit for Researchers
This section outlines key experimental approaches, reagents, and analytical methods for investigating individual variability.
Experimental Protocols
Protocol 1: Genome-Wide Association Study (GWAS) for Drug Response Phenotypes
- Objective: To identify genetic variants associated with variable response to a drug or therapy in an unbiased, hypothesis-free manner.
- Methodology:
- Cohort Selection: Recruit a large cohort of individuals with well-curated drug response phenotypes (e.g., efficacy measures, adverse drug reaction incidence).
- Genotyping: Perform high-density genotyping (e.g., using microarrays) across the genome for all participants.
- Quality Control: Filter out low-quality SNPs and individuals with high genotyping failure rates or population outliers.
- Imputation: Estimate missing genotypes using reference panels (e.g., 1000 Genomes Project) to increase genomic coverage.
- Association Analysis: Test for statistical associations between each SNP allele and the drug response phenotype, typically using a linear or logistic regression model, while controlling for covariates (e.g., age, sex, ancestry principal components).
- Replication: Validate significant associations in an independent cohort to guard against false positives [83] [85].
Protocol 2: Heritability Estimation of a Behavioral or Drug Response Trait Using an Animal Model
- Objective: To quantify the proportion of variance in a trait attributable to genetic factors in a controlled population.
- Methodology:
- Population Design: Utilize a population with known pedigree structure, such as a founder population (e.g., the Amish) or a long-term studied wild/experimental population.
- Phenotyping: Precisely measure the trait of interest (e.g., ADP-stimulated platelet aggregation before and after clopidogrel administration) in all individuals.
- Statistical Modeling: Apply the "animal model," a type of mixed linear model, to partition the phenotypic variance. The basic model is: y = Xβ + Za + e, where
yis the vector of phenotypes,βis a vector of fixed effects,ais a vector of random additive genetic effects (breeding values), andeis the residual. The variance-covariance structure ofais defined by the additive genetic relationship matrix A [82]. - Parameter Estimation: Use Restricted Maximum Likelihood (REML) or Bayesian methods to estimate the variance components and calculate heritability as h² = VA/VP
Research Reagent Solutions
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Function/Application |
|---|---|
| High-Density SNP Genotyping Arrays | Enable genome-wide profiling of common genetic variations for GWAS and population genetics [85]. |
| Lymphoblastoid Cell Lines | Immortalized cell lines from related and unrelated donors used for in vitro assessment of heritability of drug cytotoxicity and other phenotypes [83]. |
| Drug-Gene Interaction Databases | Curated knowledge bases (e.g., PharmGKB) used to map genetic variants to drug pathways and predict functional consequences [85]. |
| VCF Tools | Software for processing and calculating allele frequencies from large-scale genomic data (e.g., 1000 Genomes Project) [85]. |
| Additive Relationship Matrix (A-matrix) | A mathematical construct that describes the genetic relatedness between individuals in a population, central to the "animal model" for variance component analysis [82]. |
Data Visualization and Workflows
Discovery Pipeline for Pharmacogenomic Variants
Integrative Model of Response Variability
Measuring Efficacy and Comparative Analysis of Neuroplasticity Interventions
The relentless pursuit of objective validation in clinical neuroscience finds a promising ally in the correlation of behavioral improvements with neural biomarkers. This paradigm is fundamentally rooted in the principles of neuroplasticity—the nervous system's inherent capacity to adapt its structure and function in response to intrinsic and extrinsic stimuli [1]. Within the context of optimal performance research, the ability to quantify these neural changes provides a critical bridge between subjective clinical assessments and the underlying biological adaptations driving recovery and enhancement. For researchers and drug development professionals, establishing robust correlations between clinical scales and biomarkers is no longer ancillary; it is essential for validating therapeutic efficacy, understanding treatment mechanisms, and accelerating the development of targeted interventions.
Neuroplasticity manifests through diverse mechanisms, including synaptic plasticity (the experience-dependent strengthening or weakening of neuronal connections), functional reorganization (where brain regions shift their operational roles), and structural changes such as axonal sprouting [1]. The temporal dynamics of these processes are crucial, often occurring in phased epochs following injury: initial damage and network substitution within 48 hours, a shift to excitatory synaptic signaling and new connection formation in the following weeks, and long-term remodeling over weeks to months [1]. This conceptual framework provides the biological basis for why behavioral gains from rehabilitation or pharmacotherapy are not merely compensatory but can reflect genuine neural restoration. The ultimate goal is to move beyond correlation to causation, using validated biomarkers to predict individual treatment responses and optimize brain performance across the lifespan.
Core Neural Biomarkers: From Mechanism to Measurement
The following table summarizes the primary categories of neural biomarkers used to quantify neuroplastic changes, their specific measurement targets, and the technologies employed for their detection.
Table 1: Core Biomarkers of Neuroplasticity and Their Measurement
| Biomarker Category | Specific Measure | Measurement Technique | Biological Correlate |
|---|---|---|---|
| Functional Reorganization | Shift in neural activity locus; Change in network connectivity | functional Magnetic Resonance Imaging (fMRI), functional Near-Infrared Spectroscopy (fNIRS) | Vicariation, Equipotentiality [1] |
| Synaptic Plasticity | Long-Term Potentiation (LTP); Spike-timing-dependent plasticity (STDP) | Transcranial Magnetic Stimulation (TMS) paired with EEG/EMG, Electroencephalography (EEG) | Synaptic strength, Hebbian learning [1] |
| Structural Connectivity | White matter integrity; Axonal sprouting | Diffusion Tensor Imaging (DTI), Tractography | Neuronal regeneration, collateral sprouting [1] |
| Neurochemical & Molecular | Neurotransmitter levels (e.g., GABA, Glutamate); Neurotrophic factors (e.g., BDNF) | Magnetic Resonance Spectroscopy (MRS), Serum/Plasma Assays | Neuromodulation, synaptic efficacy [1] [3] |
Linking Biomarkers to Clinical Outcomes
The practical utility of these biomarkers is realized only when they are statistically correlated with meaningful clinical and behavioral outcomes. For instance, in stroke recovery, the shift of motor function representation from the primary damaged motor cortex to peri-lesional areas or the contralateral hemisphere, as visualized with fMRI, can be directly correlated with improvements in the Fugl-Meyer Assessment (FMA) of motor function [1]. Similarly, the concentration of circulating Brain-Derived Neurotrophic Factor (BDNF), a key mediator of synaptic plasticity, has been shown to correlate with the rate of skill acquisition in learning tasks, a relevant metric for cognitive performance protocols [3].
The concept of diaschisis, where a brain injury causes functional disruption in distant but connected areas, and its subsequent reversal, provides another compelling biomarker pathway [1]. For example, the restoration of metabolic activity in the ipsilateral thalamus following middle cerebral artery stroke, measured via perfusion imaging, can be tracked alongside the recovery of integrated neurological functions. These correlations strengthen the evidence that a treatment is facilitating widespread network reintegration, moving beyond local repair.
Experimental Protocols for Correlation Studies
Establishing causal or correlative links requires meticulously designed experiments. Below are detailed methodologies for key experiment types that integrate biomarker and behavioral assessment.
Longitudinal Intervention Study in Neurological Recovery
Objective: To determine whether a pharmacological or rehabilitative intervention (X) drives motor recovery in stroke patients by inducing functional reorganization in the motor network.
Population: Adult patients 3-months post-ischemic stroke with moderate motor deficits.
Study Design: Randomized, double-blind, sham-controlled trial with parallel groups.
Methodology:
- Baseline Assessment (Week 0):
- Clinical: Administer Fugl-Meyer Assessment (FMA) and Action Research Arm Test (ARAT).
- Biomarker: Acquire resting-state and task-based fMRI (finger-tapping paradigm) to map motor network activity. Acquire DTI to assess corticospinal tract integrity.
- Intervention Period (Weeks 1-8):
- Experimental Group: Receive active intervention X (e.g., a drug candidate believed to promote plasticity) paired with standardized physical therapy.
- Control Group: Receive matched placebo paired with the same physical therapy regimen.
- Post-Intervention Assessment (Week 9):
- Repeat all clinical and biomarker assessments from baseline.
- Follow-Up Assessment (Month 6):
- Repeat clinical assessments to evaluate persistence of effects.
Data Correlation Analysis:
- Primary Analysis: Compare the change in fMRI lateralization index (LI) from baseline to Week 9 between groups, and correlate the delta LI (∆LI) with the delta FMA (∆FMA) using Pearson's correlation or Spearman's rank.
- Secondary Analysis: Use multiple regression to model ∆FMA as a function of ∆LI, group assignment, and baseline lesion volume.
Environmental Enrichment and Cognitive Resilience Study
Objective: To investigate if an enriched environment enhances cognitive reserve and emotional resilience in healthy adults, mediated by changes in hippocampal volume and functional connectivity.
Population: Healthy adults aged 60-75.
Study Design: Longitudinal, cohort study.
Methodology:
- Baseline Assessment (Month 0):
- Clinical/Cognitive: Administer Repeatable Battery for the Assessment of Neuropsychological Status (RBANS), Resilience Scale (RS-14), and measure salivary cortisol/DHEA ratio.
- Biomarker: Acquire high-resolution structural MRI (for hippocampal volumetry) and resting-state fMRI (for hippocampal-prefrontal connectivity).
- Intervention Period (Months 1-6):
- Participants engage in a structured, enriched lifestyle program incorporating novel cognitive training, increased social interaction, and regular physical activity.
- Post-Intervention Assessment (Month 7):
- Repeat all clinical, cognitive, and biomarker assessments.
Data Correlation Analysis:
- Correlate the percentage change in hippocampal volume with the change in RBANS delayed memory index.
- Correlate the change in hippocampal-prefrontal connectivity strength with the change in resilience scores and cortisol/DHEA ratio, an indicator of allostatic load [3].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Neuroplasticity Studies
| Item/Category | Function & Application | Specific Examples |
|---|---|---|
| ELISA/Kits | Quantify protein levels of neurotrophic factors or stress hormones in serum, plasma, or CSF. Essential for linking molecular plasticity to behavior. | BDNF ELISA Kit, Cortisol ELISA Kit, DHEA-S Immunoassay [3] |
| Neuromodulation Equipment | Non-invasive brain stimulation to probe causal relationships by inducing or inhibiting plasticity in targeted circuits. | Transcranial Magnetic Stimulation (TMS) device, transcranial Direct Current Stimulation (tDCS) system |
| Activity Assays | Monitor and quantify behavioral endpoints in animal models, such as learning, memory, and affective states. | Morris Water Maze, Fear Conditioning apparatus, Open Field test |
| Immunohistochemistry Reagents | Visualize and quantify structural plasticity markers in post-mortem tissue or animal models. | Antibodies against c-Fos (neuronal activity), PSD-95 (synapses), Doublecortin (neurogenesis) |
| Cell Line Models | Investigate molecular pathways of synaptic plasticity in a controlled in vitro environment. | Primary neuronal cultures, SH-SY5Y neuroblastoma cell line |
Data Synthesis and Visualization: Mapping the Pathway to Validation
The final and most critical phase is the integrated analysis of multimodal data. This requires sophisticated statistical models to determine whether changes in neural biomarkers mediate the relationship between the intervention and clinical improvement.
A typical analytical workflow involves:
- Preprocessing and Feature Extraction: Refining raw data (e.g., MRI images, EEG signals) to extract quantifiable features (e.g., activation cluster volume, functional connectivity strength, P300 amplitude).
- Univariate Correlation: Initial tests (e.g., Pearson's r) between single biomarker deltas and single clinical score deltas.
- Multiple Regression Modeling: Building models that control for potential confounders like age, sex, baseline severity, and lesion volume.
- Mediation Analysis: The gold-standard statistical test to establish if the biomarker is part of the causal pathway. This model tests if the intervention's effect on the clinical outcome is significantly explained by its effect on the biomarker.
Diagram 2: Statistical mediation model. A significant indirect effect (Path a * Path b) provides evidence that the biomarker mediates the intervention's effect on the clinical outcome.
The rigorous correlation of clinical improvements with neural biomarkers represents a paradigm shift towards biologically grounded validation in neuroscience and drug development. By leveraging the established principles of neuroplasticity—from synaptic potentiation to large-scale network reorganization—researchers can move beyond merely observing behavioral changes to understanding and validating their underlying neural substrates. The experimental frameworks and tools outlined herein provide a roadmap for this endeavor. Successfully demonstrating these correlations not only de-risks the development of new therapeutic agents but also fundamentally advances our understanding of the brain's remarkable capacity for adaptation and optimal performance, ultimately paving the way for more personalized and effective interventions.
Abstract This whitepaper provides a systematic comparison of three dominant therapeutic classes—behavioral training, neuromodulation, and pharmacological interventions—through the unifying lens of neuroplasticity. Intended for researchers, scientists, and drug development professionals, it synthesizes current evidence, with an emphasis on quantitative outcomes and experimental methodology. The central thesis posits that the mechanism of action for each modality, while distinct, converges on the brain's inherent capacity for functional and structural reorganization. A nuanced understanding of how these approaches differentially engage neuroplastic mechanisms is critical for developing targeted, effective interventions for neurological and psychiatric conditions.
Neuroplasticity, the nervous system's ability to reorganize its structure, functions, and connections in response to experience, is the fundamental biological process underpinning learning, memory, and recovery from injury [25]. This adaptive capacity manifests through mechanisms including synaptic plasticity (e.g., long-term potentiation), neurogenesis, and the structural remodeling of brain circuits [25]. The efficacy of any therapeutic intervention aimed at altering brain function or behavior is ultimately contingent upon its ability to harness these mechanisms.
The three modalities discussed herein engage neuroplasticity in fundamentally different ways:
- Behavioral Training directly leverages experience-dependent plasticity, using structured practice and feedback to guide the strengthening of specific neural pathways.
- Neuromodulation uses electrical, magnetic, or other forms of energy to directly alter neural activity patterns, creating a permissive state for plasticity and guiding circuit reorganization.
- Pharmacological Approaches primarily modulates the neurochemical environment, influencing synaptic transmission and neuronal excitability to facilitate or inhibit plastic changes.
This review will dissect the comparative effectiveness, protocols, and mechanistic underpinnings of each approach, providing a scaffold for future research and clinical development.
Comparative Quantitative Efficacy
The following tables summarize key efficacy data from recent studies and meta-analyses across different conditions, highlighting the relative performance of each intervention type.
Table 1: Comparative Outcomes in Fibromyalgia Management A structured comparison of non-pharmacological interventions from a randomized, crossover study. [88] [89]
| Intervention | Primary Outcomes | Key Efficacy Findings | Long-Term Adaptations |
|---|---|---|---|
| Structured Exercise (HIIT) | Pain Severity (NRS), Muscle Oxygenation | Significant reduction in pain scores; pronounced improvements in muscle oxygenation [88]. | Superior for inducing basal muscle oxygenation adaptations [88]. |
| Neuromodulation (EXOPULSE Mollii Suit) | Pain Severity (NRS), Autonomic Modulation | Significant reduction in pain scores; significant improvements in heart rate variability and cortical arousal [89]. | Cumulative benefits on autonomic nervous system regulation over time [89]. |
Table 2: Network Meta-Analysis of Pharmacological Agents for COVID-19 Summary of findings from a comprehensive network meta-analysis (40 RCTs, 70 observational studies). [90]
| Pharmacological Agent | Patient Setting | Key Efficacy Finding (vs. Standard Care) | Certainty of Evidence |
|---|---|---|---|
| Corticosteroids | ICU | OR 0.54 (95% CI 0.40-0.73) for mortality [90]. | Supported by RCTs |
| Remdesivir | Non-ICU | OR 0.62 (95% CI 0.39-0.98) for mortality [90]. | Supported by RCTs |
| Tocilizumab | Non-ICU | OR 0.43 (95% CI 0.30-0.60) for mortality [90]. | Association from observational studies |
| Hydroxychloroquine+Azithromycin | Mixed | No clinical benefit; increased cardiac risk (OR 2.01 for QT prolongation) [90]. | Supported by RCTs/observational studies |
Table 3: Neuromodulation Efficacy in Specific Neurological Disorders Evidence for neuromodulation in treating drug-resistant conditions. [91] [92]
| Condition | Neuromodulation Intervention | Key Efficacy Findings |
|---|---|---|
| Drug-Resistant Epilepsy | Vagus Nerve Stimulation (VNS), Deep Brain Stimulation (DBS) | Reduces seizure frequency in patients unresponsive to drugs or surgery [91]. |
| Tinnitus | Bimodal Neuromodulation (Lenire Device) | 91.5% responder rate (THI improvement ≥7 points); mean improvement of 27.8 points on THI [92]. |
Detailed Experimental Protocols
A critical component of comparative effectiveness is understanding the rigorous methodologies used to generate the evidence.
Protocol for Evidence-Based Behavioral Skills Training (BST)
This protocol, an exemplar of structured behavioral training, is designed to train performance skills to mastery and is highly effective for teaching complex behavioral sequences [93].
- Description of the Target Skill: The trainer provides a rationale and a behaviorally-defined description of the skill, often using a performance checklist [93].
- Provide a Written Description: Trainees receive a succinct, written summary of the target behaviors, distinct from lengthier background documents, to ensure clarity and focus [93].
- Modeling/Demonstration: The trainer demonstrates the exact performance of the skill, typically via a well-scripted role-play. Video models can also be effectively used [93].
- Trainee Practice: Each trainee is required to rehearse the skill in a role-play scenario. This step is critical and often omitted in less effective training [93].
- Performance Feedback: The trainer provides immediate, individualized feedback after each practice session, specifying what was performed correctly and how to correct errors [93].
- Repeat to Mastery: Steps 4 and 5 are repeated until the trainee demonstrates the skill at a pre-established mastery criterion [93].
Protocol for a Neuromodulation-Exercise Crossover Trial
This design allows for direct within-subject comparison of interventions, controlling for individual variability [88] [89].
- Participant Recruitment: Recruit diagnosed patients (e.g., fibromyalgia per ACR criteria). Apply strict inclusion/exclusion criteria (e.g., stable medication, no recent exercise) [89].
- Baseline Assessment: Conduct pre-intervention measurements of primary outcomes (e.g., pain scales, heart rate variability, muscle oxygenation) [88] [89].
- Randomization & Group Allocation: Randomly assign participants to one of two sequences: Group A (Intervention 1 first) or Group B (Intervention 2 first) [89].
- Intervention Phase I: Administer the first assigned intervention. Example: 16 sessions over 8 weeks, with outcomes measured after the 1st, 8th, and 16th sessions [88] [89].
- Washout Period: Implement a period (e.g., 2 weeks) with no active intervention to eliminate carry-over effects from the first treatment [89].
- Intervention Phase II: Administer the second, alternative intervention for the same duration and intensity as Phase I [89].
- Final Assessment & Data Analysis: Conduct post-intervention measurements. Use statistical models (e.g., repeated-measures ANOVA) to compare effects within and between groups and across time [88] [89].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Tools for Neuroplasticity and Intervention Research
| Tool / Reagent | Primary Function / Application |
|---|---|
| EXOPULSE Mollii Suit | A non-invasive neuromodulation garment using electrical stimulation to target whole-body spasticity and pain, used in fibromyalgia research [88] [89]. |
| Lenire Device | A bimodal neuromodulation device combining sound stimulation with electrical tongue stimulation for the treatment of tinnitus; an example of a targeted non-invasive approach [92]. |
| Deep Brain Stimulation (DBS) System | An invasive neuromodulation implant for delivering electrical stimulation to deep brain targets (e.g., STN for Parkinson's disease); a gold-standard for severe, drug-resistant conditions [91]. |
| Near-Infrared Spectroscopy (NIRS) | A non-invasive optical imaging method for measuring muscle and brain tissue oxygenation, used as a biomarker for metabolic function in exercise and neuromodulation studies [88]. |
| Heart Rate Variability (HRV) Analysis | A key metric for assessing autonomic nervous system function, frequently used to measure the impact of interventions on parasympathetic and sympathetic balance [89]. |
| Tinnitus Handicap Inventory (THI) | A validated self-report questionnaire for quantifying the severity and functional impact of tinnitus, serving as a primary endpoint in clinical trials [92]. |
| Behavioral Skills Training (BST) Checklist | A performance-based checklist used to define, teach, and measure fidelity of complex behavioral skills in training studies [93]. |
Mechanisms of Action: Engaging Neuroplastic Pathways
The comparative effectiveness of each modality is rooted in its unique pathway for inducing neuroplastic change. The following diagram synthesizes these distinct routes to behavioral and neural adaptation.
Synthesis of Pathways:
- Behavioral Training → Structured Practice & Feedback → Experience-Dependent Plasticity: This pathway directly strengthens synaptic connections through mechanisms like long-term potentiation (LTP), which is considered a cellular correlate of learning and memory [25]. The focused, repetitive nature of behavioral skills training drives circuit refinement and cognitive flexibility [25] [93].
- Neuromodulation → Focal Stimulation → Activity-Dependent Plasticity: Techniques like DBS and bimodal stimulation directly alter the brain's electrical activity patterns. This can suppress pathological oscillations, activate protective circuits (e.g., antidromic activation in DBS), and create a state that is highly receptive to reorganization, thereby facilitating recovery in conditions like stroke, epilepsy, and tinnitus [91] [92]. Its effects are rooted in the brain's functional and structural plasticity [25].
- Pharmacological Approaches → Neurochemical Modulation → Chemically-Induced Plasticity: Drugs act by modifying the neurochemical environment. For example, antidepressants increase monoamine levels, which can modulate synaptic signaling and promote neurogenesis, while anti-inflammatory agents like corticosteroids can mitigate neuroinflammation, creating a more favorable environment for plastic change [90]. This approach alters the fundamental biochemical substrate of neural communication.
The evidence demonstrates that behavioral, neuromodulatory, and pharmacological approaches are all potent tools for harnessing neuroplasticity, yet their profiles of effectiveness, risk, and mechanism are distinct. No single modality is universally superior; the optimal choice is condition-specific, patient-tailored, and often combinatorial.
Future research must prioritize several frontiers:
- Personalized Protocols: Leveraging biomarkers (e.g., from fMRI, dMRI, electrophysiology) to predict which patients will respond to which modality and to optimize stimulation parameters or behavioral strategies [91] [34].
- Combination Therapies: Systematically investigating synergistic effects, such as pairing neuromodulation to "prime" the brain for enhanced responsiveness with subsequent behavioral training, a paradigm showing promise in stroke recovery [91].
- Closed-Loop Systems: Advancing towards adaptive neuromodulation devices that deliver stimulation in response to real-time neural activity (closed-loop), as seen in responsive neurostimulation for epilepsy, offering more dynamic and precise interventions [91].
- Targeting Maladaptive Plasticity: Developing strategies to identify and reverse maladaptive plastic changes that contribute to chronic pain, addiction, and other disorders, a challenge that requires a deep understanding of plasticity's dual nature [25] [34].
The ongoing synthesis of research across these domains, grounded in the principles of neuroplasticity, will continue to drive the development of more effective and transformative interventions for optimizing brain health and performance.
Neuroplasticity, the nervous system's capacity to adapt its structure and function in response to experience, forms the fundamental biological basis for behavioral adaptation and optimal performance. Understanding the dynamics of these changes requires research methodologies that can capture temporal patterns of neural reorganization. Longitudinal study designs, characterized by repeated observations of the same individuals over time, provide unique insights into neurodevelopmental trajectories and aging-related changes that cross-sectional approaches cannot reveal [94]. These designs are particularly vital for studying the time course of plasticity—revealing when changes begin, how long they persist, and how different neural systems interact across developmental epochs.
The importance of longitudinal frameworks is mathematically grounded in the concept of ergodicity. In non-ergodic processes, which are fundamental to learning and development, inter-individual variation (differences between people) cannot be generalized to intra-individual variation (changes within a person) [94]. This distinction is crucial for understanding personalized trajectories of brain development and developing individually tailored interventions for optimizing performance. Furthermore, longitudinal approaches with three or more assessment waves enable researchers to establish temporal mediation, determining whether risk or protective factors impact mental health through changes in brain structure or function, with cross-sectional mediation models often yielding different parameter estimates and conclusions [94].
Conceptual Foundations: Why Longitudinal Designs Are Essential for Neuroplasticity Research
Capturing Individual Trajectories of Change
Longitudinal research designs unlock critical information about an individual's developmental and aging trajectory that cross-sectional approaches cannot provide. While cross-sectional studies comparing different individuals at various ages have value, they inherently lack data on within-person variability and the precise shape of change curves [94]. This limitation is particularly problematic in neuroplasticity research, where individuals may follow unique developmental paths despite similar starting points or environmental exposures.
The ability to identify deviant trajectories over time represents one of the most significant advantages of longitudinal designs for both basic research and clinical applications. By tracking the same individuals across multiple timepoints, researchers can better identify those at increased risk for mental health problems and enhance our understanding of potential risk and protective factors linked to mental health [94]. This approach recognizes that mental health is not static or binary but changes within individuals throughout life, as demonstrated by a rare longitudinal study spanning 40 years that showed individuals frequently shift among different successive mental disorders [94].
Methodological Advantages for Establishing Causal Mechanisms
Longitudinal designs provide several methodological advantages for establishing causal mechanisms in neuroplasticity research:
- Temporal precedence: By measuring variables in a specific temporal sequence, longitudinal designs help establish whether changes in brain structure precede, follow, or coincide with behavioral changes [94].
- Reduced inter-individual noise: Using each participant as their own control increases statistical power by reducing variance attributable to between-person differences [95].
- Optimization of stable factors: Multiple acquisitions over time can increase signal and decrease noise, allowing researchers to simultaneously disentangle stable components from those that change over time using appropriate statistical approaches [94].
These advantages make longitudinal designs particularly valuable for studying how neuroplasticity mediates behavioral adaptation and how interventions targeting plasticity can optimize performance outcomes across different populations.
Key Longitudinal Studies in Neuroplasticity Research
Large-Scale Cohort Studies
Several large-scale longitudinal initiatives have provided unprecedented insights into neuroplasticity across the lifespan:
Table 1: Major Longitudinal Studies of Neuroplasticity
| Study Name | Sample Characteristics | Key Findings | References |
|---|---|---|---|
| Dallas Lifespan Brain Study (DLBS) | 464 participants aged 21-89; 3 assessments over 10 years | Brain network breakdown evident across lifespan; high amyloid levels in healthy adults; multiple patterns of cognitive decline | [96] |
| ABCD Study | Approximately 11,000 children across the US | Ongoing study tracking brain development and child health | [94] |
| Dunedin Study | ~1,000 individuals from birth to age 45 | Mental disorder histories shift among successive disorders; early brain health predicts mental health later in life | [94] |
| UK Biobank | 500,000 participants aged 40-69 | Large-scale database linking brain imaging, genetics, and health outcomes | [94] |
These large-scale studies demonstrate that brain changes continue throughout life and that individual trajectories vary significantly. The DLBS specifically highlighted that the causes of cognitive decline represent different "pieces in a puzzle" that can vary across individuals—some show heavily degraded white matter, others have problems with activation or brain shrinkage [96]. This heterogeneity underscores the importance of longitudinal designs that can capture individualized patterns of neuroplasticity.
Single-Case and Intensive Longitudinal Designs
While large-scale studies reveal population-level trends, single-case and intensive longitudinal designs provide complementary insights into rapid plasticity processes and individual response patterns. For example, a precision imaging study tracking a single individual from preconception through two years postpartum revealed striking decreases in gray matter volume and cortical thickness during pregnancy, along with nonlinear increases in white matter quantitative anisotropy [97]. Similarly, longitudinal investigation of pregnancy in 10 participants assessed 1-6 times during gestation found a 2.6% decline in total brain volume and a 3.9% decline in gray matter volume over the observed gestational range (12-39 weeks) [97].
These focused studies reveal that profound neuroplasticity can occur within relatively short timeframes in adulthood, challenging traditional views that significant structural brain changes are limited to early development. The pregnancy research further demonstrated that progesterone levels were associated with reductions in brain volumetric measurements, while both progesterone and estradiol were linked to increases in neurite density index in white matter tracts [97].
Quantitative Methods for Tracking Neuroplastic Changes
Advanced Neuroimaging Approaches
Modern longitudinal neuroplasticity research employs increasingly sophisticated imaging techniques that provide specific biological information beyond traditional structural imaging:
Table 2: Quantitative MRI Parameters for Tracking Neuroplasticity
| Parameter | Biological Specificity | Example Findings in Plasticity Research | References |
|---|---|---|---|
| Magnetization Transfer Saturation (MTsat) | Primarily sensitive to myelin content | Decrease in left frontal cortex after 4 weeks of balance training | [98] |
| Transverse Relaxation Rate (R2*) | Sensitive to iron content | Performance-related changes in visual cortical (increase) and limbic subcortical (decrease) areas after balance training | [98] |
| Longitudinal Relaxation Time (R1) | Sensitive to myelin, water, and iron content (reduced specificity) | Commonly used in aging and plasticity studies to track microstructural changes | [98] |
| Proton Density (PD) | Most sensitive to water content | Used in combination with other parameters to interpret microstructural changes | [98] |
| Neurite Density Index (NDI) | Proxy for axon density | Increases in white matter tracts across pregnancy, associated with hormone levels | [97] |
Quantitative MRI (qMRI) methods are particularly valuable because they provide insight into microstructural processes that underlie more gross morphological changes. Histological validation studies support the relationship between these qMRI parameters and specific biological processes [98]. For example, in a motor learning study, consideration of multiple qMRI parameters revealed that training-induced structural changes in gray matter likely reflect a mixture of various microstructural processes rather than a uniform biological mechanism [98].
Statistical Considerations for Longitudinal Data
Appropriate statistical approaches are essential for valid interpretation of longitudinal neuroplasticity data:
- Linear mixed-effects models: Account for within-subject correlations across multiple timepoints while allowing for missing data [97].
- Mediation analysis with temporal precedence: Requires at least three waves of data to establish whether brain changes mediate the relationship between interventions and behavioral outcomes [94].
- Individual trajectory modeling: Captures person-specific patterns of change that may deviate from group averages [94].
- Handling of missing data: Longitudinal studies typically experience attrition across waves, with potential bias toward less severely impaired participants as those with largest decreases in health are more likely to drop out [94].
These statistical approaches allow researchers to address fundamental questions about within-person change while accounting for the complex structure of longitudinal data.
Experimental Protocols and Methodologies
Motor Learning Protocol (Balance Training)
A recent study investigating motor learning-induced microstructural gray matter plasticity employed a rigorous longitudinal protocol with comprehensive quantitative imaging [98]:
Participants: 26 healthy young adults Intervention: 4 weeks of dynamic balance training (DBT) Imaging Sessions: 3 MRI scans (baseline, pre-training, post-training) using a multi-parameter mapping (MPM) protocol Quantitative Parameters: MTsat, R2*, R1, PD maps Analysis Approach: Voxel-wise analysis of microstructural changes in a priori regions of interest (prefrontal regions, motor areas) and whole-brain exploratory analysis
This protocol revealed regionally-specific decreases in myelin-related MTsat in the left frontal cortex and performance-related changes in iron-sensitive R2* in visual cortical and limbic subcortical areas [98]. The study demonstrates how quantitative imaging can detect subtle microstructural changes associated with motor learning over relatively short time intervals.
Cognitive Behavior Therapy for Social Anxiety Disorder
A randomized controlled trial examined neuroplasticity in response to cognitive behavior therapy for social anxiety disorder using a multimodal imaging approach [95]:
Participants: 26 participants with social anxiety disorder (SAD) and 26 matched healthy controls Intervention: 9 weeks of internet-delivered CBT vs. attention bias modification (ABM) control Imaging: Structural T1-weighted images (gray matter volume) and functional MRI (BOLD response to self-referential criticism) Clinical Measures: Liebowitz Social Anxiety Scale (LSAS-SR), Clinical Global Impression-Improvement (CGI-I), subjective anxiety during speech task
This study found significant time × treatment interactions in the amygdala, with decreases in both gray matter volume and BOLD responsivity after successful CBT [95]. The reduction in amygdala gray matter volume correlated with reduced anticipatory anxiety after treatment, and mediation analysis indicated that diminished amygdala gray matter volume mediated the relationship between decreased neural responsivity and reduced social anxiety [95]. These findings provide compelling evidence that structural neuroplasticity impacts neural responsiveness within emotion-processing circuits following effective psychological treatment.
Pregnancy-Related Neuroplasticity Protocol
A longitudinal investigation of neurobiological changes across pregnancy employed intensive repeated measures to capture dynamic plasticity during this transformative period [97]:
Participants: 10 participants assessed 1-6 times during pregnancy (median=3 sessions) Gestational Range: 12-39 weeks Imaging Protocol: Anatomical MRI (gray matter volume, cortical thickness) and multi-shell diffusion-weighted MRI (NODDI parameters: NDI, ODI) Biological Samples: Waking salivary hormones (progesterone, estradiol), hair hormones, inflammatory cytokines Analysis Approach: Linear mixed-effects models for each brain metric with gestational week as fixed effect, controlling for age, intracranial volume, and motion
This study documented profound neurobiological changes during pregnancy, including reduced gray matter volume and increased neurite density index in white matter tracts [97]. These changes were associated with hormonal fluctuations, specifically progesterone levels being linked to volumetric reductions and both progesterone and estradiol associated with white matter microstructural changes. The research highlights how hormonally-mediated plasticity can substantially reorganize brain structure in adulthood.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Resources for Longitudinal Neuroplasticity Research
| Resource Category | Specific Tools/Measures | Research Application | Examples from Literature |
|---|---|---|---|
| Neuroimaging Parameters | MTsat, R2*, R1, PD (qMRI) | Mapping microstructural correlates of plasticity (myelin, iron, water content) | Balance training study [98] |
| Diffusion Modeling | NODDI (NDI, ODI) | Characterizing white matter microstructure, axon density, orientation dispersion | Pregnancy neuroplasticity study [97] |
| Hormonal Assays | Salivary progesterone, estradiol | Linking endocrine changes to neural reorganization | Pregnancy study [97] |
| Clinical Measures | LSAS-SR, CGI-I, MADRS-S | Quantifying symptom changes in clinical populations | Social anxiety disorder trial [95] |
| Cognitive Tasks | Public speaking task, self-referential criticism paradigm | Eliciting condition-specific neural responses | Social anxiety fMRI study [95] |
| Data Resources | Dallas Lifespan Brain Study dataset | Access to longitudinal brain aging data across adulthood | DLBS repository [96] |
Methodological Challenges and Solutions
Longitudinal neuroplasticity research presents several unique methodological challenges that require careful consideration:
Data Quality and Consistency
Aging technologies and methods present a significant challenge in longitudinal studies spanning several years. As new methods become available (e.g., updates to DSM criteria, cognitive tests, MRI scanners), researchers must either ignore latest techniques to maintain measurement comparability or invest substantial effort in data harmonization across different waves [94]. One solution involves conducting pilot studies assessing the same participants using different techniques to establish cross-walk algorithms between measurement approaches.
Missing data occurs frequently in longitudinal designs as participants miss assessment waves. Attrition rates accumulate across waves, resulting in decreased statistical power and potential selection bias if participants with the most severe symptoms or declines are more likely to drop out [94]. Modern statistical approaches like full information maximum likelihood and multiple imputation can help address missing data under missing at random assumptions, but proactive retention strategies remain essential.
Measurement Intervals and Practice Effects
The choice of follow-up intervals and number of repeated measurements represents a critical design consideration. Measurement points should be spaced to capture important developmental changes while considering participant burden and costs [94]. Different neuroplastic processes operate on different timescales—from rapid changes occurring within single training sessions to slow structural changes accumulating over years—requiring careful alignment of assessment frequency with research questions.
Practice effects can confound longitudinal assessment, particularly for cognitive measures. Solutions include creating alternate test forms, extending intervals between administrations, and using tasks with limited ceiling effects. In neuroimaging, habituation to scanning environments and tasks must be considered when interpreting longitudinal changes.
Longitudinal and single-case study designs provide indispensable methodological approaches for understanding the dynamics of neuroplasticity across the lifespan. These designs reveal that brain development and adaptation follow individualized trajectories that cannot be fully captured by cross-sectional approaches. The integration of quantitative neuroimaging methods with repeated assessments allows researchers to link microstructural neural changes to behavioral adaptation and performance optimization.
Future directions in this field include:
- Multi-scale longitudinal studies connecting molecular, cellular, systems, and behavioral levels of analysis
- High-frequency assessment designs capturing rapid plasticity processes in response to targeted interventions
- Integration of multimodal data streams including genetics, neuroimaging, behavioral monitoring, and environmental measures
- Analytic advances for modeling complex, individualized change trajectories and cross-level interactions
As research in this field progresses, longitudinal and single-case designs will continue to illuminate how experience-driven neuroplasticity supports behavioral adaptation, performance optimization, and recovery from neurological and psychiatric conditions. These insights will inform the development of precisely timed interventions that harness the brain's inherent capacity for change to enhance human functioning across the lifespan.
The journey from laboratory discoveries to clinical applications, the "bench-to-bedside" pipeline, represents a critical pathway for advancing human health. Within neuroscience, this process is intricately linked to understanding neuroplasticity—the brain's remarkable capacity to adapt its structure and function in response to experience, injury, or therapeutic intervention. Neuroplasticity serves as the fundamental biological substrate for both species-general functions and individualized skill acquisition and behavioral adaptation [99]. However, the translation of preclinical findings to human applications faces significant challenges, particularly because the brain's plastic potential evolves across the lifespan. Aging brings profound changes to neural systems, including reduced synaptic flexibility, altered immune responses, and decreased neurogenesis, all of which impact the brain's resilience to injury and response to treatments [100]. This whitepaper examines strategic frameworks and methodological innovations for enhancing preclinical model evaluation, with particular emphasis on their applicability to human neuroplasticity and optimal performance research.
The imperative for robust translational models is especially pressing in developing interventions for age-related neurological conditions. Older individuals demonstrate increased susceptibility to stroke and traumatic brain injury, with age-related differences in brain plasticity significantly affecting recovery and treatment responses [100]. This reality necessitates preclinical models that accurately recapitulate the aging human brain's biological landscape rather than relying exclusively on young, healthy animals. Furthermore, as research explores interventions to enhance performance in healthy individuals, understanding the boundaries and facilitators of neuroplasticity across different physiological contexts becomes paramount.
Quantitative Frameworks for Preclinical Translation
Foundational Principles of Quantitative Biology
Technological advancements and emerging high-throughput molecular data have transformed biology into a more quantitative and multidisciplinary discipline. Quantitative chemical biology research aims to model the pharmacokinetics and pharmacodynamics of chemicals in diseased patients through more tractable in vitro systems initially [101]. This approach has generated immense promise in cancer research, where modeling drug response through high-throughput screening is followed by identifying candidate biomarkers, signaling pathways, and molecular targets. The same quantitative principles apply to neuroscience research, particularly in predicting how interventions targeting neuroplasticity might translate across species.
A core component of quantitative biology involves modeling dose-response relationships using mathematical frameworks that describe biological interactions. The Michaelis-Menten model provides a fundamental mathematical framework for enzyme-ligand or enzyme-substrate binding and catalysis, described by the equation:
v = ([S]V~max~)/([S] + K~m~)
where v represents reaction velocity, [S] is substrate concentration, V~max~ is maximum velocity, and K~m~ is the Michaelis constant [101]. This model illustrates the saturable nature of biological systems, a concept equally relevant to understanding receptor binding in neuropharmacology. For interventions targeting neuroplasticity, understanding these saturation points is crucial for establishing therapeutic windows that maximize benefit while minimizing adverse effects.
Experimental Design for Robust Quantification
Well-designed concentration-response experiments form the bedrock of quantitative translational research. Key criteria for generating reliable data include:
- Defined plateaus: Establishing well-defined top and bottom plateau values requires sufficient range of inhibitor concentrations [101]
- Adequate data points: Utilizing a minimum of 8-10 concentration data points spaced equally for accurate IC~50~ determination [101]
- Replication: Including at least three biological replicates for each data point to ensure statistical robustness [101]
- Controlled conditions: Maintaining constant enzyme concentration across experiments, with the lower limit for determining IC~50~ being half of the enzyme concentration [101]
These principles extend beyond pure pharmacology to complex interventions targeting neuroplasticity, including neuromodulation, cognitive training, and lifestyle interventions. In these contexts, "dose" may encompass parameters such as stimulation intensity, training duration, or intervention frequency, while "response" could include molecular, physiological, and behavioral outcomes.
Table 1: Quantitative Parameters in Preclinical Research
| Parameter | Definition | Translational Significance |
|---|---|---|
| IC~50~ | Inhibitor concentration yielding 50% inhibition of maximal activity | Predicts therapeutic dosing range; establishes potency comparisons |
| EC~50~ | Effective concentration to reach 50% of maximal activity | Indicates functional potency for agonists or enhancers |
| K~m~ | Michaelis constant; substrate concentration at half-maximal velocity | Quantifies enzyme-substrate affinity; informs substrate competition |
| V~max~ | Maximum reaction rate when enzyme is saturated with substrate | Reflects catalytic efficiency and capacity of biological systems |
| Hill Coefficient | Quantifies cooperativity in multi-subunit interactions | Indicates steepness of dose-response relationship; informs mechanism |
Advanced Imaging Technologies in Preclinical Research
Preclinical Ultrasound Imaging
Ultrasound imaging has evolved into a powerful preclinical tool providing real-time, quantitative anatomical and physiological information. Technological advances have overcome initial challenges related to the smaller size and rapid conscious heart rates of animal models, with spatial resolutions now approaching 30 microns and frame rates up to 350 Hz for cardiac imaging in mice [102]. These capabilities enable detailed characterization of structural and functional changes associated with neuroplastic interventions.
Multiple imaging modes enhance the utility of preclinical ultrasound:
- B-mode (Brightness-mode): Provides two-dimensional cross-sectional images in real-time, ideal for anatomical reference and tracking structural changes [102]
- M-mode (Motion-mode): Captures data along a single line with high temporal resolution, perfect for studying fast-moving structures like vessel walls or cardiac cycles [102]
- Doppler techniques: Measure blood flow velocity based on frequency shifts, enabling quantification of cerebral blood flow changes associated with neural activity [102]
- 3D and 4D imaging: Reconstructs three-dimensional volumes through sequential B-mode acquisition, with 4D adding temporal resolution to capture dynamic processes [102]
These applications are particularly relevant for neuroplasticity research, where vascular changes often parallel neural reorganization. Ultrasound can monitor neurovascular coupling—the fundamental relationship between neural activity and cerebral blood flow—that underpins many plasticity mechanisms.
Emerging Imaging Modalities
Beyond conventional ultrasound, several emerging technologies show significant promise for enhancing preclinical evaluation:
Photoacoustic imaging combines optical excitation with acoustic detection, providing spectroscopic information based on endogenous contrast agents like hemoglobin. This allows quantification of oxygen saturation (sO~2~), hemoglobin concentration, and blood flow dynamics [103]. For neuroplasticity research, this enables non-invasive monitoring of metabolic changes associated with learning, adaptation, and recovery from injury.
Radiomics represents a paradigm shift in image analysis, converting medical images into mineable high-dimensional data. By extracting numerous quantitative features from images, radiomics can identify subtle patterns not discernible through visual inspection alone [104]. In preclinical research, radiomic features (RFs) can be correlated with histological and behavioral outcomes to develop predictive models for treatment response. This approach is particularly valuable for capturing the heterogeneity of plastic responses across individuals.
Table 2: Preclinical Imaging Modalities for Neuroplasticity Research
| Modality | Key Applications | Spatial Resolution | Translational Value |
|---|---|---|---|
| High-Frequency Ultrasound | Real-time cardiac imaging, blood flow measurement, vascular dynamics | 30-100 μm | Direct clinical counterpart; non-invasive longitudinal monitoring |
| Photoacoustic Imaging | Oxygen saturation mapping, hemoglobin concentration, metabolic activity | 10-500 μm | Provides functional metabolic data without exogenous contrast |
| Micro-CT | Bone metastasis monitoring, vascular imaging (with contrast) | 1-50 μm | High-resolution structural data; excellent for bone and vascular research |
| MR Spectroscopy | Metabolic profiling, neurotransmitter quantification, pH monitoring | Voxels: 0.7-1 cm³ | Non-invasive biochemical characterization relevant to plasticity |
| Radiomics | Tumor heterogeneity quantification, treatment response prediction, phenotype classification | Pixel/voxel level | High-dimensional data extraction; identifies subvisual patterns |
Integrative Approaches for Cross-Species Translation
Bridging Macroscopic and Microscopic Measures
A significant challenge in translational neuroscience lies in connecting macroscopic observations from human neuroimaging with microscopic mechanisms accessible in animal models. To address this gap, researchers propose strengthening the dialogue between human and animal research through complementary approaches [99]:
- Enhancing interpretability of macroscopic methods by correlating them with molecular and fine-structural measures in the same animals
- Cross-species research programs using either well-controlled experimental paradigms (e.g., motor skill acquisition) or naturalistic environments
- Conceptual and computational models linking molecular events to macroscopic phenomena [99]
These approaches are particularly relevant for neuroplasticity research, where mechanisms operating at synaptic, cellular, and network levels collectively give rise to behavioral adaptations. For example, studying motor skill learning across species using comparable macroscopic metrics (e.g., fMRI in humans and functional ultrasound in rodents) while examining underlying synaptic changes in animal models can reveal conserved principles of plastic reorganization.
Reverse Translation and Clinical Data Integration
The traditional "bench-to-bedside" pipeline is usefully complemented by reverse translation—the process of using clinical observations to inform preclinical research [105]. This approach leverages existing clinical data to refine animal models and experimental questions, creating a more iterative and efficient research cycle. Quantitative clinical pharmacology plays a crucial role in this process by applying mathematical models to clinical trial and real-world data, generating knowledge that can refine preclinical models [105].
In the context of neuroplasticity, reverse translation might involve using neuroimaging findings from patients who showed exceptional recovery after stroke to design targeted interventions in animal models. Similarly, observations from expert performers (athletes, musicians) could inform studies examining the limits of experience-dependent plasticity in model systems.
Specialized Methodologies for Targeted Applications
Intraoperative Nerve Visualization
The NerveSense device exemplifies how targeted technological innovation can address specific translational challenges. This handheld imaging device uses polarized light to selectively illuminate myelinated axons based on their birefringent properties, producing real-time, dye-free visualization of peripheral nerves [106]. The system employs multiple polarization states to capture tissue-specific signatures, with nerves exhibiting a characteristic double-peak signature distinct from surrounding tissues [106].
This technology addresses a critical clinical need, as iatrogenic nerve injury remains a significant surgical complication, approaching 40% in revision cases or anatomically complex regions [106]. By enhancing intraoperative nerve visualization, the device has potential to improve surgical outcomes—a relevant consideration for neuroplasticity, as unintended nerve damage can trigger maladaptive plastic changes. The planned Phase 1 clinical trial in 2026 will assess usability, safety, and integration into surgical workflows [106].
Extracellular Vesicles as Therapeutic and Diagnostic Tools
Extracellular vesicles (EVs) have emerged as promising therapeutic tools for promoting brain repair, particularly given their role in intercellular communication and ability to cross the blood-brain barrier [100]. These nanometer-sized vesicles are secreted by virtually all neural cell types and carry diverse cargoes of proteins, lipids, and nucleic acids that can modulate recipient cell function [100].
Critically for translational research, EV efficacy is influenced by donor age—those derived from young stem cells exhibit more regenerative profiles, while aged donor EVs may carry senescence-related signals that impede recovery [100]. This finding highlights the importance of considering age-matching in preclinical studies aimed at clinical translation, especially for conditions affecting predominantly older adults.
EVs contribute to neural repair through multiple mechanisms:
- Mediating transfer of miRNAs that regulate astrocyte metabolic functions [100]
- Delivering neuroprotective factors like neuroglobin from astrocytes to neurons [100]
- Facilitating clearance of myelin debris through microglial uptake of oligodendrocyte-derived EVs [100]
- Supporting synaptic plasticity through delivery of synaptic modulators like miR-132, miR-124, and miR-324 [100]
These mechanisms position EVs as both therapeutic agents and natural mediators of plasticity, offering promising avenues for enhancing recovery after neural injury.
Methodological Protocols for Key Experiments
Preclinical Ultrasound Imaging Protocol
Comprehensive ultrasound assessment in rodent models follows a standardized protocol:
Animal Preparation:
- Anesthetize animals according to approved protocols
- Remove hair from scanning area using electric clippers followed by depilatory cream
- Apply warmed coupling gel to ensure acoustic contact without trapping air bubbles
- Maintain body temperature throughout imaging procedure [102]
Transducer Selection:
- For adult rats: 15-20 MHz transducer (image depth 3-4 cm)
- For adult mice: 30-40 MHz transducer (image depth 10-20 mm)
- For neonatal mice and zebrafish: up to 50 MHz (image depth 9 mm) [102]
Image Acquisition:
- Mount transducer in probe-holder with 3D versatile movement to minimize operator movement
- Position transducer without touching the animal, scanning through a thin gel layer
- For B-mode imaging: Acquire 2D cross-sectional images with focus set at depth of interest
- For M-mode: Select single line intersecting structures of interest for high-temporal resolution
- For Doppler: Align beam with blood flow direction or apply angle correction [102]
Image Analysis:
- Use manufacturer software or open-source alternatives for quantification
- For cardiac function: Measure chamber dimensions, wall thickness, fractional shortening
- For vascular studies: Quantify flow velocities, resistance indices, and velocity-time integrals
This protocol enables longitudinal monitoring of structural and functional changes, providing valuable data on disease progression and treatment response relevant to neuroplasticity.
Radiomics Analysis Pipeline
The radiomics workflow involves several standardized steps:
Image Acquisition and Preprocessing:
- Acquire images using appropriate modality (CT, MRI, US, PET, SPECT)
- Apply artifact correction, image registration, and intensity normalization
- Implement noise reduction algorithms as needed [104]
Image Segmentation:
- Define regions of interest (ROIs) manually or using semi-automated tools
- Utilize software platforms like 3D Slicer, ITK-SNAP, or VivoQuant
- Create binary masks where value is 1 inside ROI and 0 outside [104]
Feature Extraction:
- Use standardized software like PyRadiomics (Python-based open-source package)
- Extract features across categories:
- Shape-based: Describe geometric properties of ROI
- First-order: Derived from image histogram (e.g., mean, median, entropy)
- Texture: Quantify spatial patterns (GLCM, GLRLM, GLSZM, NGTDM, GLDM) [104]
Statistical Analysis:
- Normalize features to consistent scale
- Perform correlation analysis with outcomes of interest
- Implement machine learning for classification or predictive modeling
- Apply feature selection to reduce dimensionality and avoid overfitting [104]
This computational approach extends the utility of standard imaging by extracting subvisual patterns that may correlate with underlying biological processes, including neuroplastic changes.
Research Reagent Solutions for Translational Neuroscience
Table 3: Essential Research Reagents for Neuroplasticity Studies
| Reagent/Category | Specific Examples | Research Application | Translational Value |
|---|---|---|---|
| Extracellular Vesicles | MSC-derived EVs, neuronal exosomes, astrocyte-derived EVs | Intercellular communication studies, therapeutic delivery vehicles | Naturally cross BBB; modifiable cargo; cell-free therapeutic approach |
| Contrast Agents | Microbubbles (ultrasound), nanoparticulate contrast (CT), Gd-based (MRI) | Vascular imaging, perfusion assessment, target visualization | Clinical counterparts available; facilitate multimodal imaging |
| Molecular Probes | Senolytics, metabolic tracers, neurotransmitter analogs | Target validation, pathway analysis, mechanism of action studies | Bridge molecular and systems-level observations; clinical analogs |
| Polarization Imaging | NerveSense device, custom polarization setups | Myelinated axon visualization, surgical guidance, nerve integrity assessment | Label-free technique; real-time intraoperative application |
| Radiomics Software | PyRadiomics, 3D Slicer, custom Matlab code | High-dimensional feature extraction, pattern recognition, predictive modeling | Standardized feature extraction; compatible with clinical pipelines |
Visualization of Translational Workflows
Integrated Bench-to-Bedside Pipeline
Neuroplasticity Assessment Methodology
Effective bench-to-bedside translation requires meticulous attention to how preclinical models recapitulate the human condition, particularly for neuroplasticity research where age-related changes significantly impact treatment responses. The aging brain exhibits reduced mitochondrial efficiency, blood-brain barrier integrity, and immune regulation, all contributing to diminished plastic potential [100]. These physiological realities necessitate incorporating aged animal models in preclinical research and developing age-tailored strategies that reflect the unique biological landscape of older individuals [100].
Future progress will depend on strengthening the dialogue between human and animal research through dedicated cross-species research programs, better integration of macroscopic and microscopic measures, and computational models linking molecular events to observable phenomena [99]. By embracing quantitative frameworks, advanced imaging technologies, and reverse translation approaches, researchers can enhance the predictive validity of preclinical studies and accelerate the development of interventions that harness neuroplasticity for improved human health and performance across the lifespan.
The pursuit of optimal performance and adaptive behavior represents a central challenge in neuroscience and therapeutic development. Research now conclusively demonstrates that neuroplasticity—the brain's capacity to reorganize its structure, function, and connections in response to experience—serves as the fundamental biological mechanism underlying behavioral adaptation [50] [34]. impairments in neuroplasticity are increasingly recognized as core deficits in numerous neuropsychiatric disorders, including depression, where they manifest as cognitive inflexibility and rigid negative biases that maintain pathological states [50]. This whitepaper synthesizes current scientific evidence to present a integrated framework for designing multimodal interventions that leverage synergistic plasticity mechanisms to enhance behavioral outcomes beyond what unimodal approaches can achieve.
The conventional therapeutic paradigm has predominantly focused on single-modality interventions, whether pharmacological, behavioral, or technological. However, emerging data suggests that robust enhancement of neuroplasticity through biological or somatic treatments creates critical "windows of opportunity" wherein targeted cognitive or behavioral interventions can be more effectively integrated and consolidated [50]. This temporal synergy represents the cornerstone of next-generation neuroplasticity-based interventions. The future of cognitive enhancement and therapeutic development therefore lies in the strategic combination of complementary modalities—including pharmacological agents, brain stimulation, physical exercise, and technology-enhanced learning protocols—to engage multiple neuroplastic mechanisms simultaneously for superior and sustained outcomes.
Neurobiological Foundations of Multimodal Synergy
Core Neuroplasticity Mechanisms
At the molecular and cellular level, neuroplasticity encompasses a range of adaptive processes that can be strategically targeted by different intervention modalities. Synaptic plasticity refers to activity-dependent changes in synaptic strength and structure, including long-term potentiation (LTP) and long-term depression (LTD), which represent the primary cellular mechanisms underlying learning and memory [50] [34]. Structural plasticity involves physical changes to neuronal morphology, including the formation and elimination of dendritic spines, axonal branching, and neurogenesis [50] [107]. At the systems level, network plasticity encompasses the reorganization of functional brain networks through changes in connectivity and communication between distinct neural populations [108].
Multimodal approaches achieve synergy by concurrently engaging these complementary plasticity mechanisms. For instance, while certain pharmacological agents may enhance synaptic plasticity by increasing neuronal excitability or growth factor expression, physical exercise may simultaneously promote structural plasticity through angiogenesis and neurogenesis, and cognitive training may guide network plasticity through experience-dependent refinement of neural circuits [109]. The integration of these modalities creates conditions where the brain is both primed for change and provided with the appropriate contextual experiences to consolidate adaptive neural configurations.
Key Molecular Pathways and Targets
Table 1: Key Molecular Pathways in Neuroplasticity and Their Modulation by Different Interventions
| Molecular Pathway | Function in Plasticity | Modulating Interventions |
|---|---|---|
| BDNF Signaling | Promotes neuronal survival, differentiation, synaptic strength; enhances learning and memory | Exercise, ketamine, antidepressants, cognitive training [50] [72] |
| NMDA Receptor Activation | Critical for LTP induction; gates experience-dependent plasticity | Ketamine, D-cycloserine, glutamate modulators [50] |
| 5-HT2A Receptor Signaling | Promotes dendritic spine growth; enhances cortical connectivity | Classical psychedelics (e.g., psilocybin, 25CN-NBOH) [107] |
| Dopaminergic Reward Pathways | Reinforces adaptive behaviors; facilitates memory consolidation | Multisensory learning, behavioral activation, reward-based learning [108] |
The diagram below illustrates the convergent signaling pathways through which different intervention modalities promote neuroplasticity and behavioral adaptation:
Diagram 1: Convergent signaling pathways in multimodal neuroplasticity interventions. Different modalities target complementary molecular pathways that collectively enhance multiple neuroplasticity processes, leading to superior behavioral outcomes compared to unimodal approaches.
Recent groundbreaking research has expanded our understanding of how different interventions engage these molecular pathways. Notably, studies on classical psychedelics have revealed that psychedelic-induced neuroplasticity can occur even in cortical neurons lacking postsynaptic 5-HT2A receptors, suggesting these compounds act through both direct postsynaptic mechanisms and potentially through presynaptic receptors on thalamocortical inputs [107]. This discovery significantly expands the potential therapeutic targets for psychedelic medicine and illustrates the complexity of neuroplasticity mechanisms engaged by different intervention modalities.
Multimodal Integration Strategies: Evidence and Protocols
Biological-Behavioral Synergy in Depression Treatment
The combination of rapid-acting plasticity-enhancing biological interventions with cognitive-behavioral therapies represents a particularly promising approach for treatment-resistant depression. Research demonstrates that interventions like ketamine infusion, electroconvulsive therapy (ECT), and repetitive transcranial magnetic stimulation (rTMS) induce potent acute neuroplastic effects that can reverse the neuronal atrophy and synaptic depression characteristic of chronic stress and depression pathophysiology [50]. When administered as monotherapies, these interventions often produce transient benefits, with symptom return frequently occurring after treatment discontinuation.
The strategic integration of cognitive-behavioral interventions during the window of enhanced plasticity following biological treatments demonstrates significantly improved long-term outcomes:
Table 2: Biological-Behavioral Combination Approaches for Enhanced Outcomes in Depression
| Biological Intervention | Plasticity Effects | Combined Behavioral Intervention | Synergistic Benefits |
|---|---|---|---|
| Ketamine (NMDA antagonist) | Rapid synaptic strengthening; increased spine density; enhanced cognitive flexibility [50] | Cognitive Behavioral Therapy (CBT) during the post-infusion window | Extended antidepressant effects; reduced relapse; improved emotion regulation skills [50] |
| Electroconvulsive Therapy (ECT) | Potent acute plasticity enhancement; hippocampal neurogenesis; network reorganization [50] | Behavioral Activation Therapy following treatment course | Consolidation of neuroplastic gains; transfer of improved flexibility to daily life [50] |
| Transcranial Direct Current Stimulation (tDCS) | Increased cortical excitability; enhanced LTP-like plasticity; modulated network connectivity [109] | Computerized Cognitive Training during stimulation | Enhanced learning rates; greater transfer to untrained cognitive domains; longer maintenance of benefits [109] |
The following experimental workflow illustrates a protocol for combining ketamine with cognitive remediation to achieve synergistic effects:
Diagram 2: Experimental protocol for combining biological and behavioral interventions. The critical feature is the timing of behavioral interventions during the window of enhanced neuroplasticity following biological treatment to maximize consolidation of adaptive learning.
Exercise-Cognition- Stimulation Triad for Cognitive Enhancement
A comprehensive 4-month randomized controlled trial with 318 healthy young adults demonstrated the superior efficacy of multimodal training compared to unimodal interventions [109]. Participants were assigned to one of five conditions: (1) computer-based cognitive training alone, (2) cognitive and physical exercise training, (3) cognitive training combined with tDCS and physical exercise, (4) active control training, or (5) passive control. The findings revealed that multimodal training significantly enhanced learning relative to computer-based cognitive training alone and provided an effective method to promote skill learning across multiple cognitive domains, including executive functions, working memory, and planning and problem-solving [109].
The specific protocols for each intervention component were as follows:
Physical Exercise Training: Participants completed 28 group exercise sessions incorporating high-intensity cardiovascular and resistance training (HICRT). Sessions included dynamic stretching, walk/run portions varying in time and distance, HICRT protocols split into segments with exercises involving bodyweight, resistance bands, kettlebells, and suspension training, followed by drills with equipment like battle ropes, sandbags, and medicine balls [109].
Cognitive Training: The computer-based training consisted of six adaptive tasks targeting executive functions and working memory, administered for approximately 10 minutes per task per session using tablets. Tasks were designed to be adaptive both within and across sessions to maintain optimal challenge levels [109].
Non-Invasive Brain Stimulation: The active tDCS group received "high-definition" electrode montages (HD-tDCS) precisely targeting the dorsolateral prefrontal cortex by sending weak current from two small anodes on the left and right side of the front of the head to two receiving cathodes on the back of the head [109].
The synergistic benefits of this multimodal approach were substantial, with the combined exercise, stimulation, and games (ESG) group demonstrating superior learning trajectories and broader transfer effects compared to all other conditions. This suggests that physical exercise may prime the brain for subsequent enhancement via cognitive training, potentially through exercise-induced neurogenesis and long-term potentiation, while tDCS may further enhance plasticity and strengthen task-related cortical networks during cognitive engagement [109].
Technology-Enhanced Multisensory Learning Approaches
In educational and cognitive enhancement contexts, technology-enabled multisensory learning approaches leverage neuroplasticity principles to optimize outcomes. Research on second language acquisition in adults demonstrates that brain-inspired multisensory learning—which integrates visual, auditory, and kinesthetic modalities within authentic social contexts—engages distributed neural networks simultaneously, resulting in more robust neuroplastic adaptations [108]. These approaches are particularly effective when they incorporate:
- Immersion intensity: Creating environments ranging from limited classroom contact to complete environmental immersion
- Multimodal design: Integrating complementary sensory inputs to strengthen neural connections between language processing regions and sensorimotor areas
- Social interaction components: Activating mirror neuron systems and theory-of-mind networks to enhance pragmatic understanding
- Real-time adaptation: Using continuous performance data to dynamically adjust difficulty and content presentation [108]
Neuroimaging studies confirm that such multisensory approaches induce specific neuroplastic adaptations, including enhanced connectivity between language and executive networks, increased cortical thickness in frontal-temporal regions, and white matter reorganization supporting processing efficiency [108]. These neural changes correlate with significant improvements in working memory, attentional control, and cognitive flexibility.
Similar principles are being applied through advanced analytics platforms that use multimodal data integration to optimize learning environments. These systems employ deep temporal convolution networks and sophisticated algorithms to process audio, video, and textual data from learners, enabling real-time adaptation of educational content based on neurocognitive and behavioral metrics [110]. This approach represents the practical application of neuroplasticity principles to create dynamically optimized learning environments.
Experimental Protocols for Multimodal Research
Protocol 1: Combined Ketamine and Cognitive Remediation for Depression
Objective: To evaluate whether cognitive behavioral therapy administered during the window of enhanced neuroplasticity following ketamine infusion extends and enhances antidepressant effects.
Participants: Adults (18-65) with treatment-resistant major depressive disorder, currently experiencing a major depressive episode of at least 4 weeks duration.
Exclusion Criteria: History of psychosis, bipolar disorder, substance use disorder in past 6 months, contraindications to ketamine, pregnancy.
Intervention Protocol:
- Ketamine Administration: Single subanesthetic dose (0.5 mg/kg) administered via intravenous infusion over 40 minutes in a controlled clinical setting [50].
- CBT Initiation: First cognitive behavioral therapy session administered 24 hours post-infusion, during the period of peak neuroplastic effects.
- CBT Continuation: Seven additional CBT sessions administered twice weekly for four weeks, focusing on cognitive restructuring, behavioral activation, and emotion regulation skills.
- Assessment Timeline: Baseline, 24 hours post-infusion, 1 week, 2 weeks, 4 weeks, 8 weeks, and 12 weeks post-infusion.
Primary Outcome Measures: Montgomery-Åsberg Depression Rating Scale (MADRS) scores, cognitive flexibility measures (Wisconsin Card Sorting Test), and neuroimaging markers of functional connectivity.
Mechanistic Assessments: Blood samples for BDNF levels at baseline, 24 hours, and 4 weeks; resting-state fMRI at baseline and 4 weeks to assess network connectivity changes.
Protocol 2: Multimodal Cognitive Enhancement in Healthy Adults
Objective: To investigate synergistic effects of combined physical exercise, cognitive training, and non-invasive brain stimulation on cognitive performance in healthy young adults.
Participants: Healthy adults (18-35) with no neurological or psychiatric history, not currently engaged in regular exercise (>1x/week).
Study Design: 16-week randomized controlled trial with five conditions:
- Computer-based cognitive training only (Games)
- Cognitive training + physical exercise (EG)
- Cognitive training + physical exercise + tDCS (ESG)
- Active control training (AC)
- Passive control (PC)
Intervention Components:
- Physical Exercise: 28 supervised group exercise sessions over 16 weeks, incorporating high-intensity cardiovascular and resistance training. Sessions include warm-up, walk/run portion, HICRT protocol, drills/skills portion, and cool-down [109].
- Cognitive Training: 20 sessions of six adaptive cognitive games targeting executive functions and working memory, with difficulty adjusting to maintain ~80% accuracy [109].
- tDCS Protocol: Active HD-tDCS administered during cognitive training sessions for ESG group, with anodal electrodes over left and right dorsolateral prefrontal cortex (F3/F4), cathodes over contralateral supraorbital areas, 2mA current for 20 minutes [109].
Assessment Measures:
- Cognitive Battery: Executive function (Stroop, Task Switching), working memory (Operation Span, N-back), episodic memory (Rey Auditory Verbal Learning Test), planning and problem solving (Tower of London).
- Fitness Measures: VO2 max test at baseline and post-intervention.
- Neurophysiological Measures: Resting-state EEG, transcranial magnetic stimulation measures of cortical excitability (in subgroup).
Table 3: Research Reagent Solutions for Multimodal Neuroplasticity Studies
| Reagent/Resource | Function/Application | Example Use Cases |
|---|---|---|
| Htr2a-floxed (Htr2afl) Mice | Conditional knockout model for precise manipulation of 5-HT2A receptor expression; enables cell-type-specific interrogation of psychedelic effects [107] | Studying psychedelic-induced plasticity in 5-HT2A receptor-lacking cortical regions; dissecting presynaptic vs. postsynaptic mechanisms [107] |
| 25CN-NBOH | Selective 5-HT2A receptor agonist; research tool for precise investigation of 5-HT2A receptor-mediated plasticity mechanisms [107] | Probing structural and functional neuroplasticity; establishing dose-response relationships for spinogenesis [107] |
| High-Definition tDCS (HD-tDCS) | Non-invasive brain stimulation with focused current delivery; enables precise targeting of cortical regions with minimal diffusion [109] | Enhancing cortical excitability during cognitive training; investigating timing-dependent effects on learning consolidation [109] |
| Multimodal Learning Analytics Platforms | Integrated systems for capturing, processing, and analyzing multiple data streams (eye tracking, physiological sensors, behavioral metrics) [110] | Investigating real-time learning processes; developing personalized adaptation algorithms; identifying neurobehavioral markers of optimal performance [110] |
| RNAScope Technology | Advanced in situ hybridization for precise localization and quantification of gene expression with single-molecule sensitivity [107] | Validating genetic manipulations; mapping receptor distribution patterns; confirming cell-type-specific expression [107] |
The integration of multimodal approaches represents a paradigm shift in neuroplasticity-based interventions for enhanced behavioral adaptation and optimal performance. The evidence consistently demonstrates that strategic combination of complementary interventions—pharmacological, somatic, behavioral, and technological—produces synergistic effects that exceed what can be achieved through unimodal approaches. The critical mechanistic insight underpinning this advantage is that different interventions engage distinct yet complementary neuroplasticity mechanisms, creating conditions where the brain is simultaneously primed for change and provided with contextually appropriate experiences to consolidate adaptive neural configurations.
Future research directions should prioritize several key areas:
- Temporal Optimization: More precise mapping of the timing and duration of enhanced plasticity windows following different biological interventions to optimally schedule complementary behavioral components.
- Personalized Approaches: Development of biomarkers and profiling tools to match individuals with the specific multimodal combinations most likely to benefit their unique neurocognitive profile and goals.
- Mechanistic Elucidation: Continued investigation into the molecular and systems-level mechanisms through which different interventions interact, including the recently discovered presynaptic mechanisms of psychedelic-induced plasticity [107].
- Technology Integration: Leveraging advances in digital biomarkers, wearable sensors, and artificial intelligence to create dynamically adaptive multimodal interventions that respond in real-time to individual neurobehavioral states.
As these fields continue to converge and evolve, the strategic integration of multimodal approaches promises to transform our ability to enhance human cognition, treat neuropsychiatric disorders, and ultimately unlock the full potential of experience-dependent neuroplasticity for optimal human functioning.
Conclusion
The evidence consolidated from foundational mechanisms to clinical applications firmly establishes neuroplasticity as the central pillar for behavioral adaptation and the pursuit of optimal performance. The translation of this knowledge into clinical practice and drug development is paramount. Future research must focus on personalized intervention protocols that combine multimodal approaches—integrating behavioral training, neuromodulation, and pharmacotherapy. A key frontier lies in refining non-invasive biomarkers to precisely monitor plasticity in real-time, enabling dynamic treatment adjustment. For biomedical and clinical research, this synthesis underscores a paradigm shift towards therapies that do not merely manage symptoms but actively remodel neural networks to restore and enhance function, opening new pathways for treating a spectrum of neurological and psychiatric disorders.
References
- 1. Neuroplasticity - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK557811/]
- 2. Neuroplasticity - Wikipedia [https://en.wikipedia.org/wiki/Neuroplasticity]
- 3. Optimizing Brain Performance: Identifying mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8112903/]
- 4. Neuroplasticity of Brain Networks Through Exercise [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390317/]
- 5. Neuroplasticity in Post-Stroke Aphasia: A Systematic Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8057712/]
- 6. Exploring brain plasticity with single-cell precision [https://www.jax.org/news-and-insights/2025/september/exploring-brain-plasticity-with-single-cell-precision]
- 7. Exploring the Role of Neuroplasticity in Development, ... [https://www.mdpi.com/2076-3425/13/12/1610]
- 8. Identifying mechanisms of adaptive neurobiological plasticity [https://pubmed.ncbi.nlm.nih.gov/31356835/]
- 9. Synaptic Plasticity: Multiple Forms, Functions, and ... [https://www.nature.com/articles/1301559]
- 10. Dendritic Spine Plasticity: Function and Mechanisms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7484486/]
- 11. Editorial: Glial cells in homeostasis, neurodevelopment, ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1575105/full]
- 12. Oligodendrocytes and myelination: pioneering new frontiers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319009/]
- 13. The role of glia cell in the neural mechanism of memory ... [https://www.sciencedirect.com/science/article/abs/pii/S0306452225010085]
- 14. Neural Stem Cell‐Derived Extracellular Vesicles for Advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308169/]
- 15. Neural xenografts contribute to long-term recovery in stroke ... [https://www.nature.com/articles/s41467-025-63725-3]
- 16. Exploring the Role of Neuroplasticity in Development, Aging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10741468/]
- 17. “Adaptive plasticity” grows your brain and makes learning ... [https://bigthink.com/neuropsych/3-steps-adaptive-plasticity-grow-brain-make-learning-easier/]
- 18. Adaptive Plasticity - (Intro to Cognitive Science) [https://fiveable.me/key-terms/introduction-cognitive-science/adaptive-plasticity]
- 19. Maladaptive Plasticity and Neuropathic Pain - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4748137/]
- 20. Adaptation and maladaptation: insights from brain plasticity [https://www.sciencedirect.com/science/article/abs/pii/B9780444537522000059]
- 21. Adaptive, maladaptive, neutral, or absent plasticity [https://pmc.ncbi.nlm.nih.gov/articles/PMC9923493/]
- 22. Scientists Find Potential New Drug Target for Psychiatric ... [https://www.hopkinsmedicine.org/news/newsroom/news-releases/2025/09/scientists-find-potential-new-drug-target-for-psychiatric-and-neurological-disorders]
- 23. The psychoplastogen tabernanthalog induces neuroplasticity ... [https://pubmed.ncbi.nlm.nih.gov/40760185/]
- 24. How adaptive plasticity evolves when selected against - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6426268/]
- 25. Why Is Neuroplasticity Important? The Science of Brain ... [https://shoresidetherapies.com/updates/why-is-neuroplasticity-important-the-science-of-brain-change-in-2025]
- 26. A new Pitt study has upended decades-old assumptions about ... [https://www.pittwire.pitt.edu/accolades-honors/2025/06/03/neuroscience-synaptic-transmission-science-advances]
- 27. Large-scale reorganization of the somatosensory cortex ... [https://www.nature.com/articles/ncomms4602]
- 28. A simple model for Behavioral Time Scale Synaptic ... [https://www.nature.com/articles/s41467-024-55563-6]
- 29. Distinct types of neural reorganization during long-term ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6485743/]
- 30. Network topological reorganization mechanisms of primary ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1678035/full]
- 31. Inferring neural activity before plasticity as a foundation for ... [https://www.nature.com/articles/s41593-023-01514-1]
- 32. BRAIN 2025: A Scientific Vision - BRAIN Initiative - NIH [http://braininitiative.nih.gov/vision/nih-brain-initiative-reports/brain-2025-scientific-vision]
- 33. EEG as a marker of brain plasticity in clinical applications [https://pubmed.ncbi.nlm.nih.gov/35034760/]
- 34. The neuroplastic brain: current breakthroughs and ... [https://www.sciencedirect.com/science/article/pii/S0006899325002021]
- 35. EEG Entropy as a Biomarker of Emotion Regulation and ... [https://www.sciencedirect.com/science/article/pii/S2667242125001721]
- 36. A Practical Guide for Generating Reproducible and ... [https://apertureneuro.org/article/85104-a-practical-guide-for-generating-reproducible-and-programmatic-neuroimaging-visualizations]
- 37. Beneficial effects of physical exercise on neuroplasticity and cognition - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0149763413001012]
- 38. Effects of Physical Exercise on Neuroplasticity and Brain Function: A Systematic Review in Human and Animal Studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7752270/]
- 39. Impact of Physical Exercise Alone or in Combination with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9954055/]
- 40. Training the brain: Fact and fad in cognitive and behavioral ... [https://www.sciencedirect.com/science/article/abs/pii/S0278262612000292]
- 41. Neuromodulation technologies improve functional recovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12220701/]
- 42. Application and future directions of brain-computer ... [https://www.sciencedirect.com/science/article/pii/S2589238X2500083X]
- 43. Is non-invasive neuromodulation a viable technique to ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2024.1341707/full]
- 44. U.S. Neurological Devices Market & Trends Analysis | 2025 ... [https://idataresearch.com/product/neurological-devices-market-united-states/]
- 45. a visualization analysis based on the Web of Science database [https://pmc.ncbi.nlm.nih.gov/articles/PMC12021822/]
- 46. Engineering and Technological Advancements in Repetitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11591941/]
- 47. Modulating neuroplasticity for chronic pain relief: noninvasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11958754/]
- 48. Neurotechnology & Brain-Computer Interfaces in 2025 [https://www.ambula.io/neurotechnology-brain-computer-interfaces-in-2025/]
- 49. Emerging techniques for precision neuromodulation [https://www.the-innovation.org/article/doi/10.59717/j.xinn-life.2025.100150]
- 50. Leveraging Neuroplasticity to Enhance Adaptive Learning [https://pmc.ncbi.nlm.nih.gov/articles/PMC6380941/]
- 51. The pharmacology of neuroplasticity induced by non-invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3487028/]
- 52. Getting started with tables | Archives of Public Health | Full Text [https://archpublichealth.biomedcentral.com/articles/10.1186/s13690-017-0180-1]
- 53. Neuroplasticity and Nervous System Recovery: Cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025631/]
- 54. Influencing factors related to stroke patients' rehabilitation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325052/]
- 55. Quantitative insights into stroke recovery utilizing delayed ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1568717/full]
- 56. A comprehensive review of rehabilitation approaches for ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1608645/full]
- 57. The effect of extended early rehabilitation on the treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12451451/]
- 58. Breakthrough study identifies potential treatment for ... [https://www.news-medical.net/news/20251027/Breakthrough-study-identifies-potential-treatment-for-schizophrenia-symptoms.aspx]
- 59. Advances in Spinal Cord Injury – Insights from AIM-SCI 2025 [https://www.imrpress.com/journal/JIN/special_issues/SCI2025]
- 60. Preclinical Studies of Neuroplasticity Following Experimental ... [https://pubmed.ncbi.nlm.nih.gov/31390969/]
- 61. Neuroplasticity in Rehab: How Your Brain Adapts After Injury [https://healixtherapy.com/neuroplasticity-brain-rehab/]
- 62. Neuroplasticity after Traumatic Brain Injury - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK326735/]
- 63. Precision Rehabilitation Through Mathematical Modeling [https://pubmed.ncbi.nlm.nih.gov/40734876/]
- 64. Identifying mechanisms of adaptive neurobiological plasticity [https://www.sciencedirect.com/science/article/abs/pii/S014976341930065X]
- 65. Reversing maladaptive plasticity in chronic pain | APS [https://psychology.org.au/inpsych/2016/august/day]
- 66. The mutually reinforcing dynamics between pain and stress [https://pmc.ncbi.nlm.nih.gov/articles/PMC11609167/]
- 67. Common Brain Mechanisms of Chronic Pain and Addiction [https://www.sciencedirect.com/science/article/pii/S0896627315010338]
- 68. Chronic stress-induced neuroplasticity in the prefrontal cortex [https://www.sciencedirect.com/science/article/abs/pii/S0006899325000198]
- 69. Co-occurrence of chronic pain and anxiety/depression ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10859853/]
- 70. Increasing Neuroplasticity to Bolster Chronic Pain Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC4824292/]
- 71. Modulating neuroplasticity for chronic pain relief [https://www.nature.com/articles/s12276-025-01409-0]
- 72. Enhancing action recognition in educational settings ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1588570/full]
- 73. Neuroplasticity [https://www.neuroskills.com/neuroplasticity/]
- 74. Identifying new blood biomarkers of neuroplasticity ... [https://www.nature.com/articles/s41598-025-21936-0]
- 75. Neuroplasticity-driven timing modulations revealed by ... [https://www.sciencedirect.com/science/article/pii/S1053811920309319]
- 76. Tips to leverage neuroplasticity to maintain cognitive ... [https://www.health.harvard.edu/mind-and-mood/tips-to-leverage-neuroplasticity-to-maintain-cognitive-fitness-as-you-age]
- 77. The mPFC molecular clock mediates the effects of sleep ... [https://www.nature.com/articles/s41380-025-03276-7]
- 78. The impact of sleep deprivation on cognitive function in ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1559969/full]
- 79. The Impact of Sleep Deprivation on Brain Fog, Cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12145483/]
- 80. Epigenetic regulation of brain development, plasticity, and ... [https://www.nature.com/articles/s41386-025-02179-z]
- 81. The Role of Genetic, Environmental, and Dietary Factors in ... [https://www.mdpi.com/1422-0067/26/3/1222]
- 82. Understanding and using quantitative genetic variation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2842708/]
- 83. Pharmacogenomics: The genetics of variable drug responses [https://pmc.ncbi.nlm.nih.gov/articles/PMC3093198/]
- 84. Genetic Impact on Prostate Anatomical Variability During ... [https://pubmed.ncbi.nlm.nih.gov/17669147/]
- 85. interrogating the human genome to identify drug pathways ... [https://www.nature.com/articles/s41397-019-0096-y]
- 86. Genetic Influences on Anatomy Understanding Variations ... [https://www.pulsus.com/scholarly-articles/genetic-influences-on-anatomy-understanding-variations-implications-and-applications-12847.html]
- 87. Anatomical Variability - an overview [https://www.sciencedirect.com/topics/engineering/anatomical-variability]
- 88. Comparative efficacy of neuromodulation and structured ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11300218/]
- 89. Comparative Efficacy of Neuromodulation and Structured ... [https://www.mdpi.com/2077-0383/13/15/4288]
- 90. Comparative efficacy and safety of pharmacological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7794037/]
- 91. Neuromodulation: Update on current practice and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11103215/]
- 92. Retrospective chart review demonstrating effectiveness of ... [https://www.nature.com/articles/s43856-025-00837-3]
- 93. Evidence-Based Staff Training: A Guide for Practitioners - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3592486/]
- 94. Unique opportunities and challenges of longitudinal ... [https://www.sciencedirect.com/science/article/abs/pii/S0896627325003125]
- 95. Neuroplasticity in response to cognitive behavior therapy ... [https://www.nature.com/articles/tp2015218]
- 96. Sharing of Lifespan Brain Study Data Expected To Light New ... [https://news.utdallas.edu/health-medicine/lifespan-brain-study-data-release-2025/]
- 97. Longitudinal investigation of neurobiological changes ... [https://www.nature.com/articles/s42003-024-07414-9]
- 98. Longitudinal Changes of Quantitative Brain Tissue Properties ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11868441/]
- 99. From animal models to human individuality: Integrative ... [https://www.sciencedirect.com/science/article/pii/S089662732400727X]
- 100. The age-associated decline in neuroplasticity and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12331653/]
- 101. Quantitative Framework for Bench-to-Bedside Cancer ... [https://www.mdpi.com/2072-6694/14/21/5254]
- 102. Preclinical Ultrasound Imaging—A Review of Techniques ... [https://www.frontiersin.org/journals/physics/articles/10.3389/fphy.2020.00124/full]
- 103. Niche preclinical and clinical applications of photoacoustic ... [https://www.sciencedirect.com/science/article/pii/S2213597923000861]
- 104. Radiomics in preclinical imaging research: methods ... [https://www.nature.com/articles/s44303-025-00104-z]
- 105. Bedside to Bench: Integrating Quantitative Clinical ... [https://pubmed.ncbi.nlm.nih.gov/29105747/]
- 106. A polarized light-based handheld device for real-time, dye ... [https://peripheralnerve.org/meeting/program/2026/P1.cgi]
- 107. Psychedelic neuroplasticity of cortical neurons lacking 5- ... [https://www.nature.com/articles/s41380-025-03257-w]
- 108. Brain-Inspired Multisensory Learning: A Systematic Review of Neuroplasticity and Cognitive Outcomes in Adult Multicultural and Second Language Acquisition [https://www.mdpi.com/2313-7673/10/6/397]
- 109. Enhanced Learning through Multimodal Training: Evidence from a Comprehensive Cognitive, Physical Fitness, and Neuroscience Intervention - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5517605/]
- 110. Multimodal learning analytics for students behavior ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417425017348]