The Lesion Method: A Foundational Tool for Causal Brain-Behavior Mapping in Neuroscience Research and Drug Development
This article provides a comprehensive analysis of the lesion method, a cornerstone technique in neuroscience for establishing causal links between brain structure and function.
The Lesion Method: A Foundational Tool for Causal Brain-Behavior Mapping in Neuroscience Research and Drug Development
Abstract
This article provides a comprehensive analysis of the lesion method, a cornerstone technique in neuroscience for establishing causal links between brain structure and function. Tailored for researchers, scientists, and drug development professionals, it explores the method's historical foundations and evolution, detailing its transition from classic case studies to modern, computationally-driven approaches like voxel-based lesion-symptom mapping (VLSM). The scope encompasses core methodologies, practical applications across cognitive and clinical domains, strategies for overcoming limitations such as lesion heterogeneity and compensatory plasticity, and a comparative evaluation against other neuroimaging and neuromodulation techniques. By synthesizing recent advances and future directions, this review underscores the method's indispensable role in validating therapeutic targets and informing clinical translation.
From Phineas Gage to VLSM: The History and Core Principles of Brain Lesion Studies
The lesion method is a foundational scientific approach that studies the relationship between brain and behavior by examining changes in cognitive, emotional, or behavioral functions following focal brain damage. This method operates on the causal inference principle that if a lesion in brain structure X leads to a deficit in function Y, then X is necessary for Y. Unlike correlational neuroimaging methods, the lesion method provides stronger causal inference about brain function because the brain damage precedes and causes the behavioral changes observed. Historically, studies of individual patients with brain lesions have provided groundbreaking insights into how the brain gives rise to behavior, forming the bedrock of modern cognitive neuroscience [1].
Table 1: Foundational Historical Cases in the Lesion Method
| Patient/Case | Year | Brain Area Affected | Functional Deficit Observed | Scientific Implication |
|---|---|---|---|---|
| Phineas Gage | 1848 | Frontal Lobe | Profound personality changes; became irritable, impulsive, and disinhibited | First evidence linking frontal lobes to personality and executive function [1] |
| Louis Victor Leborgne ("Tan") | 1861 | Left Inferior Frontal Lobe (Broca's area) | Severe speech production deficit; could only say the word "tan" | Identified a brain region critical for speech production (Broca's aphasia) [1] |
| Susanne Adam | 1874 | Left Posterior Temporal Lobe (Wernicke's area) | Impaired speech comprehension; fluent but nonsensical speech | Identified a brain region critical for language comprehension (Wernicke's aphasia) [1] |
| Henry Molaison (H.M.) | 1953 | Bilateral Medial Temporal Lobes (Hippocampus) | Severe anterograde amnesia; inability to form new declarative memories | Established the critical role of the hippocampus in memory formation [1] |
| Patient S.M. | 1994 | Bilateral Amygdala | Profound lack of fear; inability to recognize fear in others | Demonstrated the amygdala's essential role in processing fear and related emotions [1] |
Modern Methodological Evolution
Contemporary lesion method research has evolved from single-case studies to sophisticated group studies and computational techniques that map symptoms onto brain circuits. A significant modern advancement is lesion network mapping, which recognizes that many brain functions do not localize to a single region but depend on distributed circuits of connected areas. This technique identifies brain networks involved in complex symptomatology by mapping lesion locations onto large-scale brain connectome data. This approach can identify consistent brain networks underlying specific symptoms, even when the lesions themselves occur in different anatomical locations [2].
This "bedside-to-bedside" pathway offers a potentially shorter route to developing targeted therapies for neurodevelopmental and neuropsychiatric disorders. By identifying the neuroanatomical basis of quantifiable symptoms across clinical cohorts, researchers can generate circuit-based hypotheses. These hypotheses can then be validated in large-scale cohorts and prospectively tested using non-invasive neuromodulation techniques like Transcranial Magnetic Stimulation (TMS), leading directly to clinical trials for symptom-based therapy [2].
Key Experimental Protocols
Protocol for Single-Case Study and Deep Phenotyping
Objective: To establish a direct causal link between a specific, focal brain lesion and a resulting behavioral or cognitive deficit in an individual patient.
Materials: High-resolution structural MRI or CT scanner, standardized neuropsychological assessment battery, clinical interview protocols, video recording equipment (if applicable for behavioral analysis).
Procedure:
- Case Identification & Characterization: Identify a patient with a focal, acquired brain lesion (e.g., from stroke, trauma, or surgical resection). Document the acute onset and nature of the behavioral change.
- Lesion Localization:
- Acquire a high-resolution T1-weighted structural MRI or CT scan.
- Trace the lesion boundaries manually on the individual's native brain scan using neuroimaging software (e.g., MRIcron, ITK-SNAP).
- If possible, normalize the lesioned brain to a standard stereotaxic space (e.g., MNI) to facilitate group comparisons or network mapping in future analyses.
- Behavioral/Cognitive Phenotyping:
- Administer a comprehensive, standardized neuropsychological assessment tailored to the hypothesized functional domain (e.g., aphasia battery for language deficits, Wisconsin Card Sorting Test for executive function).
- Conduct qualitative behavioral observation and structured interviews to document real-world functional impairments.
- Data Integration and Inference:
- Overlay the precisely mapped lesion location with the detailed behavioral profile.
- Infer that the lesioned brain area is critically necessary for the impaired function, as the deficit was absent prior to the injury and immediately followed it [1].
Protocol for Group Lesion-Symptom Mapping
Objective: To identify brain structures critical for a specific cognitive function by correlating lesion location with behavioral performance across a group of patients.
Materials: Cohort of patients with focal brain lesions, standardized behavioral task(s), computing resources with statistical software (e.g., R, MATLAB), lesion analysis toolbox (e.g., NiiStat, VLSM).
Procedure:
- Cohort Assembly: Recruit a group of patients with heterogeneous, focal brain lesions. Larger sample sizes (N > 50) increase statistical power and reproducibility [2].
- Lesion Data Processing:
- For each patient, trace the lesion on a T1-weighted MRI scan and normalize the brain to a standard template.
- Create a binary lesion map for each patient (1=voxel lesioned, 0=voxel intact).
- Behavioral Assessment: Administer the same quantitative behavioral task to all patients in the cohort. The task should be unidimensional and target a specific cognitive process (e.g., naming latency, memory accuracy, reaction time in a decision task).
- Statistical Mapping:
- Perform a voxel-based lesion-symptom mapping (VLSM) analysis. At each voxel in the brain, a statistical test (e.g., t-test, Brunner-Munzel test) compares the behavioral scores of patients with a lesion at that voxel versus those without.
- The result is a statistical map of the brain showing regions where damage is significantly associated with poor performance on the task [2].
- Validation: Results can be validated by determining if the same brain network is implicated using lesion network mapping on independent connectome data [2].
Protocol for Lesion Network Mapping
Objective: To determine whether lesions causing a specific symptom map to a common functional brain network, even if they are anatomically distinct.
Materials: Database of lesioned patients with documented symptoms, resting-state functional MRI (fMRI) connectome database from healthy controls (e.g., Human Connectome Project), network mapping software.
Procedure:
- Define Seed Lesions: Identify a set of "seed" lesions from patients who all exhibit the same specific symptom (e.g., post-stroke tremor, inability to read).
- Network Identification:
- For each seed lesion location, identify the brain regions that are functionally connected to it using a normative connectome database derived from resting-state fMRI of healthy individuals.
- This step infers the brain network that was functionally disrupted by each lesion.
- Statistical Overlap Analysis:
- Test for significant overlap between the networks associated with all the seed lesions.
- The result is a common "symptom network" – a brain circuit that is functionally disrupted across all patients with the symptom, regardless of their exact lesion location [2].
- Cross-Disorder Validation: Test if this identified network is also relevant to idiopathic populations with the same symptom (e.g., in neurodevelopmental disorders) using traditional neuroimaging [2].
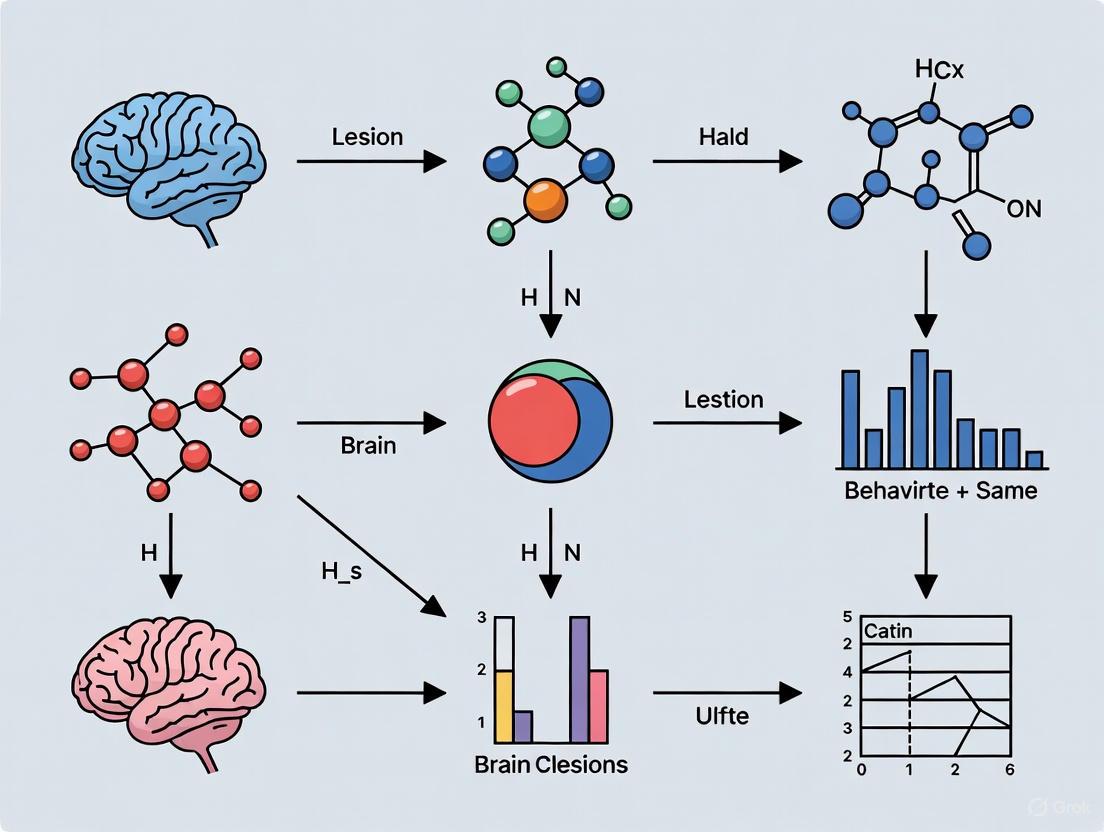
<75 chars Lesion Network Mapping Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Lesion Method Research
| Item/Reagent | Function/Application in Research |
|---|---|
| High-Resolution Structural MRI (T1-weighted) | Provides the anatomical basis for precise, in-vivo lesion delineation and localization. The fundamental raw data for any modern lesion study [2]. |
| Standardized Neuropsychological Batteries | Quantifies behavioral and cognitive deficits in a reliable, validated manner, allowing for comparison across patients and studies (e.g., Boston Naming Test, WAIS). |
| Lesion Segmentation & Normalization Software (e.g., MRIcron, ITK-SNAP) | Allows researchers to manually trace lesion boundaries on individual brain scans and normalize them to a standard stereotaxic space for group-level analysis. |
| Normative Connectome Atlas (e.g., from HCP) | A database of functional connectivity patterns from a large cohort of healthy individuals. Serves as a reference map for the lesion network mapping technique [2]. |
| Voxel-Based Lesion-Symptom Mapping (VLSM) Software | Performs voxel-wise statistical comparisons between lesion location and behavioral scores across a patient group to identify critically involved brain regions. |
| Non-Invasive Neuromodulation (TMS, tDCS) | Used to prospectively test hypotheses generated by lesion studies. Allows temporary, reversible "virtual lesions" or modulation of identified circuits to confirm causal roles [2] [3]. |
| Multimodal Imaging Integration (combining with fMRI, DTI) | Enhances causal inference from lesions by showing how a lesion disrupts functional activation or structural connectivity throughout a network during a task [3]. |
Integration with Neuromodulation and Causal Inference Challenges
The causal inferences drawn from the lesion method can be powerfully extended and tested using non-invasive neuromodulation techniques like repetitive Transcranial Magnetic Stimulation (rTMS). rTMS can create temporary, reversible "virtual lesions" or enhance activity in brain areas identified by lesion studies. This allows for prospective, interventional testing of the causal hypotheses generated by observational lesion data [2] [3].
However, drawing direct causal inferences from both permanent lesions and rTMS involves logical and methodological challenges. A key limitation is that a change in behavior following stimulation of a brain area does not automatically mean that area's normal function is the direct cause of the behavior. The effect could be indirect, resulting from the propagation of the signal through a network or from side effects of the stimulation itself (e.g., auditory clicks, scalp sensations). Stronger causal inferences require careful control conditions, combination with neuroimaging to track network effects, and acknowledgment that brain functions emerge from distributed networks rather than isolated modules [3].
<75 chars Causal Inference Challenge in Intervention
Table 3: Quantitative Outcomes of Modern Lesion-Based Therapeutic Development
| Therapeutic Approach | Target Symptom/Disorder | Key Circuit/Finding from Lesion Studies | Outcome Measure |
|---|---|---|---|
| Non-Invasive Neuromodulation (TMS/tDCS) [2] | Post-stroke motor recovery, depression, neurodevelopmental symptoms | Dorsolateral Prefrontal Cortex (for depression); Motor Network (for stroke) | Statistically significant improvement in standardized clinical rating scales (e.g., ~40-50% response rate in depression) |
| Real-time fMRI Neurofeedback [2] | Regulation of emotional or cognitive circuits | Targets identified as out-of-reach for TMS (e.g., deep limbic structures) | Successful learned modulation of target network activity; correlated symptomatic improvement |
| Deep Brain Stimulation (DBS) | Essential Tremor, Parkinson's Tremor | Thalamus (VIM nucleus) | Significant reduction (e.g., >50%) in tremor severity scores, validated across disorders [2] |
The foundational principle of correlating discrete brain lesions with specific behavioral deficits has been a cornerstone of cognitive neuroscience. The "lesion method" provides a powerful, natural experiment for inferring brain function, allowing researchers to make causal inferences about the neural substrates of behavior. This approach was pioneered through seminal case studies of patients with focal brain damage, including Broca's and Wernicke's aphasic patients and the profoundly amnesic patient H.M. Their unique neuropsychological profiles, resulting from specific brain lesions, revealed fundamental insights into the functional organization of language and memory systems. These historical cases continue to inform contemporary research methodologies and theoretical frameworks in cognitive neuroscience, establishing enduring principles about brain-behavior relationships that remain relevant for researchers, scientists, and drug development professionals seeking to understand neural circuit functions.
Broca's Area: The Functional Anatomy of Speech Production
Historical Case Foundation
In 1861, Paul Broca described patient Leborgne ("Tan"), who exhibited severely non-fluent, effortful, and agrammatical speech despite relatively preserved language comprehension [4]. Postmortem examination revealed a lesion centered in the left inferior frontal gyrus (LIPC), a region now known as Broca's area (Brodmann areas 44 and 45) [5]. Broca's examination of approximately 20 additional patients with similar speech production deficits and left frontal damage led him to conclude that this region served as a critical center for articulate language [4]. This case established both the functional specialization of this cortical region and the principle of cerebral dominance for language, with the left hemisphere being dominant in most individuals.
Modern Re-evaluation and Protocol
Modern research using high-resolution structural and perfusion-weighted MRI in chronic stroke patients has confirmed that damage to the left inferior frontal cortex (particularly the pars opercularis, LIPCpo) more accurately predicts apraxia of speech (AOS) than damage to other regions like the insula [4]. The experimental protocol for establishing this correlation involves:
- Patient Selection: Recruit patients with chronic left hemisphere stroke (>6 months post-stroke) with and without motor speech impairment.
- Clinical Assessment: Administer standardized tests for apraxia of speech (AOS) and aphasia, generating both binary (present/absent) and continuous severity scores.
- Neuroimaging Acquisition: Acquire high-resolution T1-weighted structural MRI and pulsed arterial spin labeling (PASL) to measure cerebral blood flow (CBF).
- Lesion Demarcation: Manually trace lesions on native-space MRI images before spatial normalization to standard template (e.g., MNI space).
- Statistical Analysis: Perform whole-brain voxel-wise lesion-symptom mapping and stepwise regression analyzing proportional damage in regions of interest (ROI: LIPCpo, LIPCpt, left anterior/posterior insula).
Table 1: Quantitative Structural MRI Findings Linking Broca's Area to Speech Production
| Analysis Method | Key Brain Region | Statistical Finding | Interpretation |
|---|---|---|---|
| Binary Voxel-Based Analysis | Left Inferior Frontal Gyrus, pars opercularis (LIPCpo) | Z=3.66, p<0.01 | Damage to LIPCpo strongly predicts presence of AOS |
| Continuous Voxel-Based Analysis | Left Inferior Frontal Gyrus, pars opercularis (LIPCpo) | Z=3.44, p<0.01 | Damage to LIPCpo strongly predicts severity of AOS |
| Stepwise Regression (Structural) | Left Inferior Frontal Gyrus, pars opercularis (LIPCpo) | F(1,48)=79.802, p<0.0001, R²=0.62 | LIPCpo damage is the single best predictor of AOS |
| Stepwise Regression (CBF) | Left Inferior Frontal Gyrus, pars opercularis (LIPCpo) | F(1,41)=15.431, p<0.0001, R²=0.273 | Reduced perfusion in LIPCpo predicts AOS |
Contemporary Insights from Intraoperative Mapping
Intraoperative Direct Electrical Stimulation (DES) during awake brain tumor surgery provides complementary evidence about Broca's area function. DES applied to Broca's area induces an intensity-dependent "speech arrest" without disrupting ongoing electromyography (EMG) activity in phono-articulatory muscles [6]. Quantitative EMG analysis (power spectrum and root mean square) shows no difference between baseline and stimulation periods during speech arrest [6]. This suggests Broca's area acts as a pre-articulatory phonetic encoder that gates motor program initiation rather than directly controlling muscle movement [6].
Figure 1: Broca's Area as a Pre-articulatory Gate: This model illustrates how Broca's area functions as a pre-articulatory encoder that gates the transition from language intention to motor execution. Direct Electrical Stimulation (DES) applied to this region prevents this gating function, resulting in speech arrest without affecting muscle activation patterns.
Wernicke's Area: Reinterpreting the Anatomy of Language Comprehension
Historical Context and Modern Challenges
In 1874, Carl Wernicke described a patient with fluent but meaningless speech and severe comprehension impairments, associating these deficits with a lesion in the left posterior superior temporal gyrus (pSTG) [7] [8]. This region, traditionally encompassing the posterior superior temporal gyrus and supramarginal gyrus (Brodmann areas 22, 40), became known as Wernicke's area and was historically defined as the cortical center for language comprehension [8]. Modern neuroimaging and lesion-symptom mapping studies in patients with primary progressive aphasia (PPA) and stroke have challenged this classical model, demonstrating that severe word comprehension impairments are not reliably associated with damage to this anatomically-defined Wernicke's area [7].
Experimental Protocol for Comprehension Dissociation
Research dissociating word and sentence comprehension involves specific methodological approaches:
- Participant Cohort: 72 patients with primary progressive aphasia (PPA) of neurodegenerative origin provide a clean lesion-behavior model without sudden reorganization [7].
- Language Assessment: Comprehensive testing includes the Western Aphasia Battery (Aphasia Quotient ≥60), with specific measures for single-word comprehension (e.g., picture-word matching) and sentence comprehension (e.g., syntactic processing, commands) [7].
- Structural Imaging: High-resolution T1-weighted MRI acquired for voxel-based morphometry to quantify cortical atrophy.
- Clinico-Anatomical Correlation: Peak atrophy sites correlated with comprehension scores using voxel-based lesion-symptom mapping at individual and group levels [7].
Table 2: Dissociation of Comprehension Deficits Based on Lesion Location
| Comprehension Deficit | Associated Atrophy Site | Key Statistical Finding | Syndrome Association |
|---|---|---|---|
| Severe Single-Word Comprehension Impairment | Left Anterior Temporal Lobe (Temporal Pole) | Peak atrophy invariably associated with word comprehension deficits [7] | Semantic Variant PPA |
| Sentence Comprehension Impairment | Heterogeneous Sites: Temporoparietal cortex, Broca's area, dorsal premotor cortex | Inconsistent impairment with temporoparietal damage alone [7] | Agrammatic Variant PPA |
| Relative Preservation of Single-Word Comprehension | Classical Wernicke's Area (pSTG/SMG) | Damage leaves single-word comprehension intact [7] [8] | Conduction Aphasia, Logopenic PPA |
Revised Model of Posterior Language Function
Contemporary evidence indicates the anatomically-defined Wernicke's area (pSTG/SMG) is critical for phonologic retrieval in speech production rather than comprehension [8]. This region acts as a repository for phoneme sequences needed for word production, with damage causing phonemic paraphasias (characteristic of conduction aphasia and Wernicke's aphasia) without necessarily impairing comprehension [8]. Functional MRI and lesion studies show word comprehension involves a distributed network including middle temporal gyrus, angular gyrus, and anterior temporal lobe, while sentence comprehension requires integration across temporoparietal and frontal regions [7] [8].
Figure 2: Revised Language Network Model: This diagram illustrates the dissociated functions within the posterior language network. The classical Wernicke's area (pSTG/SMG) is primarily engaged in phonologic retrieval for speech production. Comprehension involves distinct pathways connecting auditory perception to distributed semantic systems, explaining why Wernicke's area damage impairs production but not necessarily comprehension.
H.M.: The Medial Temporal Lobe and Memory Systems
Case History and Experimental Paradigm
In 1953, patient Henry Molaison (H.M.) underwent bilateral medial temporal lobe resection to treat intractable epilepsy, resulting in profound anterograde amnesia [9] [10] [11]. Despite preserved intellectual function, personality, and immediate memory, H.M. could not form new long-term declarative memories while retaining some capacity for procedural learning [10] [11]. This case provided the first conclusive evidence for medial temporal lobe (especially hippocampal) involvement in memory consolidation and revealed the fundamental distinction between different memory systems [11].
Quantitative Postmortem Analysis Protocol
Postmortem examination of H.M.'s brain provided precise anatomical verification of his lesions:
- Brain Fixation and Sectioning: Whole-brain fixation followed by serial sectioning in coronal plane (70μm thickness) aligned with anterior-posterior commissure plane [9].
- Digital Imaging and 3D Reconstruction: Acquisition of 2,401 high-resolution digital images of block surface with histological staining of sections for 3D volumetric reconstruction [9].
- Anatomical Measurement: 3D measurement tools used to calculate lesion extent and spared hippocampal tissue volume [9].
- Cytoarchitectonic Analysis: Microscopic examination of stained sections to identify residual hippocampal tissue based on distinctive cellular architecture [9].
Table 3: Quantitative Postmortem Measurements of H.M.'s Medial Temporal Lobe Lesions
| Brain Structure | Left Hemisphere Measurement | Right Hemisphere Measurement | Functional Correlation |
|---|---|---|---|
| Lesion Length (anterior-posterior) | 54.5 mm | 44.0 mm | Asymmetry may explain variable retrograde amnesia |
| Residual Entorhinal Cortex Volume | 0.03 cm³ | 0.11 cm³ | Near-complete removal disrupted hippocampal input |
| Residual Hippocampal Formation | Significant portion spared posteriorly | Significant portion spared posteriorly | Spared tissue was functionally disconnected |
| Key Structures Removed | Amygdala, entorhinal cortex, anterior hippocampus | Amygdala, entorhinal cortex, anterior hippocampus | Necessary for declarative memory formation |
Behavioral Testing and Memory Dissociations
Systematic neuropsychological testing revealed dissociations in H.M.'s memory capabilities:
- Declarative Memory Tasks: Impaired recall and recognition of facts, events, and personal experiences (episodic and semantic memory) [10] [11].
- Procedural Learning Tasks: Preserved motor skill learning (mirror tracing), perceptual learning, and classical conditioning despite no conscious memory of training sessions [10] [11].
- Perceptual Identification Tests: Demonstrated intact repetition priming effects (facilitated processing of previously encountered stimuli) [10].
These findings established the critical distinction between declarative memory (dependent on medial temporal lobe structures) and nondeclarative memory (supported by other neural systems) [10].
Figure 3: H.M.'s Memory Dissociations: This model illustrates how H.M.'s medial temporal lobe (MTL) resection disrupted the consolidation of declarative memories while sparing nondeclarative memory systems. The MTL is necessary for transferring information from immediate experience to stable long-term storage in neocortical regions but is not required for procedural learning or priming effects.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for Lesion-Behavior Correlation Studies
| Research Reagent / Material | Primary Function | Application Example |
|---|---|---|
| High-Resolution Structural MRI (T1-weighted) | Precise anatomical visualization and lesion demarcation | Quantifying lesion volume and location in stroke patients [4] |
| Diffusion Tensor Imaging (DTI) | Reconstruction of white matter pathways and disconnection analysis | Identifying involvement of arcuate fasciculus in conduction aphasia [5] |
| Perfusion-Weighted MRI (PASL) | Measurement of cerebral blood flow to identify dysfunctional tissue | Detecting hypoperfusion in Broca's area with insular lesions [4] |
| Voxel-Based Morphometry Software | Automated quantification of cortical atrophy or lesion distribution | Correlating peak atrophy sites with comprehension deficits in PPA [7] |
| Direct Electrical Stimulation (DES) | Transient, reversible functional interference during awake surgery | Mapping critical language sites by inducing speech arrest [6] |
| Standardized Neuropsychological Batteries | Comprehensive assessment of specific cognitive domains | Western Aphasia Battery for language; specific tests for declarative vs. procedural memory [7] [11] |
| Cytoarchitectonic Atlas | Microscopically-defined cortical area boundaries for precise localization | Defining Brodmann areas 44/45 beyond macroscopic landmarks [5] |
The seminal case studies of Broca's aphasic patients, Wernicke's aphasic patients, and patient H.M. established foundational principles that continue to guide cognitive neuroscience. These cases demonstrated the value of the lesion method for making causal inferences about brain-behavior relationships, revealed the functional specialization of distinct brain regions and networks, and illustrated the dissociability of cognitive processes. Modern neuroimaging techniques and analysis methods have refined our understanding of these classical cases, leading to more precise anatomical correlations and sophisticated network models. The continuing evolution of lesion-behavior research provides critical insights for diagnosing and treating neurological disorders, developing targeted cognitive interventions, and informing drug development strategies aimed at specific neural circuits. These historical foundations remind us that careful observation of individual patients, combined with innovative methodological approaches, continues to drive discovery in cognitive neuroscience.
Application Notes: Core Principles of the Lesion Method
The lesion method is a foundational scientific approach in neuroscience for correlating brain structure with function. Its underlying logic is based on a subtractive principle: by studying the behavioral capacities that are lost following damage to a specific brain region, researchers can infer the necessary function of that area [1]. If a lesion in brain area X leads to a deficit in behavior Y, it suggests that area X is necessary for the normal execution of behavior Y [12]. This method has been instrumental for over 200 years in mapping cognitive functions like language, memory, and emotion to specific neural substrates [1].
Modern applications of the lesion method have evolved from single-case studies to group lesion studies, which analyze cohorts of patients with similar brain injuries. This allows scientists to determine if lesions to certain brain areas consistently produce the same behavioral changes across different individuals, strengthening conclusions about necessity [1]. Furthermore, the integration of the lesion method with neuroimaging techniques and standardized data management tools like the Neuroscience Experiments System (NES) allows for more sophisticated analysis of how interconnected brain networks support behavior [1] [13].
Experimental Protocols
Protocol for Single-Case Study Behavioral Analysis
This protocol outlines the procedure for conducting a deep behavioral analysis of a single patient with a focal brain lesion, following the models of historic cases like patient H.M. or patient S.M. [1].
- Objective: To establish a causal link between a specific brain area and a defined cognitive or behavioral function through in-depth analysis of a single patient.
- Materials: Neuropsychological assessment batteries, video recording equipment, standardized stimulus sets, the Neuroscience Experiments System (NES) or similar data management software for collecting behavioral and participant data [13].
- Procedure:
- Patient Characterization: Record detailed medical, demographic, and neuropsychological history. Obtain informed consent.
- Lesion Mapping: Acquire high-resolution structural neuroimages (e.g., MRI or CT). Precisely reconstruct the lesion location onto a standardized brain template using appropriate software.
- Baseline Behavioral Assessment: Administer a comprehensive battery of standardized tests to establish a profile of preserved and impaired functions across multiple domains (e.g., memory, language, executive function).
- Targeted Experimental Testing: Based on the initial assessment, design and administer customized experiments to probe the specific function linked to the lesioned area. Examples include:
- Fear Induction: For amygdala lesions, expose the patient to fear-inducing stimuli (live snakes, spiders, haunted houses) and measure subjective fear reports, physiological responses, and behavioral avoidance [1].
- Memory Tasks: For medial temporal lobe lesions, test recall and recognition of new information after varying delay intervals.
- Data Integration and Analysis: Correlate the precise anatomical location of the lesion with the specific behavioral deficit. The conclusion of necessity is supported if the patient cannot perform a function they had prior to the injury, and that deficit is consistently linked to the lesioned area.
Protocol for Voxel-Based Lesion-Symptom Mapping (VLSM)
This protocol describes a group-study approach that uses modern brain imaging and statistics to correlate lesion location with behavioral performance on a voxel-by-voxel basis [12].
- Objective: To systematically identify brain regions where tissue damage is significantly associated with deficits in a specific behavioral task across a large cohort of brain-injured patients.
- Materials: Access to a cohort of patients with focal brain lesions (e.g., stroke), standardized behavioral task, high-resolution structural MRI or CT scans, computing software capable of running VLSM analysis (e.g., MRIcron, NiiStat).
- Procedure:
- Participant Selection and Recruitment: Recruit a well-characterized cohort of patients with chronic, stable focal brain lesions, typically from stroke.
- Behavioral Testing: Administer the same standardized behavioral task to all participants. The Curtiss-Yamada Comprehensive Language Evaluation (CYCLE-R) is an example used for language comprehension [12].
- Neuroimaging and Lesion Reconstruction: Obtain structural brain scans for each participant. Manually or semi-automatically trace each patient's lesion onto a standardized brain template.
- Data Preprocessing: Normalize all lesion maps to a common stereotaxic space (e.g., MNI).
- Statistical Analysis (VLSM): For each voxel in the brain, the analysis compares the behavioral scores of two patient groups: those with a lesion at that voxel and those without. A statistical test (e.g., t-test) is performed at every voxel to identify locations where damage significantly impairs performance.
- Multiple Comparisons Correction: Apply statistical correction (e.g., False Discovery Rate) to the resulting map to control for false positives arising from testing thousands of voxels.
- Interpretation: Brain regions that survive correction are interpreted as being critically necessary for the behavior in question.
Data Presentation
Table 1: Foundational single-case studies established the logic of subtractive analysis for inferring necessity [1].
| Patient (Year) | Brain Area Lesioned | Behavioral Deficit | Inferred Necessity of Brain Area |
|---|---|---|---|
| Phineas Gage (1848) | Frontal Lobe | Profound personality change; impaired planning and social conduct | Frontal lobe is necessary for personality, planning, and social behavior |
| Louis Leborgne (1861) | Left Inferior Frontal Gyrus (Broca's area) | Severely impaired speech production; could comprehend language | Broca's area is necessary for fluent speech production |
| Susanne Adam (1874) | Left Posterior Temporal Lobe (Wernicke's area) | Impaired language comprehension; fluent but nonsensical speech | Wernicke's area is necessary for understanding language |
| Henry Molaison (1953) | Bilateral Medial Temporal Lobe (Hippocampus) | Profound anterograde amnesia; inability to form new memories | Hippocampus is necessary for the formation of new long-term memories |
| S.M. (1990s) | Bilateral Amygdala | Complete absence of fear response | Amygdala is necessary for experiencing fear |
Key Brain Areas Implicated in Language Comprehension by Group Lesion Studies
Table 2: Modern group studies using VLSM have identified a network of brain areas necessary for language comprehension, moving beyond classic models [12].
| Brain Area | Key Function in Comprehension (from VLSM) | Significance |
|---|---|---|
| Posterior Middle Temporal Gyrus | Word-level comprehension | Critical for accessing lexical-semantic information |
| Anterior Superior Temporal Gyrus | Sentence-level comprehension | Involved in early stages of syntactic and auditory processing |
| Superior Temporal Sulcus & Angular Gyrus | Sentence-level comprehension | Supports integration of semantic and syntactic information |
| Mid-Frontal Cortex (Brodmann Area 46) | Sentence-level comprehension | Important for working memory demands during comprehension |
| Inferior Frontal Gyrus (Brodmann Area 47) | Sentence-level comprehension | Involved in semantic processing and selection |
Visualization of Methodologies
The Logic of the Lesion Method
Voxel-Based Lesion-Symptom Mapping Workflow
The Scientist's Toolkit
Table 3: Essential research reagents and materials for conducting modern lesion method studies.
| Research Reagent / Tool | Function in Lesion Studies |
|---|---|
| Structural MRI (Magnetic Resonance Imaging) | Provides high-resolution, 3D anatomical images of the brain for precise localization and reconstruction of lesions. |
| Standardized Neuropsychological Batteries | Assess a wide range of cognitive functions (memory, language, attention) to create a detailed profile of behavioral deficits and preserved abilities. |
| Voxel-Based Lesion-Symptom Mapping (VLSM) Software | Enables statistical analysis of the relationship between lesion location and behavioral scores on a voxel-by-voxel basis across a patient group [12]. |
| Neuroscience Experiments System (NES) | An open-source software tool that assists researchers in managing experimental data, protocols, and participant information, ensuring standardized data collection and provenance [13]. |
| Standardized Brain Atlases (e.g., MNI space) | Provide a common coordinate system for mapping individual patient lesions, allowing for group comparisons and meta-analyses. |
The lesion method, one of the oldest approaches in behavioral neuroscience, remains foundational for correlating brain structure with function. This methodology examines behavioral and cognitive changes resulting from focal brain damage to infer the functional roles of specific neural regions. Historically, studies of patients with accidental brain injuries provided groundbreaking insights into brain organization, while modern research employs more precise, experimentally controlled lesions in animal models. This article details key discoveries in localizing memory, language, and executive functions, providing application notes and experimental protocols for researchers investigating brain-behavior relationships. The principles outlined serve both basic neuroscience research and drug development efforts aimed at treating neurological and psychiatric disorders affecting these cognitive domains.
Memory Systems Localization
Key Discoveries and Anatomical Substrates
Research using the lesion method has revealed that memory is not a unitary faculty but consists of multiple dissociable systems dependent on distinct brain regions. The critical distinction between explicit (declarative) and implicit (non-declarative) memory has been clearly demonstrated through lesion studies.
Table 1: Memory Systems and Their Neural Substrates
| Memory System | Brain Substrates | Primary Functions | Key Lesion Findings |
|---|---|---|---|
| Explicit/Declarative Memory | Hippocampus, medial temporal lobe | Conscious recall of facts and events | Anterograde amnesia following medial temporal lobe lesions [14] |
| Implicit/Non-declarative Memory | Cerebellum, amygdala | Unconscious learning of skills and associations | Preserved implicit learning in amnesic patients with hippocampal damage [14] |
| Classical Conditioning (Delay) | Cerebellum | Learning of overlapping stimulus-response associations | Cerebellar lesions impair basic delay conditioning [14] |
| Trace Conditioning | Hippocampus | Learning with temporal gap between stimuli | Hippocampal lesions impair trace conditioning [14] |
The seminal case of patient H.M., who underwent bilateral medial temporal lobe resection, demonstrated that the hippocampus is critical for forming new explicit memories while leaving implicit memory systems largely intact [14]. Subsequent lesion studies further refined this model, revealing that other medial temporal lobe structures, including the perirhinal, parahippocampal, and entorhinal cortices, also contribute to declarative memory, with more profound amnesia resulting from larger lesions encompassing these areas [14].
Experimental Protocol: Trace Conditioning Paradigm
Purpose: To assess hippocampal-dependent memory in animal models using trace conditioning.
Materials:
- Animal subjects (e.g., rabbits, rodents)
- Classical conditioning apparatus with stimulus delivery systems
- Response measurement system (e.g., eyelid detector, limb flexion sensor)
- Surgical equipment for stereotaxic lesions (if creating experimental lesions)
- Histological materials for lesion verification
Procedure:
- Habituation: Expose subjects to the experimental context without stimuli.
- Pre-training Baseline: Measure baseline responses to conditioned stimulus (CS) and unconditioned stimulus (US).
- Lesion Induction (if applicable): Create bilateral hippocampal lesions using:
- Aspiration lesions: Surgical removal of hippocampal tissue
- Neurotoxic lesions: Microinjections of excitotoxins (e.g., ibotenic acid) for selective cell body destruction
- Electrolytic lesions: Electrical current to create targeted damage
- Recovery: Allow 1-2 weeks post-surgical recovery.
- Training:
- Trace Conditioning Group: Present CS (e.g., tone) for 250ms, followed by a 500ms trace interval with no stimuli, then US (e.g., corneal airpuff) for 100ms.
- Delay Conditioning Control: Present CS and US with temporal overlap.
- Testing: Assess conditioned response (CR) acquisition across multiple sessions.
- Lesion Verification: Perfuse, section, and stain brain tissue to verify lesion location and extent.
Applications: This protocol effectively differentiates hippocampal-dependent from hippocampal-independent learning. The temporal characteristics of hippocampal involvement can be examined by varying the interval between training and lesion induction [14].
Visualization: Memory Systems and Hippocampal Dependency in Trace Conditioning
Figure 1: Organization of memory systems showing distinct neural substrates for explicit and implicit memory, with specialized hippocampal involvement in trace conditioning.
Language Localization
Historical Foundations and Contemporary Models
The lesion method has been instrumental in identifying brain regions essential for language processing since Paul Broca's seminal work in the 19th century. The case of Broca's patient Lebornge established the critical role of the left inferior frontal gyrus in speech production, while Carl Wernicke's later studies revealed the importance of the left posterior superior temporal gyrus in language comprehension [15].
Henry Charlton Bastian's detailed documentation of patient Thomas A. over 18 years represented a landmark in clinico-pathological correlation methods for language localization [15]. Bastian's work pioneered systematic assessment across language modalities (speech, writing, reading, and listening), establishing a foundation for contemporary language mapping.
Table 2: Language Areas Identified Through Lesion Studies
| Brain Region | Function | Deficit from Lesion | Laterality Patterns |
|---|---|---|---|
| Broca's Area (left inferior frontal gyrus) | Speech production, language processing | Non-fluent aphasia, effortful speech | Strongly left-lateralized [16] |
| Wernicke's Area (left posterior superior temporal gyrus) | Speech comprehension, semantic processing | Fluent but meaningless speech, impaired comprehension | Strongly left-lateralized [16] |
| Arcuate Fasciculus | Connecting Broca's and Wernicke's areas | Conduction aphasia (impaired repetition) | Left-lateralized [15] |
| Supramarginal and Angular Gyri | Reading, writing, integration of sensory information | Alexia, agraphia, conduction aphasia | Variable lateralization [16] |
Contemporary models suggest differentiated lateralization patterns for distinct language processes. According to the dual-stream model of speech processing, while speech comprehension and semantic processing are typically left-lateralized, basic acoustic processing of speech input and speech articulation involve bilateral networks [16].
Experimental Protocol: Language Lateralization Assessment
Purpose: To determine hemispheric dominance for language using functional magnetic resonance imaging (fMRI) with language tasks.
Materials:
- MRI scanner (3T or higher recommended)
- Presentation software for stimulus delivery
- Response recording devices (fMRI-compatible button boxes)
- Eye-tracking equipment (optional, for monitoring attention)
- Analysis software (e.g., SPM, FSL, AFNI)
Procedure:
- Subject Screening: Recruit right-handed, monolingual adults with no neurological history.
- Task Selection: Choose language tasks targeting specific processes:
- Verbal Fluency: Generate words beginning with a specific letter
- Semantic Decision: Judge category membership of presented words
- Sentence Comprehension: Process complex syntactic structures
- Object Naming: Name pictures of objects
- Baseline Tasks: Design matched control tasks (e.g., tone discrimination for auditory tasks, visual fixation for visual tasks).
- fMRI Acquisition:
- Collect high-resolution structural images (T1-weighted)
- Acquire functional images (T2*-weighted EPI) during task performance
- Use standard parameters: TR=2000ms, TE=30ms, voxel size=3×3×3mm
- Data Analysis:
- Preprocess data (realignment, normalization, smoothing)
- Model hemodynamic response to task conditions
- Calculate Laterality Index (LI) using the formula: LI = (L - R)/(L + R)
- Define regions of interest (ROIs), particularly in inferior frontal and temporal regions
- Interpretation: LI > +0.2 indicates left lateralization; LI < -0.2 indicates right lateralization; intermediate values indicate bilateral representation.
Applications: This protocol is valuable for presurgical mapping in epilepsy and tumor patients, as well as for research on individual differences in language organization [16].
Executive Functions Localization
From Frontal Lobes to Distributed Networks
Executive functions (EFs) represent higher-level cognitive processes that control and coordinate goal-directed behavior, including working memory, cognitive flexibility, inhibition, and planning. Early lesion studies, most famously the case of Phineas Gage, highlighted the importance of the frontal lobes for executive control [17]. However, contemporary research reveals that EFs are supported by distributed thalamocortical networks rather than isolated frontal regions.
Table 3: Executive Functions and Their Neural Substrates
| Executive Function | Key Brain Regions | Associated Lesion Deficits | Assessment Tasks |
|---|---|---|---|
| Updating | Middle frontal gyrus (BA 8), supramarginal gyrus | Impaired monitoring of working memory contents | n-back tasks [18] |
| Inhibition | Inferior frontal gyrus (BA 46), mediodorsal thalamus | Deficits in suppressing prepotent responses | Stroop test, stop-signal task [18] |
| Switching | Superior frontal gyrus (BA 8), inferior parietal lobule | Perseveration, difficulty shifting task sets | Wisconsin Card Sorting Test, task-switching paradigms [18] |
| Dual-tasking | Postcentral gyrus (BA 40), frontoparietal network | Impaired simultaneous task performance | Psychological Refractory Period paradigm [18] |
A meta-analytic review of lesion studies indicates that the relationship between executive functions and the frontal lobes is more complex than initially proposed. While frontal damage often disrupts EFs, the correlation is not one-to-one, with some frontal lesions sparing certain EFs and some non-frontal lesions impairing them [19].
Experimental Protocol: Mediodorsal Thalamus Lesion and Executive Function Assessment
Purpose: To evaluate the role of the mediodorsal thalamus in executive functions using focal lesions and neuropsychological testing.
Materials:
- Human patients with focal thalamic lesions or animal subjects
- MRI/CT scanner for lesion localization
- Neuropsychological assessment tools
- Stereotaxic apparatus (for animal studies)
- Lesion mapping software
Procedure:
- Participant Selection:
- Identify patients with focal thalamic lesions (e.g., from stroke)
- Recruit matched control patients with non-thalamic lesions
- Confirm lesion location with structural neuroimaging
- Lesion Analysis (for animal studies):
- Induce focal mediodorsal thalamic lesions using stereotaxic surgery
- Use coordinate-based approach with neurotoxins for selective damage
- Include sham-operated controls
- Executive Function Assessment:
- Trail Making Test (TMT): Assess cognitive flexibility (TMT-B)
- Wisconsin Card Sorting Test (WCST): Evaluate abstraction and set-shifting
- Verbal Fluency Tests: Measure generative capacity and strategic search
- Stroop Color-Word Test: Assess inhibitory control
- Lesion Network Mapping:
- Use normative functional connectivity data
- Map networks functionally connected to lesion locations
- Identify connected cortical regions potentially affected by thalamic lesions
- Data Analysis:
- Compare executive function performance between mediodorsal thalamic lesion patients, other thalamic lesion patients, and controls
- Corregate lesion location with specific EF deficits
- Analyze functional connectivity profiles of lesion sites
Applications: This protocol helps elucidate the role of thalamocortical circuits in executive control, with implications for understanding cognitive deficits in disorders such as vascular dementia, traumatic brain injury, and Parkinson's disease [20].
Visualization: Unity and Diversity of Executive Function Networks
Figure 2: Neural correlates of executive functions showing both unity (shared frontoparietal regions) and diversity (unique regions for specific functions).
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Lesion Method Research
| Research Reagent/Material | Function | Application Examples |
|---|---|---|
| Ibotenic Acid | Excitotoxic lesion agent; selectively destroys cell bodies while sparing fibers of passage | Creating selective hippocampal or thalamic lesions in animal models [17] |
| Kainic Acid | Neurotoxin targeting glutamate receptors; induces selective neuronal death | Modeling temporal lobe epilepsy and hippocampal damage [17] |
| 6-Hydroxydopamine (6-OHDA) | Catecholaminergic neurotoxin; selectively destroys dopamine and norepinephrine neurons | Creating Parkinson's disease models with nigrostriatal pathway lesions [17] |
| MRI Contrast Agents (Gadolinium) | Enhances visualization of brain structures and lesions in magnetic resonance imaging | Precise localization of lesion extent in human and animal studies [21] |
| Functional Localizer Tasks | Standardized cognitive tasks designed to activate specific brain networks | Language lateralization fMRI protocols; executive function localization [22] [16] |
| Stereotaxic Apparatus | Precise positioning system for targeted brain interventions | Accurate lesion placement in specific nuclei or cortical regions in animal studies [17] |
The lesion method continues to provide fundamental insights into brain-behavior relationships, with modern approaches combining precise lesion localization with advanced neuroimaging and connectivity analyses. The discoveries summarized here—regarding the distributed networks supporting memory, language, and executive functions—highlight both the specialization and integration of neural systems. For researchers in both academic and pharmaceutical development contexts, these findings and protocols offer valuable approaches for investigating brain function and developing interventions for neurological and psychiatric disorders. Future directions will likely include more sophisticated temporary lesion techniques, such as optogenetics and transcranial magnetic stimulation, which allow reversible manipulation of neural circuits with temporal precision, building upon the foundational knowledge established through permanent lesion studies.
Application Notes: Advancing from Focal Lesions to Network-Level Mapping
The field of lesion mapping has undergone a paradigm shift, moving from correlating symptoms with single brain regions to mapping them onto distributed brain networks. This modern approach recognizes that lesions in disparate anatomical locations can cause identical symptoms by disrupting a common functional brain circuit [23] [24]. Lesion network mapping (LNM) has successfully identified network correlates for over 40 different neurological and psychiatric symptoms, including complex conditions like hallucinations, tics, and criminality that were previously difficult to localize [23]. This network perspective provides a more complete pathophysiological model for symptoms that defy simple anatomical explanation.
Key Quantitative Benchmarks in Modern Lesion Mapping
The following table summarizes performance data and key parameters from contemporary lesion-symptom mapping studies, highlighting the integration of machine learning and multimodal neuroimaging.
Table 1: Performance Benchmarks for Modern Lesion-Symptom Mapping Techniques
| Study Focus / Model | Behavioral Measure | Key Imaging Features | Performance (Correlation) |
|---|---|---|---|
| Machine Learning Benchmarking (Random Forest) [25] | Aphasia Quotient (AQ) | Lesion location (JHU atlas) | Moderate to High Correlation |
| Machine Learning Benchmarking (Random Forest) [25] | Philadelphia Naming Test (PNT) | Lesion location (JHU atlas) | Moderate to High Correlation |
| Support Vector Regression (SVR) Multimodal [25] | Comprehensive Aphasia Test (CAT) | Lesion Volumes | r = 0.59 |
| SVR-MLSM [25] | WAB-R Aphasia Quotient (AQ) | Multimodal Neuroimaging | r = 0.69 |
| Multimodal ML for Post-stroke Aphasia [25] | Phonology, Semantics, Fluency, Executive Demand | Structural T1 & DTI features | r = 0.50 to 0.73 |
Successful implementation of modern lesion mapping protocols relies on several key software and data resources.
Table 2: Essential Research Reagents and Resources for Lesion Network Mapping
| Resource Name | Type | Primary Function in Research |
|---|---|---|
| Lead-DBS Software [24] | Software Toolbox | Facilitates lesion network mapping and deep brain stimulation (DBS) network mapping within a standardized framework. |
| Human Connectome Project (HCP) Data [23] [24] | Reference Dataset | Provides a large-scale atlas of normative human brain connectivity (the connectome) derived from resting-state fMRI, essential for calculating functional connectivity of lesion locations. |
| JHU MRI Atlas [25] | Brain Parcellation Atlas | A commonly used brain atlas for defining regions of interest (ROIs); identified as providing high performance in ML models for predicting language outcomes. |
| AAL, BRO, AICHA Atlases [25] | Brain Parcellation Atlases | Alternative brain atlases used for parcellating neuroimaging data and extracting features for model training. |
Experimental Protocols
Protocol: Voxel-Based Lesion-Symptom Mapping (VLSM)
Application Note: This univariate technique is used for initial, voxel-level identification of brain regions where lesion presence is significantly associated with a behavioral deficit [25] [23]. It is most effective for localizing elementary neurological deficits.
Workflow:
- Data Preparation:
- Input: T1-weighted structural MRI scans from a cohort of patients with focal brain lesions.
- Lesion Segmentation: Manually trace or automatically segment lesions on each patient's MRI. Normalize all lesion maps to a standard stereotaxic space (e.g., MNI).
- Behavioral Data: Collect quantitative behavioral scores for all patients (e.g., Aphasia Quotient, naming test scores).
- Statistical Analysis:
- For each voxel in the brain, perform a statistical test (e.g., t-test, non-parametric Brunner-Munzel test) to compare behavioral scores between patients with and without a lesion at that voxel [25] [23].
- Correct for multiple comparisons across voxels using family-wise error (FWE) correction or false discovery rate (FDR).
- Output: A statistical map highlighting voxels where lesion presence significantly predicts behavioral impairment.
Protocol: Lesion Network Mapping (LNM)
Application Note: This multivariate technique maps lesion locations to brain-wide networks, revealing circuit-level correlates of symptoms, especially when lesions are anatomically heterogeneous [23] [24]. It is ideal for complex neurological or psychiatric symptoms.
Workflow:
- Define Lesion Locations:
- Input: A set of lesion masks from patients presenting with a specific symptom of interest (e.g., hallucinations).
- Control Group: A set of lesion masks from patients not presenting with the symptom.
- Generate Functional Connectivity Maps:
- For each lesion mask, use a normative connectome (e.g., from the HCP) to identify all brain regions that are functionally connected to the lesion location [23] [24]. This is done by extracting the average resting-state fMRI time series from the lesion ROI in healthy controls and correlating it with every other voxel in the brain.
- Statistical Comparison:
- Compare the connectivity maps of the symptom-positive lesions against the symptom-negative (control) lesions. Voxels showing significantly stronger connectivity to the symptom-positive lesions constitute the "symptom network" [23].
- Output: A brain-wide map identifying the network functionally connected to lesions causing a specific symptom.
Protocol: Machine Learning for Outcome Prediction
Application Note: This protocol uses machine learning (ML) models to predict continuous behavioral outcomes (e.g., language test scores) from multimodal neuroimaging data, capturing complex, non-linear relationships beyond traditional mass-univariate methods [25].
Workflow:
- Feature Extraction:
- Input: Multimodal neuroimaging data (e.g., T1, DTI, resting-state fMRI).
- Parcellation: Parcellate the brain using a defined atlas (e.g., JHU, AAL).
- Feature Calculation: From each region, extract features such as lesion presence, fractional anisotropy (FA), mean diffusivity (MD), and functional connectivity (FC) strength [25].
- Model Training with Nested Cross-Validation:
- Outer Loop: Splits data into training and test sets for performance estimation.
- Inner Loop: On the training set, perform cross-validation to tune model hyperparameters.
- Algorithms: Train and compare multiple ML models (e.g., Random Forest, Support Vector Regression, Gradient Boosting) [25].
- Validation: Evaluate the final model on the held-out test set to obtain a unbiased performance metric (e.g., Pearson's correlation).
- Output: A trained model capable of predicting behavioral scores from new patient imaging data, along with identification of features most critical for prediction.
Modern Lesion Analysis Techniques: From Voxel-Based Mapping to Clinical Translation
Voxel-Based Lesion-Symptom Mapping (VLSM) is a statistical neuroimaging technique used to correlate brain lesion locations with behavioral deficits in neurological patients. This method represents a significant advancement over traditional lesion overlay approaches, allowing for a voxel-by-voxel analysis of the relationship between brain damage and cognitive, sensory, or motor impairments without requiring a priori hypotheses about lesion location [26]. First introduced by Bates and colleagues in 2003, VLSM has since become a cornerstone technique in the field of lesion-behavior mapping, enabling researchers to identify brain regions critical for specific functions by analyzing naturally occurring lesion patterns in patient populations, most commonly stroke survivors [26] [27].
The fundamental principle underlying VLSM is that if damage to a particular brain voxel consistently leads to impairment on a specific behavioral measure, that voxel can be inferred to be critically involved in the cognitive or neural processes supporting that behavior. Unlike earlier methods that required dichotomizing patients into groups based on either lesion location or behavioral deficit, VLSM leverages the continuous nature of both lesion data and behavioral scores, increasing statistical power and spatial precision [26]. This technique has been successfully applied to study various neurological conditions including stroke, traumatic brain injury, multiple sclerosis, and surgical resections, contributing significantly to our understanding of brain-behavior relationships [26].
Core Principles of VLSM
Theoretical Foundations
VLSM operates on the fundamental assumption that if a specific brain region is necessary for a given cognitive function, then damage to that region should result in impairment of that function. This lesion-deficit approach has roots in 19th century neurology, with pioneers such as Broca, Wernicke, and Dax using autopsy data to correlate brain damage with behavioral symptoms [26]. The modern VLSM approach was inspired by univariate analysis methods used in functional magnetic resonance imaging (fMRI), adapted to leverage the natural experiments provided by brain lesions [26].
A key advantage of VLSM over traditional lesion methods is its ability to analyze continuous behavioral data without requiring arbitrary patient groupings based on syndrome classifications or cutoff scores [26]. This preserves the full richness and variability of both the neuroanatomical and behavioral data. Additionally, VLSM does not require dividing patients based on lesion location, which is particularly advantageous given that naturally occurring lesions rarely respect neat anatomical boundaries [26].
Statistical Framework
VLSM employs mass univariate testing, performing an independent statistical test at every voxel in the brain to determine whether damage to that voxel is associated with worse performance on a behavioral measure [26]. The core statistical approach involves comparing behavioral scores between patients with and without damage at each voxel, typically using one-tailed tests with the assumption that lesioned voxels are associated with worse performance [26].
Table 1: Common Statistical Tests Used in VLSM Analysis
| Test Type | Data Type | Key Characteristics | Considerations |
|---|---|---|---|
| T-test | Continuous | Parametric test; assumes normality and equal variances | Sensitive to violations of assumptions; commonly used |
| Brunner-Munzel Test | Continuous | Non-parametric; fewer assumptions than t-test | More robust when parametric assumptions are violated |
| Chi-square Test | Binomial/Categorical | Tests association between lesion status and binary outcome | Requires categorical behavioral data |
| Liebermeister Test | Binomial/Categorical | Non-parametric alternative to chi-square | More appropriate for binomial data with small sample sizes |
| Regression | Continuous | Can handle continuous lesion data (0-1) | Allows for more nuanced modeling of lesion extent |
The VLSM framework must account for multiple statistical comparisons across thousands of voxels. Family-wise error correction is typically employed to control the probability of false positives, with rigorous correction methods being a current best practice [26]. Additional considerations include covarying for potentially confounding variables such as total lesion volume and ensuring sufficient statistical power by limiting interpretation to brain regions with adequate lesion coverage [26].
VLSM Workflow
The VLSM workflow involves a series of methodical steps from data acquisition through statistical analysis and result interpretation. The following diagram illustrates the complete process:
Data Acquisition and Preprocessing
The initial phase involves collecting high-quality neuroimaging and behavioral data from patients with focal brain lesions. Structural MRI sequences (T1-weighted, T2-weighted, FLAIR) are typically acquired to visualize lesion boundaries clearly [26]. While chronic stroke patients when lesion boundaries are most stable are most commonly studied, VLSM has also been applied to acute stroke patients using diffusion-weighted imaging, providing insights into brain-behavior relationships prior to significant neural reorganization [26].
Behavioral assessment should be comprehensive and targeted to the cognitive domains of interest. For language mapping, standardized tests such as the Western Aphasia Battery-Revised (WAB-R) Aphasia Quotient or Philadelphia Naming Test (PNT) are commonly used [25]. For visual scene memory, assessments like the WMS-III Family Pictures subtest can evaluate memory for different scene elements including identity, location, and action [28]. Behavioral testing should ideally occur close in time to neuroimaging acquisition.
Lesion delineation involves manually or semi-automatically tracing lesion boundaries on each patient's native brain images to create binary lesion masks. This process requires neuroanatomical expertise and should be performed by raters blinded to behavioral data when possible. For chronic strokes, lesion boundaries are typically clear once residual edema and bleeding have resolved [26].
Spatial Normalization
A critical step in VLSM is spatial normalization, where individual patient brains are transformed into a standard coordinate space, typically the Montreal Neurological Institute (MNI) template [26]. This allows for comparison and statistical analysis across patients despite natural anatomical variability. Both the lesion masks and native brain images are transformed using linear or non-linear registration algorithms, with careful quality control to ensure proper alignment.
Normalized lesion masks are resampled to a common resolution and stored as binary images where each voxel indicates the presence (1) or absence (0) of lesion. Some VLSM implementations can also handle continuous lesion data ranging from 0 to 1 to represent partial volume effects or degree of damage [26]. The resulting collection of lesion masks forms the primary neuroanatomical dataset for subsequent analysis.
Statistical Analysis
The core VLSM analysis involves performing voxel-wise statistical tests comparing behavioral scores between patients with and without damage at each voxel. For continuous behavioral data, t-tests or Brunner-Munzel tests are commonly employed, while binomial or categorical data may use chi-square or Liebermeister tests [26]. The analysis is typically restricted to voxels that are damaged in a sufficient number of patients (often 5 or more) to ensure adequate statistical power [26] [29].
Multiple comparison correction is essential due to the thousands of statistical tests performed. Family-wise error rate (FWER) control through permutation testing or false discovery rate (FDR) correction are standard approaches [26]. Covariates such as total lesion volume, age, or time post-onset can be included in the model to control for potential confounds.
Table 2: Key Considerations in VLSM Statistical Analysis
| Analysis Aspect | Options | Recommendations |
|---|---|---|
| Statistical Test | T-test, Brunner-Munzel, Chi-square, Liebermeister | Choose based on data type and distribution; non-parametric tests often more robust |
| Multiple Comparison Correction | Family-wise Error Rate (FWER), False Discovery Rate (FDR) | FWER more conservative but controls false positives; minimum cluster extent can supplement |
| Covariates | Lesion volume, age, education, time post-onset | Always covary for lesion volume; consider other clinically relevant factors |
| Threshold Criteria | Maximum voxel statistic, submaximal clusters, contiguous clusters | Use combination approaches; report exact thresholds and correction methods |
| Statistical Power | Minimum number of lesioned voxels, effect size considerations | Limit interpretation to voxels with sufficient lesion coverage (≥5 patients) |
Result Interpretation
Significant results from VLSM analysis are typically visualized as statistical maps overlaid on template brains, with color scales representing the strength of association between lesion location and behavioral deficit [26]. These maps can be viewed using software such as ITK-SNAP or MRIcron, with reference to standardized atlases (e.g., AAL, Harvard-Oxford, JHU white matter) for anatomical localization [26].
Interpretation should consider the network nature of brain function, as lesions to critical white matter pathways can produce deficits by disconnecting brain regions even when cortical areas are spared. Recent studies have highlighted the importance of considering both focal damage and network disconnection in lesion-symptom mapping [25]. Additionally, the presence of multicollinearity between lesion locations (where damage to one region frequently co-occurs with damage to another) can complicate interpretation, potentially requiring multivariate approaches like Bayesian network analysis to disentangle true critical regions from epiphenomenal associations [29].
Advanced Applications and Methodological Considerations
Multivariate Extensions and Machine Learning
While traditional VLSM uses univariate approaches, recent advancements have incorporated multivariate lesion-symptom mapping (MLSM) and machine learning techniques to capture complex relationships between distributed lesion patterns and behavior [25]. These methods can identify patterns of damage across multiple regions that collectively predict behavioral deficits, potentially providing improved predictive accuracy compared to univariate approaches.
Machine learning models including Random Forest, Support Vector Regression, and Gradient Boosting have been applied to lesion-symptom mapping, often incorporating features from multiple neuroimaging modalities such as resting-state functional connectivity, structural connectivity, mean diffusivity, and fractional anisotropy in addition to lesion location [25]. Comparative studies suggest that combining traditional VLSM with multivariate approaches provides the most comprehensive understanding of brain-behavior relationships [25].
Limitations and Validation Studies
Despite its utility, VLSM has several important limitations. Conventional VLSM analyses can be susceptible to Type I errors due to combined effects of multicollinearity and lesion frequency, potentially identifying spurious associations [29]. Validation studies have demonstrated that supplementary analyses such as Bayesian network analysis or logistic regression can help control these errors and provide more reliable identification of critical brain regions [29].
The vascular architecture of the brain constrains natural lesion distributions in stroke patients, potentially limiting the brain regions that can be studied. Combining data from different etiologies (e.g., tumor resection, traumatic brain injury) can provide more comprehensive coverage of brain regions [26]. Additionally, VLSM identifies correlations rather than causal relationships, and careful interpretation is needed to distinguish between critical regions for a function versus regions that correlate with damage for other reasons.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Tools for VLSM Studies
| Tool Category | Specific Examples | Function/Purpose |
|---|---|---|
| Neuroimaging Acquisition | Structural MRI (T1, T2, FLAIR), Diffusion-weighted Imaging (DWI) | Visualize lesion anatomy and boundaries; assess white matter integrity |
| Spatial Normalization | MNI Template, SPM, FSL, ANTs | Transform individual brains to standard coordinate space for group analysis |
| Lesion Delineation | ITK-SNAP, MRIcron | Manual or semi-automated creation of binary lesion masks |
| Statistical Analysis | VLSM Software (https://aphasialab.org/vlsm/), R, MATLAB | Perform voxel-wise statistical tests with multiple comparison correction |
| Anatomical Labeling | AAL Atlas, Harvard-Oxford Atlas, JHU White Matter Atlas, Natbrainlab Atlas | Identify anatomical locations of significant voxel clusters |
| Behavioral Assessment | Western Aphasia Battery (WAB), Philadelphia Naming Test (PNT), WMS Family Pictures | Quantify cognitive, language, or memory deficits for correlation with lesion data |
| Visualization | ITK-SNAP, MRIcron, SurfIce | Display statistical maps overlaid on template brains |
Voxel-Based Lesion-Symptom Mapping represents a powerful method for elucidating brain-behavior relationships by leveraging naturally occurring lesion patterns in neurological patients. When implemented with rigorous statistical controls and careful methodological consideration, VLSM can identify brain regions critical for specific cognitive functions with considerable spatial precision. The technique continues to evolve with incorporation of multivariate approaches, machine learning, and multimodal neuroimaging, further enhancing its utility for cognitive neuroscience and clinical neuropsychology. As with any neuroimaging method, appropriate interpretation requires consideration of both the strengths and limitations of the approach, with results ideally converging with evidence from other methodologies such as functional neuroimaging and transcranial magnetic stimulation.
The lesion method, one of the oldest and most established approaches in neuroscience, seeks to understand brain function by studying the behavioral consequences of focal brain damage [30] [1]. For over two centuries, observations of patients with brain lesions have provided foundational insights into the neural basis of complex cognitive processes such as language, memory, and emotion [30]. Historically, this method relied on single-case studies, like the famous patients Phineas Gage, Louis Leborgne (patient "Tan"), and Henry Molaison (H.M.), each of whom dramatically illustrated the relationship between specific brain areas and behavior [1].
In contemporary neuroscience, the field has moved from studying single lesions to sophisticated multivariate lesion-behaviour mapping (LBM) and lesion network mapping (LNM) techniques [31] [24]. These advanced methods leverage large cohorts of individuals with brain lesions, high-resolution neuroimaging, and normative connectome data to statistically map the neuroanatomical regions and distributed brain networks that are necessary for specific cognitive and motor functions [31] [30]. A key strength of these methods is their ability to demonstrate causal necessity, not merely correlation, between a brain region or network and a given behavior [30].
These techniques address a critical clinical challenge: predicting long-term outcomes after brain injury. It remains difficult to make accurate prognoses due to high inter-individual variability in recovery and a historical reliance on clinical judgment rather than quantitative, empirical methods [31]. Because lesion location can be derived from routinely collected clinical neuroimaging, there is a significant opportunity to use this information to make empirically based predictions about post-stroke deficits [31]. This application note details the protocols and analytical frameworks for implementing these advanced mapping techniques in a research setting.
Theoretical Foundations and Key Concepts
From Focal Lesions to Network Dysfunction
Traditional lesion-symptom mapping operates on a fundamental principle: if a lesion in brain region X consistently causes a deficit in function Y, then region X is necessary for function Y [30] [1]. However, a limitation of this focal approach is that symptoms from anatomically disparate lesions can be similar, and lesions in the same location can produce different symptoms, suggesting that a purely focal model is insufficient [24].
Lesion network mapping resolves this paradox by positing that the behavioral effects of a focal lesion are mediated through its impact on a distributed brain network [24]. A lesion not only damages local tissue but also disrupts the function of remote, structurally and functionally connected brain regions [31]. Thus, LNM analyzes the connectivity pattern of brain lesions to identify neuroanatomic correlates of symptoms that cannot be explained by focal anatomic localization alone [24].
Core Methodological Frameworks
Two primary, complementary frameworks form the basis of modern lesion analysis:
Multivariate Lesion-Behaviour Mapping (LBM): This technique uses lesion location and behavioral data from groups of individuals with focal brain damage to produce statistically weighted maps of the neuroanatomical regions that, when damaged, are most strongly associated with specific deficits [31] [32]. It provides a direct link between anatomy and behavior.
Lesion Network Mapping (LNM): This technique uses large, high-quality normative connectome data from healthy individuals to infer the network effects of a focal lesion [31] [24]. The lesion location is used as a seed to identify which functional or structural networks are typically disrupted, thereby linking symptoms to brain networks rather than single points [24]. LNM can be performed using normative functional connectivity (FC) data, which measures correlated brain activity, or structural connectivity (SC) data, which maps white matter tracts [31] [33].
Table 1: Core Concepts in Advanced Lesion Mapping
| Concept | Description | Key Insight |
|---|---|---|
| Lesion-Behaviour Mapping (LBM) | Statistically maps anatomical regions where damage is most associated with a specific deficit [31]. | Identifies brain regions causally necessary for a behavior [30]. |
| Functional Lesion Network Mapping (fLNM) | Maps the lesion's location onto normative resting-state functional connectivity data [31] [24]. | Symptoms arise from disruption of functional brain networks. |
| Structural Lesion Network Mapping (sLNM) | Maps the lesion's location onto normative white matter tractography data [31] [33]. | Symptoms arise from disconnection of structural pathways. |
| Multimodal LNM | Combines both functional and structural connectivity data to predict behavior [33]. | Different modalities provide synergistic information, enhancing predictive power [33]. |
| Normative Connectome | A large, aggregated map of brain connections from healthy individuals used as a reference for LNM [31] [33]. | Allows inference of network disruption without acquiring advanced imaging in patients. |
Quantitative Evidence and Predictive Performance
Recent studies have robustly quantified the predictive value of these techniques, particularly for forecasting long-term outcomes after stroke. The following table summarizes key findings from pivotal research.
Table 2: Predictive Performance of Advanced Lesion Mapping Techniques
| Study & Population | Behavioral Outcome | Mapping Technique | Key Quantitative Finding |
|---|---|---|---|
| Bowren et al. (2022) [31]Independent stroke sample | 12-month cognitive & motor outcomes | LBM, functional LNM, structural LNM | All three modalities predicted significant variance in outcomes. Structural & functional LNM predicted additional variance beyond LBM alone. |
| Bowren et al. (2022) [31]Stroke patients | Language deficits | Functional LNM | Functional LNM performed best for predicting language deficits. |
| Bowren et al. (2022) [31]Stroke patients | Motor deficits | Structural LNM | Structural LNM performed best for predicting motor deficits. |
| Jimenez-Marin et al. (2022) [33]54 stroke patients | Sensorimotor behavior (combined motor/sensory tests) | Multimodal LNM (FC+SC) | The functional modality contributed more to prediction than the structural one. |
| Jimenez-Marin et al. (2022) [33]54 stroke patients | Sensorimotor behavior | Unimodal Structural LNM | Predictive performance was strongly dependent on correcting for lesion size. |
| Jimenez-Marin et al. (2022) [33]54 stroke patients | Sensorimotor behavior | Unimodal Functional LNM | Provided similar predictive performance regardless of lesion size correction. |
Experimental Protocols
This section provides a detailed, step-by-step protocol for a comprehensive multimodal lesion network mapping study, based on established methodologies [31] [33].
Protocol: Multimodal Lesion Network Mapping for Predicting Post-Stroke Outcomes
I. Study Cohorts and Data Collection
Cohort Definition:
- Derivation Cohorts: Secure data from large, chronic lesion registries (e.g., the Iowa Neurological Patient Registry for cognitive maps, the NICHE cohort for motor maps). These participants should have stable, chronic lesions (≥3 months post-onset) and comprehensive behavioral test data [31].
- Prediction Cohort: Recruit an independent sample of acute stroke patients (e.g., within 2 weeks of onset) with baseline structural MRI and longitudinal behavioral assessments at 2 weeks, 3 months, and 12 months post-stroke [31].
Behavioral Assessment:
- Cognitive Domains: Administer standardized tests for expressive language (Boston Naming Test), receptive language (Token Test), and verbal memory (Rey Auditory Verbal Learning Test) [31].
- Motor Domains: Administer upper extremity motor tests such as the Fugl-Meyer Assessment (FMA-UE) and the Action Research Arm Test (ARAT) [33].
- Sensory Domains: Administer somatosensory tests like the Erasmus-modified Nottingham Sensory Assessment (Em-NSA) and the Perceptual Threshold of Touch (PTT) [33].
Neuroimaging Data Acquisition:
- Patient Data: Acquire T1-weighted and T2-FLAIR structural MRI for all patients. Lesions must be traced manually on the structural images using software such as ITK-SNAP or MRIcron.
- Normative Connectome Data: Obtain preprocessed, high-quality normative data from public repositories like the Human Connectome Project (HCP). This should include resting-state fMRI (for functional connectivity) and diffusion-weighted MRI (for structural connectivity) from a large sample (e.g., N=1000) of healthy adults [33].
II. Image Processing and Analysis Pipeline
Lesion Preprocessing:
- Normalize all patient lesion masks into a standard stereotaxic space (e.g., MNI152).
- Check and manually correct normalization errors to ensure lesion placement accuracy.
Generating Lesion-Behaviour Maps (LBM):
- For the derivation cohorts, perform voxel-wise or multivariate regression (e.g., with SVR-LSM) between the lesion maps and behavioral scores for each tested domain.
- The output is a statistical map for each behavior, where the value at each voxel represents its weight in predicting the deficit.
Generating Lesion Network Maps (LNM):
- Seed Definition: Use the peak coordinates from the LBM results, or the entire lesion mask from each patient in the prediction cohort, as seeds [31].
- Functional LNM: For each seed, query the normative functional connectome to create a map of all brain regions functionally connected to the seed location.
- Structural LNM: For each seed, use normative tractography data to create a map of the white matter tracts structurally connected to the seed location.
- Disconnection Map: For each patient, create a final map that quantifies the overlap between their specific lesion and the normative functional or structural network. This represents the extent of network disruption.
III. Statistical Modeling and Prediction
Data Reduction:
- Concatenate the disconnection maps (or LBM maps) from all patients in the prediction cohort.
- Perform Principal Component Analysis (PCA) on this concatenated matrix to reduce dimensionality and derive principal components for use in the predictive model [33].
Model Building and Validation:
- Use a latent growth curve model or Canonical Correlation Analysis (CCA) to relate the principal components (brain data) to the longitudinal behavioral scores [31] [33].
- Employ a cross-validation framework (e.g., leave-one-out or k-fold) to train the model and assess its predictive accuracy on unseen data. Compare the variance explained by LBM, functional LNM, and structural LNM, both individually and in combination.
Figure 1: Workflow for Multimodal Lesion-Outcome Prediction
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Resources for Lesion Network Mapping Studies
| Category / Item | Specific Example / Software | Function and Application Note |
|---|---|---|
| Neuroimaging Software | ITK-SNAP, MRIcron | Manual tracing and segmentation of lesion masks from structural T1/T2-FLAIR MRI [31]. |
| Normative Connectome Data | Human Connectome Project (HCP) | Provides high-quality, preprocessed functional and structural connectivity data from healthy adults for LNM [33]. |
| Connectome Workbench | HCP Workbench Command (-cifti-palette) | A suite of command-line tools for visualization and processing of HCP-style CIFTI data [34]. |
| Python Libraries | Nilearn (plot_connectome) | A Python module for statistical learning on neuroimaging data; used for plotting connectomes and network analysis [35] [36]. |
| Statistical & Machine Learning Tools | Support Vector Regression for LSM (SVR-LSM), Canonical Correlation Analysis (CCA) | Multivariate algorithms for relating brain lesions or network disconnection to behavioral outcomes [31] [33]. |
| Standardized Behavioral Tests | Boston Naming Test (BNT), Fugl-Meyer Assessment (FMA) | Provide quantitative, domain-specific measures of cognitive and motor function for correlation with imaging data [31] [33]. |
| Standard Brain Atlas | MNI152 Space | Standard stereotaxic coordinate system for spatial normalization of all patient images, enabling group-level analysis [31]. |
Implementation and Visualization
Successful implementation requires careful attention to technical details, especially in the visualization of results. The following protocol outlines the use of the Nilearn library in Python to create a connectome plot, which is a common final step for displaying network findings.
Protocol: Visualizing Lesion Networks with Nilearn
Prepare the Inputs:
- Adjacency Matrix: Create an
n x nmatrix representing the connection strengths between all network nodes. This can be derived from the functional correlation matrix or tractography streamline counts. - Node Coordinates: Define an
n x 3list of (x, y, z) coordinates in MNI space for each network node. - Node Colors: Create a list of colors for each node. This can be a single color for all nodes, or a list of different colors to indicate different functional networks [35] [37]. Use matplotlib color names or hex codes. Ensure the list is a Python
listtype, not a NumPy array, to avoid a known issue in some Nilearn versions [35].
- Adjacency Matrix: Create an
Generate the Plot:
- Use
nilearn.plotting.plot_connectome()with the prepared inputs [36]. - Key parameters include:
node_size: To emphasize important hubs.edge_cmap: Colormap for edges (e.g., 'RdBu_r').edge_threshold: To display only the strongest connections.display_mode: For choosing the view (e.g., 'ortho', 'lzr').
- Use
Example Code Snippet:
Figure 2: Connectome Diagram Showing Node Connections
Within neuroscience research aimed at correlating specific brain areas with behavior, the lesion method represents a foundational experimental approach. This methodology is predicated on a core principle: observing behavioral changes following the precise disruption of a discrete brain region allows researchers to infer the function of that region [1] [21]. The study of historically significant patients, such as Phineas Gage and Henry Molaison, provided seminal insights into the roles of the frontal lobe in personality and the hippocampus in memory formation, respectively [1]. In modern preclinical research, this principle is systematically applied through experimentally induced lesions in animal models, enabling controlled investigation of brain function and the evaluation of pharmacological interventions for neurological and psychiatric disorders. These models serve as a critical bridge between basic neurobiology and the development of novel therapeutic agents, allowing for the precise dissection of neural circuits and the screening of potential drugs in a controlled system. This document provides detailed application notes and protocols for establishing and utilizing these models, framed within the rigorous standards required for ethical and scientifically valid research.
Animal Model Selection and Evaluation
The selection of an appropriate animal model is paramount to the success and validity of any study investigating brain-behavior relationships. A model must not only recapitulate the specific neural disruption of interest but also be amenable to the behavioral assays designed to measure functional outcomes.
Model Evaluation Criteria
Following lesion induction, a standardized histopathological evaluation is essential. It is recommended to use established systems like the “Histologic Scoring of Gastritis and Gastric Cancer in Mouse Models” as a template for creating consistent, semi-quantitative assessments of neural damage [38]. Such a system should evaluate key parameters such as:
- Location and Extent of Lesion: Precise mapping of the damaged brain area.
- Neuronal Loss: Quantification of neuronal cell death within the target region.
- Gliosis: Assessment of astrocyte and microglial activation, indicating neuroinflammation.
- Vacuolation: Presence of fluid-filled spaces indicating tissue damage.
The anatomical differences between rodent and human brains must be considered during interpretation. For instance, a behavioral deficit in a rodent following a frontal lobe lesion may not be functionally identical to the deficits observed in the famous case of Phineas Gage, underscoring the need for careful translational analysis [38] [1].
The table below summarizes key characteristics of commonly used experimentally induced lesion models in neuroscience research.
Table 1: Characteristics of Common Experimentally Induced Lesion Models
| Model Type | Primary Mechanism of Action | Typical Lesion Size (mm³) | Key Behavioral Assays | Temporal Profile of Deficit |
|---|---|---|---|---|
| Excitotoxic (e.g., Kainic Acid) | Agonism of glutamate receptors, leading to neuronal excitation and death | 0.5 - 2.0 | Spontaneous seizures, Morris Water Maze, Open Field | Acute onset (hours), can be progressive |
| Mechanical/ Aspiration | Physical disruption of brain tissue | 1.0 - 5.0 (size-dependent on procedure) | Sensorimotor tests, Cognitive tasks | Immediate (post-recovery) |
| Photothrombotic | Light-induced thrombosis causing focal ischemia | 0.1 - 1.5 | Cylinder Test, Adhesive Removal Test | Stable deficit within 24 hours |
| Stereotaxic Injection | Highly localized delivery of toxins or viruses | 0.05 - 1.0 | Dependent on targeted brain region | Dependent on injected agent |
Experimentally Induced Lesion Protocols
This section provides detailed methodologies for establishing key lesion models. All procedures must receive prior approval from the Institutional Animal Care and Use Committee (IACUC), and consultation with veterinary staff is strongly encouraged during the protocol development phase [39].
Protocol: Excitotoxic Lesion of the Hippocampus
Principle: Intracerebral injection of an excitatory amino acid, such as Kainic Acid, selectively ablates neuronal cell bodies while sparing fibers of passage, modeling temporal lobe epilepsy and hippocampal-dependent memory deficits.
Materials:
- Kainic Acid (e.g., 1 mg/mL solution in sterile saline)
- Stereotaxic apparatus
- Hamilton microsyringe (e.g., 10 µL)
- Isoflurane anesthesia system
- Standard surgical instruments
- Research Reagent Solutions:
- Kainic Acid: An agonist for ionotropic glutamate receptors, used to induce excitotoxic neuronal death.
- Isoflurane: A volatile inhalational anesthetic for inducing and maintaining surgical anesthesia.
- Sterile Saline (0.9%): A physiological buffer used for dissolving drugs and as a vehicle control.
Procedure:
- Anesthesia and Preparation: Induce and maintain anesthesia using 2-3% isoflurane in oxygen. Place the animal in the stereotaxic frame, ensuring the skull is level. Apply ophthalmic ointment to prevent corneal drying.
- Stereotaxic Surgery: Shave the scalp and disinfect the surgical site. Make a midline incision to expose the skull. Identify Bregma and calculate the target coordinates for the hippocampus (e.g., Anteroposterior: -2.0 mm, Mediolateral: ±1.5 mm, Dorsoventral: -1.8 mm from Bregma). Drill a small craniotomy at the target site.
- Microinjection: Lower a Hamilton syringe filled with the Kainic Acid solution to the target depth. Infuse 0.2 µL of the solution at a rate of 0.1 µL/min. Allow the needle to remain in place for an additional 5 minutes post-infusion to prevent backflow.
- Closure and Recovery: Slowly retract the needle. Suture the skin incision and administer a postoperative analgesic (e.g., Meloxicam, 5 mg/kg). Place the animal in a clean, warm cage and monitor until fully ambulatory.
Experimental Workflow: The following diagram visualizes the key steps involved in creating and validating an excitotoxic lesion model.
Protocol: Focal Ischemic Lesion via Photothrombosis
Principle: This technique induces a highly reproducible, focal ischemic infarct by systemically administering a photosensitive dye (e.g., Rose Bengal) and then illuminating a specific region of the exposed skull with a cold light source, activating the dye and causing local thrombosis.
Materials:
- Rose Bengal (e.g., 10 mg/mL in saline)
- Cold light source (e.g., fiber-optic lamp, 150 W)
- Stereotaxic apparatus with light guide holder
- Research Reagent Solutions:
- Rose Bengal: A photosensitive dye that, upon light activation, produces singlet oxygen, leading to endothelial damage and platelet activation, thus inducing focal thrombosis.
Procedure:
- Anesthesia and Preparation: Anesthetize the animal and secure it in the stereotaxic frame. Perform a scalp incision and carefully clear the skull surface of connective tissue.
- Dye Administration: Inject Rose Bengal intraperitoneally (100 mg/kg).
- Illumination: Position the fiber-optic light guide over the target brain region (e.g., primary motor cortex). Illuminate the area for 10-20 minutes. The light intensity and wavelength must be carefully calibrated.
- Recovery: Suture the incision, administer analgesics, and monitor the animal closely post-operatively. Behavioral deficits are typically evident within 24 hours.
Pharmacological Intervention Protocols
Once a stable lesion-induced behavioral deficit is established, the model can be used to test the efficacy of pharmacological agents. The principles of Replacement, Reduction, and Refinement (the "Three Rs") must be considered in the experimental design, ensuring the number of animals used is the minimum necessary to obtain statistically valid results [39].
Quantitative Data from Intervention Studies
The following table summarizes potential outcomes for different drug classes tested in a model of excitotoxic hippocampal lesion, illustrating how data can be structured for analysis.
Table 2: Exemplar Pharmacological Intervention Data in a Hippocampal Lesion Model
| Drug Class / Compound | Mechanism of Action | Dosage (mg/kg) | Behavioral Test | Outcome vs. Lesion-Control (Mean % Improvement) | Statistical Significance (p-value) |
|---|---|---|---|---|---|
| NMDA Receptor Antagonist | Blocks NMDA glutamate receptors | 10 | Morris Water Maze | +15% | p < 0.05 |
| GABAA Receptor Agonist | Enhances inhibitory GABAergic transmission | 2 | Open Field Test | +5% | p > 0.05 (NS) |
| Acetylcholinesterase Inhibitor | Increases synaptic acetylcholine | 1 | Passive Avoidance | +25% | p < 0.01 |
| SSRI | Selective serotonin reuptake inhibition | 15 | Forced Swim Test | +30% | p < 0.01 |
Protocol: Testing a Putative Neuroprotective Agent
Principle: Administer a drug candidate either prior to (pre-treatment) or following (post-treatment) lesion induction to assess its ability to prevent or mitigate neuronal damage and associated behavioral deficits.
Materials:
- The drug candidate (e.g., dissolved in saline or vehicle)
- Control vehicle (e.g., sterile saline)
- Syringes and needles for injection (IP, SC, or IV)
Procedure:
- Randomization and Grouping: Randomly assign animals to one of four groups (n=10-12/group is a common starting point, justified by a power analysis):
- Group 1: Sham + Vehicle
- Group 2: Sham + Drug
- Group 3: Lesion + Vehicle
- Group 4: Lesion + Drug
- Dosing Regimen:
- For pre-treatment, administer the drug or vehicle 30-60 minutes before the lesion procedure.
- For post-treatment, begin drug administration at a designated time after lesion induction (e.g., 1 hour, 6 hours) and continue for a set period (e.g., 7 days).
- Behavioral Testing: Conduct behavioral assays relevant to the function of the lesioned brain area after a suitable recovery and treatment period (e.g., 1-2 weeks post-lesion).
- Histological Analysis: Upon conclusion of behavioral testing, perfuse animals and extract brains for histological processing to quantify the extent of the lesion and neuronal survival in the drug-treated group compared to the lesion-vehicle control.
Pharmacological Screening Workflow: The pathway from initial hypothesis to conclusion in a pharmacological intervention study is outlined below.
The Scientist's Toolkit: Research Reagent Solutions
A successful lesion and pharmacological study relies on a suite of essential reagents and materials. The following table details key items and their functions.
Table 3: Essential Research Reagents for Lesion and Pharmacological Studies
| Category | Item | Primary Function |
|---|---|---|
| Lesion-Inducing Agents | Kainic Acid, Quinolinic Acid, 6-OHDA | To induce excitotoxic or selective neurotoxic lesions in specific brain regions. |
| Photosensitizers | Rose Bengal | To produce focal ischemic lesions via photothrombosis upon light activation. |
| Anesthetics & Analgesics | Isoflurane, Ketamine/Xylazine, Buprenorphine, Meloxicam | To ensure humane and pain-free surgical procedures and post-operative recovery. |
| Pharmacological Agents | NMDA antagonists, Acetylcholinesterase inhibitors, SSRIs | To test hypotheses regarding neuroprotection or functional recovery in lesion models. |
| Sterotaxic Supplies | Hamilton Syringes, Drill Bits, Sterile Saline | To enable precise, repeatable targeting of specific brain coordinates for injections. |
| Histological Reagents | Paraformaldehyde, Cresyl Violet, antibodies for GFAP/Iba1 | To fix brain tissue and verify lesion location, size, and cellular responses. |
Application Notes: Lesion Method for Correlating Brain and Behavior
The lesion method is a foundational technique in cognitive neuroscience, based on the principle that damage to a specific brain structure (X) leads to changes in a particular behavior or cognitive function (Y), allowing researchers to infer that structure X is necessary for function Y [21] [17]. Applications span the study of memory, perception, and decision-making, providing causal evidence for brain-behavior relationships that complement other neuroscientific methods.
Applications in Memory, Perception, and Decision-Making
- Memory: Studies of patients with medial temporal lobe lesions, including the hippocampus, have been pivotal in establishing the critical role of this region in forming new episodic memories [40] [21]. The declarative memory system, which includes semantic and episodic memory, is particularly dependent on these structures [40].
- Perception and Language: Lesion studies have been instrumental in localizing language functions. Damage to Broca's area results in non-fluent, effortful speech (Broca's aphasia), whereas damage to Wernicke's area results in fluent but meaningless speech and impaired comprehension (Wernicke's aphasia) [21] [17]. This double dissociation strongly supports the notion that these are distinct, specialized brain areas.
- Decision-Making and Social Behavior: The famous case of Phineas Gage, who suffered a traumatic lesion to his frontal lobes, revealed the crucial role of this region in personality, emotional regulation, and socially appropriate behavior [21] [17]. Furthermore, research indicates that the ventromedial prefrontal cortex (vmPFC) is vital for value-based decision-making, and its interaction with the hippocampus is critical when decisions rely on episodic memory [40].
Quantitative Data on Lesion Effects
Table 1: Behavioral Correlates of Specific Brain Lesions
| Brain Area Lesioned | Observed Functional Deficit | Implied Brain Function |
|---|---|---|
| Broca's Area | Non-fluent, effortful speech; difficulty with speech production and articulation [21] [17] | Speech production, language processing [21] [17] |
| Wernicke's Area | Fluent but meaningless speech; impaired language comprehension [21] [17] | Speech comprehension, language analysis [21] [17] |
| Frontal Lobes | Dramatic personality changes; impaired social conduct, planning, and decision-making [17] | Executive functions, personality, social behavior [17] |
| Hippocampus/Medial Temporal Lobe | Inability to form new episodic memories (Anterograde Amnesia) [40] [21] | Encoding of new episodic memories, navigation [40] [21] |
| Parietal-Temporal-Occipital Association Area | Agraphia (inability to write) without motor deficits [21] | Integration of sensory information for complex tasks like writing [21] |
| Ventromedial Prefrontal Cortex (vmPFC) | Disrupted value-based decision-making, especially under memory uncertainty [40] | Computation of subjective value, integration of memory signals for choice [40] |
Table 2: Lesioning Techniques and Their Characteristics
| Lesioning Technique | Key Characteristics | Primary Research Applications |
|---|---|---|
| Surgical Lesioning | Precise physical removal or disconnection of brain tissue; invasive and permanent [17] | Therapeutic interventions (e.g., epilepsy); creating animal models of brain disorders [17] |
| Chemical Lesioning | Uses selective neurotoxins to target specific neuron types; high cellular specificity [17] | Studying functions of specific neurotransmitter systems (e.g., dopamine in Parkinson's) [17] |
| Electrical (Electrolytic) Lesioning | Uses electrical currents to create localized, permanent damage; high spatial precision [17] | Animal research for mapping well-defined brain nuclei and pathways [17] |
| Reversible Inactivation | Temporarily disables brain areas via cooling, pharmacological agents, or optogenetics [17] | Establishing causal links without permanent damage; within-subject experimental designs [17] |
Experimental Protocols
Protocol 1: Investigating Memory Bias in Decision-Making Using the Lesion Method
This protocol outlines a method to investigate how episodic memory recall influences value-based decisions in patients with lesions to the hippocampus or vmPFC, compared to neurotypical controls [40].
1. Objective: To determine the causal role of the hippocampus and vmPFC in the memory bias—the preference for choice options that can be successfully retrieved from memory.
2. Materials:
- Participants: Three matched groups: (1) patients with focal hippocampal lesions, (2) patients with focal vmPFC lesions, (3) neurotypical control participants.
- Stimuli: A set of unfamiliar objects (e.g., abstract art, novel gadgets).
- Software: fMRI or EEG for neural activity recording in control participants [40] [21].
- Task Programming: Experiment software (e.g., PsychoPy, E-Prime).
3. Procedure:
- Phase 1: Encoding. Participants are presented with object-value pairs, where each object is associated with a specific monetary reward value.
- Phase 2: Memory Retrieval Practice. A subset of the objects is presented for repeated memory recall practice, creating "well-remembered" and "less-remembered" items.
- Phase 3: Decision-Making Task. Participants perform a forced-choice task between pairs of objects. Neural activity is recorded in controls via fMRI to monitor hippocampus-vmPFC connectivity [40].
- Phase 4: Memory Recognition Test. Participants complete a surprise recognition test for all objects to explicitly measure memory performance.
4. Data Analysis:
- Calculate the rate of choosing higher-valued items separately for well-remembered and less-remembered categories.
- Compare choice patterns and the strength of the memory bias across the three participant groups.
- For control group fMRI data, analyze effective connectivity (e.g., using dynamic causal modeling) between hippocampus and vmPFC during choices involving less-remembered items [40].
Protocol 2: Double Dissociation of Language Function via Natural Lesions
This protocol leverages studies of patients with naturally occurring strokes to demonstrate a double dissociation between speech production and comprehension [21] [17].
1. Objective: To provide behavioral evidence for the functional independence of Broca's area and Wernicke's area in language processing.
2. Materials:
- Participants: Two patient groups: (1) Broca's aphasia patients with damage in the left inferior frontal gyrus, (2) Wernicke's aphasia patients with damage in the left superior temporal gyrus.
- Neuroimaging: MRI or CT scans for precise lesion localization [21].
- Stimuli: Standardized language assessment tools including picture-naming tasks, conversational prompts, and auditory comprehension tests.
3. Procedure:
- Step 1: Patient Selection and Lesion Localization. Recruit patients and use structural MRI to confirm the location and extent of brain damage, categorizing them into the two groups [21].
- Step 2: Behavioral Testing.
- Speech Production Assessment: Record and analyze patients' spontaneous speech and their ability to repeat sentences.
- Speech Comprehension Assessment: Administer tests where patients must follow verbal commands or match spoken words to pictures.
- Step 3: Data Collection. Transcribe and score speech samples for fluency, grammatical correctness, and effort. Score comprehension tests for accuracy.
4. Data Analysis:
- Contrast the two groups' performance profiles. The key is to demonstrate a crossover interaction: Broca's patients should show severe deficits in production but relatively preserved comprehension, while Wernicke's patients show the opposite pattern [21] [17].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Lesion-Based Research
| Item / Reagent | Function / Application |
|---|---|
| Ibotenic Acid / Kainic Acid | Chemical lesioning agents; excitotoxins that selectively destroy neuron cell bodies while sparing passing fibers, allowing for specific functional ablation [17]. |
| Stereo-tactic Apparatus | Provides 3D coordinate guidance for precise targeting of deep brain structures during surgical, chemical, or electrical lesioning in animal models [17]. |
| Cooling Probe /Cryoloop | A reversible lesioning technique that temporarily inactivates a targeted brain region by lowering its temperature, allowing for within-subject control experiments [17]. |
| Structural MRI (Magnetic Resonance Imaging) | Non-invasive imaging for precise anatomical localization and volumetric assessment of natural lesions in human patients [21]. |
| fMRI (functional MRI) | Measures brain activity by detecting changes in blood flow. Used in conjunction with lesion studies to map functional connectivity and compensatory plasticity in intact networks [40] [21]. |
| Standardized Neuropsychological Batteries | Validated sets of tasks (e.g., Boston Diagnostic Aphasia Examination) to quantitatively assess behavioral deficits in memory, language, and executive function post-lesion [21] [17]. |
Visualizations
Lesion Method Logic and Causal Inference
Neural Circuit for Memory-Based Decision Making
Double Dissociation Experimental Logic
Application Notes: Lesion Network Mapping and Clinical Translation
The study of brain lesions remains a foundational method for correlating specific brain areas with behavior, cognitive functions, and clinical symptoms. Modern approaches have evolved from analyzing single lesions to mapping entire brain networks disrupted by a lesion, thereby informing diagnosis, prognostic predictions, and novel targets for neuromodulation therapies [41] [17].
1.1 Informing Diagnosis and Localization of Function Lesion studies have been pivotal in establishing the functional roles of specific brain regions. Historical cases, such as Phineas Gage, highlighted the role of the frontal lobes in personality and social behavior, while lesions in Broca's area were crucial for establishing its necessity in speech production [17]. Contemporary research extends this principle by using lesion-symptom mapping to identify critical nodes in the brain's functional networks. A lesion in a specific location can cause a deficit not by itself, but by disrupting the function of a connected network. This network-based understanding allows for more accurate diagnosis of the neural underpinnings of neurological and psychiatric symptoms [41].
1.2 Prognostic Applications The location and extent of a brain lesion can provide critical information for predicting functional recovery. By correlating lesion characteristics with clinical outcomes, clinicians can develop more personalized prognostic models. For instance, understanding which specific neural pathways are damaged following a stroke can help predict the potential for recovery of motor function or language abilities, guiding rehabilitation strategies and setting realistic patient expectations [17].
1.3 Discovery and Validation of Neuromodulation Targets Lesion studies directly inform neuromodulation by identifying brain areas whose disruption leads to therapeutic benefits. For example, creating focal lesions in the ventral intermediate nucleus (Vim) of the thalamus has long been a treatment for essential tremor. The success of such lesioning procedures provided the foundational evidence for targeting the same area with deep brain stimulation (DBS) [41] [17]. Modern techniques, particularly the integration of advanced imaging like diffusion MRI (dMRI) and functional MRI (fMRI), are shifting the paradigm from targeting anatomical structures to modulating specific dysfunctional brain networks identified through lesion mapping [41].
Table 1: Established and Emerging Neuromodulation Approaches Informed by Lesion Studies [41]
| Application Area | Invasive Neuromodulation | Non-Invasive Neuromodulation | Key Associated Brain Targets/Circuits |
|---|---|---|---|
| Movement Disorders (e.g., Parkinson's Disease, Essential Tremor) | Deep Brain Stimulation (DBS), Spinal Cord Stimulation (SCS) | Transcranial Magnetic Stimulation (TMS), Transcranial Direct Current Stimulation (tDCS) | Subthalamic Nucleus (STN), Globus Pallidus internus (GPi), Ventral Intermediate Nucleus (Vim), Cerebellothalamic Tract (CTT) |
| Drug-Resistant Epilepsy | Vagus Nerve Stimulation (VNS), Responsive Neurostimulation (RNS) | Non-invasive Vagus Nerve Stimulation | Anterior Nucleus of Thalamus (for DBS), Seizure Foci (for RNS) |
| Chronic Neuropathic Pain | Spinal Cord Stimulation (SCS), Dorsal Root Ganglion Stimulation | Transcutaneous Electrical Nerve Stimulation (TENS) | Dorsal Columns of Spinal Cord |
| Psychiatric Disorders (e.g., OCD, Depression) | Deep Brain Stimulation (DBS)* | Transcranial Magnetic Stimulation (TMS), Electroconvulsive Therapy (ECT) | Subgenual Cingulate, Ventral Capsule/Ventral Striatum |
| Stroke Recovery | Deep Brain Stimulation (DBS)*, Brain-Computer Interface (BCI) | Transcranial Direct Current Stimulation (tDCS), Vagus Nerve Stimulation | Peri-lesional Cortex, Corticospinal Tract |
| Hearing & Vision Loss | Cochlear Implant, Retinal Stimulation | — | Cochlea, Retina |
Note: *DBS for psychiatric disorders and stroke recovery is often investigational. DBS for Obsessive-Compulsive Disorder (OCD) is FDA-approved [41].
Table 2: Lesioning Techniques for Target Validation in Preclinical Research [17]
| Technique | Mechanism of Action | Temporality | Specificity | Primary Research Applications |
|---|---|---|---|---|
| Surgical Lesioning | Physical removal or disconnection of brain tissue. | Permanent | Low to Moderate (area-specific) | Establishing causal roles of brain regions in behavior; modeling gross brain injuries. |
| Chemical Lesioning | Application of neurotoxins (e.g., 6-OHDA) to selectively destroy specific neuron types. | Permanent | High (cell-type specific) | Modeling neurodegenerative diseases (e.g., Parkinson's); studying neurotransmitter systems. |
| Electrical (Electrolytic) Lesioning | Use of electrical current to ablate tissue. | Permanent | Moderate (precise location) | Validating functional anatomy of specific pathways in animal models. |
| Reversible Inactivation | Temporary suppression of neural activity via cooling probes or pharmacological agents (e.g., muscimol). | Temporary | High (spatially and temporally precise) | Establishing causal necessity without permanent damage; within-subject experimental designs. |
Experimental Protocols
3.1 Protocol for Lesion Network Mapping to Identify Neuromodulation Targets
Objective: To identify a common brain network shared by lesions that produce a specific therapeutic effect (e.g., tremor arrest), for the purpose of deriving a new neuromodulation target.
Materials:
- Cohort of patient structural neuroimages (MRIs) with lesions that successfully ameliorated the symptom of interest.
- Normative connectome database (e.g., from large-scale resting-state fMRI data from healthy subjects).
- Neuroimaging analysis software (e.g., FSL, SPM, or specialized connectivity toolboxes).
- Statistical computing environment (e.g., R, Python with NumPy/SciPy).
Methodology:
- Lesion Localization: Precisely segment the lesion boundaries for each patient in the cohort onto a standard brain template (e.g., MNI space).
- Seed-Based Connectivity Mapping: For each lesion mask, use the normative connectome to identify all brain regions that are functionally connected to the lesion location. This generates a "functional connectivity map" for each lesion.
- Network Overlap Analysis: Overlay the individual functional connectivity maps to identify a common brain network that is significantly connected to all, or most, of the effective lesion sites.
- Target Identification: The hub of this common network, often a distinct brain region outside the lesion locations themselves, represents a candidate neuromodulation target.
- Validation: The derived target is validated by examining whether effective DBS sites in independent patient cohorts align with this network hub, and by testing stimulation at this site in new patients [41].
3.2 Protocol for Chemical Lesioning in a Preclinical Parkinson's Disease Model
Objective: To unilaterally lesion the nigrostriatal pathway in a rodent model using the neurotoxin 6-Hydroxydopamine (6-OHDA) to validate the role of the substantia nigra and striatum in motor control and to test potential therapies.
Materials:
- Stereotaxic surgical apparatus.
- 6-Hydroxydopamine hydrochloride (6-OHDA).
- Artificial cerebrospinal fluid (aCSF) or saline with 0.02% ascorbic acid (as vehicle).
- Hamilton microsyringe for precise intracerebral infusion.
- Anesthetic (e.g., ketamine/xylazine or isoflurane).
- Post-operative analgesic and care materials.
- Behavioral testing equipment (e.g., apomorphine-induced rotation bowl, cylinder test).
Methodology:
- Pre-surgical Preparation: Anesthetize the rodent and secure its head in the stereotaxic frame. Confirm lack of pedal reflex. Shave scalp and sterilize the surgical site.
- Stereotaxic Injection: Calculate the coordinates for the target structure (e.g., medial forebrain bundle or substant nigra pars compacta). Load the 6-OHDA solution (e.g., 4-12 μg in 2-4 μL of vehicle) into the microsyringe. Lower the syringe to the target coordinates and infuse the solution slowly (e.g., 0.5 μL/min). Leave the syringe in place for an additional 5 minutes post-infusion to prevent backflow.
- Post-operative Care: Suturer or staple the wound. Administer analgesic and place the animal in a warm, clean recovery cage until fully ambulatory. Monitor daily for signs of distress.
- Behavioral Validation: After a 1-3 week recovery period, conduct behavioral tests. Administer a dopamine receptor agonist (e.g., apomorphine) and place the animal in a rotation bowl. Consistent unilateral rotation away from the side of the lesion (contralateral rotation) confirms a successful and extensive dopaminergic denervation.
- Histological Verification: Upon conclusion of the experiment, perfuse the animal and extract the brain. Section the brain and stain for tyrosine hydroxylase (TH) to visually confirm the loss of dopaminergic neurons in the substantia nigra and nerve terminals in the striatum on the lesioned side [17].
Visualizations
Lesion Network Mapping Workflow
Neuromodulation Target Derivation Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Lesion and Neuromodulation Research
| Item | Function/Application |
|---|---|
| 6-Hydroxydopamine (6-OHDA) | A selective neurotoxin used in chemical lesioning to ablate catecholaminergic (dopaminergic and noradrenergic) neurons, essential for creating preclinical models of Parkinson's disease [17]. |
| Stereotaxic Apparatus | A precision instrument used to target specific, millimeter-scale coordinates in the brain of an animal for procedures such as lesioning or electrode implantation [17]. |
| Normative Connectome Database | A large dataset of functional or structural brain connectivity from healthy individuals, used in lesion network mapping to identify the brain networks functionally connected to a lesion location [41]. |
| Diffusion MRI (dMRI) | An advanced imaging modality that maps white matter tracts in the brain. It is used to visualize and quantify the structural connectivity disrupted by a lesion or targeted by neuromodulation [41]. |
| Deep Brain Stimulation (DBS) System | An implantable medical device that delivers controlled electrical pulses to specific brain targets, providing therapeutic neuromodulation for conditions like Parkinson's disease and essential tremor [41]. |
Addressing Methodological Challenges and Enhancing Lesion Study Design
The lesion method is a foundational approach in neuroscience for correlating specific brain areas with behavior and cognitive functions. However, a significant challenge in this field is lesion heterogeneity—where patients with similar behavioral symptoms have lesions in different anatomical locations. Traditional lesion mapping methods, which rely on finding overlap in the physical location of brain damage, often fail when symptoms arise from dysfunction in a common brain network rather than a single, shared brain region [42]. This application note outlines robust, network-based strategies for selecting patient cohorts to overcome the challenge of lesion heterogeneity, thereby improving the validity and replicability of lesion-deficit research.
The Problem of Anatomical Heterogeneity
Lesion heterogeneity manifests when patients exhibiting the same syndrome, such as antisocial behavior, visual hallucinations, or central post-stroke pain, show little to no overlap in the physical location of their brain lesions [43] [42]. For instance, one study of 17 patients who developed antisocial behavior following a brain lesion found that the lesions themselves were spatially diverse, affecting areas including the medial prefrontal cortex, amygdala, and anterior temporal lobe [43].
This heterogeneity poses a critical problem for traditional group-level lesion overlap analyses, as they cannot identify a common neural substrate for the observed symptoms. The underlying principle of modern network-based solutions is that the clinical expression of a lesion is determined not solely by the damaged area itself, but by the distributed brain networks that the lesion disrupts [42] [44]. Consequently, cohort selection and analysis must evolve from a focus on lesion location to a focus on lesion network topology.
Core Strategies for Cohort Selection
To address heterogeneity, researchers should employ the following interconnected strategies during cohort selection and characterization.
Strategy 1: Lesion Network Mapping
Lesion Network Mapping (LNM) moves beyond the lesion site to identify the brain networks that are functionally connected to the lesion location.
- Protocol: Functional Connectivity of Lesion Locations
- Lesion Localization: For each patient, manually trace the brain lesion onto a standardized brain template (e.g., MNI space) to create a binary lesion mask [43] [42].
- Utilize Normative Connectomes: Use a large, high-quality normative functional connectivity dataset from healthy participants (e.g., from the Human Connectome Project) as a reference network.
- Seed-Based Connectivity Mapping: Treat each patient's lesion mask as a seed region. Calculate the whole-brain functional connectivity of this seed using the normative data. This generates a lesion network map for each patient, representing the brain regions that are typically functionally coupled with the lesioned area [42] [44].
- Identify Network Overlap: Overlay the individual lesion network maps from all patients in the cohort. Statistically identify regions where connectivity is consistently disrupted across patients, despite their anatomical lesion heterogeneity [42]. This common network node is often more directly related to the clinical syndrome than the lesion location itself.
Strategy 2: Data-Driven Subgrouping
When a cohort exhibits a broad behavioral phenotype, data-driven techniques can identify biologically meaningful subgroups.
- Protocol: Meta-Analytic Co-Activation Profiling
- Seed Definition: Use individual or group-averaged lesion masks as seeds.
- Interrogation with Task-Based fMRI Databases: Interrogate these seeds against a database of task-based functional neuroimaging studies (e.g., using meta-analytic co-activation modeling - MACM). This identifies brain regions that are consistently co-activated with the lesion seed during specific mental processes [43].
- Clustering Analysis: Apply data-driven clustering algorithms (e.g., k-means) to the resulting co-activation patterns. This can reveal distinct subgroups of patients whose lesions disrupt different functional networks, such as those for emotional face processing, general emotion processing, or reward processing [43].
- Cohort Refinement: Use these network-based subgroups to stratify the patient cohort for more homogeneous analysis, linking distinct network disruptions to specific symptom profiles.
Strategy 3: Normative Modeling for Individualized Assessment
Normative modeling characterizes how each individual patient's brain structure or function deviates from a healthy population norm, accepting and quantifying heterogeneity.
- Protocol: Mapping Person-Specific GMV Deviations
- Build a Normative Model: Train a statistical model (e.g., using hierarchical Bayesian regression) on a large dataset of healthy controls to establish the expected range of a brain phenotype (e.g., gray matter volume - GMV) for a given age and sex [44].
- Calculate Individual Deviation Maps: For each patient, compute a z-score at each brain region, quantifying how much their GMV deviates from the normative prediction.
- Define Extreme Deviations: Identify regions with statistically extreme deviations (e.g., z > |2.6|) for each patient.
- Cohort Selection Criterion: Select patients based on the presence of extreme deviations within a pre-specified functional network of interest, rather than a shared anatomical lesion site. This ensures cohort cohesion at the network level despite regional heterogeneity [44].
Experimental Workflow and Protocol
The following integrated workflow provides a detailed protocol for a study designed to overcome lesion heterogeneity.
Detailed Protocol Steps
Step 1: Patient Identification and Characterization
- Inclusion Criteria: Select patients based on a well-defined behavioral syndrome (e.g., acquired antisocial behavior) confirmed via clinical interview or standardized tools like the SCID-II [43]. The key is the behavioral phenotype, not the lesion location.
- Document Symptoms: Code specific behaviors (e.g., deceitfulness, irritability/aggressivity) as present (1) or absent (0) for quantitative analysis [43].
Step 2: Lesion Data Processing
- Imaging Acquisition: Acquire high-resolution T1-weighted anatomical MRI scans for all patients.
- Lesion Tracing: Manually trace each patient's lesion onto a standardized brain template (e.g., MNI152) using software such as MRIcron, creating a binary mask for each subject [43] [42].
Step 3: Network Analysis Core
- Normative Data: Use a publicly available normative functional connectivity dataset (e.g., from the Human Connectome Project).
- Connectivity Calculation: For each patient's lesion mask, perform seed-based functional connectivity analysis against the normative dataset to generate a lesion network map [42].
- Group-Level Network Analysis: Test the voxel-wise convergence of the individual lesion network maps across the cohort. Compare this to a null distribution generated from control lesions (e.g., from stroke databases like ATLAS) to identify network connections specific to the clinical syndrome [43] [42]. A standard two-sample t-test can be used, with significance set at p < 0.05, FDR-corrected.
Step 4: Cohort Stratification and Validation
- Subgroup Identification: If network connectivity is heterogeneous, use clustering analysis on the lesion network maps or meta-analytic co-activation profiles to identify data-driven patient subgroups [43].
- Symptom Correlation: Validate the network-based stratification by testing for significant behavioral differences between the subgroups. This confirms that the identified networks are behaviorally relevant.
Quantitative Data Presentation
Table 1: Symptom Profile of a Sample Cohort with Acquired Antisocial Behavior (n=17)
| Symptom Domain (SCID-II) | Behaviors Included | Number of Patients (%) |
|---|---|---|
| Irritability/Aggressivity | Initiation of physical fights, assaults | 12 (70.6%) |
| Limited Prosocial Emotions | Lack of remorse, callousness, lack of empathy | 10 (58.8%) |
| Irresponsibility | Failure to sustain work, honor monetary obligations | 9 (52.9%) |
| Deceitfulness | Repeated lying, conning others | 5 (29.4%) |
Source: Adapted from Frontiers in Psychiatry, 2022 [43].
Table 2: Comparison of Traditional vs. Network-Based Lesion Mapping
| Feature | Traditional Lesion Overlap | Lesion Network Mapping |
|---|---|---|
| Primary Unit of Analysis | Anatomical lesion location | Functional network of the lesion |
| Handling of Heterogeneity | Fails with spatially diverse lesions | Leverages heterogeneity to find a common network |
| Required Data | Patient lesion masks | Patient lesion masks + normative connectome |
| Key Output | Map of overlapping damaged voxels | Map of a common dysfunctional network |
| Explanatory Power | Limited for network-level symptoms | High, explains symptoms from disconnected networks |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Lesion Network Studies
| Item / Resource | Function / Application | Examples / Specifications |
|---|---|---|
| Standardized Brain Atlas | Provides a common coordinate space for lesion localization and analysis. | MNI (Montreal Neurological Institute) space |
| Normative Connectome Dataset | Serves as a reference for calculating the normal functional connectivity of a lesion location. | Human Connectome Project (HCP) data; 150+ unrelated subjects [44] |
| Lesion Segmentation Tool | Used for manual or automated tracing of lesion boundaries onto a template. | MRIcron, ITK-SNAP |
| Functional Connectivity Toolbox | Software for performing seed-based correlation and other network analyses. | FSL, CONN, DPABI |
| Neuroimaging Meta-Analysis Database | Allows for functional characterization of lesion networks via co-activation patterns. | Neurosynth, BrainMap [43] |
| Control Lesion Dataset | Provides a null distribution to test the specificity of the identified lesion network. | ATLAS (Anatomical Tracings of Lesions After Stroke) dataset [43] |
Overcoming lesion heterogeneity is not merely a statistical challenge but requires a paradigm shift from a localizationist perspective to a network-based view of brain function. The strategies outlined—Lesion Network Mapping, Data-Driven Subgrouping, and Normative Modeling—provide a robust framework for selecting and characterizing patient cohorts that are cohesive at the level of brain networks. By adopting these methods, researchers can strengthen the causal inference of the lesion method, identify novel therapeutic targets for neuromodulation based on network hubs, and ultimately develop a more precise and mechanistically grounded understanding of the brain-behavior relationship.
The lesion method, a cornerstone of neuroscience, has been instrumental in correlating specific brain areas with behavior. By studying the functional deficits that follow localized brain damage, researchers have historically identified the roles of regions such as Broca's area in speech production and the hippocampus in memory formation [1]. However, the brain's response to injury extends far beyond the immediate site of damage. A focal lesion initiates dynamic network-wide changes through two key phenomena: diaschisis, the remote disruption of brain areas connected to the lesion site, and compensatory plasticity, the brain's adaptive rewiring to restore function [45] [46]. Understanding these network effects is crucial for developing targeted therapeutic strategies, as functional recovery depends not only on the damaged area but also on the reorganization of surviving neural circuits [45].
Core Concepts and Neurobiological Basis
Diaschisis: Remote Dysfunction in Neural Networks
Diaschisis, a concept introduced by von Monakow, originally described a rapid loss of excitability in brain regions distant from but connected to a focal lesion [45]. Modern research has expanded this concept beyond excitability changes to include disruptions in functional connectivity (FC)—the temporal correlation of neural activity between different brain areas [45]. In stroke patients, acute decreases in interhemispheric connectivity are robust biomarkers of impairment, particularly for higher-order functions like memory and language that rely on distributed networks [45]. These network-level disruptions coexist with local changes in excitatory-inhibitory (EI) balance, creating a complex cascade of effects that evolve during the recovery process [45].
Compensatory Plasticity: The Relearning Mechanism
Compensatory relearning refers to the process by which the brain reorganizes its undamaged circuits to compensate for lost function. This process shares mechanisms with classical motor learning and memory formation [46]. Key structures involved include:
- Periinfarct tissue: The region surrounding the ischemic core, which enters a growth-permissive state, promoting axonal sprouting and rewiring [46].
- Contralesional homotopic regions: Undamaged areas in the hemisphere opposite the lesion that undergo functional adaptation [46].
- Cortico-striato-thalamic loops: These circuits are progressively shaped during recovery, with participating neurons adapting their activity and synaptic strengths to facilitate functional compensation [46].
The cellular environment following stroke is characterized by waves of growth-inhibiting and growth-promoting factors, creating a window of opportunity for therapeutic intervention [46]. This plastic potential can be harnessed through rehabilitation to guide compensatory relearning.
Experimental Protocols for Investigating Network Effects
Protocol: Assessing Functional Connectivity Changes in Stroke Models
Objective: To quantify changes in functional connectivity and network properties following focal ischemic lesions in a rodent model.
Materials:
- Animal model: Adult Sprague-Dawley rats (n=10 minimum per group)
- Stereotaxic apparatus
- Physiological monitoring equipment (body temperature, blood pressure, blood gases)
- MRI-compatible anesthetic delivery system
- High-field MRI scanner (7T or higher) with capability for resting-state fMRI
Procedure:
- Pre-lesion baseline imaging:
- Anesthetize animal using isoflurane (1.5-2% in O₂)
- Acquire T2-weighted structural images and 10-minute resting-state fMRI sequences (TR=1000ms, TE=15ms)
- Maintain physiological parameters within normal range (body temperature at 37±0.5°C)
Focal ischemia induction:
- Position animal in stereotaxic frame
- Perform craniotomy at coordinates targeting the sensorimotor cortex (AP: +1mm, ML: -2.5mm from Bregma)
- Induce photothrombotic lesion using Rose Bengal injection (20mg/kg IV) and 15 minutes of green light illumination (560nm)
- Alternatively, use endothelin-1 injection (3μL of 400pmol/μL) for more gradual vessel constriction
Post-lesion longitudinal imaging:
- Repeat imaging protocol at 3 days, 1 week, 2 weeks, and 4 weeks post-lesion
- Maintain identical positioning and acquisition parameters
Data processing:
- Preprocess fMRI data using standard pipeline: motion correction, temporal filtering (0.01-0.1Hz), and global signal regression
- Define regions of interest (ROIs) based on standardized atlases
- Compute correlation matrices between all ROI pairs
- Calculate graph theory metrics: global efficiency, clustering coefficient, and modularity
Behavioral correlation:
- Perform motor function tests (cylinder test, beam walking) 24 hours before each imaging session
- Correlate connectivity changes with behavioral recovery metrics
Table 1: Key Functional Connectivity Metrics in Post-Stroke Recovery
| Metric | Description | Measurement Technique | Change in Acute Phase | Change in Chronic Phase |
|---|---|---|---|---|
| Interhemispheric Connectivity | Temporal correlation between homologous regions in opposite hemispheres | Resting-state fMRI | Decreased [45] | Normalizes with recovery [45] |
| Intrahemispheric Connectivity | Temporal correlation between regions within the same hemisphere | Resting-state fMRI | Increased in lesioned hemisphere [45] | Stabilizes or decreases as interhemispheric normalizes [45] |
| Global Efficiency | Measure of network integration; inverse of average path length | Graph theory analysis | Decreased | Increases toward pre-stroke levels |
| Modularity | Degree to which network is organized into separate modules | Graph theory analysis | Increased (more segregated) | Decreases toward pre-stroke levels |
Protocol: Evaluating Cellular Plasticity Mechanisms
Objective: To examine synaptic reorganization and cellular correlates of compensatory relearning in periinfarct cortex.
Materials:
- Thy1-GFP mice (for neuronal labeling)
- Confocal microscope
- Electrophysiology setup for in vivo recordings
- Miniscope for calcium imaging
- Golgi-Cox staining kit
- Western blot equipment
Procedure:
- Lesion induction and animal preparation:
- Induce focal motor cortex lesions using photothrombosis as described in Protocol 3.1
- Implant chronic cranial windows over periinfarct cortex for optical access
- Express GCaMP6f in layer V pyramidal neurons via AAV injection for calcium imaging
Longitudinal structural imaging:
- Image dendritic spines in periinfarct cortex using two-photon microscopy at 1, 3, 7, 14, and 28 days post-lesion
- Quantify spine density, morphology, and turnover rate
- Perform axonal tracing of corticostriatal projections
Functional calcium imaging:
- Record calcium transients in awake, behaving animals during motor task performance
- Analyze population coding and functional clustering of neurons
- Correlate neural activity patterns with behavioral performance
Electrophysiological recordings:
- Perform in vivo whole-cell recordings from periinfarct neurons
- Measure changes in EI balance through miniature excitatory and inhibitory postsynaptic current analysis
- Assess homeostatic plasticity through intrinsic excitability measures
Molecular analysis:
- Process tissue for Western blotting of plasticity-related proteins (BDNF, PSD-95, GAD67)
- Use Golgi-Cox staining to quantify dendritic arborization
Table 2: Cellular and Molecular Markers of Compensatory Plasticity
| Marker | Function | Assessment Method | Change Post-Lesion | Significance for Recovery |
|---|---|---|---|---|
| BDNF | Promotes synaptic plasticity and neuronal survival | Western blot, ELISA | Increased in periinfarct cortex [46] | Facilitates relearning; potential therapeutic target |
| PSD-95 | Scaffolding protein at excitatory synapses | Immunohistochemistry | Transient decrease, then recovery | Indicator of excitatory synapse reorganization |
| GAD67 | GABA synthesis enzyme for inhibitory transmission | Immunohistochemistry | Transient increase | Reflects EI balance restoration attempts |
| Dendritic Spine Density | Structural correlate of synaptic connections | Two-photon microscopy | Initial decrease followed by overshoot | Associated with circuit rewiring [46] |
| MAP2 | Dendritic structural protein | Immunohistochemistry | Increased arborization in surviving neurons | Substrate for new connection formation |
Data Presentation and Analysis Tools
Standardized Data Tables for Network Properties
Effective presentation of network neuroscience data requires clear organization to facilitate comparison across studies and experimental conditions. The following principles should guide table construction:
- Label all rows and columns clearly with units specified for numerical data [47]
- Maintain consistent formatting throughout the table to avoid confusion [47]
- Include sample sizes and statistical measures for proper interpretation
- Separate acute, subacute, and chronic phase data to illustrate temporal dynamics
Table 3: Temporal Evolution of Network Properties Post-Stroke
| Time Point | Interhemispheric FC (r-value) | Intrahemispheric FC (r-value) | Global Efficiency | Modularity | Motor Performance (% baseline) |
|---|---|---|---|---|---|
| Baseline | 0.72 ± 0.05 | 0.65 ± 0.04 | 0.41 ± 0.03 | 0.35 ± 0.02 | 100% |
| 3 days | 0.31 ± 0.08* | 0.81 ± 0.06* | 0.28 ± 0.04* | 0.52 ± 0.05* | 42% ± 8%* |
| 1 week | 0.45 ± 0.07* | 0.78 ± 0.05* | 0.32 ± 0.03* | 0.48 ± 0.04* | 58% ± 10%* |
| 2 weeks | 0.58 ± 0.06 | 0.72 ± 0.05 | 0.37 ± 0.03 | 0.42 ± 0.03 | 75% ± 9% |
| 4 weeks | 0.69 ± 0.05 | 0.67 ± 0.04 | 0.40 ± 0.03 | 0.37 ± 0.02 | 88% ± 7% |
Note: Values represent mean ± SD; * indicates significant difference from baseline (p<0.05)
For comprehensive data analysis and publication-ready tables, the R package gtsummary provides powerful functionality to summarize complex datasets and regression models [48]. This tool automatically detects variable types and calculates appropriate descriptive statistics, facilitating reproducible research reporting.
Computational Modeling Approaches
Computational modeling serves as a framework to bridge meso- and macro-scale processes of recovery. Large-scale models of the human cortex can simulate both EI homeostasis and network-level changes, providing testable predictions about recovery trajectories [45]. These models typically incorporate:
- Individual neuron dynamics based on Hodgkin-Huxley or integrate-and-fire models
- Synaptic plasticity rules (spike-timing-dependent plasticity, homeostatic scaling)
- Network architecture derived from connectome data
- Lesion effects simulated through node removal or connection weakening
Visualization of Signaling Pathways and Workflows
Diaschisis and Compensatory Plasticity Pathways
Experimental Workflow for Network Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Diaschisis and Plasticity Studies
| Reagent/Tool | Function | Example Applications | Key Considerations |
|---|---|---|---|
| AAV-GCaMP6f | Calcium indicator for neuronal activity imaging | In vivo calcium imaging of periinfarct cortex during behavior | Select appropriate serotype for target cells; consider expression timeline |
| Photosensitizing dyes (Rose Bengal) | Light-activated vascular occlusion | Precise photothrombotic lesion induction | Optimize dose and illumination duration for lesion size control |
| BDNF assays | Quantification of neurotrophic factor levels | Monitoring plasticity-related molecular changes | Choose appropriate sampling timepoints; consider pathway activation assays |
| NeuN/GFAP/Iba1 antibodies | Identification of neurons, astrocytes, microglia | Immunohistochemical analysis of cellular responses | Validate antibody specificity for species; optimize staining protocols |
| EEG/EMG systems | Electrophysiological monitoring | Functional connectivity assessment in rodent models | Ensure compatibility with MRI environment for simultaneous acquisition |
| NES software | Experimental data management with provenance tracking | Standardized collection of heterogeneous neuroscience data [49] | Customize data models for specific experimental designs |
| Chroma.js library | Color space manipulation and accessibility checking | Data visualization with WCAG compliance [50] [51] | Implement consistent, accessible color schemes across all figures |
| gtsummary R package | Creation of publication-ready summary tables [48] | Standardized reporting of experimental results | Customize output for specific journal requirements |
The investigation of diaschisis and compensatory plasticity requires a multidisciplinary approach that spans molecular analysis, cellular imaging, network-level assessment, and behavioral correlation. The protocols and tools presented here provide a framework for systematically studying how focal brain lesions disrupt distributed networks and how adaptive plasticity mechanisms promote recovery. By employing standardized data presentation methods and accessible visualization approaches, researchers can enhance the reproducibility and translational impact of their findings. Future directions in this field should focus on integrating multiscale data through computational modeling and developing interventions that specifically target network-level reorganization to improve functional outcomes after brain injury.
Application Notes: The Role of High-Resolution DTI in the Lesion Method
The lesion method, a cornerstone of behavioral neuroscience, traditionally correlates focal brain lesions with specific cognitive deficits to map brain-behavior relationships. Advanced neuroimaging techniques, particularly high-resolution structural MRI and Diffusion Tensor Imaging (DTI), have revolutionized this approach by enabling precise quantification of both macroscopic lesions and microscopic white matter damage that often escapes conventional imaging. These techniques provide a powerful framework for understanding how disconnection within neural networks leads to behavioral and cognitive impairment, moving beyond a purely localizationist view.
Table 1: Key DTI Metrics and Their Pathophysiological Correlates in White Matter Damage
| DTI Metric | Biological Interpretation | Association with White Matter Pathology | Correlation with Behavior & Cognition |
|---|---|---|---|
| Fractional Anisotropy (FA) | Directional coherence of water diffusion; indicator of white matter tract integrity. | Decreased in demyelination, axonal loss, and structural disorganization [52] [53]. | Correlates with processing speed, executive function, and overall clinical disease severity [52] [53]. |
| Mean Diffusivity (MD) | Magnitude of overall water diffusion; inversely related to tissue density. | Increased with vasogenic edema, inflammation, and neuronal loss [54]. | Elevated MD in normal-appearing white matter correlates with cognitive impairment [52]. |
| Axial Diffusivity (AD) | Magnitude of water diffusion parallel to the primary axon direction. | Proposed to reflect axonal integrity; often decreases with axonal damage [54]. | Changes are associated with alterations in network integration and cognitive function. |
| Radial Diffusivity (RD) | Magnitude of water diffusion perpendicular to the primary axon direction. | Proposed to reflect myelin integrity; typically increases with demyelination [54]. | Increased RD is linked to slower processing speed and functional disconnection. |
| Peak Width of Skeletonized Mean Diffusivity (PSMD) | Novel marker of white matter damage derived from the histogram of skeletonized MD maps. | A sensitive and automated measure of white matter damage from small vessel disease [55]. | Strongly correlates with cognitive impairment and is elevated in conditions like occipital lobe epilepsy [55]. |
The integration of these quantitative DTI metrics into the lesion method paradigm allows researchers to establish robust structure-function correlations. For instance, studies have demonstrated that the skeleton mean diffusivity, reflecting ultrastructural tract damage, shows a closer correlation with cognitive performance in patients with symptomatic carotid artery disease than traditional lesion volumes alone [56]. Furthermore, DTI reveals that microstructural damage often extends far beyond the borders of visible lesions into the normal-appearing white matter (NAWM), which itself independently contributes to cognitive decline [54] [52]. This is critical for precision medicine, as it provides a more complete picture of network disruption, explaining behavioral variances that cannot be accounted for by focal lesion analysis alone.
Experimental Protocols for White Matter Assessment
Protocol 1: Multi-Modality Image Registration for Punctate White Matter Damage (PWMD) Analysis
This protocol is designed for the precise analysis of neonatal punctate white matter damage by combining the high anatomical resolution of T1-weighted MRI with the microstructural information from DTI [57].
Workflow Overview: The core of this protocol involves two sequential computational processes after data acquisition: DTI Super-Resolution, which enhances the detail of the DTI data, followed by Multi-Modality Image Registration, which aligns the enhanced DTI with the T1-weighted MRI to enable combined analysis.
Detailed Methodology:
MRI Acquisition:
- Acquire high-resolution T1-weighted anatomical images.
- Acquire Diffusion Tensor Imaging (DTI) data using a single-shot echo-planar imaging (EPI) sequence. Typical parameters include: a
b-valueof 1000 s/mm², and at least 32 different diffusion gradient directions to reliably estimate the diffusion tensor [55].
Image Preprocessing:
DTI Super-Resolution:
- To match the resolution of T1-weighted images and facilitate accurate fiber tractography, perform DTI super-resolution.
- This is achieved using a three-times B-spline interpolation algorithm performed in Log-Euclidean space. This space is mathematically advantageous as it prevents the occurrence of non-physical negative eigenvalues in the interpolated diffusion tensors, ensuring results are biologically plausible [57].
Multi-Modality Image Registration:
- Co-register the super-resolved DTI data with the T1-weighted anatomical scan.
- Employ a symmetric diffeomorphic registration algorithm (e.g., using tools like ANTs or similar). This method ensures smooth, invertible, and topology-preserving transformations for highly accurate alignment.
- Use the inverse of the b0 image (the non-diffusion-weighted volume) from the DTI dataset as a reference for this registration step [57].
Integrated Lesion and Tractography Analysis:
- On the registered T1-weighted image, manually or automatically segment PWMD lesions, which appear as semi-oval, cluster, or linear high-signal areas.
- Reconstruct the white matter tracts using deterministic or probabilistic tractography algorithms applied to the registered DTI data.
- Finally, create a 3D model that combines the lesion masks with the fiber tractography results. This integrated model allows for the quantitative analysis of the degree to which the PWMD lesions affect critical fiber tracts, enabling predictions about functional impact [57].
Protocol 2: Quantifying Microstructural Damage in Normal-Appearing White Matter (NAWM)
This protocol uses T1rho and DTI to detect and characterize subtle, distance-dependent microstructural changes in the perilesional NAWM in Multiple Sclerosis, which appears normal on conventional MRI [54].
Workflow Overview: After identifying lesions, this method involves creating multiple concentric "shells" or layers expanding outward from the lesion boundary. Quantitative metrics from T1rho and DTI are then measured within these layers to profile how microstructural damage changes with distance from the visible lesion edge.
Detailed Methodology:
Subject Population and MRI Acquisition:
- Recruit patients (e.g., with Relapsing-Remitting Multiple Sclerosis, RRMS) and age-matched healthy controls.
- Acquire the following MRI sequences on a 3T scanner:
- 3D T1-weighted and 3D FLAIR for anatomical reference and lesion identification.
- DTI: Use a 3D EPI sequence with
b=1000 s/mm², 32 directions, and isotropic voxels (e.g., 2.0 mm³) [54]. - T1rho Imaging: Use a T1rho-prepared turbo spin echo (TSE) sequence with a 180° refocusing pulse to reduce B0 and B1 inhomogeneity effects. This sequence is sensitive to low-frequency interactions between protons and macromolecules, providing unique contrast related to the tissue's macromolecular environment [54].
Lesion Identification and Perilesional Layering:
- Identify all non-enhancing MS lesions on the FLAIR and T1-weighted images.
- For each lesion, delineate five consecutive, concentric perilesional layers (e.g., Layer 1 being closest to the lesion margin, Layer 5 being farthest) expanding into the surrounding NAWM. This creates a set of regions of interest (ROIs) for analysis [54].
Quantitative Parameter Extraction:
- DTI Processing: Fit the diffusion tensor model to calculate maps of Fractional Anisotropy (FA), Mean Diffusivity (MD), Axial Diffusivity (AD), and Radial Diffusivity (RD).
- T1rho Mapping: Fit the signal decay across different spin-lock times (TSL) to calculate the T1rho relaxation time map.
- Extract the mean values of FA, MD, AD, RD, and T1rho within each of the five perilesional layers and within the core of the lesion itself.
- In healthy controls, extract values from the corresponding normal white matter regions.
Statistical and Correlation Analysis:
- Compare T1rho and DTI metrics between patients' layers and control white matter.
- Analyze the gradient of change for each metric across the five layers, testing for a significant trend (e.g., using ANOVA).
- Perform correlation analysis between T1rho values and DTI metrics (MD, AD, RD) in the perilesional areas. The correlation coefficients typically show a pattern of progressively lower values as the distance from the lesion increases, indicating a normalization of tissue microstructure [54].
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 2: Key Research Reagents and Computational Tools for Advanced White Matter Imaging
| Item / Software | Function / Application | Specific Use-Case & Notes |
|---|---|---|
| 3.0 Tesla MRI Scanner | High-field platform for data acquisition. | Essential for obtaining high signal-to-noise ratio (SNR) images required for DTI and quantitative T1rho mapping [55] [54]. |
| 32-Channel Head Coil | RF signal reception. | Increases SNR and parallel imaging capabilities, improving spatial resolution and reducing scan time [55]. |
| FSL (FMRIB Software Library) | Comprehensive brain MRI data analysis suite. | Used for DTI preprocessing (eddy current correction), TBSS (skeletonization), and PSMD calculation [55]. A standard tool in neuroimaging. |
| Lesion Segmentation Toolbox (LST) | Automated segmentation of white matter lesions. | Used within SPM to segment WMH from FLAIR and T1 images, enabling volumetric and topographic analysis [58]. |
| Lesion-TOADS | Automated segmentation of brain structures and lesions. | Used within MIPAV for segmenting white matter hyperintense lesions and deep grey matter structures from 3D FLAIR and T1 images [59]. |
| ANTs (Advanced Normalization Tools) | Advanced image registration and normalization. | Used for implementing symmetric diffeomorphic registration for highly accurate multi-modality image alignment [57]. |
| T1rho MRI Pulse Sequence | Quantification of tissue macromolecular content. | Custom sequence for measuring T1rho relaxation, sensitive to early pathological changes in NAWM in MS [54]. |
| Gadoteric Acid (Dotarem) | Contrast agent for MRI. | Used to differentiate between active (enhancing) and chronic MS lesions in T1-weighted post-contrast scans [54]. |
The "Partial Injury Problem" refers to the central challenge in lesion-behavior research where focal brain damage rarely affects a single, isolated cognitive process. Instead, lesions to circumscribed areas typically produce multifaceted behavioral deficits because brain regions participate in multiple, often distributed, functional networks. Traditional univariate lesion-analysis methods struggle to disentangle these complex relationships, as they examine voxels in isolation and fail to account for the network-based organization of brain function. This limitation has driven the development of multivariate and machine learning (ML) solutions that can model the complex, high-dimensional relationships between lesion anatomy and behavioral outcomes.
Multivariate lesion-symptom mapping (MLSM) represents a paradigm shift from conventional approaches. By considering the entire lesion pattern simultaneously, these methods can identify brain-behavior relationships that would be missed by traditional voxel-based lesion-symptom mapping (VLSM). Evidence demonstrates that MLSM offers substantially higher sensitivity and specificity for detecting genuine lesion-behavior relationships compared to univariate methods [60]. When applied to synthetic datasets with known ground truth, support vector regression-based MLSM showed superior performance to VLSM, correctly identifying contributing regions while minimizing false positives [60]. This advancement is crucial for developing accurate biomarkers and targeted interventions for neurological conditions.
Methodological Foundations: From Traditional Lesion Studies to Multivariate Approaches
The Evolving Role of the Lesion Method
The lesion method constitutes one of the most established approaches in neuroscience for establishing causal brain-behavior relationships [30]. Whereas functional neuroimaging techniques identify brain regions associated with cognitive processes, lesion studies demonstrate their necessity [30]. This inferential strength—the ability to establish necessity rather than mere association—remains the cornerstone of the method's utility in contemporary neuroscience. Studies of patients with focal brain damage have provided fundamental insights into the neural basis of diverse functions including language, memory, cognitive control, and social behavior [30].
Modern lesion studies have evolved substantially from early case reports. Current best practices emphasize: premorbid functioning assessment (where possible), inclusion of appropriate control groups (including patients with brain damage sparing the region of interest), consideration of lesion etiology, comprehensive neuropsychological screening, and adequate statistical power [30]. The application of dissociation logic, particularly double dissociation, remains vital for establishing the functional specificity of brain regions [30] [61].
The Multivariate Advantage
Multivariate methods address core limitations of traditional univariate approaches through several key advantages:
- Network-Level Analysis: They model the brain as an interconnected network, capturing how damage to multiple regions collectively contributes to behavioral deficits [62] [63].
- Complex Pattern Detection: Machine learning algorithms can identify complex, nonlinear relationships between lesion location and behavioral outcomes that would be missed by linear, voxel-by-voxel methods [60].
- Enhanced Sensitivity: By considering the entire lesion pattern simultaneously, multivariate approaches reduce variance and increase power to detect true effects [60].
- Prediction Capability: These models can generate individualized predictions about functional outcomes based on lesion characteristics, enabling potential clinical applications [62] [64].
Table 1: Comparison of Lesion Analysis Methods
| Feature | Univariate VLSM | Multivariate/ML Approaches |
|---|---|---|
| Analytical Approach | Voxel-by-voxel analysis | Whole-lesion pattern analysis |
| Modeling Capability | Linear relationships | Linear and nonlinear relationships |
| Network Effects | Limited accounting | Explicit modeling of distributed networks |
| Sensitivity | Moderate | High [60] |
| Specificity | Moderate | High [60] |
| Primary Output | Statistical maps of association | Predictive models with accuracy metrics |
| Clinical Application | Group-level inference | Individualized prediction [62] |
Core Experimental Protocols
Multivariate Lesion-Behavior Mapping with Support Vector Regression
Support Vector Regression for Lesion-Symptom Mapping (SVR-LSM) implements a multivariate approach using a machine learning-based regression algorithm to model the relationship between lesion maps and continuous behavioral scores [60].
Materials and Reagents:
- Patient cohort with focal brain lesions (minimum n=40 recommended for adequate power)
- High-resolution structural MRI scans (T1-weighted)
- Behavioral assessment data (continuous scores preferred)
- Computing infrastructure with sufficient RAM and processing power
- Statistical software (e.g., MATLAB, R, Python with scikit-learn)
- Lesion tracing and normalization software
Procedure:
Lesion Delineation and Spatial Normalization
- Manually trace lesion boundaries on T1-weighted MRI scans using standardized protocols
- Normalize individual lesion maps to a standard stereotaxic space (e.g., MNI152)
- Create binary lesion masks for each participant, where 1 indicates damaged tissue and 0 indicates preserved tissue
Feature Matrix Construction
- Create a participant × voxel matrix where each entry represents lesion status (0/1) for that voxel and participant
- Apply inclusion criteria to retain only voxels damaged in a minimum number of patients (typically 3-5% of sample) to ensure statistical stability
Model Training and Validation
- Implement k-fold cross-validation (typically 5- or 10-fold) to partition data into training and test sets
- Train SVR models using radial basis function (RBF) kernel to capture nonlinear relationships
- Optimize hyperparameters (regularization parameter C, kernel parameters) via grid search
- Validate model performance on held-out test data using correlation between predicted and observed behavioral scores
Statistical Inference
- Use permutation testing (typically 1000-5000 iterations) to establish statistical significance
- Generate statistical maps thresholded at family-wise error corrected p < 0.05
- Control for potential confounds (e.g., total lesion volume, age, education) by including them as covariates
The following workflow diagram illustrates the SVR-LSM analytical pipeline:
Multivariate Lesion and Connectome-Based Prediction
This protocol adapts methods developed for predicting language outcomes after stroke to the broader partial injury problem, focusing on integrating both lesion location and structural connectome information [62] [65].
Materials and Reagents:
- Multicenter prospective cohort (recommended n=150+ for prediction models)
- Advanced MRI protocols: T1-weighted, diffusion-weighted imaging (DWI)
- Standardized behavioral assessment battery appropriate to domain of interest
- High-performance computing resources for connectome modeling
- Parallel processing capabilities for large-scale data analysis
Procedure:
Data Acquisition and Preprocessing
- Acquire high-resolution T1-weighted structural images and diffusion-weighted images
- Preprocess structural images: intensity normalization, skull stripping, tissue segmentation
- Process diffusion data: eddy current correction, tensor fitting, deterministic tractography
- Reconstruct individual structural connectomes using standardized parcellation schemes
Feature Extraction
- Lesion Features: Extract lesion load metrics for predefined regions of interest
- Connectome Features: Calculate graph-theory metrics (node degree, betweenness centrality, efficiency)
- Network Disconnection: Quantify disruption to specific white matter pathways
Machine Learning Model Development
- Allocate 70-75% of sample as training cohort, remaining as test cohort
- Train multiple ML models (Random Forests, Support Vector Machines, Neural Networks)
- Implement feature selection to identify most predictive variables
- Address class imbalance using over- or undersampling techniques as needed
Model Validation and Interpretation
- Evaluate model performance in independent test cohort using AUC, accuracy, precision-recall
- Calculate feature importance metrics to identify key predictors
- Perform clinical translation analysis to determine optimal decision thresholds
Table 2: Performance Metrics of Multivariate Lesion-Behavior Mapping Methods
| Method | Sensitivity | Specificity | Prediction Accuracy | Key Advantages |
|---|---|---|---|---|
| SVR-LSM | Significantly higher than VLSM [60] | Significantly higher than VLSM [60] | Continuous behavior score prediction [60] | Captures nonlinear relationships |
| Lesion+Connectome | Not reported | Not reported | Enables individual-level prediction [62] | Integrates structural network information |
| Random Forest | Not reported | Not reported | AUC up to 0.87 in sport injury prediction [66] | Handles high-dimensional data well |
| High-Dimensional Classifiers | Detects smaller treatment effects [65] | Maintains specificity despite complexity [65] | Identifies drug effects missed by conventional stats [65] | Models complex anatomical patterns |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Computational Tools
| Item | Function/Application | Specifications |
|---|---|---|
| Structural MRI Protocols | Lesion delineation and spatial normalization | High-resolution T1-weighted (1mm³ isotropic) |
| Diffusion MRI Protocols | Structural connectome reconstruction | DWI with multiple b-values (e.g., b=1000, 2000 s/mm²), 30+ directions |
| Standardized Stereotaxic Atlas | Spatial normalization and region identification | MNI152 or ICBM152 template space |
| Lesion Tracing Software | Manual lesion delineation | MRIcron, ITK-SNAP, or similar |
| Machine Learning Libraries | Implementation of multivariate algorithms | scikit-learn, TensorFlow, PyTorch |
| Graph Analysis Toolboxes | Connectome metric calculation | Brain Connectivity Toolbox, NetworkX |
| Behavioral Assessment Batteries | Domain-specific functional measurement | Standardized, validated tests for cognitive, motor, or language domains |
| High-Performance Computing | Processing large neuroimaging datasets | Multi-core processors, sufficient RAM (64GB+), parallel processing capability |
Implementation Workflow: From Data to Discovery
The following diagram illustrates the integrated workflow for addressing the partial injury problem using multivariate and machine learning approaches:
This workflow generates interpretable models that both predict functional outcomes and identify the specific lesion features and network disruptions most critical to the observed deficits. The validation phase typically employs cross-validation or independent test cohorts to ensure generalizability, while the interpretation phase focuses on feature importance analysis to advance theoretical understanding of brain-behavior relationships [62] [63] [60].
The application of these multivariate methods has demonstrated particular success in predicting specific functional domains. For instance, in the domain of general cognitive ability, multivariate lesion-behavior mapping has identified the left temporo-parietal junction and its associated white matter tracts (particularly the arcuate fasciculus) as critically necessary for domain-general cognition [63]. This neuroanatomical localization successfully predicted observed cognitive ability in an independent cohort (r = 0.42, p < 0.001), demonstrating the generalizability of these approaches [63].
Multivariate and machine learning solutions directly address the fundamental challenges of the partial injury problem by modeling the complex, network-based organization of brain function. These approaches have demonstrated superior sensitivity and specificity compared to traditional univariate methods, while enabling individualized prediction of functional outcomes based on lesion characteristics [62] [60]. The integration of lesion location data with structural connectome information represents a particularly promising direction for future research, potentially offering more complete models of how focal damage disrupts distributed brain networks to produce behavioral deficits. As these methods continue to develop and become more accessible, they hold significant promise for advancing both theoretical understanding of brain-behavior relationships and clinical care for individuals with neurological disorders.
The lesion method, a cornerstone of behavioral neuroscience, operates on a fundamental principle: by studying the behavioral changes that follow damage to specific brain areas, researchers can infer the function of those structures [21]. This method has historically provided invaluable insights into brain-behavior relationships, famously illustrated by cases like Phineas Gage and patients with Broca's or Wernicke's aphasia, where localized damage led to specific behavioral deficits [21]. However, traditional behavioral assessments used in conjunction with lesion methods, often conducted in controlled laboratory settings, face significant limitations in ecological validity—their ability to predict real-world functioning [67].
Emerging technologies now offer powerful complements to traditional methods. This article details protocols for Ecological Momentary Assessment (EMA) and Virtual Reality (VR) tasks, framing them within lesion research to enhance the ecological validity of brain-behavior correlations. By capturing data in real-time within naturalistic contexts, these methods can provide more nuanced and clinically relevant behavioral profiles corresponding to lesion locations, addressing a critical gap in traditional neuropsychological batteries [67].
Quantitative Comparison of Behavioral Assessment Paradigms
The following table summarizes the core characteristics, advantages, and limitations of traditional and modern behavioral assessment methods relevant to lesion-behavior correlation studies.
Table 1: Comparative Analysis of Behavioral Assessment Methods for Lesion Research
| Method | Core Data Type | Administration Context | Key Advantage for Lesion Studies | Primary Limitation |
|---|---|---|---|---|
| Traditional Lab Tasks [67] | Primarily Quantitative + Structured (e.g., reaction time, accuracy scores) [68] | Controlled laboratory environment | High experimental control; well-established neural correlates | Low ecological validity; may not capture real-world cognitive demands [67] |
| Lesion Method [21] | Qualitative (behavioral observation) & Quantitative (task performance) | Clinic or lab | Direct causal inference of brain area function [21] | Natural lesions are often not neatly localized; pre-morbid data is rare [21] |
| Ecological Momentary Assessment (EMA) [69] | Qualitative + Unstructured (e.g., free-text responses) & Quantitative (e.g., scale ratings) [68] | Real-world, natural environment | High ecological validity; captures real-time experiences and context [67] [69] | Participant burden; missing data; relies on self-report [67] |
| Virtual Reality (VR) [67] | Quantitative + Structured (performance metrics in simulated environments) | Simulated real-world environment | Balance of control and ecological validity; standardized yet realistic tasks [67] | Technological and psychometric limitations; underdeveloped theoretical frameworks [67] |
Experimental Protocols for Enhanced Behavioral Data Capture
Protocol 1: Ecological Momentary Assessment (EMA) for Real-World Cognitive Phenotyping
Objective: To capture real-time, real-world cognitive challenges and behavioral correlates associated with specific brain lesions, moving beyond laboratory-based tasks [67].
Background: EMA involves repeated, real-time sampling of participants' experiences, behaviors, and cognitive functions in their natural environments, minimizing recall bias and enhancing ecological validity [69]. When applied to patients with brain lesions, it can reveal how deficits in specific domains (e.g., executive function from frontal lobe damage) manifest in daily life.
Materials and Reagents: Table 2: Research Reagent Solutions for EMA and VR Protocols
| Item | Function/Application |
|---|---|
| Smartphone with EMA App (e.g., mEMA, Ethica) | Primary device for delivering prompts, collecting self-report data, and capturing some sensor data [69]. |
| Wearable Sensor (e.g., ActiGraph, Empatica E4) | Passively collects physiological (e.g., heart rate, EDA) and activity data, providing objective context for self-reports. |
| VR Headset & Software Platform (e.g., Oculus Rift, HTC Vive) | Presents immersive, ecologically valid scenarios for cognitive and behavioral assessment in a controlled manner [67]. |
| Cloud Database (NoSQL, e.g., MongoDB) | Stores and manages large volumes of unstructured and semi-structured EMA and sensor data efficiently [70]. |
Procedure:
- Sampling Design: Choose a sampling strategy based on the research question.
- Time-Based Sampling: Program the EMA app to signal participants at random intervals within pre-defined blocks throughout their waking hours (e.g., 5-8 times per day for 7-14 days). This captures a representative sample of daily experiences [69].
- Event-Based Sampling: Instruct participants to initiate a brief survey whenever a specific event occurs that is relevant to their lesion profile (e.g., a patient with amygdala lesions initiates a survey upon feeling a strong emotion) [69].
- Survey Design: Develop brief surveys (< 2 minutes to complete) delivered upon each prompt. Questions should be designed to assess cognitive domains linked to the lesion site.
- For frontal lobe lesions: Include items on current planning demands, decision-making conflicts, or impulse control.
- For parietal lobe lesions: Inquire about navigation difficulties or attentional lapses in the current environment.
- Use a mix of scaled responses (e.g., "How difficult is it to focus right now?" 1-Not at all to 7-Extremely) and occasional open-ended questions to capture qualitative context [69].
- Passive Data Collection: Enable smartphone and wearable sensors to concurrently collect passive data, such as GPS for location, accelerometer for physical activity, and audio levels for social environment (ensuring ethical compliance and participant consent) [67] [69].
- Data Integration and Analysis:
- Data Cleaning: Handle missing data appropriately (e.g., multilevel imputation).
- Multilevel Modeling: Use statistical techniques like multilevel modeling to account for the nested data structure (multiple observations within each participant). This allows researchers to separate within-person fluctuations from between-person differences, crucial for linking momentary behaviors to stable lesion characteristics [69].
Protocol 2: Virtual Reality (VR)-Based Ecological Task Battery
Objective: To administer standardized, yet ecologically valid, cognitive and behavioral tasks in immersive virtual environments to assess the functional impact of brain lesions.
Background: VR provides a platform for creating realistic simulations of daily activities (e.g., virtual supermarket shopping, kitchen task) that engage multiple cognitive domains simultaneously, offering a better proxy for real-world functioning than traditional pen-and-paper tests [67].
Procedure:
- Scenario Selection and Development: Design or select VR scenarios that tax cognitive domains typically affected by the lesion site under study. For example, a "Virtual Week" task for assessing executive functions and memory.
- Task Administration:
- Patients perform the VR tasks in a controlled setting, wearing a head-mounted display.
- The system automatically logs detailed, quantitative performance metrics, including:
- Completion time for the overall task and sub-tasks.
- Errors of commission and omission (e.g., purchasing incorrect items).
- Navigational efficiency (path length, time spent in irrelevant zones).
- Physiological measures (if integrated with wearables), such as heart rate variability during stressful virtual events.
- Data Analysis:
- Compare performance metrics of patients with specific lesion sites against a normative control database.
- Use pattern analysis to identify which aspects of the complex task are most impaired, providing a finer-grained behavioral profile than traditional tests.
Visualization of Research Workflows
The following diagrams, created using DOT language and adhering to the specified color palette and contrast rules, illustrate the core workflows for integrating these modern assessments with lesion research.
Lesion-Behavior Correlation Research Framework
Ecological Momentary Assessment (EMA) Workflow
Lesion Studies in the Modern Neuroscience Toolkit: Validation and Convergence with Other Methods
Understanding the relationship between brain structure and function is a fundamental goal of neuroscience, particularly for researchers developing interventions for neurological disorders. The lesion method, a cornerstone of clinical neuroscience, provides unique causal inference by demonstrating that damage to a specific brain area leads to a deficit in a particular function. In contrast, modern neuroimaging techniques like functional Magnetic Resonance Imaging (fMRI) and Electroencephalography (EEG) primarily reveal correlational relationships between brain activity and behavior. fMRI measures the blood oxygenation level-dependent (BOLD) signal, an indirect hemodynamic correlate of neural activity with high spatial resolution (1-3 mm) but poor temporal resolution (1-3 seconds). EEG directly records electrical activity from pyramidal neurons with millisecond temporal resolution but has limited spatial precision [71] [72]. This application note details protocols for integrating these methods to strengthen causal inferences in brain-behavior research, framed within the context of a thesis utilizing the lesion method.
Quantitative Data Comparison: Lesion Studies, fMRI, and EEG
Table 1: Comparing Causal and Correlational Methodologies in Human Brain Research
| Feature | Lesion Studies | fMRI | EEG |
|---|---|---|---|
| Primary Data Type | Causal | Correlational | Correlational |
| Spatial Resolution | High (precise lesion mapping) | High (1-3 mm) | Low |
| Temporal Resolution | Static (snapshot of deficit) | Low (1-3 s) | High (1-10 ms) |
| Key Measured Variable | Structural damage (via CT/MRI) and behavioral deficit | Blood Oxygenation Level-Dependent (BOLD) signal | Electrical potential (µV) on scalp |
| Inference Strength | Strong causal inference (if X is damaged and function Y is lost, X is necessary for Y) | Association between brain region activation and behavior/task | Association between neural oscillatory dynamics and behavior/task |
| Main Limitations | Natural experiments, network effects, plasticity | Indirect measure of neural activity, hemodynamic lag | Poor localization, source reconstruction challenges |
Table 2: Exemplary Quantitative Findings from Integrated Studies
| Study Focus | Lesion Location | fMRI Correlation Finding | EEG Correlation Finding | Integrated Interpretation |
|---|---|---|---|---|
| Motor Function after Stroke [73] | Supratentorial including M1 (SM1+) | Not reported in source | Negative Laterality Coefficient (LC) in active movement (stronger ipsilesional ERD) | M1 lesion causes pathological over-reliance on ipsilesional hemisphere, quantifiable via EEG LC. |
| Motor Function after Stroke [73] | Supratentorial excluding M1 (SM1-) | Not reported in source | Positive Laterality Coefficient (LC) in active movement (stronger contralesional ERD) | Subcortical lesions spare M1, allowing for more typical contralateral motor cortex activation. |
| Consciousness in Severe Stroke [72] | Large Hemispheric Infarction (LHI) | Not reported in source | Elevated δ-band functional connectivity between non-ipsilesional frontal-occipital networks | LHI disrupts global neuronal integration, generating a distinct network-level EEG signature. |
| Consciousness in Severe Stroke [72] | Brainstem Infarction (BSI) | Not reported in source | Elevated δ-band absolute/relative power, attenuated α/β power | BSI impairs ascending arousal systems, causing thalamocortical deafferiration and slow-wave dominance on EEG. |
| Resting-State Networks [74] | N/A (Healthy cohort) | Spatial maps of Resting-State Networks (RSNs) via ICA | Spatio-spectral patterns (SSPs) show weak spatial similarity to BOLD RSNs | fMRI and EEG capture complementary, non-redundant aspects of low-frequency neural dynamics. |
Experimental Protocols
Protocol 1: Investigating Lesion Location-Dependent EEG Patterns in Chronic Stroke
Application: This protocol is designed to systematically evaluate how lesion location alters electrophysiological responses during motor tasks, providing a causal framework for interpreting EEG correlations [73].
Workflow Diagram: Lesion-EEG Study Protocol
Detailed Methodology:
- Participant Selection & Grouping:
- Recruit patients with a single, chronic stroke (≥3 months post-stroke) presenting unilateral motor deficits.
- Using structural MRI (T1-weighted, FLAIR sequences), a radiologist categorizes patients into three groups:
- SM1+: Supratentorial lesions involving the primary motor cortex (M1).
- SM1-: Supratentorial lesions not involving M1 (e.g., subcortical only).
- INF: Infratentorial lesions (e.g., brainstem, cerebellum).
- Include an age- and sex-matched healthy control (HC) group.
- Exclusion criteria: multiple strokes, severe cognitive impairment, orthopedic limitations, or history of epilepsy.
EEG Data Acquisition:
- Equipment: High-density EEG system (e.g., 28-channel cap).
- Settings: Sampling rate ≥256 Hz, impedance kept below 10 kΩ.
- Paradigm: Participants perform multiple blocks of three task types with their affected hand (or dominant hand for HCs):
- Active Movement: Self-paced supination or grasping.
- Passive Movement: The same movement is guided by an experimenter.
- Motor Imagery (MI): Kinaesthetically imagining the movement without physical execution.
- Record continuous EEG with event markers synchronized to task onset.
EEG Data Preprocessing (using EEGLAB/Matlab):
- Import data and apply accurate electrode co-registration.
- Re-reference to average reference.
- Apply a bandpass filter (e.g., 0.1-30 Hz) and notch filter (50/60 Hz).
- Manually inspect and remove bad channels and segments with large artifacts.
- Perform Independent Component Analysis (ICA) to identify and remove artifacts from eye movements, muscle activity, and heartbeats.
- Segment data into epochs (e.g., -2 s to +4 s around movement onset).
Quantitative EEG Analysis:
- Event-Related Desynchronization (ERD): Calculate the percentage of power decrease in the beta band (16-24 Hz) during the task compared to a baseline reference period (-2 to 0 s before task cue). Formula:
ERD% = (P_baseline - P_task) / P_baseline * 100. - Laterality Coefficient (LC): Quantify the asymmetry of ERD between the contralateral and ipsilateral motor cortices (e.g., C3 vs. C4 for right-hand movement). Formula:
LC = (ERD_ipsi - ERD_contra) / (ERD_ipsi + ERD_contra). A positive LC indicates greater contralateral ERD (typical pattern), while a negative LC indicates greater ipsilateral ERD (atypical, often post-stroke pattern). - Generate topographical maps of ERD power for group comparisons.
- Event-Related Desynchronization (ERD): Calculate the percentage of power decrease in the beta band (16-24 Hz) during the task compared to a baseline reference period (-2 to 0 s before task cue). Formula:
Protocol 2: Concurrent EEG-fMRI for Mapping Spatio-Temporal Brain Dynamics
Application: This protocol outlines the procedure for simultaneous EEG-fMRI data collection to correlate the high-temporal resolution of EEG with the high-spatial resolution of fMRI, probing the neural origins of the hemodynamic signal [74] [71].
Workflow Diagram: Simultaneous EEG-fMRI Fusion Protocol
Detailed Methodology:
- Simultaneous Data Acquisition:
- EEG inside MRI: Use an MR-compatible high-density EEG system (e.g., 64+ channels) with a dedicated amplifier and a sync unit to correct for the MRI clock drift. Critical steps include:
- Meticulous preparation to minimize impedance and prevent movement.
- Use a carbon fiber or similar non-metallic cap.
- fMRI Parameters: Acquire BOLD data using an echo-planar imaging (EPI) sequence. Concurrently acquire a high-resolution T1-weighted anatomical scan for co-registration and localization. Standard parameters: TR=2000 ms, TE=30 ms, voxel size=3x3x3 mm³.
- Paradigm: Can be resting-state (eyes open/closed fixating) or task-based (e.g., block or event-related motor/cognitive tasks).
- EEG inside MRI: Use an MR-compatible high-density EEG system (e.g., 64+ channels) with a dedicated amplifier and a sync unit to correct for the MRI clock drift. Critical steps include:
EEG Data Preprocessing (Artifact Correction):
- Gradient Artifact Removal: Use average artifact subtraction (AAS) methods, which template the artifact based on the MR volume timing (TR) and subtract it from the EEG signal.
- Ballistocardiogram (BCG) Artifact Removal: Use AAS or ICA-based methods to remove the pulse-related artifact. This often requires recording a pulse oximeter or ECG for optimal correction.
- Proceed with standard preprocessing (filtering, bad channel removal, ICA for ocular/muscle artifacts) after MR-artifact correction.
fMRI Data Preprocessing:
- Perform standard preprocessing pipelines (e.g., SPM, FSL):
- Slice-time correction.
- Realignment (motion correction).
- Co-registration of functional and structural images.
- Normalization to a standard space (e.g., MNI).
- Spatial smoothing.
- Perform standard preprocessing pipelines (e.g., SPM, FSL):
Multimodal Feature Extraction & Fusion:
- EEG Feature Extraction: Calculate the time-varying power in classical frequency bands (delta: 0.5-4 Hz, theta: 4-8 Hz, alpha: 8-13 Hz, beta: 13-30 Hz). For advanced analysis, perform source localization of band-limited power or derive Spatio-Spectral Patterns (SSPs) using decomposition techniques like ICA on a concatenated spatial and spectral domain [74].
- fMRI Feature Extraction: Extract resting-state networks (RSNs) using Group ICA. For dynamic analysis, employ sliding-window spatially-constrained ICA (scICA) to estimate time-resolved spatial maps and compute their temporal evolution and network "volume" (number of active voxels) [71].
- Fusion Analysis:
- EEG-informed fMRI (GLM): Use the convolved time-series of EEG band power (e.g., alpha) as a regressor in a General Linear Model to identify brain regions where the BOLD signal correlates with the electrophysiological rhythm.
- Temporal Correlation: Correlate the time-varying volume of fMRI networks with the time-varying power of EEG bands to establish space-frequency links [71].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Equipment for Lesion, fMRI, and EEG Research
| Item Name | Specification / Example | Primary Function in Research Context |
|---|---|---|
| MR-Compatible EEG System | Brain Products MR+, EGI Geodesic system | Enables safe and artifact-manageable recording of EEG data inside the MRI scanner for concurrent data acquisition. |
| EEG Cap | 64-channel Ag/AgCl electrode cap with pre-configured layout (10-10 system) | Standardized placement of electrodes on the scalp for consistent electrical signal recording across subjects. |
| fMRI Scanner | 3T Siemens Prisma, 3T GE Discovery, or similar | Generates high-resolution BOLD and structural images for correlational mapping and precise lesion localization. |
| SOLAR1848 EEG Device | 18-channel quantitative digital EEG device [72] | Dedicated system for clinical and research QEEG, including continuous bedside monitoring in neurocritical care. |
| Analysis Software: EEGLAB | Open-source MATLAB toolbox [72] | Provides a comprehensive environment for EEG data preprocessing, ICA, time-frequency analysis, and visualization. |
| Analysis Software: GIFT | Group ICA of fMRI Toolbox [71] | Specialized software for performing Independent Component Analysis (ICA) on fMRI data to extract resting-state networks. |
| Analysis Software: SPM / FSL | Statistical Parametric Mapping; FMRIB Software Library | Standard packages for fMRI (and structural MRI) preprocessing, statistical analysis, and voxel-based lesion-symptom mapping. |
| Neuropsychological Batteries | Fugl-Meyer Assessment (FMA), NIH Stroke Scale (NIHSS) [72] [73] | Standardized clinical tools to quantitatively assess behavioral and motor deficits for correlation with lesion location and neuroimaging metrics. |
Logical Framework for Causal Inference from Multimodal Data
Diagram: From Correlation to Causal Inference
Understanding the causal relationship between brain areas and behavior is a fundamental goal of neuroscience. The lesion method, a cornerstone of neuropsychology, provides powerful insights by examining behavioral deficits following naturally occurring brain damage; it answers the question of whether a brain region is necessary for a cognitive function [75]. However, to build a comprehensive and causally grounded model of brain function, lesion studies should be integrated with techniques that can probe and manipulate neural circuits with high precision. The integration of lesion-deficit mapping, Transcranial Magnetic Stimulation (TMS), and optogenetics creates a powerful synergistic framework for triangulating causal brain-behavior relationships across species, scales, and temporal domains.
This integration leverages the unique strengths of each method: the necessity established by human lesion studies, the reversibility and temporal control of TMS, and the cell-type-specific causal manipulation afforded by optogenetics in animal models. This document provides application notes and detailed protocols for designing experiments that synergistically combine these approaches, framed within the context of a broader thesis on the lesion method.
Theoretical Foundation: Complementary Strengths and Weaknesses
The value of integration stems from the complementary strengths and weaknesses of each technique. The table below provides a comparative overview.
Table 1: Comparative Overview of Lesion, TMS, and Optogenetics Methods
| Feature | Lesion-Deficit Mapping | Transcranial Magnetic Stimulation (TMS) | Optogenetics |
|---|---|---|---|
| Causal Inference | Establishes necessity (in humans) | Establishes necessity (reversible interference) | Establishes necessity & sufficiency |
| Spatial Resolution | Voxel-wise (mm) | ~1 cm² | Cell-type-specific (µm) |
| Temporal Resolution | Chronic (static deficit) | Excellent (ms to minutes) | Excellent (ms) |
| Invasiveness | Natural lesions (non-invasive imaging) | Non-invasive | Highly invasive (viral expression, implants) |
| Species | Humans (primary) | Humans & non-human primates | Rodents & non-human primates (primarily) |
| Key Application | Identify necessary brain networks | Test necessity & induce plasticity in humans | Circuit mapping & causal mechanism |
| Primary Limitation | Lesion location is not controlled | Limited depth penetration & spatial resolution | Invasiveness limits human translation |
The synergy is clear: a network identified as critically necessary for a behavior (e.g., attention) via voxel-based lesion-symptom mapping (VLSM) in human stroke patients [76] can be targeted for reversible disruption using TMS in healthy volunteers or patients to confirm its necessity and temporal dynamics [77]. Subsequently, the homologous circuit in an animal model can be deconstructed using optogenetics to identify the specific cell types and causal activity patterns underlying the behavior [78] [79]. This cross-species, cross-method triangulation provides a robust foundation for identifying targets for therapeutic intervention.
Integrated Experimental Protocols
This section outlines detailed protocols for experiments that integrate these three methodologies, using spatial attention and neglect as a exemplar cognitive domain.
Protocol 1: From Human Lesion Networks to Circuit Validation with TMS
Aim: To validate the functional role of a brain network identified through lesion-behavior mapping by targeting its key nodes with TMS.
Background: Previous lesion studies have identified a right-hemisphere network for spatial attention, including temporal cortex regions, the inferior parietal lobule, and white matter tracts like the superior longitudinal fasciculus [76]. This protocol tests the causal necessity of these nodes.
Materials & Reagents:
- Participants: Healthy right-handed adults; patients with spatial neglect (for clinical correlation).
- Neuroimaging: 3T MRI scanner with structural (T1-weighted) and resting-state functional MRI (fMRI) sequences.
- Neuronavigation System: For co-registering TMS with individual anatomy.
- TMS Apparatus: TMS stimulator with a figure-of-eight coil.
- Behavioral Task: Computerized visuospatial attention task (e.g., landmark task, cancellation task).
Procedure:
- Lesion Network Identification (Retrospective):
- Acquire structural MRI and behavioral data (e.g., from cancellation tasks) from a cohort of patients with right-hemisphere stroke [76].
- Create a binary lesion mask for each patient.
- Perform Voxel-based Lesion-Symptom Mapping (VLSM) or multivariate Support Vector Regression Lesion-Symptom Mapping (SVR-LSM) to identify voxels where damage predicts severity of spatial neglect [76]. This defines the "critical network."
- Target Definition for TMS:
- From the VLSM/SVR-LSM results, select the peak voxel or cluster in the cortex (e.g., in the right temporo-parietal junction) as the primary TMS target.
- As a control target, select a site not implicated by the lesion map (e.g., the vertex).
- Subject-Specific Neuronavigation:
- Acquire a high-resolution T1-weighted MRI for each healthy participant.
- Coregister the group-level TMS target from the lesion map to each participant's native MRI space using nonlinear registration.
- TMS Interference and Behavioral Assessment:
- Employ a within-subject, cross-over design where each participant receives TMS to the active target and the control site in separate sessions.
- Apply continuous Theta-Burst Stimulation (cTBS), an inhibitory TMS protocol, to the target site for 40 seconds (600 pulses) [77].
- Immediately following cTBS, administer the computerized visuospatial attention task.
- Primary Outcome: Compare task performance (e.g., reaction time, spatial bias) between active and control TMS conditions. A significant decrement after active TMS confirms the causal necessity of the lesion-derived target.
Table 2: Key Research Reagent Solutions for Integrated Protocols
| Item | Function/Description | Example Specifics |
|---|---|---|
| Viral Vector (AAV) | Delivers genes for light-sensitive proteins (opsins) to target neurons [78]. | AAV5-CaMKIIa-ChR2-eYFP (for excitatory neurons). |
| Optogenetic Opsins | Actuators for controlling neural activity with light [78]. | Channelrhodopsin-2 (ChR2) for activation; Halorhodopsin (NpHR) or Jaws for inhibition. |
| Optical Fiber Implant | Guides light from the laser source to the target brain region in vivo [79]. | 200 µm core diameter, NA 0.37, ceramic ferrule. |
| Laser System | Provides the specific wavelength of light for opsin activation/inhibition [80]. | 473 nm blue laser for ChR2; 589 nm yellow laser for NpHR. |
| TMS Neuronavigation | Tracks head and TMS coil position in real-time to ensure precise stimulation of MRI-derived targets [77]. | Infrared camera system with subject-specific MRI overlay. |
| cTBS TMS Protocol | A patterned, inhibitory TMS protocol to transiently disrupt cortical node activity [77]. | 3-pulse 50 Hz bursts repeated at 5 Hz for 40s (600 pulses). |
Protocol 2: From TMS Targets to Cell-Type-Specific Circuit Dissection with Optogenetics
Aim: To dissect the cell-type-specific components and causal activity patterns of a network node validated by TMS, using a rodent model of visual attention.
Background: The right temporo-parietal junction homolog in the rodent (e.g., posterior parietal cortex, PPC) can be investigated using optogenetics to pinpoint the microcircuitry involved.
Materials & Reagents:
- Subjects: Transgenic mice allowing cell-type-specific targeting (e.g., CaMKIIa-Cre for excitatory neurons).
- Viral Vectors: Adeno-associated viruses (AAVs) encoding light-sensitive opsins (e.g., AAV5-CaMKIIa-ChR2-eYFP for excitation, AAV5-CaMKIIa-NpHR-eYFP for inhibition) [78].
- Stereotaxic Surgery Equipment: For precise viral injection and optical fiber implantation.
- Laser System & Optical Fibers: For light delivery.
- Behavioral Apparatus: Operant chamber with bilateral light stimuli for a choice reaction time task.
Procedure:
- Stereotaxic Surgery:
- Anesthetize the mouse and secure it in a stereotaxic frame.
- Inject the opsin-encoding AAV into the right PPC using coordinates from a mouse brain atlas.
- Implant an optical fiber cannula directly above the injection site.
- Allow 3-4 weeks for robust opsin expression.
- Behavioral Training and Optogenetic Manipulation:
- Train mice on a bilateral visual attention task where they must report a brief light stimulus presented randomly on the left or right.
- During testing sessions, interleave trials with optogenetic stimulation.
- For excitation: Deliver a 473 nm blue light pulse (e.g., 10 ms, 20 Hz) simultaneously with the visual stimulus on the contralateral side.
- For inhibition: Deliver a 589 nm yellow light continuously for 2 seconds prior to and during the stimulus presentation.
- Compare performance (accuracy, reaction time) on stimulation trials vs. no-stimulation trials.
- Outcome and Integration:
- Hypothesis 1: Excitation of PPC neurons during a contralateral stimulus will enhance detection accuracy and speed.
- Hypothesis 2: Inhibition of PPC neurons will induce a contralateral deficit, mimicking the spatial neglect phenotype observed in human patients with PPC lesions and TMS disruption.
- This result provides a direct, cell-type-specific causal link between the activity of a specific neuronal population in a defined region and a behaviorally relevant cognitive process, bridging the gap between the human lesion and TMS findings.
Data Integration and Visualization Workflows
The power of this integrated approach lies in the logical flow from observation to causal testing and mechanistic dissection. The following workflow diagrams illustrate this pipeline.
Detailed Optogenetics Experimental Cycle
The protocol for circuit dissection with optogenetics follows a precise cycle of preparation, intervention, and analysis, as detailed below.
The integration of lesion data, TMS, and optogenetics represents a powerful, multi-level strategy for moving from correlational observations to causal explanations in cognitive neuroscience. The protocols outlined here provide a concrete roadmap for researchers to implement this integrative approach. By starting with the clinical reality of lesion deficits, validating network nodes with non-invasive brain stimulation in humans, and finally deconstructing circuit mechanisms with cell-type-specific precision in animal models, this framework significantly accelerates the discovery of neural mechanisms underlying behavior and the development of targeted interventions for neurological and psychiatric disorders. This synergistic toolkit is indispensable for the modern neuroscientist and drug developer aiming to bridge the gap between brain networks and complex behavior.
The quest to correlate specific brain areas with complex cognitive behaviors represents a cornerstone of modern neuroscience. The lesion method, one of the oldest techniques in neuropsychology, has been powerfully augmented by modern neuroimaging and analytical tools. This case study details the application of Voxel-Based Lesion-Symptom Mapping (VLSM) and functional Magnetic Resonance Imaging (fMRI) to validate the neural networks essential for visual scene memory. Visual scene memory—the ability to encode, maintain, and recall complex visual environments—is a critical cognitive function whose impairment has significant consequences in various neurological disorders. Understanding its neural underpinnings is therefore a primary target for both basic cognitive research and applied drug development [81]. This document provides a detailed protocol for researchers aiming to replicate and extend this line of investigation, framing it within the broader context of the lesion method for correlating brain structure and function.
Experimental Findings and Quantitative Data Synthesis
The integration of findings from lesion studies and functional neuroimaging provides a convergent, multi-method validation of the brain networks supporting visual scene memory. The quantitative data from a pivotal VLSM study and a supporting fMRI meta-analysis are summarized below.
Table 1: Quantitative Findings from a VLSM Study on Visual Scene Memory (n=93 Stroke Patients)
| Measure | Right Hemisphere (RHD) Network | Left Hemisphere (LHD) Network | Behavioral Performance Hierarchy |
|---|---|---|---|
| Primary Brain Regions | Middle and Superior Temporal gyri, Inferior Parietal regions [81] | Temporo-occipital regions, Medial Temporal Lobe (MTL) [81] | Not Applicable |
| Lesion Effect Specificity | High: Regions were specifically implicated in memory for identity, action, or location [81] | Low: Regions were mostly implicated in a non-specific manner [81] | Not Applicable |
| Memory Performance | Significantly impaired vs. healthy controls [81] | Not Reported | Identity (Highest) > Location (Intermediate) > Action (Lowest) [81] |
Table 2: Neural Correlates of Visual Working Memory from fMRI Meta-Analysis
| Cognitive Process | Associated Brain Regions | Proposed Function |
|---|---|---|
| Delay-Period Activity | Widespread Frontoparietal Network, Right Inferior Temporal Cortex [82] | Temporary maintenance and manipulation of visual information [82] |
| Memory Discriminability | Right Prefrontal Cortex, Bilateral Parietal cortex, Late visual areas (e.g., precuneus, cuneus) [83] | Control of memory interference at retrieval [83] |
| Stimulus Salience | Bilateral Medial Temporal gyrus (including hippocampus), Bilateral Prefrontal Cortex (BA 10) [83] | Representation of perceptual salience of items in memory [83] |
Detailed Experimental Protocols
Protocol 1: Voxel-Based Lesion-Symptom Mapping (VLSM) for Visual Scene Memory
This protocol outlines the procedure for conducting a VLSM study to identify brain lesions critical for visual scene memory deficits [81].
1. Participant Recruitment & Screening:
- Cohort: Recruit patients in the sub-acute phase following a first-event stroke (target n > 90). Include patients with both right-hemisphere damage (RHD) and left-hemisphere damage (LHD) [81].
- Control Group: Recruit a demographically matched healthy control group for behavioral comparison.
- Inclusion/Exclusion: Establish clear criteria, including the presence of a focal, radiologically confirmed stroke and the absence of other neurological or psychiatric conditions.
2. Behavioral Assessment:
- Task: Administer the Wechsler Memory Scale (WMS-III) Family Pictures subtest. This task requires participants to view a complex scene and later recall the identity of characters, the location of characters, and the action each character was performing [81].
- Scoring: Score performance for the immediate and delayed recall conditions separately. Generate composite scores as well as separate scores for each scene element: identity, location, and action [81].
3. Neuroimaging Data Acquisition & Lesion Mapping:
- Acquisition: Obtain high-resolution T1-weighted anatomical brain scans for all patients.
- Lesion Tracing: Manually trace the boundaries of each patient's brain lesion onto their anatomical scan using software such as MRIcron. This should be performed by a trained researcher blinded to the behavioral data.
- Spatial Normalization: Normalize all individual brain images with traced lesions into a standard stereotaxic space (e.g., MNI space) to enable voxel-wise group comparisons.
4. Voxel-Based Lesion-Symptom Mapping Analysis:
- Statistical Model: Conduct a mass-univariate analysis at each voxel in the brain. For each voxel, use a non-parametric test (e.g., Brunner-Munzel test) to compare behavioral scores between the group of patients with a lesion at that voxel and the group without a lesion there [81] [84].
- Multiple Comparisons Correction: Apply a False Discovery Rate (FDR) correction to the resulting statistical maps to control for the family-wise error rate inherent in mass-univariate testing [81].
- Conjunction Analysis: Perform a conjunction analysis to identify voxel clusters specifically associated with deficits in memory for identity, location, or action, revealing dissociable neural substrates [81].
Protocol 2: fMRI Investigation of Visual Working Memory Delay Activity
This protocol describes an fMRI experiment to investigate brain activity during the maintenance phase of visual working memory, with a focus on abstract memory representations [85].
1. Participant & Task Design:
- Participants: Healthy adult volunteers with normal or corrected-to-normal vision.
- Stimuli: Use oriented sinusoidal gratings modulated by radial or angular polar gratings. These modulators create orthogonal aperture biases for identical orientations, allowing for the dissociation of sensory-like versus abstract memory representations [85].
- Paradigm: Employ a delayed orientation matching task.
- Encoding Phase (2-3s): Present a modulated grating.
- Delay Phase (8-12s): Present a blank screen during which the participant must maintain the grating's orientation in memory.
- Probe Phase (2-3s): Present a test grating, and the participant indicates whether it matches the remembered orientation.
2. fMRI Data Acquisition:
- Scanning Parameters: Acquire T2*-weighted BOLD images with a sequence optimized for capturing signals from visual and parietal cortices (e.g., TR=2s, voxel size ~3mm³). Also, acquire a high-resolution T1-weighted anatomical scan for co-registration.
- Retinotopic Mapping: Conduct separate functional localizer scans to define visual field maps (V1, V2, V3, etc.) in each participant [85].
3. fMRI Preprocessing & Analysis:
- Preprocessing: Process BOLD data using standard pipelines (e.g., SPM, FSL, AFNI). Steps include slice-time correction, motion realignment, co-registration to the anatomical scan, spatial normalization, and smoothing.
- General Linear Model (GLM): Model the BOLD time series with separate regressors for the encoding, delay, and probe phases of the task.
- Multivariate Pattern Analysis (MVPA):
- Training: Train a pattern classifier (e.g., a linear support vector machine) to decode the remembered orientation from the fMRI activity patterns during the late delay period, using data from trials with one type of modulator (e.g., radial).
- Cross-decoding Test: Apply the trained classifier to data from trials with the other modulator (e.g., angular). Successful cross-decoding indicates that the memory representation is an abstraction, invariant to the low-level perceptual features of the stimulus [85].
- Representation Visualization: Use models of visual field map properties (e.g., a V1 encoding model) to visualize the spatial patterns of activity associated with remembering an orientation, which often recapitulate a simple line-like abstraction of the original stimulus [85].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Lesion-Behavior and fMRI Research
| Item | Function/Description | Example/Note |
|---|---|---|
| Wechsler Memory Scale (WMS-III) | Standardized neuropsychological assessment to measure multiple facets of memory, including visual scene memory via the Family Pictures subtest [81]. | Provides validated and normed scores for immediate and delayed recall of character identity, location, and action. |
| Voxel-Based Lesion-Symptom Mapping (VLSM) Software | A statistical tool for correlating the location of brain lesions with behavioral deficits on a voxel-by-voxel basis. | Software like VLSM or NiiStat implements non-parametric tests and corrects for multiple comparisons [81] [84]. |
| fMRI-Compatible Stimulus Presentation System | Software and hardware for precise delivery of visual stimuli and collection of behavioral responses inside the MRI scanner. | Systems like Psychtoolbox, E-Prime, or Presentation ensure timing accuracy synchronized with the scanner's pulse. |
| Multivariate Pattern Analysis (MVPA) Toolbox | A software package for analyzing patterns of brain activity, used for decoding cognitive states from fMRI data. | Toolboxes such as PyMVPA, The Decoding Toolbox (TDT), or CoSMoMVPA are commonly used for cross-classification analyses [85]. |
| Visual Stimuli with Orthogonal Aperture Biases | Specially designed grating stimuli (radially vs. angularly modulated) to dissociate sensory processing from abstract memory representation. | Critical for experiments testing the format of working memory representations, as described in [85]. |
Signaling Pathways and Experimental Workflows
The following diagrams illustrate the core logical and experimental workflows described in this case study.
Diagram 1: This workflow outlines the key steps in a Voxel-Based Lesion-Symptom Mapping study, from patient recruitment and behavioral testing to the final statistical analysis that produces maps linking specific brain areas to memory function [81].
Diagram 2: This diagram illustrates the logical flow of an fMRI experiment designed to test whether visual working memory representations are abstractions of sensory input. The critical test is whether a memory classifier trained on one stimulus type can generalize to another, which would indicate the memory format is abstract [85].
Diagram 3: This diagram summarizes the key brain regions that constitute the network supporting visual scene memory, as identified by both lesion [81] and fMRI [82] studies. The Core Recollection Network is a distributed system that integrates information from ventral and dorsal visual streams, medial temporal lobe memory structures, and frontal and parietal control regions.
Application Notes
Lesion methods have been foundational in neuroscience, enabling researchers to correlate specific brain areas with behavior by observing deficits that arise from damage [1]. In modern drug development, this principle is leveraged to validate novel therapeutic targets for neurological disorders. By creating precise, localized brain lesions in animal models, scientists can simulate human neurological conditions and systematically test the efficacy of pharmacological interventions designed to restore lost function or slow disease progression [21].
The convergence of the traditional lesion method with cutting-edge drug development strategies is creating a powerful synergy [86]. For instance, the high failure rates of single-target therapies in complex diseases like Alzheimer's and Parkinson's have underscored the need for robust, physiologically relevant validation models [86] [87]. Lesion models provide this by establishing a direct, causal link between a neural system and a behavioral output, thereby de-risking the subsequent drug development pipeline. The following table summarizes key neurochemical systems and the drug development insights gained from their associated lesion models.
Table 1: Key Neurochemical Systems and Associated Lesion Models in Drug Development
| Neurochemical System | Brain Area/Lesion Model | Behavioral/Cognitive Deficit | Drug Development Insight & Application |
|---|---|---|---|
| Cholinergic System | Basal Forebrain (e.g., fimbria-fornix transection) | Memory impairment, spatial learning deficits [1] | Validated cholinesterase inhibitors (e.g., donepezil) for Alzheimer's disease; guides development of pro-cholinergic agents [86]. |
| Dopaminergic System | Substantia Nigra (e.g., 6-OHDA or MPTP models) | Motor deficits (akinesia, rigidity), mimicking Parkinsonian symptoms [86] | Directly led to the development of L-DOPA; critical for pre-clinical testing of dopaminergic agonists and cell-based therapies [86]. |
| Glutamatergic System | Hippocampus (e.g., ibotenic acid lesion) | Spatial memory deficits, impaired long-term potentiation (LTP) [1] | Informs the development of NMDA receptor antagonists and ampakines for cognitive enhancement and neuroprotection. |
| GABAergic System | Basolateral Amygdala | Reduced anxiety, impaired fear conditioning [1] | Used to screen novel anxiolytic drugs that target GABA receptors without inducing excessive sedation. |
| Norepinephrine System | Locus Coeruleus | Attentional deficits, reduced arousal | Supports development of norepinephrine reuptake inhibitors for disorders like ADHD and depression. |
The utility of these models is further amplified when integrated with modern clinical development tools. Model-Informed Drug Development (MIDD) uses pharmacokinetic-pharmacodynamic (PK/PD) models from lesion studies to predict clinical dosing and efficacy, as seen with recent Alzheimer's therapies [86]. Furthermore, digital biomarkers derived from wearable sensors can quantify subtle behavioral changes in lesioned animals, providing high-resolution, objective endpoints for preclinical trials [86].
Experimental Protocols
Protocol: Unilateral 6-Hydroxydopamine (6-OHDA) Lesion Model of Parkinson's Disease
I. Purpose To create a selective, unilateral lesion of the nigrostriatal dopaminergic pathway in rodents for the pre-clinical assessment of novel dopaminergic therapies and disease-modifying agents [86].
II. Materials and Reagents Table 2: Research Reagent Solutions for 6-OHDA Lesion Model
| Item | Function/Explanation |
|---|---|
| 6-Hydroxydopamine HBr (6-OHDA) | A selective neurotoxin that is taken up by catecholaminergic neurons, inducing oxidative stress and apoptosis. |
| Desipramine Hydrochloride | A norepinephrine reuptake inhibitor; pre-injection protects noradrenergic neurons, ensuring dopaminergic specificity [21]. |
| Pargyline | A monoamine oxidase inhibitor (MAOI); pre-injection enhances the toxicity of 6-OHDA by reducing its metabolic breakdown. |
| Sterotaxic Apparatus | Precision instrument for targeting specific brain coordinates (e.g., Substantia Nigra or Striatum). |
| Apomorphine | Dopamine receptor agonist; used to induce and quantify rotational behavior in lesioned animals, a key behavioral endpoint. |
III. Step-by-Step Procedure
- Pre-treatment: Administer desipramine (25 mg/kg, i.p.) and pargyline (50 mg/kg, i.p.) 30-60 minutes before 6-OHDA surgery to protect noradrenergic neurons and enhance toxicity.
- Anesthesia and Preparation: Anesthetize the rodent (e.g., with isoflurane) and securely place it in the stereotaxic frame. Shave the scalp and disinfect the surgical site.
- Craniotomy: Make a midline incision on the scalp, retract the skin, and clean the skull. Use a dental drill to perform a small craniotomy at the calculated coordinates.
- Toxin Injection: Prepare a fresh solution of 6-OHDA (e.g., 4 µg/µL in 0.2% ascorbic acid-saline to prevent oxidation). Using a Hamilton syringe, slowly infuse 2-4 µL of the toxin unilaterally into the target site (e.g., medial forebrain bundle or striatum) at a slow, controlled rate (e.g., 0.5 µL/min).
- Post-injection and Recovery: Leave the needle in place for an additional 5 minutes to allow for diffusion, then slowly retract it. Suture the wound and provide post-operative analgesia and supportive care until the animal fully recovers.
- Behavioral Validation (3-4 weeks post-lesion):
- Apomorphine-Induced Rotation: Administer apomorphine (0.05-0.25 mg/kg, s.c.) and place the animal in a cylindrical rotometer bowl. Record full contralateral rotations for 30-60 minutes. A sustained rotational asymmetry (>6 turns/minute) confirms a successful lesion.
- Cylinder Test: Assess forelimb use by counting the number of times the animal rears and contacts the wall with either forepaw. The lesioned animal will show a significant bias toward using the unimpaired ipsilateral paw.
- Post-mortem Validation: Perfuse the animal and extract the brain. Confirm the dopaminergic cell loss through immunohistochemical staining for Tyrosine Hydroxylase (TH) in the Substantia Nigra and striatum.
Protocol: Ibotenic Acid Lesion of the Hippocampus for Memory Research
I. Purpose To create an excitotoxic lesion that destroys hippocampal cell bodies while sparing passing fibers, modeling the memory deficits observed in Alzheimer's disease and other dementias [1] [21].
II. Key Materials
- Ibotenic Acid: A glutamate agonist that overstimulates neurons, leading to excitotoxic cell death.
- Phosphate Buffered Saline (PBS): Used as the vehicle for dissolving ibotenic acid.
- Sterotaxic Apparatus: For precise hippocampal targeting.
- Morris Water Maze Apparatus: Standard equipment for assessing spatial learning and memory.
III. Step-by-Step Procedure
- Toxin Preparation: Dissolve ibotenic acid in 0.1 M PBS (pH ~7.4) to a concentration of 5-10 µg/µL.
- Surgery: Follow steps for anesthesia and stereotaxic positioning as in the 6-OHDA protocol. Perform multiple microinjections of ibotenic acid (e.g., 0.1-0.2 µL per site) at several anterior-posterior coordinates of the hippocampus.
- Post-operative Care: Allow at least 7-10 days for recovery and full expression of the lesion before behavioral testing.
- Behavioral Validation:
- Morris Water Maze: Train animals to find a hidden platform in a pool of opaque water. Key metrics include escape latency, path length, and time spent in the target quadrant during a probe trial (with the platform removed). Hippocampal-lesioned animals show significant deficits in learning and remembering the platform location [1].
- Histological Verification: Confirm the extent and location of the lesion through Nissl staining or NeuN immunohistochemistry to visualize neuronal cell loss in the hippocampus.
Visualizations
Lesion to Drug Development Workflow
Lesion Model Validation Logic
The lesion method, a cornerstone of neuroscience, investigates brain function by examining the behavioral consequences of brain damage. For over 200 years, studies of individuals with focal brain lesions have been instrumental in linking specific cognitive functions, such as speech and memory, to distinct neural substrates [1]. In the modern era, the traditional lesion method has converged with computational neuroscience. The critical challenge now lies in benchmarking the performance of various computational models that use lesion data to predict behavioral outcomes. This process rigorously tests how well these models can translate anatomical disruption into accurate forecasts of functional impairment, thereby constraining model architectures and informing their future development. This document provides application notes and detailed protocols for conducting such benchmarking studies, framed within the context of correlating brain areas with behavior.
Key Concepts and Definitions
- Lesion-Symptom Mapping (LSM): A statistical approach that assesses the relationship between brain lesions and specific behavioral deficits. Voxel-based Lesion-Symptom Mapping (VLSM) is a common univariate method that tests this relationship on a voxel-by-voxel basis [25].
- Multivariate Lesion-Symptom Mapping (MLSM): An advanced approach that combines all voxels or features into a single model to capture complex, multidimensional relationships between brain damage and behavior that univariate methods may miss [25].
- Benchmarking: The systematic process of comparing the performance of different computational models and methodologies against standardized datasets and evaluation metrics to identify optimal approaches and establish best practices [25] [88].
- Disconnectome Mapping: A technique that moves beyond focal cortical damage to model how lesions disrupt large-scale white-matter networks, often providing better behavioral predictions [25].
Quantitative Benchmarking of LSM Methodologies
Recent research has systematically evaluated various factors influencing model performance in predicting language outcomes after stroke. The tables below summarize key benchmarking results.
Table 1: Benchmarking Model Performance by Atlas and Modality for Aphasia Quotient (AQ) Prediction [25]
| Brain Atlas | Neuroimaging Modality | Best-Performing Model | Correlation (r) |
|---|---|---|---|
| JHU | Lesion Location | Random Forest | 0.69 |
| AAL | Lesion Location | Random Forest | 0.65 |
| AICHA | Lesion Location | Random Forest | 0.63 |
| BRO | Lesion Location | Random Forest | 0.61 |
| JHU | Structural Connectivity (SC) | Support Vector Regression | 0.54 |
| JHU | Resting-State Functional Connectivity (rsFC) | Gradient Boosting | 0.48 |
Table 2: Performance Comparison of Machine Learning Models in LSM [25]
| Machine Learning Model | Key Advantages | Typical Performance (r) | Notable Use Cases |
|---|---|---|---|
| Random Forest | Handles non-linear relationships, robust to overfitting | 0.60 - 0.69 | Best overall performance for lesion location data [25] |
| Support Vector Regression (SVR) | Effective in high-dimensional spaces | 0.59 - 0.67 | Multivariate LSM; combined with MLSM for improved accuracy [25] |
| Gradient Boosting | High predictive accuracy, sequential error correction | ~0.48 - 0.65 | Competitive performance with optimized parameters |
| Linear Regression | Simple, interpretable | Lower than non-linear models | Useful as a baseline model for comparison |
Table 3: Impact of Sample Size and Data Modality on Predictive Power
| Factor | Impact on Performance & Interpretation | Evidence |
|---|---|---|
| Multimodal Data Integration | Can improve accuracy but requires careful cross-validation to avoid data leakage [25]. | SVR with multimodal data yielded r=0.60-0.67 for various language scores [25]. |
| Sample Size | Larger samples (N > 200) improve model generalizability and stability of identified brain-behavior relationships [25]. | Studies with modest sample sizes may report over-optimistic performance [25]. |
| Cross-Validation | Nested cross-validation is essential for unbiased hyperparameter tuning and performance estimation [25]. | Prevents overfitting and over-optimistic performance assessment [25]. |
Experimental Protocols
Protocol: Benchmarking ML Models for Lesion-Symptom Mapping
Application Note: This protocol outlines a factorial design to benchmark machine learning models for predicting behavioral scores from neuroimaging data, suitable for large cohorts (N > 200) of stroke survivors [25].
Materials: See Section 6, "Research Reagent Solutions."
Procedure:
- Data Preparation:
- Lesion Masking: Manually trace or automatically segment lesions on T1-weighted MRI scans. Convert lesions to binary masks and normalize to a standard stereotaxic space (e.g., MNI152) [25] [88].
- Parcellation: Map each lesion mask onto several brain atlases (e.g., JHU, AAL, BRO, AICHA) to extract region-based features [25].
- Feature Extraction: For each atlas region, calculate lesion coverage. For other modalities (rsFC, SC, etc.), extract relevant features (e.g., connectivity strength) within the same parcellation scheme [25].
- Behavioral Data: Collect standardized behavioral scores (e.g., Aphasia Quotient from WAB-R, Philadelphia Naming Test scores).
Model Training & Benchmarking (Nested Cross-Validation):
- Outer Loop (Performance Estimation): Split the entire dataset into k-folds (e.g., 10-fold). Iteratively hold out one fold for testing and use the remaining folds for model development.
- Inner Loop (Hyperparameter Tuning): Within the training set from the outer loop, perform another k-fold cross-validation to tune the hyperparameters of each ML model (e.g., Random Forest, SVR).
- Model Evaluation: For each outer loop iteration, train the model with the optimally tuned hyperparameters on the entire training set and evaluate it on the held-out test set. Aggregate performance metrics (e.g., Pearson's r, MAE) across all test folds.
Analysis & Interpretation:
- Compare the aggregated performance metrics across all combinations of factors: atlas, modality, and ML model.
- Identify the top-performing pipeline(s) for the behavioral outcome of interest.
- Use feature importance measures from the best-performing model (e.g., Gini importance in Random Forest) to identify brain regions most critical for prediction.
Diagram Title: Benchmarking Workflow with Nested Cross-Validation
Protocol: Validating Lesion Segmentation for Computational Modeling
Application Note: Accurate lesion segmentation is a prerequisite for reliable LSM. This protocol describes the creation of a benchmark dataset and evaluation of segmentation models, as demonstrated in the MSLesSeg dataset for Multiple Sclerosis [88].
Materials: See Section 6, "Research Reagent Solutions."
Procedure:
- Dataset Curation:
- Collect multi-modal MRI scans (e.g., T1, T2, FLAIR) from a patient cohort, ideally with multiple timepoints to track lesion evolution [88].
- Divide the data into training and test sets, ensuring the test set is held back for final evaluation.
Expert Annotation and Ground Truth Creation:
- Have expert radiologists manually annotate lesions on all modalities using specialized software. This process is labor-intensive and requires significant expertise [88].
- Establish a consensus from multiple expert annotations to create a high-quality, reliable ground truth dataset for benchmarking.
Preprocessing Pipeline:
- Anonymization: Remove all patient-identifiable information from the scans.
- Format Conversion: Convert images from DICOM to a analysis-friendly format like NIFTI [88].
- Co-registration: Use linear registration tools (e.g., FLIRT from FSL) to align all modalities and timepoints to a standard template (e.g., MNI152) [88].
- Skull Stripping: Perform brain extraction using tools like the Brain Extraction Tool (BET) [88].
Model Benchmarking:
- Train multiple state-of-the-art deep learning segmentation models (e.g., U-Net, nnUNet) on the preprocessed training data.
- Evaluate the trained models on the held-out test set using metrics like Dice Similarity Coefficient (DSC), lesion-wise detection metrics, and Hausdorff Distance.
- Compare the performance of automated models against the expert-validated ground truth and against inter-rater variability among human experts.
Interpretation and Constraint of Models
The primary value of benchmarking lies in its power to constrain and inform computational models. The results from systematic comparisons directly challenge or validate modeling assumptions.
Diagram Title: How Benchmarking Informs and Constrains Models
Constraining Model Architecture: The superior performance of multivariate, non-linear models like Random Forest over traditional mass-univariate methods (e.g., VLSM) constrains future models to account for complex interactions between brain regions [25]. Benchmarking reveals that models failing to incorporate these interactions have lower predictive ceilings.
Constraining Feature Relevance: Benchmarking different neuroimaging modalities directly tests their explanatory power. The finding that lesion location often outperforms functional or structural connectivity in predicting certain deficits [25] constrains models for those behaviors, suggesting they must accurately map focal neural representation.
Constraining Network-Level Effects: The success of disconnectome mapping, which often predicts deficits better than focal lesion location alone, forces models to move beyond singular brain regions [25]. It constrains them to incorporate the architecture of large-scale networks and the impact of lesions on distributed information flow.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Resources for Lesion-Based Computational Modeling
| Category / Solution | Specific Examples & Tools | Function & Application Note |
|---|---|---|
| Neuroimaging Data | T1-weighted, T2-weighted, FLAIR, DTI, rs-fMRI | Provides structural, microstructural, and functional information. Note: Multimodal data often yields the best predictions but requires rigorous preprocessing [25] [88]. |
| Brain Atlases (Parcellation) | JHU, AAL, AICHA, BRO | Standardized templates for summarizing brain data in regions of interest. Note: The choice of atlas significantly impacts model performance (see Table 1) [25]. |
| Preprocessing & Registration Tools | FMRIB Software Library (FSL: FLIRT, BET), SPM, ANTs | Used for image normalization, skull-stripping, and co-registration to standard space (e.g., MNI152), which is critical for group-level analysis and comparison [88]. |
| Lesion Segmentation Tools | Manual tracing (gold standard), automated/semi-automated AI models (e.g., nnUNet) | Generates the primary lesion mask input for models. Note: AI segmentation should be benchmarked against expert manual labels, as in the MSLesSeg protocol [88]. |
| Computational Modeling Environments | Scikit-learn, TensorFlow, PyTorch, R | Provides libraries for implementing and benchmarking a wide range of machine learning models, from Random Forests to complex deep neural networks. |
| Behavioral Assessment Batteries | Western Aphasia Battery (WAB), Philadelphia Naming Test (PNT) | Standardized tools for quantifying behavioral and cognitive deficits, serving as the ground truth output for predictive models [25]. |
Conclusion
The lesion method remains an indispensable tool in the neuroscientist's arsenal, providing unparalleled causal evidence for linking specific brain areas to behavior. Its evolution from classic case studies to sophisticated, computational neuroimaging techniques has solidified its role in mapping brain networks and validating therapeutic targets. The key takeaways highlight the method's unique inferential power, its synergistic relationship with other neuroscience approaches, and its direct clinical impact on diagnosis and neuromodulation. Future directions point toward larger, multi-center collaborations, the integration of state-of-the-art ecological behavioral tasks, and the development of more powerful computational tools to model network-wide effects of focal damage. For biomedical and clinical research, these advances promise to refine our understanding of brain circuitry, accelerate the identification of novel drug targets, and ultimately improve patient outcomes in neurological and psychiatric disorders.
References
- 1. The Lesion : What Individual Patients Can Teach Us About the... Method [https://kids.frontiersin.org/articles/10.3389/frym.2022.869030]
- 2. Using causal to map symptoms to methods circuits in... brain [https://pmc.ncbi.nlm.nih.gov/articles/PMC8918299/]
- 3. Frontiers | Causal in Repetitive Transcranial Magnetic... Inferences [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2020.586448/full]
- 4. Re-establishing Broca ’ s Initial Findings - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6659403/]
- 5. sciencedirect.com/topics/immunology-and-microbiology/ broca - area [https://www.sciencedirect.com/topics/immunology-and-microbiology/broca-area]
- 6. Frontiers | Broca ’ s as a Pre-articulatory Phonetic Encoder... Area [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2018.00064/full]
- 7. The Wernicke conundrum and the anatomy of language comprehension in primary progressive aphasia - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4805066/]
- 8. The Wernicke : Modern evidence and a reinterpretation - PMC area [https://pmc.ncbi.nlm.nih.gov/articles/PMC4691684/]
- 9. Postmortem examination of patient H.M.’s brain based on histological sectioning and digital 3D reconstruction | Nature Communications [https://www.nature.com/articles/ncomms4122]
- 10. H.M.’s Contributions to Neuroscience: A Review and Autopsy Studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6007845/]
- 11. scoville & milner (1957) a case study: the memory of hm [https://www.psychologywizard.net/scoville--milner-ao1-ao3.html]
- 12. of the Lesion involved in language comprehension analysis brain areas [https://pubmed.ncbi.nlm.nih.gov/15037129/]
- 13. The Neuroscience System (NES)–A Experiments to... Software Tool [https://pmc.ncbi.nlm.nih.gov/articles/PMC8777234/]
- 14. systems in the Memory and brain of a localization - PMC memory [https://pmc.ncbi.nlm.nih.gov/articles/PMC33628/]
- 15. The Long View of Language Localization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6543764/]
- 16. Measuring language lateralisation with different language tasks: a systematic review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5659218/]
- 17. 2.7.4 Lesioning Techniques: Studying Brain Function | TutorChase [https://www.tutorchase.com/notes/ap/psychology/2-7-4-lesioning-techniques-studying-brain-function]
- 18. Characterising the unity and diversity of executive functions in a within-subject fMRI study | Scientific Reports [https://www.nature.com/articles/s41598-022-11433-z]
- 19. Executive function and the frontal lobes: a meta-analytic review - PubMed [https://pubmed.ncbi.nlm.nih.gov/16794878/]
- 20. Network Localization of Executive Function Deficits in Patients with Focal Thalamic Lesions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7606569/]
- 21. and Neuroscience Behavioural – Cognition Methods [https://pressbooks.pub/cognition/chapter/behavioural-and-neuroscience-methods/]
- 22. Efficient functional localization of language regions in the brain - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1053811923006390]
- 23. network Lesion for symptom localization: recent... mapping [https://pmc.ncbi.nlm.nih.gov/articles/PMC9724189/]
- 24. network Lesion - Wikipedia mapping [https://en.wikipedia.org/wiki/Lesion_network_mapping]
- 25. Frontiers | Benchmarking machine learning models in lesion -symptom... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2025.1573816/full]
- 26. - Voxel | SpringerLink Based Lesion Symptom Mapping [https://link.springer.com/protocol/10.1007/978-1-0716-2225-4_5]
- 27. (PDF) Voxel - based lesion symptom mapping [https://www.academia.edu/662848/Voxel_based_lesion_symptom_mapping]
- 28. Frontiers | Brain substrates of visual scene memory: a lesion-behavior mapping study [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1606051/full]
- 29. Is VLSM a valid tool for determining the functional anatomy of the brain? Usefulness of additional Bayesian network analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/30449718/]
- 30. Lesion studies in contemporary neuroscience - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6712987/]
- 31. Post-stroke outcomes predicted from multivariate lesion - behaviour ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9630711/]
- 32. Prediction of Communication Impairment in Children With Bilateral... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8841608/]
- 33. Multimodal and multidomain lesion enhances... network mapping [https://www.nature.com/articles/s41598-022-26945-x?error=cookies_not_supported&code=c56ad677-0cf4-48ef-8caf-5909dea703dd]
- 34. Connectome - Workbench Commands [https://www.humanconnectome.org/software/workbench-command/-cifti-palette]
- 35. Specify node_color for nilearn.plotting.plot_connectome - nilearn - Neurostars [https://neurostars.org/t/specify-node-color-for-nilearn-plotting-plot-connectome/5834]
- 36. nilearn.plotting.plot_connectome - Nilearn [https://nilearn.github.io/dev/modules/generated/nilearn.plotting.plot_connectome.html]
- 37. view connectome with different colors of nodes · Issue #1945 · nilearn/nilearn [https://github.com/nilearn/nilearn/issues/1945]
- 38. Frontiers | Precancerous pathways to gastric cancer: a review of... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1620756/full]
- 39. Preparing a Protocol for Submission - UCI Office of Research [https://research.uci.edu/animal-care-and-use/protocol-submission/protocol-preparation/]
- 40. and neural principles of a Cognitive bias on preferential... memory [https://pmc.ncbi.nlm.nih.gov/articles/PMC9846459/]
- 41. Neuromodulation: Update on current practice and future developments - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11103215/]
- 42. Network localization of neurological symptoms from focal brain lesions [https://pubmed.ncbi.nlm.nih.gov/26264514/]
- 43. Frontiers | The origins of evil: From lesions to the functional... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2022.969206/full]
- 44. Regional, circuit and network heterogeneity of brain abnormalities in... [https://www.nature.com/articles/s41593-023-01404-6?error=cookies_not_supported]
- 45. Excitatory-Inhibitory Homeostasis and Diaschisis : Tying the Local and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8785563/]
- 46. Frontiers | Compensatory Relearning Following Stroke: Cellular and... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2018.01023/full]
- 47. - Data | Brilliant Math & Science Wiki Presentation Tables [https://brilliant.org/wiki/data-presentation-tables/]
- 48. -Ready Presentation and Analytic Result Data Summary Tables [https://www.danieldsjoberg.com/gtsummary/]
- 49. Frontiers | The Neuroscience Experiments System (NES)–A Software Tool to Manage Experimental Data and Its Provenance [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2021.768615/full]
- 50. Text has enhanced contrast | ACT Rule | WAI | W3C [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 51. chroma.js api docs! [https://gka.github.io/chroma.js/]
- 52. integrity White with cognition and disease severity in... matter correlates [https://pubmed.ncbi.nlm.nih.gov/33141169/]
- 53. on diffusion tensor White with... matter damage imaging correlates [https://kclpure.kcl.ac.uk/portal/en/publications/white-matter-damage-on-diffusion-tensor-imaging-correlates-with-a]
- 54. Evaluation of the perilesional normal-appearing white ... matter [https://qims.amegroups.org/article/view/142414/html]
- 55. Frontiers | Small-vessel-disease-induced white in... matter damage [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1538598/full]
- 56. Lesion Topography and Microscopic White Matter Tract Damage Contribute to Cognitive Impairment in Symptomatic Carotid Artery Disease - PubMed [https://pubmed.ncbi.nlm.nih.gov/27598537/]
- 57. Neonatal White Analysis Using Matter Super- Damage ... DTI Resolution [https://pubmed.ncbi.nlm.nih.gov/37982259/]
- 58. Topographic patterns of white matter hyperintensities are associated with multimodal neuroimaging biomarkers of Alzheimer’s disease | Alzheimer's Research & Therapy | Full Text [https://alzres.biomedcentral.com/articles/10.1186/s13195-020-00759-3]
- 59. Automated quantification of deep grey matter structures and white matter lesions using magnetic resonance imaging in relapsing remission multiple sclerosis | Egyptian Journal of Radiology and Nuclear Medicine | Full Text [https://ejrnm.springeropen.com/articles/10.1186/s43055-021-00582-2]
- 60. -symptom mapping using support vector regression Multivariate lesion [https://pubmed.ncbi.nlm.nih.gov/25044213/]
- 61. Cognitive Psychology and Cognitive Neuroscience/Behavioural and Neuroscience Methods - Wikibooks, open books for an open world [https://en.wikibooks.org/wiki/Cognitive_Psychology_and_Cognitive_Neuroscience/Behavioural_and_Neuroscience_Methods]
- 62. Frontiers | Prediction of Communication Impairment in Children With... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2022.788037/full]
- 63. Multivariate Lesion-Behavior Mapping of General Cognitive Ability and Its Psychometric Constituents - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7659456/]
- 64. Frontiers | Harnessing artificial intelligence for brain disease: advances in diagnosis, drug discovery, and closed-loop therapeutics [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1615523/full]
- 65. Improving clinical trials with machine learning | UCL News - UCL – University College London [https://www.ucl.ac.uk/news/2017/nov/improving-clinical-trials-machine-learning]
- 66. methods in sport Machine prediction and prevention... learning injury [https://jeo-esska.springeropen.com/articles/10.1186/s40634-021-00346-x]
- 67. Frontiers | Current limitations in technology-based cognitive... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2025.1543005/full]
- 68. Qualitative & Quantitative vs Structured & Unstructured Data : The... [https://medium.com/@okontaagape/qualitative-quantitative-vs-structured-unstructured-data-the-data-power-couples-9ff4352e8d4b]
- 69. Momentary Ecological (EMA) | Simply Psychology Assessment [https://www.simplypsychology.org/ecological-momentary-assessment.html]
- 70. vs Unstructured Structured Explained with Examples Data [https://www.altexsoft.com/blog/structured-unstructured-data/]
- 71. Frontiers | Integrating fMRI spatial network dynamics and EEG spectral... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1484954/full]
- 72. analysis related to coma and prognosis in acute... Quantitative EEG [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03191-1]
- 73. response varies with EEG location in patients with chronic stroke lesion [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-016-0120-2]
- 74. Frontiers | Spatial (mis) match between EEG and fMRI signal patterns... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1549172/full]
- 75. Mapping human brain lesions and their functional consequences - PubMed [https://pubmed.ncbi.nlm.nih.gov/29042216/]
- 76. Using machine learning-based lesion behavior mapping to identify anatomical networks of cognitive dysfunction: spatial neglect and attention - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6765420/]
- 77. Frontiers | Precision TMS through the integration of neuroimaging and... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1682852/full]
- 78. Frontiers | Optogenetics and chemogenetics: key tools for modulating... [https://www.frontiersin.org/journals/neural-circuits/articles/10.3389/fncir.2025.1516839/full]
- 79. , memories, and mind control | @neurochallenged Optogenetics [https://neuroscientificallychallenged.com/posts/optogenetics-memories-mind-control]
- 80. Global Optogenetics Market Report 2025 , Growth, Outlook To 2034 [https://www.thebusinessresearchcompany.com/report/optogenetics-global-market-report]
- 81. Brain substrates of visual : a lesion-behavior mapping... scene memory [https://pubmed.ncbi.nlm.nih.gov/40958990/]
- 82. sciencedirect.com/science/article/pii/S1053811922003287 [https://www.sciencedirect.com/science/article/pii/S1053811922003287]
- 83. An fMRI study on memory discriminability for complex visual scenes - PubMed [https://pubmed.ncbi.nlm.nih.gov/17894398/]
- 84. Neural signatures of Trail Making Test performance: Evidence from... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6018614/]
- 85. working Visual are abstractions of percepts | eLife memories [https://elifesciences.org/articles/94191]
- 86. Neuroscience Drug : Alzheimer’s & MS Advances Development 2025 [https://www.allucent.com/resources/blog/all-about-neuroscience-drug-development]
- 87. in Alzheimer's disease: the path to Drug development 2025 [https://pubmed.ncbi.nlm.nih.gov/27646601/]
- 88. MSLesSeg: baseline and benchmarking of a new Multiple Sclerosis... [https://www.nature.com/articles/s41597-025-05250-y?error=cookies_not_supported&code=4574659f-eeb0-46c9-a9a8-2b706e2090cc]