Theoretical Frameworks for VR in Behavioral Neuroscience: From Embodied Simulation to Clinical Translation
This article synthesizes the key theoretical frameworks underpinning the use of Virtual Reality (VR) in behavioral neuroscience, tailored for researchers and drug development professionals.
Theoretical Frameworks for VR in Behavioral Neuroscience: From Embodied Simulation to Clinical Translation
Abstract
This article synthesizes the key theoretical frameworks underpinning the use of Virtual Reality (VR) in behavioral neuroscience, tailored for researchers and drug development professionals. We explore the foundational principle of 'embodied simulation,' which posits that VR and the brain share a common mechanism for predicting sensory consequences, thereby facilitating cognitive and behavioral change. The scope extends to methodological applications in diagnosing and treating disorders like anxiety, PTSD, and addiction, leveraging VR's capacity for ecologically valid cue exposure. We critically troubleshoot implementation challenges, including methodological limitations and ethical considerations. Finally, we validate the approach through comparative efficacy data and emerging neurobiological evidence of VR-induced neuroplasticity, outlining a future trajectory for personalized, mechanism-driven clinical interventions and drug discovery.
The Brain in the Machine: Foundational Theories of VR and Embodied Cognition
The brain, according to increasingly dominant neuroscience paradigms, is not a passive receiver of stimuli but an active generator of predictions about the world. It maintains an internal model—an embodied simulation—of the body and its surrounding space, which it continuously updates to minimize the discrepancy between predicted and actual sensory input [1]. This process, known as predictive coding, is fundamental to how we perceive, act, and feel [1]. Remarkably, Virtual Reality (VR) technology operates on an analogous principle. A VR system also maintains a real-time simulation of a body and its environment, predicting the sensory consequences of a user's movements and providing corresponding visual and auditory feedback [2] [3]. This shared mechanistic foundation—the creation and manipulation of embodied simulations—is why VR has emerged as such a powerful tool for behavioral neuroscience research and clinical intervention. It provides a unique medium through which researchers can systematically alter the sensory reality presented to the brain, thereby "tricking" its predictive processes to study fundamental mechanisms of cognition and behavior, and ultimately, to promote therapeutic change [2] [1] [3].
This whitepaper explores the unifying framework of embodied simulation, detailing its theoretical underpinnings, its validation through key experimental paradigms, and the practical protocols that enable its application in cutting-edge behavioral neuroscience research.
Theoretical Foundations: Predictive Coding and the Bodily Self
The Predictive Brain
At the core of the embodied simulation framework is the predictive coding theory of brain function [1]. This theory posits that the brain's primary function is to infer the causes of its sensory inputs by constantly generating and refining an internal model of the world and the body within it [1]. This model is not a static representation but a dynamic, multimodal simulation that integrates visceral (interoceptive), motor (proprioceptive), and sensory (e.g., visual, auditory) information [1]. The simulation is used to predict both upcoming sensory events and the optimal actions to deal with them. When there is a mismatch between the brain's prediction and the incoming sensory data—a prediction error—the brain updates its model to improve future predictions [1].
The Body Matrix and Presence
These continuous, multisensory simulations are thought to be integrated within a "body matrix"—a supramodal representation of the body and the peripersonal space around it [1]. This matrix, shaped by top-down predictions and bottom-up sensory signals, is crucial for maintaining the integrity of the body at both homeostatic and psychological levels [1]. It plays a key role in high-level cognitive processes such as motivation, emotion, social cognition, and self-awareness [1].
The psychological sense of "presence"—the feeling of "being there" in a virtual environment—is a direct manifestation of this process [3]. According to the "inner presence" theory, presence is not merely a product of advanced technology but a fundamental cognitive function that identifies which environment (real or virtual) is the most likely to be "real" for the self, based on which one provides the most coherent and least surprising sensory-motor experience for enacting one's intentions [3]. When a VR system provides coherent, multi-sensory feedback that aligns with the brain's own predictions, the user's body matrix begins to incorporate the virtual body and space, leading to a compelling feeling of embodiment and presence within the synthetic world [1] [3].
Experimental Evidence: Validating the Framework
The embodied simulation framework is supported by a growing body of evidence demonstrating VR's efficacy in both eliciting and modifying human experiences in controlled settings. The table below summarizes key findings from clinical and experimental studies.
Table 1: Key Experimental Evidence for VR Efficacy Based on Embodied Simulation
| Domain/Disorder | Key Experimental Findings | Implied Mechanism |
|---|---|---|
| Anxiety Disorders (Phobias, PTSD) | VR Exposure Therapy (VRET) shows outcomes superior to waitlist controls and comparable to traditional exposure therapy [2]. Effective for specific phobias, PTSD, panic disorder, and social anxiety [2]. | VR safely triggers fear networks; new, corrective learning updates the pathological internal model via prediction error minimization. |
| Eating & Weight Disorders | RCTs show VR-based treatment can have higher efficacy than gold-standard CBT at 1-year follow-up. Effective for anorexia and obesity [2]. | "Body swapping" alters the patient's dysfunctional internal body image simulation, updating the body matrix. |
| Chronic Pain Management | VR embodiment techniques can reduce pain perception and improve body perception disturbance (e.g., in Complex Regional Pain Syndrome) [1]. | VR provides counteractive visual and proprioceptive signals that update the brain's pathological pain and body representation models. |
| Social Skills Acquisition | A single VR training improves job-interview self-efficacy and reduces anxiety, with effects persisting for 4 months. More time-efficient than chat-based training [4]. | VR allows safe embodiment and practice of social interactions, updating the internal model of social self-efficacy and threat. |
Detailed Experimental Protocol: VR Body Swapping for Body Image Disturbance
This protocol is adapted from studies on eating and weight disorders, as cited in [2] and [1].
- Objective: To alter the internal body representation (body matrix) in patients with body image disturbance, such as anorexia nervosa or obesity.
- Hypothesis: First-person embodiment in a virtual body with healthier proportions will lead to a measurable behavioral and perceptual shift towards the virtual body, generalizing to the real world.
- Independent Variables: Body type of the virtual avatar (e.g., healthy BMI vs. underweight vs. overweight); Synchrony of visuotactile stimulation (synchronous vs. asynchronous).
- Dependent Variables: Skin temperature response (a measure of body ownership); Proprioceptive drift (behavioral measure of body ownership); Self-reported body size estimation; Questionnaire measures of body satisfaction and eating disorder psychopathology.
Procedure:
- Pre-Test Baseline: Measure participants' body size estimation (e.g., using a body distortion task) and collect psychometric scales.
- Setup: Participant wears a head-mounted display (HMD) and stands in a tracked space.
- Embodiment Induction:
- The participant sees a virtual body from a first-person perspective, replacing their own.
- The researcher uses a rod to synchronously touch the participant's actual body and the corresponding part of the virtual body (e.g., the shoulder). This multisensory correlation induces a sense of body ownership over the avatar [1].
- Experimental Manipulation: Participants are randomly assigned to embody an avatar with a body size different from their own (e.g., healthier BMI).
- Post-Test: Immediately after the embodiment period, re-administer the body size estimation task and psychometric measures.
- Follow-Up: Conduct assessments at 1-week, 1-month, and 1-year intervals to test for long-term generalization.
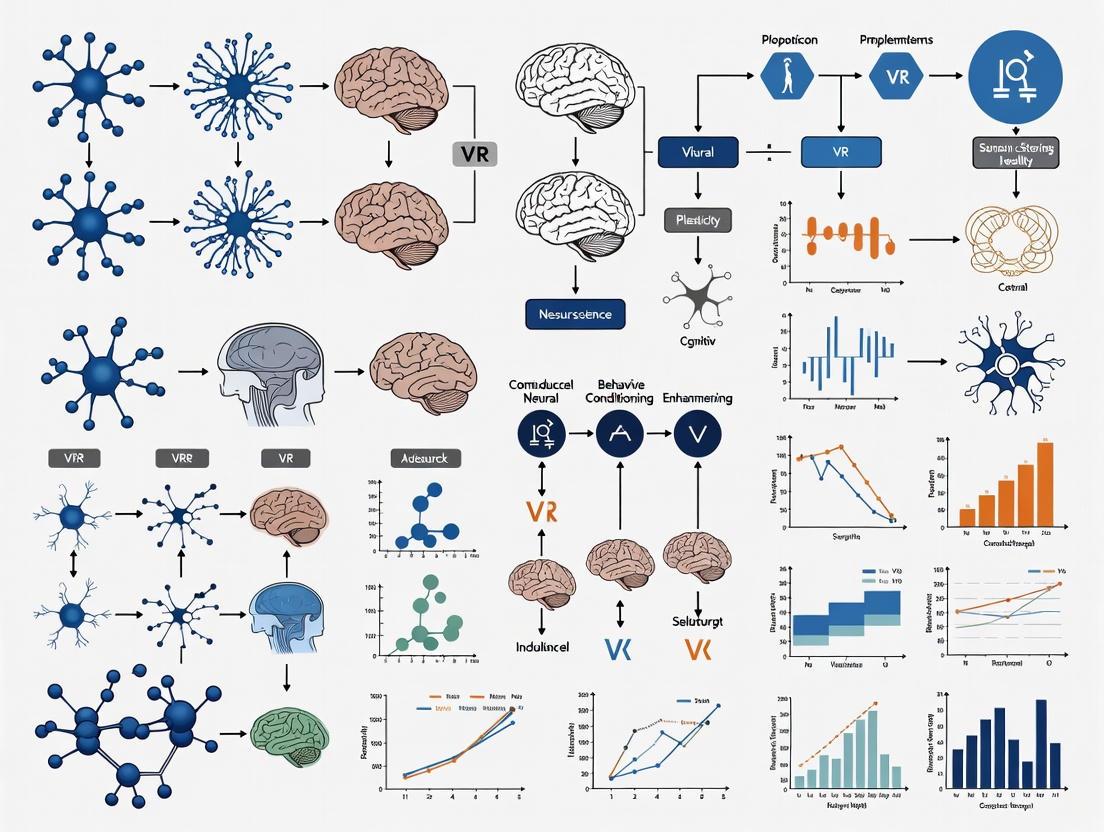
Visualization of Experimental Workflow: The following diagram illustrates the core inductive logic of the body swapping protocol.
A Model for Research: From Phenomenon to Publication
To systematically apply the embodied simulation framework in neuroscience research, a structured approach to modeling is essential. The following 10-step guide, adapted from Blohm et al. (2020), provides a robust pipeline for building computational models of brain and behavior in VR [5].
Table 2: A 10-Step Modeling Guide for Neuroscience Research in VR [5]
| Step | Action | Application to VR & Embodied Simulation |
|---|---|---|
| 1 | Find a phenomenon and a question. | Define a specific behavioral phenomenon (e.g., proprioceptive drift in body ownership) and a clear "how" or "why" question. |
| 2 | Formalize your knowledge. | List all critical observations and existing knowledge about the phenomenon and the relevant VR parameters. |
| 3 | Find the central concept. | Identify the core concept from embodied simulation theory (e.g., "minimizing sensory prediction error") that can explain your phenomenon. |
| 4 | Select a mathematical framework. | Choose a framework that fits your concept (e.g., Bayesian inference for multisensory integration). |
| 5 | Implement the model. | Write the code, defining the state variables, parameters, and dynamics that implement your chosen framework. |
| 6 | Simulate the experiment. | Use your model to generate data for the same experimental task your human subjects undergo in VR. |
| 7 | Check model behavior. | Does the model's output qualitatively match the key features of your human data? |
| 8 | Optimize model parameters. | Fit your model to the experimental data to find the best-fitting parameters. |
| 9 | Validate the model. | Test the model's predictions on a new, held-out dataset to ensure it generalizes. |
| 10 | Publish. | Share your model, code, and data to enable replication and further scientific progress. |
Visualization of the Modeling Process: The flowchart below outlines the iterative, staged process of building a successful model for neuroscience research.
The Scientist's Toolkit: Essential Research Reagents
To conduct rigorous experiments within the embodied simulation framework, specific technological and methodological "reagents" are required. The table below details these essential components.
Table 3: Key Research Reagent Solutions for Embodied Simulation Studies
| Tool Category | Specific Examples | Critical Function in Research |
|---|---|---|
| Head-Mounted Displays (HMDs) | Consumer-grade (Meta Quest, HTC Vive), Research-grade (Varjo) | Provides the immersive visual and auditory stimulus, tracking head movements to update the visual scene in real-time. Key for inducing presence. |
| Body Tracking Systems | Lighthouse tracking, Inside-out tracking, Motion capture suits (Vicon) | Tracks body and limb movements to animate a virtual avatar and/or update the user's perspective. Essential for studying agency and body ownership. |
| Haptic & Tactile Interfaces | Vibrotactile actuators, Force-feedback gloves (Dexmo), Haptic rods | Provides synchronous tactile and proprioceptive feedback to the user. Critical for inducing the rubber hand illusion and full-body ownership illusions. |
| Physiological Monitors | EEG, ECG, GSR (Galvanic Skin Response), EMG, Eye-tracking | Provides objective, continuous measures of cognitive/affective states (arousal, stress, engagement) during the VR experience, complementing self-report. |
| Software & Modeling Platforms | Unity, Unreal Engine, MATLAB, custom Bayesian modeling code | Used to create the virtual environments and to implement computational models that formalize hypotheses about the brain's predictive processes. |
The framework of embodied simulation represents a paradigm shift in behavioral neuroscience, positioning VR not merely as a fancy display technology, but as a unique tool for directly interfacing with the brain's fundamental computational mechanisms. By designing virtual environments that systematically manipulate the sensory cues contributing to the body matrix, researchers can rigorously test hypotheses about the construction of the self, emotion, and behavior. The experimental protocols and modeling guide provided here offer a concrete pathway for scientists to engage in this research.
Future work will likely focus on augmented embodiment—mapping difficult-to-perceive internal signals (e.g., neural activity, visceral state) to immersive sensory displays to enhance self-regulation [1]. Furthermore, as the parallels between the predictive brain and VR become even clearer, the vision of "embodied medicine" will advance: using targeted virtual simulations to directly alter pathological bodily processes for therapeutic effect, truly creating a "healthy mind in a healthy body" [1].
The Role of Presence and Immersion in Creating Therapeutic Realities
This technical guide examines the critical roles of presence (the subjective psychological experience of "being there" in a virtual environment) and immersion (the objective capability of the system to deliver a rich set of sensory stimuli) in creating effective virtual reality (VR) therapeutic interventions. Within theoretical frameworks for behavioral neuroscience research, these constructs provide the foundation for VR's mechanism of action across clinical applications. The interplay between technological immersion and psychologically mediated presence creates a powerful tool for manipulating perception, attention, and emotional processing—with significant implications for therapeutic outcomes in anxiety disorders, pain management, and neurological rehabilitation.
Theoretical Foundations in Behavioral Neuroscience
Defining the Core Constructs
In VR therapeutics, immersion and presence represent distinct but interrelated concepts fundamental to understanding its biological and psychological impacts. According to Slater and Wilbur's widely cited framework, immersion constitutes "an objective and quantifiable description of what any particular system does provide," while presence represents "a state of consciousness, the (psychological) sense of being in the virtual environment" [6]. This distinction is crucial for behavioral neuroscience research methodologies, as it separates the technical specifications of the VR system from the subjective experience they elicit.
From a neuroscience perspective, VR functions through embodied simulations that leverage the brain's innate predictive coding mechanisms. The brain continuously creates embodied simulations of the body in the world to regulate and control effective interaction with the environment [2]. VR technology essentially co-opts this fundamental neurological process by providing an external simulation that predicts the sensory consequences of an individual's movements, creating a compelling alternative reality that the brain accepts and processes similarly to real-world experiences [2].
Neurocognitive Mechanisms of Action
The therapeutic efficacy of VR primarily operates through several interconnected mechanisms:
Attentional Capture: VR reduces pain by "diverting attentional resources that would otherwise be used to process nociceptive signals" [6]. Functional MRI studies demonstrate that VR produces a 50% reduction in pain-related brain activity across five key regions: the primary and secondary somatosensory cortex, anterior cingulate, insula, and thalamus [6].
Emotional Processing: For anxiety disorders, VR facilitates emotional processing by activating and modifying fear memories through controlled exposure to feared stimuli in a safe environment [7]. This process allows for the incorporation of novel, incompatible information that updates maladaptive fear structures.
Embodied Cognition: By creating multisensory experiences that respond naturally to user movements, VR can alter the experience of the body and facilitate cognitive change through targeted virtual environments that simulate both external worlds and internal bodily states [2].
Quantitative Evidence for Therapeutic Efficacy
Clinical Outcomes Across Disorders
Table 1: Therapeutic Efficacy of VR Across Clinical Conditions
| Clinical Condition | Effect Size/Outcome | Comparison Condition | Research Evidence |
|---|---|---|---|
| Anxiety Disorders | Large treatment effects; small effect size favoring VRE over in-vivo | In-vivo exposure, waitlist | Meta-analytic results [7] |
| Specific Phobias | Similar efficacy to traditional evidence-based treatments | Waitlist, traditional exposure | Multiple RCTs [7] [2] |
| Flight Anxiety | Significant overall efficiency at post-test and follow-up | Control conditions, evidence-based interventions | Quantitative meta-analysis of 11 studies [2] |
| Acute Pain | 25% reduction in pain intensity; 23% increase in fun during stimulus | Semi-immersive VR, no VR | Randomized crossover study (n=72) [6] |
| Eating/Weight Disorders | Higher efficacy than gold-standard CBT at 1-year follow-up | Cognitive-behavioral therapy | 3 RCTs [2] |
| PTSD | Large effect sizes; significant symptom reduction | Waitlist, imaginal exposure | Multiple studies [7] [8] |
Presence and Immersion Metrics
Table 2: Technological and Psychological Factors Influencing Therapeutic Outcomes
| Factor | Definition | Impact on Therapeutic Outcomes | Empirical Support |
|---|---|---|---|
| Field of View | Angular extent of observable virtual world | Wider FOV increases presence and analgesia | Hoffman et al., 2006 [6] |
| Head Tracking | System ability to track and respond to head movements | Increases sense of presence and engagement | Slater & Wilbur, 1997 [6] |
| Interactivity | User ability to manipulate virtual environment | Significantly increases VR analgesia | Wender et al., 2009 [6] |
| Tactile Feedback | Haptic responses to user interactions | Enhances realism and therapeutic impact | Hoffman et al., 2023 [6] |
| Display Resolution | Number of pixels in VR goggles | Higher resolution reduces distraction and increases presence | Slater, 2018 [6] |
Experimental Protocols and Methodologies
Standardized VR Exposure Therapy Protocol
For anxiety disorders, particularly specific phobias and PTSD, VR exposure therapy (VRET) follows a structured protocol:
Sessions 1-3: Psychoeducation regarding the specific disorder, psychosocial history assessment, overview of avoidance patterns, and rationale for exposures. Introduction to the process of VR-based exposures is provided, along with basic relaxation and/or coping strategies (e.g., breathing relaxation, cognitive restructuring) [7].
Subsequent Sessions: Conduct VR exposures where patients progress at an individualized pace through a graded exposure hierarchy. Each hierarchy step is repeated until anxiety decreases significantly, as measured by subjective units of distress ratings and behavioral observation [7].
Hierarchy Development: Content is typically preselected for specific disorders, with thorough assessment of the patient's fear or traumatic experience prior to exposure to individualize progression through hierarchy steps [7].
VR Analgesia Research Protocol
A recent randomized crossover study detailed a rigorous methodology for investigating VR's pain reduction mechanisms:
- Participants: 72 college students (mean age 19 years) [6].
- Design: Repeated measures crossover with conditions randomized.
- Conditions: No VR, semi-immersive VR (narrow field of view, no head tracking, no interactivity), and immersive VR (wide field of view, head tracking, interactivity) [6].
- Pain Stimulation: Brief, painful but safe and tolerable heat stimulations.
- Measures: Pain ratings (0-10 Graphic Rating Scale), fun ratings during stimulus, and performance on an attention-demanding odd-number divided-attention task [6].
- Analysis: Comparison of pain ratings and attention task errors across conditions, with secondary analyses for gender, race, and pain catastrophizing tendencies.
Diagram 1: VR Analgesia Study Experimental Workflow
Four-Stage Protocol for VR Implementation in Psychological Research
A comprehensive framework for implementing VR in psychological research and practice involves four key stages [8]:
Equipment Selection: Considerations include technical specifications, immersion capabilities, space limitations, resource demands, and integration capabilities with other hardware. Selection should be guided by the specific clinical population and research objectives [8].
Design and Development: Requires interdisciplinary collaboration between clinicians, researchers, and software developers. Investment in skill development and resources is essential, with end-user feedback incorporated throughout development [8].
Technology Integration: Combination of VR with other technologies (e.g., physiological recording, EEG, MRI) requires creative solutions and software development expertise. Important distinctions exist between open and closed platforms regarding customization capabilities [8].
Clinical Implementation: Successful adoption depends on appropriateness, acceptability, and feasibility within healthcare systems. Considerations include therapeutic alliance maintenance during immersion, development of training tools, and addressing unique ethical issues such as risk management and consent protocols [8].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Technologies for VR Therapeutics Research
| Research Reagent | Technical Function | Therapeutic Application |
|---|---|---|
| Head-Mounted Displays (HMDs) | Provide visual and auditory immersion through head-locked displays | Primary interface for VR exposure therapy and analgesia |
| Gesture-Sensing Gloves | Enable natural interaction with virtual objects through hand tracking | Enhances sense of presence and agency in therapeutic environments |
| Vibrotactile Platforms | Deliver haptic feedback synchronized with virtual events | Increases realism and multisensory engagement |
| Eye-Tracking Systems | Measure gaze direction and pupillary responses within VR | Provides objective metrics of attention allocation during therapy |
| Physiological Monitoring | Records heart rate, skin conductance, EEG during VR sessions | Objective measurement of emotional and physiological arousal |
| Virtual Environment Software | Creates controlled, replicable therapeutic scenarios | Standardized delivery of exposure hierarchies and interventions |
| Head Tracking Systems | Updates visual display based on head position and orientation | Enhances spatial presence and reduces simulation sickness |
Signaling Pathways: Neurocognitive Mechanisms of VR Therapeutics
Diagram 2: Neurocognitive Pathways of VR Therapeutic Action
Future Directions and Research Agenda
The application of VR in behavioral neuroscience and therapeutics continues to evolve with several critical research frontiers:
Personalized VR Environments: Development of patient-specific virtual environments based on individual fear structures, trauma memories, or pain triggers [7] [8].
Neuromodulation Integration: Combination of VR with techniques such as transcranial direct current stimulation (tDCS) shows preliminary positive results for pain management and rehabilitation [2].
Advanced Biomarkers: Integration of neuroimaging, eye-tracking, and physiological monitoring to develop objective biomarkers of presence and therapeutic engagement [8] [6].
Implementation Science: Systematic study of barriers to clinical adoption, including clinician training, resource allocation, and treatment fidelity across settings [8].
Mechanism Refinement: Further elucidation of the temporal dynamics between immersion, presence, and therapeutic change, particularly through rigorous attention measurement as demonstrated in recent analgesia studies [6].
The integration of presence and immersion within theoretical frameworks for behavioral neuroscience offers powerful methodological opportunities for studying human perception, attention, and emotion in ecologically valid yet controlled environments. As technological capabilities advance and research methodologies become more sophisticated, VR continues to establish its value as both an investigative tool in neuroscience and a transformative modality in therapeutic applications.
The integration of Virtual Reality (VR) into behavioral neuroscience research represents a paradigm shift, enabling unprecedented investigation of learning and meaning-making processes. This transformation is rooted in the powerful convergence of constructivist and situated cognition theories with immersive technologies. Constructivist learning theory posits that knowledge is not passively received but actively built by the learner based on their existing cognitive structures and experiences [9]. Simultaneously, situated cognition theory maintains that learning and knowledge are fundamentally tied to the context and environment in which they are developed [9]. VR technology serves as the ideal experimental platform where these theoretical frameworks intersect, allowing researchers to create controlled yet ecologically valid environments where participants actively construct knowledge within situated contexts [9] [10].
The significance for behavioral neuroscience research lies in VR's capacity to standardize complex experimental tasks while maintaining high ecological validity. By closing "the gap between protocol intent and participant execution," VR converts multi-step instructions into timed, spatially constrained tasks with real-time coaching, yielding lower variance and cleaner audit trails than traditional methods [11]. This technological capability aligns perfectly with the needs of contemporary research, particularly in pharmaceutical development and clinical trials, where understanding the neurobehavioral mechanisms underlying learning can accelerate therapeutic discovery [11] [12].
Theoretical Foundations for VR-Enhanced Learning
Constructivist Learning Theory in Virtual Environments
Constructivism maintains that learning is an active process where learners construct new knowledge based on their prior experiences and interactions with their environment [9] [13]. The four fundamental elements of constructivist learning—situation, collaboration, conversation, and meaning construction—find unique expression in VR environments [9]. In constructivist theory, the learning process is characterized by three essential attributes: initiative (learners actively construct knowledge), diversity and heterogeneity (different individuals construct different knowledge structures), and collaborative learning (knowledge is built through social negotiation) [9].
In VR-enhanced constructivist learning, environments can be dynamically designed to present problems and scenarios that require learners to actively explore and develop their own understanding. Rather than passively receiving information, participants in VR experiments manipulate virtual objects, navigate complex spatial environments, and observe the consequences of their actions, thereby constructing mental models through direct experience [10]. This approach stands in stark contrast to traditional behavioral paradigms where stimuli and responses are often severely constrained.
Situated Cognition Theory in Virtual Environments
Situated cognition theory emphasizes that knowledge and learning are fundamentally situated in the specific context and activity in which they are developed [9]. This theoretical framework challenges the notion that knowledge can be abstracted from the situations in which it is used and argues that learning is inseparable from the environment and practice in which it occurs [9]. Situated cognition thus positions practice not as independent of learning, but as integral to it, with meaning emerging from the interaction between practice and situational context [9].
VR technology offers powerful applications for situated cognition by enabling researchers to create authentic, context-rich environments that closely mimic real-world settings while maintaining experimental control [10] [14]. These virtual environments allow for the study of cognitive processes within realistic contexts, addressing a significant limitation of traditional laboratory-based experiments. For behavioral neuroscience, this means that tasks such as spatial navigation, decision-making, and social cognition can be studied in environments that closely resemble real-world scenarios, thereby enhancing the ecological validity of findings [14] [15].
Theoretical Alignment of VR with Learning Frameworks
The pedagogical value of VR in neuroscience research and education is strongly supported by its alignment with contemporary learning theories that emphasize active, experiential, and situated engagement [10]. Embodied cognition, a theoretical framework linking motor experiences to cognitive processes, offers further support for immersive learning approaches [10]. As participants physically interact with virtual structures using motion controls and spatial navigation, they deepen their understanding through sensory-motor engagement, activating neural pathways that support deeper learning and retention [10].
Cognitive load theory also plays a critical role in designing effective VR experiments for behavioral neuroscience. The design of immersive learning experiences must balance intrinsic, extraneous, and germane cognitive load to optimize learning outcomes [10]. In neuroscience research contexts, this involves sequencing experimental tasks from simple to complex, integrating multimodal feedback, and providing appropriate scaffolding to support participants with different cognitive abilities and prior experiences [10].
Quantitative Validation of VR-Enhanced Learning
Empirical studies across multiple domains have demonstrated the efficacy of VR-enhanced learning approaches grounded in constructivist and situated cognition principles. The following table summarizes key quantitative findings from recent research:
Table 1: Quantitative Evidence for VR-Enhanced Learning Across Domains
| Domain | Performance Metric | Improvement | Research Context |
|---|---|---|---|
| General Cognitive Learning | Learning efficiency | ≥20% improvement compared to traditional methods [9] | VR-enhanced campus knowledge learning |
| Precision Motor Skills | Shot scores | 13% average improvement across visits [12] | Simulated marksmanship in immersive VR |
| Motor Learning | Hand reaction times | Significant decrease with practice [12] | Visuomotor task in interactive VR |
| Motor Learning | Spatial precision | Significant increase with practice [12] | Three-visit motor task in VR |
| Clinical Applications | Neurocognitive batteries | Standardized testing with reduced variance [11] | Clinical trial settings |
| Motor Function Assessment | Fine-motor precision | Improved tremor grading and measurement [11] | Parkinson's and MS clinical research |
These quantitative findings demonstrate that VR environments grounded in constructivist and situated cognition principles can significantly enhance learning outcomes across diverse domains. The 20% improvement in learning efficiency reported in general cognitive learning aligns with performance enhancements observed in motor learning tasks, suggesting common underlying mechanisms [9] [12]. For behavioral neuroscience research, these findings validate VR as not merely an immersive presentation tool but as a powerful platform for enhancing cognitive and motor learning processes.
The neural mechanisms underlying these performance improvements are increasingly being uncovered through neurophysiological investigations. Studies combining VR with EEG have revealed that "spectral and time-locked analyses of the EEG beta band (13-30 Hz) power measured prior to target launch and visual-evoked potential amplitudes measured immediately after the target launch correlated with subsequent reactive kinematic performance" [12]. Furthermore, practice-related changes in "launch-locked and shot/feedback-locked visual-evoked potentials became earlier and more negative with practice, pointing to neural mechanisms that may contribute to the development of visual-motor proficiency" [12].
Experimental Protocols for VR-Enhanced Learning Research
Protocol 1: Visuomotor Integration and Learning Assessment
This protocol measures neurobehavioral mechanisms underlying precision visual-motor control, adapting experimental paradigms from existing VR research [12].
Materials and Setup:
- Immersive VR system with head-mounted display and motion tracking
- EEG system with appropriate data synchronization capabilities
- Virtual environment simulating a coincidence-anticipation task (modeled after target shooting)
- Data recording system for kinematic measures and neural activity
Procedure:
- Participant Preparation: Apply EEG electrodes according to standard positioning guidelines (10-20 system). Ensure proper impedance values (<5 kΩ) for all electrodes.
- Baseline Assessment: Record resting-state EEG for 5 minutes (eyes-open and eyes-closed conditions).
- Task Familiarization: Introduce participants to the VR environment and task requirements through 10 practice trials.
- Experimental Trials:
- Present targets in random sequences across multiple trials (recommended: 60 trials per session)
- Record kinematic data including hand reaction times, trigger response times, and spatial precision
- Synchronize EEG recording with task events (target launch, participant response, feedback)
- Post-Task Assessment: Administer subjective measures of presence and cognitive load.
- Longitudinal Testing: Repeat the protocol across multiple sessions (e.g., three visits) to assess learning effects.
Data Analysis:
- Calculate performance metrics including shot scores, reaction times, and movement efficiency
- Perform spectral analysis of EEG beta band (13-30 Hz) power preceding target launch
- Analyze event-related potentials time-locked to target launch and participant response
- Correlate neural measures with behavioral performance across learning sessions
Protocol 2: Executive Function Assessment in Pediatric Populations
This protocol adapts VR methodologies for assessing executive functions in clinical pediatric populations, based on research with neurodevelopmental disorders [15].
Materials and Setup:
- Immersive VR system with appropriate safety considerations for children
- Custom VR environments targeting specific executive functions (inhibition, cognitive flexibility, working memory)
- Age-appropriate interface devices ensuring comfortable interaction
- Data logging capabilities for performance metrics
Procedure:
- Screening and Consent: Obtain informed consent from parents/guardians and assent from children. Screen for motion sickness susceptibility and visual impairments.
- Environment Orientation: Allow 5-10 minutes for participants to acclimate to the VR environment through neutral exploration.
- Executive Function Assessment:
- Inhibition Task: Virtual "go/no-go" paradigm with engaging stimuli
- Cognitive Flexibility Task: Virtual dimensional card sort task with changing rules
- Working Memory Task: Spatial navigation task with increasing memory load
- Ecological Validity Assessment: Compare VR performance with traditional neuropsychological measures and parent/teacher ratings.
- Post-Task Interview: Collect subjective feedback on engagement, presence, and task difficulty.
Data Analysis:
- Calculate accuracy rates, reaction times, and error types for each executive function domain
- Assess learning curves across task blocks and trials
- Analyze transfer effects to real-world functioning through correlational analyses with parent/teacher reports
Visualization Framework for VR Learning Processes
The following diagrams illustrate the theoretical relationships and experimental workflows central to understanding constructivist and situated learning in virtual environments.
Theoretical Integration Framework
Experimental Implementation Workflow
Research Reagent Solutions for VR Learning Studies
The following table outlines essential tools and methodologies for implementing VR learning studies grounded in constructivist and situated cognition principles.
Table 2: Essential Research Components for VR Learning Studies
| Research Component | Function | Example Applications |
|---|---|---|
| Immersive VR HMD Systems | Creates controlled yet ecologically valid environments | Motor learning, spatial navigation studies [12] [14] |
| EEG Integration Systems | Captures neural correlates of learning processes | Investigating neurophysiological mechanisms of VR learning [12] |
| Motion Tracking Systems | Quantifies kinematic movements and interactions | Precision motor control assessment, rehabilitation monitoring [12] [15] |
| Custom VR Task Environments | Implements constructivist learning principles through interactive scenarios | Executive function assessment, clinical rehabilitation [15] |
| Physiological Monitoring | Measures autonomic responses during learning | Arousal, engagement, and cognitive load assessment [14] |
| Presence and Cognitive Load Questionnaires | Assesses subjective experience and mental effort | Validating ecological validity, optimizing task difficulty [10] |
These research components enable the comprehensive investigation of learning processes within virtual environments. The integration of neural, behavioral, and subjective measures provides a multidimensional understanding of how knowledge construction occurs in situated contexts. For behavioral neuroscience research, this toolkit facilitates the exploration of fundamental questions about the relationships between brain activity, cognitive processes, and learning outcomes in environments that balance experimental control with ecological validity.
The integration of constructivist and situated cognition theories with VR technology represents a transformative approach for behavioral neuroscience research. By creating environments that support active knowledge construction within meaningful contexts, researchers can investigate learning processes with unprecedented ecological validity and experimental control. The quantitative evidence demonstrates significant improvements in learning efficiency and performance across domains, validating VR as a powerful platform for studying and enhancing human learning.
Future research directions should focus on further elucidating the neural mechanisms underlying VR-enhanced learning, optimizing individual differences in response to immersive learning environments, and developing standardized assessment protocols that leverage the unique capabilities of VR technology. As VR systems become more accessible and sophisticated, their potential to advance our understanding of learning and cognition while simultaneously enhancing real-world performance will continue to grow, offering exciting opportunities for researchers and practitioners alike.
Virtual reality (VR) has transitioned from a speculative technology to a clinically validated tool for inducing and measuring neuroplasticity—the brain's fundamental capacity to reorganize its structure, connections, and function in response to experience [16] [17]. Unlike traditional laboratory tasks, VR offers unprecedented control over multi-sensory inputs within ecologically valid, immersive environments, enabling researchers to systematically manipulate parameters to target specific neural circuits [16]. This capacity positions VR as a powerful experimental platform within behavioral neuroscience research, particularly for developing theoretical frameworks that bridge molecular mechanisms, systems-level neural reorganization, and behavioral outcomes. By creating dynamic, interactive scenarios that engage multiple sensory modalities simultaneously, VR environments foster a rich sensory experience thought to encourage synaptic reorganization and cortical remapping through mechanisms such as cross-modal plasticity [17]. For researchers and drug development professionals, VR provides not only an intervention tool but also a precise measurement platform for quantifying neuroplastic changes in response to pharmacological, behavioral, or combined therapies, offering biomarkers with high temporal resolution and functional relevance.
Core Mechanisms of VR-Induced Neuroplasticity
The therapeutic and research applications of VR are underpinned by specific, measurable mechanisms that directly engage the brain's plastic capabilities. These mechanisms work synergistically to promote adaptive neural changes.
Error-Based Learning with Real-Time Feedback
Advanced VR platforms capture real-time kinematic and performance data, creating a closed-loop system that provides immediate feedback, reinforcing correct movements and discouraging maladaptive patterns [17]. This process engages cerebellar-thalamocortical circuits and reinforcement learning pathways involving dopaminergic signaling from the ventral tegmental area to the striatum [17]. Evidence suggests such feedback facilitates the strengthening of residual pathways and accelerates recovery, with studies demonstrating improvements in balance across various neurologic conditions and forced corrective adjustments through error augmentation techniques [17].
Multisensory Integration and Cortical Reorganization
VR's capacity to concurrently engage visual, auditory, and proprioceptive systems creates a rich sensory experience that promotes cross-modal plasticity through mechanisms such as long-term potentiation (LTP) and dendritic remodeling [17]. This has been demonstrated to facilitate motor learning after stroke through reorganization from aberrant ipsilateral sensorimotor cortices to the contralateral side [17]. Environments combining auditory cues with visual stimuli in patients with traumatic brain injury and stroke with hemianopia or neglect improve compensatory scanning and attention, providing proof-of-principle for this mechanism [17].
Virtual Embodiment and Mirror Neuron Activation
VR mirror therapy leverages the mirror neuron system by reflecting movements of an intact limb, activating motor pathways of the affected side through visuomotor integration [17]. The visual reappearance of self-actions in the VR scene further stimulates activity in affected cortical areas—primarily premotor cortex and inferior parietal lobule—promoting their functional integration [17]. VR-based motor imagery exercises increase cortical mapping of areas corresponding to trained muscles and excitability of the corticospinal tract, ultimately facilitating motor relearning [17].
Reward-Mediated Learning and Cognitive Engagement
Gamification and immersive scenarios engage the brain's intrinsic reward systems, stimulating dopaminergic pathways in the ventral striatum that are crucial for motivation, reinforcement learning, and long-term potentiation [17]. The interactive, goal-oriented nature of VR enhances cognitive functions such as attention, memory, and executive control while simultaneously increasing patient adherence to therapeutic protocols—a critical factor in driving sustained neuroplastic changes [17].
Table 1: Neuroplasticity Mechanisms Targeted by VR Interventions
| Mechanism | Neural Circuits Involved | VR Application Examples | Measurable Outcomes |
|---|---|---|---|
| Error-Based Learning | Cerebellar-thalamocortical circuits, Striatal dopamine pathways | Real-time movement correction in motor rehabilitation [17] | Improved movement accuracy, Reduced compensatory patterns |
| Multisensory Integration | Superior colliculus, Parieto-insular vestibular cortex, Associative cortices | Combining visual, auditory, and balance cues for neglect rehabilitation [17] | Enhanced cross-modal processing, Improved spatial awareness |
| Mirror Neuron Activation | Premotor cortex, Inferior parietal lobule, Primary motor cortex | VR mirror therapy for stroke recovery [17] | Increased motor cortex excitability, Improved bilateral coordination |
| Reward-Mediated Learning | Ventral striatum, Prefrontal cortex, Ventral tegmental area | Gamified cognitive tasks with scoring and progression [17] | Enhanced motivation, Improved learning retention, Dopamine release markers |
Quantitative Evidence of VR-Induced Neuroplasticity
Rigorous empirical studies across neurological and psychiatric populations provide compelling evidence for VR's capacity to induce measurable neuroplastic changes at molecular, systems, and behavioral levels.
Neurophysiological Changes in Stroke Rehabilitation
A 2023 study investigating VR cognitive training in chronic stroke patients (n=30) revealed significant electrophysiological changes consistent with neuroplasticity [18]. Quantitative EEG analysis demonstrated that VR-based rehabilitation resulted in a significant increase in alpha band power (8-13 Hz) in occipital areas and elevated beta band power (13-30 Hz) in frontal regions, while no significant variations were observed in theta band power [18]. These frequency-specific changes indicate enhanced neural efficiency in sensory integration and cognitive processing networks, respectively. The experimental protocol involved 15 patients receiving neurocognitive stimulation using the VRRS Evo-4 device, while 15 controls received the same amount of conventional neurorehabilitation, with EEG recordings conducted pre- and post-intervention [18].
Multimodal Biomarkers in Adolescent Depression
A 2025 case-control study (n=115) utilizing a VR-based multimodal framework for adolescent major depressive disorder identified robust physiological biomarkers of therapeutic change [19]. Adolescents with MDD showed significantly higher EEG theta/beta ratios, reduced saccade counts, longer fixation durations, and elevated HRV LF/HF ratios (all p<.05) compared to healthy controls [19]. Both theta/beta and LF/HF ratios were significantly associated with depression severity, and a support vector machine model achieved 81.7% classification accuracy with an AUC of 0.921 based on these VR-elicted biomarkers [19]. The experimental protocol involved a 10-minute VR emotional task with a virtual agent named "Xuyu" in a magical forest environment, while synchronized EEG, eye-tracking, and HRV data were collected [19].
Table 2: Quantitative Biomarkers of Neuroplasticity in VR Studies
| Study Population | VR Intervention | Measurement Technique | Key Neuroplasticity Findings |
|---|---|---|---|
| Chronic Stroke Patients (n=30) [18] | VRRS cognitive training | Quantitative EEG | ↑ Alpha power (occipital), ↑ Beta power (frontal) |
| Adolescent MDD (n=115) [19] | 10-min emotional task with virtual agent | Multimodal (EEG+ET+HRV) | ↑ EEG theta/beta ratio, Altered oculometrics, ↑ HRV LF/HF ratio |
| Psychosis with AVHs (n=10 planned) [20] | VR + EEG neurofeedback + CBTp | EEG neurofeedback | Self-modulation of high-β activity (target) |
| Healthy Adults (Social Skills, n=114) [4] | Job interview training | Behavioral metrics | ↑ Task-specific self-efficacy, ↓ Anxiety (4-month retention) |
Integrated Neuroplasticity Pathways in VR
The following diagram illustrates the primary neuroplasticity pathways engaged during VR interventions, from multisensory input to functional recovery:
Experimental Protocols for Measuring VR-Induced Neuroplasticity
Standardized methodologies are essential for rigorous investigation of VR's effects on neural circuits. The following protocols represent current best practices in the field.
VR with Simultaneous Electrophysiology
Application: Quantifying neuroplastic changes during cognitive rehabilitation in stroke [18] and detecting biomarkers in adolescent depression [19].
Protocol Details:
- Setup: High-density EEG (64+ channels) synchronized with VR presentation system. Eye-tracking and ECG/HRV monitoring integrated for multimodal assessment [19] [18].
- Stimuli: Custom VR environments developed using frameworks like A-Frame, presenting graded cognitive-motor tasks or emotionally engaging scenarios [19].
- Procedure: Baseline recording (5 mins) → VR task period (10-30 mins) → Post-VR recording (5 mins). Task parameters adapt based on performance in closed-loop designs [18].
- Data Analysis: Time-frequency decomposition (ERD/ERS), functional connectivity metrics (coherence, phase-locking value), source localization, and correlation with behavioral measures [18].
Key Controls: Sham VR condition with matched visual stimulation but no interactive component, counterbalanced order, strict minimization of movement artifacts [18].
VR with Neurofeedback for Circuit-Specific Modulation
Application: Targeting auditory verbal hallucinations in psychosis [20] and enhancing cognitive control in various disorders.
Protocol Details:
- Setup: EEG-based neurofeedback system integrated with immersive VR environment. Real-time signal processing with <100ms latency [20].
- Neurofeedback Target: Individualized based on symptom signature (e.g., high-β power for AVHs) [20].
- Procedure: "Symptom capture" approach using individually tailored VR-based exposure exercises. Participants learn to downregulate target neural activity while progressively exposed to symptom triggers [20].
- Therapeutic Integration: Clinician-delivered CBTp concurrently with neurofeedback training (12 weekly sessions) [20].
Outcome Measures: Self-directed modulation of target neural activity, progression through VR exposure hierarchy, symptom change scores on standardized scales [20].
Experimental Workflow for VR Neuroplasticity Research
The following diagram outlines a standardized workflow for designing and executing studies investigating VR-induced neuroplasticity:
Implementing rigorous VR neuroplasticity research requires specific technological components and methodological considerations.
Table 3: Essential Research Resources for VR Neuroplasticity Studies
| Resource Category | Specific Examples | Research Function | Technical Considerations |
|---|---|---|---|
| VR Hardware Platforms | VRRS Evo-4 [18], HTC Vive, Oculus Rift | Provide immersive environments with head-mounted displays and motion tracking | Level of immersion (full vs. semi), tracking precision, compatibility with research software |
| Neurophysiology Acquisition Systems | BIOPAC MP160 [19], BrainVision, BioSemi | Synchronized recording of EEG, ECG, EDA, EMG | Integration latency, sampling rate, artifact handling capabilities |
| Software Development Frameworks | A-Frame [19], Unity3D, Unreal Engine | Creation of custom VR environments with precise experimental control | Scripting capabilities, compatibility with research equipment, community support |
| Data Analysis Toolboxes | EEGLAB, FieldTrip, Custom MATLAB/Python scripts | Processing of neural signals, behavioral metrics, and their relationships | Support for multimodal data fusion, statistical analysis, machine learning pipelines |
| Experimental Paradigms | VR mirror therapy [17], Social evaluation tasks [4], Emotional provocation [19] | Standardized protocols for inducing and measuring targeted neural processes | Psychometric validation, sensitivity to change, translational relevance |
VR represents a transformative tool for investigating and harnessing neuroplasticity within theoretical frameworks for behavioral neuroscience research. By enabling precise control over multi-sensory inputs within ecologically valid environments, VR allows researchers to target specific neural circuits and measure resulting plastic changes with high temporal resolution [16] [17]. The mechanisms outlined—error-based learning with real-time feedback, multisensory integration, virtual embodiment, and reward-mediated learning—provide a foundation for understanding how VR interventions produce measurable neuroplastic changes at molecular, systems, and behavioral levels [17].
Future research directions should focus on optimizing immersion levels for specific clinical populations [21], standardizing VR-based biomarkers for drug development trials [11], and developing closed-loop systems that automatically adapt VR parameters in real-time based on neural activity [16] [20]. For the pharmaceutical industry, VR platforms offer promising endpoints for clinical trials, potentially detecting therapeutic effects with greater sensitivity than conventional behavioral measures [11] [18]. As VR technology continues to evolve, its integration with other emerging technologies like AI-powered virtual humans [22] and wearable biosensors [19] will further enhance its utility for promoting adaptive neuroplasticity across a wide spectrum of neurological and psychiatric conditions.
From Theory to Practice: VR Methodologies for Assessment and Intervention
Virtual Reality Exposure Therapy (VRET) represents a paradigm shift in behavioral neuroscience and therapeutic intervention, grounded firmly in the principles of extinction learning. As an innovative form of exposure therapy, VRET utilizes immersive virtual environments to systematically and safely expose individuals to feared stimuli, facilitating the formation of new, non-threatening associations through inhibitory learning processes [23] [2].
The theoretical foundation of VRET rests upon its capacity to create controlled, repeatable, and customizable environments that engage the same neurobiological mechanisms as real-world exposure while offering superior experimental control for research purposes [23]. By leveraging advanced immersive technology, VRET enables researchers and clinicians to target the precise neural circuits involved in fear acquisition and extinction, particularly within amygdala-prefrontal cortex interactions [2] [24]. This technical guide explores the mechanistic basis of VRET within the context of contemporary extinction learning theories and their implications for behavioral neuroscience research and therapeutic development.
Theoretical Foundations: Extinction Learning Principles
The Mechanisms of Extinction Learning
Extinction learning involves the gradual reduction of conditioned fear responses through repeated, non-reinforced exposure to feared stimuli, resulting in the formation of new safety memories that compete with original fear memories [2]. Within immersive VR environments, this process occurs through several interconnected mechanisms:
Memory Reconsolidation Interference: VRET creates opportunities to reactivate fear memories within virtual environments and introduce mismatching information (safety cues), potentially altering the original fear memory trace upon reconsolidation [2].
Inhibitory Learning Development: The brain creates new, inhibitory associations that compete with original fear associations through repeated virtual exposure without adverse consequences, engaging prefrontal regulation of amygdala activity [2] [24].
Contextual Encoding: VR environments provide rich contextual cues that enhance the encoding and retrieval of extinction memories, with the virtual context serving as a retrieval cue for safety learning [23].
Embodied Simulation: According to neuroscience research, the brain maintains embodied simulations of the body in the world to represent and predict actions, concepts, and emotions [2]. VR works through a similar mechanism, providing users with simulated experiences that the brain processes using the same neural machinery as real experiences, thereby facilitating genuine extinction learning.
Neurobiological Substrates of VRET
Research utilizing the SONIA VR system for exploring anxiety-related brain networks has identified key neural structures engaged during virtual exposure, including the amygdala, hippocampus, striatum, medial prefrontal cortex (mPFC), hypothalamus, and the bed nucleus of the stria terminalis (BNST) [24]. These structures form interconnected subsystems regulating cognitive control, fear conditioning, uncertainty anticipation, motivation processing, and stress regulation – all of which are modulated during VRET through targeted virtual experiences [24].
Functional imaging studies reveal that successful extinction learning during VRET correlates with increased prefrontal activation coupled with diminished amygdala responsiveness, reflecting the shift from emotional reactivity to cognitive regulation [2]. The immersive nature of VR enhances engagement of these neural circuits by providing multisensory input that creates strong feelings of presence, thereby increasing the ecological validity of the extinction learning experience compared to imaginal exposure [23] [2].
VRET Efficacy: Comparative Evidence and Mechanisms
Clinical Efficacy Across Disorders
Table 1: VRET Efficacy Across Anxiety Disorders
| Disorder | Effect Size vs. Control | Comparison to In-Vivo Exposure | Long-Term Maintenance | Key Supporting Studies |
|---|---|---|---|---|
| Specific Phobias | Large effects (g > 0.80) | Equivalent efficacy | Maintained at follow-up | Systematic reviews [25] [2] |
| Social Anxiety Disorder | Moderate to large effects | Comparable outcomes | 3-12 month persistence | Meta-analysis [25] |
| PTSD | Significant symptom reduction | Non-inferiority demonstrated | Generalization to real world | Multiple RCTs [23] [2] |
| Panic Disorder | Clinical improvement | Similar mechanisms | Reduced relapse | Neuroimaging studies [2] |
Recent meta-analytic evidence demonstrates that VRET generates positive clinical outcomes in the treatment of specific phobias and social anxiety disorders that are comparable to in-vivo exposure therapy (IVET), with both approaches reporting moderate effect sizes [25]. The analysis suggested that both are equally effective at reducing social phobia and anxiety symptoms, though the limited literature makes it difficult to identify which approach is optimal for specific patient subgroups [25].
Therapeutic Mechanisms and Active Components
Table 2: Therapeutic Mechanisms in VRET
| Mechanism | VRET Application | Measurable Outcomes | Research Support |
|---|---|---|---|
| Emotional Engagement | Presence metrics, physiological arousal | Stronger extinction with higher presence | Psychophysiological studies [2] |
| Stimulus Control | Graduated exposure hierarchies | Systematic fear reduction | Clinical trials [23] [25] |
| Contextual Manipulation | Multiple virtual environments | Enhanced extinction generalization | Fear renewal paradigms [23] |
| Cognitive Reappraisal | Virtual behavioral experiments | Changed threat expectancies | Self-report measures [2] |
| Inhibitory Learning | Violation of fear expectations | Development of competing associations | Learning curves [2] [25] |
The effectiveness of VRET is mediated through multiple active components, with presence (the subjective experience of being in the virtual environment) and emotional engagement serving as crucial mediators of therapeutic outcome [2]. Research indicates that the immersive quality of VR "hijacks" the user's auditory, visual, and proprioception senses, acting as a distraction that limits the ability to process stimuli from the real world and creating potent conditions for new learning [26].
Experimental Protocols and Methodologies
Standardized VRET Protocol for Anxiety Disorders
A typical VRET protocol for anxiety disorders involves multiple structured sessions incorporating the following components:
Psychoeducation (Session 1): Explanation of the extinction learning model, rationale for virtual exposure, and introduction to the VR equipment.
Fear Hierarchy Development (Session 1): Collaborative creation of individualized fear hierarchy with subjective units of distress (SUDs) ratings for virtual scenarios.
Graduated Exposure (Sessions 2-8): Systematic progression through fear hierarchy, beginning with moderately anxiety-provoking scenarios and advancing to more challenging situations.
Within-Session Habituation: Continued exposure to each virtual scenario until SUDs decrease by 50% or more.
Between-Session Practice: Repeated practice of successfully completed exposures to strengthen extinction learning.
Relapse Prevention (Final Session): Review of progress, anticipation of future challenges, and development of maintenance plan.
Session duration typically ranges from 45-90 minutes, with the number of sessions varying based on disorder complexity (specific phobias: 1-5 sessions; PTSD: 8-15 sessions) [23] [25].
Specialized Protocol for PTSD Treatment
VRET for PTSD requires additional considerations for trauma memory processing:
Trauma Narrative Development: Detailed assessment of trauma memories to create authentic virtual scenarios.
Therapeutic Alliance Strengthening: Enhanced focus on therapist-patient rapport given the sensitivity of trauma material.
Dual Attention Components: Incorporation of grounding elements within the virtual environment to maintain connection to present safety.
Emotional Processing Measures: Regular assessment of trauma-related emotions and cognitions throughout exposure.
Meaning-Making Integration: Discussion of changed perspectives regarding trauma identity and post-traumatic growth [23].
Research demonstrates that VRET for PTSD is particularly effective when it allows for emotional engagement with trauma memories while maintaining awareness of current safety, facilitating corrective emotional experiences that modify the fear structure [23] [2].
Technical Implementation and System Requirements
Immersive Technology Specifications
Modern VRET systems utilize a range of technological components to create convincing therapeutic environments:
Head-Mounted Displays (HMDs): Modern HMDs like the Oculus Rift or HTC Vive provide high-resolution displays (≥1080x1200 per eye), wide field of view (≥100 degrees), and precise head tracking (6 degrees of freedom) to create immersive experiences [23] [26]. These HMDs are relatively easy to use and program, with good display quality and affordable prices, making them suitable for both research and clinical applications [26].
Interaction Devices: Hand controllers, data gloves, or gesture recognition systems enable natural interaction with virtual environments, enhancing agency and presence.
Physiological Monitoring: Integrated biosensors (heart rate, skin conductance, respiration) provide objective measures of emotional arousal during exposure.
Software Platforms: Game engines like Unity or Unreal Engine enable creation of customizable virtual environments with realistic graphics and physics [24].
The multi-scale interaction paradigm implemented in systems like SONIA allows users to manipulate both enlarged environmental contexts and detailed anatomical models, facilitating both situational exposure and psychoeducation about neurophysiological responses [24].
Research Reagent Solutions for VRET Studies
Table 3: Essential Research Materials for VRET Experiments
| Research Component | Function | Example Implementations |
|---|---|---|
| Standardized VR Environments | Provide consistent exposure stimuli across participants | Virtual public speaking auditorium, height scenarios, flight simulations [23] |
| Presence Questionnaires | Measure subjective immersion in virtual environments | Igroup Presence Questionnaire (IPQ), Slater-Usoh-Steed Questionnaire [26] |
| Fear Response Measures | Quantify anxiety and fear during exposure | Subjective Units of Distress (SUDs), Fear of Negative Evaluation Scale [25] |
| Physiological Recording | Objective assessment of arousal states | Skin conductance response, heart rate variability, respiratory rate [2] |
| Cognitive Assessment | Measure changes in threat-related cognitions | Dysfunctional Attitudes Scale, Thought Listing Procedures [2] |
| Neural Activity Monitoring | Identify neurobiological correlates of extinction | fMRI, EEG during or post-VRET [2] [24] |
Visualization: Extinction Learning Mechanisms in VRET
The following diagram illustrates the primary psychological and neurobiological mechanisms through which VRET facilitates extinction learning:
VRET Extinction Learning Pathway:
This visualization outlines the proposed pathway through which Virtual Reality Exposure Therapy facilitates extinction learning, connecting key psychological mechanisms with their underlying neural substrates and resulting behavioral outcomes.
Future Directions and Research Applications
Emerging Research Paradigms
The future of VRET research involves several promising directions that leverage advancing technology to enhance extinction learning:
Personalized Virtual Environments: Creation of patient-specific scenarios using photogrammetry and 3D scanning to increase relevance and emotional engagement.
Real-Time Biofeedback: Integration of physiological data to dynamically adjust virtual environments based on arousal states.
Augmented Reality Exposure: Blending of virtual elements with real environments to enhance generalization of extinction learning.
Neuromodulation Integration: Combination of VRET with non-invasive brain stimulation (tDCS, TMS) to potentiate extinction learning [2] [27].
Digital Twin Technology: Development of highly customized digital replicas of patients to model individual responses and optimize treatment parameters [27].
Implications for Drug Development
VRET protocols offer valuable paradigms for evaluating novel pharmacological agents that target learning and memory processes:
Cognitive Enhancers: VRET provides a controlled platform for testing compounds designed to facilitate extinction learning (e.g., D-cycloserine, glucocorticoids).
Fear Memory Modulators: The reconsolidation window during VRET creates opportunities to test compounds that disrupt maladaptive fear memories.
Translational Biomarkers: VRET responses can serve as functional biomarkers for target engagement in clinical trials of neurotherapeutic agents [2].
The combination of VRET with pharmacological approaches represents a promising frontier for developing enhanced treatments for anxiety, trauma, and stress-related disorders, potentially offering synergistic effects that produce more robust and durable extinction learning [2] [26].
Virtual Reality Exposure Therapy represents a theoretically grounded and empirically validated approach that leverages the core mechanisms of extinction learning to address maladaptive fear and anxiety. Its foundation in embodied simulation theory – which posits that VR shares with the brain the same basic mechanism of creating predictive models of reality – provides a compelling explanation for its efficacy [2]. By engaging both the psychological processes of emotional engagement and cognitive reappraisal, along with the neurobiological substrates of fear extinction, VRET creates optimal conditions for inhibitory learning and the development of new safety associations.
For researchers in behavioral neuroscience and drug development, VRET offers a highly controlled, precisely measurable, and ethically advantageous paradigm for investigating the mechanisms of fear extinction and testing novel therapeutic interventions. The continuing evolution of immersive technology promises to further enhance the ecological validity, accessibility, and personalization of VRET, solidifying its position as an indispensable tool in the future of mental health research and treatment.
Virtual reality (VR) technology is revolutionizing the study and treatment of addiction by providing unprecedented methodological rigor and ecological validity. By creating controlled, immersive environments that simulate real-world contexts, VR enables researchers to probe the complex mechanisms of cue reactivity and craving—core phenomena in substance use disorders (SUDs). Cue reactivity describes the patterned response to stimuli associated with substance use, while craving represents the subjective experience of urge or desire for the substance [28]. The DSM-5 recognizes craving as a crucial diagnostic criterion for SUDs and a significant predictor of relapse [28]. Traditional laboratory methods for studying craving, such as static images or videos, lack the immersive quality necessary to trigger robust, real-world craving responses. VR technology addresses this limitation by enabling the construction of complex, multi-sensory environments that incorporate both proximal cues (e.g., drugs, paraphernalia) and contextual cues (e.g., social settings, environments) that are known to trigger craving in daily life [28] [29]. This technical guide examines the theoretical frameworks, experimental paradigms, and practical applications of VR for investigating cue reactivity and craving within behavioral neuroscience research on addiction.
Theoretical Frameworks for VR in Addiction Neuroscience
Classical Conditioning and Extinction Learning
The application of VR in addiction research is predominantly grounded in classical conditioning theory. Through repeated pairings, substance-related stimuli (conditioned stimuli - CS) become associated with the drug's effects (unconditioned stimuli - UCS), eventually eliciting conditioned responses (CR) including craving and physiological reactions [28]. VR-based cue exposure therapy (CET) leverages this framework through extinction learning, where repeated presentation of drug cues without actual substance consumption weakens the conditioned response [30].
From a neurocognitive perspective, addiction represents an imbalance between reflexive (impulsive) and reflective (regulatory) systems [28]. The reflexive system, associated with limbic and striatal regions, drives automatic drug-seeking behavior, while the reflective system, dependent on prefrontal cortical areas, provides cognitive control. VR paradigms uniquely engage both systems simultaneously by presenting emotionally salient cues while requiring active behavioral responses, thus providing a window into their dynamic interaction.
Ecological Validity and Presence
A primary theoretical advantage of VR is its ability to enhance ecological validity—the degree to which experimental findings generalize to real-world settings [28] [14]. Traditional craving induction methods suffer from limited contextual cues, whereas VR environments can simulate complex real-world scenarios such as bars, parties, or social gatherings where substance use typically occurs [28] [31].
The effectiveness of VR in eliciting genuine craving responses depends critically on presence—the subjective experience of "being there" in the virtual environment [32]. Presence comprises both place illusion (the sensation of being in the virtual space) and plausibility (the illusion that events in the space are actually happening) [32]. Higher levels of presence correlate with stronger craving responses, making it a crucial psychological mechanism in VR-based addiction research [31].
Quantitative Evidence: Efficacy of VR in Craving Induction and Reduction
Table 1: Efficacy of VR-Based Interventions Across Substance Use Disorders
| Substance | Study Design | Key Findings | Effect Size/Statistics | Citation |
|---|---|---|---|---|
| Methamphetamine | RCT (N=89 men with MUD); CET vs CETA vs NS | Significant reduction in tonic craving post-intervention | CET: p=0.001; CETA: p=0.010; NS: p=0.217 | [30] |
| Methamphetamine | Within-subjects (N=150 men with MUD) | Craving in drug-use scene significantly higher than neutral scenes | p < 0.001 | [29] |
| Alcohol | Single-arm (N=21 AD patients) | Craving significantly higher during and after VR-CE vs before | χ²(2, N=21) = 33.8, p < 0.001 | [31] |
| Various (Review) | Systematic review (7 studies) | VR effective at reducing substance use and cravings in most studies | Mixed results for mood/anxiety outcomes | [33] |
Table 2: Impact of VR on Cognitive and Secondary Outcomes in SUD
| Outcome Domain | Substance | Intervention | Key Findings | Citation |
|---|---|---|---|---|
| Executive Functioning | Mixed SUD | VR cognitive training (6 weeks) | Significant improvement in experimental group vs control | [34] |
| Drug Refusal Self-Efficacy | Methamphetamine | VR CETA | Significant improvement vs neutral scenes group | [30] |
| Anxiety | Methamphetamine | VR CET | Significant reduction vs neutral scenes group | [30] |
| Treatment Dropout | Mixed SUD | VR cognitive training + TAU | Lower dropout in experimental group (8% vs 27%) | [34] |
| Global Memory | Mixed SUD | VR cognitive training | Significant improvement in visual, auditory, immediate, and delayed recall | [34] |
Experimental Protocols and Methodologies
VR Cue Exposure Paradigm for Methamphetamine Use Disorder
A comprehensive VR cue exposure paradigm for methamphetamine use disorder (MUD) was developed and validated across multiple studies [30] [29]. The protocol employs a within-subjects design with the following components:
Participant Selection:
- Sample: 150 male participants meeting DSM-5 criteria for MUD [29]
- Inclusion Criteria: Age 18-55, MA use ≥ twice monthly over past two years, minimum six consecutive months of use prior to admission, normal or corrected vision [29]
- Exclusion Criteria: Polysubstance abuse, personal or family history of psychiatric disorders, serious physical illnesses, conditions requiring ongoing medication [29]
VR Environment Development: The paradigm includes five distinct scenes presented in sequence:
- Resting scene (1 minute): Features guiding audio and system logo interface
- Neutral scene 1 (4 minutes): Underwater visuals with ambient water sounds
- MA paraphernalia scene (4 minutes): Displays eight types of MA and related tools (e.g., glass pipes) without audio
- Drug-use scene (4 minutes): Depicts social context of MA use (e.g., two men and two women using MA while playing cards in a game room) with professional actors, dynamic contextual cues, special effects, and audio including prompt, "Do you want a hit?"
- Neutral scene 2 (4 minutes): Elephant-walking grassland scene with natural sounds [30] [29]
Assessment Protocol:
- Tonic Craving: Measured using Visual Analogue Scale (VAS) ranging from 1 (no craving) to 10 (strongest craving) during withdrawal period
- Cue-Induced Craving: Assessed using VAS within VR environment after exposure to each scene type
- Clinical Measures: Methamphetamine Use Disorder Severity Scale (MUDSS), Fagerström Test for Nicotine Dependence (FTND), Alcohol Use Disorder Identification Test (AUDIT) [29]
Key Findings:
- Craving in drug-use scene was significantly higher than in neutral and paraphernalia scenes (p < 0.001)
- Cue-induced craving was significantly higher than pre-exposure withdrawal craving (p < 0.05)
- Withdrawal craving scores positively correlated with craving scores in all three VR scenarios (p < 0.01) [29]
VR-Based Cue Exposure with Aversion Therapy
A randomized controlled trial implemented an advanced protocol combining cue exposure with aversion therapy for MUD [30]:
Study Design:
- Participants: 89 men with MUD randomly assigned to CET (n=30), CETA (n=29), or neutral scenes (NS, n=30)
- Intervention Duration: 16 sessions over 8 weeks
CETA Protocol:
- Cue Exposure Component: Similar to the basic paradigm described above
- Aversion Component: Following exposure to drug cues, participants were exposed to aversive stimuli (e.g., unpleasant odors, images of negative consequences) to create negative associations with substance-related cues
- Theoretical Basis: Counter-conditioning approach creating opposing associations to weaken drug cue salience [30]
Outcome Measures:
- Primary Outcomes: Tonic craving and cue-induced craving
- Secondary Outcomes: Attentional bias, rehabilitation confidence, drug refusal self-efficacy, anxiety (GAD-7), and depression (PHQ-9)
Key Findings:
- Both CET and CETA groups demonstrated significant reductions in tonic craving post-intervention (CET: p=0.001; CETA: p=0.010)
- CET group showed significantly lower post-intervention tonic craving compared to NS group (p=0.047)
- CETA group showed significantly improved drug refusal self-efficacy compared to baseline (p=0.001) and NS group (p=0.018)
- CET group demonstrated reduced anxiety compared to NS group (p=0.014) [30]
Visualization of Neurobiological Mechanisms and Workflows
Diagram 1: Neurobiological Pathways and Experimental Workflow of VR-Induced Craving
The Researcher's Toolkit: Essential Methodological Components
Table 3: Research Reagent Solutions for VR Addiction Studies
| Component Category | Specific Tools/Measures | Function/Purpose | Example Implementation |
|---|---|---|---|
| VR Hardware Platforms | Head-Mounted Displays (HMDs) with tracking systems | Creates immersive 3D environments that respond to user movement | HTC Vive, Oculus Rift [32] |
| Craving Assessment Tools | Visual Analogue Scale (VAS) | Measures subjective craving intensity on continuous scale | 1-10 scale from "no craving" to "strongest craving" [30] [29] |
| Craving Assessment Tools | Alcohol Urge Questionnaire (AUQ) / Substance-specific urge questionnaires | Multi-dimensional assessment of craving experience | Used in alcohol VR-CE studies [31] |
| Presence Measures | Igroup Presence Questionnaire (IPQ) | Quantifies sense of "being there" in virtual environment | Subscales: spatial presence, involvement, realness [31] |
| Tolerability Measures | Simulator Sickness Questionnaire (SSQ) | Assesses cybersickness side effects | Total score indicates severity of discomfort [31] |
| Clinical Assessment | MUDSS, AUDIT, FTND | Measures disorder severity and dependence levels | MUDSS: 18 items across 4 dimensions [30] [29] |
| Affective Measures | PANAS, GAD-7, PHQ-9 | Assesses emotional states, anxiety, depression | Pre-post intervention comparison [30] [31] |
| VR Scenario Elements | Proximal cues (substance, paraphernalia) | Direct substance-related stimuli | MA pipes, alcoholic beverages, cigarettes [30] [29] |
| VR Scenario Elements | Contextual cues (social, environmental) | Situational and social context of use | Bars, parties, social gatherings [28] [31] |
| Therapeutic Components | Aversive stimuli (for CETA) | Creates negative associations with drug cues | Unpleasant odors, negative consequence images [30] |
VR technology has established itself as a powerful methodological platform for investigating cue reactivity and craving in addiction neuroscience. By bridging the gap between laboratory control and ecological validity, VR paradigms enable researchers to study craving mechanisms with unprecedented precision and real-world relevance. The evidence demonstrates that VR can successfully induce craving across multiple substances, including methamphetamine, alcohol, and nicotine, and shows promise as a therapeutic tool when combined with exposure-based and cognitive interventions.
Future research should focus on several key areas: establishing standardized VR protocols across different substance classes, investigating long-term treatment effects, exploring individual differences in VR responsiveness, and integrating neuroimaging to elucidate brain mechanisms underlying VR-induced craving. Furthermore, as VR technology becomes more accessible and sophisticated, opportunities will expand for developing personalized virtual environments that target individual-specific triggers and contexts. These advances will deepen our theoretical understanding of addiction mechanisms while contributing to more effective, neuroscience-informed interventions for substance use disorders.
Virtual Embodiment for Body Image and Eating Disorders
Virtual Reality (VR) is emerging as a transformative tool in behavioral neuroscience, particularly for investigating and treating body image disturbances and Eating Disorders (EDs). Its power lies in its ability to create controlled, immersive environments that enable the study of human behavior with enhanced ecological validity and the collection of rich behavioral data often inaccessible in traditional lab settings [14]. This technical guide details how the paradigm of virtual embodiment—the illusory perception of a virtual body as one's own—is being leveraged within specific theoretical frameworks to address the core pathologies of EDs.
A primary neuroscientific theory underpinning this work is the Allocentric Lock Theory [35]. This theory posits that individuals with EDs are "locked" into an allocentric (third-person) representation of their body, which is often negative and stored in long-term memory. This stored representation is resistant to updating from egocentric (first-person) perceptual information, such as direct sight or touch [35]. VR interventions that induce a strong sense of embodiment in a virtual body can potentially create a mismatch strong enough to "unlock" and update this maladaptive allocentric memory.
Core VR Experimental Protocols and Methodologies
This section outlines the primary experimental and therapeutic protocols that utilize virtual embodiment for EDs, detailing the specific methodologies and their underlying mechanisms.
Virtual Reality Body Exposure Therapy (VR-BET)
Objective: To reduce body-related anxiety, specifically the Fear of Gaining Weight (FGW), and to address Body Image Disturbance (BID) by allowing patients to confront their virtual body in a controlled, therapeutic context [35].
Typical Protocol:
- Setup: A head-mounted display (HMD) is used to immerse the patient in a virtual environment. A virtual body is rendered in real-time from a 3D model, often mapped to the patient's approximate body shape or based on a pre-scanned avatar.
- Procedure: In a typical session, the patient is embodied in this virtual body and views it from a first-person perspective. The therapist guides the exposure, which can be graded:
- Initial sessions may involve exposure to a virtual body with neutral proportions.
- Subsequent sessions may gradually alter the virtual body's size (e.g., towards a healthier BMI) based on therapeutic goals [35].
- Therapeutic Actions: Patients are guided to describe their virtual body and their emotional responses. The therapist uses cognitive-behavioral techniques to challenge distortions and reduce avoidance behaviors.
- Context: This protocol is typically used as an adjunct to standard treatment for Anorexia Nervosa (AN) [35].
Body Swapping and Body Illusion Paradigms
Objective: To directly alter the perceptual and affective components of body image by inducing ownership over a virtual body of a different size or shape [35].
Detailed Methodology:
- Embodiment Induction: The experiment uses multisensory correlated stimuli to induce the body ownership illusion.
- Synchronous Visuotactile Stimulation: The participant sees the virtual body being touched (e.g., on the arm or abdomen) while simultaneously receiving the same tactile stimulus on their own corresponding body part.
- Synchronous Visuomotor Stimulation: The virtual body's movements are perfectly synchronized with the participant's own movements tracked in real-time [35].
- Experimental Manipulation: Participants are embodied in a virtual body that differs from their own. Studies have used:
- A body with a healthy BMI for patients with AN.
- A body with a thinner or larger virtual body to study and modify body perception in various ED subtypes [35].
- Measurement: The strength of the embodiment illusion is quantified using standardized questionnaires (e.g., examining ownership, agency, and location). Body perception changes are measured pre- and post-embodiment using:
- Body size estimation tasks (e.g., using a virtual body adjustment method).
- Self-report measures of body satisfaction and anxiety [35].
A key finding from this line of research suggests that dissatisfaction in AN may stem less from a perceptual overestimation of body size and more from a dysfunctional desire for a thinner body, as both clinical and healthy control samples have been shown to accurately estimate their actual body dimensions [35].
VR Cue Exposure for Craving and Anxiety
Objective: To extinguish conditioned craving and anxiety responses to food-related cues in Bulimia Nervosa (BN) and Binge Eating Disorder (BED) by exposing patients to virtual food and eating scenarios in a safe, controlled environment [35].
Protocol Details:
- Virtual Environment: Patients are immersed in highly realistic virtual environments rich with food cues, such as a kitchen, restaurant, or supermarket.
- Exposure Hierarchy: The exposure is structured according to the patient's individual fear and craving hierarchy, starting with less provocative scenarios (e.g., looking at a wrapped candy bar) and progressing to more challenging ones (e.g., being surrounded by a buffet of binge foods) [35].
- Response Prevention: Patients are guided to experience the craving and anxiety without engaging in binge eating or compensatory behaviors, allowing for habituation and the extinction of the conditioned response.
- Efficacy: This approach has proven effective for patients with BN and BED who have not responded adequately to first-line treatments like standard Cognitive Behavioral Therapy (CBT) [35].
Attentional Bias Modification Training (ABMT) in VR
Objective: To rectify attention biases in EDs, where patients selectively attend to weight-related or negatively perceived body parts, using VR combined with Eye Tracking (ET) technology [35].
Methodology:
- Setup: Participants wear an HMD integrated with an eye tracker while embodied in a virtual body.
- Task: The system monitors the participant's gaze in real-time as they observe their virtual body.
- Feedback & Training: The protocol provides feedback or trains the participant to more evenly distribute their attention across their entire body, rather than fixating on specific "feared" areas. For example, one study demonstrated that a single session of VR-based ABMT could help balance attention devoted to weight-related and non-weight-related body areas in AN [35].
Table 1: Summary of Key Virtual Embodiment Protocols for Eating Disorders
| Protocol Name | Primary Disorder Target | Core Objective | Key Technical Components |
|---|---|---|---|
| VR Body Exposure Therapy (VR-BET) | Anorexia Nervosa (AN) | Reduce fear of weight gain & body image disturbance | HMD, Real-time body rendering, Therapist-guided graded exposure |
| Body Swapping/Illusions | AN, BN, BED | Alter perceptual & affective body image | HMD, Synchronous visuotactile/motor stimulation, Virtual bodies of varying sizes |
| VR Cue Exposure | BN, Binge Eating Disorder (BED) | Extinguish food craving & anxiety | Food-rich virtual environments, Individualized exposure hierarchy, Response prevention |
| ABMT with Eye Tracking | AN | Modify attentional bias to body parts | HMD with integrated eye tracking, Real-time gaze monitoring & feedback |
Quantitative Data and Efficacy Outcomes
Research into virtual embodiment has yielded promising quantitative results, though the field continues to evolve with ongoing clinical trials.
Table 2: Selected Quantitative Findings from VR Studies in Eating Disorders
| Study Focus / Intervention | Reported Outcome Measures | Key Findings / Efficacy |
|---|---|---|
| VR Body Exposure Therapy [35] | Reduction in Fear of Gaining Weight (FGW) | Effective as an adjunct to standard AN treatment for addressing FGW. |
| Body Swapping & Embodiment [35] | Accuracy of body size estimation; Body dissatisfaction | AN patients and healthy controls accurately estimated their body dimensions; suggests dissatisfaction may be driven by desire for thinness rather than perceptual distortion. |
| VR Cue Exposure Therapy [35] | Reduction in food craving and anxiety | More effective than Cognitive Behavioral Therapy (CBT) for some patients with BN and BED, particularly those who did not respond to first-level CBT. |
| ABMT with VR & Eye Tracking [35] | Attention balance to body areas | A single session helped balance attention devoted to weight-related and non-weight-related body areas in AN. |
| VR-CBT for Performance Anxiety [36] | Reduction in state anxiety (STAI-Y1) | A protocol (NCT06639841) predicts VR-CBT will reduce anxiety "very quickly." (Study planned: 2025-2026). |
The Scientist's Toolkit: Essential Research Reagents and Materials
Implementing virtual embodiment research requires a suite of specialized hardware and software.
Table 3: Key Research Reagent Solutions for Virtual Embodiment Studies
| Item / Technology | Function in Research | Specific Examples / Notes |
|---|---|---|
| Head-Mounted Display (HMD) | Provides the immersive visual and auditory experience; the primary interface for the virtual environment. | Fully immersive, room-scale HMDs (e.g., Meta Quest, HTC Vive, Valve Index). |
| Motion Tracking System | Tracks the user's head, hand, and body movements in real-time to update the virtual perspective and enable visuomotor correlation. | Outside-in (base stations) or inside-out (camera-based) tracking systems. |
| 3D Body Modeling Software | Creates the virtual avatars or bodies used in embodiment and exposure protocols. | Software for creating realistic, customizable, and morphable 3D human models. |
| Eye Tracking Integration | Monitors and records gaze patterns within the HMD; critical for Attentional Bias Modification Training (ABMT). | HMDs with built-in infrared eye-tracking cameras (e.g., Varjo, HTC Vive Pro Eye). |
| Haptic Feedback Devices | Provides synchronized tactile stimulation to induce and enhance the sense of embodiment (e.g., for visuotactile correlation). | Vibrotactile actuators, data gloves, or specialized force-feedback devices. |
| Biometric Sensors | Collects physiological data (e.g., Heart Rate, GSR) as objective measures of anxiety, craving, and emotional arousal during exposure. | Integrated or external sensors for electrodermal activity, heart rate, and EEG. |
Visualizing Workflows and Theoretical Models
The following diagrams, generated with Graphviz DOT language, illustrate the core logical relationships and experimental workflows described in this guide.
Allocentric Lock Theory and VR Intervention
This diagram illustrates the neuroscientific theory explaining the therapeutic action of virtual embodiment.
Virtual Embodiment Experimental Workflow
This diagram outlines a generalized protocol for conducting a body swapping experiment.
VR Intervention Modalities for Eating Disorders
This diagram provides a high-level overview of how different VR techniques map to specific symptom targets in eating disorders.
VR-Enhanced Cognitive Behavioral Therapy (VR-CBT) and Cognitive Rehabilitation
Virtual Reality-Enhanced Cognitive Behavioral Therapy (VR-CBT) and cognitive rehabilitation represent a paradigm shift in non-pharmacological interventions for neuropsychiatric disorders and cognitive impairment. By combining immersive, interactive digital environments with evidence-based psychological principles and cognitive training protocols, these approaches offer unprecedented opportunities for controlled, engaging, and ecologically valid therapeutic experiences. This technical guide examines the theoretical frameworks, empirical evidence, and methodological considerations for VR applications in behavioral neuroscience research, providing researchers and drug development professionals with a comprehensive resource for integrating these technologies into experimental and clinical paradigms.
The integration of VR into cognitive and behavioral interventions addresses fundamental limitations of traditional approaches by enabling precise control over stimulus presentation, creating standardized yet customizable environments, and facilitating real-time measurement of behavioral and physiological responses. These capabilities make VR particularly valuable for establishing robust, reproducible experimental protocols in neuroscience research and clinical trials.
Theoretical Frameworks and Mechanisms of Action
Neurocognitive Foundations
VR-enhanced interventions operate through multiple synergistic mechanisms that target distinct neural systems. The immersive nature of VR environments creates a strong sense of presence, which enhances emotional engagement and facilitates more potent activation of neural circuits relevant to therapeutic change [37]. This presence enables emotional engagement at a neurobiological level, particularly engaging limbic structures including the amygdala and hippocampal formation during exposure-based protocols [38].
From a cognitive perspective, VR facilitates context-dependent learning by creating environmental contexts that enhance encoding specificity and memory retrieval. The technology enables targeted cognitive activation of specific domains through carefully designed virtual scenarios that challenge executive functions, memory systems, and attentional networks in an integrated manner [39]. Furthermore, the enhanced ecological validity of VR tasks compared to traditional laboratory measures improves the translation of cognitive gains to real-world functioning, addressing a critical limitation in many existing cognitive rehabilitation approaches [40].
Learning and Neuroplasticity Mechanisms
VR environments optimally leverage principles of experience-dependent neuroplasticity through several key mechanisms:
- Errorless learning adaptation: VR allows for gradual progression of task difficulty based on individual performance thresholds, maintaining users within their zone of proximal development [34]
- Multisensory integration: Simultaneous visual, auditory, and sometimes haptic stimulation engages distributed neural networks, potentially enhancing synaptic modification and consolidation [41]
- Repetition with variation: Virtual scenarios can maintain core cognitive demands while varying contextual elements to support generalization of learning [40]
- Reinforcement learning loops: Immediate performance feedback in VR environments strengthens reward prediction error signaling in cortico-striatal circuits [37]
Quantitative Efficacy Data Across Disorders
Cognitive Rehabilitation Outcomes
Table 1: Effect Sizes of VR-Based Interventions on Cognitive Function Across Disorders
| Disorder/Condition | Primary Cognitive Domains | Effect Size (SMD/ Hedges' g) | 95% CI | Number of Studies |
|---|---|---|---|---|
| Mild Cognitive Impairment | Global cognition | 0.60 | [0.29, 0.90] | 11 [39] |
| Neuropsychiatric Disorders | Global cognition | 0.67 | [0.33, 1.01] | 21 [42] |
| Schizophrenia | Cognitive functions | 0.92 | [0.22, 1.62] | Subset of [42] |
| Traumatic Brain Injury | Global cognition | 0.64 | [0.44, 0.85] | 16 [43] |
| Substance Use Disorders | Executive functions | 0.75* | [0.33, 1.17] | 1 [34] |
*Value represents significant time × group interaction F(1,75)=20.05, p<0.001
Table 2: Comparative Efficacy of VR Intervention Types
| Intervention Type | Effect Size (SMD) | 95% CI | Key Characteristics | Optimal Applications |
|---|---|---|---|---|
| VR-based games | 0.68 | [0.12, 1.24] | Game-inspired design, intrinsic motivation | Mild Cognitive Impairment [39] |
| VR cognitive training | 0.52 | [0.15, 0.89] | Targeted, repetitive tasks | Specific cognitive domains [39] |
| Exergame-based training | 1.09 | [0.26, 1.91] | Combined physical/cognitive exercise | Neuropsychiatric disorders [42] |
| Telerehabilitation/social training | 2.21 | [1.11, 3.32] | Remote delivery, social cognition | Social functioning deficits [42] |
Mental Health Treatment Outcomes
For anxiety disorders and PTSD, VR-enhanced exposure therapy demonstrates success rates between 66% and 90% based on meta-analytic findings [44]. A landmark randomized controlled trial for VR therapy in psychosis (n=346) showed significant reduction in agoraphobic avoidance and distress compared to standard therapy alone [44]. When applied to depression treatment through behavioral activation, VR interventions show particular promise for addressing motivational deficits, with 93.8% of healthcare providers reporting higher patient engagement with VR-enhanced therapy compared to traditional methods [44].
Experimental Protocols and Methodologies
VR-CBT for Anxiety Disorders Protocol
The following diagram illustrates a standardized protocol for implementing VR-CBT for anxiety disorders:
Implementation Parameters:
- Session duration: 45-60 minutes [37]
- Frequency: 1-2 sessions per week [44]
- Exposure progression: Hierarchical based on subjective units of distress (SUDS) ratings [37]
- Biofeedback integration: Heart rate variability and skin conductance monitoring for objective anxiety assessment [37]
- Therapist control: Real-time adjustment of virtual environment parameters based on patient response [37]
Cognitive Training for MCI Protocol
The following workflow details a comprehensive VR cognitive training protocol for Mild Cognitive Impairment:
Training Parameters:
- Session duration: 30-45 minutes [39]
- Frequency: 3-5 sessions per week [40]
- Training progression: Adaptive algorithm adjusting to 80% accuracy threshold [39]
- Domain targeting: Focus on episodic memory, executive functions, and processing speed [40]
- Transfer tasks: Incorporation of real-world activities (medication management, financial tasks) [40]
Research Reagent Solutions
Table 3: Essential Research Materials and Technical Solutions for VR-CBT Studies
| Component | Specifications | Research Application | Example Metrics |
|---|---|---|---|
| Head-Mounted Display (HMD) | Minimum 90Hz refresh rate, 100°+ FOV, 6DoF tracking | Creates immersive presence, controls visual field | Presence questionnaires, cybersickness ratings [41] |
| VR Software Platform | Customizable environments, real-time parameter adjustment | Standardized stimulus presentation across participants | Environment customization logs [37] |
| Biometric Sensors | ECG, EDA, EEG integration capabilities | Objective physiological response measurement | Heart rate variability, skin conductance response [37] |
| Performance Tracking | Automated logging of user actions, reaction times, gaze patterns | Quantitative assessment of cognitive and behavioral performance | Response latency, error rates, completion accuracy [39] |
| Control Condition Software | 2D computer-based equivalent tasks | Active control for isolation of immersion effects | Comparable task demands without immersion [43] |
Technical Implementation in Research Settings
Methodological Considerations for Behavioral Neuroscience
Implementing VR in behavioral neuroscience research requires careful consideration of several technical and methodological factors. The level of immersion significantly impacts therapeutic outcomes, with fully immersive HMD-based systems demonstrating greater effect sizes (Hedges' g = 0.68) compared to non-immersive approaches [39]. This relationship is moderated by individual tolerance levels, requiring researchers to balance immersion intensity with participant comfort.
From an experimental design perspective, ecological validity can be enhanced through carefully designed virtual environments that simulate real-world contexts while maintaining experimental control. This approach addresses the "transfer problem" common in cognitive rehabilitation by promoting generalization of skills to daily functioning [40]. Additionally, multimodal assessment incorporating both performance metrics within VR and traditional neuropsychological measures provides comprehensive evaluation of intervention effects across different levels of functioning.
The diagram below illustrates the relationship between technical parameters and therapeutic mechanisms in VR interventions:
Data Collection and Analytical Approaches
VR platforms enable rich, multimodal data collection that extends beyond traditional outcome measures. Behavioral metrics such as response times, movement patterns, and gaze behavior provide continuous performance data with high temporal resolution [41]. Physiological measures including heart rate variability, electrodermal activity, and EEG can be synchronized with virtual events to capture psychophysiological responses to specific stimuli [37].
Advanced analytical approaches for VR-derived data include:
- Machine learning classification: Identifying patterns predictive of treatment response [41]
- Longitudinal growth modeling: Tracking trajectories of change across training sessions [39]
- Network analysis: Examining relationships between different cognitive domains during training [42]
- Multilevel modeling: Accounting for nested data structure (repeated measures within participants) [34]
Integration with Neuroscientific Research Paradigms
Framework for Drug Development Research
VR-enhanced cognitive assessment and intervention protocols offer significant opportunities for drug development research. These approaches can serve as sensitive endpoints for clinical trials, detecting subtle cognitive improvements that may not be captured by traditional neuropsychological measures [42]. The high-resolution data provided by VR systems enables more precise measurement of cognitive processes targeted by pharmacological interventions.
For translational neuroscience, VR protocols create opportunities for cross-species validation of cognitive tasks. Virtual environments can be designed to approximate rodent behavioral tasks (e.g., virtual Morris water maze, radial arm maze), facilitating direct comparison between human and animal model findings [38]. This approach strengthens the construct validity of cognitive measures used in preclinical and clinical stages of drug development.
Future Research Directions
The field of VR-enhanced interventions would benefit from targeted research in several key areas. Standardization of protocols across research groups would facilitate meta-analytic synthesis and direct comparison of findings [40]. Investigation of dose-response relationships would clarify optimal session duration, frequency, and total intervention length for different populations [39]. Additionally, research identifying mechanisms of action would elucidate how specific VR parameters (immersion, presence, interactivity) contribute to therapeutic outcomes [41].
From a technological perspective, development of closed-loop systems that automatically adjust task difficulty based on real-time performance could optimize the training experience for individual users [37]. Integration with neurostimulation approaches (tDCS, TMS) may create synergistic effects by combining brain stimulation with targeted cognitive engagement [34]. Finally, predictive modeling using baseline characteristics to identify individuals most likely to respond to VR-based interventions would support personalized treatment selection [42].
VR-enhanced CBT and cognitive rehabilitation represent a significant advancement in non-pharmacological interventions for neuropsychiatric and cognitive disorders. The strong theoretical foundations, growing empirical support, and methodological sophistication of these approaches make them valuable tools for behavioral neuroscience research and drug development. By providing controlled yet ecologically valid assessment and training environments, VR technologies bridge the gap between laboratory measures and real-world functioning while generating rich, multimodal data for analysis.
As the field continues to evolve, ongoing refinement of protocols, technological advancements, and mechanistic research will further clarify the optimal application of these tools across different populations and cognitive domains. For researchers and drug development professionals, VR-enhanced paradigms offer promising approaches for measuring cognitive outcomes with greater sensitivity and ecological validity than traditional methods.
Navigating the Virtual Frontier: Challenges and Optimization Strategies
Virtual reality (VR) has emerged as a revolutionary tool in behavioral neuroscience research, offering unprecedented capabilities to create controlled, immersive environments for studying brain function and behavior. By enabling ecologically valid assessments within laboratory settings, VR bridges the critical gap between artificial experimental conditions and real-world complexity [45]. The technology's capacity to simulate complex scenarios while maintaining precise experimental control makes it particularly valuable for investigating neurobehavioral processes, cognitive function, and therapeutic interventions [45] [46].
The fundamental advantage of VR in behavioral neuroscience lies in its ability to create immersive simulations that elicit naturalistic behaviors and psychological responses while maintaining rigorous experimental control. This balance between ecological validity and methodological precision has positioned VR as a transformative technology for studying the neural mechanisms underlying behavior [47]. The sense of "presence" – the psychological experience of being in the virtual environment – serves as a crucial mechanism that enables VR to activate neurobehavioral systems in ways that mirror real-world functioning [47]. This capacity makes VR particularly valuable for creating authentic contexts for neuropsychological assessment and intervention.
Current Applications and Demonstrated Efficacy
Therapeutic Applications in Mental Health
VR has demonstrated significant potential across multiple domains of mental health treatment, particularly through virtual reality exposure therapy (VRET). This approach allows for controlled, gradual exposure to fear-eliciting stimuli for conditions including phobias, anxiety disorders, and post-traumatic stress disorder (PTSD) [45]. The immersive properties of VR facilitate emotional engagement and fear activation necessary for therapeutic extinction learning, while maintaining physical safety and clinical control. Beyond anxiety disorders, VR applications have shown promise in addressing body image concerns in eating disorders through virtual embodiment techniques, and in managing psychotic symptoms through controlled exposure and reality testing [45].
Cognitive Rehabilitation and Neurobehavioral Applications
In cognitive neuroscience and rehabilitation, VR enables the creation of ecologically valid assessment environments that challenge multiple cognitive domains simultaneously, better reflecting real-world cognitive demands. Recent meta-analytic evidence supports the efficacy of VR-based interventions for cognitive rehabilitation across various neuropsychiatric conditions. As shown in Table 1, different VR approaches show varying levels of effectiveness for cognitive improvement.
Table 1: Efficacy of VR-Based Interventions on Cognitive Function in Neuropsychiatric Disorders
| Intervention Type | Standardized Mean Difference (SMD) | 95% Confidence Interval | Statistical Significance |
|---|---|---|---|
| Overall Cognitive Function | 0.67 | 0.33-1.01 | p < 0.001 |
| Cognitive Rehabilitation Training | 0.75 | 0.33-1.17 | p < 0.001 |
| Exergame-Based Training | 1.09 | 0.26-1.91 | p = 0.01 |
| Telerehabilitation & Social Functioning | 2.21 | 1.11-3.32 | p < 0.001 |
| Immersive Cognitive Training | - | - | p = 0.06 (NS) |
| Music Attention Training | - | - | p = 0.72 (NS) |
Data synthesized from 21 RCTs involving 1,051 participants with neuropsychiatric disorders [48]
For Mild Cognitive Impairment (MCI), VR-based interventions have demonstrated significant benefits, with a recent systematic review and meta-analysis reporting an overall effect size of Hedges' g = 0.6 (95% CI: 0.29 to 0.90, p < 0.05) [49]. Interestingly, VR-based games (Hedges's g = 0.68) showed slightly greater advantages for improving cognitive impairments compared to VR-based cognitive training (Hedges's g = 0.52) [49]. This suggests that engaging, game-based approaches may enhance adherence or engagement, potentially amplifying therapeutic effects.
In attention-deficit/hyperactivity disorder (ADHD), preliminary studies indicate that VR-based cognitive control training can produce significant improvements in specific cognitive domains. One study involving 29 children and adolescents with ADHD symptoms found significant improvement on the Stroop Color-Word test (F₂,₅₆=4.97; P=.001; ηp²=0.151) and parent-rated ADHD symptoms (CBCL ADHD: F₂,₅₆=3.46; P=.004; ηp²=0.110) following 20 days of VR training [50]. These findings suggest that VR may provide an engaging, adaptive platform for addressing core cognitive deficits in neurodevelopmental disorders.
Critical Methodological Challenges and Limitations
Inconsistent Methodological Approaches
The rapid proliferation of VR research has occurred without concomitant development of standardized methodological frameworks, leading to significant variability in study design, implementation, and reporting. This heterogeneity poses challenges for interpreting findings and synthesizing evidence across studies [45] [49]. Research on collaborative embodiment in VR exemplifies this issue, with studies employing diverse metrics, task designs, and collaboration methods without established standards [46]. The field lacks consensus guidelines for key methodological elements including appropriate control conditions, optimal dosing parameters, standardized outcome measures, and reporting standards for technical specifications.
Insufficient Methodological Rigor
Many VR studies suffer from methodological limitations that compromise the validity and generalizability of their findings. Common issues include small sample sizes, inadequate blinding, insufficient attention to placebo effects, and limited long-term follow-up [45] [49]. A meta-analysis of VR-based cognitive interventions noted that "the lack of rigorous research" significantly limits confidence in findings and clinical implementation [45]. Similarly, a systematic review of VR for MCI highlighted inconsistent findings across studies, attributing these discrepancies to "variations in VR intervention content" and methodological quality [49].
The problem of inadequate validation is particularly salient for neurobehavioral applications, where the relationship between VR performance and real-world functioning requires further elucidation. As noted in one study, "treatment benefits should translate into improvements in real-world functioning," yet few studies establish this ecological transfer [50]. This gap between laboratory assessment and real-world relevance represents a significant methodological challenge for the field.
Technical and Implementation Barriers
Technical limitations present substantial obstacles to methodological standardization and clinical implementation. Issues such as cybersickness, technical constraints, and the need for specialized equipment limit accessibility and scalability [45]. The level of immersion has been identified as a significant moderator of intervention effects [49], yet optimal immersion levels for different applications and populations remain undefined. Furthermore, rapid technological advancement means that hardware and software platforms become obsolete quickly, complicating the development of standardized protocols and making direct comparison across studies difficult.
Table 2: Key Technical and Methodological Challenges in VR Research
| Challenge Category | Specific Issues | Impact on Research |
|---|---|---|
| Technical Limitations | Cybersickness, technical constraints, specialized equipment requirements | Reduced accessibility, limited scalability, participant discomfort |
| Methodological Issues | Lack of standardized protocols, small sample sizes, limited long-term follow-up | Compromised validity, hindered evidence synthesis, unknown durability of effects |
| Implementation Barriers | High costs, need for technical expertise, variability in hardware/software | Reduced reproducibility, limited generalizability, healthcare inequities |
Synthesized from multiple sources [45] [49] [48]
Toward Methodological Standardization: Key Considerations
Standardized Protocol Development
Establishing evidence-based guidelines for VR intervention design and implementation is crucial for advancing the field. These should address key parameters including optimal session duration, frequency, total intervention length, and progression criteria. Based on current evidence, Table 3 outlines essential components for methodological standardization in VR research.
Table 3: Essential Components for Methodological Standardization in VR Research
| Component | Key Considerations | Recommendations |
|---|---|---|
| Technical Specifications | Immersion level, hardware, software, interaction paradigms | Detailed reporting of technical parameters; classification of immersion level (low, moderate, high) |
| Intervention Protocol | Session duration, frequency, progression criteria, adaptive algorithms | Clear documentation of dosing parameters; use of adaptive difficulty algorithms based on performance |
| Outcome Assessment | Primary and secondary outcomes, timing of assessments, transfer to real-world functioning | Multidimensional assessment including behavioral, physiological, and functional measures; long-term follow-up |
| Participant Characteristics | Clinical status, VR experience, motion sickness susceptibility | Comprehensive reporting of inclusion/exclusion criteria; assessment of cybersickness |
Synthesized from multiple sources [45] [49] [46]
Protocols should be tailored to specific populations and clinical targets, recognizing that optimal parameters likely differ across disorders, age groups, and therapeutic goals. For example, interventions for ADHD may benefit from shorter, more engaging sessions with frequent reward schedules [50], while cognitive rehabilitation for MCI may require longer, graded training programs [49] [48].
Enhanced Research Design and Reporting
Implementing methodologically rigorous designs is essential for generating conclusive evidence. This includes adequately powered randomized controlled trials (RCTs) with appropriate control conditions, blinded outcome assessment, and longer-term follow-up periods. Researchers should adhere to established reporting guidelines such as the CONSORT statement with VR-specific extensions to ensure comprehensive documentation of methodological details.
The technical specifications of VR systems must be thoroughly documented, including immersion level, hardware specifications, software characteristics, and interaction paradigms. As demonstrated by research on presence and immersion, the technical features of VR systems significantly influence user experience and intervention effects [47]. Standardized classification of immersion level based on technical parameters (e.g., stereoscopy, degrees of freedom, interaction paradigms) would facilitate cross-study comparisons [49].
Figure 1: Components of Standardized VR Research Protocols. This workflow outlines essential elements for methodological standardization in virtual reality research.
The Scientist's Toolkit: Essential Research Reagents and Materials
Advancing VR research requires specialized tools and approaches. Table 4 outlines key "research reagents" and their functions in methodological development.
Table 4: Essential Research Reagents and Methodological Tools for VR Research
| Research Reagent | Function | Application Examples |
|---|---|---|
| Adaptive Difficulty Algorithms | Automatically adjusts task difficulty based on user performance | Maintaining optimal challenge level; personalizing training intensity [50] |
| Presence and Immersion Metrics | Quantifies subjective sense of "being there" in the virtual environment | Assessing mechanism of action; optimizing technical parameters [47] |
| Physiological Synchrony Measures | Captures coordination of physiological signals between users | Studying collaborative embodiment; quantifying social interaction [46] |
| Eye Tracking Integration | Monitors gaze patterns and visual attention within VR environments | Assessing attentional processes; validating engagement metrics [46] |
| Motion Tracking Systems | Captures real-time movement data for interaction with virtual environment | Enabling naturalistic movement; studying motor behavior [45] |
| Cybersickness Assessment Tools | Measures VR-induced discomfort and nausea | Screening participants; monitoring adverse effects [45] |
Future Directions: Integrating Emerging Technologies
The future of VR in behavioral neuroscience lies in strategic integration with other emerging technologies. Artificial intelligence (AI) and machine learning approaches can personalize interventions in real-time based on user performance and physiological responses [45] [51]. Biofeedback integration enables closed-loop systems that adapt virtual environments based on psychophysiological signals, creating dynamic, responsive interventions [45].
Collaborative embodiment approaches represent another promising direction, enabling multiple users to interact within shared virtual spaces [46]. These systems have potential applications in social skills training, group therapy, and interpersonal neuroscience research. However, they also introduce additional methodological complexities related to synchronization, shared control, and multi-user interaction dynamics.
The emerging field of digital phenotyping uses VR-derived behavioral data to identify subtle patterns associated with neurological and psychiatric conditions. This approach leverages the rich behavioral data captured in VR environments to develop more sensitive, objective markers of neurobehavioral functioning.
Virtual reality holds transformative potential for behavioral neuroscience research and clinical applications, but realizing this potential requires addressing significant methodological challenges. By developing standardized protocols, implementing methodologically rigorous designs, and embracing emerging technologies, the field can overcome current limitations and establish VR as a valid, reliable tool for understanding and modifying neurobehavioral functioning. The path forward requires collaborative efforts between researchers, clinicians, and technology developers to build a robust methodological foundation that supports the valid and reliable use of VR in behavioral neuroscience.
Virtual reality (VR) holds transformative potential for behavioral neuroscience research, offering unprecedented control over immersive, ecologically valid experimental environments. [45] [21] The technology enables the precise presentation of complex, dynamic stimuli and the continuous measurement of behavioral responses in ways traditional laboratory settings cannot match. [52] [53] However, the path to its widespread adoption is fraught with significant technical and accessibility challenges. This guide provides a structured analysis of three critical hurdles—financial cost, cybersickness, and the limitations of specialized equipment—within the context of behavioral neuroscience research. For each challenge, we present quantitative assessments, detailed experimental methodologies for evaluation and mitigation, and practical frameworks to guide research design and implementation.
Quantitative Analysis of Key Hurdles
The following tables synthesize current quantitative data on the core technical and accessibility hurdles, providing researchers with a baseline for project planning and resource allocation.
Table 1: Cost and Adoption Profile of VR Hardware
| Metric | Value | Context & Implications for Research |
|---|---|---|
| U.S. Adult VR Owners | ~53 million [54] | Indicates growing user base; potential participant pool may have prior VR experience. |
| Potential Market Growth | 21% (14 million new users) [54] | Suggests increasing public familiarity, which may reduce participant training overhead. |
| Typical Cost Range for Quality Headsets | $500 - $1,000 [54] | Recurring cost for multi-device lab setups; standalone units (e.g., Quest 2) reduce need for expensive PCs. [52] |
| Consumer Satisfaction with Graphics | ~80% [54] | High-quality visual fidelity is achievable with consumer-grade hardware, supporting stimulus presentation. |
| Exclusion Due to Cybersickness | Estimates often 10-30% (see Table 2) | A significant portion of potential participants may be unable to complete studies, affecting recruitment. |
Table 2: Cybersickness Prevalence and Contributing Factors
| Factor | Description | Quantitative/Qualitative Impact |
|---|---|---|
| General Prevalence | Common user experience | 62% of VR users report nausea or dizziness. [54] |
| Symptom Profile | Similar to motion sickness | Symptoms include eye strain, nausea, dizziness, and headache. [55] |
| Technical Trigger (Latency) | Delay between user movement and display update | A primary cause of sensory conflict; modern headsets aim for <20ms to minimize this. |
| Technical Trigger (Tracking Axis) | Accuracy varies by spatial direction | Hand-tracking accuracy is highest left/right, then up/down, and noisiest along the near/far axis. [52] |
| Mitigation Strategy | Software solutions | Interventions like "Motion Reset" software are under active investigation to reduce symptoms. [55] |
Experimental Protocols for Assessing and Mitigating Hurdles
Protocol for Quantifying Cybersickness
Objective: To empirically evaluate the efficacy of an intervention (e.g., Motion Reset software) in preventing or reducing cybersickness symptoms during a controlled VR exposure. [55]
1. Participant Recruitment:
- Sample Size: Target 150 healthy adult participants (aged 18-60) for adequate statistical power. [55]
- Inclusion Criteria: Normal or corrected-to-normal vision and hearing. [55]
- Exclusion Criteria: History of vestibular disorders, photo-sensitive epilepsy, current use of anti-nausea medication, and individuals at extremes of motion sickness propensity. [55]
2. Study Design and Randomization:
- Employ a randomized, controlled, between-subjects design.
- Participants are randomly assigned to one of three arms:
- Active Intervention Arm: Experiences the VR intervention designed to prevent cybersickness (e.g., Motion Reset).
- Placebo Control Arm: Experiences a similar VR experience that does not engage the purported preventive mechanisms.
- No-Treatment Control Arm: Does not engage in any initial VR experience. [55]
3. Experimental Procedure:
- The study is conducted in a single session lasting approximately one hour. [55]
- Pre-Test Baseline: Participants complete pre-exposure questionnaires on their current state.
- Intervention/Control Phase: Groups 1 and 2 undergo their assigned VR experience, which involves viewing screens and moving around while pressing buttons on a controller.
- Stimulus Challenge Phase: All participants (including the no-treatment group) subsequently engage in a standardized, challenging VR game (e.g., Jurassic World Aftermath) for up to 20 minutes. This game is known to induce moderate cybersickness.
- During this phase, self-reported discomfort is assessed at regular intervals (e.g., every few minutes). Participants are instructed to stop if discomfort reaches a pre-defined threshold, and the duration of play is recorded as a secondary metric. [55]
4. Data Collection and Primary Endpoint:
Protocol for Validating Consumer-Grade Tracking Equipment
Objective: To determine the accuracy and reliability of kinematic data (e.g., hand position, velocity) obtained from a consumer-grade VR headset (Oculus Quest 2) against a gold-standard motion capture system. [52]
1. Apparatus Setup:
2. Experimental Conditions:
- The validation should be performed under two critical conditions:
- Tethered: The VR headset is fixed in place on a stable tripod near the participant. This minimizes the confounding effect of head movement on hand-tracking accuracy. [52]
- Untethered: The VR headset is worn normally on the participant's head. This assesses tracking performance under realistic, dynamic use, where head movements can introduce noise. [52]
- The validation should be performed under two critical conditions:
3. Movement Tasks:
- Participants perform standardized motor tasks:
- Center-Out Reaching: Reaching from a central starting point to targets at different locations (e.g., left, frontal, right). This allows assessment of positional accuracy across different spatial directions. [52]
- Grip Aperture: Performing hand opening and closing movements to assess the device's ability to track fine motor details. [52]
- Participants perform standardized motor tasks:
4. Data Analysis and Metrics:
- Kinematic Variables: Calculate key variables from both systems, including hand position, peak velocity, acceleration, and grip aperture. [52]
- Statistical Comparison: Use correlation analyses (e.g., Spearman's rank correlation) and tests for differences in means (e.g., Wilcoxon signed-rank test) to compare the Quest 2 data with the Optitrack ground truth. [52]
- Spatial Accuracy Mapping: Specifically analyze if tracking accuracy varies along different spatial axes (left/right, up/down, near/far). [52]
The Researcher's Toolkit: Key Equipment and Solutions
Table 3: Research Reagent Solutions for VR Neuroscience
| Item / Solution | Function in Research Context | Considerations and References |
|---|---|---|
| Meta Quest 2/Pro | A standalone HMD for presenting immersive stimuli and tracking hand/head kinematics. [52] [53] | Cost-effective; provides reliable position/velocity data; acceleration data can be noisy. [52] Integrated eye-tracking (Quest Pro) enables gaze-based paradigms. [53] |
| High-End Motion Capture (e.g., Optitrack) | Serves as a gold-standard system for validating the kinematic data obtained from consumer VR equipment. [52] | High cost and complexity are barriers; essential for establishing the validity of consumer-grade tools in rigorous research. [52] |
| Emotiv EPOC X EEG | A consumer-grade EEG system with 14 channels for measuring neural correlates of cognition and perception in VR. [53] | Enables hybrid Brain-Computer Interface (BCI) designs (e.g., NeuroGaze). Integration and signal quality in dynamic VR environments remain a key challenge. [53] |
| Simulator Sickness Questionnaire (SSQ) | A standardized metric for quantifying cybersickness, serving as a primary endpoint in intervention studies. [55] | Critical for monitoring participant well-being and ensuring data quality by accounting for symptom-driven performance drops. |
| Motion Reset Software | An investigational intervention designed to prevent the onset of cybersickness during VR use. [55] | Represents a class of software-based mitigation strategies; efficacy is currently being validated in clinical trials (NCT06552754). [55] |
| VRelax | A specific VR relaxation tool featuring 360° natural environments, used for stress reduction studies in clinical populations. [56] | An example of an off-the-shelf therapeutic application; studies show it can improve perceived stress and affective states. [56] |
The integration of VR into behavioral neuroscience is not a simple matter of hardware acquisition but requires a meticulous, evidence-based approach to overcome significant technical and accessibility hurdles. Researchers must strategically balance the cost-effectiveness of consumer-grade devices against their technical limitations, rigorously validating them for specific research tasks. Proactive and systematic assessment of cybersickness, using standardized protocols and emerging mitigation software, is essential to ensure participant safety and data integrity. Finally, the development of specialized equipment, particularly hybrid BCI systems, while promising, demands careful consideration of integration complexity and signal reliability. By addressing these challenges with the quantitative frameworks and methodological rigor outlined in this guide, researchers can robustly leverage VR's power to advance our theoretical understanding of brain and behavior.
The integration of Virtual Reality (VR) and Extended Reality (XR) into behavioral neuroscience research represents a paradigm shift, offering unprecedented control over experimental stimuli and the creation of ecologically valid environments. These technologies enable the simulation of complex real-world scenarios in a controlled laboratory setting, facilitating novel investigations into cognitive processes, emotional responses, and behavioral interventions [57] [58]. The unique capabilities of VR—encompassing immersive, interactive, and imaginative experiences—allow researchers to study phenomena that are dangerous, impossible, or prohibitively expensive to replicate in the real world [59].
However, the very features that make VR powerful also introduce profound ethical challenges. Within the context of theoretical frameworks for behavioral neuroscience research, the core ethical trilemma revolves around data privacy, patient autonomy, and clinical supervision. The immersion and data fidelity required for rigorous neuroscience research often involve collecting intimate, high-dimensional biometric data, thereby raising critical questions about informational privacy and security [58]. Furthermore, the persuasive and potentially reality-altering nature of immersive experiences touches upon the fundamental principle of patient autonomy, requiring a re-examination of informed consent processes [57]. Finally, the introduction of artificial intelligence (AI) into these systems complicates traditional models of clinical supervision and liability, necessitating new frameworks for ensuring patient safety and therapeutic efficacy [57] [58]. This technical guide examines these ethical implications through the lens of biomedical ethics principles—autonomy, beneficence, non-maleficence, and justice—to provide researchers with a structured approach for navigating this complex landscape.
Core Ethical Principles and VR-Specific Challenges
The application of established biomedical ethics principles to VR-based behavioral neuroscience research reveals several technology-specific challenges. The table below summarizes the core challenges and their research implications.
Table 1: Core Ethical Principles and Their VR-Specific Challenges
| Ethical Principle | Definition | VR-Specific Challenge | Research Implication |
|---|---|---|---|
| Autonomy | The right of patients/participants to choose or refuse treatment and provide informed consent [57]. | Altering autonomy by altering reality: VR's ability to create persuasive, controlled environments may subtly manipulate decision-making and challenge a participant's ability to provide truly informed consent, especially when the full scope of the experience is difficult to convey beforehand [57]. | Requires enhanced consent protocols that accurately communicate the nature and potential impact of the immersive experience. |
| Beneficence | The obligation to act in the best interest of the patient/participant [57]. | Balancing therapeutic benefit with unknown risks: While VR offers promising therapeutic benefits (e.g., exposure therapy, neurorehabilitation), the long-term psychological and neural effects of repeated immersion are not fully understood [57] [58]. | Necessitates rigorous safety monitoring and longitudinal studies to establish a clear risk-benefit profile for different populations. |
| Non-maleficence | The duty to minimize harm or risk [57]. | Psychological and physiological risks: Potential for cybersickness, physiological arousal, anxiety, and in vulnerable populations, the exacerbation of pre-existing reality distortion or psychological trauma [57]. | Mandates careful participant screening, real-time physiological monitoring, and clear emergency protocols for terminating sessions. |
| Justice | The fair distribution of benefits, burdens, and resources [57]. | Fostering inclusiveness and equity: Risks of algorithmic bias in AI-driven systems and inequitable access to advanced VR interventions due to cost, digital literacy, or disability, potentially exacerbating health disparities [57] [58]. | Requires proactive efforts in inclusive design, development of accessible interfaces, and exploration of cost-effective delivery models. |
Data Privacy and Security in VR/XR Environments
VR and XR systems are data collection engines, capable of capturing a vast array of sensitive information that extends far beyond conventional clinical data. This creates unprecedented privacy and security concerns for neuroscience research.
Nature and Sensitivity of VR-Collected Data
The data generated in VR environments can be categorized as follows:
- Biometric Data: Eye-tracking (gaze direction, pupil dilation), electrodermal activity, heart rate, and electroencephalography (EEG) data, which can reveal subconscious cognitive and emotional states [58].
- Behavioral Data: Precise kinematic movements, reaction times, path lengths, and interaction logs with virtual objects, providing a detailed picture of sensorimotor and cognitive performance [60].
- Physiological Data: Heart rate variability, skin conductivity, and brain activity patterns, which are used to index emotional states and cognitive load [61].
- Identity and Performance Data: Voice recordings, facial expressions (via inside-out tracking), and comprehensive records of a user's choices, movements, and reactions within the virtual world.
This multi-modal data is highly sensitive. When combined, it can be used to infer a participant's psychological state, identify neurological conditions, and even uniquely identify an individual based on their movement patterns.
Data Governance Gaps and Security Protocols
Current research indicates a significant lag between technological capability and ethical governance. A major scoping review highlights "weak data governance" and "opaque algorithmic processes" as primary concerns in AI-XR systems [58]. The integration of these technologies within metaverse-like frameworks further complicates data ownership and flow across platforms.
To address these gaps, researchers must implement robust security protocols. The following diagram illustrates a proposed data governance workflow for a VR-based neuroscience experiment, from data acquisition to storage and sharing.
Diagram 1: Data Governance and Security Workflow for VR Neuroscience Research. This workflow outlines a secure pipeline for handling sensitive VR-acquired data, emphasizing pseudonymization and encryption.
Experimental Protocols for Privacy-Preserving Research
Table 2: Methodological Checklist for Data Privacy in VR Studies
| Protocol Phase | Action | Technical Specification | Rationale |
|---|---|---|---|
| Pre-Study Design | Data Minimization | Define and collect only data elements essential to the research question. | Reduces the attack surface and minimizes potential impact of a breach. |
| Privacy Impact Assessment (PIA) | Conduct a formal PIA to identify and mitigate privacy risks specific to the VR protocol. | Proactive risk management, required by many institutional review boards (IRBs) and funders. | |
| Participant Onboarding | Informed Consent | Explicitly detail all data types collected, their sensitivity, storage duration, security measures, and potential third-party sharing. | Upholds autonomy and fulfills legal and ethical requirements for transparency. |
| Withdrawal Protocol | Establish a clear process for participants to withdraw their data, including complex datasets like behavioral logs. | Respects participant rights; can be technically challenging, so must be planned. | |
| Data Handling | Pseudonymization | Replace direct identifiers with a code immediately upon collection, preferably on the VR device itself. | Decouples highly sensitive identity data from behavioral and biometric data. |
| Encryption | Implement end-to-end encryption for data in transit and strong encryption for data at rest. | Protects data against interception and unauthorized access. | |
| Post-Study | Data Retention | Define and adhere to a strict data retention schedule, with automated deletion where possible. | Aligns with the principle of data minimization and reduces long-term liability. |
| Secure Disposal | Use certified data destruction methods for all copies of the research data upon expiry of the retention period. | Ensures data is irrecoverable and cannot be misused in the future. |
Patient Autonomy and Informed Consent
The immersive and potentially transformative nature of VR experiences poses unique challenges to the doctrine of informed consent, a cornerstone of autonomous decision-making in research.
The Challenge of "Altering Autonomy by Altering Reality"
VR's capacity to induce a strong sense of "presence"—the subjective feeling of being in the virtual environment—is a key mechanism of its therapeutic and experimental efficacy. However, this same mechanism can subtly manipulate a user's perceptions, emotions, and behaviors in ways that are difficult to predict and communicate in advance [57]. This is particularly salient for populations with pre-existing vulnerabilities, such as individuals with psychiatric conditions that involve reality distortion. Obtaining meaningful consent requires that the participant truly understands what the experience will be like, which is inherently limited when describing an immersive, embodied phenomenon [57].
Methodologies for Enhanced Consent Procedures
Standard consent forms are insufficient for VR research. The following table outlines advanced methodological approaches for upholding autonomy.
Table 3: Protocols for Enhanced Informed Consent in VR Studies
| Methodology | Description | Implementation Example |
|---|---|---|
| Tiered Consent | Consent is obtained in stages, allowing participants to opt into different levels of data collection or specific types of immersive experiences. | A participant may consent to a baseline VR exposure but opt out of a high-anxiety scenario or the sharing of their eye-tracking data for secondary analysis. |
| Dynamic Re-consent | The consent process is ongoing, with prompts for re-confirmation if the VR experiment dynamically shifts to a scenario that was not fully detailed in the initial consent. | If an AI-driven narrative branches into an area involving simulated social conflict, the system could pause and ask the participant to verbally confirm they wish to proceed. |
| In-Vivo Consent Monitoring | Integrating consent checks within the VR environment itself to monitor continued willingness to participate. | A virtual agent periodically appears to ask "Are you still comfortable continuing?" or the system monitors for pre-defined distress signals (e.g., rapid head movement away from a stimulus) as a potential indicator of withdrawal. |
| Graded Exposure for Consent | Allowing participants to experience a mild, non-threatening version of the VR environment during the consent process to build a more accurate expectation. | Before the full study, a participant enters a simplified, calm version of the virtual lab to acclimate to the headset and the feeling of immersion, thereby making their consent more informed. |
Clinical Supervision and Liability in Automated Systems
The integration of AI into VR systems creates a hybrid clinical environment where responsibility is shared between the human researcher/clinician and the automated system, blurring traditional lines of supervision and liability.
The Shift in Clinical Responsibility
AI-driven XR (AI-XR) systems can now perform functions that were once the exclusive domain of trained professionals, such as:
- Adaptive Task Delivery: Modifying the difficulty of a cognitive task in real-time based on participant performance [58] [60].
- Emotion Detection: Using computer vision and voice analysis to infer affective states and theoretically adapting the intervention accordingly [58].
- Conversational Interaction: Employing LLM-powered virtual agents to conduct therapeutic dialogues or collect data [58].
This automation raises critical questions: Who is liable if an AI-driven exposure therapy scenario escalates too quickly and causes harm? Who is responsible for the clinical accuracy of an AI's interpretation of a participant's biometric data? The "clinical liability and regulation" landscape for these technologies is currently underdefined [57].
Frameworks for Supervision and Accountability
To ensure safety and accountability, researchers and clinicians must adopt structured frameworks for supervision. The following diagram maps the proposed oversight and liability framework for an AI-assisted VR intervention, highlighting the shared responsibility between human and machine agents.
Diagram 2: Clinical Supervision and Liability Framework for AI-Assisted VR. This diagram delineates the shared responsibilities between human clinicians and AI systems, under the umbrella of overarching governance.
Experimental Protocols for Ensuring Safety and Oversight
Table 4: Methodological Protocols for Clinical Supervision in VR Research
| Protocol Component | Methodological Detail | Function in Risk Mitigation |
|---|---|---|
| Pre-Defined Intervention Thresholds | Establish clear, quantifiable thresholds for physiological (e.g., heart rate), behavioral (e.g., avoidance), or self-reported metrics that will trigger a manual override or session termination. | Prevents the AI system from pushing a participant beyond their tolerance limit; ensures human judgment is applied at critical junctures. |
| Comprehensive System Logging | Implement detailed logging of all AI decisions, environmental adaptations, and participant inputs during the VR session. | Creates an audit trail for post-session analysis, which is crucial for understanding adverse events, refining algorithms, and assigning liability. |
| Researcher Training and Competency | Develop specific training modules for researchers on the operational principles, limitations, and failure modes of the VR and AI systems they are using. | Ensures that human supervisors are equipped to interpret system outputs and intervene effectively, upholding the principle of non-maleficence. |
| Independent Data Safety and Monitoring Board (DSMB) | For longitudinal or high-risk studies, employ an independent DSMB to periodically review unblinded data on adverse events and study progress. | Provides an external layer of safety oversight, protecting both participants and the research team. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key components and their functions for implementing ethically-sound VR research in behavioral neuroscience.
Table 5: Research Reagent Solutions for Ethical VR Neuroscience
| Item Category | Specific Examples | Function in Research Protocol |
|---|---|---|
| XR Hardware Platforms | Head-Mounted Displays (HMDs) with eye-tracking (e.g., Varjo, HTC Vive Pro Eye); Biometric sensor kits (EEG, EDA, ECG). | Provides the immersive interface and collects high-fidelity biometric and behavioral data (gaze, pupil dilation, heart rate, brain activity) crucial for neuroscientific analysis [59] [60]. |
| Software & Simulation Engines | Unity 3D with XR Interaction Toolkit; Unreal Engine. | Enables the creation and control of controlled, replicable 3D environments and tasks for experimental stimuli delivery [60]. |
| AI & Data Analytics Packages | Python with Scikit-learn, TensorFlow/PyTorch; R for statistical analysis. | Used for developing and running emotion detection algorithms, analyzing complex kinematic and biometric data, and performing statistical modeling of outcomes [58]. |
| Data Governance & Security Tools | Encryption software (e.g., VeraCrypt); Pseudonymization scripts; Secure data transfer protocols (SFTP). | Protects participant privacy by securing data at rest and in transit, fulfilling ethical and legal data handling requirements [58]. |
| Safety & Monitoring Equipment | Real-time biofeedback dashboards; "Stop" button/gesture for participants; Two-way audio communication. | Upholds the principle of non-maleficence by allowing continuous monitoring of participant state and providing immediate means for session interruption or researcher assistance [57]. |
| Ethical Oversight Frameworks | Customized IRB protocol templates for XR; Care Ethics checklists; Co-created living ethical codes with patient advocates. | Guides the entire research process, ensuring study design, consent procedures, and data management align with established and emerging ethical standards [57] [59]. |
In behavioral neuroscience, the ecological validity of experimental paradigms is paramount. Traditional laboratory settings often struggle to replicate the complexity of real-world behaviors and emotional responses, creating a gap between experimental data and genuine human experience. Virtual Reality (VR) has emerged as a powerful tool to bridge this divide, offering unprecedented control while maintaining immersive realism [14]. However, the mere presentation of virtual environments is insufficient for optimal research outcomes; sustained participant engagement is the critical factor that determines the quality, reliability, and translational power of the collected neuroscientific and behavioral data. Disengagement leads to inconsistent performance, high attrition rates, and ultimately, compromised data integrity.
This whitepaper establishes a theoretical and practical framework for optimizing engagement in VR-based behavioral neuroscience research through the synergistic integration of three core principles: personalization, gamification, and real-time biofeedback. We posit that these are not merely technical enhancements but fundamental components of a robust experimental methodology. By systematically implementing these strategies, researchers can transform VR from a simple presentation tool into a dynamic, adaptive, and responsive research platform that actively maintains participant state within desired parameters, thereby increasing the validity of findings related to cognitive processing, affective responses, and behavioral adaptations.
Theoretical Foundations: From One-Size-Fits-All to Adaptive Paradigms
The transition from static to adaptive VR paradigms is rooted in the recognition of profound individual differences in cognitive-affective processing. A one-size-fits-all approach ignores the heterogeneity of participant responses, introducing noise and confounding variables into experimental data.
The Five-Stage Framework for Personalization
A systematic review of personalized VR interactions reveals a consistent conceptual framework underlying adaptive systems. This framework provides a scaffold for developing rigorous, replicable experimental protocols in neuroscience research [62].
This continuous feedback loop allows VR environments to move beyond static presentation and become true interactive partners in the research process. For the neuroscientist, each stage represents a point of experimental control and data collection, enabling precise manipulation of independent variables and measurement of dependent variables within a highly ecological context.
The Neurobehavioral Basis of Gamification
Gamification—the application of game-design elements in non-game contexts—operates on established neurobehavioral principles. Effective gamification taps into intrinsic motivational pathways by providing clear goals, immediate feedback, and a sense of mastery and autonomy [63]. In the context of rehabilitation, which shares with neuroscience research the challenge of maintaining engagement in repetitive tasks, Calderone et al. (2025) found that gamification significantly enhanced motivation and adherence to therapy [63]. Participants were noted to be "more motivated and took active participation, which is one of the major key factors of long-term rehabilitation" [63].
From a neuroscientific perspective, well-designed gamification elements can elicit sustained engagement by triggering dopamine-mediated reward circuits, thereby promoting continued task participation and reducing attrition—a common challenge in lengthy experimental protocols.
Technical Implementation: A Multimodal Approach
Personalization Through Multimodal Sensing and Adaptive Systems
Personalization in VR relies on the continuous assessment of user state through multiple data streams. The following table summarizes the primary input modalities and their applications in behavioral neuroscience research.
Table 1: Multimodal Inputs for VR Personalization in Research
| Input Modality | Measured Parameters | Neuroscience Application | Data Type |
|---|---|---|---|
| Physiological Sensors [64] [62] | Heart Rate, Galvanic Skin Response, EEG | Assessing anxiety, cognitive load, emotional arousal | Continuous, Objective |
| Eye-Tracking [62] | Gaze direction, Pupillometry, Blink rate | Visual attention, cognitive workload, emotional response | Continuous, Objective |
| Motion Tracking [14] [62] | Head/body position, Movement kinematics | Motor learning, spatial navigation, behavioral avoidance | Continuous, Objective |
| Performance Metrics [63] [64] | Task accuracy, Reaction time, Progression speed | Cognitive function, skill acquisition, engagement level | Discrete, Objective |
| Self-Report [45] [36] | Anxiety scales, Presence questionnaires, Preference ratings | Subjective experience, emotional state, perceived difficulty | Discrete, Subjective |
These inputs feed into adaptive systems that modify the VR experience in real-time. For example, in a study on ailurophobia (fear of cats), a smartphone-gamified VR exposure therapy was developed that could adapt based on physiological feedback [64]. The system was designed to present "fear elements indirectly to the player," with the ability to adjust stimulus intensity based on individual response profiles [64].
Gamification Design Patterns for Research Protocols
Gamification elements must be carefully selected to enhance rather than confound experimental objectives. The following table outlines evidence-based gamification strategies with specific relevance to neuroscience research paradigms.
Table 2: Gamification Elements and Their Research Applications
| Gamification Element | Description | Behavioral Effect | Research Context Example |
|---|---|---|---|
| Progression Dynamics [63] | Visual indicators of advancement through levels/tasks | Sustains motivation through achievable milestones | Cognitive assessment batteries divided into "levels" |
| Performance Feedback [63] [64] | Real-time scoring, accuracy metrics, completion time | Provides reinforcement and encourages improvement | Motor learning tasks with precision scoring |
| Adaptive Challenge [63] | Dynamic difficulty adjustment based on performance | Maintains engagement in optimal challenge zone | Cognitive tasks that scale difficulty based on performance |
| Reward Systems [63] | Points, badges, virtual collectibles | Triggers reward pathways, reinforces target behaviors | Completion badges for study protocol milestones |
| Narrative Context [64] | Thematic storyline framing the activities | Enhances emotional engagement and recall | Spatial navigation tasks embedded in exploration narratives |
Critically, gamification must be implemented in a manner that does not introduce unwanted confounding variables. For instance, in the treatment of animal phobias, researchers noted that "phobia-focused games should avoid action and combat scenarios to prevent reinforcement of fear responses" [64]. Similarly, in cognitive neuroscience research, competitive elements might induce anxiety that interferes with the target cognitive process being studied.
Real-Time Biofeedback: Closing the Loop
Real-time biofeedback transforms VR from a passive presentation medium into an interactive bio-behavioral regulation system. This closed-loop approach is particularly valuable for research on emotion regulation, stress responses, and therapeutic interventions.
A protocol for a 2025 randomized controlled trial comparing VR-assisted cognitive behavioral therapy to yoga for performance anxiety exemplifies the research application of this approach [36]. The study aims to measure whether "VR-assisted CBT reduces anxiety very quickly" through controlled exposure in virtual environments [36]. The integration of biofeedback allows for precise titration of stimulus intensity based on physiological arousal, creating individualized exposure gradients that would be impossible to standardize in real-world settings.
The implementation of biofeedback requires careful consideration of sensor selection, data processing pipelines, and the specific physiological correlates of the psychological constructs under investigation.
Experimental Protocols and Methodological Considerations
Protocol: VR with Integrated Biofeedback for Anxiety Research
Based on the methodology from the ailurophobia study [64] and the performance anxiety trial [36], the following protocol provides a template for implementing an engagement-optimized VR paradigm.
Objective: To assess the efficacy of a biofeedback-enhanced VR environment for modulating anxiety responses in a controlled setting.
Participants: Recruitment through university counseling centers and community samples with standardized baseline anxiety assessment [36].
Apparatus:
- Standalone VR headset (e.g., Pico Ultra Enterprise, Quest 3) [63]
- Physiological monitoring: Smartband/wristwatch with HR and GSR capability [64]
- Software: Custom VR environment with integrated biofeedback API
Procedure:
- Baseline Assessment: Collect pre-intervention anxiety measures (e.g., State-Trait Anxiety Inventory) [36]
- System Calibration: Establish individual physiological baselines during neutral VR exposure
- Stimulus Presentation: Graduated exposure to anxiety-eliciting virtual scenarios
- Biofeedback Integration: Real-time monitoring of physiological arousal with predetermined thresholds for stimulus adjustment
- Post-Testing: Immediate and follow-up assessment of anxiety symptoms and behavioral avoidance
Data Analysis: Comparison of physiological synchrony, habituation rates, and self-report measures between adaptive and non-adaptive VR conditions.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Resources for Engagement-Optimized VR Research
| Category | Specific Tool/Platform | Research Function | Example Application |
|---|---|---|---|
| VR Hardware | Standalone HMDs (Pico, Quest) [63] [65] | Presents immersive environments | Deployment in clinic & home settings |
| Physiological Sensors | Smartbands, ECG, GSR, EEG [64] [62] | Captures autonomic & central arousal | Real-time anxiety monitoring |
| VR Development Platforms | Unity, Unreal Engine, ANU.JS [66] | Creates custom experimental environments | Web-based immersive visualizations |
| Adaptive Toolkits | ProgressiVis [66] | Enables progressive processing pipelines | Building Progressive Visual Analytics Systems |
| Data Analysis Suites | TTK Topological ToolKit [66] | Processes complex multidimensional data | Solving practical problems in small groups |
The integration of personalization, gamification, and real-time biofeedback represents a paradigm shift for VR in behavioral neuroscience. These approaches transform VR from a passive stimulus presentation tool into an active, adaptive research platform capable of maintaining optimal engagement states throughout experimental protocols. This advancement directly addresses core methodological challenges in neuroscience, including participant attrition, variable task engagement, and the ecological validity of laboratory assessments.
Future research directions should focus on the standardization of adaptive protocols, the development of cross-platform compatibility for biofeedback integration, and the establishment of methodological guidelines for balancing experimental control with personalized adaptation. As these engagement-optimized frameworks mature, they promise to enhance the reliability, validity, and translational impact of VR-based behavioral neuroscience research, ultimately leading to more effective clinical interventions and a deeper understanding of human behavior in health and disease.
Evidence and Efficacy: Validating VR Against Traditional Methods
Virtual Reality Exposure Therapy (VRET) represents a paradigm shift in the delivery of evidence-based treatments for anxiety disorders, offering an innovative technological alternative to traditional in vivo exposure therapy (IVET). Within behavioral neuroscience research, VRET provides a uniquely controlled platform to investigate learning and extinction processes by enabling precise manipulation of virtual environments while monitoring physiological and behavioral responses [67]. This technical analysis examines the comparative efficacy of VRET against gold-standard therapies, focusing on the translational application of exposure therapy principles within digitally mediated environments. The framework allows for systematic investigation of neural mechanisms underlying extinction learning while addressing practical implementation barriers that have limited the dissemination of traditional exposure-based treatments [68] [67].
Research indicates that despite exposure therapy's established efficacy, therapists significantly underutilize these techniques, with one study of 684 psychotherapists revealing incorporation of exposure therapy in only 46.8% of anxiety disorder treatments [69]. VRET emerges as a promising solution to these implementation challenges while providing new methodologies for exploring the neurobiological foundations of therapeutic change.
Theoretical Foundations and Mechanisms of Action
Psychological and Neurobiological Mechanisms
VRET operates through multiple theoretical mechanisms that align with established learning principles while leveraging technology-mediated experiences:
Pavlovian Extinction Model: VRET applies the classical conditioning principle where repeated exposure to fear-eliciting virtual stimuli (CS) without the feared outcome (UCS) gradually weakens the conditioned fear response [70]. This extinction process forms the foundation of exposure-based treatments across anxiety disorders.
Emotional Processing Theory: According to Foa & Kozak's model, VRET modifies fear structures in memory by activating these networks and introducing disconfirming safety information within immersive virtual environments [71].
Distraction and Attentional Mechanisms: For conditions like pain management, VRET's efficacy stems from competing for limited attentional resources, reducing the cognitive capacity available for processing anxiety or discomfort [67]. Functional MRI studies demonstrate correlated reductions in pain-related brain activity during VR immersion [67].
Sense of Presence: The subjective experience of "being there" in the virtual environment is crucial for therapeutic success. Technical immersion factors (field of view, tracking, visual fidelity) combine with individual factors to generate this presence, which elicits authentic emotional responses necessary for therapeutic change [67].
Distinct Advantages of VRET for Research and Treatment
VRET provides several methodological advantages for behavioral neuroscience research and clinical application:
Stimulus Control: Researchers can precisely standardize, manipulate, and replicate exposure scenarios across participants, enhancing experimental control and reproducibility [72] [71].
Ethical Testing Ground: VRET enables confrontation with feared stimuli in safe, controlled environments without real-world risks, allowing study of extreme scenarios [71] [69].
Physiological Monitoring: Integrated biosensors can simultaneously track physiological indicators (heart rate, skin conductance, gaze patterns) during exposure, providing multimodal data on fear responses [73].
Graduated Hierarchies: Virtual environments can be systematically adjusted in real-time based on participant performance, implementing individualized exposure gradients [74] [71].
The following diagram illustrates the theoretical pathways through which VRET achieves its therapeutic effects:
Comparative Efficacy Analysis
Social Anxiety Disorder (SAD)
Research demonstrates compelling efficacy for VRET in treating Social Anxiety Disorder, with effect sizes comparable to gold-standard in vivo interventions:
Table 1: Comparative Efficacy of VRET vs. In Vivo Exposure for Social Anxiety Disorder
| Study Type | Condition | Effect Size vs. Control | Key Outcomes | Clinical Significance |
|---|---|---|---|---|
| Meta-analysis (6 studies, N=358) | VRET | Hedges' g = 0.80-1.53 [70] | Significant reduction in social anxiety symptoms | Clinically significant |
| Meta-analysis (6 studies, N=358) | In Vivo ET | Comparable to VRET [70] | Significant reduction in social anxiety symptoms | Clinically significant |
| RCT (Public Speaking Anxiety) | VRET | -1.39 vs. control [71] | Reduced public speaking anxiety | Large significant effect |
| RCT (Public Speaking Anxiety) | In Vivo ET | -1.41 vs. control [71] | Reduced public speaking anxiety | Large significant effect |
| 6-year Longitudinal | VRET vs. In Vivo | Hedges' g = -0.15 [70] | No significant difference in FNE scores | Non-significant difference |
A recent meta-analysis of 11 studies with 508 participants focusing specifically on public speaking anxiety (PSA), a predominant feature of SAD, found both VRET and IVET produced large significant effects versus control conditions (VRET: -1.39, IVET: -1.41) [71]. This confirms that the mode of exposure delivery does not substantially impact overall efficacy when therapeutic principles are properly maintained.
Broader Anxiety Applications
Beyond SAD, VRET has demonstrated efficacy across multiple anxiety conditions:
Table 2: VRET Efficacy Across Anxiety-Related Conditions
| Condition | VRET Efficacy | Comparison to Gold-Standard | Key Benefits |
|---|---|---|---|
| Specific Phobias | Highly effective [71] [67] | Comparable to in vivo [71] | Overcoming practical barriers (e.g., aviophobia) [74] |
| PTSD | Effective [71] [67] | Similar to proven therapies [69] | Safe trauma recall environment [67] |
| Panic Disorder | Effective [71] | Comparable to established treatments [71] | Controlled interoceptive exposure |
| Substance Use Disorders | Promising for craving reduction [75] | N/A (adjunct to standard care) | Cue exposure in controlled environments [75] |
Patient Perceptions and Acceptability
Crucial for implementation science, patient perceptions strongly favor VRET approaches. A cross-sectional survey study of 184 individuals with anxiety disorders found significantly higher acceptance of VRET compared to in vivo exposures [69]:
- Willingness to receive: 90.2% for VRET vs. 82% for in vivo [69]
- Comfort, enthusiasm, and perceived effectiveness: Higher for VRET across all domains [69]
- Reported concerns for in vivo: Increased anxiety, feelings of embarrassment/shame, condition exacerbation [69]
- Reported concerns for VRET: Side effects, efficacy uncertainty, insurance coverage [69]
The most frequently cited benefits of VRET included privacy, safety, ability to control exposures, comfort, absence of real-life consequences, effectiveness, and customizability [69]. These perceptual factors directly impact treatment engagement and adherence, with studies showing VRET attrition rates less than half those of in vivo exposures for SAD treatment [70].
Methodological Framework and Experimental Protocols
VR-CORE Clinical Trial Framework
The Virtual Reality Clinical Outcomes Research Experts (VR-CORE) committee has established a methodological framework for developing and testing VR treatments, adapting the FDA phase model for therapeutic development [68]:
VR1 Studies: Focus on content development using human-centered design principles, involving patients and providers through iterative feedback cycles to ensure clinical relevance and usability [68].
VR2 Studies: Early-stage testing focusing on feasibility, acceptability, tolerability, and initial clinical efficacy, typically employing single-arm or small comparative designs [68].
VR3 Studies: Randomized controlled trials comparing VR interventions against appropriate control conditions (active comparators, waitlist, or standard care) with clinically meaningful outcomes and rigorous methodology [68].
This structured approach ensures systematic development of VR interventions with appropriate evidence generation at each stage, addressing concerns about methodological rigor in digital health interventions [68] [67].
Technical Implementation and Research Reagents
Successful VRET implementation requires specific technical components and methodological considerations:
Table 3: Research Reagent Solutions for VRET Implementation
| Component | Function | Technical Specifications | Research Considerations |
|---|---|---|---|
| Head-Mounted Display (HMD) | Presents 3D virtual environments | Field of view ≥100°, resolution ≥1080p per eye, refresh rate ≥90Hz [67] | Balance immersion with comfort for extended use |
| Tracking System | Monitors head and body movement | 6 degrees of freedom, positional tracking | Movement naturalism impacts presence [72] |
| Unity Experiment Framework (UXF) | Experimental control and data collection [72] | Session-block-trial structure, multi-modal data output | Standardizes methodology across labs [72] |
| Virtual Reality Analytics Map (VRAM) | Detection of mental disorder symptoms [73] | Quantifies behavioral domains through specific VR tasks | Identifies digital biomarkers [73] |
| Biometric Sensors | Objective arousal measurement | ECG, EDA, EEG integration | Synchronization with virtual events critical [73] |
| Virtual Environment Library | Contextual variety for exposure | Multiple scenarios for generalization | Prevents context-dependent extinction [70] |
The experimental workflow for implementing a VRET study follows a structured process from design through data analysis, as illustrated below:
Key Methodological Considerations
Several methodological aspects require careful attention in VRET research:
Theoretical Fidelity: VRET implementations must maintain theoretical alignment with established psychological principles rather than focusing exclusively on technological features [67].
Dose-Response Parameters: Research should systematically vary exposure duration, frequency, and intensity to establish optimal treatment parameters [68].
Generalization Measures: Include real-world outcome assessments beyond virtual environment performance to evaluate transfer of learning [70].
Longitudinal Follow-up: Given evidence of relapse potential, studies should incorporate extended follow-up periods (6+ months) to evaluate durability of treatment effects [70].
Applications in Broarker Behavioral Neuroscience and Drug Development
VRET in Substance Use Disorders
VRET applications extend beyond anxiety disorders to substance use, where it enables controlled exposure to drug cues while measuring craving responses and physiological reactions:
Cue Exposure Therapy: Virtual environments present substance-related triggers (people, places, objects) to elicit cravings, followed by extinction training [75].
Approach Bias Modification: VR scenarios train avoidance movements in response to substance cues, targeting automatic action tendencies [75].
Cognitive Rehabilitation: Virtual environments challenge executive functions through tasks requiring inhibition, working memory, and decision-making in substance-relevant contexts [75].
A systematic review of 20 RCTs found VR interventions focusing primarily on alcohol and nicotine use disorders demonstrated positive effects on at least one outcome variable in 17 studies, with particular promise for reducing craving (proximal outcome) [75]. However, substantial heterogeneity in VR methodologies highlights the need for standardization in this emerging field [75].
Biomarker Identification and Mechanism Evaluation
VR environments provide unique opportunities for identifying digital biomarkers of psychiatric conditions through the Virtual Reality Analytics Map (VRAM) framework [73]. This approach systematically maps and quantifies behavioral domains through specific VR tasks, capturing nuanced behavioral, cognitive, and affective digital biomarkers associated with symptoms of mental disorders [73].
For drug development, VRET platforms offer sensitive tools for evaluating novel therapeutic mechanisms by:
- Providing standardized, reproducible anxiety provocation across study sites
- Enabling continuous multi-modal data collection during exposure tasks
- Allowing precise titration of stimulus intensity to detect subtle drug effects
- Measuring both subjective distress and behavioral avoidance simultaneously
Limitations and Future Research Directions
Despite promising efficacy, VRET research faces several methodological challenges that require attention:
Theoretical Immaturity: The field lacks consensus on precise mechanisms of action and theoretical models specific to VR-mediated therapy [67].
Technical Standardization: Absence of common technical standards, outcome measures, and reporting guidelines complicates cross-study comparisons [68] [67].
Media vs. Medium Confounds: Difficulty separating effects of specific virtual content (media) from the delivery platform (medium) [67].
Cost and Accessibility: Despite decreasing hardware costs, implementation barriers remain for widespread clinical dissemination [67].
Future research priorities should include:
Dismantling Studies: Isolating active ingredients of VRET through component analysis studies [68].
Optimal Dosing: Establishing session frequency, duration, and spacing parameters for different conditions [68].
Personalization Algorithms: Developing adaptive systems that adjust virtual environments in real-time based on user performance and physiology [73].
Implementation Science: Studying barriers and facilitators to VRET adoption across diverse clinical settings [69].
VRET demonstrates comparable efficacy to gold-standard in vivo exposure therapies across anxiety disorders, with particular empirical support for social anxiety disorder and public speaking anxiety. The methodological advantages of VRET—including precise stimulus control, multi-modal assessment capabilities, and enhanced acceptability—position it as both valuable clinical intervention and powerful research platform for behavioral neuroscience.
Future research should address current methodological limitations while leveraging VR's capabilities to investigate learning and extinction mechanisms, identify novel biomarkers, and develop personalized therapeutic approaches. The integration of VRET within structured development frameworks like VR-CORE's VR1-VR3 model will strengthen evidence quality while accelerating the translation of technological innovations into clinically effective interventions.
As the field advances, VRET promises to both enhance understanding of therapeutic mechanisms and expand access to evidence-based treatments for anxiety and related disorders, bridging experimental neuroscience with clinical application.
Virtual Reality (VR) technology is revolutionizing behavioral neuroscience research by overcoming the critical limitation of ecological validity that has long plagued traditional laboratory-based cue exposure paradigms. By creating immersive, controllable, and reproducible simulations of real-world environments, VR provides a sophisticated tool for assessing and intervening in cue-induced craving in substance use disorders. This technical guide synthesizes current research to detail the mechanisms, methodologies, and empirical evidence establishing VR's superiority in eliciting clinically relevant responses, thereby offering a more robust framework for both basic research and therapeutic development.
In substance use research, cue exposure therapy has been a cornerstone for understanding and treating drug craving and relapse. Traditional laboratory paradigms, however, are constrained by their limited ecological validity—the degree to which findings can generalize to real-world settings [76]. These methods often involve exposing participants to static, two-dimensional images or drug paraphernalia in sterile, controlled environments, which fails to capture the complex, multisensory, and contextual nature of real-world substance use triggers [77] [45].
VR addresses this fundamental gap by leveraging its capacity to generate immersive, interactive simulations of real-life scenarios. A successful VR experience induces a powerful sense of "presence," the subjective feeling of "being there" in the virtual environment, despite the user's awareness of its artificial nature [45]. This phenomenon is crucial because it elicits psychological and physiological reactions that closely mirror those experienced in reality, enabling researchers to study conditioned responses within a controlled yet highly realistic context.
Theoretical Frameworks: How VR Enhances Validity
The enhanced ecological validity of VR is grounded in its ability to manipulate key theoretical constructs.
- Contextual Learning and Renewal: Addiction is maintained by powerful context-dependent memories. Traditional cue exposure in a lab office often fails to generalize to other environments, a phenomenon known as the renewal effect. VR allows for the simulation of multiple, varied, and highly specific drug-use contexts (e.g., a bar, a party, a private home), facilitating extinction learning across a wider range of stimuli and settings, which can potentially weaken the renewal effect [77].
- Multisensory Integration: Real-world cravings are triggered by a confluence of visual, auditory, olfactory, and social stimuli. VR can integrate these multisensory cues in a synchronized manner, providing a more potent and realistic trigger for craving than unimodal cues used in traditional settings [30].
- Sense of Presence: The effectiveness of VR is mediated by the user's sense of presence. Research has shown that a stronger sense of physical presence (feeling physically located in the VR world) and self-presence (feeling that one's actions are impactful in the VR world) are significant predictors of increased cue-induced craving [77]. This sense of "being there" is difficult, if not impossible, to achieve with traditional methods.
Experimental Evidence: Quantitative Comparisons
Empirical studies directly comparing VR and traditional methods consistently demonstrate VR's superiority in eliciting clinically relevant responses. The table below summarizes key quantitative findings from recent research.
Table 1: Summary of Key Experimental Findings Supporting VR's Efficacy
| Study & Population | Intervention | Key Measured Outcome | Result | Implication for Ecological Validity |
|---|---|---|---|---|
| AUD Patients (n=44) [77] | Exposure to 8 alcohol-cue VR environments vs. 2 neutral VR environments. | Change in subjective craving (10-point Likert scale). | Significantly greater increase in craving post-exposure in alcohol-cue environments compared to neutral environments. | Culturally relevant VR environments successfully triggered context-specific craving. |
| MUD Patients (n=89) [30] | VR-based CET vs. VR-based CET with Aversion Therapy (CETA) vs. Neutral Scenes (NS). | Tonic craving (VAS scale); Drug refusal self-efficacy (SELD scale). | Significant reduction in tonic craving in CET (p=0.001) and CETA (p=0.010) groups post-intervention; CETA improved drug refusal self-efficacy (p=0.001). | Immersive VR enables effective therapeutic interventions like extinction and aversion therapy with real-world impact. |
| Non-ADHD Adults (n=20) [76] | VR-based Continuous Performance Test ("Pay Attention!") with 4 difficulty levels. | Commission Errors (CE) - responding to a distractor. | Higher CE in "very high" difficulty level with complex stimuli and increased distraction. | VR can titrate environmental complexity and distraction, mimicking real-world cognitive demands. |
| Neuropsychological Assessment (n=41) [78] | VR Everyday Assessment Lab (VR-EAL) vs. traditional paper-and-pencil battery. | Participant ratings of ecological validity and pleasantness. | VR-EAL rated as significantly more ecologically valid and pleasant than traditional tests. | VR enhances the participant experience and provides a more realistic assessment of everyday cognitive functions. |
Detailed Experimental Protocols
To illustrate the practical application of VR in research, below are detailed methodologies from two pivotal studies.
- Objective: To develop and validate open-source, culturally relevant VR environments for alcohol cue exposure in an Indian population.
- Participants: 44 detoxified male inpatients with AUD.
- VR Hardware: Meta Quest 2 Head-Mounted Display (HMD).
- VR Environment Development:
- Software: Insta360 STUDIO 2023, SimLab VR studio.
- Cue Environments: Eight 360° skybox images depicting alcohol-related scenarios (e.g., living room with alcohol, party venue, bar, alcohol shop).
- Control Environments: Two neutral scenarios (a living room and an empty park).
- Procedure:
- Baseline Assessment: Collect sociodemographic data, alcohol use history, and baseline craving (Penn Alcohol Craving Scale, PACS).
- Pre-Exposure Craving: Report subjective craving on a 10-point Likert scale.
- VR Exposure: Participants explore each VR environment for 3 minutes in a randomized order.
- Post-Exposure Craving: Report subjective craving immediately after exposure.
- Washout: A 15-minute interval between environments to allow craving to subside.
- Presence Measurement: After all exposures, complete the Multimodal Presence Scale (MPS).
- Debriefing: A therapist conducts a session to minimize residual craving.
- Key Findings: The alcohol-cue environments induced a significant increase in craving compared to neutral environments. Regression analyses identified baseline craving and sense of presence as key determinants of the craving response.
- Objective: To develop an ecologically valid VR-based Continuous Performance Test (CPT) with varying difficulty levels for home-based assessment.
- Participants: 20 Korean adults without ADHD.
- VR Tool: "Pay Attention!" - A VR-based CPT program.
- Protocol Design:
- Environments: Four familiar real-life scenarios (room, library, outdoors, café).
- Difficulty Levels: Four distinct levels (Low to Very High), manipulating:
- Complexity of target and non-target stimuli.
- Level and type of environmental distraction.
- Inter-stimulus intervals.
- Procedure: Participants performed 1-2 blocks per day at home for two weeks, totaling 12 blocks. Psychological assessments and EEGs were administered pre- and post-program.
- Key Findings: The study confirmed the feasibility of home-based VR assessment. Commission errors were notably higher in the "very high" difficulty level, demonstrating the program's sensitivity in measuring attention under ecologically relevant, distracting conditions.
The Scientist's Toolkit: Essential Research Reagents
The following table details key hardware, software, and assessment tools required for implementing VR cue exposure research.
Table 2: Key Research Reagents for VR Cue Exposure Studies
| Item Category | Specific Examples | Function & Research Application |
|---|---|---|
| VR Hardware | Meta Quest 2 HMD [77] | Provides the immersive visual and auditory experience. Standalone capability enhances accessibility and scalability. |
| 360° Capture | Insta360 X3 Camera [77] | Creates high-resolution, 360° panoramic images for building culturally and contextually specific environments. |
| VR Development Software | Insta360 STUDIO, SimLab VR studio [77] | Edits 360° images and builds them into interactive VR environments for presentation via HMD. |
| Craving Assessment | Visual Analogue Scale (VAS) [30], Penn Alcohol Craving Scale (PACS) [77] | Measures the subjective intensity of craving, both as a state (tonic/cue-induced) and a trait. |
| Presence Measurement | Multimodal Presence Scale (MPS) [77] | Quantifies the user's sense of "being there" in the VR environment, a key mediator of efficacy. |
| Clinical Assessment | Addiction Severity Scales (e.g., MUDSS [30]), Anxiety/Depression scales (GAD-7, PHQ-9 [30]) | Provides clinical context and measures secondary outcomes like emotional state and addiction severity. |
Visualizing Experimental Workflows and Theoretical Frameworks
The following diagrams, generated using Graphviz DOT language, illustrate the core concepts and experimental workflows discussed.
Figure 1: VR Cue Exposure Experimental Workflow
Figure 2: Ecological Validity Framework in VR
The evidence unequivocally demonstrates that VR outperforms traditional laboratory-based cue exposure by fundamentally enhancing ecological validity. Its capacity to generate immersive, multisensory, and culturally relevant environments directly addresses the primary shortcoming of traditional methods—the inability to reliably generalize findings to real-world contexts. For researchers and drug development professionals, VR provides a more powerful and predictive tool for investigating the mechanisms of craving, testing novel pharmacotherapies, and delivering innovative behavioral interventions like exposure and aversion therapy [30].
Future research should focus on large-scale randomized controlled trials to establish long-term efficacy, standardize protocols across different substance use disorders, and further integrate VR with complementary technologies such as biofeedback and artificial intelligence for personalized and adaptive therapeutic interventions [45]. As the technology becomes more accessible and affordable, VR is poised to become an indispensable component of the methodological toolkit in behavioral neuroscience and addiction research.
Virtual Reality (VR) has transcended its origins as a simulation tool to become a powerful instrument in behavioral neuroscience research, capable of eliciting robust, measurable changes in the human nervous system. The core thesis is that VR experiences, though synthetic, induce real neurobiological changes through immersive, embodied simulations that engage fundamental brain processes. This whitepaper synthesizes current evidence for VR-induced neuroplasticity, detailing the specific biomarkers and imaging methodologies that validate its therapeutic and experimental applications. The ability of VR to evoke objective, quantifiable biological responses—from molecular adaptations to systemic neural reorganization—provides a compelling validation of its use in both basic research and clinical intervention frameworks.
Theoretical Frameworks for VR-Induced Neurobiological Change
The efficacy of VR in neuroscience is grounded in its unique capacity to create embodied simulations that the brain processes in a manner analogous to real-world experiences.
- Embodied Simulation Theory: Neuroscience posits that the brain maintains an embodied simulation of the body in the world to predict actions, concepts, and emotions. VR operates on a similar principle, providing a model that predicts the sensory consequences of a user's movements, thereby aligning with the brain's intrinsic predictive coding mechanisms [2]. This alignment is fundamental to VR's ability to modulate neural circuits.
- The Stressor-Stress Framework: A critical conceptual advance differentiates the virtual stressor (the input) from the physiological stress (the output). VR-based stressors, despite their artificial nature, have been meta-analytically validated to evoke a very real suite of stress responses with robust effect sizes across autonomic and adrenocortical biomarkers [79]. This demonstrates that the brain's response is not contingent on the physical reality of a threat, but on its perceived salience and immersive quality.
- Sense of Embodiment (SoE): In VR, the Sense of Embodiment—the feeling that a virtual body is one's own—is a multi-component experience comprising sense of ownership, agency, and self-location. A strong SoE is not merely subjective; it is linked to enhanced performance in motor imagery brain-computer interfaces (MI-BCIs) and is underpinned by specific electrophysiological patterns, supporting its role as a key mechanism for therapeutic engagement [80].
Electroencephalography (EEG) Biomarkers of VR Engagement
EEG provides a high-temporal-resolution window into the brain's electrical activity during VR immersion, offering quantifiable biomarkers for cognitive and sensory states.
Table 1: Key EEG Biomarkers in VR Research
| Biomarker / Feature | Neural Correlate & Significance | VR Context & Experimental Evidence |
|---|---|---|
| Increased Beta/Gamma Power | Signifies heightened cortical activity, sensory binding, and sensorimotor integration. | A significant increase over the occipital lobe is identified as a potential biomarker for the Sense of Embodiment during virtual body ownership illusions [80]. |
| EEG Microstates | Dynamic, quasi-stable states reflecting the coordination of large-scale brain networks. | Parameters of microstate classes (B, C, D) and their transition probabilities are altered following a VR intervention for cognitive fatigue, indicating a shift in global brain functional dynamics [81]. |
| Machine Learning Classification | Uses features from EEG signals (temporal, frequency, non-linear) to automatically classify cognitive states. | Algorithms (SVC, Random Forest, etc.) achieved 86-97% accuracy in classifying user states (idle, easy, hard VR tasks), establishing a method for real-time, objective assessment of immersion level [82]. |
Experimental Protocol: EEG Biomarkers of Embodiment
- Objective: To identify EEG biomarkers for the Sense of Embodiment (SoE) under standardized conditions [80].
- Participants: 41 participants in a combined dataset.
- VR Paradigm: SoE was systematically induced and disrupted using multisensory triggers (visuomotor, visuotactile) in a virtual environment. A validated questionnaire confirmed the successful induction of the embodiment illusion.
- EEG Acquisition: Continuous EEG was recorded during VR exposure.
- Analysis: Frequency band analysis (e.g., power in Beta and Gamma bands) was conducted, revealing significant increases over the occipital lobe during states of high embodiment.
Neuroimaging and Molecular Evidence of Neuroplasticity
Beyond EEG, evidence points to VR-induced changes at the molecular, synaptic, and systems levels, demonstrating its capacity to drive neuroplasticity.
- Molecular and Synaptic Plasticity: VR experiences can trigger molecular cascades that underpin learning and memory. This includes the modulation of neurotrophic factors like Brain-Derived Neurotrophic Factor (BDNF), which is crucial for neuronal survival, synaptic growth, and cognitive function. VR-induced environments promote synaptic adaptations through mechanisms such as Long-Term Potentiation (LTP), strengthening connections in circuits engaged during the virtual task [83].
- Cortical Reorganization: Neuroimaging studies show that VR-based rehabilitation leads to functional and structural reorganization in the brain. For example, in stroke recovery, VR training is associated with increased activation in sensorimotor cortices and changes in cortical connectivity, facilitating functional restoration [83].
- Stress Neurocircuitry: VR stressors reliably activate the Hypothalamic-Pituitary-Adrenal (HPA) axis, leading to increased cortisol secretion, and provoke autonomic nervous system responses, including elevated heart rate and galvanic skin response. These biomarker responses confirm that the brain interprets virtual threats in a biologically consequential manner [79].
Experimental Protocol: VR for Cognitive Fatigue Recovery
- Objective: To investigate the effect of a VR natural scene intervention on cognitive fatigue and its underlying neurophysiological alterations using EEG microstates analysis [81].
- Participants: 10 participants.
- Fatigue Induction & Intervention: Participants performed a 20-minute 1-back task (pre-task). Subsequently, they underwent a VR intervention featuring a simulation of a Canal Town scene.
- Behavioral & EEG Measures: Performance (accuracy, reaction time) and resting-state EEG were measured before (pre-task) and after (post-task) the VR intervention.
- Analysis: Four canonical EEG microstate classes (A-D) were identified. Temporal parameters (duration, coverage, occurrence) and transition probabilities were calculated.
- Key Results: Post-VR, behavioral performance improved. Microstate analysis revealed significant changes: decreased parameters in Class D, increased parameters in Class C, and altered transitions between classes, indicating a shift in global brain network dynamics associated with recovery from fatigue.
Table 2: Multimodal Biomarkers of VR-Induced Change
| Modality | Biomarker / Change | Associated VR Effect / Implication |
|---|---|---|
| EEG Oscillations | ↑ Beta/Gamma (Occipital) | Stronger Sense of Embodiment; multisensory integration [80]. |
| EEG Microstates | Altered parameters (Classes B, C, D) & transition probabilities | Recovery from cognitive fatigue; modulation of large-scale brain networks [81]. |
| Neuroendocrine | ↑ Cortisol (Salivary) | Activation of the HPA axis in response to a virtual psychosocial stressor [79]. |
| Autonomic | ↑ Heart Rate, Galvanic Skin Response | Sympathetic nervous system arousal during virtual challenges or threats [79]. |
| Molecular | BDNF modulation, LTP-like synaptic strengthening | Foundation for long-term learning, memory, and neurorehabilitation [83]. |
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for VR Biomarker Research
| Item / Solution | Function in Research |
|---|---|
| High-Fidelity Head-Mounted Display (HMD) | Provides the immersive visual and auditory stimulus. Critical for inducing presence and embodiment. Examples: HTC Vive, Oculus Rift [84] [82]. |
| Electroencephalography (EEG) System | Records millisecond-level electrical brain activity to identify spectral biomarkers (e.g., Beta/Gamma) or microstates. Often integrated with the HMD [80] [81] [82]. |
| Biochemical Assay Kits (e.g., Salivary) | For quantifying stress and neuroplasticity biomarkers like cortisol (HPA axis) and alpha-amylase (sympathetic activity) from saliva samples [79]. |
| Validated Psychometric Questionnaires | Subjective measures for cross-validation. Examples: VRNQ (VR-induced symptoms), SSQ (simulator sickness), embodiment questionnaires [80] [84]. |
| Motion Tracking System | Tracks body and limb movements for visuomotor synchrony, a key trigger for agency and embodiment. Often built into modern HMDs [80] [84]. |
The convergence of evidence from EEG, neuroendocrine, autonomic, and molecular neuroscience firmly establishes that VR is a potent tool for inducing measurable and functionally significant neurobiological change. The identification of specific biomarkers, such as occipital beta/gamma power for embodiment or EEG microstate shifts following intervention, moves the field beyond subjective reporting and provides a robust, objective foundation for validating VR's use in research and therapy. This neurobiological validation underscores VR's unique capacity as an "ideal stressor" and a powerful driver of neuroplasticity, enabling the precise titration of virtual experiences to elicit targeted, therapeutically relevant neural responses. Future research, integrating advanced molecular imaging with real-time biomarker feedback, will further solidify VR's role in creating personalized and precise interventions in behavioral neuroscience and clinical neurorehabilitation.
The adoption of Virtual Reality (VR) in behavioral neuroscience and clinical research has accelerated markedly, promising new avenues for diagnosis, treatment, and skill acquisition. A central, critical question for researchers and drug development professionals is whether skills and learning acquired in these controlled, synthetic environments demonstrate generalization and lead to sustained, long-term outcomes in the real world. The challenge of skills transfer—the successful application of virtually acquired learning to real-world settings—remains a significant hurdle for the field [85]. This whitepaper examines the evidence for and against the transfer of learning from VR to reality, framed within theoretical models of learning and behavioral change. It further provides a detailed analysis of experimental methodologies and practical tools to help researchers design studies that robustly measure and promote this crucial transfer, with the ultimate goal of validating VR as a reliable instrument in behavioral neuroscience and clinical trials.
Theoretical Frameworks for Learning and Transfer in VR
The process of learning and transfer in VR is underpinned by several key theoretical frameworks that explain how virtual experiences can lead to real-world behavioral change.
The BehaveFIT Framework: Bridging the Intention-Behavior Gap
The Behavioral Framework for immersive Technologies (BehaveFIT) posits that VR can overcome well-documented psychological barriers that create the "intention-behavior gap"—the failure to translate intentions into actions [86]. This framework provides a structured mapping between immersive technological features and the psychological determinants of behavior.
Embodied Simulation and Constructivist Learning
From a neuroscientific perspective, a key mechanism for VR's efficacy is embodied simulation. The brain inherently uses simulation to regulate the body, and VR functions similarly by predicting the sensory consequences of a user's movements [2]. This alignment between the brain's internal modeling and the VR system's external simulation provides a powerful foundation for learning. This process is consistent with constructivist learning theory, where learners actively build meaningful mental models by organizing sensory input. In VR, this occurs when users can simultaneously hold a visual representation in their visual working memory and a corresponding verbal representation in their verbal working memory [85]. The challenge, however, is that the significant cognitive load imposed by multisensory VR environments can impede this process, particularly in populations with cognitive deficits [85].
Empirical Evidence: Quantifying Transfer and Long-Term Outcomes
The following section summarizes empirical evidence for the transfer of learning across different domains, including clinical populations, motor learning, and cognitive training.
Table 1: Empirical Evidence for VR Learning Transfer to Real World
| Domain / Study | VR Intervention / Protocol | Key Real-World Outcome Measures | Evidence of Transfer & Long-Term Benefit |
|---|---|---|---|
| Mental Health & Substance Use (MHD/SUD) [85] | Social skills training in multisensory VR environments; short, focused, and repeatable VRI scenarios. | Social participation, functional recovery, daily life skills, and psychological well-being. | Limited but promising. Sustained benefits require designs that accommodate attention and memory deficits. Sequenced learning workflows promote storage of repaired schemas in long-term memory. |
| Anxiety Disorders & PTSD [2] | Virtual Reality Exposure Therapy (VRET); graded exposure to fear-inducing stimuli in a safe, controlled environment. | Reduction in anxiety symptoms, avoidance behavior, and physiological arousal in real-world situations. | Strong evidence. VRET is equally or more effective than conventional exposure therapy, with long-term effects that generalize to the real world. |
| Motor Skill Acquisition [87] | Quiet Eye Training (QET) for golf putting; gaze behavior training followed by practice in VR or real-world. | Real-world golf putting performance (radial error, number of successful putts). | Positive transfer. QET in VR improved real-world performance irrespective of subsequent practice environment. Real-world skills also transferred to VR. |
| Neuroscience of Behavioral Change [2] | VR environments designed to alter the embodied simulation of the body and world (e.g., for pain or eating disorders). | Changes in body perception, emotional response, and cognitive schemas. | Promising. VR's capacity to simulate both external and internal worlds offers a new clinical approach for facilitating cognitive and behavioral change. |
Challenges and Limitations in Transfer
Despite promising results, the transfer of learning is not automatic. Research indicates that the human capacity to achieve sustained learning outcomes from multisensory VR is generally limited [85]. This is particularly pronounced in populations with mental health and substance use disorders, who often struggle with attention, concentration, and memory, affecting their daily functioning and learning uptake [85]. Furthermore, a study on golf putting revealed that while skills learned in the real world effectively transferred to VR, the reverse was not universally true; participants who practiced only in VR did not show the same improvement in real-world radial error, suggesting that skills practiced in VR may need additional, targeted training to facilitate real-world transfer [87].
Experimental Design and Methodologies for Measuring Transfer
For researchers designing VR intervention studies, robust experimental protocols are essential for accurately assessing learning and transfer.
Protocol for Assessing Skill Transfer (Quiet Eye Training Study)
This protocol, derived from a study on motor skill transfer, provides a template for a randomized controlled trial [87].
- Participants: Novice adults (e.g., N=46) with no prior experience in the target skill.
- Baseline Assessment: Measure real-world performance (e.g., golf putting accuracy, radial error) and relevant psychophysiological data (e.g., eye-gaze).
- Randomization: Randomly assign participants to experimental conditions (e.g., QET vs. no training, VR practice vs. real-world practice).
- Training Phase: Administer the targeted training (e.g., QET). The practice following this training can occur in VR or the real-world, depending on the condition.
- Post-Training Assessment: Immediately after training, re-measure real-world performance and psychophysiological data.
- Retention Test: Re-assess the same outcomes after a delay (e.g., one week) to measure long-term retention and sustained learning.
- Data Analysis: Compare performance improvements from baseline to post-training and baseline to retention across conditions to isolate the effect of VR training on real-world skill transfer.
Protocol for Designing VR Interventions for Clinical Populations (MHD/SUD)
This protocol focuses on designing VRIs for populations with cognitive challenges [85].
- Theoretical Foundation: Base the learning experience design on experiential learning theory and constructivist learning principles.
- Scaffolded Learning Workflow: Orchestrate learning activities in a sequenced, deliberately structured workflow. Break down complex social skills into short, focused VRI scenarios.
- Cognitive Load Management: Design scenarios that can be repeated to accommodate memory and attention deficits. The goal is to enable the restructuring of maladaptive social schemas and promote storage in long-term memory.
- Ecological Validity Assessment: The primary outcome should be the improvement of functioning, daily life skills, and social participation in real-world settings, not just performance within the VR environment.
Table 2: Research Reagent Solutions for VR Experiments
| Tool / Resource | Primary Function | Relevance to Transfer Research |
|---|---|---|
| Head-Mounted Displays (HMDs) (e.g., HTC Vive, Varjo, Oculus) [88] [89] | Provides the immersive visual experience. | Different HMDs have varying levels of fidelity and color accuracy, which can influence the realism of the simulation and thus the potential for transfer. |
| Game Engines (Unity, Unreal Engine) [88] | Software environment for creating and rendering the virtual environment. | The choice of engine and its rendering settings (e.g., color space, post-processing) can significantly impact the visual stimuli, affecting ecological validity and experimental control. |
| Eye-Tracking Integration (e.g., HTC Vive Pro Eye) [87] [90] | Measures user's point of gaze and visual attention. | Critical for protocols like Quiet Eye Training and for objectively measuring cognitive load and attention during VR tasks, which are predictors of learning success. |
| Color Calibration Tools (Spectroradiometer, Imaging Colorimeter) [88] | Characterizes and calibrates the color output of an HMD. | Ensures visual stimulus fidelity and consistency across devices and sessions, a prerequisite for reproducible psychophysical and neuroscience research. |
| Cybersickness Prediction Models (e.g., InceptionV3 + LSTM on video data) [90] | Predicts user discomfort from gameplay videos or sensor data. | Mitigates a major confound; high cybersickness can impair learning and lead to participant dropout, jeopardizing long-term outcome data. |
| Open-Source Medical Imaging XR (MIXR) [91] | Displays medical imaging data (CT, MRI) in AR/VR on portable devices. | Useful for creating highly realistic clinical training scenarios (e.g., for surgical planning or patient communication) to test transfer to clinical settings. |
The question of whether learning in VR transfers to the real world does not have a simple yes-or-no answer. The current body of research demonstrates that transfer is achievable and can be long-lasting, particularly when VR interventions are thoughtfully designed based on established principles from neuroscience and psychology. Key success factors include leveraging embodied simulation, managing cognitive load, employing scaffolded and repetitive learning workflows, and directly targeting the psychological barriers that maintain the intention-behavior gap. For researchers in behavioral neuroscience and drug development, the imperative is to move beyond simply demonstrating efficacy within the VR environment. The future lies in designing studies with robust, longitudinal methodologies that explicitly measure and optimize for the generalization of skills and the sustainability of outcomes in the complex and unpredictable real world. VR is not a panacea, but when applied with theoretical rigor and methodological precision, it is a powerful tool for fostering meaningful and lasting behavioral change.
Conclusion
The integration of VR into behavioral neuroscience is firmly grounded in powerful theoretical frameworks, most notably embodied simulation, which explains its unique efficacy by aligning with the brain's own predictive processes. The methodological applications, from VRET to cue exposure, demonstrate significant promise across a spectrum of disorders, validated by growing evidence of their comparative efficacy and capacity to induce meaningful neuroplasticity. However, the field must overcome substantial challenges related to methodological rigor, accessibility, and ethics to achieve widespread clinical implementation. The future of VR in behavioral neuroscience points toward highly personalized, data-driven interventions. The integration with artificial intelligence, biofeedback, and molecular neuroscience, as seen in the emerging 'VRID' (Virtual Reality Inspired Drugs) concept, suggests a transformative path forward. This synergy will not only refine therapeutic protocols but also open novel avenues for understanding disease mechanisms and accelerating drug discovery, ultimately bridging the gap between controlled virtual environments and real-world clinical outcomes.
References
- 1. The Neuroscience of Virtual Reality & Health [https://axonpark.com/the-neuroscience-of-virtual-reality-and-health/]
- 2. Neuroscience of Virtual Reality: From Virtual Exposure to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6354552/]
- 3. Being there but where? Sense of presence theory for ... [https://www.nature.com/articles/s41599-025-04380-3]
- 4. A psychological framework for social skill acquisition in ... [https://www.sciencedirect.com/science/article/pii/S2451958825001800]
- 5. A How-to-Model Guide for Neuroscience [https://www.eneuro.org/content/7/1/ENEURO.0352-19.2019]
- 6. Increasing presence via a more immersive VR system ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2024.1452486/full]
- 7. The use of virtual reality technology in the treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5421394/]
- 8. Considerations and practical protocols for using virtual ... [https://link.springer.com/article/10.3758/s13428-021-01543-3]
- 9. VR-Enhanced Cognitive Learning: Method, Framework, ... [https://www.mdpi.com/2076-3417/13/8/4756]
- 10. Use of emerging technologies in rehabilitation education and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12375567/]
- 11. Virtual Reality Clinical Trials: Step Inside the Future of ... [https://ccrps.org/clinical-research-blog/virtual-reality-clinical-trials-step-inside-the-future-of-medicine-2025]
- 12. Psychophysiological Markers of Performance and Learning ... [https://pubmed.ncbi.nlm.nih.gov/34496403/]
- 13. Behaviorism, Cognitivism, Constructivism: Comparing ... [https://uark.pressbooks.pub/edtech/chapter/40/]
- 14. Virtual Reality in Cognitive and Affective Neuroscience [https://www.sciencedirect.com/science/article/abs/pii/S0166432825003961]
- 15. Virtual reality programs targeting executive functions and ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2025.1583052/full]
- 16. Brain Neuroplasticity Leveraging Virtual Reality and Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11397861/]
- 17. Virtual Reality for Neurorehabilitation: Mechanisms, Modalities ... [https://currents.neurocriticalcare.org/Leading-Insights/Article/virtual-reality-for-neurorehabilitation-mechanisms-modalities-and-clinical-applications]
- 18. Effects of Virtual Reality Cognitive Training on Neuroplasticity [https://pmc.ncbi.nlm.nih.gov/articles/PMC10740852/]
- 19. A virtual reality-based multimodal framework for adolescent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12484203/]
- 20. Integrating Virtual Reality, Neurofeedback, and Cognitive ... [https://www.researchprotocols.org/2025/1/e63405]
- 21. Current status of virtual reality researches at healthcare [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1411075/full]
- 22. Virtual Humans in Virtual Reality Mental Health Research [https://xr.jmir.org/2025/1/e75087]
- 23. Clinical Virtual Reality: Emerging Opportunities for Psychiatry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6493092/]
- 24. SONIA: an immersive customizable virtual reality system for ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2023.1244096/full]
- 25. Examining the comparative effectiveness of virtual reality ... [https://www.sciencedirect.com/science/article/pii/S2589979125000046]
- 26. Virtual Reality in Pharmacy: Opportunities for Clinical, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6487969/]
- 27. AR/VR's Potential in Health Care [https://itif.org/publications/2025/06/02/arvrs-potential-in-health-care/]
- 28. The Use of Virtual Reality in Craving Assessment and Cue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4201090/]
- 29. Exploring the relationship between cue-induced craving and ... [https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-025-06986-y]
- 30. Virtual reality-based cue exposure therapy reduces ... [https://www.nature.com/articles/s41398-025-03553-7]
- 31. Craving induction through virtual reality cue-exposure for ... [https://www.nature.com/articles/s41598-024-81071-0]
- 32. Eliciting real cravings with virtual food: Using immersive ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2023.956585/full]
- 33. A Systematic Review of Virtual Reality Therapies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10557052/]
- 34. Effectiveness of a virtual reality-based cognitive training ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2025.1653783/full]
- 35. Reality as an Innovative Tool for Virtual ... Eating Disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC11610927/]
- 36. Comparative Efficacy of Virtual Reality–Assisted Cognitive ... [https://www.researchprotocols.org/2025/1/e66112]
- 37. Understanding VR for Cognitive Behavioral Therapy (CBT) [https://psytechvr.com/vr-for-cognitive-behavioral-therapy]
- 38. Virtual reality in cognitive and affective neuroscience [https://pubmed.ncbi.nlm.nih.gov/40939870/]
- 39. Effectiveness of VR-based cognitive training and games on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634598/]
- 40. Cognitive rehabilitation using virtual reality in subjective ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2025.1641693/full]
- 41. Exploring the potential of virtual reality (VR) in mental ... [https://link.springer.com/article/10.1007/s10055-025-01181-6]
- 42. Efficacy of Virtual Reality–Based Interventions on Cognitive ... [https://games.jmir.org/2025/1/e67501]
- 43. The effectiveness of digital cognitive intervention in patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537419/]
- 44. Cognitive Behavioral Therapy Techniques Enhanced with ... [https://www.xr.health/us/blog/cognitive-behavioral-therapy-techniques/]
- 45. Virtual Reality: Challenges and Perspectives in Mental Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593772/]
- 46. A Survey on Methodological Approaches to Collaborative ... [https://arxiv.org/html/2507.18877v1]
- 47. Exploring the impact of virtual reality on presence: findings ... [https://www.frontiersin.org/journals/education/articles/10.3389/feduc.2025.1560626/full]
- 48. Efficacy of Virtual Reality–Based Interventions on Cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12080969/]
- 49. Effectiveness of VR-based cognitive training and games on ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1691344/full]
- 50. Effectiveness of Virtual Reality–Based Cognitive Control ... [https://pediatrics.jmir.org/2025/1/e66617]
- 51. Evolving Clinical Studies – Interventions to Watch in 2025 [https://communities.springernature.com/posts/evolving-clinical-studies-interventions-to-watch-in-2025]
- 52. A quantitative assessment of the hand kinematic features ... [https://www.nature.com/articles/s41598-025-91552-5]
- 53. NeuroGaze: a hybrid EEG and eye-tracking brain-computer ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1695446/full]
- 54. Virtual Reality Awareness and Adoption Report [https://www.security.org/digital-security/virtual-reality-annual-report/]
- 55. Cybersickness Prevention and Mitigation in Virtual Reality for ... [https://www.centerwatch.com/clinical-trials/listings/NCT06552754/cybersickness-prevention-and-mitigation-in-virtual-reality-for-healthy-volunteers]
- 56. Exploring the Barriers to and Facilitators of Using Virtual ... [https://www.jmir.org/2025/1/e65308]
- 57. What Are the Ethical Issues Surrounding Extended Reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561320/]
- 58. Exploring the Application of AI and Extended Reality ... [https://www.jmir.org/2025/1/e72400]
- 59. Ethical concerns in contemporary virtual reality and ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1451273/full]
- 60. A Comparative Analysis of 2D and 3D Tasks for Virtual ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2016.00205/full]
- 61. A systematic literature review and meta‐analysis of virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411694/]
- 62. A Systematic Review of Personalized Interaction in VR [https://arxiv.org/html/2510.13123v1]
- 63. How Virtual Reality and Gamification Are Revolutionizing ... [https://www.avrwell.com/blog/the-future-of-physical-therapy-how-virtual-reality-and-gamification-are-revolutionizing-rehabilitation]
- 64. A Smartphone-Gamified Virtual Reality Exposure Therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10955409/]
- 65. Virtual Reality (VR) Strategic Insights: Analysis 2025 and ... [https://www.archivemarketresearch.com/reports/virtual-reality-vr-362280]
- 66. Tutorials [https://ieeevis.org/year/2025/info/program/tutorials]
- 67. Virtual Reality Clinical Research: Promises and Challenges [https://games.jmir.org/2018/4/e10839/]
- 68. Recommendations for Methodology of Virtual Reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6374734/]
- 69. Patient Perceptions of In Vivo Versus Virtual Reality ... [https://formative.jmir.org/2023/1/e47443/]
- 70. The gold-standard treatment for social anxiety disorder [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2022.1070975/full]
- 71. A Meta-Analysis of the Efficacy of Virtual Reality and In ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9158252/]
- 72. Studying human behavior with virtual reality: The Unity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7148262/]
- 73. Virtual reality analytics map (VRAM): A conceptual ... [https://www.sciencedirect.com/science/article/pii/S0732118X24000552]
- 74. PROTOCOL: Effects of virtual reality exposure therapy versus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9246294/]
- 75. Virtual Reality in Prevention and Treatment of Substance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12374077/]
- 76. Advancing ecological and clinical utility in virtual reality-based... validity [https://pmc.ncbi.nlm.nih.gov/articles/PMC10832060/]
- 77. Development and validation of an open-source virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12331004/]
- 78. cambridge.org/core/journals/journal-of-the-international... [https://www.cambridge.org/core/journals/journal-of-the-international-neuropsychological-society/article/abs/validation-of-the-virtual-reality-everyday-assessment-lab-vreal-an-immersive-virtual-reality-neuropsychological-battery-with-enhanced-ecological-validity/F926BE0A614A57245E81F1B746DEF4AF]
- 79. Virtual stressors with real impact: what virtual reality-based ... [https://www.nature.com/articles/s41398-024-03129-x]
- 80. Identifying EEG biomarkers of sense of embodiment in virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12104197/]
- 81. Neuroimaging features for cognitive fatigue and its ... [https://www.sciencedirect.com/science/article/pii/S0361923025000358]
- 82. Biomarkers of Immersion in Virtual Reality Based on ... [https://www.mdpi.com/2076-3425/14/5/470]
- 83. Review Virtual reality modulating dynamics of neuroplasticity [https://www.sciencedirect.com/science/article/abs/pii/S0306452224007474]
- 84. Validation of the Virtual Reality Neuroscience Questionnaire [https://pmc.ncbi.nlm.nih.gov/articles/PMC6901952/]
- 85. Promoting Sustained Real-Life Benefits of Virtual Reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12367355/]
- 86. Behavioral Framework of Immersive Technologies ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2021.627194/full]
- 87. Quiet Eye Training in Virtual Reality and in the Real-World [https://www.sciencedirect.com/science/article/pii/S0167945725000521]
- 88. High-fidelity color characterization in virtual reality across ... [https://opg.optica.org/oe/fulltext.cfm?uri=oe-32-13-22388]
- 89. Virtual Reality Statistics 2025: Users & Trends [https://www.demandsage.com/virtual-reality-statistics/]
- 90. Towards Cybersickness Severity Classification from VR ... [https://arxiv.org/html/2510.10422v1]
- 91. VR-prep improves visualization of medical data in ... [https://www.nature.com/articles/s41598-025-26856-7]