Virtual Reality Exposure Therapy for Anxiety Disorders: A Comprehensive Review of Efficacy, Mechanisms, and Clinical Translation
This article provides a comprehensive analysis of Virtual Reality Exposure Therapy (VRET) for anxiety disorders, tailored for researchers, scientists, and drug development professionals.
Virtual Reality Exposure Therapy for Anxiety Disorders: A Comprehensive Review of Efficacy, Mechanisms, and Clinical Translation
Abstract
This article provides a comprehensive analysis of Virtual Reality Exposure Therapy (VRET) for anxiety disorders, tailored for researchers, scientists, and drug development professionals. It synthesizes foundational theories and the evidence base for VRET, detailing its application across specific phobias, social anxiety, and PTSD. The review examines methodological protocols, practical implementation challenges, and strategies for optimization. Furthermore, it critically evaluates comparative efficacy data against traditional therapies and active control conditions, addressing the current state of validation and identifying key frontiers for future clinical research and biomedical innovation.
The Science and Evidence Base of VRET: From Theory to Clinical Reality
Application Notes: Theoretical Foundations in VR Exposure Therapy
Virtual Reality Exposure Therapy (VRET) has emerged as an effective treatment for anxiety disorders, with its mechanisms explained by several dominant theoretical frameworks. Emotional Processing Theory (EPT) posits that fear is represented as a cognitive structure in memory, containing information about feared stimuli, fear responses, and their meanings [1] [2]. According to this model, successful exposure therapy requires first activating this fear structure and then introducing corrective information to modify it [3] [2]. Within VRET, this translates to presenting patients with virtual representations of feared situations sufficient to elicit fear activation, followed by prolonged exposure that facilitates within-session and between-session habituation [3] [4].
While EPT has been foundational, contemporary research also recognizes other crucial mechanisms. The Inhibitory Learning Model emphasizes creating new, non-threat associations that compete with existing fear associations, primarily through expectancy violation - when a patient's expected negative outcome does not occur [3] [2]. Self-Efficacy Theory suggests exposure works by strengthening patients' belief in their ability to cope with anxiety-provoking situations [3] [1]. For researchers, understanding this multi-mechanistic framework is essential for optimizing VRET protocols and interpreting experimental outcomes.
The simulated nature of VR presents both opportunities and challenges for these mechanisms. VRET allows for fine-tuned manipulation of exposure scenarios, enabling researchers to systematically control difficulty levels [1]. However, since patients know the virtual environment isn't real, the role of expectancy violation becomes theoretically complex, as some objectively feared outcomes (e.g., actual social rejection) cannot occur in VR [4]. Despite this, VRET demonstrates clinical effectiveness, possibly because patients still experience subjective realism and can violate expectations about their own internal reactions (e.g., "I won't be able to cope") [1].
Key Mechanistic Constructs and Their Operational Definitions
Table 1: Core Mechanisms in Exposure Therapy and Their Measurement Approaches
| Mechanistic Construct | Theoretical Origin | Operational Definition | VRET-Specific Considerations |
|---|---|---|---|
| Fear Activation/Emotional Engagement | Emotional Processing Theory | Elevation of subjective/physiological fear at exposure onset; necessary for memory reconsolidation [2] | VR environments must provide sufficient immersion/presence to activate fear structures [5] |
| Within-Session Extinction (Habituation) | Emotional Processing Theory | Decline of fear response within a single exposure session [2] [4] | Session duration and stimulus intensity can be precisely controlled in VR [6] |
| Between-Session Extinction (Habituation) | Emotional Processing Theory | Decline of peak fear response across multiple exposure sessions [2] | Enables tracking of fear reduction across standardized, replicable VR scenarios [3] |
| Expectancy Violation | Inhibitory Learning Model | Experience of "surprise" when expected threat does not occur during exposure [3] [2] | Limited for outcomes that cannot virtually occur; more relevant for internal/coping expectations [4] |
| Self-Efficacy | Self-Efficacy Theory | Strengthened belief in one's capability to cope with anxiety-provoking situations [3] [1] | VR success experiences build confidence through mastery of progressively challenging scenarios [1] |
Quantitative Evidence Synthesis
Recent meta-analytic evidence supports VRET's efficacy relative to control conditions and traditional in-vivo exposure. The table below summarizes key quantitative findings from recent systematic reviews and meta-analyses.
Table 2: Comparative Efficacy of VRET and In-Vivo Exposure for Anxiety Disorders
| Study Focus | Comparison Groups | Effect Size Estimate | Outcome Measures | Clinical Implications |
|---|---|---|---|---|
| Specific Phobia & Social Anxiety [7] | VRET vs. IVET | Moderate, comparable effect sizes for both approaches | Reduction in phobia and anxiety symptoms | VRET generates positive outcomes comparable to in-vivo exposure [7] |
| Social Anxiety in Adolescents [3] | VRE vs. IVE vs. WL (Hypothesized) | Large pre-post effects (g=0.99) for CBT-based exposure [3] | SPAI-18, LSAS-avoidance, SPWSS | Both exposure modalities expected to significantly reduce symptoms vs. waitlist [3] |
| Public Speaking Anxiety [3] | Single-session VRET | Large reduction sustained at 1-3 month follow-ups | Public speaking anxiety measures | Brief VR interventions can produce durable effects for specific social fears [3] |
Experimental Protocols
Objective: To evaluate the efficacy and mechanisms of VR exposure versus in-vivo exposure for socially anxious adolescents.
Population: 120 adolescents (ages 12-16) with subclinical to moderate social anxiety, randomized to VRE, IVE, or waitlist control.
Session Structure (7 sessions):
- Psychoeducation and Fear Hierarchy Development: Identify 10-15 feared social situations; create individualized VR hierarchy.
- Initial Exposure Session: Begin with moderately anxiety-provoking scenarios (e.g., speaking to a small group of virtual avatars).
- Graduated Exposure Sessions: Progressively implement more challenging scenarios based on subjective units of distress (SUDS) ratings.
- Final Mastery Session: Conduct exposure to most challenging scenarios (e.g., presenting to a large, distracted audience).
Mechanism Assessments:
- Fear Activation: Peak SUDS during first 5 minutes of exposure [2]
- Within-Session Habituation: SUDS reduction from peak to end of session [2]
- Between-Session Habituation: Peak SUDS comparison across sessions [2]
- Self-Efficacy: Self-report confidence in handling social situations [3]
- Expectancy Violation: Pre-post exposure ratings of expected vs. actual outcomes [3]
Measures Timeline: Baseline, post-treatment (8 weeks), 3-month follow-up, 6-month follow-up.
Objective: To examine the feasibility and efficacy of telemedicine-based VR exposure for animal phobias.
Population: 30-60 adults with intense fear of dogs, snakes, or spiders, randomized to telemedicine-VR versus standard telemedicine.
VR Platform: Doxy.me VR clinic with animal exposure stimuli (dogs, snakes, spiders) with multiple exemplars and behavior states (idle, calm, active, aggressive) [6].
Exposure Implementation:
- Therapist Control: Therapist selects, rotates, and manipulates animals in VR environment before making visible to client.
- Graduated Exposure: Begin with static images/videos (standard TMH) or idle/calm animals (VR), progressing to active/aggressive states.
- Between-Session Practice: Clients access homework mode for self-guided exposure with full control features.
Outcome Assessment:
- Feasibility Metrics: Enrollment, retention, assessment completion, treatment fidelity.
- Clinical Outcomes: Specific phobia symptoms, anxiety, depression, therapeutic alliance, presence.
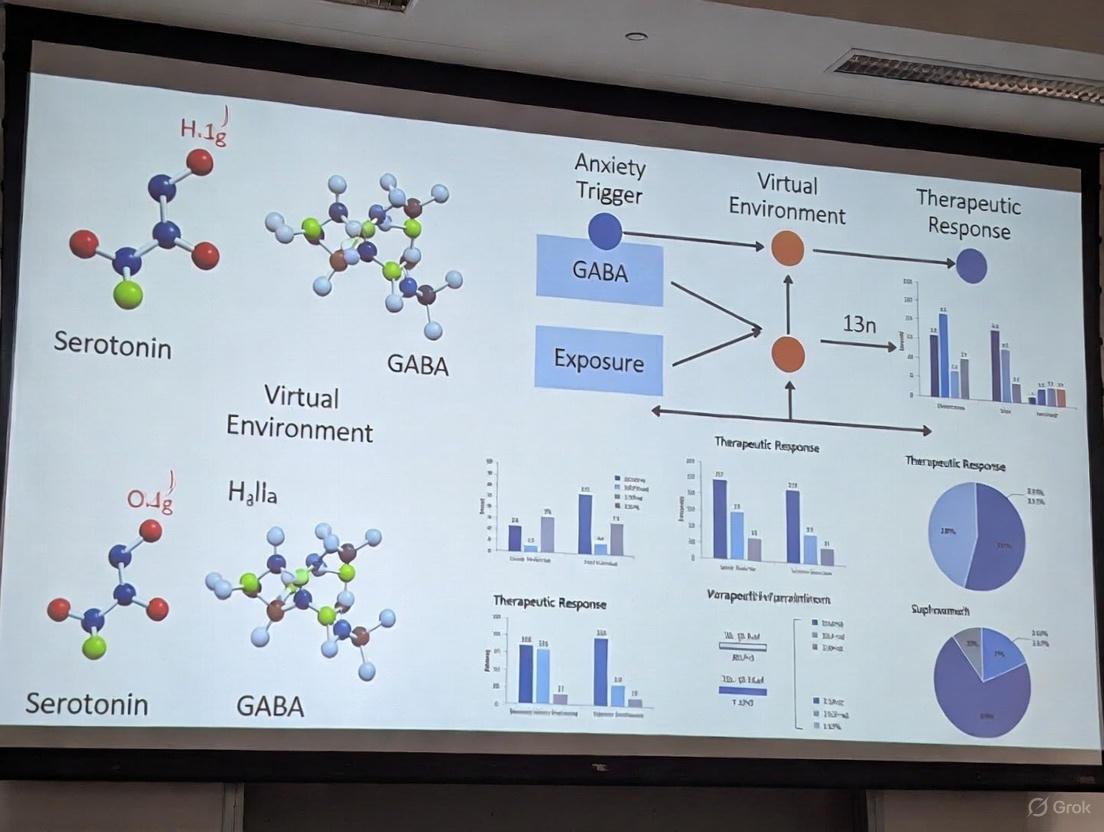
Mechanism Visualization
Theoretical Mechanisms of VR Exposure Therapy
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Platforms for VRET Research
| Research Tool | Function/Application | Research Context |
|---|---|---|
| Head-Mounted Displays (HMDs) | Provide immersive 360° visual/auditory experience; critical for presence induction [5] | Meta Quest 2 used in telemedicine trials [6]; various commercial HMDs for clinical research |
| Doxy.me VR Platform | Telemedicine VR clinic with controlled exposure stimuli (animals, social situations) [6] | Feasibility RCT for specific phobia; enables therapist-client interaction in VR environment [6] |
| Standardized Anxiety Measures | Quantify treatment outcomes and mechanism engagement | SPAI-18, LSAS-avoidance for social anxiety [3]; SUDS for in-session fear [2] |
| Presence Questionnaires | Assess subjective sense of "being there" in virtual environment | Critical mediator of VRET effectiveness; measures realism and immersion [5] |
| Behavioral Approach Tests | Objective measure of avoidance reduction pre/post treatment | Standardized assessment of functional improvement; can be in-vivo or VR-based |
| Physiological Monitoring | Objective measure of fear activation/habituation | Heart rate variability, skin conductance, cortisol measurement complement self-report |
In the realm of virtual reality exposure therapy (VRET) for anxiety disorders, the therapeutic efficacy is fundamentally governed by the ability of the virtual environment to elicit appropriate and controlled fear responses. This is achieved through the core technological principles of immersion, presence, and interactivity [8]. For researchers and clinicians, a precise understanding of these principles is not merely academic; it is essential for designing valid, effective, and reproducible digital therapeutics.
- Immersion is an objective property of the technology, referring to the extent to which a VR system can deliver a vivid, multi-sensory, and contiguous virtual environment while shutting out the physical world [9] [8].
- Presence, also known as "place illusion," is the user's subjective psychological response to the immersive system—the feeling of "being there" in the virtual environment [9] [8].
- Interactivity, or "agency," is the degree to which users can initiate and execute actions within the virtual environment and perceive plausible consequences from those actions [10] [8].
The synergy of these principles is critical in a research context. High immersion supports a strong sense of presence, which in turn is a key factor in motivating user compliance and engagement, leading to higher retention rates in clinical trials [9]. Furthermore, realistic interactivity facilitates the illusion of embodiment—the perception that one has a virtual body—which can heighten emotional intensity and improve treatment outcomes [9]. For VRET, this means that successfully inducing presence is paramount for activating the patient's core fears, thereby creating the conditions necessary for inhibitory learning and fear extinction to occur [3] [11].
Core Principles and Quantitative Definitions
A rigorous, quantitative approach to defining these principles is necessary for standardizing research methodologies and comparing findings across studies. The following table summarizes key metrics and technological factors that operationalize these concepts in experimental settings.
Table 1: Quantitative and Technological Definitions of Immersive VR Principles
| Principle | Definition | Key Technological & Subjective Metrics | Impact in VRET Research |
|---|---|---|---|
| Immersion | The objective level of sensory fidelity and breadth of information delivered by the VR system [9] [8]. | - Field of View (FoV): >100° diagonal is considered wide [9].- Display Resolution: e.g., 4K (3840x2160) per eye to reduce screen-door effect.- Refresh Rate: ≥90 Hz to minimize latency and cybersickness [10].- Tracking Accuracy: 6 Degrees of Freedom (6DoF) with sub-millimeter precision [12].- Audio: High-fidelity spatial (3D) audio. | Higher immersion correlates with a greater potential for inducing presence, making the exposure scenario more potent and ecologically valid for triggering anxiety [9] [8]. |
| Presence | The subjective feeling of "being there" in the virtual environment [8]. | - Presence Questionnaire (PQ) [8].- Slater-Usoh-Steed (SUS) Questionnaire [8].- Physiological Measures: Heart rate, skin conductance (Galvanic Skin Response), EEG correlates of arousal [8].- Behavioral Measures: Startle responses, body sway, and other unconscious behaviors [8]. | A strong sense of presence is vital for activating the fear structure in patients with anxiety disorders, enabling corrective learning during exposure sessions [3] [11]. |
| Interactivity | The degree to which users can manipulate the virtual environment and receive feedback [10]. | - Tracking Latency: <20 ms from movement to display update is critical [10].- Haptic Fidelity: Type and bandwidth of haptic feedback (e.g., vibration, force feedback).- Physics Engine Realism: Accuracy of object manipulation and collision detection [10].- Agency Questionnaires: Subjective ratings of control over virtual actions. | Realistic interaction enhances the "plausibility illusion," making the virtual world's reactions to a patient's actions believable. This is key for violating threat expectancies (e.g., "If I speak, everyone will laugh") [10] [8]. |
The relationship between these principles can be visualized as a dependency chain where technological capabilities enable psychological experiences that drive therapeutic outcomes.
Experimental Protocols for Evaluating VR Principles in Clinical Research
For research on VRET for anxiety disorders, it is essential to have standardized protocols for quantifying and validating the immersive properties of the VR environments used. Below are detailed methodologies for key experiments.
Protocol: Quantifying Presence and Immersion in a VRET Public Speaking Scenario
This protocol is designed to assess the efficacy of a VR public speaking environment intended for Social Anxiety Disorder (SAD) research.
- Objective: To measure the levels of subjective presence and physiological correlates of anxiety elicited by a VR public speaking task.
- Hypothesis: The VR environment will induce a significant sense of presence and a physiologically measurable anxiety response comparable to anticipatory anxiety in a real-world setting.
- Materials:
- VR System: A standalone or PC-powered head-mounted display (HMD) with a minimum refresh rate of 90 Hz and 6DoF tracking.
- Software: A virtual auditorium environment with a dynamic audience capable of neutral, positive, and negative behavioral cues.
- Biosensors: Electrocardiogram (ECG) for heart rate (HR) and heart rate variability (HRV), and Galvanic Skin Response (GSR) sensors.
- Psychometric Tools: Slater-Usoh-Steed (SUS) Presence Questionnaire, and the Subjective Units of Distress Scale (SUDS).
- Procedure:
- Baseline (5 mins): Participant sits quietly in a neutral, empty VR environment while baseline HR, HRV, and GSR are recorded.
- VRET Task (10 mins): Participant is immersed in the virtual auditorium and instructed to deliver a 5-minute impromptu speech to a virtual audience. The audience is programmed to display subtle negative cues (e.g., looking at phones, faint heckling) after 2 minutes.
- SUDS ratings are collected at minutes 1, 3, and 5 of the speech.
- Post-Test: Immediately following the task, the participant completes the SUS questionnaire.
- Data Analysis:
- Calculate mean SUS score (theoretical range 1-7, with higher scores indicating greater presence).
- Analyze physiological data: Compare mean HR and GSR during the speech task versus baseline using a paired t-test. A significant increase (p < .05) indicates successful fear activation.
Protocol: Evaluating the Impact of Embodiment on Anxiety
This experiment tests the hypothesis that a self-embodied avatar enhances the emotional intensity of a social scenario.
- Objective: To compare anxiety responses and sense of presence between a full avatar embodiment condition and a disembodied (floating camera) condition.
- Materials: As in Protocol 3.1, with the addition of a full-body avatar that is tracked in real-time via the HMD and controllers.
- Procedure:
- Design: A within-subjects, counterbalanced design.
- Condition A (Embodied): Participant sees their virtual body and hands in the auditorium. If they look down, they see a virtual torso and legs; hand movements are mirrored.
- Condition B (Disembodied): Participant is an invisible, floating presence in the room with no virtual body.
- Each condition involves a different but equivalently difficult 3-minute speech task.
- Measures: SUS Questionnaire and SUDS ratings are collected after each condition. Physiological data (GSR) is recorded throughout.
- Data Analysis: Use a repeated-measures ANOVA to compare SUS and peak GSR scores between the two conditions. A significant main effect of condition (favoring the embodied state) would support the role of embodiment in enhancing presence and emotional response [9].
The logical workflow for establishing the validity of a VRET environment, incorporating these protocols, is as follows:
The Scientist's Toolkit: Essential Research Reagents for Immersive VR
For research teams developing or evaluating VRET interventions, a standardized set of "research reagents"—both hardware and software—is essential for ensuring methodological consistency and reproducibility.
Table 2: Essential Research Reagents for Immersive VR Research
| Category | Item | Specification / Example | Research Function |
|---|---|---|---|
| Hardware | Head-Mounted Display (HMD) | Standalone (e.g., Meta Quest 3) or PC-connected (e.g., Varjo XR-4). Must support 6DoF tracking. | The primary delivery device for the virtual environment. Determines key immersion parameters like FoV and resolution. |
| Hardware | Biosensor Array | ECG/GSR kit from vendors like Biopac Systems or Shimmer Sensing. | Provides objective, physiological data for quantifying anxiety and arousal (e.g., HR, HRV, skin conductance) during exposure. |
| Software | Game Engine | Unity (Unity Technologies) or Unreal Engine (Epic Games). | The development platform for creating and controlling custom, clinically validated VR environments and scenarios. |
| Software | Data Logging SDK | Custom SDK or lab streaming layer (LSL). | Enables synchronous recording of in-world events (e.g., audience reaction), user actions, and biosensor data for later analysis. |
| Psychometrics | Presence Questionnaire | Slater-Usoh-Steed (SUS) or Presence Questionnaire (PQ) [8]. | The gold-standard subjective measure for quantifying the user's feeling of "being there." |
| Psychometrics | Distress & Anxiety Scales | Subjective Units of Distress Scale (SUDS) & Liebowitz Social Anxiety Scale (LSAS) [3]. | Validated clinical tools for measuring the primary and secondary outcomes of the VRET intervention. |
| Experimental Control | Scripted Scenario Protocol | A predefined sequence of events (e.g., audience behavior changes) with precise timings. | Ensures standardization and reproducibility of the exposure experience across all participants in a trial. |
The deliberate application of the technological principles of immersion, presence, and interactivity forms the foundation of scientifically rigorous VRET research. By systematically quantifying these elements through standardized protocols and employing a consistent toolkit of research reagents, scientists can develop digital exposures that are not only technologically sophisticated but also therapeutically potent. This methodological precision is crucial for advancing our understanding of anxiety disorders and for developing validated, effective, and replicable VR-based treatments that can stand alongside traditional therapeutic modalities. The future of clinical VR research lies in the continued refinement of these principles to create even more personalized and effective evidence-based interventions.
Virtual Reality Exposure Therapy (VRET) has emerged as a transformative modality within the treatment landscape for anxiety disorders. By combining the established principles of exposure therapy with immersive technology, VRET creates controlled, safe, and customizable environments for patients to confront their fears. The evidence base supporting its efficacy has expanded rapidly, necessitating comprehensive and regular synthesis. This application note examines the current meta-analytic landscape, detailing the robust evidence for VRET's effectiveness, comparing it to traditional therapeutic modalities, and providing structured protocols for its implementation in clinical research settings. Recent high-quality meta-analyses consistently demonstrate that VRET produces significant reductions in anxiety symptoms, with effect sizes that are comparable to, and in some cases superior to, traditional in-vivo exposure therapy [13] [14] [7]. This document serves as a reference for researchers and drug development professionals seeking to understand the state of the science and the methodological standards for future investigatio
Quantitative Synthesis of the Evidence Base
The efficacy of VRET is supported by a growing number of high-quality meta-analyses. The table below consolidates key quantitative findings from recent systematic reviews and meta-analyses, providing a clear comparison of effect sizes across different anxiety disorders and control conditions.
Table 1: Summary of Recent Meta-Analytic Findings on VRET for Anxiety Disorders
| Meta-Analysis (Year) | Disorder Focus | Number of Studies (Participants) | Comparison Condition | Effect Size (Hedges' g or SMD) | Key Conclusion |
|---|---|---|---|---|---|
| Tan et al. (2025) [13] | Social Anxiety Disorder | 17 RCTs | Waitlist comparator | Significant reduction in anxiety (Post & Follow-up) | VRET has greater efficacy than waitlist. |
| Tan et al. (2025) [13] | Social Anxiety Disorder | 17 RCTs | Other Interventions (e.g., CBT) | Similar effect (Post & Follow-up) | VRET demonstrates similar effect to other interventions. |
| Frontiers in Psychiatry (2025) [14] | Various Anxiety Disorders | 33 RCTs (3,182 participants) | Conventional Interventions | SMD = -0.95, 95% CI (-1.22, -0.69), p < 0.00001 | VR therapy significantly improved anxiety symptoms and level. |
| ScienceDirect Meta-Analysis (2025) [7] | Social Anxiety & Specific Phobia | RCTs with VRET & IVET arms | In-vivo Exposure (IVET) | Moderate effect sizes for both | VRET and IVET are equally effective. |
The data reveals a consistent pattern: VRET is statistically and clinically superior to waitlist or placebo controls and is non-inferior to traditional evidence-based treatments like in-vivo exposure and cognitive-behavioral therapy (CBT) [13] [7]. The large, statistically significant effect size (SMD = -0.95) reported by Zeng et al. (2025) underscores the powerful effect VRET has on alleviating anxiety symptoms across a spectrum of disorders [14]. Furthermore, the combination of VRET with CBT appears to be particularly effective for symptomatic social anxiety [13].
Detailed Experimental Protocols for VRET Implementation
To ensure methodological rigor and reproducibility in clinical trials, the following standardized protocol outlines the core components of a VRET intervention for anxiety disorders, synthesized from multiple recent studies.
Table 2: Key Components of a Standardized VRET Intervention Protocol
| Protocol Phase | Key Activities | Duration/Frequency | Tools & Measures |
|---|---|---|---|
| 1. Initial Assessment & Preparation | Comprehensive biopsychosocial intake; diagnosis confirmation; psychoeducation on disorder and VRET rationale; informed consent; establishment of therapeutic alliance. | 2-3 sessions | Clinical interviews (e.g., ADIS-5); self-report questionnaires (e.g., LSAS, SPIN, BAI); SUDS scale explanation. |
| 2. Hierarchy Development & Customization | Collaborative creation of a fear hierarchy; selection/customization of VR scenarios to match patient-specific triggers and goals. | 1 session | Fear Hierarchy Worksheet; VR software platform with customizable environment library (e.g., audience size, scene complexity). |
| 3. Graded Exposure Sessions | Gradual, systematic exposure to fear-eliciting virtual scenarios; repetition until anxiety decreases (habituation); collaborative progression through hierarchy. | 8-12 sessions, 30-60 mins each | VR Headset (e.g., Meta Quest, HTC Vive); tailored VR environments; therapist control interface for real-time adjustments; continuous SUDS monitoring. |
| 4. Post-Session Processing & Homework | Review of exposure experience; cognitive restructuring; discussion of corrective learning; assignment of in-vivo or imaginal exposure practice. | End of each session & between sessions | Homework worksheets; behavioral experiment plans. |
| 5. Follow-up Assessment | Re-administration of baseline measures to evaluate symptom reduction and treatment gains maintenance. | Post-treatment, 3-month, 6-month | Same as baseline (e.g., LSAS, SPIN); behavioral assessment tests. |
Protocol Modifications for Specific Populations
For Adolescents: The VIRTUS trial protocol highlights adaptations for adolescent populations, including a shorter intervention (seven sessions), the use of more gamified and engaging VR content to enhance motivation, and a focus on developmental-stage-appropriate fears like speaking in class or meeting new people [3].
For Self-Guided Interventions: Emerging protocols for fully self-guided VRET, such as the 14-day smartphone-based intervention for university students, involve locked daily progression, automated reminders, and culturally tailored scenarios (e.g., classroom presentations) to ensure adherence and effectiveness without therapist guidance [15].
Signaling Pathways and Theoretical Mechanisms
The efficacy of VRET is underpinned by several well-established psychological theories of fear extinction and learning. The following diagram illustrates the primary theoretical pathways through which VRET is hypothesized to exert its therapeutic effects.
The primary mechanisms identified in contemporary research are:
- Emotional Processing Theory: VRET works by activating the fear structure in memory and promoting within- and between-session habituation, leading to a reduction in the fear response over time [3] [16].
- Inhibitory Learning Theory: This dominant model posits that VRET creates new, non-threatening memories that compete with the original fear memory. The key mechanism is expectancy violation—when the patient's feared outcome (e.g., being humiliated during a speech) does not occur, new, inhibitory learning takes place [3] [11].
- Self-Efficacy Theory: Successfully navigating challenging virtual scenarios enhances the patient's belief in their ability to cope, thereby increasing self-efficacy and reducing anxiety and avoidance behaviors [3].
The Researcher's Toolkit: Essential Reagents and Materials
Implementing a rigorous VRET research program requires specific technological and assessment tools. The following table details the key components of a research-grade VRET setup.
Table 3: Essential Research Reagents and Materials for VRET Trials
| Category | Item | Specification / Example | Primary Function in Research |
|---|---|---|---|
| Hardware | VR Headset | Standalone (e.g., Meta Quest 3) or PC-tethered (e.g., HTC Vive) | Creates immersive 3D environment for stimulus delivery. |
| Hardware | Therapist Control Interface | Tablet or laptop with dedicated software | Allows real-time control and customization of VR scenarios during sessions. |
| Hardware (Optional) | Biofeedback Devices | Heart rate monitor, galvanic skin response sensor | Provides objective, physiological data on anxiety activation and habituation. |
| Software | VRET Platform | Platforms like PsyTechVR with a library of evidence-based environments | Delivers standardized, customizable anxiety-provoking scenarios (e.g., crowds, heights). |
| Software | Assessment & Data Management System | Integrated database for patient progress tracking | Ensures fidelity to protocol and facilitates data collection for outcomes. |
| Psychometrics | Primary Outcome Measures | Liebowitz Social Anxiety Scale (LSAS), Social Phobia Inventory (SPIN) | Quantifies change in disorder-specific symptom severity. |
| Psychometrics | Process Measures | Subjective Units of Distress Scale (SUDS) | Tracks momentary anxiety fluctuations during exposure sessions. |
Recent advancements have validated more accessible hardware, including smartphone-based VR headsets, which maintain efficacy while dramatically improving scalability and reducing costs, as demonstrated in studies with college students [15]. Furthermore, the integration of biofeedback devices is an emerging trend, allowing researchers to collect rich, multimodal data (subjective, behavioral, and physiological) on treatment processes and outcomes [17].
Virtual Reality Exposure Therapy (VRET) represents a paradigm shift in the treatment of anxiety disorders, leveraging immersive technology to create controlled, replicable therapeutic environments. Within the broader thesis of optimizing VRET for anxiety disorders, understanding its disorder-specific efficacy is crucial for clinical application and future research. The evidence base, while robust for certain conditions, reveals a nuanced landscape of effectiveness across the diagnostic spectrum. This variability stems from fundamental differences in the neurobiological underpinnings of anxiety disorders, which can be categorized into fear-dominant (e.g., specific phobia, agoraphobia), mixed (e.g., panic disorder, social anxiety disorder), and anxiety-dominant (e.g., generalized anxiety disorder) conditions [18]. The following application notes and protocols detail the empirical evidence and methodological frameworks for applying VRET across these disorders, providing a resource for researchers and clinical trial designers.
Efficacy Data and Comparative Outcomes
Quantitative data from meta-analyses and controlled trials provide a clear, disorder-specific breakdown of VRET's performance against both passive and active control conditions.
Table 1: VRET Efficacy Across Anxiety Disorders (vs. Waitlist/Placebo)
| Condition | Number of RCTs Included | Total N | Effect Size (Hedges' g) | Reference |
|---|---|---|---|---|
| Specific Phobias | 12 | 431 | 0.95* | [19] |
| Social Anxiety Disorder | 7 | 236 | 0.97* | [19] |
| Panic Disorder | 2 | 65 | 1.03* | [19] |
| Post-Traumatic Stress Disorder (PTSD) | 6 | 175 | 0.57* | [19] |
Note: All effect sizes are statistically significant (p < .05) and reflect outcomes at post-treatment. Hedges' g is a measure of effect size where 0.2 is considered small, 0.5 medium, and 0.8 large.
Table 2: VRET Efficacy Compared to Active Treatments (In Vivo Exposure)
| Condition | Number of RCTs Included | Total N | Effect Size (Hedges' g) | Reference |
|---|---|---|---|---|
| Specific Phobias | 5 | 206 | -0.08 | [19] |
| Social Anxiety Disorder | 6 | 245 | 0.06 | [19] |
| PTSD | 6 | 239 | 0.02 | [19] |
Note: Effect sizes near zero indicate no significant difference between VRET and the active comparator, establishing non-inferiority.
The data in Table 1 demonstrates that VRET has a large and significant effect in reducing symptoms compared to waitlist or placebo conditions across all listed anxiety disorders [19]. Table 2 confirms that for specific phobias, social anxiety disorder (SAD), and PTSD, VRET is statistically as effective as traditional in vivo exposure therapy, the established gold-standard treatment [19]. This non-inferiority is a cornerstone for the adoption of VRET, particularly for situations where in vivo exposure is impractical, difficult to control, or too costly.
Detailed Experimental Protocols
Protocol for Social Anxiety Disorder (SAD)
This protocol is adapted from clinical trials investigating pure VRET without concurrent cognitive interventions [20].
- Objective: To reduce fear of negative evaluation and avoidance of social situations.
- Duration: Typically 8-12 weekly sessions, each lasting 60 minutes.
- Core Components:
- Psychoeducation and Rationale: Provide patients with the Inhibitory Learning Model, explaining that the goal is to violate their expectancies about social catastrophes and learn new, non-threatening associations with social triggers [20].
- Hierarchy Development: Collaboratively create a list of feared social situations, ranked by subjective units of distress (SUDs). Example hierarchy:
- Low anxiety: Making eye contact with a stranger avatar.
- Medium anxiety: Asking a virtual shop clerk for help.
- High anxiety: Giving a presentation to a virtual audience.
- Very high anxiety: Being interviewed for a job by a panel of avatars.
- Virtual Exposure Sessions:
- The therapist uses a VR system capable of rendering various social environments (e.g., a café, a conference room, a busy street) and populating them with avatars.
- The therapist controls variables in real-time from a separate console, including the number and gender of avatars, their gestures (e.g., nodding, looking bored), and the style/topic of dialogue [20].
- Exposure begins with lower-ranked items and progresses gradually. Each session continues until the patient's anxiety shows a significant decrease within the session (habituation) and, more importantly, until the patient's specific catastrophic expectation (e.g., "If I pause during my speech, everyone will laugh") is violated.
- Homework Assignments: Patients are encouraged to practice the skills and confront similar social situations in real life between VRET sessions to promote generalization of learning.
Protocol for Post-Traumatic Stress Disorder (PTSD)
This protocol synthesizes elements from proven trauma-focused therapies like Prolonged Exposure.
- Objective: To reduce re-experiencing, avoidance, and hyperarousal symptoms by processing traumatic memories.
- Duration: 10-16 weekly sessions of 90 minutes.
- Core Components:
- Assessment and Trauma Interview: Identify the index trauma and specific sensory triggers (sights, sounds, smells).
- VR Environment Selection/Creation: Customize a virtual environment to closely match the patient's traumatic event (e.g., a virtual Iraq/Afghanistan landscape for combat veterans, a virtual city street for assault survivors) [21].
- Gradual Imaginal and VR Exposure:
- Patients first engage in imaginal exposure, recounting the trauma memory in the safe therapeutic context.
- This is supplemented with VR exposure, where the patient is immersed in the trauma-relevant environment. The therapist gradually introduces trauma-related stimuli (e.g., helicopter sounds, distant shouts, dimmed lighting to simulate night) based on the patient's hierarchy.
- The therapist's role is to guide the narrative and ensure the patient emotionally engages with the memory and the virtual environment without resorting to avoidance strategies [21].
- Processing and Reclaiming Safety: After each exposure, the therapist helps the patient process the experience, focusing on the discrepancy between the memory of the trauma (danger) and the current reality of being safe in the therapist's office.
Theoretical Workflow and Signaling Pathways
The efficacy of VRET is best understood through contemporary psychological models and the neurobiology of fear and anxiety. The following diagram illustrates the core therapeutic workflow and the underlying neural mechanisms it targets.
Diagram 1: VRET Therapeutic Workflow and Neurobiological Basis
This workflow is supported by distinct neurobiological pathways. Fear-dominant disorders (specific phobia, agoraphobia) primarily involve the amygdala-centered fear network [18]. VRET facilitates extinction learning by violating threat expectancies, leading to the formation of new safety memories mediated by the prefrontal cortex inhibiting amygdala activity. For anxiety-dominant disorders like GAD, which involves chronic worry regulated by the hypothalamic-pituitary-adrenal (HPA) axis, the role of exposure is less defined, explaining the emerging but less robust evidence base [18].
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing VRET trials, the following tools and measures are essential.
Table 3: Essential Materials and Tools for VRET Research
| Item / Reagent | Function in Research | Example / Notes |
|---|---|---|
| Stand-Alone VR Headset | Provides immersive stimulus delivery. Enables controlled, repeatable exposures. | Oculus Quest series (Meta). Modern stand-alone units eliminate the need for a tethered computer, enhancing clinical flexibility [19]. |
| Clinical VR Software Platforms | Provides the therapeutic environments and stimuli specific to different disorders. | Customizable platforms for PTSD (e.g., combat zones), SAD (e.g., virtual audience, job interview), and specific phobias (e.g., heights, flying) [20] [22]. |
| Liebowitz Social Anxiety Scale (LSAS) | Primary outcome measure for SAD trials. Assesses fear and avoidance across social situations. | A gold-standard, clinician-administered scale [23]. |
| Social Phobia Inventory (SPIN) | Self-report outcome measure for SAD. Captures fear of negative evaluation, physical symptoms, and fear of uncertainty [23]. | Useful for screening and tracking symptoms. |
| PTSD Checklist for DSM-5 (PCL-5) | Standardized self-report measure for assessing PTSD symptom severity. | Critical for establishing baseline and post-treatment efficacy in PTSD trials [21]. |
| Hamilton Anxiety Rating Scale (HAM-A) | Clinician-rated scale to measure overall anxiety severity. | Used in trials for GAD and other anxiety disorders to assess general anxiety symptoms [24]. |
| Therapist Control Console | Software interface allowing the therapist to control stimuli in the VR environment in real-time. | Essential for tailoring exposure intensity by adjusting variables like avatar behavior, sound effects, and environmental conditions during a session [20]. |
Virtual Reality Exposure Therapy (VRET) represents a paradigm shift in the treatment of anxiety disorders, offering distinct advantages over traditional therapeutic methods. By leveraging immersive technology, VRET enables clinicians to deliver controlled, safe, and accessible exposure therapy that would be impractical or impossible to implement in real-world settings. This application note details the mechanisms, protocols, and empirical support for VRET, providing researchers and clinical professionals with comprehensive frameworks for implementation and study. Evidence from recent randomized controlled trials and meta-analyses confirms that VRET produces outcomes comparable to in-vivo exposure while overcoming critical limitations of traditional approaches through precise stimulus control, enhanced safety parameters, and reduced treatment barriers.
Virtual Reality Exposure Therapy (VRET) has emerged as an innovative evidence-based intervention that effectively addresses core limitations of traditional exposure therapy for anxiety disorders. By creating immersive, computer-generated environments, VRET enables precise control over therapeutic stimuli while maintaining a physically safe and psychologically contained setting. The technological foundation of VRET allows for the systematic presentation of fear-eliciting stimuli that can be meticulously calibrated to match individual patient needs and tolerance levels [25]. This controlled approach facilitates the extinction learning process central to exposure therapy while minimizing the risks of premature termination, uncontrolled real-world exposure, and the practical limitations of accessing specific fear contexts.
The efficacy of VRET stems from its ability to create a powerful sense of presence—the subjective experience of "being there" in the virtual environment—while maintaining the clinical safety of the therapist's office. Neurophysiological and behavioral research indicates that individuals respond to virtual environments with anxiety reactions and coping responses similar to those evoked by real-world situations, enabling effective emotional processing and fear extinction [26]. This combination of psychological engagement within a physically safe context represents a fundamental advancement over traditional exposure methods, particularly for trauma-related disorders and specific phobias where real-world exposure may be dangerous, impractical, or ethically complicated.
Comparative Efficacy Data
Table 1: Clinical Efficacy of VRET Across Anxiety Disorders
| Disorder | Comparison Condition | Key Efficacy Metrics | Effect Size/Outcome | Reference |
|---|---|---|---|---|
| Specific Phobias | In-vivo Exposure | Symptom reduction post-treatment | Comparable effectiveness, high satisfaction rates | [27] |
| Social Anxiety Disorder | Non-VR Treatments | Reduction in anxiety symptoms | Comparable efficacy | [27] |
| PTSD | Traditional Treatments | Symptom reduction | 66%-90% success rates | [28] |
| Public Speaking Anxiety | Waitlist/Control | Reduction in state anxiety | Significant improvement after single session | [29] |
| Performance Anxiety | Yoga Interventions | STAI-Y1/Y2 reduction | Rapid symptom reduction | [30] |
Table 2: Advantages of VRET Versus Traditional Exposure Therapy
| Parameter | Traditional Exposure Therapy | Virtual Reality Exposure Therapy | Clinical Implications |
|---|---|---|---|
| Stimulus Control | Limited, environment-dependent | Precise, gradable, repeatable | Enhanced treatment fidelity |
| Safety Profile | Variable, potential real risk | High, physical safety assured | Reduced liability, ethical advantage |
| Accessibility | Geographic, temporal constraints | Flexible, potential for remote delivery | Increased treatment access |
| Standardization | Challenging across patients | Highly standardized | Improved research validity |
| Dropout Rates | Higher due to discomfort | Lower, enhanced engagement | Improved treatment completion |
| Cost-Effectiveness | Variable, often high | Increasingly affordable | Improved resource allocation |
Core Mechanisms of Action
The Controlled Exposure Paradigm
The fundamental advantage of VRET lies in its capacity for precise stimulus control within an immersive environment. Unlike traditional exposure therapy, which often relies on imagination or difficult-to-manage real-world scenarios, VRET enables clinicians to systematically manipulate multiple sensory dimensions of the exposure experience. This includes visual complexity, auditory stimuli, and even tactile elements through haptic feedback devices [26]. The therapeutic environment can be repeatedly presented with exact consistency, paused for cognitive restructuring, or immediately adjusted in response to patient distress—capabilities largely absent from traditional exposure methods.
This controlled exposure paradigm operates through several distinct mechanisms:
- Stimulus Fidelity: Modern VR systems create highly realistic environments that successfully trigger authentic fear responses while maintaining the patient's awareness of being in a safe therapeutic setting [25].
- Hierarchical Precision: Therapists can construct exposure hierarchies with fine-grained progression steps, systematically increasing stimulus intensity according to individual tolerance levels [28].
- Multi-sensory Engagement: By engaging visual, auditory, and sometimes tactile modalities, VRET facilitates more robust emotional processing than imaginal exposure alone [25].
Safety and Containment Framework
The safety advantages of VRET extend beyond physical protection to include psychological containment mechanisms that facilitate emotional processing. Patients can confront traumatic memories or phobic stimuli with the conscious awareness that the environment is computer-generated and can be terminated immediately if necessary. This safety framework enhances patient willingness to engage with challenging material and reduces treatment refusal and dropout rates [28]. For patients with post-traumatic stress disorder (PTSD), this contained environment enables gradual processing of traumatic memories without the overwhelming intensity that can occur with traditional imaginal exposure.
Diagram 1: VRET Therapeutic Protocol Workflow - This diagram illustrates the controlled, iterative process of Virtual Reality Exposure Therapy, highlighting the continuous monitoring and adjustment capabilities.
Application Notes and Protocols
Protocol for Public Speaking Anxiety
Background: Public speaking anxiety represents a prevalent form of social anxiety that responds robustly to VRET interventions. The following protocol adapts methodology from a multisite experimental study investigating positive affect moderators in VRET for public speaking anxiety [29].
Equipment and Software:
- Fully immersive VR headset with minimum 90Hz refresh rate
- Public speaking virtual environment (auditorium, conference room, or classroom)
- Biofeedback monitoring capability (heart rate, galvanic skin response)
- Standardized assessment tools (STAI-S, self-reported valence scales)
Procedure:
- Pre-assessment: Administer trait positive affect measures, optimism scales, hopefulness inventories, and self-efficacy questionnaires at baseline.
- Psychoeducation: Explain the rationale for exposure therapy, the concept of inhibitory learning, and the VRET process.
- Affect Induction: Implement positive affect induction procedures before exposure sessions when investigating emotional moderators.
- Exposure Sessions:
- Begin with a virtual audience of 5-10 neutral avatars
- Gradually increase audience size and reactivity based on patient distress metrics
- Incorporate performance elements (prepared speech, impromptu speaking)
- Utilize heart rate biofeedback to guide exposure intensity
- Within-session Processing: Conduct cognitive restructuring during session breaks based on performance feedback.
- Post-session Assessment: Measure public speaking anxiety, social phobia symptoms, and self-reported emotional valence.
- Generalization Planning: Develop real-world exposure homework assignments based on VRET progress.
Session Parameters: Single-session protocols typically run 60-90 minutes, while multi-session interventions may involve 3-8 sessions spaced weekly [29].
Protocol for PTSD and Trauma-Related Disorders
Background: VRET enables controlled engagement with trauma memories in cases where in-vivo exposure is impractical or unsafe. This protocol is particularly relevant for combat-related PTSD, accident trauma, and assault survivors.
Equipment and Software:
- High-fidelity VR system with wide field of view
- Trauma-relevant virtual environments (customizable settings)
- Olfactory and tactile feedback components (when available)
- Physiological monitoring integrated with VR software
Procedure:
- Trauma Assessment: Detailed functional analysis of trauma triggers, avoidance patterns, and symptom profile.
- Safe Space Development: Create a personalized virtual "safe space" for patient use during distress management.
- Gradual Exposure Hierarchy:
- Develop multi-sensory hierarchy from least to most triggering elements
- Begin with neutral environmental elements without trauma cues
- Gradually introduce trauma-relevant stimuli across sensory modalities
- Trauma Narrative Integration:
- Combine imaginal reliving with virtual environment exposure
- Incorporate olfactory cues (smoke, gasoline) when relevant to trauma memory
- Use tactile feedback to simulate environment-specific sensations
- Emotional Processing:
- Encourage emotional engagement while practicing coping strategies
- Alternate between trauma focus and present-centered awareness
- Utilize physiological data to guide exposure intensity
- Consolidation Sessions: Schedule periodic booster sessions to maintain treatment gains and address new triggers.
Safety Considerations: Establish clear emotional distress protocols, including immediate exit strategies from the virtual environment and enhanced grounding techniques for dissociation management [25].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for VRET Investigation
| Tool Category | Specific Examples | Research Function | Implementation Notes |
|---|---|---|---|
| VR Hardware Platforms | HTC Vive Pro, Oculus Rift S, Varjo VR-3 | Delivery of immersive environments | Selection depends on visual fidelity requirements, tracking precision, and refresh rate needs |
| Biofeedback Integration | BioPac MP160, Empatica E4, HeartMath Inner Balance | Psychophysiological monitoring | Enables real-time adaptation of virtual environments based on physiological arousal |
| Virtual Environment Software | Bravemind, Psious, Limbix, Oxford VR | Pre-built therapeutic environments | Platform selection determined by target population and customization requirements |
| Assessment Batteries | STAI, CAPS-5, SUDS, PANAS | Standardized outcome measurement | Critical for establishing treatment efficacy and comparing across studies |
| Data Analytics Platforms | Unity Analytics, Custom MATLAB Scripts | Usage pattern analysis and efficacy tracking | Enables examination of dose-response relationships and mechanism of action |
| Stimulus Presentation Tools | WorldViz Vizard, Unity 3D, Unreal Engine | Custom environment development | Required for creating disorder-specific scenarios not available commercially |
Technological Implementation and Workflow
Diagram 2: VRET System Integration and Data Flow - This diagram illustrates the technological ecosystem of VRET, highlighting the integration of patient monitoring, real-time data analysis, and therapeutic intervention.
The technological implementation of VRET requires seamless integration of hardware, software, and therapeutic protocols to achieve the documented advantages over traditional methods. Current systems leverage fully immersive VR technology with integrated biofeedback capabilities that enable real-time adaptation of therapeutic content based on psychophysiological metrics [31]. This closed-loop system represents a significant advancement beyond static exposure protocols, allowing for precision mental healthcare tailored to individual response patterns.
The workflow incorporates continuous data collection throughout the therapeutic process, including:
- Behavioral Metrics: Movement patterns, avoidance behaviors, and interaction data within the virtual environment
- Physiological Measures: Heart rate, heart rate variability, galvanic skin response, and respiratory rate
- Subjective Reports: Periodic subjective units of distress (SUDS) ratings and cognitive appraisal assessments
- Performance Data: Task completion metrics, response times, and engagement levels
This multi-dimensional data ecosystem enables researchers to examine mechanisms of change and treatment responders, ultimately refining VRET protocols for enhanced efficacy [25].
Future Directions and Research Opportunities
The rapidly evolving landscape of VRET presents numerous research opportunities and clinical innovations. Emerging areas include:
- AI-Enhanced Personalization: Integration of machine learning algorithms to dynamically adjust virtual environments based on real-time patient response patterns [25]
- Remote Treatment Delivery: Development of secure, home-based VRET protocols to increase accessibility while maintaining therapeutic efficacy [31]
- Biomarker Integration: Investigation of neurophysiological and psychophysiological biomarkers to predict treatment response and optimize protocol selection [29]
- Multi-sensory Enhancement: Incorporation of olfactory, vestibular, and haptic feedback to increase ecological validity and treatment generalization [26]
- Preventive Applications: Exploration of VRET as a preventive intervention for at-risk populations before anxiety disorders become fully manifest
The projected growth of the virtual reality therapy market from $1.8 billion in 2023 to approximately $13.9 billion by 2032 reflects both commercial interest and expanding clinical validation [31]. This investment trajectory underscores the importance of continued rigorous research to establish optimal implementation protocols, identify mechanisms of change, and ensure equitable access to these innovative therapeutic tools.
Virtual Reality Exposure Therapy represents a significant advancement in the treatment of anxiety disorders, offering demonstrable advantages over traditional methods through enhanced control, safety, and accessibility. The protocols and application notes detailed herein provide researchers and clinicians with evidence-based frameworks for implementation and further investigation. As the technology continues to evolve and research expands, VRET holds promise for transforming mental healthcare delivery through personalized, precisely controlled therapeutic experiences that effectively target the core mechanisms maintaining anxiety disorders while overcoming traditional treatment barriers.
Implementing VRET in Clinical and Research Settings: Protocols, Personalization, and Workflow
Application Notes: Core Principles and Rationale
Virtual Reality Exposure Therapy (VRET) is an evidence-based treatment that integrates virtual reality technology within a cognitive-behavioral framework to treat anxiety disorders. Its efficacy is rooted in emotional processing theory, which posits that successful treatment requires the activation and subsequent modification of pathological fear structures in memory [16]. VRET facilitates this by providing controlled, immersive environments where patients can confront feared stimuli without real-world danger, enabling corrective learning and a reduction in avoidance behaviors [16] [3].
A significant advantage of VRET is its capacity to overcome practical and logistical barriers associated with traditional in vivo exposure. It allows for the precise control of sensory stimulation, the creation of otherwise impractical or costly scenarios (e.g., a cross-country flight or a specific traumatic context), and ensures patient confidentiality during sessions [16]. Furthermore, VRET may be more acceptable to patients than traditional exposure, as indicated by lower refusal rates for VR (3%) compared to in vivo exposure (27%) in one study of specific phobias [16]. For clinicians, modern wireless VR systems with controller-free hand tracking have been shown to improve attitudes toward VRET after direct experience, highlighting the importance of usability and immersion for clinical adoption [32].
Standardized VRET Protocol for Anxiety Disorders
The following protocol outlines a standardized course of treatment, adaptable for various anxiety disorders, from specific phobias to social anxiety disorder.
Phase I: Initial Psychoeducation and Treatment Rationale (Sessions 1-2)
Objective: To establish therapeutic rapport, provide a comprehensive understanding of the anxiety disorder, and introduce the rationale for VRET.
Methods:
- Assessment: Conduct a detailed clinical interview and use standardized measures (e.g., Acrophobia Questionnaire [AQ], Liebowitz Social Anxiety Scale [LSAS], Generalized Anxiety Disorder-7 [GAD-7]) to establish a baseline and identify specific fear structures [33] [3].
- Psychoeducation: Educate the patient on the nature of their anxiety disorder using the cognitive-behavioral model. Explain the roles of avoidance, anticipatory anxiety, and the fear maintenance cycle.
- VRET Rationale: Explain the principles of exposure therapy and how VR creates a safe, controlled environment for confronting fears. Emphasize that the virtual environment is designed to feel realistic and elicit anxiety to provide opportunities for new learning. Normalize the experience of discomfort as a sign that the treatment is activating the fear network [16] [32].
- Introduction to Technology: Familiarize the patient with the VR hardware (head-mounted display, controllers, or hand-tracking). Allow them to explore a neutral virtual environment to reduce tech-related anxiety and address any concerns about simulator sickness [34] [32].
Phase II: Collaborative Hierarchy Development (Session 2)
Objective: To create a personalized and graded exposure hierarchy.
Methods:
- Stimulus Identification: Collaboratively with the patient, identify all stimuli, situations, and contextual factors related to their fear. For a fear of heights, this might include looking out a second-story window, standing on a ladder, or walking over a glass floor on a skyscraper [16] [32].
- SUDs Rating: Have the patient rate each identified situation on a Subjective Units of Distress (SUDs) scale from 0 (no anxiety) to 100 (maximum anxiety) [32].
- Hierarchy Construction: Order the situations from least (e.g., SUDs 20-30) to most anxiety-provoking (e.g., SUDs 90-100). This creates a roadmap for treatment, ensuring early success and promoting self-efficacy.
Table 1: Sample Exposure Hierarchy for Acrophobia
| Hierarchy Step | Virtual Scenario Description | Target SUDs (0-100) |
|---|---|---|
| 1 | Standing on a solid, wide platform, 2 meters high, with high railings. | 20-30 |
| 2 | Looking down from a 5-meter high interior balcony. | 40-50 |
| 3 | Walking across a narrow wooden plank, 5 meters high. | 50-60 |
| 4 | Riding a glass elevator up the outside of a tall building. | 60-70 |
| 5 | Standing on a transparent glass floor, 50 meters high. | 70-80 |
| 6 | Performing a task (e.g., retrieving an object) on a high, exposed platform with wind effects. | 80-90 |
| 7 | Being rescued from a gondola on a broken ski-lift over a cliff. | 90-100 |
Phase III: Graded Virtual Reality Exposure (Sessions 3-12+)
Objective: To systematically expose the patient to feared stimuli in virtual reality, progressing through the hierarchy to achieve habituation and inhibitory learning.
Methods:
- Session Structure: Each session begins with a brief check-in and setting an agenda. The majority of the session (approximately 30-45 minutes) is dedicated to VR exposure.
- Exposure Conduct: The patient enters the VR scenario corresponding to their current position on the hierarchy. The therapist's role is to guide, encourage, and ensure the patient remains in the situation until their anxiety begins to decrease.
- Within- and Between-Session Progress: A step is considered mastered when the patient's SUDs rating decreases significantly (e.g., by 50% or more) during a single exposure (within-session habituation) and when they report lower initial SUDs upon re-encountering the same scenario in a subsequent session (between-session habituation). Progression to the next hierarchy step is collaborative [16].
- Individualization: The therapist should use clinical judgment to tailor the exposure. This may include repeating scenes, adjusting virtual parameters (e.g., adding turbulence to a virtual flight), or focusing on specific stimuli based on the patient's fear structure [16].
- Processing: After each exposure, briefly process the experience. Discuss what the patient learned, whether their feared outcomes occurred, and how they coped, reinforcing the violation of negative expectancies [3].
Mechanisms of Change and Neural Correlates
Therapeutic change in VRET is driven by mechanisms such as expectancy violation (experiencing that a feared outcome does not occur), habituation (reduction in fear response over time), and enhanced self-efficacy (increased confidence in one's ability to cope) [3]. Neuroimaging studies provide preliminary evidence of the neural underpinnings of these changes. A 2025 fMRI study on acrophobia found that VRET led to decreased activity in the default mode network (e.g., precuneus, middle temporal gyrus) and the primary visual cortex (calcarine), regions associated with self-referential thinking and visual processing of threat. This suggests VRET may work by modulating the brain networks responsible for processing fear and contextualizing threatening stimuli [33].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for VRET Research
| Item | Function in Research | Exemplars / Notes |
|---|---|---|
| VR Hardware Platform | Provides the immersive sensory experience. Key features include display resolution, field of view, tracking capabilities, and comfort. | Modern, commercially available standalone headsets (e.g., Meta Quest系列) are recommended for their wireless freedom, controller-free hand tracking, and high resolution, which enhance immersion and reduce simulator sickness [32]. |
| Disorder-Specific VR Software | Contains the virtual environments and scenarios designed to elicit specific fears. | Commercially available or custom-built applications for disorders like acrophobia (e.g., scenarios involving cliffs, bridges), social anxiety (e.g., virtual auditorium for public speaking), and PTSD [16] [32] [3]. |
| Clinical Assessment Batteries | Quantifies symptom severity, treatment efficacy, and mechanism of change. | Primary: Disorder-specific measures (e.g., Acrophobia Questionnaire [AQ], Liebowitz Social Anxiety Scale [LSAS]). Secondary: General anxiety (GAD-7), behavioral avoidance tests (BAT), and subjective units of distress (SUDs) [33] [3]. |
| Psychophysiological Recording Equipment | Provides objective, non-verbal indices of arousal and fear activation during exposure. | Equipment to measure heart rate variability (HRV), galvanic skin response (GSR), and electroencephalography (EEG) can be synchronized with VR events to capture real-time physiological responses [16]. |
| Data Integration & Analysis Software | Manages and analyzes multi-modal data (subjective, behavioral, physiological). | Platforms like VRNetzer, which allow for interactive data visualization, or statistical software (R, Python) for analyzing clinical and experimental data [35]. |
Experimental Workflow for a VRET Session
The following diagram illustrates the standardized, iterative workflow for conducting a single VRET exposure session, from preparation to progression planning.
Virtual Reality Exposure Therapy (VRET) represents a paradigm shift in the treatment of anxiety disorders, moving beyond a one-size-fits-all approach to enable precise alignment with individual fear structures. Fear structures—comprising stimulus representations, response representations, and meaning-based interpretations—form the core pathological framework of anxiety disorders [3]. The plasticity of virtual environments offers unprecedented opportunities to deconstruct and target these elements with customized therapeutic experiences. This protocol details the methodology for individualizing VR exposure by identifying key fear components and engineering virtual scenarios that directly match these individualized profiles.
Research demonstrates that individualized VRET produces outcomes comparable to traditional in-vivo exposure while overcoming significant accessibility barriers [7] [36]. For anxiety disorders, including social anxiety disorder (SAD) and specific phobias, effective treatment requires activating the specific fear network while providing opportunities for corrective learning through expectancy violation and inhibitory learning [3]. The controlled nature of virtual environments enables therapists to systematically manipulate scenario parameters to achieve this precise activation while maintaining patient safety and therapeutic alliance.
Theoretical Foundations
Fear Structure Model in Anxiety Disorders
The efficacy of exposure therapy hinges on directly accessing and modifying pathological fear structures. According to emotional processing theory, these structures contain information about feared stimuli, fear responses, and their associated meanings [3]. In social anxiety, for instance, core fears often revolve around rejection, appearing foolish, or being the center of attention [3]. These fears manifest in avoidance behaviors that prevent disconfirmatory experiences. Virtual environments can be engineered to contain elements that specifically trigger an individual's unique fear structure while ensuring the presence of sufficient safety cues to encourage engagement.
Mechanisms of Change in Virtual Reality Exposure
VRET facilitates fear reduction through multiple established mechanisms:
- Expectancy violation: Creating mismatches between predicted and actual outcomes
- Within- and between-session habituation: Reduction of fear response through repeated exposure
- Self-efficacy enhancement: Building confidence through successful virtual experiences [3]
The inhibitory learning model posits that successful exposure creates new, non-threat associations that compete with existing fear associations [3]. VR environments optimally support this process by allowing precise control over exposure parameters to maximize expectancy violation while managing anxiety levels. For adolescents with social anxiety, the game-like features of VR may increase treatment adherence and motivation compared to traditional exposure [3].
Assessment and Fear Structure Mapping
Comprehensive assessment forms the foundation for individualizing virtual environments. The following multi-method approach ensures precise mapping of individual fear structures:
Clinical Interview and Standardized Measures
Table 1: Core Assessment Domains and Instruments
| Assessment Domain | Specific Instruments | Clinical Utility |
|---|---|---|
| Symptom Severity | SPAI-18, LSAS-avoidance [3] | Quantifies avoidance and anxiety intensity |
| Core Fear Identification | Fear Hierarchy Questionnaire, Clinical Interview [3] | Identifies specific feared outcomes and triggers |
| Functional Impairment | SPWSS, Psychosocial Functioning scales [3] | Assesses impact on daily life domains |
| Cognitive Mechanisms | Expectancy of Threat Scale [3] | Measures probability and cost estimates of feared outcomes |
Behavioral Avoidance Assessment
Virtual behavioral approach tests (V-BAT) provide objective measures of avoidance patterns. During V-BAT, patients navigate virtual environments while researchers record:
- Approach distance to feared stimuli
- Physiological correlates (heart rate, skin conductance)
- Self-reported distress levels at each proximity
- Avoidance behaviors and safety signals utilized
This data directly informs the initial exposure gradient and identifies specific environmental elements that trigger maximal fear activation.
Individual Difference Moderators
Assessment should identify potential moderators of VRET response, including:
- Clinical variables: Comorbidity, pre-intervention severity [3]
- Personality traits: Behavioral inhibition/activation, openness to experience [3]
- VR-related factors: Technological affinity, presence susceptibility [3]
- Demographic factors: Age, gender, prior treatment history
Virtual Environment Tailoring Protocols
Parameter Customization Framework
Virtual environments can be systematically tailored across multiple dimensions to match individual fear structures:
Table 2: Virtual Environment Customization Parameters
| Parameter Domain | Customization Options | Clinical Application |
|---|---|---|
| Social Environment | Audience size, composition, responsiveness [3] | Social anxiety hierarchy implementation |
| Performance Context | Formality, evaluation criteria, consequence significance [3] | Public speaking anxiety individualization |
| Sensory Elements | Visual fidelity, auditory stimuli, haptic feedback [17] | Gradual intensity modulation |
| Interactive Capacity | Agent responsiveness, user control level, consequence realism [11] | Self-efficacy enhancement through mastery experiences |
| Temporal Factors | Exposure duration, scenario progression pace [36] | Within- and between-session habituation planning |
Stimulus Calibration Protocol
The following workflow details the procedure for calibrating virtual stimuli to individual fear structures:
Social Anxiety Individualization Protocol
For social anxiety disorder, environment tailoring follows this specific pathway:
Implementation guidelines for social anxiety VRET:
- Performance anxiety: Begin with small, non-reactive virtual audiences and gradually increase audience size and responsiveness based on patient tolerance [3]
- Interaction anxiety: Program virtual humans with varying levels of social demand, starting with scripted interactions and progressing to more dynamic conversations
- Observation anxiety: Create environments where the patient is the focus of attention without performance demands
The Researcher's Toolkit: Essential Materials and Platforms
Table 3: Research Reagent Solutions for VRET Studies
| Tool Category | Specific Products/Platforms | Research Application |
|---|---|---|
| VR Hardware | Meta Quest 2/3, HTC Vive, Valve Index [17] [6] | Balanced mobility and graphical capability for clinical research |
| Therapeutic Software | Doxy.me VR, PsyTechVR [17] [6] | Pre-programmed, evidence-based virtual environments with customization capacity |
| Physiological Monitoring | Heart rate sensors, GSR devices, respiration monitors [17] | Objective fear activation measurement during exposure |
| Assessment Platforms | REDCap (Research Electronic Data Capture) [6] | Automated collection of self-report and clinical outcome data |
| Presence Measures | Igroup Presence Questionnaire (IPQ), Slater-Usoh-Steed Questionnaire | Quantification of immersion and reality perception in virtual environments |
Technical specifications for optimal VRET research implementation:
- Computer systems: Minimum NVIDIA RTX 3060 graphics, Intel i5/Ryzen 5 processor, 16GB RAM [17]
- Tracking systems: Six degrees of freedom (6DoF) controllers with inside-out tracking
- Sensory add-ons: Stereo headphones, optional haptic feedback devices [17]
- Therapist interface: Dedicated control dashboard for real-time parameter adjustment [17]
Experimental Protocol for VRET Efficacy Trials
Study Design and Participant Recruitment
This protocol outlines a randomized controlled trial (RCT) comparing individualized VRET to standard in-vivo exposure:
Participant selection:
- Target sample: 120 participants (ages 12-16 for adolescent focus; 18+ for adult studies) with subclinical to moderate social anxiety or specific phobia [3]
- Diagnostic criteria: DSM-5/ICD-10 criteria confirmed via structured clinical interview
- Exclusion criteria: Comorbid psychotic disorders, active substance dependence, seizure disorders, visual impairments uncorrectable in VR
Randomization procedure:
- 1:1 allocation to VRET or in-vivo exposure using computer-generated randomization sequences
- Stratification by anxiety severity, phobia subtype, and prior treatment history
Intervention Protocol
Both active conditions receive a seven-session exposure-based intervention with the following structure:
Table 4: Session-by-Session VRET Protocol
| Session | Primary Focus | VR Customization Elements | Duration |
|---|---|---|---|
| 1-2 | Psychoeducation & fear hierarchy building | Environment familiarization without exposure elements | 45-60 minutes |
| 3-5 | Graduated exposure | Systematic parameter adjustment based on fear activation | 45-60 minutes |
| 6 | Consolidation & cognitive restructuring | Maximum fear trigger exposure with cognitive challenges | 45-60 minutes |
| 7 | Relapse prevention & generalization | Novel scenario application of learned skills | 45-60 minutes |
For specific phobias, evidence supports efficacy with single, extended sessions (45-180 minutes), while social anxiety and agoraphobia typically require 8-12 sessions [36].
Individualization Procedures
The experimental protocol incorporates these key individualization steps:
- Pre-treatment assessment analysis to identify individual fear structure components
- Baseline VR environment calibration using test exposures with physiological monitoring
- Session-by-session parameter adjustment based on within- and between-session habituation patterns
- Dynamic difficulty adjustment during sessions based on real-time distress metrics
Outcome Measures and Data Collection
Primary and secondary outcomes assessed at baseline, post-treatment, and 3-/6-month follow-ups:
Primary outcomes:
- Social Phobia and Anxiety Inventory (SPAI-18)
- Liebowitz Social Anxiety Scale - avoidance subscale (LSAS-avoidance) [3]
Secondary outcomes:
- Social Phobia Weekly Summary Scale (SPWSS)
- General well-being indicators (resilience, depression, psychosocial functioning) [3]
Process measures:
- Expectancy violation scales
- Self-efficacy ratings
- Working alliance inventories
- Presence and immersion questionnaires
Data Analysis Plan
Statistical approaches for evaluating individualized VRET efficacy:
Primary efficacy analysis:
- Linear mixed models (LMM) to examine condition × time interactions on primary outcomes
- Intent-to-treat analysis with multiple imputation for missing data
Mechanism analysis:
- Parallel process latent growth curve modeling to test mediators (expectancy violation, self-efficacy)
- Moderation analysis to identify patient characteristics predicting optimal VRET response
Individualized effects analysis:
- Person-centered approaches (e.g., latent class growth analysis) to identify differential response trajectories
- Dose-response relationships between customization precision and outcomes
Sample size justification: 120 participants provide 80% power to detect medium effects (f = 0.25) in 3 × 4 mixed ANOVA with alpha = 0.05.
Ethical and Practical Implementation Considerations
Successful implementation of individualized VRET requires attention to:
- Therapeutic alliance: Maintain strong rapport despite technology mediation through pre-exposure preparation and post-exposure processing [11]
- Safety protocols: Monitor cybersickness symptoms and provide abort scenarios for overwhelming anxiety
- Equipment sterilization: Implement hygienic protocols for shared head-mounted displays
- Technical competence: Ensure research staff proficiency in both clinical procedures and VR operation
- Data security: Protect patient data in compliance with HIPAA and other relevant regulations [6]
This protocol provides a comprehensive framework for individualizing virtual environments in exposure therapy research. By systematically tailoring VR scenarios to match individual fear structures, researchers can maximize the efficacy and precision of VRET for anxiety disorders. The detailed methodologies, assessment approaches, and customization parameters outlined here enable rigorous investigation of how personalized virtual reality interventions can optimize therapeutic outcomes across different anxiety presentations.
Future research directions should include examining the additive benefits of physiological monitoring to guide real-time personalization, developing algorithms for automated environment adjustment, and investigating how individual difference factors moderate response to specific VR environment parameters.
Virtual Reality Exposure Therapy (VRET) represents a paradigm shift in the treatment of anxiety disorders, leveraging immersive technology to create controlled, safe, and customizable therapeutic environments. Framed within a broader thesis on VRET for anxiety disorders, this document provides detailed application notes and experimental protocols for three core clinical indications: specific phobias, social anxiety disorder (SAD), and post-traumatic stress disorder (PTSD). The efficacy of VRET is grounded in its capacity to facilitate inhibitory learning and emotional processing by systematically exposing patients to fear-eliciting stimuli without the real-world risks, thereby promoting corrective experiences and fear extinction [22] [11]. The following sections synthesize current evidence, quantify treatment effects, and delineate step-by-step protocols for researchers and clinical scientists.
The quantitative efficacy of VRET across anxiety disorders is established by multiple meta-analyses and randomized controlled trials (RCTs). The data below summarize key outcome measures for the disorders of interest.
Table 1: Meta-Analysis Findings for VRET Efficacy
| Disorder Category | Number of Studies & Participants | Pooled Effect Size (SMD/Hedges' g) | Comparison Condition | Key References |
|---|---|---|---|---|
| Anxiety Disorders (Broad) | 33 studies (n=3,182) | SMD = -0.95 [95% CI: -1.22, -0.69] | Conventional Interventions (CBT, TAU) | [37] |
| Social Anxiety Disorder (SAD) | 22 studies (n=703) | Hedges' g = -0.86 (Post-Treatment)Hedges' g = -1.14 (6-month FU) | Waitlist/Placebo | [15] |
| Social Anxiety (Stand-alone VRET) | 5 studies (Limited n) | SMD = -0.82 [95% CI: -1.52, -0.13] | Control Groups | [38] |
Table 2: Representative RCT Outcomes for Social Anxiety Disorder (SAD)
| Study Population | Intervention Protocol | Control | Primary Outcome Measure | Result |
|---|---|---|---|---|
| University Students [15] | 14-day, self-guided smartphone VRET | Waitlist | Liebowitz Social Anxiety Scale (LSAS) | Significant reduction (M= -35.7, SD=24.0) vs. control (M= -2.2, SD=13.5; p<0.001) |
| Adolescents & Adults [3] | 7-session VRE vs. In Vivo Exposure (IVE) | Waitlist | Liebowitz Social Anxiety Scale (LSAS-Avoidance) | Hypothesis: VRE and IVE will significantly reduce symptoms vs. WL (Trial Ongoing) |
| Adults (n=44) [38] | VRET (BehaVR with Pico Goblin headset) | Waitlist | Social Interaction Anxiety Scale (SIAS) | Hedge's g = -4.58 (p<0.001) at post-treatment |
Detailed Experimental Protocols
Protocol for Specific Phobias
This protocol is designed for a graded exposure approach, applicable to phobias such as acrophobia (fear of heights) or aviophobia (fear of flying). The core mechanism is gradual desensitization within a safe, controllable virtual environment [22].
Pre-Treatment Assessment:
- Diagnosis: Confirm specific phobia diagnosis using the Structured Clinical Interview for DSM-5 (SCID-5).
- Baseline Measurement: Administer the Fear of Negative Evaluation Scale (FNE-B) and a disorder-specific Fear and Avoidance Hierarchy (FAH). The FAH is a 0-100 Subjective Units of Distress Scale (SUDS) rating for 5-10 phobia-related situations.
- Tech Setup: Calibrate VR headset (e.g., Pico Goblin, Samsung Gear VR) and ensure the virtual environment (VE) software is configured for the target phobia.
Exposure Sessions (6-8 sessions, 60 minutes each):
- Psychoeducation (Session 1): Explain the rationale of exposure therapy, including the principles of habituation and inhibitory learning.
- Graded In-Virtuo Exposure (Sessions 2-6):
- Begin with the lowest-rated item on the patient's individualized FAH.
- Guide the patient to enter the VE and remain in the situation until their SUDS rating decreases by 50%.
- Use therapist-guided cognitive challenging during exposure to facilitate expectancy violation (e.g., "What did you expect to happen? What actually happened?").
- Only progress to the next hierarchy item once the patient can stably tolerate the current scenario with low anxiety.
- Relapse Prevention (Final Session): Review progress, discuss the generalization of skills to real-world situations, and create a plan for future self-directed exposure.
Post-Treatment & Follow-Up:
- Re-administer the FNE-B and FAH immediately post-treatment and at 3- and 6-month follow-ups to assess lasting effects.
Protocol for Social Anxiety Disorder (SAD)
This protocol, based on the VIRTUS trial for adolescents and adapted for adults, utilizes social VR scenarios to target fears of negative evaluation [3] [15].
Pre-Treatment Assessment:
- Diagnosis: Assess using the Liebowitz Social Anxiety Scale (LSAS) and Social Phobia Inventory (SPIN). A score of SPIN ≥ 31 and LSAS ≥ 35 indicates elevated SAD symptoms.
- Individualization: Identify core fears (e.g., public speaking, casual conversation, being observed) to tailor VR scenarios.
Exposure Sessions (7 sessions, 45-60 minutes each):
- Introduction and Goal Setting (Session 1): Establish therapeutic alliance, explain the role of avoidance, and set treatment goals.
- VR Exposure Practice (Sessions 2-6):
- Use a head-mounted display (e.g., smartphone-based VR like Google Cardboard or standalone headset) with dedicated software (e.g., Virtual Speech app).
- Exposure hierarchy for public speaking might be:
- Level 1: Speaking to a small, neutral virtual audience (2-3 avatars).
- Level 2: Speaking to a larger audience (10+ avatars).
- Level 3: Audience displays negative behaviors (e.g., looking bored, checking phones).
- Level 4: Receiving and responding to critical questions from the audience.
- In-session exercises focus on violating negative expectations (e.g., "I will stutter and everyone will laugh") to strengthen inhibitory learning.
- Patients are instructed to drop safety behaviors (e.g., speaking too fast, avoiding eye contact) during exposures.
- Review and Consolidation (Session 7): Summarize achievements, discuss any residual avoidance, and plan for in-vivo exercises.
Post-Treatment & Follow-Up:
- LSAS and SPIN are re-administered post-treatment and at 3- and 6-month follow-ups. Qualitative interviews can be conducted to explore patient experiences and acceptance [11].
Protocol for Post-Traumatic Stress Disorder (PTSD)
VRET for PTSD allows for the careful and controlled re-activation of traumatic memories to promote emotional processing and reduce avoidance [22].
Pre-Treatment Assessment:
- Diagnosis: Confirm PTSD diagnosis using the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5).
- Trauma Interview: Conduct a detailed interview to identify specific traumatic events, sensory cues (sights, sounds, smells), and primary negative cognitions.
Therapeutic Sessions (12-15 sessions, 90 minutes each):
- Stabilization and Preparation (Sessions 1-2):
- Build a strong therapeutic alliance.
- Teach emotion regulation and grounding techniques (e.g., mindfulness, controlled breathing).
- Collaboratively develop a detailed "trauma narrative."
- Trauma-Focused VR Exposure (Sessions 3-12):
- The therapist uses VR software to meticulously reconstruct the traumatic environment based on the patient's narrative (e.g., a virtual convoy for combat-related PTSD, a virtual street for a motor vehicle accident).
- The patient is guided to recount the traumatic memory in the present tense while immersed in the VE.
- The therapist can control environmental elements (e.g., time of day, weather, presence of virtual figures) to titrate the emotional intensity and ensure the patient remains within a therapeutic range of anxiety.
- Sessions are audio-recorded, and patients are asked to listen to the recordings between sessions to enhance emotional processing.
- Cognitive Restructuring and Integration (Integrated throughout):
- Use the disconfirmatory evidence from the exposure (e.g., "You survived the event, you are safe now in the therapist's office") to challenge maladaptive beliefs (e.g., "The world is entirely dangerous," "I am incompetent").
- Relapse Prevention and Closure (Final Sessions): Consolidate gains, process the therapy experience, and develop a future-oriented plan.
Post-Treatment & Follow-Up:
- Re-administer the CAPS-5 post-treatment and at 3- and 6-month follow-ups to evaluate symptom reduction and functional improvement.
Therapeutic Workflow and Signaling Pathways
The following diagram illustrates the core therapeutic workflow and the underlying psychological mechanisms activated during VRET, integrating emotional processing, inhibitory learning, and self-efficacy theories [3].
The Scientist's Toolkit: Research Reagent Solutions
For researchers aiming to replicate or build upon these protocols, the following table details essential materials and their functions.
Table 3: Essential Research Reagents and Materials for VRET Studies
| Item Category | Specific Examples | Function in Protocol | Key Considerations |
|---|---|---|---|
| VR Hardware | Pico Goblin, Samsung Gear VR, Oculus Quest, Google Cardboard | Display immersive virtual environments; patient immersion tool. | Standalone headsets offer more flexibility; smartphone-based options reduce cost [15] [38]. |
| VR Software/Platforms | BehaVR, Vizard software, Virtual Speech app | Generate and control exposure scenarios; core experimental stimulus. | Software must allow therapist-controlled customization of scenarios (audience size, character actions) [15] [38]. |
| Clinical Outcome Measures | Liebowitz Social Anxiety Scale (LSAS), Social Phobia Inventory (SPIN), Clinician-Administered PTSD Scale (CAPS-5), Fear of Negative Evaluation Scale (FNE-B) | Quantify symptom severity pre-/post-intervention; primary dependent variables. | Must be well-validated and sensitive to change. Use a battery of scales to capture multiple dimensions [37] [15] [38]. |
| Therapist Manuals | Session-by-session guides for VRE, IVE, and CBT components | Ensure treatment fidelity in RCTs; standardize procedures across therapists. | Manuals should be flexible enough to allow for individualization of exposure hierarchies [3]. |
| Data Management Tools | Endnote, SPSS, R, STATA, Review Manager (RevMan) | Manage literature, perform meta-analysis, and analyze trial data. | Essential for conducting systematic reviews and high-quality RCTs as per PRISMA guidelines [37] [38]. |
Application Notes: Efficacy and Comparative Analysis of Novel VRET Paradigms
Virtual Reality Exposure Therapy (VRET) has established efficacy for anxiety disorders, with a recent 2025 meta-analysis of 33 randomized controlled trials (RCTs) demonstrating a large and significant effect size (SMD = -0.95, 95% CI: -1.22 to -0.69, p < 0.00001) in improving anxiety symptoms compared to conventional interventions [14]. Building on this foundation, research is exploring novel paradigms to enhance accessibility, efficacy, and personalization. The following table summarizes the quantitative evidence for these emerging approaches.
Table 1: Summary of Novel VRET Paradigms: Efficacy and Key Findings
| Paradigm | Reported Efficacy & Key Findings | Population/Disorder Context | Comparative Evidence |
|---|---|---|---|
| Self-Guided VRET | Effective for reducing symptoms of social anxiety, public speaking anxiety, and specific phobias [39] [40]. Positive user experience (safety, usability, acceptability) with low attrition rates [39]. | Social Anxiety Disorder (SAD), Public Speaking Anxiety, Specific Phobias [39] [40] | Lacks long-term (>12 month) data and direct comparison to other self-help interventions (e.g., internet-based CBT) [40]. |
| Adjunct Pharmacotherapy | Proposed to boost fear extinction mechanisms during exposure [41]. Specific efficacy data for combination with VRET is limited and an area for future investigation [41]. | Anxiety-related disorders broadly; target for enhancing extinction learning [41]. | Recognized as an innovation; requires more investigation against standard VRET [41]. |
| Augmentation with Neuromodulation (tDCS) | Hypothesized to facilitate safety signaling and enhance exposure therapy outcomes, particularly for extinction-resistant fears [42]. One study found tDCS did not facilitate greater symptom reduction vs. sham [42]. | Public speaking anxiety; potential application for intergroup anxiety [42]. | An emerging paradigm; current experimental evidence does not consistently support a significant augmentation effect over VRET alone [42]. |
Despite promising results for self-guided applications, barriers to widespread clinical adoption remain significant. A 2025 survey of 694 clinicians found that gaps in knowledge and training, financial constraints, and lack of motivation were major impediments [5].
Experimental Protocols for Novel VRET Paradigms
Protocol: Self-Guided VRET for Public Speaking Anxiety
This protocol is adapted from studies on self-guided VR interventions for anxiety [39] [40].
- Objective: To evaluate the efficacy and user experience of a self-administered VRET program for reducing public speaking anxiety.
- Population: Adults with a primary diagnosis of Social Anxiety Disorder (public speaking subtype) or clinically significant public speaking anxiety.
- Intervention:
- Hardware: Use a commercially available, standalone VR headset (e.g., Meta Quest series) for accessibility and ease of use.
- Software: A self-guided VR application that presents a hierarchy of public speaking scenarios. Scenarios should vary in:
- Audience Size: From a small, empty room to a large auditorium.
- Audience Reactivity: From a passive, neutral audience to an active, negative audience (e.g., individuals looking at phones, frowning).
- Speech Formality: From an informal group discussion to a formal presentation.
- Procedure:
- Pre-Training: Participants receive psychoeducation about anxiety and exposure therapy principles via the VR app.
- Session Flow: Participants select a scenario from the hierarchy. They deliver a speech for a pre-set duration (e.g., 5-10 minutes).
- In-VR Assessment: Subjective Units of Distress (SUDs) are collected in-VR using a visual slider scale before, during, and after each speech.
- Progression: The app algorithm suggests progression to more challenging scenarios based on the participant's SUDs ratings and completion metrics. Participants complete a pre-defined number of sessions (e.g., 6-8) over several weeks.
- Outcome Measures:
Protocol: Augmenting VRET with Transcranial Direct Current Stimulation (tDCS)
This protocol is adapted from a study testing the augmentation of VRET for social anxiety with tDCS [42].
- Objective: To determine if anodal tDCS targeting the medial Prefrontal Cortex (mPFC) enhances fear extinction during VRET for public speaking anxiety, particularly in intergroup contexts.
- Population: Adults with public speaking anxiety, stratified by ethnicity to create in-group and out-group audience conditions.
- Experimental Groups:
- Active tDCS + VRET: Receives 2mA anodal tDCS over the mPFC.
- Sham tDCS + VRET: Receives identical setup but only brief, fading current to mimic sensation.
- tDCS Parameters:
- Electrode Montage: Anodal electrode over FpZ (10-20 EEG system), cathodal electrode over the right deltoid muscle.
- Stimulation Intensity & Duration: 2mA for 20 minutes, ramped up/down over 30 seconds.
- VRET Procedure:
- Stimulation Onset: tDCS begins 5 minutes before VR exposure to allow for preconditioning effects.
- VR Exposure: Participants give a series of speeches (e.g., 4 speeches, 3 minutes each) within a VR environment.
- Audience Manipulation: Half of the speeches are delivered to an in-group audience (same ethnicity as participant), and half to an out-group audience (different ethnicity). Audience behavior can be standardized or mildly negative.
- Anxiety Rating: SUDs are collected after each speech.
- Outcome Measures:
- Primary: Reduction in public speaking anxiety and intergroup anxiety scores from baseline to one-month follow-up.
- Secondary: In-session SUDs, psychophysiological measures (e.g., heart rate), and implicit association tests to measure bias [42].
Signaling Pathways and Experimental Workflows
Neural Circuitry of Fear Extinction in Augmented VRET
The following diagram illustrates the hypothesized neural pathway through which neuromodulation techniques like tDCS are theorized to augment VRET, based on fear extinction learning research [42].
Experimental Workflow for Self-Guided VRET Trial
This workflow outlines the key stages for conducting a clinical trial investigating a self-guided VRET intervention, as detailed in recent systematic reviews [39] [40].
The Scientist's Toolkit: Research Reagent Solutions
This table details the essential materials and tools required for conducting research on the novel VRET paradigms discussed.
Table 2: Essential Research Materials and Tools for Novel VRET Research
| Item Category | Specific Examples & Specifications | Primary Function in Research Context |
|---|---|---|
| VR Hardware Platform | Standalone Head-Mounted Display (HMD) (e.g., Meta Quest 3, HTC Vive Focus 3). | Provides the immersive, interactive 3D environment for exposure. Essential for both clinician-guided and self-guided protocols [14] [40]. |
| Clinical VR Software | Customizable VR environments for specific phobias (e.g., heights, spiders), social situations (e.g., parties, public speaking), or PTSD triggers. | Enables standardized, repeatable, and controllable exposure to feared stimuli. Software should allow for parameter adjustment (e.g., audience size, spider proximity) [43] [5]. |
| Neuromodulation Device | Transcranial Direct Current Stimulation (tDCS) system with EEG cap or headband for electrode placement. | Used to apply non-invasive brain stimulation (e.g., anodal tDCS at 2mA) to target regions like the mPFC, with the goal of augmenting the neural mechanisms of fear extinction during VRET [42]. |
| Outcome Assessment Batteries | Standardized clinician-rated and self-report scales. e.g., HAMA (Hamilton Anxiety Scale), LSAS (Liebowitz Social Anxiety Scale), BAI (Beck Anxiety Inventory), SUDs (Subjective Units of Distress). | Quantifies treatment efficacy and symptom change. Critical for pre-, post-, and follow-up assessments to establish empirical support [14]. |
| User Experience Metrics | System Usability Scale (SUS), custom acceptability questionnaires, cybersickness scales, attrition rate tracking. | Evaluates the feasibility, acceptability, and safety of self-guided VR interventions, which is crucial for understanding their real-world implementation potential [39] [40]. |
| Data Analysis Software | Statistical packages (e.g., R, SPSS, Python) with capabilities for mixed-model ANOVA, meta-analysis, and Bayesian statistics. | Used to analyze clinical outcome data, model learning curves, and synthesize results across studies (meta-analysis) [14]. |
Virtual Reality Exposure Therapy (VRET) is an evidence-based psychological intervention that integrates immersive virtual reality (VR) technology with the core principles of Cognitive Behavioral Therapy (CBT) [17]. Within the CBT framework, VRET specifically operationalizes the exposure component, enabling patients to confront feared stimuli, situations, or memories in a safe, controlled, and customizable virtual environment [44] [45]. This integration represents a significant advancement in therapeutic delivery, addressing key limitations of traditional in vivo (real-life) exposure, such as logistical difficulties, uncontrollability of real-world scenarios, and high patient refusal rates due to initial anxiety [45] [46]. For anxiety disorders, which have a lifetime prevalence of up to 33% and are often undertreated, VRET offers a promising modality to increase accessibility and efficacy of first-line psychological treatment [47] [14].
The theoretical rationale for embedding VRET within CBT is grounded in the same cognitive and behavioral principles that underlie traditional exposure. VRET facilitates emotional processing by allowing for the activation of fear structures and the incorporation of corrective information, and it promotes inhibitory learning by creating new, non-threat associations that compete with existing fearful beliefs [48]. The immersive nature of VR induces a sufficient sense of "presence" – the subjective feeling of being in the virtual environment – to trigger anxiety and enable effective learning and habituation [45]. Consequently, VRET is not a standalone therapy but a powerful tool for delivering exposure within a comprehensive CBT protocol that also includes psychoeducation, cognitive restructuring, and relapse prevention [47].
Theoretical and Mechanistic Basis
The efficacy of VRET within CBT is explained through established psychological models of fear and anxiety. The process can be conceptualized through a logical workflow that outlines the therapeutic pathway from technology setup to clinical outcome.
Key Psychological Mechanisms
- Inhibitory Learning: This is considered a central mechanism in modern exposure therapy [48]. VRET creates optimal conditions for inhibitory learning by repeatedly presenting fear-eliciting virtual stimuli without the feared negative outcome, allowing the brain to form new, safe associations that inhibit the original fear response [49].
- Expectancy Violation: The success of exposure depends on the degree to which the experience violates the patient's negative expectations [49]. VR environments can be meticulously calibrated to ensure this violation occurs, for example, by having a patient who fears negative evaluation during public speaking practice in front of a virtual audience that responds neutrally or positively.
- Emotional Processing and Habituation: VRET allows for prolonged and repeated exposure within a single session, facilitating a decrease in the anxiety response (habituation) and promoting the emotional processing necessary for long-term fear reduction [48].
- Dysfunctional Belief Disconfirmation: By engaging in VR-based behavioral experiments, patients can actively test and disprove maladaptive cognitions (e.g., "If my voice shakes, everyone will laugh at me"), which is a cornerstone of cognitive restructuring in CBT [45].
Efficacy Data and Comparative Outcomes
Empirical evidence from randomized controlled trials (RCTs) and meta-analyses supports the integration of VRET into CBT protocols for various anxiety disorders. The following table summarizes key quantitative findings.
Table 1: Summary of VRET Efficacy from Meta-Analyses and Systematic Reviews
| Anxiety Disorder | Comparison Condition | Effect Size (Hedges' g) / Findings | References |
|---|---|---|---|
| Social Anxiety Disorder (SAD) | Waitlist Control | Significant reduction in SAD symptoms. | [46] |
| In Vivo Exposure | Comparable efficacy to traditional exposure; some studies show superiority, others show non-inferiority. | [44] [46] [27] | |
| Public Speaking Anxiety (PSA) | Waitlist / No Treatment | Large and significant reductions (Hedges' g: -1.39 to -1.46). | [46] |
| In Vivo Exposure | Efficacies appear comparable. | [46] | |
| Specific Phobias | In Vivo Exposure | Similar effectiveness, with both methods yielding high satisfaction rates. Considered a viable treatment option. | [27] |
| Panic Disorder & Agoraphobia | Conventional CBT | Outcomes are less robust; more investigation is needed. | [27] |
| Generalized Anxiety Disorder | Non-VR Treatments | Limited number of studies; efficacy not yet firmly established. | [27] |
| Anxiety Disorders (Overall) | Conventional Interventions (e.g., CBT, TAU) | Significant improvement in anxiety symptoms and level (SMD = -0.95, 95% CI: -1.22 to -0.69). | [14] |
Beyond symptom reduction, VRET offers distinct advantages regarding patient acceptance and adherence. Studies indicate that VRET is well-accepted among patients, with one study noting that 76% of participants preferred it over conventional exposure therapy [45] [14]. It is also associated with relatively low drop-out rates, which is a critical factor for successful treatment completion [46].
Detailed Clinical Protocol for Social Anxiety Disorder
The following protocol, adapted from a published study protocol for a randomized controlled trial, outlines a standardized 10-session CBT program integrating VRET for adult patients with Social Anxiety Disorder (SAD) [45]. This protocol exemplifies the structured integration of technology into a therapeutic framework.
Table 2: Session-by-Session CBT Protocol with Integrated VRET for SAD
| Session | Core CBT Components | VRET-Specific Activities & Exposure Scenarios | Therapist's Role |
|---|---|---|---|
| 1-2: Assessment & Foundation | Clinical intake, diagnostic confirmation, psychoeducation about SAD and CBT model, treatment rationale, goal setting, establishing therapeutic alliance. | Introduction to VR equipment; demonstration of a low-anxiety virtual environment to acclimatize the patient and assess presence and reactivity. | Conductor of assessment; educator; building trust and explaining the rationale for VRET. |
| 3: Cognitive Restructuring I | Introducing the cognitive model; identifying negative automatic thoughts (NATs) related to social situations; beginning cognitive restructuring. | VRET: Initial low-intensity exposure (e.g., walking in a virtual park with few people). Patient practices identifying NATs that arise during the virtual exposure. | Active guide in cognitive techniques; controls VR scenario to ensure it matches the patient's initial capacity. |
| 4-5: Cognitive Restructuring II | Developing more advanced cognitive restructuring skills; challenging underlying assumptions and core beliefs. | VRET: Graded exposure to more challenging scenarios (e.g., having a virtual coffee with a stranger, asking a virtual shop clerk for help). Behavioral experiments are designed to test specific beliefs. | Collaboratively designs exposure exercises to directly test and disconfirm the patient's specific negative beliefs. |
| 6-8: Intensive Exposure | Continued cognitive work with a primary focus on behavioral exposure to consolidate learning and promote habituation/inhibitory learning. | VRET: High-intensity exposure scenarios (e.g., giving a presentation to a virtual audience, being the center of attention at a virtual party, making a mistake in public). Scenarios are repeated to violate expectancies. | Closely monitors patient's anxiety (SUDs); manipulates VR variables in real-time (e.g., audience size, mood) to optimize learning; encourages abandonment of safety behaviors. |
| 9: Relapse Prevention I | Consolidating learning; reviewing progress; identifying gains in cognitive and behavioral domains. | VRET: Practice a "challenge" scenario that incorporates multiple previously feared elements. Focus is on applying learned skills fluidly. | Facilitates a review of what strategies were most effective; helps the patient create a personalized coping plan. |
| 10: Relapse Prevention II & Termination | Developing a long-term maintenance plan; discussing how to handle setbacks; terminating therapy. | May include a final VR exposure as a "booster". Primary focus shifts to planning for in vivo exposures in the real world based on VR successes. | Supports the patient in looking forward; helps generalize skills from virtual to real-world contexts. |
Crossover and Follow-up: In some research designs, after the initial 10-week treatment, participants in control or alternative treatment groups may be offered crossover into the active VRET condition. A six-month follow-up assessment is standard to evaluate the long-term stability of treatment gains [45].
Technical Setup and Research Reagent Solutions
The successful implementation of a VRET-CBT protocol depends on a specific technological ecosystem. The diagram and table below detail the essential components and their functions.
Table 3: Research Reagent Solutions Toolkit for VRET-CBT Implementation
| Component | Specifications & Examples | Primary Function in Research/Therapy |
|---|---|---|
| VR Headset (HMD) | Standalone (e.g., Meta Quest series) or PC-tethered (e.g., HTC Vive). Choice depends on required graphical fidelity and portability. | Provides the immersive visual and auditory experience; the primary interface for patient exposure. |
| Therapeutic Software Platform | Evidence-based platforms (e.g., PsTechVR); libraries of 360° videos or computer-generated environments for various phobias and social situations. | Delivers the controlled exposure stimuli; allows for standardization and replication across research participants. |
| Therapist Control Dashboard | A separate interface (tablet or computer) for the therapist. | Enables real-time control of the VR environment (pausing, adjusting scenario intensity) during the session to ensure optimal therapeutic dosing. |
| Input & Tracking System | Hand controllers, motion sensors, and head tracking. | Allows for user interaction with the virtual environment (e.g., gesturing, speaking to avatars), enhancing realism and presence. |
| Biofeedback Sensors (Optional) | Wearable heart rate (HR) monitors, galvanic skin response (GSR) sensors, or respiration belts. | Provides objective, real-time physiological data on anxiety arousal, allowing the therapist to tailor the session and measure psychophysiological outcomes. |
| Validated Clinical Scales | Social Interaction Anxiety Scale (SIAS), Liebowitz Social Anxiety Scale (LSAS), Beck Anxiety Inventory (BAI), self-rated Units of Distress (SUDs). | Used for pre-/post-assessment, screening, and measuring primary and secondary outcomes in clinical trials. |
Considerations for Research and Clinical Implementation
Blended and Self-Guided Formats
Emerging research explores blending VRET with internet- and mobile-based interventions (IMIs) [49]. In these "blended" models, patients might complete VRET exercises on their own using a smartphone and a portable headset, while receiving therapeutic guidance remotely. Qualitative studies suggest that even in self-guided formats, psychotherapeutic support remains a central factor perceived by patients as contributing to their improvement [49]. This highlights that VRET is an adjunct to, not a replacement for, the therapeutic process.
Standardization and Protocol Fidelity
A significant challenge in the field is the lack of standardization in VRET protocols, which limits translatability and comparability across studies [41]. Future research should aim to develop and validate unified protocols for specific anxiety disorders, detailing the number, duration, and progression of exposures, as well as the specific cognitive techniques to be integrated at each stage.
Safety and Ethics
While generally safe, VRET requires careful implementation. Therapists must be trained to manage potential cyber-sickness (VR-induced nausea) and to ensure that the level of exposure, while provocative, does not lead to overwhelming distress or premature termination. Data privacy and security of any patient data collected through the platforms must also be ensured [46].
Navigating Challenges in VRET: Technical, Clinical, and Methodological Hurdles
Application Note: Understanding and Mitigating Adverse Effects in VR Therapy
Virtual Reality Exposure Therapy (VRET) presents a promising modality for treating anxiety disorders, but its efficacy can be compromised by technical and safety challenges. Cybersickness, visual fatigue, and equipment limitations are significant considerations that researchers and clinicians must address to ensure both patient safety and therapeutic validity. A foundational understanding of these issues is critical for designing robust clinical trials and developing effective, deployable VRET interventions.
The sense of presence—the subjective feeling of "being there" in the virtual environment—is a key therapeutic mechanism in VRET [50] [25]. However, this immersion can be disrupted by technical imperfections. Cybersickness, a form of motion sickness induced by VR, is a common negative effect characterized by symptoms like nausea, disorientation, and general discomfort [50]. Its underlying mechanism is often explained by the sensory conflict theory, which posits a discrepancy between visual system inputs (perceiving motion) and vestibular system inputs (sensing no physical movement) [50]. It is estimated that up to 80% of VR users may experience symptoms after just 10 minutes of exposure [50].
Visual fatigue encompasses symptoms such as eye strain, blurred vision, and headache, often resulting from prolonged VR use [51] [52]. A primary technical cause is vergence-accommodation conflict [51]. In the real world, our eyes simultaneously converge (rotate inward/outward) and accommodate (focus) on an object. In many VR systems, the eyes must converge on a virtual object at a simulated depth, but must still focus (accommodate) on the fixed physical plane of the headset screens. This mismatch can lead to significant visual discomfort and fatigue [51].
Equipment limitations of current Head-Mounted Displays (HMDs), such as limited field of view, inadequate display resolution, and the weight of the device, can exacerbate these issues and create barriers to clinical adoption [51] [53]. Furthermore, the physical hindrance of the hardware, including discomfort from wearing VR glasses, is a noted barrier for patients [53]. Addressing these technical and safety considerations is therefore not merely an engineering challenge but a fundamental prerequisite for successful clinical implementation.
Table 1: Common Cybersickness Symptoms and Measurement Tools
| Metric Category | Specific Measure | Description & Purpose | Typical Findings/Scale |
|---|---|---|---|
| Cybersickness Symptoms | General Discomfort, Headache, Eye Strain | Core oculomotor symptoms measured via standardized questionnaires [50]. | Increase post-VR: Discomfort +0.6, Eye Strain +0.66, Headache +0.43 (VRSQ scale) [50]. |
| Subjective Assessment | Virtual Reality Sickness Questionnaire (VRSQ) | Evaluates cybersickness severity, focusing on oculomotor and nausea domains [50]. | Quantifies symptom intensity pre- and post-VR exposure [50]. |
| Subjective Assessment | Simulation Sickness Questionnaire (SSQ) | A widely used tool for measuring simulator sickness, though noted to have methodological limitations [50]. | Assesses nausea, oculomotor, and disorientation symptoms [50]. |
| Objective Assessment | Eye Gaze Dynamics | Using deep learning models to detect visual fatigue from continuous eye-gaze patterns in VR [52]. | Detection accuracy of up to 94% in tasks with high visual attention (e.g., video viewing, reading) [52]. |
| Performance Metric | Attrition Rate | An indicator of acceptability and safety in self-guided VR therapy studies [34]. | Reported as low in self-guided VR interventions for anxiety, suggesting good tolerability [34]. |
Table 2: Technical Standards and Fatigue Detection Methods
| Area of Focus | Standard / Model | Key Parameters / Metrics | Purpose / Application Context |
|---|---|---|---|
| International Standards (Safety/Comfort) | ANSI 8400 (UL) | Real scene field of view, optical transmittance, display flicker, motion-to-photon latency [51]. | Provides guidance for commercial/industrial XR use to minimize collision/fall risks and discomfort [51]. |
| International Standards (Visual Fatigue) | ISO 9241-392 | Interpupillary distance (IPD) mismatch, interocular geometric misalignments (vertical, rotational), luminance/color differences [51]. | Offers guidance for mitigating factors that cause visual fatigue when using stereoscopic images [51]. |
| Fatigue Detection Model (Physical) | Adaptive Model using OWA & Fuzzy Logic | Aggregates multiple kinematic metrics from VR rehabilitation exercises to classify fatigue levels [54]. | Designed for physical rehabilitation (e.g., upper limb therapy); provides scalable, personalized fatigue assessment [54]. |
| Fatigue Detection Model (Visual) | Deep Learning-based Gaze Analysis | Analyzes continuous cyclopean eye-gaze trajectories (horizontal and vertical angles) [52]. | Non-intrusive, real-time detection of visual fatigue for adaptive VR systems across various tasks [52]. |
Experimental Protocols for Safety and Efficacy Assessment
Protocol for Assessing Cybersickness in a Therapeutic VR Session
This protocol is designed to quantitatively evaluate the incidence and severity of cybersickness symptoms during a VR relaxation session, as applied in recent clinical studies [50] [55].
1. Objective: To measure the propensity of a therapeutic VR environment to induce cybersickness and evaluate its overall acceptability for patients with anxiety disorders.
2. Materials and Equipment:
- A commercially available VR headset (e.g., Meta Quest 2) [50].
- A curated, immersive 360° video or interactive environment (e.g., a natural landscape like the Venice Canals) with a duration of approximately 15 minutes [50] [55].
- A quiet, controlled testing room to minimize external stimuli [50].
- Standardized questionnaires: Virtual Reality Sickness Questionnaire (VRSQ) and I-PANAS-SF (for emotion) [50].
3. Participant Setup:
- Participants should be seated on a stationary or swivel chair to prevent falls and allow for comfortable head rotation [50].
- The VR headset is fitted, ensuring the Interpupillary Distance (IPD) is correctly adjusted for each user to minimize visual strain [51].
- Instruct participants to avoid excessive or rapid head movements and to focus on natural exploration of the environment [50].
4. Procedure:
- Pre-Session Assessment: Participants complete the VRSQ and I-PANAS-SF questionnaires to establish a baseline [50].
- VR Exposure: Participants experience the 15-minute VR session. The session content should be passive (e.g., watching a 360° video) or a low-interactivity relaxation exercise [50] [55].
- Post-Session Assessment: Immediately following the session, participants complete the VRSQ and I-PANAS-SF again [50].
- Optional Longitudinal Tracking: For multi-session therapies, administer the questionnaires at multiple time points to track symptom adaptation or accumulation.
5. Data Analysis:
- Calculate the mean increase in VRSQ symptom scores (e.g., general discomfort, eye strain, headache) from pre- to post-session [50].
- Analyze I-PANAS-SF scores to determine if positive emotions predominate over negative ones despite any cybersickness symptoms [50].
- A low attrition rate and high self-reported usability scores can serve as complementary indicators of acceptability [34].
Protocol for Objective Visual Fatigue Detection using Eye-Tracking
This protocol leverages integrated eye-tracking in modern HMDs to objectively detect visual fatigue, moving beyond subjective questionnaires [52].
1. Objective: To continuously and unobtrusively monitor and classify visual fatigue levels during VR exposure using eye-gaze patterns.
2. Materials and Equipment:
- An eye-tracking-enabled VR headset (e.g., HTC Vive Pro Eye) sampling at a high frequency (≥ 250 Hz) [52].
- Software for executing standardized visual tasks and recording binocular gaze data.
3. Visual Tasks (from GazeBaseVR dataset [52]):
- Vergence Task: A target shifts between two depths, stimulating convergence and divergence eye movements. (Duration: ~1 min).
- Smooth Pursuit Task: A target moves horizontally at increasing velocities (5, 10, 20 dva/s). (Duration: ~30s per velocity).
- Video Viewing: Participants watch a short, dynamic video clip (e.g., animated film). (Duration: ~38s).
- Reading Text: Participants read a short passage of text displayed on a virtual screen. (Duration: Self-paced).
- Random Saccade Task: A target appears at random positions on the display, triggering rapid saccades. (Duration: 80-120s).
4. Procedure:
- Participants perform the battery of tasks at the beginning (baseline) and end of a prolonged VR session.
- Binocular gaze data (horizontal and vertical gaze angles for the cyclopean eye) are recorded continuously throughout all tasks at 250 Hz [52].
5. Data Analysis and Modeling:
- Feature Extraction: Gaze trajectories from the tasks are segmented and used as input features.
- Model Classification: A deep learning classifier (e.g., EKYT model) is trained to differentiate between pre-fatigue and fatigue states based on the gaze patterns [52].
- Validation: Model accuracy is validated against self-reported fatigue measures or therapist observations. Accuracies of up to 94% have been demonstrated for high-attention tasks like video viewing and reading [52].
Visualized Workflows and Pathways
VR Adverse Effects Pathway
VR Therapy Safety Protocol
The Scientist's Toolkit: Research Reagents & Essential Materials
Table 3: Essential Tools for VR Safety and Efficacy Research
| Tool / Material | Function / Purpose in Research | Exemplars / Specifications |
|---|---|---|
| VR Headset with Eye-Tracking | Enables presentation of therapeutic environments and collection of high-resolution gaze data for objective visual fatigue detection [52]. | HTC Vive Pro Eye, Varjo XR系列; Sampling rate ≥ 250 Hz [52]. |
| Standardized Questionnaires (Cybersickness) | Quantifies subjective severity of cybersickness symptoms before and after VR exposure for validated outcome measurement [50]. | Virtual Reality Sickness Questionnaire (VRSQ), Simulation Sickness Questionnaire (SSQ) [50]. |
| Standardized Questionnaires (Emotion/Presence) | Assesses emotional response and the sense of "being there" (presence), which is a key therapeutic mechanism [50] [55]. | I-PANAS-SF (Emotion) [50], Spatial Presence Experience Scale (SPES) [50]. |
| Fatigue Detection Algorithms | Provides objective, continuous classification of user fatigue states by analyzing kinematic or eye-gaze data, moving beyond subjective reports [52] [54]. | Deep learning models for gaze analysis [52]; Data fusion models (OVA with fuzzy logic) for physical fatigue [54]. |
| Visual Testing Software | Prescribes standardized visual tasks to elicit specific eye movements for consistent baseline and fatigue-state measurement across participants [52]. | Custom software implementing vergence, smooth pursuit, video viewing, reading, and random saccade tasks [52]. |
| Biofeedback Sensors (Optional) | Provides physiological data for correlational analysis or biofeedback-enhanced relaxation (e.g., modulating the virtual environment with heart rate) [56]. | EEG [56], Heart Rate Variability (HRV) Monitors [55]. |
Application Notes: The Landscape of VR Therapy Implementation
The integration of Virtual Reality Exposure Therapy (VRET) into mainstream mental healthcare, particularly for anxiety disorders, is hampered by a complex set of implementation barriers. Despite strong evidence supporting its efficacy for conditions such as specific phobias, post-traumatic stress disorder (PTSD), and social anxiety disorder, adoption rates among clinicians remain remarkably low, with one systematic review indicating only 3% of mental health professionals report using VR in clinical settings [57]. The table below synthesizes the key quantitative data on these barriers and the reported effectiveness of VRET.
Table 1: Documented Effectiveness and Key Implementation Barriers of VRET for Anxiety Disorders
| Aspect | Reported Data | Context & Sources |
|---|---|---|
| Clinical Adoption Rate | ~3% of mental health professionals | Systematic review of 20 studies (2010-2024) [57] |
| Therapist Interest Group (IG) | 10 out of 694 clinicians | Survey of Austrian clinical psychologists/psychotherapists; only 10 were active VR users [58] |
| Success Rates for Specific Phobias | 60% to 90% | Analysis of multiple peer-reviewed studies; results vary by individual and condition [59] |
| Reported Cost of VR Systems | $1,500 - $10,000+ for professional setups | Basic professional systems start at ~$1,500; comprehensive platforms can exceed $10,000 [59] |
| Primary Barriers: Financial | High costs and unfavorable cost-benefit ratio | Frequently cited by therapists as a major impediment to adoption [58] [57] |
| Primary Barriers: Professional | Lack of knowledge, training, and time | Thematic analysis identifies these as significant professional hurdles [58] |
| Primary Barriers: Technological | Cybersickness, immature technology, lack of equipment | Concerns about side effects and technical limitations [58] [25] |
| Primary Barriers: Therapeutic | Concerns about clinical applicability and the "real" therapeutic relationship | Clinician apprehension about VR's role in therapy [58] |
The barriers are not merely perceptual but are rooted in tangible structural challenges. A 2024 survey of 694 Austrian clinical psychologists and psychotherapists found that only 10 participants were using therapeutic VR, underscoring the significant gap between evidence and practice [58]. Thematic analysis from this study categorizes the barriers into four main themes: professional (e.g., lack of knowledge and training), financial (e.g., high costs), therapeutic (e.g., concerns about the therapeutic relationship), and technological (e.g., cybersickness and technical immaturity) [58]. A separate systematic review confirms that beyond cost, mental health professionals are concerned about technical limitations, treatment suitability, potential side effects, and the additional workload and time investment required [57].
Experimental Protocols for Implementation Research
For researchers aiming to develop and test strategies to overcome these dissemination barriers, the following protocols provide a methodological framework.
Protocol 1: Evaluating a Multi-Component VRET Training Program for Clinicians
Objective: To assess the efficacy of a specialized training program in increasing VRET adoption and self-efficacy among licensed mental health professionals.
Background: A primary barrier to VRET dissemination is a lack of structured training, which leads to gaps in knowledge and low confidence among clinicians [58] [57]. This protocol is designed to measure the impact of a comprehensive training intervention.
Methodology:
- Study Design: A randomized controlled trial (RCT) or a pre-post longitudinal intervention study.
- Participants: Licensed mental health professionals (e.g., psychologists, psychiatrists) with no prior VRET experience. Participants are recruited from diverse settings (hospitals, private practices, university clinics).
- Intervention Group:
- Technical Proficiency Module (2 Hours): Hands-on training with VR hardware (e.g., Meta Quest) and clinical software. Covers account setup, navigating clinician dashboards, selecting and customizing virtual environments for specific anxiety disorders, and safety protocols [60].
- Clinical Application Module (4 Hours): Covers the ethical and effective integration of VR into Cognitive Behavioral Therapy (CBT) sessions. Topics include exposure therapy principles, obtaining informed consent for VR, structuring sessions, monitoring for adverse reactions (e.g., cybersickness, anxiety spikes), and progress tracking [60].
- Supervised Practical Sessions: Participants conduct mock VRET sessions under the guidance of a certified VRET trainer, receiving feedback on both technical and clinical skills [61].
- Control Group: Receives a packet of informational literature on VRET principles and evidence.
- Outcome Measures:
- Primary: Pre- and post-training assessments of VRET knowledge and clinical self-efficacy (via validated scales).
- Secondary: Rate of actual VRET implementation in practice at 3, 6, and 12-month follow-ups. Qualitative interviews on perceived barriers and facilitators.
- Data Analysis: Mixed-effects models to compare changes in outcome measures between groups over time. Thematic analysis for qualitative data.
Protocol 2: Investigating a Blended-Care, Low-Cost VRET Delivery Model
Objective: To determine the efficacy and acceptability of a smartphone-based VRET intervention integrated with a guided mobile platform for treating specific phobias.
Background: High costs and inaccessible equipment are major barriers. This protocol tests a scalable model using affordable smartphone-VR headsets and 360° videos to deliver exposure therapy, reducing the financial and logistical burden [11].
Methodology:
- Study Design: A randomized controlled trial (RCT).
- Participants: Adults with a primary diagnosis of a specific phobia (e.g., acrophobia, aviophobia) confirmed by a structured clinical interview.
- Interventions:
- Experimental Group (Blended Mobile VRET): Participants use a smartphone inserted into a low-cost head-mounted display (e.g., Google Cardboard) to view graded, prerecorded 360° video scenarios tailored to their phobia. This is integrated with a mobile-based intervention (IMI) app that provides psychoeducation, relaxation techniques, and homework assignments. The program includes weekly guidance from a remote therapist via secure messaging or brief video calls [11].
- Active Control Group (Traditional In-Vivo Exposure): Participants receive the same number of therapist-guided sessions involving gradual, real-life exposure to phobic stimuli.
- Outcome Measures:
- Primary: Change in phobia symptom severity from baseline to post-treatment (e.g., measured by the Fear Questionnaire).
- Secondary: Measures of cost-effectiveness, participant acceptability and engagement, dropout rates, and therapeutic alliance.
- Data Analysis: Intention-to-treat analysis using ANOVA or mixed models to compare symptom reduction between groups. Qualitative thematic analysis of participant interviews regarding their treatment experience.
Visualizing Implementation Strategy
The following diagram maps the logical workflow for overcoming the primary barriers to VRET dissemination, from identifying the core problem to implementing and evaluating targeted solutions.
The Scientist's Toolkit: Research Reagent Solutions
For research teams conducting studies on VRET implementation and efficacy, the following table details essential materials and their functions within the experimental context.
Table 2: Key Research Reagent Solutions for VRET Implementation Studies
| Item Category | Specific Examples & Specifications | Primary Function in Research Context |
|---|---|---|
| VR Hardware Platform | Standalone Head-Mounted Display (HMD) (e.g., Meta Quest series); Smartphone-based HMD (e.g., Google Cardboard) [11] | The core delivery device for immersive therapeutic environments. Standalone HMDs offer high interactivity; smartphone-based systems provide a low-cost alternative for accessibility research. |
| Clinical VR Software | Specialized therapeutic platforms (e.g., Virtually Better, PsTechVR); Custom-built 360° video environments for specific phobias [59] [61] | Provides controlled, graded exposure scenarios (e.g., virtual planes, heights, social settings). Enables customization of stimuli and difficulty based on the patient's fear hierarchy. |
| Biometric Sensors | Heart rate monitor (e.g., Polar H10), electrodermal activity (EDA) sensor, smartwatches with PPG sensors [62] | Provides objective, real-time physiological data on anxiety arousal (e.g., heart rate variability) during VR exposure sessions for outcome measurement and biofeedback. |
| Standardized Clinical Assessments | Fear Questionnaire (FQ), PTSD Checklist (PCL-5), Social Phobia Inventory (SPIN) [11] | Validated tools for quantifying baseline symptom severity and pre-post intervention changes as primary or secondary outcome measures. |
| Training & Certification Materials | Structured training curricula (e.g., PsyTech VR Certification, Virtually Better's 2-day VRE training) [60] [61] | Standardizes clinician training across research conditions, ensuring fidelity in the delivery of the VRET intervention and mitigating the "lack of training" barrier. |
| Data Management System | HIPAA/GDPR-compliant cloud storage, encrypted local servers | Securely manages and stores protected health information (PHI), session data from VR software, and physiological recordings in accordance with ethical guidelines. |
Virtual Reality Exposure Therapy (VRET) represents a paradigm shift in the treatment of anxiety disorders, creating controlled, immersive digital environments where patients can confront feared stimuli without real-world danger [43]. The efficacy of VRET is well-established for specific phobias, social anxiety disorder (SAD), post-traumatic stress disorder (PTSD), and performance anxiety, with meta-analyses demonstrating effect sizes comparable to, and sometimes surpassing, traditional in vivo exposure [43] [34]. However, the burgeoning field of VR-based mental health interventions faces a critical challenge: the lack of uniform software and delivery frameworks. This protocol standardization deficit hampers reproducibility, obscures mechanistic understanding, and impedes regulatory approval pathways. For researchers, clinicians, and drug development professionals, establishing common technical specifications, treatment protocols, and evaluation metrics is not merely an academic exercise but a fundamental prerequisite for translating immersive therapeutics from promising innovation to established, evidence-based medicine.
The Current Landscape: A Fragmented Ecosystem
The VRET research and clinical landscape is characterized by significant methodological heterogeneity. A review of self-guided VR therapy for anxiety revealed variable effect sizes, high usability, and low attrition, but noted a conspicuous "lack of standardised assessments to measure user experiences" [34]. This inconsistency extends to core components of the therapeutic process.
Table 1: Key Variability in Current VRET Research and Applications
| Domain of Variability | Representative Examples from Literature | Impact on Research and Practice |
|---|---|---|
| Treatment Duration & Dosage | - 5-7 sessions for social anxiety [3]- Single session for public speaking fear [3]- 56 sessions for chronic pain (RelieVRx) [63] | Difficulties in determining optimal therapeutic dose and comparing efficacy across studies. |
| Level of Guidance | - Therapist-guided sessions in clinical settings [3] [17]- Fully self-guided interventions for accessibility [34] | Impacts scalability, cost, and the therapeutic mechanisms (e.g., role of therapist vs. software). |
| Technical Platforms & Content | - Custom-built software for research (e.g., VIRTUS trial) [3]- Commercial platforms (e.g., PsyTechVR) with pre-built scenario libraries [64] | Creates interoperability issues and limits the generalizability of findings. |
| Outcome Measurement | - Primary: SPAI-18, LSAS-avoidance [3]- Secondary: Psychosocial functioning, resilience [3]- User experience: Usability, acceptability rates [34] | Heterogeneous success metrics complicate meta-analyses and consensus on efficacy. |
This fragmentation is not trivial. It directly impacts the ability to aggregate data across studies, identify the active ingredients of successful VRET, and develop clear guidelines for clinical implementation. Furthermore, for professionals in drug development, this lack of standardization presents a significant barrier to adopting VRET as a complementary digital therapeutic or as a tool for measuring intervention outcomes in clinical trials.
A Proposed Standardized Framework for VRET Development and Delivery
To address this critical gap, we propose an integrated framework for VRET protocol standardization, synthesizing best practices from recent efficacy trials and digital therapeutic (DTx) development pipelines.
Core Software and Hardware Specifications
Standardization must begin with the foundational technological layer. Based on current research and commercial applications, a consensus on minimum and optimal specifications is possible.
Table 2: Proposed Standardized Technical Specifications for Clinical VRET
| Component | Minimum Specification | Optimal/Recommended Specification | Functional Rationale |
|---|---|---|---|
| VR Headset | Standalone (e.g., Meta Quest 2/3) [17] | PC-tethered for high fidelity (e.g., HTC Vive) [17] | Balance between immersion, graphical fidelity, and ease of clinical deployment. |
| Tracking | 3 Degrees of Freedom (3DoF) | 6 Degrees of Freedom (6DoF) with hand controllers [17] | 6DoF enables natural movement and interaction, enhancing presence and ecological validity. |
| Processing | Integrated mobile processor (standalone) | Computer with dedicated GPU (NVIDIA RTX 3060+), multi-core CPU, 16GB RAM [17] | Ensures smooth, high-frame-rate rendering to minimize simulator sickness and maximize immersion. |
| Software Platform | Library of pre-programmed, evidence-based scenarios (e.g., for public speaking, crowds) [64] [17] | Platform with customizable scenarios, real-time therapist control, and integrated biofeedback (e.g., PsyTechVR, DTx-ACT platform) [64] [63] | Enables protocol fidelity while allowing personalization to individual patient triggers and progress. |
| Biofeedback Integration | Not required | Heart rate, respiration rate monitors [17] | Provides objective, real-time data on arousal for therapist decision-making and efficacy assessment. |
Standardized Therapeutic Delivery Protocol
The therapeutic process itself must be structured to ensure both efficacy and reproducibility. The following workflow outlines a standardized protocol from patient intake to follow-up, adaptable for various anxiety disorders.
Figure 1: Standardized therapeutic workflow for VRET, from intake to follow-up.
Pre-Treatment Phase:
- Comprehensive Assessment: Utilize standardized clinician-administered interviews and self-report measures (e.g., LSAS-avoidance for social anxiety [3], STAI-Y for performance anxiety [30]) to establish diagnosis, symptom severity, and primary fear triggers.
- Psychoeducation and Informed Consent: Explain the rationale of VRET, including the role of inhibitory learning and expectancy violation [3], and address concerns regarding technology and exposure.
Per-Session Protocol (5-7 session cycle, based on the VIRTUS trial [3]):
- Customization: The therapist selects or customizes the VR scenario from a standardized library (e.g., a classroom for public speaking anxiety, a crowded mall for agoraphobia) to match the patient's individualized fear hierarchy [64] [17].
- Baseline Measurement: Collect subjective units of distress (SUDs) and physiological baseline readings (e.g., heart rate) if biofeedback is available [17].
- Graded VR Exposure: The therapist controls the intensity and duration of exposure in real-time, following a graded hierarchy. The session is conducted with the aim of facilitating inhibitory learning through expectancy violation rather than simple habituation [3].
- Post-Session Debrief: Conduct a structured debrief focusing on cognitive restructuring, discussing discrepancies between feared and actual outcomes, and reinforcing self-efficacy [3].
Post-Treatment and Follow-Up:
- Standardized Post-Treatment Assessment: Re-administer primary and secondary outcome measures immediately post-treatment and at scheduled follow-ups (e.g., 3- and 6-months) [3].
- Between-Session Tasks: Assign practice tasks, which may include additional, prescribed self-guided VR exposures or in vivo exercises to promote generalization [64].
Experimental Protocols for Efficacy Evaluation
For researchers designing trials to evaluate VRET interventions, adherence to a standardized experimental protocol is critical. The following section details a rigorous methodology based on current high-quality research protocols.
Randomized Controlled Trial (RCT) Protocol for Social Anxiety
This protocol is adapted from the VIRTUS trial, a robust RCT evaluating VRET for adolescents with social anxiety [3].
Primary Objective: To evaluate the efficacy and acceptability of VRET compared to in vivo exposure (IVE) and a waitlist control (WL) in a sample of individuals with social anxiety.
Methods:
- Participants: 120 participants (ages 12-16 for adolescent focus, adaptable to adults) with subclinical to moderate social anxiety. Power analysis should be conducted a priori to determine sample size.
- Design: Three-arm RCT (VRE vs. IVE vs. WL). Participants in the active conditions undergo a seven-session exposure-based intervention.
- Randomization: Use stratified randomization to ensure equal distribution of baseline anxiety severity and gender across groups. Implement single-blinding where outcome assessors are blinded to group assignment [30].
- Interventions:
- VRE Condition: Exposure is delivered via HMD using a software platform with a library of social scenarios (e.g., public speaking, meeting new people). Therapists control scenario parameters in real-time.
- IVE Condition: Traditional in vivo exposure involving role-play and real-world social tasks.
- WL Condition: No active intervention for the trial duration, with optional crossover to active treatment post-trial.
- Measures:
- Primary Outcomes: Social anxiety symptoms (e.g., SPAI-18, LSAS-avoidance) [3].
- Secondary Outcomes: General well-being, depression, psychosocial functioning, and proposed mechanisms of change (expectancy violation, self-efficacy) [3].
- User Experience: Acceptability, usability, and attrition rates [34].
- Assessment Points: Baseline, post-treatment, 3-month, and 6-month follow-ups.
- Data Analysis: A series of linear mixed model (LMM) analyses to examine and compare intervention effects over time, using an intention-to-treat approach.
Digital Therapeutic (DTx) Development Protocol
For the development of VR-based DTx, a structured, phase-based approach is essential for regulatory approval and clinical translation. The following framework is derived from the development of DTx-ACT, an interactive VR system for depression [63].
Figure 2: A five-phase practical framework for developing interactive VR-based digital therapeutics.
Phase 1: Preliminary Research
- Input: Identify and select an Evidence-Based Practice (EBP) with a structured protocol suitable for digital transformation, such as Cognitive Behavioral Therapy (CBT) or Acceptance and Commitment Therapy (ACT) [63].
Phase 2: Design
- Activity: Apply a Session Structuring System (SSS) to operationalize the therapy protocol into modular VR sessions, defining goals, duration, and activities at both macro (whole program) and micro (single session) levels [63].
- Activity: Design interactive VR elements, incorporating principles of gamification and multimodal arts (visual, auditory) to enhance user engagement and therapeutic adherence [63].
Phase 3: Development
- Output: Develop the immersive VR modules (e.g., five sessions, 6-12 minutes each) that incorporate therapeutic metaphors and interactive tasks [63].
- Output: Establish a data-driven evaluation framework that collects both clinical outcome data and real-time interaction data (e.g., behavioral patterns, gaze, physiological sensors) [63].
Phase 4: Advancement
- Outcome: Conduct pilot studies to validate usability, safety, and initial efficacy. Use the collected data for iterative refinement of the system [63].
Phase 5: Commercialization
- Outcome: Prepare for and undergo the regulatory approval process (e.g., FDA, NICE, MFDS) [63].
- Outcome: Develop implementation guides for clinical scaling and commercial deployment [64] [63].
The Scientist's Toolkit: Essential Research Reagents and Materials
For research teams embarking on VRET studies, a standardized toolkit of "research reagents" — the core technological and methodological components — is indispensable.
Table 3: Essential Research Reagents for VRET Investigation
| Tool Category | Specific Examples & Specifications | Primary Function in Research |
|---|---|---|
| VR Hardware Platform | Meta Quest 3 (standalone), HTC Vive Pro 2 (PC-tethered) [17] | Provides the immersive medium for stimulus delivery; choice impacts fidelity, mobility, and cost. |
| Therapeutic Software & Scenario Library | Commercial platforms (e.g., PsyTechVR [64]); Custom-built environments (e.g., VIRTUS [3]) | Standardizes the exposure stimulus across participants, ensuring protocol fidelity and reproducibility. |
| Evidence-Based Practice (EBP) Protocol | Modularized CBT or ACT protocols adapted for VR [63] | Serves as the therapeutic "active ingredient"; ensures clinical validity and mechanism-targeted intervention. |
| Outcome Measures (Validated) | Primary: SPAI-18, LSAS [3], STAI [30]Secondary: User experience questionnaires, attrition rates [34] | Quantifies therapeutic change and user engagement, enabling cross-study comparison and meta-analysis. |
| Data Acquisition & Analytics Suite | Integrated biofeedback (heart rate monitors) [17]; Interaction data logging (behavior, gaze) [63] | Provides objective, real-time physiological and behavioral data for mechanistic analysis and personalization. |
| Control Condition Materials | Waitlist protocols; Active comparators (e.g., yoga [30], in vivo exposure [3]) | Allows for the isolation of the specific effect of the VRET intervention from time and non-specific factors. |
The path forward for VRET in anxiety disorders is one of convergent standardization. The proposed frameworks for technical specifications, therapeutic delivery, experimental evaluation, and development pipelines provide a foundational roadmap. Widespread adoption of such standards will empower the field to move beyond proof-of-concept studies toward the creation of a robust, reproducible, and clinically actionable knowledge base. For the research and drug development community, this is the critical step required to unlock the full potential of immersive technology and establish VRET as a cornerstone of modern, evidence-based mental health care.
Application Notes: Clinical Workflow in Virtual Reality Exposure Therapy
Virtual Reality Exposure Therapy (VRET) has emerged as a viable and often advantageous alternative to traditional in-vivo exposure therapy (IVET) for treating anxiety disorders. Its integration into clinical practice requires careful management of therapist roles, patient acceptance factors, and session pacing to maximize therapeutic outcomes. Evidence from recent meta-analyses and clinical trials indicates that VRET produces treatment outcomes comparable to traditional methods for specific phobias and social anxiety disorder, with no statistically significant differences in efficacy between the two approaches [7]. The structured, controllable environment of VR enables precise adherence to exposure therapy principles, such as inhibitory learning, while addressing common logistical and accessibility barriers associated with in-vivo exercises [65].
A critical shift supporting modern VRET implementation is the move from traditional habituation models to the inhibitory learning model. This model does not prioritize fear reduction during exposure sessions but instead focuses on creating new, non-threatening associations with feared stimuli. Key principles guiding session pacing and content include expectancy violation (maximizing the mismatch between patient expectations and actual outcomes), variability in exposure (using unpredictable, variable exposure intensity to enhance learning), and practicing exposures across multiple contexts to reduce the contextual dependence of new learning [65]. Research demonstrates that variable exposure intensity leads to better long-term outcomes, as seen in height phobia treatment where variable exposure resulted in less anxiety at follow-up despite higher peak fear during sessions [65].
Quantitative Efficacy and Acceptance Data
The tables below summarize key quantitative findings on VRET efficacy and patient acceptance from the literature.
Table 1: Comparative Efficacy of VRET versus In-Vivo Exposure Therapy (IVET)
| Anxiety Disorder | Effect Size (Hedges' g) | Key Outcome Measures | Comparative Conclusion |
|---|---|---|---|
| Social Anxiety Disorder (SAD) | Moderate effect sizes for both VRET and IVET [7] | Social Phobia Anxiety Inventory (SPAI-18), Liebowitz Social Anxiety Scale (LSAS) [3] | VRET and IVET are equally effective at reducing social anxiety symptoms [7]. |
| Specific Phobia | Moderate effect sizes for both VRET and IVET [7] | Disorder-specific fear and avoidance measures | VRET generates positive outcomes comparable to IVET [7]. |
| Public Speaking Anxiety | Large reduction sustained at 1- and 3-month follow-ups [3] | Public speaking anxiety scales | VRET is a promising tool for adolescents, though more rigorous research is needed [3]. |
Table 2: Patient Acceptance, Adherence, and Engagement Metrics
| Factor | Metric / Finding | Context / Population |
|---|---|---|
| Treatment Attrition | 6% premature termination in remote ERP vs. 10% in in-person therapy [65] | Suggests technology-delivered interventions may improve adherence. |
| Adolescent Engagement | "Game-like features of VR and its playful elements could increase treatment adherence and motivation" [3] | Notion that individuals may be more willing to engage in VR than in-vivo exposure [3]. |
| Therapeutic Alliance | 66.7% of therapists report positive patient responses to VR-enhanced telehealth [65] | Telehealth-integrated VR (tele-VR) for exposure-resistant patients. |
Experimental Protocols
This section details a protocol for a feasibility randomized controlled efficacy trial comparing telemedicine-based VRET to standard telemedicine for specific phobia, illustrating the application of clinical workflow principles [6].
Protocol: Telemedicine-Based VRET for Animal Phobia
Objective: To assess the feasibility of a fully powered trial and conduct a preliminary examination of clinical outcomes for exposure therapy delivered via a telemedicine-based VR clinic versus standard telemedicine in adults with an intense fear of dogs, snakes, or spiders [6].
Design: A single-site, feasibility randomized controlled efficacy trial.
Participants:
- Inclusion: Adults with self-reported intense fear of dogs, snakes, or spiders.
- Sample Size: A maximum of 60 participants, with a goal of completing treatment with 30 adults [6].
Intervention Groups:
- Doxy.me VR Group: Participants receive 12 weekly sessions of exposure therapy over three months. The exposure exercise portion of each session is conducted within the Doxy.me VR app, a custom VR clinic environment. Participants are provided with Meta Quest 2 VR headsets and can also use a "homework mode" for between-session practice.
- Standard Telemental Health (TMH) Group: Participants receive 12 weekly sessions of exposure therapy over three months via conventional videoconferencing. Exposure exercises are conducted using shared multimedia (e.g., photos, videos) during video calls [6].
Methodology and Workflow:
- Recruitment & Enrollment: Participants are recruited through clinical trial websites, research recruitment sites, and flyers.
- Randomization: Eligible participants are randomly assigned on a 1:1 allocation ratio using the REDCap (Research Electronic Data Capture) randomization module.
- Baseline Assessment: A study therapist administers a baseline assessment of phobia symptoms.
- Therapy Sessions:
- All sessions are conducted remotely.
- For the Doxy.me VR group, the therapist and client meet via videoconferencing and then transition to the Doxy.me VR clinic for the exposure portion. The therapist can spawn and control virtual animals (e.g., select species, size, and behavior states like idle, calm, active, aggressive) within the shared virtual space [6].
- For the standard TMH group, the therapist shares photos and videos of the feared animals to facilitate exposure.
- Data Collection:
- Feasibility Metrics: Enrollment, retention, assessment completion, and treatment protocol fidelity.
- Clinical Outcomes: Specific phobia, anxiety, and depression symptoms, measured via self-report assessments and therapist-administered measures.
- Process Measures: Therapeutic alliance and sense of "presence" in the therapeutic environment.
- Data Analysis: Between-group differences in symptoms will be analyzed using repeated measures ANOVA, co-varying for pre-treatment scores. Data will inform power analyses for a future fully powered trial [6].
Protocol: VRET for Adolescent Social Anxiety (VIRTUS Study)
Objective: To evaluate the efficacy and acceptability of VR exposure (VRE) compared to in-vivo exposure (IVE) in a non-referred sample of socially anxious adolescents and to identify mechanisms of change (e.g., expectancy violation, habituation, self-efficacy) [3].
Design: Randomized Controlled Trial (RCT) with three arms.
Participants: 120 adolescents (ages 12–16) with subclinical to moderate social anxiety [3].
Intervention Groups:
- VRE Condition: Seven-session exposure-based intervention delivered via Virtual Reality.
- IVE Condition: Seven-session exposure-based intervention delivered via traditional in-vivo methods.
- Waitlist Control (WL) Condition.
Methodology and Workflow:
- Assessment Points: Primary and secondary measures of social anxiety and general well-being are assessed at baseline, post-treatment, and at 3- and 6-month follow-ups.
- Intervention: Participants in the active conditions undergo seven sessions of exposure therapy tailored to their social anxiety, such as public speaking, speaking in class, or meeting new people.
- Mechanisms of Change: The study quantitatively and qualitatively investigates three potential mechanisms derived from leading theoretical models:
- Emotional Processing Theory: Measured via within- and between-session habituation.
- Inhibitory Learning Theory: Measured via the degree of expectancy violation.
- Self-Efficacy Theory: Measured via changes in the belief in one's capacity to cope with feared situations [3].
- Data Analysis: A series of linear mixed model (LMM) analyses will examine and compare the effects of the interventions. Thematic analyses will explore participants' experiences and acceptance through qualitative interviews [3].
Visualizations
VRET Clinical Workflow and Therapeutic Mechanisms
The diagram below outlines the core workflow for a VRET session and the primary therapeutic mechanisms targeted at each stage, based on the inhibitory learning model.
Digital Therapeutic (DTx) Development Framework
This workflow depicts the structured, multi-phase framework for translating an evidence-based psychotherapy like ACT into an interactive VR-based Digital Therapeutic (DTx).
The Scientist's Toolkit: Research Reagent Solutions
The following table details key technological and methodological components essential for conducting rigorous VRET research.
Table 3: Essential Research Materials and Tools for VRET Studies
| Item / Solution | Function in VRET Research | Exemplar / Specification |
|---|---|---|
| Head-Mounted Display (HMD) | Primary hardware for delivering immersive VR experiences; tracks user movement and rotation. | Meta Quest 2 [6]; devices with 6 degrees of freedom (6-DOF) tracking for realistic response [63]. |
| VRET Software Platform | Provides the virtual environments and stimuli for exposure; enables therapist control over session parameters. | Doxy.me VR (telemedicine VR clinic) [6]; BraveMind (PTSD scenarios) [65]; custom platforms using Unity/Unreal engines. |
| Clinical Assessment Batteries | Standardized tools to measure primary and secondary outcomes pre-, post-, and during follow-up. | SPAI-18, LSAS (Social Anxiety) [3]; Yale-Brown Obsessive Compulsive Scale (Y-BOCS) [65]; disorder-specific fear thermometers. |
| Therapeutic Alliance Measures | Quantifies the collaborative patient-therapist relationship, a key predictor of outcomes. | Working Alliance Inventory (WAI) [6]. |
| Presence & Realism Questionnaires | Assesses the user's subjective experience of "being" in the virtual environment. | Custom or standardized scales measuring presence, realism, and reality [66]. |
| Data Capture & Management System | Securely manages participant data, randomization, and self-report assessments. | REDCap (Research Electronic Data Capture) [6]. |
| Inhibitory Learning Protocol Guide | Manualized instructions for implementing expectancy violation, variability, and multiple contexts. | Protocols based on Craske et al. [65], detailing techniques like variable-stimulus exposure [65]. |
Application Notes: The Next Generation of VR Exposure Therapy
The integration of Artificial Intelligence (AI) and biofeedback is transforming Virtual Reality Exposure Therapy (VRET) from a standardized tool into a dynamic, personalized therapeutic platform. These technologies enable systems to adapt in real-time to a user's physiological and psychological state, creating a more effective and tailored treatment for anxiety disorders. The table below summarizes the core functions and research support for these key technological integrations.
Table 1: Core Components of Next-Generation VRET Systems
| Component | Primary Function | Research Support & Measured Outcomes |
|---|---|---|
| AI-Powered Personalization | Dynamically adjusts virtual environment (VE) difficulty & content based on user performance and emotional state [67]. | Studies show: Superior efficacy of VR therapies vs. control groups [30]. A systematic review of 132 papers highlights adaptation logic using rules or machine learning [67]. |
| Multimodal Biofeedback | Provides real-time, objective data on user arousal and stress for closed-loop system adaptation [67] [68]. | Devices used: EEG, ECG, GSR, EMG, eye-tracking [67]. Protocols demonstrate: XR biofeedback training improves motor control and sense of agency in functional neurological disorders [68]. |
| Intelligent Virtual Agents | Serves as conversational partners for social skills training in safe, controllable environments [69]. | Implementation: AI (e.g., LLMs) generates natural dialogue for communication training chatbots and NPCs [67]. C2Care's "Camille" provides 24/7 support and guidance [69]. |
| Real-Time Adaptive Logic | Uses machine learning models to interpret user data and decide on system adjustments [67]. | Common Techniques: CNNs for signal classification; LSTMs for predicting user state; Reinforcement Learning for optimizing strategy [67]. |
Experimental Protocols
Protocol 1: AI- and Biofeedback-Enhanced VRET for Social Anxiety
This protocol details a methodology for a closed-loop VRET system that personalizes exposure intensity based on objective physiological data.
1. Objective: To evaluate the efficacy of a real-time adaptive VRET system, compared to a standard fixed-protocol VRET, in reducing anxiety symptoms and improving social functioning in individuals with Social Anxiety Disorder (SAD).
2. Materials and Reagent Solutions: Table 2: Essential Research Toolkit for AI-Enhanced VRET
| Item | Function/Explanation |
|---|---|
| Head-Mounted Display (HMD) | Provides immersive virtual environments. Example: Meta Quest Pro for standalone capability and integrated eye-tracking [67]. |
| Multimodal Biosensor Suite | Captures physiological data: EEG (brain activity), GSR/EDA (electrodermal activity, arousal), ECG (heart rate), EMG (muscle tension), and Eye-Tracker (gaze, pupil dilation) [67]. |
| AI Software Platform | Integrates data and executes adaptation logic. Requires a game engine (Unity/Unreal) and machine learning libraries (e.g., for CNN, LSTM, RL) to process data and control the VE [67]. |
| Validated Psychometric Scales | Measures subjective outcomes: STAI-Y (State-Trait Anxiety), PQ/IPQ (Presence), NASA-TLX (Workload), and disorder-specific scales like the Liebowitz Social Anxiety Scale (LSAS) [67] [30]. |
3. Participant Recruitment and Screening:
- Recruit adults with a primary diagnosis of SAD confirmed by a structured clinical interview.
- Exclude participants with comorbid psychotic disorders, active substance abuse, or epilepsy.
- Use stratified randomization based on baseline anxiety severity to assign participants to either the Experimental (AI-Adaptive) group or the Active Control (Fixed-Protocol VRET) group.
4. Experimental Workflow: The following diagram illustrates the real-time adaptive loop that defines the experimental condition.
5. Intervention Protocol:
- Both groups complete 8 weekly sessions of 60 minutes each.
- Experimental Group (AI-Adaptive): The system operates on the real-time adaptive loop shown above. For example, if biosensors indicate low anxiety (e.g., stable heart rate, low GSR), the system increases the scenario difficulty (e.g., adds more virtual audience members, makes them more expressive).
- Control Group (Fixed-Protocol): Participants progress through a predetermined sequence of social scenarios with standardized difficulty increases, regardless of their physiological response.
6. Data Collection and Analysis:
- Primary Outcome: Change in social anxiety symptoms (LSAS score) from baseline to post-treatment and 3-month follow-up.
- Secondary Outcomes: Changes in state anxiety (STAI-Y1) after each session, physiological habituation indices (e.g., decreasing GSR response to the same stimulus over sessions), and sense of presence (PQ).
- Analysis: Use repeated-measures ANOVA to compare group outcomes over time, and multilevel modeling to analyze the relationship between physiological data and in-session anxiety reports.
Protocol 2: VR-CBT vs. Yoga for Performance Anxiety
This protocol summarizes a rigorous comparative efficacy trial, highlighting the different therapeutic mechanisms and measurement approaches.
1. Objective: To compare the efficacy of VR-assisted Cognitive Behavioral Therapy (VR-CBT) and a yoga-based intervention in reducing performance anxiety in students [30].
2. Study Design:
- A single-blinded, randomized controlled trial with 60 participants allocated to one of two groups (n=30 each) [30].
- VR-CBT Group: Participants undergo exposure to virtual performance situations (e.g., public speaking, exams) with CBT elements integrated. The focus is on cognitive restructuring within the immersive environment [30].
- Yoga Group: Participants engage in a holistic mind-body practice involving postures (asanas), breathing techniques (pranayama), and meditation, aimed at regulating the autonomic nervous system [30].
3. Outcomes and Timing:
- Primary Outcome: Reduction in anxiety, measured by the State-Trait Anxiety Inventory (STAI-Y1 and STAI-Y2 subscales) [30].
- Secondary Outcomes: Emotional regulation and quality of life [30].
- Data Collection: At baseline, immediately after the intervention, and at a follow-up assessment [30].
4. Hypothesized Mechanism of Action: The following diagram contrasts the proposed pathways through which each intervention is expected to alleviate anxiety.
Evaluating VRET Efficacy: Meta-Analytic Evidence and Head-to-Head Comparisons with Gold Standards
Virtual Reality Exposure Therapy (VRET) has emerged as a prominent intervention in the treatment of anxiety disorders, leveraging immersive technology to create controlled, therapeutic environments. As research in this field expands, a critical evaluation of its efficacy requires a clear understanding of how its outcomes compare to both passive and active control conditions. This analysis is essential for researchers, scientists, and drug development professionals to contextualize findings and guide future clinical development. Meta-analyses provide the highest level of evidence by synthesizing results across multiple randomized controlled trials (RCTs), offering quantified effect sizes that distinguish statistically significant improvements from clinically meaningful changes. This article presents a structured analysis of these meta-analytic outcomes, provides detailed experimental protocols, and outlines essential research tools for the field.
Quantitative Meta-Analytic Outcomes
Recent meta-analyses have quantified the efficacy of VRET for anxiety disorders, consistently demonstrating significant effects compared to passive control conditions, while outcomes against active treatments are more varied. The following tables summarize these quantitative findings.
Table 1: Meta-Analytic Effect Sizes for VRET vs. Control Conditions in Anxiety Disorders
| Disorder | Number of Studies | vs. Passive Control (Hedge's g) | vs. Active Control (Hedge's g) | Key References |
|---|---|---|---|---|
| Specific Phobias | 15 | 1.07 [0.22 to 1.92] | 0.30 (Favors VRET) [70] | [70] [14] |
| Social Anxiety Disorder (SAD) | 7 | 0.83 [0.49 to 1.17] | -0.24 (Favors Active) [70] | [70] [14] |
| Panic & Agoraphobia | 7 | 0.90 [0.45 to 1.35] | No Significant Difference [70] | [70] [14] |
| Public Speaking Anxiety (PSA) | 11 (IVET & VRET) | ~1.40 (vs. control for both IVET and VRET) [71] | No Significant Difference (VRET vs. IVET) [71] | [71] [72] |
| PTSD | 6 | 0.67 (Depression only) [0.22 to 1.13] | -0.20 (Favors Active) [70] | [70] [14] |
| Generalized Anxiety Disorder | 2 | No Significant Difference | Not Reported | [70] |
Table 2: Overall Effect of VR Therapy on Anxiety from a Recent Systematic Review
| Population | Number of Studies (Participants) | Overall Effect Size (SMD) | 95% Confidence Interval | P-value |
|---|---|---|---|---|
| Adolescents & Adults with Anxiety Disorders | 33 (n=3182) | -0.95 | [-1.22, -0.69] | < 0.00001 [14] |
Abbreviations: VRET: Virtual Reality Exposure Therapy; IVET: In Vivo Exposure Therapy; SMD: Standardized Mean Difference; g: Hedge's g (effect size where ~0.2=small, ~0.5=medium, ~0.8=large)
Interpretation of Quantitative Findings
The aggregated data leads to several key conclusions:
- Against Passive Controls: VRET demonstrates large, statistically significant effect sizes across most anxiety disorders, particularly for specific phobias, social anxiety, and agoraphobia [70] [14]. This indicates VRET is substantially more effective than no treatment or waitlist conditions.
- Against Active Controls: When compared to established active treatments like traditional in vivo exposure or cognitive-behavioral therapy (CBT), VRET most often shows non-significant differences, suggesting comparable efficacy [71] [72] [70]. However, some high-quality studies indicate that for certain disorders like PTSD and SAD, active treatments might be marginally superior [70].
- Public Speaking Anxiety: Both VRET and In Vivo Exposure Therapy (IVET) show large and nearly identical effect sizes versus control conditions, and direct comparisons find them to be equally efficacious [71].
- Clinical Significance: While these effect sizes are statistically significant, researchers must also consider clinical significance—the magnitude of change that is meaningful to patients. Effect sizes are a key metric for this, with a large effect (e.g., g > 0.80) often suggesting clinical relevance, but this should be interpreted alongside other indices of meaningful change [73].
Detailed Experimental Protocols
To ensure reproducibility and high-quality research, the following protocols outline standard methodologies for RCTs in this domain, based on recent high-quality studies.
Protocol for a Three-Arm RCT (VRET vs. IVET vs. Waitlist Control)
This protocol is adapted from the VIRTUS trial, which investigates VRET for social anxiety in adolescents [3].
1. Study Design and Registration:
- Design: A randomized controlled trial (RCT) with three parallel arms.
- Arm 1: Virtual Reality Exposure (VRE).
- Arm 2: In Vivo Exposure (IVE).
- Arm 3: Waitlist Control (WL).
- Registration: The trial must be preregistered in a public registry (e.g., ClinicalTrials.gov: NCT06379633) before participant enrollment begins [3].
2. Participant Recruitment and Eligibility:
- Sample Size: Target approximately 120 participants to achieve adequate statistical power.
- Population: Adolescents or adults with a primary diagnosis of subclinical to moderate social anxiety disorder (SAD). Diagnosis should be confirmed using a structured clinical interview based on DSM-5 criteria.
- Inclusion Criteria: Ages 12-16 (for adolescent studies) or 18-65 (for adult studies); fluency in the local language.
- Exclusion Criteria: Current high suicidal ideation, psychosis, or ongoing substance-use disorder that could interfere with treatment.
3. Intervention Protocol:
- Format: Both active interventions (VRE and IVE) consist of seven weekly, individually administered exposure sessions.
- VRET Group: Exposure is conducted using a head-mounted display (HMD). Social scenarios (e.g., giving a speech to a virtual audience, meeting new people) are tailored to the individual's fear hierarchy and can be modulated in real-time by the therapist.
- IVET Group: Exposure is conducted in real-life settings. Therapists and participants work together to create in vivo social situations (e.g., initiating conversations, speaking in a group) that match the participant's fear hierarchy.
- Therapist Training: All therapists must be trained in exposure therapy principles and the specific protocol. Adherence and competence should be rated using a fidelity scale (e.g., scoring ≥ 80% on an Adherence Rating Scale) to ensure treatment integrity [74].
- Waitlist Group: Participants continue with their usual activities and are offered the intervention after the final follow-up assessment.
4. Outcome Assessment and Timing:
- Primary Outcomes: Disorder-specific anxiety symptoms, measured by standardized scales (e.g., LSAS-avoidance for social anxiety, SPAI-18).
- Secondary Outcomes: General well-being, depression, resilience, and psychosocial functioning.
- Assessment Timepoints:
- T1: Baseline (pre-intervention)
- T2: Post-treatment (within one week of final session)
- T3: 3-month follow-up
- T4: 6-month follow-up [3]
5. Data Analysis Plan:
- Primary Analysis: Use a series of linear mixed models (LMM) to examine and compare the effects of the interventions over time on the primary outcome measures.
- Mechanisms of Change: Include measures of putative mechanisms (e.g., expectancy violation, habituation, self-efficacy) to conduct mediation analyses.
- Predictors of Response: Collect data on clinical, personality, and VR-related variables to conduct moderation analyses and identify for whom the treatment works best [3].
Integrated Mixed-Methods Protocol
A mixed-methods approach, as recommended in integration principles for health services research, can provide a more comprehensive understanding of VRET's efficacy and acceptability [75] [74].
1. Quantitative Component:
- Follow the RCT protocol above to collect quantitative outcome data.
2. Qualitative Component:
- Data Collection: Conduct semi-structured qualitative interviews with a sub-sample of participants (e.g., n=15-20) from each active intervention arm post-treatment.
- Interview Content: Explore participants' experiences, perceived benefits, challenges, and acceptance of the treatment modality (VR or in vivo).
- Analysis: Use thematic analysis to identify, analyze, and report patterns (themes) within the data. This can reveal why certain mechanisms are effective and uncover barriers to implementation that quantitative data may miss [3] [74].
3. Data Integration:
- Employ a convergent mixed methods design where quantitative and qualitative data are collected concurrently and then merged during the interpretation phase [75].
- Use a joint display (a side-by-side comparison of quantitative results and qualitative themes) to illustrate how the qualitative findings explain, elaborate, or contradict the quantitative results, providing a deeper insight into the intervention's effects [75].
Visualization of Research Workflow and Mechanisms
The following diagrams, generated using Graphviz DOT language, illustrate the standard research workflow for a VRET trial and the theoretical mechanisms of action.
Figure 1: VRET RCT Workflow
Figure 2: VRET Mechanism Pathways
The Scientist's Toolkit: Research Reagent Solutions
This table details key materials and tools essential for conducting rigorous VRET research.
Table 3: Essential Research Materials and Tools for VRET Studies
| Item Category | Specific Examples & Specifications | Primary Function in Research |
|---|---|---|
| VR Hardware | Head-Mounted Display (HMD): Standalone (e.g., Meta Quest Pro) or PC-tethered (e.g., Valve Index). Controllers: Hand-tracking controllers. | Delivers the immersive virtual environment; critical for inducing a sense of presence, a key mediator of treatment效果 [70]. |
| VR Software/Environments | Customizable Social Simulators: Platforms that allow control of audience size, behavior, and responsiveness. Pre-built Scenarios: For public speaking, social interactions, and specific phobias. | Provides the controlled exposure stimuli; enables standardization and replication of exposure hierarchies across participants [3] [72]. |
| Clinical Outcome Measures | Primary Disorder-Specific Scales: e.g., Liebowitz Social Anxiety Scale (LSAS), Beck Anxiety Inventory (BAI), Panic and Agoraphobia Scale. General Well-being: e.g., WHO-5 Well-Being Index. | Quantifies the primary and secondary outcomes of the intervention; ensures validity and allows for cross-study comparisons [3] [14]. |
| Mechanism & Process Measures | Self-Efficacy Scale: Belief in one's capability to perform and cope. Expectancy Violation Scale: Degree to which a negative expectation was disconfirmed. Subjective Units of Distress (SUDS): Repeated measure of anxiety during exposure. | Tests the underlying theoretical models of change (e.g., inhibitory learning, self-efficacy); helps explain how VRET works [3]. |
| Data Management & Analysis Tools | Statistical Software: R, SPSS, Stata. Qualitative Analysis Software: NVivo, Dedoose. Linear Mixed Models (LMM) Packages: e.g., lme4 in R. |
Handles the analysis of longitudinal data from RCTs; supports the integration of quantitative and qualitative data in mixed-methods studies [3] [76]. |
Application Notes: Comparative Clinical Effectiveness
Quantitative Efficacy Analysis
Table 1: Summary of Meta-Analytic Findings on VRET versus IVET Efficacy
| Analysis Focus | Comparison | Effect Size (Hedges g) | 95% Confidence Interval | Clinical Interpretation | Source |
|---|---|---|---|---|---|
| Overall Efficacy for Social Anxiety & Specific Phobia | VRET vs. IVET | Moderate and equivalent | N/A | Both approaches are equally effective at reducing symptoms. | [7] [77] |
| Specific Phobia Subgroup | VRET vs. IVET | No significant difference | N/A | No superiority detected for either modality for specific phobias. | [78] [44] |
| Pre-Post Treatment Improvement | VRET from pre- to post-treatment | 1.20 (post), 1.06 (12-month follow-up) | N/A | Large and sustained clinical effects for VRET. | [78] [43] |
| Broader Anxiety Disorders | VRET vs. Conventional Interventions | SMD = -0.95 | -1.22 to -0.69 | VRET significantly improves anxiety symptoms and levels. | [37] |
| Earlier Meta-Analysis Finding | VRET vs. IVET | 0.34 | 0.05 to 0.63 | Slight but significant effect favoring VRET (results to be treated with caution). | [79] |
Table 2: Patient Perceptions and Practical Implementation Factors
| Factor | In-Vivo Exposure Therapy (IVET) | Virtual Reality Exposure Therapy (VRET) | Source |
|---|---|---|---|
| Patient Willingness | 82% | 90.2% | [80] |
| Key Patient Concerns | Increased anxiety, feelings of embarrassment/shame, condition exacerbation. | Risk of side effects (e.g., cybersickness), efficacy uncertainty, insurance coverage. | [80] |
| Key Advantages | Gold standard, high realism. | Privacy, safety, controllability, comfort, absence of real-life consequences, customizability. | [43] [80] |
| Therapist Barriers | Logistically difficult, time-consuming, inadequate compensation, hard to control. | Need for additional training, initial cost of equipment, potential for simulator sickness. | [43] [78] |
| Logistical Flexibility | Limited to real-world availability and safety of stimuli. | Highly adaptable, repeatable, and accessible within the therapy room. | [44] [43] |
The aggregated evidence from recent meta-analyses and systematic reviews consistently demonstrates that VRET generates positive outcomes in the treatment of Specific Phobia and Social Anxiety Disorders that are comparable to IVET [7] [77] [78]. While some earlier analyses suggested a slight potential superiority of VRET [79], the most current and comprehensive evidence indicates statistical equivalence in efficacy between the two modalities [7]. The choice of intervention can therefore be guided by practical considerations and patient preference rather than a significant efficacy gap.
Experimental Protocols
Protocol 1: Randomized Controlled Trial Comparing VRET and IVET
This protocol is adapted from the methodology of Kuleli et al. (2025) and other cited RCTs [7] [44].
2.1.1 Objective To directly compare the efficacy of Virtual Reality Exposure Therapy (VRET) and In-Vivo Exposure Therapy (IVET) in reducing symptom severity in adults diagnosed with Specific Phobia or Social Anxiety Disorder.
2.1.2 Participant Eligibility
- Inclusion Criteria: Adults (18+); primary diagnosis of Specific Phobia or Social Anxiety Disorder according to DSM-5 or ICD-10 criteria; ability to provide informed consent.
- Exclusion Criteria: Comorbid psychotic disorders, active substance abuse, high suicide risk, uncorrected visual or auditory impairment, conditions predisposing to seizures.
2.1.3 Randomization and Blinding
- Participants are randomly assigned to either VRET or IVET condition using a computer-generated sequence.
- Outcome assessors are blinded to the participant's treatment condition.
2.1.4 Intervention Arms
- VRET Condition: Exposure is delivered via a head-mounted display (HMD). The virtual environments are tailored to the individual's fear hierarchy (e.g., a virtual auditorium for social anxiety, a virtual bridge for acrophobia). The therapist controls the exposure parameters in real-time from a control screen [7] [78].
- IVET Condition: Exposure is conducted with real-world stimuli. For specific phobia, this involves gradual, direct confrontation with the feared object or situation. For social anxiety, this may involve role-playing or real-life social tasks [7].
2.1.5 Common Therapeutic Elements
- Session Structure: Both interventions consist of 5-12 weekly, individual, 60-minute sessions [79].
- Therapeutic Framework: Both are embedded within a Cognitive Behavioral Therapy (CBT) framework, including psychoeducation, fear hierarchy development, exposure exercises, and cognitive restructuring.
- Therapist Guidance: A trained therapist guides all exposure sessions.
2.1.6 Outcome Measures
- Primary Outcome: Change in disorder-specific symptom score from pre- to post-treatment (e.g., Acrophobia Questionnaire for height phobia [81]).
- Secondary Outcomes: General anxiety measures, behavioral avoidance tests (BAT), measures of quality of life, and follow-up assessments at 6 and 12 months.
Protocol 2: Standardized Workflow for VRET Session Implementation
Session Initiation and Setup
The therapist prepares the VR hardware, including the head-mounted display (HMD) and tracking sensors, and selects the appropriate virtual environment. The patient is oriented to the technology and safety procedures [78].
Patient Preparation and Cognitive Framing
The therapist reviews the individualized fear hierarchy with the patient and conducts a brief cognitive preparation to establish the rationale for exposure and set goals for the session [43].
Graduated In-Virtuo Exposure
The patient is immersed in the VR environment. The therapist guides the exposure, gradually increasing the intensity of the anxiety-provoking stimuli based on the patient's Subjective Units of Distress (SUD) and the pre-established hierarchy. The therapist can control the exposure in real-time from an external monitor [43] [78].
Processing and Within-Session Habituation
The therapist encourages the patient to remain in the situation until their anxiety decreases (habituation). The therapist also facilitates cognitive restructuring by challenging maladaptive beliefs about the feared stimuli during and after the exposure [43].
The session concludes with a review of accomplishments. The patient is often assigned "homework" to practice skills or conduct exposures in the real world to promote generalization of learning [78].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for VRET Research
| Item Category | Specific Examples & Specifications | Primary Function in Research | Technical Notes |
|---|---|---|---|
| VR Hardware Platform | Stand-alone HMD (e.g., Oculus Quest, HTC Vive); Desktop-Powered HMD. | Creates the immersive virtual environment for exposure. | Must have head-tracking, motion controllers. Check for comfort for prolonged use. [78] [81] |
| VR Software/Environments | Custom-built environments (e.g., virtual skyscraper, social gathering, spider); Off-the-shelf clinical platforms. | Presents the controlled, graded anxiety-provoking stimuli. | Software should allow therapist control over stimulus parameters (e.g., number of virtual people, height). [44] [78] |
| Diagnostic & Outcome Measures | Structured Clinical Interview (SCID); Disorder-specific scales (e.g., AQ, ATHQ); Behavioral Avoidance Test (BAT). | Ensures accurate participant diagnosis and quantifies treatment efficacy. | Use validated scales for primary outcome. BAT provides objective behavioral measure. [7] [81] |
| Data Collection & Analysis Suite | Statistical software (e.g., R, SPSS, Stata); Secure database for patient data. | Performs meta-analysis and statistical comparison of effect sizes between groups. | Plan for calculation of Hedges' g or similar effect sizes. [7] [37] |
| Psychophysiological Recording | Electro-dermal Activity (EDA) sensors; Heart Rate (HR) monitors. | Provides objective, physiological data on fear arousal during exposure. | EDA is a strong indicator of psychophysiological arousal in VR. [78] |
{#content#}
Virtual Reality Exposure Therapy (VRET) has emerged as a prominent psychotherapeutic intervention for anxiety disorders, with growing empirical support for its short-term efficacy. However, as the field progresses, critical gaps in the evidence base have become apparent, particularly concerning its long-term sustainability and how it compares directly to the gold standard of conventional Cognitive Behavioral Therapy (CBT). This application note synthesizes the current state of evidence from recent meta-analyses and randomized controlled trials (RCTs), highlighting these uncertainties. It further provides detailed experimental protocols to guide future research aimed at addressing these gaps, ensuring that findings are robust, comparable, and clinically translatable. Framed within a broader thesis on VRET for anxiety disorders, this document serves as a strategic guide for researchers, scientists, and drug development professionals navigating this evolving therapeutic landscape.
Current Evidence and Identified Gaps
Recent meta-analyses consolidate the positive short-term effects of VR-based interventions for anxiety. A 2025 meta-analysis of 33 RCTs involving 3,182 participants found that VR therapy significantly improved anxiety symptoms compared to conventional interventions (SMD = -0.95, 95% CI [-1.22, -0.69]) [14] [37]. Similarly, a 2025 RCT on Ukrainian veterans demonstrated that immersive 360° video-based VR therapy led to significant immediate reductions in anxiety (up to 14.5%) and depression (up to 12.3%) upon program completion [82]. For specific phobias and social anxiety disorder (SAD), evidence is strong, showing VRET to be comparable to in-vivo exposure therapy (IVET) [7] [83].
Despite these promising results, significant uncertainties remain, which can be categorized as follows:
- Uncertainty in Long-Term Efficacy: A major limitation across the literature is the lack of long-term follow-up data. While some studies show sustained improvements at 3-6 month follow-ups [3] [83], the evidence beyond 6-12 months is sparse. The 2025 review by Kim et al. notes that the long-term sustainability of VRET effects requires further study [41]. Furthermore, a key finding from CBT for psychosis is that initial effects were not maintained after 6-12 months, underscoring a potential vulnerability in time-limited interventions that must be investigated for VRET [84].
- Uncertainty in Comparison to Conventional CBT: The evidence for VRET being superior or even equivalent to conventional CBT is mixed. While some studies find them equally effective [7] [85], others reveal limitations. For instance, in generalized social anxiety disorder, pure VRET was found to be less effective than in-vivo exposure [83]. A large 2025 RCT for paranoia in schizophrenia spectrum disorders concluded that VR-CBT was not superior to standard CBT [84]. Furthermore, a pragmatic RCT for SAD and agoraphobia (the SoREAL trial) was underpowered and could not draw definitive conclusions on comparative efficacy, highlighting feasibility challenges in real-world settings [85].
- Methodological and Mechanistic Gaps: Over 50% of studies have a high risk of bias, and the overall quality of evidence is often low [83]. There is a notable lack of standardization in VRET protocols, software, and hardware, limiting translatability and comparability [41]. Furthermore, the underlying therapeutic mechanisms—such as the roles of inhibitory learning, habituation, and self-efficacy in a virtual context—are not well understood [3].
Table 1: Summary of Key Evidence Gaps in VRET Research for Anxiety Disorders
| Evidence Gap | Current State of Evidence | Key Uncertainties | Representative Findings |
|---|---|---|---|
| Long-Term Efficacy | Limited and inconsistent | Sustainability of effects beyond 6-12 months; need for longer follow-ups. | Effects in some studies sustained at 3-6 months [3] [83], but not maintained at 6-12 months in others [84]. |
| Efficacy vs. Conventional CBT | Mixed and disorder-dependent | Whether VRET is superior, equivalent, or inferior to gold-standard CBT across different anxiety disorders. | VRET was not superior to CBT for paranoia [84]; comparable to in-vivo exposure for social anxiety and specific phobia [7]. |
| Mechanisms of Change | Poorly understood | Application of theoretical models (e.g., inhibitory learning) in VR; predictors of treatment response. | Roles of expectancy violation, habituation, and self-efficacy in VRET are not well-explored [3]. |
| Protocol Standardization | Lacking | Lack of uniform software, delivery protocols, and dosage guidelines limits comparability and clinical translation. | Noted as a key challenge by Kim et al. (2025); high variability between studies [41] [83]. |
Proposed Experimental Protocols to Address Key Gaps
To systematically address the gaps identified in Table 1, the following detailed experimental protocols are proposed.
Protocol 1: Long-Term Efficacy and Mechanisms of Change (VRET vs. IVET)
This protocol is designed to evaluate the long-term efficacy of VRET and compare it to in-vivo exposure, while also investigating the underlying mechanisms of change.
- 1. Study Design: A randomized controlled trial (RCT) with three parallel arms: (1) VRET, (2) In-Vivo Exposure Therapy (IVET), and (3) Waitlist Control (WL). The design is assessor-blinded.
- 2. Participants:
- Sample Size: 120 participants per arm (360 total), powered to detect a moderate effect size (f=0.25, α=0.05, β=0.8).
- Inclusion: Adults (18-65) with a primary DSM-5 diagnosis of Social Anxiety Disorder (SAD), confirmed by the Mini-International Neuropsychiatric Interview (MINI).
- Exclusion: Active psychosis, high suicide risk, substance dependence, and conditions contraindicating VR use (e.g., severe epilepsy).
- 3. Interventions:
- VRET Group: Seven 90-minute sessions of therapist-guided VR exposure. Participants use a head-mounted display (HMD) to engage with standardized virtual social environments (e.g., public speaking, small talk scenarios). The scenarios are calibrated for intensity based on a pre-defined hierarchy.
- IVET Group: Seven 90-minute sessions of therapist-guided in-vivo exposure. Exercises are conducted in real-world settings and are matched to the VR scenarios in terms of therapeutic goals and hierarchy (e.g., actual public speaking, initiating conversations with strangers).
- Waitlist Control: Receive no active intervention during the study period but are offered treatment after the 6-month follow-up.
- 4. Outcome Measures:
- Primary: Liebowitz Social Anxiety Scale (LSAS) total score.
- Secondary: Social Phobia Inventory (SPIN), Beck Depression Inventory-II (BDI-II), and World Health Organization Quality of Life scale (WHOQOL-BREF).
- Assessment Time Points: Baseline (T0), post-treatment (T1, ~3 months), 6-month follow-up (T2), 12-month follow-up (T3).
- 5. Assessment of Mechanisms: To investigate how VRET works, the following mediators are measured at each time point:
- Expectancy Violation: Participants rate their fear-based expectations before and after each exposure task.
- Within- and Between-Session Habituation: Subjective Units of Distress (SUDs) are recorded every 5 minutes during exposure sessions.
- Self-Efficacy: The Self-Efficacy for Social Situations Scale (SESS) is administered.
- 6. Data Analysis: Linear Mixed Models (LMM) will be used for the primary and secondary outcomes on an intention-to-treat basis. Mediation analysis will be conducted to test the proposed mechanisms.
The following diagram illustrates the workflow and key assessment points for this protocol.
Protocol 2: Pragmatic RCT in Clinical Group Settings (VR-CBT vs. Traditional CBT)
This protocol is adapted from the SoREAL trial [85] and is designed to test the effectiveness of VR-augmented CBT under real-world clinical conditions, specifically in group therapy settings.
- 1. Study Design: A pragmatic, randomized, assessor-blinded, parallel-group trial conducted within existing outpatient mental health services.
- 2. Participants:
- Sample Size: 302 participants (calculated to detect a minimal clinically important difference), recruited from waitlists.
- Inclusion: Adults with a primary ICD-11 diagnosis of SAD or Agoraphobia, referred for standard group therapy.
- 3. Interventions: Both groups receive 14 weekly, two-hour group CBT sessions.
- VR-CBT Arm: Seven sessions incorporate 45 minutes of individualized VR exposure using HMDs. Patients choose from a library of 360° videos of social (e.g., work presentation) and agoraphobic (e.g., crowded bus, supermarket) scenarios.
- CBT Arm (Treatment as Usual): Seven sessions incorporate 45 minutes of in-vivo exposure conducted as a group (e.g., role-playing, group presentations, using the clinic elevator).
- 4. Outcome Measures:
- Primary: Phobic anxiety reduction, measured by POMP-transformed scores of the Liebowitz Social Anxiety Scale (LSAS) for SAD and the Mobility Inventory for Agoraphobia (MIA).
- Secondary: Work and Social Functioning scale, Patient Health Questionnaire-9 (depression), and EQ-5D-5L (quality of life).
- Assessment Time Points: Baseline, post-treatment (14 weeks), and 1-year follow-up from baseline.
- 5. Data Analysis: Intention-to-treat analysis using linear models, with the primary comparison being the between-group difference on the POMP-transformed score at post-treatment.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials and tools required for the implementation of the proposed VRET research protocols.
Table 2: Key Research Reagent Solutions for VRET Clinical Trials
| Item Category | Specific Examples & Specifications | Primary Function in Research |
|---|---|---|
| VR Hardware | Standalone Head-Mounted Display (HMD), e.g., Meta Quest 3, PICO 4. | Provides the immersive visual and auditory experience for exposure; standalone units offer portability for multi-site trials. |
| VR Software/Environments | Customizable 360° video libraries or computer-generated environments for SAD (e.g., pub, meeting room) and agoraphobia (e.g., elevator, supermarket). | Presents standardized, controllable, and reproducible anxiety-provoking stimuli; allows for graded exposure. |
| Clinical Outcome Measures | Liebowitz Social Anxiety Scale (LSAS), Mobility Inventory for Agoraphobia (MIA), Hamilton Anxiety Scale (HAMA). | Validated tools for quantitatively assessing the primary outcome of anxiety symptom reduction. |
| Mechanism Assessment Tools | Visual Analog Scales (VAS) for Expectancy Violation, Subjective Units of Distress (SUDs) scales, Self-Efficacy for Social Situations Scale (SESS). | Measures potential mediators of treatment effect (e.g., cognitive change, habituation) to understand how VRET works. |
| Diagnostic & Blinding Tools | Mini-International Neuropsychiatric Interview (MINI), Credibility/Expectancy Questionnaire. | Ensures accurate participant diagnosis and assesses the success of blinding in controlled trials. |
The trajectory of VRET is promising, yet its full integration into clinical practice is contingent upon resolving critical uncertainties regarding its long-term benefits and its standing relative to conventional CBT. The protocols and tools outlined herein provide a concrete framework for generating the high-quality, mechanistic, and pragmatic evidence necessary to solidify VRET's role in the treatment of anxiety disorders. Future research that is methodologically rigorous, transparent, and focused on these identified gaps will be pivotal in advancing the field from promising innovation to established evidence-based practice. {#/content#}
Application Notes: Risk of Bias and GRADE in VRET Research
For systematic reviews evaluating Virtual Reality Exposure Therapy (VRET) for anxiety disorders, a structured approach to assessing methodological rigor is non-negotiable. This involves two core components: evaluating the risk of bias (RoB) in individual randomized controlled trials (RCTs) and judging the overall certainty of evidence for each outcome across studies.
The recommended tool for assessing risk of bias in randomized trials is the Cochrane Risk-of-Bias tool, version 2 (RoB 2) [86] [87]. This tool requires reviewers to make a judgement on the risk of bias for a specific trial result, as bias can vary for different outcomes within the same study [86]. The assessment is structured into five mandatory domains through which bias might be introduced [86]:
- Bias arising from the randomization process.
- Bias due to deviations from intended interventions.
- Bias due to missing outcome data.
- Bias in measurement of the outcome.
- Bias in selection of the reported result.
Judgements for each domain and for the overall study are categorized as 'Low' risk of bias, 'Some concerns', or 'High' risk of bias [86]. The overall risk of bias for a result is derived from the least favourable judgement across all domains [86].
The Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) framework is then used to rate the overall certainty of the body of evidence for a given outcome as High, Moderate, Low, or Very Low [70] [88]. In the context of VRET, evidence from RCTs starts as high certainty but can be rated down for limitations, including RoB, as well as for imprecision, inconsistency, indirectness, and publication bias [70].
Application to VRET Literature: Current meta-analyses in this field are often characterized by a high proportion of studies with a high risk of bias or some concerns, leading to a low or very low certainty of evidence according to GRADE [70]. Common issues identified include lacking information on randomization methods and blinding of outcome assessors, as well as small sample sizes that lead to imprecise effect estimates [70] [88]. For example, in a recent meta-analysis by Zeka et al. (2025), approximately half of the included studies had a high risk of bias, and the certainty of evidence was generally judged as low to very low [70]. This directly impacts the confidence in conclusions about VRET's efficacy, suggesting that while findings are encouraging, they should be interpreted with caution pending more robust evidence [70].
Experimental Protocols
Protocol for Assessing Risk of Bias Using RoB 2
Objective: To systematically assess the risk of bias for each individual study result included in a systematic review of VRET for anxiety disorders.
Materials:
- Cochrane RoB 2 tool (latest version) [86].
- Full-text copies of all included study publications.
- Any available trial protocols, registrations, or supplementary materials.
Workflow: The following diagram outlines the procedural steps for conducting a Risk of Bias assessment.
Step-by-Step Procedure:
- Select Results for Assessment: Focus the assessment on the specific results that will be incorporated into the review's meta-analyses and 'Summary of findings' table. Do not select results based on the likely risk-of-bias judgement [86].
- Specify the Effect of Interest: Pre-define in the review protocol whether the effect of interest is the effect of assignment to intervention (the intention-to-treat effect) or the effect of adhering to the intervention (the per-protocol effect). For most VRET reviews addressing efficacy, the effect of assignment is the principal effect of interest [86].
- Answer Signalling Questions: For each of the five domains, answer the series of 'signalling questions'. The response options are: 'Yes', 'Probably yes', 'Probably no', 'No', and 'No information'. Support all answers with direct quotes or unambiguous references to the study text [86].
- Propose Domain Judgements: Based on the pattern of answers to the signalling questions, use the RoB 2 algorithm to propose a judgement ('Low' / 'Some concerns' / 'High') for each domain [86].
- Propose Overall Judgement: The overall risk of bias for the result is the least favourable judgement across the five domains. Review authors can override this proposed judgement with justification [86].
- Document and Justify: For every signalling question answer and domain judgement, provide a written justification. This ensures transparency and reproducibility.
Domain-Specific Considerations for VRET Trials:
- D1: Randomization Process: Assess whether the allocation sequence was random and concealed until participants were enrolled. A common limitation in VRET trials is poor reporting of concealment methods [70].
- D2: Deviations from Intended Interventions: If the effect of assignment is of interest, assess whether participants and personnel were blinded, and if analyses were appropriate for this effect (e.g., intention-to-treat). Blinding is often challenging in VRET trials versus psychological placebo, but knowledge of the assigned intervention can influence behaviour and outcome assessment [86].
- D3: Missing Outcome Data: Assess the proportion of missing data, whether reasons are balanced across groups, and whether appropriate methods were used to handle missing data (e.g., multiple imputation) [86].
- D4: Measurement of the Outcome: Assess whether the method of measuring the outcome was appropriate and whether the outcome assessor was blinded. For patient-reported outcomes in VRET (e.g., anxiety scales), the risk is high if participants are unblinded [86] [70].
- D5: Selection of the Reported Result: Assess whether the reported result is likely to have been selected from multiple eligible outcome measurements or analyses. Compare the published paper against a pre-registered protocol or trial registration to detect selective reporting [86].
Protocol for Assessing Certainty of Evidence Using GRADE
Objective: To rate the overall certainty of the body of evidence for each critical and important outcome.
Materials:
- Risk-of-bias assessments for all included studies.
- Data and results from meta-analyses.
- GRADE handbook or guidance.
Workflow: The following diagram illustrates the process of rating the certainty of evidence, starting from a baseline quality and evaluating factors that can lower or raise it.
Step-by-Step Procedure:
- Start with a Baseline Certainty: For outcomes from RCTs, the baseline certainty is High [88].
- Evaluate Reasons to Rate Down the Certainty: Consider five factors:
- Risk of Bias: Rate down if a substantial proportion of the evidence comes from studies with a high risk of bias [70].
- Imprecision: Rate down if the confidence interval for the pooled effect is wide and includes both a meaningful benefit and no benefit (or harm), or if the sample size is small. This is a frequent issue in VRET meta-analyses, which often include few studies per disorder [70] [88].
- Inconsistency: Rate down if there is unexplained heterogeneity in results (e.g., wide variation in point estimates, low p-value in chi-square test for heterogeneity).
- Indirectness: Rate down if the evidence differs from the review's PICO question in terms of population, intervention, comparator, or outcome.
- Publication Bias: Rate down if there is suspicion that published studies are an unrepresentative sample of all completed studies (e.g., suggested by funnel plot asymmetry).
- Evaluate Reasons to Rate Up the Certainty: This is less common but can occur for evidence from observational studies if a large magnitude of effect is observed [88].
- Arrive at a Final Certainty Rating:
- High: Very confident that the true effect lies close to the estimate.
- Moderate: Moderately confident; the true effect is likely close, but may be substantially different.
- Low: Confidence in the effect estimate is limited; the true effect may be substantially different.
- Very Low: Very little confidence; the true effect is likely to be substantially different.
Data Presentation
Table 1: Common Risk of Bias Issues in Recent VRET Meta-Analyses
This table synthesizes limitations reported in recent systematic reviews of VRET for mental health disorders.
| Risk of Bias Domain (RoB 2) | Common Issue in VRET Trials | Impact on GRADE Certainty |
|---|---|---|
| Randomization Process | Lack of information on sequence generation and allocation concealment [70]. | Often leads to rating down for Risk of Bias. |
| Deviations from Interventions | Difficulty blinding participants to VRET versus non-VR therapy [70]. | May contribute to rating down for Risk of Bias, particularly for patient-reported outcomes. |
| Missing Outcome Data | Incomplete reporting of attrition and use of inappropriate methods (e.g., complete-case analysis) [70]. | Can lead to rating down for Risk of Bias. |
| Measurement of the Outcome | Lack of blinding of outcome assessors for clinician-rated scales [70]. | Often leads to rating down for Risk of Bias. |
| Selection of Reported Result | Lack of comparison with a pre-registered protocol to assess selective reporting [70]. | Can lead to rating down for Risk of Bias or Publication Bias. |
| -- (Across Domains) | Small Sample Sizes [70] [88] | A key factor leading to rating down for Imprecision. |
Table 2: Illustrative GRADE Evidence Profile: VRET vs. Passive Control for Specific Phobias
This table provides an example of how the certainty of evidence is evaluated for a specific outcome. The data is illustrative, based on findings from Zeka et al. (2025) and Liu et al. (2025) [70] [88].
| Outcome | Anticipated Absolute Effect (95% CI) | № of Participants (Studies) | Certainty of the Evidence (GRADE) | Comments |
|---|---|---|---|---|
| Phobia Symptom Reduction (post-treatment) | Hedge's g 1.07 higher (0.22 higher to 1.92 higher) [70] | ~500 (15 RCTs) [70] | @@Low¹,² | VRET likely reduces symptoms, but true effect may vary. |
| Social Anxiety Symptom Reduction (post-treatment) | Hedge's g 0.83 higher (0.49 higher to 1.17 higher) [70] | ~300 (7 RCTs) [70] | @@Moderate¹ | Further research may change confidence in estimate. |
GRADE Explanation:
- Risk of Bias: Rated down 1 level due to a high proportion of studies with some concerns or high risk of bias [70].
- Imprecision: Rated down 1 level for specific phobias due to wide confidence intervals that include both a large and a small effect [70].
The Scientist's Toolkit: Research Reagent Solutions
This table details key methodological tools and their applications for conducting rigorous systematic reviews in the VRET field.
| Tool / Resource Name | Function / Application | Key Considerations for VRET Research |
|---|---|---|
| Cochrane RoB 2 Tool [86] [87] | Assesses risk of bias in individual randomized trials. | Critical. Use the standard RoB 2 for parallel-group trials. Focus on blinding (Domain 2 & 4) and fidelity of the VR intervention. |
| GRADE Framework [70] [88] | Rates the overall certainty of a body of evidence for a specific outcome. | Critical. Consistently rate down for imprecision due to small study pools and for risk of bias. |
| ROBVIS Visualization Tool [89] | A web app for creating publication-quality "traffic light" plots of RoB 2 assessments. | Recommended. Enhances transparency and clarity when reporting RoB findings in publications and supplements. |
| PRISMA 2020 Statement | Provides a reporting guideline for systematic reviews and meta-analyses. | Mandatory. Ensures complete and transparent reporting of the review process. |
| Network Meta-Analysis (NMA) | Compares multiple interventions simultaneously, even without head-to-head trials [88]. | Emerging. Can rank VRET against other active therapies (e.g., CBT, ACT) and control conditions. |
Virtual Reality (VR) has emerged as a transformative technology for clinical research, moving beyond a novel intervention to become a robust engine for capturing objective, high-dimensional endpoint data. This is particularly salient within virtual reality exposure therapy (VRET) for anxiety disorders, where the technology enables standardized, ecologically valid assessment protocols that overcome the limitations of traditional self-report measures [90] [91]. By creating controlled, replicable virtual environments, researchers can elicit and measure pathological behaviors and physiological responses in a manner that is both clinically meaningful and scientifically rigorous. The capacity to present standardized anxiety-inducing scenarios—such as social situations for social anxiety disorder or physical sensations for panic disorder—while simultaneously capturing multi-modal data (behavioral, physiological, and subjective) provides an unprecedented opportunity for comprehensive biomarker development [90] [92]. This technological paradigm shift addresses critical methodological challenges in mental health research, including recall bias, lack of ecological validity, and inter-rater variability, ultimately enabling more sensitive detection of treatment effects and facilitating personalized therapeutic approaches [93] [90].
VR-Derived Endpoints: Categories and Metrices
The rich data capture capabilities of VR systems enable the derivation of novel endpoints across multiple domains. These metrics can be broadly categorized into behavioral, physiological, and composite endpoints, each offering distinct insights into patient functioning and treatment response.
Table 1: Categories of VR-Derived Endpoints for Anxiety Disorders Research
| Endpoint Category | Specific Metrics | Clinical/Research Utility | Example Anxiety Disorder Application |
|---|---|---|---|
| Behavioral | Avoidance duration, gaze tracking (dwell time on threats), path deviation, virtual interaction latency, task persistence [93] [90]. | Quantifies avoidance and safety behaviors objectively; measures attention bias. | Social Anxiety Disorder: Time to initiate conversation with a virtual avatar [91]. |
| Physiological | Heart Rate Variability (HRV), electrodermal activity, respiratory rate, electroencephalogram (EEG) [90] [92]. | Provides objective, quantifiable measures of autonomic arousal and stress response. | Panic Disorder: HRV metrics during a virtual relaxation scenario [90]. |
| Subjective (in-VR) | Virtual Reality Assessment of Panic Disorder (VRA-PD) subjective anxiety scores [90]. | Captures state anxiety in real-time within the evocative context, reducing recall bias. | Panic Disorder: Anxiety scores during a virtual exposure to physical sensations [90]. |
| Performance-Based | Error counts in cognitive-motor tasks, reaction time, accuracy on standardized neurocognitive batteries [93]. | Assesses the functional impact of anxiety on cognitive load and dual-tasking ability. | Generalized Anxiety Disorder: Performance on a working memory task while exposed to virtual worry triggers. |
| Composite | Machine learning models integrating behavioral, physiological, and subjective data streams [90]. | Provides a holistic, individualized prediction of treatment response or diagnostic status. | Panic Disorder: Classifying early treatment responders using a combination of HRV and anxiety scores [90]. |
Experimental Protocol: VR Assessment for Predicting Early Treatment Response in Panic Disorder
The following protocol, adapted from a 2025 study, details a methodology for using VR to predict early treatment response in Panic Disorder (PD), serving as a template for rigorous VR clinical trial design [90].
Background and Rationale
Early treatment response (ETR) is a critical prognostic factor in PD. This protocol uses a VR-based assessment tool (VRA-PD) to create an ecologically valid and safe environment for eliciting and measuring panic-relevant responses. The core rationale is that behavioral and physiological metrics captured during controlled VR exposure will provide more sensitive predictors of ETR than conventional clinical interviews and questionnaires alone [90].
Materials and Equipment
- VR Hardware: Standalone or PC-connected Head-Mounted Display (HMD) with integrated eye-tracking (e.g., Meta Quest Pro, HTC Vive Focus 3).
- Physiological Sensors: A wearable chest strap or finger sensor capable of capturing electrocardiogram (ECG) for Heart Rate Variability (HRV) analysis [90] [92].
- Software: The Virtual Reality Assessment of Panic Disorder (VRA-PD) software, which should include at least two modules: a neutral/relaxation scenario (e.g., a peaceful virtual beach) and an anxiety/panic induction scenario (e.g., a scenario designed to elicit sensations related to panic, such as mild breathlessness or elevated heart rate via audiovisual cues) [90].
- Data Integration Framework: A software framework like ManySense VR [92] or the OpenXR Data Recorder (OXDR) [94] to synchronize and record data from the HMD, physiological sensors, and in-VR subjective ratings.
Step-by-Step Procedure
- Participant Setup and Baseline (5 minutes): After obtaining informed consent, fit the participant with the physiological sensor and HMD. Ensure the equipment is comfortable and calibrated. Begin the VR neutral/relaxation scenario. Instruct the participant to simply relax and observe the environment.
- VR Exposure and Data Capture (15 minutes):
- Neutral Scenario (5 minutes): Record baseline physiological data (HRV) and obtain a baseline subjective anxiety rating (e.g., 0-100 scale) via an in-VR prompt.
- Anxiety-Inducing Scenario (10 minutes): Seamlessly transition the participant to the anxiety-inducing scenario. Continue recording physiological data. Present periodic in-VR prompts (e.g., every 2 minutes) for the participant to rate their current subjective anxiety.
- Post-Session Assessment (5 minutes): Upon exiting VR, administer standard clinical scales, including the Panic Disorder Severity Scale (PDSS) and the Anxiety Sensitivity Index (ASI) [90].
- Data Processing and Feature Extraction: Process the raw, synchronized data to extract key features for analysis:
- Physiological Features: Calculate time-domain (SDNN, RMSSD) and frequency-domain (LF, HF power) HRV metrics from the ECG data for both neutral and anxiety scenarios, and compute change scores [90].
- Behavioral Features: Extract total duration in the scenario, instances of looking away from the primary stimulus (via eye-tracking), and head movement variability.
- Subjective Features: Calculate the peak subjective anxiety score and the average anxiety score during the anxiety scenario.
- Outcome Prediction Modeling: Integrate the extracted VR-based features with conventional clinical data (e.g., baseline PDSS and ASI scores). Use a machine learning model (e.g., CatBoost classifier, as used in the foundational study) to classify participants as "early responders" or "delayed responders" based on a pre-defined clinical outcome (e.g., ≥40% reduction in PDSS score at 2-month follow-up) [90].
Key Validation Considerations
- Context-of-Use Declaration: Pre-register the specific VR hardware models, tracking mode, and firmware versions to be used across all trial sites to ensure consistency [93].
- Agreement Studies: Conduct studies to establish the agreement between VR-derived endpoints and traditional clinical assessments using methods like Bland-Altman plots [93].
- Control for Learning Effects: For repeated assessments, use multiple equivalent versions of VR scenarios or account for practice effects in the statistical analysis [93].
The Researcher's Toolkit for VR Data Capture
Implementing a robust VR data capture system requires a suite of technical tools and frameworks designed to handle the multi-modal, high-frequency data streams inherent in VR research.
Table 2: Essential Research Reagent Solutions for VR Clinical Trials
| Tool/Solution | Category | Primary Function | Implementation Note |
|---|---|---|---|
| ManySense VR [92] | Data Collection Framework | An extensible, Unity-based framework for unifying data collection from diverse sources (eye trackers, EEG, physiological sensors). | Ideal for building context-aware VR applications; supports easy addition/removal of sensors. |
| OpenXR Data Recorder [94] | Data Collection Toolkit | A Unity toolkit for capturing OpenXR-standardized data (head pose, controller input) at a fixed polling rate, independent of frame rate. | Ensures consistent data capture for machine learning; supports NDJSON and binary formats. |
| VRA-PD Software [90] | Assessment Application | A specialized VR application containing scenarios for assessing panic disorder (anxiety induction and relaxation). | Serves as a validated model for developing disorder-specific VR assessments. |
| CatBoost Classifier [90] | Analytical Model | A machine learning model effective for classifying treatment response using heterogeneous data (clinical, behavioral, physiological). | Handles categorical features well; provides feature importance metrics (e.g., SHAP values). |
Signaling Pathways and Workflows
The process of transforming a raw VR session into a predictive clinical insight involves a structured workflow for data acquisition, integration, and model interpretation. The following diagram illustrates this multi-stage pipeline.
VR Clinical Data Analysis Workflow
A critical component of the analytical workflow is understanding which features most strongly drive the predictive model's output. The following diagram conceptualizes the results of a SHAP (SHapley Additive exPlanations) analysis, which identifies the most important predictors from a combined VR and clinical dataset.
Key Predictors of VR-Based Treatment Response
The integration of VR for objective data capture represents a paradigm shift in clinical trials for anxiety disorders. The methodologies and frameworks outlined provide a roadmap for developing validated, regulatory-ready endpoints that leverage VR's unique capacity for standardized, multi-modal data acquisition. By adopting a rigorous, phased approach to validation and leveraging specialized toolkits for data handling, researchers can unlock deeper insights into treatment efficacy and patient heterogeneity, ultimately accelerating the development of more personalized and effective mental health interventions.
Conclusion
Virtual Reality Exposure Therapy represents a promising and empirically supported intervention for anxiety disorders, with particular strength in treating specific phobias and social anxiety. Its efficacy is demonstrated to be comparable to traditional in-vivo exposure, while offering distinct advantages in control, safety, and accessibility. For the field to mature, future efforts must prioritize overcoming key challenges: conducting large-scale, rigorous RCTs to solidify long-term efficacy and expand applications to diverse disorders; establishing standardized treatment protocols to enhance reproducibility and clinical translation; and deeply exploring the neural mechanisms of action to optimize therapeutic impact. For biomedical research, VRET presents a powerful tool for conducting exquisitely controlled clinical experiments, validating novel pharmacotherapeutic and neuromodulatory adjuvants, and capturing rich, objective behavioral data, ultimately accelerating the development of next-generation mental health treatments.
References
- 1. Understanding the Mechanisms Behind Virtual Reality ... [https://www.psychologicalscience.org/news/2025-feb-virtual-reality-exposure-therapy.html]
- 2. Mechanisms of Change in Exposure Therapy for Anxiety and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12373099/]
- 3. VIRTUS: virtual reality exposure training for adolescents with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12008921/]
- 4. The Underlying Working Mechanisms in Virtual-Reality ... [https://cris.maastrichtuniversity.nl/en/publications/opening-the-black-box-the-underlying-working-mechanisms-in-virtua/]
- 5. Barriers to adopting therapeutic virtual reality [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1549090/full]
- 6. Examining a Telemedicine-Based Virtual Reality Clinic in ... [https://www.researchprotocols.org/2025/1/e65770]
- 7. Examining the comparative effectiveness of virtual reality ... [https://www.sciencedirect.com/science/article/pii/S2589979125000046]
- 8. What is Presence in Virtual Reality (VR) | IxDF [https://www.interaction-design.org/literature/topics/presence?srsltid=AfmBOoqZ2Qkuw8hPz1chkJ3TS3fz9Zk11bLV1POWxqCzb99stNLBzCOP]
- 9. Virtual Reality (VR) Research - The Complete Pocket Guide [https://imotions.com/blog/learning/research-fundamentals/virtual-reality-vr-research-the-complete-pocket-guide/?srsltid=AfmBOooVaf_0JlMzWfrKnU7-vtxvw2GGWWHOqCoG7CZHEOqj3Hb0h_Hm]
- 10. VR Game Design Principles for Immersive and Enjoyable ... [https://www.fxmweb.com/insights/vr-game-design-principles-for-immersive-and-enjoyable-experiences.html]
- 11. Blended Mobile-Based Interventions With Integrated Virtual ... [https://humanfactors.jmir.org/2025/1/e60957]
- 12. Design guidelines - VR [https://developers.google.com/vr/develop/experimental/6dof-design-guidelines]
- 13. Virtual reality exposure therapy for social anxiety disorders: a meta-analysis and meta-regression of randomized controlled trials - PubMed [https://pubmed.ncbi.nlm.nih.gov/39161295/]
- 14. Frontiers | Effectiveness of virtual reality therapy in the treatment of anxiety disorders in adolescents and adults: a systematic review and meta-analysis of randomized controlled trials [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1553290/full]
- 15. Smartphone-based self-help virtual reality exposure ... [https://link.springer.com/article/10.1007/s10055-025-01195-0]
- 16. The use of virtual reality technology in the treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5421394/]
- 17. What is Virtual Reality Exposure Therapy? A Complete ... [https://psytechvr.com/virtual-reality-exposure-therapy-vret]
- 18. Clinical features and genetic mechanisms of anxiety, fear ... [https://www.nature.com/articles/s41380-025-03155-1]
- 19. Virtual reality (VR) treatments for anxiety disorders are ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10592498/]
- 20. Take a Look at Me Now: The Use of Virtual Reality in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12050102/]
- 21. Virtual reality exposure therapy for posttraumatic stress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6713125/]
- 22. The use of virtual reality in the treatment of mental ... [https://www.sciencedirect.com/science/article/pii/S2666560324000562]
- 23. Social Anxiety Disorder - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK555890/]
- 24. Anxiety disorders, PTSD and OCD: systematic review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11991790/]
- 25. Virtual Reality: Challenges and Perspectives in Mental Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593772/]
- 26. Clinical Virtual Reality: Emerging Opportunities for Psychiatry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6493092/]
- 27. A systematic review of randomized controlled trials on ... [https://www.sciencedirect.com/science/article/pii/S1876139925001653]
- 28. Virtual Reality Therapy: The Future of Trauma & Anxiety ... [https://hupcfl.com/virtual-reality-therapy-the-future-of-trauma-and-anxiety-healing/]
- 29. Moderating Role of State and Trait Positive Affect in Virtual ... [https://www.researchprotocols.org/2025/1/e80010]
- 30. Comparative Efficacy of Virtual Reality–Assisted Cognitive ... [https://www.researchprotocols.org/2025/1/e66112]
- 31. Virtual Reality Therapy Market Report | Global Forecast ... [https://dataintelo.com/report/global-virtual-reality-therapy-market]
- 32. Virtual Reality Exposure Therapy for Fear of Heights [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2021.671871/full]
- 33. How Does Virtual Reality Exposure Treatment Change the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12283208/]
- 34. Review article Self-guided virtual reality therapy for anxiety [https://www.sciencedirect.com/science/article/pii/S1386505625001194]
- 35. The VRNetzer platform enables interactive network ... [https://www.nature.com/articles/s41467-021-22570-w]
- 36. Tips for Effective Implementation of Virtual Reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8490820/]
- 37. Effectiveness of virtual reality therapy in the treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11904249/]
- 38. Stand-alone virtual reality exposure therapy as a treatment for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10552696/]
- 39. [PDF] Self-Guided Virtual Reality Therapy for Anxiety [https://www.semanticscholar.org/paper/Self-Guided-Virtual-Reality-Therapy-for-Anxiety%3A-A-Graham-Drinkwater/9f8c9d1a7b6fb5e881bc354edce58060e21a1c28]
- 40. [2501.17375] Self-Guided Virtual Reality Therapy for Anxiety [https://arxiv.org/abs/2501.17375]
- 41. Virtual Reality in the Treatment of Anxiety-Related Disorders [https://pubmed.ncbi.nlm.nih.gov/40679554/]
- 42. Augmenting Virtual Reality Exposure Therapy for Social and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10920400/]
- 43. Using Virtual Reality Exposure Therapy to Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6823515/]
- 44. PROTOCOL: Effects of virtual reality exposure therapy versus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9246294/]
- 45. STUDY PROTOCOL: EXPOSURE IN VIRTUAL REALITY FOR ... [https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-020-2453-4]
- 46. Virtual Reality exposure therapy in the treatment of public ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12244110/]
- 47. Clinical Practice Guidelines for Cognitive-Behavioral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7001348/]
- 48. Virtual reality exposure therapy for reducing social anxiety ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2023.1061323/full]
- 49. Blended Mobile-Based Interventions With Integrated Virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12062763/]
- 50. Understanding Cybersickness and Presence in Seated VR [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027998/]
- 51. Visual performance standards for virtual and augmented ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1575870/full]
- 52. Deep Learning-Based Visual Fatigue Detection Using Eye ... [https://arxiv.org/html/2510.12994v1]
- 53. Exploring the Barriers to and Facilitators of Using Virtual ... [https://www.jmir.org/2025/1/e65308]
- 54. An Adaptive Fatigue Detection Model for Virtual Reality ... [https://www.mdpi.com/2078-2489/16/2/148]
- 55. Virtual Reality and Relaxation for the Treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11856863/]
- 56. Virtual Reality for Anxiety Reduction Demonstrated by ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2018.01280/full]
- 57. Mental Health Professionals' Attitudes Towards Virtual ... [https://link.springer.com/article/10.1007/s41347-025-00499-x]
- 58. Barriers to adopting therapeutic virtual reality - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11958971/]
- 59. VR Therapy Careers: Virtual Reality Mental Health 2025 [https://careersinpsychology.org/why-virtual-reality-transform-mental-health-treatment/]
- 60. PsyTech VR Certification for CBT Clinicans [https://psytechvr.com/certification]
- 61. Virtual Reality Exposure (VRE) Therapy Training [https://virtuallybetter.com/vre-training/]
- 62. Psychologists are finding more ways to use virtual reality in ... [https://www.apa.org/monitor/2025/10/virtual-reality-therapy]
- 63. Developing interactive VR-based digital therapeutics for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12174457/]
- 64. PsyTech VR Therapy | Mental Health & Wellness App for Meta ... [https://psytechvr.com/]
- 65. Evidence-Based Results Using VR and Telehealth [https://yung-sidekick.com/blog/exposure-therapy-goes-digital-evidence-based-results-using-vr-and-telehealth]
- 66. Moving from Virtual Reality Exposure-Based Therapy to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3941080/]
- 67. [论文审查] Adapting to the User: A Systematic Review of ... [https://www.themoonlight.io/zh/review/adapting-to-the-user-a-systematic-review-of-personalized-interaction-in-vr]
- 68. Platform Technology for Extended Reality Biofeedback ... [https://www.researchprotocols.org/2025/1/e70620]
- 69. 人工智能在 [https://www.c2.care/zh/artificial-intelligence-in-mental-health-cn/]
- 70. Immersive virtual reality for the treatment of mental health ... [https://www.nationalelfservice.net/treatment/digital-health/immersive-virtual-reality-for-the-treatment-of-mental-health-disorders/]
- 71. A Meta-Analysis of the Efficacy of Virtual Reality and In ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9158252/]
- 72. Virtual Reality exposure therapy in the treatment of public ... [https://www.sciencedirect.com/science/article/pii/S277240852400139X]
- 73. Statistical significant change versus relevant or important ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1480399/]
- 74. A mixed methods pilot feasibility study of the unified ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1524243/full]
- 75. Achieving Integration in Mixed Methods Designs—Principles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4097839/]
- 76. Understanding the mental health of doctoral researchers [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-020-01443-1]
- 77. Bournemouth University Research Online [BURO] - Examining the... [https://eprints.bournemouth.ac.uk/40914/]
- 78. Virtual Reality in Anxiety - An Overview - Neurotorium [https://neurotorium.org/article/virtual-reality-in-anxiety-an-overview/]
- 79. Virtual reality exposure therapy for anxiety disorders: a meta-analysis [https://www.crd.york.ac.uk/CRDWeb/ShowRecord.asp?ID=12008103413]
- 80. Patient Perceptions of In Vivo Versus Virtual Reality ... [https://formative.jmir.org/2023/1/e47443/]
- 81. Virtual reality treatment versus exposure in vivo [https://pubmed.ncbi.nlm.nih.gov/12038644/]
- 82. Effectiveness of immersive VR therapy in reducing stress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12016277/]
- 83. Current State of Evidence for VRET in Psychotherapy [https://virtuallytheremedia.com/en/blog/literature-6/current-state-of-evidence-for-vret-in-psychotherapy-43]
- 84. Virtual reality-based versus standard cognitive behavioral ... [https://www.nature.com/articles/s41591-025-03880-8]
- 85. Group Cognitive Behavioral Therapy With Virtual Reality ... [https://mental.jmir.org/2025/1/e73815]
- 86. Chapter 8: Assessing risk of bias in a randomized trial [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-08]
- 87. Systematic Reviews: Reporting the quality/risk of bias [https://guides.himmelfarb.gwu.edu/systematic_review/reporting-quality-risk-of-bias]
- 88. Effects of different interventions on anxiety disorders in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12379421/]
- 89. Risk of Bias Tools - Systematic Review Guide [https://beckerguides.wustl.edu/SystematicReviews/riskofbias]
- 90. Simulated virtual reality experiences for predicting early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631630/]
- 91. Virtual reality-based exposure with 360° video as part of ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1588181/full]
- 92. Data Collection Framework for Context-Aware Virtual Reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9228658/]
- 93. Virtual Reality Clinical Trials: Step Inside the Future of ... [https://ccrps.org/clinical-research-blog/virtual-reality-clinical-trials-step-inside-the-future-of-medicine-2025]
- 94. A Toolkit for Virtual Reality Data Collection [https://arxiv.org/html/2412.17490v1]