Virtual Reality in Behavioral Neuroscience: Advancing Research, Therapy, and Drug Discovery
This article explores the transformative integration of Virtual Reality (VR) in behavioral neuroscience, addressing a core audience of researchers, scientists, and drug development professionals.
Virtual Reality in Behavioral Neuroscience: Advancing Research, Therapy, and Drug Discovery
Abstract
This article explores the transformative integration of Virtual Reality (VR) in behavioral neuroscience, addressing a core audience of researchers, scientists, and drug development professionals. It covers the foundational principles establishing VR as a tool for studying neuroplasticity and context-dependent behaviors. The scope extends to methodological innovations across human and preclinical research, including novel protocols for psychosis, ADHD, and motor rehabilitation. The review critically examines troubleshooting for technical and ethical challenges in implementation and provides a comparative analysis of VR's efficacy against conventional therapies. Finally, it validates VR's role through empirical evidence and discusses its emerging function in accelerating therapeutic discovery via platforms like eBrain for in silico drug testing.
The Neuroscience of Presence: How VR Creates Controlled, Ecologically Valid Environments for Research
Leveraging Immersion and Presence to Elicit Naturalistic Brain and Behavioral Responses
Virtual reality (VR) has emerged as a transformative tool in behavioral neuroscience, creating a critical middle ground between rigorous experimental control and essential ecological validity [1]. Unlike traditional laboratory paradigms that often rely on repetitive, passive sensory stimulation, VR establishes a closed-loop system where a participant's actions directly shape their sensory experience [1]. This interaction fosters immersion, an objective property of the technology, and presence, the subjective psychological sense of "being there" in the virtual environment [2]. The core premise of this application note is that by strategically designing VR to maximize presence, researchers can elicit more naturalistic brain and behavioral responses, thereby enhancing the translational value of preclinical and clinical research, including drug development.
Theoretical Foundations and Key Factors
The efficacy of VR in eliciting naturalistic responses hinges on the relationship between immersion and presence. Immersion is determined by the technology's ability to provide rich, multisensory stimuli and seamless interactivity, while presence is the user's psychological response to that immersion [2]. Key factors influencing this relationship include:
- Vibrancy and Fidelity: The breadth (number of senses engaged) and depth (quality and realism) of sensory information. Higher fidelity, which includes detailed 3D objects and realistic object behavior, strengthens the immersive illusion [2].
- Interactivity and User Control: The system's responsiveness (speed), the range of possible interactions (range), and the naturalness of the mapping between user actions and environmental changes (e.g., head tracking) are crucial for a sense of agency and presence [2].
- Embodied Simulation: Neuroscience suggests that VR is effective because it shares the brain's fundamental mechanism for regulating the body in the world: embodied simulation. VR maintains a model of the body and space, predicting the sensory consequences of movement, much like the brain does, allowing for targeted alteration of bodily experience and cognitive change [3].
Quantitative Data on Presence and Cybersickness
The following tables summarize empirical data on how different VR environmental factors influence key user experiences, including presence and cybersickness, which are critical for designing valid experiments.
Table 1: Impact of Static vs. Dynamic VR Environments on User Experience (n=30) [4]
| Metric | Static Environment | Dynamic Environment | Significance & Notes |
|---|---|---|---|
| Stress Level | No significant change from baseline (p=0.464) | Significant decrease (p=0.002) | Dynamic environments can induce relaxation. |
| Experienced Relaxation | No significant change (p=0.455) | Significant increase (p<0.001) | Aligns with stress reduction findings. |
| Cybersickness Symptoms | Minor disturbances only | Progressive, significant increase | Dynamic stimuli increase sensory conflict and cognitive load. |
Table 2: WCAG Color Contrast Ratios for Accessible Visual Design [5] [6]
| Element Type | Minimum Ratio (AA Rating) | Enhanced Ratio (AAA Rating) |
|---|---|---|
| Standard Body Text | 4.5:1 | 7:1 |
| Large-Scale Text (≥18pt or 14pt bold) | 3:1 | 4.5:1 |
| UI Components & Graphics (icons, graphs) | 3:1 | Not defined |
Detailed Experimental Protocols
Protocol 1: Comparing Spatial Presence and Emotional Response in Static vs. Dynamic Environments
This protocol is adapted from a study investigating how different VR environments influence spatial presence and emotional states [4].
1. Objective: To assess and compare the sense of spatial presence, emotional response, and cybersickness symptoms induced by static and dynamic virtual reality environments.
2. Materials and Equipment:
- VR Headset: Oculus Meta Quest 2 or equivalent, capable of displaying 360° content.
- Software: A platform for displaying 360° videos (e.g., YouTube VR).
- Content: Two 20-minute videos: (A) a static environment (e.g., a tranquil beach panorama); (B) a dynamic environment (e.g., a roller coaster ride).
- Questionnaires:
- Spatial Presence Experience Scale (SPES): To quantify the feeling of presence.
- I-PANAS-SF (International Positive and Negative Affect Schedule): To evaluate emotional states.
- Virtual Reality Sickness Questionnaire (VRSQ): To measure cybersickness symptoms.
- Swivel Chair: To allow participants to rotate and explore the 360° environment freely.
3. Procedure:
- Participant Preparation: Recruit healthy adult participants. Obtain informed consent. Record baseline physiological or self-reported measures of stress and relaxation.
- Baseline Assessment: Administer the I-PANAS-SF and VRSQ to establish pre-exposure states.
- VR Exposure:
- Participants experience both the static and dynamic environments in a counterbalanced order to control for sequence effects.
- Each session lasts 20 minutes, with a minimum 20-minute break between sessions to dissipate any potential cybersickness.
- Participants are instructed to sit on the swivel chair and explore the environment naturally.
- Post-Exposure Assessment: Immediately after each VR session, re-administer the SPES, I-PANAS-SF, and VRSQ.
- Data Analysis:
- Use paired t-tests or non-parametric equivalents to compare pre- and post-exposure scores for each environment.
- Compare SPES and VRSQ scores between the static and dynamic conditions using ANOVA or similar statistical models.
Protocol 2: Assessing Memory Confusion Between Virtual and Real Worlds
This protocol is based on a study demonstrating that VR experiences can blur the line with reality, affecting memory and behavior [7].
1. Objective: To determine the extent to which elements and events from a virtual environment are later confused with or transferred to reality.
2. Materials and Equipment:
- VR System: A headset and software capable of creating a highly interactive virtual room.
- Virtual Content: A detailed virtual model of a physical room, including a virtual experimenter avatar and objects like a chair and a tablet.
- Real-World Room: A physical room that corresponds to the virtual model.
3. Procedure:
- Day 1 - VR Session:
- Participants enter the VR environment and interact with a virtual experimenter.
- The avatar instructs participants to sit on a virtual chair. The presence or absence of a corresponding real chair is noted.
- The avatar places a virtual tablet into a virtual drawer. Participants observe this action.
- Day 7 - Real-World Follow-up:
- Participants are brought into the corresponding real-world room.
- Researchers observe if participants spontaneously attempt to sit where the virtual chair was or check for the real chair's presence.
- Participants are asked to find a tablet. Researchers record if they look in the drawer where the virtual tablet was placed.
- Data Analysis:
- Calculate the percentage of participants who (a) sat without checking for the real chair, and (b) used the VR memory to locate the tablet in the real world.
- Use Bayesian analysis to provide robust evidence for the effect size of the confusion.
Visualization of Workflows and Relationships
VR Immersion-Presence Pathway
Experimental Workflow for VR Studies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Immersive VR Neuroscience Research
| Item | Function & Rationale |
|---|---|
| Head-Mounted Display (HMD) e.g., Meta Quest 2 [4] | Provides the visual and auditory immersive experience. Must have high resolution, refresh rate, and precise head-tracking to maximize immersion and minimize latency-induced cybersickness. |
| VR-Compatible Swivel Chair | Allows participants to physically rotate and explore 360° environments, enhancing realism and spatial presence compared to a fixed seat [4]. |
| Spatial Presence Experience Scale (SPES) | A validated self-report questionnaire to quantitatively measure the subjective feeling of "being there" in the virtual environment, a key dependent variable [4]. |
| Virtual Reality Sickness Questionnaire (VRSQ) | A critical tool for monitoring adverse effects like nausea and dizziness, which can confound behavioral and neural data and act as a covariate in analysis [4]. |
| Biometric Acquisition System (EEG, fNIRS, GSR) | Enables the collection of objective physiological and neural correlates of presence, emotional arousal, and cognitive load, complementing self-report data [1]. |
| Color Contrast Analyzer (e.g., WebAIM's) | Ensures that any text or graphical elements in the VR environment meet WCAG guidelines, guaranteeing legibility for all participants and avoiding confounding based on visual ability [5] [6]. |
| Dynamic vs. Static VR Content | Dynamic content (e.g., roller coasters) is potent for inducing strong emotional and physiological responses, while static content (e.g., beaches) is useful for control conditions or relaxation studies [4]. |
VR as a Tool for Precise Manipulation of Environmental Context and Sensory Stimuli
Virtual Reality (VR) has emerged as a transformative tool in behavioral neuroscience, enabling researchers to exert unprecedented control over environmental context and sensory stimuli. By generating immersive, computer-generated environments, VR bridges the critical gap between highly controlled laboratory settings and the ecological validity of real-world experiences [8]. This capability allows for the precise presentation and systematic manipulation of complex, dynamic stimuli within realistic contexts, facilitating the rigorous investigation of brain-behavior relationships. The technology is particularly potent for studying processes like spatial navigation, learning, and emotional responses, as it can evoke neural and behavioral responses that parallel those observed in the real world [9] [10]. The following sections provide detailed application notes and experimental protocols for leveraging VR in neuroscience research and drug development.
Quantitative Data on VR Efficacy and Manipulation
Data from recent studies demonstrates the quantitative impact of VR manipulations on behavioral and physiological outcomes. The table below summarizes key findings from research on sensory manipulation and attentional modulation.
Table 1: Quantitative Effects of VR Environmental Manipulations on Behavioral and Physiological Outcomes
| Study Focus | Experimental Manipulation | Key Behavioral/Psychophysiological Findings | Implications for Neuroscience Research |
|---|---|---|---|
| Pain Perception in Chronic Low Back Pain [11] | Visual-proprioceptive feedback manipulated during lumbar extension:- E- (Understated): VR showed 10% less movement.- E+ (Overstated): VR showed 10% more movement. | - E- condition increased pain-free Range of Motion (ROM) by 20% vs. control (p=0.002) and by 22% vs. E+ (p<0.001).- Patients with higher kinesiophobia and disability showed greater improvement in E-. | VR can directly modulate sensorimotor processing and pain thresholds, useful for testing analgesics and neuropsychiatric drugs. |
| Sustained Attention with Visual Distractors [12] | Performance on a virtual classroom task compared under conditions with and without visual distractors. | - Distractors significantly increased commission errors, omission errors, and multipress responses.- P300 latency significantly prolonged at CPz, Pz, and Oz electrodes.- Sample and fuzzy entropy increased in frontal, central, and parietal regions. | Provides a validated paradigm and EEG biomarkers for probing attention and cognitive control, relevant for ADHD and schizophrenia research. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful VR experimentation requires a suite of hardware and software "reagents." The following table details the core components of a VR research system.
Table 2: Key Research Reagent Solutions for VR Neuroscience
| Item Category | Specific Examples / Common Models | Critical Function in VR Research |
|---|---|---|
| Head-Mounted Display (HMD) | HTC Vive Pro, Oculus Rift S [11] [13] | Provides the immersive visual experience; key variations include display resolution, field of view, and tracking capabilities. |
| Tracking System | Base stations (e.g., HTC Lighthouse), integrated inside-out tracking [13] | Precisely monitors the user's head and limb position in 3D space, enabling naturalistic movement and interaction. |
| Physiological Data Acquisition | EEG systems, Electrocardiogram (ECG), Electrodermal Activity (EDA) sensors [12] [14] | Provides objective, continuous physiological measures of cognitive load, arousal, and emotional state (e.g., P300, heart rate variability). |
| VR Development Platform | Unity, Unreal Engine [8] | Software environment used to design, build, and program the virtual environments and experimental logic. |
| Interaction Controllers | HTC Vive controllers, Oculus Touch [13] | Allows users to interact with and manipulate virtual objects, enriching the sense of presence and enabling complex behavioral tasks. |
Experimental Protocols
Protocol 1: VR with Neurofeedback for Auditory Verbal Hallucinations
This protocol, adapted from a current clinical trial, outlines a method for studying and treating symptoms of psychosis [9].
- Objective: To investigate the feasibility and initial efficacy of a hybrid treatment (Hybrid) integrating VR, neurofeedback, and cognitive behavioral therapy for psychosis (CBTp) for modulating auditory verbal hallucinations (AVHs).
- Materials:
- VR System: A head-mounted display capable of rendering immersive environments.
- Neurofeedback System: Electroencephalography (EEG) system for real-time measurement of high-β band power.
- Software: Custom VR software that includes an exposure hierarchy and a visual interface for neurofeedback (e.g., a bar graph representing β-power).
- Procedure:
- Participant Screening: Recruit participants with a diagnosis of a psychotic disorder and experiencing AVHs. Obtain informed consent.
- Baseline Assessment: Conduct clinical interviews and baseline symptom ratings (e.g., using the Positive and Negative Syndrome Scale).
- VR Environment Creation (Symptom Capture): Collaboratively design a personalized VR environment with the participant that incorporates triggers for their AVHs (e.g., a busy street, a specific room).
- Exposure and Neurofeedback Sessions:
- Participants receive 12 weekly, face-to-face sessions.
- In each session, the participant is immersed in the personalized VR environment, which is calibrated to a specific level on a pre-defined exposure hierarchy.
- Concurrently, EEG is recorded. Participants are instructed to use mental strategies to downregulate the high-β power activity associated with their symptoms, guided by the real-time visual neurofeedback display.
- The clinician provides CBTp throughout the session to support cognitive restructuring and coping strategy development.
- Progression: As participants achieve mastery at one level of the exposure hierarchy (e.g., successful self-regulation of neural target), they progress to a more challenging level in subsequent sessions.
- Post-Intervention Assessment: Repeat clinical ratings and user experience surveys (assessing acceptability, helpfulness, engagement, and safety on a 5-point Likert scale) at the end of the 12 sessions.
- Analysis:
- Primary Outcomes: Feasibility and acceptability, defined by consent rates, session completion rates, and user experience ratings (a pre-set threshold for success is >70% of participants rating 3 or above on the 5-point scale).
- Secondary Outcomes: Change in clinical symptom scores, ability to self-regulate the target EEG band, and progression through the VR exposure hierarchy.
Protocol 2: Manipulating Visual-Proprioceptive Feedback to Modulate Pain
This protocol details a method for investigating the influence of top-down visual processes on pain perception, a key area for analgesic drug development [11].
- Objective: To determine whether manipulating visual-proprioceptive feedback in VR can alter the threshold of movement-evoked pain in individuals with chronic low back pain (LBP).
- Materials:
- VR System: HTC Vive Pro headset with trackers placed on the participant's waist and feet.
- Motion Capture: Electro-goniometer to measure the precise lumbar range of motion (ROM).
- Software: A custom VR application (e.g., a virtual gymnasium) where an avatar's movement and a visual bar's height are linked to the participant's lumbar extension.
- Procedure:
- Participant Recruitment: Recruit adults with non-specific chronic LBP. Exclude those with specific spinal pathologies.
- Baseline Questionnaires: Administer scales for pain intensity (NRS), kinesiophobia, disability, and catastrophising.
- Calibration: Calibrate the VR system so the participant's actual lumbar extension is accurately mirrored by their avatar and the virtual bar.
- Experimental Task:
- Participants perform lumbar spine extension until the onset of pain under three conditions in a randomized order:
- Control (E): Lumbar extension without VR.
- Understated Feedback (E-): VR visual feedback is manipulated to show 10% less movement than the actual ROM (GainExt = 0.9).
- Overstated Feedback (E+): VR visual feedback is manipulated to show 10% more movement than the actual ROM (GainExt = 1.1).
- For each condition, the task is repeated 3 times, and the pain-onset ROM is recorded by the electro-goniometer.
- Participants perform lumbar spine extension until the onset of pain under three conditions in a randomized order:
- Data Collection: Record the ROM at pain onset for each repetition in each condition.
- Analysis:
- Use Friedman tests to assess within-group differences in ROM across the three conditions (E, E-, E+).
- Conduct post-hoc analyses to compare specific conditions.
- Use regression analyses to determine if baseline levels of kinesiophobia, disability, or catastrophising moderate the effect of the visual manipulation.
Best Practices and Methodological Framework
The integration of VR into rigorous neuroscience and drug development requires adherence to a structured methodological framework. The VR Clinical Outcomes Research Experts (VR-CORE) committee has proposed a phased model to guide this process [15]:
- VR1 Studies (Content Development): This initial phase focuses on treatment development using human-centered design principles. It involves:
- Inspiration through Empathizing: Conducting observations and interviews with patient and provider end-users to understand their needs, struggles, and expectations.
- Ideation through Team Collaboration: Sharing insights within a multidisciplinary team to generate ideas through storyboarding and mind mapping.
- VR2 Studies (Early Testing): These trials assess feasibility, acceptability, tolerability, and initial clinical efficacy. They are typically smaller in scale and may use open-label designs.
- VR3 Studies (Efficacy Trials): These are randomized, controlled trials (RCTs) that compare the VR intervention against an appropriate control condition to evaluate its efficacy on clinically important outcomes.
When combining VR with other physiological measures like EEG, several technical considerations are paramount [12] [8]. The VR system and the physiological recording system must be synchronized to ensure data can be accurately aligned. Furthermore, developers must account for potential electromagnetic interference between the VR hardware and sensitive bio-sensors, which may require specialized shielding or filtering during data processing.
Virtual reality (VR) has emerged as a powerful tool in behavioral neuroscience for inducing functional neuroplasticity within sensory-motor pathways. This application note synthesizes current evidence demonstrating that VR-based interventions promote cortical reorganization through mechanisms including multisensory integration, error-based learning, and dopaminergic reward pathways. We provide standardized protocols and analytical frameworks for researchers investigating VR-induced neuroplasticity, with particular relevance for developing novel therapeutic interventions in neurological and psychiatric disorders. Quantitative data from recent studies confirm that VR training significantly modulates brain activity patterns, enhances synaptic plasticity markers, and improves functional outcomes across patient populations.
Virtual reality (VR) technology has transitioned from a speculative tool to a validated platform for investigating and inducing neuroplasticity in behavioral neuroscience research. Neuroplasticity—the brain's remarkable capacity to reorganize its structure, function, and connections in response to experience—represents a fundamental mechanism through which VR interventions produce therapeutic effects [16]. The integration of VR in neuroscience facilitates exploration of complex neural processes in controlled, immersive environments that simulate real-world scenarios while allowing precise manipulation of sensory inputs and measurement of corresponding neurological responses [16].
VR environments create a dynamic interface between sensory inputs, motor responses, and cognitive engagements, triggering a cascade of neuroplastic changes that alter synaptic connections, neural circuitry, and functional brain networks [16]. These mechanisms are particularly relevant for drug development professionals seeking non-pharmacological adjuvants or evaluating neuroplasticity-enhancing compounds. The translational potential of VR-induced neuroplasticity spans multiple neurological conditions including stroke, traumatic brain injury, multiple sclerosis, and neuropsychiatric disorders where synaptic reorganization is compromised [16] [17].
Theoretical Framework: Mechanisms of VR-Induced Neuroplasticity
Neurobiological Foundations
VR-induced neuroplasticity operates through several interconnected mechanisms that promote structural and functional reorganization of neural circuits:
Multisensory Integration: VR concurrently engages visual, auditory, and proprioceptive systems, creating rich sensory experiences that encourage synaptic reorganization through cross-modal plasticity [17]. This multi-sensory stimulation is particularly effective for facilitating cortical remapping in damaged neural pathways.
Error-Based Learning with Real-Time Feedback: Advanced VR platforms capture real-time kinematic data, enabling immediate feedback and task adjustment that reinforces correct movements while discouraging maladaptive patterns [17]. This closed-loop system mirrors principles of motor learning by strengthening residual pathways through error correction mechanisms.
Reward Mechanisms and Cognitive Engagement: Gamification and immersive scenarios inherent to VR environments stimulate dopaminergic pathways in the ventral striatum, which are crucial for motivation, learning consolidation, and long-term potentiation [17]. The interactive, goal-oriented nature of VR enhances cognitive functions including attention, memory, and executive control while promoting adherence to therapeutic protocols.
Molecular Correlates of VR-Induced Plasticity
At the molecular level, VR experiences trigger cascades that promote synaptic strengthening and neural reorganization:
Neurotrophic Factor Modulation: VR stimulation increases expression of brain-derived neurotrophic factor (BDNF), which supports neuronal survival, dendrite arborization, and spine formation [16]. Enhanced BDNF signaling facilitates long-term potentiation (LTP), the primary cellular mechanism underlying learning and memory.
Synaptic Protein Synthesis: VR environments activate mTORC1 signaling pathways, leading to increased synthesis of synaptic proteins such as GluR1, PSD95, and synapsin 1, thereby enhancing synaptic density and function in cortical regions [16] [18].
Glutamatergic System Engagement: Through NMDA receptor activation, VR experiences promote calcium influx that triggers intracellular signaling cascades essential for synaptic modification, mirroring mechanisms targeted by rapid-acting antidepressant compounds [18].
Quantitative Evidence: Electrophysiological and Behavioral Outcomes
EEG Measures of Cortical Reorganization
Recent studies utilizing electroencephalography (EEG) have provided quantitative evidence of VR-induced neuroplasticity at the network level:
Table 1: EEG Spectral Power Changes Following VR Intervention in Chronic Stroke Patients [19]
| EEG Band | Brain Region | Change Post-VR | Functional Correlation |
|---|---|---|---|
| Theta | Diffuse | No significant change | N/A |
| Alpha | Occipital areas | Significant increase | Visual processing enhancement |
| Beta | Frontal areas | Significant increase | Sensorimotor integration, cognitive control |
| Alpha/Beta Ratio | Primary motor circuit | Significant decrease | Enhanced motor readiness |
This study demonstrated that VR-based cognitive training resulted in significant EEG-related neural improvements in the primary motor circuit, with specific changes in power spectral density and time-frequency domains observed in patients with moderate-to-severe ischemic stroke in the chronic phase (at least 6 months post-event) [19]. The findings suggest that VR interventions can modulate neural oscillations even during late-stage recovery when conventional rehabilitation approaches show limited efficacy.
Clinical and Functional Outcomes
VR interventions produce measurable improvements in functional outcomes across neurological conditions:
Table 2: Functional Outcome Measures Following VR Interventions Across Patient Populations
| Condition | Intervention Type | Outcome Measures | Results | Reference |
|---|---|---|---|---|
| Multiple Sclerosis | VR vs. Sensory-Motor training | T25FW, TUG, MSQOL-54 | Significant improvements in both groups (T25FW: P=0.002 SN; P=0.001 VR) | [20] |
| Chronic Stroke | VR-based cognitive training | EEG band power, clinical scales | Significant increase in alpha and beta power; functional improvement | [19] |
| Amblyopia | Dichoptic VR training | Visual acuity, contrast sensitivity | 1-4 lines visual acuity improvement | [21] |
The comparative study in MS patients revealed that both VR and sensory-motor interventions significantly improved Timed 25-Foot Walk (T25FW) and Timed Up and Go (TUG) performance, with the VR group showing particularly strong improvements in quality of life measures [20]. These functional gains correlate with the neuroplastic changes observed in electrophysiological studies, providing a comprehensive picture of VR-induced recovery mechanisms.
Experimental Protocols
Protocol 1: VR Cognitive Training for Stroke Rehabilitation
Objective: To evaluate VR-induced neuroplasticity in chronic stroke patients using EEG measures and functional outcomes.
Population: Adults with moderate-to-severe ischemic stroke in chronic phase (>6 months post-stroke); experimental group (n=15, mean age=58.13±8.33) and control group (n=15, mean age=57.33±11.06) [19].
VR System: VRRS Evo-4 machine with customizable cognitive exercises targeting attention, memory, executive functions, and visuo-spatial processing [19].
Intervention Parameters:
- Session Duration: 45-60 minutes
- Frequency: 3 sessions/week
- Total Program: 8 weeks (24 sessions)
- Progression: Gradual increase in task difficulty based on performance
Control Condition: Conventional neurorehabilitation matched for duration and frequency but without VR components.
Outcome Measures:
- Primary Electrophysiological: Resting-state EEG with power spectral analysis of theta, alpha, and beta rhythms
- Secondary Clinical: Oxford Cognitive Screen, Barthel Index, Modified Rankin Scale [19]
Data Analysis:
- Pre-process EEG signals using standardized filters (0.5-45 Hz bandpass, notch filter at 50/60 Hz)
- Compute power spectral density via Fast Fourier Transform
- Compare pre-post changes in absolute and relative band power
- Statistical analysis using repeated measures ANOVA with group (VR vs control) as between-subject factor
Protocol 2: Sensory-Motor Integration Training for Multiple Sclerosis
Objective: To compare effects of VR versus sensory-motor training on gait, balance, and quality of life in MS patients.
Population: MS patients with Expanded Disability Status Scale (EDSS) scores of 2-6 receiving Rituximab therapy; sample size of 30 participants randomized to VR (n=10), sensory-motor (n=10), or control (n=10) groups [20].
VR System: Commercially available VR system with balance and gait activities requiring weight shifting, obstacle avoidance, and dual-task performance.
Intervention Parameters:
- Session Duration: 45 minutes
- Frequency: 3 sessions/week
- Total Program: 8 weeks (24 sessions)
- Intensity: Progressive increase based on participant performance
Control Condition: Routine care without structured balance training.
Outcome Measures:
- Primary: Timed 25-Foot Walk (T25FW), Timed Up and Go (TUG)
- Secondary: Multiple Sclerosis Quality of Life 54 Instrument (MSQOL-54), Pittsburgh Sleep Quality Index (PSQI) [20]
Assessment Timeline: Baseline and post-intervention (8 weeks)
Data Analysis:
- Within-group changes: Paired t-tests or Wilcoxon signed-rank tests
- Between-group differences: ANCOVA adjusting for baseline scores
- Effect sizes calculation using Cohen's d
Signaling Pathways and Experimental Workflows
Molecular Pathways of VR-Induced Neuroplasticity
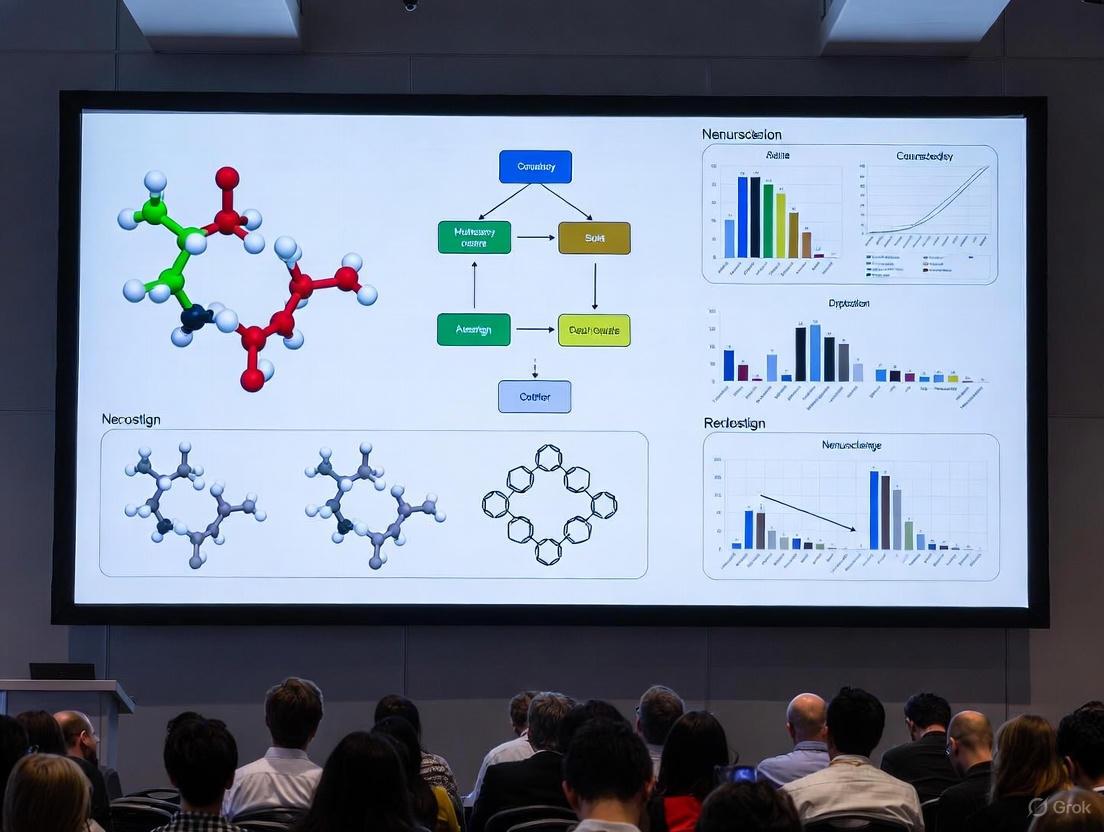
Diagram 1: Molecular pathways of VR-induced neuroplasticity. This pathway illustrates the sequence from multisensory VR stimulation through molecular cascades to functional improvements, highlighting key targets for therapeutic intervention.
Experimental Workflow for VR Neuroplasticity Research
Diagram 2: Experimental workflow for VR neuroplasticity research. This workflow outlines a standardized approach for investigating VR-induced neuroplasticity, from participant recruitment through data analysis.
Research Reagent Solutions
Table 3: Essential Research Tools for VR Neuroplasticity Investigations
| Tool Category | Specific Examples | Research Application | Key Parameters |
|---|---|---|---|
| VR Platforms | VRRS Evo-4, HMDs (Oculus Rift, HTC Vive), Jintronix | Create controlled, immersive environments for sensory-motor and cognitive training | Level of immersion, tracking precision, feedback capabilities [19] [17] |
| Neuroimaging Systems | EEG systems, fNIRS, fMRI-compatible VR | Quantify neurophysiological changes, functional connectivity, and cortical reorganization | Temporal resolution, spatial resolution, compatibility with movement [19] |
| Behavioral Assessment | Oxford Cognitive Screen, Barthel Index, TUG, T25FW | Evaluate functional outcomes correlated with neuroplastic changes | Sensitivity to change, reliability, validity for population [19] [20] |
| Molecular Assays | BDNF ELISA, synaptic protein Western blots, mTOR pathway markers | Validate molecular mechanisms of VR-induced plasticity in animal models | Specificity, sensitivity, throughput capacity [16] [18] |
| Data Analytics | EEG spectral analysis, kinematic tracking software, statistical packages | Process multimodal data streams and identify significant patterns | Algorithm accuracy, processing speed, visualization capabilities [19] |
VR technology represents a powerful, non-invasive approach to inducing targeted neuroplasticity across sensory-motor pathways and cognitive networks. The protocols and frameworks provided herein offer standardized methodologies for researchers investigating VR-driven neuroplastic changes, with particular utility for preclinical studies of neuroplasticity-enhancing compounds and mechanisms. Future research directions should focus on optimizing VR parameters for specific neural circuits, identifying biomarkers predictive of response, and developing closed-loop systems that adapt in real-time to neural activity for precision neurorehabilitation.
Virtual reality (VR) has emerged as a transformative tool in behavioral neuroscience, enabling researchers to study context-dependent learning and memory with unprecedented experimental control. Context-dependent memory is defined as the phenomenon where memory recall is stronger when the retrieval environment matches the original environment in which the memory was formed [22]. This encompasses not only external environmental cues but also internal states and temporal elements bound to the learning process.
The theoretical foundation for this work rests on the encoding specificity principle, which states that successful remembering depends on the overlap between encoding and retrieval situations [22]. VR technology allows investigators to create highly distinctive, controlled learning contexts that can be systematically manipulated to examine how contextual cues become bound to memories and facilitate or impair their subsequent recall.
This technological approach has gained significant traction, with bibliometric analyses revealing exponential growth in VR and mental health publications since 2020, featuring robust international collaboration networks and diverse research clusters spanning virtual reality, exposure therapy, mild cognitive impairment, and serious games [23]. The integration of VR into neuroscience research represents a paradigm shift from traditional maze-based assays to automated, precisely controlled systems that offer enhanced compatibility with large-scale neural recording techniques [24].
Comparative VR Platforms in Animal and Human Research
Rodent VR Platforms for Context-Dependent Research
Recent advances in rodent VR systems have addressed previous limitations in flexibility and performance. The platform developed by Xu Chun's Lab exemplifies this progress, featuring a high-performance system assembled from modular hardware and custom-written software with upgradability [25] [26]. This system includes six curved LCD screens covering a 270° view angle, a styrofoam cylinder for locomotion, a motion detector, and integrated neural recording capabilities [26].
The key advantage of this approach is the maximized experimental control it provides over contextual elements while maintaining compatibility with head-fixed neural recordings. Using this platform, researchers have successfully trained mice to perform context-dependent cognitive tasks with rules ranging from discrimination to delayed-sample-to-match while recording from thousands of hippocampal place cells [25]. Through precise manipulations of context elements, investigators discovered that context recognition remained intact with partial context elements but was impaired by exchanges of context elements between different environments [25].
Human VR Platforms for Contextual Memory Research
Human VR research utilizes both fully immersive head-mounted displays and desktop-based systems, with the latter offering better compatibility with neuroimaging techniques [27]. These platforms create controlled virtual environments that serve as contextual backgrounds for learning episodes. In a notable study on foreign vocabulary learning, participants navigated through distinctive desktop VR contexts while learning words from two phonetically similar languages [28].
A critical factor in human VR research is the concept of "presence" – the user's subjective experience of the VR environment as a place they have actually inhabited rather than merely watching passively [28]. This sense of presence appears to modulate the strength of context-dependent memory effects, with those experiencing higher levels of presence showing stronger contextual facilitation of memory.
Table 1: Comparative Analysis of VR Platforms in Rodent and Human Research
| Feature | Rodent VR Platform | Human VR Platform |
|---|---|---|
| Display System | Six curved LCD screens (270° view) [25] | Head-mounted displays or desktop systems [27] |
| Locomotion Interface | Styrofoam cylinder [25] | Hand controllers, keyboard, or physical walking [27] |
| Performance | High frame rate; real-time processing [25] | Varies by system; desktop-based common for neuroimaging [27] |
| Neural Recording Compatibility | Large-scale hippocampal recording [25] | EEG, fMRI, MEG compatibility [28] |
| Key Advantage | Precise control of contextual elements [25] | Balance between control and ecological validity [28] |
Experimental Protocols
Rodent Context Discrimination Task
Objective: To investigate how mice recognize and respond to distinct virtual contexts, and how manipulation of contextual elements affects behavior and neural representations.
Animals: Adult C57BL/6J mice (>8 weeks old) are housed under a 12-h light/dark cycle with food and water available ad libitum until water restriction begins for behavioral training [25].
Surgical Procedures:
- Implant a custom-made head plate fixed to the skull with dental acrylic for head-fixation during VR training [25].
- For calcium imaging, inject AAV2/9-CaMKII-GCaMP6f vector into hippocampal CA1 using stereotactic coordinates (AP: -1.82 mm, ML: -1.5 mm, DV: -1.5 mm relative to bregma) [25].
- Two weeks post-injection, implant a GRIN lens above the injection site during a second surgery [25].
Behavioral Training:
- Pre-training: After 1-2 days of water restriction, habituate mice to running on a rotating Styrofoam cylinder. Gradually introduce black-and-white gratings on a VR linear track, starting with a 25-cm track and progressively extending to 100 cm as the mouse achieves >70 trials per session [25].
- Context Discrimination Training: Train mice in a linear track (100 cm) consisting of an 80-cm context and a 20-cm corridor. The context is composed of four visual elements: left/right walls, top floor (ceiling), and front door, with distinct versions for different contexts [25].
- Reward Paradigm: Associate water reward with specific context areas. Mice receive reward (1.5-2.0 μL per drop) for licking in the correct context according to the task rules [25].
Data Collection:
- Monitor licking behavior as an indicator of context recognition.
- Record neural activity using calcium imaging during VR navigation.
- Analyze place cell responses to different contextual elements [25].
Human Context-Dependent Memory Protocol
Objective: To examine how distinctive VR learning contexts affect the acquisition, interference, and retention of similar materials, and the role of mental context reinstatement in recall.
Participants: Native English speakers without prior knowledge of Swahili or Chinyanja, typically aged 18-35 years.
VR Environment Setup:
- Create two highly distinctive desktop VR environments using 3D modeling software.
- Ensure environments are visually distinct but equally complex to avoid confounds [28].
Experimental Procedure:
- Group Assignment: Randomly assign participants to single-context (learn both languages in one VR environment) or dual-context (learn each language in its unique VR environment) groups [28].
- Learning Phase: Across two consecutive days, participants encode 80 foreign vocabulary items from two phonetically similar Bantu languages (Swahili and Chinyanja).
- Testing Phase:
- Conduct initial tests within the learning context(s) as participants navigate along a predetermined path.
- Administer transfer test outside of the learning context (without VR) to assess generalization.
- Implement controlled mental reinstatement protocol before each recall trial in transfer test [28].
- fMRI Component (for neural reinstatement analysis):
- Scan dual-context participants during recall using fMRI.
- Measure reinstatement of brain activity patterns associated with original encoding contexts [28].
Data Collection:
- Record recall accuracy for vocabulary items.
- Measure intrusion errors (producing translation from wrong language).
- Administer presence questionnaire to assess subjective experience of VR environments [28].
- Collect fMRI data during retrieval attempts.
Key Findings and Data Analysis
Quantitative Outcomes Across Species
Research using VR platforms has yielded robust quantitative data on context-dependent memory processes in both rodent and human models.
Table 2: Performance Metrics in Context-Dependent Memory Tasks
| Measure | Rodent Studies | Human Studies |
|---|---|---|
| Learning Performance | Successful learning of context-dependent rules (discrimination to delayed-sample-to-match) [25] | 42% (±17%) recall of foreign words after two exposures [28] |
| Context Manipulation Effects | Context recognition intact with partial elements; impaired by exchanges of elements [25] | 92% retention in dual-context vs 76% in single-context after one week [28] |
| Transfer Performance | N/A | 48% (±18%) recall during non-VR transfer test [28] |
| Physical Movement Benefit | N/A | Significantly better spatial memory in walking vs stationary conditions [27] |
Neural Mechanisms of Context-Dependent Memory
The hippocampus plays a central role in context-dependent memory across species, coding for and detecting novel contexts [22]. In rodents, researchers have recorded from thousands of hippocampal place cells during VR navigation, revealing how these cells represent different contextual elements [25]. The interaction of multiple brain regions including the perirhinal cortex, lateral entorhinal cortex, medial entorhinal cortex, postrhinal cortex, and the hippocampus processes different types of contextual information [22].
Human neuroimaging studies using fMRI have confirmed that reinstatement of brain activity patterns associated with the original encoding context during word retrieval is associated with improved recall performance [28]. This neural reinstatement appears to be a key mechanism supporting context-dependent memory.
Research comparing physical versus virtual navigation has demonstrated that stationary VR paradigms may disrupt typical neural representations of space. Studies utilizing augmented reality (AR) to enable physical movement during spatial memory tasks have found evidence for increased amplitude of theta oscillations during walking compared to stationary conditions, suggesting enhanced engagement of hippocampal networks during ambulatory navigation [27].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Technologies
| Item | Function | Example Application |
|---|---|---|
| Modular VR Platform | Provides customizable virtual environments with controlled contextual elements | Rodent context discrimination tasks [25] |
| Desktop VR System | Presents immersive environments compatible with neuroimaging | Human vocabulary learning studies [28] |
| Calcium Imaging | Records neural activity from large populations of cells | Monitoring hippocampal place cells in rodents [25] |
| fMRI | Measures brain-wide activity patterns during cognitive tasks | Assessing neural reinstatement in humans [28] |
| AR Spatial Memory Task | Enables study of spatial memory with physical movement | Comparing ambulatory vs. stationary navigation [27] |
| Presence Questionnaire | Quantifies subjective experience of VR environments | Assessing relationship between presence and memory [28] |
Methodological Considerations and Technical Implementation
Implementation Workflow
Successful implementation of VR platforms for context-dependent memory research requires careful attention to technical details and methodological considerations.
Comparative Platform Specifications
The technical specifications of VR platforms significantly influence their applicability for different research questions. Rodent systems prioritize compatibility with neural recording techniques, with custom-built platforms offering high frame rates and real-time processing capabilities that support precise experimental control during large-scale neural recordings [25]. These systems typically employ multiple curved LCD screens covering up to 270° to create immersive environments, with locomotion captured through motion detection of a styrofoam cylinder [26].
Human research platforms balance immersion with practical constraints, utilizing either head-mounted displays for full immersion or desktop systems for better neuroimaging compatibility [27]. A critical consideration in human research is the measurement of "presence" - the subjective experience of the virtual environment as real - which appears to modulate context-dependent memory effects [28].
Emerging evidence suggests that physical movement during encoding and retrieval enhances spatial memory performance compared to stationary VR paradigms [27]. This has important implications for platform selection, with augmented reality (AR) approaches offering a promising middle ground by allowing physical navigation while maintaining experimental control through virtual object overlay in real environments.
VR platforms have revolutionized the study of context-dependent learning and memory across species, enabling unprecedented experimental control while maintaining ecological validity. The complementary approaches of rodent and human research have yielded insights into the behavioral and neural mechanisms underlying context-dependent memory, highlighting the central role of the hippocampus and related medial temporal lobe structures.
Future directions include further integration of VR with advanced neural recording techniques, development of more sophisticated contextual manipulation paradigms, and translation of basic research findings into clinical applications for conditions such as Alzheimer's disease, PTSD, and other disorders characterized by context-dependent memory impairments [22]. The continued refinement of VR platforms promises to further enhance our understanding of how environmental contexts shape learning and memory across species.
From Lab to Clinic: Methodological Advances and Therapeutic Applications in Neuropsychiatry and Rehabilitation
Virtual reality (VR) has emerged as a transformative tool in behavioral neuroscience and mental health research, offering unprecedented capabilities for both symptom assessment and therapeutic intervention. By creating immersive, computer-generated environments, VR enables researchers and clinicians to study and treat psychiatric conditions with a level of ecological validity and experimental control previously unattainable in traditional laboratory or clinical settings [29]. The fundamental strength of VR lies in its ability to transport individuals into simulated worlds that feel authentic while allowing precise manipulation of environmental variables and real-time capture of behavioral, physiological, and cognitive data [29] [30]. This capability is particularly valuable for disorders such as psychosis, ADHD, and anxiety disorders, where symptoms are often context-dependent and difficult to reliably elicit in standard assessment environments.
The theoretical underpinnings of VR therapy draw from multiple psychological frameworks, with cognitive-behavioral principles forming a central foundation. For anxiety disorders, VR facilitates graded exposure therapy by presenting fear-eliciting stimuli in a controlled, safe environment, enabling inhibitory learning and extinction [30]. In psychosis research, VR allows experimental manipulation of social environments to study paranoid ideation and social cognitive processes [29]. For ADHD, VR-based interventions leverage principles of neuroplasticity and reinforcement learning to target deficits in attentional control, cognitive flexibility, and self-regulation [31]. The technology also aligns with the cognitive-energetic model of ADHD, which addresses deficits in motivational regulation that can be targeted through adaptive, immersive tasks [31].
A significant advancement in the field has been the development of standardized frameworks for VR clinical trials. The Virtual Reality Clinical Outcomes Research Experts (VR-CORE) committee has established a phased model mirroring pharmaceutical development pipelines [15]. This framework includes VR1 studies focusing on content development through human-centered design, VR2 studies assessing feasibility and initial efficacy, and VR3 studies comprising rigorous randomized controlled trials [15]. This systematic approach ensures methodological rigor in developing and validating VR interventions across mental health conditions.
Clinical Applications and Empirical Evidence
VR for Anxiety Disorders
Virtual Reality Exposure Therapy (VRET) represents the most established application of VR in mental health treatment. VRET operates on the same principles as traditional exposure therapy but delivers controlled exposures through immersive simulation rather than imagination or in vivo confrontation [30]. This approach offers distinct advantages, particularly for situations where real-world exposure is impractical, costly, or dangerous (e.g., fear of flying, combat-related PTSD) [30]. Meta-analyses comparing VRET to both control conditions and traditional evidence-based treatments for anxiety disorders consistently demonstrate medium-to-large effect sizes [8].
The efficacy of VRET stems from its ability to create a strong sense of presence while maintaining clinician control over the exposure parameters. Patients understand the virtual environment is artificial, yet their psychological and physiological responses mirror those experienced in real-life situations [30]. This phenomenon enables effective fear activation and subsequent extinction learning while providing patients with a greater sense of control, as they can terminate the experience at any moment [30]. Research indicates that this controllability enhances self-efficacy and may improve treatment adherence compared to traditional methods.
Table 1: Empirical Support for VRET in Anxiety Disorders
| Disorder | Research Findings | Strength of Evidence |
|---|---|---|
| Specific Phobias | Significant reduction in fear and avoidance behaviors; equivalent effects to in vivo exposure for acrophobia, aviophobia, spider phobia [30]. | Strong: Multiple RCTs and meta-analyses |
| Social Anxiety | Customized social scenarios effectively trigger anxiety; enables practice of social skills; reduces symptom severity [30]. | Moderate: Growing evidence base |
| PTSD | Enables controlled re-experiencing of traumatic memories; effective alternative for treatment-resistant cases [30]. | Moderate: Supported by RCTs |
| Panic Disorder | Safe exposure to interoceptive and situational triggers in controlled environment; reduces panic frequency and severity [8]. | Moderate: Evidence from clinical trials |
VR for Psychosis
VR applications for psychosis represent a innovative approach to studying and treating symptoms that are difficult to assess through traditional methods. Researchers have developed virtual environments specifically designed to elicit and measure paranoid ideation, social avoidance, and interpretive biases in controlled settings [29]. For example, participants can be immersed in a virtual subway train or elevator populated by neutral avatars, allowing researchers to objectively quantify paranoid responses to ambiguous social stimuli [29].
These paradigms enable precise experimental manipulations that illuminate underlying mechanisms. One seminal study placed participants in two conditions: one where they were taller than other virtual characters and another where they were shorter [29]. Results demonstrated that in the shorter condition, participants reported more negative social comparison and greater paranoia, with social comparison fully mediating the relationship between height manipulation and paranoid feelings [29]. This suggests that negative perceptions of self relative to others may drive paranoid ideation.
VR also shows promise for intervention in psychosis. Beyond assessment, virtual environments can be used for social skills training, allowing individuals to practice social interactions in a safe, graded manner. Cognitive remediation approaches using VR can target specific cognitive deficits associated with psychosis, such as executive functioning and social cognition [30]. The ability to customize difficulty levels and provide immediate feedback makes VR particularly suitable for these therapeutic applications.
VR for ADHD
VR-based interventions for ADHD represent a paradigm shift from conventional approaches, addressing core neurocognitive deficits through immersive, adaptive training environments. Unlike traditional cognitive training, VR can create ecologically valid scenarios that mimic real-world challenges with attentional control, impulse regulation, and task persistence [31]. These simulations can be systematically graded in difficulty and tailored to individual symptom profiles, providing optimal challenges that promote neuroadaptive plasticity [31].
Theoretical models informing VR interventions for ADHD include Barkley's executive dysfunction model and the dual-pathway model, which emphasize deficits in inhibitory control, sustained attention, and motivational regulation [31]. VR environments can target these domains through carefully designed tasks that require continuous performance, response inhibition, and cognitive flexibility within distracting contexts. The reinforcing properties of immersive gaming elements can enhance engagement and adherence, particularly important for pediatric populations [31].
Preliminary research indicates promising applications across the lifespan. For children with ADHD, VR classrooms can assess and train sustained attention despite typical classroom distractions [31]. For adults, VR can simulate workplace environments to practice organizational skills and time management. However, the evidence base remains emergent, with researchers calling for more rigorous randomized controlled trials comparing VR interventions to established treatments [31].
Table 2: VR Applications Across Psychiatric Disorders
| Disorder | Assessment Applications | Therapeutic Applications | Key Mechanisms |
|---|---|---|---|
| Anxiety Disorders | Behavioral avoidance; physiological reactivity; subjective distress [29] | Graded exposure; extinction learning; self-efficacy enhancement [30] | Controlled exposure; emotional processing; inhibitory learning |
| Psychosis | Paranoid ideation; social distance; interpretation biases [29] | Social skills training; reality testing; cognitive remediation [30] | Normalization of experiences; social cognitive training; behavioral experiment |
| ADHD | Sustained attention; impulse control; cognitive flexibility [31] | Cognitive training; behavioral inhibition; self-regulation [31] | Neuroplasticity; reinforcement learning; attentional control |
Experimental Protocols and Methodological Framework
VR Clinical Trial Phases (VR-CORE Model)
The VR-CORE framework provides a structured methodology for developing and testing VR interventions, ensuring scientific rigor comparable to pharmaceutical trials [15]. The model comprises three distinct phases:
VR1 Studies: Content Development VR1 studies focus on intervention development using human-centered design principles. This phase emphasizes deep engagement with patient and provider stakeholders to ensure relevance, usability, and therapeutic alignment [15]. Key activities include:
- Recruitment of diverse patient populations representing varying ages, comorbidities, and technological comfort levels
- Observation of patients in clinically relevant contexts to understand behavioral patterns and environmental influences
- Individual interviews and focus groups to identify needs, struggles, expectations, and treatment preferences
- Expert interviews with clinicians to integrate therapeutic expertise and clinical practicality
- Journey mapping to define the sequence of events patients will experience within the VR intervention [15]
This participatory design process helps avoid technological solutions that fail to address genuine clinical needs or align with therapeutic mechanisms.
VR2 Studies: Feasibility and Initial Efficacy VR2 trials conduct early-stage testing to establish feasibility, acceptability, tolerability, and preliminary clinical effects [15]. These studies typically employ smaller sample sizes and focus on:
- Acceptability metrics: Patient satisfaction, perceived usefulness, and willingness to continue treatment
- Feasibility indicators: Recruitment rates, completion rates, protocol adherence, and implementation barriers
- Tolerability assessment: Incidence of cybersickness, emotional distress, or other adverse effects
- Clinical outcomes: Preliminary evidence of symptom reduction using validated measures
- Dose-response relationships: Optimal session duration, frequency, and total treatment length [15]
VR2 studies provide essential data for refining interventions and informing power calculations for subsequent randomized trials.
VR3 Studies: Randomized Controlled Trials VR3 trials constitute full-scale randomized controlled studies comparing the VR intervention to appropriate control conditions [15]. Methodological considerations include:
- Control group selection: Active controls (standard care, alternative treatments) or attention-placebo controls
- Blinding procedures: While participants cannot be blinded to VR exposure, outcome assessors and statisticians should remain blinded
- Primary outcomes: Clinically meaningful endpoints validated for the target population
- Sample size justification: Adequate power based on VR2 effect size estimates
- Generalizability: Inclusion criteria reflecting real-world patient diversity [15]
These trials provide the definitive evidence base for clinical efficacy and guide implementation decisions.
Protocol for VR Exposure Therapy in Anxiety Disorders
The following protocol outlines a standardized approach for implementing VRET for anxiety disorders, adaptable to specific phobias, social anxiety, and PTSD:
Session 1: Psychoeducation and Treatment Rationale
- Establish therapeutic alliance and explain VR technology
- Present treatment rationale based on exposure principles
- Develop individualized fear hierarchy with patient input
- Introduce coping strategies (e.g., diaphragmatic breathing, cognitive restructuring)
- Conduct brief VR orientation with neutral environment
Sessions 2-8: Graduated Exposure
- Begin with least feared scenario from hierarchy
- Use subjective units of distress (SUDS) ratings every 2-3 minutes
- Continue exposure until SUDS decreases by 50% within session
- Progress to next hierarchy item when SUDS stabilizes at low level
- Vary exposure parameters to enhance generalization (e.g., different virtual contexts, stimulus intensities)
Session 9: Relapse Prevention
- Review progress and skills acquired
- Develop maintenance plan for continued practice
- Address anticipatory anxieties about real-world application
- Schedule booster sessions if indicated [30] [8]
Throughout treatment, clinicians should monitor for cybersickness and adjust protocols accordingly. Between-session practice, either in vivo or with take-home VR systems, enhances generalization of treatment gains.
VR Exposure Therapy Clinical Protocol
Protocol for VR Social Stress Paradigm in Psychosis Research
This protocol details the implementation of a VR social stress test for assessing paranoid ideation, adaptable for both research and clinical assessment purposes:
Environment Setup
- Create a socially challenging virtual environment (e.g., subway car, elevator, cafe)
- Populate with neutral avatars with pre-programmed behaviors
- Standardize avatar appearance, number, and proximity to participant
- Implement eye-tracking and movement tracking capabilities
Experimental Conditions
- Neutral condition: Avatars display neutral expressions and behaviors
- Stress condition: Manipulate social stressors (e.g., avatar height differences, direct gaze, crowded spaces)
- Control condition: Minimal social stimuli for baseline comparison
Assessment Measures
- Primary outcome: Paranoia scale scores post-exposure
- Behavioral measures: Interpersonal distance, eye contact avoidance, escape behaviors
- Physiological measures: Heart rate variability, galvanic skin response synchronized with VR events
- Cognitive measures: Interpretation biases, social threat appraisal [29]
Procedure
- Baseline assessment (pre-VR symptoms, physiological measures)
- VR orientation (neutral environment)
- Randomized exposure to experimental conditions (counterbalanced)
- Continuous symptom ratings during exposure
- Post-exposure debriefing and assessment
This protocol enables precise quantification of paranoid responses to social stimuli while controlling for environmental variables that confound real-world assessment.
Implementation Framework and Technical Considerations
Successful implementation of VR in clinical research and practice requires attention to technical specifications, ethical considerations, and practical barriers. The following framework addresses key implementation components:
Equipment Selection and Technical Specifications
Choosing appropriate VR hardware represents a critical first step in developing VR research or clinical programs. Key considerations include:
Head-Mounted Display (HMD) Selection
- Display resolution: Higher resolution reduces screen-door effect and enhances presence
- Refresh rate: ≥90Hz minimizes latency and reduces cybersickness risk
- Tracking capabilities: Inside-out vs. external sensor tracking based on mobility needs
- Comfort and adjustability: Particularly important for extended sessions
- Integrated sensors: Eye-tracking, facial expression analysis enhance research utility
Software and Development Platforms
- Game engines: Unity or Unreal Engine for custom environment development
- Content availability: Pre-built environments for common phobias and scenarios
- Customization capacity: Ability to modify environments for individual needs
- Data export functionality: Compatibility with statistical analysis packages
Accessory Equipment
- Physiological monitoring: Heart rate, GSR, EEG synchronization capabilities
- Input devices: Hand controllers, data gloves for interaction tracking
- Safety equipment: Boundary systems for room-scale VR [8]
Table 3: Technical Specifications for Research-Grade VR Systems
| Component | Minimum Specification | Optimal Specification | Research Applications |
|---|---|---|---|
| HMD Resolution | 1280×1440 per eye | 1920×2160 per eye | All applications; critical for presence |
| Refresh Rate | 90Hz | 120Hz | Reduces cybersickness; enhances realism |
| Field of View | 100° | 110°-130° | Peripheral relevance for anxiety contexts |
| Tracking | Rotational + positional | Room-scale with sub-millimeter precision | Social interaction studies; movement analysis |
| Eye Tracking | Not required | 60-120Hz sampling rate | Attention research; social gaze monitoring |
| Audio | Integrated headphones | Spatial 3D audio | Environmental immersion; auditory processing |
Ethical Considerations and Risk Management
VR implementation raises unique ethical considerations that require proactive management:
Privacy and Data Security
- VR systems capture extensive behavioral and physiological data requiring protection
- Implement encryption for data storage and transmission
- Develop clear data retention and disposal policies
- Obtain informed consent specifically addressing biometric data collection [31]
Psychological Risk Mitigation
- VR exposure may temporarily increase anxiety or trigger emotional reactions
- Establish protocols for session termination and distress management
- Screen for contraindications (e.g., seizure disorders, severe dissociation)
- Provide adequate debriefing following emotionally challenging exposures [30]
Equity and Access
- High equipment costs may limit accessibility in resource-constrained settings
- Consider mobile-based VR alternatives to enhance dissemination
- Address technological literacy barriers through simplified interfaces
- Develop culturally adapted content for diverse populations [31]
Clinical Governance
- Establish competency standards for VR-assisted therapy
- Develop supervision protocols for novice clinicians
- Create maintenance procedures for equipment sanitation and functionality [8]
Implementing VR research requires both technical equipment and methodological resources. The following toolkit outlines essential components for establishing a VR research program:
Table 4: Essential VR Research Resources
| Resource Category | Specific Tools/Solutions | Research Function | Key Considerations |
|---|---|---|---|
| VR Hardware Platforms | HTC VIVE Pro Eye, Oculus Rift S, Varjo VR-3 | Display immersive environments; track user movement/behavior | Resolution, refresh rate, FOV, integrated sensors, comfort |
| VR Development Software | Unity 3D, Unreal Engine, VRTK | Create custom virtual environments; program interactive elements | Learning curve, asset availability, compatibility with analysis tools |
| Behavioral Data Capture | Eye-tracking modules, motion capture, controller input | Quantify attention, movement, interaction patterns | Sampling rate, data synchronization, export formats |
| Physiological Monitoring | BioPac Systems, Empatica E4, Shimmer GSR+ | Objective arousal measures (HRV, EDA, EMG) | Wireless operation, synchronization with VR events, data quality |
| Quantitative Analysis Tools | R, Python, Displayr, SPSS | Statistical analysis of behavioral, subjective, physiological data | Handling multimodal data streams, visualization capabilities |
| Experimental Design Frameworks | VR-CORE guidelines [15] | Phase-appropriate study design (VR1, VR2, VR3) | Regulatory compliance, methodological rigor, stakeholder engagement |
VR Research Program Core Components
Successful VR research programs integrate multiple technical systems within a rigorous methodological framework. The hardware platform forms the foundation for delivering immersive experiences, while development software enables environment customization. Behavioral and physiological capture systems provide objective outcome measures, with analysis tools facilitating data interpretation. Throughout this process, established design frameworks like the VR-CORE model ensure scientific rigor and clinical relevance [15]. This integrated approach enables researchers to leverage VR's unique capabilities while maintaining methodological standards required for advancing evidence-based mental health interventions.
Integrating VR with Neurofeedback and EEG for Real-Time Neural Self-Regulation
The integration of virtual reality (VR), electroencephalography (EEG), and neurofeedback (NFB) represents a transformative frontier in behavioral neuroscience research. This synergy creates closed-loop systems capable of monitoring and modulating brain function within controlled, yet ecologically valid, immersive environments [32] [33]. Such neuroadaptive technology enables real-time neural self-regulation, where a user's brain signals directly influence elements of a virtual world, facilitating operant learning of brain activity patterns [34] [35]. For researchers and drug development professionals, this paradigm offers a powerful tool for investigating neural correlates of behavior and testing the efficacy of neurotherapeutic interventions with a level of precision and engagement previously unattainable [34] [36]. The field is rapidly advancing due to hardware miniaturization, the development of dry electrodes, and the commercial availability of high-quality head-mounted displays (HMDs), making sophisticated VR-EEG setups more accessible and practical for research and clinical applications [33].
Application Notes: Efficacy and Mechanisms
The combined application of VR and EEG-NFB is being explored across a wide spectrum of health conditions and cognitive domains. Understanding its evidenced efficacy and underlying mechanisms is crucial for designing robust experiments.
Documented Efficacy Across Domains
A recent systematic review assessed the efficacy of VR-based EEG-NFB for relieving health-related symptoms, classifying it according to established guidelines for psychophysiological interventions. The findings are summarized in the table below.
Table 1: Efficacy of VR-Based EEG Neurofeedback for Health-Related Symptom Relief
| Domain | Efficacy Classification | Key Findings and Potential Applications |
|---|---|---|
| Attention | Probably Efficacious | Shows promise for conditions like ADHD, potentially offering a more engaging alternative to traditional cognitive training [34]. |
| Emotions & Mood | Possibly Efficacious | Applied for anxiety disorders and depression; VR allows for graded exposure and emotional regulation in personalized scenarios [34] [3]. |
| Anxiety Disorders | Supported by Meta-Reviews | VR exposure therapy favorably compares to existing treatments for anxiety, phobias, and PTSD, with long-term effects generalizing to the real world [3]. |
| Pain Management | Possibly Efficacious | VR's immersive nature is a proven distractor from acute pain; NFB may enhance this by teaching self-regulation of neural circuits involved in pain perception [34] [3]. |
| Relaxation | Possibly Efficacious | Used for stress reduction; immersive natural environments paired with NFB on rhythms like SMR can enhance physical relaxation and mental alertness [34] [35]. |
| Other Domains (Impulsiveness, Memory, etc.) | Possibly Efficacious | Preliminary evidence supports investigation into impulsiveness (e.g., in ADHD), memory (post-stroke rehabilitation), and self-esteem [34]. |
Neurocognitive Mechanisms of Action
The potency of integrated VR-NFB stems from its engagement of key neurocognitive processes:
Embodied Simulation and Presence: Neuroscience suggests the brain uses embodied simulations to regulate the body and predict actions, concepts, and emotions [3]. VR operates on a similar principle, providing a sensory simulation that predicts the user's movements, thereby inducing a strong sense of presence—the subjective feeling of "being there" in the virtual environment [3] [37]. This presence is crucial for eliciting genuine cognitive and emotional responses, making therapy and assessment more ecologically valid [38]. Research indicates that a decreased power in the parietal alpha rhythm is a neurophysiological correlate of an increased sense of presence, suggesting a direct link between specific brain activity and the subjective VR experience [37].
Enhanced Motivation and Engagement: Traditional NFB tasks can be repetitive and demotivating [34]. Integrating NFB into an immersive, game-like VR environment significantly increases user motivation, interest, and adherence to training protocols [34] [35]. For instance, stroke patients undergoing VR-NFB rehabilitation reported high enjoyability and a desire to continue training beyond the required period [35].
Targeting "Hot Cognitions": Traditional cognitive therapies often rely on "cold cognitions"—abstract self-reflection detached from emotional arousal. VR-NFB allows for a "symptom capture" approach, where therapy is applied while the symptom is actively being elicited in a controlled virtual space [36]. This allows individuals to practice regulation strategies against "hot" (emotionally charged) cognitions, which may lead to more robust and generalizable learning [36].
Experimental Protocols
This section provides detailed methodologies for implementing VR-EEG-NFB experiments, from basic research to clinical application.
Protocol 1: Basic SMR Up-Regulation with 3D vs. 2D Feedback
This protocol is adapted from a sham-controlled study investigating the effect of feedback modality on NFB performance [35].
Aim: To compare the efficacy of a 3D VR-based feedback paradigm against a conventional 2D bar feedback paradigm for up-regulating the sensorimotor rhythm (SMR, 12-15 Hz) in a single training session.
Research Reagent Solutions: Table 2: Essential Materials for SMR Up-Regulation Protocol
| Item | Specification/Function |
|---|---|
| EEG Amplifier | g.tec gUSBamp RESEARCH amplifier or equivalent, sampling rate ≥ 256 Hz [35]. |
| EEG Electrodes | 16 active Ag/AgCl electrodes (including F3, Fz, F4, C3, Cz, C4, Pz, EOG channels); gel-based for optimal signal quality [35]. |
| VR Headset | Head-Mounted Display (HMD) capable of running custom paradigms (e.g., Oculus Rift, HTC Vive) [35]. |
| Software | Real-time signal processing software (e.g., BCILab, OpenVIBE) and a 3D game engine (Unity, Unreal Engine) for creating feedback environments [33]. |
Procedure:
- Participant Preparation: Apply EEG electrodes according to the 10-20 system. The primary feedback electrode is Cz. Impedances for scalp electrodes should be kept below 5 kΩ [35].
- Baseline Recording (3 minutes): Participants watch the feedback paradigm move autonomously while relaxing. The individual mean and standard deviation of SMR (12-15 Hz) power from this run are calculated to set the initial threshold for NFB. Thresholds for Theta (4-7 Hz) and Beta (16-30 Hz) are also set for artifact control [35].
- Group Randomization: Randomly assign participants to one of four groups: 2D Real Feedback, 2D Sham Feedback, 3D Real Feedback, or 3D Sham Feedback [35].
- Feedback Training (6 runs of 3 minutes each):
- 2D Group: Participants see a simple bar on the VR headset. They are instructed to increase the bar's height by generating the correct mental state [35].
- 3D Group: Participants are immersed in a virtual forest environment. They control a ball rolling along a path; successful SMR up-regulation moves the ball forward [35].
- Real Feedback: The visual feedback is directly controlled by the participant's live SMR power.
- Sham Feedback: The visual feedback is pre-recorded or yoked to another participant's performance, unbeknownst to the participant [35].
- Instructions: Instruct participants to be physically relaxed, minimize blinking, and find a mental strategy to increase SMR power.
- Data Analysis: Calculate the average SMR power for each feedback run. Perform a repeated-measures ANOVA with factors Group (2D vs. 3D) and Feedback Type (Real vs. Sham) on the SMR power across runs.
Workflow Diagram:
Protocol 2: Targeted Intervention for Auditory Verbal Hallucinations (AVH)
This protocol outlines a pilot study for a novel hybrid therapy ("Hybrid") for psychosis, integrating VR, NFB, and cognitive behavioral therapy (CBT) [36].
Aim: To investigate the feasibility, acceptability, and preliminary efficacy of a hybrid VR-NFB-CBT intervention for reducing distress from auditory verbal hallucinations (AVHs) in individuals with psychosis.
Research Reagent Solutions: Table 3: Essential Materials for AVH Intervention Protocol
| Item | Specification/Function |
|---|---|
| EEG System | Portable EEG system with capability for real-time beta power analysis. |
| VR Headset & Software | HMD with software to create and customize virtual environments that simulate a patient's specific AVH triggers [36]. |
| Clinical Assessment Tools | Standardized scales for AVH severity (e.g., Psychotic Symptom Rating Scales, PSYRATS) and general psychopathology (e.g., PANSS). |
Procedure:
- Screening & Personalization: Recruit participants with persistent AVHs. Conduct in-depth interviews to identify idiosyncratic triggers (e.g., specific social situations, environments) and characteristics of the voices. Use this information to personalize the VR environments [36].
- EEG Target Identification: Identify a neural target associated with symptom provocation. In the Hybrid study, this is high-beta power over relevant cortical areas [36].
- Intervention Sessions (12 weekly, face-to-face sessions):
- Symptom Provocation: The participant enters the personalized VR environment designed to elicit their AVHs at a manageable level ("hot cognition") [36].
- Neurofeedback Regulation: While in the provocative VR environment, the participant receives real-time NFB (e.g., a visual bar) representing their high-beta power. The goal is to learn strategies to down-regulate this activity [36].
- Cognitive Behavioral Therapy for Psychosis (CBTp): A clinician guides the participant through CBTp techniques during VR-NFB to help them develop cognitive and behavioral strategies for responding to voices and reality testing [36].
- Hierarchy Progression: As the participant gains mastery, the intensity of the VR triggers is gradually increased, following an exposure hierarchy [36].
- Outcome Measures:
- Feasibility/Acceptability: Consent rates, session completion rates, and user experience surveys on a 5-point Likert scale [36].
- Clinical Efficacy: Pre- and post-intervention changes in AVH distress and frequency (PSYRATS), general symptoms (PANSS), and functioning.
- Engagement of Targets: Ability to self-regulate the high-beta target and progression up the VR exposure hierarchy [36].
Workflow Diagram:
The Scientist's Toolkit: Technical Considerations
Successfully implementing a VR-EEG-NFB system requires careful consideration of hardware and software components.
Table 4: Research Reagent Solutions for VR-EEG-NFB Systems
| Component | Key Considerations | Examples & Notes |
|---|---|---|
| EEG Amplifier | Portability, number of channels, sampling rate, wireless capability. | Portable amplifiers (e.g., by Brain Products, g.tec) allow for more natural movement in VR [37]. |
| EEG Electrodes | Type: Gel-based (high signal quality, longer setup) vs. Dry/Semi-dry (fast setup, comfort, potentially more noise). Placement: Full scalp vs. focused headbands (e.g., for frontal metrics only) [33]. | Pillar-style dry electrodes can improve contact in hair-covered areas [33]. Textile headbands (e.g., Bitbrain Ikon) are user-friendly but limited to frontal cortex [33]. |
| VR Headset (HMD) | Resolution, refresh rate, field of view, inside-out vs. outside-in tracking, comfort for extended use. | Consumer-grade HMDs (e.g., Oculus Quest, HTC Vive) are now widely used in research due to their quality and affordability [33]. |
| Integration Software | Real-time signal processing, artifact handling, and a robust link to the VR rendering engine. | Platforms like Unity or Unreal Engine are standard for VR development. Middleware like Lab Streaming Layer (LSL) is critical for synchronizing EEG and VR events [33]. |
| Integrated Systems | All-in-one solutions with EEG sensors embedded directly into the HMD strap. | Systems like Cognixion ONE offer convenience but may be limited to frontal electrodes and susceptible to artifact [32] [33]. |
Navigating Technical Challenges
- Signal Quality and Artifacts: VR environments introduce significant motion artifacts and electromagnetic interference. Use active electrodes and advanced artifact removal algorithms (e.g., ICA, PCA) that are optimized for real-time processing [33].
- Synchronization: Precise timing between brain events and VR events is critical. Employ a dedicated synchronization system (e.g., via LSL or hardware triggers) to ensure the integrity of the data [33].
- Comfort and Usability: The physical integration of an EEG cap and a VR headset can cause discomfort and pressure points, potentially limiting session duration. Innovative designs using flexible materials and optimizing weight distribution are active areas of development [33] [37].
The integration of VR with EEG and neurofeedback constitutes a paradigm shift in behavioral neuroscience, enabling the study and modulation of brain function with unprecedented ecological validity and user engagement. The protocols and guidelines provided here offer a foundation for researchers to explore this frontier. While challenges in signal quality, hardware integration, and the need for larger-scale efficacy trials remain, the potential is vast [34] [33]. As the technology continues to mature, VR-EEG-NFB is poised to become an indispensable tool for both fundamental research into brain-behavior relationships and the development of next-generation, personalized therapeutic interventions for a range of neurological and psychiatric conditions.
Application Notes: Efficacy and Key Considerations
The integration of Virtual Reality (VR) into motor rehabilitation represents a paradigm shift in neurorehabilitation, leveraging brain-computer interfaces to promote neural plasticity and functional recovery. Application of this technology must be grounded in a firm understanding of its demonstrated efficacy, its underlying mechanisms, and the practical factors influencing its implementation.
Quantitative Efficacy in Stroke and TBI Rehabilitation
Recent meta-analyses provide robust, quantitative evidence supporting VR-based interventions for motor recovery. The following tables summarize key outcomes for Stroke and Traumatic Brain Injury (TBI) populations.
Table 1: Efficacy of Combined VR and Mirror Therapy (MT) in Stroke Motor Recovery [39] [40]
| Outcome Measure | Population | Mean Difference (MD) / Standardized Mean Difference (SMD) | 95% Confidence Interval | P-value | Clinical Significance Notes |
|---|---|---|---|---|---|
| Upper Extremity Motor Function (Fugl-Meyer Assessment - UE) | Stroke (7 RCTs) | MD 3.50 | 1.47 to 5.53 | <0.001 | Statistically significant but below the Minimal Clinically Important Difference (MCID: 4.25-7.25) |
| Hand Dexterity (Box and Block Test) | Stroke (7 RCTs) | MD 1.09 | 0.14 to 2.05 | 0.03 | Statistically significant improvement |
| Manual Function Test | Stroke (7 RCTs) | MD 2.15 | 1.22 to 3.09 | <0.001 | Statistically significant improvement |
Table 2: Efficacy of Digital Cognitive Interventions in TBI [41] [42]
| Cognitive Domain | Number of Studies | Standardized Mean Difference (SMD) | 95% Confidence Interval | Heterogeneity (I²) |
|---|---|---|---|---|
| Global Cognitive Function | 16 | 0.64 | 0.44 to 0.85 | 0% |
| Executive Function | 16 | 0.32 | 0.17 to 0.47 | 15% |
| Attention | 16 | 0.40 | 0.02 to 0.78 | 0% |
| Social Cognition | 16 | 0.46 | 0.20 to 0.72 | 0% |
| Memory | 16 | Not Significant (NS) | - | - |
| Psychosocial Outcomes (e.g., Depression) | 16 | NS (VR had a positive effect) | - | - |
Neurobiological and User Experience Considerations
The efficacy of VR rehabilitation is supported by its impact on neural mechanisms and user engagement.
- Neural Mechanisms: VR therapy induces changes in neural plasticity, with positive correlations observed between these changes and functional recovery post-stroke. The mechanism is partly explained by the activation of mirror neuron systems, which are engaged both when patients execute a motor action and when they observe the same action in a virtual environment, facilitating motor learning [39] [40].
- User Experience & Adherence: A qualitative meta-synthesis of stroke survivors' experiences (n=145 across 16 studies) identified key meta-themes influencing rehabilitation success [43]. Patients reported perceived benefits and hindering factors, emphasizing the importance of emotional support from family and peers, professional support from healthcare providers, and financial support from governments. Furthermore, rehabilitation motivation is a critical factor for adherence and outcomes, which can be enhanced by immersive and engaging VR scenarios [43].
Experimental Protocols
To ensure reproducibility and standardization in research, the following protocols detail the methodology for implementing VR-based motor rehabilitation.
Protocol 1: Combined VR and Mirror Therapy for Upper Extremity Stroke Rehabilitation
This protocol is adapted from a recent systematic review and meta-analysis of RCTs investigating the combined effect of VR and MT [39] [40].
- Primary Objective: To improve upper extremity motor function and hand dexterity in sub-acute and chronic stroke patients (>3 months post-stroke).
- Population: Adults diagnosed with stroke. Exclusion criteria: significant comorbidities (e.g., severe orthopedic conditions), severe aphasia, or uncontrolled epilepsy.
- Intervention Group:
- Technology: Use either an Immersive VR (IVR) system with a head-mounted display and motion-tracking controllers, or a Non-Immersive VR (NIVR) system presented on a 2D screen with input devices (e.g., motion-sensing gloves, joysticks).
- Core Therapeutic Principle: Integrate mirror therapy principles into the VR platform. The virtual environment should display a mirrored, real-time avatar of the patient's unaffected limb, performing symmetrical movements, to create the illusion of movement in the affected limb.
- Dosage: 30-60 minute sessions, 3-5 times per week, for a total of 4-8 weeks.
- Task Progression: Begin with simple, gross motor tasks (e.g., reaching, pushing a virtual ball). Progressively increase difficulty to include fine motor tasks (e.g., pinching, grasping, and manipulating virtual objects) based on patient performance.
- Control Group: Active control receiving conventional mirror therapy (using a physical mirror box) or dose-matched conventional occupational therapy.
- Primary Outcome Measures:
- Fugl-Meyer Assessment for Upper Extremity (FMA-UE): Assess motor impairment.
- Box and Block Test (BBT): Assess manual dexterity.
- Manual Function Test (MFT): Assess upper limb function.
- Data Collection: Assess outcomes at baseline (pre-intervention), immediately post-intervention, and at a 3-month follow-up to evaluate retention. Use intention-to-treat analysis.
Protocol 2: Non-Immersive VR for Cognitive Rehabilitation in TBI
This protocol is derived from a systematic review and meta-analysis on digital cognitive interventions for TBI [42].
- Primary Objective: To improve global cognitive function, executive function, and attention in patients with Traumatic Brain Injury.
- Population: Adults with a confirmed diagnosis of TBI. Exclusion criteria: other major neurological conditions (e.g., stroke, dementia).
- Intervention Group:
- Technology: Non-Immersive VR (NIVR) or computer-based cognitive training delivered via a standard 2D desktop/laptop monitor. Interaction is through a mouse, keyboard, or touchscreen.
- Software: Utilize certified medical-grade software or validated serious games designed for cognitive rehabilitation. Tasks should target specific cognitive domains.
- Dosage: 45-60 minute sessions, 2-3 times per week, for a minimum of 8 weeks. Evidence suggests a greater number of training sessions may enhance cognitive benefits [42].
- Adaptivity: The software must dynamically adjust the difficulty level of tasks (stimulus intensity, processing speed, working memory load) based on the patient's real-time performance to maintain an optimal challenge level.
- Control Group: Passive control (waitlist) or active control (traditional, non-computerized cognitive rehabilitation therapy).
- Primary Outcome Measures:
- Global Cognition: Montreal Cognitive Assessment (MoCA) or similar.
- Executive Function: Trail Making Test (TMT) Part B, Stroop Test.
- Attention: Continuous Performance Test (CPT), TMT Part A.
- Social Cognition: The Awareness of Social Inference Test (TASIT).
- Data Collection: Assess outcomes at baseline and immediately post-intervention.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Technologies for VR Rehabilitation Research
| Item / Technology | Function / Rationale in Research | Representative Examples |
|---|---|---|
| Immersive VR (IVR) System | Provides a fully immersive experience; ideal for studying presence and ecological validity in rehabilitation. | Head-Mounted Displays (e.g., HTC Vive [43], Oculus Rift) with 3D interaction devices/motion-tracking gloves [39]. |
| Non-Immersive VR (NIVR) System | Offers a more accessible, cost-effective platform for studying task-specific motor and cognitive retraining. | 2D computer screens or gaming consoles (e.g., Wii, Xbox Kinect) with input devices like mice, joysticks, or CyberGloves [39]. |
| Motion Tracking Technology | Precisely quantifies movement kinematics (range of motion, velocity, accuracy) for objective outcome measures. | CyberGloves, CyberGrasps, force sensors, or camera-based systems integrated with VR platforms [39]. |
| Neurofeedback Apparatus | Allows for the investigation and modulation of neural correlates of recovery by providing real-time feedback on brain activity. | Electroencephalography (EEG) systems integrated with the VR environment to allow self-modulation of neural oscillations [36]. |
| Standardized Outcome Batteries | Ensures consistent, valid, and reliable measurement of motor and cognitive function across studies for comparative analysis. | Fugl-Meyer Assessment (FMA), Box and Block Test (BBT), Trail Making Test (TMT), Montreal Cognitive Assessment (MoCA). |
Visualizing Workflows and Mechanisms
The following diagrams, created using DOT language, illustrate the logical workflow of a combined VR therapy protocol and the hypothesized neurobiological mechanisms of action.
VR-MT Protocol Workflow
Neurobiology of VR Rehabilitation
Virtual reality (VR) has emerged as a transformative tool in behavioral neuroscience, enabling researchers to study complex cognitive processes in controlled, immersive environments. For preclinical research, particularly in rodent models, VR allows for the precise manipulation of environmental contexts while facilitating stable neural recording. However, many existing VR tools have been limited by inflexible design, low performance, and incompatibility with large-scale neural recording technologies [25] [44]. The development of high-performance, configurable VR platforms addresses these limitations, providing an integrated solution for investigating the neural mechanisms of context-dependent cognition. This integration is crucial for advancing our understanding of brain function and for improving the translational value of preclinical drug development.
Platform Specifications and Quantitative Performance Metrics
A high-performance VR platform for rodents is characterized by its modular hardware and custom software, designed for maximum flexibility, upgradability, and integration with neural recording apparatus. Key technological features include real-time processing, a high frame rate for VR display, and continuous high-sampling-rate data acquisition [25]. The table below summarizes the core performance metrics and capabilities of an advanced system as described in recent literature.
Table 1: Performance Specifications of a High-Performance Rodent VR Platform
| Feature | Specification | Research Advantage |
|---|---|---|
| Frame Rate | High frame rate (significantly above 30 Hz) [25] | Ensures smooth visual flow, critical for realistic navigation and reliable neural coding. |
| Data Acquisition | Continuous, high-sampling-rate streaming to local disk [25] | Enables precise timestamping of behavior, neural activity, and system events for fine-grained analysis. |
| System Control | Trial-by-trial switching between contexts; editable context elements [25] | Allows for sophisticated behavioral protocols (e.g., delayed-sample-to-match) and direct testing of how specific cues drive behavior. |
| Neural Recording | Compatible with large-scale recording (e.g., two-photon calcium imaging) [25] | Facilitates the simultaneous recording from thousands of neurons, such as hippocampal place cells, during behavior. |
| 3D Map Editing | Independent editing of virtual 3D maps using professional-grade software [25] | Provides flexibility in experimental design without requiring laborious programming, accessible to small laboratories. |
Detailed Experimental Protocol: Context-Dependent Cognitive Tasks
The following protocol outlines the procedures for utilizing a high-performance VR platform to train head-fixed mice in a context-dependent cognitive task, combined with large-scale hippocampal calcium imaging.
Animals and Surgical Procedures
- Animals: Use adult wild-type C57BL/6J mice. House them under a standard 12-hour light/dark cycle.
- Water Restriction: Begin water restriction 1-2 days before pre-training, reducing body weight to 80-90% of the initial level. Maintain body weight above 85% throughout training by providing 0.5 mL - 0.8 mL of water daily [25].
- Head Plate Implantation: Implant a custom-made head plate under isoflurane anesthesia, fixing it to the skull with dental acrylic. This provides stable head-fixation during VR sessions [25].
- Viral Injection and GRIN Lens Implantation (for calcium imaging):
- Inject an AAV vector carrying a calcium indicator (e.g., AAV2/9-CaMKII-GCaMP6f) into the hippocampal CA1 region.
- After a 2-week incubation period, perform a second surgery to implant a gradient index (GRIN) lens above the injection site. This involves a craniotomy and careful aspiration of brain tissue above the hippocampus until the surface is visible.
- Lower the GRIN lens to a position above CA1 and fix it with dental resin [25].
Behavioral Training in VR
The training is a multi-stage process that gradually acclimates the mouse to the VR system and shapes its behavior.
Diagram Title: VR Behavioral Training Workflow
- Stage 1: Habituation (1 week). Head-fix the mouse on a rotating Styrofoam cylinder. Conduct daily sessions of 15-30 minutes to habituate the animal to head-fixation and running on the cylinder [25].
- Stage 2: Pre-training in VR.
- Initial Exposure: Introduce the mouse to a short (25 cm) virtual linear track with black-and-white gratings on the walls. Provide a small water reward (1.5-2 µL per drop, up to 4 drops per trial) upon successful traversal.
- Track Extension: Once the mouse completes more than 70 trials in a session, progressively extend the track length to 50 cm and then to 100 cm. The pre-training is complete when the mouse can perform over 70 trials in a 100 cm track session [25].
- Stage 3: Formal Task Training (Place-Dependent Reward).
- Track Design: Use a linear track (e.g., 100 cm) composed of a distinct context zone (e.g., 80 cm) and a corridor (e.g., 20 cm).
- Task Rule: Associate a water reward with one specific zone (context or corridor). The mouse receives a reward only if it licks within the reward-associated zone. Over learning sessions, the mouse will learn to concentrate its licks in the rewarded area [25].
- Stage 4: Context Discrimination Task. To study more complex cognition, the context can be composed of multiple visual elements (e.g., wall patterns, ceiling, floor). The animal must learn to discriminate between different contexts to guide its behavior, such as licking for reward only in a specific context [25].
Data Analysis and Neural Decoding
The integration of VR with large-scale neural recording generates complex, high-dimensional datasets. Advanced analytical tools are required to extract meaningful patterns.
- Large-Scale Neural Recording: While the mouse performs the VR task, record neural activity using two-photon calcium imaging through the implanted GRIN lens, targeting thousands of neurons in regions like the hippocampus [25].
- Neural Data Visualization with Rastermap: A powerful method for visualizing and interpreting large-scale neural recordings is Rastermap. This algorithm sorts neurons along a one-dimensional axis based on their activity patterns, creating a raster plot that reveals population-wide coordination [45].
- Clustering: The activity profiles of all recorded neurons are first clustered, typically into 100 distinct clusters, using k-means.
- Similarity Matrix: An asymmetric similarity matrix between clusters is computed based on the peak cross-correlation of their activities at non-negative time lags.
- Optimization: The algorithm optimizes the ordering of clusters so that the neural similarity matrix resembles a predefined target matrix, which combines both global and local (sequential) structure.
- Visualization: The final sorted raster plot allows researchers to observe sequences of neural activity and responses to stimuli or behaviors clearly [45].
Diagram Title: Rastermap Analysis Pipeline
The Scientist's Toolkit: Essential Research Reagents and Materials
Successfully implementing this integrated approach requires a suite of specialized materials and reagents. The following table details the key components.
Table 2: Essential Research Reagents and Materials for Integrated VR-Neural Recording
| Item | Function/Description | Example/Note |
|---|---|---|
| Custom VR Software | Controls VR environment presentation, stimulus delivery, and data logging. | Flexible, lightweight software supporting high frame rates and trial-by-trial context switching [25]. |
| Modular VR Hardware | Displays the virtual environment and tracks the animal's locomotion. | Includes high-refresh-rate displays, a spherical treadmill, and optical sensors for tracking [25] [44]. |
| Calcium Indicator | Genetically encoded sensor for visualizing neural activity. | AAV2/9-CaMKII-GCaMP6f for expression in excitatory neurons [25]. |
| GRIN Lens | Miniaturized lens implanted in the brain for in vivo microscopy. | Provides an optical pathway for two-photon imaging of deep brain structures like the hippocampus [25]. |
| Two-Photon Microscope | For high-resolution, large-scale recording of calcium activity in behaving animals. | Enables recording from thousands of neurons simultaneously [25]. |
| Data Analysis Toolbox | Software for processing and visualizing neural population data. | Rastermap algorithm for sorting and visualizing neural activity patterns [45]. |
Discussion and Future Perspectives
The confluence of high-performance VR and large-scale neural recording represents a significant preclinical innovation. This synergy allows researchers to deconstruct complex behaviors, such as context recognition, and link them to specific neural representations. For instance, using these platforms, it has been shown that context recognition can be impaired by the exchange of contextual elements but remains intact with only partial cues, providing novel insights into the stability of neural representations [25].
The future of this field points toward even greater integration and sophistication. The application of artificial intelligence to adapt VR scenarios in real-time based on animal behavior is a promising direction [46]. Furthermore, the development of more advanced computational tools, like Rastermap, will be crucial for deciphering the ever-larger datasets generated by these technologies [45]. As these platforms become more accessible and user-friendly, they will empower more laboratories to undertake research that bridges complex behavior, neural circuit dynamics, and the evaluation of therapeutic interventions, ultimately accelerating progress in neuroscience and drug development.
Navigating the Virtual Frontier: Addressing Technical, Clinical, and Ethical Implementation Hurdles
Mitigating Cybersickness and Sensory Overstimulation in Vulnerable Populations
Cybersickness, a form of visually induced motion sickness, presents a significant barrier to the widespread adoption of virtual reality (VR) in behavioral neuroscience research and clinical applications. Characterized by symptoms including nausea, disorientation, and oculomotor strain, cybersickness arises from a sensory conflict between visual motion cues and vestibular system signals indicating physical stillness [47] [48]. Symptoms can be exacerbated in vulnerable populations, such as individuals with neurodevelopmental disorders or those undergoing neuropsychiatric treatment, who may also experience sensory overstimulation from immersive environments [31] [49]. As VR becomes increasingly integrated into behavioral phenotyping, therapeutic interventions, and drug development pipelines, establishing robust protocols to mitigate adverse effects is paramount for both ethical application and data reliability. This document outlines evidence-based application notes and experimental protocols to manage these risks, ensuring safer and more effective VR integration in research settings.
Quantitative Evidence and Symptom Measurement
A multi-method approach is recommended for quantifying cybersickness, as subjective self-reports and objective physiological measures capture distinct aspects of the experience. The following table summarizes the core measurement tools and their applications.
Table 1: Cybersickness and Presence Assessment Metrics
| Metric Category | Specific Tool / Measure | Primary Output/Measures | Application Context |
|---|---|---|---|
| Subjective Self-Report | Simulator Sickness Questionnaire (SSQ) [48] [50] | Scores for Nausea, Oculomotor, Disorientation, and Total Severity | Pre-/post-VR immersion assessment |
| Fast Motion Sickness Scale (FMS) [51] | Single score (0-20) for instantaneous discomfort | Continuous, in-VR rating of symptom intensity | |
| Igroup Presence Questionnaire (IPQ) [52] | Sense of "being there" in the virtual environment | Correlating presence with cybersickness severity | |
| Objective Physiological | Electroencephalography (EEG) [48] | Power in Delta (1-4 Hz), Theta (4-7 Hz), and Alpha (7-13 Hz) bands | Real-time, passive quantification of cybersickness correlate |
| Performance Metrics [53] | Task completion time, error rates, gait stability | Assessing functional impairment due to cybersickness |
Recent studies provide quantitative evidence on the efficacy of various mitigation strategies. The data below consolidates key findings for easy comparison.
Table 2: Efficacy of Cybersickness Mitigation Strategies
| Mitigation Strategy | Study Design | Key Quantitative Findings | Reported Effect Size / Statistics |
|---|---|---|---|
| Eye-Hand Coordination Task [47] | Within-subjects (N=47); post-VR ride task | Mitigation of nausea, vestibular, and oculomotor symptoms post-immersion | Significant increase in symptoms after ride; partial recovery after task (p<.05) |
| Pleasant Odor Imagery (OI) [51] | Within-subjects (N=30); boat simulation with OI | Decreased SSQ scores and increased immersion tolerance | Positive OI associated with longer tolerance and reduced symptom intensity |
| Locomotion Tunneling [50] | 5-day longitudinal (N=24 novice users) | Significant symptom reduction by Day 4; resurgence upon scene change | High tunneling most effective for highly susceptible users |
| Gaming Experience [47] | Correlation analysis within cohort | Proficiency in First-Person Shooter (FPS) games associated with reduced cybersickness | Gaming skill was a key predictor of lower symptom severity |
| EEG Correlates [48] | Correlation of EEG with self-report (joystick) | Delta-, Theta-, and Alpha-wave power increase correlated with self-reported sickness | Statistically significant correlation (p<.05) established |
Detailed Experimental Protocols
Protocol for Eye-Hand Coordination Mitigation
This protocol is designed to assess and alleviate cybersickness symptoms following intense VR exposure, leveraging sensory-motor recalibration [47].
1. Objective: To evaluate the efficacy of a structured eye-hand coordination task in reducing cybersickness symptoms after a sickness-inducing VR experience.
2. Materials:
- VR System: A fully immersive HMD (e.g., Meta Quest series).
- Cybersickness Induction Stimulus: A high-motion VR scenario (e.g., a 12-minute virtual rollercoaster ride).
- Mitigation Task: A virtual peg-in-hole task or a VR version of the Deary-Liewald Reaction Time (DLRT) task.
- Assessment Tools:
- Cybersickness in Virtual Reality Questionnaire (CSQ-VR) or Simulator Sickness Questionnaire (SSQ).
- Task performance metrics (e.g., completion time, error rate).
3. Procedure:
- Pre-Immersion Baseline: Administer the CSQ-VR/SSQ to establish a baseline symptom level.
- VR Immersion: Participants undergo the 12-minute rollercoaster ride to induce cybersickness.
- Post-Immersion Assessment (T1): Immediately after the ride, administer the CSQ-VR/SSQ inside the VR environment.
- Mitigation Task: Participants engage in the eye-hand coordination task for a set duration (e.g., 15 minutes). The task involves precise manipulation of virtual objects, such as placing pegs into corresponding holes.
- Post-Task Assessment (T2): After task completion, administer the CSQ-VR/SSQ again.
- Data Analysis: Compare scores across T1 and T2 using paired-sample t-tests or non-parametric equivalents. Analyze correlation between task performance metrics and symptom reduction.
4. Notes:
- This protocol is particularly suitable for studies involving novice VR users or populations with known vestibular sensitivity.
- The timing of assessment (inside VR vs. after exiting) is critical, as symptoms can decrease upon HMD removal [47].
Protocol for Odor Imagery Intervention
This protocol uses mental simulation of smells, a low-cost and accessible alternative to physical odor diffusion, to leverage emotional regulation for symptom relief [51].
1. Objective: To determine the impact of pleasant, intense Odor Imagery (OI) on the intensity and duration of VR-induced cybersickness.
2. Materials:
- VR System: HMD (e.g., HTC Vive) running a wave-based boat simulation or similar nauseogenic environment.
- OI Calibration Set: Seven pictures known to evoke strong odor images (e.g., rose, lavender, peppermint, strawberry).
- Assessment Tools:
- Fast Motion Sickness Scale (FMS).
- Simulator Sickness Questionnaire (SSQ).
- Vividness of Olfactory Imagery Questionnaire (fVOIQ) for screening.
3. Procedure:
- Screening & Calibration (Visit 1):
- Screen participants using the fVOIQ.
- Present the seven pictures and have participants rate the evoked mental image for pleasantness and intensity on a 1-4 scale.
- Select the picture with the highest combined score for the participant's main session.
- Baseline VR Immersion (Visit 1):
- Record baseline FMS and SSQ scores.
- Immerse the participant in the boat simulation for a maximum of 14 minutes with a neutral visual frame. Use FMS every minute; terminate if FMS ≥16.
- Administer SSQ post-immersion.
- OI Intervention VR Immersion (Visit 2, ≥6 months later):
- Record baseline FMS and SSQ.
- Immerse the participant in the same boat simulation, but with the individualized picture displayed at the center of the visual field.
- Instruct the participant to focus on the smell evoked by the picture.
- Monitor FMS every minute and terminate if FMS ≥16.
- Administer SSQ post-immersion.
- Data Analysis: Use Wilcoxon signed-rank tests to compare SSQ total scores and immersion duration between the control (Visit 1) and intervention (Visit 2) sessions.
4. Notes:
- This protocol is ideal for populations where additional hardware for odor diffusion is impractical or could act as a confounder.
- The mechanism is hypothesized to be the redirection of attentional resources and emotional regulation via pleasant sensory simulation [51].
Diagram 1: Odor Imagery Intervention Workflow. This flowchart outlines the two-visit protocol for assessing the impact of pleasant odor imagery on cybersickness.
The Scientist's Toolkit: Research Reagent Solutions
This section details essential materials and digital "reagents" for conducting cybersickness research.
Table 3: Essential Research Tools for Cybersickness Studies
| Tool / Solution | Specification / Example | Primary Function in Research |
|---|---|---|
| Head-Mounted Display (HMD) | Meta Quest 3, HTC Vive Pro | Presents the immersive virtual environment; key for generating sensory conflict. |
| Cybersickness Questionnaire | SSQ [48], CSQ-VR [47], VRSQ [52] | Gold-standard subjective metric for quantifying symptom severity pre- and post-immersion. |
| Real-Time Symptom Monitor | Fast Motion Sickness Scale (FMS) [51], Joystick Input [48] | Allows for continuous, in-VR assessment of symptom development without breaking immersion. |
| Physiological Data Acquisition | EEG Headset (e.g., Emotiv, NeuroScan) | Provides objective, neural correlates of cybersickness (increased Delta/Theta/Alpha power) [48]. |
| Eye-Hand Coordination Task | Virtual Peg-in-Hole, VR Deary-Liewald Task [47] | A standardized "treatment" activity used to promote sensory recalibration and mitigate symptoms post-exposure. |
| Locomotion Tunneling Software | Dynamic Field of View Restrictor [50] | A software-based mitigation technique that reduces peripheral optic flow during virtual movement. |
| Standardized Nauseogenic Stimulus | Virtual Rollercoaster [47], Boat on Waves [51] | A reliable, reproducible VR experience known to induce moderate cybersickness for experimental consistency. |
Integrated Workflow for Vulnerable Population Research
Vulnerable populations, such as individuals with ADHD, psychosis, or the elderly, require additional safeguards against sensory overstimulation and cybersickness, which can confound research results and cause distress [31] [49]. The following integrated workflow diagram provides a structured approach for safely incorporating VR into studies with these cohorts.
Diagram 2: Safe VR Integration for Vulnerable Populations. This workflow ensures a structured, ethical, and data-driven approach for conducting VR research with vulnerable cohorts.
Application Notes for Behavioral Neuroscience
- Individual Differences are Central: Susceptibility to cybersickness is highly variable. Key predictors include motion sickness history, gaming experience (FPS proficiency is protective), and static field dependence [47] [51]. Pre-screening with questionnaires like the MSSQ is essential for cohort stratification and statistical control.
- The Exit Transition is a Data Point: The act of exiting VR is a dynamic sensory adaptation process, not an instantaneous return to baseline [47] [53]. Symptoms, particularly nausea and vestibular discomfort, can decrease significantly upon HMD removal. Therefore, the timing of symptom assessment (inside VR vs. immediately after exit) must be standardized and reported, as it significantly impacts ratings.
- Pass-Through AR Carries VR Risks: Pass-through Augmented Reality (PT-AR), used in devices like the Apple Vision Pro and Meta Quest 3, is technologically a form of VR that presents a digital video stream of the real world. It can induce cybersickness-like symptoms (e.g., disorientation, loss of body coordination) that impair real-world task performance, blurring the lines between VR side effects and AR usability [53]. This is critical for studies planning to use PT-AR for "real-world" simulation.
- Longitudinal Adaptation is Possible: Novice users can adapt to VR over repeated exposures. One study showed significant cybersickness mitigation after four days of brief, controlled exposure, though symptoms can resurge with a change in virtual environment [50]. For longitudinal studies, this adaptation curve should be accounted for in the design, either as a covariate or a phenomenon of interest.
In behavioral neuroscience, the choice between immersive and non-immersive virtual reality (VR) systems represents a critical trade-off between experimental control and ecological validity. These technologies exist along a reality-virtuality continuum, with non-immersive systems (typically desktop-based) on one end and fully immersive head-mounted displays (HMDs) on the other [54]. Non-immersive VR relies primarily on standard monitors, mice, and other input devices, providing a cost-effective and highly controlled environment [55]. In contrast, immersive VR using HMDs fully engages the user's field of vision, creating a multisensory experience that generates a powerful psychological sense of "presence" - the feeling of actually being within the virtual environment [54] [30]. This sense of presence emerges from a complex interplay of technological capabilities and individual user factors [55]. For researchers investigating spatial learning, fear conditioning, cognitive rehabilitation, or other behavioral paradigms, understanding the comparative efficacy, methodological considerations, and practical limitations of these systems is fundamental to valid experimental design.
Comparative Efficacy: Quantitative Analysis Across Domains
Cognitive and Behavioral Outcomes
Recent meta-analyses and controlled studies reveal a complex landscape where the superiority of one system over another is highly task-dependent and influenced by methodological factors.
Table 1: Comparative Efficacy in Cognitive and Behavioral Domains
| Domain | Immersive VR (HMD) Findings | Non-Immersive VR Findings | Key References |
|---|---|---|---|
| Spatial Learning & Navigation | Mixed results; some studies show enhanced engagement but potential for poorer spatial recall when physical movement is restricted. | Can outperform HMD-VR in spatial recall (e.g., map drawing) when movement is limited, possibly due to better integration of idiothetic cues. | [55] |
| Memory & General Cognition | No direct memory performance enhancement over non-immersive VR in some studies, despite increased sense of presence. | Can be equally effective for memory tasks and general cognitive assessment, offering a stable, controlled environment. | [55] [56] |
| User Engagement & Experience | Consistently superior for sense of immersion, pleasantness, and intention to repeat similar experiences. Higher emotional response. | Lower ratings on immersion and pleasantness compared to HMD settings, but often higher usability and lower simulator sickness. | [55] [57] |
| Cognitive Training Outcomes | Semi-immersive VR found most effective for improving cognitive function in older adults with Mild Cognitive Impairment (MCI). All VR types beneficial versus control. | Effective for cognitive training, though may be less effective than semi-immersive systems for certain clinical populations. | [56] |
| Therapeutic Applications | High efficacy in exposure therapy for phobias and PTSD; superior distraction for pain management. | Less studied for therapeutic use, potentially less effective for interventions requiring a strong sense of "being there." | [58] [54] [30] |
Moderating Variables and Individual Differences
The efficacy of immersive versus non-immersive VR is not uniform across all users. Critical moderating variables must be considered during experimental design:
- Simulator Sickness: A significant barrier to HMD use, with studies indicating that women are more likely to experience simulator sickness in immersive VR [55]. Non-immersive systems generally present a lower risk [55].
- Age and Technological Familiarity: Older adults and those less familiar with technology often demonstrate better performance and comfort with non-immersive VR, whereas younger, tech-experienced users adapt more readily to HMDs [55].
- Gender and Task Context: Gender differences in immersion, presence, and performance are inconsistent and often depend on the specific VR context and task, necessitating careful sample characterization and potentially stratified analysis [55].
Experimental Protocols for Behavioral Neuroscience
Protocol: Spatial Learning and Memory Assessment
This protocol is adapted from studies comparing spatial memory in HMD and non-immersive VR environments, such as virtual museum or maze navigation [55].
Objective: To assess the impact of immersion level on spatial learning, memory recall, and user experience. Primary Dependent Variables: Accuracy of spatial recall (e.g., map drawing, object location), pathfinding efficiency, subjective ratings of presence and simulator sickness.
Methodology:
- Environment: Utilize an identical virtual environment (e.g., a digital twin of a museum or a complex maze) across both experimental conditions. The environment should contain multiple distinct landmarks and navigational challenges [55].
- Participants: Randomly assign participants to either the HMD group (e.g., HTC Vive Pro, Oculus Rift) or the non-immersive group (high-resolution monitor, mouse/keyboard). Sample size should be sufficiently powered (e.g., n>40 per group) to detect moderate effects, with stratification for age, gender, and gaming experience [55].
- Procedure:
- Familiarization Phase (5 mins): Allow participants to freely explore a neutral, non-test area to acclimate to the controls and the VR system.
- Encoding Phase (10 mins): Instruct participants to navigate from a start point to a designated target location within the virtual environment. The route should be repeatable.
- Recall Phase (5 mins): After a short distractor task, require participants to (a) draw a top-down map of the environment from memory, including key landmarks, and (b) verbally recall the sequence of landmarks and turns from the encoding phase.
- Data Collection:
- Behavioral: Record navigation paths, time to completion, and errors during the encoding phase. Score hand-drawn maps for accuracy of layout and landmark placement.
- Self-Report: Administer standardized questionnaires immediately post-task: The Igroup Presence Questionnaire (IPQ) and the Simulator Sickness Questionnaire (SSQ) [55].
Diagram 1: Spatial memory assessment workflow.
Protocol: VR Exposure Therapy (VRET) for Fear Conditioning and Extinction
This protocol outlines the use of immersive VR for studying fear extinction, a core process in exposure therapy for anxiety disorders and PTSD [30].
Objective: To create a controlled, replicable paradigm for fear conditioning and extinction within an immersive virtual environment, and to compare reactivity and extinction rates to those elicited by non-immersive systems or imaginal exposure. Primary Dependent Variables: Skin conductance response (SCR), heart rate variability (HRV), subjective units of distress (SUDs), and self-reported fear.
Methodology:
- Stimuli and Environment: Develop a neutral virtual environment (e.g., a series of rooms). Select a neutral stimulus (CS+, e.g., a specific virtual object or sound) to be paired with an aversive unconditional stimulus (US, e.g., a mild electric shock or a loud, unpleasant sound). A second, similar stimulus (CS-) is never paired with the US.
- Participants: Recruit participants with elevated fear sensitivity or specific phobias. Randomize to HMD, non-immersive, or an active control (e.g., imaginal exposure) group.
- Procedure:
- Acquisition (Day 1): In the virtual environment, repeatedly present the CS+ followed by the US. Present the CS- without the US. Measure psychophysiological responses (SCR, HRV) to both CS+ and CS-.
- Extinction (Day 2): 24 hours later, re-expose participants to the same virtual environment. Repeatedly present both the CS+ and CS- without the US.
- Recall Test (Day 7): One week later, conduct a final session to test for spontaneous recovery of the fear response.
- Data Collection:
- Continuously record SCR and HRV throughout all phases.
- After each CS presentation, collect SUDs ratings.
- Post-session, administer fear and presence questionnaires.
Diagram 2: VR fear conditioning and extinction protocol.
The Scientist's Toolkit: Research Reagent Solutions
Selecting the appropriate hardware and software is fundamental to operationalizing these protocols. The following table details key components for building a VR research laboratory.
Table 2: Essential Research Reagents and Hardware Solutions
| Item | Function/Application | Examples & Specifications |
|---|---|---|
| Head-Mounted Display (HMD) | Provides fully immersive VR experience. Critical for studies requiring high presence. | Meta Quest 3: Standalone, wireless, cost-effective (~$499). Ideal for large-scale deployments [59] [60]. HTC Vive Pro: High-fidelity, PC-connected. Preferred for medical/industrial simulations requiring precision [59] [57]. |
| Desktop VR Setup | Provides non-immersive VR experience. High-resolution monitor, standard computer mouse and keyboard. | High-Refresh-Rate Monitor (e.g., 144Hz+). Ensures smooth visual presentation and reduces lag, a key factor in user comfort and performance [55]. |
| VR Development Platform | Software environment for creating and customizing virtual experimental environments. | Unity 3D with VR SDKs. Widely used platform for creating custom research environments, as seen in recent cognitive training studies [57]. |
| Biometric Sensors | Objective measurement of physiological arousal and emotional response during VR tasks. | Skin Conductance Response (SCR) Amplifiers, Heart Rate (ECG) Monitors, Eye-Tracking (integrated into some HMDs). Essential for fear conditioning, pain, and engagement studies [30]. |
| Standardized Questionnaires | Quantifying subjective user experience, a critical dependent variable. | Igroup Presence Questionnaire (IPQ): Measures sense of presence [55]. Simulator Sickness Questionnaire (SSQ): Assesses VR-induced nausea and discomfort [55]. System Usability Scale (SUS): Evaluates perceived usability of the system [57]. |
The choice between immersive and non-immersive VR is not a matter of which is universally better, but which is more appropriate for the specific research question and context. Immersive HMD-based systems are unparalleled for inducing a strong sense of presence and are therefore the gold standard for research requiring high ecological validity, such as exposure therapy, spatial navigation in large environments, and studies of social interaction. However, they come with higher costs, greater technical complexity, and the risk of simulator sickness. Non-immersive, desktop-based systems offer superior control, higher usability, lower cost, and are less prone to induce adverse effects, making them ideal for cognitive tasks where precise input and stability are paramount, or for use with populations sensitive to simulator sickness.
Researchers should base their selection on a clear hypothesis regarding the role of "presence" in their paradigm. For the behavioral neuroscientist, immersive VR opens the door to studying brain and behavior in ecologically rich environments that were previously impossible to control in the laboratory, while non-immersive VR provides a robust and accessible tool for conducting highly standardized cognitive assessments. A combined, programmatic approach that utilizes both technologies as appropriate will likely yield the most comprehensive insights into brain function and behavior.
Ensuring Data Privacy and Security for Behavioral and Biometric Data
The integration of Virtual Reality (VR) into behavioral neuroscience research presents unprecedented opportunities for eliciting and measuring complex behavioral, physiological, and neural responses in ecologically valid environments. However, this convergence also introduces significant data privacy and security challenges, particularly concerning the collection, storage, and processing of highly sensitive behavioral and biometric data. These data types, which can include gaze patterns, kinematic movement data, electrodermal activity, heart rate variability, and neural activity patterns, often constitute personally identifiable information that can reveal intimate aspects of an individual's cognitive processes, emotional states, and health conditions. This document establishes essential protocols for ensuring the ethical integrity and security of VR-based research within a broader neuroscience framework, addressing critical gaps in current regulatory frameworks that have not fully adapted to the unique privacy implications of immersive technologies.
Data Classification and Risk Assessment
Table 1: Classification of Behavioral and Biometric Data Types in VR Research
| Data Category | Specific Data Types | Privacy Sensitivity Level | Identifiability Risk | Example in VR Context |
|---|---|---|---|---|
| Overt Behavioral Data | Head & hand tracking, controller inputs, task performance metrics | Medium | Low to Medium | Reaction times in a cognitive task; success/failure in a virtual maze [61]. |
| Covert Behavioral Data | Gaze tracking, pupillometry, facial expressions via embedded cameras | High | High | Recording of a subject's unconscious gaze patterns towards emotional stimuli [62]. |
| Physiological Biometric Data | Electroencephalography (EEG), Heart Rate (HR), Electrodermal Activity (EDA) | High | High | EEG recordings during a VR fear-conditioning paradigm; EDA during a social stress test [61]. |
| Neuroimaging Data | functional Magnetic Resonance Imaging (fMRI) data synchronized with VR | Very High | Very High | Brain activation maps collected while a participant navigates a virtual environment. |
| Self-Reported & Clinical Data | Demographic information, psychometric scale scores, clinical interviews | High | High | Pre- and post-intervention State-Trait Anxiety Inventory scores linked to VR exposure [62]. |
A rigorous data classification scheme is the foundation of any robust security protocol. The data types enumerated in Table 1 must be considered highly sensitive. The risk is amplified in VR research because behavioral and biometric data can be combined to create a unique and enduring biometric signature for an individual. For instance, gait patterns, eye-movement sequences, and neurophysiological responses are difficult to alter and can be used to re-identify individuals even from anonymized datasets. A risk assessment must be conducted prior to any study initiation, evaluating the potential for harm resulting from unauthorized access, data linkage, or accidental disclosure.
Experimental Protocols for Secure Data Handling
The following protocol outlines a secure methodology for a typical VR-integrated behavioral neuroscience experiment, such as one investigating anxiety or social cognition [62] [61].
Protocol: Secure VR Data Acquisition and Management
Objective: To securely collect, transfer, and store multimodal data (behavioral, biometric, and self-report) during a VR-based intervention, ensuring participant confidentiality and data integrity.
Materials:
- VR Headset with integrated eye-tracking and motion sensors
- Biometric acquisition system (e.g., EEG, EDA, HR monitor)
- Secure data server or encrypted workstation
- Cryptographic software for data encryption
- Pseudonymization script/tool
Detailed Methodology:
Pre-Session Setup and Participant Onboarding:
- Informed Consent: Obtain explicit, documented consent that specifically details the types of behavioral and biometric data to be collected, the purposes of collection, data storage durations, security measures, and potential risks of re-identification.
- Participant Pseudonymization: Assign a unique, random participant ID (e.g.,
VP_001) that is not derived from personal information. Maintain a secure, encrypted, and physically separate master key file that links the participant ID to their identifiable information (Name, contact details). Access to this master key must be strictly limited.
Secure Data Acquisition During VR Session:
- Data Labeling: All data streams (e.g., motion tracking
.csvfiles, EEG.edffiles, video recordings of behavior) must be tagged with the participant ID only—never with personal identifiers. - On-Device Security: If data is cached temporarily on the VR device or acquisition hardware, ensure that storage is encrypted. Data should be transferred to a secure central server at the earliest opportunity.
- Network Transfer: All data transmitted from the VR station and biometric equipment to the analysis server must occur over a secure, encrypted connection (e.g., SFTP, HTTPS, or a secure local network segment). Public Wi-Fi networks are strictly prohibited for data transfer.
- Data Labeling: All data streams (e.g., motion tracking
Post-Session Data Processing and Storage:
- Secure Storage: All research data must be stored on secure, access-controlled servers with robust encryption-at-rest. Cloud storage solutions must be vetted for compliance with relevant data protection regulations (e.g., GDPR, HIPAA).
- Data Anonymization for Sharing: For data intended for open science repositories or collaboration, apply a rigorous anonymization process. This involves removing all direct identifiers and applying techniques to reduce re-identification risk from the dataset itself (e.g., adding noise to precise kinematic data, down-sampling high-frequency biometric signals where scientifically permissible).
- Data Retention and Disposal: Establish a clear data retention policy aligned with ethical approval. Upon expiry of the retention period, data must be securely and irreversibly deleted using methods that render electronic data non-recoverable (e.g., physical destruction of storage media or using certified data-wiping software).
Signaling Pathway: Data Security and Access Control Logic
The following diagram visualizes the logical workflow and security checks for data access within a research protocol, ensuring that only authorized personnel can interact with sensitive datasets.
Data Access Authorization Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Resources for Secure VR and Biometric Research
| Item / Solution | Function in Research Protocol | Security & Privacy Consideration |
|---|---|---|
| VR Development Platform (e.g., Unity3D with XR plugin) | Presents experimental stimuli and records behavioral metrics (position, timing, input). | Must be configured to avoid logging personal data. All local data should be encrypted before transmission [62] [61]. |
| Biometric Acq. Software (e.g., EEGlab, AcqKnowledge) | Acquires, visualizes, and pre-processes raw physiological signals. | Software should support export of data in non-proprietary, anonymized formats. Access to the software and its data exports should be password-protected. |
| Secure Data Server | Centralized, encrypted storage for all research data. | Must be physically secure and accessible only via multi-factor authentication and role-based access controls (RBAC). |
| Pseudonymization Tool (e.g., custom Python/R script) | Automates the replacement of direct identifiers with a study ID. | The master lookup table must be stored separately from the research data, with the highest level of encryption and access control. |
| Data Encryption Software | Encrypts data both during transfer (in transit) and on disks (at rest). | Use strong, industry-standard protocols (e.g., AES-256 for data at rest, TLS 1.2+ for data in transit). |
| Ethics & Governance Framework (e.g., IRB-approved protocol) | Provides the legal and ethical foundation for data collection and handling. | Must explicitly address the unique risks of VR and biometric data, including long-term storage and potential future uses. |
Safeguarding data privacy and security is not merely a technical obstacle but a fundamental ethical imperative in VR-based behavioral neuroscience research. The protocols and guidelines outlined herein provide a foundational framework for researchers to navigate this complex landscape. By implementing rigorous data classification, secure experimental protocols, robust access controls, and transparent data management practices, the scientific community can harness the power of VR while upholding the highest standards of research integrity and participant trust. As the technology evolves, these protocols must be regularly reviewed and adapted to address emerging threats and ethical considerations.
Overcoming Cost Barriers and Enhancing Scalability in Low-Resource Settings
The integration of Virtual Reality (VR) into behavioral neuroscience research represents a paradigm shift, enabling unprecedented ecological validity in experimental design. VR technology creates immersive, computer-simulated environments that allow researchers to study complex behaviors and neural mechanisms in controlled laboratory settings that closely mimic real-world contexts [30] [63]. By utilizing head-mounted displays (HMDs) and motion-tracking technology, VR elicits a strong sense of presence – the psychological impression of "being there" in the virtual environment – which triggers realistic psychological and physiological responses in participants [30] [64]. This capability is particularly valuable for studying behaviors that are difficult to reliably elicit in traditional lab settings, such as specific fear responses, social interactions, or complex spatial navigation.
However, the implementation of VR in research faces significant challenges, particularly regarding cost barriers and scalability in resource-constrained settings. Despite proven efficacy for conditions ranging from anxiety disorders to psychosis [30] [65], VR remains largely confined to well-funded research institutions and specialized clinical settings [64]. A recent survey of 694 clinical psychologists and psychotherats revealed that only 10 reported using therapeutic VR in their practice, primarily citing financial constraints, lack of training, and technological limitations as barriers to adoption [64]. This application note addresses these challenges by providing practical strategies and detailed protocols for implementing VR research in low-resource settings without compromising scientific rigor.
Current Cost Barriers and Economic Considerations
Understanding the specific financial constraints limiting VR adoption is essential for developing effective implementation strategies. The primary barriers identified in recent research include initial equipment costs, ongoing maintenance, and specialized training requirements.
Table 1: Primary Barriers to VR Implementation in Research and Clinical Settings
| Barrier Category | Specific Challenges | Reported Impact |
|---|---|---|
| Financial Barriers | High initial equipment costs, unfavorable cost-benefit ratio, ongoing maintenance expenses | Cited as primary limitation by 76% of non-adopters [64] |
| Technological Barriers | Cybersickness concerns, hardware/software limitations, lack of technical support, rapid obsolescence | 42% of researchers reported technical immaturity as significant concern [64] |
| Professional Barriers | Lack of VR knowledge, insufficient training opportunities, limited implementation time | Only 14% of clinicians reported access to VR training programs [64] |
| Therapeutic/Research Barriers | Questions about clinical applicability, concerns about therapeutic relationship impact | 31% expressed concerns about applicability to their specific research populations [64] |
Despite these barriers, economic analyses demonstrate the potential long-term value of VR implementations. A cost-effectiveness study of VR-based cognitive behavioral therapy for paranoid ideation found an average incremental cost of €48,868 per quality-adjusted life year (QALY) over six months, with 99.98% of simulations showing improved QALYs [65]. When relevant baseline differences were considered in sensitivity analyses, costs decreased to €42,030 per QALY gained, demonstrating the economic viability of VR interventions [65].
Strategies for Cost-Effective VR Implementation
Hardware Selection and Scalability Solutions
Implementing VR in low-resource settings requires strategic hardware selection that balances performance with affordability. Commercial off-the-shelf (COTS) HMDs provide a viable alternative to specialized medical-grade equipment without sacrificing functionality.
Table 2: Cost-Saving Strategies for VR Implementation in Research
| Strategy | Implementation Approach | Potential Cost Reduction |
|---|---|---|
| Utilize Commercial HMDs | Deploy consumer-grade VR headsets (e.g., Meta Quest series) rather than specialized medical equipment | Can reduce hardware costs by 60-80% compared to specialized systems [64] |
| Open-Source Software | Utilize freely available development platforms (Unity3D, Unreal Engine) and open-source VR tools | Eliminates licensing fees totaling $5,000-20,000 annually for commercial packages |
| Modular Design | Develop reusable VR environments with customizable parameters for different research protocols | Reduces development costs by 30-50% through asset reuse across multiple studies |
| Collaborative Resource Sharing | Establish multi-institutional equipment sharing programs and collaborative development initiatives | Can decrease per-institution costs by 40-60% through shared resource pools |
The adoption of commercial HMDs has been facilitated by significant advancements in consumer VR technology. Modern systems like the Oculus Rift (released in 2016) and subsequent generations have dramatically enhanced the accessibility, affordability, and quality of VR hardware available to researchers [64]. These systems provide high-fidelity multisensory experiences with 360° fields of view and movement tracking sufficient for most research applications [64].
Protocol Standardization and Implementation Frameworks
Standardizing VR protocols across research settings enhances scalability while reducing implementation costs. The following workflow illustrates a structured approach to deploying VR research in resource-constrained environments:
Workflow Implementation Notes:
- Define Research Objectives: Clearly specify the behavioral domains and neural mechanisms under investigation to guide appropriate technology selection [63]
- Hardware Selection: Prioritize commercial HMDs with adequate technical specifications for the research questions while maintaining cost-effectiveness [64]
- Protocol Development: Adapt existing validated protocols when possible to reduce development costs and enhance comparability across studies [30] [63]
- Researcher Training: Utilize standardized training modules to ensure protocol fidelity while minimizing personnel costs [64]
Detailed Experimental Protocols
VR-Based Inhibitory Control Assessment (Adapted Simon and Flanker Tasks)
This protocol demonstrates how classical cognitive paradigms can be adapted to VR environments to enhance ecological validity while maintaining experimental control [63].
Background and Rationale: Inhibitory control is a core executive function typically assessed using computerized paradigms like the Simon and Flanker tasks. Traditional laboratory-based assessments have limited ecological validity, as they fail to capture the complexity of real-world environments where inhibitory control operates [63]. VR adaptations maintain the experimental control of laboratory settings while increasing the real-world relevance of assessments.
Materials and Equipment:
Table 3: Research Reagent Solutions for VR Inhibitory Control Assessment
| Item | Specifications | Research Function |
|---|---|---|
| VR Headset | Commercial HMD (e.g., Meta Quest 2/3) with minimum 90Hz refresh rate and 6DOF tracking | Presents immersive environments and tracks head movements for naturalistic interaction |
| Response Controller | Standard VR motion controllers with trigger input capability | Records participant responses with millisecond accuracy |
| Virtual Environment | Classroom or office setting with controlled lighting and minimal distractions | Provides ecologically valid context while maintaining experimental control |
| Stimulus Avatars | Human-like avatars with consistent appearance and animation parameters | Serves as target stimuli in adapted cognitive tasks to enhance ecological validity |
| Data Collection Software | Custom Unity or Unreal application with integrated data logging | Records response times, accuracy, and movement metrics for subsequent analysis |
Procedure:
- Environment Setup: Configure a virtual classroom environment containing a participant desk and two response zones located to the left and right sides
- Participant Orientation: Instruct participants to don the HMD and familiarize themselves with the virtual environment during a 5-minute acclimation period
- Task Instructions:
- For Simon Task: "Press the left controller trigger when the avatar appears on the left side, and the right trigger when the avatar appears on the right side, regardless of where the avatar is facing"
- For Flanker Task: "Press the trigger corresponding to the direction the central avatar is facing, while ignoring the direction of the flanking avatars"
- Stimulus Presentation:
- Present avatars in congruent (e.g., avatar on left side facing left) and incongruent (e.g., avatar on left side facing right) conditions
- Utilize randomized trial sequences with inter-trial intervals varying between 1,500-2,500ms to prevent anticipatory responses
- Data Collection:
- Record response accuracy and reaction times for each trial
- Calculate interference scores (difference between incongruent and congruent trials) as primary dependent measures
- Collect head movement and gaze direction data as potential covariates
Implementation Considerations for Low-Resource Settings:
- Utilize freely available avatar models from online repositories to reduce development costs
- Implement modular task designs that allow for easy modification of environmental parameters
- Employ open-source data analysis pipelines (e.g., Python scripts) to minimize software licensing costs
Virtual Reality Exposure Therapy (VRET) Protocol for Anxiety Research
This protocol adapts clinical VR exposure therapy for research applications investigating fear extinction and anxiety mechanisms [30].
Background and Rationale: VRET facilitates controlled exposure to fear-eliciting stimuli in a safe environment, making it particularly valuable for studying anxiety mechanisms and extinction learning [30]. The protocol leverages VR's capacity to create immersive, customizable environments that can be systematically manipulated to examine specific fear parameters.
Materials and Equipment:
- VR system with HMD capable of displaying high-fidelity environments
- Biometric monitoring equipment (heart rate, skin conductance) synchronized with VR presentation
- Customizable virtual environments graded according to fear hierarchy
- Stimulus presentation software with precise timing control
Procedure:
- Fear Assessment: Conduct pre-assessment to identify specific fear stimuli and establish individualized fear hierarchies
- Baseline Measurement: Record physiological and subjective anxiety responses to neutral virtual environments
- Gradual Exposure: Present fear-relevant virtual environments in ascending order of difficulty based on established fear hierarchy
- Response Monitoring: Continuously track subjective anxiety ratings (e.g., SUDS) and physiological indicators throughout exposure sessions
- Cognitive Restructuring: Incorporate cognitive challenging techniques within VR environment when applicable to research questions
- Extinction Testing: Assess fear responses to previously fear-eliciting virtual stimuli after completion of exposure protocol
Cost-Saving Adaptations:
- Utilize commercially available VR environments when appropriate for research objectives
- Implement automated exposure protocols with minimal researcher involvement for scalable implementation
- Develop reusable environment templates that can be modified for different fear stimuli
Technical Implementation and Troubleshooting
Successful implementation of VR research in low-resource settings requires proactive management of common technical challenges. The following table outlines frequent implementation barriers and evidence-based solutions:
Table 4: Technical Challenges and Solutions in Low-Resource VR Implementation
| Technical Challenge | Impact on Research | Recommended Solutions |
|---|---|---|
| Cybersickness | Participant attrition, data quality issues, ethical concerns | Limit session duration to 20-30 minutes; ensure stable frame rates (>90Hz); provide adequate acclimation periods [64] |
| Hardware Limitations | Reduced immersion, technical failures, data loss | Implement regular maintenance schedules; establish equipment sharing agreements; maintain backup systems for critical components [64] |
| Software Compatibility | Protocol inconsistencies, data integration challenges | Utilize cross-platform development tools; establish standardized file formats; implement rigorous quality assurance testing [30] |
| Technical Expertise Gaps | Protocol deviations, suboptimal implementation | Develop comprehensive training materials; establish mentoring programs with experienced VR researchers; create detailed implementation guides [64] |
Data Management and Analysis Considerations
Robust data management practices are essential for maintaining research quality in resource-constrained settings. VR research generates multimodal data streams including behavioral responses, physiological measures, and movement tracking data that require specialized handling approaches.
Standardized Data Collection:
- Implement automated data logging with timestamp synchronization across all measurement modalities
- Establish standardized naming conventions and file structures to facilitate data sharing and aggregation
- Create comprehensive data dictionaries documenting all variables and measurement parameters
Analysis Approaches:
- Utilize open-source analysis tools (e.g., R, Python) to minimize software costs while maintaining analytical flexibility
- Implement quality control checks for VR data, including movement artifact detection and trial validity assessment
- Apply appropriate statistical methods for nested data structures (e.g., trials within participants)
The integration of VR into behavioral neuroscience research need not be prohibitively expensive or technologically daunting. By implementing strategic approaches such as utilizing commercial hardware, developing modular protocols, and establishing collaborative networks, researchers can overcome traditional cost barriers while maintaining methodological rigor. The protocols outlined in this application note provide concrete templates for implementing VR research across diverse domains including cognitive assessment and fear extinction research.
Future advancements in VR technology will likely continue to reduce implementation barriers while expanding research capabilities. Particularly promising developments include the integration of artificial intelligence for adaptive virtual environments, biofeedback for closed-loop systems, and wireless streaming for enhanced mobility [30]. Additionally, the growing availability of open-source VR tools and shared resource repositories will further enhance accessibility for researchers working in low-resource settings.
As VR technology becomes increasingly sophisticated and affordable, its potential to transform behavioral neuroscience research continues to expand. By adopting the cost-saving strategies and standardized protocols outlined in this application note, researchers can harness the power of VR to investigate complex behaviors with unprecedented ecological validity, even within significant resource constraints.
Evidence and Efficacy: Validating VR Against Gold Standards and Across Modalities
Virtual Reality (VR) has emerged as a promising adjunct or alternative to conventional therapy (CT) in stroke motor rehabilitation. By providing immersive, engaging, and task-oriented environments, VR-based interventions promote motor learning and neuroplasticity. This application note synthesizes current evidence and provides detailed protocols for implementing VR therapy in research settings, focusing on its comparative effectiveness for upper and lower limb motor recovery post-stroke.
Quantitative Data Synthesis
Recent meta-analyses provide robust, quantitative evidence for the efficacy of VR interventions compared to conventional therapy.
Table 1: Effectiveness of VR on Upper Limb Motor Recovery
| Outcome Measure | Number of Studies (Participants) | Effect Size [95% CI] | P-value | Certainty of Evidence |
|---|---|---|---|---|
| Upper Limb Function (vs. Alternative Therapy) | 67 (2,830) | SMD 0.20 [0.12 to 0.28] | N/A | Low [66] |
| Upper Limb Function (in addition to Usual Care) | 21 (689) | SMD 0.42 [0.26 to 0.58] | N/A | Moderate [66] |
| Activities of Daily Living (ADL) | Multiple (N/A) | Favors VR | < 0.05 | Low to Moderate [67] |
SMD: Standardized Mean Difference. SMD of 0.2 represents a small effect, 0.5 a moderate effect [66].
Table 2: Effectiveness of VR on Lower Limb Motor Recovery
| Outcome Measure | Number of Studies (Participants) | Effect Size [95% CI] or Mean Difference | P-value | Certainty of Evidence |
|---|---|---|---|---|
| Balance (Berg Balance Scale) | 24 (768) | MD 3.29 [0.52 to 6.06] | 0.02 | N/A [68] |
| Mobility (Timed Up and Go test) | 24 (768) | MD -1.67 seconds [-2.89 to -0.46] | 0.007 | N/A [68] |
| Balance (Overall) | 24 (871) | SMD 0.26 [0.12 to 0.40] | N/A | Low [66] |
| Gait Speed (10-Meter Walk Test) | 24 (768) | MD -0.91 [-3.33 to 1.50] | 0.46 | N/A [68] |
| Gait Velocity | 14 (N/A) | No significant improvement | > 0.05 | N/A [67] |
MD: Mean Difference. A negative MD in TUG indicates improvement [68].
Key Moderating Factors:
- Therapy Dosage: Interventions with ≥20 sessions showed significantly greater improvements in balance (BBS improved by 5.14 points) and mobility (TUG reduced by 1.98 seconds) [68].
- Stroke Chronicity: Patients in the chronic phase (>6 months post-stroke) demonstrated greater improvements in balance from VR therapy compared to those in earlier phases [68].
- VR Modality: Semi-immersive VR (SI-VR) showed the most consistent motor benefits (88.24% of studies reporting improvements), followed by non-immersive (NI-VR) (66.67%) and immersive VR (I-VR) (50%) [69].
Experimental Protocols
Protocol for a Randomized Controlled Trial on VR for Lower Limb Rehabilitation
This protocol is adapted from a recent meta-analysis and systematic review [68].
Objective: To evaluate the effectiveness of a VR-based intervention versus conventional therapy in improving balance and mobility in adult stroke survivors.
Population (P):
- Inclusion: Adults (≥18 years) diagnosed with stroke (ischemic or hemorrhagic); stable medical condition; some degree of lower limb motor impairment.
- Exclusion: Other significant neurological diseases; severe cognitive impairment (e.g., Mini-Mental State Examination <24); uncontrolled cardiovascular issues; severe visual deficits [68] [70].
Intervention (I):
- Technology: Use a semi-immersive (SI-VR) or non-immersive (NI-VR) system. SI-VR may use large screens or projector-based systems, while NI-VR can employ a standard monitor or TV screen [69].
- Tasks: Implement goal-directed, functional tasks such as weight-shifting, virtual walking, obstacle avoidance, and reaching for objects in a 3D environment.
- Dosage: 20-30 sessions, 3-5 times per week, for 60-90 minutes per session (including conventional therapy components) [68].
- Progression: Gradually increase the difficulty of tasks by adjusting speed, complexity, and duration based on patient performance.
Control (C):
- Conventional Therapy (CT): Time-matched conventional physiotherapy and occupational therapy. This includes balance training, gait training, strength exercises, and functional task practice, without the use of VR [68] [67].
Outcomes (O):
- Primary:
- Balance: Berg Balance Scale (BBS)
- Mobility: Timed Up and Go (TUG) test
- Secondary:
- Gait: 10-Meter Walk Test (10MWT), stride length, step length
- Other: Functional Reach Test (FRT), Falls Efficacy Scale-International (FES-I) [68]
Workflow Diagram:
Protocol for Upper Limb VR Training with Neurostimulation
This protocol integrates VR with neuromodulation techniques, reflecting cutting-edge research [71].
Objective: To investigate the combined effect of non-invasive brain stimulation and VR training on upper limb motor function in chronic stroke patients.
Population: Chronic stroke patients (>6 months) with persistent upper limb paresis.
Intervention:
- Preparatory Neuromodulation (10-20 minutes):
- Apply Low-Intensity Focused Ultrasound (LIFUS) or transcranial Direct Current Stimulation (tDCS) to the ipsilesional motor cortex to increase cortical excitability [71].
- VR Motor Training (60 minutes):
Control:
- Sham Control: Identical procedure, but with sham (placebo) neuromodulation and/or conventional upper limb therapy without VR.
Outcomes:
- Primary: Fugl-Meyer Assessment for Upper Extremity (FMA-UE)
- Secondary: Action Research Arm Test (ARAT), Box and Block Test (BBT), Functional Independence Measure (FIM) [67].
Signaling Pathways and Neurophysiological Mechanisms
VR therapy facilitates motor recovery by promoting neuroplasticity through multiple, interconnected mechanisms.
Mechanism Diagram:
- Enhanced Engagement and Repetition: VR's engaging nature increases patient motivation and adherence, leading to a higher number of movement repetitions, a cornerstone of motor learning [66] [70].
- Multisensory Feedback and Neuroplasticity: VR provides intensive, task-specific practice with real-time visual, auditory, and sometimes haptic feedback. This rich sensory input stimulates cortical reorganization and strengthens neural connections in sensorimotor networks [68] [71].
- Cortical Reorganization: Evidence suggests VR can promote a shift from aberrant ipsilateral to contralateral sensorimotor cortex activation patterns, which is associated with locomotor recovery in stroke patients [68]. It can also help correct interhemispheric imbalance by increasing excitability in the affected hemisphere and reducing hyperexcitability in the unaffected hemisphere [71].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Assessments for VR Stroke Research
| Item Category | Specific Examples | Function / Rationale |
|---|---|---|
| VR Hardware Systems | Head-Mounted Displays (HMDs) for I-VR; Large projection screens for SI-VR; Standard monitors with gaming consoles (Nintendo Wii, Microsoft Kinect) for NI-VR [69]. | Creates the interactive and immersive environment for rehabilitation. The choice depends on the desired level of immersion and budget. |
| Software & Platforms | Custom-built rehabilitation tasks (e.g., object manipulation, virtual walking); Commercially available games adapted for therapy (e.g., from Wii Sports); Robotic interface control software [69] [67]. | Provides the specific exercises and activities for motor training. Must be adaptable to individual patient abilities. |
| Robotic & Haptic Devices | Robotic exoskeletons (e.g., for arm or hand); Haptic gloves; Arm supports [69]. | Provides active or passive assistance to movement, enables precise measurement of movement kinematics, and adds tactile feedback to enhance realism. |
| Primary Outcome Measures | Upper Limb: Fugl-Meyer Assessment (FMA), Action Research Arm Test (ARAT), Wolf Motor Function Test (WMFT) [67]. Lower Limb: Berg Balance Scale (BBS), Timed Up and Go (TUG) test, 10-Meter Walk Test (10MWT) [68]. | Gold-standard clinical scales to quantitatively assess motor function, balance, and mobility. |
| Secondary Outcome Measures | Functional Independence Measure (FIM), Barthel Index (BI), Modified Barthel Index (MBI) [70] [67]. | Assesses improvement in activities of daily living (ADLs) and overall functional independence. |
| Neurophysiological Tools | Electroencephalography (EEG), functional MRI (fMRI), Transcranial Magnetic Stimulation (TMS) [71] [72]. | Used in mechanistic studies to objectively measure changes in brain activity, connectivity, and cortical excitability induced by VR therapy. |
Within the broader thesis on virtual reality (VR) integration in behavioral neuroscience research, pilot studies represent a critical first step in the scientific pipeline. They are preliminary investigations designed to answer the question "Can this study be done?" rather than "Does this intervention work?" [73] [74]. The primary aim of a pilot study is to assess the feasibility, acceptability, and safety of the methods and procedures intended for a future, larger-scale efficacy trial [73] [75] [76]. In the context of developing novel VR-based interventions for conditions such as psychosis or ADHD, these studies are indispensable for refining complex protocols, ensuring technological usability, and verifying that the intervention is tolerable to the target clinical population [36] [31]. By focusing on these preliminary outcomes, researchers can identify and rectify methodological issues, optimize resource allocation, and ultimately increase the likelihood of success in definitive clinical trials.
Misconceptions about the role of pilot studies are common. A fundamental principle is that pilot studies are not designed to test hypotheses about intervention efficacy [73] [75]. Due to their small sample sizes, they are statistically underpowered for this purpose, and any estimates of effect size are unstable and potentially misleading if used for power calculations for a subsequent main trial [73] [74]. Similarly, while safety and tolerability can be monitored, the small scale of a pilot study means it can only detect very frequent or extreme adverse events; an absence of safety concerns in a pilot cannot be interpreted as definitive evidence of safety [73]. Properly conducted, a pilot study serves as a vital dress rehearsal, ensuring that every component of the research protocol, from recruitment to data collection, is viable before committing to a full-scale trial [75] [76].
Core Feasibility and Acceptability Outcomes
Feasibility and acceptability are multifaceted constructs that encompass the practical aspects of conducting the trial and the perception of the intervention from the stakeholder's perspective. Evaluating these domains involves a combination of quantitative metrics and qualitative feedback [77].
Table 1: Key Feasibility and Acceptability Assessment Domains
| Domain | Definition | Key Indicators & Metrics [75] [77] [76] |
|---|---|---|
| Recruitment Capability | The ability to identify and enroll eligible participants from the target population. | Number screened per month; number enrolled per month; proportion of eligible individuals who consent; time to enroll target sample size. |
| Retention & Adherence | The ability to keep participants in the study and their willingness to comply with the intervention protocol. | Retention rates for study measures; session attendance rates; homework completion; reasons for dropouts. |
| Intervention Fidelity | The degree to which the intervention is delivered as intended by the researchers. | Treatment-specific fidelity rates assessed by observer checklists; interventionist competence ratings. |
| Acceptability | The perception among stakeholders that the intervention is agreeable, palatable, or satisfactory. | Acceptability ratings via surveys; qualitative feedback on burden, satisfaction; treatment-specific preference ratings. |
| Data Collection Procedures | The feasibility and burden of the planned assessment methods. | Completion rates and times for assessments; proportion of planned data collected; perceived burden scores. |
The assessment of these domains should be guided by pre-specified, quantitative progression criteria that define the threshold for deeming the study feasible enough to proceed to a larger trial [75] [76]. For example, a study might set a benchmark that at least 70% of participants rate the intervention as acceptable (e.g., a score of 3 or above on a 5-point Likert scale) and that at least 70% attend a pre-defined minimum number of sessions [36] [73]. The use of mixed methods—integrating quantitative data (e.g., recruitment rates, survey scores) with qualitative data (e.g., open-ended interviews, focus groups)—is highly recommended to provide a comprehensive understanding of why certain protocols are or are not feasible and acceptable [77]. This integrated approach allows researchers to not only quantify a problem but also to understand its underlying causes and generate solutions.
Safety and Tolerability Assessment
In pilot studies, the assessment of safety and tolerability focuses on identifying any unforeseen adverse events (AEs) or unintended consequences associated with the experimental intervention or the research procedures themselves. This is particularly crucial when deploying emerging technologies like VR in clinical populations, where risks such as cybersickness, sensory overstimulation, or emotional dysregulation must be carefully monitored [31].
The protocol for safety monitoring should be established a priori and include:
- Systematic Reporting: All AEs, whether anticipated or unanticipated, should be documented using standardized forms, detailing their nature, severity, duration, and perceived relationship to the study intervention.
- Active Monitoring: Researchers should not rely solely on spontaneous reports from participants. Structured check-ins and standardized questionnaires (e.g., for cybersickness) should be used at regular intervals before, during, and after VR sessions [31].
- Oversight: A data safety monitoring board (DSMB) or an independent safety monitor may be appointed to review accumulating safety data, especially in higher-risk studies.
It is critical to recognize the limitations of pilot studies for safety assessment. Due to small sample sizes, pilot studies are only capable of detecting very common or severe adverse events [73]. Therefore, while the occurrence of serious AEs would likely halt further development, the absence of AEs in a pilot study cannot be interpreted as conclusive evidence of safety. Instead, the pilot study confirms that the methods for monitoring safety are feasible and that no major, frequent red flags emerged, justifying a larger trial with greater power to detect less common side effects [73] [75].
Experimental Protocol: A Hybrid VR-Neurofeedback Case Study
The following protocol is adapted from a published pilot study, "Hybrid," which integrates VR, electroencephalography (EEG)-based neurofeedback, and cognitive behavioral therapy (CBT) for treating auditory verbal hallucinations (AVHs) in psychosis [36] [78]. It serves as a model for a feasibility pilot study within a behavioral neuroscience context.
Study Aims and Design
- Primary Aim: To investigate the feasibility, acceptability, safety, and usability of the Hybrid intervention package.
- Secondary Aim: To explore treatment efficacy and the engagement of treatment targets (neural and psychological) [36] [78].
- Design: A pilot, unblinded, single-arm interventional study.
Participant Recruitment and Eligibility
- Sample Size: N=10, consistent with the small-scale nature of a pilot [36].
- Recruitment: Participants are recruited from clinical services in Melbourne, Australia. Feasibility indicators include the number approached, prescreened, eligible, and ultimately enrolled [36].
- Progression Criterion: A pre-defined benchmark (e.g., >70% of those deemed eligible consent to participate) would be set to judge recruitment feasibility for a future trial.
Intervention Protocol
Participants receive the Hybrid intervention weekly over 12 face-to-face sessions. Each session integrates three core components:
- VR-based Symptom Triggering: Individually tailored VR environments are used to progressively expose participants to scenarios that trigger their AVHs. This elicits "hot cognitions" (symptoms as they actively occur) rather than relying on abstract "cold cognitions" [36].
- EEG-Neurofeedback: During VR exposure, participants receive real-time visual feedback on their high-β band neural activity, a target linked to their symptoms. They are trained to develop mental strategies to downregulate this activity [36].
- Clinician-Delivered CBTp: A therapist is present throughout to support the participant, help them contextualize their experiences, and apply CBT for psychosis (CBTp) principles to the symptoms elicited in the VR environment [36].
Data Collection and Feasibility Measures
Data is collected at multiple time points (baseline, during each session, post-intervention) to assess the primary feasibility aims.
Table 2: Primary Feasibility and Acceptability Measures for the Hybrid Protocol
| Measure Type | Specific Tool / Metric | What It Assesses |
|---|---|---|
| Quantitative Feasibility | Consent rate; study completion rate; number of sessions attended; rate of successful EEG data acquisition. | Recruitment capability, retention, practicality of technical setup. |
| Quantitative Acceptability | User experience surveys on a 5-point Likert scale (post-intervention). Items cover acceptability, helpfulness, engagement, and perceived safety [36]. | Participant satisfaction and perceived burden. |
| Qualitative Feedback | Open-ended questions within the user experience survey or semi-structured interviews [36] [77]. | In-depth understanding of user perspectives, unexpected issues, suggestions for improvement. |
| Safety Monitoring | Adverse event reporting form; structured check for cybersickness/dizziness post-VR. | Tolerability and risk profile of the combined intervention. |
Analysis Plan
- Feasibility/Acceptability: Quantitative metrics (e.g., consent rates, Likert scale scores) are analyzed descriptively (e.g., means, percentages). The pre-set benchmark (e.g., ≥70% of participants rating acceptability as 3 or above) is used to determine success [36]. Qualitative data from open-ended questions are analyzed thematically to provide context and richness to the quantitative scores [77].
- Secondary Outcomes: Preliminary signals of efficacy (e.g., symptom change scores) are analyzed with extreme caution, focusing on confidence intervals and trends, not inferential statistics or p-values, as the study is not powered for these endpoints [73] [75].
The Scientist's Toolkit: Research Reagent Solutions
For researchers implementing complex, technology-driven pilot studies like the Hybrid protocol, specific tools and materials are essential. The following table details key "research reagents" and their functions in this context.
Table 3: Essential Research Materials for a VR-Neurofeedback Pilot Study
| Tool / Material | Specification / Example | Primary Function in the Protocol |
|---|---|---|
| VR Hardware & Software | Immersive head-mounted display (HMD); VR development platform (e.g., Unity, Unreal Engine). | Creates controlled, ecologically valid environments to safely elicit target symptoms (e.g., AVHs) for in-vivo therapeutic exposure [36] [79]. |
| EEG System | Research-grade EEG amplifier with multiple electrodes; real-time signal processing software. | Acquires neural data for neurofeedback; allows participants to learn self-regulation of brain activity linked to their symptoms [36]. |
| Neurofeedback Platform | Custom software for calculating power in specific frequency bands (e.g., high-β) and displaying it as real-time visual feedback. | Provides the interface for participants to volitionally modulate their brain activity, a core mechanism of the intervention [36]. |
| Feasibility & Acceptability Measures | Custom user experience surveys with 5-point Likert scales; semi-structured interview guides. | Quantifies and qualifies feasibility outcomes like acceptability, perceived safety, and engagement, which are the primary aims of the pilot [36] [77]. |
| Clinical Outcome Measures | Standardized scales for target symptoms (e.g., Psychotic Symptom Rating Scales, PSYRATS). | Assesses preliminary signals of clinical change for secondary/exploratory aims; not for definitive efficacy testing [36] [75]. |
| Data Integration Framework | Mixed methods research design plan; joint display templates for analysis. | Enables systematic integration of quantitative feasibility metrics with qualitative feedback to generate comprehensive insights [77]. |
A rigorously designed pilot study focused on feasibility, acceptability, and safety is the cornerstone of a successful research program, especially in innovative fields like VR-based behavioral neuroscience. By systematically evaluating recruitment, retention, protocol practicality, and stakeholder perceptions, researchers can de-risk the substantial investment required for a full-scale randomized controlled trial. The Hybrid protocol exemplifies how to structure such a study for a complex intervention, leveraging mixed methods to build a compelling case for future efficacy testing. Adherence to these principles ensures that subsequent trials are methodologically sound, ethically conducted, and have the highest possible chance of generating meaningful, translatable scientific evidence.
Virtual Reality (VR) simulators, augmented with Artificial Intelligence (AI), are revolutionizing the assessment of psychomotor skills by providing quantitative, objective, and high-fidelity metrics. This transformation is particularly critical in fields requiring high levels of manual dexterity and procedural competence, such as surgery, endoscopy, and clinical nursing. Traditional assessment methods often rely on subjective expert observation, which can be prone to bias and inconsistency [80]. VR simulators address these limitations by creating controlled, replicable, and safe environments where every aspect of a user's performance can be precisely measured [81] [1]. When integrated with AI-driven data analysis, these systems move beyond simple task completion times to provide a nuanced evaluation of skill, identifying subtle differences between novice and expert practitioners and enabling personalized feedback and training regimens [82] [80]. This document details the application of these technologies within behavioral neuroscience and clinical training research, providing specific protocols and analytical frameworks.
Quantitative Metrics for Psychomotor Assessment
VR simulators facilitate the extraction of robust, quantitative metrics that provide a multidimensional view of psychomotor performance. These metrics can be broadly categorized into those assessing motion efficiency, procedural precision, and cognitive load.
Core Performance Metrics
The following table summarizes key quantitative metrics used for objective assessment of psychomotor skills in VR environments.
Table 1: Key Quantitative Metrics for Psychomotor Skills Assessment in VR
| Metric Category | Specific Metric | Definition and Measurement | Research Findings |
|---|---|---|---|
| Motion Efficiency | Motion Path Length | Total 3D distance traveled by the instrument or hand controller [81]. | Shorter path lengths indicate more direct and efficient movements, characteristic of expert performance [81]. |
| Economy of Movement | A derivative metric evaluating the optimality of the movement path relative to an ideal trajectory. | Experts demonstrate significantly higher economy of movement than novices [81]. | |
| Motion Smoothness | Quantifies the fluidity of movement, often calculated from velocity and acceleration profiles [81]. | Jerky, irregular movements are associated with novice skill levels and higher cognitive load. | |
| Procedural Precision | Endpoint Accuracy | Precision in reaching a target location, measured as error from the center of the target [81]. | A fundamental measure of visuo-motor control and fine motor skills. |
| Time to Completion | Total time taken to complete a defined task or procedure. | While useful, this metric is most informative when combined with accuracy and quality measures [82]. | |
| Error Counts | Tally of specific errors, such as "wall strikes" in endoscopic navigation or incorrect instrument force [82] [80]. | Novice endoscopists exhibited a significantly higher number of wall strikes compared to experienced practitioners [82]. | |
| Task-Specific Success | Success Rate | Percentage of a task completed correctly (e.g., "balloons popped" in a targeting task) [82]. | Intermediate endoscopists popped significantly more balloons per trial than novices (P = 0.001) [82]. |
The Impact of Experimental Factors on Performance
Research shows that performance metrics are influenced by controllable experimental or procedural factors. A study on surgical dexterity systematically evaluated these factors using VR simulations [81].
Table 2: Impact of Experimental Factors on Surgical Dexterity Metrics in VR [81]
| Experimental Factor | Impact on Quantitative Metrics |
|---|---|
| Posture | Seated posture significantly improved surgical precision and efficiency compared to a standing posture. |
| Handedness | Using the dominant hand resulted in markedly better performance in both endpoint accuracy and motion path efficiency. |
| Visual Magnification | Enhanced visual magnification (10x) led to superior precision and smoother movements compared to normal (1x) view. |
Application Notes & Experimental Protocols
This section provides detailed methodologies for implementing VR and AI in psychomotor skills research, adaptable for various clinical and neuroscience contexts.
Protocol 1: Differentiating Skill Levels in Psychomotor Tasks
This protocol is designed to validate a VR simulator's ability to distinguish between novice and expert performance.
1. Objective: To quantitatively assess and differentiate the psychomotor skills of novice and experienced practitioners using a VR simulator. 2. Background: Previous research has successfully used the GI Mentor II simulator to show that intermediately experienced endoscopists pop significantly more balloons in a targeting task (P = 0.001) and have fewer wall strikes than novices [82]. 3. Materials & Reagents: Table 3: Research Reagent Solutions for Skill Differentiation Protocol
| Item | Function in Experiment |
|---|---|
| VR Simulator (e.g., GI Mentor II, Sensable PHANTOM Omni) | Provides the virtual environment and task; captures raw kinematic data [82] [81]. |
| Head-Mounted Display (HMD) or 3D Monitor | Creates an immersive visual experience for the user [81]. |
| Haptic Feedback Device | Provides realistic tactile resistance and force feedback during interactions [81]. |
| Data Acquisition Software (e.g., C++ with OpenHaptics) | Records time-series data of instrument position, rotation, velocity, and events [81]. |
4. Experimental Workflow: The following diagram outlines the key stages of the experimental protocol.
Diagram 1: Experimental workflow for skill-level differentiation studies.
5. Data Analysis:
- Preprocessing: Filter and segment motion data into dynamic (movement towards target) and static (holding at target) phases for granular analysis [81].
- Feature Extraction: Calculate metrics from Table 1 for each participant and trial.
- Statistical Testing: Use non-parametric tests (e.g., Mann-Whitney U) to compare group means for each metric, as the data may not be normally distributed [82].
Protocol 2: Evaluating the Efficacy of VR-Assisted Learning
This protocol measures the impact of VR-based training interventions on psychomotor skill acquisition, using a controlled study design.
1. Objective: To evaluate the effect of VR-assisted learning on the acquisition and retention of psychomotor competence compared to traditional simulation methods. 2. Background: A quasi-experimental study with midwifery students demonstrated that VR-assisted training led to significantly higher psychomotor competence in Leopold's Maneuvers and maternal assessment compared to a control group trained with traditional methods (p = 0.000) [83]. 3. Materials & Reagents: In addition to the items in Table 3, this protocol requires:
- Control Group Materials: Traditional training tools (e.g., high-fidelity manikins, physical assessment checklists).
- Satisfaction Questionnaire: A tool to measure user acceptance and perceived utility of the VR training [83]. 4. Experimental Workflow:
Diagram 2: Controlled trial workflow for evaluating VR learning efficacy.
5. Data Analysis:
- Compare pre-test and post-test scores within and between groups using ANOVA or t-tests.
- Analyze long-term skill retention and transfer to real-world clinical settings during the follow-up assessment [83].
- Correlate system usability scores (e.g., System Usability Scale) with performance improvement.
Protocol 3: Optimizing Training Schedules with Spaced Learning
This protocol investigates how the distribution of practice sessions impacts the rate and robustness of psychomotor skill acquisition.
1. Objective: To determine the optimal spacing interval for VR simulator training to maximize surgical psychomotor skill acquisition. 2. Background: A systematic review found that spaced training across multiple sessions was more effective for skill acquisition than a single, massed training session. Spacing across consecutive days appeared particularly effective [84]. 3. Experimental Workflow:
- Group Division: Divide participants into groups following different training schedules (e.g., massed training vs. spacing over days vs. spacing over weeks).
- Standardized Task: All groups practice the same VR task for the same total duration.
- Assessment: Administer skill assessments at the end of training and after a delay to measure retention.
AI-Driven Data Analysis and Assessment Frameworks
AI and computational models are crucial for transforming raw VR data into objective assessments.
The Weighted Possibilistic Assessment Algorithm
A sophisticated AI approach for online assessment uses a Weighted Possibilistic method based on fuzzy measures [80]. This system compares a trainee's performance data against pre-defined expert models, accounting for the varying importance of different performance variables.
Logical Workflow of the AI Assessor:
Diagram 3: AI-powered assessment using a Weighted Possibilistic approach.
This method provides an interval-based score, offering a more nuanced assessment than a simple pass/fail. It has demonstrated high accuracy, correctly classifying procedures with over 90% accuracy in a bone marrow harvest simulation [80].
Data Processing and Feature Extraction Pipeline
The raw data from VR sensors must be processed to extract meaningful features.
1. Data Acquisition: High-precision devices (e.g., Sensable PHANTOM Omni) capture 3D positional data of instruments at high frequency [81]. 2. Preprocessing:
- Filtering: Remove high-frequency noise from motion signals.
- Segmentation: Divide continuous data streams into logical chunks (e.g., using a sliding window) corresponding to specific task phases [81]. 3. Feature Extraction: Calculate the metrics outlined in Table 1 from the segmented data for input into AI assessment models.
The integration of VR simulators with AI-driven analytics provides an unprecedented capability for the objective, quantitative, and scalable assessment of psychomotor skills. The protocols and frameworks detailed herein offer a roadmap for researchers in behavioral neuroscience and clinical training to rigorously evaluate skill acquisition, differentiate competency levels, and optimize training paradigms. By leveraging quantitative metrics such as motion path efficiency and endpoint accuracy, and employing sophisticated AI models like the Weighted Possibilistic approach, the field can move towards standardized, evidence-based assessment that enhances both professional training and patient safety.
Virtual reality (VR) is emerging as a revolutionary tool in mental health, offering new approaches for treating psychiatric disorders within behavioral neuroscience research frameworks [30]. Its ability to create immersive, controlled environments allows patients to face psychological challenges safely, facilitating novel investigation and therapeutic modulation of cognitive and affective processes [85] [86]. This integration of VR technology enables researchers to study neural, physiological, and cognitive bases of human behavior with enhanced ecological validity compared to traditional laboratory settings [86]. Technological advancements are making VR more accessible to research institutions, allowing collection of behavioral data typically inaccessible in conventional paradigms [86]. This article synthesizes current meta-analytic evidence for VR's therapeutic efficacy across mental health disorders and provides detailed protocols for its implementation in behavioral neuroscience research.
Quantitative Synthesis of VR Efficacy Across Disorders
Recent meta-analyses demonstrate VR's significant therapeutic potential across multiple psychiatric conditions. The synthesized evidence below presents standardized effect sizes from large-scale quantitative reviews.
Table 1: Meta-Analytic Effect Sizes for VR Interventions Across Disorders
| Disorder | Intervention Type | Effect Size | Outcome Measures | Evidence Strength |
|---|---|---|---|---|
| Anxiety Disorders (General) | VR Therapy | SMD = -0.95 [-1.22, -0.69] [87] | Anxiety symptoms and levels | Strong [87] [88] |
| Specific Phobias | VRET | Significant effects vs. waitlist; equivalent to in-vivo exposure [88] | Fear, avoidance behaviors | Very Strong [88] |
| Social Anxiety Disorder | VRET/CBT | g = 0.82 vs. passive controls [88] | Social anxiety symptoms | Strong [88] |
| PTSD | VRET | g ≈ 0.62 vs. waitlist [88] | PTSD symptoms, depressive comorbidity | Moderate [30] [88] |
| Aggression/Conduct Problems | VR Social-Emotional Training | g = -0.47 (self-reported aggression) [89] | Aggression, anger, impulsiveness | Moderate [89] [61] |
| Depression | VR-CBT | g = 0.73 [0.25, 1.21] [88] | Depressive symptoms | Limited but Promising [88] [90] |
| ADHD | VR Attention Training | SMD = -0.33 (attention deficits) [88] | Sustained attention, vigilance | Promising [88] [90] |
A 2025 meta-analysis of 33 randomized controlled trials (RCTs) involving 3,182 participants with anxiety disorders demonstrated that VR therapy significantly improved anxiety symptoms compared to conventional interventions [87]. The substantial effect size (SMD = -0.95) highlights VR's robust potential for anxiety-related conditions. Similar large effects have been documented for specific phobias, with VR exposure therapy (VRET) showing equivalent efficacy to traditional in-vivo exposure but with significantly higher acceptance and lower dropout rates (3% vs. 27%) [88].
For conditions like PTSD, VR shows moderate effects compared to waitlist controls but comparable efficacy to other active therapies (g = 0.25) [88]. In externalizing disorders, VR interventions significantly reduce observer-reported aggression (g = -0.27), self-reported aggression (g = -0.47), anger (g = -0.74), and impulsiveness (g = -0.47) [89]. The overall weighted mean difference favors VR interventions over control conditions (g = -1.05) [89], though heterogeneity in interventions and samples necessitates careful implementation.
Detailed Experimental Protocols
Protocol 1: VR Exposure Therapy (VRET) for Anxiety Disorders
Application Note: VRET facilitates controlled, gradual exposure to anxiety-provoking stimuli while practicing coping mechanisms in immersive environments [30]. This protocol is adapted from multiple RCTs for specific phobias and social anxiety [88].
Equipment Setup:
- Hardware: Standalone VR headset (e.g., Oculus Quest 2, HTC Vive) with head-mounted display (HMD) and integrated headphones
- Software: Customizable VR environments with parameter controls for stimulus intensity, duration, and complexity
- Safety: Comfortable seating, adequate physical space, emergency stop mechanism
Session Structure:
- Pre-session Assessment (10 minutes): Administer standardized anxiety measures (e.g., SUDS, BAI) and check equipment function
- Psychoeducation (5 minutes): Explain VRET rationale, exposure principles, and subjective units of distress (SUDS) scale
- VR Exposure (30-45 minutes):
- Begin with least anxiety-provoking scenario (e.g., small spider at distance for arachnophobia)
- Gradually increase stimulus intensity based on patient's SUDS ratings (target 70-80% anxiety)
- Implement exposure until habituation occurs (≥50% reduction in SUDS)
- Incorporate cognitive restructuring during exposure
- Post-session Processing (10 minutes): Discuss learning, coping effectiveness, and real-world application
- Homework Assignment: Practice skills in real-world settings using response prevention
Dosage Parameters:
- Effective with either extended sessions (45-180 minutes) or 8-12 shorter sessions (15+ minutes each) [88]
- Typical treatment course: 4-12 weekly sessions depending on disorder severity
- Between-session practice recommended to generalize learning
Modification Guidelines:
- For social anxiety: Adjust audience size, responsiveness, and social scrutiny levels
- For panic disorder/agoraphobia: Modify physical space complexity, exit accessibility, and crowd density
- For PTSD: Customize trauma-relevant stimuli with careful titration to avoid retraumatization
Protocol 2: VR Social-Emotional Learning for Conduct Problems
Application Note: This protocol, based on the Impact VR program, targets underlying mechanisms of conduct disorder rather than surface behaviors [61]. It focuses on retraining emotional recognition, empathy, and social cue interpretation through gamified learning.
Equipment Setup:
- Hardware: Standalone VR headset with hand tracking capabilities
- Software: Impact VR or similar social-emotional learning platform with scenario customization
- Environment: Clinical setting or controlled space allowing physical movement
Session Structure (25 minutes/session, 4 weekly sessions):
- Facial Expression Recognition (5 minutes): Identify emotions from avatars with varying intensity levels
- Emotional Trigger Identification (5 minutes): Recognize personal and contextual triggers in social scenarios
- Problem-Solving Simulations (10 minutes): Navigate interactive stories requiring empathy and perspective-taking
- Strategy Development (5 minutes): Practice and refine coping strategies for challenging social situations
Therapeutic Targets:
- Emotion Processing: Enhanced recognition of fear, anger, and sadness in facial expressions
- Empathy Building: Perspective-taking through role-reversal exercises
- Social Cognition: Accurate interpretation of ambiguous social cues
- Impulse Control: Pausing between trigger and response implementation
Clinical Implementation:
- Can be administered with minimal staff supervision after initial setup
- Particularly effective for youth with callous-unemotional traits who are resistant to traditional therapy [61]
- Appropriate for clinical, educational, and juvenile justice settings
Protocol 3: VR-Based Mindfulness for Transdiagnostic Applications
Application Note: VR mindfulness addresses limitations of traditional delivery, including geographic barriers, time constraints, and participant dropout (15-30% in conventional programs) [91]. The immersive nature enhances presence and attention regulation while reducing external distractions.
Equipment Setup:
- Hardware: VR headset with comfortable fit for meditation postures
- Software: Immersive mindfulness applications with biofeedback capability
- Environment: Quiet space conducive to relaxation exercises
Session Structure (20-30 minutes):
- Pre-session Baseline (2 minutes): Collect resting physiological measures (heart rate, respiration)
- Environment Immersion (3 minutes): Gradual transition to serene virtual setting (e.g., beach, forest)
- Focused Attention Meditation (10-15 minutes): Breath awareness with visual/anchor support
- Body Scan (5 minutes): Systematic attention movement through virtual embodiment
- Transition Period (3 minutes): Preparation for return to physical environment
Theoretical Framework:
- PAC Model: Presence-Attention-Compassion mechanisms enhance traditional mindfulness [91]
- Embodied Cognition: Multisensory immersion facilitates more visceral emotional engagement
Clinical Applications:
- Stress Reduction: Significant improvements in perceived stress compared to traditional mindfulness
- Anxiety/Depression: Complements standard CBT protocols
- Pain Management: Enhanced distraction and coping skill development
Visualizing VR Therapeutic Mechanisms
The following diagrams illustrate key therapeutic mechanisms and experimental workflows in VR-based interventions.
VR Therapy Mechanism Diagram | This diagram illustrates the primary therapeutic mechanisms through which VR interventions achieve clinical effects, including presence induction, controlled exposure, and emotional engagement.
VR Research Protocol Workflow | This workflow diagram outlines standardized procedures for implementing and evaluating VR-based therapeutic interventions in clinical research contexts.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Materials for VR Behavioral Neuroscience
| Category | Specific Items | Research Function | Implementation Notes |
|---|---|---|---|
| Hardware Platforms | Oculus Quest系列, HTC Vive, PlayStation VR | Create immersive environments with head-mounted displays (HMDs) | Standalone devices preferred for clinical settings; PC-connected for high-fidelity research [30] |
| Biofeedback Integration | EEG headsets, ECG sensors, GSR devices, Eye-tracking | Collect physiological data synchronized with VR experience | Enable real-time adaptation and objective outcome measurement [30] [92] |
| Software Platforms | Unity 3D, Unreal Engine, specialized clinical VR applications | Develop and customize therapeutic environments | Balance customization capability with clinical validation [88] |
| Assessment Tools | HAMA, SAS, BAI, CAPS, BDI | Standardized outcome measurement pre/post intervention | Ensure psychometric validity and comparability across studies [87] |
| Safety Equipment | Stable chairs, clear physical space, emergency stop mechanisms | Prevent cybersickness and ensure physical safety | Particularly important for vulnerable populations [30] |
Successful implementation requires careful consideration of both technical specifications and clinical requirements. The hardware must balance immersion with comfort to minimize cybersickness, which can impact adherence and data quality [30]. Software platforms should allow sufficient customization to implement individualized exposure hierarchies while maintaining treatment fidelity. Integrated biofeedback systems enable investigation of physiological mechanisms underlying therapeutic change, providing valuable biomarkers for treatment response [92].
The meta-analytic evidence synthesized in this review demonstrates VR's robust therapeutic potential across multiple psychiatric disorders, with particularly strong support for anxiety conditions, specific phobias, and emerging promise for externalizing disorders. The standardized protocols and visualization tools provided offer researchers practical frameworks for implementing VR interventions within behavioral neuroscience paradigms. Future directions should focus on large-scale RCTs with longer follow-up periods, mechanistic studies examining neural correlates of VR-induced change, and development of standardized reporting guidelines for VR-based research [30] [88]. As VR technology continues to evolve and become more accessible, its integration into behavioral neuroscience research promises to advance both theoretical understanding and clinical application for diverse mental health conditions.
Conclusion
The integration of VR into behavioral neuroscience marks a paradigm shift, moving research and therapy from abstract settings into dynamic, ecologically valid environments. The key takeaways confirm VR's capacity to induce measurable neuroplasticity, its efficacy in treating conditions from psychosis to motor impairments, and its growing value in preclinical drug discovery pipelines through platforms like eBrain. Future directions must focus on developing standardized clinical protocols, creating more affordable and accessible systems, and establishing robust ethical frameworks. The convergence of VR with artificial intelligence and molecular imaging promises a new era of personalized, data-driven interventions, solidifying VR's role as an indispensable tool for the next generation of neuroscience research and clinical translation.
References
- 1. Naturalistic neuroscience and virtual reality [https://www.frontiersin.org/journals/systems-neuroscience/articles/10.3389/fnsys.2022.896251/full]
- 2. Exploring the impact of virtual reality on presence: findings ... [https://www.frontiersin.org/journals/education/articles/10.3389/feduc.2025.1560626/full]
- 3. Neuroscience of Virtual Reality: From Virtual Exposure to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6354552/]
- 4. Assessment of Spatial Presence Experiences and Symptoms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12194036/]
- 5. Color contrast - Accessibility - MDN Web Docs - Mozilla [https://developer.mozilla.org/en-US/docs/Web/Accessibility/Guides/Understanding_WCAG/Perceivable/Color_contrast]
- 6. Elements must meet minimum color contrast ratio thresholds [https://dequeuniversity.com/rules/axe/4.8/color-contrast]
- 7. Confusing virtual reality with reality – An experimental study [https://www.sciencedirect.com/science/article/pii/S2589004225009162]
- 8. Considerations and practical protocols for using virtual ... [https://link.springer.com/article/10.3758/s13428-021-01543-3]
- 9. JMIR Research - Integrating Virtual Reality, Neurofeedback... Protocols [https://www.researchprotocols.org/2025/1/e63405]
- 10. Virtual reality in behavioral and... | Nature neuroscience Neuroscience [https://www.nature.com/articles/nn948?error=cookies_not_supported&code=fbbd00bd-294f-4288-9edc-d2c28df511a8]
- 11. Visual feedback manipulation in virtual reality alters ... [https://www.nature.com/articles/s41598-025-08094-z]
- 12. Frontiers | Impact of Visual Distractors in Virtual Reality Environments... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1705660/abstract]
- 13. Setup and procedures for the VR experiments [https://bio-protocol.org/exchange/minidetail?id=6123665&type=30]
- 14. Assessing virtual reality presence through physiological ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1530770/full]
- 15. Recommendations for Methodology of Virtual Reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6374734/]
- 16. Review Virtual reality modulating dynamics of neuroplasticity [https://www.sciencedirect.com/science/article/abs/pii/S0306452224007474]
- 17. Virtual Reality for Neurorehabilitation: Mechanisms, Modalities ... [https://currents.neurocriticalcare.org/Leading-Insights/Article/virtual-reality-for-neurorehabilitation-mechanisms-modalities-and-clinical-applications]
- 18. Neuroplasticity in cognitive and psychological mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7047599/]
- 19. Effects of Virtual Reality Cognitive Training on Neuroplasticity [https://pmc.ncbi.nlm.nih.gov/articles/PMC10740852/]
- 20. Comparative effects of sensory motor and virtual reality ... [https://www.nature.com/articles/s41598-025-05048-3]
- 21. The Potential of Virtual Reality for Inducing Neuroplasticity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7341422/]
- 22. Context-Dependent Memory - an overview [https://www.sciencedirect.com/topics/neuroscience/context-dependent-memory]
- 23. A Bibliometric Study of the Evidence About Applying Virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399854/]
- 24. From Mazes to Automation: Modernizing Working Memory ... [https://www.sciencedirect.com/science/article/abs/pii/S0166432825003936]
- 25. A Virtual Reality Platform for Context-Dependent Cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10170012/]
- 26. A Virtual Reality Platform for Context-Dependent Cognitive ... [http://english.cebsit.cas.cn/lab/xuchun/news/202211/t20221110_323378.html]
- 27. Improved spatial memory for physical versus virtual navigation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12247154/]
- 28. Enhancing learning and retention with distinctive virtual ... [https://www.nature.com/articles/s41539-022-00147-6]
- 29. Virtual reality as a clinical tool in mental health research and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7366939/]
- 30. Virtual Reality: Challenges and Perspectives in Mental Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593772/]
- 31. Integrating virtual reality into ADHD therapy [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1591504/full]
- 32. Combining VR with electroencephalography as a frontier of ... [https://www.sciencedirect.com/science/article/pii/S2666998624002680]
- 33. EEG and Virtual Reality: Building The Neuroadaptive Future [https://www.bitbrain.com/blog/eeg-virtual-reality]
- 34. The Efficacy of Virtual Reality-Based EEG Neurofeedback ... [https://link.springer.com/article/10.1007/s10484-025-09730-0]
- 35. Effects of virtual reality-based feedback on neurofeedback ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2022.952261/full]
- 36. Integrating Virtual Reality, Neurofeedback, and Cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12000783/]
- 37. The influence of time and visualization on neurofeedback ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1476264/full]
- 38. Current virtual reality-based rehabilitation interventions in ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2024.1441615/full]
- 39. Combined Immersive and Nonimmersive Virtual Reality ... [https://www.jmir.org/2025/1/e73142]
- 40. Combined Immersive and Nonimmersive Virtual Reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12513685/]
- 41. Virtual reality and cognitive function rehabilitation after ... [https://pubmed.ncbi.nlm.nih.gov/40208002/]
- 42. The effectiveness of digital cognitive intervention in ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1651443/full]
- 43. Virtual reality-based rehabilitation experience of stroke survivors [https://pmc.ncbi.nlm.nih.gov/articles/PMC12330812/]
- 44. An Immersive Virtual Reality System for Rodents in ... [https://link.springer.com/article/10.1007/s11633-021-1307-y]
- 45. Rastermap: a discovery method for neural population ... [https://www.nature.com/articles/s41593-024-01783-4]
- 46. Virtual Reality Animal Behavioral Studies New Frontier [https://jivagorolo.com/2025/11/01/virtual-reality-animal-behavioral-studies-new-frontier/]
- 47. Mitigating Cybersickness in Virtual Reality: Impact of Eye– ... [https://www.mdpi.com/2813-2084/3/4/27]
- 48. Quantifying VR cybersickness using EEG | Virtual Reality [https://link.springer.com/article/10.1007/s10055-021-00517-2]
- 49. Exploring the potential of virtual reality (VR) in mental ... [https://link.springer.com/article/10.1007/s10055-025-01181-6]
- 50. How Long Does It Take to Alleviate Discomfort? A ... [https://arxiv.org/html/2508.01070v1]
- 51. Is it all in your head? Reducing virtual reality induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11896048/]
- 52. Understanding Cybersickness and Presence in Seated VR [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027998/]
- 53. Are you drunk? No, I am CybAR sick! – interacting with the ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1533236/full]
- 54. Virtual Reality in Pharmacy: Opportunities for Clinical, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6487969/]
- 55. Comparing Immersive and Non-Immersive VR: Effects ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384383/]
- 56. Comparative Efficacy of Various of Virtual Reality ... [https://www.sciencedirect.com/science/article/abs/pii/S152586102500458X]
- 57. Feasibility, Usability, and Effects of Leisure-Based Cognitive ... [https://games.jmir.org/2025/1/e66673]
- 58. Virtual Reality Uses by 2025: The Pervasive Future of ... [https://inairspace.com/blogs/learn-with-inair/virtual-reality-uses-by-2025-the-pervasive-future-of-digital-interaction?srsltid=AfmBOopQCIocMtthFMSgaRQm-7eDmoY5OvGuaaUIlOKvdw9GQRoKyxs2]
- 59. Virtual Reality Trends of 2025: Future of VR Technology [https://hqsoftwarelab.com/blog/virtual-reality-trends/]
- 60. Immersive Learning in 2025: AI & XR Trends - Edstutia LLC [https://edstutia.com/immersive-learning-2025/]
- 61. Virtual reality program reduces aggression and conduct ... [https://www.vcuhealth.org/news/virtual-reality-program-reduces-aggression-and-conduct-problems-in-youth-vcu-study-finds/]
- 62. Comparative Efficacy of Virtual Reality–Assisted Cognitive ... [https://www.researchprotocols.org/2025/1/e66112]
- 63. Assessing Inhibitory Control in the Real World Is Virtually ... [https://www.mdpi.com/2076-328X/12/11/444]
- 64. Barriers to adopting therapeutic virtual reality [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1549090/full]
- 65. Cost-Effectiveness of Virtual Reality Cognitive Behavioral ... [https://www.jmir.org/2020/5/e17098/]
- 66. Virtual reality for stroke rehabilitation - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178777/]
- 67. The Effects of Virtual Reality Training on Post-Stroke Upper ... [https://e-bnr.org/DOIx.php?id=10.12786/bn.2025.18.e2]
- 68. Effect of Virtual Reality–Based Therapies on Lower Limb ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12310189/]
- 69. A systematic review on the use of virtual reality in post- ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1653968/full]
- 70. Virtual reality as a potential therapy in a rehabilitation ... [https://www.frontiersin.org/journals/rehabilitation-sciences/articles/10.3389/fresc.2025.1539175/full]
- 71. How Biomedical Innovation is Transforming Stroke Recovery [https://medschool.duke.edu/stories/how-biomedical-innovation-transforming-stroke-recovery]
- 72. Neural anticipation of virtual infection triggers an immune ... [https://www.nature.com/articles/s41593-025-02008-y]
- 73. Pilot Studies: Common Uses and Misuses | NCCIH [https://www.nccih.nih.gov/grants/pilot-studies-common-uses-and-misuses]
- 74. What Is a Pilot Study - Benefits, Methods & Examples [https://casp-uk.net/news/what-is-a-pilot-study]
- 75. Guidelines for Designing and Evaluating Feasibility Pilot ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8849521/]
- 76. Guidance for conducting feasibility and pilot studies for ... [https://pilotfeasibilitystudies.biomedcentral.com/articles/10.1186/s40814-020-00634-w]
- 77. Applying mixed methods to pilot feasibility studies to inform ... [https://pilotfeasibilitystudies.biomedcentral.com/articles/10.1186/s40814-022-01178-x]
- 78. Protocol of a Pilot, Unblinded, Single-Arm Interventional Study ... [https://findanexpert.unimelb.edu.au/scholarlywork/1986645-integrating-virtual-reality--neurofeedback--and-cognitive-behavioral-therapy-for-auditory-verbal-hallucinations-(hybrid)--protocol-of-a-pilot--unblinded--single-arm-interventional-study]
- 79. Editorial: Virtual, mixed and augmented reality in cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11223571/]
- 80. Psychomotor skills assessment in medical training based ... [https://www.sciencedirect.com/science/article/abs/pii/S0950705114001841]
- 81. Quantitative metrics for evaluating surgical dexterity using ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0318660]
- 82. Objective psychomotor skills assessment of experienced ... [https://www.sciencedirect.com/science/article/abs/pii/S1091255X03001483]
- 83. Virtual reality-assisted learning: enhancing psychomotor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542202/]
- 84. a systematic review on spacing in VR simulator-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10009969/]
- 85. Virtual Reality in Cognitive and Affective Neuroscience [https://www.sciencedirect.com/science/article/abs/pii/S0166432825003961]
- 86. Virtual reality in cognitive and affective neuroscience [https://pubmed.ncbi.nlm.nih.gov/40939870/]
- 87. Effectiveness of virtual reality therapy in the treatment ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1553290/full]
- 88. Current State of Evidence for VRET in Psychotherapy [https://virtuallytheremedia.com/en/blog/literature-6/current-state-of-evidence-for-vret-in-psychotherapy-43]
- 89. Effectiveness of Virtual Reality interventions for aggression ... [https://www.sciencedirect.com/science/article/pii/S1359178925000035]
- 90. Evaluating virtual reality technology in psychotherapy [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2024.1480788/full]
- 91. The Effectiveness of Virtual Reality–Based Mindfulness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12260462/]
- 92. Impact of Visual Distractors in Virtual Reality Environments ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1705660/full]